Globalize your Research

Case Study of a Middle-Aged Woman’s OCD Treatment Using CBT and ERP Technique
- Clinical Medical Reviews and Reports
Introduction
Case report, case formulation, intervention, preparation phase of erp, middle phase of erp, steps of hierarchy, booster sessions, quick links.
- Aims and scope
- Article processing charges
- Editorial board
- Editorial Workflow
Research Article | DOI: https://doi.org/10.31579/2690-8794/102
- Deepshikha Paliwal 1*
- Anamika Rawlani 2
1 M.Sc. Clinical Psychology, Dev Sanskriti University, Ranchi, India. 2 M.Phil Clinical Psychology, RINPAS Ranchi, India.
*Corresponding Author: Deepshikha Paliwal, M.Sc. Clinical Psychology, Dev Sanskriti University, Ranchi, India.
Citation: Deepshikha Paliwal and Anamika Rawlani (2022) Case Study of a Middle-Aged Woman’s OCD Treatment Using CBT and ERP Technique. Clinical Medical Reviews and Reports 4(3): DOI: 10.31579/2690-8794/102
Copyright: © 2022, Deepshikha Paliwal, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 01 September 2021 | Accepted: 04 December 2021 | Published: 10 January 2022
Keywords: OCD; CBT; ERP; salkovskis’s model
Introduction : This is a case report of a middle-aged woman, who was experiencing “obsessive” thoughts related to the “Bindi” (decorative piece wear by women on the forehead) and cleaning “compulsions”. Present case report discusses the patient’s assessment, case formulation, treatment plan and the effectiveness of the CBT and ERP sessions in reducing OCD symptoms.
Methodology: The patient was treated with Cognitive Behavior Therapy (CBT) along with Exposure Response Prevention (ERP) technique. The assessment of the case was done with the Y-BOCS rating scale, Beck’s Depression Inventory, Obsessive Beliefs Questionnaire, and Behavior Analysis Performa which suggested the higher severity level of the patient’s symptoms. Parallel to the assessment sessions, detailed case history related to the onset of the problem, difficulties faced because of the disorder, childhood incidences, family chart, marital issues, and medical history were discussed with the patient. Based on the reported details, the case was formulated according to the Salkovoskis inflated sense of responsibility model. After the case formulation, the treatment plan was designed which involved ERP sessions and restructuring of the cognitive distortions (beliefs, thoughts, and attitude).
Results: After the completion of the twenty-five therapy sessions, the patient reported improvement in the coping of anxiety-provoking thoughts and reduced level of the washing compulsions. The effects of the therapy were checked and found maintained up to two months follow up.
Conclusion: CBT and ERP technique is an effective treatment in reducing obsessive and compulsive symptoms of the patient.
Have you ever felt like a sudden urge to hurt somebody? What if such urges continuously appear in your head? What would you do to stop these urges? Would you be able to continue your day to day life normally with such urges? Clinical Psychologists studied the repetitive occurrence of unwelcoming thoughts, urges, doubts, and images which create anxiety. They gave it the term “Obsessions”. These obsessions are dreadful, frightening, and intolerable to the extent that they might hinder the natural flow of one’s personal, professional, and social life. The person who suffers from such anxiety-provoking thoughts tries to deal with the distress caused by such ‘obsessions’ by adopting some behavior or activity which temporarily relieve them from the anxiety and the feared consequences. This behavior could be anything like washing hands, cleaning, repeatedly checking the door, or repeating some phrases in the head. Psychologists called such repetitive behaviors or activities as “Compulsions”. According to APA (1994), if the presence of obsessions and/or compulsions is time-consuming (more than an hour a day), cause major distress, and impair work, social, or other important functions then the person will be diagnosed with Obsessive-Compulsive Disorder (OCD). Recent epidemiological studies suggest that OCD affects between 1.9 to 2.5% of the world population at some point in their lives, creating great difficulties on a professional, academic and social level (DSM-IV-TR, 2001). OCD affects all cultural and ethnic groups and, unlike many related disorders, males and females are equally affected by this disorder (Rasmussen & Eisen, 1992). OCD is one of the most incapacitating of anxiety disorders having been rated as a leading cause of disability by the World Health Organization (1996). The major cause of OCD is still unknown; there could be some genetic components responsible for it (DSM-5). Child abuse or any stress-inducing event could be the risk factor involved in the history of OCD patients. The severity of the symptoms related to obsessions and compulsions provides the basis of the diagnosis in OCD which rules out any other drug-related or medical causes. Clinical Psychologists use rating scales like Y-BOCS (Fenske & Schwenk, 2009), self-reports, and Behavior Analysis Performa to assess the severity level of the symptoms. Based on the severity, the treatment plan is designed. Treatment of OCD involves psychotherapy and antidepressants. Psychotherapy such as Cognitive Behavior Therapy (CBT) is an effective psycho-social treatment of OCD (Beck, 2011). In CBT, a “problem-focused” approach is used to treat the diagnosed psychological disorder by challenging and changing core beliefs, negative automatic thoughts, and cognitive distortions of the patient. CBT involves Exposure Response Prevention (ERP) as a technique to treat OCD in which the patient is exposed to the cause of the problem and not allowed to repeat the ritual behavior (Grant, 2014). ERP has promising results with 63% of OCD patients showing favorable responses after following the therapy sessions (Stanley & Turner, 1995).
This is a case of a 31 years old woman, who belongs to a middle socio-economic background, currently living with her in-laws, husband, and daughter. The patient was experiencing obsessive thoughts related to the contamination spread by ‘bindi’ along with the compulsive behavior of washing and cleaning from the last five years. The patient reported that she always tried to check the contact of ‘Bindi’ with anything because that contact makes her incapacitate to control the situation. She took two and three hours (on daily basis) in washing and cleaning her home, scrubbing her daughter, cleaning the daughter’s school bag after returning from school, husband’s bag, and other usable items, so that she can stop the contamination from spreading everywhere. The patient has a history of facing interpersonal issues with family members since her childhood. Her father was alcohol dependent and the mother was the patient of depression. The financial condition of the family was not good. When the patient was 17 years old, her father died due to kidney failure, and her mother got hospitalized because of depression. From a very young age, the patient had to bear the responsibility of the family by taking tuitions. At first, she developed the fear of contamination at the age of 19, when she was in her graduation’s first year, for that she was taken to the Psychiatrist. She responded well to the medicines and stopped showing all the symptoms. At the age of 25, when the patient got pregnant she again developed the fear of contamination, which made her husband and in-laws uncomfortable and family disputes began. Her husband took her to the psychiatrist who referred her for the psychotherapy but she didn’t attend the psychotherapy sessions properly and continuously lived with the obsessions and compulsions up to the present referral where the patient was assessed with Y-BOCS rating scale, BDI, EBQ, and Behavioral Analysis Performa. Based on the assessment, she was diagnosed with OCD having symptoms of obsessions related to the contamination by ‘Bindi’ and washing compulsions. Detailed case history related to the onset of the problem, childhood incidences, family history, marital history, medical history, and other relevant information were also collected. The case was formulated according to Salkovoskis’s inflated sense of responsibility model as the patient’s reported details were signifying the negative interpretations of her responsibility for self and others. After the case formulation, the treatment plan was designed which involved sessions of ERP technique along with the alteration of cognitive distortions (ideas, beliefs, and attitudes) through the cognitive restructuring method of CBT.
1. Yale-Brown Obsessive-Compulsive Scale (YBOCS):
In cognitive-behavioral studies, Y-BOCS is used to rate the symptoms of OCD. This scale was designed by Goodman et al. (1989) to know the baseline and the recovery rate of the ‘severity of obsessions’, ‘severity of compulsions’ and ‘resistance to symptoms’. This is a five-point Likert scale that clinicians administer through a semi-structured interview in which a higher score indicates higher disturbances. The excellent psychometric properties of this scale quantify the severity of the obsessions and compulsions as well as provide valuable qualitative information which makes it very useful for both diagnosis of the OCD and the designing of its treatment plan.
2. Beck Anxiety Inventory (BAI):
Aaron T. Beck (1988) developed BAI as a four-point Likert scale which consists of 21 items of ‘0 to 3’ scores on each item (Higher score means higher anxiety). If the Patient’s scores are from 0 to 7 then interpret as ‘minimal anxiety’, 8 to 15 as ‘mild anxiety’, 16 to 25 as ‘moderate anxiety’, and 30 to 63 as ‘severe anxiety’. BAI assesses common cognitive and somatic symptoms of anxiety disorder and is considered effective in discriminating between the person with or without an anxiety disorder. This scale provides valuable clinical information but is not used by clinicians for diagnostic purposes.
3. Obsessive Belief Questionnaire (OBQ):
OBQ is used to assess the beliefs and appraisals of OCD patients which are critical to their pathogenesis of obsessions (OCCWG, 1997, 2001). This scale consists of 87 belief statements within six subscales which represent key belief domains of OCD. The first subscale is ‘Control of thoughts’ (14 items), the second is ‘importance of thoughts’ (14 items), third is, responsibility (16 items), fourth is ‘intolerance of uncertainty’ (13 items), the fifth is an overestimation of threat (14 items), and sixth is ‘perfectionism’ (16 items). Response on this measure is the general level of agreement of the respondents with the items on a 7 point rating scale that ranges from (-3) “disagree very much” to (+3) “agree very much”. On the respective items summing of the scores is done to calculate the subscale scores.
4. Behavior Analysis Performa
This study used ‘Behavior Analysis Performa’ to do the functional analysis of the patient’s behavior. This Performa collects the details of the patient’s behavioral excess, deficits, and assets, his or her motivational factors behind maintaining and reinforcing ill behaviors, as well as, the medical, cultural, and social factors which contributed to the development of the illness.
Based on the reported details and the assessment, the case was formulated according to the Salkovoskis model (1985). This model suggests that the patient’s main negative interpretation revolves around the idea that his or her actions might have harmful outcomes for self or others. This interpretation of responsibility increases selective attention and maintains negative beliefs (Salkovskis, 1987). Here, in this case, the patient had to face the disturbing family environment which significantly has a role in the formation of maladaptive schemas related to her negative view of self, the world, and the future. The patient’s beliefs assessment reports signified that her major dysfunctional assumptions were ‘if harm is very unlikely, I should try to prevent it at any cost’ and ‘if I don’t act when I foresee danger then I am to blame for any consequences’. Intrusive thought for her was that ‘bindi contaminates dirt’ and neutralizing action for this intrusive thought was ‘washing and cleaning things’. She paid her keen attention to the thought that ‘I should not be get touched with bindi’ and misinterpreted and over signified it by avoiding bindi and preventing the contamination. Her safety behavior included avoiding going out, (especially beauty parlors and cosmetic shops), and getting touched with anyone on roads and market places. The result of such avoidance was tiredness, anxiousness, aggressiveness, and distressed mood state. The graphical representation of the case formulation is shown in Appendix 1 at the end of this paper.
After the case formulation, the treatment plan was designed. The patient had dysfunctional assumptions related to her responsibility for self and others. She had obsessions related to the contamination spread by ‘Bindi’ associated with washing and cleaning compulsions. As she was taken by her husband for the therapy, so it was important to socialize her and her family with the OCD to develop insight for the disorder. After socializing them with OCD, they were taught the basic structure of the cognitive behavior model that how patient’s thoughts, emotions, physical sensations, and behavior all are interrelated and affect each other in a vicious circle.
In the preparatory phase, the patient was introduced with the ERP technique, how does it work and how much her cooperation and will power are required for the success of this technique. After introducing the ERP technique to her, behavioral analysis was done with the patient by using a down-arrow method to make the list of the situations she uses as safety strategies and maintains her negative beliefs.
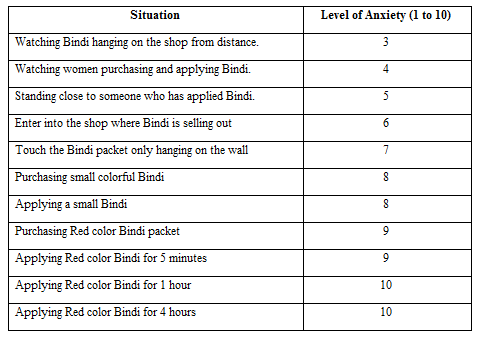
In the next session, the patient was told to imagine her exposure with different situations which she avoids and asked her to rate the level of anxiety in all the situations on a scale of 1 to 10. After this imaginary exposure, a hierarchy was made from the least anxiety-provoking event to the high anxiety-provoking event. Here is the list of different situations which the patient rated based on the level of anxiety:
In this phase, the patient was gradually exposed with the least anxiety-provoking situation to the highest-anxiety provoking situation. The patient’s husband worked as a co-therapist and accompanied her in all the situations and observed her anxiety levels and other behaviors. The patient was asked to rate her anxiety level on a scale of 1 to 10 after every exposure.
- In the first step of exposure, patient was instructed to go out with the husband in the market area where ‘Bindi’ was hanging on the walls , she was instructed to watch them from some distance and observe her level of anxiety varying with time . She was strictly instructed not to avoid the situation and to face the anxiety levels without skipping. In the next session, she was asked what she exactly felt when she was watching the bindi packets, she replied that at first sight of bindi she felt disgusted and wanted to go away but she gave self instructions to her that these are very far and cannot contaminate her so she kept sitting there and with time her anxiety level also came down.
