

Conducting research during the COVID-19 pandemic
Advice from psychological researchers on protecting participants, animals and research plans.

COVID-19 is not just altering everyday life; it’s also upending psychological research. As universities and colleges across the country go virtual, researchers are scrambling to protect their human participants and animal subjects, their scholarship and their careers.
“The research that will be affected first are studies that involve bringing groups of people together in close proximity,” says Jeff Zacks, PhD, of Washington University in St. Louis, who chairs APA’s Board of Scientific Affairs (BSA). “But this is going to slow everybody down for 2020.”
To mitigate the impact, Zacks, his fellow BSA members and other experts offer the following advice.
Prepare to work remotely
Check in with your program officer, modify your research and analysis, protect your human participants and animal subjects, cross-train staff, maintain communication with your team, do the things that you never have time for, support junior colleagues, keep things in perspective.
For information about how the pandemic will affect existing and future research awards and other information about National Institutes of Health (NIH) research, see the NIH FAQ and NIH’s information for applicants and recipients of NIH funding .
For similar information about National Science Foundation (NSF) research, see the NSF FAQ .
The Council on Government Relations is compiling a list of institutional and agency responses to the pandemic.
Have an idea for research about preventing or treating COVID-19? See NSF’s Dear Colleague Letter about how to submit a research proposal.
Additional Information
- Psychologist leads innovative approach to tackle psychological toll of COVID-19
- COVID-19 isn’t just a danger to older people’s physical health
Contact APA Office of Public Affairs
You may also like.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 16 June 2020
COVID-19 impact on research, lessons learned from COVID-19 research, implications for pediatric research
- Debra L. Weiner 1 , 2 ,
- Vivek Balasubramaniam 3 ,
- Shetal I. Shah 4 &
- Joyce R. Javier 5 , 6
on behalf of the Pediatric Policy Council
Pediatric Research volume 88 , pages 148–150 ( 2020 ) Cite this article
147k Accesses
81 Citations
19 Altmetric
Metrics details
The COVID-19 pandemic has resulted in unprecedented research worldwide. The impact on research in progress at the time of the pandemic, the importance and challenges of real-time pandemic research, and the importance of a pediatrician-scientist workforce are all highlighted by this epic pandemic. As we navigate through and beyond this pandemic, which will have a long-lasting impact on our world, including research and the biomedical research enterprise, it is important to recognize and address opportunities and strategies for, and challenges of research and strengthening the pediatrician-scientist workforce.
The first cases of what is now recognized as SARS-CoV-2 infection, termed COVID-19, were reported in Wuhan, China in December 2019 as cases of fatal pneumonia. By February 26, 2020, COVID-19 had been reported on all continents except Antarctica. As of May 4, 2020, 3.53 million cases and 248,169 deaths have been reported from 210 countries. 1
Impact of COVID-19 on ongoing research
The impact on research in progress prior to COVID-19 was rapid, dramatic, and no doubt will be long term. The pandemic curtailed most academic, industry, and government basic science and clinical research, or redirected research to COVID-19. Most clinical trials, except those testing life-saving therapies, have been paused, and most continuing trials are now closed to new enrollment. Ongoing clinical trials have been modified to enable home administration of treatment and virtual monitoring to minimize participant risk of COVID-19 infection, and to avoid diverting healthcare resources from pandemic response. In addition to short- and long-term patient impact, these research disruptions threaten the careers of physician-scientists, many of whom have had to shift efforts from research to patient care. To protect research in progress, as well as physician-scientist careers and the research workforce, ongoing support is critical. NIH ( https://grants.nih.gov/policy/natural-disasters/corona-virus.htm ), PCORI ( https://www.pcori.org/funding-opportunities/applicant-and-awardee-faqs-related-covid-19 ), and other funders acted swiftly to provide guidance on proposal submission and award management, and implement allowances that enable grant personnel to be paid and time lines to be relaxed. Research institutions have also implemented strategies to mitigate the long-term impact of research disruptions. Support throughout and beyond the pandemic to retain currently well-trained research personnel and research support teams, and to accommodate loss of research assets, including laboratory supplies and study participants, will be required to complete disrupted research and ultimately enable new research.
In the long term, it is likely that the pandemic will force reallocation of research dollars at the expense of research areas funded prior to the pandemic. It will be more important than ever for the pediatric research community to engage in discussion and decisions regarding prioritization of funding goals for dedicated pediatric research and meaningful inclusion of children in studies. The recently released 2020 National Institute of Child Health and Development (NICHD) strategic plan that engaged stakeholders, including scientists and patients, to shape the goals of the Institute, will require modification to best chart a path toward restoring normalcy within pediatric science.
COVID-19 research
This global pandemic once again highlights the importance of research, stable research infrastructure, and funding for public health emergency (PHE)/disaster preparedness, response, and resiliency. The stakes in this worldwide pandemic have never been higher as lives are lost, economies falter, and life has radically changed. Ultimate COVID-19 mitigation and crisis resolution is dependent on high-quality research aligned with top priority societal goals that yields trustworthy data and actionable information. While the highest priority goals are treatment and prevention, biomedical research also provides data critical to manage and restore economic and social welfare.
Scientific and technological knowledge and resources have never been greater and have been leveraged globally to perform COVID-19 research at warp speed. The number of studies related to COVID-19 increases daily, the scope and magnitude of engagement is stunning, and the extent of global collaboration unprecedented. On January 5, 2020, just weeks after the first cases of illness were reported, the genetic sequence, which identified the pathogen as a novel coronavirus, SARS-CoV-2, was released, providing information essential for identifying and developing treatments, vaccines, and diagnostics. As of May 3, 2020 1133 COVID-19 studies, including 148 related to hydroxychloroquine, 13 to remdesivir, 50 to vaccines, and 100 to diagnostic testing, were registered on ClinicalTrials.gov, and 980 different studies on the World Health Organization’s International Clinical Trials Registry Platform (WHO ICTRP), made possible, at least in part, by use of data libraries to inform development of antivirals, immunomodulators, antibody-based biologics, and vaccines. On April 7, 2020, the FDA launched the Coronavirus Treatment Acceleration Program (CTAP) ( https://www.fda.gov/drugs/coronavirus-covid-19-drugs/coronavirus-treatment-acceleration-program-ctap ). On April 17, 2020, NIH announced a partnership with industry to expedite vaccine development ( https://www.nih.gov/news-events/news-releases/nih-launch-public-private-partnership-speed-covid-19-vaccine-treatment-options ). As of May 1, 2020, remdesivir (Gilead), granted FDA emergency use authorization, is the only approved therapeutic for COVID-19. 2
The pandemic has intensified research challenges. In a rush for data already thousands of manuscripts, news reports, and blogs have been published, but to date, there is limited scientifically robust data. Some studies do not meet published clinical trial standards, which now include FDA’s COVID-19-specific standards, 3 , 4 , 5 and/or are published without peer review. Misinformation from studies diverts resources from development and testing of more promising therapeutic candidates and has endangered lives. Ibuprofen, initially reported as unsafe for patients with COVID-19, resulted in a shortage of acetaminophen, endangering individuals for whom ibuprofen is contraindicated. Hydroxychloroquine initially reported as potentially effective for treatment of COVID-19 resulted in shortages for patients with autoimmune diseases. Remdesivir, in rigorous trials, showed decrease in duration of COVID-19, with greater effect given early. 6 Given the limited availability and safety data, the use outside clinical trials is currently approved only for severe disease. Vaccines typically take 10–15 years to develop. As of May 3, 2020, of nearly 100 vaccines in development, 8 are in trial. Several vaccines are projected to have emergency approval within 12–18 months, possibly as early as the end of the year, 7 still an eternity for this pandemic, yet too soon for long-term effectiveness and safety data. Antibody testing, necessary for diagnosis, therapeutics, and vaccine testing, has presented some of the greatest research challenges, including validation, timing, availability and prioritization of testing, interpretation of test results, and appropriate patient and societal actions based on results. 8 Relaxing physical distancing without data regarding test validity, duration, and strength of immunity to different strains of COVID-19 could have catastrophic results. Understanding population differences and disparities, which have been further exposed during this pandemic, is critical for response and long-term pandemic recovery. The “Equitable Data Collection and Disclosure on COVID-19 Act” calls for the CDC (Centers for Disease Control and Prevention) and other HHS (United States Department of Health & Human Services) agencies to publicly release racial and demographic information ( https://bass.house.gov/sites/bass.house.gov/files/Equitable%20Data%20Collection%20and%20Dislosure%20on%20COVID19%20Act_FINAL.pdf )
Trusted sources of up-to-date, easily accessible information must be identified (e.g., WHO https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov , CDC https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html , and for children AAP (American Academy of Pediatrics) https://www.aappublications.org/cc/covid-19 ) and should comment on quality of data and provide strategies and crisis standards to guide clinical practice.
Long-term, lessons learned from research during this pandemic could benefit the research enterprise worldwide beyond the pandemic and during other PHE/disasters with strategies for balancing multiple novel approaches and high-quality, time-efficient, cost-effective research. This challenge, at least in part, can be met by appropriate study design, collaboration, patient registries, automated data collection, artificial intelligence, data sharing, and ongoing consideration of appropriate regulatory approval processes. In addition, research to develop and evaluate innovative strategies and technologies to improve access to care, management of health and disease, and quality, safety, and cost effectiveness of care could revolutionize healthcare and healthcare systems. During PHE/disasters, crisis standards for research should be considered along with ongoing and just-in-time PHE/disaster training for researchers willing to share information that could be leveraged at time of crisis. A dedicated funded core workforce of PHE/disaster researchers and funded infrastructure should be considered, potentially as a consortium of networks, that includes physician-scientists, basic scientists, social scientists, mental health providers, global health experts, epidemiologists, public health experts, engineers, information technology experts, economists and educators to strategize, consult, review, monitor, interpret studies, guide appropriate clinical use of data, and inform decisions regarding effective use of resources for PHE/disaster research.
Differences between adult and pediatric COVID-19, the need for pediatric research
As reported by the CDC, from February 12 to April 2, 2020, of 149,760 cases of confirmed COVID-19 in the United States, 2572 (1.7%) were children aged <18 years, similar to published rates in China. 9 Severe illness has been rare. Of 749 children for whom hospitalization data is available, 147 (20%) required hospitalization (5.7% of total children), and 15 of 147 required ICU care (2.0%, 0.58% of total). Of the 95 children aged <1 year, 59 (62%) were hospitalized, and 5 (5.3%) required ICU admission. Among children there were three deaths. Despite children being relatively spared by COVID-19, spread of disease by children, and consequences for their health and pediatric healthcare are potentially profound with immediate and long-term impact on all of society.
We have long been aware of the importance and value of pediatric research on children, and society. COVID-19 is no exception and highlights the imperative need for a pediatrician-scientist workforce. Understanding differences in epidemiology, susceptibility, manifestations, and treatment of COVID-19 in children can provide insights into this pathogen, pathogen–host interactions, pathophysiology, and host response for the entire population. Pediatric clinical registries of COVID-infected, COVID-exposed children can provide data and specimens for immediate and long-term research. Of the 1133 COVID-19 studies on ClinicalTrials.gov, 202 include children aged ≤17 years. Sixty-one of the 681 interventional trials include children. With less diagnostic testing and less pediatric research, we not only endanger children, but also adults by not identifying infected children and limiting spread by children.
Pediatric considerations and challenges related to treatment and vaccine research for COVID-19 include appropriate dosing, pediatric formulation, and pediatric specific short- and long-term effectiveness and safety. Typically, initial clinical trials exclude children until safety has been established in adults. But with time of the essence, deferring pediatric research risks the health of children, particularly those with special needs. Considerations specific to pregnant women, fetuses, and neonates must also be addressed. Childhood mental health in this demographic, already struggling with a mental health pandemic prior to COVID-19, is now further challenged by social disruption, food and housing insecurity, loss of loved ones, isolation from friends and family, and exposure to an infodemic of pandemic-related information. Interestingly, at present mental health visits along with all visits to pediatric emergency departments across the United States are dramatically decreased. Understanding factors that mitigate and worsen psychiatric symptoms should be a focus of research, and ideally will result in strategies for prevention and management in the long term, including beyond this pandemic. Social well-being of children must also be studied. Experts note that the pandemic is a perfect storm for child maltreatment given that vulnerable families are now socially isolated, facing unemployment, and stressed, and that children are not under the watch of mandated reporters in schools, daycare, and primary care. 10 Many states have observed a decrease in child abuse reports and an increase in severity of emergency department abuse cases. In the short term and long term, it will be important to study the impact of access to care, missed care, and disrupted education during COVID-19 on physical and cognitive development.
Training and supporting pediatrician-scientists, such as through NIH physician-scientist research training and career development programs ( https://researchtraining.nih.gov/infographics/physician-scientist ) at all stages of career, as well as fostering research for fellows, residents, and medical students willing to dedicate their research career to, or at least understand implications of their research for, PHE/disasters is important for having an ongoing, as well as a just-in-time surge pediatric-focused PHE/disaster workforce. In addition to including pediatric experts in collaborations and consortiums with broader population focus, consideration should be given to pediatric-focused multi-institutional, academic, industry, and/or government consortiums with infrastructure and ongoing funding for virtual training programs, research teams, and multidisciplinary oversight.
The impact of the COVID-19 pandemic on research and research in response to the pandemic once again highlights the importance of research, challenges of research particularly during PHE/disasters, and opportunities and resources for making research more efficient and cost effective. New paradigms and models for research will hopefully emerge from this pandemic. The importance of building sustained PHE/disaster research infrastructure and a research workforce that includes training and funding for pediatrician-scientists and integrates the pediatrician research workforce into high-quality research across demographics, supports the pediatrician-scientist workforce and pipeline, and benefits society.
Johns Hopkins Coronavirus Resource Center. Covid-19 Case Tracker. Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html (2020).
US Food and Drug Administration. Coronavirus (COVID-19) update: FDA issues emergency use authorization for potential COVID-19 treatment. FDA News Release . https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-emergency-use-authorization-potential-covid-19-treatment (2020).
Evans, S. R. Fundamentals of clinical trial design. J. Exp. Stroke Transl. Med. 3 , 19–27 (2010).
Article Google Scholar
Antman, E. M. & Bierer, B. E. Standards for clinical research: keeping pace with the technology of the future. Circulation 133 , 823–825 (2016).
Food and Drug Administration. FDA guidance on conduct of clinical trials of medical products during COVID-19 public health emergency. Guidance for Industry, Investigators and Institutional Review Boards . https://www.fda.gov/regulatory-information/search-fda-guidance-documents/fda-guidance-conduct-clinical-trials-medical-products-during-covid-19-public-health-emergency (2020).
National Institutes of Health. NIH clinical trials shows remdesivir accelerates recovery from advanced COVID-19. NIH New Releases . https://www.nih.gov/news-events/news-releases/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19#.XrIX75ZmQeQ.email (2020).
Radcliffe, S. Here’s exactly where we are with vaccines and treatments for COVID-19. Health News . https://www.healthline.com/health-news/heres-exactly-where-were-at-with-vaccines-and-treatments-for-covid-19 (2020).
Abbasi, J. The promise and peril of antibody testing for COVID-19. JAMA . https://doi.org/10.1001/jama.2020.6170 (2020).
CDC COVID-19 Response Team. Coronavirus disease 2019 in children—United States, February 12–April 2, 2020. Morb. Mortal Wkly Rep . 69 , 422–426 (2020).
Agarwal, N. Opinion: the coronavirus could cause a child abuse epidemic. The New York Times . https://www.nytimes.com/2020/04/07/opinion/coronavirus-child-abuse.html (2020).
Download references
Author information
Authors and affiliations.
Department of Pediatrics, Division of Emergency Medicine, Boston Children’s Hospital, Boston, MA, USA
Debra L. Weiner
Harvard Medical School, Boston, MA, USA
Department of Pediatrics, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA
Vivek Balasubramaniam
Department of Pediatrics and Division of Neonatology, Maria Fareri Children’s Hospital at Westchester Medical Center, New York Medical College, Valhalla, NY, USA
Shetal I. Shah
Division of General Pediatrics, Children’s Hospital Los Angeles, Los Angeles, CA, USA
Joyce R. Javier
Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to conception and design, data acquisition and interpretation, drafting the manuscript, and providing critical revisions. All authors approve this final version of the manuscript.
Pediatric Policy Council
Scott C. Denne, MD, Chair, Pediatric Policy Council; Mona Patel, MD, Representative to the PPC from the Academic Pediatric Association; Jean L. Raphael, MD, MPH, Representative to the PPC from the Academic Pediatric Association; Jonathan Davis, MD, Representative to the PPC from the American Pediatric Society; DeWayne Pursley, MD, MPH, Representative to the PPC from the American Pediatric Society; Tina Cheng, MD, MPH, Representative to the PPC from the Association of Medical School Pediatric Department Chairs; Michael Artman, MD, Representative to the PPC from the Association of Medical School Pediatric Department Chairs; Shetal Shah, MD, Representative to the PPC from the Society for Pediatric Research; Joyce Javier, MD, MPH, MS, Representative to the PPC from the Society for Pediatric Research.
Corresponding author
Correspondence to Debra L. Weiner .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Pediatric Policy Council are listed below Author contributions.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Weiner, D.L., Balasubramaniam, V., Shah, S.I. et al. COVID-19 impact on research, lessons learned from COVID-19 research, implications for pediatric research. Pediatr Res 88 , 148–150 (2020). https://doi.org/10.1038/s41390-020-1006-3
Download citation
Received : 07 May 2020
Accepted : 21 May 2020
Published : 16 June 2020
Issue Date : August 2020
DOI : https://doi.org/10.1038/s41390-020-1006-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Catalysing global surgery: a meta-research study on factors affecting surgical research collaborations with africa.
- Thomas O. Kirengo
- Hussein Dossajee
- Nchafatso G. Obonyo
Systematic Reviews (2024)
Lessons learnt while designing and conducting a longitudinal study from the first Italian COVID-19 pandemic wave up to 3 years
- Alvisa Palese
- Stefania Chiappinotto
- Carlo Tascini
Health Research Policy and Systems (2023)
Pediatric Research and COVID-19: the changed landscape
- E. J. Molloy
- C. B. Bearer
Pediatric Research (2022)
Cancer gene therapy 2020: highlights from a challenging year
- Georgios Giamas
- Teresa Gagliano
Cancer Gene Therapy (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 08 September 2020
Preparing for a pandemic: highlighting themes for research funding and practice—perspectives from the Global Research Collaboration for Infectious Disease Preparedness (GloPID-R)
- Alice Norton 1 , 2 ,
- Louise Sigfrid 1 ,
- Adeniyi Aderoba 3 , 4 ,
- Naima Nasir 3 , 5 ,
- Peter G. Bannister 6 ,
- Shelui Collinson 7 ,
- James Lee 3 ,
- Geneviève Boily-Larouche 8 ,
- Josephine P. Golding 9 ,
- Evelyn Depoortere 10 ,
- Gail Carson 1 ,
- Barbara Kerstiëns 10 &
- Yazdan Yazdanpanah 11
BMC Medicine volume 18 , Article number: 273 ( 2020 ) Cite this article
8068 Accesses
5 Citations
23 Altmetric
Metrics details
Peer Review reports
Funders and researchers around the world are responding to the COVID-19 pandemic at urgent speed, with greater effectiveness and collaboration than ever before. In the past 8 months, the global health research community has collectively generated and shared a huge amount of knowledge in particular into the clinical characterisation, behavioural insights, genetics, epidemiology, viral pathogenesis, clinical management and diagnosis of COVID-19. This is built on substantial prior preparation, with researchers, public health professionals, funders and multilateral bodies in this field having anticipated and prepared for a pandemic for many years. Further knowledge is needed however to control this pandemic and for safe easing of public health measures.
The Global Research Collaboration for Infectious Disease Preparedness (GloPID-R) is an international network of global health funders and stakeholders formed in 2013 to ensure preparedness for a coordinated research response to epidemics and pandemics [ 1 ]. GloPID-R aims to address challenges to effective research in epidemics and pandemics, through both preparedness and response activities.
In December 2019, as part of its preparedness activities, GloPID-R convened a Frontiers meeting with their funded clinical trial networks and cohorts along with key stakeholders involved in emerging epidemic and pandemic preparedness and response globally. The aim was to identify how these groups might collaborate in delivering a coordinated research response in the event of an epidemic or pandemic. Now that we are in the midst of the COVID-19 pandemic, it is important to highlight and reflect on the recommendations identified by these participants, to inform the ongoing research funding and practice during the COVID-19 pandemic as well as preparedness for future outbreaks.
Preparedness themes for research funding and practice
Research cohorts are valuable tools for building pandemic research responses.
Active cohort studies have the potential to play a key role in emerging epidemic and pandemic research. Longitudinal cohorts generate a wealth of data from individual participants about clinical and laboratory outcomes, which allow for a better understanding of effect modifiers such as genetic factors, chronic disease, socio-demographic factors and long-term outcomes than is possible from other study designs. Established cohorts can also function as a broker between emerging disease researchers and the community addressing challenges to the acceptance of research [ 2 ].
There was a call for newly funded cohorts to be designed to be both usable and re-usable in the event of new emerging research questions.
Research capacity and activity mapping are essential to facilitate collaboration and improve targeting of resources
Improved mapping of both global research capacity and ongoing global research activities was identified as necessary to improve identification of opportunities for collaboration and ‘pivoting’ or ‘supplementing’ of ongoing research efforts in outbreaks and improve coordination as pandemics shift globally.
Research collaboration especially between clinical trial networks and cohorts is essential to improve research outcomes
Coordination, in particular across clinical trials and cohorts, is needed to make the most effective use of scarce resources to ensure that studies are not underpowered due to changes in infection rates in differing geographical areas.
Sustainability of funding and research capacity during inter-epidemic periods is key to ensure quality research can be initiated rapidly for epidemics and pandemics
Setting up completely new studies during epidemics and pandemics takes substantial time from the funding commitment, developing necessary infrastructure, research processes and approvals and most importantly trust within the community and leads to fragmentation. Therefore, it may be more efficient to build on large existing studies with baseline continuous research activities, which allow the recruitment of patients from the outset of an outbreak.
Strengthening local research capacity and working closely with governments, local and regional partners and communities to develop and lead national research plans are necessary to ensure critical activities.
Rapid research and funding systems and rapid data sharing are needed to facilitate knowledge generation to improve practice within epidemics and pandemics
Rapid mobilisation of research funds and resources, early engagement with ethics committees and staged approved ethical protocols, adaptive studies and trial designs were all identified as necessary steps to reduce the significant prior delays in initiating research activities in the epidemic response. Funders acknowledged that for many, current funding structures are often not flexible enough to allow quick pivoting or redirection of resources.
Rapid data sharing is needed to accelerate health benefits and outcomes, to facilitate timely dissemination of data to the public for action, and to prevent misinformation. The GloPID-R Data Sharing Roadmap [ 3 ] highlights the key steps to address to enable global data sharing, and the meeting highlighted the need to share emerging barriers and potential solutions in its implementation.
Ethics and social science need to be core to broader epidemic pandemic and research response activities
Ethics should be at the heart of decision-making and an opportunity for researchers to ensure that the optimal value is being obtained from the research for all stakeholders involved, including communities and individuals. Solutions to improve acceptance and uptake of research by healthcare workers and participants are also crucial along with the need for greater inclusion and translation to the practice of qualitative and social sciences studies in epidemics.
These six preparedness recommendations have already been mirrored and in many cases directly informed practice during the COVID-19 research response (see Table 1 ).
There is potential for further leveraging and global coordination of both existing cohorts and clinical trial networks to improve research quality and outcomes during epidemics and pandemics.
Timely, effective epidemic research to improve health outcomes can only be achieved if multidisciplinary research structures, regulatory functions, funding, partnerships and trust are built and maintained sustainably during inter-epidemic periods. Building sustainable research capacity and capability globally needs to be central to research on the COVID-19 pandemic and for future epidemics and pandemics. Sustainable active studies and multidisciplinary networks, with pre-approved protocols positioned strategically globally, need to build upon this.
Conclusions
Lessons learned from the COVID-19 research response need to be incorporated into a multidisciplinary framework to facilitate rapid, coordinated research funding and support structures for researchers, to provide an even faster and coordinated research response, avoiding redundancy. New funder principles for research in epidemics provide the first step toward this [ 7 ].
Availability of data and materials
Not applicable
Matthiessen L, et al. Coordinating funding in public health emergencies. Lancet. 2016;(2016). https://doi.org/10.1016/S0140-6736(16)30604-3 .
Sigfrid L, et al. Addressing political, economic, administrative, regulatory, logistical, ethical, and social challenges to clinical research responses to emerging epidemics and pandemics: a systematic review. Lancet. 2019;394(2).
Norton A, Pardinaz-Solis R & Carson G. 2019. GloPID-R Roadmap for data sharing in public health emergencies. Available from: https://www.glopid-r.org/wp-content/uploads/2019/06/glopid-r-roadmap-for-data-sharing.pdf .
UKCDR and GloPID-R COVID-19 Research Project Tracker, 2020, https://www.ukcdr.org.uk/funding-landscape/covid-19-research-project-tracker/ .
Principles for data sharing in public health emergencies. GloPID-R data sharing working group. London: Figshare; 2017. Available from: doi: https://doi.org/10.6084/m9.figshare.4733590 [cited 2020 Jul 07].
A Coordinated Global Research Roadmap: 2019 Novel Coronavirus. Available at: https://www.glopid-r.org/wp-content/uploads/2020/03/who-2019-novel-coronavirus-global-research-roadmap.pdf .
Norton A, Mphahlele J, Yazdanpanah Y, Piot P, Bayona MT. Strengthening the global effort on COVID-19 research. The Lancet. 2020;396(10248):375.
Download references
Acknowledgements
Meeting participants:
Adeniyi Aderoba (University of Oxford, Oxford, UK; University of Medical Sciences Teaching Hospital, Ondo State, Nigeria); John Amuasi (ALERRT, Kumasi, Ghana); Amrish Baidjoe (EAN, RECON, London, UK); Peter Bannister (Brighton & Sussex Medical School, Brighton, UK); Genevieve Boily-Larouche (CIHR, Ottawa, Canada); Elaine Boylan (MRC, London, UK); Serge Breysse (GloPID-R, Paris, France); David Carr (Wellcome Trust, London, UK); Gail Carson (GloPID-R, Oxford, UK); Amol Chaudhari (CEPI, London, UK); Guy Cochrane (EMBL-EBI, Hinxton, UK); Shelui Collinson (NHS, London, UK); Chioma Dan-Nwafor (Nigeria Centre for Disease Control (NCDC), Abuja, Nigeria); Xavier De Lamballerie (UVE, Marseille, France); Evelyn Depoortere (European Commission); Lennie Derde (REMAP-CAP, Utrecht, Netherlands); Eric Dortenzio (REACTing, Paris, France); Tamara Giles Vernick (Institut Pasteur, Paris, France); Nina Gobat (PREPARE, ECRAID, Oxford, UK); Josie Golding (Wellcome Trust, London, UK); Herman Goossens (PREPARE, ECRAID, Brussels, Belgium); Jean Marie Habarugira (EDCTP, Hague, Netherlands); Ana Maria Henao Restrepo (WHO, Geneva, Switzerland); David Heymann (LSHTM, London, UK); Elisabeth Higgs (NIH, HHS, USG, Bethesda, USA); Bruno Hoen (Institut Pasteur, Paris, France); William Hsiao (BCCDC PHL, Vancouver, Canada); Thomas Jaenisch (ReCoDID, Heidelberg, Germany); Nina Jamieson (ISARIC, Oxford, UK); Marie Jaspard (ALIMA, Paris, France); Barbara Kerstiëns (European Commission); Trudie Lang (TGHN, Oxford, UK); Joanne Langley (Dalhousie University, Halifax, Canada); James Lee (ISARIC, Oxford, UK); Katherine Littler (WHO, Geneva, Switzerland); Dermot Maher (TDR, Geneva, Switzerland); Denis Malvy (Bordeaux University Hospital, Bordeaux, France); Gustavo Matta (FIOCRUZ, Rio de Janeiro, Brazil); Romans Matulevics (ISARIC, Oxford, UK); Laura Merson (IDDO, Oxford, UK); Shoji Miyagawa (AMED, Tokyo, Japan); Naima Nasir (University of Oxford, Oxford, UK; APIN-Supported HIV Treatment Centre, Jos University Teaching Hospital, Jos, Nigeria); Robert Newton (ALPHA, LSHTM, Entebbe, Uganda); Alice Norton (GloPID-R, Oxford, UK); Piero Olliaro (ISARIC, Oxford, UK); Hitoshi Oshitani (Tohoko University Graduate School of Medicine, Sendai, Japan); Barbara Rath (PEDSIDEA, Vienna Vaccine Safety Initiative, Berlin, Germany); David Robertson (University of Edinburgh, Edinburgh, UK); Cathy Roth (DFID, London, UK); Kathy Rowan (REMAP-CAP, London, UK); Nahoko Shindo (WHO, Geneva, Switzerland); Louise Sigfrid (ERGO, Oxford, UK); Stefanie Sowinski (European Commission); David Vaughn (BMGF, Seattle, USA); Richard Wilder (CEPI, London, UK); Annelies Wilder Smith (LSHTM, London, UK); Jimmy Whitworth (LSHTM, London, UK); Katharine Wright (Nuffield Council on Bioethics, London, UK); Yazdan Yazdanpanah (GloPID-R, Paris, France); and Lay-Myint Yoshida (Nagasaki University, Nagasaki, Japan).
The GloPID-R Secretariat is funded through the European Union’s Horizon 2020 Research and Innovation Programme under grant agreement 643434.
Author information
Authors and affiliations.
GloPID-R Secretariat, University of Oxford, Oxford, UK
Alice Norton, Louise Sigfrid & Gail Carson
UK Collaborative on Development Research, London, UK
Alice Norton
Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Adeniyi Aderoba, Naima Nasir & James Lee
University of Medical Sciences Teaching Hospital, Ondo, Ondo State, Nigeria
Adeniyi Aderoba
APIN-Supported HIV Treatment Centre, Jos University Teaching Hospital, Jos, Nigeria
Naima Nasir
Brighton and Sussex Medical School, Brighton, UK
Peter G. Bannister
Clinical Research Department, London School of Hygiene and Tropical Medicine, London, UK
Shelui Collinson
Institute of Infection and Immunity Canadian Institutes of Health Research (CIHR), Government of Canada, Ottawa, Canada
Geneviève Boily-Larouche
Wellcome, London, UK
Josephine P. Golding
European Commissions’ Directorate-General for Research & Innovation, European Commission, Brussels, Belgium
Evelyn Depoortere & Barbara Kerstiëns
INSERM, Paris, France
Yazdan Yazdanpanah
You can also search for this author in PubMed Google Scholar
Contributions
All authors read and approved the final manuscript.
Corresponding author
Correspondence to Alice Norton .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Norton, A., Sigfrid, L., Aderoba, A. et al. Preparing for a pandemic: highlighting themes for research funding and practice—perspectives from the Global Research Collaboration for Infectious Disease Preparedness (GloPID-R). BMC Med 18 , 273 (2020). https://doi.org/10.1186/s12916-020-01755-y
Download citation
Received : 30 July 2020
Accepted : 19 August 2020
Published : 08 September 2020
DOI : https://doi.org/10.1186/s12916-020-01755-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preparedness
- Clinical trials
- Collaboration
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Office of the Dean for Research

