Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 12, Issue 7
- Emotional impact on healthcare providers involved in medical assistance in dying (MAiD): a systematic review and qualitative meta-synthesis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-2445-1466 Saumil Yogendra Dholakia 1 ,
- Alireza Bagheri 2 ,
- Alexander Simpson 3
- 1 Department of Mental Health, The Ottawa Hospital , University of Ottawa , Ottawa , Ontario , Canada
- 2 Research affiliate Center for Healthcare Ethics , Lakehead University , Thunder Bay , Ontario , Canada
- 3 Forensic Psychiatry , Centre for Addiction and Mental Health , Toronto , Ontario , Canada
- Correspondence to Dr Saumil Yogendra Dholakia; saumil.dholakia{at}mail.utoronto.ca
Background Medical assistance in dying (MAiD) traverses challenging and emotionally overwhelming territories: healthcare providers (HCPs) across jurisdictions experience myriad of affective responses secondary to possible tensions between normative and interwoven values, such as sanctity of life, dignity in death and dying and duty to care.
Objective To determine the emotional impact on HCPs involved in MAiD.
Methods Inclusion restricted to English language qualitative research studies from four databases (OVID Medline, EMBASE, CINAHL and Scopus), from beginning until 30 April 2021, and grey literature up to August 2021 were searched. Key author, citation and reference searches were undertaken. We excluded studies without rigorous qualitative research methodology. Included studies were critically appraised using the Joanna Briggs Institute’s critical appraisal tool. Analysis was conducted using thematic meta-synthesis. The cumulative evidence was assessed for confidence using the Confidence in the Evidence from Reviews of Qualitative Research approach.
Results The search identified 4522 papers. Data from 35 studies (393 physicians, 169 nurses, 53 social workers, 22 allied healthcare professionals) employing diverse qualitative research methodologies from five countries were coded and analysed. The thematic meta-synthesis showed three descriptive emotional themes: (1) polarised emotions including moral distress (n=153), (2) reflective emotions with MAiD as a ‘sense-making process’ (n=251), and (3) professional value-driven emotions (n=352).
Discussion This research attempts to answer the question, ‘what it means at an emotional level’, for a MAiD practitioner. Legislation allowing MAiD for terminal illness only influences the emotional impact: MAiD practitioners under this essential criterion experience more polarised emotions, whereas those practising in jurisdictions with greater emphasis on allaying intolerable suffering experience more reflective emotions. MAiD practitioner’s professional values and their degree of engagement influence the emotional impact, which may help structure future support networks. English language literature restriction and absence of subgroup analyses limit the generalisability of results.
- medical ethics
- medical law
- international health services
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. Data set 'Codes and themes-qualitative analysis_MAiD_HCP_emotional impact' submitted and published at ZENODO and is available at DOI: 10.5281/zenodo.6778236. No unpublished data.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2021-058523
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
An eligibility criteria and subsequent search strategy that focuses on emotional impact of medical assistance in dying (MAiD) on healthcare providers (HCPs) with qualitative research methodology.
Use of Joanna Briggs Institute’s critical appraisal tool for assessment of risk of bias and use of the Confidence in the Evidence from Reviews of Qualitative Research approach for assessing the methodological limitations, relevance, coherence and adequacy of the evidence after completion of meta-synthesis.
Qualitative signals of absence of subgroup analysis, eligibility criteria limited to published English language literature and fast-moving pace of research on emotional impact of MAiD on HCPs likely contribute to significant publication bias.
Generalisability of evidence limited by presence of selection bias in included studies.
Introduction
Medical assistance in dying (MAiD) poses ethically complex challenges that can be a major source of distress to participating healthcare providers (HCPs)—especially since MAiD may involve navigating conflicting personal and professional values. These values are contextual, dynamic and often not in alignment with each other; for example, professional values of duty to care and reducing suffering in case of terminal illness through MAiD may conflict with the moral value of preserving sanctity of human life, as the later may involve forbidding any action that hastens a patient’s death in the dying process. 1 2 In the context of assisted death, an HCP often has to navigate value conflicts between respect for autonomy and patient’s right to self-determination versus respect for individual human life, and human life in general. Except for Switzerland, all other countries require HCPs to be at the forefront in discussing and executing eligible requests for assisted death within their defined jurisdictions. 3
Assisted death in selected jurisdictions: overview and current status
The number of jurisdictions across the world with medically assisted death legislation continues to grow. Switzerland, Netherlands, Belgium, Luxembourg, Canada, besides jurisdictions in the USA (Oregon, Vermont, California, Washington State, Colorado, the District of Columbia, Hawaii, Maine and New Jersey) alongside the states of Victoria, Tasmania and South Australia in Australia and Columbia in South America, and most recently Spain and New Zealand, have legalised medically assisted death in some form. 3 4 Assisted death legislations in Canada, the State of Victoria in Australia and the Benelux countries include both assisted suicide and euthanasia. Jurisdictions in the USA and Switzerland allow only assisted suicide.
Broadly speaking, the ‘Benelux’ countries ( Be lgium, Ne therlands and Lux embourg) have less restrictive rules in place for MAiD than the American jurisdictions that permit this practice. For example, Benelux countries allow advanced directives, and terminal of illness is not a requirement for MAiD eligibility in Belgium and Netherlands. Jurisdictions in the USA, on the other end, have strict eligibility criteria that the illness must be terminal and there must be some timeline to foreseeability of natural death—commonly 6 months in most jurisdictions.
Intact decision-making capacity translating to ability to give informed consent for MAiD, voluntariness of request and suffering from a terminal illness are the mainstay of the eligibility criteria for MAiD, with each criterion receiving variable emphasis, depending on the legislative jurisdiction. For example, ‘reasonable foreseeability of natural death’ criterion was removed from Canada’s MAiD eligibility criteria following recent changes in the legislation. 5–8
HCPs and MAiD: current knowledge and knowledge gaps
From an ethics perspective, among the HCPs, the physician’s role in providing MAiD is perhaps the most ambiguous. Historically, medicine as a profession is rooted in the ethical principle of ‘first, do no harm’ while providing care. While this is true, medical futility and the sense of powerlessness and loss of control at end of life are a reality in modern medical practice, which is often reflected as physician ambivalence to participate in MAiD. 9–11
While this sense of moral ambiguity may distance physicians from the practice of MAiD, nurses also share the complex attitudes and polarised feelings towards MAiD. 12 This complexity is often due to the dual role that nurses play in most healthcare systems around the world: on one end, they act as a strong advocate for patient’s wishes, whereas on the other end, they only have a supportive role in medical decision-making process. A recent synthesis of qualitative studies describing registered nurses’ experiences with MAiD from Belgium, Netherlands and Canada showed that while the nurses played a central role in providing important ‘wrap-around’ care for patients and family, their participation in MAiD required significant moral work. 13
A recent scoping review exploring the challenges faced by HCPs while handling MAiD requests found lack of clear guidelines/protocols, role ambiguity, difficulties in evaluating capacity/consent, conscientious objection, lack of interprofessional collaboration and difficulties in assessing nature and severity of suffering as major barriers in developing comprehensive care models for implementation of MAiD. 14 Furthermore, the scoping review also pointed out that HCPs need substantial degree of time and emotional commitment to participate in a MAiD request. A scoping review and thematic meta-synthesis of qualitative studies exploring HCPs’ attitudes towards assisted death practices in Belgium, Netherlands, Israel, Australia, Germany and the USA showed that their attitudes were shaped by a deep sense of moral responsibility and contextual care relationships. 15
This empirical evidence provides valuable insights on experiences and attitudes of HCPs towards MAiD; however, the nature and extent of emotional impact remains unexplored. Preliminary evidence suggests that the shift away from the medicine’s fundamental values of cure/control of disease to hastening death with the aim of alleviating intolerable suffering can have significant emotional effects on participating HCPs. These can range from feeling overwhelmed with a sense of powerlessness on one end, to a rewarding and a positive experience on the other. 16 17
To determine the emotional impact on HCPs involved in MAiD.
Search strategy, screening and eligibility criteria
The inclusion and exclusion criteria were developed in line with the Sample, Phenomenon of Interest, Design, Evaluation, Research type. 18 In order to ensure qualitative richness of themes, we included all qualitative research studies and excluded surveys, personal anecdotes, attitudes and experiences without in-depth qualitative analysis published on this topic.
Relevant definitions
For the sake of this review, we define an HCP as a person ‘lawfully entitled under the law of a province to provide health services in the place in which the services are provided by that person’. 19 This definition includes pharmacists, nurses, nurse practitioners, social workers, spiritual health practitioners, psychotherapists and clinical psychologists who are legally authorised to practise within their respective scope of practice. We included ‘Assisted suicide assistant’ and provider in ‘Right to die’ societies in Switzerland as unique MAiD care providers who contact the eligible participant and liaise with the physician and pharmacist in the conduct of MAiD.
For the sake of this review, the term ‘MAiD’ refers to 20 :
The administering by a physician or nurse practitioner of a substance to a person, at their request, that causes their death (euthanasia).
The prescribing or providing by a physician or nurse practitioner of a substance to a person at their request, so that they may self-administer the substance and, in doing so, cause their own death (assisted suicide).
Eligibility criteria
Includes worldwide published literature on the research question in English language, inclusive of all age groups; articles published up to 30 April 2021.
Includes all qualitative studies evaluating the emotional impact through qualitative research methodologies like grounded theory, semistructure interviews, narrative inquiry or others, and describes/mentions:
‘HCPs’ and ‘MAiD’ as defined above.
The emotional impact on HCPs in terms of emotions/affective responses experienced or expressed while accessing, discussing, participating or caring for the patient who has made a valid MAiD request.
Excludes case studies, anecdotes or studies without a description or mention of a rigorous qualitative research methodology.
Search strategy
An iteratively developed search strategy was developed and piloted with the help of three librarians with expertise in systematic review search strategies. Considering the interdisciplinary nature of the objective, the search strategy was conducted on OVID Medline, CINAHL, EMBASE and Scopus databases. The search terms included three main domains—MAiD, HCPs and qualitative research methodology and their synonyms. Full search strategy on the four databases is available in online supplemental appendix 1 .
Supplemental material
In addition to database searches, the study team conducted a grey literature search 21 which was informed by search methods outlined by Godin et al , 22 using the same search terms and their synonyms. Grey literature was retrieved between 10 December 2018 and 1 March 2019, and updated on 10 August 2020, and 10 August 2021, from:
Databases including Google Scholar, the Canadian Electronic Library and the Canadian Institute for Health Information.
OpenGrey, Bielefeld Academic Search Engine and the OAIster catalogue of open access resources that includes digital thesis sources like the WorldCat.
The grey literature search strategy and results are included in online supplemental appendix 1 . For the purpose of feasibility, reports from the year 2000 and beyond were retrieved. In addition, backward citation tracking was conducted by hand searching the reference lists of all included papers.
Study selection process
All identified records were imported into the reference management software, Zotero, and duplicates removed by the lead researcher (SYD). Twenty per cent of the titles and abstracts of peer-reviewed records were independently screened by two reviewers (AS and AB) based on the eligibility criteria; SYD screened the remaining 80% for eligibility and reviewed the results with AS and AB in regular team meetings. Given that a substantial portion of grey literature did not include abstracts, the grey literature screening process was initiated at the full-text phase. SYD consulted the keywords of yielded academic records if the title and abstract lacked clarity in relation to core concepts and reviewers AB and AS independently assessed any records for any discrepancy and/or uncertainty regarding their inclusion. The researchers met at the beginning, middle and end of the screening process to ensure consistency. SYD, AS and AB independently screened the full texts of the academic and grey literature, applying the same inclusion and exclusion criteria in successive team meetings to resolve any discrepancies.
Patient and public involvement
No patients were involved.
Assessment of risk of bias
We used the Joanna Briggs Institute’s critical appraisal tool for use in systematic reviews: checklist for qualitative research to critically appraise the included studies over 10 constructs. These constructs range from congruency to philosophical construct to theoretical and cultural location of the researcher. 23 The results of the assessment of risk of bias were independently reviewed by AB and AS and are presented in detail in online supplemental appendix 2 .
The search results and reasons for exclusion at each stage of screening were recorded and represented in the adapted Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram in figure 1 .
- Download figure
- Open in new tab
- Download powerpoint
PRISMA flow diagram: The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram details our search and selection process applied during the review. JBI, Joanna Briggs Institute; MAiD, medical assistance in dying.
Data analysis
Data extraction and data analysis.
We adopted a thematic synthesis approach to analyse and synthesise data. Thematic synthesis is an adaptation of thematic analysis and provides a set of established methods and techniques that help synthesise qualitative research outcomes, especially when there is heterogeneity in the outcome variables. 24 This approach is especially useful in our case since it enables us to examine the meaning, significance and social constructions around the emotional experience of an HCP involved in MAiD. SYD independently coded each line of text according to its meaning and content. Codes were listed as ‘free’ codes, without any hierarchical structure. AB and AS cross-checked the coded data for any discrepancy. Subsequent thematic synthesis was done by SYD, AB and AS in the following two stages:
Stage 1: identifying the similarities between the codes
All relevant qualitative data from the selected studies were extracted manually from the Results, Discussion and Conclusion sections and are represented in online supplemental appendix 3, table 2 . The codes were inductively grouped into descriptive themes so that patterns could be identified. The use of line-by-line coding enabled us to undertake translation of concepts from one study to another. Based on the similarities and differences of emerging codes, descriptive themes were generated, and each theme was entered as boxes and codes from each study illustrated in those boxes, so that constant comparison analysis process could be done (see online supplemental appendix 3, table 3 ).
Stage 2: development of analytical themes
In this last stage, the descriptive themes were further interpreted using reciprocal translation and constant comparison methods to develop analytical themes. At this stage, the meaning of the patterns of the descriptive themes was analysed against the research question so that a narrative component could be developed.
Once thematic synthesis was completed, each researcher independently evaluated the cumulative evidence from individual studies for methodological limitations, relevance, coherence and adequacy using the Confidence in the Evidence from Reviews of Qualitative Research (CERQual) approach (see table 1 ). 25
- View inline
Descriptive themes and illustrative quotes
All researchers met during regular research review meetings to resolve any discrepancies and achieve consensus over the assessment.
This systematic review was a part of an academic capstone project and was not registered with any international database. The review protocol is available from the research team on request.
In addition to employing the PRISMA checklist for systematic reviews, we used the Enhancing Transparency in Reporting the Synthesis of Qualitative Research checklist to improve the reporting of our meta-synthesis (see online supplemental appendix 4 ).
Characteristics of included studies
Thirty-five qualitative research studies were included in the review. The included literature was based in five countries: the USA (7), Netherlands (9), Canada (14), Belgium (1), Switzerland (3), and one study was an international study with participants from the USA and Netherlands. The data included 393 physicians, 169 nurses, 53 social workers in hospice care, 11 allied healthcare professionals (7 personal support workers, 1 pharmacist, 1 genetic technologist and 2 psychologists) and 8 directors of sociomedical institutions and 3 sociocultural animators (applied sociologists who work alongside communities at grass roots to develop and facilitate programmes that support action for local and social changes). A detailed description of the included studies is included in online supplemental appendix 3, table 2 .
Thematic synthesis
Stage 1: descriptive themes.
Three descriptive emotional themes were derived from the thematic synthesis:
Dimension 1: Strong, internalised and polarised emotions ( studies referenced 26–36 ). These included three subordinate categories/genres:
Positive emotions of ‘reward’, ‘relief’, ‘active openness’ and ‘overwhelming but uplifting’ feelings.
Negative emotions of ‘powerlessness’, ‘guilt’, ‘emotional exhaustion’, ‘vicarious suffering’ and fear of a slippery slope and losing control.
Individual conscience-based emotions of ‘moral shudder’ and moral distress. This emotional dimension was strongly embedded in the cultural and political milieus and the interpersonal communication strategies used by the HCPs.
Dimension 2: Reflective, discourse-based emotions ( studies referenced 26 30 36–46 )
These included emotions of ‘growing with the patient’s experience’, MAiD as a ‘sense-making process’, ‘de-tabooing the philosophical meaning of death through MAiD’ and various degrees of ‘dynamic conflict’ secondary to a reflective sense of insecurity. These emotions were descriptively laid on a platform of ‘interpretative therapeutic engagement’, where they seemed to aid in the larger philosophical and societal discourse around MAiD. 46
Dimension 3: Emotions that resonate with professional values ( studies referenced 28 30 34 39 47–61 )
These included emotions that resonated with professional values like ‘competency and perfection’, ‘intimate care’, ‘ colloque singulier ’ (singular language of trust and conscience in context of therapeutic relationship) and various degrees of commitment ranging from ‘contractual’ to ‘sacrificial’.
Table 1 illustrates some of the quotes demonstrating the descriptive emotional themes.
Stage 2: analytical themes
Analytical themes in thematic synthesis typically ‘go beyond’ the findings of the primary studies and generate additional concepts, understandings or hypothesis. At this stage, we used the descriptive themes to answer the review question as to how and why did the HCPs participating in MAiD experience such complex emotions. Each reviewer, initially independent and then as a group, inferred the factors that likely influence the experience of the descriptive themes by questioning how HCPs participating in MAiD represent themselves, or their emotions in the context of their larger healthcare environment. This process was repeated until the new themes were sufficiently abstract to explain all our initial descriptive themes. Altogether, this process resulted in generation of two analytical themes:
Legislative emphasis on terminal illness as a necessary inclusion criterion for MAiD influences the emotional impact. In jurisdictions that legislate MAiD with the central aim to alleviate intolerable suffering in context of terminally ill medical conditions (eg, the USA), the HCPs experience strong polarised emotions that are modulated by their individual cultural/religious background. The extent of emotional impact ranges from positive emotions of reward/relief on one end, to negative (burden, emotional exhaustion) and conscientious-based moral distress on the other. This is in sharp contrast to the emotional impact on HCPs in jurisdictions that legislate MAiD with an emphasis on alleviating intolerable suffering without terminal illness being a necessary requirement (eg, Benelux countries, Switzerland and, more recently, Canada). The HCPs in these jurisdictions experience the emotional impact of MAiD as a ‘sense-making’ process—this allows them to reflect on the emotional dissonance between basic emotions and emotions that conform to legislative rules.
Values associated with the HCPs’ profession and their degree of engagement in the MAiD process are strong influential factors that shape the emotional impact of MAiD. For example, because of their everyday involvement with patients and emphasis on professional values of helping others, compassion and patient advocacy, the emotional impact on nurses involved in MAiD (studies referenced 28 30 34–36 39 41 42 45 53 55 57 60 61 ) demonstrated strong and polarised positive as well as negative emotions. As one nursing participant noted:
… it’s the hardest nursing. I’ve worked [in the emergency department], I’ve worked medicine floor, this is the hardest nursing there is, having somebody pass away, you actually feel something pulled out of you when that person passes. There’s something missing. … If you take care of somebody for an extended time and they pass away, you just feel, I just feel coldness, or whatever. You just feel drained…. 36 (p 57)
Appraising the quality of evidence: the Grading of Recommendations Assessment, Development and Evaluation CERQual approach
Evidence from qualitative evidence syntheses is increasingly incorporated into decision-making processes and the Grading of Recommendations Assessment, Development and Evaluation (GRADE) CERQual approach allows the user to make a transparent assessment of how much confidence decision-makers and other users can place in individual review findings from syntheses of qualitative evidence. In order to ascertain the degree of confidence, we graded the evidence in terms of adequacy, relevance, coherence as well as methodological limitations using the GRADE CERQual approach. 25 Table 2 illustrates a summary of the findings and the GRADE CERQual profile.
Grading of Recommendations Assessment, Development and Evaluation (GRADE) Confidence in the Evidence from Reviews of Qualitative Research (CERQual) evidence profile
Difference in MAiD legislation in Benelux and non-Benelux countries: key features
The substantive and procedural requirements for MAiD across global jurisdictions rest on three main pillars: patients’ right for self-determination expressed through voluntariness of request and a valid informed consent process, foreseeability of natural death due to terminal medical illness and subjective nature of individual suffering. 62 63 The key difference between the legislations for MAiD in Benelux countries and countries like the USA is the differential emphasis on eminent or foreseeability of death. The MAiD legislations in Belgium, Netherlands, Switzerland and, more recently, Canada have a more permissive legal framework that allows people to access MAiD as a service to end their intolerable suffering that has no prospect of improvement but is not necessarily terminal.