- In the second step of the hierarchy she was instructed for sitting at a distance from the cosmetics shop and observe the ladies entering and purchasing bindi there , her husband was told to work as a co-therapist and checks the anxiety levels and reactions of his wife during the exposure. In the next session, she was again asked for the thoughts and levels of anxiety during the observation, husband reported that at first she showed some anger and was looking very anxious while observing the ladies with bindi but when he reminded her about the nature of therapy, she managed to sit there and sometime later became relaxed.
- In the third step of the hierarchy patient was instructed to enter into the cosmetic shop and remain stand there for a short while without purchasing anything and to face the levels of anxiety varying with time. In the session, she was asked to report the anxiety level. She reported that just when she entered the shop she was trying to not get touched with anything and felt like she would lose her control and became very anxious but with self instructions she managed herself to stand there after sometime anxiety level came down and she felt little relaxed.
- In the fourth step, the patient was instructed to enter into the cosmetic shop and to purchase some common items other than ‘Bindi’ . In the next session, husband reported that she was attentively noticing the shopkeeper’s movements. Though, she purchased some ribbons but denied to touch them and asked him to put them in his bag and told him to give only the fixed amount of ribbon’s cost to the shopkeeper so that exchange could not be needed from shopkeeper’s contaminated hands. The husband also observed that during the whole exposure, the patient was looking very distressed and anxious and was involved in safety strategies and managed to calm down only when he reminded her about the process of therapy. The patient was then asked to report her anxiety level in this step of exposure.
- In the fifth step, patient was instructed to go into the market and purchase a packet of small colorful bindi and face the anxiety levels . In the next session, she was asked to express the anxiety and rate it on a scale of 1 to 10. The patient reported that when she was purchasing the bindi, she felt dreadful and thought that she would take bath after returning home. Somehow, she purchased the packet and gave it to the husband to put it in his bag. After returning home, she got involved in her daughter’s work but thoughts of washing and bathing were going on in her mind. Later on, she could not get the time for bathing and she instructed herself to bath in the morning, after this thought she felt very relaxed and had this feeling of winning over her obsessions.
- In the sixth step, patient was instructed to purchase some colorful bindi packets and try to keep them with herself and strictly prevent herself from hand-washing for one hour. In the next session, she reported that this time she was not that anxious while purchasing bindi packets but after putting them in her bags she was trying to avoid getting touched with her daughter and mother in law because her mother in law would enter into the kitchen and contaminate everything. Meanwhile, her daughter ran towards her and hugged her. Immediately, she became very restless and angry with the daughter and thought about to wash her. However, she felt incapacitated as her daughter ran everywhere in the house and touched everything. She got anxious but managed this thought of contamination and decided to not wash anything. After this, she felt relaxed.
- In the seventh step of the hierarchy, the patient was instructed to apply a small bindi on her forehead and restricted to not wash her hands for at least four hours . In the next session, she reported that she applied the bindi and her husband and her mother-in-law were feeling very happy but she felt anxious and closed her fist for not touching anything till hand-washing. After some time, in other household works, she forgot about it but suddenly when she realized that she had applied bindi, she immediately washed her hands but even then kept wearing it for the whole day.
- In the eighth step, the patient was instructed to apply red color velvet medium size Bindi and prevent hand washing for minimum of two hours . In the next session, she reported that now her level of anxiety has fallen down and now she feels less anxious after applying bindi and managed to not wash her hands for two hours without any much restlessness.
- In the ninth step of the hierarchy, the patient was instructed to apply red color velvet medium size Bindi and prevent hand washing for minimum of four hours and try to make herself normal and gradually start touching things in these hours. In the next session, she reported that now she feels capable to face her feelings of disgust with bindi and manages to make her mind for not washing things after getting touched with the bindi. Though some thoughts of contamination keep coming in between but she immediately reminds herself that ‘Bindi’ can’t contaminate anything.
- In the tenth step of hierarchy, the patient was instructed to apply bindi on her forehead and keep some of them in her bag preventing washing her hands for maximum hours possible. In the next session, she reported that now she feels more capable to conquer over her thoughts of contamination and more determined to not washing and cleaning after such obsessions.
With each ERP session, the patient came to realize that the nature of anxiety is that it goes up with the triggering event but with the passage of time, automatically comes down. She also developed the insight that she had fear from the thoughts of contamination and with its associated anxiety more than ‘Bindi’ itself.
After the ERP sessions, the patient was given two booster sessions in which she was taught the ways to deal with the anxiety after the termination of therapy in her day to day life situations. In those sessions, she was asked to imagine her home, her room, and herself with Bindi on her forehead and doing household chores like cooking, cleaning the things, etc. When the patient was asked to express herself during the imagination, she reported that she is feeling more confident now to stick on her thought that bindi can’t contaminate, it’s her idea and there is no use of washing hands and other things because of the fear of contamination. Her husband and mother-in-law were also instructed to remind her again and again about the things she learned during the therapy sessions. After the declaration of the patient that she is feeling better now and ready to face the anxiety on her own, therapy sessions were terminated.
One month later, the patient was contacted for the follow-up and asked about her coping with the anxiety through telephonic conversation. She reported that thoughts of contamination came in her mind but she is in better condition than previous after taking the ERP sessions.
After two months, the patient came for the session again with the complaints that sometimes she became weak and washed her hands with the thought of contamination. After washing, she repented on her behavior which lowers down her confidence in conquering over the illness. Then she was instructed that washing hands strengthens the thought of contamination so she should avoid it as much as possible but this doesn’t mean that she has not gained anything with the therapy, she was reminded about her previous condition that how much it was unbearable for her to even think about the bindi but now she is applying it on her forehead which shows that only the traces of the illness left, most of it is already recovered. In this way, the patient became relaxed and felt more determined to continue with the learnings during the sessions.
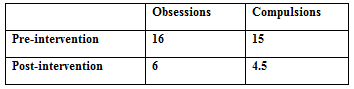
After the termination of the therapy sessions, the patient’s obsessive and compulsive symptoms were found reduced on the Y-BOCS symptom checklist:
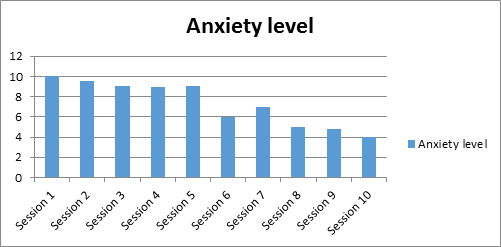
With the graded exposure sessions, her anxiety level also came down from the rating of 10 in the beginning sessions to the rating of 4 in the endings sessions on a scale of 1 to 10.
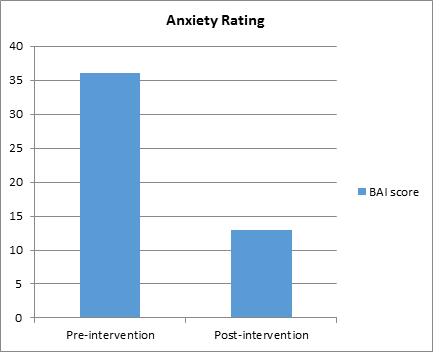
The patient’s BAI score was also fallen down from pre-intervention- 36 (Extreme level of anxiety) to post intervention- 13 (mild level of anxiety) which suggests 36% reduction in the anxiety level of the patient.
Previous research findings considered CBT as the most promising treatment of OCD (Stanley & Turner, 1995; Foa et al, 1999). CBT emphasizes the integration of cognitive-behavioral strategies like discussion techniques (Guided Discovery) and behavioral experiments (ERP) to formulate the problem and direct the treatment. Therapists try to identify the key distorted beliefs along with patients and allow them to test their beliefs which develop and maintain compulsive behaviors. This case identified the contamination with ‘Bindi’ as the pathological belief which was maintaining the compulsive behaviors of washing and cleaning. The cognitive hypothesis of Salkovoskis (1985) proposed that the origin of obsessional thinking lies in normal intrusive ideas, images, thoughts, and impulses which a person finds unacceptable, upsetting, or unpleasant. The occurrence and content of these intrusive cognitions are negatively interpreted as an indication that the person may be ‘responsible for harm’ or ‘prevent the harm’. Such an interpretation is likely followed by emotional reactions such as anxiety or depression. These emotional reactions lead to discomfort and neutralizing (Compulsive) behaviors like washing, cleaning, checking, avoidance of situations related to the obsessive thought, seeking reassurance, and attempts to exclude these thoughts from the mind. The present case supported this hypothesis of Salkovoskis’s model as intrusive thought of the patient was contamination spread by ‘Bindi’ which negatively interpreted as ‘I can avoid the likely harms by avoiding the contamination spread by Bindi’, such negative interpretation was raising her anxiety levels, making her attentive selective towards the ‘Bindi’, maintaining her compulsive acts and complying her to adopt the safety strategies.
Rachman (1983) predicted that behavioral experiments, in which the patient is exposed to the feared object, these intrusive thoughts are challenged by changing the pattern of thinking and behaving. Hodgson & Rachman (1972) initiated the series of clinical studies on patients with contamination and predicted that immediate washing reduces the anxiety. In one of their experimental study, they noted a similar degree of anxiety reduction when the patient was asked not to perform a compulsive act for one hour. They termed this phenomenon as ‘spontaneous decay’ which was established as the basis of ERP. Also, Foa & Kozak (1986) proposed that exposure techniques activate the network of cognitive fear and patients get new experience which is different from the existing pathological beliefs. This case confirmed this hypothesis as the patient initially thought that her exposure with ‘Bindi’ might cause some uncertain consequence with her but prolonged exposures provided her new experience that she could manage with her fear and anxiety which resulted in the improved coping with obsessional beliefs about contamination and urge to wash and clean. Her improved coping is evident in the statistically significant reduction of her scores on the standard measures like the Y-BOCS symptom checklist, BAI, and OBQ.
The results of this case study add on the value of CBT (that involves ERP technique) in the treatment of obsessive thinking related to the ‘fear of contamination’ and compulsive behavior of ‘washing and cleaning’. However, there is a need for more such case studies with more precision and effective treatment designs to provide valuable information related to the nature of OCD and its treatment.
In this case of OCD, patient’s symptoms were reduced to a manageable level and found maintained for two months which provides an evidence of the effectiveness of CBT and ERP technique in the treatment of OCD.
- American psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (DSM-4). 4th ed. Washington, DC. Author. View at Publisher | View at Google Scholar
- American psychiatric Publishing. (2013). Diagnostic and statistical manual of mental disorders; (DSM-5) 5th ed. Washington, DC.. 237-242. View at Publisher | View at Google Scholar
- Abramowitz, J. S. (2001): Treatment of Scrupulous Obsessions and Compulsions Using Exposure and Response Prevention: A Case Report. Cognitive and Behavioral Practice, 8, 79-85 View at Publisher | View at Google Scholar
- Beck, J. S. (2011). Cognitive behavior therapy: Basics and beyond (2nd ed.), New York, NY: The Guilford Press, 19-20 View at Publisher | View at Google Scholar
- Beck, A.T. (1976). Cognitive Therapy and the Emotional Disorders. New York: International Universities Press. View at Publisher | View at Google Scholar
- Beck, A.T., Steer, R.A. (1990).Manual for the Beck Anxiety Inventory. San Antonio, TX: Psychological Corporation. View at Publisher | View at Google Scholar
- Fenske J.N., Schwenk T.L. (2009). Obsessive Compulsive Disorder: diagnosis and management. American Family Physician. 80, 3, 239-45. View at Publisher | View at Google Scholar
- Foa, E. B., Abramowitz J. S, Franklin, M. E, Kozak, M. J., (1999). Behavior Therapy, 30, 717-724. View at Publisher | View at Google Scholar
- Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: exposure to corrective infor- mation. Psychological Bulletin, 99, 20-35. View at Publisher | View at Google Scholar
- Grant, J. E. (2014). Clinical Practice: Obsessive Compulsive Disorder. The New England Journal of Medicine, 371, 7, 646-53. View at Publisher | View at Google Scholar
- Hodgson, R. J., & Rachman, S. (1972). The effects of contamination and washing in obsessional patients. Behavior Research and Therapy, 10, 111-117. View at Publisher | View at Google Scholar
- Obsessive Compulsions Cognitions Working group. (1997). Cognitive Assessment of obsessive compulsive disorder. Behavioral Research and Therapy, 35, 667-681. View at Publisher | View at Google Scholar
- Obsessive Compulsions Cognitions Working group. (1997). Development and initial validation of the obsessive beliefs questionnaire and the interpretation of intrusions inventory: Part 1. Behavioral Research and Therapy, 41, 863-878. View at Publisher | View at Google Scholar
- Rachman, S (1997). A cognitive theory of obsessions. Behavioral research theories. Vol . 35, 9, 793-802 View at Publisher | View at Google Scholar
- Rachman, S. (1983). Irrational thinking with special reference to cognitive therapy. Advances in Behavior Research and Therapy, 1, 63-88. View at Publisher | View at Google Scholar
- Salkovskis, P. M., & Warwick, H. M. (1985). Cognitive therapy of obsessive-compulsive disorder: treating treatment failures. Behavioral Psychotherapy, 13, 3, 243-255. View at Publisher | View at Google Scholar
- Salkovskis, P. M., & Westbrook, D. (1987). Obsessive-compulsive disorder: clinical strategies for improving behavioral treatments. In H. R. Dent, Clinical psychology: research and developments. London: Croom Helm. View at Publisher | View at Google Scholar
- Stanley, M. A., & Turner, S. M. (1995). Current status of pharmacological and behavioral - ment of obsessive-compulsive disorder. Behavior Therapy, 26, 163-186. View at Publisher | View at Google Scholar
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Virginia E. Koenig
Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Delcio G Silva Junior
Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Ziemlé Clément Méda
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