COVID-19 Research Proposals
Princeton University has authorized funding to support faculty research projects that consider biomedical, health-related and fundamental science related to the COVID pandemic, as well as those that impact corresponding policy, social, and economic topics.
Read the full details in this email from Dean for Research Pablo Debenedetti . Proposals were due by 11 p.m. on Sunday, April 5, 2020 and awards were announced on Friday, April 10, 2020.

Greater Good Science Center • Magazine • In Action • In Education
11 Questions to Ask About COVID-19 Research
Debates have raged on social media, around dinner tables, on TV, and in Congress about the science of COVID-19. Is it really worse than the flu? How necessary are lockdowns? Do masks work to prevent infection? What kinds of masks work best? Is the new vaccine safe?
You might see friends, relatives, and coworkers offer competing answers, often brandishing studies or citing individual doctors and scientists to support their positions. With so much disagreement—and with such high stakes—how can we use science to make the best decisions?
Here at Greater Good , we cover research into social and emotional well-being, and we try to help people apply findings to their personal and professional lives. We are well aware that our business is a tricky one.
Summarizing scientific studies and distilling the key insights that people can apply to their lives isn’t just difficult for the obvious reasons, like understanding and then explaining formal science terms or rigorous empirical and analytic methods to non-specialists. It’s also the case that context gets lost when we translate findings into stories, tips, and tools, especially when we push it all through the nuance-squashing machine of the Internet. Many people rarely read past the headlines, which intrinsically aim to be relatable and provoke interest in as many people as possible. Because our articles can never be as comprehensive as the original studies, they almost always omit some crucial caveats, such as limitations acknowledged by the researchers. To get those, you need access to the studies themselves.
And it’s very common for findings and scientists to seem to contradict each other. For example, there were many contradictory findings and recommendations about the use of masks, especially at the beginning of the pandemic—though as we’ll discuss, it’s important to understand that a scientific consensus did emerge.
Given the complexities and ambiguities of the scientific endeavor, is it possible for a non-scientist to strike a balance between wholesale dismissal and uncritical belief? Are there red flags to look for when you read about a study on a site like Greater Good or hear about one on a Fox News program? If you do read an original source study, how should you, as a non-scientist, gauge its credibility?
Here are 11 questions you might ask when you read about the latest scientific findings about the pandemic, based on our own work here at Greater Good.
1. Did the study appear in a peer-reviewed journal?
In peer review, submitted articles are sent to other experts for detailed critical input that often must be addressed in a revision prior to being accepted and published. This remains one of the best ways we have for ascertaining the rigor of the study and rationale for its conclusions. Many scientists describe peer review as a truly humbling crucible. If a study didn’t go through this process, for whatever reason, it should be taken with a much bigger grain of salt.
“When thinking about the coronavirus studies, it is important to note that things were happening so fast that in the beginning people were releasing non-peer reviewed, observational studies,” says Dr. Leif Hass, a family medicine doctor and hospitalist at Sutter Health’s Alta Bates Summit Medical Center in Oakland, California. “This is what we typically do as hypothesis-generating but given the crisis, we started acting on them.”
In a confusing, time-pressed, fluid situation like the one COVID-19 presented, people without medical training have often been forced to simply defer to expertise in making individual and collective decisions, turning to culturally vetted institutions like the Centers for Disease Control (CDC). Is that wise? Read on.
2. Who conducted the study, and where did it appear?
“I try to listen to the opinion of people who are deep in the field being addressed and assess their response to the study at hand,” says Hass. “With the MRNA coronavirus vaccines, I heard Paul Offit from UPenn at a UCSF Grand Rounds talk about it. He literally wrote the book on vaccines. He reviewed what we know and gave the vaccine a big thumbs up. I was sold.”
From a scientific perspective, individual expertise and accomplishment matters—but so does institutional affiliation.
Why? Because institutions provide a framework for individual accountability as well as safety guidelines. At UC Berkeley, for example , research involving human subjects during COVID-19 must submit a Human Subjects Proposal Supplement Form , and follow a standard protocol and rigorous guidelines . Is this process perfect? No. It’s run by humans and humans are imperfect. However, the conclusions are far more reliable than opinions offered by someone’s favorite YouTuber .
Recommendations coming from institutions like the CDC should not be accepted uncritically. At the same time, however, all of us—including individuals sporting a “Ph.D.” or “M.D.” after their names—must be humble in the face of them. The CDC represents a formidable concentration of scientific talent and knowledge that dwarfs the perspective of any one individual. In a crisis like COVID-19, we need to defer to that expertise, at least conditionally.
“If we look at social media, things could look frightening,” says Hass. When hundreds of millions of people are vaccinated, millions of them will be afflicted anyway, in the course of life, by conditions like strokes, anaphylaxis, and Bell’s palsy. “We have to have faith that people collecting the data will let us know if we are seeing those things above the baseline rate.”
3. Who was studied, and where?
Animal experiments tell scientists a lot, but their applicability to our daily human lives will be limited. Similarly, if researchers only studied men, the conclusions might not be relevant to women, and vice versa.
Many psychology studies rely on WEIRD (Western, educated, industrialized, rich and democratic) participants, mainly college students, which creates an in-built bias in the discipline’s conclusions. Historically, biomedical studies also bias toward gathering measures from white male study participants, which again, limits generalizability of findings. Does that mean you should dismiss Western science? Of course not. It’s just the equivalent of a “Caution,” “Yield,” or “Roadwork Ahead” sign on the road to understanding.
This applies to the coronavirus vaccines now being distributed and administered around the world. The vaccines will have side effects; all medicines do. Those side effects will be worse for some people than others, depending on their genetic inheritance, medical status, age, upbringing, current living conditions, and other factors.
For Hass, it amounts to this question: Will those side effects be worse, on balance, than COVID-19, for most people?
“When I hear that four in 100,000 [of people in the vaccine trials] had Bell’s palsy, I know that it would have been a heck of a lot worse if 100,000 people had COVID. Three hundred people would have died and many others been stuck with chronic health problems.”
4. How big was the sample?
In general, the more participants in a study, the more valid its results. That said, a large sample is sometimes impossible or even undesirable for certain kinds of studies. During COVID-19, limited time has constrained the sample sizes.
However, that acknowledged, it’s still the case that some studies have been much larger than others—and the sample sizes of the vaccine trials can still provide us with enough information to make informed decisions. Doctors and nurses on the front lines of COVID-19—who are now the very first people being injected with the vaccine—think in terms of “biological plausibility,” as Hass says.
Did the admittedly rushed FDA approval of the Pfizer-BioNTech vaccine make sense, given what we already know? Tens of thousands of doctors who have been grappling with COVID-19 are voting with their arms, in effect volunteering to be a sample for their patients. If they didn’t think the vaccine was safe, you can bet they’d resist it. When the vaccine becomes available to ordinary people, we’ll know a lot more about its effects than we do today, thanks to health care providers paving the way.
5. Did the researchers control for key differences, and do those differences apply to you?
Diversity or gender balance aren’t necessarily virtues in experimental research, though ideally a study sample is as representative of the overall population as possible. However, many studies use intentionally homogenous groups, because this allows the researchers to limit the number of different factors that might affect the result.
While good researchers try to compare apples to apples, and control for as many differences as possible in their analyses, running a study always involves trade-offs between what can be accomplished as a function of study design, and how generalizable the findings can be.
The Science of Happiness
What does it take to live a happier life? Learn research-tested strategies that you can put into practice today. Hosted by award-winning psychologist Dacher Keltner. Co-produced by PRX and UC Berkeley’s Greater Good Science Center.
- Apple Podcasts
- Google Podcasts
You also need to ask if the specific population studied even applies to you. For example, when one study found that cloth masks didn’t work in “high-risk situations,” it was sometimes used as evidence against mask mandates.
However, a look beyond the headlines revealed that the study was of health care workers treating COVID-19 patients, which is a vastly more dangerous situation than, say, going to the grocery store. Doctors who must intubate patients can end up being splattered with saliva. In that circumstance, one cloth mask won’t cut it. They also need an N95, a face shield, two layers of gloves, and two layers of gown. For the rest of us in ordinary life, masks do greatly reduce community spread, if as many people as possible are wearing them.
6. Was there a control group?
One of the first things to look for in methodology is whether the population tested was randomly selected, whether there was a control group, and whether people were randomly assigned to either group without knowing which one they were in. This is especially important if a study aims to suggest that a certain experience or treatment might actually cause a specific outcome, rather than just reporting a correlation between two variables (see next point).
For example, were some people randomly assigned a specific meditation practice while others engaged in a comparable activity or exercise? If the sample is large enough, randomized trials can produce solid conclusions. But, sometimes, a study will not have a control group because it’s ethically impossible. We can’t, for example, let sick people go untreated just to see what would happen. Biomedical research often makes use of standard “treatment as usual” or placebos in control groups. They also follow careful ethical guidelines to protect patients from both maltreatment and being deprived necessary treatment. When you’re reading about studies of masks, social distancing, and treatments during the COVID-19, you can partially gauge the reliability and validity of the study by first checking if it had a control group. If it didn’t, the findings should be taken as preliminary.
7. Did the researchers establish causality, correlation, dependence, or some other kind of relationship?
We often hear “Correlation is not causation” shouted as a kind of battle cry, to try to discredit a study. But correlation—the degree to which two or more measurements seem connected—is important, and can be a step toward eventually finding causation—that is, establishing a change in one variable directly triggers a change in another. Until then, however, there is no way to ascertain the direction of a correlational relationship (does A change B, or does B change A), or to eliminate the possibility that a third, unmeasured factor is behind the pattern of both variables without further analysis.
In the end, the important thing is to accurately identify the relationship. This has been crucial in understanding steps to counter the spread of COVID-19 like shelter-in-place orders. Just showing that greater compliance with shelter-in-place mandates was associated with lower hospitalization rates is not as conclusive as showing that one community that enacted shelter-in-place mandates had lower hospitalization rates than a different community of similar size and population density that elected not to do so.
We are not the first people to face an infection without understanding the relationships between factors that would lead to more of it. During the bubonic plague, cities would order rodents killed to control infection. They were onto something: Fleas that lived on rodents were indeed responsible. But then human cases would skyrocket.
Why? Because the fleas would migrate off the rodent corpses onto humans, which would worsen infection. Rodent control only reduces bubonic plague if it’s done proactively; once the outbreak starts, killing rats can actually make it worse. Similarly, we can’t jump to conclusions during the COVID-19 pandemic when we see correlations.
8. Are journalists and politicians, or even scientists, overstating the result?
Language that suggests a fact is “proven” by one study or which promotes one solution for all people is most likely overstating the case. Sweeping generalizations of any kind often indicate a lack of humility that should be a red flag to readers. A study may very well “suggest” a certain conclusion but it rarely, if ever, “proves” it.
This is why we use a lot of cautious, hedging language in Greater Good , like “might” or “implies.” This applies to COVID-19 as well. In fact, this understanding could save your life.
When President Trump touted the advantages of hydroxychloroquine as a way to prevent and treat COVID-19, he was dramatically overstating the results of one observational study. Later studies with control groups showed that it did not work—and, in fact, it didn’t work as a preventative for President Trump and others in the White House who contracted COVID-19. Most survived that outbreak, but hydroxychloroquine was not one of the treatments that saved their lives. This example demonstrates how misleading and even harmful overstated results can be, in a global pandemic.
9. Is there any conflict of interest suggested by the funding or the researchers’ affiliations?
A 2015 study found that you could drink lots of sugary beverages without fear of getting fat, as long as you exercised. The funder? Coca Cola, which eagerly promoted the results. This doesn’t mean the results are wrong. But it does suggest you should seek a second opinion : Has anyone else studied the effects of sugary drinks on obesity? What did they find?
It’s possible to take this insight too far. Conspiracy theorists have suggested that “Big Pharma” invented COVID-19 for the purpose of selling vaccines. Thus, we should not trust their own trials showing that the vaccine is safe and effective.
But, in addition to the fact that there is no compelling investigative evidence that pharmaceutical companies created the virus, we need to bear in mind that their trials didn’t unfold in a vacuum. Clinical trials were rigorously monitored and independently reviewed by third-party entities like the World Health Organization and government organizations around the world, like the FDA in the United States.
Does that completely eliminate any risk? Absolutely not. It does mean, however, that conflicts of interest are being very closely monitored by many, many expert eyes. This greatly reduces the probability and potential corruptive influence of conflicts of interest.
10. Do the authors reference preceding findings and original sources?
The scientific method is based on iterative progress, and grounded in coordinating discoveries over time. Researchers study what others have done and use prior findings to guide their own study approaches; every study builds on generations of precedent, and every scientist expects their own discoveries to be usurped by more sophisticated future work. In the study you are reading, do the researchers adequately describe and acknowledge earlier findings, or other key contributions from other fields or disciplines that inform aspects of the research, or the way that they interpret their results?

Greater Good’s Guide to Well-Being During Coronavirus
Practices, resources, and articles for individuals, parents, and educators facing COVID-19
This was crucial for the debates that have raged around mask mandates and social distancing. We already knew quite a bit about the efficacy of both in preventing infections, informed by centuries of practical experience and research.
When COVID-19 hit American shores, researchers and doctors did not question the necessity of masks in clinical settings. Here’s what we didn’t know: What kinds of masks would work best for the general public, who should wear them, when should we wear them, were there enough masks to go around, and could we get enough people to adopt best mask practices to make a difference in the specific context of COVID-19 ?
Over time, after a period of confusion and contradictory evidence, those questions have been answered . The very few studies that have suggested masks don’t work in stopping COVID-19 have almost all failed to account for other work on preventing the disease, and had results that simply didn’t hold up. Some were even retracted .
So, when someone shares a coronavirus study with you, it’s important to check the date. The implications of studies published early in the pandemic might be more limited and less conclusive than those published later, because the later studies could lean on and learn from previously published work. Which leads us to the next question you should ask in hearing about coronavirus research…
11. Do researchers, journalists, and politicians acknowledge limitations and entertain alternative explanations?
Is the study focused on only one side of the story or one interpretation of the data? Has it failed to consider or refute alternative explanations? Do they demonstrate awareness of which questions are answered and which aren’t by their methods? Do the journalists and politicians communicating the study know and understand these limitations?
When the Annals of Internal Medicine published a Danish study last month on the efficacy of cloth masks, some suggested that it showed masks “make no difference” against COVID-19.
The study was a good one by the standards spelled out in this article. The researchers and the journal were both credible, the study was randomized and controlled, and the sample size (4,862 people) was fairly large. Even better, the scientists went out of their way to acknowledge the limits of their work: “Inconclusive results, missing data, variable adherence, patient-reported findings on home tests, no blinding, and no assessment of whether masks could decrease disease transmission from mask wearers to others.”
Unfortunately, their scientific integrity was not reflected in the ways the study was used by some journalists, politicians, and people on social media. The study did not show that masks were useless. What it did show—and what it was designed to find out—was how much protection masks offered to the wearer under the conditions at the time in Denmark. In fact, the amount of protection for the wearer was not large, but that’s not the whole picture: We don’t wear masks mainly to protect ourselves, but to protect others from infection. Public-health recommendations have stressed that everyone needs to wear a mask to slow the spread of infection.
“We get vaccinated for the greater good, not just to protect ourselves ”
As the authors write in the paper, we need to look to other research to understand the context for their narrow results. In an editorial accompanying the paper in Annals of Internal Medicine , the editors argue that the results, together with existing data in support of masks, “should motivate widespread mask wearing to protect our communities and thereby ourselves.”
Something similar can be said of the new vaccine. “We get vaccinated for the greater good, not just to protect ourselves,” says Hass. “Being vaccinated prevents other people from getting sick. We get vaccinated for the more vulnerable in our community in addition for ourselves.”
Ultimately, the approach we should take to all new studies is a curious but skeptical one. We should take it all seriously and we should take it all with a grain of salt. You can judge a study against your experience, but you need to remember that your experience creates bias. You should try to cultivate humility, doubt, and patience. You might not always succeed; when you fail, try to admit fault and forgive yourself.
Above all, we need to try to remember that science is a process, and that conclusions always raise more questions for us to answer. That doesn’t mean we never have answers; we do. As the pandemic rages and the scientific process unfolds, we as individuals need to make the best decisions we can, with the information we have.
This article was revised and updated from a piece published by Greater Good in 2015, “ 10 Questions to Ask About Scientific Studies .”
About the Authors
Jeremy Adam Smith
Uc berkeley.
Jeremy Adam Smith edits the GGSC’s online magazine, Greater Good . He is also the author or coeditor of five books, including The Daddy Shift , Are We Born Racist? , and (most recently) The Gratitude Project: How the Science of Thankfulness Can Rewire Our Brains for Resilience, Optimism, and the Greater Good . Before joining the GGSC, Jeremy was a John S. Knight Journalism Fellow at Stanford University.
Emiliana R. Simon-Thomas
Emiliana R. Simon-Thomas, Ph.D. , is the science director of the Greater Good Science Center, where she directs the GGSC’s research fellowship program and serves as a co-instructor of its Science of Happiness and Science of Happiness at Work online courses.
You May Also Enjoy

How to Form a Pandemic Pod

In a Pandemic, Elbow Touches Might Keep Us Going

Why Your Sacrifices Matter During the Pandemic

How to Keep the Greater Good in Mind During the Coronavirus Outbreak

Why Is COVID-19 Killing So Many Black Americans?