MAiD legislation and its shaping effect on the emotions of the involved HCP
An important take-home message from this evidence synthesis is how legislations have a shaping effect on emotional responses. The HCPs who practise in the Benelux countries and Switzerland seem to experience more reflective emotions over strong polarising emotions expressed by HCPs who practise in non-Benelux countries like the USA. Canada seems to have a unique transitional position—with the emphasis of the legislation going the Benelux countries’ way, the HCPs’ emotional experiences show a mixture of emotions driven by their professional values as well as the ongoing societal discourse on MAiD. This observation conforms to Michel Foucault’s position on how law acts as an element in the expansion of power(s) 64 ; legislatures along with other platforms of knowledge expression modulate every fibre of human society. Our thematic synthesis points out that the law that limits application of MAiD to terminal illnesses provides for a broader range of emotional expression. Thus, legislation on MAiD across the globe provides the HCP with a locus of administrative control which then decides how the emotional discourse around MAiD is shaped; the question is— how do we want the emotional discourse around MAiD to be shaped?
MAiD legislation, societal values and emotional impact on the involved HCP: a complex relationship
On one end, attitudes of physicians towards MAiD have shown reflective trends to legislative standards; countries like Belgium and Netherlands find much stronger physician support than their USA counterparts. 65 On the other end, public support towards MAiD has been reflective of the prevailing societal cultural and religious practices; central and eastern European countries have shown a decline in support with corresponding increase in religiosity as opposed to western European countries. 66 67 While an assisted-death legislation with its rules and safeguards provides an obligatory ‘top-down’ framework to embed MAiD within healthcare, it does not necessary reflect the integration of MAiD within the value-based relationships that have traditionally defined an individual’s healthcare. 68 Hence, although a MAiD legislation to integrate MAiD into healthcare is a likely reflection of a consensus position of a society, it does challenge the moral environments within which HCPs practise medicine, thereby influencing the emotional impact on HCP. HCPs’ subsequent attempt to align themselves with their own professional values, legislative standards and public perceptions can lead to intense emotional responses, both within their internal, personal and external professional spaces.
Emotional discourse among HCPs involved in MAiD: HCP role and ethics of care
The right to choose when and how to die has always been a contentious issue across various societies. 69–71 Public discourse on MAiD is shaped through societal emphasis on individual as well as contextual factors associated with assisted death—these often range from religious beliefs regarding sanctity of human life and personal meaning of death to loss of autonomy associated with illness-related intolerable suffering. With advancing medical technologies, the potential to prolong life has increased significantly, 72 73 and the HCPs assume a central position to shape the discourse around assisted death.
In countries where MAiD is legalised but is restricted to terminal illnesses with imminent chance of death, the position of an HCP continues to be one that of a provider of ‘Care’. Here, the moral dimension of ‘Care’ continues to be defined as ‘everything we do to maintain, continue or repair our world so that we can live in it as well as possible’. 74 The value of care in healthcare systems has been traditionally associated with attentiveness, responsibility, nurturance, compassion and meeting others’ needs. 75 While emotional responses to legal requests of hastening death are affected by policies, professional identity, commitment to patient autonomy, personal values and beliefs, the patient–clinician relationship and will vary on a case-by-case basis, 76 this systematic review raises an important question—how does legalising MAiD with emphasis on alleviating intolerable suffering without the context of a terminal illness change the moral dimensions of care?
HCPs involved in MAiD experience a myriad of emotions that include positive/negative emotions; reflective, ‘sense-making’ emotions; and/or professional value-driven emotions. Emphasis on terminal illness only as an essential criterion, MAiD practitioner’s individual professional values and their degree of engagement influence this rich and diverse emotional discourse.
Limitations of the review
This review is limited by its focus of emotional impact on HCPs only and the obvious selection bias in the included studies—those who could and volunteered to express their emotions are represented in the review. The review is also limited with absence of subgroup analysis with respect to HCPs’ age, years of experience and the influence of gender on the results. Restriction to English language studies likely carries a high risk of publication bias.
There are several gaps in our understanding of the emotional impact on HCPs involved in MAiD that would benefit from further research. Intolerable suffering is a common eligibility requirement for assisted death, although HCPs often struggle to understand and assess the nature and normative function of suffering. Is it the very nature of the emotional tone of suffering which is overwhelming or is it more to do with what lies underneath that makes suffering ‘intolerable’? Is there room for humanistic narratives around meaning behind and endurance of one’s suffering? Such questions confront MAiD practitioners and an in-depth exploration of this nebulous concept of intolerable suffering in context of assisted death may help HCPs navigate their emotional experience while providing MAiD.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This is a systematic review and meta-synthesis of already published and accessible research data and does not require ethics committee or institutional board approval.
Acknowledgments
The authors acknowledge the valuable contribution of Erica Lenton, Heather Cunningham (library services, Gerstein Library, University of Toronto) and Fiona Inglis (library services, Centre for Addiction and Mental Health, University of Toronto) to consultations and assistance with devising the search strategy.
- Simpson AIF
- Incardona N ,
- Parliament of Canada
- Health Canada
- Department of Justice
- Eggertson L
- Dierckx de Casterlé B ,
- Greig M , et al
- Fujioka JK ,
- McDonald PL , et al
- Haverkate I ,
- van der Heide A ,
- Onwuteaka-Philipsen BD , et al
- Government of Canada
- ↵ Government of Ontario Ministry of Health and Ministry of Long Term Care Medical Assistance in Dying [Internet] . Available: http://health.gov.on.ca/en/pro/programs/maid/#maid [Accessed 06 Aug 2019 ].
- Stapleton J ,
- Kirkpatrick SI , et al
- Joanna Briggs Critical Appraisal Tools
- Lockwood C ,
- Glenton C , et al
- Voorhees JR ,
- Rietjens JAC ,
- van der Heide A , et al
- van Marwijk H ,
- van Royen P , et al
- De Bal N , et al
- Georges J-J ,
- Castelli Dransart DA ,
- Scozzari E ,
- Elger B , et al
- Nuhn A , et al
- Bouthillier M-E ,
- Buchbinder M ,
- Brassfield ER ,
- Snijdewind MC ,
- van Tol DG ,
- van der Heide A
- Beuthin R ,
- Vernooij-Dassen MJ ,
- Dekkers WJ , et al
- Townsley AA
- Hopwood M-C , et al
- Wright DK ,
- Chirchikova M ,
- Daniel V , et al
- Norton EM ,
- Ten Cate K ,
- van de Vathorst S
- Melchor F ,
- Miller PJ ,
- Mesler MA ,
- Pasman HRW , et al
- Harvath TA ,
- Miller LL ,
- Smith KA , et al
- van de Scheur A ,
- van der Arend A
- Bélanger E ,
- Wright DK , et al
- Gamondi C ,
- Borasio GD ,
- Oliver P , et al
- Khoshnood N ,
- Hopwood M-C ,
- Lokuge B , et al
- Durant K-L ,
- Kortes-Miller K
- Schiller CJ , et al
- Mathews JJ ,
- Hausner D ,
- Avery J , et al
- The Council of Canadian Acadamies
- Emanuel EJ ,
- Onwuteaka-Philipsen BD ,
- Urwin JW , et al
- Van Landeghem P ,
- Carpentier N , et al
- Schiller CJ ,
- Roussel J , et al
- Gómez-Vírseda C ,
- Street AF ,
- The Lancet Respiratory Medicine
- Christy K ,
- Grierson L , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
- Data supplement 4
Twitter @saumil1980, @DrSandySimpson
Contributors Study conception and design: SYD, AB, AS. Development of eligibility criteria: SYD, AB, AS. Search strategy developed by Erica Lenton, Heather Cunningham (library services, Gerstein Library, University of Toronto) and Fiona Inglis (library services, Centre for Addiction and Mental Health, University of Toronto) in close consultation with Dr Saumil Dholakia and reviewed by AB and AS. Study selection and data extraction process by Dr Saumil Dholakia and independently reviewed by AB and AS. SYD performed the assessment of risk of bias, which was independently reviewed by AB and AS. Guarantor: SYD. All three authors were involved equally in performing the qualitative meta-synthesis and CERQual assessment. Draft manuscript preparation: SYD with multiple reviews, feedback and edits in form as well as content by AB and AS. All authors reviewed the results and approved the final version of the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Medical Assistance in Dying: An Ethnographic Study on the Practitioner’s Decision Making in Eligibility Assessments
Journal title, journal issn, volume title, description, collections, libraries & cultural resources.
- 403.220.8895
- Research article
- Open access
- Published: 17 February 2020
The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death
- Barbara Pesut ORCID: orcid.org/0000-0002-1063-7190 1 ,
- Sally Thorne 2 ,
- Catharine J. Schiller 3 ,
- Madeleine Greig 1 &
- Josette Roussel 4
BMC Nursing volume 19 , Article number: 12 ( 2020 ) Cite this article
17k Accesses
44 Citations
24 Altmetric
Metrics details
Medical Assistance in Dying (MAiD) was legalized in Canada in June, 2016. The Canadian government’s decision to legislate assisted dying, an approach that requires a high degree of obligation, precision, and delegation, has resulted in unique challenges for health care and for nursing practice. The purpose of this study was to better understand the implications of a legislated approach to assisted death for nurses’ experiences and nursing practice.
The study used a qualitative approach guided by Interpretive Description. Semi-structured interviews were conducted with 59 registered nurses and nurse practitioners. Interviews were audio-recorded, transcribed, and managed using qualitative analysis software. Analysis followed a procedure of data immersion, open coding, constant comparative analysis, and the construction of a thematic and interpretive account.
Nurses in this study described great variability in how MAiD had been enacted in their work context and the practice supports available to guide their practice. The development of systems to support MAiD, or lack thereof, was largely driven by persons in influential leadership positions. Workplaces that supported a range of nurses’ moral responses to MAiD were most effective in supporting nurses’ well-being during this impactful change in practice. Participants cited the importance of teamwork in providing high quality MAiD-related care; although, many worked without the benefit of a team. Nursing work related to MAiD was highly complex, largely because of the need for patient-centered care in systems that were not always organized to support such care. In the absence of adequate practice supports, some nurses were choosing to limit their involvement in MAiD.
Conclusions
Data obtained in this study suggested that some workplace contexts still lack the necessary supports for nurses to confidently meet the precision required of a legislated approach to MAiD. Without accessible palliative care, sufficient providers, a supportive team, practice supports, and a context that allowed nurses to have a range of responses to MAiD, nurses felt they were legally and morally at risk. Nurses seeking to provide the compassionate care consistent with such a momentous moment in patients’ lives, without suitable supports, find themselves caught between the proverbial rock and hard place.
Peer Review reports
All forms of assisted suicide were illegal in Canada until February 2015 when the Supreme Court of Canada (SSC) released its landmark decision Carter v Canada (Attorney General) (“ Carter ”) [ 1 ] . In its ruling, the SCC struck down the Criminal Code’s prohibition on assisted suicide for competent adults in certain clinical circumstances, on the basis that such a prohibition unjustifiably violated the Canadian Charter of Rights and Freedoms (“ Charter ”).
The SCC’s ruling gave the federal government time to craft a legislative framework to regulate assisted dying. In June 2016, medical assistance in dying (MAiD) was legalized in An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying) , a statute still colloquially known as Bill C-14 [ 2 ]. The government had crafted a new concept, MAiD, within this legislation rather than continue to use an existing term, such as “physician assisted suicide” or “physician assisted dying”. This new terminology represented a recognition that a team of healthcare providers, not only physicians, is typically required to implement such a complex procedure [ 3 ]. In Bill C-14 , MAiD is defined as: a) the administration by a medical practitioner or nurse practitioner of a substance to a person, at their request, that causes their death; or b) the prescribing or providing by a medical practitioner or nurse practitioner of a substance to a person, at their request, so that they may self-administer the substance and in doing so cause their own death Only 6 of the 6749 medically assisted deaths recorded in Canada between December 10, 2015 and October 31, 2018 were self-administered [ 4 ].
According to Bill C-14 , to be eligible for MAiD, an individual must meet all of the following criteria: (a) they are eligible for health services funded by a government in Canada; (b) they are at least 18 years of age and capable of making decisions with respect to their health; (c) they are suffering from a grievous and irremediable medical condition; d) they have made a voluntary request for medical assistance in dying that was not made as a result of external pressure; and (e) they give informed consent to receive medical assistance in dying after having been informed of the means that are available to relieve their suffering, including palliative care [ 2 ]. Once Bill C-14 was passed, provincial and territorial governments, as well as provincial and territorial regulatory bodies for the health professions, became responsible for enacting policies, procedures and processes to guide MAiD-related healthcare practice in Canada.
Implications of a legislated approach to MAiD
The Canadian government chose to enact legislation that would regulate assisted suicide, but there were other options available to them. Luzon modeled five approaches to assisted death based upon obligations, precision, and delegation:
Obligation means that people are legally bound by a rule, so that their behavior is subject to examination under the general rules, procedures, and discourse of the law. Precision means that rules unequivocally define the conduct they require, authorize, permit, or prohibit. Delegation refers to the body that has been granted authority (by the public) to determine, implement, interpret, and apply the rules. All three dimensions can vary in degree. Based on these characteristics, legalization may be hard (where all three properties are maximized), soft (where some properties are maximized and others minimized), and null (where all three properties are minimized). [emphasis added] (5 p. 7)
The five possible legal framework responses to assisted death are as follows. The first would involve maintaining the status quo , such that assisted death would continue to be treated as a crime; this would have been an obviously problematic approach given the existence of the Carter decision. The second is defense in which it would be recognized that there may, at times, be situations in which a valid defense to assisted death can be made. The third involves de-prioritization ; this response would allow laws against assisted suicide to remain in place but it would not be viewed as a priority of the justice system to prosecute those who are involved in assisted dying or to impose criminal sanctions upon them. The fourth is de-criminalization in which no precise laws are provided; this was the approach used by the Canadian government after the Criminal Code prohibition on abortion was struck down by the SCC in the 1988 R v Morgentaler case. The fifth is legislation in which “ there is a specific binding law (high in obligation), a precise, specific, clear rule for every practice (high in precision), and the designated third party to which the state delegates authority is the legislature (high in delegation). ” (5 p. 14)
Canada chose the fifth approach to assisted death which, according to Luzon, entails a hard approach characterized by a high degree of obligation, precision, and delegation [ 5 ]. To that end, Bill C-14 incorporated numerous safeguards and requirements into the MAiD process. For example, eligibility for MAiD must be determined by two practitioners, either physicians or nurse practitioners, who are independent of one another (the second practitioner must also be independent of the patient). Once the patient has been determined to be eligible, he or she must then submit a written request for MAiD in the presence of two independent witnesses. In addition, there is a mandatory reflection period of at least 10 days between the signing of that written request by the patient and the day that MAiD is actually provided, although this can be shortened in certain clinical circumstances [ 2 ]. These, and other, safeguards were written into the legislation by the government to decrease the possibility that the MAiD procedure could be used inappropriately.
The nursing role in MAiD
Not only has Canada taken the ‘hardest’ approach to assisted death, but it is also the first country to allow nurse practitioners to act as MAiD assessors and providers. Although it is important to note that this role for nurse practitioners is further regulated at the provincial level and so not all nurse practitioners are allowed by the provincial health regions to act as MAiD assessors or providers. In Canada, registered nurses who do not hold a nurse practitioner credential also play important roles in MAiD. The important role of the registered nurse is also evident in studies from other countries where assisted death is legal [ 6 , 7 , 8 , 9 , 10 , 11 ]. For example, our synthesis of qualitative studies from Belgium, the Netherlands, and Canada of registered nurses’ experiences with assisted death suggested that nurses perform a central role in negotiating initial inquiries about assisted death, that nurses provide important ‘wrap-around’ care for patients and family, and that participating in an assisted death was impactful for nurses and required significant moral work [ 12 ].
In consideration of the importance of the registered nursing role, and the new role for nurse practitioners in Canada, we conducted a study in which we explored the policy, practice, and ethical implications of MAiD for nursing. This was a two-phased study in which we first conducted systematic reviews of the literature [ 12 , 13 , 14 ] and then a qualitative study of Canadian nurses’ experiences with MAiD. As part of the literature synthesis we gathered and analyzed nursing regulatory documents that were created to guide nursing practice in MAiD from the 10 provinces and 3 territories in Canada [ 13 ]. We discovered substantial variability in the degree to which these regulatory bodies chose to provide additional guidelines for nurses beyond what was provided in the MAiD legislation. As such, we were interested in better understanding how nurses were experiencing the enactment of the legislation in their practice related to MAiD, and thus explored this qualitatively. In this paper, we report on findings from the qualitative phase of the study that revealed the impact of Canada’s legislated approach to assisted death on nurses’ experiences, and on nursing practice, in Canada.
This qualitative study was guided by Interpretive Description, a pragmatic approach to developing knowledge for a practice discipline [ 15 ].
Participants
Data was collected through 60 interviews with 59 participants (see Table 1 for demographic data). Recruitment of this sample occurred via bulletins that were distributed to key stakeholders and prospective participants using convenience, purposive, and snowball sampling techniques. For example, we advertised through the Canadian Nurses’ Association, through health regions, and through the Canadian Association of MAiD Assessors and Providers. We asked interview participants to pass the study information on to others. We sought to gain participation from all English-speaking provinces. We did not specifically target the Canadian territories as the interim reports on MAiD produced by Health Canada suggested that few cases were occurring in those areas [ 4 ]. Eligibility criteria required that participants were registered nurses or nurse practitioners, who had previously cared for patients requesting or receiving MAiD, or those registered nurses or nurse practitioners who had decided, for whatever reason, not to participate in the MAiD process. No participants dropped out of the study or requested that their data be removed from the study. These 59 participants had significant experience with MAiD. For example, 24 of the 59 participants had conducted more than 25 conversations with patients about MAiD, and 11 of the 59 participants had been involved with more than 25 patients who went on to receive MAiD.
Data collection and analysis
Data was collected in the fall of 2018 and the spring of 2019, approximately 2 years after the MAiD legislation was enacted. Semi-structured interviews, conducted by telephone, were used to garner an in-depth understanding of nurses’ experiences with MAiD. Telephone interviews were necessary to reach nurses from across Canada. Interviews were conducted by the principal investigator and research coordinator. Participants were provided with a detailed consent form at least 24 h prior to the interview to ensure that they understood the focus and objectives of the study. Interviews were conducted only after the signed consent was received. Interviewers reiterated the rationale for conducting the study prior to the interview, and participants were provided with an opportunity to ask questions. A semi-structured interview guide was developed for this study, piloted and refined prior to data collection (Additional file 1 ). Examples of interview questions included: (i) Can you tell us how the process of MAiD occurs in your practice context? (ii) What resources and practice supports are available to assist you in caring for MAiD patients? (iii) Tell us about your experiences with MAiD? The average length of interviews was 55 min. In totality, 2992 min of interview data were collected and subsequently analyzed.
Interview data were audio-recorded, transcribed verbatim, de-identified, checked for accuracy and uploaded into NVivo 12TSN for data analysis and management. Transcripts included emotions evident during the interview (e.g., crying). All audio recordings were reviewed by the principal investigator and detailed field notes were written and referred back to during the analytic process. Data were analyzed following the logic of Interpretive Description [ 15 ]. Open codes were developed and negotiated by two investigators (BP & MG) after an immersion process of reading and re-reading multiple transcripts. These codes were further refined with input from two additional investigators (ST & JR). These open codes were then used to code the remaining data. Codes were further refined in an iterative process of data collection and analysis by using constant comparative data analysis techniques, a technique developed initially within Grounded Theory [ 16 ]. Once all of the transcripts had been coded, data contained within these codes were summarized to construct a thematic and interpretive account of Canadian nurses’ experiences with MAiD. In this paper we discuss the experiences related to Canada’s legislated approach to MAiD.
Nurses interviewed for this study described great variability in how MAiD had been enacted within their geographic and work context and how that variability had influenced their experiences with MAiD. This variability was largely influenced by three themes: (1) the leadership taken by influential persons within systems, (2) the presence and nature of a multi-disciplinary team, and (3) the systems’ complexity and capacity to support MAiD.