Mina Sherif Soliman Georgy
We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

Layla Shojaie
The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Sing-yung Wu
Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Orlando Villarreal
Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Katarzyna Byczkowska
Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Anthony Kodzo-Grey Venyo
Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Pedro Marques Gomes
Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

Bernard Terkimbi Utoo
This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Prof Sherif W Mansour
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dr Shiming Tang
Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

Raed Mualem
International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Andreas Filippaios
Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dr Suramya Dhamija
Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

Bruno Chauffert
I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

Baheci Selen
"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

Jesus Simal-Gandara
I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

Douglas Miyazaki
We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

Dr Griffith
I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

Dr Tong Ming Liu
I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

Husain Taha Radhi
I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

Tania Munoz
“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

George Varvatsoulias
Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Khurram Arshad
Our collaborations.
Lorem ipsum dolor sit amet, consectetur adipisicing elit. Culpa, repudiandae, suscipit repellat minus molestiae ea.

Case Report: Obsessive compulsive disorder in posterior cerebellar infarction - illustrating clinical and functional connectivity modulation using MRI-informed transcranial magnetic stimulation
Urvakhsh Meherwan Mehta Roles: Conceptualization, Data Curation, Formal Analysis, Funding Acquisition, Investigation, Methodology, Writing – Original Draft Preparation, Writing – Review & Editing Darshan Shadakshari Roles: Data Curation, Investigation, Resources, Writing – Review & Editing Pulaparambil Vani Roles: Data Curation, Investigation, Methodology, Supervision, Writing – Review & Editing Shalini S Naik Roles: Methodology, Project Administration, Writing – Review & Editing V Kiran Raj Roles: Data Curation, Formal Analysis, Visualization, Writing – Review & Editing Reddy Rani Vangimalla Roles: Data Curation, Formal Analysis, Visualization, Writing – Review & Editing YC Janardhan Reddy Roles: Supervision, Writing – Review & Editing Jaya Sreevalsan-Nair Roles: Formal Analysis, Investigation, Visualization, Writing – Review & Editing Rose Dawn Bharath Roles: Conceptualization, Formal Analysis, Investigation, Methodology, Supervision, Visualization, Writing – Review & Editing
This article is included in the Wellcome Trust/DBT India Alliance gateway.
Obsessive Compulsive Disorder, Cerebellar cognitive affective syndrome, Neuromodulation, Functional brain connectivity, Cerebellar infarct, Theta burst stimulation
Revised Amendments from Version 1
The new version provides more clinical details about the patient, in response to the review comments raised. These include details and justifications for past treatment, iTBS treatment details, rationale for performing an MRI scan and follow-up information beyond the earlier reported period of three months.
See the authors' detailed response to the review by Shubhmohan Singh See the authors' detailed response to the review by Peter Enticott
Introduction
Cortico-striato-thalamocortical circuitry dysfunction is central to an integrated neuroscience formulation of obsessive-compulsive disorder (OCD) 1 , 2 . However, more recent large-scale brain connectivity analyses implicate the role of the cerebello-thalamocortical networks also 3 . Here, we report a case of OCD secondary to a cerebellar lesion. We test the mediating role of the cerebellum in the manifestation of OCD by manipulating the frontal-cerebellar network using MRI-informed transcranial magnetic stimulation (TMS).
Case report
A 21-year-old male, an undergraduate student from rural south India, presented to our emergency with suicidal thoughts. History revealed three years of academic decline, pathological slowness in routine activities (e.g., bathing, eating, dressing up, and using the toilet), repetitive ‘just-right’ behaviors (e.g., wiping his mouth after eating, clearing his throat, pulling down his shirt, mixing his food in the plate and walking back and forth until ‘feeling satisfied’). As a result, he spent up to three hours completing a meal or his toilet routines. Before presentation to us, he had received trials with two separate courses of electroconvulsive therapy (ECT) – six bitemporal ECTs at first, followed by nine bifrontal) spaced about two months apart. ECT was prescribed because of a further deterioration in his condition over the prior 18-months, with reduced oral intake, weight loss, grossly diminished speech output, and passing urine in bed (as he would remain in bed secondary to his obsessive ambitendency, as disclosed later). His oral intake and speech output improved with both ECT treatments, only to gradually worsen over the next few weeks. Given the potential catatonic phenomena (withdrawn behaviour and mutism) in the background of ongoing academic decline, slowness and stereotypies, he was also treated with oral olanzapine 20mg for eight weeks and risperidone 6mg for six weeks with minimal change in his slowness and repetitive behaviors. He did not receive any antidepressant medications. Psychotherapy was also not considered given the limited feasibility due to the severe withdrawal and near mutism. We could not elicit any contributory clinical history of prodromal or mood symptoms from adolescence when we evaluated his past psychiatric and medical history. Two months after the last ECT treatment, he presented to our emergency services with suicidal thoughts. He was admitted, and mental status examination revealed aggressive (urges to harm himself by jumping in front of a moving vehicle or touching electric outlets) and sexual obsessions with mental compulsions and passing urine in bed (as he could not go to the toilet in time due to obsessive ambitendency). The Yale-Brown Obsessive-Compulsive Scale (YBOCS) severity score was 29 4 . He had good insight into obsessions, but not the ‘just right’ repetitive behaviors; it was, therefore, challenging to engage him in psychotherapy. We treated him with escitalopram 40mg and brief psychoeducation before being discharged. After three months, his obsessions had resolved, but pathological slowness, ‘just right’ phenomena, and passing urine in bed had worsened (YBOCS score 31).
We then obtained a plain and contrast brain MRI, to rule out an organic aetiology given the atypical nature of symptoms (apparent urinary incontinence) and the poor treatment response. The MRI revealed a wedge-shaped lesion in the right posterior cerebellum, suggestive of a chronic infarct in the posterior inferior cerebellar artery territory ( Figure-1A ). MR-angiogram revealed no focal narrowing of intracranial and extracranial vessels. Electroencephalography, cerebrospinal fluid analysis, autoimmune and vasculitis investigations were unremarkable. Echocardiogram was normal and the sickling test for sickle cell anemia was also negative. We specifically inquired about history of loss of consciousness, seizures or motor incoordination, but these were absent. His neurological examination with a detailed focus on cerebellar signs was unremarkable. The International Cooperative Ataxia Rating Scale (ICARS) score was zero. The Cerebellar Cognitive Affective Syndrome (CCAS) scale revealed >3 failed tests – in domains of attention, category switching, response inhibition, verbal fluency, and visuospatial drawing, suggestive of definite CCAS 5 .
Cerebellar lesion detection ( A & B ), its functional connectivity map ( C ) and MRI-guided transcranial magnetic stimulation delivery ( D ). Average blood oxygen level-dependent (BOLD) signal time-series were extracted from voxels within a binarized lesion-mask that overlapped with the right crus II ( 1A & 1B ). This was used as the model predictor in a general linear model to determine the brain regions that temporally correlated with the lesion-mask using FSL-FEAT 11 . The resultant seed-to-voxel connectivity map (z-thresholded at 4) was used to identify the best connectivity of the seed with voxels in the pre-supplementary motor area (pre-SMA; MNI x=3; y=13; z=58; 1C ). Six-hundred pulses were delivered as triplet bursts at theta frequency and 90% of the resting motor threshold (50 Hz; 2s on; 8s off) using a MagPro X100 (MagVenture, Denmark) device under MR-guided neuronavigation using the Brainsight stereotaxic system (Rogue Research, Montreal, Canada) with a figure-of-eight coil held with the handle in line with the sagittal plane, pointing toward the occiput to stimulate the pre-SMA site ( 1D ).
MRI-informed neuromodulation
Owing to inadequate treatment response and the possibility of OCD secondary to the cerebellar lesion, we discussed with the patient about MRI-informed repetitive transcranial magnetic stimulation (rTMS) and obtained his consent. The presence of a lesion involving a node (cerebellum) within the cerebello-thalamo-cortical circuit – a key pathway for error monitoring 6 and inhibitory control 7 – cognitive processes typically impacted in OCD prompted us to utilize a personalized-medicine approach to treatment. We acquired a resting-state functional-MRI echoplanar sequence (8m 20s; 250-volumes) in duplicate – before, and one-month after rTMS treatment on a 3-Tesla scanner (Skyra, Siemens), using a 20-channel coil with the following parameters: TR/TE/FA= 2000ms/30ms/78; voxel=3mm isotropic; FOV=192*192.
Image processing was performed using the FMRIB Software Library (FSL version-5.0.10) 8 . Figure 1 describes how we obtained a seed-to-voxel connectivity map to identify the best connectivity of the cerebellar lesion-seed with voxels in the pre-supplementary motor area (pre-SMA; MNI x=3; y=13; z=58) – a commonly used site for neuromodulation in OCD 9 . This area demonstrates connections with the non-motor (ventral dentate nucleus) parts of the posterolateral cerebellum 10 and contributes to error processing and inhibitory control along with the cerebellum 7 .
We augmented escitalopram with rTMS, administered as intermittent theta-burst stimulation (iTBS) to the pre-SMA coordinates ( Figure-1D ). Six-hundred pulses were delivered as triplet bursts at theta frequency and 90% of the resting motor threshold (50 Hz; 2s on; 8s off) using a MagPro X100 (MagVenture, Farum, Denmark) device under MR-guided neuronavigation using the BrainSight stereotaxic system (Rogue Research, Montreal, Canada) with a figure-of-eight (MagVenture MCF-B-70) coil held with the handle in line with the sagittal plane, pointing toward the occiput to stimulate the pre-SMA site. We hypothesized that iTBS 12 to the pre-SMA could adaptively engage the cerebellum lesion, with which it shares neuronal oscillation frequencies, and hence improve the disabling symptoms. He received 27 iTBS sessions, once daily over the next month. Following ten sessions, he began to show a reduction in his repetitive behaviors, and by the 15 th session, he acknowledged that his behaviors were irrational. The YBOCS severity score had reduced to 24 (~22.5% improvement), which remained the same, even at the end of 27 sessions of iTBS treatment. There was no change in the CCAS and ICARS scores. The clinical benefits remained unchanged until three months of follow-up. Subsequently, we observed a gradual reversal to pre-TMS symptom severity. Maintenance TMS was suggested but was not feasible due to logistic reasons and therefore he was initiated on oral fluoxetine that was gradually increased to 80mg/day, with which we observed minimal change in symptoms over the next four months.
Post-neuromodulation functional connectivity visualization
The pre- and post-rTMS scans 13 were parcellated into 48-cortical, 15-subcortical, and 28-cerebellar regions as per the Harvard-Oxford 14 and the Cerebellum MNI-FLIRT atlases 15 . Average BOLD-signal time-series from each of these nodes, obtained after processing within FSL version-5.0.10, were then concatenated to obtain a Pearson’s correlation matrix between 91 nodes, separately for the pre- and post-TMS studies.
We analyzed the two 91 × 91 matrices using the Rank-two ellipse (R2E) seriation technique for node clustering 16 ( Figure 2 ). This technique reorders the nodes by moving the ones with a higher correlation closer to the diagonal. Thus, blocks along the diagonal of the matrix visualization show possible functional coactivating clusters.
Rank-two ellipse seriation-based visualization of correlation matrix before ( A ) and after ( B ) rTMS treatment. The dotted-black boxes denote the cerebellar network and other connected networks, where the green boxes show the inter-network overlap. Thus, we see that the overlapped region in ( 2A ) has now transitioned to three different overlapped areas in ( 2B ), which shows the increase in the overlap between modular networks after treatment. Cerebellar nodes are denoted in black, cortical nodes in blue and subcortical nodes in green. The lesion node (right crus II) and the region of neuro-stimulation are given in red; R2E= Rank-two ellipse.
We observed (a) extended connectivity of the cerebellar network after iTBS treatment as evidenced through its diminished modularity – the larger cerebellar cluster/block had an increased overlap with both anterior and posterior brain networks as observed along the diagonal in ( Figure 2B ), and (b) formation of better-defined sub-clusters within the larger cerebellar cluster indicating improved within-network modularity of distinct functional cerebellar networks [e.g., vestibular (lobules IX and X) and cognitive-limbic (crus I/II and vermis)].