How Does COVID-19 Affect Trust in Government?
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Competing with a pandemic: Trends in research design in a time of Covid-19
Roles Conceptualization, Data curation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliation Department of Radiation Oncology, University of Southern California, Los Angeles, California, United States of America
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Division of Nephrology and Hypertension, Department of Medicine, University of Southern California, Los Angeles, California, United States of America
- Shelly X. Bian,

- Published: September 10, 2020
- https://doi.org/10.1371/journal.pone.0238831
- Reader Comments
Introduction
During the Covid-19 pandemic, major journals have published a significant number of Covid-19 related articles in a short period of time. While this is necessary to combat the worldwide pandemic, it may have trade-offs with respect to publishing research from other disciplines.
To assess differences in published research design before and after the Covid-19 pandemic.
We performed a cross-sectional review of all 322 full-length research studies published between October 1, 2019 and April 30, 2020 in three major medical journals. We compared the number of randomized controlled trials (RCTs) and studies with a control group before and after January 31, 2020, when Covid-19 began garnering international attention.
The number of full-length research studies per issue was not statistically different before and after the Covid-19 pandemic (from 3.7 to 3.5 per issue, p = 0.17). Compared to before January 31, 2020, 0.7 fewer non-Covid-19 studies per issue were published versus after January 31, 2020 (p<0.001), a change that was offset by Covid-19 studies. Among non-Covid-19 studies, 0.9 fewer studies with a control group per issue were published after January 31, 2020, with RCTs contributing to nearly all the decline (p<0.001, p = 0.001, respectively). In the same timeframe, non-Covid-19 studies without a control group and non-Covid-19 studies without randomization experienced relatively small changes that did not meet our threshold for statistical significance (increases of 0.1 and 0.1 per issue, p = 0.80, p = 0.88, respectively).
Limitations
Using a simple heuristic for assessing research design and lack of generalizability to the general medical literature.
Conclusions
In summary, the increase in Covid-19 studies coincided with a decrease of mostly non-Covid-19 RCTs.
Citation: Bian SX, Lin E (2020) Competing with a pandemic: Trends in research design in a time of Covid-19. PLoS ONE 15(9): e0238831. https://doi.org/10.1371/journal.pone.0238831
Editor: Daniele Fanelli, London School of Economics and Political Science, UNITED KINGDOM
Received: June 10, 2020; Accepted: August 25, 2020; Published: September 10, 2020
Copyright: © 2020 Bian, Lin. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are available at DOI 10.17605/OSF.IO/A2HQR .
Funding: This work was supported in part by the National Institutes of Health (NIH) through the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): EL receives support from NIDDK K08DK118213. EL also receives support from the University Kidney Research Organization. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Competing interests: The authors have declared that no competing interests exist.
The Covid-19 pandemic has severely disrupted medical research, from shutting down laboratory facilities, to delaying clinical trials, to halting funding [ 1 , 2 ]. Simultaneously, the volume of Covid-19 research has proliferated as experts from all disciplines seek to combat the new threat [ 3 , 4 ]. In the months following the onset of Covid-19, there has been an unprecedented increase in the number of registered clinical trials, preprints, and publications related to Covid-19 [ 5 ].
As of May, 2020, ClinicalTrials.gov listed over 1000 Covid-19 studies. Although some will advance our clinical knowledge, many are small, poorly designed, redundant, and unlikely to prove clinically useful [ 6 ]. Meanwhile the peer review process for Covid-19 studies has accelerated substantially. An analysis of 14 medical journals found a 50% reduction in average turnaround time from submission to publication for Covid-19 related research. This study, however, did not include several of the most influential journals including The Journal of the American Medical Association , The Lancet , and The New England Journal of Medicine [ 7 ]. The proliferation of Covid-19 literature has permeated into non-peer reviewed preprint websites, such as BioRxiv and MedRxiv. As of May 7, MedRxiv and BioRxiv had close to 2800 Covid-19 related articles combined. This has led to several editorials expressing concern over the quality of Covid-19 related research [ 8 , 9 ].
Many people look to most influential medical journals as having the highest standards for publication. The shifting of our research priorities is appropriate and necessary to address the pandemic. However, this diversion may also have unintended consequences on research in other disciplines. To evaluate whether the Covid-19 pandemic had negative effects on published research in other disciplines, we studied characteristics of Covid-19 and non-Covid-19 related research in three of the most cited medical journals: The Journal of the American Medical Association , The Lancet , and The New England Journal of Medicine . Although prior studies have evaluated the proliferation, quality, and design of Covid-19 related publications, none to our knowledge have addressed the pandemic’s effect on the study design of non-Covid-19 medical research. In this cross-sectional study, we investigated whether the design of published non-Covid-19 research changed in three of the highest impact medical journals aimed at a predominantly clinical audience after the onset of the Covid-19 pandemic.
Identifying research studies
We reviewed all full-length research studies published between October 1, 2019 and April 30, 2020 in three of the highest impact medical journals, The New England Journal of Medicine (NEJM) , the Journal of the American Medical Association (JAMA) , and The Lancet . These included “Original Articles” from NEJM (including “Brief Reports” and “Special Reports”), “Original Research” from JAMA (including “Preliminary Communications” and “Special Communications”), and “Research Articles” from The Lancet .
Many Covid-19 studies are case series published as short research studies and letters to the editor. In a sensitivity analysis, we additionally included short research studies published in letter format: “Correspondences” from NEJM and The Lancet and “Research Letters” from JAMA . The Correspondence sections from the NEJM and The Lancet have a broad range and include letters addressing previous articles, primary research, and opinions. From these, we manually identified all letters with a primary data collection effort (including case series and translational research) or secondary analysis of already collected data. We included all of JAMA’s Research Letters. We excluded sections dedicated for case reports (e.g., the “Case Records from the Massachusetts General Hospital in The New England Journal of Medicine ” or “Brief Reports” from JAMA ) but included case reports or case series published as short research studies or letters to the editor. Our publication selection process is outlined in a Prisma flow diagram in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0238831.g001
We assigned each study an organ system (S1 Table in S1 Appendix ) and determined whether it was (i) Covid-19 related, (ii) a study with a control group, and (iii) a randomized controlled trial (RCT). We defined Covid-19-related research as having any Covid-19 related words in the title of the article including “Covid-19”, “novel coronavirus”, “2019-nCoV”, “Coronavirus disease 2019”, or SARS-CoV-2”. We defined a control group as whether the investigators performed a hypothesis-driven analysis, comparing two or more groups. Studies describing trends over time were considered uncontrolled unless the investigators tested a specific hypothesis, such as analyzing the putative effect of a policy intervention. Both authors reviewed all studies, adjudicating conflicts by consensus (see S1 Appendix for additional formal designations).

Statistical analyses
We compared study characteristics before and after the end of January 2020, when Covid-19 began garnering international attention. We defined the pre-Covid-19 era as January 31, 2020 and prior, and the post-Covid-19 era as February 1, 2020 and after. We chose this cutoff because the last week of January, 2020 marked the public announcement of the first cases of Covid-19 outside of China. Simultaneously, the World Health Organization (WHO) began warning other countries of the virus’ global spread and the importance of formulating strategic plans for virus containment around this time. Furthermore, the first Covid-19 publication in the three medical journals of interest was published on February 15, 2020 in The Lancet .
We first plotted the number of published Original Research studies, studies that were Covid-19 related, studies with and without a control group, and studies that were RCTs over time. We performed this descriptive analysis by assigning each issue to a given week, anchoring to the Monday of that week. We computed the average number of studies per week before and after the end of January 2020 to visually demonstrate changes in before and after Covid-19.
Subsequently, we assessed per issue differences in study type before and after the end of January 2020. For each of the three journals examined, issues are published weekly with the rare exception of an omitted week. We used the Mann-Whitney-Wilcoxan test to assess whether the average number of Covid-19 related studies, studies with and without a control group, and studies that were RCTs per issue was different before and after January 31, 2020. We performed analyses using the number of studies per issue instead of the proportion of studies per issue because counts reflect the zero-sum nature of publications and provide meaningful information on the volume of studies published. For instance, a large decrease in the total number of published studies might not change the proportion of published RCTs but would likely decrease the number of published RCTs. Because the total number of published studies per issue did not change substantially over time, this distinction was unlikely material to our results.
Our primary focus was on all full-length research studies and on the non-Covid-19 related subgroup of studies. In a sensitivity analyses, we expanded our sample to all research studies including those in letter format.
To assess changes in publication by organ system, we aggregated the total number of full-length research articles into pre-Covid-19 and post-Covid-19 cohorts. We did this because of the scarcity of some organ systems at an issue level. Because the pre-Covid-19 study period had more months, we plotted the percent of published full-length research studies before and after the onset of Covid-19. For each organ system, we compared the significance of the change in proportion before and after Covid-19 using Fisher’s exact test.
We acknowledge that we did not pre-register our study with a predetermined statistical protocol. Additionally, we performed a large number of statistical tests. Therefore, we performed a conservative Bonferroni correction [ 10 ] to adjust the threshold for rejecting the null hypothesis. Because we performed 21 tests in our primary analysis, we required a p-value of 0.0024 when determining whether a difference was statistically significant.
We identified 322 total full-length research studies, 188 before and 134 after the end of January, 2020. The distribution of full-length research articles by journal for each month is detailed in Table 1 .
https://doi.org/10.1371/journal.pone.0238831.t001
The total number of full-length research studies did not statistically differ before and after Covid-19 (from 3.7 to 3.5 per issue, p = 0.17). After January 2020, non-Covid-19 full-length studies decreased by 0.7 per issue on average (p<0.001), which was offset by Covid-19 full-length studies. The total number of full-length studies with a control group decreased by 0.8 per issue on average (p<0.001) and the number of RCTs decreased by 0.9 per issue (p = 0.001). Fig 2 shows changes in full-length articles by week, which usually includes 1 issue from each journal.
Figure includes all full-length research studies in counts per week. A) Covid-19 versus non-Covid-19 studies, B) controlled versus uncontrolled studies, C) RCTs versus non-RCTs. P-values estimated using a two-sample t-test. The gray vertical lines denote January 31, 2020, the boundary between the pre- and post-Covid-19 eras. Solid horizontal lines denote average values of the solid dots and dashed horizontal lines denote average values of the hollow dots.
https://doi.org/10.1371/journal.pone.0238831.g002
Among non-Covid-19 full-length studies, the number of studies with a control group decreased by 0.9 per issue on average with RCTs contributing to nearly all the decline (p<0.001, p = 0.001, respectively). In the same timeframe, non-Covid-19 full-length studies without a control group and non-Covid-19 full-length studies without randomization did not statistically differ (p = 0.80, 0.88, respectively). Fig 3 shows weekly changes in full-length non-Covid-19 articles.
Figure includes all non-Covid-19 full-length research studies in counts per week. A) controlled versus uncontrolled studies B) RCTs versus non-RCTs. P-values estimated using a two-sample t-test. The gray vertical lines denote January 31, 2020, the boundary between the pre- and post-Covid-19 eras. Solid horizontal lines denote average values of the solid dots and dashed horizontal lines denote average values of the hollow dots.
https://doi.org/10.1371/journal.pone.0238831.g003
Cardiology and obstetrics/gynecology had the largest declines in full-length published studies, from 23% to 13% (9% decline, p = 0.04) and from 4% to 0% (4% decline, p = 0.02, respectively. Meanwhile infectious diseases had the largest increase, from 9% to 28% (19% increase, p<0.001) ( Fig 4 , Table 2 ).
P-values were estimated using Fisher’s Exact Test. (an asterisk, *, denotes p < 0.0025). January 31, 2020 is the boundary between the pre- and post-Covid-19 eras.
https://doi.org/10.1371/journal.pone.0238831.g004
https://doi.org/10.1371/journal.pone.0238831.t002
In a sensitivity analysis, we included an additional 104 short research studies (57 pre- and 47 post-Covid-19) typically published in Letter format. The sensitivity analysis included a total of 426 research studies, 425 pre- and 181 post-Covid-19 and was not materially different from our primary analysis.
The total number of studies overall did not statistically differ before and after Covid-19 (from 4.9 to 4.8 per issue, p = 0.95). After January 31, 2020, non-Covid-19 studies decreased by 1.2 per issue on average (p<0.001), which was offset by Covid-19 studies. We observed a decrease in number of studies pre- and post-Covid-19 with a control group of 0.9 per issue on average (p = 0.001), which was almost entirely explained by a decrease in RCTs (p = 0.002). Fig 5 shows weekly changes in all articles.
Figure includes full-length research studies as well as research studies in Letter form in counts per week. A) Covid-19 versus non-Covid-19 studies, B) controlled versus uncontrolled studies, C) RCTs versus non-RCTs. P-values estimated using a two-sample t-test. The gray vertical lines denote January 31, 2020, the boundary between the pre- and post-Covid-19 eras. Solid horizontal lines denote average values of the solid dots and dashed horizontal lines denote average values of the hollow dots.
https://doi.org/10.1371/journal.pone.0238831.g005
Among non-Covid-19 studies, the number of studies with a control group decreased by 0.9 per issue on average with RCTs contributing to nearly all the decline (p<0.001, p = 0.002, respectively). In the same timeframe, non-Covid-19 studies without a control group and non-Covid-19 studies without randomization did not statistically differ (p = 0.27, 0.26, respectively). Fig 6 shows weekly changes in all non-Covid-19 articles.
Figure includes all non-Covid-19 full-length research studies as well as research studies in Letter form. A) controlled versus uncontrolled studies B) RCTs versus non-RCTs. P-values estimated using a two-sample t-test.
https://doi.org/10.1371/journal.pone.0238831.g006
In contrast, none of the Covid-19 studies (20 full-length and 21 in letter format) were RCTs, and only one had a control group. Table 3 shows changes in articles per issue in all articles as well as full-length articles before and after January 31, 2020.
https://doi.org/10.1371/journal.pone.0238831.t003
We found that in three of the highest impact medical journals, the increase in Covid-19-related research studies coincided with a concomitant decrease in non-Covid-related RCTs. Unsurprisingly, most Covid-19 studies published in the first three months of the pandemic comprised case reports and case series. No Covid-19 related RCT’s were published from February 1, to April 30, 2020. We observed a decreasing trend in cardiology and obstetrics/gynecology studies post-Covid-19, though the decrease did not meet our threshold for statistical significance.
Prioritizing Covid-19 research is critical to combating the pandemic [ 1 ]. The medical community needs and expects the quick dissemination of Covid-19 research. However, hasty research may result in suboptimal study designs, though some have argued for the need to balance scientific rigor for speed [ 11 ]. Similarly, Kim et. al. recently argued in the Annals of Internal Medicine has stated that “Given the urgency of the situation, some limitations… may be acceptable, including the small sample size, use of an unvalidated surrogate end point, and lack of randomization or blinding” [ 8 ]. Still, researchers and publishers must use caution. In the last month alone, four high-profile Covid-19 articles have been retracted from the Annals of Internal Medicine , The Lancet , and NEJM due to inadequate scientific rigor [ 12 – 15 ]. We similarly observed a large increase in Covid-19 studies that did not have a control group, mostly case reports and series. As Covid-19 researchers have time to apply more rigorous methods to their studies, RCTs and studies with control groups will undoubtedly become more widespread. In the meantime, researchers and journal editors will need to balance the trade-off between accommodating the rapid dissemination of information with Covid-19 research that do not report a control group.
However, we were concerned to observe substitutions occurring at the expense of non-Covid-19 studies with a control group, with substitutions occurring almost entirely at the expense of RCTs. In comparison, we observed minimal changes among non-Covid-19 studies without a control group. If we project these changes over a course of 6 months (a conservative time frame for the Covid-19 pandemic), non-Covid-19 studies with a control group could decrease by 60 and non-Covid-19 RCTs by 70 in these three medical journals combined. Notably, in the field of obstetrics/gynecology, zero studies were published in the post-Covid-19 era despite constituting 4% of full-length publications prior to the outbreak. The decline in non-Covid-19 publications with a control group and especially RCTs likely has multiple reasons. Publication of already accepted studies may be postponed in lieu of emerging Covid-19 research. Journals in the JAMA Network have received 53% more submissions in the first quarter of 2020 than in the first quarter of 2019 [ 16 ]. The flood of submissions and the demand for Covid-19 related work presents publishers and editors with the dilemma of accepting fewer non-Covid-19 publications, quality notwithstanding.
Reviewers and editors might also perceive non-Covid-19 research as overall less relevant given the pandemic. The WHO, national disease organizations, and media have Covid-19 in the forefront of public health. Since January, 2020, COVID-19 papers have been downloaded more than 150 million times, according to the International Association of Scientific, Technical and Medical Publishers [ 17 ]. Major publications have a responsibility to assess the interest of their readership and adjust their publication profile accordingly. Finally, authors might delay submissions until after the pandemic subsides because of unavoidable disruptions in their research or a perception that non-Covid-19 research is viewed less favorably. Many laboratories and non-Covid-19 clinical trials have closed due to social distancing [ 18 ]. Additionally, resources and priorities may have shifted away from non-Covid-19 research to support Covid-19 studies [ 19 ].
Unfortunately, these rejections and delays contribute to a growing backlog of unpublished non-Covid-19 research, hindering future dissemination. The backlog will likely worsen as non-Covid-19 research resumes with long-term negative consequences to published research [ 9 ]. Disruptions in medical research attributable to Covid-19 could thus mirror public health experts’ concerns about delays in non-Covid-19 medical care [ 20 ].
Limitations of our study include using a simple heuristic for assessing study design (e.g., RCT versus not, controlled versus uncontrolled), not accounting for contemporaneous idiosyncratic events (e.g., vaping), and not observing submitted but unpublished work. Additionally, we did not produce a written protocol and preplanned analysis prior to data collection. We also limited our sample to three select high impact journals, and our results do not necessarily generalize to the entire medical literature. We were unable to estimate changes pre- and post-Covid-19 by organ system with precision, likely owing to small sample size. Finally, we used the 3 months preceding the start of Covid-19 to assess the pre-Covid-19 baseline for the three journals of interest. However this surrogate may not be a suitable counterfactual for these journals in the absence of Covid-19. Thus, our findings should be corroborated in a wider sample of journals and time periods.
Substitutions of non-Covid-19 research are inevitable. To alleviate delays in publication, editors could consider establishing dedicated channels for Covid-19 studies that do not compete with non-Covid-19 studies.
Supporting information
S1 appendix. additional details for “competing with a pandemic: research quality in a time of covid-19”..
https://doi.org/10.1371/journal.pone.0238831.s001
Acknowledgments
We would like to thank Gemma Lin for her review of the manuscript.
- View Article
- Google Scholar
- 10. Mittelhammer RC, Judge GG, Miller DJ. Econometric Foundations. Cambridge University Press; 2000. 73–74 p.
- 17. COVID-19 Research Downloaded More Than 150 Million Times, Reports STM [Internet]. International Association of Scientific, Technical and Medical Publishers. [cited 2020 Jul 27]. Available from: https://www.prnewswire.co.uk/news-releases/covid-19-research-downloaded-more-than-150-million-times-reports-stm-824020806.html
- 20. Wong, Laura E, Hawkins, Jessica E, Langness S, Murrell, Karen L, Iris, Patricia, Sammann A. Where Are All the Patients? Addressing Covid-19 Fear to Encourage Sick Patients to Seek Emergency Care. NEJM Catal. 2020;

- < Previous
Home > Public Health > IPH_CAPSTONE > 126
Public Health Capstone Projects
Research proposal: covid-19 pandemic and birth experiences: describing the relationship between policies and the birth experiences of georgia mothers.
Katherine Thornburgh Follow
Date of Award
Fall 1-8-2021
Degree Type
Capstone Project
Degree Name
Master of Public Health (MPH)
Public Health
First Advisor
Sarah McCool, PhD, MPH, MHA
Second Advisor
Kathleen Baggett, Ph.D.
RESEARCH PROPOSAL: COVID-19 PANDEMIC AND BIRTH EXPERIENCES: DESCRIBING THE RELATIONSHIP BETWEEN POLICIES AND THE BIRTH EXPERIENCES OF GEORGIA MOTHERS
KATHERINE RAECHEL THORNBURGH
B.S., KENNESAW STATE UNIVERSITY
December 5, 2020
INTRODUCTION: A pandemic such as COVID-19 increases stress during pregnancy or early development that can have an adverse effect on the health of an individual. Additionally, COVID-19 affects pregnancy and birth experiences by reducing the number of support personnel and the number of in-person appointments, and possibly potentially separating mother and newborn in the case of a suspected or confirmed COVID-19 status.
The purpose of this capstone is to present a compelling research proposal titled, “COVID-19 Pandemic and Birth Experiences: Describing the Relationship Between Policies and the Birth Experiences of Georgia Mothers” with the following aims:
Specific Aim 1: Describe mothers’ perspectives of COVID-19 policies on their birth experiences and birth plans. To meet this aim, a semi-structured interview will be conducted that inquires on the changes made to mothers’ intended birth plan and how COVID-19 policies affected mothers’ birth experiences—both negatively and positively.
Specific Aim 2: Describe mothers’ perceptions of fair and equitable treatment during pregnancy. To meet this aim, a semi-structured interview will be given to respondents that inquires on personal perceptions of fair and equitable treatment. To meet this aim, respondents will be asked if they felt that all of their questions regarding their pregnancy were being answered, if they felt adequately prepared for labor and post-partum care, and whether they felt their birth experiences met their expectations.
This qualitative data will describe general themes in perception of quality of care and equitable care for various racial, socioeconomic, and insurance coverage status groups.
METHODS: A descriptive, cross-sectional study will be conducted in Georgia, statewide, to describe mothers’ perspectives of COVID-19 policies on their birth experiences, birth plans, and their perceptions of fair and equitable treatment during pregnancy, labor and delivery and post-partum. The study sample will be acquired via an adapted State Electronic Notifiable Disease Surveillance System (SENDSS) case investigation form. Semi-structured interviews will be conducted.
https://doi.org/10.57709/20616398
Recommended Citation
Thornburgh, Katherine, "Research Proposal: COVID-19 Pandemic and Birth Experiences: Describing the Relationship Between Policies and the Birth Experiences of Georgia Mothers." , Georgia State University, 2021. doi: https://doi.org/10.57709/20616398
File Upload Confirmation
Since December 15, 2020
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
- Submit Project
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Why the Pandemic Probably Started in a Lab, in 5 Key Points

By Alina Chan
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “Viral: The Search for the Origin of Covid-19.”
This article has been updated to reflect news developments.
On Monday, Dr. Anthony Fauci returned to the halls of Congress and testified before the House subcommittee investigating the Covid-19 pandemic. He was questioned about several topics related to the government’s handling of Covid-19, including how the National Institute of Allergy and Infectious Diseases, which he directed until retiring in 2022, supported risky virus work at a Chinese institute whose research may have caused the pandemic.
For more than four years, reflexive partisan politics have derailed the search for the truth about a catastrophe that has touched us all. It has been estimated that at least 25 million people around the world have died because of Covid-19, with over a million of those deaths in the United States.
Although how the pandemic started has been hotly debated, a growing volume of evidence — gleaned from public records released under the Freedom of Information Act, digital sleuthing through online databases, scientific papers analyzing the virus and its spread, and leaks from within the U.S. government — suggests that the pandemic most likely occurred because a virus escaped from a research lab in Wuhan, China. If so, it would be the most costly accident in the history of science.
Here’s what we now know:
1 The SARS-like virus that caused the pandemic emerged in Wuhan, the city where the world’s foremost research lab for SARS-like viruses is located.
- At the Wuhan Institute of Virology, a team of scientists had been hunting for SARS-like viruses for over a decade, led by Shi Zhengli.
- Their research showed that the viruses most similar to SARS‑CoV‑2, the virus that caused the pandemic, circulate in bats that live r oughly 1,000 miles away from Wuhan. Scientists from Dr. Shi’s team traveled repeatedly to Yunnan province to collect these viruses and had expanded their search to Southeast Asia. Bats in other parts of China have not been found to carry viruses that are as closely related to SARS-CoV-2.

The closest known relatives to SARS-CoV-2 were found in southwestern China and in Laos.
Large cities
Mine in Yunnan province
Cave in Laos
South China Sea

The closest known relatives to SARS-CoV-2
were found in southwestern China and in Laos.
philippines

The closest known relatives to SARS-CoV-2 were found
in southwestern China and Laos.
Sources: Sarah Temmam et al., Nature; SimpleMaps
Note: Cities shown have a population of at least 200,000.

There are hundreds of large cities in China and Southeast Asia.

There are hundreds of large cities in China
and Southeast Asia.

