- Open access
- Published: 04 July 2015

Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates
- Gilbert Abotisem Abiiro 1 , 2 &
- Manuela De Allegri 1
BMC International Health and Human Rights volume 15 , Article number: 17 ( 2015 ) Cite this article
21k Accesses
76 Citations
18 Altmetric
Metrics details
There is an emerging global consensus on the importance of universal health coverage (UHC), but no unanimity on the conceptual definition and scope of UHC, whether UHC is achievable or not, how to move towards it, common indicators for measuring its progress, and its long-term sustainability. This has resulted in various interpretations of the concept, emanating from different disciplinary perspectives. This paper discusses the various dimensions of UHC emerging from these interpretations and argues for the need to pay attention to the complex interactions across the various components of a health system in the pursuit of UHC as a legal human rights issue.
The literature presents UHC as a multi-dimensional concept, operationalized in terms of universal population coverage, universal financial protection, and universal access to quality health care, anchored on the basis of health care as an international legal obligation grounded in international human rights laws. As a legal concept, UHC implies the existence of a legal framework that mandates national governments to provide health care to all residents while compelling the international community to support poor nations in implementing this right. As a humanitarian social concept, UHC aims at achieving universal population coverage by enrolling all residents into health-related social security systems and securing equitable entitlements to the benefits from the health system for all. As a health economics concept, UHC guarantees financial protection by providing a shield against the catastrophic and impoverishing consequences of out-of-pocket expenditure, through the implementation of pooled prepaid financing systems. As a public health concept, UHC has attracted several controversies regarding which services should be covered: comprehensive services vs. minimum basic package, and priority disease-specific interventions vs. primary health care.
As a multi-dimensional concept, grounded in international human rights laws, the move towards UHC in LMICs requires all states to effectively recognize the right to health in their national constitutions. It also requires a human rights-focused integrated approach to health service delivery that recognizes the health system as a complex phenomenon with interlinked functional units whose effective interaction are essential to reach the equilibrium called UHC.
Peer Review reports
Universal health coverage (UHC) has been acknowledged as a priority goal of every health system [ 1 – 5 ]. The importance of this goal is reflected in the consistent calls by the World Health Organization (WHO) for its member states to implement pooled prepaid health care financing systems that promote access to quality health care and provide households with the needed protection from the catastrophic consequences of out-of-pocket (OOP) health-related payments [ 2 , 6 – 8 ]. This call has also been endorsed by the United Nations [ 5 ].
In the existing literature, different conceptual terminology, such as universal health care [ 9 ], universal health care coverage [ 10 , 11 ], universal health system, universal health coverage, or simply universal coverage, have been used to refer to basically the same concept [ 9 , 12 – 14 ]. Stuckler et al. [ 15 ] noted that “universal health care” is often used to describe health care reforms in high income countries while “universal health coverage” is associated with health system reforms within low- and middle-income countries (LMICs). Given that the poor, marginalized and most vulnerable populations mostly reside in LMICs, this paper places relatively high emphasis on such settings. Hence, we adopt the term universal health coverage (UHC) [ 2 ] throughout the paper.
It is argued that health system reforms aimed at UHC can be traced back to the emergence of organized health care in the 19th century, in response to labor agitations calling for the implementation of social security systems [ 16 – 18 ]. This phenomenon first started in Germany under the leadership of Otto von Bismarck, and later spread throughout other parts of Europe such as Britain, France and Sweden [ 16 – 18 ]. Later in 1948, the concept of UHC was implicitly enshrined in the WHO constitution which recognized that “the enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, and political belief, economic or social condition ” [ 19 ]. This fundamental human right was reaffirmed in the “ Health for all ” declaration of the Alma Ata conference on primary health care in 1978 [ 20 ].
In 2005, the concept of UHC was once again acknowledged and for the first time explicitly endorsed by the World Health Assembly (WHA) as the goal of sustainable health care financing [ 6 ]. The World Health Assembly resolution (WHA58.33) explicitly called for the implementation of health care financing systems centered on prepaid and pooling mechanisms aimed at achieving UHC [ 6 ]. Based on this Resolution, WHO defined UHC as “access to key promotive, preventive, curative and rehabilitative health interventions for all at an affordable cost, thereby achieving equity in access” [ 6 ] . The 2008 World Health Report re-emphasized prepayment and pooling systems as essential instruments for UHC by categorically stating that UHC entails “ pooling pre-paid contributions collected on the basis of ability to pay, and using these funds to ensure that services are available, accessible and produce quality care for those who need them, without exposing them to the risk of catastrophic expenditures” [ 7 ] . In 2010, the World Health Report, further stressed the role of health system financing for UHC by arguing that “ countries must raise sufficient funds, reduce the reliance on direct payments to finance services, and improve efficiency and equity” [ 2 ] . The concept of UHC as reflected in these WHO reports seems to be focused more on improving the health care financing function of a health system. The 2013 World Health Report built on prior work resulting in a call for research evidence to facilitate the transition of countries towards UHC [ 8 ]. The United Nations, the World Bank, the Gates Foundation, Oxfam, United States Agency for International Development (USAID), the International Labour Organization, United Nations Children’s Fund (UNICEF), Rockefeller Foundation, Results for Development Institute, the Joint Learning Network, among other international and regional development organizations have also in various ways recently endorsed and promoted the move towards UHC [ 5 , 21 – 25 ]. Considering the key role of the WHO and these other global actors in shaping the health policy debate at the global level, this recent history demonstrates a consistent and increasing international interest in the concept and debates surrounding UHC [ 2 , 26 ].
To date, the literature continues to present a clear consensus on the importance of UHC [ 23 , 27 – 29 ]. UHC was described by the Director General of WHO as “ the single most powerful concept that public health has to offer” [ 30 ]. Its potential to improve the health of the population, especially for the poor, has been demonstrated [ 31 , 32 ]. It is viewed as the phenomenon that will result in the third global transition and hence greatly influence the (re-) organization and financing of global health systems [ 29 ]. As an essential catalyst for poverty reduction and economic growth [ 14 , 33 , 34 ], UHC is regarded as a prerequisite for sustainable development [ 35 ]. It has therefore been advocated for as an important health goal in the post-2015 global development agenda [ 35 – 40 ]. The Lancet Commission on Investing in Health reports that this goal can be progressively attained by 2035 [ 34 ].
Despite the global consensus on its importance, consensus on the conceptual definition, meaning, and scope of UHC are still missing [ 12 , 26 , 41 ]. Likewise, no consensus exists on whether UHC is achievable or not; on how to move towards it [ 3 , 22 , 42 , 43 ]; on common indicators for measuring progress towards it [ 13 , 24 , 28 , 29 , 44 ]; and on its long-term sustainability [ 27 ]. The absence of a clear consensus on the conceptual definition of UHC has resulted in various interpretations of the concept, emanating from different disciplinary perspectives. These different interpretations reveal distinct, but interlinked dimensions of UHC [ 2 ]. This paper seeks to explore these various interpretations and representations of the concept of UHC from a multidimensional perspective and to discuss the various dimensions of UHC emerging from these interpretations. The arguments presented in this paper are based on a synthesis of the literature emerging from recent global debates on UHC. We adapted the WHO framework [ 2 ] to guide the presentation of our synthesis of the conceptual debates currently being advanced in the literature. Inspired by the WHO framework, our conceptual reasoning is that advancing UHC requires a healthy interaction across the three coverage dimensions: population coverage, financial protection and access to health services, held together by the view of health as a legal human right.
Discussions
Universal health coverage as a legal right to health.
A group of scholars, building their opinions from a legal and human rights perspective, enshrined in various international covenants and treaties [ 45 – 49 ], argue that the concept of UHC implies the existence of a legal framework to ensure that every resident gets access to affordable health care [ 15 , 50 , 51 ]. This portrays UHC as a reformulation of the “ health for all” goal of the Alma Ata Declaration [ 15 , 22 , 52 – 54 ]. The view of UHC as a legal obligation imposed on all states that ratified the convention on the right to health [ 45 ], implies that UHC calls for all States to create legal entitlements to health care for all their residents [ 50 , 55 , 56 ], thereby placing the responsibility for the delivery of UHC on national governments [ 5 , 17 , 57 ]. To guarantee a comprehensive right to health, the legal obligation of the state needs to reach beyond mere health service provision to include deliberate efforts to advance improvements in structures which are recognized to act as important social determinants of health such as, education, housing, sanitation and portable water as well as equitable gender and power relations [ 58 – 60 ]. The goal of UHC and the responsibility of moving towards it, therefore, need to be mandated by national laws [ 4 , 61 , 62 ]. Backman et al. [ 63 ] report that only 56 states have constitutional provisions that legally recognize the right to health and argue that even within these states, much work is still needed to ensure that this right is guaranteed in actual practice for all. Kingston et al. [ 55 ] also argue that even the state-centered view of the right to health is based on a false assumption that all people have legal nationalities. They insist that this false assumption is the cause for the medical exclusion of some migrants, especially illegal immigrants, from accessing institutionalized health care within their countries of residence. This situation is even more serious in LIMCs, where states find it difficult to raise sufficient revenues to finance health care for their legal citizenry. The vague definition of the right to health for non-nationals premised on the individual state’s economic ability and willingness to guarantee it [ 46 ], is therefore a potential recipe for social exclusion on the basis of nationality. Current debates on UHC therefore need to seriously reflect on ways by which the rights of stateless individuals to health care can also be guaranteed within the framework of UHC.
Acknowledging financial constraints to enforcing the right to health within poor-resource settings, some scholars explicitly call for international assistance for health as a way of strengthening the right to health component of UHC [ 62 , 64 ]. This, they argue, can be implemented through the establishment of a global fund to finance UHC [ 65 ] thereby presenting health as a global public good [ 66 ]. The notion of creating a common fund for UHC also recognizes the transnational nature of emerging global health problems and the inherent global interdependency needed to deal with such problems [ 67 ]. The possibility of funding global efforts towards UHC from this global fund is being explored. Initial results reveal conflicting expectations and interests between the potential donors/financiers and beneficiary countries [ 65 ]. The rights-based arguments for UHC therefore suggest a shift on the ethical spectrum of international assistance for health, from the concept of international health, where international assistance for health is viewed as a form of charity, towards that of global health [ 62 , 67 – 69 ] which is driven by the cosmopolitan ethical preposition that states should assist each other on the basis of humanitarian responsibility [ 68 , 69 ] and solidarity [ 67 ]. This cosmopolitan ethical view has the potential of facilitating efforts at raising more international assistance to facilitate UHC within its broader dimensions currently being advanced by WHO and other global experts.
Population coverage as a dimension of universal health coverage
Another group of scholars [ 22 , 61 ], also supportive of the rights-based perspective, argue that UHC implies “ equal or same entitlements” to the benefits of a health system. This reflects the notion of universal enrollment into health-related social security or risk protection systems [ 17 , 70 ] or population coverage under public health financing systems [ 2 ]. This notion therefore puts people (population) at the center of UHC [ 71 ]. Universal population coverage is to be understood in relation to the tenets of the right to health [ 45 ] as the absence of systemic exclusion of certain population groups (especially the poor and vulnerable) from the coverage of public prepaid funds and the ability of all residents to enjoy the same entitlements to the benefits of such public funding, irrespective of their nationality, race, sexual orientation, gender, political affiliations, socio-economic status or geographic locations [ 2 , 12 , 22 , 53 , 55 , 61 , 72 – 74 ].
To distinguish between aggregate and equity-based measures of population coverage, both WHO & the World Bank [ 24 ] have defined population coverage along two dimensions. Thus; achieving a 100 % coverage of the total population as an aggregate measure, or ensuring a relatively good proportion of coverage of the poorest 40 % compared to the rest of the population as an equity-based measure [ 24 ]. The overall notion of equity, defined as progressive income-rated contributions to health financing and need-based entitlements to health services, is embedded in almost all conceptual definitions of universal population coverage [ 2 , 4 , 75 – 77 ]. Implicit in the notion of equity is the concept of income and risk cross-subsidization [ 78 ], whereby the rich cross-subsidize the poor, whilst the healthy cross-subsidize the sick [ 61 ]. Notwithstanding this, other scholars have warned that universal population coverage, although desirable, must be carefully pursued to avoid creating a situation of which official entitlements will be offered to all people yet the existing health system may not have sufficient capacity to deliver quality health care for all the population [ 79 , 80 ]. This is referred to as adverse incorporation or inclusion [ 79 ].
Financial protection as a dimension of universal health coverage
From the perspective of health economics, UHC is viewed as a means of protection against the economic consequences of ill health [ 81 , 82 ]. A guaranteed financial protection requires the implementation of a health care financing mechanism that does not require direct (substantial) out-of-pocket (OOP) payments, official or informal, such as user fees, copayments and deductibles, for health care at the point of use [ 23 , 74 , 81 , 83 ]. This is the reason why the international community has endorsed financing health care from pooled prepaid mechanisms such as tax (general or dedicated) revenue, and contributions from social health insurance (usually for formal sector employees), private health insurance, and micro health insurance as essential pre-requisites for moving towards universal financial protection [ 6 ]. The existing literature does not reveal a consensus on the best prepayment mechanism or the right mix of prepayment systems that will guarantee adequate financial protection [ 22 , 84 ]. A report by Oxfam [ 22 ] suggests that within the context of LMICs, different development partners each promote their ideologically favored prepayment mechanisms as a strategy towards achieving UHC. Both the WHO and the academic community, however, recommend that such ideological prescriptions should be abandoned in favor of mixed pooling systems that can coordinate funds from different prepaid sources, in a manner that reflects context-specific UHC needs [ 2 , 28 ]. This recommendation is also rooted in the recognition that no country, not even high income ones, has achieved complete coverage, relying solely on one single financing strategy [ 4 ]. Within a mixed pooling system, there is the need to ensure proper monitory of both private and public inputs that go into the financing system.
The WHO recommends two measures for assessing progress towards financial protection: the incidence of catastrophic health care expenditure and the incidence of impoverishment resulting from OOP payments for health care [ 25 ]. The proportion of total health care expenditure incurred through OOP payments is normally used as an indicator of financial protection at the national level [ 2 ]. WHO recommends a maximum OOP expenditure threshold of 15–20 % of total health care expenditure as a requirement for financial protection [ 2 ]. At the household level, a quantitative measure of financial protection is the proportion of households incurring OOP healthcare expenditure exceeding 40 % of their household’s non-subsistence (i.e., non-food) expenditure [ 85 ] or 10 % of total household expenditure [ 86 ]. It must be noted that direct medical cost of seeking health care is not the only barrier to financial protection. A good estimate of catastrophic health care expenditure must therefore reflect all relevant costs including non-medical costs such as the cost of travelling to a health facility and loss of earnings while being treated among others. These quantitative measures, estimated on the basis of actual health care cost incurred, however, only reflect the true situation of financial risk protection if all those who need care can actually utilize health services [ 87 ]. It is argued that, such utilization-focused quantitative cost estimates are often not able to capture the quantum of needed healthcare that is forgone due to fear of impoverishment associated with utilization [ 87 ]. Effective universal financial protection can, therefore, be attained not only if the population does not incur (substantial) OOP payments and critical income losses due to payment for health care, but if there are no fears of and delays in seeking healthcare due to financial reasons, no borrowing and sale of valuable assets to pay for healthcare, and no detentions in hospitals for non-payment of bills [ 2 , 61 , 80 , 86 , 88 – 90 ].
Access to services as a dimension of universal health coverage
From the perspective of public health, it is argued that a UHC package should include a comprehensive spectrum of health services in line with the WHO’s conceptualization of UHC as “ access to key promotive, preventive, curative and rehabilitative health interventions … ” [ 2 , 6 ]. From a feasibility view point, other scholars, however, argue that the focus should be on the provision of a minimum basic package to cover priority health needs for which there are effective low-cost interventions [ 91 ] . Some of these scholars insist that this package should include priority services in line with the health-related Millennium Development Goals (MDGs) [ 14 , 24 ], thereby suggesting a continuous focus on vertical disease-specific interventions. While some of these scholars argue that the expansion and effective implementation of disease-specific interventions, especially those focused on prevention, can improve health and reduce health system costs, opponents insist that all disease-specific interventions create fragmentation and undermine broader efforts aimed at system-wide strengthening [ 92 , 93 ]. The opposing scholars call for a focus on primary health care [ 7 , 15 , 94 ], to the extent that Yates [ 74 ] calls for a clear timetable, proposing 2015 as deadline, for the achievement of universal access to primary health care.
A number of authors further distinguish between official health service coverage, defined in terms of entitlement to services, and actual effective coverage, defined in terms of real access and utilization of health services according to need [ 13 , 44 , 51 ]. It follows that attempts to measure UHC should focus on indicators that measure actual effective service coverage in relation to people’s ability to obtain real access to services, without facing barriers on both the demand and the supply side [ 13 , 51 , 70 ]. Real access, is further defined as access in relation to the availability of health services, personnel and facilities; geographical accessibility of health services; acceptability defined in relation to appropriate client-provider interactions, timeliness, appropriateness and quality of services; and affordability in terms of medical and transport costs of services relative to clients’ ability-to-pay [ 73 , 80 , 95 – 106 ]. A guaranteed sufficient capacity of the local health system, in terms of adequate health infrastructure, qualified human resources, equipment and tools, to deliver quality health care is therefore an essential component of the access dimension of UHC [ 2 , 11 , 107 ]. It is interesting to note that “ Availability, Acceptability, Affordability and Quality (AAAQ)” of health services as essential sub-components of real access are directly rooted in the human rights conceptual framework and captured in broader discussions on the right to health [ 45 , 63 ].
Considering its interactive facets, it can be concluded that UHC emerges from the literature as a multi-dimensional concept, operationalized in terms of population coverage of health-related social security systems, financial protection, and access to quality health care according to need [ 17 ], and pursued within the framework of health care as an international legal obligation grounded in international human rights laws [ 45 , 46 , 48 , 49 ]. As an essential pre-condition for moving towards UHC in LMICs, there is therefore the need for all states to abide by the international human rights obligation imposed on them and thereby legally recognize the right to health in their national constitutions. It is only on this basis that the needed national and political commitment can be enhanced for a successful move towards universal population coverage of health-related social security systems, financial protection and access to services, which are essential components of a guaranteed comprehensive right to health and hence UHC. UHC can thus be understood as a broad legal, rights-based, social humanitarian, health economics and public health concept [ 15 , 17 , 27 , 42 ]. As such, it transcends a mere legal extension of the coverage of prepaid financing systems such as health insurance or tax-based systems to all residents, to ensuring that other financial and health system bottlenecks are removed to enhance effective financial protection and equitable access to services for all. As an overall health system strengthening tool, UHC can only be achieved through a human rights-focused integrated approach that recognizes the health system as a complex phenomenon with interlinked functional units whose effective interaractions are essential to reach the equilibrium called UHC. It follows that in LMICs, interventions aimed at strengthening health systems need to attract as much attention and funding as currently being deployed towards disease-specific interventions within the framework of the MDGs. Such an action has the capability of improving local service delivery capacity and hence of building resilient and responsive health systems to facilitate the move towards UHC. The move towards UHC should therefore be conceptualized as a continuous process of identifying gaps in the various interactive UHC dimensions, and designing context-specific strategies to address these gaps in accordance with the international legal obligations imposed on states by international agreements on the right to health. As a global issue, international assistance based on the principle of global solidarity is indispensable in the move towards UHC in LMICs.
Abbreviations
Availability, Acceptability, Affordability, Quality
Low - and Middle-Income Countries
Millennium Development Goals
Out-of-pocket
Universal Health coverage
United Nations Children’s Fund
United States Agency for International Development
World Health Assembly
World Health Organization
Garrett L, Chowdhury AMR, Pablos-Méndez A. All for universal health coverage. Lancet. 2009;374:1294–9.
Article PubMed Google Scholar
WHO. The World Health Report 2010 - Health Systems Financing: the path to universal coverage. Geneva: World Health Organization; 2010.
Google Scholar
Mills A, Ally M, Goudge J, Gyapong J, Mtei G. Progress towards universal coverage: the health systems of Ghana, South Africa and Tanzania. Health Policy Plan. 2012;27 suppl 1:i4–12.
Kutzin J. Health financing for universal coverage and health system performance: concepts and implications for policy. Bull World Health Organ. 2013;91:602–11.
Article PubMed PubMed Central Google Scholar
United Nations’ General Assembly. Global Health and Foreign policy. Agenda item 123. The Sixty-seventh session (A/67/L.36). New York: United Nations; 2012.
World Health Organization. Sustainable health financing, universal coverage and social health insurance. Geneva: World Health Organization; 2005.
WHO. World Health Report 2008 - primary health care - now more than ever. Geneva: World Health Organization; 2008.
WHO. WHO | World Health Report 2013: research for universal health coverage. Genena: World Health Organization; 2013.
Reddy KS, Patel V, Jha P, Paul VK, Kumar AKS, Dandona L. Towards achievement of universal health care in India by 2020. A call to action. Lancet. 2011;377:760–8.
Gorin S. Universal health care coverage in the United States: Barriers, prospects, and implications. Health Soc Work. 1997;22:223–30.
Article CAS PubMed Google Scholar
Collet T-H, Salamin S, Zimmerli L, Kerr EA, Clair C, Picard-Kossovsky M, et al. The quality of primary care in a country with universal health care coverage. J Gen Intern Med. 2011;26:724–30.
O’Connell T, Rasanathan K, Chopra M. What does universal health coverage mean? Lancet. 2013;6736:13–5.
de Noronha JC. Universal health coverage: how to mix concepts, confuse objectives, and abandon principles. Cad Saúde Pública. 2013;29:847–9.
Kieny M-P, Evans DB. Universal health coverage. East Mediterr Health J. 2013;19:305-6.
Stuckler D, Feigl AB, Basu S, McKee M. The political economy of universal health coverage. In: Background paper for the global symposium on health systems research. Geneva: World Health Organization; 2010.
Bärnighausen T, Sauerborn R. One hundred and eighteen years of the German health insurance system. Are there any lessons for middle-and low-income countries. Soc Sci Med. 2002;54:1559–87.
Savedoff W, de Ferranti D, Smith A, Fan V. Political and economic aspects of the transition to universal health coverage. Lancet. 2012;380:924–32.
McKee M, Balabanova D, Basu S, Ricciardi W, Stuckler D. Universal health coverage: a quest for all countries but under threat in some. Value Health. 2013;16(1, Supplement):S39–45.
WHO. Constitution of the World Health Organization. Geneva: World Health Organisation; 1948.
Declaration of Alma-Ata. International Conference on Primary Health Care, Al ma-Ata, USSR, 6–12 September 1978. http://www.euro.who.int/__data/assets/pdf_file/0009/113877/E93944.pdf . Accessed 4 May, 2015.
Bristol N. Global action towards Universal health coverage: a report for the CSIS Global Health Policy Center. Washington DC: Centre for strategic and International Studies; 2014.