Systems: influential leaders setting the tone
Nurses described work contexts that ranged from a virtual absence of any MAiD-related guidelines to highly structured systems in which a comprehensive set of supports existed to guide nursing practice. In some contexts, policies and procedures were established fairly quickly. For example, one participant described how, after the legislation was passed, key leaders in the health region immediately established a working group to work intensively over a weekend to construct the policies and procedures that would guide immediate practice. However, in other contexts those first MAiD cases were done with little direction, “ We really had no idea what we were doing because we hadn’t actually made any policy or guidelines yet .” P42 Even many months after the legislation, some nurses were still working within a healthcare policy and procedure void. These findings were similar for both registered nurses and nurse practitioners, although nurse practitioners had the structure provided for them within Bill C-14 . Nurses, however, sometimes found themselves trying to assist in a MAiD procedure with no practice guidelines in their places of work. This created uncertainty in their practice, particularly when nurses remained the primary caregivers of patients contemplating or undergoing MAiD, which also involved high levels of interaction with their families. “ So, my big concern is if someone does approach me with a written request, what do I do from there? And I know the health region has developed no policies pertaining to what the process is .” P26.
Much of this variability in the degree of practice support was a result of the decisions (or lack of decisions) made by persons in influential leadership positions either immediately preceding or following the legalization of MAiD. For example, one participant mentioned that a change in government soon after the Carter decision had slowed down the development of MAiD guidelines in their province which in turn heighted the perception of risk. “ With the change in government, things were a little bit stalled and questions weren’t necessarily being answered. I think there were a lot of physicians and NPs maybe a little bit nervous about how things were working .” P1 Some health authorities assigned key individuals to lead the development of practice supports. A number of innovations were developed, including regional interdisciplinary MAiD teams, designated persons to work alongside and support individuals considering whether to undergo MAiD, and therapeutic interventions designed to address the underlying suffering that had contributed to a MAiD request. However, leaders also developed organically as they championed the MAiD process. For example, this nurse participated in a provision while her clinical leader was away. “ Because she was away, I informally became the leader of MAiD on our unit .” P50.
Leaders responsible for palliative care were particularly influential in the development of structures and processes to support MAiD. The beliefs of these leaders about the acceptability of MAiD, its fit with palliative care, and perhaps most importantly, their recognition that MAiD would generate a range of moral responses in their colleagues, determined the direction and outcomes of these practice supports. For example, in one jurisdiction, MAiD assessment responsibilities were assigned to nurse practitioners who were engaged in palliative care. This decision meant that palliative care and MAiD were both integrated within nursing responsibilities. As logical as this decision seemed from a workflow perspective, it resulted in unique tensions, particularly for those palliative nurses who objected to MAiD due to either their moral values or their beliefs about its fit with a palliative care philosophy.
Another example of influence was how leaders constructed workplace policies to support a range of moral responses to MAiD. We specifically use the term ‘range of moral responses,’ rather than conscientious objection, to reflect the uncertainty about MAiD that was characteristic of nurses in this study. Few openly declared themselves as conscientious objectors; instead, more were uncertain about how they felt about MAiD. Nurses described workplace policies that varied dramatically in how they accommodated their nurses’ willingness, or not, to participate in MAiD and the uncertainty that caused. At one end of the spectrum, nurses were allowed to take a day off without pay if they were uncomfortable with MAiD and it was occurring on their unit. At the other end of the spectrum, nurses were expected to provide all non-MAiD related care, no matter how they felt about MAiD. These policies reflected very different approaches to nurses’ moral well-being. As employees of healthcare, nurses felt they had little control over the ways in which their workplaces were structured to accommodate their comfort level with MAiD. For example, one nurse stated, “ we need some sort of support groups or guidelines for conscientious objectors. I have heard that other countries have more lenient processes for conscientious objectors so that they don’t feel stigmatized .” P54.
Nurses perceived physicians, and in particular palliative physicians, to be important influencers in how MAiD processes developed. For example, one participant described how the medical director influenced the implementation of MAiD on her palliative unit. “ Our medical director at the time wasn’t on board and that trickled down to all of us .” P57 Unlike nurses who were employees of healthcare, physicians were perceived as having more latitude to choose whether, how, and to what extent they would support the MAiD process. In some cases, nurses described how physicians worked with them to seamlessly integrate MAiD with palliative care. In other cases, nurses described physicians who erected barriers to patient involvement with MAiD. These barriers could include telling patients that they were not quite ready for MAiD, or suggesting that it could not be done in the community where patients were living, or simply ignoring patient requests. The strongest type of physician resistance described by participants was the withdrawal of palliative care services once a patient had chosen MAiD. This withdrawal of services made it difficult for nurses to support good pain and symptom management while the patient was awaiting MAiD. Nurses responded strongly to this withdrawal of palliative services: “ So we have a serious practice issue here. I’m mad as hell.” P24.
However, participants also suggested that relationships between those who provided palliative care and those who provided MAiD were becoming more congenial over time. “ We have come a long way because people are not so angry or defensive.” P31 In some cases, this was because MAiD teams had been formed outside of palliative care teams and they had learned to work together. In other cases, palliative clinicians were becoming more comfortable with MAiD as an option, either within or outside of palliative care. Despite this apparent easing of relationships between MAiD and palliative providers, there remained significant concerns related to the inadequacy of palliative care systems in Canada and the impact that MAiD could have in the face of this inadequacy. For example, one participant suggested that the workload generated by MAiD could be a significant barrier for palliative care clinicians who were already working to maximum capacity. Another participant suggested that palliative care, which already carried a fair bit of stigma because of its relationship to death, would become further stigmatized with the introduction of MAiD. Ultimately, this perception would lead to even less acceptability and uptake of palliative care by patients. But what created wider concern for nurses was the inadequate accessibility to palliative care services for some patients in Canada. Under Bill C-14 , clinicians are required to offer palliative care to clients who are considering a MAiD death. Participants reflected on the irony of how much attention had gone into supporting accessibility to MAiD without corresponding attention paid to overall accessibility to palliative care. “ We use this rhetoric that it’s somebody’s right to die and I don’t want to debate that part but I think it’s also their right to have access to care done by clinicians who are knowledgeable about palliative care.” P23 This participant was reflecting on the paucity of specialized palliative care but also on the lack of palliative care knowledge within primary care where most palliative care happens. This same participant went on to describe how providers’ lack of palliative care knowledge unwittingly contributed to patient suffering. This tension between a system that caused undue suffering because of ignorance of good palliative care, and a system designed to relieve that suffering through MAiD, put this nurse in an intense state of tension:
This is the crazy thing for me to consider … it's a shame and it's something that I grieve to think that our system, as it is, can contribute so much to the suffering of somebody on so many different levels. … on top of whatever illness process that is causing suffering. But that our health care system contributes to suffering, and is doing nothing about our own contribution to that suffering, but then uses that very suffering to activate access to MAiD. It's absolutely ridiculous to me. P23
In light of the tensions between palliative care and MAiD, participants had thoughtfully considered what they thought might be the ideal relationship between the two systems. One participant described it as “ parallel lines with crossover points .” P24 MAiD providers would work along one continuum while palliative care providers would work along the other continuum. But, if and when a client should choose to cross over from palliative care to MAiD, then palliative care would continue as an unbroken commitment to patients.
In summary, nurses in this study were working within systems that differed greatly in their response to MAiD. Some were highly organized whereas others were devoid of policies, procedures, and formal direction. Much of this variability was attributed to the way in which influential leaders, particularly those with responsibilities for palliative care, had chosen to approach MAiD. Further, perspectives of these influential palliative leaders had in turn been influenced by the broader challenges of palliative care accessibility in the Canadian context.
Teamwork: Two’s a team
Nurses in this study participated in MAiD teams to varying degrees. At one end of the spectrum, nurses worked in isolation, being lone assessors and/or providers who worked only peripherally with other assessors and providers. At the other end of the spectrum were nurses who were integrated into well-connected teams dedicated to providing MAiD. In the middle were nurses who worked organically and closely with a few physicians but who were outside of a formal team structure. Even as they found themselves with varying degrees of team support, participants described teamwork as essential to a successful MAiD process. MAiD was a new procedure, and participants described the time it took for physicians and nurses to create a MAiD process that worked well and to feel comfortable with that process. Nurses suggested that, at minimum, two people should be present at every provision of MAiD, one to do the provision and one to look after family and friends and to troubleshoot situations that arose during the process. Having a second person was particularly important in light of the impactful nature of the experience and the need to ensure a seamless, trouble-free provision. For example, this nurse talked about a difficult provision and the importance of a supportive physician. “ It was just me, the doctor and the patient and it was a bad feeling, dark, no windows. Afterward I had to wait for the funeral home and I said to the physician, ‘you can go.’ He said, ‘I’m not leaving you.’ So, it was just so nice to have that support from the physician .” P37 As physicians were often “ piloted in ” to perform the procedure, it was the nurses who ultimately learned what worked well and who were often in a position to provide support and mentorship to those physicians who performed the procedure less frequently. For example, one nurse remembered supporting a physician through his first provision:
What struck me about that day was my physician colleague, how his hands were shaking. And I remember putting my hand on his shoulder and just kind of nodding because we were there together and he had never done this before but we had spent a lot of time together previously. P1
In the latter part of this quote, the nurse acknowledges that it was her previous relationship with the physician that allowed her to support him better. These supportive relationships within the MAiD team were acknowledged as an integral part of the process of a successful MAiD provision. Relationships facilitated the ability to know how each person would respond to such an impactful event, the ability for the nurse to step in and troubleshoot without offending the physician, and the ability to effectively debrief after the process. For example, this nurse described an experience of working with a physician who was unwittingly excluding the family’s access to the patient at the last moment, but she did not feel that she and the physician had enough of an established relationship for her to correct him:
She [the client] was turned towards him [the physician] and her family was at her back and I thought what a shame that we couldn't take a moment and turn her to her family. But that was the first time I'd worked with that clinician. I didn't have any relationship with him at all. P2
Another participant spoke of supporting a physician new to the MAiD process who was concerned that the patient had not died after administering the medication. Even though the nurse was certain that the patient had died, she took the stethoscope and listened for the heartbeat for a prolonged period of time so that the physician would be reassured. Such examples told a compelling story of the need for mutual support throughout the process of MAiD provision.
Participants also reflected on who might be excluded from the team, but who would nevertheless be deeply impacted by a MAiD death. For example, intravenous (IV) team members play an important role in the establishment and maintenance of the IVs upon which the success of MAiD administration rests. IV team members often establish the IV many hours before the provision to ensure that it is ready. During this insertion they often visit with patients and hear their story. As one nurse described it, you don’t put in the IV before you establish the relationship. But, even though these IV team members had established a relationship with the client, they did not have the team support when the client went on to receive MAiD. This nurse described encountering one such IV nurse. “ I remember an IV nurse starting an IV and for some reason she was waiting outside the door, the door was closed. I can’t remember exactly why but she was crying and I comforted her but, you know, she does not get the support we get on the unit .” P6.
Privacy issues attaching to disclosure of a MAiD death also influenced who received support as part of the team. Home care nurses, acute care nurses, and residential care aids and nurses were frequently left out of the process for privacy reasons. Home care nurses described caring for long term clients who were not imminently dying and then being notified that they had suddenly passed away. The nurse would then follow up with the family and would be told that the client had received MAiD. It was not uncommon for these nurses to wonder why patients and families had not discussed this option with them, particularly in light of their long-term relationships. Nurses in general experienced this as being left out of the loop and, in some cases, it changed their practice in relation to MAiD:
We had no idea they [clients and family] were thinking about it or mentioning it and no one had a clue and we’d just get notified that they’d passed away, which was really bizarre in the beginning. So, I think that was a turning point for me to make sure they knew all of their options and that they felt safe discussing all of their health with me. And no matter what they chose, they had those options on the table and that they could feel supported through the whole process if that’s what they chose. P12
Stories from residential care were particularly challenging because of the close and enduring relationships that exist between clients and care aides. Clients might choose to keep their decision to access MAiD private, in part because they did not want to spend their last day saying goodbye or justifying their decisions. However, care aides were then taken by surprise by the death:
Her request was not to tell any of the staff members until afterwards. Her care aides took that very poorly because they didn’t know. They were with her right to the last minute and it was a normal day. They took her to dinner, they took her out for a smoke, they took her back to her room. But then, they were told that she had died. P28
So, while teamwork was considered the ideal of care, many were left out of the team for various reasons, and as a result did not receive the supports that those who were directly involved in the MAiD team experienced. Further, because MAiD was an impactful experience, those who had learned to work well together formed strong teams that were difficult for others to break into. For example, much of the MAiD referral process across Canada involves a centralized coordinator, often a nurse, who then assigns the patient to willing assessors and providers. These willing individuals are often the ‘go to’ people who work well together. As a result, others who would like to develop experience with the MAiD process may be inadvertently excluded, as was the case of the following participant:
So, you have these pairs of teams and I think it speaks to the powerfulness of the experience. You need to work with a team that you're trusting in. Right? But there's an interesting sort of dynamic with that because, if you're a primary provider and you have a secondary person you use all the time, then you're just going to ask your secondary person. P2
In summary, participants cited the importance of teamwork both to support a seamless MAiD process and to support those involved in this impactful experience. However, the ability to work within a team where relationships were well established had benefits beyond mutual support. It also facilitated the seamless organization of what was potentially a highly complex process.
Processes: patient-centered aspirations in a complex system
Participants in this study described the complexity of facilitating a MAiD-related death. This complexity developed, in part, from the desire for a patient-oriented process. Participants recognized that MAiD would be the final act of healthcare they would perform for a client and that it would occur in a client’s last moment of life. This led to an intense desire to get the MAiD process ‘right’ and to provide the most person-centered care in the limited time that clients had left. For example, one nurse contrasted her previous practice in hospital to her current practice in MAiD using the analogy of a wheel and spokes. In her hospital practice she was the wheel and her patients were the spokes; in her MAiD practice that was reversed. However, this was a difficult aspiration to accomplish within a system that was generally not oriented toward providing patient-centered care. The achievement of such a patient-oriented perspective was plagued by difficulties.
This patient-centered perspective meant that nurses prioritized a MAiD-related request and/or provision over other duties. “ I will be dropping everything else that I’m doing when we have a MAiD case. It doesn’t matter what other priorities we have on the go, and I have lots of priorities because I’m the practice lead for a few areas.” P2 Priority tasks in a MAiD situation included assessing clients in a timely manner, coaching and educating clients and their families through the decision-making process, and most importantly, organizing a time and space for death in accordance with patient wishes. In some cases, this prioritization was driven by health policies that stipulated that patient requests had to be addressed within a specified time frame (typically a short one). In other cases, it was driven by the urgency of the request because clients were at risk of becoming incapacitated and then would not be able to provide the requisite final consent.
Once a request for MAiD had been initiated, nurses had to perform these priority tasks within systems that were organized to accommodate MAiD to varying degrees. This rural nurse spoke of the disruptions of continuity of care of caused by the MAiD care system. “The client goes to their doctor, he refers to the MAiD steering committee, and I don’t know who those people are, they refer to my supervisor and it comes back to me. This is probably a patient that I already know.” P39 In contrast, a seamless system included the presence of an organized referral system, willing MAiD assessors and providers, continuity of care with the existing system, ready access to MAiD-related paperwork and patient records, and a physical space within which to provide MAiD. However, even with all of these factors in place, the system could quickly become overwhelmed when a number of patients were requesting MAiD at the same time. For example, many patients and physicians preferred to schedule the death in the evenings or on weekends. This could prove challenging for MAiD providers, particularly for those who were engaged in MAiD as part of their regular Monday to Friday workload. One nurse described how she eventually had to set boundaries around her time. Even though she was supportive of MAiD, and was committed to its accessibility, she admitted that she did not want to spend all of her weekends providing MAiD.
Nurses also became overwhelmed when they were the only providers willing to engage in MAiD. One nurse practitioner shared that she had become the ‘go to’ person because the physicians in her community were not willing to perform MAiD. She was not sure whether this was because of moral reasons or a lack of adequate financial remuneration. But, she was quickly coming to the end of her emotional resources as a sole provider with limited support.
Participants also described having difficulty accessing patient records for their assessment process. This was particularly challenging when requests were urgent or when assessments were conducted over holidays. Further, there was little agreement about the amount of background information that should be provided to, or shared between, independent assessors. Physical space in which to provide MAiD could also be challenging, particularly for those patients who chose not to have MAiD performed in their home. In some cases, institutions where MAiD could occur (e.g., hospital, residence, or hospice) had policies that prohibited patient admissions that were solely for MAiD; however, nurses suggested that this accessibility was improving.
The ability to negotiate responsibilities was also an important part of system capacity. This was particularly relevant when there were dedicated MAiD teams. For example, one participant described how challenging it could be to decide whether a client should be referred to social work or to the MAiD team if a client expressed a wish for a hastened death. This was particularly the case if nurses did not have the time for the in-depth conversation that would enable them to better understand the intent of the request. Without this understanding, it was risky to do an immediate referral if the client was seeking support and it was risky to not do an immediate referral if it could be interpreted as limiting accessibility. Once a MAiD referral was made, it could be difficult to distinguish between the care responsibilities of regular providers and MAiD providers:
So, it’s been a bit of a challenge to delineate what we’re doing in relationship to the request for assisted dying and what normal care still continues to be. So, that’s just a lot of conversations and we go and we meet with teams to say this is our bucket and this is your bucket and we’re all playing in the same sandbox to support the patient, but we all need to help each other. P3
Once a MAiD request had been confirmed, and a time set for provision, nurses were also responsible to organize the support individuals, such as the IV team or pharmacists. In some cases, the IV team required 24 h advance notice to accommodate workload and conscientious objectors. Throughout this process, participants were confronted with complex organizational tasks, within systems that supported those tasks to varying degrees, and with the expectation that they would do their very best for this patient’s final hours.
Specific legislative requirements added a further layer of complexity to the system. For example, the legislation requires that one of the two MAiD assessors must also be the MAiD provider. However, in a person-centered approach, patients can indefinitely prolong the time between assessment and provision. This delay can have a number of implications. It might mean that the client presentation changes since the initial assessment, as described by this participant:
About a month after I saw her for a secondary assessment I realized I've now become her primary provider. But because it's been so long I don't know whether to sign the Form C (clinician assessment form) or not because she actually doesn't have intolerable suffering at this point in time. She goes out for lunch every day with her friends like she's always done. But what happens if next week things turn upside down for her? Somebody else is going to have to come in and do the whole secondary assessment again. You know, without a system in place, it just makes things like that complicated that don't need to be complicated. P30
The participant in the quote above found herself becoming the provider rather than the secondary assessor, but at least she was involved in both. In other situations, nurse practitioners were expected to be providers when they had not completed either of the original two required assessments. This usually occurred when there was a long delay between assessment and provision and the original assessors were no longer available. This placed these nurses in a difficult position, particularly if their assessment differed from the original assessment.
An additional legislative complexity involved the paperwork associated with a MAiD death as well as the coroner interview required post-MAiD in some jurisdictions. This paperwork became more complex with the new reporting requirements introduced by Health Canada in 2018. Nurses described having to endure these reporting requirements right after an impactful and exhausting MAiD administration. The most troubling aspect of these new reporting requirements was the need to defend one’s actions, similar to what one might do in a court of law. The legality of their participation was in question as described by this participant:
The sense is that we have to prove that what we did was okay and that it was right. Our fear is that they're going to challenge us or ask a question that we won't have an answer to. That will put us in a position of feeling like, "Uh oh. What did I do now?" The new legislation [reporting requirements], make it worse. P30
This same participant went on to describe the ironic nature of the self-reporting process that entailed grading one’s diligence in following the legislation:
It is a three-page table that documents in a grid format how we're going to get into trouble if we do things wrong. I mean, that blows my mind, to be honest. I'm thinking, "Is this really necessary? I'm not planning on doing anything wrong (laughs). Why do you have to grade it?" It is a bit bizarre, you know. Not having done due diligence for foreseeable death is a score of 4 which means you get reported to your college. There are some 5s that mean you get reported to the police. But you think, "Hmm, okay. So, if I have provided this service to someone who shouldn't have qualified under the law and who wasn't actually dying then I essentially killed them. That's reported to my college? That should be murder, right? P30
In this anecdote, the participant shows her struggle with the rules of a complex legislated and reporting process that determines the line between assisted death and murder and takes little account of her moral commitment to doing the right thing.