The pandemic started roughly 1,000 miles away, in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away,
in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away, in Wuhan,
home to the world’s foremost SARS-like virus research lab.
- Even at hot spots where these viruses exist naturally near the cave bats of southwestern China and Southeast Asia, the scientists argued, as recently as 2019 , that bat coronavirus spillover into humans is rare .
- When the Covid-19 outbreak was detected, Dr. Shi initially wondered if the novel coronavirus had come from her laboratory , saying she had never expected such an outbreak to occur in Wuhan.
- The SARS‑CoV‑2 virus is exceptionally contagious and can jump from species to species like wildfire . Yet it left no known trace of infection at its source or anywhere along what would have been a thousand-mile journey before emerging in Wuhan.
2 The year before the outbreak, the Wuhan institute, working with U.S. partners, had proposed creating viruses with SARS‑CoV‑2’s defining feature.
- Dr. Shi’s group was fascinated by how coronaviruses jump from species to species. To find viruses, they took samples from bats and other animals , as well as from sick people living near animals carrying these viruses or associated with the wildlife trade. Much of this work was conducted in partnership with the EcoHealth Alliance, a U.S.-based scientific organization that, since 2002, has been awarded over $80 million in federal funding to research the risks of emerging infectious diseases.
- The laboratory pursued risky research that resulted in viruses becoming more infectious : Coronaviruses were grown from samples from infected animals and genetically reconstructed and recombined to create new viruses unknown in nature. These new viruses were passed through cells from bats, pigs, primates and humans and were used to infect civets and humanized mice (mice modified with human genes). In essence, this process forced these viruses to adapt to new host species, and the viruses with mutations that allowed them to thrive emerged as victors.
- By 2019, Dr. Shi’s group had published a database describing more than 22,000 collected wildlife samples. But external access was shut off in the fall of 2019, and the database was not shared with American collaborators even after the pandemic started , when such a rich virus collection would have been most useful in tracking the origin of SARS‑CoV‑2. It remains unclear whether the Wuhan institute possessed a precursor of the pandemic virus.
- In 2021, The Intercept published a leaked 2018 grant proposal for a research project named Defuse , which had been written as a collaboration between EcoHealth, the Wuhan institute and Ralph Baric at the University of North Carolina, who had been on the cutting edge of coronavirus research for years. The proposal described plans to create viruses strikingly similar to SARS‑CoV‑2.
- Coronaviruses bear their name because their surface is studded with protein spikes, like a spiky crown, which they use to enter animal cells. T he Defuse project proposed to search for and create SARS-like viruses carrying spikes with a unique feature: a furin cleavage site — the same feature that enhances SARS‑CoV‑2’s infectiousness in humans, making it capable of causing a pandemic. Defuse was never funded by the United States . However, in his testimony on Monday, Dr. Fauci explained that the Wuhan institute would not need to rely on U.S. funding to pursue research independently.

The Wuhan lab ran risky experiments to learn about how SARS-like viruses might infect humans.
1. Collect SARS-like viruses from bats and other wild animals, as well as from people exposed to them.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of human cells.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of
human cells.

In Defuse, the scientists proposed to add a furin cleavage site to the spike protein.
3. Create new coronaviruses by inserting spike proteins or other features that could make the viruses more infectious in humans.

4. Infect human cells, civets and humanized mice with the new coronaviruses, to determine how dangerous they might be.

- While it’s possible that the furin cleavage site could have evolved naturally (as seen in some distantly related coronaviruses), out of the hundreds of SARS-like viruses cataloged by scientists, SARS‑CoV‑2 is the only one known to possess a furin cleavage site in its spike. And the genetic data suggest that the virus had only recently gained the furin cleavage site before it started the pandemic.
- Ultimately, a never-before-seen SARS-like virus with a newly introduced furin cleavage site, matching the description in the Wuhan institute’s Defuse proposal, caused an outbreak in Wuhan less than two years after the proposal was drafted.
- When the Wuhan scientists published their seminal paper about Covid-19 as the pandemic roared to life in 2020, they did not mention the virus’s furin cleavage site — a feature they should have been on the lookout for, according to their own grant proposal, and a feature quickly recognized by other scientists.
- Worse still, as the pandemic raged, their American collaborators failed to publicly reveal the existence of the Defuse proposal. The president of EcoHealth, Peter Daszak, recently admitted to Congress that he doesn’t know about virus samples collected by the Wuhan institute after 2015 and never asked the lab’s scientists if they had started the work described in Defuse. In May, citing failures in EcoHealth’s monitoring of risky experiments conducted at the Wuhan lab, the Biden administration suspended all federal funding for the organization and Dr. Daszak, and initiated proceedings to bar them from receiving future grants. In his testimony on Monday, Dr. Fauci said that he supported the decision to suspend and bar EcoHealth.
- Separately, Dr. Baric described the competitive dynamic between his research group and the institute when he told Congress that the Wuhan scientists would probably not have shared their most interesting newly discovered viruses with him . Documents and email correspondence between the institute and Dr. Baric are still being withheld from the public while their release is fiercely contested in litigation.
- In the end, American partners very likely knew of only a fraction of the research done in Wuhan. According to U.S. intelligence sources, some of the institute’s virus research was classified or conducted with or on behalf of the Chinese military . In the congressional hearing on Monday, Dr. Fauci repeatedly acknowledged the lack of visibility into experiments conducted at the Wuhan institute, saying, “None of us can know everything that’s going on in China, or in Wuhan, or what have you. And that’s the reason why — I say today, and I’ve said at the T.I.,” referring to his transcribed interview with the subcommittee, “I keep an open mind as to what the origin is.”
3 The Wuhan lab pursued this type of work under low biosafety conditions that could not have contained an airborne virus as infectious as SARS‑CoV‑2.
- Labs working with live viruses generally operate at one of four biosafety levels (known in ascending order of stringency as BSL-1, 2, 3 and 4) that describe the work practices that are considered sufficiently safe depending on the characteristics of each pathogen. The Wuhan institute’s scientists worked with SARS-like viruses under inappropriately low biosafety conditions .

In the United States, virologists generally use stricter Biosafety Level 3 protocols when working with SARS-like viruses.
Biosafety cabinets prevent
viral particles from escaping.
Viral particles
Personal respirators provide
a second layer of defense against breathing in the virus.
DIRECT CONTACT
Gloves prevent skin contact.
Disposable wraparound
gowns cover much of the rest of the body.

Personal respirators provide a second layer of defense against breathing in the virus.
Disposable wraparound gowns
cover much of the rest of the body.
Note: Biosafety levels are not internationally standardized, and some countries use more permissive protocols than others.

The Wuhan lab had been regularly working with SARS-like viruses under Biosafety Level 2 conditions, which could not prevent a highly infectious virus like SARS-CoV-2 from escaping.
Some work is done in the open air, and masks are not required.
Less protective equipment provides more opportunities
for contamination.

Some work is done in the open air,
and masks are not required.
Less protective equipment provides more opportunities for contamination.
- In one experiment, Dr. Shi’s group genetically engineered an unexpectedly deadly SARS-like virus (not closely related to SARS‑CoV‑2) that exhibited a 10,000-fold increase in the quantity of virus in the lungs and brains of humanized mice . Wuhan institute scientists handled these live viruses at low biosafet y levels , including BSL-2.
- Even the much more stringent containment at BSL-3 cannot fully prevent SARS‑CoV‑2 from escaping . Two years into the pandemic, the virus infected a scientist in a BSL-3 laboratory in Taiwan, which was, at the time, a zero-Covid country. The scientist had been vaccinated and was tested only after losing the sense of smell. By then, more than 100 close contacts had been exposed. Human error is a source of exposure even at the highest biosafety levels , and the risks are much greater for scientists working with infectious pathogens at low biosafety.
- An early draft of the Defuse proposal stated that the Wuhan lab would do their virus work at BSL-2 to make it “highly cost-effective.” Dr. Baric added a note to the draft highlighting the importance of using BSL-3 to contain SARS-like viruses that could infect human cells, writing that “U.S. researchers will likely freak out.” Years later, after SARS‑CoV‑2 had killed millions, Dr. Baric wrote to Dr. Daszak : “I have no doubt that they followed state determined rules and did the work under BSL-2. Yes China has the right to set their own policy. You believe this was appropriate containment if you want but don’t expect me to believe it. Moreover, don’t insult my intelligence by trying to feed me this load of BS.”
- SARS‑CoV‑2 is a stealthy virus that transmits effectively through the air, causes a range of symptoms similar to those of other common respiratory diseases and can be spread by infected people before symptoms even appear. If the virus had escaped from a BSL-2 laboratory in 2019, the leak most likely would have gone undetected until too late.
- One alarming detail — leaked to The Wall Street Journal and confirmed by current and former U.S. government officials — is that scientists on Dr. Shi’s team fell ill with Covid-like symptoms in the fall of 2019 . One of the scientists had been named in the Defuse proposal as the person in charge of virus discovery work. The scientists denied having been sick .
4 The hypothesis that Covid-19 came from an animal at the Huanan Seafood Market in Wuhan is not supported by strong evidence.
- In December 2019, Chinese investigators assumed the outbreak had started at a centrally located market frequented by thousands of visitors daily. This bias in their search for early cases meant that cases unlinked to or located far away from the market would very likely have been missed. To make things worse, the Chinese authorities blocked the reporting of early cases not linked to the market and, claiming biosafety precautions, ordered the destruction of patient samples on January 3, 2020, making it nearly impossible to see the complete picture of the earliest Covid-19 cases. Information about dozens of early cases from November and December 2019 remains inaccessible.
- A pair of papers published in Science in 2022 made the best case for SARS‑CoV‑2 having emerged naturally from human-animal contact at the Wuhan market by focusing on a map of the early cases and asserting that the virus had jumped from animals into humans twice at the market in 2019. More recently, the two papers have been countered by other virologists and scientists who convincingly demonstrate that the available market evidence does not distinguish between a human superspreader event and a natural spillover at the market.
- Furthermore, the existing genetic and early case data show that all known Covid-19 cases probably stem from a single introduction of SARS‑CoV‑2 into people, and the outbreak at the Wuhan market probably happened after the virus had already been circulating in humans.

An analysis of SARS-CoV-2’s evolutionary tree shows how the virus evolved as it started to spread through humans.
SARS-COV-2 Viruses closest
to bat coronaviruses
more mutations

Source: Lv et al., Virus Evolution (2024) , as reproduced by Jesse Bloom

The viruses that infected people linked to the market were most likely not the earliest form of the virus that started the pandemic.

- Not a single infected animal has ever been confirmed at the market or in its supply chain. Without good evidence that the pandemic started at the Huanan Seafood Market, the fact that the virus emerged in Wuhan points squarely at its unique SARS-like virus laboratory.
5 Key evidence that would be expected if the virus had emerged from the wildlife trade is still missing.

In previous outbreaks of coronaviruses, scientists were able to demonstrate natural origin by collecting multiple pieces of evidence linking infected humans to infected animals.
Infected animals
Earliest known
cases exposed to
live animals
Antibody evidence
of animals and
animal traders having
been infected
Ancestral variants
of the virus found in
Documented trade
of host animals
between the area
where bats carry
closely related viruses
and the outbreak site

Infected animals found
Earliest known cases exposed to live animals
Antibody evidence of animals and animal
traders having been infected
Ancestral variants of the virus found in animals
Documented trade of host animals
between the area where bats carry closely
related viruses and the outbreak site

For SARS-CoV-2, these same key pieces of evidence are still missing , more than four years after the virus emerged.

For SARS-CoV-2, these same key pieces of evidence are still missing ,
more than four years after the virus emerged.
- Despite the intense search trained on the animal trade and people linked to the market, investigators have not reported finding any animals infected with SARS‑CoV‑2 that had not been infected by humans. Yet, infected animal sources and other connective pieces of evidence were found for the earlier SARS and MERS outbreaks as quickly as within a few days, despite the less advanced viral forensic technologies of two decades ago.
- Even though Wuhan is the home base of virus hunters with world-leading expertise in tracking novel SARS-like viruses, investigators have either failed to collect or report key evidence that would be expected if Covid-19 emerged from the wildlife trade . For example, investigators have not determined that the earliest known cases had exposure to intermediate host animals before falling ill. No antibody evidence shows that animal traders in Wuhan are regularly exposed to SARS-like viruses, as would be expected in such situations.
- With today’s technology, scientists can detect how respiratory viruses — including SARS, MERS and the flu — circulate in animals while making repeated attempts to jump across species . Thankfully, these variants usually fail to transmit well after crossing over to a new species and tend to die off after a small number of infections. In contrast, virologists and other scientists agree that SARS‑CoV‑2 required little to no adaptation to spread rapidly in humans and other animals . The virus appears to have succeeded in causing a pandemic upon its only detected jump into humans.
The pandemic could have been caused by any of hundreds of virus species, at any of tens of thousands of wildlife markets, in any of thousands of cities, and in any year. But it was a SARS-like coronavirus with a unique furin cleavage site that emerged in Wuhan, less than two years after scientists, sometimes working under inadequate biosafety conditions, proposed collecting and creating viruses of that same design.
While several natural spillover scenarios remain plausible, and we still don’t know enough about the full extent of virus research conducted at the Wuhan institute by Dr. Shi’s team and other researchers, a laboratory accident is the most parsimonious explanation of how the pandemic began.
Given what we now know, investigators should follow their strongest leads and subpoena all exchanges between the Wuhan scientists and their international partners, including unpublished research proposals, manuscripts, data and commercial orders. In particular, exchanges from 2018 and 2019 — the critical two years before the emergence of Covid-19 — are very likely to be illuminating (and require no cooperation from the Chinese government to acquire), yet they remain beyond the public’s view more than four years after the pandemic began.
Whether the pandemic started on a lab bench or in a market stall, it is undeniable that U.S. federal funding helped to build an unprecedented collection of SARS-like viruses at the Wuhan institute, as well as contributing to research that enhanced them . Advocates and funders of the institute’s research, including Dr. Fauci, should cooperate with the investigation to help identify and close the loopholes that allowed such dangerous work to occur. The world must not continue to bear the intolerable risks of research with the potential to cause pandemics .
A successful investigation of the pandemic’s root cause would have the power to break a decades-long scientific impasse on pathogen research safety, determining how governments will spend billions of dollars to prevent future pandemics. A credible investigation would also deter future acts of negligence and deceit by demonstrating that it is indeed possible to be held accountable for causing a viral pandemic. Last but not least, people of all nations need to see their leaders — and especially, their scientists — heading the charge to find out what caused this world-shaking event. Restoring public trust in science and government leadership requires it.
A thorough investigation by the U.S. government could unearth more evidence while spurring whistleblowers to find their courage and seek their moment of opportunity. It would also show the world that U.S. leaders and scientists are not afraid of what the truth behind the pandemic may be.
More on how the pandemic may have started

Where Did the Coronavirus Come From? What We Already Know Is Troubling.
Even if the coronavirus did not emerge from a lab, the groundwork for a potential disaster had been laid for years, and learning its lessons is essential to preventing others.
By Zeynep Tufekci

Why Does Bad Science on Covid’s Origin Get Hyped?
If the raccoon dog was a smoking gun, it fired blanks.
By David Wallace-Wells

A Plea for Making Virus Research Safer
A way forward for lab safety.
By Jesse Bloom
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Alina Chan ( @ayjchan ) is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “ Viral : The Search for the Origin of Covid-19.” She was a member of the Pathogens Project , which the Bulletin of the Atomic Scientists organized to generate new thinking on responsible, high-risk pathogen research.
- Share full article
Advertisement
- Reference Manager
- Simple TEXT file
People also looked at
Review article, challenges during review of covid-19 research proposals: experience of faculty of medicine, ain shams university research ethics committee, egypt.