Oxfam. Universal Health Coverage : Why health insurance schemes are leaving the poor behind. Oxford: Oxfam International; 2013.
World Bank WHO. WHO/World Bank Ministerial-level Meeting on Universal Health Coverage 18–19 February 2013. Geneva: World Health Organization’s headquarters; 2013.
WHO, World Bank. Monitoring Progress towards Universal Health Coverage at Country and Global Levels: A Framework. Joint WHO/World Bank Group Discussion Paper. Geneva: World Health Organization; 2013.
World Bank, WHO. Towards Universal Health Coverage by 2030. Washington DC: World Bank Group; 2014.
Latko B, Temporão JG, Frenk J, Evans TG, Chen LC, Pablos-Mendez A, et al. The growing movement for universal health coverage. Lancet. 2011;377:2161–3.
Borgonovi E, Compagni A. Sustaining universal health coverage: the interaction of social, political, and economic sustainability. Value Health. 2013;16(1, Supplement):S34–8.
Kutzin J. Anything goes on the path to universal health coverage? No. Bull World Health Organ. 2012;90:867–8.
Rodin J, de Ferranti D. Universal health coverage. The third global health transition? Lancet. 2012;380:861–2.
Chan M. Best days for public health are ahead of us, says WHO Director-General. Geneva, Switzerland: Address to the 65th World Health Assembly; 2012.
Lee Y-C, Huang Y-T, Tsai Y-W, Huang S-M, Kuo KN, McKee M, et al. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res. 2010;10:225.
Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health? Lancet. 2012;380:917–23.
The World Bank. World Development Report 1993. Investing in Health. New York: Oxford University Press; 1993.
Book Google Scholar
Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, et al. Global health 2035: a world converging within a generation. Lancet. 2013;382:1898–955.
Evans DB, Marten R, Etienne C. Universal health coverage is a development issue. Lancet. 2012;380:864–5.
D’Ambruoso L. Global health post-2015: the case for universal health equity. Global Health Action. 2013;6:19661.
Sheikh M, Cometto G, Duvivier R. Universal health coverage and the post 2015 agenda. Lancet. 2013;381:725–6.
United Nations. Adopting consensus text, General Assembly encourages member states to plan, pursue transition of National Health Care Systems towards Universal Coverage. In: Sixty-seventh General Assembly Plenary 53rd Meeting (AM). New York: Department of Public Information • News and Media Division; 2012.
Vega J. Universal health coverage. The post-2015 development agenda. Lancet. 2013;381:179–80.
Victora C, Saracci R, Olsen J. Universal health coverage and the post-2015 agenda. Lancet. 2013;381:726.
Sengupta M. Universal Health Coverage: Beyond rhetoric. In: McDonald DA, Ruiters G, editors. Municipal Services Project, Occasional Paper No 20 - November 2013. http://www.alames.org/documentos/uhcamit.pdf . Accessed 14 May, 2015.
Holmes D. Margaret Chan: committed to universal health coverage. Lancet. 2012;380:879.
Horton R, Das P. Universal health coverage: not why, what, or when—but how? Lancet. 2014;384:2101.
Article Google Scholar
Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012;380:933–43.
Office of the United Nations High Commissioner for Human Rights, WHO. The Right to Health: Joint Fact Sheet WHO/OHCHR/323. Geneva: World Health Organization; 2007.
United Nations’ General Assemby. International Covenant on Economic, Social and Cultural Rights: Adopted and opened for signature, ratification and accession by General Assembly resolution 2200A (XXI) of 16 December 1966 entry into force 3 January 1976, in accordance with article 27. New York: United Nations; 1966.
Young S, The U.S. Fund for UNICEF Education Department. The United Nations Convention on the Rights of the Child: An Introduction -A Middle School Unit (Grades 6–8). U.S. Malawi: Fund for UNICEF/Mia Brandt; 2006.
United Nations. Convention on the Rights of Persons with Disabilities. New York: United Nations; 2006.
United Nations General Assemby. Convention on the Elimination of All Forms of Discrimination against Women. New York: United Nations; 1979.
Bárcena A. Health protection as a citizen’s right. Lancet. 2014;6736:61771–2.
Scheil-Adlung X, Bonnet F. Beyond legal coverage: assessing the performance of social health protection. Int Soc Secur Rev. 2011;64:21–38.
Forman L, Ooms G, Chapman A, Friedman E, Waris A, Lamprea E, et al. What could a strengthened right to health bring to the post-2015 health development agenda?: interrogating the role of the minimum core concept in advancing essential global health needs. BMC Int Health Hum Rights. 2013;13:48.
Fried ST, Khurshid A, Tarlton D, Webb D, Gloss S, Paz C, et al. Universal health coverage: necessary but not sufficient. Reprod Health Matters. 2013;21:50–60.
Hammonds R, Ooms G. The emergence of a global right to health norm - the unresolved case of universal access to quality emergency obstetric care. BMC Int Health Hum Rights. 2014;14:4.
Kingston LN, Cohen EF, Morley CP. Debate: limitations on universality: the “right to health” and the necessity of legal nationality. BMC Int Health Hum Rights. 2010;10:11.
Yamin AE, Frisancho A. Human-rights-based approaches to health in Latin America. Lancet. 2014;6736(14):61280.
Rosen G. A History of Public Health. Maryland: John Hopkins University Press; 1993.
Wilkinson R, Marmot M. Social determinants of health. The solid facts. Copenhagen: World Health Organization; 1998.
Marmot M, Wilkinson R. Social determinants of health. New York: Oxford University Press; 2005.
WHO. Social determinants of health: report by the Secretariat EB132/14. Geneva: World Health Organization; 2012.
McIntyre D. Health service financing for universal coverage in east and southern Africa, EQUINET Discussion Paper 95. Harare: Regional Network for Equity in Health in East and Southern Africa (EQUINET); 2012.
Ooms G. From international health to global health: how to foster a better dialogue between empirical and normative disciplines. BMC Int Health Hum Rights. 2014; 14:36.
Backman G, Hunt P, Khosla R, Jaramillo-Strouss C, Fikre BM, Rumble C, et al. Health systems and the right to health: an assessment of 194 countries. Lancet. 2008;372:2047–85.
Ooms G, Latif LA, Waris A, Brolan CE, Hammonds R, Friedman EA, et al. Is universal health coverage the practical expression of the right to health care? BMC Int Health Hum Rights. 2014; 14:3.
Ooms G, Hammonds R. Financing Global Health Through a Global Fund for Health? Working Group on Financing | PAPER 4. London: CHATHAM HOUSE (The Royal Institute of International Affairs); 2014.
Chen LC, Evans T, Cash R. Health as a global public good. In: Kaul I, Stern M, Grunberg I, editors. Global public goods: international cooperation in the 21st century. New York: Oxford University Press; 1999. p. 284–304.
Chapter Google Scholar
Frenk J, Gómez-Dantés O, Moon S. From sovereignty to solidarity: a renewed concept of global health for an era of complex interdependence. Lancet. 2014;383:94–7.
Stuckler D, McKee M. Five metaphors about global-health policy. Lancet. 2008;372:95–7.
Lencucha R. Cosmopolitanism and foreign policy for health: ethics for and beyond the state. BMC Int Health Hum Rights. 2013;13:29.
Knaul FM, González-Pier E, Gómez-Dantés O, García-Junco D, Arreola-Ornelas H, Barraza-Lloréns M, et al. The quest for universal health coverage: achieving social protection for all in Mexico. Lancet. 2012;380:1259–79.
The Lancet. Universal health coverage post-2015: putting people first. Lancet. 2014;384:2083.
Allotey P, Verghis S, Alvarez-Castillo F, Reidpath DD. Vulnerability, equity and universal coverage – a concept note. BMC Public Health. 2012;12 Suppl 1:S2.
Ravindran TS. Universal access: making health systems work for women. BMC Public Health. 2012;12 Suppl 1:S4.
Yates R. Universal health care and the removal of user fees. Lancet. 2009;373:2078–81.
McIntyre D. What healthcare financing changes are needed to reach universal coverage in South Africa? SAMJ: S Afr Med J. 2012;102:489–90.
Mills A, Ataguba JE, Akazili J, Borghi J, Garshong B, Makawia S, et al. Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet. 2012;380:126–33.
Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health. 2014;13:1–72.
Goudge J, Akazili J, Ataguba J, Kuwawenaruwa A, Borghi J, Harris B, et al. Social solidarity and willingness to tolerate risk- and income-related cross-subsidies within health insurance: experiences from Ghana, Tanzania and South Africa. Health Policy Plan. 2012;27 suppl 1:i55–63.
Hickey S, Du Toit A. Adverse incorporation, social exclusion and chronic poverty, CPRC Working Paper 81. Chronic Poverty Research Centre: Manchester, UK; 2007.
Abiiro GA, Mbera GB, De Allegri M. Gaps in universal health coverage in Malawi: a qualitative study in rural communities. BMC Health Serv Res. 2014;14:234.
Palmer N, Mueller DH, Gilson L, Mills A, Haines A. Health financing to promote access in low income settings—how much do we know? Lancet. 2004;364:1365–70.
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure. A multicountry analysis. Lancet. 2003;362:111–7.
McIntyre D, Ranson MK, Aulakh BK, Honda A. Promoting universal financial protection: evidence from seven low-and middle-income countries on factors facilitating or hindering progress. Health Res Policy Syst. 2013;11:36.
Kutzin J, Ibraimova A, Jakab M, O’Dougherty S. Bismarck meets Beveridge on the Silk Road: coordinating funding sources to create a universal health financing system in Kyrgyzstan. Bull World Health Organ. 2009;87:549–54.
Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Affair. 2007;26:972–83.
Cleary S, Birch S, Chimbindi N, Silal S, McIntyre D. Investigating the affordability of key health services in South Africa. Soc Sci Med. 2013;80:37–46.
Moreno-Serra R, Millett C, Smith PC. Towards improved measurement of financial protection in health. PLoS Med. 2011;8, e1001087.
Dekker M, Wilms A. Health insurance and other risk-coping strategies in Uganda. The case of Microcare Insurance Ltd. World Dev. 2009;38:369–78.
Kruk ME, Goldmann E, Galea S. Borrowing and selling to pay for health care in low- and middle-income countries. Health Aff. 2009;28:1056–66.
Leive A, Xu K. Coping with out-of-pocket health payments: empirical evidence from 15 African countries. Bull World Health Organ. 2008;86:849–56.
Sachs JD. Achieving universal health coverage in low-income settings. Lancet. 2012;380:944–7.
Adam T, Hsu J, de Savigny D, Lavis JN, Røttingen J-A, Bennett S. Evaluating health systems strengthening interventions in low-income and middle-income countries: are we asking the right questions? Health Policy Plan. 2012;27 suppl 4:iv9–19.
PubMed Google Scholar
Rao KD, Ramani S, Hazarika I, George S. When do vertical programmes strengthen health systems? A comparative assessment of disease-specific interventions in India. Health Policy Plan. 2014;29:495–505.
Sustainable Development Solutions Network. Health in the framework of development: Technical Report for the Post-2015 Development Agenda. New York: Sustainable Development Solutions Network: Global Inititative for the United Nation; 2014.
Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–20.
CAS PubMed PubMed Central Google Scholar
Arnold C, Theede J, Gagnon A. A qualitative exploration of access to urban migrant healthcare in Nairobi, Kenya. Soc Sci Med. 2014;110:1–9.
Dillip A, Alba S, Mshana C, Hetzel MW, Lengeler C, Mayumana I, et al. Acceptability – a neglected dimension of access to health care: findings from a study on childhood convulsions in rural Tanzania. BMC Health Serv Res. 2012;12:113.
Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19:69–79.
Evans DB, Hsu J, Boerma T. Universal health coverage and universal access. Bull World Health Organ. 2013;91:546–546A.
Goudge J, Gilson L, Russell S, Gumede T, Mills A. Affordability, availability and acceptability barriers to health care for the chronically ill: longitudinal case studies from South Africa. BMC Health Serv Res. 2009;9:75.
Jacobs B, Ir P, Bigdeli M, Annear PL, Damme WV. Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012;27:288–300.
Macha J, Harris B, Garshong B, Ataguba JE, Akazili J, Kuwawenaruwa A, et al. Factors influencing the burden of health care financing and the distribution of health care benefits in Ghana, Tanzania and South Africa. Health Policy Plan. 2012;27 suppl 1:i46–54.
McIntyre D, Thiede M, Birch S. Access as a policy-relevant concept in low- and middle-income countries. Health Econ Policy Law. 2009;4(Pt 2):179–93.
O’Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cad Saúde Pública. 2007;23:2820–34.
Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–40.
Silal SP, Penn-Kekana L, Harris B, Birch S, McIntyre D. Exploring inequalities in access to and use of maternal health services in South Africa. BMC Health Serv Res. 2012;12:120.
Meessen B, Malanda B. No universal health coverage without strong local health systems. Bull World Health Organ. 2014;92:78–78A.
Download references
Acknowledgement
GAA was funded by a scientific contract from the Institute of Public Health, University of Heidelberg, Germany, and a senior research assistant contract from the University for Development Studies, Ghana. MDA is fully funded by a core position in the Medical Faculty of the University of Heidelberg, Germany.
Author information
Authors and affiliations.
Institute of Public Health, Medical Faculty, University of Heidelberg, Heidelberg, Germany
Gilbert Abotisem Abiiro & Manuela De Allegri
Department of Planning and Management, Faculty of Planning and Land Management, University for Development Studies, University Post Box 3, Wa, Upper West Region, Ghana
Gilbert Abotisem Abiiro
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Gilbert Abotisem Abiiro .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
GAA conceptualized and designed the study, undertook the literature search, data extraction and analysis, and drafted the paper. MDA supported the conceptualization and design of the study and paper drafting, and critically reviewed the drafts and contributed to its finalization. Both authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/4.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Abiiro, G.A., De Allegri, M. Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates. BMC Int Health Hum Rights 15 , 17 (2015). https://doi.org/10.1186/s12914-015-0056-9
Download citation
Received : 15 January 2015
Accepted : 29 June 2015
Published : 04 July 2015
DOI : https://doi.org/10.1186/s12914-015-0056-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Universal health coverage
- Multi-dimensional concept
- Rights-based
- Population coverage
- Financial protection
- Access to health services
- Health system
- Conceptual literature
- Global debates
BMC International Health and Human Rights
ISSN: 1472-698X
- General enquiries: [email protected]
Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates
Affiliations.
- 1 Institute of Public Health, Medical Faculty, University of Heidelberg, Heidelberg, Germany. [email protected].
- 2 Department of Planning and Management, Faculty of Planning and Land Management, University for Development Studies, University Post Box 3, Wa, Upper West Region, Ghana. [email protected].
- 3 Institute of Public Health, Medical Faculty, University of Heidelberg, Heidelberg, Germany. [email protected].
- PMID: 26141806
- PMCID: PMC4491257
- DOI: 10.1186/s12914-015-0056-9
Background: There is an emerging global consensus on the importance of universal health coverage (UHC), but no unanimity on the conceptual definition and scope of UHC, whether UHC is achievable or not, how to move towards it, common indicators for measuring its progress, and its long-term sustainability. This has resulted in various interpretations of the concept, emanating from different disciplinary perspectives. This paper discusses the various dimensions of UHC emerging from these interpretations and argues for the need to pay attention to the complex interactions across the various components of a health system in the pursuit of UHC as a legal human rights issue.
Discussion: The literature presents UHC as a multi-dimensional concept, operationalized in terms of universal population coverage, universal financial protection, and universal access to quality health care, anchored on the basis of health care as an international legal obligation grounded in international human rights laws. As a legal concept, UHC implies the existence of a legal framework that mandates national governments to provide health care to all residents while compelling the international community to support poor nations in implementing this right. As a humanitarian social concept, UHC aims at achieving universal population coverage by enrolling all residents into health-related social security systems and securing equitable entitlements to the benefits from the health system for all. As a health economics concept, UHC guarantees financial protection by providing a shield against the catastrophic and impoverishing consequences of out-of-pocket expenditure, through the implementation of pooled prepaid financing systems. As a public health concept, UHC has attracted several controversies regarding which services should be covered: comprehensive services vs. minimum basic package, and priority disease-specific interventions vs. primary health care. As a multi-dimensional concept, grounded in international human rights laws, the move towards UHC in LMICs requires all states to effectively recognize the right to health in their national constitutions. It also requires a human rights-focused integrated approach to health service delivery that recognizes the health system as a complex phenomenon with interlinked functional units whose effective interaction are essential to reach the equilibrium called UHC.
Publication types
- Research Support, Non-U.S. Gov't
- Health Services Accessibility
- Internationality
- Universal Health Insurance*
- Open access
- Published: 04 January 2024
Building a resilient health system for universal health coverage and health security: a systematic review
- Ayal Debie ORCID: orcid.org/0000-0002-5596-8401 1 , 4 ,
- Adane Nigusie 2 ,
- Dereje Gedle 3 ,
- Resham B. Khatri 3 &
- Yibeltal Assefa 3
Global Health Research and Policy volume 9 , Article number: 2 ( 2024 ) Cite this article
1823 Accesses
5 Altmetric
Metrics details
Resilient health system (RHS) is crucial to achieving universal health coverage (UHC) and health security. However, little is known about strategies towards RHS to improve UHC and health security. This systematic review aims to synthesise the literature to understand approaches to build RHS toward UHC and health security.
A systematic search was conducted including studies published from 01 January 2000 to 31 December 2021. Studies were searched in three databases (PubMed, Embase, and Scopus) using search terms under four domains: resilience, health system, universal health coverage, and health security. We critically appraised articles using Rees and colleagues’ quality appraisal checklist to assess the quality of papers. A systematic narrative synthesis was conducted to analyse and synthesise the data using the World Health Organization’s health systems building block framework.
A total of 57 articles were included in the final review. Context-based redistribution of health workers, task-shifting policy, and results-based health financing policy helped to build RHS. High political commitment, community-based response planning, and multi-sectorial collaboration were critical to realising UHC and health security. On the contrary, lack of access, non-responsive, inequitable healthcare services, poor surveillance, weak leadership, and income inequalities were the constraints to achieving UHC and health security. In addition, the lack of basic healthcare infrastructures, inadequately skilled health workforces, absence of clear government policy, lack of clarity of stakeholder roles, and uneven distribution of health facilities and health workers were the challenges to achieving UHC and health security.
Conclusions
Advanced healthcare infrastructures and adequate number of healthcare workers are essential to achieving UHC and health security. However, they are not alone adequate to protect the health system from potential failure. Context-specific redistribution of health workers, task-shifting, result-based health financing policies, and integrated and multi-sectoral approaches, based on the principles of primary health care, are necessary for building RHS toward UHC and health security.
Resilient health system (RHS) is essential to ensure universal health coverage (UHC) and health security. It is about the health system’s preparedness and response to severe and acute shocks, and how the system can absorb, adapt and transform to cope with such changes [ 1 , 2 ]. Resilient health system reflects the ability to continue service delivery despite extraordinary shocks to achieving UHC [ 3 ]. A study in Nepal showed that adoption of coexistence strategy on the continuation of the international community on strengthening the health sector with the principle of “do-no-harm” and impartiality at the time of conflicts improve the health outcomes [ 4 ].
In 2015, the United Nations (UN) General Assembly adopted a new development agenda aiming to transform the world by achieving the Sustainable Development Goals (SDGs) by 2030 [ 5 ], based on the lessons from the Millennium Development Goals (MDGs) [ 6 ]. The SDGs seek to tackle the “unfinished business” of the MDGs era and recognise that health is a major contributor and beneficiary of sustainable development policies [ 7 ]. One of the 17 goals has been devoted specifically to health: “ensure healthy lives and promote well-being for all ages” [ 6 ]. All UN Member States have agreed to achieve UHC (target 3.8) by 2030, as part of the SDGs [ 8 ]. The 2030 UHC target was intended to reach at least 80% for the UHC service coverage index and 100% for financial protection [ 9 ]. Universal health coverage is achieved when everyone has access to essential healthcare services without financial hardship associated with paying for care [ 10 ].
Universal health coverage and health security are two sides of the same coin. They are interconnected and complementary goals that require strong health systems and public health infrastructure to ensure that everyone has access to essential health services [ 11 ]. Universal health coverage and health security require an integrated and multi-sectorial system strengthening to provide quality and equitable healthcare services across populations [ 12 ].
A resilient health system provides the foundation for both [ 11 ]. Strengthening the World Health Organisation’s (WHO’s) six health system building blocks, including service delivery, health workforce, health information systems, health financing, leadership and governance, and access to essential medicines and infrastructures are essential to achieve UHC and health security [ 13 ]. The 13th WHO programme is structured in three interconnected strategic priorities to ensure SDG-3 including: achieving UHC, addressing health emergencies, and promoting healthier populations [ 14 ].
In the World Health Organisation (WHO) European Region, health security emphasises on the analysis of infectious diseases, natural and human-made disasters, conflicts and complex emergencies, and potential future challenges from global changes, particularly climate change [ 15 ]. Health security is also considered as the activities required, both proactive and reactive, to minimise the danger and impact of acute public health events that endanger people’s health across geographical regions and international boundaries [ 16 ]. The links between health system and health security have started to emerge in several national strategic plans and global initiatives, such as the Global Health Security Agenda (GHSA) and One Health, which aim to better facilitate the implementation of the International Health Regulations (IHR) [ 17 ]. The aim of IHR is to prevent, detect, and respond to the international spread of disease in effective and efficient manner [ 18 ]. The GHSA also help countries to build their capacity to prevent, detect, and respond to infectious disease threats [ 19 ].
Although almost all nations are progressing towards UHC, the advancement in low and low-middle income countries (LLMICs) is slow [ 20 ]. This is because the ethos and organisations of many health systems are more suitable for yesterday’s disease burden than tomorrow [ 21 , 22 ]. Health systems of various nations faced numerous shocks, including public health, social, economic and political crises associated with COVID-19 [ 23 ]. The COVID -19 pandemic has made an unprecedented impact on the international community and exposed the vulnerabilities of the present global health architecture [ 24 ]. The COVID-19 pandemic is a perfect reminder that countries, individually and collectively, require a strong RHS now more than ever; however, there was no adequate evidence on the strategies toward RHS to improving UHC and health security. Thus, this study can inform the global health community on the lessons of RHS and its applications to UHC in pandemic and beyond. This review generally aimed to address the following research questions: 1) What are the existing evidence on the impact of RHS for UHC and health security? 2) What are the essential elements and characteristics of RHS for UHC and health security as per the WHO building blocks? and 3) What examples exist to demonstrate on how to build RHS core components for UHC and health security?
