- Open access
- Published: 07 August 2023

A scoping review of trauma informed approaches in acute, crisis, emergency, and residential mental health care
- Katherine R. K. Saunders 1 ,
- Elizabeth McGuinness 1 ,
- Phoebe Barnett 2 , 3 , 4 ,
- Una Foye 1 ,
- Jessica Sears 5 ,
- Sophie Carlisle 6 ,
- Felicity Allman 2 , 7 ,
- Vasiliki Tzouvara 8 ,
- Merle Schlief 2 ,
- Norha Vera San Juan 1 ,
- Ruth Stuart 1 ,
- Jessica Griffiths 1 ,
- Rebecca Appleton 2 ,
- Paul McCrone 9 , 10 ,
- Rachel Rowan Olive 11 , 12 ,
- Patrick Nyikavaranda 11 , 12 ,
- Tamar Jeynes 11 ,
- Lizzie Mitchell 11 ,
- Alan Simpson 1 , 7 ,
- Sonia Johnson 2 &
- Kylee Trevillion 1
BMC Psychiatry volume 23 , Article number: 567 ( 2023 ) Cite this article
5326 Accesses
1 Citations
47 Altmetric
Metrics details
Experiences of trauma in childhood and adulthood are highly prevalent among service users accessing acute, crisis, emergency, and residential mental health services. These settings, and restraint and seclusion practices used, can be extremely traumatic, leading to a growing awareness for the need for trauma informed care (TIC). The aim of TIC is to acknowledge the prevalence and impact of trauma and create a safe environment to prevent re-traumatisation. This scoping review maps the TIC approaches delivered in these settings and reports related service user and staff experiences and attitudes, staff wellbeing, and service use outcomes.
We searched seven databases (EMBASE; PsycINFO; MEDLINE; Web of Science; Social Policy and Practice; Maternity and Infant Care Database; Cochrane Library Trials Register) between 24/02/2022-10/03/2022, used backwards and forwards citation tracking, and consulted academic and lived experience experts, identifying 4244 potentially relevant studies. Thirty-one studies were included.
Most studies (n = 23) were conducted in the USA and were based in acute mental health services (n = 16). We identified few trials, limiting inferences that can be drawn from the findings. The Six Core Strategies (n = 7) and the Sanctuary Model (n = 6) were the most commonly reported approaches. Rates of restraint and seclusion reportedly decreased. Some service users reported feeling trusted and cared for, while staff reported feeling empathy for service users and having a greater understanding of trauma. Staff reported needing training to deliver TIC effectively.
TIC principles should be at the core of all mental health service delivery. Implementing TIC approaches may integrate best practice into mental health care, although significant time and financial resources are required to implement organisational change at scale. Most evidence is preliminary in nature, and confined to acute and residential services, with little evidence on community crisis or emergency services. Clinical and research developments should prioritise lived experience expertise in addressing these gaps.
Peer Review reports
Introduction
The concept of providing ‘trauma informed care’ (TIC) in healthcare settings has developed in response to increasing recognition that potentially traumatic experiences throughout the life course are associated with subsequent psychological distress and a range of mental health problems [ 1 , 2 , 3 , 4 ]. ‘Trauma’ has no universally agreed definition. The Substance Abuse and Mental Health Services Administration (SAMHSA) defined trauma as ‘an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being’ [ 5 ]. Traumatic experiences include physical, sexual and/or emotional abuse, neglect, exposure to violence or conflict, physical or mental illness (personal experience or that of a family member), and systemic or social traumas [ 6 , 7 ].
Individuals engaged with mental health services report high levels of childhood and adulthood trauma [ 2 , 8 , 9 , 10 ], and there is a high prevalence of trauma among service users in acute services, including among women [ 2 , 11 ], those with psychosis [ 12 , 13 ], and “personality disorder” diagnoses [ 14 ] (which is a particularly controversial diagnosis [ 15 ] as a result of the stigma associated with this diagnostic label and disparities in quality of care experienced [ 16 , 17 , 18 , 19 ]). Electronic health record evidence shows that service users with a history of abuse during childhood have more comorbidities and are more likely to have inpatient admissions versus service users without a similar history [ 20 ]. Similarly, among people with long-term mental health conditions, rates of childhood trauma and adversity are high, with both experiences theorised as aetiological factors for mental health conditions [ 21 , 22 , 23 ]. Staff in acute services are also affected by trauma experienced at work, which are highlighted as a source of stress and create a cycle of ‘reciprocal traumatisation’ [ 24 , 25 ].
Inpatient, crisis, emergency, and residential mental health care settings (typology of care categories adapted from an exploration of the range, accessibility, and quality of acute psychiatric services [ 26 ]) are used by service users experiencing severe mental health episodes. Such settings include acute wards, community crisis teams, psychiatry liaison teams within emergency departments, and mental health crisis houses. These settings can be experienced as destabilising and retraumatising as a result of compulsory detention under mental health legislation, e.g., the Mental Health Act in the UK [ 27 ] and routine staff procedures for managing the behaviour of distressed service users in inpatient settings, including seclusion and restraint [ 6 , 28 ]. These experiences can also constitute a traumatic experience in their own right [ 24 , 29 ]. Power imbalances in these settings can create abusive dynamics, as well as mirror previous abusive relationships and situations [ 6 ], engendering mistrust and creating a harmful environment.
In principle, TIC centres an understanding of the prevalence and impact of trauma, recognises trauma, responds comprehensively to trauma and takes steps to avoid re-traumatisation [ 5 ]. The TIC literature in healthcare is varied and lacks an agreed definition. However, Sweeney and Taggart (2018) [ 6 ], who both write from dual perspectives as researchers and trauma survivors, developed an adapted definition of TIC, [ 5 , 30 , 31 ] which we have used as a working definition throughout this scoping review as a result of its comprehensiveness. They define TIC as ‘a programme or organisational/system approach that: [i] understands and acknowledges the links between trauma and mental health, [ii] adopts a broad definition of trauma which recognises social trauma and the intersectionality of multiple traumas, [iii] undertakes sensitive enquiry into trauma experiences, [iv] refers individuals to evidence-based trauma-specific support, [v] addresses vicarious trauma and re-traumatisation, [vi] prioritises trustworthiness and transparency in communications, [vii] seeks to establish collaborative relationships with service users, [viii] adopts a strengths-based approach to care, [ix] prioritises emotional and physical safety of service users, [x] works in partnership with trauma survivors to design, deliver and evaluate services.’ This comprehensive definition includes elements covered by SAMSHA [ 32 ], the UK Office for Health Improvement & Disparities [ 33 ] and the NHS Education for Scotland (NES) Knowledge and Skills Framework for Psychological Trauma [ 34 ]. Understanding how experiences of trauma impact on individuals presenting in mental health services can support service users to feel heard, understood and able to cope or recover, and can support staff to have a greater understanding of the mental health difficulties and symptoms experienced by service users [ 6 , 31 , 35 ]. For TIC to be implemented, these tenets must be embedded within both formal and informal policy and practice [ 36 ], which can be challenging in these settings.
TIC within inpatient, crisis, emergency, and residential mental health care settings is newly established; there is no research mapping system-wide trauma informed approaches in these settings. The aim of this scoping review is to identify, map and explore the trauma informed approaches used in these settings, and to review impacts on and experiences of service users and staff. We also highlight gaps and variability in literature and service provision. TIC is a broad term, and it has been applied in numerous and varied ways in mental health care. In this review, we describe each application of TIC as a ‘trauma informed approach’.
This scoping review will answer the following primary research question:
What trauma informed approaches are used in acute, crisis, emergency, and residential mental health care?
Within each trauma informed approach identified, we will answer the following secondary research questions:
What is known about service user and carer expectations and experiences of TIC in acute, crisis, emergency, and residential mental health care?
How does TIC in acute, crisis, emergency, and residential mental health care impact on service user outcomes?
What is known about staff attitudes, expectations, and experiences of delivering TIC in acute, crisis, emergency, and residential mental health care?
How does TIC impact on staff practices and staff wellbeing in acute, crisis, emergency, and residential mental health care?
How does TIC in acute, crisis, emergency, and residential mental health care impact on service use and service costs, and what evidence exists about their cost-effectiveness?
Study design
This scoping review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR [ 37 ]), using a framework for conducting scoping reviews [ 38 ]. The PRISMA-ScR checklist can be seen in Appendix 1. The protocol was registered with the Open Science Framework ahead of conducting the searches ( https://osf.io/2b5w7 ). The review was steered by a team including academic experts, clinical researchers, and experts by experience and/or profession, with lived experience researchers contributing to the development of the research questions, the data extraction form, the interpretation, and the manuscript draft.
Eligibility criteria
Service users, or people who support or care for service users, of any age (both adults and children), gender or sexuality, or staff members (of any gender and sexuality) were included.
We included studies that focused (or provided disaggregated data) on care delivered within acute, crisis, emergency settings, or residential mental health settings; acute and crisis settings include inpatient, community-based crisis, hospital emergency department, acute day units and crisis houses. Forensic mental health and substance use acute, crisis and inpatient settings were also included. We excluded studies from general population prison settings, where there is debate as to whether TIC can be delivered in carceral settings ( 39 ), and residential settings where the primary purpose of the setting was not to provide mental health or psychiatric care (e.g., foster care or residential schools).
Intervention
Trauma informed care interventions. Programmes aiming to reduce restrictive practices in psychiatric settings were not included without explicit reference to TIC within the programme.
We included studies reporting any positive and adverse individual-, interpersonal-, service- and/or system-level outcomes, including outcomes from the implementation, use or testing of TIC. Individual-level outcomes are related to service user or staff experiences, attitudes, and expectations; interpersonal outcomes occur because of interactions between staff and service users; service-level outcomes include TIC procedures that occur on an individual service level; and system-level outcomes refer to broader organisational outcomes related to TIC implementation. We included studies exploring service user, staff and carer expectations and experiences of TIC approaches.
Types of studies
We included qualitative, quantitative, or mixed-method research study designs. To map TIC provision, service descriptions, evaluations, audits, and case studies of individual service provision were also included. We excluded reviews, conference abstracts with no associated paper, protocols, editorials, policy briefings, books/book chapters, personal blogs/commentaries, and BSc and MSc theses. We included non-English studies that our team could translate (English, German, Spanish). Both peer-reviewed and grey literature sources were eligible.
Search strategy
A three-step search strategy was used. Firstly, we searched seven databases between 24/02/2022 and 10/03/2022: EMBASE; PsycINFO; MEDLINE; Web of Science; Social Policy and Practice; Maternity and Infant Care Database (formerly MIDIRS); Cochrane Library Trials Register. An example full search strategy can be seen in Appendix 2. Searches were also run in one electronic grey literature database (Social Care Online); two pre-print servers (medRxiv and PsyArXiv), and two PhD thesis websites (EThOS and DART). The search strategy used terms adapted from related reviews [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ]. We added specific health economic search terms. No date or language limits were applied to searches. Secondly, forward citation searching was conducted using Web of Science for all studies meeting inclusion criteria. Reference lists of all included studies were checked for relevant studies. Finally, international experts, networks on TIC in mental health care, and lived experience networks were contacted to identify additional studies.
Study selection
All studies identified through database searches were independently title and abstract screened by KS, KT and NVSJ, with 20% double screened. All full texts of potentially relevant studies were double screened independently by KS and KT, with disagreements resolved through discussion. Screening was conducted using Covidence [ 50 ]. Studies identified through forwards and backwards citation searching and expert recommendation were screened by KS, EMG, and NVSJ.
Charting and organising the data
A data extraction form based on the research questions and potential outcomes was developed using Microsoft Excel and revised collaboratively with the working group. Information on the study design, research and analysis methods, population characteristics, mental health care setting, and TIC approach were extracted alongside data relating to our primary and secondary outcomes. The form was piloted on three included papers and relevant revisions made. Data extraction was completed by KS, EMG, VT, SC, and FA, with over 50% double extracted to check for accuracy by KS and EMG.
Data synthesis process
Data relevant for each research question was synthesised narratively by KS, EMG, JS, UF, VT, FA, and MS. Question 1 was grouped by approach and reported by setting. Where data was available, evidence for questions 2–6 was synthesised within each TIC approach.
Both quantitative and qualitative data were narratively synthesised together for each question. Areas of heterogeneity were considered throughout this process and highlighted. The categorisation and synthesis of the trauma informed approaches were discussed and validated by KS, EMG, JS, and KT.
The database search returned 4146 studies from which 2759 potentially relevant full-text studies were identified. Additional search methods identified 96 studies. Overall, 31 studies met inclusion criteria and were included in this review. The PRISMA diagram can be seen in Fig. 1 . Characteristics of all included studies are shown in Table 1 .
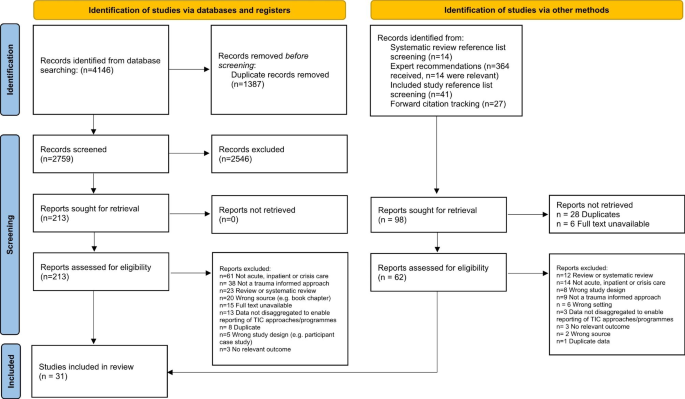
PRISMA diagram demonstrating the search strategy. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: https://doi.org/10.1136/bmj.n71 . For more information, visit: http://www.prisma-statement.org/
Study characteristics
The models reported most commonly were the Six Core Strategies (n = 7) and the Sanctuary Model (n = 6). Most included studies were based in the USA (n = 23), followed by the UK (n = 5), Australia (n = 2), and Japan (n = 1). Most studies were undertaken in acute services (n = 16) and residential treatment services (n = 14), while one was undertaken in an NHS crisis house. Over a third of studies were based in child, adolescent, or youth mental health settings (n = 12), while six were based in women’s only services. See Table 1 for the characteristics of all included studies.
Twenty-one studies gave no information about how they defined ‘trauma’ within their models. Of the ten studies that did provide a definition, four [ 51 , 52 , 53 , 54 ] referred to definitions from a professional body [ 5 , 55 , 56 ]; three studies [ 57 , 58 , 59 ] used definitions from peer-reviewed papers or academic texts [ 60 , 61 , 62 , 63 ]; in two studies [ 64 , 65 ], authors created their own definitions of trauma; and in one study [ 66 ], the trauma definition was derived from the TIC model manual. See full definitions in Appendix 3. Some studies reported details on participants’ experiences of trauma, these are reported in Table 1 .
What trauma informed approaches are used in inpatient, crisis, emergency, and residential mental health care?
Thirty-one studies in twenty-seven different settings described the implementation of trauma informed approaches at an organisational level in inpatient, crisis, emergency, and residential settings. The different models illustrate that the implementation of trauma informed approaches is a dynamic and evolving process which can be adapted for a variety of contexts and settings.
Trauma informed approaches are described by model category and by setting. Child and adolescent only settings are reported separately. Full descriptions of the trauma informed approaches can be seen in Appendix 3. Summaries of results are presented; full results can be seen in Appendix 4.
Six Core Strategies
Seven studies conducted in four different settings implemented the Six Core Strategies model of TIC practice for inpatient care [ 51 , 59 , 65 , 67 , 68 , 69 , 70 ]. The Six Core Strategies were developed with the aim of reducing seclusion and restraint in a trauma informed way [ 71 ]. The underpinning theoretical framework for the Six Core Strategies is based on trauma-informed and strengths-based care with the focus on primary prevention principles.
Inpatient settings: child and adolescent services
Four studies using Six Core Strategies were conducted in two child and adolescent inpatient settings using pre/post study designs [ 59 , 67 , 68 , 69 ]. Hale (2020) [ 67 ] describes the entire process of implementing the intervention over a 6-month period and establishing a culture change by 12 months, while Azeem et al’s (2015) [ 69 ] service evaluation documents the process of implementing the six strategies on a paediatric ward in the USA over the course of ten years.
Inpatient settings: adult services
Two studies focused on the use of the Six Core Strategies in adult inpatient and acute settings [ 51 , 65 ]. One further study, Duxbury (2019) [ 70 ], adapted the Six Core Strategies for the UK context and developed ‘REsTRAIN YOURSELF’, described as a trauma informed, restraint reduction programme, which was implemented in a non-randomised controlled trial design across fourteen adult acute and inpatient wards in seven hospitals in the UK.
How does the Six Core Strategies in inpatient, crisis, emergency, and residential mental health care impact on service user outcomes?
Five studies, only one of which had a control group [ 70 ], reported a reduction in restraint and seclusion practices after the implementation of the Six Core Strategies [ 59 , 67 , 68 , 69 , 70 ]. Two studies [ 51 , 65 ] did not report restraint and seclusion data.
What is known about staff attitudes, expectations, and experiences of delivering the Six Core Strategies in inpatient, crisis, emergency, and residential mental health care?
Staff reported an increased sense of pride in their ability to help people with a background of trauma [ 59 ], which came with the skills and knowledge development provided [ 51 ]. Staff also showed greater empathy and respect towards service users [ 51 , 65 ].
Staff recognised the need for flexibility in implementing the Six Core Strategies, and felt equipped to do this; as a result they reported feeling more fulfilled as practitioners [ 51 ]. Staff shifted their perspectives on service users and improved connection with them by viewing them through a trauma lens [ 65 ]. Staff also reported improved team cohesion through the process of adopting the Six Core Strategies approach [ 51 ]. It was emphasised that to create a safe environment, role modelling by staff was required [ 65 ].
How does the Six Core Strategies impact on staff practices and staff wellbeing in inpatient, crisis, emergency, and residential mental health care?
Service users were reportedly more involved in their own care; they reviewed safety plans with staff, and were involved in their treatment planning, including decisions on medication [ 51 , 65 ]. Staff and service users also engaged in shared skill and knowledge building by sharing information, support, and resources on healthy coping, and trauma informed care generally [ 51 , 65 ]. Staff adapted their responses to service user distress and adopted new ways of managing risk and de-escalating without using coercive practices [ 51 , 59 ]. Finally, service user-staff relationships were cultivated through a culture of shared learning, understanding, and trust [ 65 ].
How does the Six Core Strategies in inpatient, crisis, emergency, and residential mental health care impact on service use and costs and what evidence exists about their cost-effectiveness?
One study reported a reduction in the duration of hospital admission [ 59 ], which was largely attributed to the reduction in the amount of documentation that staff had to complete following crisis interventions.
The Sanctuary Model
Six studies, referring to five different settings [ 57 , 58 , 72 , 73 , 74 , 75 ], employed the ‘Sanctuary Model’ [ 76 ] as a TIC model of clinical and organisational change. One further study [ 72 ] combined the ‘Sanctuary Model’ with ‘Seeking Safety’, an integrated treatment programme for substance misuse and trauma. All studies were conducted in child and adolescent residential emotional and behavioural health settings in the USA.
The Sanctuary Model is a ‘blueprint for clinical and organisational change which, at its core, promotes safety and recovery from adversity through the active creation of a trauma-informed community’ [ 76 ]. It was developed for adult trauma survivors in short term inpatient treatment settings and has formally been adapted for a variety of settings including adolescent residential treatment programmes. No studies explored the use of the Sanctuary Model as a TIC approach in adult inpatient or acute settings, and no studies specifically tested the efficacy of The Sanctuary Model in child and adolescent settings. Studies employing the Sanctuary Model used a range of designs including longitudinal, qualitative methods, service evaluations/descriptions and a non-randomised controlled design.
What is known about service user and carer expectations and experiences of the Sanctuary Model in acute, crisis and inpatient mental health care?
In a service description, Kramer (2016) [ 57 ] reported that service users experienced clear interpersonal boundaries with staff, facilitated by healthy attachments and organisational culture. Service users also experienced staff responses as less punitive and judgemental.
How does the Sanctuary Model in acute, crisis and inpatient mental health care impact on service user outcomes?
Kramer (2016) [ 57 ] described decreasing rates of absconscion, restraint, and removal of service users from the programme post-implementation of the Sanctuary Model, which the authors hypothesised was due to the safe environment, and the movement towards a culture of hope.
What is known about staff attitudes, expectations, and experiences of delivering the Sanctuary Model in acute, crisis and inpatient mental health care?
Staff received the Sanctuary Model positively [ 72 , 73 ] and it gave them a sense of hopefulness [ 75 ]. However, it was widely acknowledged that it was resource intensive for staff to implement TIC in practice and additional training may be needed [ 73 ].
Korchmaros et al. (2021) [ 72 ] reported that the Sanctuary Model components most likely to be adopted were those that staff found most intuitive, though staff generally did not believe the model was acceptable in its entirety for their clinical setting. As staff communication improved, so did physical safety for staff and service users, and team meeting quality [ 75 ]. Staff appreciated the improved safety – or perception of such – after implementing the Sanctuary Model [ 73 , 75 ].
Staff reported that the Sanctuary Model promoted a healthy organisational culture with a commitment to a culture of social responsibility, social learning [ 57 ] and mutual respect [ 73 ].
How does the Sanctuary Model impact on staff practices and staff wellbeing in acute, crisis and inpatient mental health care?
Following implementation, staff focused more on service user recovery through teaching service users adaptive ways of coping and encouraging empathy and compassion towards service users [ 58 , 73 , 75 ]. Staff reported a holistic and compassionate understanding of the associations between trauma, adversity and service user behaviour [ 73 ]. Staff also reported sharing more decisions with service users [ 73 ] and collaboratively involving service users in their treatment care, safety plans, and in the development of community rules [ 73 , 75 ]. Staff felt able to communicate information, ideas, and their mistakes more openly, and their ability to model healthy relationships was seen as a fundamental to treatment [ 75 ].
How does the Sanctuary Model in acute, crisis and inpatient mental health care impact on service use and costs and what evidence exists about their cost-effectiveness?
One study reported a reduction in staff compensation claims due to a reduction in harms from physical interventions [ 72 ].
Comprehensive tailored trauma informed model
We categorised eight models [ 52 , 53 , 77 , 78 , 79 , 80 , 81 , 82 ] as ‘comprehensive tailored TIC models’. This reflects models that are holistic and multi-faceted, but do not closely follow an established TIC intervention model or blueprint and have instead been developed locally or to specifically complement the needs of a specific setting.
Residential settings: child and adolescent services
Three studies describe comprehensive tailored trauma informed models in child and adolescent residential treatment settings [ 77 , 78 , 79 ]. At an organisational level, key features of the tailored approaches include whole staff training using a trauma informed curriculum [ 77 , 78 , 79 ], creating a supportive, therapeutic environment and sense of community, using a family-centred approach, structured programmes of psychoeducational, social and skills groups [ 77 , 79 ] and collaborative working across different agencies [ 78 , 79 ].
Residential settings: adult women-only substance misuse service
Three studies [ 53 , 80 , 81 ] describe a gender-specific trauma informed treatment approach in a female only environment. Key components include providing training for all staff on trauma and trauma informed approaches, team support and supervision from a trained trauma therapist, social and life skills groups [ 53 ]; individual therapy and family support programme [ 81 ]; trauma informed group therapies and psychoeducation [ 53 , 80 ]; the implementation of a ‘gender specific, strengths based, non-confrontational, safe nurturing environment’ and strategic level meetings to identify structural barriers and gaps across different agencies [ 80 ]. Zweben et al. (2017) [ 81 ] focused specifically on family-centred treatment for women with severe drug and alcohol problems.
Inpatient settings: adults and children/adolescents
The ‘Patient Focussed Intervention Model’ [ 82 ] was implemented in a variety of settings including residential child and adolescent, adult acute and adult longer term inpatient stays. This model was developed using a collaborative process with involvement from service users, staff, administrators, and external collaborators with continuous quality improvement. The model incorporated (i) an individual TIC treatment model, which emphasised a patient-centred approach to building a culture and environment which is soothing and healing (e.g., by making changes to the physical environment and providing animal assisted therapy), (ii) the Sorensen and Wilder Associates (SWA) aggression management program [ 83 ] and (iii) staff debriefing after incidents of aggression.
Inpatient settings: women-only forensic service
Stamatopoulou (2019) [ 52 ] used qualitative research methods to explore the process of transitioning to a TIC model in a female forensic mental health unit [ 52 ] using the ‘trauma informed organisational change model’ [ 84 ]. Components included (i) staff training on trauma-informed care, (ii) co-produced safety planning through five sessions of Cognitive Analytic Therapy [ 85 ], (iii) a daily ‘Trauma Champion’ role for staff, and (iv) reflective practice groups for staff and service users.
What is known about service user and carer expectations and experiences of comprehensive tailored trauma informed models in inpatient, crisis, emergency, and residential mental health care?
In a study by Tompkins & Neale (2018) [ 53 ], service users reported being unaware that the service they were attending was trauma informed and were therefore not anticipating being encouraged to confront and reflect on their traumas [ 53 ]. However, the daily structure and routine timetable created a secure environment for their treatment experience. Service users who remained engaged with the service felt cared for by staff, and that the homely atmosphere in the service supported them to feel secure.
How do comprehensive tailored trauma informed models in inpatient, crisis, emergency, and residential mental health care impact on service user outcomes?
Three studies reported data on seclusion and restraints; all indicated a decrease [ 78 , 81 , 82 ]. Brown et al. (2013) [ 78 ] quantitatively reported reductions in the use of both seclusion and restraint in the year following Trauma Systems Therapy implementation, and the reduction in use of physical restraints was significant and sustained over the following eight years. Goetz et al. (2012) [ 82 ] also quantitatively reported that seclusion and restraint rates halved following implementation of the Patient Focused Intervention Model, as well as reductions in: (i) staff injuries, (ii) hours in seclusion and restraint and (iii) the number of aggressive patient events. However, while the number of seclusion room placements was lower, the average number of restraints among children and young people was higher in TIC compared to usual care.
Using a pre-post design, Zweben et al. (2017) [ 81 ] reported that service users receiving TIC reported fewer psychological and emotional problems after a month, compared to on entry to the programme, as well as reduced drug and alcohol misuse. Service user average length of stay was higher among those in the programme, compared to those not enrolled. Finally, as court and protective services became aware of the service users’ improvements, reunifications with children approached 100%.
What is known about staff attitudes, expectations, and experiences of delivering comprehensive tailored trauma informed models in inpatient, crisis, emergency, and residential mental health care?
Two papers reported on staff attitudes and experiences [ 52 , 53 ]. Some staff experienced introduction of TIC as overwhelming, leaving them unsure about what was expected from them throughout the training and implementation process, and that it might have been more successful had it been implemented in stages [ 52 ]. Some staff also felt unsure of what TIC entailed even after training, and it took time for staff to feel competent and confident [ 53 ]. Staff who had the least awareness of TIC experienced the greatest change anxiety when they were told of its implementation. When there were conflicting views within the team, the consistency of implementation was reduced [ 52 ]. Conversely, however, staff reported a sense of achievement in having implemented TIC and consequently an increased sense of job satisfaction.
Staff reported that their own traumatic experiences can inform the way they communicate and react to situations in the clinical environment, and they needed help to set boundaries and avoid emotional over involvement [ 53 ]. Implementing TIC broke down barriers between their private and professional selves, and there was an increased awareness of the personal impact of their work.
How do comprehensive tailored trauma informed models impact on staff practices and staff wellbeing in inpatient, crisis, emergency, and residential mental health care?
Stamatopoulou (2019) [ 52 ] reported that with the introduction of TIC, staff moved away from a solely diagnosis-based understanding of distress and developed an ability to formulate connections between service users’ backgrounds and their clinical presentations. As a result, staff showed empathy and respect towards service users and approached sensitive situations with service users more mindfully. Staff adopted new ways of managing risk [ 52 ] and service users were collaboratively involved in the development of treatment care plans [ 53 ]. Goetz et al. (2012) [82] also reported reduced staff injuries in the first year after implementing TIC.
There was an increased focus on staff wellbeing as well as greater awareness of staff personal boundaries and experiences of trauma and adversity, which led to staff feeling as though they had more in common with service users than expected [ 52 ]. Staff also discussed the importance of protecting their wellbeing by maintaining personal and professional boundaries, practicing mindfulness, and attending mutual aid groups [ 53 ].
Wider group relationships were reportedly redefined, and the impact of the work on staff wellbeing was acknowledged, specifically the ways in which staff’s own trauma informed their reactions to incidents on the ward [ 52 ]. Staff reported a greater sense of team connectedness, and that their individual professional identities were reconstructed.
How do comprehensive tailored trauma informed models in inpatient, crisis, emergency and residential mental health care impact on service use and costs and what evidence exists about their cost-effectiveness?
Staff had concerns over the sustainability of the model, especially in an organisation that could not offer the time or money required for service development [ 52 ]. Fidelity to a model varied depending on which staff were working; for instance, when agency staff or new joiners were working, fidelity was low and crisis incidents increased.
Adolescents in residential treatment receiving TIC spent significantly less time in treatment compared to those receiving traditional treatment, with the receipt of trauma informed psychiatric residential treatment (TI-PRT) accounting for 25% of the variance in length of stay [ 77 ]. Similarly, authors observed reduced length of hospital admissions after the introduction of their TIC approach [ 79 ].
Safety focused tailored trauma informed models
Two studies [ 86 , 87 ] tailored their own trauma-informed approach to create a culture of safety and (i) reduce restrictive practices and (ii) staff injuries. A third study [ 88 ] utilised a Trauma and Self Injury (TASI) programme, which was developed in the National High Secure Service for Women.
Inpatient settings: adults and child/adolescent services
Blair et al. (2017) [ 86 ] conducted a pilot trauma informed intervention study with the aim of reducing seclusions and restraints in a psychiatric inpatient hospital facility. Intervention components included the use of Broset Violence Checklist (BVC) [ 89 , 90 , 91 ]; 8-hour staff training in crisis intervention; two-day training in “Risking Connections” [ 92 ]; formal reviewing of restraint and seclusion incidents; environmental enhancements; and individualised plans for service users.
Borckardt et al. (2011) [ 87 ] reported a ‘trauma informed care engagement model’ to reduce restraint and seclusion across five various inpatient units (acute, child and adolescent, geriatric, general and a substance misuse unit). The intervention components included TIC training, changes in rules and language to be more trauma sensitive, patient involvement in treatment planning and physical changes to the environment.
Jones (2021) [ 88 ] reported the TASI programme in a high security women’s inpatient hospital, which aimed to manage trauma and self-injury with a view to reducing life threatening risks to service users and staff. The programme: (i) promotes understanding of trauma through staff training, staff support and supervision on the wards, (ii) provides psychoeducation and wellbeing groups for service users, (iii) focuses on the improvement of the therapeutic environment, (iv) promotes service users’ ability to cope with their distress, and (v) provides individual and group therapy.
What is known about service user and carer expectations and experiences of safety focused tailored trauma informed models in inpatient, crisis, emergency, and residential mental health care?
In Jones (2021) [ 88 ], some women reported feeling initially overwhelmed by and underprepared to acknowledge and work on their trauma experiences, and sometimes felt their distress was misunderstood by the nurses in their setting, which could lead to an escalation [ 88 ]. Service users felt connected to themselves, to feel safe and contained, particularly in comparison to previous inpatient experiences. Overall, however, the service did not make the women feel as though their problems were fully understood.
How do safety-focused tailored trauma informed models in inpatient, crisis, emergency, and residential mental health care impact on service user outcomes?
Reductions in the number of seclusions and restraint were reported [ 86 , 87 ]. Specifically, the trauma informed change to the physical therapeutic environment was associated with a reduction in the number of both seclusion and restraint [ 87 ]. The duration of restraints reportedly increased, while duration of seclusion decreased [ 86 ].
What is known about staff attitudes, expectations, and experiences of delivering safety focused tailored trauma informed models in inpatient, crisis, emergency, and residential mental health care?
In Jones (2021) [ 88 ], nurses emphasised that shared understanding and trust were instrumental in connecting and communicating with the women in their service [ 88 ]. Nurses also cultivated service user-staff therapeutic relationships, which they experienced as intensely emotional. The nurses reported becoming more critical of other staff members they perceived as lacking compassion towards the service users. Finally, staff felt that a barrier to the nurse-service user relationship was the staff’s inability to share personal information and vulnerability back to the service user.
How do safety focused tailored trauma informed models impact on staff practices and staff wellbeing in inpatient, crisis, emergency, and residential mental health care?
Staff developed new tools and adapted their responses to trauma and distress, and service users were also involved in some, but not all, staff training [ 88 ]. There were changes to information sharing practices [ 52 ]; information on service users’ history and intervention plans were more openly shared within the team to ensure all staff had the same information and did not need to risk re-traumatising service users by asking for information again. Service users also reported being more involved in their treatment planning [ 51 , 87 ] and medication decisions [ 65 ].
Trauma informed training intervention
Three studies focused on trauma informed training interventions for staff [ 66 , 93 , 94 ]. All studies used a pre/post design to evaluate effectiveness.
Gonshak (2011) [ 66 ] reported on a specific trauma informed training programme called Risking Connections [ 92 ] implemented in a residential treatment centre for children with ‘severe emotional disabilities’. Risking Connections is a training curriculum for working with survivors of childhood abuse and includes (i) an overarching theoretical framework to guide work with trauma and abuse (ii) specific intervention techniques (iii) a focus on the needs of trauma workers as well as those of their clients.
Niimura (2019) [ 93 ] reported a 1-day TIC training intervention, covering items including the definition of trauma, evidence on trauma and behavioural, social, and emotional responses to traumatic events, on attitudes of staff in a psychiatric hospital setting. Aremu (2018) [ 94 ] reported a training intervention to improve staff engagement which they identified as a key component of TIC. The intervention was a 2-hour training on engaging with patients, however the specific content of the training is not specified.
What is known about staff attitudes, expectations, and experiences of delivering trauma informed training interventions in inpatient, crisis, emergency, and residential mental health care?
Following training, half of staff reported feeling their skills or experience were too limited to implement changes and also that staff experienced difficulties when trying to share the principles of trauma informed care with untrained staff [ 93 ]. However, TIC training did produce positive attitude shifts towards TIC.
How do trauma informed training interventions impact on staff practices and staff wellbeing in inpatient, crisis, emergency, and residential mental health care?
Staff modified their communication with service users by altering their tone and volume, and adopted new ways of managing risk without using coercive practices [ 93 ]. There was also a reported a reduction in the use of as-needed medication [ 94 ].
How do trauma informed training interventions in inpatient, crisis, emergency, and residential mental health care impact on service use and costs and what evidence exists about their cost-effectiveness?
One study reported that educating staff about TIC in residential settings was time intensive and may require frequent or intense “booster” sessions following the initial training [ 66 ]. In terms of evaluation, it took time to implement TIC in the residential setting and then to collect related outcome data.
Other TIC models
This category reports studies which have made attempts to shift the culture towards trauma-informed approaches but have not made full-scale clinical and organisational changes to deliver a comprehensive trauma informed model [ 28 , 54 , 64 , 95 ].
Isobel and Edwards’ (2017) [ 64 ] case study on an Australian inpatient acute ward described TIC ‘as a nursing model of care in acute inpatient care’. This intervention was specifically targeted at nurses working on acute inpatient units but did not involve members of the multi-disciplinary team.
Beckett (2017) [ 95 ] conducted a TIC improvement project on an acute inpatient ward (which primarily received admissions through the hospital emergency department) using workforce development and a participatory methodology. Staff devised workshops on trauma informed approaches, through which six key practice areas were identified for improvement by the staff team.
Jacobowitz et al. (2015) [ 54 ] conducted a cross-sectional study in acute psychiatric inpatient wards to assess the association between TIC meetings and staff PTSD symptoms, resilience to stress, and compassion fatigue. Neither the content nor the structure of the ‘trauma informed care meetings’ were described in further detail.
Crisis house setting
Prytherch, Cooke & March’s (2020) [ 28 ] qualitative study of a ‘trauma informed crisis house’, based in the UK, gives a partial description of how trauma informed approaches were embedded in the service delivery and design.
What is known about service user and carer expectations and experiences of other TIC models in inpatient, crisis, emergency, and residential mental health care?
Prytherch, Cooke and March (2020) [ 28 ] reported that their TIC model created a positive experience for service users by making them feel worthwhile, respected and heard by staff [ 28 ]. Service users valued being trusted by staff, for example, to have their own room keys and to maintain their social and occupational roles, which were a key source of self-worth. While service user experiences were often positive, they found being asked directly about trauma challenging. This was invalidating for those who did not initially identify as having experienced trauma. Some service users also felt the TIC programme could only support them so far, as it did not incorporate or address wider societal injustices, such as issues related to housing and benefits, that can contribute to and exacerbate distress.
How do other TIC models in inpatient, crisis, emergency, and residential mental health care impact on service user outcomes?
Beckett et al. (2017) [ 95 ] reported that in the three years after the TIC workshops, rates of seclusion dropped by 80%, as did the length of time spent in seclusion, with most seclusions lasting less than an hour.
What is known about staff attitudes, expectations, and experiences of delivering other TIC models in inpatient, crisis, emergency, and residential mental health care?
Staff found an increased sense of confidence and motivation in managing emotional distress and behavioural disturbance [ 95 ]. Staff also showed increased respect, understanding and compassion towards service users.
Similarly, staff expressed hope for improved care in future, on the basis that they were better skilled to deliver care that was consistent and cohesive, while also being individual and flexible [ 64 ]. They reported a need for clarity and consistency in their role expectations and felt that changes in practice needed to be introduced slowly and framed positively. Conversely, others felt the changes introduced were too minimal to be significant and did not much vary from existing practice. Some staff expressed a fear of reduced safety that could follow changes to longstanding practice. Ambivalence to change stemmed from different degrees of understanding of TIC among staff, and others felt personally criticised by the newly introduced approach, specifically that their previous practice had been labelled traumatising.
How do other TIC models impact on staff practices and staff wellbeing in inpatient, crisis, emergency, and residential mental health care?
Some staff modified their communication with service users, e.g., reducing clinical jargon and focusing on the strengths of the service users [ 95 ]. Regular opportunities for service users and staff to discuss and reflect on information, concerns, and experiences were established. Staff received training in physical safety and de-escalation procedures; subsequently, the need for security staff on the ward decreased. Finally, in terms of staff wellbeing, staff PTSD symptoms increased with an increase in signs of burnout and length of time between attending trauma-informed care meetings [ 54 ].
Key findings
TIC approaches implemented in acute, crisis, emergency, and residential mental health settings were broad and varied. Studies that utilised either the Six Core Strategies model [ 71 ] or the Sanctuary Model [ 76 ] followed a clear structure to enact organisation and clinical change. Other studies implemented TIC models tailored to their specific settings, some with a particular emphasis on improving safety. The value of staff training was highlighted across studies, but the content of training was often described in limited detail, making it difficult to draw inferences around its comprehensiveness. Two principles from Sweeney and Taggart (2018) [ 6 ] that were often underrepresented in the TIC models were (i) recognising social traumas and the intersectionality of multiple traumas and (ii) working in partnership with trauma survivors to design, deliver and evaluate services. This indicates missed opportunities to use lived experience to develop services. Trauma itself was poorly defined, raising the question of whether TIC implementation can be truly meaningful without a clear framework of what trauma itself entails.