- 1 Faculty of Medicine, Ain Shams University, Cairo, Egypt
- 2 Misr International University, US Naval Medical Research Unit No.3 (NAMRU-3), Cairo, Egypt
- 3 Faculty of Medicine, October 6 University, Giza, Egypt
The COVID-19 pandemic resulted in an overwhelming increase in research studies submitted to research ethics committees (RECs) presenting many ethical challenges. This article aims to report the challenges encountered during review of COVID-19 research and the experience of the Faculty of Medicine, Ain Shams University Research Ethics Committee (FMASU REC). From April 10, 2020, until October 13, 2020, the FMASU REC reviewed 98 COVID-19 research protocols. This article addressed the question of how to face an overwhelming amount of research submitted to the REC while applying the required ethical principles. Ethical challenges included a new accelerated mode of review, online meetings, balance of risks vs. benefits, measures to mitigate risks, co-enrolment in different studies, protection of a vulnerable COVID-19 population, accelerated decisions, online research, how to handle informed consent during the pandemic, and justification of placebo arm.
Introduction
The majority of the RECs in North African countries are registered with the Office for Human Research Protections and have Federal Wide Assurance (FWA) active numbers ( 1 ). Egypt has a National Ethics Committee, active institutional committees and the Egyptian Medical Research Regulation Law for the regulation of clinical trials and human research ethics issued December 2020; the Egyptian National Ethical Committee collaborates with the United Nations Educational, Scientific and Cultural Organization ( 2 ).
The FMASU REC was established in October 2007, to review research conducted at the Faculty of Medicine, Ain Shams University, in Cairo, Egypt. It holds a Federal Wide Assurance Number (FWA 00017585). The committee trained 220 staff members as reviewers working in 32 faculty departments over 23 training events. Since its establishment, the FMASU REC reviewed 414 international and multicentre projects, 5,033 theses, and free research. Since April 10, 2020, the FMASU REC reviewed 98 COVID-19 research studies, Figure 1 .
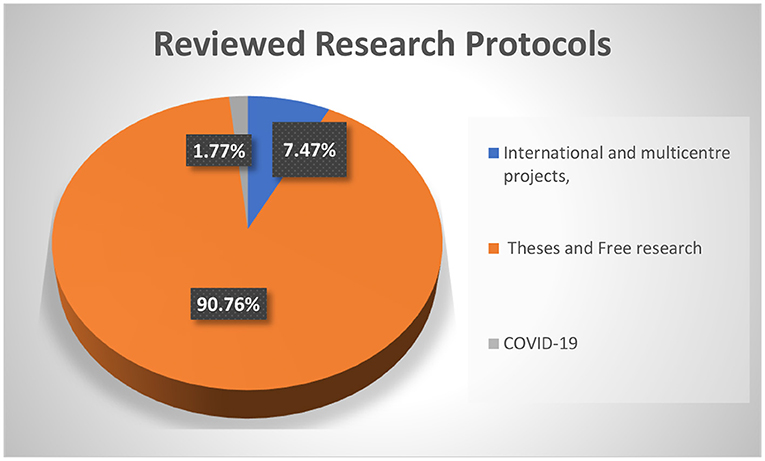
Figure 1 . FMASU REC Workload from January 1st, 2008 to October 13th, 2020.
During the COVID-19 pandemic in the year 2020, investigators began research to understand the novel virus, its epidemiology and pathogenicity, as well as to find ways for prevention and control, including discovering a treatment and/or vaccine. Worldwide, more than 4,900 studies and trials have been registered on “ Clinicaltrials.gov ” since the start of the pandemic ( 3 ). This rise in the number of emerging COVID-19 research projects has recently resulted in an overwhelming number of research project submissions to RECs.
To ensure ethical research during the COVID-19 pandemic, the World Health Organization (WHO) summarized the key universal ethical standards that should be adhered to by researchers, review bodies, funders, publishers, and manufacturers during a pandemic ( 4 ), identifying the main ethical standards as scientific validity, reasonable risk-benefit ratio, fair and voluntary participation, and independent review ( 5 ).
The European Network of Research Ethics Committees (EUREC) issued a statement that was adopted by the EUREC Board on April 27, 2020, stressing the fact that the administrative processes for reviewing research protocols during the COVID-19 pandemic must be accelerated and simplified if these protocols are related to the treatment, prevention or diagnosis of infections caused by SARS-CoV-2 ( 6 ). However, all research must be guided by the principle that RECs will not compromise the quality of the review process under these extraordinarily stressful circumstances. Furthermore, an accelerated procedure cannot be at the expense of the safety of research participants. The recognized ethical principles must always be respected, and the free and informed consent procedure must remain in accordance with international and national regulations.
In Egypt, there are 115 university hospitals ( 7 ) conducting research on human beings which needs approval from institutional RECs which are either internationally recognized and have an international FWA number and/or are registered with the Ministry of Health and Population (MOHP), or are newly developed and have been submitted for registry with the MOHP. International projects need other final approval from the MOHP REC.
The Clinical Medical Research Regulation Law (the Egyptian law for the conduct of research) was issued on December 23, 2020; its bylaws are currently being written. The Egyptian law is aligned with international guidelines for health research ethics review. The research studies protocols described in this manuscript were submitted during the period April 10 to October 13, 2020, to Ain Shams REC and were reviewed according to the international guidelines.
This article tried to answer the question of how the REC can effectively apply ethical principles when faced with an overwhelming number of research projects submitted.
The aim of this article is to report the challenges encountered and the experience of the FMASU REC during review of COVID-19 research, starting from April 10 to October 13, 2020, and to give an overview about the challenges that the committee faced and how it overcame them.
Modified Standard Operating Procedures
The article tried to illustrate how a governmental university REC in a low-middle income country modified its standard operating procedures (SOPs) to cope with a fast-track review of the overwhelming COVID-19 research and continue reviewing non-COVID-19 research. During the first wave of the pandemic there were no international guidelines for reviewing COVID-19 research. This challenge was increased by a scarcity of information about the disease, governmental lockdown periods, and lack of extra budget allocation.
The FMASU REC was confronted by multiple challenges in reviewing COVID-19 research during the pandemic, necessitating out-of-the box solutions to maintain an effective, accelerated review while at the same time practicing the ethical principles required.
The researchers, as well as the REC members, were encouraged to transform these challenges into opportunities. The SOPs followed by the REC were updated, regarding protocol submission changes to adopt digital submission route, rather than hard-copy paper submissions. Training of the employees on the use of digital technology for submissions and archiving followed. An electronic signature for the head of the committee was introduced. An accelerated, fast-track mode for reviewing protocols was adopted to cope with the pace of the pandemic. While the reviewers had previously been allowed up to 1 month for response for randomized controlled trials (RCTs), they were now expected to respond within one-seven days during the pandemic. The expedited process was meant to help in generating desperately needed knowledge out of the submitted research.
The REC resorted to on-line conferencing to overcome the inability to hold face-to-face meetings due to the Faculty lockdown. The first wave of research was received on April 10, 2020, with seven research projects reviewed in two online meetings over 3 days, including five clinical trials and two observational studies. That new mode of reviewing was dynamic, accelerated, and fast-tracked, in accordance with international guidelines and the REC's updated SOPs.
As the number of submitted research protocols increased rapidly, the REC had to increase the frequency of meetings to every other day, then every week or 2 weeks instead of the previous monthly schedule. Reviewing was done in a shorter time as the institution and investigators were expecting a rapid response. The usual review process that was adhered to by the REC was as follows: all the above minimal-risk protocols were initially reviewed by two reviewers and then discussed in full board meetings. To acquire a faster review track of the COVID-19-related proposals, clinical trials, or repurposed drugs, the number of initial reviewers was increased to three members, then discussed in full board online meetings. The number of members attending the virtual meetings ranged from 9 to 13 members, out of the 15 members comprising the committee.
For this article we reviewed the list of all protocols submitted to FMASU REC for review during the COVID-19 time from April 10, 2020, until October 13, 2020. We listed the titles, principal investigators (PI) names, date of submission and date of response to the investigators. We analyzed the frequencies from these data. We also reviewed the meeting minutes to pin out the most interesting and challenging issues that were discussed during the meetings. Additionally, we reviewed the current procedures and changes that were instituted to the SOPs. Finally, we asked the members to provide their input about their concerns in the review process during the COVID-19 time. Last, we incorporated all the data into the article.
Review Processes
Reviewing research during COVID-19 pandemic lockdown included shortened average duration of review, rapid request for clarifications and reply of investigators and quick provision of decisions. The duration of review was shortened to a minimum of 1 day and a maximum of 7 days. Before the pandemic, for more than minimal risk (low risk studies) and commercially-sponsored studies, the REC adopted a two-reviewer system, followed by discussion by the full Board. During the pandemic, to accomplish a shorter review time, this system was replaced by a three-member review, followed by the online meeting. As for minimal risk studies, the pre-pandemic system was also a two-reviewer, expedited review system, while during the pandemic for COVID-19 protocols, two reviewers were still assigned to review each protocol, but in a shorter reviewing period of 1-7 days.
To overcome the challenges of the short review time, the reviewing process of COVID-19 research stressed the rationale or justification as tackled by many researchers all over the world, the research question, hypothesis, social value, and benefits to the community. The novelty of the research idea was also an important point of discussion during the review process.
“Good science is itself an ethical requirement, as it is meaningless to apply ethical principles to a scientifically flawed product or plan. Bad science can only be bad ethics” ( 8 ). A rigorous revision of the research methodology was conducted, including study design, sample size and type, study procedures, randomization, and blinding. Many studies needed redesigning to specify inclusion and exclusion criteria of subjects, or to rigorously define the diagnosis of mild, moderate, and severe COVID-19 cases according to the National Guidelines reported and updated by the Egyptian MOHP.
Ensuring the well-being of researchers and research participants in the context of a pandemic was a very important objective of the REC. For research participants' well-being, hospital beds and equipment disinfection were under control of the Infection Control Unit, thus conforming to all international guidelines. As for mental health studies (some included healthcare professionals as well as patients), the committee recommended providing medical assistance for those who had high scores (e.g., recommending adding a paragraph in the questionnaire telling participants that if they had high scores for depression, to seek medical consultation). As for researchers, the REC insisted on following international, local governmental, and institutional recommendations. They were supplied with personal protective equipment including surgical, N95 masks, face shields, and goggles.
The REC was rigorous about sample size calculation in the protocol, urging the investigators to have a precise, predefined sample-size calculation, in order to receive REC approval of the study. As a standard procedure, the investigators were required, as a prerequisite before submission to the REC, to refer to the accredited statistics unit at the Department of community medicine in FMASU, to obtain the sample size calculation for any research. While some researchers chose to conduct a pilot study and a convenience sampling because of lack of sufficient data for new or repurposed drugs, the investigators had to provide strong justifications in such instances. The REC required an interim analysis and power calculation, to see if the sample size was large enough, or needed revision to find out if the efficacy of the tested drugs had been reached.
Special Concerns During Review
The balance of risks and benefits is a pivotal element for the protection of human subjects in research. The REC exerted a great effort to mitigate research risks to provide maximum possible protection of research participants. The REC members spent long hours reviewing recent COVID 19-related publications, with special emphasis on adverse events reported involving drugs under trial and drug interactions. Clarifications were required on how to minimize the risks of these side effects, and suggestions were offered to the researchers. For instance, REC recommended additional investigations such as a baseline electrocardiogram, complete blood counts, requested exclusion of high-risk participants, or recommended increased frequency of monitoring visits.
The COVID-19 submitted protocols posted a novel risk-benefit evaluation to the reviewers. For example, in many instances, the REC could not ignore the risk to the researchers who had to interact face-to-face with COVID-19 patients in intensive care units (ICU). The REC had to ensure performance of enrolment and study procedures in unconventional circumstances, such as instances when researchers might not have been allowed in the research setting. The ICU physicians and nurses had to be trained to perform the study procedures. The PI had to keep close contact with the ICU staff and get monitoring reports about the enrolled participants. Whenever possible, the PI could see the patients following the standard safety infection control precautions.
One of the challenges faced by the FMASU REC was the lack of or insufficient animal studies and combining of Phases II and III for testing new drugs. The REC did not encounter Phase I protocols at that time. While the side effects and risks of the proposed therapies were not yet fully studied, Phase II usually includes more patients, and combining Phases II and III usually results in larger sample sizes than Phase II alone.
The REC responded by evaluating the risks and benefits, while maintaining strict requirements for risk minimization. The direct, potential patient benefit was the hope for effectiveness of new drugs, and the indirect benefit was withdrawing drugs from the list of potential drugs if proven non-effective.
The REC faced a big challenge with the large number of protocols, exceeding by far the routine work of the committee. Repurposed drugs, innovative drugs, and vaccines necessitate enormous steps to be approved. During the first 6 months of the pandemic, there was a relatively greater flow of RCTs, Phase III (2/5.85%) and Phase II (15/0.52%), compared to the period before the pandemic. The majority of studies were low risk observational studies (79.86%). Low risk studies are usually reviewed in an expedited manner by two reviewers, but in a shorter reviewing period of 1-7 days. The duration of the initial review was shortened to a minimum of 1 day and a maximum of 7 days compared to a minimum 1-month clinical trial review time, according to the REC SOPs. The total review time in the first rush of protocols during the pandemic was 1 week, but later the total review time was within 1 month, depending on how rapidly the investigators responded to the REC's comments.
The REC members devoted all their time to pandemic work, as most of the submitted protocols, even the non-commercial research, were to find an effective treatment for the emerging COVID-19 disease, either through using a repurposed drug, steroids, or antiviral drugs used earlier in management of Ebola virus, HCV, HIV, or antimalarial drugs. The flow of routine research as multicentre studies between Egyptian research centers, international centers and single center, non-commercial international project submissions, amendments, renewals and theses was slower than before the pandemic, but was reviewed in the same, accelerated manner.
The thesis topics submitted during the early wave of the COVID-19 pandemic were not yet related to the pandemic, but later in 2020 the topics were related to COVID-19.
The refusal rate was minimal; one study was deferred until more information could be obtained, as per the REC reviewers' request. Further details cannot be mentioned in this manuscript for protection of the confidentiality of the research topics.
The most frequent types of research submitted to the REC during the COVID-19 pandemic were observational studies (76.86%) to know the nature of this new emerging disease, followed by Phase III RCTs (5.85%), trying to find the most effective treatment through novel or repurposed drugs, such as drugs previously used in diseases other than COVID-19 such as EBOLA, Hepatitis C Virus, Human Immune Deficiency Virus and malaria Table 1 .
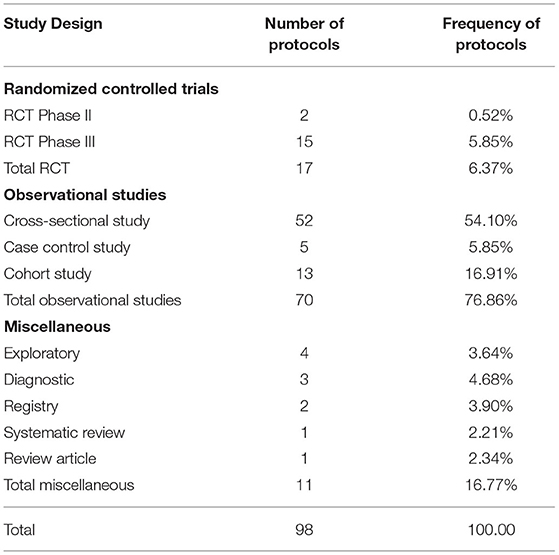
Table 1 . Frequency of clinical trial phases reviewed by FMASU REC from April to October 2020.
The protocols might not have been written as state of the art, as investigators submitted them in an expedited manner. This necessitated more frequent and more rapid than usual communication between the FMASU REC and the investigators. In some instances, the REC required the investigators to provide more information to be able to make informed decisions. The direct communication between the REC members and the investigators was effective in enhancing the quality of the protocols and their scientific validity, in view of the scarce and controversial information concerning COVID-19.
Defining the target population of COVID-19 patients and the vulnerability of this population was another challenge. The investigators had to define their study population with regard to the severity of the disease, the state of consciousness, and addressing what the REC defined as a new vulnerability group; the COVID-19 patients were desperate for treatment and might have agreed to participate in any research project without proper consideration. The protection of moderate and severe cases of COVID-19, as vulnerable groups, was extremely important to the REC. Therefore, the REC insisted that mild and moderate cases give consent for themselves and did not allow a legally-authorized representative to give consent on their behalf.
Allowing enrolment of severe disease cases engendered a wide range of discussion. Although the severe cases were in great need of the benefit of any drug at a time when no proven cure was available, the opposing committee members were hesitant to allow severely ill cases to be enrolled in the studies, if the investigators could not provide enough preliminary evidence of a potential direct benefit. Some investigators requested that in severe cases, the ICU manager might sign the consent on behalf of the subjects, but the REC refused this idea and insisted that the patient be conscious enough to give his or her own consent. Otherwise, the investigators would have to obtain the legal guardian's consent outside the isolation hospital due to rules on who was allowed in an isolation hospital.
Reviewing Telemedicine Studies
The review process had previously been accomplished through hard copies and online communication, as per the preference of the involved REC reviewers. During the pandemic, the shift to electronic communication became mandatory among researchers, the REC administrative office, the REC board, and the reviewers. The institution administration, as well, supported this shift and provided online meeting platforms in support of the digital transformation.
The COVID-19 pandemic resulted in greater use of online surveys and telemedicine. Telemedicine for clinical care started in 2016 at the Faculty of Medicine, Ain Shams University in the Neurology Department to help communication with patients being seen in clinical practice and was later extended to include other departments. To counteract the effects of the lockdown due to COVID-19, FMASU offers different telemedicine services, including consultation and outpatient clinics. Seven departments offer these services: Family Medicine, Clinical Oncology, Internal Medicine, Psychiatry, Paediatrics, Geriatrics and Obstetrics and Gynaecology. Services are offered through a secure link, where data, images and laboratory results can be uploaded and stored in the patient's medical record. The REC received this new type of telemedicine research as another challenge, Table 2 . The use of online surveys to study the behavioral and psychiatric well-being of the community by different age groups, different study populations and in different places, was a new type of research for the REC to review, constituting 13% of the submitted COVID-19 research at that time and the second most frequent type of studies to be reviewed after therapeutic research (18%). The lack of experience in reviewing this type of research was challenging. Breeching of confidentiality and assurance were the major concerns. Additionally, telemedicine services are not common in developing countries like Egypt due to high illiteracy rate, 24.6% in July 2019 as announced by the Central Agency for Public Mobilization and Statistics ( 9 ). While the REC tried to ensure optimization of the research protocol and data collection and follow up, the REC experienced difficulties in interpretation of the PIs or physicians' instructions and data collection by phone. However, the REC also requested that the patient have an educated relative beside him to ensure proper comprehension of the instructions of the PI and for easier communication.
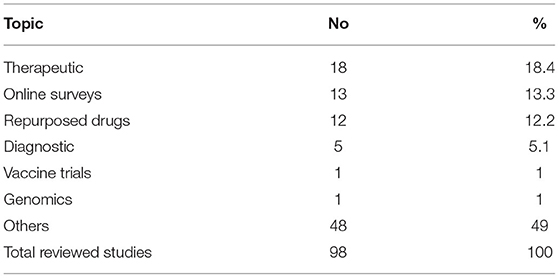
Table 2 . Most common COVID-19 research topics reviewed by FMASU REC from April to October 2020.
Ain Shams University includes eight hospitals and several health centers. The total number of beds affiliated with the university is 2,300. Research is allowed in all hospitals and health centers except the specialized hospitals (the Specialized Hospital on within the FMASU campus and the Obour Specialized Hospital in Obour city).
During the first wave of the pandemic from February to October 2020, two main hospitals were transformed into isolation hospitals for moderate and severe adult cases, Obour Specialized Hospital, and the Geriatric Hospital; one new hospital was established, Al Maidany Hospital. Ain Shams student dorms were transformed into hospitals to receive moderate COVID-19 cases. The Internal Medicine and Surgery Departments were allocated for adult COVID-19 cases and the Paediatric Department for pediatric COVID-19 cases. The rest of the hospitals offered the same services as usual, except that every patient being admitted was instructed to do a Polymerase Chain Reaction (PCR) test before admission. If the PCR was positive, the patient would be transferred to Obour Specialized Isolation Hospital.
Ain Shams University designated some of its hospitals and ICUs as “Isolation Hospitals” for the management of COVID-19 patients, which became the target for many, if not all, of the COVID-19 research studies. In view of the overwhelming number of research protocols, more than one research protocol targeted the same population in the same isolation hospital or ICU. In a few instances, the same PI was involved in more than one study. While there are no regulations against this, the REC was concerned about the involvement of the same patient in more than one study. The FMASU REC did not allow enrolment of subjects in more than one ongoing clinical trial. This decision conflicts with Cinnella and Gertner who reported that co-enrolment does not affect the safety of patients, the study outcome, or side effects, provided that the inclusion and exclusion criteria are appropriately set ( 10 , 11 ).
Before COVID-19, the REC stressed on selecting the appropriate control groups for the study, especially regarding how healthy controls were selected. For the COVID-19 protocols the controls were usually sick patients, hence risk mitigation was the major issue. During review of COVID-19 protocols, the REC noticed that several RCTs control groups did not receive interventional medication and had similar characteristics and inclusion criteria, e.g., the severity of the disease. To decrease the number of subjects included in the studies, the REC suggested the use of the same set of controls, whenever applicable and possible, in more than one study. This meant that the subjects were enrolled only once, and their data was shared with other investigators performing their studies at the same time in the same place. The intervention arm, however, included different subjects, receiving different medications according to the trial they were enrolled in. The committee also required the intervention group to control group ratio to be 1:1, and not more, in order to avoid enrolment of more subjects than required in the RCTs.
In many clinical trials placebo control arm is recommended, especially where the effect of the drug is still not well-documented, or as obvious as in cancer research where a drug causes shrinkage of the tumor ( 12 ). For the placebo-controlled trials, the REC decided that all participants must receive the updated standard of care treatment as per the Egyptian MOHP protocol for COVID-19 patients, while the participants receive the new drug under trial as add-on therapy. This way the clinical trial design was an add-on design, where the controls received the standard care MOHP protocol, rather than receiving a sham medication. The REC thought that this could minimize the risk, although the standard protocols at the start of the pandemic had no clear evidence of benefit.
The inclusion of the Egyptian MOHP COVID-19 management protocol was a challenge to the investigators, as the treatment protocol was constantly updated according to new information arising in that arena. The FMASU REC recommended that the standard of care set by the Egyptian MOHP always be updated in the submitted protocols and provided to all COVID-19 study participants.
Regarding the clinical trial endpoints, the FMASU REC had lengthy discussions on the use of measurable achievement vs. patient-related outcomes in the pandemic research. Several protocols used “the time to clinical improvement” as the measure for outcome. Clinical improvement in some studies was defined as the time from randomization to either an improvement of two points on a six or eight-category ordinal scale. Some members of the committee considered the scale as very subjective and required the use of more objective or measurable outcomes. The FMASU REC resorted to the time to clinical improvement scale, in addition to the patient-related outcome scales, the investigators should use more objective outcome measures in their studies, such as persistent positive PCR tests after treatment, or time until the emergence of antibodies against the novel virus. The use of objective tests as outcomes would be a dynamic process as new information is published.
Ensuring the provision of a clear informed consent form was a big challenge for the committee, and certainly for the investigators as well. The motivational force behind the willingness of the patients to enroll in the clinical trials is complex, and therapeutic misconception had to be clearly avoided in the consent language. Due to the scarcity of available information about the virus and the use of novel drugs, the committee ensured that the investigators simplify the information provided to the participants in a manner that the participants could comprehend, as there were so many unknown facts about the virus. The committee understood how challenging it was to describe and explain unknown risks to the potential participants. Still, the FMASU REC required the explanation of risks to be clear and in a language the participants could understand. Furthermore, the prospect of direct benefits was in no way to be promised or overestimated. The FMASU REC members conducted a meticulous review of the wording of the informed consent to ensure the message was clearly communicated to the potential participants and their guardians, regarding the lack of scientific evidence of the efficacy of the used drugs, as well as the unknown side effects, while still providing convincing rationale for the performance of the study.
Additional minor concerns in some of the studies included the completion of a diary for drug doses to be completed by the patients. The FMASU REC was concerned about how a severely ill participant would record his/her daily doses of drugs under trial, especially for the non-educated participants. The FMASU REC requested that this be confined to moderate or highly educated cases only.
The FMASU REC requested the timely reporting of all adverse events as soon as they occurred, not only the serious ones as per the standard procedures which assign a medical monitor in all COVID-19 clinical trials. The medical monitor should be a medical doctor, not involved in the study, but who observes the progress of the study and provides reports to the FMASU REC in case of adverse events. In studies assessing psychological risks to healthcare workers, the FMASU REC requested that participants who tested positive on screening, receive free management and referral to receive psychiatric help if proven to be suffering from anxiety or depression.
Common modifications and clarifications requested by the FMASU REC were the inclusion criteria and the age range of the recruited subjects. Enrolment of subjects not receiving other medicines under trial was a challenge during review. Detailed data of the study procedures were requested in many submitted research studies. More frequent progress reports were requested.
To mitigate risks, more frequent electrocardiograms, complete blood counts, x-rays, and chest Computed Tomographies were requested to safeguard against serious adverse events of the drugs under investigation, such as Hydroxychloroquine and other repurposed drugs. Regarding the control groups in the RCTs, the REC recommended that controls obtain the standard MOHP protocol for COVID-19 management. The REC requested monthly progress reports and swift notification of serious adverse events.
The innovative approaches adopted by the REC in the earlier wave of the COVID-19 pandemic were acceleration of submission of pre-requisite paperwork needed for application, increased frequency of virtual meetings, expansion of meeting agendas, direct contact with the PIs by phone and fast-track review within 1-7 days (compared to the usual 1-month review of clinical trials according to the SOPs.
FMASU REC experience, being active for 13 years since 2007 would be beneficial for other Egyptian RECs, numbering approximately 85 committees in 2021 with variable experience. Seventy Egyptian RECS are linked through a non-governmental body named the Egyptian Network of Research Ethics Committees (also known as ENREC), established in 2008, that enhances REC networking, standardizing the SOPs among RECs all over Egypt, the exchange of knowledge of research review challenges and obstacles, as well as finding solutions through regular annual meetings ( 13 ). Thirty-five RECs are registered with the MOHP.
Data confidentiality is fundamental in both COVID-19 and non-COVID-19 research to protect the life, health, dignity, integrity, right to self-determination, privacy, and confidentiality of personal information of research subjects. It has been practiced since the establishment of the committee according to the Declaration of Helsinki ( 14 ).
During the review of COVID-19 research, the REC was more diligent in reviewing the parts of the protocol where the investigators detailed the precautions for data confidentiality, including databases and computer files, as well as paper copies of questionnaires and informed consents. REC members followed the REC review checklist to review the protocols with confidentiality adequately listed in the checklist. Digital tracking technologies were not allowed, so there were no concerns regarding generated data confidentiality.
Some of the strengths of this analysis at the organizational level were REC resilience and at the research level, the researchers continued conduct of research in spite of the discussed challenges in order to generate knowledge for this new disease and to accomplish investigator career progress. Regarding the research participants: COVID-19 investigation results, including PCR, lab and radiology and all medications given to research participants were provided free of charge. Participants were offered the autonomy to participate in research under strict REC oversight during that period, which was characterized by little and misinformation. Regarding inclusiveness and diversity, participants included healthcare professionals, literate and illiterate patients, and the elderly without discrimination in research enrolment while maintaining equity of healthcare.
Our research prioritization during the COVID-19 pandemic is in line with that of Kheng-Wei Yeoh and Ketan Shah, who provided recommendations for RECs on research prioritization and fast-tracking research, without compromising the participants' safety and well-being. Priority should be given to research that helps find a cure for the patients, while other research should be re-evaluated for public health concerns and precautions incorporated into the studies. As for the design, the authors recommend incorporating the study design into clinical care and look for new information due to the increased demand ( 15 ).
The Pan American Health Organization (PAHO), website on April 15, 2020 published guidance for the development of SOPs for RECs for the review of research during the COVID-19 pandemic. In addition to the revised SOPs, the PAHO recommended that RECs should accelerate reviews and initiate a system for follow up on COVID-19 research ( 16 ).
Due to confidentiality issues, the authors provided minimal details about the studies. We would have liked to expand on the types of research, but many of the studies included new drugs about which we could not provide details. Another limitation is that this article's scope is limited to the performance of the REC and the challenges it faced, rather than a predesigned research study or survey.
During the COVID-19 pandemic the FMASU REC was overwhelmed with a huge number of COVID-19 -related research protocols. The increased amount of research protocols to be reviewed in a short time presented several logistic and ethical challenges. The committee had to adopt different methods of review to ensure adherence to the ethical principles. The ethics training background of the members proved beneficial to balance the risks and benefits to the patients among novel ethical dilemmas.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
This study was self-funded by the authors, who have not received any monetary or financial support for the writing and publishing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to acknowledge the efforts of all the FMASU REC members and office staff during the first wave of the COVID-19 pandemic and FMASU administration's support.
Abbreviations
RECs, Research ethics committees; EUREC, European Network of Research Ethics Committees; FMASU REC, Faculty of Medicine, Ain Shams University Research Ethics Committee; ICU, Intensive care units; MOHP, Ministry of Health and Population; PAHO, Pan American Health Organization; PCR, Polymerase Chain Reaction; PI, Principal investigator; RCTs, Randomized controlled trials; SOPs, Standard operating procedures; WHO, World Health Organization.
1. Marzouk D, Abd El Aal W, Saleh A, Sleem H, Khyatti M, Mazini L, et al. Overview on health research ethics in Egypt and North Africa. Eur J Public Health . (2014) 24(Suppl. 1):87–91. doi: 10.1093/eurpub/cku110
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Sisi Passes Law Regulating Clinical Medical Research in Egypt. Egypt: Independent Gazette (2020). Available online at: https://egyptindependent.com/sisi-passes-law-regulating-clinical-medical-research-in-egypt/ (accessed February 28, 2021)
Google Scholar
3. Available, online at: https://clinicaltrials.gov/ct2/results?cond=COVID-19 (accessed March 3, 2021)
4. Guidance for Managing Ethical Issues in Infectious Disease Outbreaks . Geneva: World Health Organization (2016). Available online at: https://apps.who.int/iris/bitstream/handle/10665/250580/9789241549837-eng.pdf?sequence=1&isAllowed=y (accessed November 10, 2020)
5. Ethical Standards for Research During Public Health Emergencies: Distilling Existing Guidance to Support COVID-19 R&D. Geneva: World Health Organization (2020). Available online at: https://apps.who.int/iris/bitstream/handle/10665/331507/WHO-RFH-20.1-eng.pdf?sequence=1&isAllowed=y (accessed November 10, 2020)
6. Position of the European Network of Research Ethics Committees (EUREC) on the Responsibility of Research Ethics Committees during the COVID-19 Pandemic (2020). Available online at: https://ancei.es/wp-content/uploads/2020/05/EUREC-Positionpaper_COVID_19.pdf (accessed December, 2020)
7. Ministry of Higher Education and Scientific Research. Available online at: http://portal.mohesr.gov.eg/ar-eg/Pages/Home.aspx (accessed June, 2021)
8. Molyneux M. New ethical considerations in vaccine trials. Hum Vaccines Immunother . (2017) 13:2160–3. doi: 10.1080/21645515.2016.1272744
9. Central Agency for Public Mobilization and Statistics (CAPMAS) (2019). Available online at: https://dailynewsegypt.com/2020/09/08/egypts-illiteracy-rate-decreased-to-24-6-in-july-2019-capmas/ (accessed August 2, 2021)
10. Cinnella G. Enrolling patients into multiple trials: it is time for glasnost. Crit Care Med . (2015) 43:485–6. doi: 10.1097/CCM.0000000000000756
11. Gertner E. COVID-19 trial co-enrolment and subsequent enrolment. Lancet . (2020) 396:461–2. doi: 10.1016/S0140-6736(20)31537-3
12. Schilsky RL. Placebos in Cancer Clinical Trials (2018). Available online at: https://www.cancer.net/research-and-advocacy/clinical-trials/placebos-cancer-clinical-trials (accessed February 28, 2021)
13. Egyptian Network of Research Ethics Committees (2008). Available online at: http://www.enrec.org (accessed July, 2021)
14. WMA Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects (2021). Available online at: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed July, 2021)
15. Kheng-Wei Y, Ketan S. Research ethics during a pandemic (COVID-19). Int Health . (2021) 13:374–5. doi: 10.1093/inthealth/ihaa054
16. Available, online at: https://iris.paho.org/handle/10665.2/52086 (accessed August 1, 2021)
Keywords: research ethics committees, Faculty of Medicine Ain Shams University, COVID-19 research, ethical challenges, accelerated review
Citation: Marzouk D, Sharawy I, Nakhla I, El Hodhod M, Gadallah H, El-Shalakany A, Elwakil R, Moussa MM, Ismail A and Tash FM (2021) Challenges During Review of COVID-19 Research Proposals: Experience of Faculty of Medicine, Ain Shams University Research Ethics Committee, Egypt. Front. Med. 8:715796. doi: 10.3389/fmed.2021.715796
Received: 27 May 2021; Accepted: 29 September 2021; Published: 02 November 2021.
Reviewed by:
Copyright © 2021 Marzouk, Sharawy, Nakhla, El Hodhod, Gadallah, El-Shalakany, Elwakil, Moussa, Ismail and Tash. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diaa Marzouk, diaamarzouk@med.asu.edu.eg