Conclusions
We illustrate a case of OCD possibly secondary to a posterior cerebellar infarct, supporting the role of the cerebellum in the pathophysiology of OCD 3 . That OCD was perhaps secondary to the posterior cerebellar lesion is supported by several lines of evidence. Firstly, there seemed to be a possible temporal correlation between the duration of OCD and the chronic nature of the cerebellar lesion. Despite the challenges in inferring a precise temporal relationship based on clinical history, the signal changes with free diffusion and atrophy indicated that the infarct was indeed chronic, supporting the symptom onset at about three years before presentation. Previous studies have indeed reported OCD in posterior cerebellar lesions 17 – 19 . Secondly, the clinical phenotype was somewhat atypical, characterized by severe ambitendency, precipitating urinary incontinence, and poor insight into compulsions along with comorbid CCAS. Thirdly, our patient was resistant to an anti-obsessional medication but improved partially with neuromodulation of the related circuit. The MRI-informed iTBS engaged the lesion-area by targeting its more superficial connections in the frontal lobe. The changes in clinical observations paralleled the changes in cerebellar functional connectivity – enhanced within-cerebellum modularity and expanded cerebellum to whole-brain connectivity.
This report adds to the growing evidence-base for the involvement of the posterior cerebellum in the pathogenesis of OCD. Drawing conclusions from a single case study and the absence of a placebo treatment will prevent any confirmatory causal inferences from being made. The opportunity to examine network-changes that parallel therapeutic response in an individual with lesion-triggered psychiatric manifestations not only helps mapping symptoms to brain networks at an individual level 13 but also takes us a step further to refine methods to deliver more effective personalized-medicine in the years to come.
Data availability
Underlying data.
Harvard Dataverse: PICA OCD Raw fMRI files NII format. https://doi.org/10.7910/DVN/X12BZD 20 .
This project contains the following underlying data:
- postTMS_fmri.nii (raw post TMS fMRI file)
- preTMS_fmri.nii (Raw pre TMS fMRI file)
Reporting guidelines
Harvard Dataverse: PICA OCD case report CARE guidelines for case reports: 13-item checklist. https://doi.org/10.7910/DVN/2XKSXL 21 .
Data are available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication).
Written informed consent for publication of their clinical details and clinical images was obtained from the patient.
Acknowledgments
We thank our patient and his parents for permitting us to collate this data for publication.
- 1. Dougherty DD, Brennan BP, Stewart SE, et al. : Neuroscientifically Informed Formulation and Treatment Planning for Patients With Obsessive-Compulsive Disorder: A Review. JAMA Psychiatry. 2018; 75 (10): 1081–1087. PubMed Abstract | Publisher Full Text
- 2. Rotge JY, Guehl D, Dilharreguy B, et al. : Meta-Analysis of Brain Volume Changes in Obsessive-Compulsive Disorder. Biol Psychiatry. 2009; 65 (1): 75–83. PubMed Abstract | Publisher Full Text
- 3. Sha Z, Edmiston EK, Versace A, et al. : Functional Disruption of Cerebello-thalamo-cortical Networks in Obsessive-Compulsive Disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2020; 5 (4): 438–447. PubMed Abstract | Publisher Full Text | Free Full Text
- 4. Goodman WK, Price LH, Rasmussen SA, et al. : The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989; 46 (11): 1006–1011. PubMed Abstract | Publisher Full Text
- 5. Argyropoulos GPD, van Dun K, Adamaszek M, et al. : The Cerebellar Cognitive Affective/Schmahmann Syndrome: a Task Force Paper. Cerebellum. 2020; 19 (1): 102–125. PubMed Abstract | Publisher Full Text | Free Full Text
- 6. Ide JS, Li CR: A cerebellar thalamic cortical circuit for error-related cognitive control. NeuroImage. 2011; 54 (1): 455–464. PubMed Abstract | Publisher Full Text | Free Full Text
- 7. Norman LJ, Taylor SF, Liu Y, et al. : Error Processing and Inhibitory Control in Obsessive-Compulsive Disorder: A Meta-analysis Using Statistical Parametric Maps. Biol Psychiatry. 2019; 85 (9): 713–725. PubMed Abstract | Publisher Full Text | Free Full Text
- 8. Woolrich MW, Jbabdi S, Patenaude B, et al. : Bayesian analysis of neuroimaging data in FSL. NeuroImage. 2009; 45 (1 Suppl): S173–186. PubMed Abstract | Publisher Full Text
- 9. Gomes PVO, Brasil-Neto JP, Allam N, et al. : A randomized, double-blind trial of repetitive transcranial magnetic stimulation in obsessive-compulsive disorder with three-month follow-up. J Neuropsychiatry Clin Neurosci. 2012; 24 (4): 437–443. PubMed Abstract | Publisher Full Text
- 10. Akkal D, Dum RP, Strick PL: Supplementary Motor Area and Presupplementary Motor Area: Targets of Basal Ganglia and Cerebellar Output. J Neurosci. 2007; 27 (40): 10659–10673. PubMed Abstract | Publisher Full Text | Free Full Text
- 11. Woolrich MW, Ripley BD, Brady M, et al. : Temporal Autocorrelation in Univariate Linear Modeling of FMRI Data. NeuroImage. 2001; 14 (6): 1370–1386. PubMed Abstract | Publisher Full Text
- 12. Huang YZ, Edwards MJ, Rounis E, et al. : Theta burst stimulation of the human motor cortex. Neuron. 2005; 45 (2): 201–206. PubMed Abstract | Publisher Full Text
- 13. Fox MD: Mapping Symptoms to Brain Networks with the Human Connectome. N Engl J Med. 2018; 379 (23): 2237–2245. PubMed Abstract | Publisher Full Text
- 14. Frazier JA, Chiu S, Breeze JL, et al. : Structural brain magnetic resonance imaging of limbic and thalamic volumes in pediatric bipolar disorder. Am J Psychiatry. 2005; 162 (7): 1256–1265. PubMed Abstract | Publisher Full Text
- 15. Diedrichsen J, Balsters JH, Flavell J, et al. : A probabilistic MR atlas of the human cerebellum. NeuroImage. 2009; 46 (1): 39–46. PubMed Abstract | Publisher Full Text
- 16. Chen CH: Generalized Association Plots: Information Visualization via Iteratively Generated Correlation Matrices. Stat Sin. 2002; 12 (1): 7–29. Reference Source
- 17. Schmahmann JD, Sherman JC: The cerebellar cognitive affective syndrome. Brain J Neurol. 1998; 121 (Pt 4): 561–579. PubMed Abstract | Publisher Full Text
- 18. Schmahmann JD, Weilburg JB, Sherman JC: The neuropsychiatry of the cerebellum - insights from the clinic. Cerebellum. 2007; 6 (3): 254–267. PubMed Abstract | Publisher Full Text
- 19. Wolff JEA, Hüttermann U, Askins MA: Quantifying health status outcomes in pediatric medulloblastoma patients. Anticancer Res. 2007; 27 (1B): 523–529. PubMed Abstract
- 20. Mehta U: PICA OCD Raw fMRI files NII format. Harvard Dataverse, V1. 2020. http://www.doi.org/10.7910/DVN/X12BZD
- 21. Mehta U: PICA OCD case report CARE guidelines for case reports: 13 item checklist. Harvard Dataverse, V1. 2020. http://www.doi.org/10.7910/DVN/2XKSXL
Comments on this article Comments (0)
Open peer review.
Competing Interests: No competing interests were disclosed.
Reviewer Expertise: Cognitive neuroscience
- Respond or Comment
- COMMENT ON THIS REPORT
Is the background of the case’s history and progression described in sufficient detail?
Are enough details provided of any physical examination and diagnostic tests, treatment given and outcomes?
Is sufficient discussion included of the importance of the findings and their relevance to future understanding of disease processes, diagnosis or treatment?
Is the case presented with sufficient detail to be useful for other practitioners?
- This is a very interesting case report, even without the intervention component (which itself is a fascinating approach to neuromodulation). I particularly appreciated the approach to regional (SMA)
- This is a very interesting case report, even without the intervention component (which itself is a fascinating approach to neuromodulation). I particularly appreciated the approach to regional (SMA) targeting, which involved resting state fMRI to detect functional connectivity with the affected cerebellar region. The report itself is very clear and well-written.
- ECT appears to have been provided in the context of a depressive episode, but were other (e.g., psychotherapy, pharmacotherapy) treatments initially trialled? It would be useful to present any clinical history from adolescence, although this may not be feasible.
- Please describe the reason for conducting MRI; why was this not undertaken earlier?
- Was iTBS the “standard” course (i.e., 600 pulses, trains comprising 3 pulses at 50 Hz, repeated for 2 seconds at 5 Hz, followed by an 8-second ITI)? How was intensity determined (e.g., 70%RMT, 80%AMT)? Specify the stimulator, coil type, and neuronavigation method.
- Given that the duration of both the cerebellar lesion and OCD symptoms seems quite unclear, it is somewhat difficult to suggest a temporal relationship (as stated in the Conclusion).
- Was the patient followed-up over a longer-term period? I would be interested to know if these improvements are lasting (i.e., longer than 3 months), although again this might not be possible.
Reviewer Expertise: Neuromodulation, psychiatry
- Author Response 11 Sep 2020 Urvakhsh Mehta , Department of Psychiatry, National Institute of Mental Health and Neurosciences, India, Bangalore, 560029, India 11 Sep 2020 Author Response We thank this reviewer for the time taken to provide constructive feedback and the encouraging comments on this report. Competing Interests: None We thank this reviewer for the time taken to provide constructive feedback and the encouraging comments on this report. We thank this reviewer for the time taken to provide constructive feedback and the encouraging comments on this report. Competing Interests: None Close Report a concern Reply -->
Reviewer Status
Alongside their report, reviewers assign a status to the article:
Reviewer Reports
- Shubhmohan Singh , Postgraduate Institute of Medical Education and Research, Chandigarh, India
- Peter Enticott , Deakin University, Geelong, Australia
Comments on this article
All Comments (0)
Competing Interests Policy
Provide sufficient details of any financial or non-financial competing interests to enable users to assess whether your comments might lead a reasonable person to question your impartiality. Consider the following examples, but note that this is not an exhaustive list:
- Within the past 4 years, you have held joint grants, published or collaborated with any of the authors of the selected paper.
- You have a close personal relationship (e.g. parent, spouse, sibling, or domestic partner) with any of the authors.
- You are a close professional associate of any of the authors (e.g. scientific mentor, recent student).
- You work at the same institute as any of the authors.
- You hope/expect to benefit (e.g. favour or employment) as a result of your submission.
- You are an Editor for the journal in which the article is published.
- You expect to receive, or in the past 4 years have received, any of the following from any commercial organisation that may gain financially from your submission: a salary, fees, funding, reimbursements.
- You expect to receive, or in the past 4 years have received, shared grant support or other funding with any of the authors.
- You hold, or are currently applying for, any patents or significant stocks/shares relating to the subject matter of the paper you are commenting on.
Stay Updated
Sign up for content alerts and receive a weekly or monthly email with all newly published articles
Register with Wellcome Open Research
Already registered? Sign in
Not now, thanks
Are you a Wellcome-funded researcher?
If you are a previous or current Wellcome grant holder, sign up for information about developments, publishing and publications from Wellcome Open Research.
We'll keep you updated on any major new updates to Wellcome Open Research
The email address should be the one you originally registered with F1000.
You registered with F1000 via Google, so we cannot reset your password.
To sign in, please click here .
If you still need help with your Google account password, please click here .
You registered with F1000 via Facebook, so we cannot reset your password.
If you still need help with your Facebook account password, please click here .
If your email address is registered with us, we will email you instructions to reset your password.
If you think you should have received this email but it has not arrived, please check your spam filters and/or contact for further assistance.
CLINICAL CASE STUDY article
A clinical case study of the use of ecological momentary assessment in obsessive compulsive disorder.