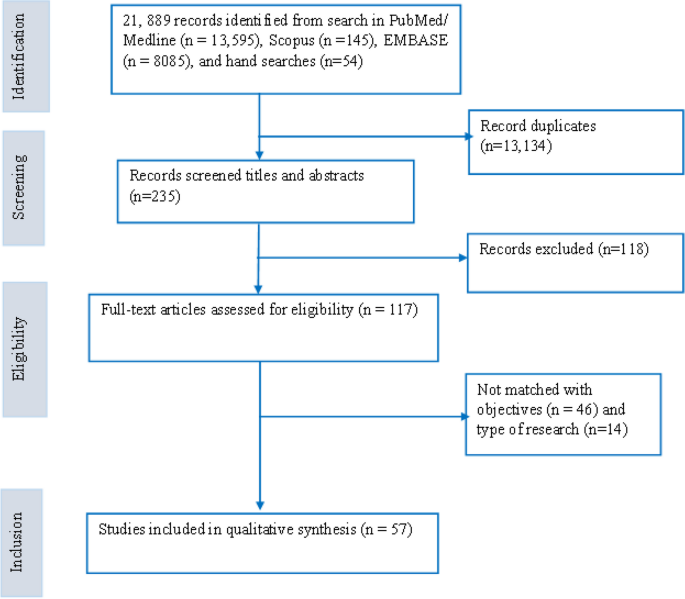
Registration and search strategy
This review was conducted and reported following enhancing transparency in reporting the synthesis of qualitative research (ENTERQ). Following ENTERQ guidelines, the systematic review was registered with the international prospective register of systematic reviews (PROSPERO) on 02 January 2022 with registration: CRD42020210471. Studies were searched in three databases (PubMed, Embase and Scopus) using search terms of under four broader domains, including resilience, health system, universal health coverage, and health security. Additional literatures were identified by searching in Google and Google Scholar. The search strategies were built using the four domains of search terms, and “Title/Abstract” by linking “AND” and “OR” Boolean operator terms as appropriate (Additional file 1 ). We also used the ENTERQ checklist for reporting the articles (Additional file 2 ).
Inclusion and exclusion criteria
All articles in relation to RHS towards UHC and health security were included in the review. Inclusion criteria were articles written in the English language published from 01 January 2000 to 31 December 2021. Qualitative, quantitative, and mixed methods studies were eligible for inclusion. Exclusion criteria were perspectives, commentary, expert’s opinion, conference papers, debates, conference reports, letters to the editor, and editorials. We presented this paper as a narrative review, following some components of the preferred reporting of systematic review and meta-analysis (PRISMA) guideline for scoping review (Additional file 3 ).
Selection process
The primary author (AD) imported all retrieved articles into the Endnote library to remove duplicates. After removing the duplicates, three authors (AD, AN and DG) independently screened the articles by title and abstract based on inclusion criteria. The senior authors (RBK and YA) mediated the discrepancies between the three reviewers through discussion. Finally, we retained and reviewed the full texts of all relevant studies for final data synthesis.
Data extraction and framework for synthesis
We used the Rees and colleagues’ appraisal instrument as a guiding tool to appraise the quality of included articles in the review [ 25 ]. The quality appraisal instrument is a comprehensive tool designed to assess the quality, rigor of research studies, covers key aspects of research design, data collection, analysis, and reporting. This includes rigour in sampling, rigour in data collection, rigour in data analysis, findings supported by the data, breadth and depth of findings, extent of the study privilege perspectives, reliability or trustworthiness, and usefulness[ 25 ]. A template was developed to extract relevant data from each eligible study. After reading the selected studies, key findings were extracted into the template, including information about the first author, year of publication, type of article, study design, and key summary findings. Three independent reviewers (AD, AN and DG) extracted the data. The senior authors (RBK and YA) verified the extracted information. The successes and challenges of RHS for UHC and health security were extracted using health system building blocks.
We analysed the findings using the WHO health system building blocks, including service delivery, health workforce, health information systems, medicines and infrastructures, healthcare financing, and leadership and governance [ 13 ]. We analysed the key challenges and successes of RHS for UHC and health security using the WHO health system frameworks. Framework analysis provides a systematic approach to analysing large amounts of textual data using pre-determined framework components. This allows the analyst and those commissioning the research to move between multiple layers of abstraction without losing sight of raw data [ 26 ].
Search results
A total of 21,889 records were identified in the initial literature search. After removing 13,134 duplicates, 235 articles were screened by titles and abstracts, and 118 were excluded. Next, 117 studies were reviewed using the full texts, and finally, 57 articles met the inclusion criteria and were analyzed in the systematic review (Fig. 1 ). Of these, 32 articles were primary studies, and 25 articles investigated the application of RHS on UHC. In addition, nine articles explained RHS's implications on UHC and health security. Of these, approximately one-third (19 articles) were conducted in various African nations, while 19 articles were from Asian countries. The remaining articles were from other parts of the world. The study also reviewed articles on various aspects of health system building blocks, including health service delivery, health workforce, health information systems, health financing, leadership/governance, and medicines and infrastructure. The number of articles reviewed for each aspect were 17, 9, 10, 13, 22, and 10, respectively.
ENTREQ flow diagram for the articles included in the review
Successes and challenges of RHS
This review used the six-health system building blocks to achieve UHC and health security. These include service delivery, health workforce, health information system, health financing, medicines, diagnostics and infrastructures, and leadership and governance (Table 1 ).
Service delivery
Of the total reviewed articles, 17 described their healthcare service delivery findings. Good service delivery provides comprehensive and person-centered healthcare services with full accountability [ 27 ]. Continuation of healthcare service delivery in the face of extraordinary shocks facilitated UHC progress [ 3 ]. Studies reported that health service inputs, access to transportation, communication infrastructures, capacity building, referral systems, intersectoral actions, and electronic healthcare platforms could facilitate service delivery and improve access to health services [ 13 , 28 ]. Operational integration between health service continuity and emergency response through proactive planning across all income nations reduced health services disruptions during emergencies [ 29 ]. Community resources, cohesion, and physical accesses were significant assets to improve service utilisation and quality [ 30 ].
An inward migration or mass casualty incidents compromised the quality of services and increased deaths attributed to delays in treatment [ 30 ]. In the Ebola crisis, the long-standing lack of access to basic primary health care to isolate and treat infected people fueled the epidemic’s spread resulting in a death toll [ 31 ]. Uneven health facilities distribution and lack of well-trained personnel and supplies led to geographical inequities and poor healthcare access [ 32 , 33 ]. A combination of public health security threats, both new and reemerging infectious diseases, challenged ensuring health security [ 34 ]. For example, the health service delivery, mainly the lives of many children, was at risk associated with the lack of treatment for common childhood illnesses in Liberia during the Ebola outbreak [ 35 , 36 ]. Exclusion from work due to health problems can easily result in economic impoverishment and inequitable healthcare access, which will undoubtedly worsen health status [ 37 ]. For instance, socially excluded population groups received health services from a dysfunctional publicly provided health system marked by gaps and often invisible barriers in Guatemala and Peru, which undermines the progress towards UHC [ 38 ]. The changes in frequency, intensity, spatial extent, duration, and timing of extreme weather and climate events were also exposed to health threats [ 39 ]. For example, extreme weather events caused an increase in disease prevalence, such as malaria and other vector-borne diseases, malnutrition, food insecurity and food-borne diseases [ 40 ]. Inadequate primary health care system capacity to provide responsive health services to storm and flood-related health problems was another challenge [ 41 ].
Health workforce
In our review, nine articles reported their findings on the successes and challenges of health workforces towards UHC and health security. A well-performing health workforce provides responsive, fair and efficient health services to achieve the best health outcomes [ 27 ]. Task-shifting policy, ensuring accountability and ad hoc redistribution of health workers had a knock-on effect on health services delivery and building RHS [ 42 , 43 , 44 ]. Training on disaster preparedness and management, and rewarding packages, such as incentives and hazard allowance, facilitated healthcare workers willing to participate in disaster management [ 45 ]. Monitoring and evaluating frontline health workers levels of preparedness against public health emergency threats periodically by their higher-level hierarchy was crucial for early detection and control of health threats [ 46 ].
Lack of skilled and inadequate health workforce distribution was the major obstacle to containing an outbreak, and deaths were attributed to treatment delays [ 35 , 43 ]. Low perception of risks by tourists/ pilgrims, ineffective training, poor control of risk factors, and shortages of infrastructures were the challenges in combating contagious diseases [ 47 ]. Healthcare workers’ practices on effective pandemic management, including corona-virus disease (COVID)-19 were constrained by individual factors, such as education, residence, work station location, hygiene promotion, and social distance management [ 42 ]. Patient assessments by non-indigenous health workers during an emergency were also barriers to early identification and management of acute health events [ 30 ].
Health information system
In this review, ten articles described the contributions and challenges of health information on RHS to realise UHC and health security. A well-functioning HIS ensures the production, analysis, dissemination and use of reliable information for policy decisions [ 27 ]. Building accountability, knowledge culture management, and evidence through regular data quality audit strengthened health management information systems (HMIS) [ 44 ]. Integrated disease surveillance, flexible automation and data processing improved clinical care and health system preparedness to tackle health threats [ 48 , 49 , 50 ]. Strengthening the health system’s capacity was another key measure to rapidly process and communicate test results for pandemic responses [ 51 ].
Poor surveillance, late timing of responses and lack of triggers weakened the functionality of plans and exposed to a high burden of diseases [ 52 ]. Poor data management, misinformation on the risk and transmission, lack of awareness, resources and insufficient electronic reporting system were responsible for the spread of diseases [ 51 , 53 , 54 ]. For instance, misinformation during the Ebola outbreak affected most communities in putting measures in place to stop the spread of the virus [ 54 ]. People approached traditional healers who lacked knowledge on treating certain health shocks in modern medicine was the major problems in early responses [ 35 ].
Medical products, diagnostics, and infrastructures
Of the reviewed articles, 10 reported their findings on the successes and constraints of medical products, diagnostics, and infrastructures to realise UHC and health security. Equitable access to essential medical products, vaccines and technologies to assure quality, safety, efficacy and cost-effective healthcare services to users was the attribute of a well-functioning health system [ 27 ]. To attain UHC, strengthening local preparedness, planning, manufacturing, and coordinating public–private initiatives and training in LMICs was important [ 55 ]. The key factors to facilitate early detection were the provision of rapid, cost-effective, sensitive, and specific diagnostic centers through the inauguration of national centers [ 53 , 56 ]. Identifying emergency medicines, adaptable mobile health care units and systems for mobilisation of health professionals contributed to successful interventions to curb health emergencies [ 57 ].
High patient load, lack of diagnostics, destruction of health facilities and lack of specific funds for medicine procurement may compromise the health system’s hardware (health facilities and supplies) and contained public health threats [ 3 , 30 , 32 , 57 ]. For instance, inadequate essential logistics such as blood, oxygen cylinders, ergometrine and sulphadoxine paramita mine in Ghana was the causes for low level of preparedness to control maternal mortality [ 58 ]. Shortages of medical supplies, personal protective equipment (PPE), and electricity increased the rate of Ebola infections during the outbreak [ 35 ]. Most medicine outlets experienced longer lead times associated with the poor inter-country transportation and limited manufacturing capacity, which were also Namibia's main challenges [ 55 ].
Health financing
In this study, 13 articles described their findings on the contributions and limitations of healthcare financing to realise UHC and health security. A good health financing system raised adequate funds for health to ensure people can use needed services and be protected from financial catastrophes [ 27 ]. Under a publicly funded health financing system that fits well with values and population preferences improved compliance, sustainability, and equity [ 59 ]. An integrated financing mechanism through high income and risk cross-subsidies reduced reliance on OOP payments, maximises risk pools and resource allocation mechanisms facilitated to achieve UHC [ 60 ]. Universal health coverage can substantially improve human security through securing finances [ 61 ]. Universal health coverage indicators were also positively associated with the gross domestic product (GDP) per capita and the share of health spending channels [ 62 ]. Income redistribution improved equity in health care service delivery [ 63 ].
Lack of adequate funds and non-affordable medical costs were the main barriers to universal financial protection and poor management of an outbreak [ 33 , 35 ]. In Burundi, for example, performance-based financing without accompanying access to incentives for the poor was the critical challenge to improve equity in health [ 64 ]. Health equity advancement challenges secured dedicated funds to support transformative learning opportunities and build infrastructures [ 65 ]. Because of causalities, the health sector requires additional financial support to address the increased demand for health services; however, movement restrictions limit people’s access to participate in gainful activities [ 30 ]. Low funds from international donors were erratic and far below the amounts required to meet the health needs at crisis time [ 66 ]. People could not trade their commodities because of the fear of attacks exposing service users to lack finances [ 30 ]. Falling in financial access to health services has resulted in political demonstrations and violent unrest [ 67 ].
Leadership and governance
Our review found that 22 articles reported their findings on health system governance (HSG) to realise UHC and health security. Good HSG ensured strategic policy frameworks combined with effective oversight, coalition, appropriate regulations, system design and accountability [ 27 ]. Building strong partnerships, ensuring accountability, coordination, rationalisation, and connection of pandemic planning across sectors and jurisdictions resulted in better preparedness [ 48 , 68 ]. Clear communication channels, multisectoral, and multilevel controls were essential to translate policy into actions [ 52 , 56 ]. Vertical and horizontal integration, centralised governance, responsible leadership, and social capital at community level were needed to address health shocks and homogenous implementation of health interventions [ 54 , 69 , 70 ]. Fueling high-performing teams and increasing investment in early warning and detection systems required leadership resilience to enable action at all levels [ 71 , 72 ].
Working alone the state had proven only partially effective, a situation exacerbated by the natural tendency within the public to ignore as irrelevant to themselves [ 73 ]. In addition, lack of clarity of stakeholder roles, poor leadership and absence of clear government policy for the delivery channels and financial coverage led to fragmentation and poor health system response [ 35 , 52 , 66 ]. For instance, weak governance and decision-making processes, such as high bureaucracy, low prevention culture, and lack of coordination between primary, social and hospital care providers, indicated virus’s rapid spread in the French population in the first wave of COVID-19 [ 74 ].
Moving away from a one-size fits-to all approach in guiding pandemic response, service delivery, political commitment, fair contribution and distribution of resources are helpful to speed up the path towards UHC [ 75 ]. For example, village health volunteers in Thailand, Zanmi Lazante’s Community Health Program in Haiti, Agentes Polivalentes Elementares in Mozambique, Village Health Teams in Uganda, lady health workers in Pakistan, BRAC in Bangladesh, Family Health Program in Brazil, and Health Extension Program in Ethiopia are successful community-based models contributed immensely to achieve health development goals [ 76 ]. In addition, community participation and coordination between different stakeholders significantly impact the prevention of encephalitis in Japan [ 77 ], and early detection of cases and collection of mortality data in Cambodia [ 78 ]. On the contrary, it was difficult for the system to automatically adjust its structure to reduce uncertainty and ascertain complex adaptive behaviour when facing public health emergencies [ 79 ].
With an overarching political will, well-integrated and locally grounded health system can be more resilient to external shocks [ 80 ]. Political leadership was critical during the crisis, which helped the government to develop a response strategy and effective implementation [ 81 ]. For instance, Singapore’s dexterous political environment allowed the government to institute measures to control COVID-19 swiftly [ 56 ]. On the other hand, political instability or war in Syria affected healthcare services by destroying physical health care infrastructures [ 3 ].
In this review, we developed a resilient health system framework that could assist countries in their endeavor toward universal health coverage and health security. The framework involves an integrated and multi-sectoral approach that considers the health system building blocks and contextual factors. The input components of the framework include health financing, health workforce, and infrastructure, while service delivery is the process component, and UHC and health security are the impact program components. The framework also considers health system performance attributes, such as access, equity, quality, safety, efficiency, sustainability, responsiveness, and financial risk protection. Additionally, the cross-cutting components of the framework are leadership and governance, health information systems (HIS), and contextual factors (e.g., political, environmental/climate, socioeconomic, and community engagement) that can affect the health system at any stage of the program components (Fig. 2 ).

Resilient health system framework for UHC and health security
We also indicated that RHS is critical to achieving UHC because it enables the provision of accessible, quality, and equitable health services, while also protecting people from financial risks associated with illness or injury. Such systems are built on strong primary healthcare services, effective governance and leadership, adequate financing, reliable health information systems, and a well-trained and motivated health workforce [ 42 , 43 , 44 ]. Resilient health systems are better equipped to deliver high-quality healthcare services to all people, including those who are marginalised or living in poverty. This, in turn, investing in RHS is essential for achieving UHC, promoting health equity, and building more sustainable and equitable societies. On the contrary, lack of healthcare access, skilled health workforces, and uneven distribution of health facilities and health workers [ 32 , 33 , 35 , 43 ] were the challenges to achieving health sector goals.
Lack of access, non-responsive and inequitable healthcare services were the challenges to achieve UHC and health security [ 31 , 32 , 33 ]. Such challenges can be solved by primary health care approach which is an effective strategy to provide accessible, acceptable, equitable and affordable health services to achieve UHC [ 82 , 83 ]. Community-based and differentiated service delivery models are also important platforms for improving healthcare delivery, access, outcomes, and to meet the specific needs and preferences of different groups of patients [ 84 , 85 ]. Community-based service delivery model can bring healthcare services closer to where people live and work, and overcome barriers to healthcare access such as transportation, distance, and cost [ 84 ]. This service delivery model has also the potential to facilitate a more effective response during healthcare crises by minimising top-down approaches and maximising bottom-up strategies through empowering local communities to take ownership of their health and wellbeing [ 86 ]. Additionally, differentiated service delivery model can meet the specific needs and preferences of different groups of patients. For example, providing family planning services within HIV clinics helps women living with HIV to access both services at the same time [ 85 ]. Similarly, considering a health system away from a one-size-fits-all approach to healthcare delivery is essential in meeting the needs of diverse patient populations [ 87 ].
Lack of skilled and inadequate distribution of health workforces were another major obstacle to contain an outbreak and deaths attributed to delays in treatment [ 35 , 43 ]. Conducting integrated supportive supervision, maintenance of human resource information systems, and national task shifting policy are important strategies that can help to address critical health workforce gaps and maldistribution [ 42 , 44 ]. Healthcare workers' pre-service and in-service training opportunities are indeed key to providing quality care. Healthcare workers who receive adequate pre-service and in-service training are better equipped to provide quality care to patients, and also to adapt to new challenges and changing healthcare needs over time [ 88 ]. Training in disaster preparedness and offering rewarding packages can also play an essential role in enhancing the willingness of healthcare workers to participate in disaster management [ 45 ]. For instance, Kenya's Field Epidemiology and Laboratory Training Program (FELTP) has played a significant role in strengthening the capacity of healthcare workers to detect, document, respond, and report unusual health events [ 89 ]. In addition, monitoring frontline health levels is an essential part of preparedness against public health emergencies. This can involve monitoring healthcare facility capacities and the overall preparedness of the healthcare system to respond to an emergency [ 46 ].
Poor infrastructure, absence of emergency stockpiles, inadequate logistics, and shortages of medical supplies can be potential obstacles to achieving UHC during health emergencies [ 30 , 35 , 57 , 58 ]. A strong public health infrastructure can help to ensure that healthcare resources are distributed equitably, based on need rather than ability to pay. This is particularly important during a pandemic, when resources may be scarce and demand for healthcare services is high [ 90 ]. Integrating pharmaceutical supply chain activities with modern technologies and establishing strong relationships between manufacturers, distributors, prescribers, and insurance organizations can help ensure that essential supplies and logistics are available promptly [ 91 ]. Efficient procurement and an effective supply chain management system are essential components of a well-functioning healthcare system. They can help ensure that essential medicines, medical supplies, and equipment are available where and when they are needed, which is critical to achieving UHC and providing quality healthcare services to all individuals, regardless of their ability to pay [ 92 ].
The main challenges for universal financial protection were inadequate healthcare funds [ 35 ]. Context specific health financing mechanisms are essential to provide strong and sustainable health financing and move towards UHC [ 44 , 93 ]. Additionally, cross-subsidisation from rich to poor and low-risk to high-risk groups provide universal access for the entire population [ 94 ]. Similarly, reducing of health systems reliance on OOP payments and maximising risk pools were supportive to achieving UHC [ 60 ]. Universal health coverage can play a significant role in improving human security by providing financial protection against the cost of healthcare. In many countries, people face significant financial barriers to accessing healthcare services, and as a result, they may be forced to forgo necessary care or incur significant debt to pay for it. The example of Thailand is a good illustration of the potential benefits of UHC. Thailand implemented a comprehensive UHC program in the early 2000s, which provided coverage for all citizens and legal residents. Over the course of a decade, this program helped to reduce the annual impoverishment rate due to medical costs from 2.71% to 0.49% [ 61 ].
Poor leadership and absence of clear government policy led to fragmentation and poor health system response [ 35 , 66 ]. It is essential to involve a diverse range of stakeholders in pandemic preparedness and response efforts to ensure that a comprehensive and effective response is implemented. Collaborative efforts that include input from various stakeholders are more likely to lead to successful outcomes in mitigating the impact of a pandemic [ 73 , 95 ]. Good leadership is essential for effective outbreak response because it helps to coordinate and guide the efforts of different stakeholders, including health workers, community leaders, and government officials. A strong leader can help to build trust and confidence among the community, mobilise resources, and ensure that everyone is working together towards a common goal [ 54 ]. Health systems governance is essential for creating RHS that can respond to emerging health challenges, such as pandemics, as well as ongoing health concerns. By building strong partnerships and accountability mechanisms, health systems can better address the needs of individuals and communities, and improve overall health outcomes [ 48 ]. Cultivating bottom-up and top-down forms of accountability is also important to improve the quality and coverage of health services [ 96 ].
This study will provide an insight on RHS framework for achieving UHC and health security with an integrated and multi-sectoral approach that considers the health system building blocks and contextual factors. The limitations of this review include that the study did not quantitatively estimate the extent of resilient health system for UHC and health security. This is because we used articles based on various quantitative, qualitative, and mixed methods. In addition, we used the Rees et al. appraisal instrument as a guiding framework for the eligibility criteria [ 25 ]. The Rees specifies some methodological criteria for diverse types of studies but does not have a cut-off point for excluding studies.
This review provides evidence of the successes and challenges of RHS and its impact on achieving UHC globally. The review will also give an insight into the key determinants of RHS to achieve long term health sector goals. It will raise health programmers’ awareness of the importance of RHS and initiate an idea for future discussion and arguments on the subject. The review will also help policymakers and government officials to revise and update their strategic plans and policy directions. This review will also assist policy makers in introducing accountability within public institutions to provide more inclusive and equitable health services without excluding any population groups to achieve UHC. This review will help policymakers to formulate an agreed core set of global and national indicators to improve their health systems performance. This review will also help future researchers as baseline information.