For nurses, the end result of trying to accomplish impactful patient-centered care within a complex system was excessive workload and emotional burden. This resulted in some nurses setting boundaries around their MAiD practice:
I don’t find the provisions so emotionally draining, but it’s more the logistics and it’s a lot of work. The logistics of filling in 16 pieces of paper and making sure they’re all correct so you don’t get into trouble because the consequences are pretty significant. Then there’s organizing the pharmacy, going to pick up the medication, and organizing with the family, organizing with the nurse. Like, there is so much that goes into it. And that part can be so draining. And making it all happens as it should, you know, so that everything lines up. So, I think it’s important not to do too many cases. And that’s what I’ve been focusing on, making sure I’m not taking too much on. P25
This nurse was choosing to set limits on her MAiD-related practice. But for other participants, the cost of working within a system that did not adequately support them was simply too much. The risks of not providing good care or of running afoul of the legal system were just too great.
“Working in this haphazard framework you worry that patients are going to fall through the cracks because, you know, we all have busy worlds. Half of the practitioners I work with on an every-other-day basis say they’re not going to do this anymore.” P30.
Findings from this study describe the impact of a legislated approach to assisted death on Canadian nursing practice and nurses’ experience. Such findings illustrate the proverbial rock and hard place in which nurses’ have obligations in relation to the MAiD legislation but find themselves in the complex situation of trying to negotiate best practices with variable support. Nurses in this study described a high degree of variability in policies and procedures, system processes, and team support across Canadian jurisdictions. They further described the importance of teamwork in facilitating such an impactful event. Finally, they described the complexity of facilitating a patient-centered death within a system that was not always well structured to support their efforts. These factors influenced their experiences with assisted death, and their willingness to take part, beyond any considerations of conscientious objection.
In discussing these findings, it is important to remember the limitations of this study. This was a qualitative study that explored the experiences of 59 registered nurses and nurse practitioners. This data was gathered just 2 years post legislation. As such, it represents nurses’ early experiences with MAiD and complements other early studies of nurses’ experiences in the Canadian context [ 17 , 18 ]. Further, these interviews were conducted by telephone rather than in person. However, in reflecting on the richness, depth, and variability of participant responses, conducting these interviews by telephone may have provided a layer of necessary anonymity for such a controversial topic.
As discussed in the introduction to this paper, the legislated approach to MAiD requires delegation, precision, and obligation [ 5 ]. In this discussion, we will first explore some of the reasons for the variability of practice supports described in this study and relate those to the way that healthcare responsibilities are delegated in Canada. We will then discuss how adequate practice supports are essential to nurses’ abilities to meet the requirements of precision under the MAiD legislation. Finally, we will highlight the tensions that arise in nursing practice as a result of particular obligations inherent in the legislation.
Delegation: supports as a reflection of sociocultural context
In a country that has chosen a ‘hard’ [ 5 ] approach to MAiD, it is intriguing that the development of nursing practice supports have been so variable across the country. In Canada, responsibility for healthcare rests with the provinces and territories. Provincial and territorial governments in turn delegate this responsibility to health authorities through policy direction and financing. Provinces and territories have structured their health authorities differently; some have one health authority for the entire province (e.g., Alberta and Manitoba), others have multiple authorities within a province (e.g., British Columbia and Newfoundland). Health authorities are designed, in part, to be responsive to the needs of their particular population [ 19 ]. Having multiple health authorities across the country can be inefficient when a task as complex as generating MAiD policies and supports is required. However, the variability in available practice supports that was described in these findings may also be an artifact of the interaction between the sociocultural context of each region and the nature of MAiD.
A number of factors make MAiD a contentious healthcare policy issue. First, MAiD is unique in its healthcare outcome. The intent of MAiD, unlike any other procedure done in healthcare, is always to definitively produce death [ 20 ]. Second, MAiD is a morally contentious act. Canadians have a range of responses to MAiD, from believing it to be a morally repugnant act to believing it to be a deeply compassionate act to relieve suffering [ 21 ]. Third, MAiD is new to Canada. Even though healthcare providers have always received requests to hasten death, only now do they have the legal authority to do so [ 22 , 23 ]. Further, the experience of the death itself is vastly different from a normal death [ 8 ]. Such a different, morally complex, and new procedure is likely to be negotiated in profoundly different ways depending upon the sociocultural context. Provinces and territories are known to each be unique sociocultural contexts that are ultimately reflected in their healthcare policy and practice. Provinces in which the majority of citizens would reject MAiD as an option, may also be less likely to prioritize the implementation of MAiD-related structures. As important as it is to reflect the unique values and beliefs of the individuals of a particular region, nurses and other healthcare providers can also be placed in a challenging position. Canadians in certain clinical circumstances can claim a legal right to assisted death , but nurses residing within some jurisdictions may not have adequate systems in place to support their practice in fulfilling that right.
Precision: practice supports in a legislated context
A legislated approach requires a high degree of precision, or a “precise, specific, clear rule for every practice.” (5 p.14) Our review of Canadian nursing regulatory documents indicated that these rules are found in legislation; regulatory guidelines; professional liability guidelines; and employer standards, guidelines, and policies [ 13 ]. Findings from this current study indicated that the necessary rules were present in some contexts but notably absent in others. In addition to these rules, participants spoke of a need for practice supports that would enable them to fulfill the requirements and obligations associated with a MAiD death. They understood that specific rules can only be enacted properly within a context of adequate support and, more importantly, when there was a mismatch between the required precision and contextual supports, nurses recognized that their practice was at risk. For example, the reporting guidelines required by Health Canada [ 24 ] were precise and specific in how they evaluated whether a MAiD procedure complied with the law. But, nurses at times perceived that they did not have adequate resources to meet those requirements. This was evident when nurses indicated they did not have access to required palliative care, to a supportive team, to policies, procedures and systems that would guide their practice, or to a sufficient number of assessors and providers to support the number of patients seeking MAiD. A perceived lack of a supportive system put some nurses in an untenable position. They were engaging in a high-risk practice that contained precise criteria to differentiate between “ MAiD and murder. ” But they were doing so within what one nurse described as “ haphazard ” systems that do not support the necessary degree of precision. Further, it is important to note that while there are reporting systems in place in Canada, there is no specific oversight and review of MAiD practices. This makes it difficult for practitioners to benchmark good practice other than through their own self-report. Also, there is little data upon which to further develop national policies and best practices. The result was that some practitioners were choosing to limit their involvement in MAiD or refuse to engage in it altogether. However, it is important to remember that, when these practice supports were in place, nurses who participated in this study felt confident in their ability to meet precision requirements.
Not all of the uncertainty in this study was related to a lack of precision at the healthcare policy level. Some related this lack of precision to ambiguity in the legislative language itself. Of particular concern is the definition given in Bill C-14 to “grievous and irremediable medical condition,” one of the eligibility requirements for MAiD. A “grievous and irremediable medical condition” is defined within Bill C-14 as requiring four criteria to be met, two of which are that death has become “reasonably foreseeable” and that the “illness, disease or disability or state of decline is causing enduring and intolerable physical or psychological suffering.” The concepts of “reasonably foreseeable” death and “intolerable suffering” in particular have been the subject of significant and ongoing controversy in healthcare, legal and patient advocacy communities [ 25 , 26 , 27 ]. Indeed, since, Bill C-14, the Quebec Superior Court has struck down the requirement that death be “reasonably foreseeable.” [ 28 ] Such controversy was reflected within this study as well. Nurses reported that a reasonably foreseeable death was being interpreted differently by different clinicians. Documents that have attempted to clarify this language from a legal perspective (e.g., 26) may not necessarily be congruent with clinicians’ clinical and moral judgement. This may explain some of the findings in which nurses felt that physicians were placing access barriers in front of patients seeking MAiD. What nurses interpreted as physicians limiting accessibility by telling patients they were not ready for MAiD yet, may actually have been a physician interpretation that the patient’s death was not yet foreseeable . If the death was not foreseeable, then provision of MAiD would violate the legislation and render the assisted death a criminal act. Such lack of precision in terminology led to divergent opinions and practice, and ultimately tensions, among clinicians.
In terms of the language of “irremediable suffering,” nurses in this study believed that such suffering could only be defined by the patient. However, this created doubt in their abilities to adhere to the legislation. This was evident in the difficulty experienced by a participant in checking the box on the reporting guidelines to confirm that the client was enduring irremediable suffering while knowing that the client was still participating in daily enjoyable activities. Such leeway in interpretation made it difficult for nurses in this study to feel as though they were fulfilling their obligation to practice within clear and specific rules. This uncertainty was compounded when nurses could not draw upon the collective wisdom of a supportive team.
Obligation: accessibility and participation
A legislative approach to assisted death also implies a high degree of obligation. Normally, this implies an obligation to fulfill rules in a precise manner [ 5 ]. But the ideal of obligation has taken on a new dimension within Canada because the MAiD legislation was developed because of an appeal to Charter of Rights and Freedoms guarantees. As such, MAiD in Canada has been framed as a right, and as a right, it brings issues of accessibility to the fore. If Canadians have a legal right to MAiD, then the healthcare system has a responsibility to make MAiD accessible (particularly given the Canada Health Act , which confirms accessibility as one of the five essential conditions of the Canadian health system). This idea has generated much debate in Canada. Some MAiD proponents have argued that accessibility means that MAiD should be discussed alongside other end-of-life options, even if the patient has not specifically requested information about MAiD [ 29 ]. Accessibility to MAiD may also be challenging in rural and remote areas where there may be few providers willing to provide MAiD, and where taking on MAiD-related responsibilities can have significant implications for those rural practitioners who also provide palliative care [ 3 , 30 ]. This is particularly difficult when many parts of rural and remote Canada still do not have access to good palliative care [ 31 ]. Gaps in accessibility to palliative care explain, in part, data in this study about how palliative care providers have resisted the development of MAiD. Some practitioners have expressed their concern that the philosophies of assisted dying and palliative care are incompatible with one another while others have argued that the two philosophies may not actually be contradictory [ 32 , 33 ]. However, if the political will to provide accessibility to palliative care is not as strong as the political will to provide accessibility to MAiD, then inevitably it will be easier for patients to access MAiD than to access palliative care. This is of even greater concern when one considers the potential end-of-life healthcare cost savings generated by MAiD-related deaths in Canada [ 34 ].
The obligation to make MAiD accessible influenced nurses’ experiences both positively and negatively. Some nurses worked within well-resourced teams dedicated to patient-centered access, thus fulfilling their ideal of MAiD access for patients who wanted it. However, facilitating accessibility could be more problematic outside of such a team structure. Those nurses who felt that they were obligated to provide MAiD because others in their community refused to do so, found themselves in a difficult position. This was evident in the data when nurses had to erect boundaries around their involvement, either because they were trying to organize this precise act within a poorly designed system or because they were experiencing ill effects of trying to do this emotionally laborious task alone. But, in a climate that focusses on an obligation to access, it is difficult for nurses to decline to participate, particularly as employees of healthcare. For example, in this study, once a decision-maker had chosen to embed a MAiD role within a particular nursing role to improve access, it then became difficult for nurses to decline to participate in MAiD and still fulfill their employment obligations. A number of nurses in this study reflected on how they had never imagined that they would be asked to participate in such an act within their nursing career. Notably, in this study, nurses’ decision to not participate was not always because of a conscientious objection. Rather, that decision could often be attributed to a lack of resources and support, to a difference in philosophies (e.g., palliative care and MAiD), or to a belief that MAiD was inappropriately overshadowing other important healthcare priorities. These reasons for non-participation have been discussed in the literature related to institutional participation in MAiD [ 35 ]. In these situations, and in situations where nurses were conscientious objectors, nurses’ experiences were influenced by how responsive and respectful leaders were in accommodating their decision of whether or not to participate in MAiD.
Clinical implications
MAiD legislation in Canada has led to a dramatically new form of practice There is an opportunity to unpack multiple layers of nursing practice experience to better understand both the implications of the structural context of practice and the moral impact of various care settings and teamwork arrangements. Findings of this study demonstrate the powerful impact of organizational leadership on the workplace policies and culture that significantly determine how nurses experience this new care option. We can also see how the potentially conflicting worldviews of different practice sectors, in this case the specialist palliative care sector and the sector involved in MAiD provision, not only shape the care options accessible to patients, but also the nuances of nursing engagement with patients who are considering or completing MAiD. These data demonstrate a full range of care cultures, from those that place all concerned in states of extreme tension to those that create space for the ambiguity and complexity characteristic of MAiD at this time in Canadian history. As more and more nurses across the international context encounter patients for whom MAiD is a possibility, it will be increasingly important that procedures and supports be put in place to support nursing practice. This is particularly essential where a legislated, or hard, approach to assisted death requires precision, obligation, and delegation. Further, robust policies, and perhaps more importantly, supportive procedures, are required to ensure that nurses can choose to participate, or not, in this radical new end of life care option. Those who choose to participate require supported practice; those who choose not to participate need the freedom to do so without fear that it will negatively influence their colleagues or their employment options. This will be particularly relevant in international contexts where assisted death becomes embedded within health systems, similar to how it has been enacted in Canada.
The nature of the Canadian legislation has spawned new and intimate practice teams that support practitioners to provide patient-centered, high quality care, and mutual support during such a momentous time. However, these data also reveal the potential disruption of currently existing teams and a lack of recognition of the supportive work done by those who may not be directly involved in MAiD assessment and provision. It further reveals the difficulties encountered by those who act as MAiD assessors and providers without the presence of a supportive team. So, although the MAiD legislation provides specificity as to the roles and obligations of assessors and providers, such work cannot be solely delegated to these individuals. Comprehensive care must consider the many collateral persons who provide support throughout the care trajectory, from the time patients first consider MAiD through to the stage of bereavement. All members of the care team clearly feel the need for guidance and insight as to how to manage the moral tensions associated with providing the best care possible through to the end. Further, members of these teams require expertise in how to assess and negotiate the complex patient request for death that may or may not reflect and request for MAiD. Belgian law stipulates that the nursing team should be consulted regarding patient euthanasia requests, although no such requirement exists in the Netherlands [ 12 ]. Evidence derived from nurses in Belgium has attested to the complexity of these conversations. (7, 8) Countries considering the legalization of assisted death should carefully consider the impact of teamwork on best practices, including those having to do with communicating with patients and families.
These findings have permitted a glimpse into the morally difficult and organizationally complex work that a legislated approach to MAiD places upon nurses who are already often coping with highly challenging work environments. Variable practice supports, leadership philosophies, team structures, and system and legislative supports greatly influenced whether nurses were able to confidently meet the hard requirements of a legislated approach. Clearly, in light of a legislated approach to MAiD that requires high degrees of delegation, precision, and obligation we have much work to do in supporting nursing through basic and continuing educational programming, care pathways and best practice guidelines, and workplace teams and environments. Further, we must continue to try to understand the important lessons that the experience of nurses of being caught “between a rock and a hard place” can offer with respect to what this radical new care options mean for all concerned.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to participant confidentiality.
Abbreviations
Canadian Nurses Association
Medical Assistance in Dying
Carter. v. Canada (Attorney General), 2015 1SCR331. https://scc-csc.lexum.com/scc-csc/scc-csc/en/item/14637/index.do . Accessed 15 Nov 2019.
Bill C-14: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying) , SC 2016 , c 3. http://www.parl.ca/DocumentViewer/en/42-1/bill/C-14/royal-assent . Accessed 15 Nov 2019.
Schiller CJ. Medical assistance in dying in Canada: focus on rural communities. J for Nurse Pract. 2017;13(9):628–34.
Article Google Scholar
Health Canada. Fourth Interim Report on Medical Assistance in Dying. https://www.canada.ca/en/health-canada/services/publications/health-system-services/medical-assistance-dying-interim-report-april-2019.html2019 . Accessed 15 Nov 2019.
Luzon G. The practice of euthanasia and assisted suicide meets the concept of legalization. Crim Law Philos. 2018. https://doi.org/10.1007/s11572-018-9474-9 .
Denier Y. Dierckx de Casterle B, De Bal N, Gastmans C. involvement of nurses in the euthanasia care process in Flanders (Belgium): an exploration of two perspectives. J Palliat Care. 2009;25(4):264–74.
Denier Y, Gastmans C, De Bal N, Dierckx de Casterle B. Communication in nursing care for patients requesting euthanasia: a qualitative study. J Clin Nurs. 2010;19(23–24):3372–80.
Denier Y, Dierckx de Casterle B, De Bal N, Gastmans C. “It's intense, you know.” Nurses' experiences in caring for patients requesting euthanasia. Med Health Care Philos. 2010;13(1):41–8.
Dierckx de Casterle B, Denier Y, De Bal N, Gastmans C. Nursing care for patients requesting euthanasia in general hospitals in Flanders, Belgium. J Advan Nurs. 2010;66(11):2410–20.
van de Scheur A, van der Arend A. The role of nurses in euthanasia: a Dutch study. Nurs Ethics. 1998;5(6):497–508.
Suva G, Penney T, McPherson C. Medical assistance in dying: a scoping review to inform nurses’ practice. J Hosp Palliat Nurs. 2019;21(1):46–53.
Pesut B, Thorne S, Greig M, Fulton A, Janke R, Vis-Dunbar M. Ethical, policy, and practice implications of nurses’ experiences with assisted death: a synthesis. Adv Nurs Sci. 2019;42(3):216–30.
Pesut B, Thorne, S., Stager, M.L., Schiller, C., Penney, C., Hoffman, C., Greig, M., & Roussel, J. Medical assistance in dying: a narrative review of Canadian nursing regulatory documents. Pol Polit Nurs Pract 2019;20(3):113–130.
Pesut B, Greig M, Thorne S, Storch J, Burgess M, Tishelman C, Chambaere K, Janke R. Nursing and euthanasia: A narrative review of the nursing ethics literature. Nurs Ethics. 2019; Published online May 21;2019:1–16.
Google Scholar
Thorne S. Interpretive description: qualitative research for applied practice. 2nd ed. New York: Routledge; 2016.
Book Google Scholar
Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine Publishing Company; 1967.
Beuthin R. Cultivating compassion: the practice experience of a medical assistance in dying coordinator in Canada. Qual Health Res. 2018;28(11):1679–91.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;53:511 online July 4.
Hurley J. Regionalization and the allocation of healthcare resources to meet population needs. Healthcare Pap. 2004;5(1):34–9.
Gamble N. Can euthanasia be classified as a medically beneficial treatment? Ethics Med. 2018;34(2):103–11.
Wasylenko E. Becoming dead: two solitudes? Healthc Manage Forum. 2017;30(5):262–5.
Rodriguez-Prat A, van Leeuwen E. Assumptions and moral understandings of the wish to hasten death: a philosophical review of qualitative studies. Med Health Care Philos. 2018;21(1):63–75.
Wright DK, Chirchikova M, Daniel V, Bitzas V, Elmore J, Fortin M-L. Engaging with patients who desire death: interpretation, presence, and constraint. Can Onc Nur J. 2017;27(1):56–64.
Government of Canada. Guidance for reporting on medical assistance in dying Canada.ca. 2018. https://www.canada.ca/en/health-canada/services/medical-assistance-dying/guidance-reporting-summary.html . Accessed 15 Nov 2019.
Reel K. Denying assisted dying where death is not ‘reasonably foreseeable’: intolerable overgeneralizations in Canadian end-of-life law. Can J of Bioeth. 2018;1(3):71–81.
Downie J, Scallion K. Foreseeably unclear: the meaning of the “reasonably foreseeable” criterion for access to medical assistance in dying in Canada. Dalhouse Law J. 2018. https://doi.org/10.2139/ssrn.3126871 .