Service users were able to engage with their traumatic experiences and the implementation of TIC practice improved their ability to communicate their traumas. However, it is important to highlight that service users should not be required to share their experiences of trauma. The focus of TIC approaches in relation to empowering service users should also extend to giving them autonomy over when and how they disclose their traumatic experiences to staff [ 96 ]. While service users felt cared for, trusting, and trusted by staff working in TIC services, some distressing elements of service user experiences were not reflected in the TIC materials e.g., lack of access to housing or benefits, indicating a need for closer adaptation of TIC to the needs of service user populations.
Staff initially felt overwhelmed, anxious, criticised, and even reluctant at the introduction of TIC, though TIC positively influenced staff empathy, compassion, and wellbeing. Staff required time to build their skills and confidence, which once developed, led to pride and satisfaction in their roles. There were potential implications of delivering TIC for staff with histories of trauma also, e.g., providing staff with support and supervision to process those experiences. Future research could explore how trauma informed changes impact on staff turnover, a key concern in providing consistent care in inpatient and residential care settings.
Reductions in restraint and seclusion were observed, although the quality of evidence is limited as most studies are pre/post designs and lacked a comparison group. However, a broader question remains around whether services that continue to use restraint and seclusion (even in a reduced capacity) can be considered trauma informed.
There was a lack of economic evidence available, which highlights an area for future research. If TIC reduces rates of seclusion and restraint, reduces length of stays, as well as creates a more therapeutic environment (as reported in this review), this may have a positive economic impact, as conflict is costly [ 97 ] and patient satisfaction is associated with reduced costs [ 98 ]. There was also a lack of data on carers, perhaps due to our focus on specific settings, and very little evidence on hospital emergency departments (where care may be experienced as traumatising [ 99 ]), and on community-based crisis assessment services, home treatment, or acute day units, which future research could investigate.
Strengths and limitations
Our broad literature search retrieved evidence on TIC approaches in a variety of mental health settings. However, by nature of reviewing existing academic and grey literature, we are behind the curve of survivor thought and experience of TIC implementation. For example, information on the potential harms of poorly implemented TIC has been documented by people with lived experience [ 100 ], such as feeling required or coerced to confront their traumatic experiences. There was heterogeneity in the reporting of outcome measures across studies, limiting the generalisability of our conclusions. There was more data on residential mental health care settings compared to other settings, mirroring other review findings [ 101 ]; this may be due to their longer-term nature, which may be more amenable to the implementation and evaluation of TIC. This limits our understanding of TIC implementation and outcomes in other settings.
Although scoping review methodology does not require a quality assessment process, we noted significant methodological weaknesses across the included studies; they were primarily cross sectional, with few employing a control group or a randomised design, limiting our ability to draw causal conclusions about the impacts of TIC. Given the nature of this topic, particularly around mental healthcare reform, it is likely that work published in this area is subject to a range of potential biases that we were not able to examine in this study.
Implications for policy
A central tenet of TIC is empathy and understanding of the role of trauma in shaping mental health outcomes, which are positioned as being at the core of how mental health services can best support service users. Arguably, these principles should be a basic requirement of all mental health services, whether labelled as trauma informed or not. Introducing TIC into services may be a method by which basic practices can be integrated and maintained in a structured way [ 6 ]. This requires system-level change, which may be both time and financially resource intensive depending on, for example, the size of the organisation and staff, the time needed to design and provide training, and the policies and procedures which require revising. In theory, the introduction of TIC may challenge pre-existing clinical hierarchies through increased control and autonomy offered to service users and front-line staff, and so buy-in [ 58 ] and positive role modelling [ 65 ] from senior leaders within the service is vital for successful implementation.
Implications for practice
Delivering TIC in inpatient and residential settings requires clear and decisive leadership as well as clear staff roles [ 36 ]. In addition, TIC needs to be implemented, reviewed and evaluated collaboratively with service users to ensure it is delivering safe and appropriate care, otherwise services may continue to cause significant harm [ 100 ]. TIC could be included in pre-registration education across healthcare professions [ 102 , 103 ] and new starters may benefit from training as part of their inductions. Consistent staff supervision also supports the effective delivery of TIC [ 104 ]. These requirements result in a sustainability challenge as the creation and delivery of training is resource intensive, and staff turnover rates are high [ 105 ]. Clinicians should be aware of the intersection between trauma experiences, mental health, and social disadvantage, and the practical role that they may play at this intersection (e.g., providing supporting letters for housing or benefits). Clinical staff should also understand that issues relating to housing and welfare benefits, for example, can exacerbate mental health problems and responses to previous traumas, or even constitute traumatic experiences themselves [ 106 , 107 ]. Finally, clinicians should be conscious not to cause further harm through the delivery of TIC [ 100 ]; confronting and dealing with trauma should always be the choice of the service user, and receipt of TIC should not be dependent on service user willingness to engage with their traumatic experiences.
Implications for future research
We have identified significant evidence gaps around TIC implementation in non-inpatient acute care, including emergency, crisis teams, crisis houses, and acute day hospitals. Most evidence is concentrated within the USA, and there is a paucity of data on TIC elsewhere. Very few studies included control or comparison groups, crucially limiting our ability to determine the nature and strength of change due to TIC. With the development of other approaches to improving inpatient care, for example, Safewards [ 108 ], robust research methodologies must clarify the specific advantages of TIC. Future primary research could explore implementation of TIC in emergency and crisis mental health care settings, where it may be more difficult to implement a consistent and sustainable TIC approach as service users are engaged for shorter time periods. Future research could also consider the potential negative and harmful impacts of TIC. The present study could be extended to map the use of TIC in forensic settings, where poor mental health and experiences of trauma are also highly prevalent.
This scoping review has demonstrated the range of TIC approaches used in acute, crisis, and residential settings as well as a range of outcomes relating to service users and staff experiences, attitudes, and practises. TIC implementation requires commitment and strong leadership to enact organisational change, as well as appropriate training and supervision for staff and the involvement of service users in the design and delivery of approaches. Future research requires robust methods to accurately measure the impacts of TIC approaches and their potential benefits over existing care practices, through the utilisation of comparator conditions to TIC models. Research would also benefit from exploring how TIC impacts on carers; how trauma is understood in emergency services (settings that are frequently used by trauma survivors); and prioritising the expertise and views of those with lived experience with respect to how best to deliver TIC across mental health services.
Lived experience commentary
Written by LM and RRO.
As survivors of trauma from both within and outside mental health services, we welcome approaches which recognise its importance, and are pleased to see the range of perspectives which have been studied. We hope future research can engage with more work from outside the global north, which dominates in this paper.
However, from reading this literature, we do not know whether as patients we could always distinguish a trauma-informed service from any other - particularly given implementation challenges described in services with high levels of inconsistency, agency staff, new starters, and/or staff scepticism. At times trauma-informed care seems to be a means to an end which should already be universal, i.e., treating service users with respect and supporting our autonomy.
It does not particularly matter to us whether a service is trauma-informed on paper if the support staff change day by day and cannot or will not put the theory into practice. Nor does it matter that staff believe themselves to be validating our trauma, if they also retain power: if we can be physically held down; if the versions of ourselves written in their notes overwrite our autobiographies; if we have to surrender control of our most painful experiences in exchange for care. We have experienced some of these; we have heard about others happening to our peers, sometimes in the name of TIC (e.g. https://www.psychiatryisdrivingmemad.co.uk/post/trauma-informed-care-left-me-more-traumatised-than-ever ).
We welcome several studies showing reductions in restraint in trauma-informed environments (although note that this was not a universal finding). But we question whether a system founded on such violence can be anything other than traumatising in its own right. A version of TIC implemented in an under-resourced, fundamentally carceral system carries all the risks of harm associated with that system - with the added gaslighting of framing it as trauma-informed harm. As such, everyone involved in providing care they view as trauma-informed should consider what power over our stories and our bodies they are willing and able to give back.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Edwards DW, Scott CL, Yarvis RM, Paizis CL, Panizzon MS. Impulsiveness, impulsive aggression, personality disorder, and spousal violence. Violence Vict. 2003;18(1):3.
Article PubMed Google Scholar
Trevillion K, Oram S, Feder G, Howard LM. Experiences of domestic violence and Mental Disorders: a systematic review and Meta-analysis. PLoS ONE. 2012;7(12):e51740.
Article PubMed PubMed Central CAS Google Scholar
Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, et al. editors. Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo clinic proceedings; 2010: Elsevier.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–e66.
Huang LN, Flatow R, Biggs T, Afayee S, Smith K, Clark T et al. SAMHSA’s Concept of Truama and Guidance for a Trauma-Informed Approach. 2014.
Sweeney A, Taggart D. Mis) understanding trauma-informed approaches in mental health. Taylor & Francis; 2018. pp. 383–7.
Cohodes EM, Kribakaran S, Odriozola P, Bakirci S, McCauley S, Hodges H, et al. Migration-related trauma and mental health among migrant children emigrating from Mexico and Central America to the United States: Effects on developmental neurobiology and implications for policy. Dev Psychobiol. 2021;63(6):e22158.
Article PubMed PubMed Central Google Scholar
Khalifeh H, Moran P, Borschmann R, Dean K, Hart C, Hogg J, et al. Domestic and sexual violence against patients with severe mental illness. Psychol Med. 2015;45(4):875–86.
Article PubMed CAS Google Scholar
Oram S, Flynn SM, Shaw J, Appleby L, Howard LM. Mental illness and domestic homicide: a population-based descriptive study. Psychiatric Serv. 2013;64(10):1006–11.
Article Google Scholar
Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health surveys. Br J psychiatry. 2010;197(5):378–85.
Fisher H, Morgan C, Dazzan P, Craig TK, Morgan K, Hutchinson G, et al. Gender differences in the association between childhood abuse and psychosis. Br J Psychiatry. 2009;194(4):319–25.
Inyang B, Gondal FJ, Abah GA, Dhandapani MM, Manne M, Khanna M et al. The role of childhood trauma in psychosis and schizophrenia: a systematic review. Cureus. 2022;14(1).
Bebbington PE, Bhugra D, Brugha T, Singleton N, Farrell M, Jenkins R, et al. Psychosis, victimisation and childhood disadvantage: evidence from the second British National Survey of Psychiatric Morbidity. Br J Psychiatry. 2004;185(3):220–6.
Porter C, Palmier-Claus J, Branitsky A, Mansell W, Warwick H, Varese F. Childhood adversity and borderline personality disorder: a meta‐analysis. Acta psychiatrica Scandinavica. 2020;141(1):6–20.
Dale O, Sethi F, Stanton C, Evans S, Barnicot K, Sedgwick R, et al. Personality disorder services in England: findings from a national survey. BJPsych Bull. 2017;41(5):247–53.
Campbell K, Clarke K-A, Massey D, Lakeman R. Borderline personality disorder: to diagnose or not to diagnose? That is the question. Int J Ment Health Nurs. 2020;29(5):972–81.
Evans S, Sethi F, Dale O, Stanton C, Sedgwick R, Doran M et al. Personality disorder service provision: a review of the recent literature. Mental Health Review Journal. 2017.
Ring D, Lawn S. Stigma perpetuation at the interface of mental health care: a review to compare patient and clinician perspectives of stigma and borderline personality disorder. J Mental Health. 2019:1–21.
Sheridan Rains L, Echave A, Rees J, Scott HR, Lever Taylor B, Broeckelmann E, et al. Service user experiences of community services for complex emotional needs: a qualitative thematic synthesis. PLoS ONE. 2021;16(4):e0248316.
Werbeloff N, Hilge Thygesen J, Hayes JF, Viding EM, Johnson S, Osborn DP. Childhood sexual abuse in patients with severe mental illness: demographic, clinical and functional correlates. Acta psychiatrica Scandinavica. 2021;143(6):495–502.
Coughlan H, Cannon M. Does childhood trauma play a role in the aetiology of psychosis? A review of recent evidence. BJPsych Adv. 2017;23(5):307–15.
Rafiq S, Campodonico C, Varese F. The relationship between childhood adversities and dissociation in severe mental illness: a meta-analytic review. Acta psychiatrica Scandinavica. 2018;138(6):509–25.
Matheson S, Shepherd AM, Pinchbeck R, Laurens K, Carr VJ. Childhood adversity in schizophrenia: a systematic meta-analysis. Psychol Med. 2013;43(2):225–38.
Spandler H, McKeown M. Exploring the case for truth and reconciliation in mental health services. Mental Health Review Journal. 2017.
Rössler W. Stress, burnout, and job dissatisfaction in mental health workers. Eur Arch Psychiatry Clin NeuroSci. 2012;262(2):65–9.
Johnson S, Dalton-Locke C, Baker J, Hanlon C, Salisbury TT, Fossey M, et al. Acute psychiatric care: approaches to increasing the range of services and improving access and quality of care. World Psychiatry. 2022;21(2):220–36.
Akther SF, Molyneaux E, Stuart R, Johnson S, Simpson A, Oram S. Patients’ experiences of assessment and detention under mental health legislation: systematic review and qualitative meta-synthesis. BJPsych Open. 2019;5(3).
Prytherch H, Cooke A, Marsh I. Coercion or collaboration: service-user experiences of risk management in hospital and a trauma-informed crisis house. Psychosis. 2021;13(2):93–104.
Cohen LJ. Psychiatric hospitalization as an experience of trauma. Arch Psychiatr Nurs. 1994;8(2):78–81.
Elliott DE, Bjelajac P, Fallot RD, Markoff LS, Reed BG. Trauma-informed or trauma‐denied: principles and implementation of trauma‐informed services for women. J community Psychol. 2005;33(4):461–77.
Sweeney A, Filson B, Kennedy A, Collinson L, Gillard S. A paradigm shift: relationships in trauma-informed mental health services. BJPsych Adv. 2018;24(5):319–33.
Substance A, Mental Health Services A. Substance abuse and Mental Health Administration’s (SAMSHA) concept of trauma and guidance for a trauma-informed approach. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. p. 27.
Google Scholar
Office for Health Improvement & Disparities. Working definition of trauma-informed practice. In: Disparities OfHI, editor.; 2022.
NHS Education for Scotland. Transforming Psychological Trauma: A Knowledge and Skills Framework for the Scottish Workforce. 2017.
Sweeney A. Trauma-informed mental healthcare in the UK: what is it and how can we further its development? Mental Health Review Journal. 2016;21(3):174–92.
Bryson SA, Gauvin E, Jamieson A, Rathgeber M, Faulkner-Gibson L, Bell S, et al. What are effective strategies for implementing trauma-informed care in youth inpatient psychiatric and residential treatment settings? A realist systematic review. Int J mental health Syst. 2017;11(1):1–16.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Miller NA, Najavits LM. Creating trauma-informed correctional care: a balance of goals and environment. Eur J psychotraumatology. 2012;3(1):17246.
Lloyd-Evans B, Slade M, Jagielska D, Johnson S. Residential alternatives to acute psychiatric hospital admission: systematic review. Br J Psychiatry. 2009;195(2):109–17.
Niccols A, Milligan K, Sword W, Thabane L, Henderson J, Smith A. Integrated programs for mothers with substance abuse issues: a systematic review of studies reporting on parenting outcomes. Harm Reduct J. 2012;9(1):1–11.
Carpenter RA, Falkenburg J, White TP, Tracy DK. Crisis teams: systematic review of their effectiveness in practice. The Psychiatrist. 2013;37(7):232–7.
Iozzino L, Ferrari C, Large M, Nielssen O, De Girolamo G. Prevalence and risk factors of violence by psychiatric acute inpatients: a systematic review and meta-analysis. PLoS ONE. 2015;10(6):e0128536.
de Andrade D, Elphinston RA, Quinn C, Allan J, Hides L. The effectiveness of residential treatment services for individuals with substance use disorders: a systematic review. Drug Alcohol Depend. 2019;201:227–35.
Staniszewska S, Mockford C, Chadburn G, Fenton S-J, Bhui K, Larkin M, et al. Experiences of in-patient mental health services: systematic review. Br J Psychiatry. 2019;214(6):329–38.
Stewart NA, Wilkinson-Tough M, Chambers GN. Psychological interventions for individuals with a diagnosis of borderline personality disorder in forensic settings: a systematic review. J Forensic Psychiatr Psychol. 2019;30(5):744–93.
Alford M, O’Rourke S, Doyle P, Todd L. Examining the factors associated with impulsivity in forensic populations: a systematic review. Aggress Violent Beh. 2020;54:101409.
Alsuhaibani R, Smith DC, Lowrie R, Aljhani S, Paudyal V. Scope, quality and inclusivity of international clinical guidelines on mental health and substance abuse in relation to dual diagnosis, social and community outcomes: a systematic review. BMC Psychiatry. 2021;21(1):1–23.
Malik N, Facer-Irwin E, Dickson H, Bird A, MacManus D. The effectiveness of trauma-focused interventions in prison settings: a systematic review and meta-analysis. Violence, & Abuse: Trauma; 2021. p. 15248380211043890.
Covidence. Covidence systematic review software. 2017.
Chandler G. Reducing Use of Restraints and Seclusion to create a culture of Safety. J PsychoSoc Nurs Ment Health Serv. 2012;50:29–36.
Stamatopoulou V. Transitioning to a trauma informed forensic unit: staff perceptions of a shift in organisational culture. 2019.
Tompkins CNE, Neale J. Delivering trauma-informed treatment in a women-only residential rehabilitation service: qualitative study. Drugs: Educ Prev Policy. 2018;25(1):47–55.
Jacobowitz W, Moran C, Best C, Mensah L. Post-traumatic stress, trauma-informed care, and compassion fatigue in psychiatric hospital staff: a correlational study. Issues Ment Health Nurs. 2015;36(11):890–9.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub; 2013.
Association AP. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC2000.
Kramer MG. Sanctuary in a residential treatment center: creating a therapeutic community of hope countering violence. Therapeutic communities: The International Journal of therapeutic communities. 2016.
Rivard J, Bloom S, McCorkle D, Abramovitz R. Preliminary results of a study examining the implementation and effects of a trauma recovery framework for youths in residential treatment. Therapeutic Community: The International Journal for Therapeutic and Supportive Organizations. 2005;26.
Hale R. Implementation of a trauma-informed Care Program for the reduction of Crisis Interventions. Walden University; 2019.
Black PJ, Woodworth M, Tremblay M, Carpenter T. A review of trauma-informed treatment for adolescents. Can Psychol. 2012;53(3):192.
Cook A, Blaustein M, van der Spinazzola J. Complex trauma in children and adolescents: white paper from the national child traumatic stress network complex trauma task force. Los Angeles: National Center for Child Traumatic Stress. 2003;35(5):390–8.
n der Kolk B. Posttraumatic stress disorder and the nature of trauma. Solomon MFaS, D.J, editors, editor. New York, NY2003.
Scheidlinger S. Group interventions for treatment of psychological trauma. New York. 2004:64.
Isobel S, Edwards C. Using trauma informed care as a nursing model of care in an acute inpatient mental health unit: a practice development process: TRAUMA INFORMED MODEL OF CARE. Int J Ment Health Nurs. 2016;26.
Chandler G. From traditional inpatient to trauma-informed treatment: transferring control from staff to patient. J Am Psychiatr Nurses Assoc. 2008;14:363–71.
Gonshak AB. Analysis of trauma symptomology, trauma-informed care, and student-teacher relationships in a residential treatment center for female adolescents. Electronic Theses and Dissertations: University of Louisville; 2011.
Hale R, Wendler MC. Evidence-based practice: implementing trauma-informed care of children and adolescents in the inpatient psychiatric setting. J Am Psychiatr Nurses Assoc. 2020:1078390320980045.
Azeem MW, Aujla A, Rammerth M, Binsfeld G, Jones RB. Effectiveness of six core strategies based on trauma informed care in reducing seclusions and restraints at a child and adolescent psychiatric hospital. J Child Adolesc Psychiatric Nurs. 2011;24(1):11–5.
Azeem MW, Reddy B, Wudarsky M, Carabetta L, Gregory F, Sarofin M. Restraint reduction at a pediatric psychiatric hospital: a ten-year journey. J Child Adolesc Psychiatric Nurs. 2015;28(4):180–4.
Duxbury J, Baker J, Downe S, Jones F, Greenwood P, Thygesen H, et al. Minimising the use of physical restraint in acute mental health services: the outcome of a restraint reduction programme (‘REsTRAIN YOURSELF’). Int J Nurs Stud. 2019;95:40–8.
Huckshorn KA, CAP I, Director N. Six core strategies to reduce the use of seclusion and restraint planning tool. Washington, DC: National Association of State Mental Health Program Directors; 2005.
Korchmaros JD, Greene A, Murphy S. Implementing trauma-informed research-supported treatment: Fidelity, Feasibility, and acceptability. Child Adolesc Soc Work J. 2021;38(1):101–13.
Prchal KM. Implementing a new treatment philosophy in a residential treatment center for children with severe emotional disturbances: a qualitative study. Columbia University; 2005.
Farragher B, Yanosy S. Creating a trauma-sensitive culture in residential treatment. Therapeutic Communities. 2005;26(1):97–113.
Rivard JC, McCorkle D, Duncan ME, Pasquale LE, Bloom SL, Abramovitz R. Implementing a trauma recovery framework for youths in residential treatment. Child Adolesc Soc Work J. 2004;21(5):529–50.
Bloom SL. Creating sanctuary: toward the evolution of sane societies. Routledge; 2013.
Boel-Studt S. A quasi-experimental study of trauma-informed Psychiatric Residential treatment for children and adolescents. Res Social Work Pract. 2015;27.
Brown AD, McCauley K, Navalta CP, Saxe GN. Trauma systems therapy in residential settings: improving emotion regulation and the social environment of traumatized children and youth in congregate care. J family violence. 2013;28(7):693–703.
Forrest S, Gervais R, Lord KA, Sposato A, Martin L, Beserra K, et al. Building communities of care: a comprehensive model for trauma-informed youth capacity building and behavior management in residential services. Residential Treat Child Youth. 2018;35(4):265–85.
Cadiz S, Savage A, Bonavota D, Hollywood J, Butters E, Neary M, et al. The portal project: a layered approach to integrating trauma into alcohol and other drug treatment for women. Alcoholism Treat Q. 2005;22(3–4):121–39.
Zweben JE, Moses Y, Cohen JB, Price G, Chapman W, Lamb J. Enhancing family protective factors in residential treatment for substance use disorders. Child Welfare. 2015;94(5):145–66.
PubMed Google Scholar
Goetz SB, Taylor-Trujillo A. A change in culture: violence prevention in an acute behavioral health setting. J Am Psychiatr Nurses Assoc. 2012;18(2):96–103.
Wilder SS, Sorensen C. Essentials of aggression management in health care. Pearson; 2001.
Harris ME, Fallot RD. Using trauma theory to design service systems. Jossey-Bass/Wiley; 2001.
Ryle A, Poynton AM, Brockman BJ. Cognitive-analytic therapy: active participation in change: a new integration in brief psychotherapy. John Wiley & Sons; 1990.
Blair EW, Woolley S, Szarek BL, Mucha TF, Dutka O, Schwartz HI, et al. Reduction of seclusion and restraint in an inpatient psychiatric setting: a pilot study. Psychiatr Q. 2017;88(1):1–7.
Borckardt JJ, Madan A, Grubaugh AL, Danielson CK, Pelic CG, Hardesty SJ, et al. Systematic investigation of initiatives to reduce seclusion and restraint in a state psychiatric hospital. Psychiatric Serv. 2011;62(5):477–83.
Jones J. How distress is understood and communicated by women patients detained in high secure forensic healthcare, and how nurses interpret that distress: an exploration using a multi-perspective interpretative phenomenological analysis. University of Derby (United Kingdom); 2021.
Almvik R, Woods P. The Brøset Violence Checklist (BVC) and the prediction of inpatient violence: some preliminary results. Psychiatric Care. 1998;5:208–13.
Almvik R, Woods P, Rasmussen K. The Brøset Violence Checklist: sensitivity, specificity, and interrater reliability. J interpers Violence. 2000;15(12):1284–96.
Woods P, Almvik R. The Brøset violence checklist (BVC). Acta psychiatrica Scandinavica. 2002;106:103–5.
Saakvitne KW, Gamble S, Pearlman LA, Lev BT. Risking connection: A training curriculum for working with survivors of childhood abuse. 2000.
Niimura J, Nakanishi M, Okumura Y, Kawano M, Nishida A. Effectiveness of 1-day trauma‐informed care training programme on attitudes in psychiatric hospitals: A pre–post study. Int J Ment Health Nurs. 2019;28(4):980–8.
Aremu B, Hill PD, McNeal JM, Petersen MA, Swanberg D, Delaney KR. Implementation of trauma-informed care and brief solution-focused therapy: a quality improvement project aimed at increasing engagement on an inpatient psychiatric unit. J PsychoSoc Nurs Ment Health Serv. 2018;56(8):16–22.
Beckett P, Holmes D, Phipps M, Patton D, Molloy L. Trauma-informed care and practice: practice improvement strategies in an inpatient mental health ward. J PsychoSoc Nurs Ment Health Serv. 2017;55(10):34–8.
Tarzia L, Bohren MA, Cameron J, Garcia-Moreno C, O’Doherty L, Fiolet R, et al. Women’s experiences and expectations after disclosure of intimate partner abuse to a healthcare provider: a qualitative meta-synthesis. BMJ open. 2020;10(11):e041339.
Flood C, Bowers L, Parkin D. Estimating the costs of conflict and containment on adult acute inpatient psychiatric wards. Nurs Econ. 2008;26(5):325–32.
Sabes-Figuera R, McCrone P, Csipke E, Craig TK, Rose D, Sharma B, et al. Predicting psychiatric inpatient costs. Soc Psychiatry Psychiatr Epidemiol. 2016;51(2):303–8.
DeLeo K, Maconick L, McCabe R, Broeckelmann E, Rains LS, Rowe S et al. Experiences of crisis care among service users with complex emotional needs or a diagnosis of’personality disorder’, and other stakeholders: systematic review and meta-synthesis of the qualitative literature. BJPsych Open. 2022;8(2).
Langley LP. Eleanor. Death By A Thousand Cuts: Report into the Tees, Esk and Wear Valleys NHS Foundation Trust “BPD+” Protocol. 2022.
Muskett C. Trauma-informed care in inpatient mental health settings: a review of the literature. Int J Ment Health Nurs. 2014;23(1):51–9.
Wilson A, Hutchinson M, Hurley J. Literature review of trauma-informed care: implications for mental health nurses working in acute inpatient settings in Australia. Int J Ment Health Nurs. 2017;26(4):326–43.
Goddard A, Jones RW, Esposito D, Janicek E. Trauma informed education in nursing: a call for action. Elsevier; 2021. p. 104880.
Rothwell C, Kehoe A, Farook S, Illing J. The characteristics of effective clinical and peer supervision in the workplace: a rapid evidence review. Newcastle: Newcastle University; 2019.
Woltmann EM, Whitley R, McHugo GJ, Brunette M, Torrey WC, Coots L, et al. The role of staff turnover in the implementation of evidence-based practices in mental health care. Psychiatric Serv. 2008;59(7):732–7.
Tsai J, Schick V, Hernandez B, Pietrzak RH. Is homelessness a traumatic event? Results from the 2019–2020 National Health and Resilience in Veterans Study. Depress Anxiety. 2020;37(11):1137–45.
Wickham S, Bentley L, Rose T, Whitehead M, Taylor-Robinson D, Barr B. Effects on mental health of a UK welfare reform, Universal Credit: a longitudinal controlled study. The Lancet Public Health. 2020;5(3):e157–e64.
Bowers L. Safewards: a new model of conflict and containment on psychiatric wards. J Psychiatr Ment Health Nurs. 2014;21(6):499–508.
Download references
Acknowledgements
We would like to thank the NIHR LEWG for their contributions to this project, including researcher T.K. We would like to acknowledge the academic and lived experience experts who shared resources with us, and recommended papers for inclusion.
This paper presents independent research commissioned and funded by the National Institute for Health Research (NIHR) Policy Research Programme, conducted by the NIHR Policy Research Unit (PRU) in Mental Health. The views expressed are those of the authors and not necessarily those of the NIHR, the Department of Health and Social Care or its arm’s length bodies, or other government departments. JS was funded by an NIHR pre-doctoral clinical academic fellowship (2021–2022) and by the Psychiatry Research Trust in partnership with KCL (2022–2023).
Author information
Authors and affiliations.
NIHR Mental Health Policy Research Unit, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, David Goldberg Building, De Crespigny Park, SE5 8AF, London, UK
Katherine R. K. Saunders, Elizabeth McGuinness, Una Foye, Norha Vera San Juan, Ruth Stuart, Jessica Griffiths, Alan Simpson & Kylee Trevillion
NIHR Mental Health Policy Research Unit, Division of Psychiatry, University College London, London, UK
Phoebe Barnett, Felicity Allman, Merle Schlief, Rebecca Appleton & Sonia Johnson
Centre for Outcomes Research and Effectiveness, Research Department of Clinical, Educational, & Health Psychology, University College London, London, UK
Phoebe Barnett
National Collaborating Centre for Mental Health, Royal College of Psychiatrists, London, UK
South London and Maudsley NHS Foundation Trust, London, UK
Jessica Sears
Section of Women’s Mental Health, King’s College London, London, UK
Sophie Carlisle
School of Medical Education, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, UK
Felicity Allman & Alan Simpson
Care for Long Term Conditions Research Division, King’s College London, London, UK
Vasiliki Tzouvara
Institute for Lifecourse Development, University of Greenwich, London, UK
Paul McCrone
School of Health Sciences, University of Greenwich, London, UK
NIHR Mental Health Policy Research Unit Lived Experience Working Group, Division of Psychiatry, University College London, London, UK
Rachel Rowan Olive, Patrick Nyikavaranda, Tamar Jeynes, T. K & Lizzie Mitchell
Department of Primary Care & Public Health, Brighton & Sussex Medical School, University of Sussex, Brighton, UK
Rachel Rowan Olive & Patrick Nyikavaranda
You can also search for this author in PubMed Google Scholar
Contributions
Formulating the research question(s): SJ, KT, AS, KS, PB, PM, NVSJ, RS, RRO, TJ, PN, TK, LM. Designing the study: SJ, KT, AS, KS, PB, PM, NVSJ, RS, LM, RRO, TJ, PN, TK. Conducting the study (including analysis): KS, KT, EM, JS, UF, FA, PB, SC, VT, MS, NVSJ, JG. Writing and revising the paper: KS, KT, SJ, AS, EM, JS, RS, UF, PB, SC, VT, MS, NVSJ, RA, JG, RRO.
Corresponding author
Correspondence to Katherine R. K. Saunders .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1 (PRISMA-ScR) Checklist
Supplementary material 2 embase search terms, supplementary material 3 table of trauma informed care models, supplementary material 4 table of study characteristics and results, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Saunders, K.R.K., McGuinness, E., Barnett, P. et al. A scoping review of trauma informed approaches in acute, crisis, emergency, and residential mental health care. BMC Psychiatry 23 , 567 (2023). https://doi.org/10.1186/s12888-023-05016-z
Download citation
Received : 30 January 2023
Accepted : 10 July 2023
Published : 07 August 2023
DOI : https://doi.org/10.1186/s12888-023-05016-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Systematic review
- Open access
- Published: 05 May 2023
Barriers and enablers for the implementation of trauma-informed care in healthcare settings: a systematic review
- Yan Huo 1 ,
- Leah Couzner 1 ,
- Tim Windsor 1 ,
- Kate Laver 2 ,
- Nadeeka N. Dissanayaka 3 , 4 , 5 &
- Monica Cations ORCID: orcid.org/0000-0002-9262-0463 1
Implementation Science Communications volume 4 , Article number: 49 ( 2023 ) Cite this article
7553 Accesses
5 Citations
3 Altmetric
Metrics details
Healthcare services can be re-traumatising for trauma survivors where they trigger memories of past distressing events and exert limits to a survivor’s sense of autonomy, choice, and control. The benefits of receiving trauma-informed healthcare are well established; however, factors that promote or impede the implementation of trauma-informed care are not yet well characterised and understood.
The aim of this review was to systematically identify and synthesise evidence regarding factors that promote or reduce the implementation of TIC in healthcare settings.
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) 2.0 guidelines. Scopus, MEDLINE, Proquest, PsycINFO and grey literature were searched for original research or evaluations published between January 2000 and April 2021 reporting barriers and/or facilitating factors for the implementation of trauma-informed care in a healthcare setting. Two reviewers independently assessed the quality of each included study using the Mixed Methods Appraisal Tool (MMAT) Checklist.
Twenty-seven studies were included, 22 of which were published in the USA. Implementation occurred in a range of health settings, predominantly mental health services. The barriers and facilitators of implementing trauma-informed care were categorised as follows: intervention characteristics (perceived relevance of trauma-informed care to the health setting and target population), influences external to the organisation (e.g. interagency collaboration or the actions of other agencies) and influences within the organisation in which implementation occurred (e.g. leadership engagement, financial and staffing resources and policy and procedure changes that promote flexibility in protocols). Other factors related to the implementation processes (e.g. flexible and accessible training, service user feedback and the collection and review of initiative outcomes) and finally the characteristics of individuals within the service or system such as a resistance to change.
Conclusions
This review identifies key factors that should be targeted to promote trauma-informed care implementation. Continued research will be helpful for characterising what trauma-informed care looks like when it is delivered well, and providing validated frameworks to promote organisational uptake for the benefit of trauma survivors.
Registration
The protocol for this review was registered on the PROSPERO database (CRD42021242891).
Peer Review reports
Contributions to the literature
The impacts of psychological trauma have important implications for the provision and receipt of healthcare.
This systematic review identifies key factors that should be targeted to promote trauma-informed care implementation, including interagency collaboration, staff and leadership buy-in, aligning implementation strategies with existing policies and procedures, allocation of adequate human and financial resources, flexibility in organisational policies and procedures, ongoing and tailored training, participatory co-design, and the collection and monitoring of data.
Identifying factors that influence implementation success across trauma-informed care initiatives can help to inform the selection of implementation strategies and planning.
Up to 70% of the population will experience exposure to one or more psychologically traumatic event in their lifetime [ 1 ]. Psychologically traumatic events are those events perceived by the individual as threatening to their safety and/or overwhelming to their ability to understand and make sense of the experience [ 2 ]. While most people will recover from traumatic stress, exposure to these events can have lasting adverse effects including reduced quality of life and risk for psychological disorders, non-suicidal self-injury, and suicide [ 3 , 4 ].
The impacts of psychological trauma on interpersonal skills, perception, problem-solving, and other core abilities and experiences have important implications for the provision and receipt of healthcare. Healthcare services can present risk for re-traumatisation where they trigger memories of past distressing events and exert limits to a survivor’s sense of autonomy, choice, and control [ 5 , 6 ]. Hypervigilance to threat and impaired emotion regulation skills mean that care behaviours and environments can trigger a fight or flight response that can manifest as externalising (e.g. aggression) or internalising behaviour (e.g. withdrawal). This can result in the use of seclusion and restraint, which have major negative impacts on quality of life and quality of healthcare services [ 7 ].
Recognition of these impacts prompted the development of trauma-informed care in mental health and other settings where most service users have experienced psychological trauma [ 7 , 8 , 9 ]. Trauma-informed care (TIC) is a care approach in which services are organised to ensure that all staff have a basic understanding of the potential impact of traumatic stress and can amend care to promote safety, choice, autonomy, collaboration, and respect. Staff in TIC settings are not necessarily expected to treat the symptoms of trauma, but pathways for care recipients to access treatments for trauma are known and used by all staff [ 10 ].
Organisational interventions aiming to promote the delivery of trauma-informed care have been implemented in healthcare settings in several contexts, including mental health services, inpatient emergency departments, hospital wards, and palliative care [ 10 , 11 ]. For the purposes of this review, trauma-informed organisational interventions refer to organisation-level interventions (as opposed to individual clinician or service user interventions) aiming to improve staff awareness and understanding of traumatic stress across an organisation (or within a specific group of staff), and/or establishing organisational policies and processes to meet trauma-related needs. Efforts to improve the capability of clinicians to deliver trauma therapies and treatments are out of scope of this review.
Research has demonstrated that organisational interventions to promote delivery of trauma-informed healthcare can promote well-being among survivors, improve staff skills and collaboration, reduce the use of seclusion and restraint, and reduce the prevalence of the secondary effects of trauma including drug and alcohol use [ 6 ]. However, the implementation of TIC involves a paradigm shift that requires a complex organisational change process encompassing workforce upskilling, organisational change, development of clear referral pathways, environmental change, and other implementation strategies [ 12 , 13 ]. Such broad change requires significant time and resources, and evaluation of outcomes at the organisational and/or systems level. Factors that promote or impede implementation of TIC are not yet well characterised and understood [ 10 ]. Understanding contextual, organisational, and implementation-specific factors that promote the uptake and effectiveness of an intervention can help to guide more efficient and sustainable implementation. This review, which sits on the ‘green line’ of the implementation science subway [ 14 ], is a critical step toward identifying and designing effective implementation strategies to implement TIC more widely.
As such, the aim of this review was to systematically identify and synthesise evidence regarding factors that promote or reduce the effectiveness and/or implementation of TIC in healthcare settings.
The research questions to be answered were:
What facilitating factors improve the effectiveness and/or implementation of TIC in healthcare settings?
What factors act as barriers that limit the effectiveness and/or implementation of TIC in healthcare settings?
We conducted a systematic review following the guidance of the Cochrane Qualitative and Implementation Methods Group Guidance Series and report our findings according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2.0 (PRISMA 2.0) guidelines [ 15 ]. A checklist of PRISMA 2.0 items is presented in Supplementary Table S 1 . The review protocol was registered on the PROSPERO database (CRD42021242891).
Data sources and searches
We conducted a search of Scopus, MEDLINE, Proquest, and PsycINFO for English language studies published from January 2000 to April 2021. The search strategy is presented in Supplementary Table S 2 and combined concepts related to the intervention (TIC), the setting (healthcare settings), and the outcome (barriers and facilitating factors for implementation). Reference lists of all included studies were hand-searched for additional records. We also searched grey literature via a Google search, Open Grey Europe, the Grey Literature Report, Web of Science, and report publications from relevant peak bodies (e.g. the International Society for Traumatic Stress Studies, American Psychiatric Association, Phoenix Australia).
Eligibility criteria
We included studies published since the year 2000 and in English, reporting original research or evaluation, and that reporting barriers and/or facilitating factors for the effectiveness or implementation of a TIC initiative in a healthcare setting. Studies published prior to 2000 were excluded because the TIC framework was not well-defined in research before this time [ 8 ]. Studies were excluded if they did not report original research or evaluation data (e.g. literature reviews, study protocols), were published prior to the year 2000, could not be accessed by the research team, or were not available in English.
Intervention and implementation strategies
Studies included in this review described strategies to implement TIC. TIC has been criticised for lacking an agreed operational definition [ 16 ] and what constitutes ‘trauma-informed care’ varies between settings. For this review, interventions or systems of care specifically described as “trauma-informed” were included. Similarly to previous reviews on TIC (e.g. [ 17 ]), we were deliberately broad in accepting the authors’ definition of TIC given the lack of an existing operational definition. Broadly, we accepted studies that described efforts to improve staff awareness and understanding of psychological trauma and organisational policies and processes to better to meet trauma-related needs.
Included studies described implementation at the organisational level. In this case, ‘initiative’ is used to describe a discrete strategy or set of strategies aiming to implement the principles of TIC within the organisation. An organisational initiative was defined as any initiative listed in the Cochrane Effective Practice and Organisation of Care Review Group data collection taxonomy [ 18 ] Sects. 2.1.3 (e.g. revision of professional roles, environmental changes, consumer participation in governance) or educational strategies listed in 2.1.1 (e.g. distribution of educational materials, local opinion leaders) as long as they were conducted at an organisation level. That is, educational strategies had to be delivered within an organisation/system to all staff or key staff who were expected to diffuse the information to others. System-level interventions to improve access or pathways to suitable trauma treatments were included.
Studies describing interventions targeted at individual clinicians (e.g. professional development to deliver a particular therapy for PTSD) or individual service users (e.g. evaluating the effectiveness of particular PTSD treatments) were excluded.
‘Healthcare organisations’ included primary, secondary and tertiary healthcare settings (e.g. acute and subacute hospital services, primary care, outpatient clinics, residential mental health treatment centres, ambulatory care, etc.). Mental health services, including drug and alcohol services, were included. Child welfare and out-of-home care services (including residential welfare centres) were excluded unless they included a healthcare component.
Finally, included studies were required to measure and report quantitative and/or qualitative data regarding factors that influenced initiative or implementation outcomes. Barriers were defined as any factor reported to impede implementation efforts, and facilitators were any factors reported to enable implementation.
Study screening and data extraction
One reviewer (YH) screened all titles and removed irrelevant papers. Abstracts and full texts were screened for eligibility by two reviewers (YH and MC) using an eligibility checklist based on the criteria described above. Disagreements about inclusion were resolved via discussion between the reviewers, and a third reviewer (LC) was consulted where consensus could not be reached. Study authors were contacted where more information was required to confirm eligibility for inclusion in this review. Data extraction was conducted by one reviewer (YH) using a data extraction spreadsheet that was piloted with five studies before being finalised and being used with the remaining studies. The accuracy of data extraction was validated by a second reviewer. Extracted data included the study’s first author and year of publication, design, setting, population, number of sites, initiative elements (e.g. implementation strategies), outcome data type (e.g. qualitative, quantitative, mixed), evaluation method, implementation outcomes reported, barriers identified, and facilitating factors identified. Intervention outcomes were out of scope of this review so were not reported here.
Quality assessment
The Mixed Methods Appraisal Tool (MMAT) Checklist, shown in Supplementary Table S 3 , was used to assess the quality of each included study. The validity, robustness, and applicability of each included study was appraised by two team members (YH and BW-H) independently and in duplicate [ 19 ].
Data management, analysis, and synthesis
The implementation strategies used in each study were synthesised into broad categories and mapped to the ERIC compilation of implementation strategies independently by two authors (YH and MC). These authors examined the features of each strategy and aligned these features with the most closely related category, and disagreements (which occurred for 8 out of 27 studies) were resolved on discussion with a third reviewer (LC).