The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine (2021)
Chapter: 8 major findings and research questions, 8 major findings and research questions, introduction.
The COVID-19 pandemic, which began in late 2019, created unprecedented global disruption and infused a significant level of uncertainty into the lives of individuals, both personally and professionally, around the world throughout 2020. The significant effect on vulnerable populations, such as essential workers and the elderly, is well documented, as is the devastating effect the COVID-19 pandemic had on the economy, particularly brick-and-mortar retail and hospitality and food services. Concurrently, the deaths of unarmed Black people at the hands of law enforcement officers created a heightened awareness of the persistence of structural injustices in U.S. society.
Against the backdrop of this public health crisis, economic upheaval, and amplified social consciousness, an ad hoc committee was appointed to review the potential effects of the COVID-19 pandemic on women in academic science, technology, engineering, mathematics, and medicine (STEMM) during 2020. The committee’s work built on the National Academies of Sciences, Engineering, and Medicine report Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine: Opening Doors (the Promising Practices report), which presents evidence-based recommendations to address the well-established structural barriers that impede the advancement of women in STEMM. However, the committee recognized that none of the actions identified in the Promising Practices report were conceived within the context of a pandemic, an economic downturn, or the emergence of national protests against structural racism. The representation and vitality of academic women in STEMM had already warranted national attention prior to these events, and the COVID-19
pandemic appeared to represent an additional risk to the fragile progress that women had made in some STEMM disciplines. Furthermore, the future will almost certainly hold additional, unforeseen disruptions, which underscores the importance of the committee’s work.
In times of stress, there is a risk that the divide will deepen between those who already have advantages and those who do not. In academia, senior and tenured academics are more likely to have an established reputation, a stable salary commitment, and power within the academic system. They are more likely, before the COVID-19 pandemic began, to have established professional networks, generated data that can be used to write papers, and achieved financial and job security. While those who have these advantages may benefit from a level of stability relative to others during stressful times, those who were previously systemically disadvantaged are more likely to experience additional strain and instability.
As this report has documented, during 2020 the COVID-19 pandemic had overall negative effects on women in academic STEMM in areas such productivity, boundary setting and boundary control, networking and community building, burnout rates, and mental well-being. The excessive expectations of caregiving that often fall on the shoulders of women cut across career timeline and rank (e.g., graduate student, postdoctoral scholar, non-tenure-track and other contingent faculty, tenure-track faculty), institution type, and scientific discipline. Although there have been opportunities for innovation and some potential shifts in expectations, increased caregiving demands associated with the COVID-19 pandemic in 2020, such as remote working, school closures, and childcare and eldercare, had disproportionately negative outcomes for women.
The effects of the COVID-19 pandemic on women in STEMM during 2020 are understood better through an intentionally intersectional lens. Productivity, career, boundary setting, mental well-being, and health are all influenced by the ways in which social identities are defined and cultivated within social and power structures. Race and ethnicity, sexual orientation, gender identity, academic career stage, appointment type, institution type, age, and disability status, among many other factors, can amplify or diminish the effects of the COVID-19 pandemic for a given person. For example, non-cisgender women may be forced to return to home environments where their gender identity is not accepted, increasing their stress and isolation, and decreasing their well-being. Women of Color had a higher likelihood of facing a COVID-19–related death in their family compared with their white, non-Hispanic colleagues. The full extent of the effects of the COVID-19 pandemic for women of various social identities was not fully understood at the end of 2020.
Considering the relative paucity of women in many STEMM fields prior to the COVID-19 pandemic, women are more likely to experience academic isolation, including limited access to mentors, sponsors, and role models that share gender, racial, or ethnic identities. Combining this reality with the physical isolation stipulated by public health responses to the COVID-19 pandemic,
women in STEMM were subject to increasing isolation within their fields, networks, and communities. Explicit attention to the early indicators of how the COVID-19 pandemic affected women in academic STEMM careers during 2020, as well as attention to crisis responses throughout history, may provide opportunities to mitigate some of the long-term effects and potentially develop a more resilient and equitable academic STEMM system.
MAJOR FINDINGS
Given the ongoing nature of the COVID-19 pandemic, it was not possible to fully understand the entirety of the short- or long-term implications of this global disruption on the careers of women in academic STEMM. Having gathered preliminary data and evidence available in 2020, the committee found that significant changes to women’s work-life boundaries and divisions of labor, careers, productivity, advancement, mentoring and networking relationships, and mental health and well-being have been observed. The following findings represent those aspects that the committee agreed have been substantiated by the preliminary data, evidence, and information gathered by the end of 2020. They are presented either as Established Research and Experiences from Previous Events or Impacts of the COVID-19 Pandemic during 2020 that parallel the topics as presented in the report.
Established Research and Experiences from Previous Events
| Leading up to the COVID-19 pandemic, the representation of women has slowly increased in STEMM fields, from acquiring Ph.D.s to holding leadership positions, but with caveats to these limited steps of progress; for example, women representation in leadership positions tends to be at institutions with less prestige and fewer resources. While promising and encouraging, such progress is fragile and prone to setbacks especially in times of crisis (see ). | |
| Social crises (e.g., terrorist attacks, natural disasters, racialized violence, and infectious diseases) and COVID-19 pandemic-related disruptions to workload and schedules, added to formerly routine job functions and health risks, have the potential to exacerbate mental health conditions such as insomnia, depression, anxiety, and posttraumatic stress. All of these conditions occur more frequently among women than men. As multiple crises coincided during 2020, there is a greater chance that women will be affected mentally and physically (see and ). |
___________________
1 This finding is primarily based on research on cisgender women and men.
| Structural racism is an omnipresent stressor for Women of Color, who already feel particularly isolated in many fields and disciplines. Attempts to ensure equity for all women may not necessarily create equity for women across various identities if targeted interventions designed to promote gender equity do not account for the racial and ethnic heterogeneity of women in STEMM (see , , and ). |
Impacts of the COVID-19 Pandemic during 2020
| While some research indicates consistency in publications authored by women in specific STEMM disciplines, like Earth and space sciences, during 2020, several other preliminary measures of productivity suggest that COVID-19 disruptions have disproportionately affected women compared with men. Reduced productivity may be compounded by differences in the ways research is conducted, such as whether field research or face-to-face engagement with human subjects is required (see ). | |
| Many administrative decisions regarding institutional supports made during 2020, such as work-from-home provisions and extensions on evaluations or deliverables, are likely to exacerbate underlying gender-based inequalities in academic advancement rather than being gender neutral as assumed. For example, while colleges and universities have offered extensions for those on the tenure track and federal and private funders have offered extensions on funding and grants, these changes do not necessarily align with the needs expressed by women, such as the need for flexibility to contend with limited availability of caregiving and requests for a reduced workload, nor do they generally benefit women faculty who are not on the tenure track. Furthermore, provision of institutional support may be insufficient if it does not account for the challenges faced by those with multiple marginalized identities (see and ). | |
| Organizational-level approaches may be needed to address challenges that have emerged as a result of the COVID-19 pandemic in 2020, as well as those challenges that may have existed before the pandemic but are now more visible and amplified. Reliance on individual coping strategies may be insufficient (see and ). | |
| The COVID-19 pandemic has intensified complications related to worklife boundaries that largely affect women. Preliminary evidence |
| from 2020 suggests women in academic STEMM are experiencing increased workload, decreased productivity, changes in interactions, and difficulties from remote work caused by the COVID-19 pandemic and associated disruptions. Combined with the gendered division of nonemployment labor that affected women before the pandemic, these challenges have been amplified, as demonstrated by a lack of access to childcare, children’s heightened behavioral and academic needs, increased eldercare demands, and personal physical and mental health concerns. These are particularly salient for women who are parents or caregivers (see ). | |
| During the COVID-19 pandemic, technology has allowed for the continuation of information exchange and many collaborations. In some cases technology has facilitated the increased participation of women and underrepresented groups. However, preliminary indicators also show gendered impacts on science and scientific collaborations during 2020. These arise because some collaborations cannot be facilitated online and some collaborations face challenges including finding time in the day to engage synchronously, which presents a larger burden for women who manage the larger share of caregiving and other household duties, especially during the first several months of the COVID-19 pandemic (see ). | |
| During the COVID-19 pandemic in 2020, some professional societies adapted to the needs of members as well as to broader interests of individuals engaged in the disciplines they serve. Transitioning conferences to virtual platforms has produced both positive outcomes, such as lower attendance costs and more open access to content, and negative outcomes, including over-flexibility (e.g., scheduling meetings at non-traditional work hours; last-minute changes) and opportunities for bias in virtual environments (see ). | |
| During the COVID-19 pandemic in 2020, many of the decision-making processes, including financial decisions like lay-offs and furloughs, that were quickly implemented contributed to unilateral decisions that frequently deviated from effective practices in academic governance, such as those in crisis and equity-minded leadership. Fast decisions greatly affected contingent and nontenured faculty members—positions that are more often occupied by women and People of Color. In 2020, these financial decisions already had negative, short-term effects and may portend long-term consequences (see ). | |
| Social support, which is particularly important during stressful situations, is jeopardized by the physical isolation and restricted social interactions that have |
| been imposed during the COVID-19 pandemic. For women who are already isolated within their specific fields or disciplines, additional social isolation may be an important contributor to added stress (see ). | |
| For women in the health professions, major risk factors during the COVID-19 pandemic in 2020 included unpredictability in clinical work, evolving clinical and leadership roles, the psychological demands of unremitting and stressful work, and heightened health risks to family and self (see ). |
RESEARCH QUESTIONS
While this report compiled much of the research, data, and evidence available in 2020 on the effects of the COVID-19 pandemic, future research is still needed to understand all the potential effects, especially any long-term implications. The research questions represent areas the committee identified for future research, rather than specific recommendations. They are presented in six categories that parallel the chapters of the report: Cross-Cutting Themes; Academic Productivity and Institutional Responses; Work-Life Boundaries and Gendered Divisions of Labor; Collaboration, Networking, and Professional Societies; Academic Leadership and Decision-Making; and Mental Health and Well-being. The committee hopes the report will be used as a basis for continued understanding of the impact of the COVID-19 pandemic in its entirety and as a reference for mitigating impacts of future disruptions that affect women in academic STEMM. The committee also hopes that these research questions may enable academic STEMM to emerge from the pandemic era a stronger, more equitable place for women. Therefore, the committee identifies two types of research questions in each category; listed first are those questions aimed at understanding the impacts of the disruptions from the COVID-19 pandemic, followed by those questions exploring the opportunities to help support the full participation of women in the future.
Cross-Cutting Themes
- What are the short- and long-term effects of the COVID-19 pandemic on the career trajectories, job stability, and leadership roles of women, particularly of Black women and other Women of Color? How do these effects vary across institutional characteristics, 2 discipline, and career stage?
2 Institutional characteristics include different institutional types (e.g., research university, liberal arts college, community college), locales (e.g., urban, rural), missions (e.g., Historically Black Colleges and Universities, Hispanic-Serving Institutions, Asian American/Native American/Pacific Islander-Serving Institutions, Tribal Colleges and Universities), and levels of resources.
- How did the confluence of structural racism, economic hardships, and environmental disruptions affect Women of Color during the COVID-19 pandemic? Specifically, how did the murder of George Floyd, Breonna Taylor, and other Black citizens impact Black women academics’ safety, ability to be productive, and mental health?
- How has the inclusion of women in leadership and other roles in the academy influenced the ability of institutions to respond to the confluence of major social crises during the COVID-19 pandemic?
- How can institutions build on the involvement women had across STEMM disciplines during the COVID-19 pandemic to increase the participation of women in STEMM and/or elevate and support women in their current STEMM-related positions?
- How can institutions adapt, leverage, and learn from approaches developed during 2020 to attend to challenges experienced by Women of Color in STEMM in the future?
Academic Productivity and Institutional Responses
- How did the institutional responses (e.g., policies, practices) that were outlined in the Major Findings impact women faculty across institutional characteristics and disciplines?
- What are the short- and long-term effects of faculty evaluation practices and extension policies implemented during the COVID-19 pandemic on the productivity and career trajectories of members of the academic STEMM workforce by gender?
- What adaptations did women use during the transition to online and hybrid teaching modes? How did these techniques and adaptations vary as a function of career stage and institutional characteristics?
- What are examples of institutional changes implemented in response to the COVID-19 pandemic that have the potential to reduce systemic barriers to participation and advancement that have historically been faced by academic women in STEMM, specifically Women of Color and other marginalized women in STEMM? How might positive institutional responses be leveraged to create a more resilient and responsive higher education ecosystem?
- How can or should funding arrangements be altered (e.g., changes in funding for research and/or mentorship programs) to support new ways of interaction for women in STEMM during times of disruption, such as the COVID-19 pandemic?
Work-Life Boundaries and Gendered Divisions of Labor
- How do different social identities (e.g., racial; socioeconomic status; culturally, ethnically, sexually, or gender diverse; immigration status; parents of young children and other caregivers; women without partners) influence the management of work-nonwork boundaries? How did this change during the COVID-19 pandemic?
- How have COVID-19 pandemic-related disruptions affected progress toward reducing the gender gap in academic STEMM labor-force participation? How does this differ for Women of Color or women with caregiving responsibilities?
- How can institutions account for the unique challenges of women faculty with parenthood and caregiving responsibilities when developing effective and equitable policies, practices, or programs?
- How might insights gained about work-life boundaries during the COVID-19 pandemic inform how institutions develop and implement supportive resources (e.g., reductions in workload, on-site childcare, flexible working options)?
Collaboration, Networking, and Professional Societies
- What were the short- and long-term effects of the COVID-19 pandemic-prompted switch from in-person conferences to virtual conferences on conference culture and climate, especially for women in STEMM?
- How will the increase in virtual conferences specifically affect women’s advancement and career trajectories? How will it affect women’s collaborations?
- How has the shift away from attending conferences and in-person networking changed longer-term mentoring and sponsoring relationships, particularly in terms of gender dynamics?
- How can institutions maximize the benefits of digitization and the increased use of technology observed during the COVID-19 pandemic to continue supporting women, especially marginalized women, by increasing accessibility, collaborations, mentorship, and learning?
- How can organizations that support, host, or facilitate online and virtual conferences and networking events (1) ensure open and fair access to participants who face different funding and time constraints; (2) foster virtual connections among peers, mentors, and sponsors; and (3) maintain an inclusive environment to scientists of all backgrounds?
- What policies, practices, or programs can be developed to help women in STEMM maintain a sense of support, structure, and stability during and after periods of disruption?
Academic Leadership and Decision-Making
- What specific interventions did colleges and universities initiate or prioritize to ensure that women were included in decision-making processes during responses to the COVID-19 pandemic?
- How effective were colleges and universities that prioritized equity-minded leadership, shared leadership, and crisis leadership styles at mitigating emerging and potential negative effects of the COVID-19 pandemic on women in their communities?
- What specific aspects of different leadership models translated to more effective strategies to advance women in STEMM, particularly during the COVID-19 pandemic?
- How can examples of intentional inclusion of women in decision-making processes during the COVID-19 pandemic be leveraged to develop the engagement of women as leaders at all levels of academic institutions?
- What are potential “top-down” structural changes in academia that can be implemented to mitigate the adverse effects of the COVID-19 pandemic or other disruptions?
- How can academic leadership, at all levels, more effectively support the mental health needs of women in STEMM?
Mental Health and Well-being
- What is the impact of the COVID-19 pandemic and institutional responses on the mental health and well-being of members of the academic STEMM workforce as a function of gender, race, and career stage?
- How are tools and diagnostic tests to measure aspects of wellbeing, including burnout and insomnia, used in academic settings? How does this change during times of increased stress, such as the COVID-19 pandemic?
- How might insights gained about mental health during the COVID-19 pandemic be used to inform preparedness for future disruptions?
- How can programs that focus on changes in biomarkers of stress and mood dysregulation, such as levels of sleep, activity, and texting patterns, be developed and implemented to better engage women in addressing their mental health?
- What are effective interventions to address the health of women academics in STEMM that specifically account for the effects of stress on women? What are effective interventions to mitigate the excessive levels of stress for Women of Color?
This page intentionally left blank.
The spring of 2020 marked a change in how almost everyone conducted their personal and professional lives, both within science, technology, engineering, mathematics, and medicine (STEMM) and beyond. The COVID-19 pandemic disrupted global scientific conferences and individual laboratories and required people to find space in their homes from which to work. It blurred the boundaries between work and non-work, infusing ambiguity into everyday activities. While adaptations that allowed people to connect became more common, the evidence available at the end of 2020 suggests that the disruptions caused by the COVID-19 pandemic endangered the engagement, experience, and retention of women in academic STEMM, and may roll back some of the achievement gains made by women in the academy to date.
The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine identifies, names, and documents how the COVID-19 pandemic disrupted the careers of women in academic STEMM during the initial 9-month period since March 2020 and considers how these disruptions - both positive and negative - might shape future progress for women. This publication builds on the 2020 report Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine to develop a comprehensive understanding of the nuanced ways these disruptions have manifested. The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine will inform the academic community as it emerges from the pandemic to mitigate any long-term negative consequences for the continued advancement of women in the academic STEMM workforce and build on the adaptations and opportunities that have emerged.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)
- PMC10530798