Downie J, Chandler JA. Interpreting Canada's medical assistance in dying legislation. Montreal, Quebec: Institute for Research on Public Policy; 2018. http://irpp.org/wp-content/uploads/2018/03/Interpreting-Canadas-Medical-Assistance-in-Dying-Legislation-MAiD.pdf . Accessed 15 Nov 2019
Thanh Ha T, Grant K. Quebec court strikes down restriction to medically assisted dying law, calls it unconstitutional. Globe and Mail; 2019.
Daws T, Landry JT, Viens P, Beuthin R, Maynard E, Reggler JG, et al. Bringing up medical assistance in dying (MAiD) as a clinical care option. Can Assoc MAiD Assessors Providers. 2019:1–10. https://camapcanada.ca/wp-content/uploads/2020/01/Bringing-up-Medical-Assistance-In-Dying.pdf .
Collins A, Leier B. Can medical assistance in dying harm rural and remote palliative care in Canada? Can Fam Physician. 2017;63(3):186–90.
PubMed PubMed Central Google Scholar
Canadian Institute for Health Information. Access to palliative care in Canada. 2018. https://www.cihi.ca/sites/default/files/document/access-palliative-care-2018-en-web.pdf . Accessed 15 Nov 2019.
Radbruch L, Leget C, Bahr P, Muller-Busch C, Ellershaw J, De Conno F, et al. Euthanasia and physician-assisted suicide: a white paper from the European association for palliative care. Pall Med. 2016;30(2):104–16.
Dierickx S, Deliens L, Cohen J, Chambaere K. Involvement of palliative care in euthanasia practice in a context of legalized euthanasia: a population-based mortality follow-back study. Pall Med. 2018;32(1):114–22.
Trachtenberg AJ. Cost analysis of medical assistance in dying in Canada. CMAJ. 2017;189(3):E101–5.
Shadd P, Shadd J. Insitutional non-participation in assisted dying: changing the conversation. Bioeth. 2017;00:1–9.
Download references
Acknowledgements
The authors would like to acknowledge the participants who gave so generously of their time and stories.
Funding for this study was provided through a CIHR Project Grant 201610PJT 376065. BP is supported, in part, by the Canada Research Chairs program. Neither funding sources had any role in the design of the study; collection, analysis, and interpretation of data; or in the writing of the manuscript.
Author information
Authors and affiliations.
Canada Research Chair in Health, Ethics, and Diversity, University of British Columbia Okanagan, 1147 Research Road, Okanagan, Kelowna, BC, V1V 1V7, Canada
Barbara Pesut & Madeleine Greig
University of British Columbia, T201-2211 Wesbrook Mall, Vancouver, BC, V6T 2B5, Canada
Sally Thorne
University of Northern British Columbia, Prince George, BC, V2N 4Z9, Canada
Catharine J. Schiller
Policy, Advocacy and Strategy, Canadian Nurses Association, 50 Driveway, Ottawa, Ontario, K2P 1E2, Canada
Josette Roussel
You can also search for this author in PubMed Google Scholar
Contributions
BP: study design, data collection and analysis, manuscript writing. ST: study design, data analysis, manuscript writing. CJS: manuscript writing and revision. MG: data collection and analysis, manuscript writing. JR: data analysis, manuscript revision. All authors read and approved the final manuscript.

Author’s information
BP studies medical assistance in dying as part of a larger research focus on palliative and end-of-life care.
ST’s interest in MAiD develops upon her longstanding research interest in the impact of health care provider communication on cancer and chronic illness experience.
CJS is a nurse and non-practicing lawyer who teaches in the BScN and MScN programs at the University of Northern British Columbia. She has published about the implications of MAiD for nurses and nurse practitioners who practice in rural and remote Canadian communities.
MG coordinates the CIHR-funded study exploring the practice, policy and ethical implications of Canadian nursing roles in MAiD.
JR’s current role as a program lead, nursing practice and policy at the Canadian Nurses Association (CNA) is pivotal to understanding the implications of research findings and the development of a national policy. Josette was responsible for the Canadian Nurses Association policy and advocacy work on medical assistance in dying, successfully resulting in Bill C-14 recognizing and protecting the important role registered nurses and nurse practitioners play in medical assistance in dying. Josette led the development of the National Nursing Framework on Medical Assistance in Dying in Canada.
Corresponding author
Correspondence to Barbara Pesut .
Ethics declarations
Ethics approval and consent to participate.
This study received ethical approval from the University of British Columbia Okanagan Behavioural Research Ethics Board. Reference H17–01295. Written informed consent was provided by all study participants.
Consent for publication
Not applicable.
Competing interests
JR is employed by the Canadian Nurses’ Association, a national professional association and advocacy organization for Canadian nursing.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Interview guide, Policy, Practice, and Ethical Implications of Medical Assistance in Dying: Semi-Structured Interview Guide. This was the initial guide that received ethical approval; however, it is important to note that this was a draft guide. In keeping with semi-structured interviews, additional questions may have been asked.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Pesut, B., Thorne, S., Schiller, C.J. et al. The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nurs 19 , 12 (2020). https://doi.org/10.1186/s12912-020-0404-5
Download citation
Received : 08 April 2019
Accepted : 31 January 2020
Published : 17 February 2020
DOI : https://doi.org/10.1186/s12912-020-0404-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- (3-10) Assisted death
- Medical assistance in dying
- Palliative care
- Nursing practice
- Assisted suicide
- Legislation
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Study protocol
- Open access
- Published: 21 July 2021
Medical Assistance in Dying in patients with advanced cancer and their caregivers: a mixed methods longitudinal study protocol
- Madeline Li ORCID: orcid.org/0000-0002-3977-7437 1 , 2 na1 ,
- Gilla K. Shapiro ORCID: orcid.org/0000-0002-2214-8263 1 , 3 na1 ,
- Roberta Klein 1 ,
- Anne Barbeau 1 ,
- Anne Rydall ORCID: orcid.org/0000-0002-4692-9101 1 ,
- Jennifer A. H. Bell ORCID: orcid.org/0000-0003-3617-6852 1 , 2 , 4 ,
- Rinat Nissim ORCID: orcid.org/0000-0002-3624-5806 1 , 2 ,
- Sarah Hales ORCID: orcid.org/0000-0001-6404-8124 1 , 2 , 3 ,
- Camilla Zimmermann ORCID: orcid.org/0000-0003-4889-0244 1 , 2 , 3 , 5 ,
- Rebecca K. S. Wong 1 , 6 &
- Gary Rodin ORCID: orcid.org/0000-0002-6626-6974 1 , 2 , 3
BMC Palliative Care volume 20 , Article number: 117 ( 2021 ) Cite this article
7059 Accesses
6 Citations
7 Altmetric
Metrics details
The legal criteria for medical assistance in dying (MAiD) for adults with a grievous and irremediable medical condition were established in Canada in 2016. There has been concern that potentially reversible states of depression or demoralization may contribute to the desire for death (DD) and requests for MAiD. However, little is known about the emergence of the DD in patients, its impact on caregivers, and to what extent supportive care interventions affect the DD and requests for MAiD. The present observational study is designed to determine the prevalence, predictors, and experience of the DD, requests for MAiD and MAiD completion in patients with advanced or metastatic cancer and the impact of these outcomes on their primary caregivers.
A cohort of patients with advanced or metastatic solid tumour cancers and their primary caregivers will be recruited from a large tertiary cancer centre in Toronto, Ontario, Canada, to a longitudinal, mixed methods study. Participants will be assessed at baseline for diagnostic information, sociodemographic characteristics, medical history, quality of life, physical and psychological distress, attitudes about the DD and MAiD, communication with physicians, advance care planning, and use of psychosocial and palliative care interventions. Measures will subsequently be completed every six months and at the time of MAiD requests. Quantitative assessments will be supplemented by qualitative interviews in a subset of participants, selected using quota sampling methods.
This study has the potential to add importantly to our understanding of the prevalence and determinants of the DD, MAiD requests and completions in patients with advanced or metastatic cancer and of the experience of both patients and caregivers in this circumstance. The findings from this study may also assist healthcare providers in their conversations about MAiD and the DD with patients and caregivers, inform healthcare providers to ensure appropriate access to MAiD, and guide modifications being considered to broaden MAiD legislation and policy.
Peer Review reports
Following the decision of the Supreme Court of Canada on February 6, 2015 to decriminalize medical assistance in dying (MAiD), [ 1 ] the Federal Parliament of Canada passed Bill C-14 on June 17, 2016 to establish the legal eligibility criteria for MAiD. These criteria included the presence of a serious and incurable medical condition, an advanced state of irreversible decline in capability, enduring and intolerable physical or psychological suffering, and a reasonably foreseeable natural death [ 2 ]. Bill C-14 excluded mature minors or those with mental illness as the sole underlying medical condition. Legislative review of these criteria are now underway, and the passage of Bill C-7 on March 17, 2021 removed the requirements of a "reasonably foreseeable natural death" [ 3 , 4 ].
Over 21,500 people in Canada chose to end their lives through assisted dying in the first five years of MAiD, more than 67% of whom had advanced cancer [ 4 ]. The frequency of MAiD in Canada is increasing annually, [ 5 ] although the overall proportion of medically assisted deaths is in the middle of the international rates reported. These range from 0.3% of deaths in Oregon, United States, to 4.6% in the Netherlands [ 4 , 6 ]. In 2019, MAiD deaths in Canada represented approximately 2.5% of all deaths, [ 4 ] and 6.3% of cancer-related deaths [ 4 , 7 ]. Footnote 1
In 2007, we completed a longitudinal study of the desire for death (DD) in individuals with advanced cancer [ 8 ]. This early research confirmed that the DD occurs on a continuum from the passive wish that the end would come earlier than it would otherwise naturally occur, referred to as the desire for hastened death (DHD) or the wish to hasten death (WTHD), [ 9 , 10 , 11 ] to a more active desire to end life, reflected in requests for MAiD [ 12 ]. The DD is uncommon in patients with advanced cancer receiving active treatment, [ 8 ] but is reported in up to half of all individuals in palliative care, [ 13 , 14 , 15 ] and may paradoxically coexist with the will to live [ 16 ]. This paradox underlines the complexity of psychological states related to the DD and the importance of reflective conversations before action on such wishes is taken [ 17 ].
Research examining attitudes and correlates of the WTHD in patients with advanced cancer has largely been cross-sectional, retrospective or conducted in settings where assisted dying is not permitted [ 18 , 19 , 20 , 21 , 22 ]. In research conducted in palliative care settings, a transient WTHD was found in 11–55% of patients, while 3–20% reported a more pervasive and persistent wish to die [ 13 ]. In a Canadian survey of 377 cancer patients with a prognosis of less than six months, Wilson and colleagues [ 13 ] found that almost 70% reported no WTHD, more than 18% acknowledged a transient WTHD, and over 12% reported a clear and persistent WTHD on the Desire for Death Rating Scale [ 14 ]. These findings are consistent with our previous study in which more than 65% of patients with advanced cancer indicated they wanted to continue living regardless of the pain or suffering that their disease might cause, and only 1.2% reported a clear WTHD on the Schedule of Attitudes towards Hastened Death (≥10) [ 8 ]. This difference between the two studies is likely due to the Wilson study sampling patients closer to the end of life, whereas we studied ambulatory patients recruited from oncology clinics.
Studies have also found that the DD fluctuates widely over time, [ 8 , 14 , 23 , 24 ] even during the last two weeks of life [ 25 ]. In a sample of almost one thousand American patients with advanced disease, Emanuel and colleagues found that more than 10% reported seriously considering assisted death for themselves. However, on follow-up two to six months later, approximately half had changed their minds, and an almost equal number who had not initially been interested in assisted death were then considering it [ 26 ].
The DD in patients with advanced cancer may arise from a complex interaction of factors, such as the experience or fear of uncontrolled physical or psychological suffering, the wish to maintain a sense of personal autonomy, or the desire to avoid burdening others (Fig. 1 ) [ 27 , 28 ]. It has also been associated with pain, high disease burden, low self-esteem, poor spiritual well-being, attachment insecurity, being unmarried, younger age, and having a history of psychiatric illness [ 18 , 25 , 26 , 29 , 30 , 31 , 32 ]. Some of these factors, such as those related to self-esteem, spiritual well-being, and attachment security, may be modifiable through specific psychotherapies, such as Managing Cancer and Living Meaningfully, [ 33 ] a brief, supportive-expressive intervention developed by our team and now being delivered internationally. Attachment security refers to an individual’s expectations and preferences regarding support from significant others in times of need and the capacity to make use of such support to relieve distress [ 34 ]. A secure attachment style, reflecting comfort with closeness and reliance on others, has been shown to protect against depression in cancer patients [ 35 ]. An avoidant attachment style, characterized by inflexible self-reliance, the need for personal control, and reluctance to accept support from others, has been associated in cancer patients with problematic relationships with oncologists [ 36 ] and requests for assisted dying [ 30 , 37 ].

MAiD, Medical Assistance in Dying; WTHD, Wish to Hasten Death
Physical symptom burden has been found to predict the DD [ 8 , 26 , 29 ] in patients with advanced cancer, although the motivation for MAiD in those who request and receive it is more often related to the loss of meaning, autonomy, and identity [ 19 , 38 , 39 ]. Some studies have found that religious observance and religious denomination have been linked to attitudes about assisted dying [ 40 , 41 ]. The influence of social and demographic factors on MAiD requests also deserves further exploration. Research thus far indicates that MAiD completion is more common in those who are older, Caucasian, more highly educated, and more affluent [ 38 , 39 ].
Dramatic changes have occurred over the past decade in Canada and throughout the world in public attitudes and expectations about death and dying, in access to psychosocial and palliative care for cancer patients, and, most recently, in the availability of MAiD. These changes may increase the likelihood that individuals with advanced disease and their caregivers will reflect upon and communicate the DD, engage in advance care planning, or consider actions to end their lives. While patients who request MAiD most often have access to specialized palliative care in settings where this is available, [ 4 , 42 , 43 ] the extent to which early palliative and supportive care interventions and empathic communication with healthcare providers about the goals of care at the end of life can affect the DD and requests for MAiD is unknown. Further, although caregivers are likely to be affected by patients’ DD and MAiD requests, [ 44 , 45 , 46 , 47 , 48 , 49 ] there is only limited research evaluating their experiences and support needs in these circumstances [ 20 , 26 , 48 ].
Caregivers typically experience a dramatic change in their daily lives and roles following the diagnosis of cancer or advanced disease in a loved one, related to the loss of family income [ 48 ] and the requirements for practical, social, and emotional support [ 47 , 49 ]. They must often shoulder the physical and psychological burden of caregiving, while also facing the suffering and threat of mortality in their loved one, their own fear of facing the future alone, and the financial strain caused by the illness. Although decisions about assisted dying may have an impact on primary caregivers, we know relatively little about the impact of their distress on the emergence and persistence of the DD and MAiD requests in patients with advanced cancer [ 50 ]. Understanding the experience of caregivers in relation to MAiD is therefore an important area in need of further research.
Optimal end-of-life care for patients with advanced cancer requires healthcare providers to engage in conversations with those who express a DD and/or who request MAiD. Cross-sectional research has identified some factors associated with the DD and MAiD requests, but it is not possible from such studies to distinguish confounding from correlational and causal factors, or to determine the course of an individual’s desire for MAiD in the face of advanced cancer.
We will be conducting a longitudinal study to examine the prevalence, trajectory, predictors, and nature of the desire for MAiD in a geographic setting where MAiD is legally available. The goals of this mixed methods study are to estimate the prevalence of the DD in patients with advanced cancer; to understand the trajectory and contributors to the DD, MAiD requests and MAID completion; and to elucidate the experience and support needs of their primary caregivers. The findings of this study could inform the training of healthcare providers regarding conversations with patients with advanced cancer and their caregivers about goals of care at the end of life, the DD, and MAiD as well as psychotherapeutic conversations about the DD. This information will also support the review of legislation to ensure appropriate access to MAiD.
To determine in patients with advanced cancer:
The prevalence of the DD, MAiD requests, and MAiD completions.
The trajectory and predictors of the DD, MAiD requests, and MAiD completions.
To examine the predictors of distress in primary caregivers of patients with advanced cancer.
Study design
This research is a prospective, longitudinal, mixed methods study conducted with patients with advanced or metastatic cancer and their primary caregivers. This study was approved on September 2, 2020, by the University Health Network Research Ethics Board (UHN REB #18–6182), and all participants will provide informed consent. Any protocol amendments will be submitted to the UHN REB for approval, and important changes that could impact participants’ willingness to continue in the study will be communicated to them in a timely manner. Data collection is expected to begin by January 2021.
Participants and setting
We plan to retain a longitudinal cohort of 600 patients with advanced or metastatic cancer and 300 of their primary caregivers recruited from the outpatient medical oncology clinics at the Princess Margaret Cancer Centre (PM), University Health Network, in Toronto, Canada’s largest comprehensive cancer treatment, education and research centre. This sample size is required to test our proposed regression model for predictors of MAiD requests and completions (Fig. 1 ), in which we will need at least 110 patients with at least two data points (baseline and one follow-up) [ 8 ], based on five to ten observations required for each of the 11 predictors included in our SEM [ 51 ]. Given that MAiD accounts for almost 5% of cancer deaths, and this represents 26% of MAiD requests at PM [ 39 ], we estimate ~ 115 subjects requesting MAiD and ~ 30 subjects receiving MAiD among 600 recruited patients.
To accommodate an anticipated 25% drop-out rate, we will recruit 800 patients and 400 primary caregivers over approximately 3.5 years for a final sample size of 600 patients and 300 primary caregivers. This is feasible given that PM provides care for approximately, 3200 Stage III or IV cancer patients per year, 60% of whom are expected to meet inclusion criteria; a conservative estimate is that 50% will provide informed consent, yielding approximately 960 eligible and consenting participants per year.
Participant recruitment and eligibility
Patients will be included if they: 1) are age 18 years or older; 2) are able to speak and read English sufficiently well to provide informed consent and complete questionnaires and/or interviews; and 3) have been diagnosed with advanced or metastatic solid tumour cancers of any type. Exclusion criteria will include: 1) significant cognitive impairment documented in their medical record or indicated by a score of < 20 on the Short Orientation-Memory-Concentration Test (SOMC); and 2) lack of sufficient proficiency in the English language to provide informed consent and complete the questionnaires and/or interviews. Trained research personnel will conduct the informed consent discussion with eligible and interested patients. Eligible patients who decline to participate will be asked their permission to allow the research team to document basic demographics to allow for later assessment of generalizability. Participants who begin the study will be considered withdrawn if they are later unable to participate due to a deterioration in cognitive functioning or physical capacity.
Individuals identified by participants as their primary caregivers will be approached by research personnel for recruitment if they are: 1) age 18 years or older; and 2) able to speak and read English sufficiently well to provide informed consent and complete questionnaires and/or interviews. A primary caregiver may be the spouse or partner of the patient, a relative or other family member, or a close friend. Caregivers may continue to participate in this study even if the patient participant subsequently withdraws from the study.
Study measures
Questionnaire package.
At baseline, patients and caregivers will complete both sets of baseline-only and follow-up measures. All participants will provide sociodemographic information at baseline. The Short Orientation-Memory-Concentration Test (SOMC) [ 52 ] will be conducted with patients at baseline in order to test patient’s cognitive function; this measure may be repeated at follow-up at the discretion of the research assistant. See Tables 1 and 2 for a description of the key study measures listed below, and Fig. 2 for the schedule of participant assessments.