The aspiration for UHC and health security will be realised only through a RHS. Advanced healthcare infrastructures and adequate number of health care workers are essential to build a RHS; however, they are not adequate to protect the health systems from potential failures. The health system’s ideology, traditions in policymaking and management, orientation of service delivery, capacities, motivation, and morale of healthcare workers can affect the nation’s health system. Context-specific redistribution of health workers, task-shifting policy, and result-based health financing policy are helpful in building RHS. It is high time that countries transform their health systems through an integrated and multi-sectoral approach to serve as a road map to realise UHC and health security. We are also recommending for future research studies to focus on building a RHS that can support UHC and ensure health security. Such future studies shall be conducted at the national, regional and sub-regional levels to provide context-specific guidance.
Availability of data and materials
Not applicable.
Acknowledgements
The first author would like to acknowledge other authors for their contribution in searching, extracting, and writing this article. The first author would also extend his gratitude, particularly for the last two senior authors (RBK and YA), for their exceptional dedication in shaping this review.
Author information
Authors and affiliations.
Departement of Health Systems and Policy, Institute of Public Health, University of Gondar, Gondar, Ethiopia
Departement of Health Education and Behavioral Sciences, Institute of Public Health, University of Gondar, Gondar, Ethiopia
Adane Nigusie
School of Public Health, The University of Queensland, Brisbane, Australia
Dereje Gedle, Resham B. Khatri & Yibeltal Assefa
College of Medicine and Public Health, Flinders University, Adelaide, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation: AD and YA. Data curation: AD, AN and DG. Formal analysis: AD, AN, DG, RBK and YA. Methodology: AD, AN, DG, RBK and YA. Supervision: RBK and YA. Writing – original draft: AD. Writing – review & editing: AD, AN, DG, RBK and YA.
Corresponding author
Correspondence to Ayal Debie .
Ethics declarations
Ethics approval and consent to participate.
Ethical approvals were not required as the study was a systematic review of articles. The study was registered with PROSPERO number CRD42020210471.
Consent for publication
Competing interests.
All authors declared that they have no competing interest.
Supplementary Information
Additional file 1..
Search strategy.
Additional file 2.
ENTREQ checklist.
Additional file 3.
PRISMA-ScR checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Debie, A., Nigusie, A., Gedle, D. et al. Building a resilient health system for universal health coverage and health security: a systematic review. glob health res policy 9 , 2 (2024). https://doi.org/10.1186/s41256-023-00340-z
Download citation
Received : 31 March 2022
Accepted : 05 December 2023
Published : 04 January 2024
DOI : https://doi.org/10.1186/s41256-023-00340-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health security
Global Health Research and Policy
ISSN: 2397-0642
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 07 March 2022
Universal healthcare coverage, patients' rights, and nurse-patient communication: a critical review of the evidence
- Abukari Kwame ORCID: orcid.org/0000-0003-3231-3100 1 &
- Pammla M. Petrucka 2
BMC Nursing volume 21 , Article number: 54 ( 2022 ) Cite this article
7506 Accesses
5 Citations
4 Altmetric
Metrics details
The Sustainable Development Goals adopted by world leaders on September 25, 2015, aimed to end poverty and hunger, promote gender equity, empower women and girls, and ensure human dignity and equality by all human beings in a healthy environment. These development goals were premised on international human rights norms and institutions, thereby acknowledging the relevance of human rights in achieving each goal. Particularly, sustainable development goal 3, whose objective is to achieve universal health coverage, enhance healthy lives, and promote well-being for all, implicitly recognizes the right to health as crucial. Our focus in this paper is to discuss how promoting patients’ rights and enhancing effective nurse-patient communication in the healthcare setting is a significant and necessary way to achieve universal health coverage. Through a critical review of the empirical research evidence, we demonstrated that enhancing patients’ rights and effect nurse-patient communication will promote people-centered care, improve patients’ satisfaction of care outcomes, increase utilization of care services, and empower individuals and families to self-advocate for their health. These steps directly impact primary healthcare strategies and the social determinants of health as core components to achieving universal health coverage. We argue that without paying attention to the human rights dimensions or employing human rights strategies, implementing the other efforts will be inadequate and unsustainable in protecting the poorest and most vulnerable populations in the achievement of goal 3.
Peer Review reports
On September 25, 2015, world leaders at the United Nations (UN) General Assembly adopted a set of 17 sustainable development goals (SDGs) and 69 targets in an agenda titled Transforming our World: The 2030 Agenda for Sustainable Development, in which global leaders pledged to take bold and transformative steps to free the world and all people from poverty and hunger, to promote gender equity and empower women and girls, and to ensure that human dignity and equality are enjoyed by all human beings in a healthy environment [ 1 ]. These far-reaching, people-centered, and transformative sets of goals and targets focused on ensuring that “no one is left behind” as the world forges ahead to achieve economic, social, and environmental sustainability in its development programs, practices, and policies by 2030.
Recognizing the values of human dignity and equality and the impact development programs, practices, and policies have on these values, the SDGs were anchored on international human rights law, norms, and provisions, as emphasized in the Preamble, the Declaration, and other sections of the agenda document. In particular, the significance of health as a human right and the need for universal access to health by all was captured in SDG3, whose focus is to "ensure healthy lives and promote well-being for all, at all ages." [ 1 , p. 14] Yet, despite recognizing the right to health in SDG3 and the significance of implementing the SGDs with attention to human rights principles as emphasized in the SDGs Agenda, the right to health is only implicitly referenced in targets 3.7 and 3.8 of SDG3.
Without much attention to human rights and the right to health principles in the universal health coverage (UHC) discourse or strategies to implement the targets, the approaches outlined in SDG3 will be inadequate to protect the poorest and most vulnerable populations in the achievement of SDG3 [ 2 , 3 ]. Implementing UHC ensures that all people can obtain the health services they desire without suffering significant financial hardship when accessing those services [ 4 ]. For UHC to thrive, there must be equity in access to care services so that all those who need these services can get them. In addition, care services must be of high quality to improve the health of the people receiving them, and accessing the services must guarantee financial-risk protection such that the cost of using the service does not put undue financial stress on the users [ 4 , 5 ].
Moreover, as a right to health issue, UHC recognizes the importance of the social determinants of health (SDH), the role of primary healthcare, and the impact of both internal and external healthcare institutional factors [ 5 , 6 , 7 , 8 ]. Furthermore, healthcare issues, such as coverage vs. access, access vs. quality, and care itself, are significant in the UHC discourses. These issues need to be critically examined, as Fried et al. [ 5 ] argued that access to healthcare services does not often guarantee quality services or satisfaction of care outcomes. We explore the question: How does a consideration of patient rights and the right to health contribute to achieving SDG3 and the global discourse of universal health coverage? Thus, we aim to present and discuss the UHC of SDG3 from a rights-based approach. Further, we will examine how effective nurse-patient communication and respect for patients' rights are crucial to achieving UHC; hence, emphasizing the right to health and patients' rights in the UHC discourse is desired now than ever. To achieve this paper's objectives, we will first discuss UHC as a human rights issue. Next, we examine the right to health and patients' rights, effective nurse-patient communication, and patient-centered care as crucial to achieving UHC. We then present a position statement for consideration in health policy, decision-making, and practice before concluding the paper.
Critical review methodology was adopted in this paper. Grant and Booth [ 9 ] argued that a critical literature review explores and evaluates the diverse body of previous research to take stock of what is significant which may result in a model or hypothesis building. Also, Pare´ et al. [ 10 ] argued that one strength of critical reviews is their ability to highlight problems and gaps in research about a topic with the aim of strengthening knowledge development by giving a focus and direction for studies or to improve practice. Scholars have noted that despite the relevance of critical reviews, it has “no formal requirement to present methods of the search, synthesis, and analysis explicitly” as done in systematic reviews, and that “the interpretative elements are necessarily subjective and the resulting product is the starting point for further evaluation” [ 9 , p. 97; 10 ]. Thus, we adopted a critical stance in this paper by engaging with the literature to argue that achieving universal healthcare access by 2030 depends on taking note of the issues we discuss into consideration in nursing care practices, health policy, education, and management.
Despite the limitations of a critical review methodology, some scientific literature review principles were implemented in this study. The paper originated from the first author’s doctoral comprehensive exams organized in February 2021. Included articles were recommended by four expert interdisciplinary doctoral committee members including the second author. Each committee member was asked to recommend at least ten relevant articles on the topic. The objective of the written exam was to discuss the relevance of patient rights and the right to health in advancing the global discourse on universal healthcare coverage (UHC) as crucial to achieving the health sustainable development goal. Recommendations were made by the committee members after a follow-up oral exam. The first author then conducted a further literature search using keywords such as patient rights, the right to health, universal healthcare coverage, SDG3, patient-centered care, patient-centered communication, and nurse-patient communication . CINAHL, PubMed, Medline, and Google Scholar databases were searched.
The aim of conducting a further literature search was to broaden the discussion to include the significance of patient-centered care practices in achieving universal healthcare access. All included studies in this critical review were empirical research that investigated the healthcare issues around the keyword in different care settings published in English and open access. All relevant articles were read, and findings relevant to our review question were identified, organized, and discussed in this paper.
Universal health coverage as a human rights issue
The right to health and respect for patient rights in healthcare practices are crucial to achieving health for all and universal healthcare access. Particularly, human rights principles of equity, respect for human dignity, non-discrimination, participation, and transparency in healthcare practice and management, health policy design, and implementation are significant to ensuring health for all by 2030 [ 11 ]. Human rights and the right to health are advocated for in many international human rights documents. For instance, Article 25(1) of the 1948 United Nations (UN) Universal Declaration of Human Rights (UDHR) and Articles 2.2 and 12 of the 1966 International Covenant on Economic, Social, and Cultural Rights (ICESCR) have all underscored health as a human right [ 11 , 12 ].
Furthermore, in nursing care, the revised Code of Ethics for Nurses observes that "inherent in nursing is a respect for human rights, including cultural rights, the right to life and choice, to dignity and to be treated with respect" [ 13 , p. 2]. It further states that the enjoyment of these rights must not be restricted by a person's "age, colour, creed, culture, disability or illness, gender, sexual orientation, nationality, political [affiliation], race or social status" [ 13 , p. 2]. And the significance of human rights in achieving UHC is further emphasized; “nurses value health care as a human right, affirming the right to universal access to health care for all” [ 13 , p. 18]. This assertion acknowledges the interrelatedness of health, human rights, and other socio-cultural dimensions of being human.
As noted earlier, furthering an SDH approach in UHC implementation will require examining the impact of culture and contextual factors on access to health and healthcare service utilization. In particular, care providers' respect for cultural diversity in care and displaying cultural competency and sensitivity to care can promote access [ 12 , 13 ]. Therefore, UHC as a human rights issue is essential, which we addressed further in the next section, under the right to health and patients' rights in the context of health for all by 2030.
Universal health coverage, the right to health, and patients' rights
The right to health is a global concern espoused in several international human rights norms, laws, protocols, and instruments, as indicated in the previous section. The right to health constitutes freedoms and entitlements and recognizes the impact of socio-cultural factors on health. Nonetheless, the right to health does not mean the right to be healthy, given that individual biological and socio-economic conditions differ [ 12 ]. The right to health is an inclusive right and privileges non-discrimination and human dignifying practices in healthcare access. It upholds crucial human rights principles, including respect for human dignity, informed consent, self-determination, and participation in healthcare decision-making [ 12 , 13 , 14 ]. For instance, General Comment No. 14 enjoins on State parties the responsibility of making healthcare facilities, services, and personnel available and accessible (easy to reach, affordable, informative). Care services must be acceptable (respectful of medical ethics and culturally appropriate) and of high-quality regarding the services provided, staff, medicines, and facilities/equipment [ 14 ].
Furthermore, patients' rights are human rights principles emanate from healthcare practices and interactions among care providers, patients, and caregivers. In the European Declaration on the Rights of Patients , patients' rights are defined as fundamental human rights in health care, aiming to protect patients' dignity and integrity and respect for the patient as a person [ 15 ]. Therefore, the right to health and patients' rights are collectively termed 'human rights in patient care' which outlines the core principles of respect for patients' dignity, privacy, informed consent, and self-determination as critical human rights that must be maintained in healthcare practices and interactions [ 13 , 16 ]. Per these rights, patients and their caregivers must be fully involved in their care needs, as the ICN Code of Ethics for Nurses [ 13 ] obligates care providers to provide care services that are person-centered, and respect and value patients' cultural and social characteristics and preferences. Thus, patients and their families must be treated uniquely based on their care needs and circumstances.
For instance, historical antecedents in health research, biomedical experiments, and healthcare practices have shown that communities and specific cultural groups were unethically treated. Moreover, happenings in many modern healthcare institutions are replete with abusive and discriminatory care practices, as cited studies in this and the subsequent sections will show. Hence, the right to health and patients' rights have become critical human rights issues in several countries. National patients' rights charter, service pledges, codes of ethics, and standards of practices for various healthcare professional groups are being developed to safeguard patients' rights. Examples of these documents include the Helsinki Declaration for medical research [ 17 ], the ICN Code of Ethics for Nurses , [ 13 ] the International Code of Ethics for Midwives , [ 18 ] and national patients' charters such as the Patients' Charter of Ghana , [ 19 ] the Charter of Patients' Rights in Egypt , [ 20 ] and patient charters of several other countries [ 21 ].
These national patients' rights charters have stipulated specific rights and responsibilities of patients that healthcare professionals must uphold and preserve in their care practices and the care process.
Patients' rights are essentially part of the right to health, which, when respected and upheld, can significantly contribute to UHC achievement. First, UHC advocates making healthcare accessible and affordable for all, however, healthcare practices that do not respect patients' rights could lead to inadequate care outcomes and care satisfaction [ 22 ]. Moreover, substandard and undignifying patient-provider interactions could prevent future access and utilization of healthcare services and facilities, despite these being available, as observed by Ojwang [ 23 ] and Ojwang et al. [ 24 ] in studies on patients' rights in Kenyan hospitals. These studies found that, although some patients were treated with dignity and respect, many others were often ignored, discriminated against, intimidated, grouped, and labeled based on their social status. Ojwang et al. [ 24 ] argued that these acts by nurses threatened patients' rights to dignity and humanness and often led to patients complaining, criticizing, protesting, and accusing nurses, as ways to assert their rights. These incidents can affect care quality and uptake, especially among vulnerable patients.
The value of patients' rights and effective patient-provider communication and interaction is crucial to achieving UHC. Following this argument, the critical questions to ask are how can effective nurse-patient communication and patient-centered care practices contribute to UHC? How can a study on nurse-patient communication and patients' rights contribute to the UHC discourse's advancement?
Universal healthcare coverage, healthcare systems, and patients' rights
We acknowledge that advocating a human-rights-based approach to UHC would have implications for healthcare policy implementation and care practices. First, achieving UHC means making healthcare services in all healthcare systems, including traditional medical systems (traditional complementary and alternative medical systems), available, accessible, affordable, and high quality. The traditional medical systems provide healthcare to over 60% of global populations in developing and developed countries. Hence, nation-states and their governments will need to embrace integrative healthcare systems and incorporate traditional medical systems practices and services into their national healthcare policies, planning, financing, and monitoring/evaluation practices [ 25 ]. The WHO has noticed that existing barriers, such as geographical and institutional barriers, “the predominance of curative, hospital-based, and disease-based healthcare services” are responsible for poor access to care services over the years [ 26 , p. 35]. Other studies have shown that differences in belief systems about health, illness, and healing between western biomedical and traditional indigenous practitioners constitute a significant barrier to medical system integrations [ 26 , 27 ].
Another critical factor is that funding for traditional medicine and services is low as governments and their health ministries have challenges budgeting and planning for health services provided by traditional healers [ 26 ]. For instance, Carrie et al. observed that “although the overall cost of delivering traditional medicines may be lower than the price of modern medicine, lack of sufficient funding and coverage to enable access may limit the use of traditional medicine in communities” [ 27 , p. 5]. Despite the challenges in achieving integrative healthcare systems, the WHO [ 25 ] argues that accessing qualified traditional and complementary medicine is a positive way to achieve universal health coverage.
Besides, issues of patients' rights, cultural sensitivity, and humility will need a holistic examination within different healthcare systems and practices to avoid the marginalization of specific cultural groups. Some societies, cultural groups, and vulnerable populations have had historical experiences of trauma, injustice, and discrimination with their national healthcare systems and healthcare providers. As a result, many of these cultural groups and populations have distrusted their national healthcare systems and care professionals. Hence, to achieve UHC, the historical experiences, unique circumstances, and medical worldviews of these cultural groups and societies must be considered when designing healthcare policies and practice guidelines to achieve health for all, a position taken strongly by the revised ICN Code of Ethics for Nurses [ 13 ].
Furthermore, the interpretation and application of patient rights principles in particular cultural contexts, medical systems, and healthcare practices (e.g., spiritual healing) may require critical lenses. Many patients' rights principles appear to honour individuality and individual autonomy. However, healthcare decision-making in many cultural contexts is a collective process, sometimes without engaging the patient. Care providers working with an individualistic understanding of human rights and patient rights (influenced mainly by Western ideals) will have to widen their knowledge of human and patient rights to embrace individual rights within collective values. Thus, the compatibility of cultural values, beliefs, and perspectives with Western notions of human rights and patient rights may need a rethink. Healthcare policymakers and care professionals need to reflect on the challenges in implementing UHC policies when collective values and norms overshadow individual rights in positive ways.
UHC, effective nurse-patient communication, and patient-centered care practices
Patient-centered care (PCC) is an approach to care and interpersonal interaction between care providers and patients during care. It embodies providing care services that respect and respond to patients' unique care needs and preferences [ 27 ]. In PCC, patients' experiences, stories, and knowledge must be valued and considered, and patients must engage in the care process as collaborators [ 27 , 28 ]. The first element of the ICN Code of Ethics for nurses––nurses and people––emphasized PCC in nursing care [ 13 ]. It focuses on nurses' interactions with people who access care in the healthcare setting and requires that nurses promote a conducive environment in which the human rights, values, customs, and spiritual beliefs of individuals, families, and communities are respected [ 13 , 29 , 30 ].
The nurse-patient dyad is crucial because nurses constitute a strong healthcare workforce and have more contact hours with patients [ 13 ]. They carry out various care functions, including recording patients' history and vital statistics, caring for patients' hygiene needs (e.g., bathing/washing and dressing patients), and maintaining ward hygiene [ 31 ]. Also, nurses perform some health administrative functions, such as logging cases, and completing forms for patient transfer or health insurance coverage [ 31 , 32 ].
As nurses continue to engage in medical teams and assume new roles with increasing expertise, their social positions and power dynamics also continue to evolve in the clinical space [ 33 , 34 ]. This emerging reality makes the social relationship between nurses and patients very complex across different care settings [ 33 ]. Due to patients’ varying healthcare needs, their dependence on health professionals for care and support, and the knowledge position nurses occupy, there can be a power imbalance in clinical interactions, mostly in favour of nurses. For instance, in a case study on patient involvement in routine palliative clinical care situations, Glasdam et al. [ 34 ] observed that nurses did not readily take up patients’ invitation to dialogue or the knowledge they provide about their body state. The authors argued that the “distribution of power and knowledge between patients and nurses condition nurses to set the agenda and assess when and at what level it is relevant to take up patients’ invitations to involve them in their own case” [ 35 , p. 1618]. According to Glasdam et al., “nurses have the power to define when and how the involvement of patients is going to happen in clinical routine care situations in nursing practice.” [35, p. 1624] Despite the findings by these scholars, we think that different care situations, patients’ contextual variables/backgrounds, and knowledge state could influence the power dimensions in nurse-patient clinical interactions. For details on power dynamics in nurse-patient interactions, see Glasdam et al. [ 34 ] and Mattar e Silva et al. [ 35 ] on physician-nurse power relationships.
Moreover, traditionally paternalizing perceptions about patients as passive participants in care routines are changing as patient empowerment principles are advocated in healthcare ethics and practice [ 36 ]. For instance, Delaney [ 36 ] noted that healthcare organizations and professionals have become more receptive to patient engagement in Australia with the knowledge that patient involvement in their care can enhance safety and care quality. Moreover, the ICN [ 37 ], in its position statement on informed patients, expects nurses, patients, and the public to get involved in research that explores the nature and quality of patient information and how it affects health outcomes and nursing care. Thus, nurses have responsibilities of respecting patients' unique values, needs, beliefs, and rights; disseminating appropriate information for effective decision-making; protecting patients' and caregivers' confidentiality. In addition, nurses must demonstrate professionalism, including "respectfulness, responsiveness, compassion, trustworthiness, and integrity" while providing care, as emphasized in empirical studies and the ICN code of ethics [ 13 , p. 2; 38 ]. The dynamism in nurse-patient communication and interaction makes it an imperative and fruitful ground for engaging in discourses of UHC and patients' rights.
Another essential issue in patient-provider interactions that borders on patient rights is patient autonomy in clinical interactions. As a reviewer rightly observed, patients’ expectation of their degree of autonomy could be compromised when traditional models of bioethics that socialize and position the patient as a passive participant in medical interactions are invoked. Hence, to encourage patient freedom in care, the ICN [ 39 ] position statement on nurses and human rights obligates nurses, and by extension, other care providers, to respect patients’ health rights at all times and in all places, including how they express their care needs, worries, and wishes. Nonetheless, several factors can affect patients' expectation of autonomy, including their health status, socio-cultural backgrounds, knowledge of their illness, and previous experiences with healthcare institutions and care providers. Furthermore, notions of “good and bad patient,” as observed by Campbell et al. [ 40 ], can influence patients’ expectations of their autonomy in clinical interactions.
Generally, however, studies have shown that when care is patient-centered and human dignity preserving, patient disclosure increases, length of stay in hospitals reduces, and patients become empowered to take care of their health [ 24 , 38 ]. Moreover, PCC fosters patients' and caregivers' active participation in healthcare decision-making to improve care quality, [ 41 ] an essential UHC component. PCC, as a patients' rights practice in care, reduces negative attitudes and personal behaviours from both care providers and patients, thereby reducing conflicts, discrimination, abuse, and disrespect, and increases the uptake of care services and positive nurse-patient relationships [ 32 , 42 ].
Communication in nurse-patient clinical interactions is effective if patients are (i) provided the needed information about their health conditions, (ii) engaged in the care processes as significant dialogic partners, (iii) listened to, or given the option to choose from alternative care plans and procedures [ 38 , 41 ]. Effective nurse-patient communication is therapeutic and forms an essential component of PCC. Therefore, the ICN position statement on cultural and linguistic competence recommends that nurses must communicate verbally and in writing in ways sensitive to patients' needs and in a language that patients can understand, if possible, through the use of trained interpreters and translators [ 43 ]. Moreover, effective communication in the nurse-patient dyad can reduce misunderstandings between care providers and patients. For instance, Crawford et al. [ 44 ] maintain that providing equitable and quality health care is compromised when communication difficulties are present, even when healthcare is accessible.