- Brain, Behaviour and Mental Health Research Group, School of Psychology and Speech Pathology, Curtin University, Perth, WA, Australia
Accurate assessment of obsessions and compulsions is a crucial step in treatment planning for Obsessive-Compulsive Disorder (OCD). In this clinical case study, we sought to determine if the use of Ecological Momentary Assessment (EMA) could provide additional symptom information beyond that captured during standard assessment of OCD. We studied three adults diagnosed with OCD and compared the number and types of obsessions and compulsions captured using the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) compared to EMA. Following completion of the Y-BOCS interview, participants then recorded their OCD symptoms into a digital voice recorder across a 12-h period in reply to randomly sent mobile phone SMS prompts. The EMA approach yielded a lower number of symptoms of obsessions and compulsions than the Y-BOCS but produced additional types of obsessions and compulsions not previously identified by the Y-BOCS. We conclude that the EMA-OCD procedure may represent a worthy addition to the suite of assessment tools used when working with clients who have OCD. Further research with larger samples is required to strengthen this conclusion.
Introduction
Obsessive-Compulsive Disorder (OCD) is a disabling anxiety disorder characterized by upsetting, unwanted cognitions (obsessions) and intense and time consuming recurrent compulsions ( American Psychiatric Association, 2000 ). The idiosyncratic nature of the symptoms of OCD ( Whittal et al., 2010 ) represents a challenge to completing accurate and comprehensive assessments, which if not achieved, can have a deleterious effect on the provision of effective treatment for the disorder ( Kim et al., 1989 ; Taylor, 1995 ; Steketee and Barlow, 2002 ; Deacon and Abramowitz, 2005 ).
Accurately assessing the full range of symptoms of OCD requires reliable and psychometrically sound diagnostic instruments and measures ( Taylor, 1995 , 1998 ; Rees, 2009 ) alongside the standard clinical interview. Although the most commonly used psychometric instrument for assessing OCD, the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) ( Goodman et al., 1989a , b ), has acceptable reliability and convergent validity, it has been criticized by Taylor (1995) for weak discriminant validity. Taylor also highlighted that it remains susceptible to administration variance, relies on client memory recall, and is time consuming to administer. As with all measures completed retrospectively, selective memory biases affect the type of information reported by clients about their symptoms ( Clark, 1988 ; Stone and Shiffman, 2002 ; Stone et al., 2004 ). Glass and Arnkoff (1997 , p. 912) have summarized several disadvantages of structured inventories; first, they contain prototypical statements which may fail to capture the idiosyncratic nature of the client's actual thoughts; second, they can be affected by post-hoc reappraisals of what clients feel, as the data is subject to memory recall biases; and finally they may fail to adequately capture the client's internal dialog due to the limitations of the best fit question structure.
Discrepancies have been reported between data collected in the client's natural environment ( in situ ) and those based on the client's later recall ( de Beurs et al., 1992 ; Marks and Hemsley, 1999 ; Stone et al., 2004) . Such discrepancies may be further affected by factors such as the complexity and diversity of obsessions and compulsions, not to mention the ego-dystonic nature of many OCD clients' obsessional thoughts. It seems likely that clients with distressing ego-dystonic obsessions, for example, those involving sexual, aggressive, and/or religious themes may experience a heightened level of discomfort in reporting their obsessions in a face to face assessment with a clinician, thus reducing their willingness to accurately report ( Taylor, 1995 ; Newth and Rachman, 2001 ; Grant et al., 2006 ; Rees, 2009 ). This may contribute to an underreporting of these obsessions, and hence an inaccurate understanding and a restriction of the clinician's ability to adequately treat the client ( Grant et al., 2006 ; Rachman, 2007 ).
Exposure and response prevention, cognitive therapy, and pharmacological interventions have been shown to be effective in the treatment of OCD ( Abramowitz, 1997 , 2001 ; Foa and Franklin, 2001 ; Steketee and Barlow, 2002 ; Fisher and Wells, 2008 ; Chosak et al., 2009 ). Self-monitoring is a useful therapeutic technique that provides essential information to assist in the development of exposure hierarchies and behavioral experiments used in cognitive therapy ( Tolin, 2009 ). Clients typically observe and record their experiences of target behaviors, including triggers, environmental events surrounding those experiences, and their response to those experiences ( Cormier and Nurius, 2003 ). Such self-monitoring can be used to both assist assessment and/or as an intervention. Cormier and Nurius (2003) explained that the mere act of observing and monitoring one's own behavior and experiences can produce change. As people observe themselves and collect data about what they observe, their behavior may be influenced.
A form of self-monitoring and alternative to the typical clinic-based assessment of OCD is the use of sampling from the client's real-world experiences, a procedure known as Ecological Momentary Assessment (EMA) ( Schwartz and Stone, 1998 ; Stone and Shiffman, 1994 , 2002 ). EMA does not rely on measurements using memory recall within the clinical setting, but rather allows for collection of information about the client's experiences in their natural setting, potentially improving the assessment's ecological validity ( Stone and Shiffman, 2002 ). In situ sampling techniques have been successfully used in psychology, psychiatry, and occupational therapy (for a more detailed account see research by Morgan et al., 1990 ; de Beurs et al., 1992 ; Kamarack et al., 1998 ; Litt et al., 1998 ; Kimhy et al., 2006 ; Gloster et al., 2008 ; Putnam and McSweeney, 2008 ; Trull et al., 2008 ). Generally it is agreed that EMA offers broader assessment within the client's natural environment, as it includes random time sampling of the client's experience, recording of events associated with the client's experience, and self-reports regarding the client's behaviors and physiological experiences ( Stone and Shiffman, 2002 ). Because this assessment method accesses information about the client's situation, the difficulties of memory distortions like recall bias are reduced ( Schwartz and Stone, 1998 ; Stone and Shiffman, 2002 ).
Given that accurate assessment of obsessions and compulsions is a critical aspect of treatment planning and that reliance on self-report and clinician interview has some known limitations, the purpose of this study was to investigate the utility of EMA as a potential adjunct to the conventional assessment of OCD. Specifically, we sought to compare the amount and type of information regarding obsessions and compulsions collected via EMA vs. standard assessment using the gold-standard symptom interview for OCD. As this is a pilot clinical case study, we offer the following tentative hypothesis: (1) EMA will yield additional types of obsessions and compulsions not captured by the Y-BOCS.
Participants and Setting
Participants were recruited through clients presenting to the OCD clinic at Curtin University. They were assessed using the Structured Clinical Interview for DSM-IV (SCID-IV) ( First et al., 1997 ). Inclusion in the study was based on receiving a primary diagnosis of OCD, and a Y-BOCS ( Goodman et al., 1989a , b ) score of more than 16, placing their OCD symptom severity within the clinical range ( Steketee and Barlow, 2002 ). Participants were excluded if they presented with current suicidal ideation, psychotic disorders, apparent organic causes of anxiety, were severely depressed, or if they had an intellectual disability. One potential participant was excluded post evaluation despite meeting the inclusion criteria, as she did not own a mobile phone, and reported having “blackouts” throughout the day. The three participants all had OCD symptoms in the “severe” range according to the YBOCS. In order to ensure that participants remain anonymous, pseudonyms have been used.
Participant A
Mary was a 28-year-old female who lived with her husband and small dog. She reported that for approximately 1 year she had been experiencing distressing intrusive thoughts in relation to harming her loved ones, herself, or her dog; for example, by stabbing, electrocution, or breaking the dog's neck. Mary said that she also had reoccurring thoughts and images that her husband or other family members might die. She reported engaging in some rituals, for example straightening pillows and rearranging tea-towels; but mostly reported using “safety nets” in response to her unwanted cognitions; for example ensuring that she was not alone (to prevent self-harm); avoidance and removal of feared object; extensive reassurance seeking from family members. According to the Y-BOCS measure, Mary scored a subtotal of 14 for Obsessions and a subtotal of 18 for Compulsions, giving an overall total of 32, classifying her symptoms as “severe” ( Steketee and Barlow, 2002 ).
Mary reported that her OCD first occurred after her grandmother passed away about 6 years ago. She explained they had a very close relationship, she said she found it “unbearably distressing” to visit her while she was dying. Mary reported that on one occasion whilst in a coma, her grandmother sat up and gasped, which she found extremely frightening and still remembers it in vivid detail. She reported that she experienced thoughts that her grandmother was in pain and was going “into the unknown, to a scary place.” Mary reported feeling afraid of death and that if someone “even closer” to her died she “would not be able to cope” and that she would “lose control completely.” She stated that her biggest fear was that her husband, mother or father might die. Mary reported that she has been on various anti-depressants for about 10 years. She stated that recently her psychiatrist prescribed Solian (an antipsychotic) which she tried, and found was very effective at blocking out the intrusive thoughts. However, she ceased taking the medication due to nausea.
Participant B
John was a 5-year-old man who lived with his wife and adult son. He reported a long history of distressing intrusive thoughts, and compulsive behaviors. They are summarized in three ways. First, those that relate to religious obsessions, specifically the occult and satanic experiences/fear of being “possessed.” He reported responding to these unwanted cognitions by either washing his hands to cleanse himself; using more than six pieces of toilet paper to wipe after defecating to prevent the devil entering him via his anus; or looking for the number “555,” which represents “God. This is good.” John reported that failing to act in these ways would risk causing harm to his wife and son. Second, those that relate to checking compulsions, specifically when driving, and also checking that doors are locked—which he reported doing 4–12 times per night. He reported that if he thought he heard a “bump” when driving he would have to turn back to check he had not run anyone over, or would seek reassurance from his son or wife if they were passengers in the car with him. He stated that he feared that harm would come to his wife and son if he didn't perform these checks. Third, John said that he arranged shoes so that they were “lined up” and that the clothes in the cupboard were in the “right order.” He also reported the need to compulsively clean his son's bedroom, and that he wouldn't feel “right” until he had done so. According to the Y-BOCS measure, John scored a subtotal of 13 for Obsessions and a subtotal of 15 for Compulsions, giving an overall total of 28, classifying his symptoms as “severe” ( Steketee and Barlow, 2002 ).
John reported that his symptoms have been present for at least the last 29 years. He reported that his OCD first occurred after he had a “break-down” and tried to commit suicide by stabbing himself in the stomach before he turned 25 years of age. In the years leading up to this, John reported two poignant experiences which appear relevant to the development of his symptoms; he reported being involved in the euthanizing of two dogs whilst working as a Ranger's assistant; and that when he was young, he and his girlfriend at the time had a pregnancy termination. John reported feeling that these were “blasphemous” acts, and posed the question “Is God punishing me?” John reported that he had been on several different anti-depressants for about 19 years, with varying degrees of success and side-effects. He reported that he had seen a psychiatrist every 6 weeks for “many years” and finds being able to talk helpful.
Participant C
Paul was a 35-year-old man, who reported distressing intrusive thoughts and images in relation to harm coming to others as a consequence of him not checking that he had done what he is “supposed to do.” For example, he was concerned that someone at work would be harmed if he forgot to adequately cover shifts on the roster (something he is responsible for); or when a client of the service he coordinates was recently given a stereo, Paul reported that he feared that harm would come to the client if he didn't correctly check it to see if it was faulty, something he felt responsible to do.
Paul reported that only his partner knew of his difficulties. He stated that he did not allow his anxiety to interfere too much with his occupational functioning; however he did report that the main reason he does not practice in his profession is because of his OCD. According to the Y-BOCS measure, Paul scored a subtotal of 12 for Obsessions and a subtotal of 13 for Compulsions, giving an overall total of 25, classifying his symptoms as “severe” ( Steketee and Barlow, 2002 ).
Paul reported that his intrusive thoughts have “always been there.” He explained that one of the first clear memories he has of them, was when he was seven years old and he saw the film the “The Omen.” He reported remembering checking his head for the numbers “666.” Additionally, he reported remembering that he was concerned for his mother's safety. He reported that he had never taken medication for his OCD. He stated that he saw two therapists when he lived in the UK at an OCD center in London approximately 18 months ago. Paul said that he did not gain much from the first therapist, but believes that second therapist assisted him to look at his cognitions as “just thoughts.”
Materials and Methods
All screening of participants, interviewing and assessment, as well as administration of the study, was conducted by the first author, who was a provisionally registered psychologist undergoing postgraduate training at the time of the research, and was supervised by the second author, an experienced OCD clinician and academic. Potential participants were recruited from the Curtin OCD clinic. They were screened via telephone to ascertain their suitability for the study. A face-to-face assessment session using the Structured Clinical Interview for DSM-IV (SCID-IV; First et al., 1997 ) was conducted to determine a primary OCD diagnosis, followed by the administration of the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) interview and checklist ( Goodman et al., 1989b ) to identify the participants' obsessions and compulsions and their symptom severity. The Y-BOCS is the most widely used scale for OCD symptoms assessment and is considered by researchers to be the “gold standard” measure for symptom severity ( Deacon and Abramowitz, 2005 ; Himle and Franklin, 2009 ). It consists of two parts; a checklist of prelisted types of obsessions, usually endorsed by the clinician based on disclosures made by the client; and the severity scale which requires the client to rate the severity of their experience by answering the questions based on their recall. Goodman et al. (1989) note that the Y-BOCS has shown adequate interrater agreement, internal consistency, and validity.
Suitable participants then attended a second session where they signed consent forms and were given instructions about the study procedure. During the data collection using the Ecological Momentary Assessment data (EMA-OCD), participants used an Olympus WS-110 digital voice recorder to record their experiences throughout a 12 h period. Participants used their existing mobile phones to receive prompts via the mobile phone Short Message Service (SMS) to record their responses to the research questions. All three participants were then provided with an envelope containing the Olympus WS-100 digital voice recorder, a spare battery, and the participant prompt questions (see Table 1 ).
Table 1. Prompt questions .
Participants were asked to turn their mobile phones on during the data collection day by 10 am, ready to receive their SMS prompts. The researcher manually sent SMS prompts to the participants at random intervals; at least every 2 h (across 1 day, from 10 am to 10 pm), for a minimum of 10 data entries in keeping with research using EMA procedures (see, Stone and Shiffman, 2002 ); asking them to complete their responses to all four questions as details on the EMA-OCD Participant Questions Sheet. Participants were instructed not to respond to the SMS prompts if driving, and were asked to respond as quickly as possible to the prompts. Data was then downloaded from the voice recorder to the researcher's computer, and transcribed. During this process all identifying details were removed. During the debrief session open-ended questions were used to gather as much information as possible regarding the participant's experiences of the study, and suggestions for improvements. During the data collection day the researcher completed a journal to record his observations and reflections related to the use of the EMA. At the completion of the EMD-OCD data collection, each of the participants was provided with a debrief session (Mary by phone, and John and Paul, face to face). The debrief session focused on their experiences of the research and use of the digital voice recorder; and provided the opportunity for them to discuss anything else that arose they wished to tell the researcher. As stated above, the data was downloaded and transcribed by the first author. The Y-BOCS obsession and compulsion categories were used as a framework to compare the data generated from the EMA-OCD procedure. After the complete de-identified data set was tabled, it was provided to a second person who was an expert in OCD for verification of categories. In the case of any discrepancies agreement was reached via consensus.