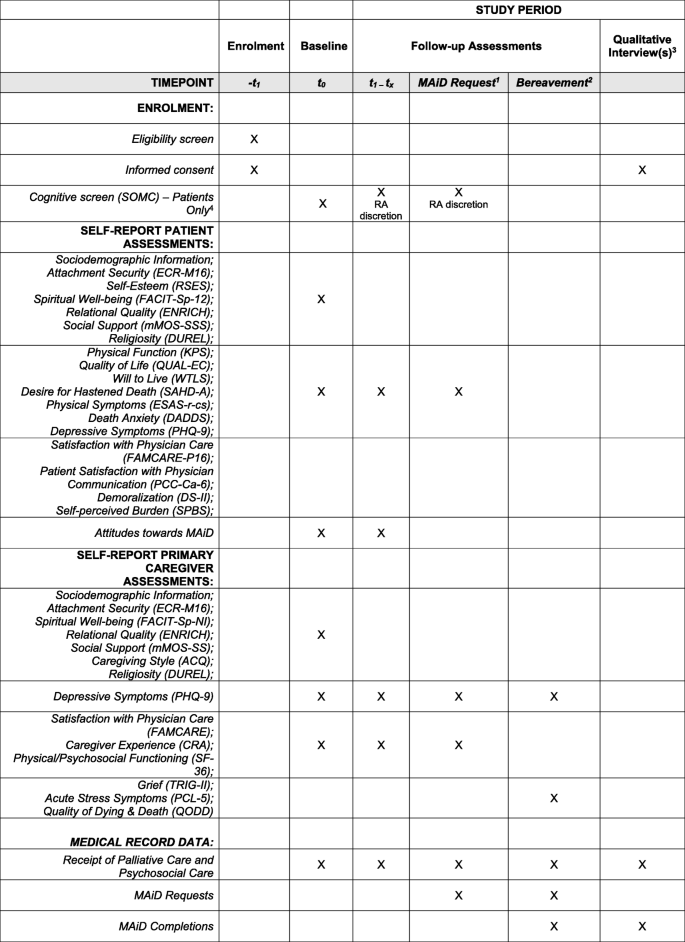
1 If a patient requests MAiD during the study, even if it falls between the 6 monthly scheduled time points, the patient and their primary caregiver (if applicable), will be invited to complete a follow-up assessment and a qualitative interview at this time. 2 In the event that a patient dies during the study (whether by MAiD or other causes), the patient’s primary caregiver (if applicable), will be approached within 6 months of the patient’s death to complete a final follow-up bereavement assessment and a qualitative interview. 3 In addition to qualitative interviews with patients requesting MAiD and their participating caregivers, and bereavement interviews with participating caregivers whose loved ones die during the study, a subset of participants (patients and caregivers) will be identified through purposeful sampling and invited to complete one or more qualitative interview(s) at the 6 monthly follow-up time points over the course of the study. 4 The SOMC may be re-administered at the discretion of the study research assistant if they feel the patient’s cognitive status may be impaired or have declined since the previous assessment. In the event that a patient fails a cognitive screen during the study, they will be withdrawn by the study principal investigator
Patient Baseline-Only Measures : Attachment Security: Brief Modified Experiences in Close Relationships scale (ECR-M16) [ 89 ]; Spiritual Well-being: Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being scale (FACIT-Sp-12, 58) Relational Quality: ENRICH Marital Satisfaction Scale (ENRICH) [ 74 ]; Social Support: The modified Medical Outcomes Study Social Support Survey (mMOS-SSS) [ 75 , 76 ]; Religiosity: The Duke University Religion Index (DUREL) [ 77 ]; and, Self-Esteem : The Rosenberg Self-Esteem Scale (RSES) [ 64 ].
Patient Baseline and Follow-up Measures: Physical Function: The Karnofsky Performance Status index (KPS) [ 53 , 54 ]; Quality of Life: The Quality of Life at the End of Life Scale-Cancer scale (QUAL-EC) [ 55 , 56 ]; Will to Live: The Will to Live Scale (WTLS) [ 57 ]; Desire for Hastened Death: The Schedule of Attitudes towards Hastened Death–Abbreviated (SAHD-A) [ 58 ]; Depressive Symptoms: Patient Health Questionnaire-9 (PHQ-9) [ 59 ]; Physical Symptoms: Edmonton Symptom Assessment System-Revised, including constipation and sleep disturbance (ESAS-r-cs) [ 60 , 61 , 62 ]; Death Anxiety: Death and Dying Distress Scale (DADDS) [ 65 , 66 , 67 ]; Patient Satisfaction with Physician Communication: Patient-Centered Communication-Cancer-6 items (PCC-Ca-6) [ 68 ]; Satisfaction with Physician Care: Modified FAMCARE Scale – Patient-16 items (FAMCARE-P16) [ 63 ]; Demoralization: Demoralization Scale-II (DS-II) [ 70 , 79 ]; and, Self-Perceived Burden: Self-Perceived Burden Scale (SPBS) [ 71 ]. Participants will also answer several questions to assess their attitudes towards MAiD.
Caregiver Baseline-Only Measures: Attachment Security: Brief Modified Experiences in Close Relationships scale (ECR-M16) [ 89 ]; Spiritual Well-being: Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being–Non-illness version (FACIT-Sp-NI) [ 72 , 73 ]; Relational Quality: ENRICH Marital Satisfaction Scale (ENRICH) [ 74 ]; Social Support: The modified Medical Outcomes Study Social Support Survey (mMOS-SSS) [ 75 , 76 ]; Caregiving Style: The Adult Caregiving Questionnaire [ 78 ]; Religiosity: The Duke University Religion Index (DUREL) [ 77 ].
Caregiver Baseline and Follow-up Measures: Depressive Symptoms: Patient Health Questionnaire-9 (PHQ-9) [ 59 ]; Satisfaction with Physician Care: FAMCARE Scale (FAMCARE) [ 69 ]; Caregiver Experience: The Caregiver Reaction Assessment scale [ 80 ]; Physical and Psychosocial Functioning: The Medical Outcomes Study Short-Form 36 (SF-36) [ 82 ].
We will also administer measures to caregivers six months post-patient death: Grief: The Texas Revised Inventory of Grief-Part II (TRIG-II) [ 83 , 84 ]; Traumatic Stress Symptoms: The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) [ 85 , 86 ]; Quality of Death: The Quality of Dying and Death questionnaire (QODD) [ 87 ]; and, Depressive Symptoms: Patient Health Questionnaire-9 (PHQ-9) [ 59 ].
Chart Review Form: Patients’ medical records will be reviewed at baseline and at each follow-up in order to document: i) medical diagnosis, date of diagnosis, and current cancer stage; ii) medical history including current comorbid medical and psychiatric diagnoses; iii) treatments received, including the timing of psychosocial oncology and/or palliative care interventions; and iv) emergent DD/suicidality events. We will obtain from the MAID clinical database the reasons of the patient and/or assessor-rated reasons for MAiD requests, MAiD approvals, MAiD completions, and non-completions.
Qualitative Interview: A semi-structured interview will be used. This interview guide will be further developed and reviewed as the constant comparative analysis progresses [ 90 ]; emerging themes in earlier interviews will serve to refine interview questions and probes. Open-ended enquiry will be made in the initial interview to understand the illness experience, including; caregiver stress, burden, support needs and support received, emotional and physical distress; attitudes about MAiD and advance directives. All interviews will be audiotaped, transcribed verbatim, verified and de-identified prior to analysis.
Data collection procedures
Baseline assessment.
Participants will be given the option of taking the questionnaire package home and returning the completed package in a self-addressed stamped envelope or completing it online. Participants will also be provided the option of having the questions read to them by a member of the research team as some participants may require this assistance due to their state of health. Medical data will be extracted from review of the medical record of each patient.
Longitudinal follow-up assessments
Participants will complete follow-up questionnaires every six months until study completion, unless they voluntarily withdraw, are unable to participate due to impairment in cognitive or physical functioning or die. An additional assessment will be made at the time of a MAiD request. Following the assessment, the medical record review will be updated. Where applicable, the date of death will be obtained from the medical record. In the case of patient death, participating primary caregivers will be followed-up approximately six months after this event to complete a bereavement assessment.
Qualitative assessments
Qualitative interviews will be conducted in a subset of the study participants. A quota sampling method [ 51 ] will be used to select a subset of patients and primary caregivers for one or more qualitative interview(s), conducted at six monthly intervals. Purposeful sampling will be based on high and low outcomes on the Schedule of Attitudes towards Hastened Death-Abbreviated (SAHD-A) (for patients) [ 58 ], caregiving burden and distress measures (for caregivers), and sociodemographic representation (for both patients and caregivers). We estimate that the saturation point will be reached at 10–15 participants per group, but we will recruit participants until saturation is reached. A grounded theory approach with constant-comparative analysis [ 90 ] will be used to identify themes and to determine the sample size at saturation point [ 91 ]. The interviews will last up to 60 min, depending upon the participants’ ability to participate, and will be conducted by a trained interviewer at the convenience of the participants over the telephone, in the clinic, or using a UHN-approved online platform. A frequency of six-monthly intervals was chosen in order to minimize participant burden but still capture as much of their longitudinal experience as possible. Enquiry will be made in follow-up interviews about issues raised in the first interview. Should a participating patient request MAiD, they, and their primary caregiver (if applicable), will be invited to complete an interview at that time, even if it falls between scheduled time points. Should a participating patient die during the study, either from MAiD or other causes, their primary caregiver (if applicable) will also be invited to complete one final semi-structured interview approximately six months after the patient’s death.
Data analysis
Survey data.
Descriptive statistics, desegregated by sex and gender, will be calculated to provide summary information about the characteristics of the participants at baseline. For each assessment time, descriptive statistics will be calculated for the DD outcomes and all other predictive variables. Prevalence of the DD, as measured by the SAHD-A, will be compared to our historical dataset [ 92 ]. The distributions of the continuous variables will be examined for non-normality, and transformations will be employed where necessary. Bivariate associations between DD variables and baseline medical and sociodemographic factors, as well as associations of these baseline variables with physical, psychosocial, and psychological risk factors will be described by calculating subgroup means and standard deviations for categorical variables and correlation coefficients for continuous variables.
The analysis of the longitudinal data will be conducted using mixed linear models (MLM), [ 93 ] which can take into account incomplete data and both time-varying and time-invariant predictors. To accommodate anticipated variations in individual profiles, random effects models will be fitted. MLM logistic regression will be used to determine predictors of both MAiD requests and completions. Similar exploratory analyses will be conducted to identify associations with emergent suicidality. We will replicate the MLM analysis from our previous study of the DD, [ 8 ] now incorporating receipt (or not) of psychosocial and/or palliative care interventions, and death anxiety as additional predictors of the DD (Fig. 1 ). To examine the statistical significance of interactions among medical, sociodemographic, physical, and psychosocial factors as suggested by the exploratory analyses, relevant interaction terms will be included in the MLMs. To avoid over-fitting the model, only those interactions regarded as clinically relevant will be tested in the model.
Qualitative interviews
A grounded theory approach will guide the qualitative data collection and analysis [ 94 ]. Conceptual categories and themes for coding will be derived directly from analyzing the interview material, with a view to inspecting deviant or negative cases in order to refine emerging propositions or hypotheses. This iterative process will continue until theoretical saturation is reached. The data analysis will use an inductive, constant comparison method to code or index the data. Once all data that matches that theme have been located, the process will be repeated to identify further themes or categories. Categories will be added to reflect the nuances in the data as possible. Cross-indexing will allow for the analysis of data items that fit into more than one category. Systematic comparative analysis will be used to identify differences and similarities between men and women, and those with and without a high DD (for patients), and with and without high caregiving burden and/or distress (for caregivers). Categories will also be examined in a longitudinal manner to identify patterns of emergence and development of categories over time and these finding will be compared to the quantitative data, particularly for the impact of goals of care conversations on desire for MAiD. Our analysis will be informed by our previous qualitative study on the DD [ 12 ].
Methodological strengths
This project is a longitudinal study of the course, predictors, and nature of the desire for MAiD in patients with advanced cancer in a geographic setting where MAiD is legally available. It includes quantitative and qualitative methods and uses a comprehensive battery of validated scales to measure the physical and psychosocial variables that we hypothesize are associated with the DD and MAiD requests and completions. The large study sample of patients and caregivers is a strength of the study design, enabling the evaluation of hypotheses in sub-groups. The study also will collect a wide range of sociodemographic information, which will enable the evaluation of the social determinants of the DD and MAiD, as well as examination of health equity in the receipt of MAiD. The quality of the research data collected will be ensured by having experienced, trained research personnel follow best research practices and institutional guidelines, including the use of standardized source notes and documentation of study participation in the patient’s clinical research record, to ensure rigour in the data collection processes. Research personnel will employ direct online data entry whenever possible; duplicate data entry for questionnaires completed in hard copy; and verification of transcribed interviews and all data extracted through medical chart review (e.g., disease and treatment-related data, supportive care services data, MAiD clinical data). Processes for confidentiality and secure storage of data have been ensured through REB approval, and data will be retained for 10 years post study completion as per REB guidelines at our institution. Further, all studies at PM are subject to internal audit by the Cancer Clinical Research Unit and/or the UHN Research Quality Integration teams, both of whom are independent of the study team.
Foreseeable limitations and mitigation strategies
The main challenge of this study is the requirement to recruit a large sample of patients with advanced or metastatic cancer and their primary caregivers. However, in our previous research experience with this population, we found that a 60% recruitment rate is achievable, without adverse effects from completion of a battery of measures of this kind [ 8 ]. Although there are a relatively large number of measures, we have minimized participant burden by limiting the number of measures administered longitudinally, selecting measures that are relatively brief or have been shortened from their original versions, offering the option of printed copy and online questionnaire completion at the hospital or at home, providing assistance with completion of questionnaires as requested in-person, online, or over the telephone, and conducting the qualitative interviews at the participants’ convenience. Participants with significant suicidality, physical or emotional distress identified by the research staff will be offered referral for psychosocial oncology and palliative care services in the Department of Supportive Care at PM, with notification to the attending oncologist with the patient’s consent. For caregivers (including bereaved caregivers) who express significant distress when completing the measures or qualitative interviews, a referral to the Department of Supportive Care’s Caregiver Clinic at PM for bereavement and/or psychosocial support will be offered.
Knowledge translation
Integral to the goals of this study is knowledge translation in the form of training healthcare providers to respond appropriately to expressions of the DD from patients in this new era of MAiD. Our findings will be directly incorporated into UHN MAiD training workshops, invited speaker engagements and the UHN MAiD website, to inform MAiD teams. Dissemination will occur through publications and conference presentations locally, nationally, and internationally, and as well as via the website of the Global Institute of Psychosocial, Palliative and End-of-Life Care (GIPPEC; see www.gippec.org ) and the Canadian Association of MAiD Assessors and Providers (CAMAP; see camapcanada.ca), thus bridging the knowledge to action gap.
Study implications
Data from this study will contribute significantly to our understanding of the DD in a setting where MAiD is legal, and inform critical questions regarding the utility of advance directives for MAiD, the management of depression in MAiD assessment, and how to guide healthcare providers in responding to DD statements with advanced cancer patients. The findings from this study will inform the training of oncologists and other healthcare providers in conversations about the DD and MAiD, and the assessment for MAiD eligibility through identifying distinctions between the DD, depressive suicidality, and the desire for MAiD in patients with advanced cancer. The results will also provide an evidence base to inform proposed changes in MAiD legislation, including the potential permissibility of MAiD in mental illness and as an advance directive.
Availability of data and materials
The datasets to be generated and/or analysed during the current study will not be publicly available due to institutional privacy and confidentiality guidelines. Additional information may be available from the corresponding authors on reasonable request.
The percentage of total cancer-related deaths in Canada was calculated by dividing MAID-related cancer deaths in 2020 (5,248) [ 4 ] by total cancer deaths in 2020 (83,300) [ 7 ].
Abbreviations
Caregiver Reaction Assessment scale
Death and Dying Distress Scale
Desire for Death
Desire for Hastened Death
Demoralization Scale-II
Diagnostic and Statistical Manual for Mental Disorders, 5th Edition
Duke University Religion Index
modified Experiences in Close Relationships scale
ENRICH Marital Satisfaction Scale (ENRICH)
Edmonton Symptom Assessment System-Revised (including constipation and sleep disturbances)
Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being scale
Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being-Non-Illness version
Modified FAMCARE Scale for Patients
Karnofsky Performance Status index
Medical Assistance in Dying
Mixed Linear Models
modified Medical Outcomes Study - Social Support Survey
Patient-Centered Communication-Cancer-6 items
Posttraumatic Stress Disorder Checklist for DSM-5
Patient Health Questionnaire-9
Princess Margaret Cancer Centre
Quality of Dying and Death questionnaire
Quality of Life at the End of Life – Cancer scale
Schedule of Attitudes towards Hastened Death-Abbreviated
short Orientation-Memory-Concentration Test
Self-Perceived Burden Scale
Texas Revised Inventory of Grief – Part II
University Health Network
Wish to Hasten Death
Will to Live Scale.
Carter v. Canada (Attorney General). Supreme Court Judgments 2015 SCC5. [Available from: https://scc-csc.lexum.com/scc-csc/scc-csc/en/item/14637/index.do . Accessed 16 July 2021.
Statutes of Canada. Chapter 3. An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying) Canada2016. [Available from: https://laws-lois.justice.gc.ca/eng/annualstatutes/2016_3/fulltext.html . Accessed 16 July 2021.
Bill C-7: An Act to amend the Criminal Code (medical assistance in dying). 2020. [Available from: https://www.justice.gc.ca/eng/csj-sjc/pl/charter-charte/c7.html ]. Accessed 16 July 2021.
Health Canada. Second Annual Report on Medical Assistance in Dying in Canada: 2020. Ottawa, ON; June 2021. [Available from: https://www.canada.ca/content/dam/hc-sc/documents/services/medical-assistance-dying/annual-report-2020/annual-report-2020-eng.pdf ]. Accessed 16 July 2021.
Health Canada. Fourth interim report on medical assistance in dying in Canada. In: Health Canada, editor. Ottawa: Health Canada; 2019. p. 1–12.
Rodin G, Shapiro GK, Wales J, Li M. Assisted dying in Canada: lessons from the first 3 years. In: Board RE, Bennet MI, Lewis P, Wagstaff J, Selby P, editors. End of life choices for cancer patients an international perspective. Oxford: EBN Health; 2020. p. 41–9.
Google Scholar
Canadian Cancer Society. Snapshot of incidence, mortality aand survival estimates by cancer type. Toronto: Canadian Cancer Society; 2020. [Available from: https://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/Canadian%20cancer%20statistics%20supplementary%20information/2020/2020_cancer-specific-stats.pdf?la=en ]. Accessed 16 July 2021.
Rodin G, Zimmermann C, Rydall A, Jones J, Shepherd FA, Moore M, et al. The desire for hastened death in patients with metastatic cancer. J Pain Symptom Manag. 2007;33(6):661–75. https://doi.org/10.1016/j.jpainsymman.2006.09.034 .
Monforte-Royo C, Villavicencio-Chávez C, Tomás-Sábado J, Balaguer A. The wish to hasten death: a review of clinical studies. Psychooncology. 2011;20(8):795–804. https://doi.org/10.1002/pon.1839 .
Article PubMed Google Scholar
Balaguer A, Monforte-Royo C, Porta-Sales J, Alonso-Babarro A, Altisent R, Aradilla-Herrero A, et al. An international consensus definition of the wish to hasten death and its related factors. PLoS One. 2016;11(1):e0146184. https://doi.org/10.1371/journal.pone.0146184 .
Latha KS, Bhat SM. Suicidal behaviour among terminally ill cancer patients in India. Indian J Psychiatry. 2005;47(2):79–83. https://doi.org/10.4103/0019-5545.55950 .
Article CAS PubMed PubMed Central Google Scholar
Nissim R, Gagliese L, Rodin G. The desire for hastened death in individuals with advanced cancer: a longitudinal qualitative study. Soc Sci Med. 2009;69(2):165–71. https://doi.org/10.1016/j.socscimed.2009.04.021 .
Wilson KG, Dalgleish TL, Chochinov HM, Chary S, Gagnon PR, Macmillan K, et al. Mental disorders and the desire for death in patients receiving palliative care for cancer. BMJ Support Palliat Care. 2016;6(2):170–7. https://doi.org/10.1136/bmjspcare-2013-000604 .
Chochinov H, Wilson K, Enns M, Mowchun N, Lander S, Levitt M, et al. Desire for death in the terminally ill. Am J Psychiatry. 1995;152(8):1185–91. https://doi.org/10.1176/ajp.152.8.1185 .
Mystakidou K, Parpa E, Katsouda E, Galanos A, Vlahos L. The role of physical and psychological symptoms in desire for death: a study of terminally. Psychooncology. 2006;15(4):355–60. https://doi.org/10.1002/pon.972 .
Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity in the terminally ill: a cross-sectional, cohort study. Lancet. 2002;360(9350):2026–30. https://doi.org/10.1016/S0140-6736(02)12022-8 .