The core aim of this paper was the synthesise data about barriers and facilitating factors for implementation. As such, this process involved a more detailed, two-step process modelled on the method of a recent review of barriers and facilitating factors for person-centred care in long-term care settings [ 20 ]. First, two authors (YH and MC) independently used a thematic analysis approach to group barriers and facilitating factors into recurrent themes (e.g. lack of collaboration, time constraints). Themes were consolidated on discussion and a second independent round of coding was conducted by both reviewers with new emerging themes added to the codebook iteratively. A final, third round of coding was conducted by one reviewer for refinement (MC). In the second step of the synthesis, the themes were mapped to the Consolidated Framework for Implementation Research (CFIR) by both reviewers [ 21 ]. All discrepancies were resolved via discussion. Mapping to CFIR aimed to provide organised guidance to researchers, service providers, and policy makers about the key contextual and initiative features that promote or limit success when implementing TIC. CFIR is a determinant framework designed to predict or explain barriers and facilitators to implementation success [ 22 ], and is therefore well suited to our aim of capturing, organising and describing common barriers and facilitators to implementing TIC organisational interventions.
The initial search identified 3051 original results, of which 170 were retrieved in full text and screened against the review inclusion and exclusion criteria. Most exclusions were due to the implementation occurring in a non-health-related care setting. A total of 27 studies were included, reported across 28 publications (Supplementary Figure S 1 ).
Study characteristics and implementation strategies
Characteristics of the included studies are described in Table 1 . Of the 27 included studies, 22 described efforts to implement TIC into healthcare settings in the United States of America (USA). The remaining five studies were conducted in Australia ( n = 3) and Canada ( n = 2). Implementation occurred in mental health settings ( n = 15), maternal and women’s health settings ( n = 2), paediatric health settings ( n = 2), primary care clinics ( n = 3), emergency departments ( n = 1), or across whole systems within a geographical area including health, policy, child welfare, and other social services ( n = 4). Implementation occurred within single health sites for eight studies, and the remainder reported implementation in multiple sites or across a whole service system. Nine of the studies explicitly described using existing implementation frameworks, theories and/or models to design and evaluate their implementation strategies, including the Exploration, Preparation, Implementation and Sustainment (EPIS) framework [ 23 , 24 ], the Service Integration Framework [ 25 , 26 ], Chen’s theoretical framework for program evaluation [ 27 , 28 ], CFIR [ 21 , 29 ], and models of rapid cycle implementation [ 30 , 31 ]. Other studies conducted a review of TIC implementation literature but did not explicitly design their strategy or evaluation against a specific framework (e.g. [ 32 , 33 ]).
Strategies used to implement the principles of TIC were similar across the included studies. Mapped to the ERIC compilation of implementation strategies [ 55 ], all but one study included some form of staff education and training, ranging from a single educational meeting (e.g. [ 41 , 43 ]), implementing train-the-trainer strategies [ 32 , 50 , 53 ], providing regular clinical supervision [ 27 , 36 , 38 , 52 ], creating learning collaboratives [ 32 , 47 ], modelling change [ 37 , 40 , 41 , 34 ], developing educational materials for new employees [ 32 , 42 , 48 , 34 ], to conducting ongoing training (e.g. [ 39 ]). Some programs identified and prepared ‘champions’, who received (or had pre-existing) a higher level of training and were available as peer mentors [ 47 , 34 ], while others committed resources to the ongoing availability of experts for consultation [ 25 , 35 , 36 , 37 , 44 , 45 ].
Most studies paired staff training and education with other implementation strategies to embed TIC throughout services. Several initiatives included activities to build buy-in and a shared rationale for implementing TIC within the organisation, including by developing position statements (e.g. [ 25 ]), aligning strategic planning with the TIC principles (e.g. [ 54 , 34 ]), conducting team building exercises (e.g. [ 44 , 45 ]), and establishing written agreements between participating agencies (e.g. [ 54 ]). Several initiatives chose to establish a team of staff responsible for implementation and monitoring [ 29 , 35 , 38 , 42 ] while others elected a single staff member to drive and oversee implementation (e.g. [ 27 ]). Other common implementation strategies included organising quality monitoring systems, including increasing the availability and/or routine use of screening for trauma-related needs [ 23 , 25 , 30 , 40 , 41 , 44 , 45 , 52 ], education outreach activities to other agencies [ 23 , 44 , 45 ], mandating change via policy and procedure change [ 32 , 33 , 36 , 39 , 40 , 42 , 54 , 34 ], and clinical team group debriefing and care planning after critical incidents [ 36 , 40 , 42 , 44 , 45 , 47 , 34 ].
Evaluation methods and quality appraisal
Most of the included studies examined barriers and facilitating factors for implementation of TIC using mixed-methods including staff interviews and/or focus groups, process data (e.g. uptake of screening tools and training attendance), and outcome data (e.g. rates of seclusion and restraint use). Eight studies reported across nine papers described author reflections on barriers and facilitating factors for implementation rather than reporting formal data [ 27 , 32 , 36 , 38 , 40 , 42 , 44 , 45 , 34 ]. This approach is subject to a high risk of bias, as assessed using the MMAT (see Supplementary Table S 4 for full methodological quality appraisal). The methodological quality of the other included studies was moderate, with most reporting clear research questions, well-justified data collection methods, and representative data collection from a diverse group of staff and/or service users. Common methodological limitations included that few of the studies reporting quantitative data considered the impact of confounding factors in their analysis, and the mixed-methods studies rarely attempted or described their approach to data integration. Importantly, none of the included studies explicitly compared implementation strategies to each other and so could not identify which were more effective than others.
Barriers and facilitating factors for implementation
Barriers and facilitating factors for implementing TIC across the included studies are described in Table 2 and mapped to the CFIR framework in Table 3 .
Intervention characteristics
Characteristics of the intervention (TIC) were reported to influence implementation across seven studies, always related to the perceived relevance of TIC to the setting and their target population. Three studies reported that staff did not perceive that the principles of TIC were suitable for their organisation or that their service users were too diverse to make delivery of TIC possible [ 23 , 27 , 29 ]. Four other studies reported that a high level of perceived relevance of TIC among staff was a facilitating factor for implementation in their sites [ 41 , 44 , 48 , 52 ].
Outer setting
Seven studies reported barriers and facilitating factors associated with the outer setting (that is, influences external to the organisation itself). One study noted that other services implementing TIC set a precedent and created a sense of peer pressure for the organisation to also pursue implementation [ 40 ]. A culture of interagency collaboration was noted as a facilitating factor in some studies, particularly where funding was allocated for administrative support to coordinate and monitor the collaboration [ 44 , 45 , 53 , 54 ]. Simonich et al. [ 53 ], Huntington et al. [ 44 ] and Mantler et al. [ 49 ] all noted that the implementation of TIC in other agencies servicing their clients was important to implementation success in their own organisation. That is, even where clients received TIC services from their organisation, this was undermined by other agencies delivering care that reduced client trust and sense of safety with healthcare providers. Outreach and training to other organisations was a facilitating factor for implementation in two of these studies [ 44 , 53 ]. Broader policy, funding arrangements, and regulation (external to the organisation) that was not consistent with the delivery of TIC was noted as a barrier to implementation in one study [ 48 ].
Inner setting
Factors related to the inner setting (the organisation or system in which implementation occurred) were reported as barriers or facilitating factors for implementation across 25 of the 27 studies. In many cases, this referred to the culture of the organisation and climate for implementation. Common facilitating factors included high levels of engagement and commitment from organisational leadership [ 23 , 25 , 32 , 36 , 40 , 42 , 44 , 45 , 54 , 34 ], the alignment of TIC with existing organisation strategic plans or policies [ 32 , 42 , 34 ], a culture of support for staff and evidence-based practice (including giving staff adequate time to learn and adopt new practices) [ 27 , 30 , 39 ], and allocation of adequate financial and staffing resources to promote implementation [ 23 , 27 , 40 , 54 ]. Where financial resources were not allocated to the initiative, or these were insufficient, this was a barrier to implementation [ 32 , 35 , 44 , 47 , 48 , 49 ]. One study also noted that although the provision of financial resources was a facilitating factor, the uneven distribution of these resources (favouring changes to the physical environment over investment in staff and human resources) was a barrier to change [ 27 ].
Other common barriers to implementation included competing priorities and staff time constraints [ 23 , 25 , 29 , 30 , 32 , 35 , 40 , 41 , 43 , 44 , 45 , 46 , 47 , 48 ], a lack of collaboration between teams within the organisation [ 27 ], and policies that were incompatible with delivering TIC. In particular, organisational policies that afforded limited flexibility to how staff delivered services and how service users engaged with the service were key barriers to implementation. Policy and procedure change that promoted flexibility in care protocols and offered service users more choice and control over their care were noted as facilitating factors across studies [ 33 , 37 , 39 , 42 , 44 , 45 , 48 , 49 ].
Characteristics of individuals
Characteristics of individuals were reported as barriers and facilitating factors for implementation in nine studies. In all cases, this focussed on staff resistance to change as a barrier [ 23 , 25 , 27 , 30 , 40 , 44 , 45 , 48 , 50 ] and staff openness as a facilitating factor for implementation success [ 27 , 29 , 50 ].
All but one of the included studies noted barriers and facilitating factors related to the process of implementation. Most studies identified design and delivery elements of their staff training program as promoting or limiting implementation success. For example, delivery of training to a variety of staff at all levels of the organisation, a flexible format that could be tailored according to needs, practical training elements (e.g. role plays), onsite delivery, ongoing trainings and availability of resources, (as opposed to a once-off session), embedding training into new employee orientation, and making training compulsory were identified as facilitating factors across several studies [ 25 , 29 , 30 , 46 , 47 , 48 , 50 , 51 , 52 , 53 ]. Provision of ongoing modelling, mentoring, and expert consultation promoted uptake and practice change [ 25 , 29 , 35 , 36 , 37 , 40 , 41 , 42 , 47 , 48 , 34 ]. Three studies noted that while staff knowledge and confidence in delivering TIC improved, these staff noted a lack of skills training and process changes to actually implement TIC within their organisation [ 33 , 35 , 48 ].
Several studies noted that including service users in implementation efforts promoted implementation success. Relevant strategies included involving a service user as a co-facilitator of training programs, service user inclusion in senior leadership positions and/or implementation teams, seeking regular service user feedback, and designing initiatives in collaboration with service users [ 36 , 40 , 44 , 50 , 51 , 34 ]. Huntington et al. [ 44 ] noted that resources and flexibility had to be embedded into the initiative to promote service user engagement (e.g. payment for involvement, prioritising service user schedules). In contrast, a lack of engagement of service users was noted as a barrier to implementation in one study [ 25 ].
Finally, several studies reported that establishing mechanisms to collect and regularly review data about the uptake and outcomes of the initiative was a key facilitating factor for change [ 30 , 36 , 40 , 42 , 34 ]. Others noted a lack of data collection and evaluation within their study as a barrier to implementation, particularly sustainability [ 25 , 38 , 54 ].
This systematic review sought to identify and synthesise evidence about barriers and facilitating factors for implementing TIC into healthcare settings. Given the very high community prevalence of psychological trauma exposure (up to 90% across the lifespan) [ 1 ], and the important impacts of trauma exposure when receiving healthcare [ 5 , 6 ], TIC aims to ensure that care services are safe, empowering, collaborative, and restore power to the care recipient [ 7 ]. Implementing TIC into healthcare settings usually requires change at the organisation level to ensure that all staff understand the impacts of psychological trauma, and that processes are in place to modify care behaviour to reduce the risk of re-traumatisation [ 10 , 39 ]. Like other complex interventions, adaptation of the TIC principles is required for implementation in each specific organisational context [ 56 ]. Identifying factors that influence implementation success across initiatives can help to inform the selection of implementation strategies and planning.
Results of this review demonstrate that factors related to the inner organisational setting and process of implementation are most often reported as influencers of TIC implementation success. Implementation was promoted where organisation leadership were highly engaged and committed to TIC and where sufficient resources were allocated to making change in practice. These facilitating factors are commonly reported as essential in efforts to implement innovation in healthcare [ 57 , 58 , 59 ], and staff who report having inadequate time for change (whether this is real or perceived) are less likely to implement innovation [ 58 ]. Strategies that build innovation into existing processes and procedures are most likely to be sustained and become the ‘normal’ thing to do [ 60 ]. For example, in a TIC initiative, this may mean building debriefing into existing case conferencing processes or adding screening items to existing procedures. Several studies included in this review noted that the addition of new processes on top of the existing workload was difficult to facilitate particularly where these processes did not fit into standard consultation times (e.g. 29).
Training staff about psychological trauma is also an essential step in the delivery of TIC particularly in health settings where mental health is not the primary focus of treatment [ 61 ]. The mental health literacy of the workforce in these settings can be low, especially where there are limited mental health clinicians on staff [ 6 , 10 , 11 ]. In our review, implementation strategies related to education and training were more comprehensive and multicomponent in non-mental health settings (e.g. primary care, maternal health) than in mental health settings where mental health literacy was high. Our review demonstrates that training efforts are more likely to lead to TIC implementation where they are targeted to staff across all levels of an organisation, with a flexible delivery format, and delivered on an ongoing basis rather than once-off. Training must also be compulsory, as voluntary trainings are unlikely to be well attended [ 50 , 51 ]. The ongoing availability of experts and mentors (also known as change agents ) was also an important facilitating factor across studies, consistent with evidence that regular, individualised follow-up is an integral component of success in quality improvement efforts [ 62 ]. This may be particularly important for TIC as service users may have complex needs as they contend with the physical, mental, and socio-economic sequelae of their experiences [ 7 ].
The process of implementing TIC is promoted where both staff and service users are engaged in both designing the implementation strategy and monitoring its ongoing progress. The value of engaging service users in the co-design of quality improvement initiatives is increasingly recognised and is mutually beneficial for both the service provider and the service user [ 63 ]. In the case of TIC, service users can provide nuanced insights about how services can be delivered flexibly and prioritise the needs and preferences of the care user [ 44 ]. Flexibility in organisational policy and procedure was a key facilitating factor for implementation across the included studies [ 33 , 37 , 39 , 42 , 44 , 45 , 48 , 49 ]. In addition, several studies included in this review described the value of infrastructure to collect and monitor data in initiatives to implement TIC. Data collection and monitoring facilitates ongoing review of resource allocation to strategies that are most effective and promotes staff engagement and buy-in [ 64 ].
Factors related to the characteristics of the intervention (TIC) and the individuals within the service generally focused on the sense of relevance of TIC for the service and service users, as well as staff openness to change. This is consistent with evidence that any intervention perceived by staff as not useful, not applicable to their clients, or not harmonious with their current practice is difficult to implement in practice [ 58 ]. Efforts to build ‘buy-in’ among staff are a crucial element of the knowledge-to-action pipeline [ 65 ]. Identifying and upskilling key opinion leaders and advocates for the intervention among the staff (including frontline staff who are well regarded among their peers), aligning the intervention with existing organisational policies and procedures, and creating incentives for use that are meaningful to the staff are key strategies to build staff buy-in [ 66 ]. Using participatory co-design methods together with staff to design implementation strategies can help to increase openness to change [ 67 ]. These were identified as facilitating factors in studies included in this review [ 32 , 42 , 34 ]. Failure to build staff buy-in can result in low staff morale and staff turnover [ 66 ]. Strategies should ensure that staff recognise the prevalence of trauma exposure among their clients and the impacts of these experiences when receiving care, and demonstrate how implementing TIC can support progress toward organisational goals (e.g. reducing responsive behaviour, need for seclusion and restraint, and staff and patient injury) [ 68 ].
Strengths and limitations
Key strengths of most of the identified studies included detailed information about the setting in which implementation occurred and examination of how these factors influenced implementation outcomes. The use of mixed-methods in 15 studies allowed an in-depth triangulation of data [ 27 , 29 , 30 , 35 , 36 , 38 , 39 , 41 , 42 , 43 , 46 , 52 , 53 , 54 , 34 ]. However, limitations included that most of the included studies were case studies describing a discrete implementation site or region, without a control condition. This limits comparability. In addition, eight studies reported the reflections of the authors, rather than the collection and analysis of empirical data [ 27 , 32 , 36 , 38 , 40 , 42 , 44 , 45 , 34 ]. The results of these studies should therefore be interpreted with caution. None of the included studies explicitly compared the effectiveness of different implementation strategies to each other, and this would be helpful in future work to guide strategy selection and design. Finally, very few studies included a critical analysis of the author’s own role in the implementation and presentation of results. Given that authors were commonly actively involved in implementation, their underlying assumptions, beliefs and experiences are likely to have influenced data collection, analysis and reporting. Future efforts to reduce bias might include the use of external evaluation teams or the inclusion of reflexivity statements in analysis and reporting [ 69 ].
Strengths of this review include our broad search strategy that captured initiatives to implement TIC across countries and healthcare settings. Our synthesis generated common themes across diverse initiatives and mapped them to an existing framework to maximise interpretability. Limitations of this review include that we excluded any papers not published in English and this may limit the generalisability of the results. The lack of an operational definition of TIC and the breadth of interventions delivered at the system or organisation level in the included studies may also limit comparability and the conclusions that can be drawn from the results. However, core elements of the implementation strategies were common across studies (e.g. staff training, routine screening) promoting comparability. Future reviews may be helpful for synthesising common implementation strategies used for TIC in more depth. Our coding and mapping to the CFIR framework may have been influenced by subjectivity, though our use of multiple coders and multiple rounds of coding reduces this risk. In addition, we did not assess the relative strength of each influencing factor. That is, factors that were reported less often across studies may nonetheless have a more powerful influence on implementation. The exclusion of an evaluation of relative strength of the influencing factors was primarily determined by few of the included studies providing such an analysis. Future studies that examine the strength of influence of each factor on implementation outcomes will be helpful for filling this research gap.
There have been recent calls to implement TIC as a universal model of care across healthcare [ 68 ], aged care [ 6 ], and social care services [ 9 ] in recognition of the major impacts of trauma exposure in the receipt of care and the potential harm to care recipients and providers that can result from inappropriate care. However, implementing TIC usually requires a complex organisational change process including both staff behaviour change and organisational policy and procedure change to facilitate staff change [ 10 ]. This review identifies key factors that should be targeted to promote TIC implementation, including interagency collaboration, staff and leadership buy-in, aligning implementation strategies with existing policies and procedures, allocation of adequate human and financial resources, flexibility in organisational policies and procedures, ongoing and tailored training, participatory co-design, and the collection and monitoring of data. Continued research will be helpful for characterising what TIC looks like when it is delivered well, and providing validated frameworks to promote organisational uptake for the benefit of trauma survivors.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Reynolds K, Pietrzak RH, Mackenzie CS, Chou KL, Sareen J. Post-traumatic stress disorder across the adult lifespan: findings from a nationally representative survey. Am J Geriatr Psychiatry. 2016;24(1):81–93.
Article PubMed Google Scholar
Center for Substance Abuse Treatment. A treatment protocol for trauma-informed care in behavioral health services. United States: US Department of Health and Human Services; 2014.
Google Scholar
Bolton D, Hill J, O’Ryan D, Udwin O, Boyle S, Yule W. Long-term effects of psychological trauma on psychosocial functioning. J Child Psychol Psychiatry. 2004;45(5):1007–14.
Park S, Hong JP, Jeon HJ, Seong S, Cho MJ. Childhood exposure to psychological trauma and the risk of suicide attempts: the modulating effect of psychiatric disorders. Psychiatry Investig. 2015;12(2):171.
Hamberger LK, Barry C, Franco Z. Implementing trauma-informed care in primary medical settings: evidence-based rationale and approaches. J Aggress Maltreatment Trauma. 2019;28(4):425–44.
Article Google Scholar
Cations M, Laver KE, Walker R, Smyth A, Fernandez E, Corlis M. The case for trauma-informed aged care. Int J Geriatr Psychiatry. 2020;35(5):425–9.
Muskett C. Trauma-informed care in inpatient mental health settings: A review of the literature. Int J Ment Health Nurs. 2014;23(1):51–9.
Harris M, Fallot RD. Envisioning a trauma-informed service system: a vital paradigm shift. New Dir Ment Health Serv. 2001;2001(89):3–22.
Elliott DE, Bjelajac P, Fallot RD, Markoff LS, Reed BG. Trauma-informed or trauma-denied: Principles and implementation of trauma-informed services for women. J Community Psychol. 2005;33(4):461–77.
Quadara A. Implementing trauma-informed systems of care in health settings: The WITH study. Melbourne: ANROWS; 2015.
Cations M, Laver K, Couzner L, Flatman S, Bierer P, Ames C, et al. Trauma-informed care in geriatric inpatient units to improve staff skills and reduce patient distress: a co-designed study protocol. BMC Geriatr. 2021;21(1):492.
Article PubMed PubMed Central Google Scholar
SAMHSA’s Trauma and Justice Strategic Initiative. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
Mental Health Coordinating Council. Trauma-informed care and practice: Towards a cultural shift in policy reform across mental health and human services in Australia – a national strategic direction. Position paper and recommendations of the National Trauma-Informed Care and Practice Advisory Working Group. New South Wales; 2013. Retrieved 10 October 2022 from https://www.mhcc.org.au/wp-content/uploads/2018/05/nticp_strategic_direction_journal_article__vf4_-_jan_2014_.pdf .
Lane-Fall MB, Curran GM, Beidas RS. Scoping implementation science for the beginner: locating yourself on the “subway line” of translational research. BMC Med Res Methodol. 2019;19(1):133.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Berliner L, Kolko DJ. Trauma informed care: A commentary and critique. Child Maltreat. 2016;21(2):168–72.
Bendall S, Eastwood O, Cox G, Farrelly-Rosch A, Nicoll H, Peters W, et al. A systematic review and synthesis of trauma-informed care within outpatient and counseling health settings for young people. Child Maltreat. 2021;26(3):313–24.
Cochrane Effective Practice and Organisation of Care Review Group (EPOC). Data Collection Checklist. Ottawa, Canada: Cochrane Effective Practice and Organisation of Care Group. 2002. Available from: https://methods.cochrane.org/sites/methods.cochrane.org.bias/files/public/uploads/EPOC%20Data%20Collection%20Checklist.pdf .
Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract. 2018;24(3):459–67.
McArthur C, Bai Y, Hewston P, Giangregorio L, Straus S, Papaioannou A. Barriers and facilitators to implementing evidence-based guidelines in long-term care: a qualitative evidence synthesis. Implement Sci. 2021;16(1):1–25.
Means AR, Kemp CG, Gwayi-Chore MC, Gimbel S, Soi C, Sherr K, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implement Sci. 2020;15(1):17.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75.
Beidas RS, Adams DR, Kratz HE, Jackson K, Berkowitz S, Zinny A, et al. Lessons learned while building a trauma-informed public behavioral health system in the City of Philadelphia. Eval Program Plann. 2016;59:21–32.
Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework. Implement Sci. 2019;14(1):1–16.
Amaro H, McGraw S, Larson MJ, Lopez L, Nieves R, Marshall B. Boston consortium of services for families in recovery: a trauma-informed intervention model for women’s alcohol and drug addiction treatment. Alcohol Treat Q. 2005;22(3–4):95–119.
Konrad EL. A multidimensional framework for conceptualizing human services integration initiatives. New Dir Eval. 1996;1996(69):5–19.
Dorr K. An evidence based evaluation of patient outcomes after the implementation of a new model of care for adolescent inpatient psychiatry [PhD Thesis]. Harrisonburg: James Madison University; 2019.
Chen HT. Applying mixed methods under the framework of theory-driven evaluations. New Dir Eval. 1997;1997(74):61–72.
Purbeck CA, Briggs EC, Tunno AM, Richardson LM, Pynoos RS, Fairbank JA. Trauma-informed measurement-based care for children: Implementation in diverse treatment settings. Psychol Serv. 2020;17(3):311.
Sala-Hamrick KJ, Isakson B, De Gonzalez SDC, Cooper A, Buchan J, Aceves J, et al. Trauma-informed pediatric primary care: Facilitators and challenges to the implementation process. J Behav Health Serv Res. 2021;48(3):363–81.
Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf. 2013;23(4):290–8.
Loomis B, Epstein K, Dauria EF, Dolce L. Implementing a Trauma-Informed Public Health System in San Francisco. California Health Educ Behav. 2019;46(2):251–9.
Korchmaros JD, Greene A, Murphy S. Implementing trauma-informed research-supported treatment: fidelity, feasibility, and acceptability. Child Adolesc Soc Work J. 2021;38(1):101–13.
Azeem MW, Reddy B, Wudarsky M, Carabetta L, Gregory F, Sarofin M. Restraint reduction at a pediatric psychiatric hospital: A ten‐year journey. J Child Adolesc Psychiatr Nurs. 2015;28(4):180–4.
Bartlett JD, Barto B, Griffin JL, Fraser JG, Hodgdon H, Bodian R. Trauma-informed care in the Massachusetts child trauma project. Child Maltreat. 2016;21(2):101–12.
Caldwell B, Albert C, Azeem MW, Beck S, Cocoros D, Cocoros T, et al. Successful seclusion and restraint prevention effort in child and adolescent programs. J Psychosoc Nurs Ment Health Serv. 2014;52(11):30–8.
Chandler G. From traditional inpatient to trauma-informed treatment: Transferring control from staff to patient. J Am Psychiatr Nurses Assoc. 2008;14(5):363–71.
Conover K, Sharp C, Salerno A. Integrating trauma-informed care principles in behavioral health service organizations. Psychiatr Serv. 2015;66(9):1004–1004.
Damian AJ, Gallo J, Leaf P, Mendelson T. Organizational and provider level factors in implementation of trauma-informed care after a city-wide training: an explanatory mixed methods assessment. BMC Health Serv Res. 2017;17(1):1–10.
Dike CC, Lamb-Pagone J, Howe D, Beavers P, Bugella BA, Hillbrand M. Implementing a program to reduce restraint and seclusion utilization in a public-sector hospital: Clinical innovations, preliminary findings, and lessons learned. Psychol Serv. 2020;18:663–70.
Dueweke AR, Hanson RF, Wallis E, Fanguy E, Newman C. Training pediatric primary care residents in trauma-informed care: A feasibility trial. Clin Pediatr (Phila). 2019;58(11–12):1239–49.
Hale R, Wendler MC. Evidence-based practice: Implementing trauma-informed care of children and adolescents in the inpatient psychiatric setting. J Am Psychiatr Nurses Assoc. 2020;29(2):161–70.
Hall A, McKenna B, Dearie V, Maguire T, Charleston R, Furness T. Educating emergency department nurses about trauma informed care for people presenting with mental health crisis: A pilot study. BMC Nurs. 2016;15(1):1–8.
Huntington N, Moses DJ, Veysey BM. Developing and implementing a comprehensive approach to serving women with co-occurring disorders and histories of trauma. J Community Psychol. 2005;33(4):395–410.
Moses DJ, Reed BG, Mazelis R, D’Ambrosio B. Creating trauma services for women with co-occurring disorders. Subst Abuse Ment Health Serv Adm. 2003;1(01):1–53.
Jee SH, Conn AM, Milne-Wenderlich A, Krafft C, Chen M, Steen M, et al. Providing trauma-informed pediatric care for underserved populations: Reflections on a teaching intervention. Dev Child Welf. 2020;2(1):21–36.
Koury SP, Green SA. Developing trauma-informed care champions: A six-month learning collaborative training model. Adv Soc Work. 2017;18(1):145–66.
Levine S, Varcoe C, Browne AJ. “We went as a team closer to the truth”: impacts of interprofessional education on trauma-and violence-informed care for staff in primary care settings. J Interprof Care. 2021;35(1):46–54.
Mantler T, Wolfe B. Evaluation of trauma-informed integrated health models of care for women: a qualitative case study approach. Partn Abuse. 2018;9(2):118–36.
McEvedy S, Maguire T, Furness T, McKenna B. Sensory modulation and trauma-informed-care knowledge transfer and translation in mental health services in Victoria: Evaluation of a statewide train-the-trainer intervention. Nurse Educ Pract. 2017;25:36–42.
McNamara M, Cane R, Hoffman Y, Reese C, Schwartz A, Stolbach B. Training hospital personnel in trauma-informed care: assessing an interprofessional workshop with patients as teachers. Acad Pediatr. 2021;21(1):158–64.
Palfrey N, Reay RE, Aplin V, Cubis JC, McAndrew V, Riordan DM, et al. Achieving service change through the implementation of a trauma-informed care training program within a mental health service. Community Ment Health J. 2019;55(3):467–75.
Simonich HK, Wonderlich SA, Erickson AL, Myers TC, Hoesel J, Wagner S, et al. A statewide trauma-focused cognitive behavioral therapy network: Creating an integrated community response system. J Contemp Psychother. 2015;45(4):265–74.
Tuck SG, Summers AC, Bowie J, Fife-Stallworth D, Alston C, Hayes S, et al. B’More Fit for Healthy Babies: using trauma-informed care policies to improve maternal health in Baltimore city. Womens Health Issues. 2017;27:S38–45.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;30(374):n2061.
Willis CD, Saul J, Bevan H, Scheirer MA, Best A, Greenhalgh T, et al. Sustaining organizational culture change in health systems. J Health Organ Manag. 2016;30(1):2–30.
Correa VC, Lugo-Agudelo LH, Aguirre-Acevedo DC, Contreras JAP, Borrero AMP, Patiño-Lugo DF, et al. Individual, health system, and contextual barriers and facilitators for the implementation of clinical practice guidelines: a systematic metareview. Health Res Policy Syst. 2020;18(1):74.
Karrer M, Hirt J, Zeller A, Saxer S. What hinders and facilitates the implementation of nurse-led interventions in dementia care? A scoping review BMC Geriatr. 2020;20(1):1–13.
Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med. 2010;8(1):63.
Menschner C, Maul A. Key ingredients for successful trauma-informed care implementation. Incorporated Trenton: Center for Health Care Strategies; 2016.
Alagoz E, Chih MY, Hitchcock M, Brown R, Quanbeck A. The use of external change agents to promote quality improvement and organizational change in healthcare organizations: a systematic review. BMC Health Serv Res. 2018;18(1):42.
Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient-Patient-Centered Outcomes Res. 2014;7(4):387–95.
Berkel C, Gallo CG, Sandler IN, Mauricio AM, Smith JD, Brown CH. Redesigning Implementation Measurement for Monitoring and Quality Improvement in Community Delivery Settings. J Prim Prev. 2019;40(1):111–27.
Chaudoir SR, Dugan AG, Barr CH. Measuring factors affecting implementation of health innovations: a systematic review of structural, organizational, provider, patient, and innovation level measures. Implement Sci. 2013;8(1):22.
Meyers DC, Durlak JA, Wandersman A. The Quality implementation framework: a synthesis of critical steps in the implementation process. Am J Community Psychol. 2012;50(3):462–80.
Augustsson H, Richter A, Hasson H, von Thiele SU. The need for dual openness to change: a longitudinal study evaluating the impact of employees’ openness to organizational change content and process on intervention outcomes. J Appl Behav Sci. 2017;53(3):349–68.
Racine N, Killam T, Madigan S. Trauma-Informed care as a universal precaution: beyond the adverse childhood experiences questionnaire. JAMA Pediatr. 2020;174(1):5–6.
Reid AM, Brown JM, Smith JM, Cope AC, Jamieson S. Ethical dilemmas and reflexivity in qualitative research. Perspect Med Educ. 2018;7(2):69–75.
Download references
Acknowledgements
The authors would like to acknowledge the contribution of Dr Bethany Wilton-Harding to screening and data extraction for this review.
This study is funded by the South Australian Hospital Research Foundation and the Australian Government Medical Research Future Fund. MC is supported by an Early Career Fellowship from the South Australian Hospital Research Foundation and a National Health and Medical Research Council Medical Research Future Fund Emerging Leadership Investigator Grant. KEL is supported by an Australian Research Council Discovery Early Career Researcher Award. ND is supported by a NHMRC Boosting Dementia Research Leadership Fellowship.
Author information
Authors and affiliations.
College of Education, Psychology and Social Work, Flinders University, Adelaide, SA, Australia
Yan Huo, Leah Couzner, Tim Windsor & Monica Cations
College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia
UQ Centre for Clinical Research, Faculty of Medicine, University of Queensland, Brisbane, QLD, Australia
Nadeeka N. Dissanayaka
School of Psychology, The University of Queensland, Brisbane, QLD, Australia
Department of Neurology, Royal Brisbane and Woman’s Hospital, Brisbane, QLD, Australia
You can also search for this author in PubMed Google Scholar
Contributions
YH screened all titles, abstracts and full-text articles, performed data extraction and analysis and assessed the validity, robustness and applicability of each included study. LC resolved disagreements regarding the inclusion of studies, performed data extraction and contributed to drafting the manuscript. TW, KL and ND contributed to the planning and concept and editing of the review. MC initiated the concept of the review, undertook analysis and was responsible for drafting the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Monica Cations .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. .
PRISMA Checklist; Search strategy; PRISMA diagram; Results of quality appraisal; Mixed-methods appraisal tool questions. The tile contains tables that provide additional information about the systematic review process. This includes the search strategy, PRISMA checklist and diagram, and tables pertaining to the quality appraisal undertaken.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Huo, Y., Couzner, L., Windsor, T. et al. Barriers and enablers for the implementation of trauma-informed care in healthcare settings: a systematic review. Implement Sci Commun 4 , 49 (2023). https://doi.org/10.1186/s43058-023-00428-0
Download citation
Received : 24 October 2022
Accepted : 05 April 2023
Published : 05 May 2023
DOI : https://doi.org/10.1186/s43058-023-00428-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Trauma-informed care
- Health services
- Psychological trauma
- Posttraumatic stress disorder
- Care quality and safety
Implementation Science Communications
ISSN: 2662-2211
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 14 September 2022
Trauma-informed care in the UK: where are we? A qualitative study of health policies and professional perspectives
- Elizabeth Emsley 1 ,
- Joshua Smith 1 ,
- David Martin 2 &
- Natalia V. Lewis 3
BMC Health Services Research volume 22 , Article number: 1164 ( 2022 ) Cite this article
10k Accesses
7 Citations
15 Altmetric
Metrics details
Trauma-informed (TI) approach is a framework for a system change intervention that transforms the organizational culture and practices to address the high prevalence and impact of trauma on patients and healthcare professionals, and prevents re-traumatization in healthcare services. Review of TI approaches in primary and community mental healthcare identified limited evidence for its effectiveness in the UK, however it is endorsed in various policies. This study aimed to investigate the UK-specific context through exploring how TI approaches are represented in health policies, and how they are understood and implemented by policy makers and healthcare professionals.
A qualitative study comprising of a document analysis of UK health policies followed by semi-structured interviews with key informants with direct experience of developing and implementing TI approaches. We used the Ready Extract Analyse Distil (READ) approach to guide policy document review, and the framework method to analyse data.
We analysed 24 documents and interviewed 11 professionals from healthcare organizations and local authorities. TI approach was included in national, regional and local policies, however, there was no UK- or NHS-wide strategy or legislation, nor funding commitment. Although documents and interviews provided differing interpretations of TI care, they were aligned in describing the integration of TI principles at the system level, contextual tailoring to each organization, and addressing varied challenges within health systems. TI care in the UK has had piecemeal implementation, with a nation-wide strategy and leadership visible in Scotland and Wales and more disjointed implementation in England. Professionals wanted enhanced coordination between organizations and regions. We identified factors affecting implementation of TI approaches at the level of organization (leadership, service user involvement, organizational culture, resource allocation, competing priorities) and wider context (government support, funding). Professionals had conflicting views on the future of TI approaches, however all agreed that government backing is essential for implementing policies into practice.
Conclusions
A coordinated, more centralized strategy and provision for TI healthcare, increased funding for evaluation, and education through professional networks about evidence-based TI health systems can contribute towards evidence-informed policies and implementation of TI approaches in the UK.
Peer Review reports
Individual, interpersonal and collective trauma is a highly prevalent and costly public health problem [ 1 ]. The WHO World Mental Health Survey identified that 70% of participants had experienced lifetime traumas, including physical violence, intimate partner sexual violence, and trauma related to war [ 2 ]. People experiencing socio-economic disadvantage, women, minoritized ethnic groups, and the LGBTQ + community are disproportionally affected by violence and trauma [ 3 , 4 ]. Adverse childhood experiences (ACEs) are stressful or traumatic events that occur during childhood or adolescence [ 5 ]. In England, a household survey found that nearly half of adults had experienced at least one ACE, including childhood sexual, physical or verbal abuse, as well as household domestic violence and abuse (DVA) [ 6 ]. DVA is considered to be a chronic and cumulative cause of complex trauma [ 7 ]. Up to 29% women and 13% men have experienced DVA in their lifetime, at a cost of £14 billion a year to the UK economy [ 7 , 8 , 9 ].
Cumulative trauma across the lifespan is associated with multiple health consequences [ 10 ]. The links between cumulative adversity from ACEs, DVA and other traumatic experiences are explained within the ecobiodevelopmental framework and the concept of toxic stress [ 11 ]. In a systematic review and meta-analysis of 37 observational studies of health behaviours and adult disease, patients with four or more ACEs were at higher risk of a range of poorer health outcomes including cardiovascular disease and mental ill health, versus those with no ACEs history [ 12 ]. Individuals and families who have experienced violence and trauma seek support from healthcare and other services for the physical, psychological and socioeconomic consequences of trauma [ 1 , 13 ]. In the household survey in England and Wales, adults who had experienced four ACEs were twice as likely to attend their general practice repeatedly, compared with those with no ACEs history, and incidence of health service use rose as the ACEs experiences increased [ 14 ]. In a systematic review 47% of patients in mental health services had experienced physical abuse and 37% had experienced sexual abuse [ 15 ].
If the high prevalence and negative impacts of trauma are not recognised and addressed in healthcare services, there may be negative consequences for patients and healthcare professionals. Patients may not disclose trauma or recognise the impact of trauma on their health [ 16 ]. Patients may also be at risk of re-triggering and re-traumatization, for example by the removal of choice regarding treatment, judgemental responses following a disclosure of abuse, seclusion and restraint [ 17 , 18 , 19 ]. Re-traumatization within health services can affect both patients and members of staff, with the latter experiencing vicarious trauma [ 20 ]. The resulting chronic stress may impact on staff members’ ability to empathise and support others [ 21 ]. Many healthcare staff themselves have lived experience of trauma. A recent systematic review of healthcare professionals’ own experience of DVA, reported a pooled lifetime prevalence of 31.3% (95% CI [24.7%, 38.7%] [ 22 ].
Over last 20 years, several frameworks for a trauma-informed (TI) approach at the health systems level have been developed [ 13 , 17 , 23 , 24 , 25 , 26 , 27 , 28 ]. These frameworks aim to prevent re-traumatization in healthcare services and mitigate the high prevalence and negative effects of violence and trauma on patients and healthcare professionals. A TI approach (synonyms TI care, TI service system) starts from the assumption that every patient and healthcare professional could potentially have been affected by trauma [ 13 ]. By realising and recognising these experiences and their impacts, we can respond by providing services in a trauma-informed way to improve healthcare experience and outcomes for both patients and staff. The process of becoming a TI system is guided by key principles of safety, trust, peer support, collaboration, empowerment and cultural sensitivity [ 13 ]. The most cited frameworks for a system-level TI approach are those by Harris and Fallot [ 29 ], and the US Substance Abuse and Mental Health Services Administration (SAMHSA) [ 13 ]. These frameworks highlight that it is necessary to, firstly, change organizational culture and environments (organizational domain) and then change clinical practices (clinical domain) by incorporating the four TI assumptions and six TI principles throughout the ten implementation domains within a health system [ 13 ] . Other authors proposed similar constructs for the framework of TI approach, often using slightly differing terminology [ 29 , 30 ]. The authors consistently highlighted that the framework of TI approach is not a protocol but rather high-level guidance applicable to any human service system and should be tailored to the organizational and wider contexts. The process of becoming a TI system is described as a transformation journey rather than a one-off activity.
Despite a 20-year history of the TI approach framework, several reviews have found limited evidence for their effectiveness in health systems, with most studies conducted in North America and only one qualitative study in the UK [ 31 , 32 , 33 ]. Despite little evidence of acceptability, effectiveness, and cost effectiveness in the UK context, policies and guidelines at national, regional and organisational levels recommend implementing TI approaches in healthcare organisations and systems. It is important to understand how TI approaches are being introduced into policy documents, and how these policies are being interpreted and applied within UK healthcare. This study aims to understand the UK-specific context for implementing a TI approach in healthcare by exploring:
How are TI approaches represented in UK health policies?
How are TI approaches understood by policy makers and healthcare professionals?
How are TI approaches implemented in the UK?
This study of UK policy and practice will help us understand what TI approaches mean for policy makers and professionals to inform future UK-specific policy and TI approaches in healthcare.
To answer our research questions, and consider perspectives from different standpoints, we conducted a multi-method qualitative study comprised of a document analysis of UK health policies followed by semi-structured interviews with key informants. Document analysis explored how TI approaches are represented in UK health policy while interviews explored professional views on how they are understood and implemented. We used the Ready Extract Analyse Distil (READ) approach [ 34 ], to guide the review of health policies and the framework method [ 35 ], to analyse data. The framework method is suitable for applied health research conducted by multi-disciplinary teams with varied experiences of qualitative analysis.
Data collection
Data collection occurred between October 2020 and June 2021, with researchers and interviewees based in remote settings due to social distancing restrictions during the COVID-19 pandemic. Sample size was informed by the concept of information power [ 36 ], and restricted by the available funding and a tight timeline.