Pandemic Preparedness: A Scoping Review of Best and Worst Practices from COVID-19
Alessia maccaro.
1 School of Engineering, University of Warwick, Library Rd., Coventry CV4 7AL, UK; [email protected] (K.S.); [email protected] (L.P.); [email protected] (D.P.)
Camilla Audia
2 Global Sustainable Development, School for Cross-Faculty Studies, University of Warwick, Library Rd., Coventry CV4 7AL, UK; [email protected]
Katy Stokes
Haleema masud.
3 Institute of Advanced Studies, University of Warwick, Library Rd., Coventry CV4 7AL, UK; [email protected]
Sharifah Sekalala
4 School of Law, University of Warwick, Library Rd., Coventry CV4 7AL, UK; [email protected]
Leandro Pecchia
5 Department of Engineering, University Campus Bio-Medico of Rome, Via Alvaro del Portillo 21, 00128 Roma, Italy
Davide Piaggio
Associated data.
The data presented in this study are available upon reasonable request from the authors of this manuscript.
The COVID-19 pandemic highlighted the scale of global unpreparedness to deal with the fast-arising needs of global health threats. This problem was coupled with a crisis of governance and presented in the context of globally hitting climate crisis and disasters. Although such a pandemic was predictable due to the known effects of human intervention on the surrounding environment and its devastating secondary effects, such as climate change and increased zoonoses, most countries were unprepared to deal with the scale and scope of the pandemic. In this context, such as that of the climate crisis, the Global North and Global South faced several common challenges, including, first and foremost, the scarcity of resources required for health, policy, wellbeing and socioeconomic wellness. In this paper, we review the most recent evidence available in the literature related to pandemic preparedness and governance, focusing on principles and practices used during the COVID-19 pandemic, and we place it in the context of a European Parliament Interest Group meeting (this event took place on 21 March 2023 during the “European Health Tech Summit”) to ground it within ongoing discussions and narratives of policy and praxis. The review identified key practices and principles required to better face future health threats and emergencies. Beyond health practices relying on technology and innovation, it is useful to mention the importance of contextualising responses and linking them to clear goals, improving the agreement between science and policymaking, thus building trust and enabling transparent communication with the general public based on clear ethical frameworks.
1. Introduction
The COVID-19 pandemic highlighted gaps in both national healthcare systems and wider preparedness policies. The post-pandemic Global Health Security (GHS) index report confirmed that no country was fully prepared to tackle an emerging public health emergency threat [ 1 ]. The difference between the GHS index ranking and the real-world performance of countries, as determined via COVID-19 performance indicators, suggests that the GHS index might have underestimated the preparedness level of certain countries while overestimating that of other countries [ 2 ]. While some joint strategies were adopted at an international level, similar challenges stemming from the same emergency were tackled in different ways across the globe. It is now evident that inadequate consideration of the contextual cultural particularisms of different countries undermines the uptake of specific measures; in this paper, we reflect on the lessons learned and discuss ways in which they can support future preparedness [ 3 ].
Despite the challenges involved, it is possible to envisage the global exchange in knowledge and a universal approach (open to all) to pandemic preparedness and governance that considers different local contexts. Some authors of this paper have previously published various investigations in pursuit of this goal, promoting the application of the fields of biomedical engineering and ethics to biomedical engineering, with specific focus on frugal medical device design and regulation and pandemic management [ 3 , 4 , 5 , 6 , 7 ]. While there has been progress in sharing medical data, the authors argue that a globalised response, which would be grounded in contextualised approaches, can be achieved if there is buy-in to move beyond a global (but too generic) versus siloed (with no globalised view) divide. The response to COVID-19 demonstrated that a generic uncontextualised approach can lead countries to feel less represented in general decisions and turn to self-referentialism, causing friction in the uptake of some health measures (e.g., vaccine hesitancy in some countries) [ 3 , 7 ]. Furthermore, the management of the COVID-19 pandemic highlighted a lack of interconnectivity between countries and the absence of an up-to-date interoperable legislative framework to allow countries to collectively, efficiently, and rapidly respond to the pandemic [ 8 ]. Finally, subsequent analyses of metrics and indicators of the GHS further indicated that a country’s response to prior health threats should be incorporated into future GHS index reports [ 2 ]. In sum, COVID-19 highlighted the fundamental importance of reflecting on the possibility of preparing for the future (i.e., preparedness) and drawing lessons from the past. Creating spaces for reflexivity and learning has been put forward as a key element in sustainable, just, and long-term resilience in terms of disaster risk reduction [ 9 ]. In this review, we understand preparedness to be a set of precautionary measures to be taken in case of potential disasters and a key aspect of emergency management; the current situation, in the aftermath of a pandemic, offers space for learning and reflection for the future.
According to the United Nations, disaster preparedness involves “forecasting and taking precautionary measures before an imminent threat when warnings are possible” [ 10 ]. Preparedness is a relatively young concept, and its appearance is linked to a shift in the approach relative to disasters (e.g., hurricanes, pandemic, etc.), namely from a reactive approach enacted in response to calamities to a proactive approach, with measures put in place to contain possible catastrophes. Despite plenty of empirical examples and practices, preparedness is still lacking at the theoretical level, mainly due to a lack of conceptual refinement and terminological agreement [ 11 , 12 , 13 , 14 , 15 ]. Nevertheless, despite facing pandemics since they were first recorded (i.e., the Plague of Athens in 430 BC), global preparedness (prevention, prompt response, and restoration) is lacking [ 16 ]. It is noteworthy that in March 2020, Google trends reported the highest peak of interest in pandemic preparedness since 2004, with this moment being aligned with COVID-19 outbreak. There has also been increased governmental and scientific interest (e.g., the Engineering X Pandemic Preparedness programme led by the Royal Academy of Engineering) [ 17 ].
Publishing guidelines and tools for enacting emergency responses (e.g., infection prevention and control (IPC)) during the COVID-19 pandemic proved to be insufficient to warrant effective preparedness and adequate governmental response. One of the alleged reasons behind this is the much-criticised slow and cautious approach of the World Health Organization (WHO) in terms of warning about the human transmissibility of the virus, declaring a Public Health Emergency of International Concern (PHEIC), and endorsing the public use of face masks and other containment/prevention strategies. Governments did not outshine the WHO, as their inter-coordination was also inadequate to this respect [ 18 ].
However, the WHO, despite welcoming the general recommendations presented in the paper by Sachs et al. [ 18 ], does not agree with some parts of that report, which are considered to be “omissions” and “misinterpretations”.
For the purposes of this paper, we aim to look at measures and practices of countries who reacted, responded, and restored their systems during the COVID-19 pandemic. This study is rooted in the consideration that being prepared, in the sense of having an absolute, normative, or prescriptive plan to control future pandemics, is ultimately unachievable. Moreover, in our ever-more globalised world, the risk of future pandemics is higher than ever [ 19 ]. Effective governance and decision-making rely on the outcomes and responsible communication of scientific research (e.g., concerning the characteristics of the pathogenic threat or the efficacy of IPC strategies) conducted with rigour and integrity, regardless of the urgency and pressure of the situation.
This article situates the findings from the literature within the context of a European Parliament Interest Group (EPIG) event that took place on 21 March 2023 during the “European Health Tech Summit”.
This article, therefore, collects the evidence available in the literature related to preparedness and governance during the COVID-19 pandemic, focusing on lessons learned for future policies and worst and best practices. We used the proceedings of this meeting to triangulate our review and ground it in the ongoing praxis regarding learning from COVID-19 and reflecting on practices to be better prepared, as well as more resilient, in the event of a future health threat [ 9 ]. Future work may include a Delphi study to scope and raise consensus on these recommendations among international experts to co-create a theoretical–practical framework to guide the transdisciplinary management of future healthcare emergencies.
This paper presents the results of a scoping review triangulated with results of the EPIG event; the organisation of and participation in the event was supported by the Policy Support Fund of the University of Warwick.
2.1. Scoping Review
A scoping review was performed. In order to check whether our work would be original and not duplicating possibly already existent works, before starting this study, we performed an initial check on Scopus to analyse the existing reviews on the same topic. Since no similar work was found, we proceeded with the aforementioned scoping review.
2.2. Search Strategy
The scoping review was conducted according to the PRISMA guidelines for performing scoping reviews (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [ 20 , 21 ]. The review was performed following the Population (P), Concept (C), and Context (C) model [ 22 ]:
- P—Governance and preparedness practices;
- C—Lessons learned and best and worst practices;
- C—The global COVID-19 pandemic.
A systematic search was conducted on Scopus in February 2023, using the search string displayed in Table 1 . The search string was combined with the AND operator for three main topics, i.e., the pandemic, policies, and best/worst practices. Scopus was chosen due to the fact that it is a database that also includes other databases (e.g., MEDLINE) and collects texts of a medical, scientific, technical, and social nature.
The search string used to perform the systematic search, divided into the three main topics.
| Core Topic | Search String |
|---|---|
| Pandemic | (TITLE-ABS-KEY ((pandemic OR epidemic OR emergenc* OR disaster) AND (COVID* OR “SARS CoV 2” OR coronavirus OR SARS-CoV-2)) |
| Policies | TITLE-ABS-KEY (((preparedness OR governance OR management OR prevention OR control) AND (polic* OR polit* OR guidelin* OR regulat* OR law OR decree) OR (governmental AND response) OR ((containment OR prevention) AND strateg*))) |
| Best worst practices | TITLE-ABS-KEY ((best OR worst) AND practice*)) |
2.3. Study Eligibility
The only inclusion criterion was as follows:
- Scientific articles focusing on the management of the COVID-19 health emergency.
The exclusion criteria were as follows:
- Articles not published in the English language;
- Articles in which the full texts were not accessible;
- Articles published before 2019;
- Article of the following types: letters to editors, editorials, commentaries, and review articles;
- Articles focusing on topics other than the political management of pandemics (e.g., military lessons or specific clinical interventions);
- Articles reporting specific case studies (e.g., geriatric patient management);
- Articles reporting modelling studies.
2.4. Study Selection
Two authors independently screened the studies by title and abstract, while three authors completed the full text screening based on the inclusion and exclusion criteria, with conflicting decisions being mitigated by an additional independent reviewer. Relevant data were then extracted using an ad hoc extraction table to facilitate the analysis and narrative synthesis.
2.5. Data Extraction
Relevant data were extracted and collected in an ad hoc Excel sheet and organised by author, year, title, geographical focus (countries or global), theme (infodemic, evaluation of intervention, governance, etc.), keywords (/subtheme), aims/objectives, applied methods, practices/interventions studied, key findings, best practices, worst practices, and any other findings related to informing evidence-based policy. The summarised version of this sheet is presented in Table 2 and Table 3 .
Characteristics of included studies.
| Location | Study Type * | Practices Addressed | |
|---|---|---|---|
| Herstein et al., 2022 [ ] | Global | Narrative analysis of practices | Using a pre-existing network as a platform for managing future emergencies |
| Irwin, 2020 [ ] | Sweden | Case study | COVID-19 responses and media representations |
| Jegede et al., 2020 [ ] | Nigeria | Narrative analysis of practices | Measures: COVID-19 and previous epidemics/pandemics |
| Lee, Lim, 2021 [ ] | ASEAN | Data envelopment analysis | Efficiency of IPC measures |
| Mersha et al., 2021 [ ] | Ethiopia | Cross-sectional study | Precautionary measures conducted by health professionals (hand sanitizing, etc.) |
| Min, Lee, 2022 [ ] | OECD countries | Data envelopment analysis | Relationship between a nation’s cultural dimensions and its COVID-19 control measures’ efficiency scores. |
| Moeenian et al., 2022 [ ] | Iran | Grounded theory strategy | Social innovations |
| Ngoy et al., 2022 [ ] | AFRO WHO region | Retrospective policy tracing and descriptive statistical analysis | COVID-19 response strategies, plans, regulations, press releases, government websites, and grey and peer-reviewed literature |
| Pennestrì et al., 2021 [ ] | Lombardy (Italy) | Narrative data analysis | Regional responses |
| Prajitha et al., 2021 [ ] | Kerala (India) | Quantitative descriptive study | Regional responses |
| Saleh et al., 2022 [ ] | Nigeria | Narrative analysis of practices | NCDC learning mechanisms derived from the Lassa and COVID-19 outbreaks |
| Agnew, 2021 [ ] | USA | Narrative analysis of practices | Political ideology |
| Ansah et al., 2021 [ ] | Singapore | Narrative analysis of practices | Mitigation vs. containment |
| Atsawarungruangkit et al., 2020 [ ] | Global; Asia, Europe, North America | Narrative analysis of practices | Case identification |
| Bartels et al., 2021 [ ] | North Carolina | Qualitative | Message testing, rapid design, COVID-19, social distancing, emergency preparedness, etc. |
| Braithwaite et al., 2021 [ ] | Global; 36 OECD, Singapore, Malaysia, Taiwan and Iran | Cross-sectional study | Governance approaches |
| Canario Guzmánet al., 2022 [ ] | Central America, Dominican Republic | Qualitative | Governance approaches, ethics, etc. |
| Chowdhury, Jomo, 2020 [ ] | Asia, South America | Case study | Containment measures (physical distancing, contact tracing, etc.) |
| Coral et al., 2022 [ ] | Ecuador | Narrative analysis of practices | Governance practices |
| Evans, 2022 [ ] | UK | Narrative analysis of practices | Use of evidence in policy decisions |
| Goodyear-Smith et al., 2022 [ ] | Australia, South Africa, Egypt, Nigeria | Narrative analysis of practices | Primary healthcare policies |
| Halfmann et al., 2022 [ ] | Europe, Africa | Narrative analysis of practices, including SWOT (Strengths, Weaknesses, Opportunities, and Threats,) analysis, surveys, interviews, etc. | Innovation governance |
| Upadhyay et al., 2022 [ ] | 13 ITEC countries | Qualitative analysis, including workshops, Delphi survey, etc. | Various pandemic preparedness strategies and responses |
| Zhang et al., 2021 [ ] | China, Germany | Narrative and statistical analysis of practices | Non-pharmaceutical interventions |
* Study types were either directly taken from the text or inferred based on the applied methods. ASEAN: Association of Southeast Asian Nations, OECD: Organisation for Economic Co-operation and Development, ITEC: Indian Technical and Economic Cooperation, AFRO: World Health Organization African Region, SWOT: Strengths, Weaknesses, Opportunities, and Threats, NHS: National Health Service.
Outcomes of the included studies in terms of areas for improvement and specific lessons learned and opportunities for future actions. NGO: Non-Government Organisation, PHEOC framework: the Framework for a Public Health Emergency Operations Centre, HIC: High-Income Country, LIC: Low-Income Country.
| Areas for Improvement | Lessons Learned and Opportunities for Future Actions | |
|---|---|---|
| Herstein et al., 2022 [ ] | Adapting to surges in capacity | Rapid information exchange facilitated the adoption of treatments/protocols. Networks can act as platforms to share preliminary findings and real-time data before their publication in scientific/medical communities. |
| Irwin, 2020 [ ] | Faster generation of data related to disease to inform policies of disease burden | Trust between the public and the government can reduce the impact of disease control measures on mental health and incidences of abuse/domestic issues. |
| Jegede et al., 2020 [ ] | Increasing the resilience of the health infrastructure to ensure that it is able to respond under pandemic conditions | Pandemic countermeasures need to be contextually sensitive. Communications during a pandemic need to be ethically sensitive. |
| Lee, Lim, 2021 [ ] | Combining medical and economic measures | Restrictions should be accompanied by sufficient financial support and public campaigning to inform and educate. The cancellation of public events should be prioritised ahead of the closure of schools and workplaces. |
| Mersha et al., 2021 [ ] | Attitudes to precautionary measures: availability and knowledge of these measures | Pandemic preparedness can be improved through capacity-building measures, training, motivation, and the recognition of health professionals. |
| Min, Lee, 2022 [ ] | Integrating cultural considerations to country-wide measures, such as face-covering mandates and lockdowns | Outbreak responses should be tailored to the cultural traits of the country/region. |
| Moeenian et al., 2022 [ ] | - | Social innovation can be effectively used at the national level with appropriate speed and agility to tackle pandemics. A redistributive framework and surveillance systems should be used as the basis of development, rather than to focus on economic growth. Institutions could be established by government to facilitate communication with NGOs to align the policies of executive bodies with the goals of NGOs. |
| Ngoy et al., 2022 [ ] | - | Layered coordination is efficient at facilitating efforts, and high political engagement is key. |
| Pennestrì et al., 2021 [ ] | Improving communication between central government directives and local healthcare systems to avoid delays in crisis management | Requirements for funding should be clearly set and be respected by private providers to avoid disproportionate investment negatively impacting public health provision. Keeping patients out of hospitals is key. |
| Prajitha et al., 2021 [ ] | - | Healthcare-based social justice and equity should underpin outbreak responses, leveraging lessons from past viral outbreaks. Public–private partnerships ensured adequate manpower and material resources. Community participation and social capital are key to achieving successful responses. |
| Saleh et al., 2022 [ ] | Improving the documentation of practices to make them easily available in future outbreaks | Instituting the PHEOC framework significantly improved responses. Prior successes and challenges need to be used to adapt public health responses. |
| Agnew, 2021 [ ] | Improving coordination across tiers of government to enable a coherent response | Polyphonic federalism can mitigate the disastrous effects of a pandemic, as opposed to the either/or opposition between decentralisation and centralisation that has latterly tended to prevail in the United States. The US Army Corps of Engineers and the vaccine development programme, known as Operation Warp Speed, provided the basis for achieving excellent responses. |
| Ansah et al., 2021 [ ] | - | Timing (rapid response) and using lessons learned from previous outbreaks is essential. Early public health measures for ‘aggressive containment’ (contact tracing and quarantine) were likely responsible for the suppression of COVID-19 cases in Singapore. |
| Atsawarungruangkit et al., 2020 [ ] | Improving the capture of the wider population, including asymptomatic cases, patients unable to access testing, patients with barriers to health system access, etc. | Different countries demonstrate a wide variety of successful approaches. Response efforts need to be coordinated by health organisations and the public and private sectors, including the insurance industry and citizens. |
| Bartels et al., 2021 [ ] | Improving collaboration between policy makers and researchers to generate evidence most useful for decision-making | Lean and agile principles can be applied to an interdisciplinary communication model to reduce the time required to make evidence-based decisions, linking policy makers, public health officials, and researchers. |
| Braithwaite et al., 2021 [ ] | Improving understanding of the effects of lockdowns | The current measures and capacity of nations is insufficient to deal with pandemics. Wide testing was key to managing COVID-19. Trust in governments is key to ensure the uptake of measures. Governments must be mindful of the impact of policies (costs, disruptions, etc.). |
| Canario Guzmánet al., 2022 [ ] | Improving health regulation and international cooperation | A research ethics system implies an ability to formulate strategic policy direction, ensure good regulation, set and monitor ethical standards, and ensure account ability and transparency. Policy should promote collaboration and joint strategies. |
| Chowdhury, Jomo, 2020 [ ] | Adapting measures to country-specific cultural and socioeconomic contexts is needed | Recommend moving away from so-called ‘best practices’ to ensure context aware outbreak responses. Inclusive and transparent policy-making is key. Measures chosen must not perpetuate inequalities. |
| Coral et al., 2022 [ ] | Adapting measures to context instead of using ‘cut and paste’ approaches (HICs to LICs) | Trans-disciplinarity, co-production, and localised measures are needed. The so-called ‘best practices approach’ should be avoided. |
| Evans, 2022 [ ] | Reducing the time taken to put development measures into practice | Move towards a middle ground where usable science is understood in a holistic/sociologic manner to a ensure scientific state combined with a reasonable timeline for policy-making. |
| Goodyear-Smith et al., 2022 [ ] | Improving equity in vaccination strategy and the availability/capacity of testing | Integrated response between primary care and public health, as well as policy-making and public health, was key to pandemic response. Telehealth was a key element of outbreak response in many countries. |
| Halfmann et al., 2022 [ ] | - | - |
| Upadhyay et al., 2022 [ ] | Incorporating multisectoral responses, communication and community engagement, and testing capacity are crucial | - |
| Zhang et al., 2021 [ ] | - | Successful approaches vary depending on the overall goal of intervention and the local context. |
2.6. Data Synthesis
To synthesise the extracted data, a narrative synthesis method was used [ 47 ]. This approach enabled the authors to organise the results according to practices and principles, which were compared to and contrasted with the wider literature. This method allowed us to make further considerations, which are presented and contextualised in the discussions section below.
2.7. Triangulation Phase
On 21 March 2023, an EPIG was held during the “European Health Tech Summit”. This event took place in the form of two sessions (i.e., “Innovation and technology as gateways for a safer and healthier future—The impact of COVID-19 and lessons learned” and “Ensuring European and global preparedness for future crises”) with a panel of experts presenting cutting-edge research related to COVID-19 and telemedicine, followed by a dedicated Q&A slot. The event was hosted live and online to reach a wider audience. Speakers at the event include Members of the European Parliament, academics from European universities, and members of the European Commission. The sessions looked at the impacts of the COVID-19 pandemic on critical devices availabilities, discussed the importance of societal connections and broad cooperation, and debated the importance of telemedicine. The event was co-organised by the European Alliance of Medical and Biological Engineering and Science (EAMBES), the University of Warwick, and Member of the European Parliament Dr. Stelios Kympouropoulos (European People’s Party Coordinator of the Special Committee for COVID-19 (COVI) and Vice-Coordinator of the Committee for Public Health (SANT)).
The authors attended the event and used its notes and proceedings to ground the scoping review’s results in ongoing debates around science–policy–society interactions to improve preparedness. In particular, the authors focused on some of the discussions related to the potential of telemedicine and e-health solutions to revolutionise healthcare delivery (and the challenges); the ideas on pandemic management, which focused on users’ and media perspectives during a pandemic; the importance of bridging a gap between theoretical solutions (clinical guidelines) and real-world implementation; and, finally, the role played by collaboration during a pandemic. These themes were critically reflected upon, used to situate the scoping reviews’ findings, and presented in the discussions.
The search on Scopus and the study selection process is illustrated in Figure 1 . Indeed, the search returned 903 records, of which 24 met our inclusion criteria.