Care and clinical communication become patient-centered when nurses value patients' beliefs, respect patients' cultural backgrounds, and provide care according to patients' needs, preferences, and unique conditions [ 13 ]. It also entails communicating in ways that engage patients and their caretakers and actively listening to patients' concerns [ 13 , 37 , 39 ]. Patient-centered care practices will curtail patient stigmatization and discrimination, especially against people living with HIV/AIDS, mental health illnesses, and the poor, illiterate, and vulnerable patients [ 22 , 32 ]. Besides, effective nurse-patient communication can increase access to healthcare, patient disclosure, patients' participation in healthcare decision making, positive satisfaction of care outcomes, and accurate healthcare data, essential in promoting UHC [ 32 ].
A Note for consideration in health policy and decision-making
Universal health coverage and providing health for all have been a global agenda for decades and captured as the right to health in most international human rights norms and instruments, as highlighted in this paper. However, improving access to healthcare and ensuring better health for the world's poor, marginalized, and vulnerable populations (e.g., women, children, the elderly, people with disabilities, and Indigenous peoples) has never been vigorously pursued than in the twenty-first century. Starting from early 2000, world leaders at the United Nations agreed to eight development goals achievable within the next 15 years, as the 2015 UN Millennium Development Goals (MDGs). Three of these goals: MDG4 (reduce child mortality), MDG5 (reduce maternal mortality), and MDG6 (Combat HIV/AIDS, malaria, and other diseases), were primarily targeted at health and improving healthcare access to the most vulnerable global populations. Significant gains were made in these goals despite several different challenges. For example, governments were not strictly required to provide disaggregated data in monitoring and reporting the MDGs. Instead, they focused on achieving quantified targets without much emphasis on quality, and attention to human rights-based targets in the MDGs was lacking (see [ 2 ] for other critiques).
Following the MDGs' challenges, a more progressive, people-centered, and interdependent set of development goals was adopted again in September 2015, as Sustainable Development Goals (SDGs), achievable by 2030. An overarching health goal, the SDG3, has broader targets and indicators than were found in the health MDGs. Although achieving this particular goal and the rest require financial, logistics, and other resources, emphasizing the human rights dimensions and principles in their implementation process is paramount. Without this focus, the SDGs would likely suffer the same faith as the MDGs. Hence, in this section, critical recommendations are outlined for consideration of health policy and decision-making regarding taking a human rights and patients' rights approach to the UHC/SDG3.
First, awareness of patients' rights must be a critical healthcare decision priority in many countries through public health campaigns. Healthcare advocacy campaigns within healthcare institutions must include information on patients' rights and responsibilities. As a significant sector of the health workforce, nurses should verbally inform, explain to, and educate patients with poor health literacy about patient rights. When patients' rights to dignity, informed consent, participation, among others, are preserved during clinical interactions, abuse and discrimination are reduced, and patient disclosure and uptake of healthcare services increase, [ 36 , 37 , 45 ]. Without much attention to this quality aspect of care, access to available healthcare services will be affected. Many women often refuse facility-based delivery or accessing maternity care in hospitals due to abuse, discrimination, and disrespect. Instead, they prefer home delivery attended by traditional birth attendants [ 22 , 42 , 46 ]. Also, abuse of patients' rights and lack of privacy, confidentiality, and respect, coupled with other ethical dilemmas in HIV/AIDs care settings, affected the uptake of HIV/AIDS care services among this patient population [ 47 ].
Secondly, patients' rights regulatory schemes must be instituted in healthcare institutions to enforce patient rights charter regulations and the implementation of nursing ethical codes and standards of practice, and to promote equity and environmental justice when accessing healthcare, as emphasized in the ICN [ 13 , 39 ]. That is, upholding healthcare ethical standards and patients' rights in healthcare practices will significantly reduce abuse, discrimination, marginalization, and improve care outcomes [ 48 ].
Advocating and advancing patients’ rights in nursing practice and care must begin from healthcare educational institutions. Nursing educators must incorporate effective nurse-patient communication and patients' rights models as core components of nursing curricula for knowledge acquisition [ 13 ]. Thus, effective nurse-patient communication is crucial to promoting patient-centered care and patient rights in clinical interactions.
Also, healthcare managers can elevate patient rights responsibilities among care professionals by providing regular in-service training on approaches to preserve patients' rights and implement effective communication in practice [ 28 , 37 , 48 , 49 , 50 ]. These in-service training will bolster care professionals' quality, which is critical to achieving UHC [ 8 ] and a right to health obligation healthcare institutions must fulfil [ 12 , 14 , 39 ]. Nursing managers should continue to improve nurses' expertise, skills, cultural competence, and quality of care [ 13 , 32 , 51 ]. The active engagement of care managers in the nurse-patient dyad through monitoring and evaluation practices will further support better nurse-patient relationships, patient-centered care practices, and address nurses' personal and professional challenges [ 36 , 52 ]. For instance, Delaney [ 36 ] argues that traditional healthcare management styles focused on illness, intervention, and medication have limitations on optimizing health. Adjusting and aligning clinical care management that honour patients' needs and input have positive outcomes. Moreover, adopting transformational leadership, collaborative and innovative practices can support patients’ participation in, understanding of, and recovery from ill-health. The 21 st -century nurse faces many demands and challenges, including increasing patient needs, high patient turnout, added administrative duties (e.g., filling diverse forms), and limited time to interact with patients. As a result, there should be an ongoing dialogue between management level officers on how to support healthcare staff to provide quality and patient-centered care that is ethical and patients' dignity preserving.
Advocating for UHC is crucial and forms one route to healthcare access. Yet, improving care quality and patient satisfaction constitutes another significant matter that needs attention. Broadening UHC implementation processes to include discourses on effective nurse-patient communication, respecting patients' rights, and promoting the right to health is essential to achieving ‘Health for All’ by 2030. Shifting healthcare policy, education, decision-making, and practice to embody the socio-biology and social determinants of health approaches is a priority. The impact of culture and other contextual factors on healthcare access are significant and deserving in UHC discourse.
Healthcare institutional internal structures, hierarchies, and practices that hamper good nurse-patient communication and patients' rights need critical examination. Nurses and nursing managers have active roles to ensure that care is patient-centered and based on human rights, patients' rights, and the right to health principles. Without incorporating a human rights lens and approaches to the implementations of the SDG3, the targets and indicators may be inadequate to protect the poor and vulnerable populations in the global effort to achieve UHC access by 2030.
A limitation of this study, which generally applies to critical reviews is its methodology, which puts less emphasis on literature search and analysis criteria. Thus, the outcome of such a review might be interpreted by some scholars as less scientific. Nonetheless, our critical engagement with the literature and the recommendations made by the expert doctoral committee on both the included studies and an earlier version of the paper will overcome this limitation.
Availability of data and materials
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Abbreviations
Acquire Immune Deficiency Syndrome
Committee on Economic, Social, and Cultural Rights
Human Immunodeficiency Virus
International Covenant on Economic, Social and Cultural Rights
International Council of Nurses
Millennium Development Goal(s)
Non-communicable diseases
Patient-centered care
Primary health care
Sustainable Development Goals
Sustainable Development Goal 3
- Social determinants of health
Tuberculosis
Universal Declaration of Human Rights
Universal health coverage
United Nations International Children Emergency Fund
World Health Organization
United Nations General Assembly. Transforming our world: The 2030 Agenda for Sustainable Development. United Nations. Seventieth session, Agenda items 15 and 116. 2015. http://www.un.org/en/development/desa/population/migration/generalassembly/docs/globalcompact/A_RES_70_1_E.pdf .
Chapman AR. Assessing the universal health coverage target in the sustainable development goals from a human rights perspective. BMC Int Health and Hum Rts. 2016;16(33):1–9. https://doi.org/10.1186/s12914-016-0106-y .
Article Google Scholar
Williams C, Hunt P. Neglecting human rights: accountability, data and sustainable development goal 3. The Int J Hum Rts. 2017;21(8):1114–43. https://doi.org/10.1080/13642987.2017.1348706 .
World Health Organization. What is universal health coverage? 2020. http://www.who.int/news-room/q-a-detail/what-is-health-coverage . Accessed Jan 5, 2021.
Fried ST, Khurshid A, Tarlton D, et al. Universal health coverage: Necessary but not sufficient. Reproduct Health Matters. 2013;21(42):50–60. https://doi.org/10.1016/S0968-8080(13)42739-8 .
Arredondo A, Recamán AL, Castrejón B. Universal health coverage in the framework of the 2030 global agenda for sustainable development: Agreements and challenges. Viewpoints. 2020;10(1):1–4. https://doi.org/10.7189/jogh.10.010316 .
Boidin B. Sustainable development goals: An opportunity for health in Africa? Glob Health Promotion. 2019;26(1):91–4. https://doi.org/10.1177/1757975916677513 .
World Health Organization (WHO) and the United Nations Children's Fund (UNICEF). A vision for primary healthcare in the 21st century: Towards universal health coverage and the Sustainable Development Goals. WHO and UNICEF. 2018. WHO/HIS/SDS/2018.15.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. https://doi.org/10.1111/j.1471-1842.2009.00848.x .
Article PubMed Google Scholar
Paré G, Trudel M-C, Jaana M, Kitsiou S. Synthesizing information systems knowledge: A typology of literature reviews. Inf Manag. 2015;52(2):183–99. https://doi.org/10.1016/j.im.2014.08.008 .
Perehudoff SK, Alexandrov NV, Hogerzeil HV. The right to health as the basis for universal health coverage: A cross-national analysis of national medicines policies of 71 countries. PLoS ONE. 2019;14(6):e0215577. https://doi.org/10.1371/journal.pone.0215577 .
United Nations Office of the High Commissioner for Human Rights (OHCHR). Fact Sheet No. 31, The Right to Health. OHCHR. 2008. http://www.refworld.org/docid/48625a742.html . Accessed Jan 15, 2021.
International Council of Nurses. ICN Code of Ethics for Nurses, Revised. ICN. 2021. http://www.icn.ch/system/files/2021-10/ICN_Code-of-Ethics_EN_Web_0.pdf . Accessed Feb 05, 2022.
United Nations Committee on Economic Social and Cultural Rights. General Comment No. 14 on the Right to the Highest Attainable Standard of Health (art. 12). Document E/C.12/2000/4. Office of the High Commissioner for Human Rights. 2000. http://www.refworld.org/docid/4538838d0.html . Accessed Jan 16, 2021.
World Health Organization. A declaration on the promotion of patients’ rights in Europe: European consultation on the rights of patients. Amsterdam: WHO Regional Office for Europe; 1994.
Google Scholar
Cohen J, Ezer T. Human rights in patient care: a theoretical and practical framework. Health & Hum Rt. 2013;15(2):7–19.
World Medical Association (WMA). WMA Declaration of Helsinki: Ethical principles for research involving human subjects. Amended by 64th WMA General Assembly, Fortaleza, Brazil, October 2013: WMA. 1964. http://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ . Accessed Jan 18, 2021.
International Confederation of Midwives. International Code of Ethics for Midwives. The Hague: Laan Van Meedervoort. CD2008_001 V2014 ENG. 2014. http://www.internationalmidwives.org . Accessed Dec 18, 2020.
Ghana Health Service. The Patient's Charter. Ghana Health Service. 2002. http://www.ghanahealthservice.org/ghs-subcategory.php?cid . Accessed Dec 22, 2020.
Mohammed SE, Seedhom EA, Ghazawy ER. Awareness and practice of patient rights from a patient perspective: An insight from upper Egypt. Int J for Quality in Health Care. 2018;30(2):145–51. https://doi.org/10.1093/intqhc/mzx182 .
Rider ME, Makela CJ. A comparative analysis of patients’ rights: An international perspective. Int J Consumer Stud. 2003;27(4):302–15.
Miltenburg SA, Lambermon F, Hamelink C, Meguid T. Maternity care and human rights: what do women think? BMC Int Health and Hum Rts. 2016;16(17):1–10. https://doi.org/10.1186/s12914-016-0091-1 .
Ojwang BO. (2011). Communicating patients' rights in Kenyan hospitals: An analysis of nurse-client interactions. In: Musa BA, Donatob JK, editors. Communication, culture, and human rights in Africa: Communication, society, and change series. University Press of America; 2011 Vol 1. p. 253–63.
Ojwang BO, Ogutu EA, Matu PM. Nurses’ impoliteness as an impediment to patients’ rights in selected Kenya hospitals. Health & Hum Rts. 2010;12(2):101–17. https://doi.org/10.2307/healhumarigh.12.2.101 . http://www.jstor.org/stable/ . Accessed Jan 22, 2021.
World Health Organization. WHO Traditional medicine strategy 2014–2023. WHO Press. Geneva. 2013. http://www.who.int/medicines/publications/traditional/trm_strategy14_23/en/ . Accessed Jan 22, 2021.
Carrie H, Mackey TK, Laird SN. Integrating traditional indigenous medicine and western biomedicine into health systems: a review of Nicaraguan health policies and miskitu health services. Int J Equity Health. 2015;14(1):1–7. https://doi.org/10.1186/s12939-015-0260-1 .
Krah E, de Kruijf J, Ragno L. Integrating traditional healers into the health care system: challenges and opportunities in rural Northern Ghana. J Community Health. 2018;43:157–63. https://doi.org/10.1007/s10900-017-0398-4 .
Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington: The National Academies Press; 2001. https://doi.org/10.17226/10027 .
Book Google Scholar
Johnsson A, Wagman P, Boman A, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people: An ethnographic study. J Clinic Nurs. 2018;27:e1651–9. https://doi.org/10.1111/jocn.14315 .
Stievano A, Tschudin V. The ICN code of ethics for nurses: a time for revision. Nurs Health Policy Perspectives. 2019;66(2):154–6. https://doi.org/10.1111/inr.12525 . http://www.onlinelibrary.wiley.com/doi/pdf/ . Accessed Jan 15, 2021.
White J, Phakoe M, Rispel LC. 'Practice what you preach’: nurses’ perspectives on the code of ethics and service Pledge in five South African hospitals. Glob Health Action. 2015;8(1):1–8. https://doi.org/10.3402/gha.v8.26341 .
Haskins MLJ, Phakathi S, Grant M, Horwood MC. Attitudes of nurses towards patient care at a rural district hospital in the Kwazulu-Natal Province of South Africa. Afr J Nurs Midwifery. 2014;16(1):31–43. http://www.hdl.handle.net/10520/EJC155722 . Accessed Jan 10, 2021.
Harvey K, Koteyko N. Exploring health communication: Language in action. New York NY: Routledge; 2013.
Glasdam S, Jacobsen CB, Boelsbjerg HB. Nurses’ refusal of patient involvement in their own palliative care. Nurs Ethics. 2020;27(8):1618–30. https://doi.org/10.1177/0969733020929062 .
Article PubMed Central Google Scholar
Mattar e Silva TW, Velloso ISC, Araújo MT, Fernandes AdRK. Configuration of power relations in physicians and nurses’ professional practices. Rev Bras Enferm Psychiatr Nurs Mental Health. 2020;73(Suppl 1):e20180629. https://doi.org/10.1590/0034-7167-2018-0629 .
Delaney LJ. Patient-centred care as an approach to improving health care in Australia. Collegian. 2018;25:119–23. https://doi.org/10.1016/j.colegn.2017.02.005 .
International Council of Nurses. Informed patients, position statement. ICN. 2015. http://www.icn.ch/sites/default/files/inline-files/E06_Informed_Patients.pdf . Accessed Jan 14, 2021.
Martin-Ferreres ML, De Juan Pardo MA, Porras DB, Moya JLM. An ethnographic study of human dignity in nursing practice. Nurs Outlook. 2019;67(4):393–403. https://doi.org/10.1016/j.outlook.2019.02.010 .
International Council of Nurses. Nurses and human rights position statement. ICN. 2011. http://www.icn.ch/sites/default/files/inline-files/E10_Nurses_Human_Rights%281%29.pdf . Accessed Jan 12, 2021.
Campbell C, Scott K, Skovdal M, et al. A good patient? How notions of ‘a good patient’ affect patient-nurse relationships and ART adherence in Zimbabwe. BMC Infect Dis. 2015;15:404. https://doi.org/10.1186/s12879-015-1139-x .
Article CAS PubMed PubMed Central Google Scholar
Joolaee S, Joolaei A, Tschudin V, Bahrani N, Nikbakht NA. Caring relationship: The core component of patients’ rights practice as experienced by patients and their companions. J Med Ethics Hist Med. 2010;3(4):1–7.
Dzomeku VM, Mensah ABB, Nakua EK, et al. “I wouldn’t have hit you, but you would have killed your baby:”Exploring midwives’ perspectives on disrespect and abusive care in Ghana. BMC Pregnancy Childbirth. 2020;20(15):1–12. https://doi.org/10.1186/s12884-019-2691-y .
International Council of Nurses. Cultural and linguistic competence position statement. ICN. 2013. http://www.icn.ch/sites/default/files/inline-files/B03_Cultural_Linguistic_Competence.pdf . Accessed Jan 10, 2021.
Crawford T, Candlin S, Roger P. New perspectives on understanding cultural diversity in nurse-patient communication. Collegian. 2017;24(1):63–9. https://doi.org/10.1016/j.colegn.2015.09.001 .
Spinnewijn L, Aarts J, Verschuur S, et al. Knowing what the patient wants: a hospital ethnography studying physician culture in shared decision making in the Netherlands. BMJ Open. 2020;10(3):e032921.1-9. https://doi.org/10.1136/bmjopen-2019-032921 .
Moyer CA, Adongo PB, Aborigo RA, Hodgson A, Engmann CM. “They treat you like you are not a human being”: Maltreatment during labour and delivery in rural northern Ghana. Midwifery. 2014;30(2):262–8. https://doi.org/10.1016/j.midw.2013.05.006 .
Kaposy C, Greenspan NR, Marshall Z, et al. Clinical ethics issues in HIV care in Canada: An institutional ethnographic study. BMC Med Ethics. 2017;18(9):1–13. https://doi.org/10.1186/s12910-0171-3 .
Owusu-Dapaah E. Empowering patients in Ghana: Is there a case for human rights-based healthy care law? 2015:91–114. http://www.ssrn.com/abstract=2821895 . Accessed Jan 12, 2021.
Donkor NT, Andrews LD. Ethics, culture and nursing practice in Ghana. Int Nurs Rev. 2011;58(1):109–14.
Article CAS Google Scholar
Korsah AK. Nurses’ stories about their interactions with patients at the holy family hospital, Techiman. Ghana Open J Nurs. 2011;1:1–9. https://doi.org/10.4236/ojn.2011.11001 .
Nwosu J, Inyama V, Emeka C. Effect of nurse-patient relationships on patients recovery at NKST hospital Mkar, Gboko, Benue State. Afr J Nurs Midwifery. 2017;5(2):695–703. http://www.internationalscholarsjournals.org . Accessed Jan 10, 2021.
Kwame A, Petrucka PM. Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: a scoping review. Int J Afr Nurs Sci. 2020;12:100198. https://doi.org/10.1016/j.ijans.2020.100198 .
Download references
Acknowledgements
An earlier version of this study was submitted as part of author AK's written Ph.D. Comprehensive Exam, which AK's Ph.D. committee reviewed. We express our gratitude to the committee members for their valuable comments, suggestions, and critique.
The authors have no financial obligations to declare.
Author information
Authors and affiliations.
College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Abukari Kwame
College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Pammla M. Petrucka
You can also search for this author in PubMed Google Scholar

Contributions
PMP conceived the topic and recommended some relevant articles. AK conducted the literature search, read all the articles, and drafted the manuscript. PMP revised and reviewed the manuscript for intellectual content. Both authors read and approved the submitted version of the manuscript.
Authors’ information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan. Kwame holds a BA in Geography and Linguistics from the University of Ghana and two Master of Philosophy degrees in Indigenous Studies and English Linguistics from UiT, The Arctic University of Norway, Tromso. Kwame's research interests include patients’ rights in nurse-patient clinical communication, language use in social interaction, health communication, medical anthropology, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is Interim Associate Dean, Research & Graduate Studies, and professor in Nursing at the College of Nursing, University of Saskatchewan. She has extensive experience in qualitative and indigenous research methodologies and has published extensively in nursing. Pammla's research areas include child and maternal health, Indigenous peoples' health, global health, and vulnerable populations. Also, she is a co-editor of the BMC Nursing journal and a reviewer for many academic journals.
Corresponding author
Correspondence to Abukari Kwame .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that there are no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kwame, A., Petrucka, P.M. Universal healthcare coverage, patients' rights, and nurse-patient communication: a critical review of the evidence. BMC Nurs 21 , 54 (2022). https://doi.org/10.1186/s12912-022-00833-1
Download citation
Received : 24 November 2021
Accepted : 23 February 2022
Published : 07 March 2022
DOI : https://doi.org/10.1186/s12912-022-00833-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Universal healthcare access
- Patient-rights
- The right to health
- Sustainable development goals
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 11 December 2021
Political economy analysis of universal health coverage and health financing reforms in low- and middle-income countries: the role of stakeholder engagement in the research process
- Giulia Loffreda ORCID: orcid.org/0000-0003-4895-1051 1 ,
- Kéfilath Bello 2 , 3 ,
- Joël Arthur Kiendrébéogo 3 , 4 , 5 , 6 ,
- Isidore Selenou 7 , 8 ,
- Mohamed Ali Ag Ahmed 3 , 9 ,
- Jean Paul Dossou 2 , 3 ,
- Sophie Witter 1 &
- Maria Paola Bertone 1
Health Research Policy and Systems volume 19 , Article number: 143 ( 2021 ) Cite this article
6590 Accesses
2 Citations
9 Altmetric
Metrics details
Progress towards universal health coverage (UHC) is an inherently political process. Political economy analysis (PEA) is gaining momentum as a tool to better understand the role of the political and economic dimensions in shaping and achieving UHC in different contexts. Despite the acknowledged importance of actors and stakeholders in political economy considerations, their role in the PEA research process beyond “study subjects” as potential cocreators of knowledge and knowledge users has been overlooked so far. We therefore aimed to review the approaches with reference to stakeholder engagement during the research process adopted in the current published research on the political economy of UHC and health financing reforms, and the factors favouring (or hindering) uptake and usability of PEA work.
We reviewed the literature to describe whether, when and how stakeholders were involved in the research process of studies looking at the political economy of UHC and health financing reforms, and to identify challenges and lessons learned on effective stakeholder engagement and research uptake. We used a standardized search strategy with key terms across several databases; we screened and included articles that focused on PEA and UHC. Additionally, we conducted a short survey of the authors of the included studies to complement the information retrieved.