Document search
We defined policy as ‘a statement of the government’s position, intent or action’ [ 37 ], and considered this definition at the level of a nation, local authority or organization. Two researchers (EE, NVL) identified key policy and related contextual documents, which provided background information on TI approaches. We identified documents through: (i) searches for peer reviewed and grey literature in our earlier systematic review on TI primary care and community mental healthcare [ 31 ], (ii) snowballing of references from included documents, (iii) signposting by interview participants and experts in the field of TI care. Researchers retrieved documents meeting the inclusion criteria: adult healthcare, UK-focus and discussion of TI approaches. We excluded documents on child healthcare, trauma-specific interventions and non-UK focus.
Qualitative interviews
We conducted virtual semi-structured interviews with professionals at decision making levels who have direct experience of developing and implementing TI approaches in the UK healthcare system. We agreed to recruit up to 10 professionals from national and local governments and healthcare organisations. Researchers sent an expression of interest letter via email and Twitter to: (i) individuals and professional networks of policy makers, (ii) authors of included policy documents, (iii) individuals recommended by interview participants. Interested individuals contacted study researchers who checked their eligibility, sent participant information leaflets, answered questions, and arranged interviews with those eligible and willing to proceed. Interviews were conducted over the Zoom video call platform. Researchers obtained verbal informed consent, asked demographic questions, and followed a flexible topic guide to ensure primary issues were covered during all interviews but allowing participants to introduce unanticipated issues. The topic guide explored participant experiences of developing and implementing TI approaches and their views on how TI approaches have come to be represented in policy and implementation (Additional file 1 ). The interviews were audio-recorded with consent, professionally transcribed verbatim, and anonymised.
Data analysis started alongside data collection, to help refine and guide further data collection [ 35 ]. We followed the four-step READ approach to document review in health policy research: 1) ‘Ready your materials’ which involves agreeing the type and quantity of documents to analyse, 2) ‘Extract data’ whereby key document information such as basic data and concepts are organized, 3)’Analyse data’ when data is interpreted and findings are developed, 4) ‘Distil your findings’ which involves assessing whether there is sufficient data to answer the research question and findings are refined into a narrative [ 34 ].
In step one, two researchers (EE, NVL) agreed to use purposive sampling to gather 24 documents representing a broad range of document categories including primary legislation, parliamentary documents, NHS and Public Health England strategy and planning documents, service-user perspectives, evaluation reports, and guidance on ‘how to do’ TI approach [ 38 ]. EE ordered included documents chronologically. In step two, EE read and re-read all included documents and used a customized Excel form to extract data on document title, authors, year, source, objectives, target audience, focus, key messages, referenced evidence, policies/guidelines, and recommendations. During data extraction, researchers made notes about how each document answered the following questions: What is TI care? TI care for whom? Why TI care? EE and NVL met regularly to discuss preliminary ideas for analysis.
In step three, we imported all included documents and interview transcripts into NVivo R project and applied the framework method [ 35 ]. To address variability in definitions and terminology regarding TI approaches, we included key concepts from the well-known SAMHSA system-level framework [ 13 ], as a basis for our coding frame, for example the six TI principles. First, all researchers read four documents and two interview transcripts and independently manually coded text relevant to our research questions using a combination of inductive and deductive coding [ 39 ]. Deductive coding helped to identify concepts related to TI care, even if the document itself did not specifically use the “trauma-informed” term. The researchers then met to compare initial thematic codes and agree on a ‘working analytical framework’ which was imported into NVivo and applied to the documents and interviews transcripts. We refined the framework by adding and merging thematic codes identified subsequently, ran matrix coding queries by data sub-sets (documents, interviews), and combined codes into final analytical themes that answered our research questions. During the analysis stage, researchers met bi-weekly to finalise the dataset, develop and refine coding frame and themes. We wrote reflective diaries and analytical notes and discussed how our clinical backgrounds in general practice and psychiatry, and varied experiences of qualitative research, could have influenced the analysis.
In step four, we stopped document review when we reached the pre-specified number of documents and discussed common findings. First, we illustrated how TI approaches have developed in the UK over time by creating an integrated timeline with document publication dates, the years when interview participants began working in this area, and broader contextual factors from national news and related media. Then we integrated findings from the analysis of documents and interviews through three iterative cycles of developing final analytical themes cutting across documents and interviews. Researchers produced written accounts of the themes, and tables with illustrative quotes that explained how TI approaches have been represented in policy documents, understood, and implemented in the UK.
Policy documents
We identified 50 documents and selected 24 policy documents at national, local, and organizational levels. The remaining 26 documents provided context and a background on TI approaches. The documents included were published over nine years (2012–2021) and considered all UK nations, multiple sectors, government policy and service-user voices. The documents either mentioned a TI approach or discussed related concepts such as a patient choice and safety of services (Table 1 ).
Mirroring the historical development of TI approaches from mental health services [ 13 , 29 ], across both documents and interviews, mental health was the most referenced sector ( n = 24), followed by women’s health ( n = 11), healthcare for rough-sleepers ( n = 7), primary care ( n = 4) and major incident management ( n = 1). The level of application of the TI approach varied from one organization [ 55 ], to a public health board [ 59 ], to NHS-wide [ 48 , 50 ]. The geographic coverage of policy documents ranged from UK wide ( n = 10) to regional application ( n = 24). Scotland emerged as a leading region with the TI knowledge and skills framework for the Scottish Workforce [ 25 ].
The timeline of TI approaches and related concepts in the UK showed a steady growth between 2012 and 2021 with parallel developments from top-down and bottom-up (Fig. 1 ).
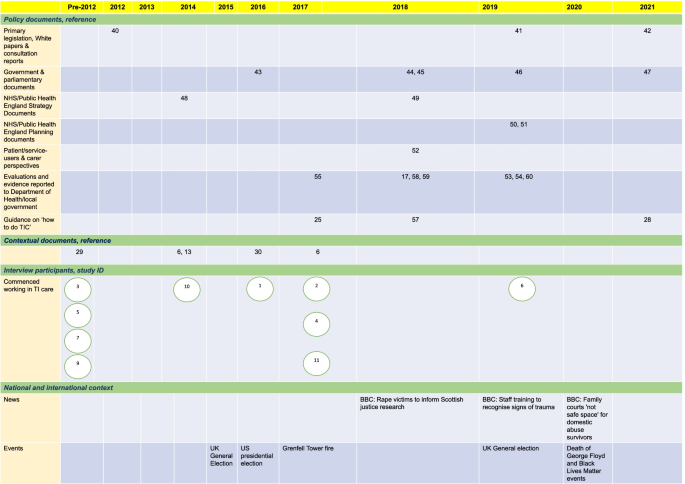
An integrated timeline of how TI approaches have developed in the UK. Document publication dates, the years when interview participants began working in this area, and broader contextual factors from national news and related media are captured. The number/s in each cell correspond to a document reference [ 6 , 13 , 17 , 25 , 28 , 29 , 30 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 59 , 60 ]
We identified few documents prior to 2012, with the Health and Social Care Act published in 2012. Although the Act did not specifically use the term TI care, it discussed related concepts of a greater voice for patients, enabling patient choice and safety of services. We found a noticeable clustering of documents in 2018 and 2019. Potential contributions could be the release of key contextual documents such as the US SAMHSA guidance and the National ACEs Study in the preceding years [ 13 , 14 ]. Other possible reasons could be the high-profile MeToo and Black Lives Matter movements and tragedies like Grenfell fire. Relevant news articles, including calls for rape victim support and professional training on trauma, came to the fore in 2018–2021. These events and activities have brought the issues of trauma, vulnerable populations, intersectionality, and racial justice to the foreground and may have helped achieve a focus on TI approaches as a responsive system-level framework.
In total, 21 professionals expressed interest, 2 did not have direct experience of TI approach at the system level, 8 did not respond by the deadline, 11 provided consent and were interviewed. Interviews lasted between 32 and 68 min (mean 52 min). We achieved a maximum variation sample representing diversity of gender (4 men, 7 women), organizations (public, private, third sector), professional role (frontline to leadership positions), and direct experience of developing and/or implementing TI approaches in healthcare (from 2 to 25 years). Most participants developed and implemented TI approaches in England, at the level of organizations and local authorities (Table 2 ).
Three out of ten interview participants had been involved in developing and implementing TI approaches prior to the release of the first document in 2012, with the rest becoming involved in 2017, just prior to the clustering of documents in 2018 and 2019 indicating a pivotal wave of popularity of the TI approach framework at this time. Participants explained that their clinical practice facilitated interest in the topic.
Our framework analysis has produced three analytical themes with seven sub-themes:
How TI approaches are represented in UK health policies
How ti approaches are understood, ti care as different from other practices, ti care as a contextually tailored organizational approach.
TI care as a remedy to challenges;
How TI approaches are implemented
Piecemeal implementation and a need for a shared vision, factors that facilitated or hindered implementation, the evidence-policy gap, the future of ti care in the uk.
We found that the TI approach is referenced in government initiatives and included in policies at a national level, as well as in NHS and non-NHS organizations, local authorities, and devolved nations; however, there was no dedicated strategy or a position statement, nor was there an agreed terminology and framework, or a robust evidence base in the UK. Despite growing endorsement of TI approaches in policy documents (Fig. 1 ), positive statements at the national and NHS level were not backed up with legislation, guidance, funding commitment, and resource allocation.
We found divergent interpretations of a TI approach versus other concepts related to trauma, such as ACEs, psychologically informed environments and standard good clinical practice. One participant unified concepts such as TI care, ACEs and psychologically informed environments in recognising past traumatic experiences. Another participant detached the terms ACEs and TI care, reflecting that ACEs have become well known in research whereas a TI approach is a pragmatic way of supporting those who have experienced trauma. All documents and most participants clearly differentiated between a TI approach at the system level and standalone TI practices (e.g., routine enquiry about ACEs, one-off training about trauma). However, some participants considered standalone TI practices to be a TI approach. Documents and most interviewees differentiated TI approach from a good clinical practice by incorporation of the TI assumptions and principles [ 25 ].
In line with the SAMHSA guidance [ 13 ], document and interview data showed that the framework of a TI approach needs to be tailored to the organizational and wider context. Policy documents advised organizations to clarify what TI care means for them, and that application of the framework should depend on the needs of service users and organisations [ 25 , 28 , 52 , 54 , 59 , 60 ]. Several documents suggested that this organizational tailoring should be informed by service-users through co-production and co-design of services [ 17 , 28 , 49 , 52 , 53 , 54 , 55 , 60 , 61 ].
TI care as a remedy to challenges
In all policy documents and in nine interviews, TI approaches were presented as a remedy to a variety of problems within health systems. Sixteen of twenty-five documents justified a TI approach as a way for addressing the high prevalence and negative impact of violence and trauma on patients, with eleven documents considering its impact on staff. The growing international evidence base for the impact of psychological trauma and the need for service response was used in documents and interviews to justify TI approaches as a pragmatic solution to these concerns. However, the documents and interview participants justified the need for TI care by citing US and Welsh epidemiological studies on ACEs, DVA and patient accounts of being re-traumatized in services. We found no references to intervention studies that demonstrated effectiveness, cost-effectiveness, or acceptability of TI approaches in the UK.
In the NHS Long Term Plan, TI care was also identified as a component of a new model of integrated care [ 50 ]. A TI approach has also been presented as a solution to addressing the collective trauma of the COVID-19 pandemic for patients and staff [ 62 ].
Interviewees confirmed the piecemeal implementation of TI approaches in the UK and felt that a shared national vision would be beneficial. Participants agreed that the implementation of TI approaches varied across the UK, with Scotland having more strategic coordinated implementation (additional file 2 , quote 1). We found that different regions and organizations reinvented the TI approach wheel, with interviewees expressing a need for national coordination. Participants expressed the need for adequate allocated resources and a more unified approach across organizations and sectors as a solution to the patchy implementation in England (additional file 2 , quote 2). They gave examples of the bottom-up networking initiatives driven by experts in TI care who created opportunities for sharing best practice and resources for implementing TI approaches. Participants cited a UK-wide Trauma Informed Community of Action and local TI care working groups.
One participant from England suggested that whilst the SAMSHA definition of TI approach was widely cited, they did not feel there was an agreed set of components and activities for implementing the framework in practice. This participant felt that a consensus on shared practice standards was a necessary next step for TI care in the UK.
At the organization level, some participants felt high level leadership support was needed, and if lacking is a barrier to implementing a TI approach. To achieve effective implementation leaders with power and those with passion were felt to be important. The concept of organizational champions garnered support when “ champions act as influencers and their credibility within services adds to the potential for buy-in from other staff ”, fostering sustainable change [ 53 ]. One participant warned against a reliance on top-down leadership, explaining that when a senior leader leaves an organization’s priorities can change. The participant also felt that change driven from the top-down, might lead to resistance from front-line staff (additional file 2 , quote 3). Some interviewees reaffirmed the view that people with lived experience should be involved in leading implementation of TI approaches (additional file 2 , quote 4).
Some interviewees felt that passionate individuals alone cannot create effective change without support at the organization level (additional file 2 , quote 5). Collective responsibility and organizational commitment were highlighted as an essential factor to support individuals with passion. In contrast, unsupportive organizational culture and high-pressure environments was perceived as a barrier (additional file 2 , quote 6). One document cited scarcity of resources and low staff morale, as well as a resistance to new initiatives and upheaval [ 52 ]. Competing demands and opportunity costs were also raised (additional file 2 , quote 7).
At the wider context level, documents highlighted the value of political support capable of influencing practice nationally [ 17 ]. Some interviewees explained disconnected and decentralized implementation of TI approaches across the UK by a shortage of political will and leadership in the central UK government, compared with those of the devolved administrations in Scotland and Wales (additional file 2 , quote 8). Proposed explanations included smaller territories, populations and governments, and “ more of a left-leaning social conscience politics” (Participant 3). Another interviewee called for a united parliamentary leadership recognised by government and capable of influencing policy.
Inadequate funding and commissioning of services was also described as a barrier, partly explaining regional differences in implementation of TI care (additional file 2 , quote 9). The COVID-19 pandemic was perceived as a barrier that contributed to the backlog of initiatives and work in the pipeline (additional file 2 , quote 10).
UK policies on implementation of TI approaches were not supported by UK-specific, methodologically robust, evidence for effectiveness, cost effectiveness and acceptability. Participants explained the policy-evidence gap by citing methodological challenges of evaluating system-level transformation and a need for commitment from commissioners and funders (additional file 2 , quote 11). In addition, participants who developed and implemented TI approaches in their organizations and regions did not have the capacity to evaluate their initiatives and disseminate the findings (additional file 2 , quote 12).
Participants had differing views on the future of TI care in the UK, although most agreed on its permanency. Some interviewees felt that TI approaches have already gained a critical momentum in the UK. In contrast to comments about TI care as a passing trend or ‘buzzword’ in the absence of in depth understanding, several interviewees voiced confidence that TI approach is here to stay, and will evolve, being incorporated into policy as well as being adopted more widely. Others were less optimistic and were concerned that insufficient political backing means policy endorsement will not translate to meaningful practice change.
Some participants thought that TI care should become a mandatory consideration with stronger central policy or monitoring by national watchdogs. They felt that the support of additional nation-wide regulatory measures could be beneficial. In contrast, some interviewees showed scepticism, fearing the creation of further ‘box-ticking’ measures. They feared that efforts to police or monitor providers could create a burden of empty bureaucracy without improving practice (additional file 2 , quote 13).
Our document analysis of health policies and interviews with professionals found differing representation, understanding, and implementation of TI approaches in the UK with wide variations between geographical areas, services, and individual professionals. Cross-sectoral endorsement of TI approaches in policies was not supported by high-level legislation or funding, and a UK-specific evidence base. Despite divergent and conflicting interpretations of TI approaches, the common understanding was that it differs from other practices by integrating TI principles at the organisational level and it should be tailored to the organization and wider contexts. It can also address NHS problems from integrated care to post-COVID recovery. We found more centralized implementation of TI approaches in Scotland and Wales versus piecemeal implementation in England. The implementation of TI approaches in England was driven from the bottom-up by passionate dedicated leaders at the level of organization or local authority, who called for more coordinated working supported by the UK government and NHS leaders. We identified factors that facilitated or hindered implementation of TI approaches at the level of organization (leadership, service user involvement, organizational culture, resource allocation, competing priorities) and wider context (government support, funding). The evidence-policy gap in TI care implementation can be explained by limited funding and evaluation capacity. Professionals had differing views on the future of TI approaches, however all agreed that without political backing at the government level, policy endorsement will not translate into meaningful implementation.
Our finding of a marked difference in the landscape of TI approaches in healthcare systems between the devolved nations, with evidence of a unified national strategy emerging in Scotland and Wales and notably absent in England could have several explanations. These include smaller territories, populations, and governments in devolved nations, with clear buy-in from government-level leadership in Scotland. Our analysis highlighted the initiatives of local decision-makers in England who have developed and implemented TI approaches in their own organizations and local authorities. The absence of a national strategy in England contributed to the piecemeal implementation, with some regions leading the way, and others silent. As local TI leads have been left to ‘find their own way’, they may not always have been aware of similar initiatives in other organizations and regions. A proposed solution was bottom-up initiatives aiming to bring the local TI leads together to share resources and good practice. This finding indicates the need for a leader on TI approaches within or linked to the UK government who can support and strengthen the bottom-up initiatives.
Another important finding is confirmation of the evidence-policy gap, with proposed reasons emerging in the analysis. Interview participants explained an absence of UK evidence on the effectiveness of TI approaches by a need for more interest from commissioners and funders, as well as a lack of physical and methodological capacity to evaluate system-level TI approaches. The former can be resolved through funding calls and comprehensive, transparent evaluation. The latter can be addressed by funding evaluations and raising awareness regarding available methodologies and tools for evaluating TI system change interventions [ 32 , 33 ].
Our finding of differing understanding of TI-approaches is in line with prior literature [ 63 ]. We found that some participants interpreted standalone TI practices (e.g., ACEs enquiry, one-off training about TI care) as a TI approach. Such interpretations are not supported by evidence. Authors of the ACEs study explained that the ACEs score is not a diagnostic tool, therefore care should be taken if used as part of community-wide screening, with rigorous evaluation of its use [ 64 ]. Recent reviews also found limited evidence on outcomes from routine enquiry, recommending further research [ 65 , 66 ]. Several systematic reviews demonstrated that standalone awareness raising did not result in change in behaviour and practices among healthcare professionals [ 67 , 68 ].
These misunderstandings can be explained by the conceptual mutability of a TI approach framework, lack of awareness about existing frameworks, and a need for coordinated working led by experts in TI approaches. The evidence of emerging working groups and UK-wide professional networks on TI care is promising. However, these initiatives require adequate funding and coordination to sustain momentum and develop further. These professional networks can become the platform for education about evidence-based TI approaches contributing to increasing value and reducing waste in research and implementation in this field.
This study is methodologically robust with perspectives drawn from UK policy documents and professionals, who have direct experience of developing and implementing TI approaches. Data analysis occurred alongside data collection, to help refine and guide further data collection. The limitations include no professional informants from devolved nations and no participants at the level of UK government. Due to time and funding restrictions, we could only recruit 11 professionals and did not interview patients including those with lived experience of trauma. Our small sample size could have resulted in underrepresentation of views of some stakeholders. Future research should recruit informants from these groups to draw a complete picture of the landscape of TI approaches in the UK.
Although health policies endorse implementation of TI approaches in the UK, they do not provide specific legislation, strategy or funding and are not supported by evidence of effectiveness. Understanding and implementation of TI approaches varies between regions, organizations, and individual professionals; however, all agree that if implemented at the system level and contextually tailored, TI approaches can mitigate varied problems withing NHS. The implementation of TI approaches in the UK is driven by local experts in TI care. A coordinated, more centralized strategy and enhanced provisioning for TI healthcare, including increased funding for evaluation and education through TI professional networks, can contribute towards evidence-informed policies and implementation of TI approaches in the UK.
Availability of data and materials
Data are available at the University of Bristol data repository, data.bris, at https://doi.org/10.5523/bris.2awc5pqkavac12d6jm1qp9wetm .
For reference: Lewis, N. (2022): TAPCARE policy review study. https://doi.org/10.5523/bris.2awc5pqkavac12d6jm1qp9wetm
All methods were performed in accordance with relevant guidelines and regulations as detailed here: https://www.biomedcentral.com/getpublished/editorial-policies#research+involving+human+embryos%2C+gametes%2C+and+stem+cells .
Abbreviations
Adverse childhood experiences
Coronavirus disease
Domestic violence and abuse
National Health Service
Substance Abuse and Mental Health Services Administration
Trauma-informed
United Kingdom
United States of America
Magruder KM, McLaughlin KA, Elmore Borbon DL. Trauma is a public health issue. Eur J Psychotraumatol. 2017;8(1):1375338.
Article Google Scholar
Kessler RC, et al. Trauma and PTSD in the who world mental health surveys. Eur J Psychotraumatol. 2017;8(sup5):1353383.
Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. Am J Community Psychol. 2007;40(3–4):313–32.
Ellis AE. Providing trauma-informed affirmative care: Introduction to special issue on evidence-based relationship variables in working with affectional and gender minorities. Pract Innov. 2020;5(3):179–88.
Prevention, C.f.D.C.a., Adverse Childhood Experiences (ACEs): preventing early trauma to improve adult health, in CDC Vital Signs. 2019.
Bellis MA, et al. National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England. BMC Med. 2014;12:72.
Scottish government. NHS Education for Scotland, S.G. Domestic abuse- and trauma-informed practice: companion document.
Statistics, O.f.N., Percentage of adults aged 16 to 74 years who were victims of domestic abuse in the last year, by ethnic group: year ending March 2018 to year ending March 2020, in Crime Survey for England and Wales (CSEW). 2020.
Rhys Oliver, B.A., Stephen Roe, Miriam Wlasny The economic and social costs of domestic abuse. 2019. 77.
Sacchi L, Merzhvynska M, Augsburger M. Effects of cumulative trauma load on long-term trajectories of life satisfaction and health in a population-based study. BMC Public Health. 2020;20(1):1612.
Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–46.
Hughes K, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–66.
Administration, S.A.a.M.H.S., SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach . Department of Health and Human Services USA, 2014: p. 27.
Bellis M, et al. The impact of adverse childhood experiences on health service use across the life course using a retrospective cohort study. J Health Serv Res Policy. 2017;22(3):168–77.
Mauritz MW, et al. Prevalence of interpersonal trauma exposure and trauma-related disorders in severe mental illness . Eur J Psychotraumatol. 2013;4:4.
Heron RL, Eisma MC. Barriers and facilitators of disclosing domestic violence to the healthcare service: a systematic review of qualitative research. Health Soc Care Community. 2021;29(3):612–30.
Department of Health and Social Care, A. The Women’s Mental Health Taskforce: Final report. 2018. 73.
Sweeney A, et al. A paradigm shift: relationships in trauma-informed mental health services. BJPsych advances. 2018;24(5):319–33.
Schippert ACSP, Grov EK, Bjørnnes AK. Uncovering re-traumatization experiences of torture survivors in somatic health care: A qualitative systematic review. PLoS ONE. 2021;16(2):e0246074–e0246074.
Article CAS Google Scholar
Jimenez RR, et al. Vicarious trauma in mental health care providers. J Interprofessional Educ Pract. 2021;24:100451.
Sweeney A, et al. Trauma-informed mental healthcare in the UK: what is it and how can we further its development? Ment Health Rev J. 2016;21:174–92.
Dheensa, S., et al., Healthcare Professionals' Own Experiences of Domestic Violence and Abuse: A Meta-Analysis of Prevalence and Systematic Review of Risk Markers and Consequences. Trauma Violence Abuse, 2022: p. 15248380211061771.
Harris M, F.R., Using trauma theory to design service systems. San Francisco. CA: Jossey-Bass; 2001.
Google Scholar
S, H. Medical Directors' Recommendations on Trauma-informed Care for Persons with Serious Mental Illness. 2018. 1–20.
Scottish government. NHS Education for Scotland, S.G. Transforming psychological trauma: a knowledge and skills framework for the Scottish workforce. 2017. 124.
Government of Canada. Canada, G.o. Trauma and violence-informed approaches to policy and practice. 2018.
Kimberg L, W.M., Trauma and trauma-informed care. New York. NY: Springer, Berlin Heidelberg; 2019.
Clare Law, L.W., Mickey Sperlich, Julie Taylor, A good practice guide to support implementation of trauma-informed care in the perinatal period . 2021: p. 42.
Harris M, Fallot RD. Envisioning a trauma-informed service system: a vital paradigm shift. New Dir Ment Health Serv. 2001;89:3–22.
Bowen EA, Murshid NS. Trauma-informed social policy: a conceptual framework for policy analysis and advocacy. Am J Public Health. 2016;106(2):223–9.
Dawson S, et al. Trauma-informed approaches to primary and community mental health care: protocol for a mixed-methods systematic review. BMJ Open. 2021;11(2):e042112.
Purtle J. Systematic review of evaluations of trauma-informed organizational interventions that include staff trainings. Trauma Violence Abuse. 2020;21(4):725–40.
Heidi Melz, C.M., Erin Ingoldsby, Karen Cairone, Mary Mackrain Review of Trauma-Informed Initiatives at the Systems Level. Trauma-Informed Approaches: Connecting Research, Policy, and Practice to Build Resilience in Children and Families. 2019. 37.
Dalglish SL, Khalid H, McMahon SA. Document analysis in health policy research: the READ approach. Health Policy Plan. 2021;35(10):1424–31.
Gale NK, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Williams N. Government policy - a spotter’s guide. 2012.
Hughes G. New models of care: the policy discourse of integrated care. People, Place and Policy Online. 2017;11:72–89.
Virginia Braun, V.C., Successful Qualitative Research. A Practical Guide for Beginners. London: Sage Publishing; 2013.
Parliament, U., Health and Social Care Act. 2012: https://www.legislation.gov.uk/ukpga/2012/7/introduction/enacted .
Government H. Transforming the response to domestic abuse: consultation response and draft bill. 2019.
Government H. Integration and Innovation: working together to improve health and social care for all D.o.H.a.S. Care, Editor. 2021.
Office, H., Ending Violence against Women and Girls. 2016: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/522166/VAWG_Strategy_FINAL_PUBLICATION_MASTER_vRB.PDF .
Government S. Public Health Priorities for Scotland. 2018.
Government H. HM Government: Serious Violence Strategy. 2018.
Home Office. Ending violence against women and girls 2016–2020: refresh strategy H. Office, Editor. 2019.
Government H. C.O. Department of Health and Social Care, Editor. COVID-19 Mental Health and Wellbeing Recovery Action Plan. 2021.
NHS England. NHS Five Year Forward View. 2014. 41.
Health and Justice, A.F.a.S.A.R.C.S.T. Strategic Direction for Sexual Assault and Abuse Services: Lifelong care for victims and survivors: 2018 - 2023. 2018. 28.
NHS, The NHS Long Term Plan. 2019. p. 136.
NHS, NHS Mental Health Implementation Plan 2019/20–2023/24. 2019.
Jo Wilton, A.W. Engaging with complexity: Providing effective trauma-informed care for women. 2019. 26.
Lauren Bear, G.D., Jessica Southgate A sense of safety: Trauma-informed approaches for women. 2019. 24.
Bunting L, M., L, Mooney, S, MacDonald, M, Coulter, S, Hayes, D, Forbes, T, Developing trauma informed practice in Northern Ireland: Key messages. 2019, Queen’s University Belfast. p. 33.
Kennedy, A. Successes and struggles keeping trauma in mind: development of a trauma informed adult mental health service.
Royal College of Psychiatrists, C.C.f.Q.I. Ten evidence-based reasons for embedding values-based ‘Enabling Environments’ in health care.
S, R., Trauma-informed approaches. Trauma-informed care: implications for practice. 2018: https://www.nottinghamshire.gov.uk/media/1533199/traumainformedcare.pdf .
C, G., Trauma-informed care in response to adverse childhood experiences. Nursing Times, 2018. 114: 7, 46–49.
Highland N. The Annual Report of the Director of Public Health: Adverse Childhood Experiences. Resilience and Trauma Informed Care: A Public Health Approach to Understanding and Responding to Adversity; 2018. p. 82.
Network, N.E.C.N.a.t.N.E.a.N.C.A.H.S., Developing real world system capability in trauma informed care: learning from good practice . Trauma Informed Community of Action, 2020: p. 24.
Steven Thirkle, A.K., Paras Patel, Petia Sice ROOTS: A reflective framework for mapping the implementation journey of trauma-informed care 2021. 38.
Fenney D. The role of trauma-informed care during the Covid-19 pandemic. 2021.
Sweeney A, Taggart D. (Mis)understanding trauma-informed approaches in mental health. J Ment Health. 2018;27(5):383–7.
Anda RF, Porter LE, Brown DW. Inside the adverse childhood experience score: strengths, limitations, and misapplications. Am J Prev Med. 2020;59(2):293–5.
Ford K, et al. The evidence base for routine enquiry into adverse childhood experiences: a scoping review. Child Abuse Negl. 2019;91:131–46.
Gentry SV, Paterson BA, Does screening or routine enquiry for adverse childhood experiences (ACEs) meet criteria for a screening programme? A rapid evidence summary. J Public Health. 2021;fdab238.
Zaher E, Keogh K, Ratnapalan S. Effect of domestic violence training: systematic review of randomized controlled trials. Can Fam Physician. 2014;60(7):618-24-e340-7.
Kalra N, et al. Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst Rev. 2021;5:CD012423.
PubMed Google Scholar
Download references
Acknowledgements
We would like to thank all the interview participants and those with an interest in TI approaches who kindly shared policy documents and background literature with the study group. We would like to acknowledge the contributions of Dr Sandi Dheensa in reviewing the draft manuscript.
This report is independent research funded by the National institute for Health and Care Research (NIHR), Research Capability Funding stream via NHS Bristol, North Somerset and South Gloucestershire Clinical Commissioning Group. NVL was also supported by the NIHR Bristol Biomedical Research Centre (grant BRC-1215-20011). The views expressed are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
Centre for Academic Primary Care, Bristol Medical School, University of Bristol, Bristol, UK
Elizabeth Emsley & Joshua Smith
Centre for Academic Mental Health, Bristol Medical School, University of Bristol, Bristol, UK
David Martin
NIHR Bristol Biomedical Research Centre, University Hospitals Bristol and Weston NHS Foundation Trust and University of Bristol, Bristol, UK
Natalia V. Lewis
You can also search for this author in PubMed Google Scholar
Contributions
NVL conceived, designed, and led the study. EE, NVL, JS and DM collected and analysed documents and interview data. EE and NVL wrote the first draft of the manuscript with input from DM and JS. All authors contributed to subsequent revision and approved the final version.
Corresponding author
Correspondence to Elizabeth Emsley .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Faculty of Health Sciences Research Ethics Committee at University of Bristol (Ref 114665, 11 February 2021). Interview participants provided verbal informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. .
Interview topic guide.
Additional file 2.
Analytical themes with subthemes and supporting quotes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Emsley, E., Smith, J., Martin, D. et al. Trauma-informed care in the UK: where are we? A qualitative study of health policies and professional perspectives. BMC Health Serv Res 22 , 1164 (2022). https://doi.org/10.1186/s12913-022-08461-w
Download citation
Received : 16 March 2022
Accepted : 05 August 2022
Published : 14 September 2022
DOI : https://doi.org/10.1186/s12913-022-08461-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological trauma
- Mental health
- Primary health care
- Public health
- Qualitative research
- Policy making
- Health policy
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Meet the Team
- Meet the Board
- Careers at CSW
- Competencies & Credentials
- Federal, State, & Local Systems Change
- Improving Practices & Outcomes
- Racial Equity and Inclusion
- Research & Evaluation
- Trauma & Resilience at Work
- Workforce Benchmarking Network
- Support CSW
An Introduction to Trauma-Informed Research
- March 19, 2024
- Blog , Research & Evaluation , Trauma & Resilience at Work
Attention to mental health has increased over the last few years, brought on by the collective trauma of the COVID-19 pandemic and the racial trauma of race-based police brutality among other personal and community traumas. Research shows that trauma can negatively impact people’s ability to succeed and thrive at work and in life. [i] Researchers who conduct qualitative research with workers, learners, and community members who may be affected by trauma are increasingly asking how they can design and implement trauma-informed research practices that are respectful of their participants’ lived experiences and do not perpetuate harm.
Why Shape Research to be Trauma-Informed?
Implementing trauma-informed research best practices provides researchers ways to reduce or address the potential harm that could arise from qualitative research. Trauma-informed research also garners more realistic and useful information. If participants feel safe and trust the researcher, they will stay engaged and provide more truthful and richer answers, which can lead to more effective and relevant workforce and post-secondary solutions and programs.
Trauma-informed research also complements and builds on other important approaches researchers are incorporating into their work, including human-centered design, racial equity, participatory research, and cultural responsiveness. The workforce field is continually learning how critical it is to center the voice of participants in research and programs, truly understand their lived experiences, and design research and programs that are grounded in real lives. This requires talking with participants in careful, authentic, and intentional ways, which means taking a trauma-informed approach.
What is Trauma?
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), trauma is “an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.” [ii]
A key aspect of this definition is that trauma is an individualized experience: different people may experience trauma differently, depending on their mental health, chemistry, biology, and other life experiences. Researchers should not assume that all individuals who have experienced traumas such as gun violence, poverty, racism, etc., will have experienced them as traumatic events. However, adopting a universal trauma-informed approach to research will be responsive to those folks who have experienced trauma and is a healthy practice with participants who have not experienced trauma.
Another important aspect of this definition is that individuals who experience trauma, or trauma re-triggering, experience it very intensely. Their bodies and brains feel as though they are being attacked, threatened, or harmed. Their automatic physical and behavioral responses may seem over-reactionary. If they are triggered by a research question or a set of questions, their brains may go into survival mode—fight, flight, freeze, or submit—deactivating the logical processing and executive functioning part of their brains. This is not an experience any researcher wishes participants to have and threatens the validity and quality of any qualitative data that researchers may collect.
Two other notable components of the SAMHSA definition are that trauma has lasting effects and can harm an individual’s functioning and well-being across multiple life dimensions. Traumatic experiences can continue to haunt an individual and hurt their ability to succeed in life, in relationships, and at work, especially if it is not processed through therapy. On the other hand, traumatic experiences can get buried, forgotten by an individual for years, but then possibly emerge by some sort of trigger and then affect the individual’s functioning. [iii]
How Might Trauma Show Up in Qualitative Research?
Qualitative researchers in the fields of workforce development or post-secondary education may ask participants about their education levels and experiences, income and finances, employment history, justice involvement, familial situation, housing, and other personal information to understand the impact of services and how to improve them. Folks with lower levels of education, living in poverty, struggling financially are likely to have had traumatic experiences on any or all of these dimensions—as children and/or adults. [iv] Additionally, participants who have experienced discrimination, racism, or harassment in their work and education settings may also have trauma responses to research questions about their past work and learning experiences.
Talking about these challenges in an interview or focus group may retrigger them, causing a trauma response. For example, if a focus group participant lost their job and experienced homelessness for several months living in their car with their family in a dangerous neighborhood, seemingly simple questions like, “have you ever been unemployed” or “have you ever experienced homelessness” might send their brain into survival mode, impairing their ability to answer the questions.
Our brains and bodies are connected, so trauma responses show up as mental and/or physical conditions or behaviors. Physical responses to trauma triggering interviews, focus groups, or sometimes even survey questions may include increased heart rate, hypersensitivity and scanning for danger, stomach churning, sweating, or fidgeting. These are all signs that the brain and body are preparing to fight or flee danger—in this case, trauma that has been stirred up.
Additional behaviors may show up as one or more of the four common survival mode responses:
- Fight : the participant may go into defense mode and put up their guard. Their mind may be racing with questions such as why is this stranger asking such personal questions, what are they going to do with my personal information, are my answers going to come back to hurt me? They may give short, curt, perfunctory answers or respond sarcastically. In rare instances, they may verbally lash out if their brains and bodies are feeling threatened.
- Flight : the participant may try to end the uncomfortable or seemingly unsafe situation early. They may be scanning for an escape route, like asking to go to the bathroom and then leave the building or use up time. They may walk out of the interview or focus group.
- Freeze : the participant’s brain may seize up. It may be so flooded with anxiety and survival mode thinking that the participant may not hear or see the questions being asked or hear them clearly. Their thoughts may be jumbled, producing confusing, conflating, or conflicting answers. They may experience brain fog and answer incoherently. They may not even be able to verbally respond.
- Fawn : the participant surrenders to what they perceive as a dangerous situation and just gives up. This may manifest as a “so what” attitude and giving no energy or effort to answering questions intentionally or authentically. Answers provided may be far from the truth, severely skewing the qualitative information.
What is a Trauma-Informed Research Approach?
Trauma-informed research or research that incorporates the tenants of trauma-informed care is an approach that considers principles of trauma-informed care and designs and conducts the research with the awareness that an informant may have experienced trauma. SAMHSA provides a framework for a trauma-informed approach, which is useful for many types of work including research, programming, and even organizational culture change.