Kremeike K, Galushko M, Frerich G, Romotzky V, Hamacher S, Rodin G, et al. The DEsire to DIe in palliative care: optimization of management (DEDIPOM) - a study protocol. BMC Palliat Care. 2018;17(1):30. https://doi.org/10.1186/s12904-018-0279-3 .
Freeman S, Smith TF, Neufeld E, Fisher K, Ebihara S. The wish to die among palliative home care clients in Ontario, Canada: a cross-sectional study. BMC Palliat Care. 2016;15:24.
Article PubMed PubMed Central Google Scholar
Güell E, Ramos A, Zertuche T, Pascual A. Verbalized desire for death or euthanasia in advanced cancer patients receiving palliative care. Palliat Support Care. 2015;13(2):295–303. https://doi.org/10.1017/S1478951514000121 .
Hendry M, Pasterfield D, Lewis R, Carter B, Hodgson D, Wilkinson C. Why do we want the right to die? A systematic review of the international literature on the views of patients, carers and the public on assisted dying. Palliat Med. 2013;27(1):13–26. https://doi.org/10.1177/0269216312463623 .
Pacheco J, Hershberger PJ, Markert RJ, Kumar G. A longitudinal study of attitudes toward physician-assisted suicide and euthanasia among patients with noncurable malignancy. Am J Hosp Palliat Care. 2003;20(2):99–104. https://doi.org/10.1177/104990910302000207 .
Levene I, Parker M. Prevalence of depression in granted and refused requests for euthanasia and assisted suicide: a systematic review. J Med Ethics. 2011;37(4):205–11. https://doi.org/10.1136/jme.2010.039057 .
Hudson PL, Kristjanson LJ, Ashby M, Kelly B, Schofield P, Hudson R, et al. Desire for hastened death in patients with advanced disease and the evidence base of clinical guidelines: a systematic review. Palliat Med. 2006;20(7):693–701. https://doi.org/10.1177/0269216306071799 .
Johansen S, Hølen JC, Kaasa S, Loge JH, Materstvedt LJ. Attitudes towards, and wishes for, euthanasia in advanced cancer patients at a palliative medicine unit. Palliat Med. 2005;19(6):454–60. https://doi.org/10.1191/0269216305pm1048oa .
Rosenfeld B, Pessin H, Marziliano A, Jacobson C, Sorger B, Abbey J, et al. Does desire for hastened death change in terminally ill cancer patients? Soc Sci Med. 2014;111:35–40. https://doi.org/10.1016/j.socscimed.2014.03.027 .
Emanuel EJ, Fairclough DL, Emanuel LL. Attitudes and desires related to euthanasia and physician-assisted suicide among terminally ill patients and their caregivers. JAMA. 2000;284(19):2460–8. https://doi.org/10.1001/jama.284.19.2460 .
Article CAS PubMed Google Scholar
Ohnsorge K, Gudat H, Rehmann-Sutter C. What a wish to die can mean: reasons, meanings and functions of wishes to die, reported from 30 qualitative case studies of terminally ill cancer patients in palliative care. BMC Palliat Care. 2014;13(1):38. https://doi.org/10.1186/1472-684X-13-38 .
Monforte-Royo C, Villavicencio-Chávez C, Tomás-Sábado J, Mahtani-Chugani V, Balaguer A. What lies behind the wish to hasten death? A systematic review and meta-ethnography from the perspective of patients. PLoS One. 2012;7(5):e37117. https://doi.org/10.1371/journal.pone.0037117 .
Filiberti A, Ripamonti C, Totis A, Ventafridda V, De Conno F, Contiero P, et al. Characteristics of terminal cancer patients who committed suicide during a home palliative care program. J Pain Symptom Manag. 2001;22(1):544–53. https://doi.org/10.1016/S0885-3924(01)00295-0 .
Article CAS Google Scholar
Smith KA, Harvath TA, Goy ER, Ganzini L. Predictors of pursuit of physician-assisted death. J Pain Symptom Manag. 2015;49(3):555–61. https://doi.org/10.1016/j.jpainsymman.2014.06.010 .
Article Google Scholar
Rosenfeld B, Breitbart W, Stein K, Funesti-Esch J, Kaim M, Krivo S, et al. Measuring desire for death among patients with HIV/AIDS: the schedule of attitudes toward hastened death. Am J Psychiatry. 1999;156(1):94–100. https://doi.org/10.1176/ajp.156.1.94 .
Rodin G, Lo C, Mikulincer M, Donner A, Gagliese L, Zimmermann C. Pathways to distress: the multiple determinants of depression, hopelessness, and the desire for hastened death in metastatic cancer patients. Soc Sci Med. 2009;68(3):562–9. https://doi.org/10.1016/j.socscimed.2008.10.037 .
Rodin G, Lo C, Rydall A, Shnall J, Malfitano C, Chiu A, et al. Managing Cancer and living meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J Clin Oncol. 2018;36(23):2422–32. https://doi.org/10.1200/JCO.2017.77.1097 .
Tan A, Zimmermann C, Rodin G. Interpersonal processes in palliative care: an attachment perspective on the patient-clinician relationship. Palliat Med. 2005;19(2):143–50. https://doi.org/10.1191/0269216305pm994oa .
Lo C, Lin J, Gagliese L, Zimmermann C, Mikulincer M, Rodin G. Age and depression in patients with metastatic cancer: the protective effects of attachment security and spiritual well-being. Ageing Soc. 2010;30(2):325–36. https://doi.org/10.1017/S0144686X09990201 .
Hillen MA, de Haes HC, Stalpers LJ, Klinkenbijl JH, Eddes EH, Verdam MG, et al. How attachment style and locus of control influence patients' trust in their oncologist. J Psychosom Res. 2014;76(3):221–6. https://doi.org/10.1016/j.jpsychores.2013.11.014 .
Oldham RL, Dobscha SK, Goy ER, Ganzini L. Attachment styles of Oregonians who request physician-assisted death. Palliat Support Care. 2011;9(2):123–8. https://doi.org/10.1017/S1478951510000660 .
Emanuel EJ, Onwuteaka-Philipsen BD, Urwin JW, Cohen J. Attitudes and practices of euthanasia and physician-assisted suicide in the United States, Canada, and Europe. JAMA. 2016;316(1):79–90. https://doi.org/10.1001/jama.2016.8499 .
Blanke C, LeBlanc M, Hershman D, Ellis L, Meyskens F. Characterizing 18 years of the death with dignity act in Oregon. JAMA Oncol. 2017;3(10):1403–6. https://doi.org/10.1001/jamaoncol.2017.0243 .
Danyliv A, O’Neill C. Attitudes towards legalising physician provided euthanasia in Britain: the role of religion over time. Soc Sci Med. 2015;128:52–6. https://doi.org/10.1016/j.socscimed.2014.12.030 .
Moulton BE, Hill TD, Burdette A. Religion and trends in euthanasia attitudes among U.S. adults, 1977–2004. Sociol Forum. 2006;21(2):249–72. https://doi.org/10.1007/s11206-006-9015-5 .
Li M, Watt S, Escaf M, Gardam M, Heesters A, O'Leary G, et al. Medical assistance in dying - implementing a hospital-based program in Canada. N Engl J Med. 2017;376(21):2082–8. https://doi.org/10.1056/NEJMms1700606 .
Downar J, Fowler RA, Halko R, Huyer LD, Hill AD, Gibson JL. Early experience with medical assistance in dying in Ontario, Canada: a cohort study. CMAJ. 2020;192(8):E173–E81. https://doi.org/10.1503/cmaj.200016 .
Gamondi C, Fusi-Schmidhauser T, Oriani A, Payne S, Preston N. Family members' experiences of assisted dying: a systematic literature review with thematic synthesis. Palliat Med. 2019;33(8):1091–105. https://doi.org/10.1177/0269216319857630 .
Hales BM, Bean S, Isenberg-Grzeda E, Ford B, Selby D. Improving the medical assistance in dying (MAID) process: a qualitative study of family caregiver perspectives. Palliat Support Care. 2019;17(5):590–5. https://doi.org/10.1017/S147895151900004X .
Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. The hidden morbidity in cancer: spouse caregivers. J Clin Oncol. 2007;25(30):4829–34. https://doi.org/10.1200/JCO.2006.10.0909 .
Girgis A, Lambert SD, McElduff P, Bonevski B, Lecathelinais C, Boyes A, et al. Some things change, some things stay the same: a longitudinal analysis of cancer caregivers' unmet supportive care needs. Psychooncology. 2013;22(7):1557–64. https://doi.org/10.1002/pon.3166 .
Sklenarova H, Krümpelmann A, Haun MW, Friederich HC, Huber J, Thomas M, et al. When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer. 2015;121(9):1513–9. https://doi.org/10.1002/cncr.29223 .
Wang T, Molassiotis A, Chung BP, Tan JY. Unmet care needs of advanced cancer patients and their informal caregivers: a systematic review. BMC Palliat Care. 2018;17(1):96. https://doi.org/10.1186/s12904-018-0346-9 .
Goldberg R, Nissim R, An E, Hales S. Impact of medical assistance in dying (MAiD) on family caregivers. BMJ Support Palliat Care. 2021;11(1):107-14. https://doi.org/10.1136/bmjspcare-2018-001686 .
Norman G, Streiner D. Biostatistics: The bare essentials. 3rd Edition. Shelton, Connecticut: People's Medical Publishing House; 2008.
Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–9. https://doi.org/10.1176/ajp.140.6.734 .
Karnofsky DA, Burchenal JH. The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM, editor. Evaluation of chemotherapeutic agents. New York: Columbia University Press; 1949. p. 191–205.
Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol. 1984;2(3):187–93. https://doi.org/10.1200/JCO.1984.2.3.187 .
Lo C, Burman D, Swami N, Gagliese L, Rodin G, Zimmermann C. Validation of the QUAL-EC for assessing quality of life in patients with advanced cancer. Eur J Cancer. 2011;47(4):554–60. https://doi.org/10.1016/j.ejca.2010.10.027 .
Grünke B, Philipp R, Vehling S, Scheffold K, Härter M, Oechsle K. Ea. measuring the psychosocial dimensions of quality of life in patients with advanced cancer: psychometrics of the German quality of life at the end of life-Cancer-psychosocial questionnaire. J Pain Symptom Manag. 2018;55(3):985–91. https://doi.org/10.1016/j.jpainsymman.2017.11.006 .
Carmel S. The will-to-live scale: development, validation, and significance for elderly people. Aging Ment Health. 2017;21(3):289–96. https://doi.org/10.1080/13607863.2015.1081149 .
Kolva E, Rosenfeld B, Liu Y, Pessin H, Breitbart W. Using item response theory (IRT) to reduce patient burden when assessing desire for hastened death. Psychol Assess. 2017;29(3):349–53. https://doi.org/10.1037/pas0000343 .
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x .
Watanabe SM, Nekolaichuk C, Beaumont C, Johnson L, Myers J, Strasser F. A multi-Centre comparison of two numerical versions of the Edmonton symptom assessment system in palliative care patients. J Pain Symptom Manag. 2011;41(2):456–68. https://doi.org/10.1016/j.jpainsymman.2010.04.020 .
Hannon B, Dyck M, Pope A, Swami N, Banerjee S, Mak E, et al. Modified Edmonton symptom assessment system including constipation and sleep: validation in outpatients with cancer. J Pain Symptom Manag. 2015;49(5):945–52. https://doi.org/10.1016/j.jpainsymman.2014.10.013 .
Hui D, Bruera E. The Edmonton symptom assessment system 25 years later: past, present and future developments. J Pain Symptom Manag. 2017;53(3):630–43. https://doi.org/10.1016/j.jpainsymman.2016.10.370 .
Lo C, Burman D, Rodin G, Zimmerman C. Measuring patient satisfaction in oncology palliative care: psychometric properties of the FAMCARE-patient scale. Qual Life Res. 2009;18(6):747–52. https://doi.org/10.1007/s11136-009-9494-y .
Rosenberg M. Society and the adolescent self-image. Middletown: Wesleyan University Press; 1989.
Lo C, Hales S, Zimmermann C, Gagliese L, Rydall A, Rodin G. Measuring death-related anxiety in advanced cancer: preliminary psychometrics of the death and dying distress scale. J Pediatr Hematol Oncol. 2011;33(Supplement 2):S140–5. https://doi.org/10.1097/MPH.0b013e318230e1fd .
Krause S, Rydall A, Hales S, Rodin G, Lo C. Initial validation of the death and dying distress scale for the assessment of death anxiety in patients with advanced cancer. J Pain Symptom Manag. 2015;49(1):126–34. https://doi.org/10.1016/j.jpainsymman.2014.04.012 .
Shapiro GK, Mah K, Li M, Zimmerman C, Hales S, Rodin G. Validation of the Death and Dying Distress Scale in Patients with Advanced Cancer Psychooncology. 2020.
Reeve BB, Thissen DM, Bann CM, Mack N, Treiman K, Sanoff HK, et al. Psychometric evaluation and design of patient-centered communication measures for cancer care settings. Patient Educ Couns. 2017;100(7):1322–8. https://doi.org/10.1016/j.pec.2017.02.011 .
Kristjanson L. Validation and reliability testing of the FAMCARE scale: measuring family satisfaction with advanced cancer care. Soc Sci Med. 1993;36(5):693–701. https://doi.org/10.1016/0277-9536(93)90066-D .
Robinson S, Kissane DW, Brooker J, Hempton C, Michael N, Fischer J, et al. Refinement and revalidation of the demoralization scale: the DS-II - external validity. Cancer. 2016;122(14):2260–7. https://doi.org/10.1002/cncr.30012 .
Simmons LA. Self-perceived burden in cancer patients: validation of the self-perceived burden scale. Cancer Nurs. 2007;30(5):405–11. https://doi.org/10.1097/01.NCC.0000290816.37442.af .
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of Cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–9. https://doi.org/10.1200/JCO.1993.11.3.570 .
Salsman JM, Garcia SF, Yanez B, Sanford SD, Snyder MA, Victorson D. Physical, emotional, and social health differences between posttreatment young adults with cancer and matched healthy controls. Cancer. 2014;120(15):2247–54. https://doi.org/10.1002/cncr.28739 . Accessed 16 July 2021.
Fowers BJ, Olson DH. ENRICH marital satisfaction scale: a brief research and clinical tool. J Fam Psychol. 1993;7(2):176–85. https://doi.org/10.1037/0893-3200.7.2.176 .
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. https://doi.org/10.1016/0277-9536(91)90150-B .
Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified medical outcomes study social support survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–16. https://doi.org/10.1016/j.jclinepi.2012.04.007 .
Koenig HG, Büssing A. The Duke University religion index (DUREL): a five-item measure for use in epidemiological studies. Religions. 2010;1(1):78–85. https://doi.org/10.3390/rel1010078 .
Kunce LJ, Shaver PR. An attachment-theoretical approach to caregiving in romantic relationships. In: Bartholomew K, Perlman D, editors. Attachment processes in adulthood, vol 5. Advances in personal relationships. London: Jessica Kingsley Publishers; 1994. p. 205–37.
Robinson S, Kissane DW, Brooker J, Michael N, Fischer J, Franco M, et al. Refinement and revalidation of the demoralization scale: the DS-II - internal validty. Cancer. 2016;122(14):2251–9. https://doi.org/10.1002/cncr.30015 .
Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992;15(4):271–83. https://doi.org/10.1002/nur.4770150406 .
Li M, Macedo A, Crawford S, Bagha S, Leung YW, Zimmermann C, et al. Easier said than done: keys to successful implementation of the distress assessment and response tool (DART) program. J Oncol Pract. 2016;12(5):e513–26. https://doi.org/10.1200/JOP.2015.010066 .
McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–63. https://doi.org/10.1097/00005650-199303000-00006 .
Faschingbaur T, Zisook S, DeVaul R. The Texas revised inventory of grief. In: Zisook S, editor. Biopsychosocial aspects of bereavement. Washington: American Psychiatric Press, Inc.; 1987. p. 109–24.
Ringdal GI, Jordhoy MS, Ringdal K, Kaasa S. Factors affecting grief reactions in close family members to individuals who have died of cancer. J Pain Symptom Manag. 2001;22(6):1016–26. https://doi.org/10.1016/S0885-3924(01)00363-3 .
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–98. https://doi.org/10.1002/jts.22059 .
Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL- 5) in veterans. Psychol Assess. 2016;28(11):1379–91. https://doi.org/10.1037/pas0000254 .
Patrick DL, Engelberg RA, Curtis JR. Evaluating the quality of dying and death. J Pain Symptom Manag. 2001;22(3):717–26. https://doi.org/10.1016/S0885-3924(01)00333-5 .
Hales S, Zimmermann C, Rodin G. The quality of dying and death: a systematic review of measures. Palliat Med. 2010;24(2):127–44. https://doi.org/10.1177/0269216309351783 .
Lo C, Walsh A, Mikulincer M, Gagliese L, Zimmermann C, Rodin G. Measuring attachment security in patients with advanced cancer: psychometric properties of a modified and brief experiences in close relationships scale. Psychooncology. 2009;18(5):490–9. https://doi.org/10.1002/pon.1417 .
Strauss A, Corbin J. Basics of qualitative research. London: Sage; 1990.
Patton M. Qualitative evaluation and research methods. Newbury Park: Sage; 1990.
Lo C, Zimmermann C, Rydall A, Walsh A, Jones JM, Moore MJ, et al. Longitudinal study of depressive symptoms in patients with metastatic gastrointestinal and lung cancer. J Clin Oncol. 2010;28(18):3084–9. https://doi.org/10.1200/JCO.2009.26.9712 .
Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer; 2000.
Rennie D, Nissim R. The grounded theory method and humanistic psychology. In: Schneider K, Pierson J, Bugental J, editors. The handbook of humanistic psychology: leading edges in theory, practice, and research. 2nd ed. Thousand Oaks: Sage; 2015. p. 297–308.
Download references
Acknowledgements
We would like to thank Cassandra Graham for her input on the grant submission.
This study is funded by a competitive, peer-reviewed project grant awarded to ML and GR, co-principal investigators, from the Canadian Institutes of Health Research, Canada’s federal funding agency for health research (Grant No: CIHR PJT 401506; https://cihr-irsc.gc.ca ). An earlier version of our manuscript protocol underwent peer review by the funding body. GKS is supported by the Edith Kirchmann Postdoctoral Fellowship at PM, and by a CIHR 2019 Fellowship Award (CIHR MFE 171271). The funders of the study played no role in the study design, data collection, data analysis, data interpretation, or writing of this report.
Author information
Madeline Li and Gilla K. Shapiro are co-first authors.
Authors and Affiliations
Department of Supportive Care, Princess Margaret Cancer Centre, University Health Network, 620 University Avenue, 12th Floor, Toronto, Ontario, M5G 2C1, Canada
Madeline Li, Gilla K. Shapiro, Roberta Klein, Anne Barbeau, Anne Rydall, Jennifer A. H. Bell, Rinat Nissim, Sarah Hales, Camilla Zimmermann, Rebecca K. S. Wong & Gary Rodin
Department of Psychiatry, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada
Madeline Li, Jennifer A. H. Bell, Rinat Nissim, Sarah Hales, Camilla Zimmermann & Gary Rodin
Global Institute of Psychosocial, Palliative and End-of-Life Care (GIPPEC), University of Toronto and Princess Margaret Cancer Centre, Toronto, Ontario, Canada
Gilla K. Shapiro, Sarah Hales, Camilla Zimmermann & Gary Rodin
Joint Centre for Bioethics, University of Toronto, Toronto, Ontario, Canada
Jennifer A. H. Bell
Department of Medicine, University of Toronto, Toronto, Ontario, Canada
Camilla Zimmermann
Department of Radiation Oncology, University of Toronto, Toronto, Ontario, Canada
Rebecca K. S. Wong
You can also search for this author in PubMed Google Scholar
Contributions
ML and GKS are co-first authors of this work. ML, GKS, AB, RK, AR, and GR made substantial contributions to the study design and writing of the manuscript. ML, GKS, RK, AB, AR, JAHB, RN, SH, CZ, RKSW and GR substantively revised the manuscript, read and approved the final submitted version, and guarantee the integrity of this work.