Fifty articles met the inclusion criteria and were included in the analysis. We found overall little evidence of systematic engagement of stakeholders in the research process, which focused mostly on the data collection phase of the research (i.e., key informant interviews). Our study identifies some reasons for the varying stakeholder engagement. Challenges include PEA requiring specific skills, a focus on sensitive issues, and the blurriness in researchers’ and stakeholders’ roles and the multiple roles of stakeholders as research participants, study subjects and research users. Among the approaches that might favour usability of PEA work, we identified early engagement, coproduction of research questions, local partners and personal contact, political willingness, and trust and use of prospective analysis.
Conclusions
Stakeholder engagement and research uptake are multifaceted concepts and complex processes, particularly when applied to PEA. As such, stakeholder engagement in the research process of PEA of UHC and health financing reforms is limited and underreported. Despite the challenges, however, stakeholder engagement remains key to ensuring relevance, usability and research uptake of PEA studies. More efforts are required to ensure engagement at different stages of the research process and better reporting in published articles.
Peer Review reports
Introduction
Achieving universal health coverage (UHC) means ensuring access to healthcare for all as well as financial risk protection (Box 1 ) and is one of the targets of the Sustainable Development Goals (SDG 3.8).
Box 1: WHO’s definition of UHC
UHC means that all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship.
This definition of UHC embodies three related objectives:
Equity in access to health services—everyone who needs services should get them, not only those who can pay for them.
The quality of health services should be good enough to improve the health of those receiving services.
People should be protected against financial risk, ensuring that the cost of using services does not put people at risk of financial harm.
Source: WHO. 2019. Universal Health Coverage and Health Financing. https://www.who.int/health_financing/universal_coverage_definition/en/
It is increasingly recognized that progress towards UHC is an inherently political process, in the sense that it entails contestation over power and resources, is influenced by interests, ideas and ideologies, and as such is incremental and context-specific [ 1 , 2 ]. Because of the political nature of UHC processes, political economy analysis (PEA), which brings together the economics of reforms with the politics of change, is deemed to be particularly relevant to investigate them [ 3 ].
In recent years, the empirical and theoretical literature applying PEA to UHC and health financing reforms has been growing [ 4 , 5 , 6 , 7 ]. This literature increasingly calls for specific awareness on the political dimensions and the economy of UHC, as well as “the imperative for the technical to engage the political—and vice versa” [ 8 ]. Much of the concluding reflections of a recent systematic review of the political economy of UHC [ 8 ] focus on methodological aspects of PEA of UHC and how/what could provide an appropriate framing to bring together political and technical analyses. In line with Sparkes et al. [ 9 ], the authors find that “there is a need to build the theoretical and practical frameworks that would enable competent and consistent analysis, the necessary funding to expand that research and the policy preparedness to engage its findings and implications” [ 8 ].
Our study builds on these reviews and propositions. However, we depart from the content and methodological focus to explore an aspect of the PEA of UHC which has been somewhat overlooked so far, that of stakeholder engagement. We noted that all frameworks and theoretical work available stress the central role of agency/actors and stakeholders [ 9 , 10 ], and that existing literature proposes methods and approaches to capture their roles (such as stakeholder mapping [ 11 ] or social network analysis [ 12 ]). In parallel, there is an increasing awareness of the importance of stakeholders not only as “study subjects” but also as cocreators of knowledge and knowledge users [ 13 , 14 ], in order to ensure the applicability and relevance of the research and its findings. In practice, however, it appears that knowledge coproduction might present specific challenges when applied to PEA of UHC. While we describe the challenges and identify potential approaches to address them in a companion empirical paper [ 15 ], here our aim is to explore the existing literature on the political economy of UHC to explore the role of, and approaches to, stakeholder engagement during the research process and attempt to identify lessons learned on barriers and facilitators to stakeholder engagement for PEA of UHC.
To achieve this, our review focuses on the dynamics of stakeholder engagement during research processes that use a political economy lens (i.e., PEA or other similar approaches). By “stakeholders” we mean any actor or institution with an interest or concern in the topic under study and its outcome [ 16 ], whether at national, subnational but also global level. For the case of UHC, it might include, for example, policy-makers at the ministry of health, ministry of finance, presidential office, and other relevant institutions, health managers at the district level, donors at the national or global level, implementing agencies (e.g., health insurance agencies), professional organizations or representative body (e.g., doctors’ associations, nurses’ association, relevant trade unions, and similar), private and private not-for-profit sectors (e.g., associations of private health providers, associations of faith-based providers, pharmaceutical companies), national and international nongovernmental organizations, civil society organizations and community-based organizations (CBOs)/community groups, healthcare beneficiaries or patients and lay community members. Importantly, researchers themselves are potentially included among the stakeholders. Indeed, because of their positionality in relation to the study setting, their ideologies and values and the reflexivity they exercise in relation to their work might place them in a position where they are effective stakeholders on the topic of analysis [ 17 ]. As a caveat, while we tend to refer to stakeholders as a homogeneous group for the purposes of the analysis in this study, it is important to acknowledge that the term includes a multiplicity of actors (as listed above) with differing and often conflicting ideologies, interests and power. This necessarily has an impact on the approaches to, and the outcomes of engaging with each category of stakeholder [ 18 ].
We refer to “stakeholder engagement” as the process of actively engaging actors who are involved in the UHC and health financing reforms at different stages of the research process (not only at the final stage, i.e., the “dissemination” of results). This is in line with current definitions and approaches to research uptake which stress that, to be successful, it should focus not only on the communication of the research, but also on the engagement and capacity-building of key actors, as well as the monitoring and evaluation of uptake [ 19 ]. For UHC and its PEA, stakeholder engagement is particularly important, especially to ensure research uptake of findings for effective policy-making and policy implementation [ 20 ]. Evidence suggests that there is low uptake of UHC research findings [ 21 ], which could be linked to the complex interactions among ideas, ideologies and interests of the actors involved in the UHC process [ 22 , 23 , 24 ]. This points towards the need to engage stakeholders at different stages of a research process to ensure that ideas and interests are clearly identified, and research framed and conducted in such a way as to increase its chances of having a policy and practice impact.
Rationale and research objectives
The motivation for this body of research is to unpack the “so what?” question of PEA work on UHC, that refers to understanding and providing the empirical implications of the research carried out. Our starting point is the realization that, while the literature acknowledges the relevance and importance of exploring the political elements of UHC processes, one of the main challenges of PEA (and policy analysis, more broadly) for UHC and health financing reforms is that it might not always find immediate application for ongoing and future policy-making and policy implementation processes. It is often retrospective and targeted to research-oriented audiences with a methodological focus, while its uptake and usability by policy-makers and stakeholders is less explored. Stakeholder engagement, and in particular early and continuous stakeholder and research user engagement, is widely acknowledged by both researchers and funding organizations to be a central and essential element for successful research uptake [ 25 , 26 , 27 , 28 ]. With this study, we aimed to review the approaches with reference to stakeholder engagement during the research process adopted in the current published research on the political economy of UHC and health financing reforms, and the factors favouring (or hindering) uptake and usability of PEA work. In terms of thematic focus, we put particular attention to health financing reforms, since this element of UHC has been particularly emphasized in the literature [ 29 ]. We decided to focus our study on low- and middle-income countries (LMICs) for several reasons: Firstly, the literature on health policy and policy processes has historically focused on high-income countries (HIC); therefore, the aim of this paper is to deepen health policy analysis work in settings that may have been overlooked by this field of research [ 3 ]. With regard to UHC, and health reforms in general, LMICs express context-specific dynamics that differ from those of HICs; examples of these peculiar aspects may include a set of important political and policy actors (international actors—multilateral organizations such as the International Monetary Fund, the World Bank, WHO and the United Nations itself, bilateral donors, international nongovernmental organizations, and the more recently influential philanthropic organizations and public–private partnerships). In a context of high donor dependency, donors represent key stakeholders; donor rules shape the composition and structure of actors in the networks, which enables the entry and dissemination of new ideas and shifts in the overall balance of interest power, ultimately leading to policy change [ 30 ]. Global health actors usually have a high degree of influence on national health systems in LMICs, and the effects can be seen through different mechanisms, some with positive effects and others with negative effects. Examples of the latter could be the distortion of national health priorities [ 31 , 32 ], provoking conflicts among national actors over resources and national priorities [ 33 ], spreading oversimplified solutions [ 34 ], limiting the scope of policy debate [ 35 ] and weakening national capacity when trying to regulate unhealthy commodities [ 36 ]. Finally, LMICs are generally characterized by a higher degree of fragmentation of health systems compared to HICs (e.g., pluralism with a mix of private and public sector providers; HIV/AIDS initiatives and vertical programmes).
The specific research questions guiding this review are as follows:
What was the role of stakeholders during the different phases of the research process including (i) funding and commissioning of the research, (ii) design of the research, (iii) data collection stage, (iv) data analysis stage, (v) communication and dissemination of results, and (vi) monitoring and evaluation of research uptake?
What are the approaches to stakeholder engagement that researchers adopted during the research process which emerge from the literature?
Which factors/elements of these approaches favour uptake and usability of PEA work?
Study design
We conducted a narrative review looking at stakeholder engagement during the different phases of the research process in studies of UHC and health financing reforms, adopting a political economy framework. We adopted this study design because we considered it to be best suited to answer our research questions. However, as outlined in the PRISMA diagram in Annex 1, Fig. 4 , we proceed following systematic review guidelines [ 37 ] to ensure a systematic approach to our review. We complemented information extracted from the literature reviewed with a survey sent to the authors of the included studies.
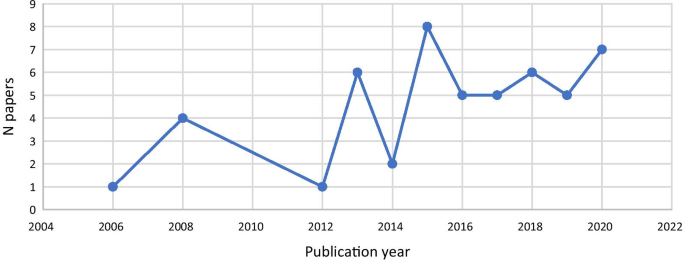
Publication years of included studies
Search strategy
After different attempts made to optimize the literature search, we used the following search terms: (“political economy”) AND ((“universal health coverage”) OR (“health financing”)), and relevant variations adapted to the different databases (i.e., Medline/PubMed, Scopus, Google Scholar, WHO IRIS, World Bank) we searched (see Box 2 ). We then compared the list of articles included in Rizvi et al. to ensure that our list was as comprehensive as possible.
Box 2. Databases searched and corresponding search strategies
Study selection and inclusion criteria.
In order to be included in the study, articles had to meet the following inclusion criteria:
Focuses on concepts relating to UHC and health financing reforms, including universal coverage/universal healthcare reforms, social health protection, social health insurance, health financing reforms, health expenditure/allocation, in line with Rizvi et al. [ 8 ].
Adopts a political economy perspective or framing, including PEA, policy analysis, policy-making analysis, policy implementation analysis, political settlements analysis, social network analysis, science–policy interface, as well as stakeholder mapping, stakeholder value network analysis, stakeholder impact analysis, in line with Rizvi et al. [ 8 ].
Any type of empirical study, including case studies, comparative case studies, qualitative studies and mixed-methods studies, from peer-reviewed and published grey literature. However, editorials, commentaries and papers presenting theoretical frameworks were excluded.
Setting: LMICs.
Language restrictions: English, French and Spanish.
Time frame: from 2005 (when universal coverage was cited in a World Health Assembly resolution [ 38 ]) to October 2020, in line with Rizvi et al. [ 8 ].
Title and abstract screening of the retrieved articles was conducted on an Excel sheet. After removal of duplicates, titles and abstracts were first screened by two reviewers (GL, MB) based on the above selection criteria. Studies were then either included for full-text screening, excluded, or marked as “maybe”. Studies marked as “maybe” were reviewed in a second round of screening by one of the reviewers, and any disagreement was resolved by consultation.
Data extraction
Qualitative, textual data were extracted from the documents identified into an Excel sheet, using a series of predefined themes/elements in relation to the possible approaches to/elements of stakeholder engagement at the different stages of the research process. Examples of the themes include engagement in research design, data collection and data analysis. In addition, descriptive elements of the study were also extracted to track information on, for example, topic of focus (e.g., aspect of UHC or health financing reform), country of relevance, authorship and type of study (Annex 2 ).
Survey of authors of selected studies
During the data extraction process, we noted that information on the research uptake process is often not included in the published articles, due to space constraints or because it was not considered relevant for the publication. Therefore, in order to collect additional information on stakeholder engagement undertaken during the research process, we also contacted the authors of the included studies via email and asked them to fill in an online survey (developed using Microsoft Forms) with questions regarding the process of stakeholder engagement and research uptake (for the survey questions, see Annex 4 ). We contacted all corresponding authors, although email addresses for 12 authors were returned as not valid. Out of the remaining 39 authors successfully contacted, we received 17 responses (44%).
Data synthesis and analysis
Basic bibliometric analysis was conducted for the documents found. The analysis of the findings adopted a narrative approach to the synthesis of the qualitative evidence. The information extracted was analysed using the themes/elements of the data extraction matrix and looking across documents [ 39 ]. This allowed identification of patterns or differences (as well as gaps) in the approaches to stakeholder engagement described in the existing literature. We also tried to understand the reasons behind the differences observed in stakeholder engagement, for example, whether they are linked to the funder, the research team, the specific topic being looked at or the findings (e.g., degree of sensitivity). For the survey component, we conducted qualitative thematic analysis, adding complementary and additional information to the data extraction matrix. Where possible, we triangulated the information provided in the survey with that included in the corresponding published article. Findings from the literature review and the authors’ survey were synthesized and are presented together in the section below.
Characteristics of included studies
After title, abstract and full text screening, 50 studies met the inclusion criteria (PRISMA flowchart provided in Annex 3 ). Included studies were published between 2005 and 2020. There was a steady increase in the number of publications over the years, with a peak in 2015 ( n = 8) (Fig. 1 ).
The majority of studies ( n = 36) focused on health financing reforms (e.g., social or national health insurance), and the remaining ( n = 14) on UHC in general. As per our inclusion criteria, all included studies were in LMICs (based on the World Bank classification [ 40 ]). The largest number of studies focused on Ghana ( n = 6), Mexico ( n = 5), India ( n = 5) and Thailand ( n = 4) (Fig. 2 ), potentially reflecting major successful UHC reforms that have taken place in those countries. Indeed, research focus often seemed to be related to a policy or reform that had been successfully introduced or implemented, and very few papers looked at unsuccessful or failed reforms (e.g., [ 41 ]).
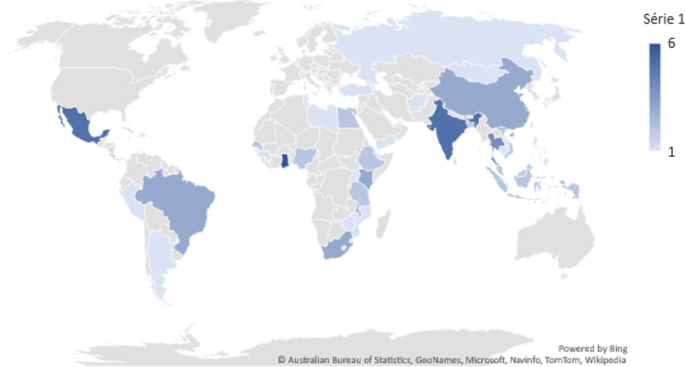
Countries under study in the included articles
Approaches to PEA and study methods
Papers included in the review adopted a variety of PEA and policy analysis approaches. While specific approaches and frameworks used differed, all aimed to understand the contextual factors and the dynamics among actors, ideas and institutions and the contestation of power and resources, with prominence given to some or all these elements. All studies included an empirical component (which was one of the inclusion criteria), so that many adopted a case study or a comparative case study design, using qualitative or mixed-methods approaches.
Most studies ( n = 48, 94%) adopted a retrospective approach, looking back at policy processes that had happened in the past and had reached a conclusion. Only three papers carried out a prospective analysis. They used this approach to understand bottlenecks and facilitators to achieve UHC and to propose ways to improve the efficiency of health financing. One of the papers drew on a panel discussion with relevant stakeholders (e.g., Ministry of Health and Finance, WHO representatives) [ 42 ]; the other two studies aimed to revise a resource allocation formula and its implementation [ 43 ] and to predict the role played by BRICS [Brazil, Russia, India, China, South Africa] countries in the UHC movement [ 44 ].
Stakeholder engagement in the research process
Researchers as stakeholders.
In an attempt to reflect on the role of researchers as stakeholders, and recognizing that the design and intention of a study might depend on researchers' values, ideologies, positionality, affiliation, role, and so on, we looked at the affiliation of the authors (first author only) in relation to the study setting. Our findings show that 54% ( n = 27) of first authors conducted the studies in a country different from their affiliation (of which 85% were affiliated with HIC institutions and studied a LMIC; the remaining were based in a LMIC institution and studied another LMIC), while for the rest of the first authors (46%, n = 23) the country under study corresponded to their country’s affiliation. Regarding the survey, out of 17 responses received, 11 authors were based in HIC institutions and led studies in LMICs. Five LMIC-affiliated authors conducted studies in their country of affiliation and one author in a different LMIC country. From this analysis it appears that more than a third (40%) of first authors and survey respondents conducted work in the same country as their affiliation. However, we do not have enough information on the authors’ backgrounds to fully unpack their position as stakeholders in the UHC arena. As a consequence, in the analysis below, we refer only to non-researcher stakeholders in our considerations. We further reflect on this point in the “Discussion” section.
Research funding
Funding was clearly reported for 30 papers (58%), but it was not detailed whether the funders were part of the political economy landscape being studied. Funding for the research seems to commonly originate from external funders, such as bilateral and multilateral development agencies (World Bank, United Kingdom’s Department for International Development [DFID], WHO), foundations (Rockefeller Foundation) and research funding organizations (International Development Research Centre [IDRC], Overseas Development Institute [ODI], European Union’s Seventh Framework Programme). Only a few were funded by local research centres or universities. There is no clear evidence of whether the research funders might have influenced the research processes and findings.
Research design
Engagement of stakeholders at the stage of research design is rarely reported in the literature we reviewed. Indeed, only one study, looking at the process of establishing the national health insurance scheme in Uganda, reported stakeholder engagement at the research design stage [ 45 ]. It was mentioned that the study was part of the work programme of the Ugandan health sector, defined and approved by the government, donors and all stakeholders, as indicated in the second National Health Policy and Health Sector Strategic and Investment plans.
However, the published literature may provide an underestimation of the stakeholders’ involvement at the design stage, as we obtained further information from the authors’ survey. Five respondents mentioned that either stakeholders were engaged in the design process by providing the conceptual framework for the study, or they initiated the research process by demanding specific evidence. In other cases, policy-makers were part of the research team and contributed to the research design, or the researchers were also policy-makers. Several authors in the studies reviewed acknowledged their role and participation in the policy reform of the country or being closely connected with the policy-making process.
Data collection
Several papers ( n = 22, 43%) did not include any stakeholders in the data collection process (i.e., only document review was conducted). The remaining ( n = 29, 57%) involved stakeholders, mainly as key informants being interviewed and/or sharing relevant documentation. We could not find evidence of stakeholders who were driving or leading the process of data collection.
The average number of stakeholders interviewed was 20. The actors involved in data collection were mostly government representatives or ministries (e.g., ministry of health, finance) and health workers/health system officials (Fig. 3 ). The actors least involved were civil society, researchers and the private sector, such as insurance companies.
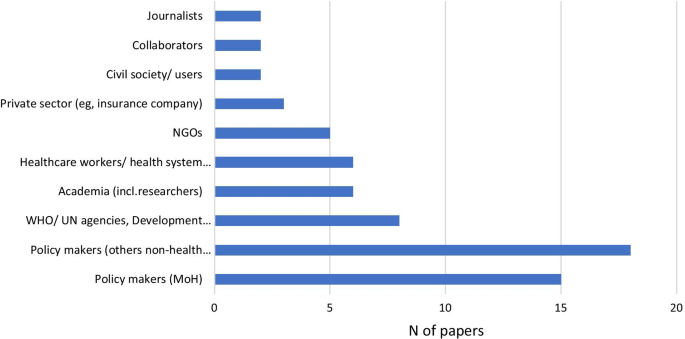
Main types of actors mentioned in the included papers that have been engaged in the data collection process
Data analysis
In terms of data analysis, reporting in the published literature might be somewhat underestimating the role of stakeholders for the interpretation and analysis of the data. Three papers reported the involvement of stakeholders for the validation of findings. For instance, with reference to social health insurance in Nigeria, Onoka et al. [ 46 ] mentioned that they conducted a post-study workshop where they presented the preliminary findings to study participants in order to discuss and validate the analysis and reach consensus on the results of the analysis. Similarly, Tangcharoensathien et al. [ 47 ] involved policy actors, civil society representatives and academia in the data analysis for their study in Thailand, while Musango et al. [ 42 ] based their study on a joint panel discussion with ministries, WHO Regional Office for Africa and others who participated in the meeting. In addition to this (unreported in the respective published documents), a few ( n = 3) authors confirmed in the survey that they had shared preliminary findings with stakeholders, who were able to provide feedback.
Knowledge translation: communication and dissemination of findings, and monitoring and evaluation of research uptake
Two studies, by Musango et al. and Twea et al., reported how findings were shared and disseminated [ 42 , 43 ]. In these studies, the dissemination was part of the discussions that took part as part of the research process. However, as for the elements above, these findings are likely to reflect an underreporting, potentially due to limited space in published papers or the information not being considered a priority for academic publications. The authors’ survey brought more information to our attention. For instance, several authors ( n = 11) reported that they disseminated results via workshops with policy-makers or health workers, via meetings (e.g., with parliament committee, municipal officers, panels) and via conferences on health financing. They also acknowledged that essential factors for successful policy uptake are early engagement with stakeholders, coproduction of research questions, and local partners establishing key linkages with stakeholders.
However, follow-up and monitoring of the usage of research findings and actual research uptake appear to be somewhat limited, even allowing for a time lag between publication and research uptake. Information based on the survey shows that some of the authors ( n = 7) were aware that findings were being used, for example by development partners (World Bank) or local parliaments, or they mentioned that the authors themselves held a position that allowed for uptake of research findings and recommendations.
Recommendations included in articles reviewed
Following the point above, it seems important to analyse the types of recommendations that were made in the studies reviewed—including looking into whether they were methodological or policy recommendations and whether they pointed to general lessons learned versus context-specific ones.
Almost all papers ( n = 43, 84%) included some type of recommendations grounded in the analysis conducted. Recommendations were made on research, such as operational or methodological aspects, as well as on policy- or governance-related aspects, or both types. Policy recommendations represented the majority of those included ( n = 35, 68%). Overall, the approach was general (rather than context-specific), referring for example to the need to strengthen political commitment and leadership, to adopt multisectoral approaches, or to improve resource allocation and integration of financing mechanisms to achieve UHC. Other recommendations, at the intersection of PEA methods and policy, underscored the importance of taking into account interests, ideologies and power of politically and economically influential groups, the contestation of ideas and consensus among social groups, and the need to consider contextual features, such as fragmentation of health systems and the implications for UHC, among others. Only a few papers ( n = 11, 21%) included context-specific recommendations.