Researchers can use this approach to inform trauma-informed research by intentionally considering the following:
- Safety : how do you help participants feel physically, emotionally, and psychologically safe in the research? For example, do they feel safer in a focus group if they sit near the exit? How do you help them feel valued and recognized?
- Trustworthiness and transparency : how do you establish trust with research participants? A key factor in building trust is transparency, so how do you maximize transparency in the research process?
- Peer support : Researchers are intelligent people often from highly respected, sometimes well-known academic institutions. This role has embedded in it much perceived authority and power, which may be intimidating to research participants. And yet, participants are human beings, just like researchers and are providing critical and essential information that without, the research would not be possible. So, how do you as a researcher consider and treat the participant as a peer and support them in the research process as such?
- Collaboration and mutuality : This principle is similar to the one above. How do you collaborate with the participant in the research rather than treating them as research subjects? How do you show mutual respect for the participant and their lived experience expertise?
- Empowerment, voice, and choice : Providing a safe space, respecting, and valuing research participants will empower them to share their experiences and knowledge with you authentically. How do you reciprocate and truly listen to their voice and experiences, even if they are different from your expectations, predictions, and possibly even your values and beliefs? Providing choice helps people feel psychologically safe and empowered, so how do you provide choice opportunities for participants, even if it is as simple as which chair to sit in, which pen to use, or the research location.
- Cultural humility and responsiveness : Do you understand fundamentals about the research participant’s cultural background and social identities, i.e., do you ask for gender pronouns, do you know whether the person’s culture views looking someone directly in the eye is a sign of respect or disrespect? How do you show respect for and honor the participant’s cultural background and personal identities?
How Do I Conduct Trauma-Informed Research?
Workforce and post-secondary researchers should plan for and embed trauma-informed practices throughout the research process− before, during, and after qualitative research activities. Below is a list of suggested steps to take when planning research activities with community members. These steps were informed by other trauma-informed and trauma-responsive research resources, CSW’s research, and the research and training of our Trauma and Resilience at Work team. Many of these steps also reflect other research approaches that are heavily intertwined with a trauma-informed approach, such as cultural responsiveness, racial equity, participatory research, and human-centered design.
It should be noted that these steps are appropriate for workforce and post-secondary research with participants who may have experienced trauma. A more extensive protocol and protections are needed for researchers who study trauma and traumatic experiences.
Before the research begins, researchers should consider the following practices:
Consider the research purpose and needs : Be clear at the outset about the purpose of the research and if you and your organization are the right fit to conduct research in this community or if you need partners embedded in the community.
Understand the community context : Conduct baseline community research to understand relevant demographics and potential traumas participants may have experienced.
Select appropriate research methods : Research activities should be chosen based on fit with the research purpose and consideration of the potential nature of questions and impact. For example, the information sought by the researcher is sensitive, would participants feel safe discussing it with a group of strangers?
Thoughtfully identify facilitators and roles : Consider the number of researchers needed to implement best practices and other possible factors in selection, including personal identities such as gender, race and ethnicity, lived experience, etc.
Use informed consents : Design a consent and outreach process that ensures participants understand what your research and dissemination entail so that they can make informed decisions on their participation.
Determine ethical compensation : Decide appropriate compensation amounts that recognize contributions and time but do not provide undo pressure to agree to a situation that is not healthy or safe.
Select appropriate locations for in-person research : Ensure that the location chosen for interviews, focus groups, or other qualitative research activities will allow participants to feel safe (e.g., not near police station or government building) and that there are areas where they can step out if needed to take a break (i.e., a bathroom, etc.).
Support participants with refreshments : If the research is in-person, offering water can help participants feel cared for. Sipping water can help a triggered person regulate their nervous system. If online, encourage and welcome participants to get a beverage or a snack to help them feel more comfortable and at ease.
Develop protocols aligned to the purpose of the research : Ensure research questions reflect the research purpose only and do not expand the scope merely out of curiosity. Respect the time and information participants are sharing with you.
Develop protocols with members of the community : Keep participatory and culturally responsive best practice in mind and co-develop protocols with the community and/or ensure appropriate vetting of the questions and research process. This can be with:
- Partner organizations embedded in the community
- Advisory boards
- Compensated representatives from the community
Develop an intentional recruitment strategy : Also include partner organizations embedded in the community in recruitment to help increase trust.
Plan how you will provide support if needed (both virtual and in-person) : Design a consistent process for facilitators to identify and intervene if a conflict or situation arises or they notice anyone experiencing the trauma responses covered earlier. This plan should include researching culturally appropriate resources and support organizations in advance for any needed follow-up. The plan might include:
- Asking the focus group to pause, noting that you may be covering heavy content, and suggest a few deep breaths. Doing this as a group helps to avoid singling anyone out, which reinforces safety
- Offer everyone a two-minute break
- Offer water or a restroom break
When conducting the research, researchers should consider the following practices:
Reiterate consent & rights : Reiterate research intent and purpose and remind participants of their right to leave at any time, take care of their needs, or not answer specific questions. Describe the research in a way non-researcher participants will understand. And make sure to ask for questions before beginning.
Remind participants of key locations for meeting basic needs , i.e., exit, water, bathrooms, etc., if in person.
Balance power and maintain a kind presence : Do not react or judge participants’ presence, behavior, or answers; be aware of your unconscious bias and reactions; dress thoughtfully and in a way that will not intimidate participants. Exercise empathy.
Begin with a warm-up activity to build trust and rapport : This could include sharing names, pronouns, etc., as well as a short ice breaker activity. If the researcher is asking for a lot of personal information from the participants, it will feel fairer and more comfortable if you share a bit about yourself (this is an example of exercising the peer support principle).
State the topic first before advancing to a new topic and new questions : This provides continual informed consent and allows participants to make choices for themselves. It increases transparency and psychological safety (no surprises).
Use active listening : After a participant has answered a question, you may want to repeat back to them what you heard, mirroring their language as much as possible. This helps them feel seen and heard and avoids the researcher interpreting the answer through their own lens and experiences. This technique also may encourage the participant to expound upon their answer, providing a deeper level of information.
Meet participants’ energy levels : This helps participants feel safe and build rapport with the researcher.
Support participants as needed & as aligned to the plan developed during planning . If participants appear to be getting triggered, acknowledge that the content of the discussion can be difficult and that, if participants are feeling uncomfortable or unsafe, that’s a completely normal response to discussing difficult topics. Provide options to help them return to a feeling of safety, e.g., break, water, bathroom, discuss other topics in the protocol. Return to difficult topics if and when the participants are ready.
Be flexible : Meet participants where they are. If you can’t ask all the questions, need to stop, or adjust protocol, you are engaging in trauma-informed practices.
Communicate with facilitation partner : Have a plan in place for communicating about and enacting safety plans to maintain participant and facilitator safety, e.g., safe words or phrases if a facilitator identifies a potentially triggered participant (or is triggered themselves).
Debrief the research activity with the participants, especially if they appeared impacted : This is a method for helping participants process or metabolize a potentially difficult experience. You can frame the debrief as follows: “I am always looking to improve our research process and would love any comments on what went well today and one or two suggestions for small things I could improve in our process…”
After conducting the research, researchers should consider the following practices:
Follow up with participants : If someone was impacted by the research experience, then it can be helpful to check in later or offer resources depending on the situation.
Follow up with facilitators : If there was a difficult or emotional situation, then it may also be appropriate to follow up with colleagues as well.
Continually confirm the process : Discuss with other facilitators how the process is going and where there may be a need for tweaks to ensure the safety and comfort of all participating even if this means not all research activities will be uniform.
Disseminate the information collected with care and respect for the participants : Follow best culturally responsive and participatory practices around dissemination to ensure participants’ stories and experiences are thoughtfully reported. Consider if the information being shared was about your mother, father, brother, sister, or children, would you describe it in the same way?
There are many different ways that you and/or your team can get started on learning more about and implementing trauma-informed research practices in your workforce and post-secondary education research. Some initial organizational steps include:
- Update any research guides or protocols you have with this information.
- Provide staff training on trauma, trauma-informed approaches, cultural responsiveness, racial equity and inclusion, active listening, and other related strategies and practices.
- Develop organizational protocols and practices around researcher self-care and safety to acknowledge and avoid potential trauma triggering and secondary trauma.
- Develop and implement a process for debriefing research experiences and continually evaluating and augmenting organizational procedures.
Every organization operates differently and with different practices, approaches, and ethical considerations. There may be many other different, or more appropriate, actions for you and your organization to take for your work and the communities you work in. These are meant to be a jumping off point for those in the field looking to get started with trauma-informed research. Some of the many resources out there are included below. If you have questions or want to talk through any of the aforementioned, please reach out to us at [email protected].
- Learn more about our Trauma & Resilience at Work team
- Learn more about our Research & Evaluation Team
Additional Resources:
- Think of Us, Trauma Responsiveness in Participatory Research
- Urban Institute Guidelines to Incorporate Trauma-Informed Care Strategies in Qualitative Research
- Trauma and Resilience Quick Guides
- A Trauma-Informed Approach to Workforce
[i] Robert F Anda, Vladimir I Fleisher, Vincent J Felitti, Valerie J Edwards, Charles L Whitfield, Shanta R Dube, David F Williamson. 2004. “Childhood Abuse, Household Dysfunction, and Indicators of Impaired Adult Worker Performance.” The Permanente Journal . Winter;8(1):30-8. https://www.thepermanentejournal.org/doi/10.7812/TPP/03-089?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed . Accessed March 5, 2024.
[ii] Substance Abuse and Mental Health Services Administration: Practical Guide for Implementing a Trauma-Informed Approach. SAMHSA Publication No. PEP23-06-05-005. Rockville, MD: National Mental Health and Substance Use Policy Laboratory. Substance Abuse and Mental Health Services Administration, 2023.
[iii] Bessel van der Kolk, M.D. 2014. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. Chapter 12.
[iv] Merrick MT, Ford DC, Ports KA, Guinn AS. ”Prevalence of Adverse Childhood Experiences From the 2011-2014 Behavioral Risk Factor Surveillance System in 23 States.“ JAMA Pediatrics. 2018;172(11):1038–1044. doi:10.1001/jamapediatrics.2018.2537