The PRISMA flowchart highlighting the selection process.
The characteristics of the included studies are illustrated in Table 2 . Most studies provided a narrative analysis of practices related to preparedness or pandemic response strategies. Three studies also used statistical methods to further analyse the impacts of practices [ 28 , 30 , 46 ]. Two studies gathered perceptions towards the deployment/communication of practices from groups such as healthcare professionals [ 37 , 45 ]. A broad range of practices was addressed, ranging from specific containment measures (e.g., social distancing, contact tracing, etc.) to overall governance strategies (e.g., the political ideology, high-level coordination of practices, etc.). These studies presented a vast number of practices and principles, ranging from public health control measures to public attitudes, as well as from media communication to government action. This paper aims to analyse them from a preparedness point of view; in other words, we draw on biomedical engineering, bioethics, and political ecology theories to understand how these actions, tools, principles, and practices can lead to better outcomes in the future. In the Anthropocene, which is characterised by ‘wicked problems’, preparedness has become an ever-more important pillar of sustainable disaster risk management practices [ 48 ]. Addressing complex issues requires a transdisciplinary approach, in which insights from various disciplines are harmonised, drawing from diverse expertise to foster novel insights [ 49 ]. Traditional siloed disciplines may offer deep knowledge but can fail to recognise the interconnectivity of systems involved. In the context of preparedness during the COVID-19 pandemic, this transdisciplinarity approach aids in understanding the intricate intersections of ecology, urbanisation, public health, socio-economic factors, and global connectivity. This paper embraces a transdisciplinary perspective, which will enable holistic strategies that account for the multifaceted nature of the challenges faced in the Anthropocene [ 50 ].
Based on the existing literature and guided via thematic analysis, we present the results in two different sections, i.e., practices and principles. Table 3 summarises areas for improvement, specific lessons learned, and opportunities for future action derived from each paper.
3.1. Practices
In this section, we present data regarding COVID-19 management practices, such as science–policy communication, contextualising responses, innovation technologies, and health practices.
3.1.1. Science–Policy–Society Communication
The COVID-19 pandemic brought significant public attention to the role played by science in policy-making, as well as the importance of the local socio-cultural context. Evans [ 42 ] presented lessons learned, from the perspective of the UK, from science-driven policy-making and the communication of policy decisions to the public. The study presented the challenges involved in establishing the reasonable levels of evidence required to undertake certain decisions, particularly when facing novel crises. The article noted that there is a difficult trade off in terms of the level of evidence required for a policy decision and the time taken to reach that decision and enact an effective policy. The paper also showed that it can be very difficult for governments to request the ‘right kind of advice’ from the scientific community—a challenge which may be remedied through better policy–research interactions and coordinated efforts. This study also addressed the need to improve the communication of science in general, in particular in relation to the communication of uncertainty. In a similar vein, Irwin [ 24 ] highlighted the need for the media to capture different ideas at different moments of the pandemic. This study stated that science–policy struggles did not appear in the news and the media generalised the impact of COVID-19, failing to report differences in its impact between different regions. According to Irwin, the media does not always distinguish between expertise, data, facts, and science, which is key for building trust between governments, populations, and the scientific community and reducing a pandemic’s impact on mental health.
Similar challenges in terms of widespread sensible communication were found by Upadhyay et al. [ 45 ], who analysed the perceptions of healthcare professionals in Indian Technical and Economic Cooperation (ITEC) countries towards the preparedness and responses of their countries during the COVID-19 pandemic. The top three most reported challenges were a lack of awareness among the public (67%), the undertesting of the susceptible population (81.4%), and a lack of appropriate personal protective equipment (PPE) (71.1%). Min et al. [ 28 ] explored communication in a similar way and looked at cultural perspectives and their impacts on control measures in the context of COVID-19 in Organisation for Economic Cooperation and Development (OECD) countries. Their argument was built on striking evidence that shows how a relationship between a nation’s cultural dimensions and its COVID-19 efficiency scores were important. The paper puts forward the idea that focusing on country-wide measures is not a particularly efficient approach; socio-economic context is key in finding appropriate measures, which must be tactfully communicated, to encourage a greater uptake and, ultimately, higher efficiency in pandemic management.
Bartels et al.’s [ 37 ] work on the case of North Carolina also focused on how public health officials communicated with each other and the general public. The state developed an interdisciplinary rapid-message testing model for COVID-19 to quickly create, test, and share messages with public health officials for use in health campaigns and policy briefings. The model focused on motivations for social distancing, rather than barriers to compliance, because behavioural scientists argue that how much a message motivates or discourages action is strongly correlated with actual behaviour and, therefore, provides a promising entry point for health behaviour decisions. Their study reported that survey participants rated messages focused on protecting themselves and others higher than those focused on norms and fear-based approaches. In fact, pairing behaviours with motivations increased participants’ desire to respect social distance measures across all themes and subgroups. Overall, this interdisciplinary model was a good example of rapid-message testing that reduced the time needed to deliver evidence-based messages and increased the relevance of research for policy makers and public health officials. However, the proposed model also has several limitations, such as key behaviours across the country changing as the pandemic evolved and the difficulties involved in achieving a representative sample in surveys. These characteristics limited the generalisability of the findings to the target audience.
3.1.2. Institutional Fragmentation: From Local Responses to Global Outcomes
Several of the identified studies emphasised the benefits of local and flexible responses to outbreaks. Zhang et al. [ 46 ] provided a comparison between non-pharmaceutical policies enacted in China and Germany in response to COVID-19, emphasising that policy choices reflected the differing goals of the two countries. In their work, they state that China’s aim was eliminating the virus, which was reflected by the employment of more stringent policies, such as locking down the worst-hit areas and initiating residential closed management. In contrast, Germany focused on restricting gatherings and contacts to reduce transmission, as their aim was the mitigation rather than elimination of diseases, and more specifically, the protection of high risk-groups. All of the analysed policies were shown to be effective, as they were all associated with a reduction in cases at different levels. For example, in China, the expansion of medical insurance coverage to suspected patients granted the highest association with a reduction in cases, while in Germany, the highest association was found for the ‘no-contact protocol’.
Agnew [ 34 ] showed the case of the Unites States government, where the conflict between different political ideologies (i.e., nationalism, federalism, etc.) and the politicisation of the pandemic, e.g., the use of the pandemic by President Trump for electoral purposes, led to the mismanagement of the healthcare emergency. This chaotic administrative approach and the conflict between the decentralisation and centralisation of management without coordination across tiers of government, according to the author, should have been replaced with a more polyphonic practice of federalism that would have led to better management of the pandemic. In turn, Moeenian et al. [ 29 ] proposed a different take based on a specific practice implemented in Iran. In this study, the focus is on the roles played by Non-Governmental Organisations (NGOs) in the Global South or emerging economies, as well as how they can be useful in the context of pandemic preparedness. The authors found that if the policies of existing bodies were aligned with those of NGOs, there was less of a chance of duplication and more efficient management and division of tasks. The study suggests that governments should establish institutions to facilitate communication with NGOs as, in some contexts, they have more speed and agility to tackle pandemics locally and influence national levels of efficiency. Similar results in terms of the higher efficacy of high political engagement combined with layered coordination were found by Ngoy et al. [ 30 ], who looked at coordination mechanisms that were used in the early stages of managing the COVID-19 pandemic in the WHO’s AFRO region.
Along similar lines, we considered Pennestrí et al.’s [ 31 ] evaluation of Lombardy’s response to the pandemic, which strove to improve coordination of not only overall institutional and governmental structures, but also healthcare facilities. The authors proposed to do so by leveraging telemedicine technology, especially in the early stages of a pandemic, to allow the remote monitoring and treatment of non-severe patients unless direct contact was necessary. Another key argument was made in the paper regarding the private medical sector and the need for clear requirements to be respected by private providers to tackle the cherry picking of patients and funding, as these have issues negative impacts on public health provision. In a different context, but putting forward a similar argument, we found Prajitha et al.’s [ 32 ] paper on the Indian State of Kerala’s initial response to the pandemic. The authors agreed with arguments outlining a need to reduce institutional fragmentation and push the analysis to prove that the impact of synergy between social capital, robust public health systems, participation, and volunteerism lead to stronger health system preparedness. Kerala’s example was brought forward as the government, learning from responses to past viral outbreaks, was able to base its healthcare on social justice and equity, including public–private partnerships that ensured adequate manpower and material resources, combined with community participation and awareness. Braithwaite et al.’s [ 38 ] paper also provided interesting conclusions around health practices. In their cross-sectional study of 40 health systems’ responses to COVID-19 (36 countries in the OECD area, plus Singapore, Malaysia, Taiwan, and Iran), they looked at data up to April 2020 regarding each government’s capacity to respond to a pandemic, stringency measures, and approaches to testing, as well as COVID-19 cases and deaths. The authors highlighted that even in situations in which a national government’s pre-pandemic capacity to respond was lacking, successfully adopting early stringent public health measures in response to COVID-19, such as testing and tracing, still made a substantial difference. In line with the other literature, the study shows that stringent measures are not sustainable in the longer term and broad-based testing and tracing was key in managing the virus. An interesting perspective is given around a government’s capacity to plan for different socioeconomic, cultural, and ethnic backgrounds, as policies will affect various people differently. In particular, the authors highlight the negative and knock-on effects of lockdowns in terms of the economy, as well as social justice.
3.1.3. Health Practices
This review would not be complete if it did not address best and worst practices regarding health measures prior to, during, and closely after the pandemic. Here, we present key data from authors who analysed these measures in different countries. Goodyear-Smith et al. [ 43 ] compared COVID-19 preparedness and responses in four countries (Australia, South Africa, Egypt, and Nigeria). A key finding of the study was the crucial role played by an integrated response between primary care and public health services in responding to the pandemic. The authors noted this finding has long been recognised as a crucial element of epidemic response. The study also found that there was inequity in the vaccination strategy, as well as testing, between High- and Low-Income Countries. This issue was demonstrated by the reduced capacity for testing in Nigeria and Egypt in contrast to Australia. Saleh et al. [ 33 ] highlighted that in order to improve pandemic responses, there must be accurate documentation of the strategies employed and lessons learned from previous outbreaks. In Nigeria, the Framework for a Public Health Emergency Operations Centre (PHEOC Framework) outlined by the WHO was used to create hubs for stakeholders across the public health structure in order to provide a platform for the learning, training, and documentation of practices. Ansah et al. [ 35 ] analysed the Singaporean Government’s intervention in the management of COVID-19 pandemic, which prioritised the mitigation strategy (which aims to limit movement at the population level; social distancing/community lockdown) to that of containment (quarantine based on contact tracing or their location). The authors stated that contact tracing, testing, and aggressive containment are key procedures that should be combined with social distancing, which is vital in slowing COVID-19, but much less effective when used alone. Among the best practices used to suppress the number of COVID-19 infections in Singapore, the authors pinpoint the following examples: (a) the timing of the intervention; (b) the contact tracing, in which Singapore had a strong experience learned from SARS and physical and operational infrastructure; (c) the revision of the Infectious Disease Act (IDA), which ensures that all measures needed to control any future outbreaks could be implemented. Along similar lines, Lee and Lim [ 26 ] put forward the idea that medical and economic measures should always come together in the case of viruses similar to COVID-19, which require containment or lockdowns to be effectively managed in the early stages of a pandemic. This approach is in line with the articles identified, which argue for context-specific measures and use Data Envelopment Analysis to show the way in which restrictions, when combined with sufficient and appropriate income support, livelihood aid, and public campaigning to inform and educate, made countries perform better from both economic and medical perspectives.
More specifically, in terms of correct practices, Atsawarungruangkit et al. [ 36 ] compared the criteria used to identify suspected cases of COVID-19 in 10 countries across Asia, Europe, and North America (China, Germany, Iran, Italy, Japan, South Korea, Taiwan, Thailand, the United Kingdom, and United States of America). Moving from the consideration that the rapid and accurate identification of suspected cases is critical in slowing spread of the virus that causes the disease, the authors aimed to highlight discrepancies in the various criteria used by international agencies and highly impacted individual countries around the world. The authors show that there was no one-size-fits-all guideline in this pandemic, and no best practice criterion has yet been defined. Every country has set its own criteria based on the principle of ALARA (As Low As Reasonably Achievable) based on available resources and the situation of the country, including budget, economic impact, insurance coverage, etc. The criteria defined by all of the reviewed countries were focused on specific symptoms and epidemiological risk assessment and may fail to capture or severely under-represent certain populations, including (a) asymptomatic cases, (b) patients with a financial barrier to accessing laboratory tests (owing to a lack of insurance coverage and high testing costs), and (c) patients with a legal barrier to accessing the health care system (including undocumented immigrants and homeless individuals). The proportion of cases in the latter two groups is dictated to a large extent by the government policies of individual countries. This paper clearly highlighted the need for the coordination of efforts not only by public health organisations, but also the public and private sectors, including health care systems and the insurance industry, and most importantly, citizens themselves.
3.1.4. Innovation Technology
Only two studies directly addressed the roles played by healthcare innovations in response to pandemics.
Halfmann et al. [ 44 ] proposed a theoretical framework for the creation and management of innovations in healthcare and Information And Communication Technology (ICT). The authors suggest 11 steps, which are outlined in an “innovation wheel”, focusing on monitoring, analysis, and development, as well as innovation management. Guidance is provided for each task to improve the innovation process and strengthen the systematic early dialog between stakeholders, especially between the Global North and Global South, which was found to be key in the process. This paper offers a framework to build capacity for innovation dimensions (such as partnership mobilisation, evaluation and monitoring, literacy, etc.) and emphasizes the active engagement of all stakeholders. This method is an interesting and novel instrument to help overcome current and future barriers in planetary health innovation management and support potential breakthrough discoveries in ICT. Goodyear-Smith et al. [ 43 ], tangentially to their main focus, also found that among all four countries evaluated, there was rapid adoption of telehealth in response to COVID-19. Telehealth was used to facilitate contact tracing and reduce the number of transmissions in health facilities. However, it is noteworthy that the ability to leverage technology and innovation is context dependent; Coral-Almeida et al.’s [ 41 ] study showed how the pandemic has negatively impacted digital access through an analysis of the management and impact of COVID-19 in Ecuador. The authors noted a widening of the digital divide and a need for a policy platform that promotes digital literacy and access, particularly among less advantaged socioeconomic groups.
3.2. Principles
In this section, we present the results of studies that address the risks of framing policies/interventions in terms of so-called ‘best practices’ [ 39 , 40 ]. For example, initiatives such as prescribed social distancing or isolation are entirely unfeasible if applied in crowded living situations. Instead, approaches should be localised, co-produced, and bottom-up in nature to ensure that effective practices are upheld without unwanted economic and social consequences.
3.2.1. Building Trust and Ways of Communication with the General Public
Canario Guzman et al. [ 39 ] called for a strengthening of research ethics and regulatory frameworks to facilitate strategic policy decisions that coordinate research efforts, aligning with priorities and ensuring accountability and transparency. The authors highlighted the importance of collaboration and knowledge sharing, both within and between national regulatory bodies. These findings were consistent with those of Chowdhury and Jomo [ 40 ], who emphasised that transparency and coordination in policymaking are crucial for building and maintaining trust between citizens and government. Mersha et al. [ 27 ] showed an interesting and specific aspect of trust-building activities, i.e., between government and healthcare professionals. Their study showed that in the context of South Omo (Ethiopia), there was a gap between the attitudes towards precautionary measures and their implementation in practice. In their paper, they argued that capacity-building activities aimed at healthcare professionals are a core part of pandemic preparedness and should be provided to ensure that the general public can follow them by copying their attitudes and actions.
3.2.2. Ethical Guidelines to Mediate the Relationship between Science and Policy-Making
Only two papers specifically addressed ethical concerns. Herstein et al. [ 23 ] described the functions of an existing preparedness network for global infectious diseases, focusing on the importance of rapid information exchange, which allowed the rapid adoption of treatments and protocols. The authors argued that using pre-existing or repurposing older networks as platforms for sharing preliminary information and giving access to real-time data before they are available in scientific or medical communities is a crucial step to take when preparing for further pandemics. Jegede et al. [ 25 ] argued that a framework and ethical guidelines are extremely valuable during a pandemic; building on the discourse around contextually sensitive measures, the authors showed that ethically sensitive communication and appropriate countermeasures had a positive impact on the public in the Global South.
4. Discussion
Preparedness strategies for health-related emergencies prior to COVID-19 were largely overlooked, leaving communities underequipped [ 16 ]. The literature and scoping reviews have shown that the time during a pandemic is not an ideal situation for building and training preparedness in terms of either resources or ethics [ 51 ]. However, as COVID-19 is no longer a PHEIC, looking back in hindsight and analysing practices and summarising the lessons learned from this major health challenge is now essential to improve our preparedness and foster evidence-based policymaking [ 9 , 52 ]. After analysing the existing literature reviews published since 2019 on the topic of interest (following the same search strategy presented above), it was found that only five were systematic. These reviews focused on the effectiveness of different strategies in terms of preventing the spread of COVID-19, and most of them included data up to 2020. In this context, the EPIG event helped to frame the literature and discussion by grounding it in existing and ongoing debates on preparedness practices, concepts, and principles. We are now able to learn more about how the world reacted to COVID-19 and which best and worst practices are emerging from the management of the pandemic worldwide.
Science–policy–society interactions play crucial roles in shaping the landscape of global health principles and practices. This review argues that post-pandemic reflections can help in bridging the gap between scientific research and public policy, especially if guided by community-led, culturally sensitive, and context-specific approaches.
Intuitively, we understand that state-of-the art research and the best available data and evidence should be used to guide public health decisions; however, in practice, the science–policy–society interface is much more complex. This review shows that an embedded model of communication, where there is specific attention to the roles played by scientific accuracy, policy-making needs, and societal contexts [ 53 ] as connected and communicating processes, is key in managing a pandemic. The EPIG event reported on the importance of interdisciplinary and sustainable collaboration amongst stakeholders, including policy makers, biomedical engineers, scientists, and society. This collaboration is key in terms of achieving sustainable and equitable data access and sharing, as well as advancing ideas for managing pandemics that can be easily adapted to diverse local contexts, moving beyond the Global South/Global North divide. In line with this European Parliament-level debate, we argue that in order to achieve harmonious communication between science, policy, and society, we need transdisciplinarity [ 54 ], as well as context-specific solutions, to improve communication. In attempting to avoid a siloed debate around a specific topic, we aimed to develop a Concept of Global Health that was in line with the latest declarations related to Agenda 2030 and the Sustainable Development Goals [ 55 ]. This method also offers interesting overlaps with the latest responsible co-production of knowledge approaches, acknowledging that communities (and, generally, society) should be at the forefront of knowledge co-creation to ensure their culture, priorities, and behaviours are respected, which, in turn, ensures a useful, usable, and, ultimately, used preparedness response [ 9 , 56 , 57 ].
There were extreme differences in pandemic management not only between countries, but also between administrative areas (states, regions, and municipalities) within countries. The review puts forward two key examples (Italy and the USA), where a regional fragmentation and a federal/state dichotomy prevented the more effective implementation of pandemic measures. In line with current research, we argue that these times of crises show systemic weaknesses that can be addressed once the emergency is called off, meaning that the countries can be better prepared for the next potential crisis [ 9 , 58 ]. Moreover, the politicisation of the decision-making process related to COVID-19 and the consequent impact on death rates and economic measures opened up significant questions about international law and cooperation during a pandemic [ 59 ]. The debate was also brought forward by the EPIG session, which called for a strong yet flexible global regulatory framework able to reflect rapid advancements in available technologies.
This approach is paramount in the context of the innovative technologies found in the literature. In fact, it can be noted that common themes emerge, such as the importance of contextualised approaches, which was a key finding in the included studies. We should indeed reflect on a minimum common denominator, such as Nussbaum’s “capabilities” of individuals and their “functionings” to be guaranteed and implemented in a manner appropriate to the specific context, in order to offer tailored responses to health threats [ 60 ]. Therefore, self-determination is one of the key factors: low-resource settings should shape their responses with regard to their own traditional beliefs [ 61 ], avoiding exacerbations of pre-existing gaps between the rich and the poor [ 62 ] and aiming to find a commonly shared perspective, i.e., that of human rights. The non-contextualised responses and practices can lead to no benefit and even be detrimental. For example, not taking into account the local Beninese culture of relying on traditional medicine and religious/mystical aspects or underestimating the lingering traces of colonialism slowed the uptake of allegedly “Western” approaches for COVID-19 management (e.g., plot theories of “whites” conspiring against the local population) [ 3 ]. The EPIG spoke of “responsible technologies”, which is a concept that incorporates sustainability, frugality, and social justice, meaning that healthcare innovation (digital technologies, such as contact tracing apps, telemedicine, etc.) can be globally deployed to enable accessible, affordable, and resilient healthcare that is integrated in a sustainable and equitable manner.
The included studies highlighted that there are common underlying principles that can be applied in a contextual framework to ensure fast and effective strategies and communication mechanisms. These mechanisms should be based on timely scientific evidence and available both to health practitioners and the general public. Improving communication, in this sense, also entails looking at mechanisms that maintain academic/scientific integrity while allowing the quicker turnaround of science–policy–society interactions. This approach means making full use of context-specific entry points that will promote a specific behaviour or behavioural change, using pre-existing networks and playing to countries’ strengths, which may mean many different (but coordinated) approaches, rather than a single, and sometimes inappropriate, pandemic strategy. While this concept is not new, it needs to be reiterated to ensure that further medical emergencies can be more efficiently managed.
This review also stresses the importance of fostering the creation and management of innovations in health emergencies. Indeed, this approach is aligned with a major challenge highlighted by Pecchia at the EPIG event, who sustained the inadequacy of the PPE standards and identified them as the culprit for slowing down the scaling up of the PPE production in the first wave of COVID-19. As reflected in both the literature and the discussions at the EPIG, telemedicine offers an opportunity to include the most remote and low-resource areas and reduce pressures on health services. However, there is a risk that inappropriate up-scaling of telemedicine may unintentionally exacerbate the digital divide [ 19 ]. Collaboration between countries is essential in this respect.
Finally, building trust remains a key step involved in improving the uptake of policies and measures and the willingness to adhere to regulations, as backed up by the decades of literature on social sciences [ 63 ]. While managing a crisis, decision makers and official bodies may lack the time and space to involve local communities, households, citizens, and people who will be most affected by their measures, resulting in actions that may lack ownership and seem more top down than co-produced [ 64 ]. In line with other recent studies [ 8 ], this review argues that sound ethical guidelines, ideally based on lessons learned in times of a pandemic, co-produced with relevant actors and globally generalisable (to be contextually adaptable) are a much-needed tool. This outcome stems from the need to frame science–policy–society communication in a way that keeps it grounded in data but flexible to potential bottom-up changes, easily adaptable, and ultimately useful, as well as used by the affected population. This review contributes to filling a gap and constitutes a starting point for a global reflection on the principles, ethics, and tools required to improve future preparedness.
Table 4 summarises the best and worst practices derived from the scoping review, as discussed in this study.
Best and worst practices of pandemic management based on our scoping review.
| Best Practices: | Worst Practices: |
|---|---|
| using hindsight to analyse practices and summarise lessons from the pandemic can improve future preparedness and evidence-based policymaking. | : The significant oversight of health-related emergency preparedness strategies led to communities being ill-equipped during the onset of COVID-19. |
| : A model where scientific accuracy, policy-making needs, and societal context are interconnected. This approach enhances the management of pandemics by ensuring that all stakeholders are aligned. | : Examples from Italy and the USA showed that regional differences in response strategies hindered effective pandemic management. |
| : it is crucial to involve communities, households, and citizens in decision-making to foster ownership and adherence. | : The politicisation of pandemic decisions impacted public health outcomes and the economy, highlighting the need for international cooperation and a unified approach. |
| : approaches tailored to local cultures, beliefs, and contexts lead to more effective and accepted health responses, thus avoiding one-size-fits-all strategies. | : For instance, neglecting the cultural aspects of regions like Benin slowed down the adoption of certain health practices. |
| : Technologies like contact tracing apps and telemedicine can be instrumental in pandemic responses. However, they must be deployed with sustainability, frugality, and social justice in mind. | : there is a risk with technologies like telemedicine; if not appropriately scaled, they might widen the digital divide. |
| : fast, accurate, and evidence-based communication mechanisms tailored to different stakeholders are pivotal. | : examples show that the rapid and widespread proliferation of both accurate and inaccurate information during a pandemic hinders the ability of a government to make informed decisions. |
| : promoting sustainable collaboration between policy makers, biomedical engineers, scientists, and society is essential for equitable data access and sharing. | when different departments, agencies, disciplines, and stakeholders operated in isolation without effective communication during COVID-19, there was a lack comprehensive and cohesive responses to the emergency and fewer opportunities for synergistic solutions derived from transdisciplinary cooperation. |
A few limitations of this study can be highlighted in this study. While Scopus is one of the largest citations databases covering peer-reviewed journals, being interdisciplinary in content and international in coverage, it does not include all existing evidence. Since our aim was to give an overall image of the existing practices involved in pandemic preparedness, we decided to limit our search to only refereed papers published in recognised international journals or selected conference proceedings. The results of this study could be extended by considering other indexes or grey literature. We also acknowledge a few gaps in the existing literature regarding pandemic management, including key data regarding policy collaboration and data sharing. Moreover, pandemics disproportionately affect more vulnerable populations; more research is needed not only on how COVID-19 may have impacted inequalities, but also on how preparedness can include mechanisms to avoid further unfairness. While decision-making frameworks used in pandemic planning and management are growing in use and sophistication, most policies and pathways are fragmented, siloed, and slow to integrate the needs of populations, especially marginalised groups, as they often sit outside of formal processes and structures. As we argue for a comprehensive ethical framework to be developed, we imply that research needs to boldly take the next step towards more collaborative, transdisciplinary, and transformative approaches to pandemic management, providing concrete entry points to ensure that these processes reduce, rather than reinforce, inequalities. A potential Delphi study to co-produce ethical guidelines and a practical toolbox for the transdisciplinary management of future healthcare emergencies would be a next step, as it would include participants from across global settings, disciplines, and fields.
5. Conclusions and Ethical Reflections
This work aimed to clarify, through a multi-methodological study of the global response to COVID-19, the best approaches to adopt during a pandemic emergency at an interdisciplinary level. Our scoping literature review, which was contextualised by the EPIG event, pinpointed key elements of best practices for pandemic management and governance (e.g., evidence based and effective IPC strategies, science–policy communication, contextualised responses, innovative technologies, and ethical guidelines). As we analysed these elements by drawing on multiple disciplines, as well as including a non-academic event, we argued that they can be considered to be a framework that could be prepared to enable the management of future health emergencies and should be placed at the core of future global conversations.
While our findings offer an essential roadmap for future health emergencies, the unpredictable nature of such events underscores a vital point: how do we practically prepare for the unknown? Sheila Jasanoff argues that the issue is related to “overestimating the certainty of our predictions and our capacity for control” [ 65 ]. Regarding COVID-19, she argues that it was the most anticipated of potential unexpected events. Moreover, she claims that “the shock of our era should remind us that such Promethean dreams [the dream to be able to master everything and outtake Nature] need to be curbed by the limits of prediction” [ 65 ].
As Jasanoff posits, perhaps it is time to shift from a purely technocratic mindset to one of “technologies of humility”. From a tangible standpoint, this approach means fostering more inclusive and diverse decision-making platforms, integrating both citizens’ voices and transdisciplinary expertise, thereby expanding the scope of perspectives within our governance structures [ 65 ].
A systematic mindset that deals with such unpredictable dangers should be cultivated using humility as a model [ 65 ]. Humility “occupies the nebulous zone between preparedness and precaution by asking a moral question: not what we can achieve with what we have, but how we should act given that we cannot know the full consequences of our actions” [ 65 ]. Humility anticipates consequences but, rather than absolving our responsibility for unforeseen consequences, “it demands that we ask in advance what new vulnerabilities might be produced by our bravest acts of preparedness, in theaters of public health, economy, environment, or war” [ 65 ]. We suggest that this approach could be combined with time and space to enable reflection and learning [ 9 ]. This multifaceted approach offers an opportunity to review and critically analyse best and worst practices with the aim of indicating a path forward. In this review, we do not predict or presume to control the unforeseen future; rather, we aim to maintain our “ethical vigilance” in order to move beyond a passive/reactive approach and towards an active and conscious disposition towards the unknown, while building sustainable, just, and equitable long-term resilience.
In reflecting on the global response to COVID-19, it is evident that a holistic and integrated approach is a necessity. The pitfalls of a siloed strategy, as observed in regional fragmentation and politicisation, underscore the imperative of seamless collaboration across disciplines, borders, and societal sectors. The merits of best practices, particularly those emphasising the harmonious confluence of science, policy, and society, underscore the importance of transdisciplinary and context-specific solutions, as well as the ethically sound co-production of knowledge. As we analyse the management of COVID-19, the overarching lesson is that true preparedness demands not only foresight, but also a unified, adaptable, and inclusive approach. Only through such integration can we hope to navigate the complexities of future health emergencies, fostering resilience and safeguarding global well-being.
In practical terms, we conclude that governance structures could benefit from creating dedicated spaces in which to perform reflective dialogues, i.e., sessions in which societal partners from diverse backgrounds critically evaluate both the successes and failures of previous strategies. These forums could serve as “learning labs/reflection spaces”, enabling us to adapt and innovate while acknowledging the inherent limitations of our foresight. Such an approach, being grounded in humility and active learning, positions us not as mere reactors to unforeseen events but as proactive stewards charting a course to enable sustainable and equitable resilience in an unpredictable world.
Funding Statement
This research was funded by the Wellcome Trust, award number 225238/Z/22/Z and by the Policy Support Fund of the University of Warwick. For the purpose of open access, the author has applied for a Creative Commons Attribution (CC BY) licence for any Author Accepted Manuscript version arising from this submission. The APC was funded by the Wellcome Trust, award number 225238/Z/22/Z.
Author Contributions
Conceptualization, A.M. and D.P.; methodology, C.A. and K.S.; formal analysis, C.A., K.S. and H.M.; data curation, C.A., K.S. and H.M.; writing—original draft preparation, A.M., C.A., K.S. and D.P.; writing—review and editing, A.M., D.P., C.A., K.S., S.S. and L.P.; visualization, C.A. and K.S.; supervision, D.P., A.M., L.P. and S.S.; funding acquisition, S.S., D.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study did not require ethical approval.
Informed Consent Statement
Not applicable.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest. The funders had no role in the design of the study; the collection, analyses, or interpretation of data; the writing of the manuscript; or the decision to publish the results.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

IMAGES
VIDEO
COMMENTS
For similar information about National Science Foundation (NSF) research, see the NSF FAQ. The Council on Government Relations is compiling a list of institutional and agency responses to the pandemic. Have an idea for research about preventing or treating COVID-19? See NSF's Dear Colleague Letter about how to submit a research proposal.
The COVID-19 pandemic has resulted in unprecedented research worldwide. The impact on research in progress at the time of the pandemic, the importance and challenges of real-time pandemic research ...
COVID-19 pandemic has severely impacted the crude, stock market, gold and metals and almost all areas of the global market [ 1 ]. Large research laboratories and corporate houses are working with a high speed to develop medicines and vaccines for the prevention and treatment of this dreaded disease. To deal with these current health management ...
Conducting such research has its challenges. The objective of this chapter is to review the impact of SARS-CoV-2 on ongoing and new pregnancy research during the pandemic, describe the challenges encountered and summarize the key strategies necessary for a successful research environment. Keywords: COVID-19, Pregnancy, Research, Pandemic.
Research cohorts are valuable tools for building pandemic research responses. Active cohort studies have the potential to play a key role in emerging epidemic and pandemic research. Longitudinal cohorts generate a wealth of data from individual participants about clinical and laboratory outcomes, which allow for a better understanding of effect ...
Fig. 6 shows that the impact of parameter η (average time that infected people have symptoms) on the dynamics of unreported symptomatic, reported symptomatic, and recovered individuals. The number of both unreported and reported infected people are significantly increased when the value of η becomes smaller, see Figs. 6 (a) and 6(b).
Research Administration. COVID-19 Information for Researchers. COVID-19 Research Proposals. Princeton University has authorized funding to support faculty research projects that consider biomedical, health-related and fundamental science related to the COVID pandemic, as well as those that impact corresponding policy, social, and economic topics.
In response to the coronavirus pandemic, we have witnessed a huge number of epidemiological, clinical and laboratory studies which are helping policy makers to understand how best to manage the current and future clinical and public health responses. In addition to impacting on infection and mortality rates due to COVID-19, government responses to reducing viral spread and 'flattening the ...
NIH aims to actualize the response to the COVID-19 pandemic by supporting research to understand SARS-CoV-2 and mitigate the threat of COVID-19 for the health of all people. NIH will build on existing research initiatives—and accelerate the development of new ones—that are focused on the five research priorities detailed in this strategic plan.
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages. The results of the analysis showed ...
When hundreds of millions of people are vaccinated, millions of them will be afflicted anyway, in the course of life, by conditions like strokes, anaphylaxis, and Bell's palsy. "We have to have faith that people collecting the data will let us know if we are seeing those things above the baseline rate.". 3.
The COVID-19 pandemic has propelled the research and higher education sectors to the forefront of public attention. Laboratory capacity has been crucial for diagnostic testing; experts in infectious diseases, epidemiology, public health, mathematical modelling, and economics are central to national policy making and media coverage; clinical research has been vital to improving COVID-19 ...
Introduction During the Covid-19 pandemic, major journals have published a significant number of Covid-19 related articles in a short period of time. While this is necessary to combat the worldwide pandemic, it may have trade-offs with respect to publishing research from other disciplines. Objectives To assess differences in published research design before and after the Covid-19 pandemic.
ABSTRACT RESEARCH PROPOSAL: COVID-19 PANDEMIC AND BIRTH EXPERIENCES: DESCRIBING THE RELATIONSHIP BETWEEN POLICIES AND THE BIRTH EXPERIENCES OF GEORGIA MOTHERS By KATHERINE RAECHEL THORNBURGH B.S., KENNESAW STATE UNIVERSITY December 5, 2020 INTRODUCTION: A pandemic such as COVID-19 increases stress during pregnancy or early development that can have an adverse effect on the health of an ...
A research and policy agenda for the post-pandemic world. The COVID-19 pandemic response has engaged the academic, public, private and health sectors in the real-time development of technologies and practices to enable predictive, preventive, personalised and participatory (P4) health. Myriad cases of collaborative innovation across these ...
Define your research question and objectives. 3. Review the literature and demonstrate your contribution. Be the first to add your personal experience. 4. Describe your methodology and plan. Be ...
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of "Viral: The Search for the Origin of Covid-19." This article has been updated to reflect news ...
The COVID-19 pandemic resulted in an overwhelming increase in research studies submitted to research ethics committees (RECs) presenting many ethical challenges. This article aims to report the challenges encountered during review of COVID-19 research and the experience of the Faculty of Medicine, Ain Shams University Research Ethics Committee (FMASU REC). From April 10, 2020, until October 13 ...
Science needs time, and good science needs a lot of it for data to grow and knowledge to evolve, but this process is ill-prepared to handle the rush for solutions to the COVID crises. ... which even the pandemic cannot stop. Whether this was the best option will certainly be analyzed in retrospect. Congenital anomalies alone account for over ...
In these times of rapid change, with high levels of uncertainty, anxiety, social isolation, and financial pressure, mental health worldwide is likely to be at risk. Researchers are rightly ensuring that mental health research is included in the response to the coronavirus disease 2019 (COVID-19) pandemic.1 Here, we reflect on ethical issues to consider when conducting research on self-harm ...
In academia, senior and tenured academics are more likely to have an established reputation, a stable salary commitment, and power within the academic system. They are more likely, before the COVID-19 pandemic began, to have established professional networks, generated data that can be used to write papers, and achieved financial and job security.
The COVID-19 pandemic has profoundly influenced the world. In wave after wave, many countries suffered from the pandemic, which caused social instability, hindered global growth, and harmed mental health. Although research has been published on various mental health issues during the pandemic, some profound effects on mental health are ...
The COVID-19 pandemic highlighted the scale of global unpreparedness to deal with the fast-arising needs of global health threats. This problem was coupled with a crisis of governance and presented in the context of globally hitting climate crisis and disasters. Although such a pandemic was predictable due to the known effects of human ...