Recommendations were mostly aimed at policy-makers and researchers adopting PEA approaches, with only a few papers explicitly targeting donors and international organizations.
This review aimed to shed light on stakeholder engagement at different stages of the research process related to PEA applied to UHC and health financing reforms. We found overall little evidence of systematic engagement of stakeholders in the research process, as detailed in the published papers. Unsurprisingly, it was revealed that stakeholder engagement is better achieved for some phases of the research process (i.e., data collection, mainly through key informant interviews), while other stages entail little or no engagement (such as research design and analysis). Stakeholders have a passive role as key informants, but do not seem to drive or lead the data collection process. Knowledge translation, such as active dissemination and communication of research findings, was described in some instances, while less was done in terms of monitoring research uptake in the long term—although there is an obvious bias in reporting on these elements, maybe due to the timing of the publication, which might predate the longer research uptake process. However, additional information from the authors’ survey did not radically change the picture.
There are different potential reasons for the varying engagement at different stages of the research process. These include the fact that PEA approaches require specific skills and knowledge (especially at the design and analysis stages) that are not always available to (non-researcher) stakeholders. Additionally, it is important to recognize that PEA often discusses sensitive topics around power dynamics, agendas and interests of those same stakeholders that should be engaged in the research process [ 15 ]. Such discussions can be challenging and therefore left to the margin or the end of the research, or not included in the published document. Our analysis also reflects on the fact that researchers are stakeholders themselves because of their ideas, values and ideologies around UHC. Researchers can be affiliated to (research) institutions in the same country that is being studied and, in some cases—although we lack full information on authors’ backgrounds to assess the frequency in our review—they might be closely involved in the reform process directly. Indeed, in such cases researchers’ and policy-makers’ positions can be multifaceted and blurred in practice. The blurriness or closeness between researcher and policy-making roles and the multiple role of stakeholders (in particular, policy-makers) as research participants, study subjects and research users pose specific challenges for PEA in terms of stakeholder engagement and research uptake, which we further describe in our empirical paper [ 15 , 48 ]. However, this scenario can also bring opportunities; for instance, researchers engaged in policy have access to useful and nuanced insight into the political processes, which could help to integrate different perspectives and learnings into their work. Several PEA approaches that are participatory in nature could be considered and, when possible, adopted. Despite the fact that these methods still require more theoretical and practical conceptualization, such approaches do follow the principles of coproduction in research [ 48 , 49 , 50 , 51 ]. In addition to these general principles, examples of specific methods, borrowed from other disciplines (such as system thinking and social sciences), that are participatory in nature and that can be perfectly suitable for conducting and complementing PEA research include participatory stakeholder mapping jointly conducted with stakeholders [ 52 ], participatory power mapping [ 53 ], group model-building [ 54 ], and mixed-methods approaches to social network analysis [ 55 , 56 ].
The concept of engagement also highlights the need to differentiate between stakeholders and “rights holders”, who is to consider as such and why, when, and how these two positions overlap. Particularly, when discussing governance and policy processes, a social equity approach and ownership of local knowledge can help to clarify the conceptualization of who becomes a stakeholder and who a rights holder. In line with the decolonialization discourse, clarifying the positionality of researchers and other stakeholders in the (co)production of context-specific knowledge can help in making progress towards equitable partnerships and engagement [ 57 ].
In addition to these challenges in effectively engaging with stakeholders for PEA of UHC and health financing reforms research, our analysis also acknowledges the general underreporting of stakeholder engagement in the published papers, which emerges from the survey that we conducted in parallel to the literature review. There is a sense that published literature is aimed at researchers and not directly at evidence users, and the information on engagement is therefore not included. However, parallel (unreported) processes for engagement and research uptake are sometimes put in place. The low reporting of such processes might be due to journal requirements in terms of word limit or to the timing of publication compared to research uptake processes, as well as to the sense that this information is not a priority for an academic publication. There might also be the consideration that journal articles or published research reports are not the best tool for disseminating findings to non-research audiences [ 58 ], so that there is a need to adopt other approaches (such as policy briefs, meetings) [ 59 ].
Similarly, recommendations tend to be aimed at other researchers and focus on the approach itself, stressing the relevance of policy analysis and PEA approaches to understanding UHC and health financing reforms, and highlighting methodological challenges and lessons learned in conducting this type of analysis. Context-specific recommendations are rarely included, as published research usually aims for generalizability of findings rather than context specificity [ 60 ]. This focus might create a challenge for effective research uptake, and again would require separate context-specific recommendations to be disseminated through other means.
Finally, this review highlighted that research tends to focus on “successful” reforms and to be retrospective in design. While this approach is useful for understanding what has happened and to draw lessons learned from positive cases, it also means that it might be too late to inform real-time policy processes and/or provide specific guidance for failed or stalled reform processes. The focus on successful reforms may also reflect a publication bias towards positive outcomes.
Approaches, factors and elements that might favour uptake and usability of PEA work
Our findings highlight the role of stakeholder engagement during the research process and identify some important challenges that are specific to stakeholder engagement (and research uptake) when using PEA for the analysis of UHC and health financing reforms. They also help identify specific approaches, factors and elements that might favour uptake and usability of PEA work. In particular, in line with the broader literature on the topic [ 38 , 39 ], responses from the survey stress that early engagement is key for successful policy uptake, together with coproduction of research questions. They also suggest the importance of local partners to reach out to stakeholders in a meaningful and effective way. However, there is limited evidence on the broader, more structural factors that impact stakeholder engagement, such as institutional factors, health policy research approaches and policy culture, and it is difficult to draw conclusions based on our findings. Other studies have identified personal contact, political willingness and trust among the factors that contribute to effective evidence use. Capacity-building initiatives can help to address the divide between health research and policy-makers and bridge these two worlds [ 58 ].
Additionally, the literature suggests that engaging in prospective PEA to examine policy-making and implementation processes as they happen would allow research to go beyond the current focus on stakeholder consensus on technical issues and has the potential to actively engage (some) stakeholders, and create an “epistemic community” around a shared, explicit understanding of the political dynamics that promote or hinder change, and thus influence policy change [ 61 , 62 , 63 , 64 , 65 ].
Finally, as coproduction of knowledge, stakeholder engagement and research uptake processes become increasingly embedded and critical parts of the research process [ 33 , 35 ], it is important that these are designed and reported on (including in the published articles) in a more systematic and standardized way, including and particularly for studies adopting PEA and policy analysis approaches.
Limitations
This is the first review that focused on understanding stakeholder engagement in the research process for studies of the political economy of UHC and health financing reforms. However, there are some limitations in our methodology and findings. This paper aimed to be an exploratory review, as neither the topic nor the aim lent itself to a systematic search and identification of the literature. Consequently, we might not have retrieved all relevant papers, and we did not assess the quality of included studies. However, care was taken during the search and selection stages to keep key words and criteria as broad as feasible, and to triangulate our included articles with a recent review on the same topic [ 8 ]. In addition, the purposeful search that we carried out helped to provide a snapshot of the literature and identify general tendencies and exceptional or outlying cases that help us draw some key findings. Despite this, we acknowledge that it is likely that there are studies of PEA of UHC and health financing reforms that remain outside the public domain, for example, because they were carried out by development partners before designing a programme or because of the sensitive nature of the topic. In fact, only a few studies were funded by local bodies, which may reflect a lack of local demand and/or too sensitive a nature for local funders to tackle these topics.
In other cases, some studies of PEA of UHC and health financing reforms, including specifically the details on stakeholder engagement that we are interested in, might have been left unpublished or under-/unreported in the available literature, or published without an explicit labelling of PEA. To address this issue, we complemented the literature review with an author survey, which undoubtedly helped to add relevant information that we may have missed otherwise. However, the response rate for the survey was relatively low, making our findings less robust and complete.
In recent years, there has been a growing awareness of the importance and relevance of political economy factors that influence policy-making and implementation processes for UHC and health financing reforms. This has led to increased attention to the study and the analysis of those factors, including adopting PEA and related approaches. However, while PEA offers analysis that is compelling to explain the politics of reforms, some questions remain open in terms of the policy relevance and usability of the lessons learned from PEA, considering ongoing and future reform processes and the need to inform actions or interventions ex ante. While stakeholder engagement is unlikely to be the only step or action required to ensure research uptake of findings, it is recognized as a critical one.
In this study, we reviewed the literature to describe whether, when and how stakeholders were involved in the research process for PEA of UHC and health financing reforms, and attempted to identify challenges and summarize the key learnings on what works and what could work for stakeholder engagement and research uptake in this area. Our analysis shows that, while stakeholder engagement and research uptake are always multifaceted concepts and complex processes, they are even more so when applied to PEA. In a companion empirical paper, we explore these issues from an empirical perspective based on our own experience of engaging stakeholders in a project involving PEA of UHC, and attempt to chart a way forward.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Brazil, Russia, India, China, South Africa
Community-based organizations
Department for International Development
European Union
International Development Research Centre
Low- and middle-income countries
Overseas Development Institute
Political economy analysis
- Universal health coverage
Kutzin J. Anything goes on the path to universal health coverage? Bull World Health Organ. 2012;90:867.
Article Google Scholar
Shiffman J. Political context and health financing reform. Heal Syst Reform. 2019;5(3):257–9. https://doi.org/10.1080/23288604.2019.1633894 .
Lucy Gilson et al. A health policy analysis reader: the politics of policy change in low- and middle-income countries. WHO; 2018.
Kelsall T, et al. Political settlements and pathways to universal health coverage. London: Overseas Development Institute; 2016.
Google Scholar
McDonnell A, Urrutia AF SE. Reaching universal health coverage: a political economy review of trends across 49 countries. London Overseas Dev Institute; 2019.
Chemouni B. The political path to universal health coverage: power, ideas and community-based health insurance in Rwanda. World Dev. 2018;106:87–98.
Lavers T. Towards Universal Health Coverage in Ethiopia’s ‘developmental state’? The political drivers of health insurance. Soc Sci Med. 2019;228:60–7.
Rizvi SS, Douglas R, Williams OD, Hill PS. The political economy of universal health coverage: a systematic narrative review. Health Policy Plan. 2020;35(3):364–72. https://doi.org/10.1093/heapol/czz171 .
Article PubMed Google Scholar
Sparkes SP, Bump JB, Özçelik EA, Kutzin J, Reich MR. Political economy analysis for health financing reform. Heal Syst Reform. 2019;5(3):183–94. https://doi.org/10.1080/23288604.2019.1633874 .
Reich MR. Political economy analysis for health. WHO Bull; 2019.
BSR (Business for Social Responsibility). Stakeholder Mapping; 2011.
Wonodi CB, Privor-Dumm L, Aina M, Pate AM, Reis R, Gadhoke P, et al. Using social network analysis to examine the decision-making process on new vaccine introduction in Nigeria. Health Policy Plan. 2012;27(Suppl_2):ii27-38. https://doi.org/10.1093/heapol/czs037 .
Tangcharoensathien V, Sirilak S, Sritara P, Patcharanarumol W, Lekagul A, Isaranuwatchai W, et al. Co-production of evidence for policies in Thailand: from concept to action. BMJ. 2021;372:m4669.
Gilson L, Barasa E, Brady L, Kagwanja N, Nxumalo N, Nzinga J, et al. Collective sensemaking for action: researchers and decision makers working collaboratively to strengthen health systems. BMJ. 2021;372:m4650.
Bello K, Bertone MP, et al. Engaging stakeholder in the political economy analysis of UHC: identifying challenges and a potential way ahead (report in progress); 2021.
Varvasovszky Z, Brugha R. A stakeholder analysis. Health Policy Plan. 2000;15(3):338–45. https://doi.org/10.1093/heapol/15.3.338 .
Article PubMed CAS Google Scholar
Walt G, Shiffman J, Schneider H, Murray SF, Brugha R, Gilson L. “Doing” health policy analysis: methodological and conceptual reflections and challenges. Health Policy Plan. 2008;23(5):308–17.
Lancaster K. Confidentiality, anonymity and power relations in elite interviewing: conducting qualitative policy research in a politicised domain. Int J Soc Res Methodol. 2017;20(1):93–103. https://doi.org/10.1080/13645579.2015.1123555 .
Dfid. Research uptake: a guide for DFID-funded research programmes; 2016. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/514977/Research_uptake_guidance.pdf .
Vanyoro KP, Hawkins K, Greenall M, Parry H, Keeru L. Local ownership of health policy and systems research in low-income and middle-income countries: a missing element in the uptake debate. BMJ Glob Heal. 2019;4(4):e001523. Available from: http://gh.bmj.com/content/4/4/e001523.abstract .
Nnaji CA, Wiysonge CS, Okeibunor JC, Malinga T, Adamu AA, Tumusiime P, et al. Implementation research approaches to promoting universal health coverage in Africa: a scoping review. BMC Health Serv Res. 2021;21(1):414. https://doi.org/10.1186/s12913-021-06449-6 .
Article PubMed PubMed Central Google Scholar
Reich MR, Harris J, Ikegami N, Maeda A, Cashin C, Araujo EC, et al. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387(10020):811–6. Available from: https://www.sciencedirect.com/science/article/pii/S0140673615600022 .
Lavers T, Hickey S. Conceptualising the politics of social protection expansion in low income countries: the intersection of transnational ideas and domestic politics. Int J Soc Welf. 2016;25(4):388–98. https://doi.org/10.1111/ijsw.12210 .
Greer SL, Méndez CA. Universal health coverage: a political struggle and governance challenge. Am J Public Health. 2015;105(Suppl 5):S637–9.
NIHR. Global Health Systems and Policy Research Awards Programme Development Awards single stage application form guidance; 2019. Available from: https://www.nihr.ac.uk/documents/nihr-global-health-systems-and-policy-research-awards-programme-development-awards-single-stage-application-form-guidance/21474 .
NIHR I. A resource guide for community engagement and involvement in global health research; 2019. Available https://www.nihr.ac.uk/documents/researchers/manage-your-funding/NIHR-Community-Engagement-Involvement-Resource-Guide-2019.pdf .
Kok MO, Gyapong JO, Wolffers I, Ofori-Adjei D, Ruitenberg J. Which health research gets used and why? An empirical analysis of 30 cases. Heal Res Policy Syst. 2016;14(1):36. https://doi.org/10.1186/s12961-016-0107-2 .
Boaz A, Hanney S, Borst R, O’Shea A, Kok M. How to engage stakeholders in research: design principles to support improvement. Heal Res Policy Syst. 2018;16(1):60. https://doi.org/10.1186/s12961-018-0337-6 .
Giedion U, Alfonso EA, Díaz Y. The impact of universal coverage schemes in the de-veloping world: a review of the existing evidence; 2013.
Shearer JC, Abelson J, Kouyaté B, Lavis JN, Walt G. Why do policies change? Institutions, interests, ideas and networks in three cases of policy reform. Health Policy Plan. 2016;31(9):1200–11. https://doi.org/10.1093/heapol/czw052 .
Shiffman J, Peter Schmitz H, Berlan D, Smith SL, Quissell K, Gneiting U, et al. The emergence and effectiveness of global health networks: findings and future research. Health Policy Plan. 2016;31(suppl_1):110–23. https://doi.org/10.1093/heapol/czw012 .
Storeng KT, Béhague DP. “Guilty until proven innocent”: the contested use of maternal mortality indicators in global health. Crit Public Health. 2017;27(2):163–76. https://doi.org/10.1080/09581596.2016.1259459 .
Kapilashrami A, McPake B. Transforming governance or reinforcing hierarchies and competition: examining the public and hidden transcripts of the Global Fund and HIV in India. Health Policy Plan. 2013;28(6):626–35. https://doi.org/10.1093/heapol/czs102 .
Ogden J, Walt G, Lush L. The politics of ‘branding’ in policy transfer: the case of DOTS for tuberculosis control. Soc Sci Med. 2003;57(1):179–88.
Rushton S, Williams OD. Frames, paradigms and power: global health policy-making under neoliberalism. Glob Soc. 2012;26(2):147–67. https://doi.org/10.1080/13600826.2012.656266 .
Hawkins B, Holden C. A corporate veto on health policy? Global constitutionalism and investor-state dispute settlement. J Health Polit Policy Law. 2016;41(5):969–95. https://doi.org/10.1215/03616878-3632203 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. https://doi.org/10.1186/s13643-021-01626-4 .
WHO. Sustainable health financing, universal coverage and social health insurance, WHA58.33; 2005.
Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. Sage, editor. London; 2003.
World Bank Country Classification; 2021.
Bertone MP, Wurie H, Samai M, Witter S. The bumpy trajectory of performance-based financing for healthcare in Sierra Leone: agency, structure and frames shaping the policy process. Global Health. 2018;14(1):99. https://doi.org/10.1186/s12992-018-0417-y .
Musango L, Orem JN, Elovainio R, Kirigia J. Moving from ideas to action - developing health financing systems towards universal coverage in Africa. BMC Int Health Hum Rights. 2012;12(1):30. https://doi.org/10.1186/1472-698X-12-30 .
Twea P, Manthalu G, Mohan S. Allocating resources to support universal health coverage: policy processes and implementation in Malawi. BMJ Glob Heal. 2020;5(8):e002766. Available from: http://gh.bmj.com/content/5/8/e002766.abstract .
Tediosi F, Finch A, Procacci C, Marten R, Missoni E. BRICS countries and the global movement for universal health coverage. Health Policy Plan. 2016;31(6):717–28. https://doi.org/10.1093/heapol/czv122 .
Basaza RK, O’Connell TS, Chapčáková I. Players and processes behind the national health insurance scheme: a case study of Uganda. BMC Health Serv Res. 2013;13(1):357. https://doi.org/10.1186/1472-6963-13-357 .
Onoka CA, Onwujekwe OE, Uzochukwu BS, Ezumah NN. Promoting universal financial protection: constraints and enabling factors in scaling-up coverage with social health insurance in Nigeria. Heal Res Policy Syst. 2013;11(1):20. https://doi.org/10.1186/1478-4505-11-20 .
Tangcharoensathien V, Patcharanarumol W, Kulthanmanusorn A, Saengruang N, Kosiyaporn H. The political economy of UHC reform in Thailand: lessons for low- and middle-income countries. Heal Syst Reform. 2019;5(3):195–208. https://doi.org/10.1080/23288604.2019.1630595 .
Ozano K, Khatri R. Reflexivity, positionality and power in cross-cultural participatory action research with research assistants in rural Cambodia. Educ Action Res. 2018;26(2):190–204. https://doi.org/10.1080/09650792.2017.1331860 .
Beran D, Pesantes MA, Berghusen MC, Hennig BJ, Jacobi J, Lazo-Porras M, et al. Rethinking research processes to strengthen co-production in low and middle income countries. BMJ. 2021;372:m4785. Available from: http://www.bmj.com/content/372/bmj.m4785.abstract .
Tembo D, Hickey G, Montenegro C, Chandler D, Nelson E, Porter K, et al. Effective engagement and involvement with community stakeholders in the co-production of global health research. BMJ. 2021;372:n178. Available from: http://www.bmj.com/content/372/bmj.n178.abstract .
Agyepong IA, Godt S, Sombie I, Binka C, Okine V, Ingabire M-G. Strengthening capacities and resource allocation for co-production of health research in low and middle income countries. BMJ. 2021;372:n166. Available from: http://www.bmj.com/content/372/bmj.n166.abstract .
Michael Reich PAC. A Guide to Applied Political Analysis for Health Reform; 2020.
Guevara-Hernandez F, et al. Participatory power mapping: a collective identification of development actors in a small cattle village of Chiapas, Mexico. Int J Technol Dev Stud. 2010;1:5.
Noubani A, Diaconu K, Ghandour L, El Koussa M, Loffreda G, Saleh S. A community–based system dynamics approach for understanding factors affecting mental Health and Health seeking behaviors in Beirut and Beqaa regions of Lebanon. Global Health. 2020;16(1):28. https://doi.org/10.1186/s12992-020-00556-5 .
Crossley N, Edwards G. Cases, mechanisms and the real: the theory and methodology of mixed-method social network analysis. Sociol Res Online. 2016;21(2):217–85. https://doi.org/10.5153/sro.3920 .
Hanneman RA, Mark R. Introduction to social network methods. Riverside: University of California, Riverside; 2005. (published in digital form at http://faculty.ucr.edu/~hanneman/ ).
Khan M, Abimbola S, Aloudat T, Capobianco E, Hawkes S, Rahman-Shepherd A. Decolonising global health in 2021: a roadmap to move from rhetoric to reform. BMJ Glob Heal. 2021;6(3):e005604. Available from: http://gh.bmj.com/content/6/3/e005604.abstract .
Hawkes S, Aulakh BK, Jadeja N, Jimenez M, Buse K, Anwar I, et al. Strengthening capacity to apply health research evidence in policy making: experience from four countries. Health Policy Plan. 2016;31(2):161–70.
Lorenc T, Tyner EF, Petticrew M, Duffy S, Martineau FP, Phillips G, et al. Cultures of evidence across policy sectors: systematic review of qualitative evidence. Eur J Public Health. 2014;24(6):1041–7. https://doi.org/10.1093/eurpub/cku038 .
Hawkins, Benjamin, Justin P. The ‘good governance’ of evidence in health policy; 2016.
Gilson L, McIntyre D. The interface between research and policy: experience from South Africa. Soc Sci Med. 2008;67(5):748–59. Available from: https://www.sciencedirect.com/science/article/pii/S0277953608000920
Oliver K, Innvar S, Lorenc T, Woodman J, Thomas J. A systematic review of barriers to and facilitators of the use of evidence by policymakers. BMC Health Serv Res. 2014;14(1):2. https://doi.org/10.1186/1472-6963-14-2 .
Buse K. Addressing the theoretical, practical and ethical challenges inherent in prospective health policy analysis. Health Policy Plan. 2008;23(5):351–60.
Journal Club Team TWCH. “Not just a journal club—it’s where the magic happens”: knowledge mobilization through co-production for health system development in the Western Cape Province, South Africa. Int J Heal Policy Manag. 2020; https://www.ijhpm.com/article_3874.html .
Ongolo-Zogo P, Lavis JN, Tomson G, Sewankambo NK. Assessing the influence of knowledge translation platforms on health system policy processes to achieve the health millennium development goals in Cameroon and Uganda: a comparative case study. Health Policy Plan. 2018;33(4):539–54.
Download references
This research was funded by the National Institute for Health Research (NIHR) through a Development Award of the NIHR Global Health Policy and Systems Research Programme (Project Reference: 130266), using UK aid from the United Kingdom Government to support global health research. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the United Kingdom Department of Health and Social Care.
Author information
Authors and affiliations.