Meet the Author
Vickie choitz.
Vickie Choitz is the Director of Trauma and Resilience at Work. The CSW Trauma and Resilience at Work team advances workplaces and workforces that are culturally responsive, trauma-informed, healing-centered, resilience-building, and supportive of mental well-being. Continue Reading >>

Megan Elyse Williams
Megan is the Director of Research and Evaluation at CSW. Her current work includes supporting research and evaluation activities at CSW, as well as the staff engaged in them, and ensuring CSW’s research and evaluation methodologies and activities are current, ethical, and culturally responsive. Continue Reading >>
Comments are closed.

Exploring Examples of Trauma-Informed Care Questions to Guide Intake

When offering any kind of Trauma-Informed Care, you’re likely to meet people who will be hesitant to open up. Whether you’re working in mental health care, education, legal support, or social work, some of those “awkward” and even painful questions are key to learning the needs of the people you’re serving .
So, what are some examples of Trauma-Informed Care questions and approaches where the right approach can make a world of difference?
Letting the Situation Be Your Guide
In Healing-Focused Care, we prefer to focus on the individual ‘s strengths. The goal is always to empower the served person to make positive choices and take steps toward healing . As practitioners, it’s essential to realize that every situation you encounter will be unique, and there’s no set approach or a Trauma-Informed Care questionnaire that will fit all.
As an example, when performing an initial intake, you want the conversation to dictate the flow of the intake versus letting the intake or assessment dictate the flow of the conversation.
When you carry out a Trauma-Informed Care assessment, your goal is to learn about the person’s journey thus far. Why are they coming to your organization? What do you need to learn from them to ensure that the services offered by your organization are the right match for their needs? What can you learn about this person?
Sound deep for an intake? It can be. When offering Trauma-Informed Care , questions can be personal and even difficult. The goal is always to avoid “retriggering” the person’s trauma while allowing them a safe space to open up and connect .
When things get deep and personal, following a set of specific ” Trauma-Informed Care questions” can actually feel impersonal and distant. It’s important to let the conversation happen naturally rather than read off an assessment list and check the boxes.
We often think of Healing-Focused Care as primarily applicable in mental health settings, but the Healing-Focused Care model can apply to all sorts of different situations, service environments, and role types. For example, an educator may use Trauma-Informed Care questions to help guide a meeting with a new student. A parole officer may use similar questions to build rapport with their client. Likewise, hospital staff may want to use a Healing-Focused Care approach when discussing medical history and other sensitive topics.
Any time we’re dealing with human topics, sensitivity will put people at ease and help them feel comfortable opening up and beginning to share .
At Share Collaborative, we’re not here to “tell people” or “ train people ” on how they should approach their clients. We’re not interested in telling you a bunch of questions you should ask on an intake assessment. Each context is different. As I write this to you and you’re there in front of your screen reading, I have no idea what you do, the needs of the clients, or your organization’s approach.
What we love to share and teach (and yes, what some refer to as train) is how to ask questions. The approach is, in our opinion, the most crucial aspect of any intake or human interaction . What is the vibe, the energy of the asker? What is the vibe of the listener? How can they play off each other and come together to connect in a safe, effective, and healing-focused way?
Set-up Context and Ground
When the conversation starts, it’s helpful to set up the context. The background helps establish the environment and puts everyone in the right frame of mind.
Ask yourself, why are you going to have this conversation? What is the intention of this conversation, and what is the purpose? The purpose of the discussion will act as your guiding star throughout the interaction . Should things go off the rails, come back to the purpose.
Similarly, ask why you want to learn this information about the client. What will happen to it? Where will the information go? Transparency is key in providing trauma-informed, healing-focused care.
One answer applies in every context in the wide variety of areas that I’ve served in, such as youth, families, AODA, criminal justice, schools, and workforce development. The purpose of the conversation is to LEARN . “I’m employing the structure of this intake or assessment to learn how I, along with my team, can be helpful to you, the served person.”
To that end, the first question you may ask is something to establish context. For example:
- What do you already know about what is the purpose of our time together today?
If it feels appropriate to the situation, you could show them the intake form or assessment. Again, it’s important to be transparent. Some people feel more comfortable when they’re aware of the types of questions that will be asked and know a little about what to expect.
On a similar note, you may then want to ask:
- What questions do you have about the conversation we’re going to get into?
You can ensure them that there are grounding techniques that you can walk through in case the questions stir up some discomfort. Review the list of techniques together to agree upon something that feels comfortable to them. Aside from listening to their favorite death metal song turned up to 11, there is likely a grounding technique that they can do in or just outside your office (or in whatever space you may be holding the conversation).
The next question you might ask is:
- What helps you return to the present? Or…
- What helps you cool your jets? Or…
- What helps you recombobulate? (Your version of any of these questions will be just fine!)
As you provide context and grounding techniques, keep the conversation as short and sweet as possible . Do your best to go at the other person’s pace and in a way that feels appropriate to their needs. The next question you might ask is something along the lines of:
- Are we good to go?
This question helps them check in and empowers them to decide that the conversation can move forward. It’s always important to go at the PACE of the person.
Start the Trauma-Informed Care Assessment Questions Broadly
If you’ve ever watched a late-night talk show or even an interview on the news, you’ve likely heard of a “softball question.” These questions are typically broad and easy. They help establish a connection and build comfort.
Starting with an open-ended question allows the guest (or, in this case, the person you’re serving) to riff on however they feel . They can discuss and share what they want to share. This type of question puts them in control and offers them the power position in the conversation, and that’s where you want them to be.
Powerlessness is the very essence of the invisible wound—the trauma. So right away, you’re avoiding creating a power void. You’re helping them get comfortable and feel empowered. Before you jump into any “must ask” questions on the intake form or assessment, the question you may want to ask is:
- What would you like me to know about you and your journey?
Once again, your version of the question will do just fine. Like most conversations, you’ll likely start off less personal and get more so as the conversation goes on. In the early part of a Trauma-Informed Care assessment, you’re creating safety.
I often remind myself that “Slow is smooth. Smooth is fast. Fast is good.” This means that when you take your time early on and set up the proper context on the front end, it will take less time to complete the intake and assessment as you go on (for most encounters, as you likely know).
The initial few questions may seem unnecessary, but it’s in those early moments that you’re really seeing the other person as a fellow human being. You’re not just there to “fill out a questionnaire” and do an intake. You’re there to help them on their journey and to understand them —to hold a safe space for them in the moment so they can begin their journey of healing-focused care.
As you listen (the most essential part of asking any question), the person will often start to answer some of the questions on your intake form or assessment. You can sit back, listen to them, and begin to check off the boxes and fill in the blanks.
Allow the Conversation to Dictate the Flow
Now you’re in the heart of performing the care assessment. You might feel the urge to adhere to a strict order and read off the questions.
The conversation will be more comfortable, open, and productive if you instead allow it to unfold as needed. That means allowing the conversation to dictate the intake or assessment’s flow , rather than the assessment form dictating the flow of the conversation.
We often get worried that we’re going to miss something or forget to ask, but we can circle back around as needed if we’re familiar with the assessment before we begin. Remember that we have the magical capacity to turn pages and click-through screens. So if someone starts answering questions from page one and then offers insight that answers something on page three, section two, jot it down, reflect it, and listen.
For example, you might find that when you reflect what they say, it can lead you on to another section of the assessment. Or if you need to get a little more information, you can try the wonderful question:
- Can you tell me more about that? (Again, your version will be totally fine.)
Or do both! Reflect what they shared and invite them to share more about it. When you know what information you need to glean from the conversation, you can always let it come back around to where you need to go. The more you listen and offer a safe, caring space to share, the more they will be willing to open up and offer the information .
Wrapping Up the Intake Conversation
As you complete the intake conversation, there’s can be a tendency to want to wrap up and move forward to the next step. But throughout the conversation, especially at the end, take time to genuinely and substantively affirm them for sharing.
The goal of Healing-Focused Care is to help the served person move forward with positive steps in their healing journey . It takes a great deal of strength and bravery to delve into our traumas, especially with someone we don’t know well (as in any human services setting). Even if we’ve elected to put ourselves in a situation such as mental health counseling or educational settings , we as humans may still have a hard time opening up to someone we just met in such a vulnerable way.
As Trauma-Informed Care providers, one of the best ways to build rapport and help close the conversation in a nurturing, healing-focused way is with affirmation . For example, you may want to say something like:
- You’ve demonstrated a lot of bravery today—not only in sharing this with me but also in keeping your head up and continuing to work hard to not only survive but thrive from some of these super painful experiences. Thank you. I’m honored that you’ve shared this with me.
As with all the Trauma-Informed Care questions and conversation examples here, your version of the statement will be just fine. The main thing is to own what we’re saying and sincerely mean it . Connecting with someone during their healing journey can be powerful for them as well as for us as care providers.
Please reach out for more information on the Healing-Focused Care model and ways to help your team provide substantiative Trauma-Informed Care. We’d love to work with you on the next steps of your journey.
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
How to Incorporate Trauma-Informed Care Into Clinical Care

Many patients have experienced some form of trauma, which can have lasting adverse effects on physical and mental health. Adopting a trauma-informed care (TIC) approach is integral to improving health outcomes and creating better patient-provider relationships.
“Trauma-informed care is really about creating a space where every person, including people who have experienced trauma, feel safe, feel included, and feel understood as a whole person,” says Stephanie Hargrove, PhD , clinical psychologist and assistant professor at Duke. A comprehensive approach must include making changes at all levels within a health care practice, including nonclinical staff, who have significant interactions with patients and are critical to ensuring patients feel safe.
Hargrove recently shared tips, based on six core principles of TIC developed by the Substance Abuse and Mental Health Services Administration, for how providers can incorporate TIC into their organization’s clinical practices and policies.
Continue to the full article on the Duke Health website to read the tips.
Youth, caregiver and healthcare professional perspectives on planning the implementation of a trauma-informed care programme: A qualitative study
Affiliations.
- 1 University of Ottawa, Ottawa, Ontario, Canada.
- 2 Children's Hospital of Eastern Ontario (CHEO), Ottawa, Ontario, Canada.
- 3 Princess Margaret Cancer Centre, Toronto, Ontario, Canada.
- 4 CHEO Research Institute, Ottawa, Ontario, Canada.
- 5 University of Missouri-Kansas City, Kansas City, Missouri, USA.
- 6 Li Ka Shing Knowledge Institute, St. Michael's Hospital, Unity Health Toronto, Toronto, Ontario, Canada.
- 7 Epidemiology Division and Institute of Health Policy, Management, and Evaluation, Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada.
- 8 Queen's Collaboration for Health Care Quality: A JBI Centre of Excellence, School of Nursing, Queen's University Kingston, Kingston, Ontario, Canada.
- 9 Ottawa Hospital Research Institute, Ottawa, Ontario, Canada.
- 10 University of Ottawa Heart Institute, Ottawa, Ontario, Canada.
- PMID: 38450840
- DOI: 10.1111/jan.16095
Aims: To explore youth, caregiver and staff perspectives on their vision of trauma-informed care, and to identify and understand potential considerations for the implementation of a trauma-informed care programme in an inpatient mental health unit within a paediatric hospital.
Design and methods: We applied the Interpretive Description approach, guided by complexity theory and the Implementation Roadmap, and used Applied Thematic Analysis methods.
Findings: Twenty-five individuals participated in individual or group interviews between March and June 2022, including 21 healthcare professionals, 3 youth and 1 caregiver. We identified two overarching themes. The first theme, 'Understanding and addressing the underlying reasons for distress', related to participants' understanding and vision of TIC in the current setting comprising: (a) 'Participants' understanding of TIC'; (b) 'Trauma screening and trauma processing within TIC'; (c) 'Taking "a more individualized approach"'; (d) 'Unit programming'; and (e) "Connecting to the community". The second theme, 'Factors that support or limit successful TIC implementation' comprises: (a) 'The need for a broad "cultural shift"'; (b) 'The physical environment on the unit'; and (c) 'Factors that may limit successful implementation'.
Conclusion: We identified five key domains to consider within trauma-informed care implementation: (a) the centrality of engagement with youth, caregivers and staff in trauma-informed care delivery and implementation, (b) trauma-informed care core programme components, (c) factors that may support or limit success in implementing trauma-informed care within the mental health unit and (d) hospital-wide and (e) the importance of intersectoral collaboration (partnering with external organizations and sectors).
Impact: When implementing TIC, there is an ongoing need to increase clarity regarding TIC interventions and implementation initiatives. Youth, caregiver and healthcare professional participants shared considerations important for planning the delivery and implementation of trauma-informed care in their setting. We identified five key domains to consider within trauma-informed care implementation: (a) the centrality of relational engagement, (b) trauma-informed care programme components, (c) factors that may support or limit successful implementation of trauma-informed care within the mental health unit and (d) hospital-wide and (e) the importance of intersectoral collaboration. Organizations wishing to implement trauma-informed care should consider ongoing engagement with all relevant knowledge user groups throughout the process.
Reporting method: Standards for Reporting Qualitative Research (SRQR).
Patient or public contribution: The local hospital research institute's Patient and Family Advisory Committee reviewed the draft study methods and provided feedback.
Keywords: child nursing; focus groups; mental health; patient perspectives; psychiatric nursing; qualitative approaches; quality of care; research implementation.
© 2024 The Authors. Journal of Advanced Nursing published by John Wiley & Sons Ltd.
Grants and funding
- CHEO Psychiatry Associates Research Fund
Ask a Librarian
- Recognizing Trauma in College Students
- Trauma as a Disability
- Books on Understanding Trauma
- UW Resources
- Pierce County Resources
- Videos and Podcasts
- Trauma Informed Approach in Higher Education
- Trauma Informed Pedagogy
- Trauma Informed Librarianship
- University of Washington Libraries
- Library Guides
- Understanding Trauma
Understanding Trauma: Trauma Informed Approach in Higher Education
Trauma informed approach.
A trauma-informed approach acknowledges that students' behaviors are influenced by their life experiences. Additionally, a trauma-informed approach:
- Recognizes the widespread impact of trauma and identifies potential paths toward recovery
- Identifies the signs and symptoms of trauma in individuals
- Integrates knowledge about trauma into policies, procedures, and practices
- Strives to actively prevent re-traumatization and secondary trauma
Principles of Trauma Informed Care
Trauma-informed care is a framework that emphasizes understanding, compassion, and empowerment in working with individuals who have experienced trauma. At its core are several key principles:
- Safety: Creating an environment that is physically and emotionally safe for patrons is paramount. This includes establishing clear boundaries, maintaining confidentiality, and ensuring that library spaces are welcoming and free from potential triggers.
- Trustworthiness and Transparency: Building trust with patrons is essential in a trauma-informed approach. Librarians should strive to be honest, reliable, and transparent in their interactions, respecting the autonomy and agency of each individual.
- Peer Support and Collaboration: Encouraging peer support and fostering collaborative relationships within the library community can help individuals feel connected and supported. This can involve facilitating support groups, partnering with community organizations, or simply providing opportunities for patrons to engage with one another.
- Empowerment and Choice: Recognizing the strengths and resilience of patrons, librarians can empower individuals by offering choices and opportunities for self-direction. This might involve providing access to resources, information, and programming that align with patrons' interests and needs.
- Cultural, Historical, and Gender Sensitivity: Acknowledging the diverse backgrounds and experiences of patrons is essential in trauma-informed care. Librarians should be mindful of cultural differences, historical trauma, and gender-related issues, striving to create inclusive and affirming spaces for all individuals.
- Reference : Trauma Informed Care Implementation Resource Center
- What is Trauma Informed Care?
- Supporting the Social/Emotional Needs of College Students through Trauma Informed Practice (TIP)
- Building Trauma-Informed Approaches in Higher Education
- Homelessness and Housing Insecurity in Higher Education: A Trauma‐Informed Approach to Research, Policy, and Practice
This video provides an overview of trauma-informed principles and their significance for organizations across various sectors. It distinguishes between "trauma-informed" and "trauma-focused" approaches, while also discussing evolving trends in mental health treatment. Leaders, supervisors, professionals, students, and individuals curious about trauma will benefit from watching this informative presentation.
This lecture from Pasadena City College shares how to implement a trauma informed approach in higher education, the significance of adopting a trauma-informed approach and its potential benefits for students, faculty, and staff within their institution. Additionally, it explores strategies to broaden and strengthen their capacity as a trauma-informed college or university.
The short video aims to engage members of the higher education community in thoughtful conversation about why a trauma-informed approach matters and how it may positively impact students, faculty and staff at their institution of higher education as well as how to expand and enhance their capacity as a trauma-informed college or university.
- << Previous: Videos and Podcasts
- Next: Trauma Informed Pedagogy >>
- Last Updated: Mar 21, 2024 1:54 PM
- URL: https://guides.lib.uw.edu/understanding-trauma
- Infographics
ACEs and Toxic Stress: Frequently Asked Questions
For answers to more frequently asked questions about ACEs, please scroll down below the infographic .

Content in This Guide
Step 1: toxic stress 101.
- : Toxic Stress
- : Toxic Stress Derails Healthy Development
- You Are Here: ACEs and Toxic Stress
Step 2: The Science and Social Causes of Toxic Stress
- : Excessive Stress Disrupts Brain Architecture
- : InBrief: The Science of Neglect
- : Social and Behavioral Determinants of Toxic Stress
Step 3: Preventing and Addressing Toxic Stress
- : Resilience
- : Tackling Toxic Stress
- : Video: What We Can Do About Toxic Stress
What are ACEs?
The term “ACEs” is an acronym for Adverse Childhood Experiences. It originated in a groundbreaking study conducted in 1995 by the Centers for Disease Control and the Kaiser Permanente health care organization in California. In that study, “ACEs” referred to three specific kinds of adversity children faced in the home environment—various forms of physical and emotional abuse, neglect, and household dysfunction. The key findings of dozens of studies using the original ACEs data are: (1) ACEs are quite common, even among a middle-class population: more than two-thirds of the population report experiencing one ACE, and nearly a quarter have experienced three or more. (2) There is a powerful, persistent correlation between the more ACEs experienced and the greater the chance of poor outcomes later in life, including dramatically increased risk of heart disease, diabetes, obesity, depression, substance abuse, smoking, poor academic achievement, time out of work, and early death.
How do ACEs relate to toxic stress?
ACEs research shows the correlation between early adversity and poor outcomes later in life. Toxic stress explains how ACEs ”get under the skin” and trigger biological reactions that lead to those outcomes. In the early 2000s, the National Scientific Council on the Developing Child coined the term “ toxic stress ” to describe extensive, scientific knowledge about the effects of excessive activation of stress response systems on a child’s developing brain, as well as the immune system, metabolic regulatory systems, and cardiovascular system. Experiencing ACEs triggers all of these interacting stress response systems. When a child experiences multiple ACEs over time—especially without supportive relationships with adults to provide buffering protection—the experiences will trigger an excessive and long-lasting stress response, which can have a wear-and-tear effect on the body, like revving a car engine for days or weeks at a time.
Importantly, the Council also expanded its definition of adversity beyond the categories that were the focus of the initial ACE study to include community and systemic causes—such as violence in the child’s community and experiences with racism and chronic poverty—because the body’s stress response does not distinguish between overt threats from inside or outside the home environment, it just recognizes when there is a threat, and goes on high alert.
What is trauma, and how does it connect to ACEs and toxic stress?
While trauma has many definitions, typically in psychology it refers to an experience of serious adversity or terror—or the emotional or psychological response to that experience. Trauma-informed care or services are characterized by an understanding that problematic behaviors may need to be treated as a result of the ACEs or other traumatic experiences someone has had, as opposed to addressing them as simply willful and/or punishable actions.
What can we do to help mitigate the effects of ACEs?
People who have experienced significant adversity (or many ACEs) are not irreparably damaged . There is a spectrum of potential responses to ACEs and their possible chain of developmental harm that can help a person recover from trauma caused by toxic stress.
More ACEs Resources Centers for Disease Control and Prevention : More about the original ACEs study and subsequent research. ACEs Too High : A site focused on news and research around ACEs. Substance Abuse and Mental Health Services Administration : Information on trauma-informed approaches and trauma-specific interventions.
- At the most intensive end of the spectrum are therapeutic interventions, ranging from in-patient treatment to regular sessions with a mental health professional, which are designed specifically to deal with serious trauma.
- Trauma-informed care or practice is less intensive, but affects how practitioners in a range of fields, such as social work, medicine, and education, work with people who have experienced toxic stress, and reflects an awareness of the harm that has occurred and takes that into account. There are also many less-intensive practices that can help individuals reduce the effects of stress—from meditation and breathing exercises, to physical exercise and social supports.
- ACEs-based screening and referral is an increasingly common approach, in which individuals are given an ACE score based on a brief survey of their own personal history of ACEs. This can indicate a general, non-specific sense of increased risk based on population-level probabilities, but it cannot predict accurately how any one individual will fare. In other words, a high ACE score can serve as a rough first screener to identify people who may benefit from services, but it cannot tell you what specifically you are at risk for, nor what to do about it.
- The ideal approach to ACEs is one that prevents the need for all levels of services: by reducing the sources of stress in people’s lives, whether basic needs like food, housing, and diapers, or more entrenched sources of stress, like substance abuse, mental illness, violent relationships, community crime, discrimination, or poverty. Supporting responsive relationships with a parent or caregiver can also help to buffer a child from the effects of stress, and helping children and adults build their core life skills—such as planning, focus, and self-control—can strengthen the building blocks of resilience. These three principles— reducing stress, building responsive relationships, and strengthening life skills —are the best way to prevent the long-term effects of ACEs.
Full Text of the Graphic
“ACEs” stands for “Adverse Childhood Experiences.” These experiences can include things like physical and emotional abuse, neglect, caregiver mental illness, and household violence.
The more ACEs a child experiences, the more likely he or she is to suffer from things like heart disease and diabetes, poor academic achievement, and substance abuse later in life.
Toxic Stress Explains How ACEs “Get Under the Skin.”
Experiencing many ACEs, as well as things like racism and community violence, without supportive adults, can cause what’s known as toxic stress . This excessive activation of the stress response system can lead to long-lasting wear-and-tear on the body and brain.
The effect would be similar to revving a car engine for days or weeks at a time.
We Can Reduce the Effects of ACEs and Toxic Stress.
For those who have experienced ACEs, there are a range of possible responses that can help, including therapeutic sessions with mental health professionals, meditation, physical exercise, spending time in nature, and many others.
The ideal approach, however, is to prevent the need for these responses by reducing the sources of stress in people’s lives. This can happen by helping to meet their basic needs or providing other services.
Likewise, fostering strong, responsive relationships between children and their caregivers, and helping children and adults build core life skills , can help to buffer a child from the effects of toxic stress .
ACEs affect people at all income and social levels, and can have serious, costly impact across the lifespan. No one who’s experienced significant adversity (or many ACEs) is irreparably damaged, though we need to acknowledge trauma’s effects on their lives. By reducing families’ sources of stress, providing children and adults with responsive relationships, and strengthening the core life skills we all need to adapt and thrive, we can prevent and counteract lasting harm .
Related Topics: toxic stress
Explore related resources.
- Reports & Working Papers
- Tools & Guides
- Presentations

Videos : Toxic Stress Derails Healthy Development

Reports & Working Papers : From Best Practices to Breakthrough Impacts

Videos : InBrief: The Science of Neglect

Reports & Working Papers : The Science of Neglect: The Persistent Absence of Responsive Care Disrupts the Developing Brain

Reports & Working Papers : Excessive Stress Disrupts the Architecture of the Developing Brain
Reports & Working Papers : A Science-Based Framework for Early Childhood Policy

Podcasts : About The Brain Architects Podcast

Briefs : Health and Learning Are Deeply Interconnected in the Body: An Action Guide for Policymakers

Videos : How Early Childhood Experiences Affect Lifelong Health and Learning

Briefs : InBrief: Applying the Science of Child Development in Child Welfare Systems

Briefs : InBrief: The Science of Early Childhood Development

Briefs : InBrief: The Impact of Early Adversity on Children’s Development

Videos : InBrief: The Impact of Early Adversity on Children’s Development

Presentations : PBS NewsHour Q&A: Childhood Trauma and COVID-19

Reports & Working Papers : Persistent Fear and Anxiety Can Affect Young Children’s Learning and Development

Videos : Child Development Core Story

Infographics : How Racism Can Affect Child Development

Videos : Science X Design: Three Principles to Improve Outcomes for Children

Presentations : Social and Behavioral Determinants of Toxic Stress

Videos : Stress and Resilience: How Toxic Stress Affects Us, and What We Can Do About It

Podcasts : The Brain Architects Podcast: COVID-19 Special Edition: A Different World

Podcasts : The Brain Architects Podcast: COVID-19 Special Edition: Creating Communities of Opportunity

Podcasts : The Brain Architects Podcast: COVID-19 Special Edition: How Do We Rebuild and Re-Envision Early Childhood Services?

Podcasts : The Brain Architects Podcast: Toxic Stress: Protecting the Foundation
Reports & Working Papers : The Science of Early Childhood Development: Closing the Gap Between What We Know and What We Do

Partner Resources : The Toxic Stress of Early Childhood Adversity: Rethinking Health and Education Policy
Videos : Three Core Concepts in Early Development

Tools & Guides , Partner Resources : Training Module: “Build My Brain”

Infographics : What Is COVID-19? And How Does It Relate to Child Development?