Number of reported symptoms
Table 2 provides a summary of the frequency and type of symptoms recorded during both the face-to-face session, which will be referred to as the Y-BOCS data and the EMA-OCD phase for the study, which will be referred to as the EMA–OCD data. As can be seen when comparing the data contained in the two columns, there are variations between the Y-BOCS data and the EMA-OCD data. All three participants reported more categories of both obsessions and compulsions in the Y-BOCS data, compared to that reported in the EMA-OCD data.
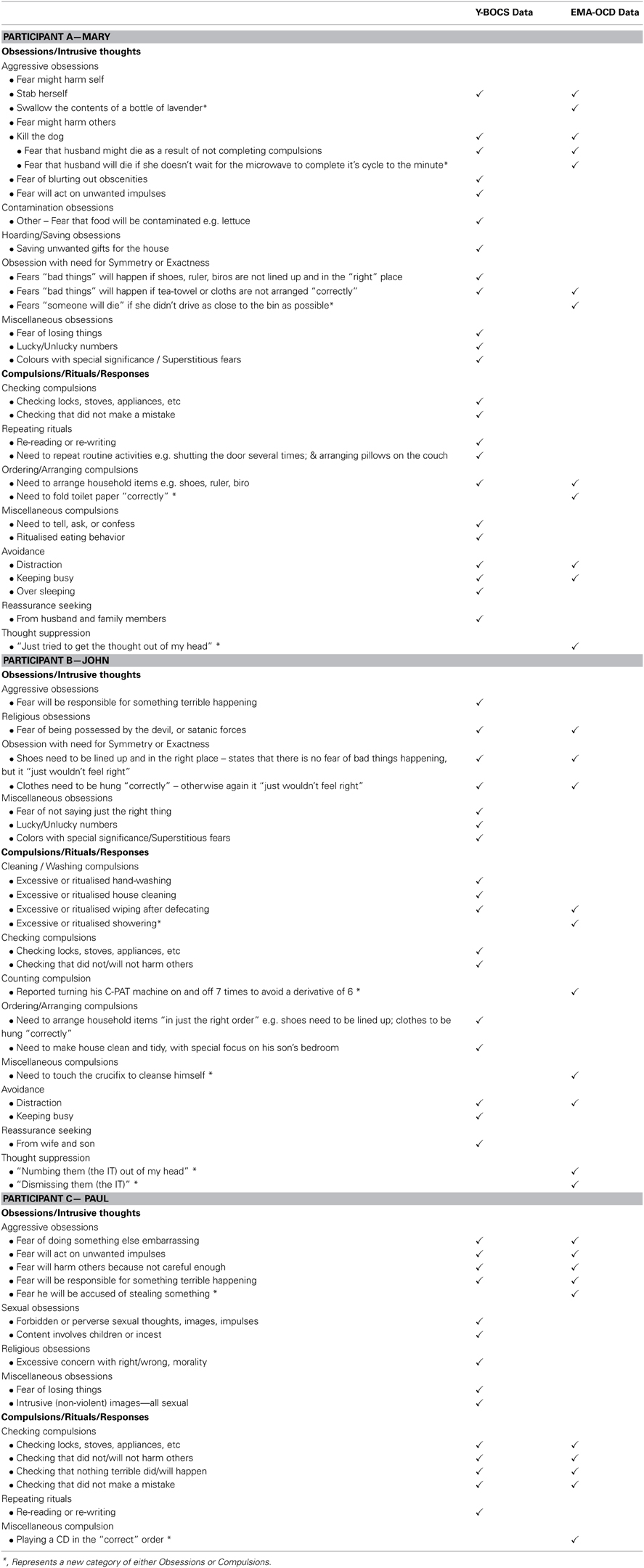
Table 2. Summary by participant of Y-BOCS data and EMA-OCD data .
Mary reported experiencing five categories of Y-BOCS Obsessions and six categories of Compulsions in the Y-BOCS data. In the EMA-OCD data she reported experiencing two categories of Y-BOCS Obsessions, and three categories of Y-BOCS Compulsions. John reported experiencing four categories of Y-BOCS Obsessions and five categories of Compulsions in the Y-BOCS data. In the EMA-OCD data he reported experiencing two categories of Y-BOCS Obsessions, and five categories of Y-BOCS Compulsions. Paul reported experiencing four categories of Y-BOCS Obsessions and two categories of Compulsions in the Y-BOCS data. In the EMA-OCD data he reported experiencing one category of Y-BOCS Obsessions, and two categories of Compulsions.
Comparison of content of symptoms
Both Mary and Paul reported previously unidentified Obsessions or intrusive thoughts in the EMA-OCD data, compared to the Y-BOCS data; and all three participants reported previously unidentified compulsions/rituals/responses in the EMA-OCD data. As can be seen in Table 2 , Mary reported two intrusive thoughts in the EMA-OCD data that were not recorded in the Y-BOCS data. Additionally, she reported a previously unreported obsession under the obsession category Obsession with need for Symmetry or Exactness , not reported in the Y-BOCS data. Mary also reported variations on her compulsive behaviors and the presence of thought suppression not identified during the administration of the Y-BOCS. The EMA-OCD data indicated that John substituted one of his compulsions for an alternative anxiety reducing act, which was not recorded in the Y-BOCS data and suggests the identification of a previously unreported compulsion. Additionally, the EMA-OCD data indicated that John engaged in thought suppression to neutralize his intrusive thoughts. Likewise, John's reported compulsive behaviors also varied between data sets. In the EMA-OCD data he reported three previously unreported compulsive behaviors, and like Mary also the presence of thought suppression. In addition to the above, the EMA-OCD data indicated that John substituted one of his rituals for another, when he touched a crucifix instead of performing his usual hand washing ritual to cleanse him-self of the potential satanic possession. This was not something reported in the Y-BOCS data.
This study investigated the utility of EMA as an adjunct assessment approach for OCD. Each of our study hypotheses was supported. As predicted the EMA procedure resulted in the identification of additional types of obsessions and compulsions not captured by the Y-BOCS interview. The finding that the EMA procedure identifies obsession and compulsion symptoms not captured by the Y-BOCS suggests that further studies in this area are warranted. As a pilot case study we cannot generalize from these initial findings but our results indicate that a larger study replicating the procedure used here, is justified. Importantly, the three participants in our study were representative of quite typical OCD clients in that they had severe levels of symptoms and had OCD for a number of years. The EMA procedure we used was found to be satisfactory to all three participants. Feedback from the participants at the de-briefing session included suggestions that this process would be helpful for therapy because it would provide the therapist and client with rich and current material regarding their symptom patterns. From a clinician's point of view, collecting the EMA data is not onerous because the entries are simply short answers collected on 12 occasions and thus is not a time-consuming exercise.
The EMA procedure as used in this study could provide clinicians with a new method by which to gain a current and accurate snap-shot of clients symptoms as they occur in real-time. This information could augment information gained from standard pencil and paper measures but also provide an “active” process which may help to engage clients in the therapeutic process. It seems likely that using a procedure like EMA with OCD clients will assist in understanding their OCD experiences, and thus assist in generating valuable information, supporting accurate assessment, client conceptualization, and ultimately treatment.
Despite these valuable findings, there are limitations of this study. As a pilot study and exploratory in nature, it is only possible to draw limited interpretations from the data provided. However, the preliminary findings of this study support the benefit of conducting further research into this procedure, where it may be possible to draw more empirically valid findings from a larger and more statistically powerful sample. Second, due to the lack of availability of date stamping, participants were asked to record the time they made each recording. Unfortunately this was not routinely provided by all participants, and hence creates an unanswerable question regarding the accuracy of the data recorded. As Stone and Shiffman (2002) discuss, a potential problem relates to participants recording their data based on their recall of what was occurring at the time of the SMS prompt, rather than immediately. Hence introducing possible memory bias, and undermining the premise of the study. Although this is certainly an unwanted variable, based on the EMA-OCD data provided it seems that except for Mary, both John and Paul responded promptly to the SMS messages, or recorded the time if they didn't. Mary on the other hand, reported during the debrief session that she was unable to record the time for the initial targets, but did so for subsequent SMS prompts. It was not possible to ascertain from her data the delay in time between the first SMS prompts and her recordings. In future applications of this procedure, it is recommended that the device used provides automatic date-stamping to address this limitation. Indeed, it may be possible to adapt the EMA methodology for use with smart phones via a dedicated OCD application.
Concluding Remarks
The findings from this study of three patients with severe OCD suggest that the use of EMA provides important additional information regarding obsessions and compulsions and may thus be a useful adjunct to the clinical assessment of OCD.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the three participants for taking part in this study.
Abramowitz, J. S. (1997). Effectiveness of psychological and pharmacological treatments for obsessive-compulsive disorder: a quantitative review. J. Consul. Clin. Psychol . 65, 44–52. doi: 10.1037/0022-006X.65.1.44
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text
Abramowitz, J. S. (2001). Treatment of scrupulous obsessions and compulsions using exposure and response prevention: a case report. Cogn. Behav. Pract . 8, 79–85. doi: 10.1016/S1077-7229(01)80046-8
CrossRef Full Text
American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders, 4th Edn . Washington, DC: American Psychiatric Association.
Chosak, A., Marques, L., Fama, J., Renaud, S., and Wilhelm, S. (2009). Cognitive therapy for obsessive-compulsive disorder: a case example. Cogn. Behav. Pract . 16, 7–17. doi: 10.1016/j.cbpra.2008.01.005
Clark, D. A. (1988). The validity of measures of cognition: a review of the literature. Cogn. Ther. Res . 12, 1–20. doi: 10.1007/BF01172777
Cormier, S., and Nurius, P. S. (2003). Interviewing and Change Strategies for Helpers: Fundamental Skills and Cognitive Behavioral Interventions . Pacific Grove, CA: Thomson Brooks/Cole.
Deacon, B. J., and Abramowitz, J. S. (2005). The Yale-Brown Obsessive Compulsive Scale: factor analysis, construct validity, and suggestions for refinement. J. Anxiety Disord . 19, 573–585. doi: 10.1016/j.janxdis.2004.04.009
de Beurs, E., Lange, A., and Van Dyck, R. (1992). Self-monitoring of panic attacks and retrospective estimates of panic: discordant findings. Behav. Res. Ther . 30, 411–413. doi: 10.1016/0005-7967(92)90054-K
First, M. B., Spitzer, R. L., Gibbon, M., and Williams, J. B. W. (1997). Structured Clinical Interview for DSM-IV Axis I Disorders Patient Edition (SCID-IP Version 2.0) . New York, NY: Biometrics Research Department, New York State Psychiatric Institute.
Fisher, P. L., and Wells, A. (2008). Metacognitive therapy for obsessive–compulsive disorder: a case series. J. Behav. Ther. Exp. Psychiatry 39, 117–132. doi: 10.1016/j.jbtep.2006.12.001
Foa, E. B., and Franklin, M. E. (2001). “Obsessive-compulsive disorder,” in Clinical Handbook Of Psychological Disorders , ed D. H. Barlow (New York, NY: Guilford Press), 209–263.
Glass, C. R., and Arnkoff, D. B. (1997). Questionnaire methods of cognitive self-statement assessment. J. Consul. Clin. Psychol . 65, 919–927. doi: 10.1037/0022-006X.65.6.911
Gloster, A. T., Richard, D. C. S., Himle, J., Koch, E., Anson, H., Lokers, L., et al. (2008). Accuracy of retrospective memory and covariation estimation in patients with obsessive–compulsive disorder. Behav. Res. Ther . 46, 642–655. doi: 10.1016/j.brat.2008.02.010
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Delgado, P., Heninger, G. R., et al. (1989a). The yale-brown obsessive compulsive scale: ii. validity. Arch Gen. Psychiatry 46, 1012–1016. doi: 10.1001/archpsyc.1989.01810110054008
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., et al. (1989b). The yale-brown obsessive compulsive scale: i. development, use, and reliability. Arch Gen. Psychiatry 46, 1006–1011. doi: 10.1001/archpsyc.1989.01810110048007
Grant, J. E., Pinto, A., Gunnip, M., Mancebo, M. C., Eisen, J. L., and Rasmussen, S. A. (2006). Sexual obsessions and clinical correlates in adults with obsessive-compulsive disorder. Comprehen. Psychiatry 47, 325–329. doi: 10.1016/j.comppsych.2006.01.007
Himle, M. B., and Franklin, M. E. (2009). The more you do it, the easier it gets: exposure and response prevention for OCD. Cogn. Behav. Pract . 16, 29–39. doi: 10.1016/j.cbpra.2008.03.002
Kamarack, T. W., Shiffman, S. M., Smithline, L., Goodie, J. L., Paty, J. A., Gyns, M., et al. (1998). Effects of task strain, social conflict, and emotional activation on ambulatory cardiovascular activity: daily life consequences of recurring stress in a multiethnic adult sample. Health Psychol . 17, 17–29. doi: 10.1037/0278-6133.17.1.17
Kim, J. A., Dysken, M. W., and Katz, R. (1989). Rating scales for obsessive compulsive disorder. Psychiat. Anna . 19, 74–79.
Kimhy, D., Delespaul, P., Corcoran, C., Ahn, H., Yale, S., and Malaspina, D. (2006). Computerized experience sampling method (ESMc): assessing feasibility and validity among individuals with schizophrenia. J. Psychiat. Res . 40, 221–230. doi: 10.1016/j.jpsychires.2005.09.007
Litt, M. D., Cooney, N. L., and Morse, P. (1998). Ecological momentary assessment (EMA) with treated alcoholics: methodological problems and potential solutions. Health Psychol . 17, 48–52. doi: 10.1037/0278-6133.17.1.48
Marks, M., and Hemsley, D. (1999). Retrospective versus prospective self-rating of anxiety symptoms and cognitions. J. Anxiety Disord . 13, 463–472. doi: 10.1016/S0887-6185(99)00015-8
Morgan, J., McSharry, K., and Sireling, L. (1990). Comparison of a system of staff prompting with a programmable electronic diary in a patient with Korsakoff's Syndrome. Int. J. Soc. Psychiatry 36, 225–229. doi: 10.1177/002076409003600308
Newth, S., and Rachman, S. (2001). The concealment of obsessions. Behav. Res. Ther . 39, 457–464. doi: 10.1016/s0005-7967(00)00006-1
Putnam, K. M., and McSweeney, L. B. (2008). Depressive symptoms and baseline prefrontal EEG alpha activity: a study utilizing Ecological Momentary Assessment. Biol. Psychol . 77, 237–240. doi: 10.1016/j.biopsycho.2007.10.010
Rachman, S. (2007). Unwanted intrusive images in obsessive compulsive disorders. J. Behav. Ther. Exp. Psychiatry 38, 402–410. doi: 10.1016/j.jbtep.2007.10.008
Rees, C. S. (2009). Obsessive-Compulsive Disorder: A Practical Guide to Treatment . East Hawthorn, VIC: IP Communications.
Schwartz, J. E., and Stone, A. A. (1998). Strategies for analyzing ecological momentary assessment data. Health Psychol . 17, 6–16. doi: 10.1037/0278-6133.17.1.6
Steketee, G., and Barlow, D. H. (2002). “Obsessive-compulsive disorder,” in Anxiety and its Disorders: The Nature and Treatment of Anxiety and Panic, 2nd Edn . ed D. H. Barlow (New York, NY: Guilford Press), 516–550.
Stone, A., and Shiffman, S. (2002). Capturing momentary, self-report data: a proposal for reporting guidelines. Ann. Behav. Med . 24, 236–243. doi: 10.1207/s15324796abm2403_09
Stone, A. A., Broderick, J. E., Shiffman, S. S., and Schwartz, J. E. (2004). Understanding recall of weekly pain from a momentary assessment perspective: absolute agreement, between- and within-person consistency, and judged change in weekly pain. Pain , 107, 61–69. doi: 10.1016/j.pain.2003.09.020
Stone, A. A., and Shiffman, S. (1994). Ecological momentary assessment (EMA) in behavorial medicine. Ann. Behav. Med . 16, 199–202.
Taylor, S. (1995). Assessment of obsessions and compulsions: reliability, validity, and sensitivity to treatment effects. Clin. Psychol. Rev . 15, 261–296. doi: 10.1016/0272-7358(95)00015-h
Taylor, S. (1998). “Assessment of obsessive-compulsive disorder,” in Obsessive-Compulsive Disorder: Theory, Research, and Treatment , eds R. P. Swinson, M. M. Antony, S. Rachman, and M. A. Richter (New York, NY: Guildford Press), 229–258.
Tolin, D. F. (2009). Alphabet Soup: ERP, CT, and ACT for OCD. Cogn. Behav. Pract . 16, 40–48. doi: 10.1016/j.cbpra.2008.07.001
Trull, T. J., Solhan, M. B., Tragesser, S. L., Jahng, S., Wood, P. K., Piasecki, T. M., et al. (2008). Affective instability: measuring a core feature of borderline personality disorder with ecological momentary assessment. J. Abnorm. Psychol . 117, 647–661. doi: 10.1037/a0012532
Whittal, M. L., Robichaud, M., and Woody, S. R. (2010). Cognitive treatment of obsessions: enhancing dissemination with video components. Cogn. Behav. Pract . 17, 1–8. doi: 10.1016/j.cbpra.2009.07.001
Keywords: obsessive-compulsive disorder (OCD), ecological momentary assessment, ecological momentary assessment data, anxiety disorders, assessment
Citation: Tilley PJM and Rees CS (2014) A clinical case study of the use of ecological momentary assessment in obsessive compulsive disorder. Front. Psychol . 5 :339. doi: 10.3389/fpsyg.2014.00339
Received: 10 March 2014; Accepted: 01 April 2014; Published online: 17 April 2014.
Reviewed by:
Copyright © 2014 Tilley and Rees. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Clare S. Rees, Brain, Behaviour and Mental Health Research Group, School of Psychology and Speech Pathology, Curtin University, Perth, WA, Australia e-mail: [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Clinical Trials
Obsessive-compulsive disorder (ocd).
Displaying 6 studies
The purpose of this study is to examine the effectiveness of parent coached exposure therapy (PCET) through baseline comparisons, to compare effectiveness of individual PCET and individual standard cognitive behavioral therapy (CBT), to compare efficiency of individual PCET and individual standard CBT, to compare effectiveness of group intensive PCET, individual PCET, and individual standard CBT, and acceptability.
This study will evaluate the safety and effectiveness of deep brain stimulation in treating people with severe and otherwise treatment-resistant obsessive-compulsive disorder.
Cognitive Behavioral Therapy with fear provoking exposures is the most effective therapy for anxiety disorders. Investigators aim to enhance this therapy with the use of virtual reality exposures and to make therapy more available and accessible for patients with anxiety disorders. The societal benefit of increased access to therapy is that, if successful, it will increase the number of patients who receive appropriate treatment for an anxiety disorder.
The purpose of this study is to gather information from patients and parents with regard to the usability of a web based module for psychoeducation (education on how to deal with a mental health condition) and adequacy of content coverage.
The purpose of this study is to evaluate the randomized controlled mixed methods of a Virtual Reality (VR) exposure therapy system in patients with anxiety and obsessive compulsive disorders.
The purpose of this study is to evaluate the long-term impact of treatment with sertraline on aspects of cognitive, emotional and physical development and maturation at puberty, in pediatric subjects ages 6 to 16 years (inclusive) with a diagnosis of anxiety disorder, depressive disorder or obsessive compulsive disorder.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
- International edition
- Australia edition
- Europe edition