Institute for Global Health and Development, Queen Margaret University, Edinburgh, UK
Giulia Loffreda, Sophie Witter & Maria Paola Bertone
Centre de Recherche en Reproduction Humaine et en Démographie, CERRHUD, Cotonou, Benin
Kéfilath Bello & Jean Paul Dossou
Department of Public Health, Institute of Tropical Medicine, Antwerp, Belgium
Kéfilath Bello, Joël Arthur Kiendrébéogo, Mohamed Ali Ag Ahmed & Jean Paul Dossou
Recherche Pour la Santé et le Développement, RESADE, Ouagadougou, Burkina Faso
Joël Arthur Kiendrébéogo
Heidelberg Institute of Global Health, Medical Faculty and University Hospital, Heidelberg University, Heidelberg, Germany
Department of Public Health, Health Sciences Training and Research Unit, University Joseph Ki-Zerbo, Ouagadougou, Burkina Faso
Research for Development International, Yaoundé, Cameroon
Isidore Selenou
École de Santé Publique de l’Université de Montréal, Montréal, Canada
Faculty of Medicine and Odontostomatology of Bamako, Bamako, Mali
Mohamed Ali Ag Ahmed
You can also search for this author in PubMed Google Scholar
Contributions
The research idea arose from a workshop held as part of the research consortium The Political economy of universal health coverage: building capacity and engagement of francophone Africa, of which all authors are members. All authors contributed to the design of the study and to the protocol. GL conducted the literature search, GL and MB screened the papers, analysed the data and wrote the draft manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Giulia Loffreda .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
See Fig. 4 .
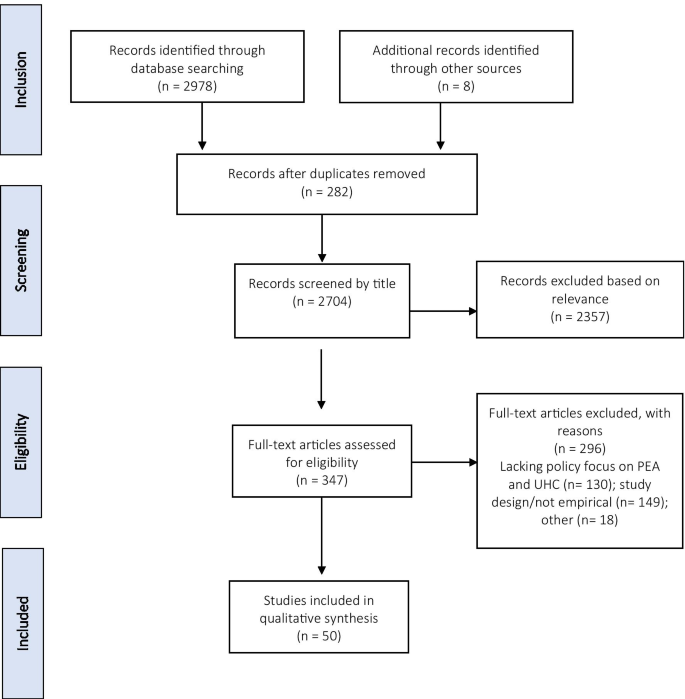
PRISMA flow diagram
See Table 1 .
See Table 2 .
Annex 4. Survey to authors on the process of stakeholder engagement
What was the role of stakeholders during the different phases of the research process? Please specify any of the below (and provide details, if you wish):
Funding/commissioning of the research
Design of the research and/or identification of the research question(s)
Data collection stage (for example, stakeholders were interviewed and/or contributed to documents to be reviewed)
Data analysis stage (for example, collaborative analysis, review/validation of early findings, etc.)
Communication/dissemination of results (for example, workshop or meetings to present and discuss results)
Monitoring and evaluation of research uptake (for example, feedback on use of research findings and recommendations).
Please provide details for those phases that you selected above.
Following the publication of this paper, have you conducted specific activities to facilitate the uptake of the findings? If yes, what type of activities and what type of stakeholders did you engage? Do you know what was the outcome of those research uptake activities (e.g., in terms of direct/indirect influence on policy and practice)?
Did you make any specific recommendations to the stakeholders that are specific to the setting of the study and are not included in the study itself?
Are you aware whether any of the recommendations or the findings of your study have been considered and/or used by stakeholders to shape policy and/or practice?
Based on your experience with this work, what do you think are the factors and approaches to stakeholder engagement that might favour uptake and usability of your PEA? Or conversely, the factors that hampered uptake and usability of your PEA or made its use challenging?
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Loffreda, G., Bello, K., Kiendrébéogo, J.A. et al. Political economy analysis of universal health coverage and health financing reforms in low- and middle-income countries: the role of stakeholder engagement in the research process. Health Res Policy Sys 19 , 143 (2021). https://doi.org/10.1186/s12961-021-00788-w
Download citation
Received : 05 July 2021
Accepted : 28 October 2021
Published : 11 December 2021
DOI : https://doi.org/10.1186/s12961-021-00788-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Political economy
- Health financing
- Stakeholder engagement
- Research uptake
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Medicina (Kaunas)

Universal Healthcare in the United States of America: A Healthy Debate
Gabriel zieff.
1 Department of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; ude.cnu.liame@rrekz (Z.Y.K.); [email protected] (L.S.)
Zachary Y. Kerr
Justin b. moore.
2 Department of Implementation Science, Wake Forest School of Medicine, Winston-Salem, NC 27157, USA; ude.htlaehekaw@eroomsuj
This commentary offers discussion on the pros and cons of universal healthcare in the United States. Disadvantages of universal healthcare include significant upfront costs and logistical challenges. On the other hand, universal healthcare may lead to a healthier populace, and thus, in the long-term, help to mitigate the economic costs of an unhealthy nation. In particular, substantial health disparities exist in the United States, with low socio–economic status segments of the population subject to decreased access to quality healthcare and increased risk of non-communicable chronic conditions such as obesity and type II diabetes, among other determinants of poor health. While the implementation of universal healthcare would be complicated and challenging, we argue that shifting from a market-based system to a universal healthcare system is necessary. Universal healthcare will better facilitate and encourage sustainable, preventive health practices and be more advantageous for the long-term public health and economy of the United States.
1. Introduction
Healthcare is one of the most significant socio–political topics in the United States (U.S.), and citizens currently rank “healthcare” as the most important issue when it comes to voting [ 1 ]. The U.S. has historically utilized a mixed public/private approach to healthcare. In this approach, citizens or businesses can obtain health insurance from private (e.g., Blue Cross Blue Shield, Kaiser Permanente) insurance companies, while individuals may also qualify for public (e.g., Medicaid, Medicare, Veteran’s Affairs), government-subsidized health insurance. In contrast, the vast majority of post-industrial, Westernized nations have used various approaches to provide entirely or largely governmentally subsidized, universal healthcare to all citizens regardless of socio–economic status (SES), employment status, or ability to pay. The World Health Organization defines universal healthcare as “ensuring that all people have access to needed health services (including prevention, promotion, treatment, rehabilitation and palliation) of sufficient quality to be effective while also ensuring that the use of these services does not expose the user the financial hardship” [ 2 ]. Importantly, the Obama-era passage of the Affordable Care Act (ACA) sought to move the U.S. closer to universal healthcare by expanding health coverage for millions of Americans (e.g., via Medicaid expansion, launch of health insurance marketplaces for private coverage) including for citizens across income levels, age, race, and ethnicity.
Differing versions of universal healthcare are possible. The United Kingdom’s National Health Services can be considered a fairly traditional version of universal healthcare with few options for, and minimal use of, privatized care [ 3 ]. On the other hand, European countries like Switzerland, the Netherlands, and Germany have utilized a blended system with substantial government and market-based components [ 4 , 5 ]. For example, Germany uses a multi-payer healthcare system in which subsidized health care is widely available for low-income citizens, yet private options—which provide the same quality and level of care as the subsidized option—are also available to higher income individuals. Thus, universal healthcare does not necessarily preclude the role of private providers within the healthcare system, but rather ensures that equity and effectiveness of care at population and individual levels are a reference and expectation for the system as a whole. In line with this, versions of universal healthcare have been implemented by countries with diverse political backgrounds (e.g., not limited to traditionally “socialist/liberal” countries), including some with very high degrees of economic freedom [ 6 , 7 ].
Determining the degree to which a nation’s healthcare is “universal” is complex and is not a “black and white” issue. For example, government backing, public will, and basic financing structure, among many other factors must be extensively considered. While an in-depth analysis of each of these factors is beyond the scope of this commentary, there are clear advantages and disadvantages to purely private, market-based, and governmental, universal approaches to healthcare, as well as for policies that lie somewhere in-between. This opinion piece will highlight arguments for and against universal healthcare in the U.S., followed by the authors’ stance on this issue and concluding remarks.
2. Argument against Universal Healthcare
Though the majority of post-industrial Westernized nations employ a universal healthcare model, few—if any—of these nations are as geographically large, populous, or ethnically/racially diverse as the U.S. Different regions in the U.S. are defined by distinct cultural identities, citizens have unique religious and political values, and the populace spans the socio–economic spectrum. Moreover, heterogenous climates and population densities confer different health needs and challenges across the U.S. [ 8 ]. Thus, critics of universal healthcare in the U.S. argue that implementation would not be as feasible—organizationally or financially—as other developed nations [ 9 ]. There is indeed agreement that realization of universal healthcare in the U.S. would necessitate significant upfront costs [ 10 ]. These costs would include those related to: (i) physical and technological infrastructural changes to the healthcare system, including at the government level (i.e., federal, state, local) as well as the level of the provider (e.g., hospital, out-patient clinic, pharmacy, etc.); (ii) insuring/treating a significant, previously uninsured, and largely unhealthy segment of the population; and (iii) expansion of the range of services provided (e.g., dental, vision, hearing) [ 10 ].
The cost of a universal healthcare system would depend on its structure, benefit levels, and extent of coverage. However, most proposals would entail increased federal taxes, at least for higher earners [ 4 , 11 , 12 ]. One proposal for universal healthcare recently pushed included options such as a 7.5% payroll tax plus a 4% income tax on all Americans, with higher-income citizens subjected to higher taxes [ 13 ]. However, outside projections suggest that these tax proposals would not be sufficient to fund this plan. In terms of the national economic toll, cost estimations of this proposal range from USD 32 to 44 trillion across 10 years, while deficit estimations range from USD 1.1 to 2.1 trillion per year [ 14 ].
Beyond individual and federal costs, other common arguments against universal healthcare include the potential for general system inefficiency, including lengthy wait-times for patients and a hampering of medical entrepreneurship and innovation [ 3 , 12 , 15 , 16 ]. Such critiques are not new, as exemplified by rhetoric surrounding the Clinton Administration’s Health Security Act which was labeled as “government meddling” in medical care that would result in “big government inefficiency” [ 12 , 15 ]. The ACA has been met with similar resistance and bombast (e.g., the “repeal and replace” right-leaning rallying cry) as a result of perceived inefficiency and unwanted government involvement. As an example of lengthy wait times associated with universal coverage, in 2017 Canadians were on waiting lists for an estimated 1,040,791 procedures, and the median wait time for arthroplastic surgery was 20–52 weeks [ 17 ]. Similarly, average waiting time for elective hospital-based care in the United Kingdom is 46 days, while some patients wait over a year (3). Increased wait times in the U.S. would likely occur—at least in the short term—as a result of a steep rise in the number of primary and emergency care visits (due to eliminating the financial barrier to seek care), as well as general wastefulness, inefficiency, and disorganization that is often associated with bureaucratic, government-run agencies.
3. Argument for Universal Healthcare
Universal healthcare in the U.S., which may or may not include private market-based options, offer several noteworthy advantages compared to exclusive systems with inequitable access to quality care including: (i) addressing the growing chronic disease crisis; (ii) mitigating the economic costs associated with said crisis; (iii) reducing the vast health disparities that exist between differing SES segments of the population; and (iv) increasing opportunities for preventive health initiatives [ 18 , 19 , 20 , 21 ]. Perhaps the most striking advantage of a universal healthcare system in the U.S. is the potential to address the epidemic level of non-communicable chronic diseases such as cardiovascular diseases, type II diabetes, and obesity, all of which strain the national economy [ 22 , 23 ]. The economic strain associated with an unhealthy population is particularly evident among low SES individuals. Having a low SES is associated with many unfavorable health determinants, including decreased access to, and quality of health insurance which impact health outcomes and life expectancies [ 24 ]. Thus, the low SES segments of the population are in most need of accessible, quality health insurance, and economic strain results from an unhealthy and uninsured low SES [ 25 , 26 ]. For example, diabetics with low SES have a greater mortality risk than diabetics with higher SES, and the uninsured diabetic population is responsible for 55% more emergency room visits each year than their insured diabetic counterparts [ 27 , 28 ]. Like diabetes, hypertension—the leading risk factor for death worldwide [ 29 ], has a much higher prevalence among low SES populations [ 30 ]. It is estimated that individuals with uncontrolled hypertension have more than USD 2000 greater annual healthcare costs than their normotensive counterparts [ 31 ]. Lastly, the incidence of obesity is also much greater among low SES populations [ 32 ]. The costs of obesity in the U.S., when limited to lost productivity alone, have been projected to equate to USD 66 billion annually [ 33 ]. Accessible, affordable healthcare may enable earlier intervention to prevent—or limit risk associated with—non-communicable chronic diseases, improve the overall public health of the U.S., and decrease the economic strain associated with an unhealthy low-SES.
Preventive Initiatives within A Universal Healthcare Model
Beyond providing insurance coverage for a substantial, uninsured, and largely unhealthy segment of society—and thereby reducing disparities and unequal access to care among all segments of the population—there is great potential for universal healthcare models to embrace value-based care [ 4 , 20 , 34 ]. Value-based care can be thought of as appropriate and affordable care (tackling wastes), and integration of services and systems of care (i.e., hospital, primary, public health), including preventive care that considers the long-term health and economy of a nation [ 34 , 35 ]. In line with this, the ACA has worked in parallel with population-level health programs such as the Healthy People Initiative by targeting modifiable determinants of health including physical activity, obesity, and environmental quality, among others [ 36 ]. Given that a universal healthcare plan would force the government to pay for costly care and treatments related to complications resulting from preventable, non-communicable chronic diseases, the government may be more incentivized to (i) offer primary prevention of chronic disease risk prior to the onset of irreversible complications, and (ii) promote wide-spread preventive efforts across multiple societal domains. It is also worth acknowledging here that the national public health response to the novel Coronavirus-19 virus is a salient and striking contemporary example of a situation in which there continues to be a need to expeditiously coordinate multiple levels of policy, care, and prevention.
Preventive measures lessen costs associated with an uninsured and/or unhealthy population [ 37 ]. For example, investing USD 10 per person annually in community-based programs aimed at combatting physical inactivity, poor nutrition, and smoking in the U.S. could save more than USD 16 billion annually within five years, equating to a return of USD 5.60 for every dollar spent [ 38 ]. Another recent analysis suggests that if 18% more U.S. elementary-school children participated in 25 min of physical activity three times per week, savings attributed to medical costs and productivity would amount to USD 21.9 billion over their lifetime [ 39 ]. Additionally, simple behavioral changes can have major clinical implications. For example, simply brisk walking for 30 min per day (≥15 MET-hours/week) has been associated with a 50% reduction in type II diabetes [ 40 ]. While universal healthcare does not necessarily mean that health policies supporting prevention will be enacted, it may be more likely to promote healthy (i) lifestyle behaviors (e.g., physical activity), (ii) environmental factors (e.g., safe, green spaces in low and middle-income communities), and (iii.) policies (e.g., banning sweetened beverages in public schools) compared to a non-inclusive system [ 34 , 35 , 36 ].
Nordic nations provide an example of inclusive healthcare coupled with multi-layered preventive efforts [ 41 ]. In this model, all citizens are given the same comprehensive healthcare while social determinants of health are targeted. This includes “mobilizing and coordinating a large number of players in society,” which encourages cooperation among “players” including municipal political bodies, voluntary organizations, and educational institutions [ 41 ]. Developmental and infrastructural contributions from multiple segments of society to a healthcare system may also better encourage government accountability compared to a system in which a select group of private insurers and citizens are the only “stakeholders.” Coordinated efforts on various non-insurance-related fronts have focused on obesity, mental health, and physical activity [ 41 ]. Such coordinated efforts within the Nordic model have translated to positive health outcomes. For example, the Healthcare Access and Quality (HAQ) Index provides an overall score of 0–100 (0 being the worst) for healthcare access and quality across 195 countries and reflects rates of 32 preventable causes of death. Nordic nations had an average HAQ score of 95.4, with four of the five nations achieving scores within the top 10 worldwide [ 42 ]. Though far more heterogenous compared to Nordic nations, (e.g., culturally, geographically, racially, etc.), the U.S. had a score of 89 (29th overall) [ 42 ]. To provide further context, other industrialized nations, which are more comparable to the U.S. than Nordic nations, also ranked higher than the U.S. including Germany (92, 19th overall), Canada (94, 14th overall), Switzerland (96, 7th overall), and the Netherlands (96, 3rd overall) [ 42 ].
4. Conclusions
Non-inclusive, inequitable systems limit quality healthcare access to those who can afford it or have employer-sponsored insurance. These policies exacerbate health disparities by failing to prioritize preventive measures at the environmental, policy, and individual level. Low SES segments of the population are particularly vulnerable within a healthcare system that does not prioritize affordable care for all or address important determinants of health. Failing to prioritize comprehensive, affordable health insurance for all members of society and straying further from prevention will harm the health and economy of the U.S. While there are undoubtedly great economic costs associated with universal healthcare in the U.S., we argue that in the long-run, these costs will be worthwhile, and will eventually be offset by a healthier populace whose health is less economically burdensome. Passing of the Obama-era ACA was a positive step forward as evident by the decline in uninsured U.S. citizens (estimated 7–16.4 million) and Medicare’s lower rate of spending following the legislation [ 43 ]. The U.S. must resist the current political efforts to dislodge the inclusive tenets of the Affordable Care Act. Again, this is not to suggest that universal healthcare will be a cure-all, as social determinants of health must also be addressed. However, addressing these determinants will take time and universal healthcare for all U.S. citizens is needed now. Only through universal and inclusive healthcare will we be able to pave an economically sustainable path towards true public health.
Author Contributions
Conceptualization, G.Z., Z.Y.K., J.B.M., and L.S.; writing-original draft preparation, G.Z.; writing-review and editing, Z.Y.K., J.B.M., and L.S.; supervision, L.S. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
VIDEO
COMMENTS
Literature showed that modern healthcare access and coverage were in extension stages during the PHC era flagshipped with "health for all (HFA)", prolifically achieving vaccination, communicable disease control, and the use of modern contraceptive methods. ... Historical review; Universal health coverage, health, healthcare access, equity ...
INTRODUCTION. In recent years, there has been an increased push for universal health coverage (UHC) at the global level. UHC is defined by the World Health Organization (WHO) as "ensuring that all people obtain the health services they need, of good quality, without suffering financial hardship when paying for them" [].This concept was initially created in 1883 after Germany introduced ...
A scoping review of the studies on UHC and its dimensions is crucial to map and characterize the existing studies towards UHC. This will help to identify key concepts, gaps in the research, and types and sources of evidence to inform practice, policymaking, and research [ 11 ]. The goals of this scoping review towards universality of UHC were ...
Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries. The primary objective of this scoping review was to summarize the existing ...
Background: The Universal Health Coverage (UHC) is a very important and effective policy in the health system of countries worldwide.Using the experiences and learning from the best practices of successful countries in the UHC can be very helpful. Therefore, the aim of the present study is to provide a scoping review of successful global interventions and practices in achieving UHC.
Universal health coverage (UHC) has been acknowledged as a priority goal of every health system [1-5].The importance of this goal is reflected in the consistent calls by the World Health Organization (WHO) for its member states to implement pooled prepaid health care financing systems that promote access to quality health care and provide households with the needed protection from the ...
According to our literature review, we identified 15 articles that discussed the role of universal health coverage (UHC) on countries' health system performance in times of public health crises, none of which provided quantitative evidence to substantiate UHC's potential role in building health system resilience against external shocks like ...
Abstract and Figures. Introduction Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the ...
Abstract and Figures. Background The progress of Universal health coverage (UHC) is measured using tracer indicators of key interventions, which have been implemented in healthcare system. UHC is ...
39 Universal health coverage (UHC) is a multi-dimensional concept that includes population coverage, services coverage. 40 and financial protection as its building blocks, as well as all individuals and communities (equity), quality, and types of. 41 health services in its integrated definition (1).
Discussion: The literature presents UHC as a multi-dimensional concept, operationalized in terms of universal population coverage, universal financial protection, and universal access to quality health care, anchored on the basis of health care as an international legal obligation grounded in international human rights laws. As a legal concept ...
Resilient health system (RHS) is crucial to achieving universal health coverage (UHC) and health security. However, little is known about strategies towards RHS to improve UHC and health security. This systematic review aims to synthesise the literature to understand approaches to build RHS toward UHC and health security. A systematic search was conducted including studies published from 01 ...
Discussion. The literature presents UHC as a multi-dimensional concept, operationalized in terms of universal population coverage, universal financial protection, and universal access to quality health care, anchored on the basis of health care as an international legal obligation grounded in international human rights laws.
Article PDF Available Literature Review. Universal healthcare coverage, patients' rights, and nurse-patient communication: a critical review of the evidence. March 2022; BMC Nursing 21(54)
A scoping review of the studies on UHC and its dimensions is crucial to map and character-ize the existing studies towards UHC. This will help to identify key concepts, gaps in the research, and types and sources of evidence to inform practice, policymaking, and research [11].
Despite the limitations of a critical review methodology, some scientific literature review principles were implemented in this study. The paper originated from the first author's doctoral comprehensive exams organized in February 2021. ... affirming the right to universal access to health care for all" [13, p. 18]. This assertion ...
The UN has declared universal health coverage an urgent global goal. Efforts to achieve this goal have been supported by rigorous research on the scientific, technical, and administrative aspects of health systems design. Yet a substantial portion of the world's population does not have access to essential health services. There is growing recognition that achieving universal health coverage ...
Article PDF Available Literature Review. ... Universal health coverage (UHC) means that all people can access health services of good quality without experiencing financial hardship. Three health ...
Progress towards universal health coverage (UHC) is an inherently political process. Political economy analysis (PEA) is gaining momentum as a tool to better understand the role of the political and economic dimensions in shaping and achieving UHC in different contexts. Despite the acknowledged importance of actors and stakeholders in political economy considerations, their role in the PEA ...
Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries.
2. Argument against Universal Healthcare. Though the majority of post-industrial Westernized nations employ a universal healthcare model, few—if any—of these nations are as geographically large, populous, or ethnically/racially diverse as the U.S. Different regions in the U.S. are defined by distinct cultural identities, citizens have unique religious and political values, and the populace ...