Infographics : What Is Inflammation? And Why Does it Matter for Child Development?
How to Incorporate Trauma-Informed Care Into Clinical Care
Tips to help patients feel safe, included, and understood.
Many patients have experienced some form of trauma, which can have lasting adverse effects on physical and mental health. Adopting a trauma-informed care (TIC) approach is integral to improving health outcomes and creating better patient-provider relationships.
“Trauma-informed care is really about creating a space where every person, including people who have experienced trauma, feel safe, feel included, and feel understood as a whole person,” says Stephanie Hargrove, PhD , clinical psychologist and assistant professor at Duke. A comprehensive approach must include making changes at all levels within a health care practice, including nonclinical staff, who have significant interactions with patients and are critical to ensuring patients feel safe.
Below, Hargrove shares tips, based on six core principles of TIC developed by the Substance Abuse and Mental Health Services Administration, for how providers can incorporate TIC into their organization’s clinical practices and policies.
1. Safety Creating a safe environment begins in the waiting area. A respectful and welcoming environment might feature a rainbow flag denoting the clinic is proud to serve the LGBTQ+ community, with literature and signage available in multiple languages, as well as accessibility options for patients with disabilities.
2. Trustworthiness and transparency “Give clear directions of where people should go and who they should talk to,” Hargrove says. “Make it so that patients know what’s happening and feel they have a choice in what’s going on.” Explain to patients what to expect before, during, and after the exam.
3. Collaboration and mutuality Ensure patients feel they are part of the decision-making process. “Inviting patients to ask questions, and asking questions to learn about what they’ve already tried to do to address their health issues balances out the power dynamic between providers and patient,” Hargrove says.
4. Collaboration and mutuality Ensure patients feel they are part of the decision-making process. “Inviting patients to ask questions, and asking questions to learn about what they’ve already tried to do to address their health issues balances out the power dynamic between providers and patients,” Hargrove says.
5. Empowerment and choice Inform patients that everything that happens during an exam is within their control, and they can consent and opt out at any time. Offer alternatives if they feel uncomfortable with some treatment options, and allow patients to tell you what makes them comfortable.
6. Cultural, historical, and gender issues “People coming from diverse backgrounds might have had traumatic experiences in hospital systems,” Hargrove says. Patients may need more support when interacting with health care systems that have historically harmed people from similar backgrounds. Including a family member in the visit might help patients feel more comfortable.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

“What Does it Mean to be Trauma-Informed?”: A Mixed-Methods Study of a Trauma-Informed Community Initiative
Robey b. champine.
1 Division of Public Health, Michigan State University College of Human Medicine, Flint, MI 48502 USA
2 Division of Prevention and Community Research, Yale School of Medicine, New Haven, CT 06511 USA
Erin E. Hoffman
3 College of Science and Health, Department of Psychology, DePaul University, Chicago, IL 60604 USA
Samantha L. Matlin
4 The Scattergood Foundation, 1501 Cherry Street, Philadelphia, PA 19102 USA
Michael J. Strambler
Jacob kraemer tebes.
Trauma during childhood has the potential to adversely affect one’s physical, cognitive, emotional, and social development across the life span. However, the adverse effects of trauma can be prevented and mitigated through holistic services and supports that are trauma-informed. The Pottstown Trauma-Informed Community Connection (PTICC) is a community-based initiative that aims to build a trauma-informed community through training diverse stakeholders (e.g., school staff, providers, community leaders, parents) on the potential signs and symptoms of child trauma and how to create safe physical and emotional environments for children and families. This paper presents findings from a mixed-methods study of education and community partners’ ( N = 82) experiences in PTICC and their understandings of what it means to become trauma-informed. Paired sample t -tests found significant changes in participants’ beliefs about trauma-informed practice, but there were no changes in participants’ perceptions of the impacts of PTICC on their use of trauma-informed practices and supports. Focus groups with education ( n = 6) and community ( n = 5) partners found that participants regarded being “trauma-informed” as reframing one’s perspective, being more self-reflective, acquiring skills to respond more effectively to others who have experienced trauma, and having a sense of hope for the future. Findings also revealed perceived benefits of trauma training and challenges associated with getting others to buy-in to trauma-informed work. Potential methodological considerations for future community-engaged research in building trauma-informed communities are discussed. These considerations include the need to address ceiling effects, disaggregate data, and mitigate challenges associated with participant engagement.
- The adverse effects of trauma can be prevented and mitigated through holistic services that are trauma-informed.
- Participation in PTICC was linked to enhanced understanding of what it means to be “trauma-informed”.
- This mixed-methods study raised methodological considerations for future research in building trauma-informed communities.
Experiences of trauma are ubiquitous and linked to a host of adverse health outcomes across the life span, including chronic diseases, depression, and substance use (Chang et al., 2020 ; Sowder et al., 2018 ). Approximately one half of all U.S. adults report at least one traumatic event in their lives (National Institute of Mental Health [NIMH], 2017 ), and more than two thirds of children report at least one adverse childhood experience (ACE) by the age of 16 (Substance Abuse and Mental Health Services Administration [SAMHSA], 2020 ). Trauma, including traumatic stress, is defined as an event, series of events, or set of circumstances that an individual or group experiences as physically and/or emotionally harmful (SAMHSA, 2014 ). These events and circumstances include poverty, violence, discrimination, homelessness, natural disasters, and, as underscored by Coronavirus Disease 2019 (COVID-19), pandemics (Bridgland et al., 2021 ; Krystal et al., 2021 ; SAMHSA, 2014 ). Trauma disproportionately burdens populations of color, indigenous communities, and members of sexual minority groups, thus necessitating a trauma-informed social justice response (SAMHSA 2014 ; Scheer and Poteat, 2018 ; Stolbach & Anam, 2017 ).
Adopting a Multilevel Trauma-Informed Approach
The adverse effects of trauma can be prevented and mitigated through holistic services and supports that are trauma-informed and fit diverse clinical, organizational, and community settings (Middleton et al., 2019 ; Temkin et al., 2020 ). A trauma-informed approach is characterized by a realization of the widespread impacts of trauma and various pathways to recovery; the recognition that experiences of trauma may be accompanied by specific signs and symptoms; a comprehensive and integrative response; and efforts to prevent re-traumatization (Harris & Fallot, 2001 ; SAMHSA, 2014 ; Tebes et al., 2019 ). This approach emphasizes safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment, voice, and choice; and addresses cultural, historical, and gender issues (SAMHSA, 2014 ).
Of note, there are different ways in which scholars have conceptualized trauma-informed work across disciplines. “Trauma-specific services” are interventions that seek to address trauma symptoms or other responses individuals and groups have after they have experienced a trauma (e.g., Trauma-Focused Cognitive Behavioral Therapy [TF-CBT)] (DeCandia et al., 2014 ). In contrast, “trauma-informed care” refers to a universal framework that involves making changes to programs, policies, and practices to understand, identify, and address trauma (DeCandia et al., 2014 ; Hanson et al., 2018 ). These efforts include workforce development (e.g., training staff to understand trauma and its potential impacts), the delivery of evidence-based trauma-focused services, and organizational practices (e.g., promoting a culture of safety, enhanced collaboration) (Hanson et al., 2018 ). These practices can collectively be viewed as representing a trauma-informed approach that encompasses awareness, understanding, and action (Hanson et al., 2018 ). As described by Hanson et al., ( 2018 ), being “trauma-informed” can take different forms depending on a person’s role (e.g., teacher, service provider, law enforcement professional, parent). Consistent with this work, scholarship has emphasized the need for a trauma-informed approach that is multilevel and prioritizes population health through prevention and promotion programs, policies, and practices, given the pervasive nature of trauma and its potentially harmful impacts on individuals, groups, and communities (Magruder et al., 2017 ; Matlin et al., 2019 ; Tebes et al., 2019 ).
Matlin et al. ( 2019 ) proposed a three-dimensional model that presents different components of trauma-informed practice. The model differentiates between two types of approaches that at a practice can adopt: treatment/healing or prevention/promotion, consistent with previous research on the use of risk prevention and health promotion approaches to trauma (Bloom, 2013 ; Matlin et al., 2019 ). Whereas a treatment/healing approach is focused on reducing signs and symptoms of distress in the aftermath of a traumatic event, a program, policy, or practice that adopts a prevention/promotion approach seeks to reduce the likelihood of a disruption from occurring in the first place following a traumatic event (Matlin et al., 2019 ). Next, the model specifies the socio-ecological level at which such efforts can be directed: individual (e.g., personal attitudes, beliefs, behaviors), relational (e.g., family, couple, peer), organizational (e.g., schools, workplaces, neighborhoods), or community/system (e.g., cities, towns, child welfare and educational systems) (Matlin et al., 2019 ). Finally, the model specifies the intervention target of such efforts. Whereas trauma-specific efforts target individuals and groups who have experienced trauma (e.g., trauma-specific services), universal interventions emphasize providing trauma-informed care to all individuals in a setting or population (e.g., school district). This model elucidates a range of responses to adversity, with priority given to universal interventions that emphasize risk reduction and health promotion and are implemented at the community/systems level; these interventions offer the greatest potential for population health impact (Bloom, 2013 ; Matlin et al., 2019 ; Tebes et al., 2019 ). The intervention presented in this article, the Pottstown Trauma-Informed Community Connection (PTICC) ( n.d. ), is an example of such a universal intervention, as it engaged parents, teachers, providers, and leaders throughout a community in efforts to understand childhood trauma and its widespread effects and how to implement programs, polices, and practices that aim to prevent risk and promote health.
Trauma-Informed Community-Based Interventions
A growing body of research has examined the processes involved in building a community’s capacity for trauma-informed practice by expanding existing work on therapeutic communities (Arnold et al., 2020 ; Báez et al., 2019 ; Longhi et al., 2019 ; Matlin et al., 2019 ; Pinderhughes et al., 2015 ; Tebes et al., 2019 ). The Sanctuary Model (Esaki et al., 2013 ) is a trauma-informed organizational change intervention based on the concept of therapeutic communities. These communities emphasize active and collective participation among stakeholders in creating a system of healing (Esaki et al., 2013 ). The Sanctuary Model is a blueprint for promoting positive clinical and organizational change that promotes safety and recovery through the creation of a trauma-informed community (Esaki et al., 2013 ).
The Children’s Resilience Initiative (CRI) in Walla Walla, Washington
The CRI was launched in 2010 with the following goals: to educate the community of Walla Walla, Washington about ACEs and the science of brain development and to build community resilience (SAMHSA, 2017 ). This initiative involved engaging a coalition with community residents and stakeholders (e.g., schools, city government, law enforcement, health and social service providers) to identify their needs and challenges, increase public awareness of childhood trauma, and reshape programs, policies, and practices to be trauma-informed (SAMHSA 2017 ). Evaluation findings indicated that, in one high-school, after trauma-informed practices were implemented, students demonstrated increased resilience and academic achievement (SAMHSA, 2017 ). In addition, school disciplinary policies were transformed to emphasize student self-regulation practices, and teachers became more attuned to potential underlying causes of student problem behaviors (SAMHSA, 2017 ). Teams were also trained to help ensure the sustainability of CRI (SAMHSA, 2017 ). In short, this initiative was grounded in the principles of a trauma-informed approach and, through its emphasis on community empowerment, helped to promote positive and sustained community-wide change (SAMHSA, 2017 ).
Pottstown Trauma-Informed Community Connection (PTICC)
The authors of this article were actively involved in the development, implementation, and evaluation of another community-based, trauma-informed initiative known as PTICC, which is the focus of the analyses presented herein. This initiative began in 2014, following the creation of the Pottstown Trauma Task Force, which consisted of representatives including early childhood providers, law enforcement officials, members of the faith community, and behavioral health and social service providers from the community of Pottstown, PA (see Matlin et al., 2019 for a more detailed description). The Task Force partnered with outside researchers and consultants and used an ongoing participatory process to conceptualize, implement, and translate PTICC (Matlin et al., 2019 ). The primary goal of this initiative was to build a trauma-informed community through training diverse stakeholders in the potential signs and symptoms of child trauma and how to create safe physical and emotional environments for children and families (PTICC Website, n.d.).
PTICC activities were guided by three work groups focused on building capacity in the following areas: education and training, communications, and networking (Matlin et al., 2019 ). Social and emotional learning (SEL) curricula were embedded within the Pottstown School District to strengthen children’s competencies in self-regulation and to engage families (Matlin et al., 2019 ). SEL is focused on cultivating self-awareness, self-management, responsible decision-making, healthy relationship skills, and social awareness among students Collaborative for Academic, Social, and Emotional Learning (CASEL, 2021 ). In PTICC, SEL curricula were aligned with trauma-informed principles in support of the community initiative (Sichel et al., 2021 ).
PTICC participants were invited to complete trainings on ACEs, trauma, trauma-informed practice, SEL, and resilience (Matlin et al., 2019 ). During the initial phase of this initiative, a key objective was to enhance beliefs favorable to the use of trauma-informed practice; changes in the services network and related system supports for trauma-informed practice would be introduced once key community stakeholders, such as education and community service providers, were trained. Early findings suggested that PTICC helped to enhance participants’ knowledge about trauma-informed practice, which was essential to building a trauma-informed community (Matlin et al., 2019 ). One of the measures used was the Attitudes Related to Trauma-Informed Care (ARTIC) Scale (Baker et al., 2016 ), which was based on an earlier measure developed to evaluate a staff trauma training model. The items were derived from key stakeholder feedback, expert opinions, and scholarly literature (Baker et al., 2016 ). The new measure has been validated with human health and service providers and school-based staff (Baker et al., 2016 , 2021 ) and is an efficient and cost-effective measure of attitudes toward trauma-informed care.
Methodological Challenges Associated with Community-Based Research
Despite the community-wide benefits associated with the implementation of initiatives such as CRI and PTICC that aim to reduce adverse outcomes linked to ACEs and foster resilience, challenges exist in how to account for the dynamic impacts of such work on stakeholders. As noted by Longhi et al. ( 2019 ) in their assessment of the capacity building strategies used in Walla Walla, WA, too many factors may be at play to be easily measured and controlled in evaluations of such complex community initiatives in which “system changes rarely follow a logical sequential set of linear causal steps” (p. 15). In addition, non-experimental studies preclude inferences of causality, making it difficult to understand the impacts of complex initiatives on primary stakeholders (Longhi et al., 2019 ).
Other methodological considerations include the issue of ceiling effects, or when a high proportion of participants have maximum scores on the observed variable(s). The abilities of quantitative measures may be limited by their lack of variability and sensitivity and insufficient range of measurement, resulting in skewed scores (Andrew et al., 2011 ; McBee, 2010 ). Ceiling effects are often observed in the use of participant satisfaction scales (Andrew et al., 2011 ). It is feasible that community stakeholders who are committed to the values of trauma-informed practice and their enhancement at the onset of an intervention may not show meaningful growth on quantitative assessments of such a commitment over time because they had moderate to high average scores at the onset.
Benefits of mixed-methods research
Mixed-methods research can help to offset potential limitations associated with the use of quantitative measures (e.g., ceiling effects; Andrew et al., 2011 ). These methods involve collecting and analyzing qualitative and quantitative data within the same study, often from the same data sources (Creswell, 2009 ). Integrating qualitative and quantitative methodologies allows one method to clarify the other and can generate rich responses that complement or expand on quantitative findings (Aresi et al., 2017 ), or help explain them (Tebes and Kraemer 1991 ). For example, interviews or focus groups can provide insight into educators’ successes and challenges in implementing trauma-informed practices. Mixed-methods approaches are useful in assessing initiatives that involve multilevel systems (Wisdom & Creswell, 2013 ) and can provide a nuanced understanding of how initiatives impact the community by triangulating data across sources and participant groups (Aresi et al., 2017 ). Scholars have recently called for more mixed-methods research to better understand trauma-informed practices and contextual factors that influence their implementation (Mihelicova et al., 2018 ).
Present Study
The purpose of this study was to contribute to the growing research on trauma-informed communities by examining the views and experiences of two stakeholder groups involved in PTICC. As noted earlier, PTICC is a multilevel systems intervention that used a participatory process to build a trauma-informed community in Pottstown, PA. This three-year initiative engaged youth, families, community leaders, and representatives from various service sectors (e.g., education, health care, law enforcement) in trainings and activities to enhance their understandings of ACEs, trauma, trauma-informed practice, SEL, and resilience, and how to effectively respond to signs of traumatic stress, prevent further traumatization, and promote thriving. See Matlin et al. ( 2019 ) for a description of the PTICC implementation process and overall preliminary findings.
In this study, survey and focus group data from two specific groups of stakeholders (i.e., education and community partners) were analyzed to address the following research questions:
- Did participants show increased favorable beliefs toward trauma-informed practice?
- Did participants show increased favorable perceptions of the impacts of PTICC on their day-to-day use of trauma-informed practices and supports in the previous six months?
- Based on analysis of focus group data, how did the groups describe the perceived impacts of PTICC? What were the similarities and differences between groups?
- Based on analysis of the survey and focus group data together, what were the areas of convergence and divergence in participants’ trauma-informed beliefs and perceived impacts of PTICC?
This sample was derived from a longitudinal evaluation of a larger multilevel trauma-informed initiative that was conducted between 2016 and 2019 in partnership with the community of Pottstown, Pennsylvania. Only the method and results relevant to this study are presented.
Participants
Survey participants.
A total of 96 participants completed at least one survey over the course of the study. However, of these participants, 14 were excluded from the present analysis, given that they represented professional sectors that fell outside the categories of interest (i.e., arts, sports, and leisure; family; and religious) because they did not comprise a large proportion of the sample, resulting in a total of 82 participants. Of these 82 participants, 63 (76.8%) were community partners from sectors in areas including business and philanthropy; government and law enforcement; health care; and social services. In addition, 19 (23.2%) participants were staff from the Pottstown School District or outside organizations that provided educational services to children and families. Individual demographic data on participants were not collected, a limitation that is described in the Discussion section. Of the 82 participants, 50 provided survey data at more than one time point; 39 (78.0%) were community partners; and 11 (22.0%) were education partners.
Focus Group Participants
Convenience samples of school district staff and community partners were recruited to participate in two focus groups. A sample of parents/caregivers was also recruited to participate; however, given the small sample ( n = 3) and limited survey data from this group, these data were excluded from this analysis. Members of the PTICC Steering Committee (including parents, community leaders, educators, providers) spread the word to PTICC participants about the opportunity to participate in focus groups and provided those interested with contact information for the researchers. Immediately prior to the focus groups, demographic information was collected from all participants using a brief questionnaire that was developed for the present study. One group of participants included community partners ( n = 5, Age Range = 20 to 59 years) who worked in the fields of mental health, social services, and criminal justice. All partners (100%) identified as female and as non-Latinx. The majority of participants (80.0%) identified as White or European American.
The second group consisted of Pottstown School District staff ( n = 6, Age Range = 20 to 49 years), including principals. Half (50.0%) of the sample was female, and all staff identified as non-Latinx (100%). In addition, half (50.0%) identified as White or European American and the other half as Black or African American.
Individuals who attended at least one in-person PTICC meeting were invited to complete an online Semi-Annual Survey. Participants received an email link via Qualtrics to complete a 55-item survey that asked them about their current trauma-related knowledge, beliefs, and prior training and to report on their perceived impacts of PTICC on their behaviors in the previous six months. Over the course of the study, three surveys were administered across successive six-month periods (Time 1: January – June 2017; Time 2: July – December 2017; and Time 3: January – June 2018). Each survey took about 20 min to complete and participants received a $10 gift card.
In December 2017, the focus groups were co-facilitated by the first, second, and third authors who used semi-structured protocols. The focus groups were conducted in a school conference room during the day and in the evening to accommodate participants’ schedules. Participants signed assent forms immediately prior to participating. Each group took approximately 45 min to complete and food was provided to thank participants for their time. The groups were audio-recorded and transcribed by trained researchers. This study was approved by the University’s Institutional Review Board and all participants provided informed consent.
Survey Measures
The semi-annual survey consisted of several scales that were analyzed in this study and are summarized below.
Trauma-Informed Practice Beliefs
Participants completed an adapted version of the ten-item Attitudes Related to Trauma-Informed Practice (ARTIC-10; Baker et al., 2016 ) scale and the five-item ARTIC-System Support subscale (Baker et al., 2016 ). Each item consisted of two statements that reflected more and less favorable beliefs toward trauma-informed practice. Participants indicated their beliefs by using a seven-point, Likert-type scale that reflected their belief at work in the past two months. Items included “Individuals I serve could act better if they really wanted to” versus “Individuals I serve are doing the best they can with the skills they have,” and “Ups and downs are part of my work, so I don’t take it personally” versus “The unpredictability and intensity of my work makes me think I’m not fit for this job.” Items were recoded, as appropriate, and an overall mean score was calculated, such that higher scores indicated more favorable beliefs toward trauma-informed practice. Scores showed adequate reliability: Time 1 (α = 0.77), Time 2 (α = 0.76), and Time 3 (α = 0.77).
Trauma-Informed Practice System Supports
The ARTIC-System Support (ARTIC-SS) subscale (Baker et al., 2016 ) consisted of five items that used the same response rubric as the ARTIC-10. Items assessed participants’ views of support they received in their workplaces for implementing trauma-informed practice. Items included “I have the support I need to work in a trauma-informed way” versus “My organization/group talks about trauma-informed practice, but it is really business as usual,” and “I do not have enough support to implement trauma-informed practice” versus “I have enough support to implement trauma-informed practice.” Items were recoded, as appropriate, and an overall mean score was calculated, such that higher scores indicated more perceived organizational support for trauma-informed practice. Scores showed adequate reliability: Time 1 (α = 0.76), Time 2 (α = 0.79), and Time 3 (α = 0.73).
Perceived Use of Trauma-Informed Practices and Supports
Participants completed a six-item scale developed for use in this study that asked them to indicate to what extent PTICC influenced their use of trauma-informed practices and supports in the previous six months. The items were scored on a five-point, Likert-type scale, ranging from 1 (Not at all) to 5 (A great deal). An overall mean score was calculated, with higher scores indicating more favorable perceptions of PTICC’s influences on their use of trauma-informed practices and supports. Items assessed self-perceived changes in respondents’ knowledge of trauma (e.g., “To what extent have PTICC’s efforts… improved your knowledge about trauma, ACEs, resilience, and healthy development?”) and relevant actions (e.g., …increased your application of trauma-informed and adverse childhood experiences (ACEs) concepts in your work?). These items are consistent with the elements of a trauma-informed approach described in the Introduction section, which reflect knowledge and action (Hanson et al., 2018 ). Scores showed adequate reliability: Time 1 (α = 0.88), Time 2 (α = 0.85), and Time 3 (α = 0.82).
Focus Group Protocols
The protocols were developed for this study and included eight questions that asked participants about their experiences in the initiative and its perceived impacts on their trauma-related knowledge, attitudes, and skills. Questions included “Please tell us how you got involved in PTICC,” “What types of training or educational experiences have you participated in through your work or through PTICC about childhood trauma or adverse childhood experiences?,” “What does it mean to you to be ‘trauma-informed’?,” and “How, if at all, has participating in PTICC changed how you work as a professional?”
Analytic Strategy
Descriptive statistics were tabulated for all of the quantitative measures. Given the relatively small sample of participants representing the Education sector ( n = 19), no between-group analyses were conducted. Instead, paired sample t -tests were used to assess potential overall changes in participant scores on the ARTIC-10, ARTIC-SS, and Perceived Use of Trauma-Informed Practices and Supports measures. Each participant was assigned a unique Participant ID that allowed us to track their longitudinal data. The data were analyzed using IBM SPSS Statistics Version 26 software.
In regard to the focus group data, the first and second authors conducted thematic analysis (TA; Braun & Clarke, 2006 ) of participants’ responses to assess their PTICC-related views and experiences. This method is appropriate for identifying and describing patterns or themes that emerge in qualitative data and for exploring an array of questions using inductive or deductive approaches (Braun & Clarke, 2006 ). First, the authors fully immersed themselves in the data by independently reading and re-reading each transcript and making notes of themes that they observed. Next, they discussed their findings and transformed the themes into an initial set of codes that they summarized in separate codebooks for each participant group. Using the codebooks, they independently coded the transcripts and met to resolve any discrepancies in their coding decisions. Kappa coefficients indicated adequate interrater reliability: 0.82 for community partners and 0.77 for education partners. The data were analyzed using NVivo Version 12 software.
Quantitative Findings
Table Table1 1 summarizes descriptive statistics (overall and by participant group) for the following measures: ARTIC-10, ARTIC-SS, and Perceived Use of Trauma-Informed Practices and Supports. As shown in the table, participants had moderate to high average scores on the three measures across the three time points.
Descriptive statistics for ARTIC-10, ARTIC-SS, and perceived use of trauma-informed practices and supports by sample ( n = 82)
Note . ARTIC Attitudes Related to Trauma-Informed Care, PTICC Pottstown Trauma-Informed Community Connection
Changes in Beliefs Toward Trauma-Informed Practice
A series of paired sample t -tests examined whether, in the overall sample, there were significant changes in participants’ beliefs about trauma-informed practice, as measured by the ARTIC-10. Results are summarized in Table Table2 2 .
Paired sample t-tests examining changes in ARTIC-10, ARTIC-SS, and perceived use of trauma-informed practices and supports
Note . ARTIC Attitudes Related to Trauma-Informed Care, PTICC Pottstown Trauma-Informed Community Connection.
From Time 1 to Time 2, there was a significant decrease in trauma-informed beliefs. However, from Time 2 to Time 3, there was a significant increase in participants’ trauma-informed beliefs. There was also a significant increase in belief scores from Time 1 to Time 3.
Changes in Trauma-Informed Practice Beliefs about Systems Supports
Although no changes were expected in beliefs about trauma-informed practice related to systems supports so early in this initiative, we examined these data to gauge their empirical relationship to beliefs about trauma-informed practice. In contrast to evidence of changes in beliefs about the use of trauma-informed practice, there was no significant increase in participants’ perceptions of system supports for trauma-informed practice on the ARTIC-SS.
Changes in Perceived Use of Trauma-Informed Practices and Supports
A series of paired sample t -tests examined whether, in the overall sample, there were significant changes in participants’ perceptions of their use of trauma-informed practices and supports in the previous six months. As shown in Table Table2, 2 , findings indicated no significant changes from Time 1 to Time 2, from Time 2 to Time 3, or from Time 1 to Time 3.
Focus Group Findings
Participants in both focus groups offered thoughtful observations about their PTICC involvement, what it had meant to them thus far, and challenges of becoming trauma-informed. Four overarching themes emerged from the focus groups. First, and perhaps most important, education and community partners shared details about what it meant to them to be trauma-informed. Second, focus group participants described how becoming trauma-informed cultivated hope for the future. Third, many described benefits of trauma-related training through PTICC, but also the need for increased and ongoing training. And finally, participants spoke of the challenges of getting buy-in from various groups for a trauma-informed perspective. These findings are summarized in Table Table3 3 and are described in detail below.
Summary of findings from focus groups with community partners ( n = 5) and pottstown school district staff ( n = 6)
What It Means to Become Trauma-Informed
Focus group participants were most engaged when describing what it meant to be trauma-informed, and identified three components: (1) a shift in their perspective to include greater awareness and understanding of the potential signs of traumatic stress among children and adults; (2) a deeper understanding of their own adverse experiences, especially as children, that prompted reflection on how their own adverse experiences may have impacted their thoughts and interactions later in life; and (3) acquisition of skills and behaviors of how to thoughtfully respond to trauma in the context of their work or family.
Trauma-informed means…reframing one’s perspective
For many, becoming trauma-informed meant reframing one’s perspective on the world in critical ways. As one community partner stated:
I think [trauma-informed] means looking at a person and the people around them and the community in a very different lens. It’s so absolutely important to see, you know, the whole… ‘What’s wrong with you?’ How many times did we say that for a long time? Just reframing that and recognizing relationships.
Similarly, one school staff member described how being trauma-informed involved “looking below the surface”:
…when you’re looking at things through a trauma lens, you’re not just looking at immediately what’s in front of you. Like I love that iceberg illustration…you’re looking at all of those things that are under the surface and those things that aren’t around that add to the current state…
Community and education partners provided numerous examples of how they experienced (or witnessed in others) transformations in understanding trauma and its potential impacts on children’s development. For instance, as noted by a community partner, “…I think by informing the families, I think this initiative is helping the families understand [trauma] and the teachers understand it.” Similarly, as two school staff members stated: “[The initiative] really gives me an opportunity to build on past knowledge and to really grow and learn new things” and
I’ve learned from these children that they do have a lot of stuff going on at home and they freely tell me sometimes and that helps me to kind of put that lens on that says ‘Okay, this is stuff that they’re going through that’s going to have an impact on the behaviors that they’re having at school…so let me realize that when I’m speaking to them…
As each of these examples illustrates, becoming trauma-informed involves opening a new window on the world, what one called a “trauma lens,” that makes it difficult to return to previous personal and professional ways. This perspective includes a new language, shared by others who were trauma-informed, about what was newly visible for the first time.
Trauma-informed means…being more self-reflective
Community and education partners also indicated that being “trauma-informed” meant reflecting internally on how their own adverse experiences may have impacted their thoughts and interactions. One community partner described her experiences in PTICC as therapeutic: “It’s almost been like a therapy for me, from stuff experienced in childhood, stuff experienced as an adult…” Similarly, as one school staff member stated when speaking about her own trauma experience in childhood: “I think that being able to understand how it actually did affect me and how [it may affect someone] whose had multiple experiences with something, that’s significant.”
The reflection among focus group participants that was prompted by describing what it meant to be trauma-informed was quite common, suggesting that becoming trauma-informed can have both unintended positive and negative effects. Clearly, reflection on one’s own traumatic experiences can trigger painful memories or a sense of loss due to the experience, but it can also foster greater understanding and empathy of others who may have experienced trauma.
Trauma-informed means…acquiring skills to respond more effectively to others who have experienced trauma
School and community partners each described how PTICC helped them acquire skills and behaviors to respond more effectively to others, at work or in their family, who have experienced trauma. For example, several school staff described positive changes in teachers’ reactions to problematic student behaviors. As one participant said:
…most of the lessons and the things that they talk about usually were happening moments after [an incident] had happened…where now,…teachers are teaching [the lesson] ahead of time and exposing students to it in the hopes that it’s reinforcing when life presents itself…
Other participants also noted how the initiative positively impacted their own parenting practices. As one person said, “[the training] helps me to be more aware as a parent in addition to what I’m doing with my work…”
A Sense of Hope for the Future
A sentiment shared by individuals in the community partners group, with which all others agreed, was that the community partner meetings cultivated a sense of hope for the future. If, as noted above, becoming trauma-informed includes acquiring a deeper understanding of what it means to experience trauma and respond to it that is informed through self-reflection, it is not surprising that becoming trauma-informed can help cultivate a sense of hope for the future. One participant described how PTICC provided her with an underlying sense of hope that she, in collaboration with others, could help to improve the lives of individuals affected by trauma. In particular, she linked this favorable aspect of the initiative to the community engagement efforts, noting:
I found that the community partners meetings are…energizing. For me, there’s a hope factor. A lot of the work that I’ve done…doesn’t have a lot of hope. So, I think part of it, for me, is that [the initiative] offers…a hope factor…that’s tangible.
Perceived Benefits of Trauma-Related Training
Participants in both groups identified the trauma-related training they received through PTICC as critical to becoming trauma-informed. One school staff member reflected on how the training appeared to be a useful tool for parents:
…what I found (is)… they’re finding [the training] really helpful because what it has done is it’s giving them insight not only into their child but also their own upbringing. And so it provides a tool that they would not have otherwise had.
In addition, as one parent shared, “I heard about ACEs and stuff like that at school, but it was super skated over. Your presentation gave me more than the school’s, than like in college.”
Participants in both groups also emphasized the need for more trainings and resources to enhance their own trauma-related knowledge and skills or those of others. Community partners described challenges associated with translating the more clinical-oriented trauma training that they received to individuals from non-clinical backgrounds. As one partner stated:
…aside from the mental health training that has happened, which I think is beneficial, but I’d like to see more, it’s hard because I’m trained in trauma as a clinician, but then giving it to people who aren’t…I don’t know. I don’t know if there can be something…not a better training, because I think it was good, but something a little bit stronger.
Similarly, school staff discussed the need for more training targeted toward their teachers to aid them in actively applying what they learned. According to one school staff member:
…[the teachers] understand trauma…they understand why it’s important, but…at least I feel like in our building, we’re in the phase now of moving from ‘Okay, we understand it’ to making sure that we’re putting it into practice…
Challenges in Getting Others to “Buy-In”
Both groups of focus group participants noted challenges in getting other adults to buy in to trauma-related training and activities, and their potential benefits. School staff described how some parents of their students took offense to training provided to their children in how to handle stressful and potentially traumatic situations. For instance, as one participant said, “…some parents were saying ‘Well, you know, you’re coming into my house, telling me how to raise my kid.” School staff also discussed broader challenges associated with getting parents actively involved in PTICC. For instance:
I think we can always do more to engage parents and it’s just always a challenge because, as we all know, the parents that we really want to get out and get the message to are not the ones that come out for a whole variety of reasons…
Similar challenges were described by school staff in the varied responses of parents to trauma-informed practices taking place in the schools:
…you have this group of parents that really love it and embrace it because it’s like ‘Oh wow, my kid’s coming home and he’s saying these things to me so I know that it’s going throughout the school,’ but then you have the other parents who take that firm stance ‘Let me tell you something, son… This is my house and we’re gonna follow my rules.’ So that’s where there’s a little bit of conflict in it.
Comparison of Survey and Focus Group Findings
Analysis of the survey data found relatively favorable scores on participants’ beliefs about trauma-informed practice and their perceived impacts of PTICC on their behaviors. These findings are largely in alignment with the positive PTICC-related experiences described by participants in the focus groups. In the focus groups, although both groups described positive experiences, the school staff cited more concrete examples of how PTICC appeared to positively impact students, parents, and themselves (in their roles as both educators and as parents).
Based on the survey data, between Time 1 and Time 2, participants showed a significant decrease in their favorable beliefs about trauma-informed practice. This finding conflicts, in part, with feedback from the focus groups. Both groups described how the PTICC trainings enhanced their understandings of ACEs, how to recognize the signs and symptoms of child traumatic stress, and effectively respond. However, based on the survey data, favorable beliefs appeared to improve with time, as PTICC progressed. Focus group data still helped to elucidate some intervention-related challenges that occurred during this time. For instance, both groups cited the need for more training in how to apply what they were learning to different scenarios. Perhaps these limitations of the training contributed to a decline in participants’ endorsement of trauma-informed beliefs during the first half of the intervention.
This study aimed to enhance understanding of the experiences of two key stakeholder groups, education and community partners, involved in a community-based trauma-informed initiative, PTICC. The study used a mixed-methods approach to assess potential increases in participants’ favorable beliefs toward trauma-informed practice and perceived impacts of PTICC on their behaviors. Overall, education and community participants reported moderate to high (or relatively favorable) scores in regard to these beliefs and perceived impacts of the intervention, with participants’ beliefs appearing to become more favorable over time, as the intervention expanded within the community. As expected, there were no changes in participants’ perceptions of organizational system support for trauma-informed practice, given that groups were held less than one year into the initiative. Also, no changes were observed in participants’ perceived impacts of PTICC, but this finding may have been because scores were already relatively high to begin with.
Qualitative focus group analyses complement these quantitative findings to provide rich, detailed information about participants’ experiences in this community-wide initiative to promote the use of trauma-informed practice. Educators and community service providers identified several benefits of trauma-informed training and agreed that being “trauma-informed” meant reframing one’s perspective, becoming more self-reflective, and acquiring skills to respond more effectively to those who have experienced trauma. Focus group participants also noted that being trauma-informed cultivated a sense of hope for the future. This finding is consistent with prior research on ACEs and resilience. Müller and Kenney ( 2021 ) discussed how professional workshops and trainings on childhood trauma have helped to “[reframe] the biology of early life adversity as a ‘science of hope’” (p. 1236) through emphasizing the potential for positive developmental change linked to supportive environments and relationships. However, focus group participants also identified challenges associated with becoming trauma-informed, including achieving buy-in from community partners, school staff, and parents. This finding aligns with prior research describing resistance that researchers and providers may encounter from youth, caregivers, and colleagues in response to trauma-informed work, which may be perceived as patronizing and radical (Isobel, 2016 ).
These findings enhance understanding of how diverse stakeholders experienced a dynamic and complex community-level intervention to promote trauma-informed practice, but also illustrate several important methodological considerations. These were described in brief in the Introduction section and are explored in greater depth below.
Considerations for Future Community-Engaged Evaluation Research
Addressing ceiling effects.
In our work with PTICC, the community’s commitment to building a network of support and becoming trauma-informed was strikingly evident. In 2008, the Pottstown School District established an initiative, known as the Pottstown Early Action for Kindergarten Readiness (PEAK), in partnership with early childhood education programs to address the links between ACEs and school readiness (Matlin et al., 2019 ). This initiative helped to spread awareness of the effects of trauma on child development and laid a strong foundation for PTICC. Many of the education and community stakeholders involved in the conceptualization of PTICC drew from their earlier experiences with PEAK to help inform the design, delivery, and assessment of PTICC in collaboration with the research team. Given that messaging about ACEs had already permeated the community when PTICC launched, we anticipated that stakeholder buy-in to PTICC and the trauma-informed principles it emphasized would be strong. Therefore, it was not surprising that survey respondents had high average scores on the constructs of interest at the onset of their participation. These initial high scores left little room to observe a sufficient range of responses in subsequent measurements.
The issue of ceiling effects is well-documented in the longitudinal research literature (e.g., Chyung et al., 2020 ; Fries et al., 2011 ; McBee, 2010 ). Of note, given the small sample in this study, we did not find it prudent to directly test for potential ceiling effects using methods such as the Tobit, or censored, regression model (McBee, 2010 ). However, it is recommended that researchers consider adequately testing for this measurement issue, particularly in community-engaged research in which the potential for ceiling effects is high. In addition, Chyung et al. ( 2020 ) suggested that increasing the number of survey response options and using fully labeled and positively packed scales may help to reduce the risk of ceiling effects.
Disaggregating Data
A limitation of our study was the size and scope of the longitudinal sample and unbalanced number of participants in the education and community partner sectors. As a result, we did not have rich enough data to permit analysis of individual-level trajectories in a large group beyond two time points of data collection and were unable to test for potential between-group differences in trauma-informed beliefs and perceived impacts of PTICC. Although these data can help to paint an initial picture of findings, this study would have benefitted from assessment of data from a larger group over a more extended period of time to allow for assessment of individual growth that may not yet have occurred by the second data collection point. Given the Pottstown School District’s role as a long-time and key stakeholder in the community, we might expect significant differences between school staff members’ commitment to trauma-informed beliefs and that of smaller and newer groups to the initiative (e.g., those sub-groups that comprised our Community Partners sample). It is recommended that future community-engaged research on trauma-informed practice consider disaggregating data by sites or groups to uncover more meaningful and varied patterns of outcomes while avoiding more generalized analytical approaches (Tirrell et al., 2021 ). It would also be helpful to follow-up with individuals who discontinue their participation in similar initiatives to learn potential barriers to participation and how to improve retention.
Mitigating Challenges Associated with Participant Recruitment and Buy-in
As noted earlier, we experienced challenges in recruiting large samples of diverse community partners and parents/caregivers in our study. Focus group findings helped to reveal potential reasons for their lower engagement in PTICC. For instance, one community partner from the field of criminal justice stated that trauma-informed practice was a “hard sell” in her discipline, which tends to be more punitive-oriented. School staff also stated that some parents were hesitant to become involved in PTICC for fear of being labeled as a “bad parent” or being “taught how to parent.”
These findings emphasize the need to adequately identify and attend to potential stakeholder concerns at the onset of a community-based intervention and to prioritize efforts to build trust and camaraderie with all groups. Building and maintaining trust is an essential component of community-based participatory research (Christopher et al., 2008 ) and, in our study, perhaps more attention could have been focused on engaging with PTICC’s Family Advisory Committee to identify and mitigate potential barriers to parent/caregiver participation.
In addition, we experienced challenges in retaining a longitudinal sample of participants across groups. Although participants were invited to provide survey data at three time points, many discontinued their participation after the second data collection, for reasons unknown. Perhaps it would have been helpful to follow-up with this sub-group to better understand their reasons for discontinuing their participation. In addition, it would have been informative to re-collect quantitative and qualitative data at least six months post-intervention to assess whether any outcomes were sustained, which was not possible due to limited resources.
Implications for Community Capacity Building
This study underscores the importance of building “collaborative capacity” in community coalition work to promote trauma-informed systems change (Foster-Fishman et al., 2001 ; Matlin et al., 2019 ). Collaborative capacity refers to the conditions that help a coalition to facilitate collaboration and sustained positive community change (Foster-Fishman et al., 2001 ). These conditions include member capacity (e.g., knowledge, skills, motivation), relational capacity (e.g., shared vision, power sharing), organizational capacity (e.g., effective leadership, communication), and programmatic capacity (e.g., clear and feasible goals) (Foster-Fishman et al., 2001 ).
In the context of PTICC, a Steering Committee, or coalition, comprised of consultants/researchers and local leaders in education, social and behavioral health services, philanthropy, and law enforcement played an instrumental role in building capacity across these domains through an ongoing participatory process (Matlin et al., 2019 ). This group formed a shared vision around building a trauma-informed community and connected with key members throughout the community (e.g., from the school district) to spread awareness of ACEs and trauma-informed practice (Matlin et al., 2019 ). In particular, working groups focused on building member capacity (e.g., though the delivery of trainings on ACEs and resilience) and relational capacity (e.g., through fostering cross-sectoral collaboration on trauma-informed) and helped to translate the vision of the Steering Committee into action, as reinforced by the study’s findings (Matlin et al., 2019 ).
This community capacity building process mirrors that described in the Children’s Resilience Initiative (CRI) in Walla Walla, Washington (Longhi et al., 2019 ), as described earlier. Similarly to PTICC, the success of CRI was driven by the “iterative interplay” of several key elements of capacity building, including the formation of a small group of community leaders who identified a common vision and goals and helped to facilitate cross-sectoral collaboration and the sustainment of trauma-informed processes and principles (Longhi et al., 2019 ). This work involved shifts in knowledge, skills, and mindsets; the formation of trusting and collaborative relationships; and changes in organizational policies and practices (Longhi et al., 2019 ).
We recommend that future community-engaged work prioritizes strengthening member, relational, organizational, and programmatic capacities to empower communities to effect systems change (Foster-Fishman et al., 2001 ). This process starts with building a clearly defined and shared vision and facilitating cross-sectoral collaboration to infuse this vision across organizations and enact it (Matlin et al., 2019 ).
Trauma during childhood has the potential to adversely affect one’s physical, cognitive, emotional, and social development across the life span. However, trauma-informed approaches have the potential to buffer young people and their families against adverse events by enhancing awareness and understanding of the signs and impacts of childhood trauma and how to effectively prevent re-traumatization and foster resilience. Findings from our mixed-methods study of PTICC help to elucidate what it means to be trauma-informed, positive gains of participation in a community-based, trauma-informed initiative, and various implementation challenges for such initiatives. We discuss findings in the context of key methodological considerations for future community-engaged work seeking to build trauma-informed communities and present recommendations for building community capacity for change.
Acknowledgements
This work was supported, in part, by the Pottstown School District, The Scattergood Foundation, Yale School of Medicine, and the National Institute on Drug Abuse (T32DA019426; Tebes, PI). We are grateful to Laurie Kolka and the Pottstown School District, and the Pottstown Trauma-Informed Community Connection (PTICC) steering committee and community partners. We also thank colleagues at The Consultation Center at Yale and The Scattergood Foundation for their assistance, including: Aly Ferguson, Susan Florio, Caitlin O’Brien, and Samantha Pittenger.
Compliance with Ethical Standards
The authors declare no competing interests.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Andrew S, Salamonson Y, Everett B, Halcomb EJ, Davidson PM. Beyond the ceiling effect: Using a mixed methods approach to measure patient satisfaction. International Journal of Multiple Research Approaches. 2011; 5 :52–63. doi: 10.5172/mra.2011.5.1.52. [ CrossRef ] [ Google Scholar ]
- Aresi G, Henderson DX, Hall-Campbell NF, Ogley-Oliver EJF. Practicing community psychology through mixed methods participatory research designs. The Journal of New Paradigm Research. 2017; 73 (7):473–490. [ Google Scholar ]
- Arnold KT, Pollack Porter KM, Frattaroli S, Durham RE, Mmari K, Clary LK, Mendelson T. Factors that influenced adoption of a school-based trauma-informed universal mental health intervention. Prevention Science. 2020; 21 :1081–1092. doi: 10.1007/s11121-020-01144-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Báez JC, Renshaw KJ, Bachman LEM, Kim D, Smith VD, Stafford RE. Understanding the necessity of trauma-informed care in community schools: A mixed-methods program evaluation. Children & Schools. 2019; 41 (2):101–110. doi: 10.1093/cs/cdz007. [ CrossRef ] [ Google Scholar ]
- Baker CN, Brown SM, Overstreet S, Wilcox PD. Validation of the Attitudes Related to Trauma-Informed Care Scale (ARTIC) Psychological Trauma: Theory, Research, Practice, and Policy. 2021; 13 (5):505–513. doi: 10.1037/tra0000989. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baker CN, Brown SM, Wilcox PD, Overstreet S, Arora P. Development and psychometric evaluation of the Attitudes Related to Trauma-Informed Care (ARTIC) Scale. School Mental Health: A Multidisciplinary Research and Practice. Journal. 2016; 8 (1):61–76. [ Google Scholar ]
- Bloom SL. Creating sanctuary: Toward the evolution of sane societies. New York, NY: Routledge; 2013. [ Google Scholar ]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006; 3 (2):77–101. doi: 10.1191/1478088706qp063oa. [ CrossRef ] [ Google Scholar ]
- Bridgland, V. M. E., Moeck, E. K., Green, D. M., Swain, T. L., Nayda, D. M., Matson, L. A., Hutchison, N. P., & Takarangi, M. K. T. (2021). Why the COVID-19 pandemic is a traumatic stressor. PLoS One . 10.1371/journal.pone.0240146. [ PMC free article ] [ PubMed ]
- Chang X, Jiang X, Mkandarwire T, Shen M. Associations between adverse childhood experiences and health outcomes in adults aged 18-59 years. PLoS ONE. 2020; 14 (2):e0211850. doi: 10.1371/journal.pone.0211850. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Christopher S, Watts V, McCormick AK, Young S. Building and maintaining trust in a community-based participatory research partnership. American Journal of Public Health. 2008; 98 (8):1398–1406. doi: 10.2105/AJPH.2007.125757. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chyung SY, Hutchinson D, Shamsy JA. Evidence-based survey design: Ceiling effects associated with response scales. Performance Improvement. 2020; 59 (6):6–13. doi: 10.1002/pfi.21920. [ CrossRef ] [ Google Scholar ]
- Collaborative for Academic, Social, and Emotional Learning (CASEL) (2021). SEL: What are the core competence areas and where are they promoted? https://casel.org/sel-framework/ .
- Creswell JW. Research design: Qualitative, quantitative, and mixed methods approaches. 3rd ed. Thousand Oaks, CA: Sage Publications; 2009. [ Google Scholar ]
- DeCandia, C. J., Guarino, K., & Clervil, R. (2014). Trauma-informed care and trauma-specific services: A comprehensive approach to trauma intervention. American Institutes for Research . https://www.air.org/sites/default/files/downloads/report/Trauma-Informed%20Care%20White%20Paper_October%202014.pdf .
- Esaki N, Benamati J, Yanosy S, Middleton JS, Hopson LM, Hummer VL, Bloom SL. The Sanctuary Model: Theoretical framework. Families in Society: The Journal of Contemporary Social Services. 2013; 94 (2):87–95. doi: 10.1606/1044-3894.4287. [ CrossRef ] [ Google Scholar ]
- Foster-Fishman PG, Berkowitz SL, Lounsbury DW, Jacobson S, Allen NA. Building collaborative capacity in community coalitions: A review and integrative framework. American Journal of Community Psychology. 2001; 29 (2):241–261. doi: 10.1023/A:1010378613583. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fries J, Rose M, Krishnan E. The PROMIS of better outcome assessment: Responsiveness, floor and ceiling effects, and internet administration. The Journal of Rheumatology. 2011; 38 (8):1759–1764. doi: 10.3899/jrheum.110402. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hanson, R. F., Lang, J. M., Fraser, J. G., Agosti, J. R., Ake, G. S., Donisch, K. M., & Gewirtz, A. H. (2018). Trauma-informed care: Definitions and statewide initiatives. In J. B. Klika, & J. R. Conte (Eds), The APSAC handbook on child maltreatment (4th edn., pp. 272–291). Thousand Oaks, CA: SAGE.
- Harris, M., & Fallot, R. (2001). Using trauma theory to design service systems. New Directions for Mental Health Services, 89 . Jossey Bass. [ PubMed ]
- Isobel S. Trauma informed care: A radical shift or basic good practice? Australian Psychiatry. 2016; 24 (6):589–591. doi: 10.1177/1039856216657698. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krystal JH, Alvarado J, Ball SA, Fortunati FG, Hu M, Ivy ME, Kapo J, Olson KD, Rohrbaugh RM, Sinha R, Tebes JK, Vender RJ, Yonkers KA, Mayes LC, Mayes LC. Mobilizing an institutional supportive response for healthcare workers and other staff in the context of COVID-19: The Yale experience. General Hospital Psychiatry. 2021; 68 :12–18. doi: 10.1016/j.genhosppsych.2020.11.005. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Longhi D, Brown M, Barila T, Fromm Reed S, Porter L. How to increase community-wide resilience and decrease inequalities due to adverse childhood experiences (ACEs): Strategies from Walla Walla, Washington. Journal of Prevention & Intervention in the Community. 2019; 9 :1–17. [ PubMed ] [ Google Scholar ]
- Magruder KM, McLaughlin KA, Bornon DLE. Trauma is a public health issue. European Journal of Psychotraumatology. 2017; 8 (1):1375338.. doi: 10.1080/20008198.2017.1375338. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Matlin SL, Champine RB, Strambler MJ, O’Brien CO, Hoffman E, Whitson M, Kolka L, Tebes JK. A community’s response to adverse childhood experiences: Building a resilient, trauma-informed community. American Journal of Community Psychology. 2019; 64 (3-4):451–466. doi: 10.1002/ajcp.12386. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McBee M. Modeling outcomes with floor or ceiling effects: An introduction to the Tobit Model. Gifted Child Quarterly. 2010; 54 (4):314–320. doi: 10.1177/0016986210379095. [ CrossRef ] [ Google Scholar ]
- Middleton JS, Bloom SL, Strolin-Goltzman J, Caringi J. Trauma-informed care and the public child welfare system: The challenges of shifting paradigms: Introduction to the special issue on trauma-informed care. Journal of Public Child Welfare. 2019; 13 (3):235–244. doi: 10.1080/15548732.2019.1603602. [ CrossRef ] [ Google Scholar ]
- Mihelicova M, Brown M, Shuman V. Trauma-informed care for individuals with serious mental illness: An avenue for community psychology’s involvement n community mental health. American Journal of Community Psychology. 2018; 61 :141–152. doi: 10.1002/ajcp.12217. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Müller R, Kenney M. A science of hope? Tracing emergent entanglements between the biology of early life adversity, trauma-informed care, and restorative justice. Science, Technology, & Human Values. 2021; 46 (6):1230–1260. doi: 10.1177/0162243920974095. [ CrossRef ] [ Google Scholar ]
- National Institute of Mental Health (NIMH). 2017. Post-traumatic stress disorder. https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd.shtml .
- Pinderhughes, H., Davis, R. A., & Williams, M. (2015). Adverse community experiences and resilience: A framework for addressing and preventing community trauma . Kaiser Permanente. https://www.preventioninstitute.org/publications/adverse-community-experiences-and-resilience-framework-addressing-and-preventing .
- Pottstown Trauma-Informed Community Connection (PTICC). (n.d.). https://pottstownmatters.org/ .
- Scheer, J. R., & Poteat, V. P. (2018). Trauma-informed care and health among LGBTQ intimate partner violence survivors. Journal of Interpersonal Violence . 10.1177/0886260518820688. [ PMC free article ] [ PubMed ]
- Sichel, C., Strambler, M. J., Matlin, S., Garcia, & Tebes, J. K. (2021). Integrating school climate and trauma-informed practice: An empirical proof of concept. ( Under review)
- Sowder KL, Knight LA, Fishalow J. Trauma exposure and health: A review of outcomes and pathways. Journal of Aggression, Maltreatment & Trauma. 2018; 27 (10):1041–1059. doi: 10.1080/10926771.2017.1422841. [ CrossRef ] [ Google Scholar ]
- Stolbach BC, Anam S. Racial and ethnic health disparities and trauma-informed care for children exposed to community violence. Pediatric Annals. 2017; 46 (10):e377–e381. doi: 10.3928/19382359-20170920-01. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (July 2014). SAMHSA’s concept of trauma and guidance for a trauma-informed approach . SAMHSA’s Trauma and Justice Strategic Initiative. https://ncsacw.samhsa.gov/userfiles/files/SAMHSA_Trauma.pdf .
- Substance Abuse and Mental Health Services Administration (2017). Spotlight: Building resilient and trauma-informed communities. Walla Walla, WA: Mobilizing the community for resilience. https://store.samhsa.gov/product/Spotlight-Building-Resilient-and-Trauma-Informed-Communities-Walla-Walla-WA-Mobilizing-the-Community-for-Resilience/SMA17-5020 .
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2020). Understanding child trauma. https://www.samhsa.gov/child-trauma/understanding-child-trauma .
- Tebes JK, Champine RB, Matlin SL, Strambler MJ. Population health and trauma-informed practice: Implications for programs, systems, and policies. American Journal of Community Psychology. 2019; 64 (3-4):494–508. doi: 10.1002/ajcp.12382. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tebes JK, Kraemer DT. Quantitative and qualitative knowing in mutual support research: Some lessons from the recent history of scientific psychology. American Journal of Community Psychology. 1991; 19 (5):739–756. doi: 10.1007/BF00938042. [ CrossRef ] [ Google Scholar ]
- Temkin D, Harper K, Stratford B, Sacks V, Rodriguez Y, Bartlett JD. Moving policy toward a whole school, whole community, whole child approach to support children who have experienced trauma. Journal of School Health. 2020; 90 (12):940–947. doi: 10.1111/josh.12957. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tirrell JM, Gansert PK, Dowling EM, Williams K, Iraheta G, Lerner JV, King PE, Sim ATR, Lerner RM. Interrogating ergodicity and specificity in youth development programs in El Salvador. Journal of Applied Developmental Psychology. 2021; 73 :101243. doi: 10.1016/j.appdev.2021.101243. [ CrossRef ] [ Google Scholar ]
- Wisdom, J., & Creswell, J. W. (2013). Mixed methods: Integrating quantitative and qualitative data collection and analysis while studying patient-centered medical home models . AHRQ Agency for Healthcare Research and Quality. https://pcmh.ahrq.gov/page/mixed-methods-integrating-quantitative-and-qualitative-data-collection-and-analysis-while .