I have OCD. Some cognitive behavioral therapy techniques were totally wrong for me
Many practitioners consider CBT the gold standard of therapy, but does it work for everyone?
T he first time I learned about cognitive behavioral therapy (CBT), I felt the pleasure of recognition and of superiority. I was in high school, and it would be years before I visited a therapist of any kind, but from what I gathered online, CBT consisted of what I was already doing.
The modality grew from a core belief that irrational thoughts are responsible for emotional suffering, according to Rachael Rosner, a historian writing a biography of Aaron Beck, the father of CBT. It followed that changing these thoughts could alleviate the distress.
Perhaps you’re afraid that your headache is a sign of a brain tumor. The CBT “ thought record ” technique might advise you to gather the facts for and against this fear. Is there a family history of brain tumors? Could the headache be caused by dehydration? Then, you reframe it into a more realistic, and presumably less panicked, position.
This back-and-forth volley already described my inner monologue. Years later, I chose for my first therapist one who practiced an old-school form of CBT that reinforced these habits.
It was easy to find such a therapist. Though exact statistics are scarce, CBT is a common modality. Many practitioners consider it the gold standard of psychotherapy and use it for conditions including anxiety and depression. By 2002, the Washington Post was claiming : “For better or worse, cognitive therapy is fast becoming what people mean when they say they are ‘getting therapy’.”
Its concepts “are very mainstream now”, says Sahanika Ratnayake, a philosopher of medicine and psychiatry. “You hear people talking about ‘cognitive distortions’ and ‘reframing your thoughts’ and this idea that how you think about something changes how you feel about it.”
Yet despite being fluent in these techniques, I remained trapped in rumination. Knowing all the cognitive distortions – types of negative bias or irrational thinking – didn’t lessen the worry. No matter how much evidence I gathered to prove that a worry was unlikely, I couldn’t forget that improbable things do happen. People were struck by lightning, planes did crash, headaches did turn out to be tumors. Eventually, I switched to psychodynamic therapy (more focused on feelings, more helpful for me) but continued my inner debate tournament.
Then, in my 30s, I was diagnosed with obsessive compulsive disorder (OCD), a condition marked by intrusive thoughts and physical or mental compulsions to get rid of the thoughts. This delay wasn’t uncommon: diagnosing OCD can take up to 14 to 17 years , in part because it can be hard to differentiate from other disorders such as anxiety. During that time, those thought-challenging techniques can backfire. They did for me.
T he story of modern CBT is, in part, the story of being in the right place at the right time: the US in the 1980s. After the Diagnostic and Statistical Manual of Disorders III, the handbook for diagnosing mental disorders, came out in 1980, the National Institute of Mental Health started requiring that researchers conduct randomized controlled trials for therapy if they wanted funding. By then, Rosner says, Beck had already created a manual for CBT so that it could be standardized and studied in this way. This meant CBT therapists could adapt quickly to the new rules, and the techniques took off.
As insurance companies warmed to CBT, therapists developing new modalities liked to associate with CBT too, partly so these forms could also be covered by insurance, according to Ratnayake. Today, CBT is a broad label that can include mindfulness skills and distress tolerance skills, for instance.
Still, it’s the original ideas around adapting irrational thoughts – the “cognitive” part of CBT – that seem to have trickled most into the mainstream. Behavioral and exposure-based CBT techniques are effective, but therapists can be less likely to use these methods , says Dean McKay, a psychology professor at Fordham University. Articles mentioning CBT tend to emphasize the “distorted thinking” aspect, as do most free worksheets – all contributing to the mistaken idea that CBT is primarily about being rational.
Cognitive techniques work for many. But “the typical OCD sufferer already knows the evidence”, adds McKay, who has researched the potential harms of CBT-type interventions . For them, evidence-gathering becomes just “another form of reassurance”. Reassurance (“of course you won’t die after eating food off the ground”) helps people with OCD feel better in the short term but reinforces the fear long term (“what if I’m the freak exception who will die?”), so they end up needing more and more comfort.
Katie O’Dunne, a minister and interfaith chaplain with OCD, experienced a compulsive cycle of reassurance related to intrusive fears about hurting others. Her therapist asked O’Dunne to list all the great things she’d done and remember that she was a nice person. It worked, briefly. Then her brain would start circling the same questions again: “It made the intrusive thoughts stronger because they would come back and find new ways to poke holes in the logic.”
O ddly enough, the first-line treatment for OCD is a form of CBT – just not the type that many would associate with the label. The difference in approach is clear in these practice phrases from a guidebook for people with OCD : There is no way I can guarantee I won’t stab my husband. Despite my best efforts, my neglect might cause a fire at work. I can’t be sure that my spouse will remain faithful to me.
This type of treatment, called exposure and response prevention (ERP), doesn’t try to dispute thoughts. It encourages patients to expose themselves to fears, either in a real or imagined situation , accept that it could happen – and not do anything to relieve the fear. Instead of reaching for the reams of evidence that you won’t stab your husband, live with the possibility that you might.
after newsletter promotion
To me, this approach was more helpful. As someone who would obsess over the 0.0001% chance I could be struck by lightning , acknowledging that chance feels like facing reality.
When I stopped trying to think rationally, my mind felt freed. I no longer needed to constantly remind myself to stop catastrophizing. I had permission to stop sifting through piles of research in a search for certainty. Instead, I started practicing ERP whenever the fears began. I can never be 100% certain that I won’t develop my mother’s disease , I would think, despite “knowing” that her illness was due (almost certainly) to bad luck.
At first, I flinched at the idea and pressure grew in my chest. But with time and repetition, my mind became less prone to these looping thoughts. And I began thinking about how this approach could help beyond OCD.
O ’Dunne, the chaplain, leads online groups for people navigating faith and OCD, but the community has started to include those without the disorder. “A lot of people who have navigated religious trauma or spiritual abuse or really rigid spiritual communities have been told for such a long time that they have to have certainty,” she says. “It’s been such a harmful dynamic.” To her, ERP isn’t just a treatment but rather “a beautiful, healthy lifestyle of uncertainty”.
In fact, “ intolerance of uncertainty ” is correlated with many conditions, including generalized anxiety, OCD, social anxiety and eating disorders, according to Mark Freeston , a psychologist at Newcastle University who has studied the concept since the 1990s. Instead of focusing on cognitive distortions, Freeston and collaborators help patients accept physical signals of uncertainty.
For example, patients play a children’s game where they pass around a spring-loaded toy. Because people know the outcome – the toy pops up – but not when it’ll happen, they learn to identify “temporal uncertainty” and realize that the feeling doesn’t mean a situation is dangerous. They can experience uncertainty and still be OK. In a study of group treatment that Freeston and his collaborators plan to submit for publication, they found that “making friends with uncertainty” helps decrease anxiety, even if the treatment never addresses a specific worry.
In the end, it’s not that challenging one’s thoughts doesn’t work (it can) or that behavioral strategies work for everyone (they won’t). Some people respond to evidence; they feel its rational force and are comforted. Others may prefer art therapy or internal family systems , a protocol that asks clients to work with different “parts” of their psyche. Approaches that involve analyzing the past can bring insight for some; for others, including people with OCD, focusing on the origin of intrusive thoughts can distract from getting better.
There are many reasons we might suffer, and no approach works for everyone – but for myself and many, with and without OCD, the cognitive form of CBT was the one most often held up to be obviously and generally helpful. For me, this led to simplistic and misguided understandings, both of CBT itself and of what I needed. I loved CBT’s cognitive strategies because the self-questioning came naturally, but for precisely that reason, I needed a treatment that did the opposite. I just wish it hadn’t taken so long.
- Well actually
- Mental health
- Obsessive-compulsive disorder
Most viewed
- Open access
BMC Psychiatry
61 Accesses
Metrics details
Peer Review reports
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
[Intensive exposure treatment for obsessive compulsive disorder in old age]
- PMID: 38650516
The absence of treatment studies for obsessive compulsive disorder (OCD) in older adults and the fact that OCD typically starts at a young age and often follows a chronic, fluctuating course quickly leads to therapeutic nihilism for older adults with OCD. In this case report, we present a 72-year-old man with OCD symptoms from the age of 35, who has only been treated with medication and psychotherapy for a recurrent depressive disorder. After a short, intensive exposure and response prevention treatment (four days in two weeks), the OCD symptoms and the depressive symptoms were fully in remission and all medications (venlafaxine, olanzapine, depakine) were discontinued. Treatment gains were maintained with persistent remission until 18 months follow up. This case report shows that a comorbid depressive disorder may lead to undertreatment of OCD. It also shows that long standing OCD can be successfully treated in older adults.
Publication types
- Case Reports
- English Abstract
- Depressive Disorder / drug therapy
- Depressive Disorder / therapy
- Implosive Therapy / methods
- Obsessive-Compulsive Disorder* / therapy
- Treatment Outcome
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.
- Cite this article
You have full access to this open access article

146 Accesses
Explore all metrics
Similar content being viewed by others

Treatment of Scrupulosity in Childhood Obsessive-Compulsive Disorder
Avoid common mistakes on your manuscript.
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Case Study Details. John is a 56-year-old man who presents to you for treatment. His symptoms started slowly; he tells you that he was always described as an anxious person and remembers being worried about a lot of things throughout his life. For instance, he reported he was very afraid he'd contract HIV by touching doorknobs, even though he ...
1. Introduction. According to the DSM-5, Obsessive-Compulsive Disorder (OCD) is characterized by the presence of obsessions and/or compulsions. Obsessions are recurrent and persistent thoughts, urges, or images that are experienced as intrusive and unwanted, whereas compulsions are repetitive behaviors or mental acts that an individual feels driven to perform in response to an obsession or ...
The client Hope provides a good example of a very positive outcome from sustained, multifaceted psychotherapy with a 30-year-old woman presenting with obsessive compulsive disorder (OCD), fear of flying, panic disorder without agoraphobia, nightmare disorder, and a childhood history of separation anxiety disorder. Based on ratings at the beginning of therapy and end of therapy on a structured ...
The psychological treatment of choice for OCD, in both adults and children and backed by numerous clinical trials, is cognitive-behavioral therapy (CBT), particularly exposure with response prevention (EX/RP) [ 45 ]. It is superior to medications alone, with effect sizes ranging from 1.16-1.72 [ 46, 47 ].
Obsessive-compulsive disorder (OCD) is a chronic, distressing and substantially impairing neuropsychiatric disorder, characterized by obsessions or compulsions. The current case describes a 44-year-old adult female diagnosed with OCD. The patient had an incomplete response to several SSRIs alone during her past treatment, and led a poor-quality ...
Treatment of OCD: A Case Study of a Man with Checking Associated with Not-Just-Right Experiences Obsessive Compulsive Disorder (OCD) is defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-V; American Psychiatric Association, 2013) as the
"We found that the more OCD-specific form of therapy, the one based on exposure to the focus of obsession and compulsion, was better for relieving symptoms, which in itself is a valuable finding from this head-to-head randomized comparison of two treatment options," says Stephan Taylor, M.D., the study's senior author and a professor of psychiatry at Michigan Medicine, U-M's academic ...
Obsessive-compulsive disorder (OCD) is the fourth most common mental illness worldwide, with 1%-3% prevalence in the general population. 1 The hallmark of OCD is the presence of recurrent or persistent thoughts, impulses, or images (obsessions) experienced as distressing by the person and are attempted to be suppressed by performing repetitive mental or behavioral acts (compulsions). 2 ...
The mean age at the onset of OCD ranges from 22 to 36 years, with the disorder developing in only 15 percent of patients older than 35 years. 3 Men tend to have an earlier age at onset than women ...
Obsessive-compulsive disorder (OCD) is a mental disorder where people feel the. need to check things repeatedly, perform certain routines repeatedly (called "rituals"), or have. certain thoughts repeatedly (called "obsessions"). Obsessive compulsive disorder (OCD) is a. debilitating neuropsychiatric disorder with a lifetime prevalence of 2 to ...
Psych2021, 3 891. there is physical proximity to individuals categorized as a potential risk group, leading to the adoption of protective measures that are often maladaptive and often associated with comorbidities such as anxiety disorders or depressive mood [6]. During this pandemic, the rapid and global spread of information coupled with the ...
Introduction: This is a case report of a middle-aged woman, who was experiencing "obsessive" thoughts related to the "Bindi" (decorative piece wear by women on the forehead) and cleaning "compulsions".Present case report discusses the patient's assessment, case formulation, treatment plan and the effectiveness of the CBT and ERP sessions in reducing OCD symptoms.
One study suggested that good quality case formulation in the early stages of CBT for OCD improved the working alliance and reduced patients' distress, although there was no association with treatment outcome (Nattrass et al., Reference Nattrass, Kellett, Hardy and Ricketts 2015).
Treatment implications. This case study illustrated CBT treatment for a 10-year-old girl with contamination-related obsessions. ERP is a highly effective treatment for children and adolescents with OCD (Freeman et al., 2018). Treatment should be tailored to a child's developmental stage for it to be tolerable, understandable, and beneficial.
Methods: A case report of a young adult male describing obsessive-compulsive symptoms, probably secondary to an infarct in the cerebellar right crus II, combined with an examination of behavioral and functional connectivity changes following TMS treatment. Results: Obsessions, compulsions, and pathological slowing were observed in the ...
Cognitive-behavioral therapy (CBT) remains one of the most effective treatments for obsessive-compulsive disorder (OCD). In this update of a previous article (), we define CBT, review the evidence for the efficacy of CBT for OCD, provide a case example and sample treatment plans, and discuss family factors that affect treatment outcome.In addition, we discuss group and family-based modalities ...
Paediatric obsessive compulsive disorder [] is a chronic condition with lifetime prevalence estimates ranging from 0.25 [] to 2-3% [].OCD is often associated with severe disruptions of family functioning [] and impairment of peer relationships as well as academic performance [].Mean age of onset of early onset OCD is 10.3 years, with a range from 7.5 to 12.5 years [] or at an average of 11 ...
Accurate assessment of obsessions and compulsions is a crucial step in treatment planning for Obsessive-Compulsive Disorder (OCD). In this clinical case study, we sought to determine if the use of Ecological Momentary Assessment (EMA) could provide additional symptom information beyond that captured during standard assessment of OCD.
Abstract. A patient's own account of her obsessive-compulsive disorder is presented. She describes her distressing experiences, the impact of the disturbance on her and her family's life and her subsequent improvement using the technique of exposure and response prevention. The treatments available are discussed and the benefits of self ...
This study will evaluate the safety and effectiveness of deep brain stimulation in treating people with severe and otherwise treatment-resistant obsessive-compulsive disorder. Virtual Reality System to Increase Access to Exposure Therapy for Anxiety and OCD Rochester, MN. Cognitive Behavioral Therapy with fear provoking exposures is the most ...
This delay wasn't uncommon: diagnosing OCD can take up to 14 to 17 years, in part because it can be hard to differentiate from other disorders such as anxiety. During that time, those thought ...
Participants and procedure. The present study involved secondary data analysis of the previously published trial that that demonstrated that D-Cycloserine (DCS) did not improve treatment cET outcomes for difficult-to-treat OCD patients [].The patent study used a triple blind, three-armed, placebo-controlled design in which patients within each stratum were randomized to 100 mg D-Cycloserine ...
Treatment studies have also examined the efficacy of ERP relative to and in combination with medication. ... The case of OCD and PTSD. Annu Rev Clin Psychol. 2016; 12:1-28 ... Tart CD, Cottraux J, Powers MB, Smits JA, et al. Behavioral versus cognitive treatment of obsessive-compulsive disorder: An examination of outcome and mediators of ...
The absence of treatment studies for obsessive compulsive disorder (OCD) in older adults and the fact that OCD typically starts at a young age and often follows a chronic, fluctuating course quickly leads to therapeutic nihilism for older adults with OCD. In this case report, we present a 72-year-old man with OCD symptoms from the age of 35 ...
One of the most effective treatments for Obsessive Compulsive Disorder (OCD) is Cognitive Behavior Therapy (CBT) with Exposure and Response Prevention (ERP). Cognitive Behavioral Therapy (CBT) is a treatment that teaches clients specific skills and focuses on the ways that a person's cognitions (i.e., thoughts), emotions, and behaviors are connected and affect one another.
"Scrupulosity" is a common but understudied subtype of obsessive-compulsive disorder (OCD) characterized by religious obsessions and compulsions. Although scrupulosity is a common manifestation of OCD, it has not been adequately addressed in treatment studies. The aim of this study was to understand the conceptual nuances of scrupulosity, its diagnosis, the unique differences in ...
Other promising results in treatment-resistant OCD for protocols targeting OFC and other cortical regions, such as dorsolateral prefrontal cortex and dorsomedial prefrontal cortex, are found in case reports and small uncontrolled studies and have to be confirmed in well designed trials (Brunelin et al., 2018; Rachid, 2019).
It's normal for children of all ages to develop a few habits or rituals to help ease the steep learning curve of growing up. What sets OCD apart is the intensity and rigidity of the thoughts and rituals. Rather than helping a child cope, these behaviors interfere with their daily life. Eventually, OCD begins to hinder a child's development.
Perceptual consequences of online group speech treatment for individuals with Parkinson's disease: A pilot study case series. ... GMG was responsible for study conceptualisation, recruitment of speakers with PD, remote voice recordings, treatment cosupervision, data organisation and analysis, and manuscript elaboration and editing. ...
Obsessive-compulsive disorder (OCD) is a clinically heterogeneous disorder with many possible subtypes.[] The lifetime prevalence of OCD is around 2-3%.[] Evidence points to a bimodal distribution of the age of onset, with studies of juvenile OCD finding a mean age at onset of around 10 years, and adult OCD studies finding a mean age at onset of 21 years.[2,3] Treatment is often delayed in ...