Initiatives
Our community.
- Education & Admissions
Ohio State celebrates successful medical residency match day at the Ohio Union
Author: Kelli Trinoskey
- College Updates
- Internship and Residency

For most medical students, the culmination of four years of medical school — hours of study, clinical rotations and tough exams — is Match Day, the celebratory announcement of their residency position placement. In advance of Match Day, M4 students from around the country rank the residency programs they hope to join in their order of preference, while the programs simultaneously rank the learners. The National Resident Matching Program then runs this data through an algorithm, which works to maximize the preferences of all parties.
“Match Day is medicine’s own version of March Madness,” said Carmine A. Grieco, MD , associate dean for Student Life at The Ohio State University College of Medicine.
Dr. Grieco, along with Carol R. Bradford, MD, MS, FACS , dean of the Ohio State College of Medicine, and other leaders shared a few words of encouragement before students opened their official match envelopes at this crucial point of their journey.
“It is a day that you will remember for the rest of your lives,” Dr. Bradford said. “As you embark on this new chapter, you hold the key to your success. Regardless of what program you match into, you will be continuing on your journey of lifelong learning.”
On March 15, nearly 200 medical students at the college gathered with faculty, staff, family and friends at the Ohio Union to discover where they — these soon-to-be physicians — would begin the next chapter of their medical careers.
Dr. Grieco kicked off the ceremony, acknowledging the excitement of this momentous day, when future doctors learn the location and specialty of their residency. Jennifer McCallister, MD , associate dean of Medical Education, congratulated students on their years of hard work and dedication that led to this day.
“You have stepped up and stepped together as leaders and advocates of change at our medical center and in our profession,” said Dr. McCallister. ”Today is the day to pause and catch your breath and reflect on all of your hard work.”
Daniel Clinchot, MD , vice dean for Education, put the significance of these accomplishments into perspective by sharing that this year, 193 medical students at the College of Medicine matched in more than 24 specialties. Nationwide, there were 44,000 applicants for just 41,000 positions. It was the largest Match Day in the history of the National Resident Matching Program.
“35% of our medical students matched in Ohio,” said Dr. Clinchot. “The most popular specialties were internal medicine, pediatrics, emergency medicine and orthopedic surgery.” An amazing 68 learners chose a primary care specialty.
One M4, Alyssa Thompson, learned that she will be staying in Ohio, but heading south to Cincinnati for a pediatrics residency in the extensive program at Cincinnati Children's Hospital Medical Center .
“It was my first choice,” said Thompson. “I will take a lot with me. At Ohio State, I learned so much about how to be a better doctor, be more empathetic and understand the way decisions are made in medicine.”
Aaron Craft, former Ohio State Buckeye basketball star and fourth-year medical student, found out he matched in otolaryngology at The Ohio State University Wexner Medical Center. He and his wife opened his envelope together and immediately hugged with joy and relief.
“We have a lot of specialists here in the field and I’ve learned a lot from them already,” said Craft. “I am really excited to learn more.”
Craft, his wife and their two small children will stay in Columbus as he undergoes five years of residency, expanding his training in diagnosing and treating conditions of the head and neck and learning both nonsurgical and surgical treatments.
Congratulations to The Ohio State University College of Medicine Class of 2024!
2024 Match Day

More from Ohio State

Kristy Townsend, PhD, receives prestigious research award from W.M. Keck Foundation to study brain and adipose tissue connections

Understanding impact of traumatic situations key to providing trauma-informed care

Historic growth for College of Medicine research funding surpasses $400 million

IMAGES
VIDEO
COMMENTS
Trauma-informed and resilience-informed approaches to care may help address these concerns across health and social care research. These approaches take an empowerment-based response to adversity, and are suitable for integration and extension as Trauma and Resilience Informed Research Principles and Practice (TRIRPP) for studies beyond the ...
While there is a growing body of the literature on trauma-informed care, ... Interpersonal violence and reproductive coercion/Questions from previous family planning clinic-based studies (Revised Conflict Tactics Scale 2, Perception of Abuse), reproductive coercion measured by 10 questions ... Psychological Trauma: Theory, Research, Practice ...
Providing a comprehensive literature review on trauma, traumatic stress, trauma-informed care (TIC), and trauma-related interventions is a daunting task when considering the quantity and prolific production of research in this area in the past 20 years. To manage the volume of information, this literature review mainly focuses on reviews and meta-analyses rather than seminal work to address ...
Trauma is often viewed as an individual or interpersonal issue. This paper expands the definition of trauma to include the impact collective and structural elements on health and well-being. The need for a trauma-informed response is demonstrated, with instruction as to how to implement this type of care in order to resist re-traumatization.
Trauma exposure has been associated with negative mental and physical health outcomes across the lifespan.1-8 These negative outcomes burden our healthcare system and have significant costs (e.g., mental health services, medical services, child welfare). In recognition of the potential consequences of trauma exposure, organizations and systems ...
This is called trauma-informed care. Dr L. Elizabeth Lincoln is a primary care physician at MGH who has trained medical professionals and students about approaching patient care with an understanding of trauma. She explains: "Trauma-informed care is defined as practices that promote a culture of safety, empowerment, and healing.
Trauma- (and violence-) informed care (T(V)IC) ... Again, however, we selected the more efficient approach to answer this more specific research question. The most pressing need for future research is the development of a TVIC measure that "does it all."
Experiences of trauma in childhood and adulthood are highly prevalent among service users accessing acute, crisis, emergency, and residential mental health services. These settings, and restraint and seclusion practices used, can be extremely traumatic, leading to a growing awareness for the need for trauma informed care (TIC). The aim of TIC is to acknowledge the prevalence and impact of ...
The impacts of psychological trauma have important implications for the provision and receipt of healthcare. This systematic review identifies key factors that should be targeted to promote trauma-informed care implementation, including interagency collaboration, staff and leadership buy-in, aligning implementation strategies with existing policies and procedures, allocation of adequate human ...
The brief is a product of Advancing Trauma-Informed Care, ... (ACE) study. 1,2,3 Because of the ACE study, and other subsequent research, health care policymakers and providers increasingly recognize that exposure to traumatic events, especially as children, heighten ... Questions remain for the field regardinghow to conceptualize trauma and ...
service-providing organizations, policymakers, researchers, and research funders. II.he Key Questions T The key questions were posted for public comment on 4/28/23 for three weeks. Researchers ... How is Trauma Informed Care (TIC) defined in theory and research and according to professional guidelines or other clinical, system, or policy-level ...
Trauma-informed and resilience-oriented (TIRO) screening and assessment measures provide clear guidance for care organizations and mobile crisis units to support not only the individual receiving services but also the staff delivering care - a trauma-informed team is a team who provides better care both to those they serve and to each other.
Trauma-informed (TI) approach is a framework for a system change intervention that transforms the organizational culture and practices to address the high prevalence and impact of trauma on patients and healthcare professionals, and prevents re-traumatization in healthcare services. Review of TI approaches in primary and community mental healthcare identified limited evidence for its ...
First, a trauma-informed organization's mission is grounded in trauma-informed care principles and practices. Trauma-informed care is the organization's way of doing business, and thus everyone in the organization needs to understand and embrace it. "Essentially, it boils down to understanding that staff have their own trauma histories ...
This TIP, Trauma-Informed Care in Behavioral Health Services, ... including research, theoretical papers, commentaries, and lessons learned from treatment facilities. ... it involves explaining the value and type of trauma-related questions that may be asked during an intake process, educating clients about trauma to help normalize traumatic ...
If they are triggered by a research question or a set of questions, their brains may go into survival mode—fight, flight, freeze, or submit—deactivating the logical processing and executive functioning part of their brains. ... Trauma-informed research or research that incorporates the tenants of trauma-informed care is an approach that ...
Research is continuing in the attitudes and understanding of TIC, with five publications discussing the development and validation of a psychometric evaluation of the Attitudes Related to Trauma-Informed Care (ARTIC) Scale, which has been used to explore a persons' self -rated attitude towards TIC (Baker et al., Citation 2016; Citation 2021 ...
Attention to childhood trauma and the need for trauma-informed care has contributed to the emerging discourse in schools related to teaching practices, school climate, and the delivery of trauma-related in-service and preservice teacher education (Cole et al., 2005; Crosby, 2015; Day et al., 2015; Oehlberg, 2008).Psychological trauma includes experiences or events that are perceived as harmful ...
When offering Trauma-Informed Care, questions can be personal and even difficult. The goal is always to avoid "retriggering" the person's trauma while allowing them a safe space to open up and connect. When things get deep and personal, following a set of specific " Trauma-Informed Care questions" can actually feel impersonal and distant.
Adopting a trauma-informed care (TIC) approach is integral to improving health outcomes and creating better patient-provider relationships. "Trauma-informed care is really about creating a space where every person, including people who have experienced trauma, feel safe, feel included, and feel understood as a whole person," says Stephanie ...
Aims: To explore youth, caregiver and staff perspectives on their vision of trauma-informed care, and to identify and understand potential considerations for the implementation of a trauma-informed care programme in an inpatient mental health unit within a paediatric hospital. Design and methods: We applied the Interpretive Description approach, guided by complexity theory and the ...
Trauma-informed care (TIC) involves a broad understanding of traumatic stress reactions and common responses to trauma. Providers need to understand how trauma can affect treatment presentation, engagement, and the outcome of behavioral health services. This chapter examines common experiences survivors may encounter immediately following or long after a traumatic experience.
Trauma-informed care is a framework that emphasizes understanding, compassion, and empowerment in working with individuals who have experienced trauma. ... backed by neuroscience research. It delves into how trauma can impact brain structure, outlines challenges specific to various groups, and suggests intervention strategies for acute and ...
At the most intensive end of the spectrum are therapeutic interventions, ranging from in-patient treatment to regular sessions with a mental health professional, which are designed specifically to deal with serious trauma. Trauma-informed care or practice is less intensive, but affects how practitioners in a range of fields, such as social work ...
Contextual Questions. CQ1. How is Trauma Informed Care (TIC) defined in theory and research and according to professional guidelines or other clinical, system, or policy-level guidance or recommendations? ... Table 1 provides details on the population, interventions, comparators, outcomes, timing, and setting (PICOTS) for the research questions ...
Adopting a trauma-informed care (TIC) approach is integral to improving health outcomes and creating better patient-provider relationships. ... "Inviting patients to ask questions, and asking questions to learn about what they've already tried to do to address their health issues balances out the power dynamic between providers and patients ...
How do different stakeholders define and implement trauma-informed practices in a community setting? This mixed-methods study explores the perspectives and experiences of participants in a trauma-informed community initiative, and identifies the key themes and challenges of becoming trauma-informed. The study also provides insights and recommendations for future trauma-informed interventions.
The patient was a victim of sexual trauma and found the quietness of the room and lack of detailed explanation of the exam to be triggering for her. Realizing this to be an area we could improve, I reached out to Jessica Griffin, PsyD and Zlatina Kostova, PhD and worked on developing a Radiology specific training for Trauma Informed Care.
Kristy Townsend, PhD, receives prestigious research award from W.M. Keck Foundation to study brain and adipose tissue connections. Understanding impact of traumatic situations key to providing trauma-informed care . Historic growth for College of Medicine research funding surpasses $400 million . Follow us on Facebook; Follow us on X;