Corresponding authors
Correspondence to Madeline Li or Gilla K. Shapiro .
Ethics declarations
Ethics approval and consent to participate.
This study was approved on September 2, 2020 by the University Health Network Research Ethics Board (UHN REB #18–6182). All participants will provide written informed consent. Data collection is expected to begin by January 2021.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Li, M., Shapiro, G.K., Klein, R. et al. Medical Assistance in Dying in patients with advanced cancer and their caregivers: a mixed methods longitudinal study protocol. BMC Palliat Care 20 , 117 (2021). https://doi.org/10.1186/s12904-021-00793-4
Download citation
Received : 26 November 2020
Accepted : 09 June 2021
Published : 21 July 2021
DOI : https://doi.org/10.1186/s12904-021-00793-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Desire for hastened death
- Medical assistance in dying
- Medical communication
- Palliative care
- Assisted dying
- Will to live
BMC Palliative Care
ISSN: 1472-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Paradoxes, nurses' roles and Medical Assistance in Dying: A grounded theory
Affiliation.
- 1 14847University of Québec in Trois-Rivières, Trois-Rivières, QC, Canada.
- PMID: 35758866
- PMCID: PMC9667088
- DOI: 10.1177/09697330221109941
Background: In June 2016, the Parliament of Canada passed federal legislation allowing eligible adults to request Medical Assistance in Dying (MAID). Since its implementation, there likely exists a degree of hesitancy among some healthcare providers due to the law being inconsistent with personal beliefs and values. It is imperative to explore how nurses in Quebec experience the shift from accompanying palliative clients through "a natural death" to participating in "a premeditated death."
Research question/aim/objectives: This study aims to explore how Quebec nurses personally and professionally face the new practice of MAID and their role evolution.
Research design: A grounded theory design was used.
Participants and research context: We recruited 37 nurses who participated in or coordinated at least one MAID. Semi-structured interviews and focus groups were conducted and audiotaped. Data collection and analysis followed Strauss and Corbin steps.
Ethical considerations: Ethics approval was received from the investigator's affiliated University. Participants were informed regarding the research goal, signed a written consent, and were assigned pseudonyms.
Findings/results: Results show that nurses experienced the wide range of paradoxe during MAID centering around the following eight elements: 1) confrontation abouth death, 2) choice, 3) time of death, 4) emotional load, 5) new Bill, 6) relationship with the person, 7) communication skills, and 8) healthcare setting. The shifting of views and values in this new role is presented by the contradiction of opposites.
Conclusions: A better understanding of the paradox experienced by nurses involved with MAID paves the way for the development of interventions.
Keywords: Medical assistance in dying; end of life; ethics; grounded theory; nurse role; paradoxes.
- Grounded Theory
- Medical Assistance
- Nurse's Role
- Palliative Care
- Suicide, Assisted*
- Share full article
Advertisement
Supported by
Doctor-Assisted Death Is Legal in 10 States. Could New York Be No. 11?
Activists have renewed attention on legislation related to the emotional issue of so-called medical aid in dying that has long languished in Albany.

By Erin Nolan and Grace Ashford
Reporting from the State Capitol in Albany, N.Y.
The sounds of protest came forcefully from the Assembly chamber gallery, the chants echoing the words emblazoned on handmade banners that were held aloft: “Stop the suffering, pass the bill!”
But as New York State troopers began to remove some of the protesters — some holding canes, others slowed by the effects of cancer treatment — it was clear that this demonstration held personal and immediate resonance to those participating.
The protest was the latest in an increasingly desperate series of demonstrations aimed at persuading state legislators to pass a bill that would legalize so-called medical aid in dying , allowing terminally ill people access to life-ending medication for the first time in the state.
New York is one of 19 states where lawmakers are considering bills that would legalize medical aid in dying, a practice that is legal in 10 states and Washington, D.C.
The bill in New York would allow mentally competent, terminally ill adults with no more than six months to live to request prescriptions from their doctors for life-ending medication. The patients would have to be able to ingest the medication on their own, and only the person seeking to die could request the prescription.
“I’m not someone who enjoys conflict or who has much experience in civil disobedience,” said Jules Netherland, a protester who was detained in the Capitol. “But I really believed this was the only way to get people’s attention.”
Roughly a decade has passed since the first medical aid in dying bill was introduced in Albany, and it has yet to reach the floor for a vote.
But the proposal has gained momentum this year, because of endorsements from groups like the Medical Society of the State of New York, a trade group of roughly 20,000 doctors, and the efforts of activists like Dr. Netherland, who has a Ph.D. in medical sociology and was diagnosed with Stage 4 breast cancer last year.
Opponents worry that some patients might choose to end their lives based on an inaccurate prognosis or after being pressured to do so. And while the current bill is restricted to terminally ill people, they worry that lawmakers could expand eligibility for medical aid in dying after any initial legislation is passed.
“Even if there is just one case of abuse or coercion, or even if there is just one mistake, that is a dead person,” said Colleen Barry, a nurse and board member of Euthanasia Prevention Coalition USA.
With roughly a week left in the 2024 legislative session, the bill faces an uphill climb in the Legislature, which Democrats control, especially without the official support of Gov. Kathy Hochul or the leaders of the Assembly and Senate.
Still, Assemblywoman Amy Paulin, the chairwoman of the body’s Health Committee, said that it had gradually garnered support since she first sponsored it in 2016.
“It’s an emotional vote,” not unlike those on abortion or marriage equality, said Ms. Paulin, who represents parts of Westchester County and is motivated by the memory of her sister, who could not get such aid when she was dying of ovarian cancer. “A lot of my colleagues have come to me with stories that drove them to change their minds. It’s about life, and it’s about choice. More members are feeling that and living that and understanding that.”
But it is precisely the emotional gravity of the issue that has some in leadership hesitating, according to numerous lawmakers.
“I just think that, as a culture, in terms of the country, there has not been a lot of conversation about dying,” the State Senate majority leader, Andrea Stewart-Cousins, said of the proposal earlier this year, adding that she was not opposed to having that conversation.
Opponents, including the Center for Disability Rights and the New York State Catholic Conference , warn that even this narrow application of aid in dying will invariably lead to broader use. They point to places, mostly outside the United States, where the practice is available not only to patients struggling with terminal physical illnesses, but also to those with mental illnesses as well.
The vast majority of people who have availed themselves of such laws in the United States were facing terminal physical illnesses — most commonly cancer. But rare exceptions, like a 36-year-old Colorado woman who was prescribed life-ending medication after a diagnosis of “terminal anorexia nervosa,” have sparked controversy and raised questions about suffering, autonomy and the role and responsibilities of physicians.
The American Medical Association is formally opposed to physician-assisted suicide, which it describes as “ fundamentally incompatible with the physician’s role as healer. ” For many years, the Medical Society of the State of New York agreed.
But recent conversations around the legislation — which not only restricts the practice to terminally ill people but also allows individual providers to opt out based on their own convictions — caused the group to reverse course and endorse the measure .
Supporters of the practice say that legalizing medical aid in dying would help untold numbers of people avoid suffering and die peacefully. They point to polls like one commissioned earlier this year by YouGov that found 72 percent of New Yorkers supported “death with dignity.”
Between 1994, when Oregon became the first state to legalize the practice, and 2020, 8,451 people received prescriptions under medical aid in dying laws. Of those, 5,329 took the life-ending medication, according to a 2022 study published in the Journal of the American Geriatrics Society .
Barbara Thomas, 87, fought tears as she tried to imagine a reality where that would have been an option for her husband, Bob Thomas, who died 15 months after he was diagnosed with glioblastoma multiforme — a type of terminal brain cancer — in the fall of 2010.
“I think it would have been much more loving. We could have all gathered,” she said, pausing to blink back tears. “He would have, I’m sure, preferred to be able to have everyone around so he could speak to them all, give them his wishes for their lives and hear them say what they liked about him.”
Instead, Mr. Thomas, a proud outdoorsman who enjoyed fly fishing, hunting, camping and hiking, spent most of his final months in his bed at home in West Milton, N.Y., tired and frail, Ms. Thomas said.
“Sometimes we would just lay in the bed and cry about what an impossible situation we were in,” she recalled.
Twice, Mr. Thomas asked his wife to bring him his gun and help him kill himself, Ms. Thomas said. She never did it, but it pained her to see how miserable he was and to know there was nothing she could do to alleviate his suffering.
“He was the person I had lived with longer than any other person — longer than my parents, longer than any of my children,” Ms. Thomas said, adding that they had been married for 55 years. “We were still in love.”
To her, allowing people like her husband to choose when and how they die is “the compassionate, loving thing to do.”
Erin Nolan is a reporter covering New York City and the metropolitan region. She is a member of the 2023-24 Times Fellowship class. Email her at [email protected] . More about Erin Nolan
Grace Ashford covers New York government and politics for The Times. More about Grace Ashford
Politics in the New York Region
Congestion Pricing: Gov. Kathy Hochul announced that she was shelving the long-awaited plan to implement congestion pricing , citing economic concerns, just weeks before it was to go into effect.
Doctor-Assisted Death: Legislation related to the emotional issue of so-called medical aid in dying has long languished in Albany. But a new push to legalize the practice has gained momentum .
Plastic Waste: As plastic continues to fill landfills and oceans, New York lawmakers are considering a proposal to limit single-use plastic products. Here’s what to know about the legislation .
A Quiet Suspension: A little-known New York State fund that paid the medical expenses of children who suffered neurological injuries as a result of medical malpractice during childbirth has been suspended .
Limiting Donations to Israel: Representative Alexandria Ocasio-Cortez, who rarely wades into state politics, publicly backed a bill that could strip New York nonprofits of their tax-exempt status if their funds are used to support Israel’s military or settlements.
Transgender Student-Athlete Rules: A parent group in New York City asked for a review of rules that let students play on sports teams that align with their gender identity. Democratic officials responded angrily .
With Calgary woman starving herself to death, court of appeal scrambling to expedite MAID case
Judge's order prevents 27-year-old woman from accessing maid.

Social Sharing
Lawyers and judges are scrambling to expedite the case of a Calgary woman who was approved for medical assistance in dying (MAID) but is, instead, starving herself to death.
The 27-year-old woman, who can only be identified as M.V. because of a publication ban, was set to receive MAID in February but her father, known as W.V., has been fighting in court to prevent that from happening.
Earlier this year, W.V. got a temporary injunction, blocking his daughter's MAID access. Although a Court of King's Bench judge ultimately sided with his daughter, a judicial stay of that decision is in place so that W.V. can appeal.
The stay prevents M.V. from accessing MAID until the case is heard by the Alberta Court of Appeal in October. But, according to an application filed in court on Tuesday, M.V. stopped eating and drinking on May 28.
Death: not 'if' but 'how'
In an affidavit filed in support of that application, M.V. says she "would greatly prefer to receive MAID to reduce [her] suffering."
M.V., whose only publicly known diagnoses are autism and ADHD, has never disclosed in court the conditions she suffers from that led to her approval and her father does not believe she qualifies for MAID.
- Calgary woman whose MAID access currently blocked by courts now starving herself to death
Lawyers and Court of Appeal Justice Jolaine Antonio gathered on video conference Wednesday morning to figure out next steps.
"Unfortunately this is not a situation where the question is 'Will this occur?' it's 'How will this occur?'" said M.V.'s lawyer Evan Jovanovic, speaking about his client's death.
'Expediting the appeal'
Antonio says the law doesn't allow her to do what M.V.'s lawyers have asked for and instead requested the parties consider an expedited appeal to be heard by a panel of judges in the last week of June.
"Our office would certainly move heaven and earth to be able to get this heard as quickly as possible," said Jovanovic.
"However, we cannot give any guarantees as to what our client's position would be … the decision would ultimately be hers as to how she would react to that and to what steps she would take."
Calgary judge rules 27-year-old can go ahead with MAID death despite father's concerns
Antonio directed Jovanovic and co-counsel Austin Paladeau to make contact with M.V.: "not that I'm looking for her permission, just her position on expediting the appeal," said the judge.
"I can't intrude on your relationship with her," said Antonio.
"If there is any aspect of this that involves questions larger than herself it would merit getting into a hearing before obviating any need for a hearing."
'Change to suffering 'self-inflicted'
Although she agreed to "adjust accordingly," W.V.'s lawyer Sarah Miller expressed frustration that M.V. not only consented to the stay, she was also offered a date of June 10 for appeal arguments but chose the Oct. 7 date.
"The only current change to her suffering is self-inflicted and there's nothing that this court can do to stop her from choosing a modality of suicide independent of MAID," said Miller.
"If she so chooses to commit suicide, that is her prerogative, but it is not for the court to get involved to assist her in that or to rubber stamp that process."
Father asks court to stop 27-year-old daughter's MAID death, review doctors' sign-off
Antonio gave M.V.'s lawyers until the end of day Wednesday to get back to her with their client's position.
If the appeal is heard in three weeks, lawyers will have to move at "blinding speed" with "draconian" filing deadlines, Antonio acknowledged.
"Everyone here, the court included, wishes good outcomes for [M.V.]," said the judge.
"We are having this conversation in order to find a way to do what is best. I hope that she will join us through her actions in that dialogue."
ABOUT THE AUTHOR

CBC Calgary crime reporter
Meghan Grant is a justice affairs reporter. She has been covering courts, crime and stories of police accountability in southern Alberta for more than a decade. Send Meghan a story tip at [email protected] or follow her on Twitter.
- Follow her on Twitter
Related Stories
- Top stories from CBC Calgary
- Trial to begin Thursday in murder-conspiracy case tied to Coutts border blockade
- RCMP probe of livestock slaughter operations leads to charges

Autistic Calgary woman seeking Medical Assistance in Dying has begun starving herself to death
The autistic Calgary woman whose access to Medical Assistance in Dying was blocked is now starving herself to death and a stay preventing her from utilizing MAiD should be lifted, her lawyer says.
In an application filed Tuesday at the Alberta Court of Appeal, lawyer Austin Paladeau is seeking an order overturning a consented stay of a lower court ruling pending appeal.
Paladeau’s client, identified only as M.V., agreed to the stay on April 8, pending an appeal by counsel for her father of a Court of King’s Bench ruling saying she was entitled to assisted suicide.
“The consent order was entered into on the basis that the appeal of Justice (Colin) Feasby’s decision setting aside the injunction preventing any person providing M.V. with medical assistance in dying would be resolved following the (appeal) hearing,” Paladeau’s application says.
“The material change in circumstance is that M.V. has commenced voluntary stoppage of eating and drinking (VSED),” it says.
“Her death is now imminent and the question is whether she will pass away from VSED or have access to MAiD.”
In a document in support of his application, Paladeau says the Calgary woman has not been eating or drinking since May 28.
The supporting document says the new development means there has been a change in the test for determining whether an injunction can continue.
“This has shifted the balance of harms analysis,” it says.
“It is no longer a question of whether M.V. will be able to end her life by accessing MAiD; it is now a question of whether M.V. will die a drawn-out death by VSED or a painless death by MAiD.”
The document says “even if M.V. concedes every other issue on appeal … the immediate, intolerable suffering of VSED means that the stay should be lifted.”
- Advocacy groups can intervene in appeal involving autistic Calgary woman seeking Medical Assistance in Dying
- Father appeals ruling that allows woman with autism to seek Medical Assistance in Dying
On March 25, Feasby ruled a temporary injunction blocking the woman’s access to MAiD had to be lifted, paving the way for her to seek the life-ending medical procedure. Feasby stayed his ruling for 30 days to allow the father an opportunity to appeal.
The daughter had originally scheduled a medical procedure to end her life on Feb. 1, but the original injunction blocked that from happening. The father’s lawyers, Sarah Miller and Emily Amirkhani appealed Feasby’s ruling and both sides agreed on April 8, to have the decision further stayed pending the appeal decision.
But Paladeau’s court documents say with M.V.’s death now imminent and the hearing, scheduled for Oct. 7, is now moot.
In his ruling Feasby said as heartbreaking as it was for the father to see his daughter’s life ended, the injunction preventing her from ending her life was causing her irreparable harm.
“An injunction would deny M.V. the right to choose between living or dying with dignity. Further, an injunction would put M.V. in a position where she would be forced to choose between living a life she has decided is intolerable and ending her life with medical assistance.
“This is a terrible choice and should not be forced on M.V., as attempting to end her life without medical assistance would put her at increased risk of pain, suffering and lasting injury.”
X: @KMartinCourts


IMAGES
VIDEO
COMMENTS
death and dying. I did this by first understanding the medico-legal institutional discourse on medical assistance in dying through Canadian legislation. 1.2 Medical Assistance in Dying: Canadian Legislation 1.2.1 Carter v. Canada [2015] The SCC declared on the 6th of February 2015 in Carter v. Canada [2015] that sections
Keywords: History, Medical assistance in dying, Philosophy of dying, Euthanasia, Suicide. In Athens, 399 BCE, the Greek philosopher Socrates - imprisoned and sentenced to death by hemlock on the charges of impiety and corrupting Athenian youth - famously raised a cup of the poison to his lips. [ 1] Descriptions of Socrates' equanimity at ...
In 2015, the Canadian Supreme Court declared that an absolute Criminal Code prohibition on assisted suicide and euthanasia was unconstitutional. In response, the Canadian parliament enacted Bill C-14 in 2016 permitting assisted suicide and euthanasia for the end-of-life context, which it termed "Medical Assistance in Dying" (MAiD).
Chapter 1: MAiD in the Canadian Context and Thesis Road Map Medical assistance in dying (MAiD) has been a hotly debated topic across much of the western world for several decades. With the passing of Bill C-14 in Canada on June 17, 2016, MAiD became legal. Medical assistance in dying can include voluntary euthanasia, where a
The practice variously known as "medically assisted dying," "medical aid in dying," "physician aid in dying," "physician-assisted suicide," "death with dignity," and "euthanasia" has long been contentious, and the question of what to call it has become increasingly contentious as well. 1 There has been a growing push, particularly among U.S. proponents of legalizing the ...
A thesis submitted in conformity with the requirements for the degree of Master of Laws Faculty of Law University of Toronto ... 2017 Abstract Canada's Medical Assistance in Dying (MAID) law continues to be a dividing issue. While it has been decided that only a few qualifying Canadians suffering from severe conditions may request
Code and to make related amendments to other Acts (medical assistance in dying), effectively legalizing medical assistance in dying (MAiD) within Canada. Canada is the first country to include Nurse Practitioners as assessors and providers of assisted dying, a role traditionally reserved only for physicians (Pesut et al., 2020).
Medical assistance in dying (MAiD) was legalised federally in Canada after the Supreme Court decision in Carter v Canada (Attorney General) [2015] 1 SCR 331. The federal legislative framework for MAiD was established via Bill C-14 in 2016. Caregivers and patients were central to Carter and subsequent litigation and advocacy, which resulted in ...
For example, a health care provider could be "unwilling or unable to support the provision of either the patient's usual care or care specific to Medical Assistance in Dying" (AHS, 2018, p. 8). The policies reviewed also addressed the rights and responsibilities of institutions to conscientiously object to assessing and/or providing MAID ...
Background Medical assistance in dying (MAiD) traverses challenging and emotionally overwhelming territories: healthcare providers (HCPs) across jurisdictions experience myriad of affective responses secondary to possible tensions between normative and interwoven values, such as sanctity of life, dignity in death and dying and duty to care. Objective To determine the emotional impact on HCPs ...
In a historic ruling on the 6th of February 2015, the Supreme Court of Canada declared that sections of the Criminal Code of Canada prohibiting medical assisted dying were no longer valid. Following the court's mandate, government laws and provincial policies were passed to facilitate the implementation of this ruling. Regulatory bodies implemented frameworks and policies on the healthcare ...
Medical Assistance in Dying (MAiD) was legalized in Canada in June, 2016. The Canadian government's decision to legislate assisted dying, an approach that requires a high degree of obligation, precision, and delegation, has resulted in unique challenges for health care and for nursing practice. The purpose of this study was to better understand the implications of a legislated approach to ...
Objective: To describe the positive aspects of medical assistance in dying legalization from the perspectives of hospice palliative care providers engaging in medical assistance in dying. Design: In this qualitative descriptive study, we conducted an inductive thematic analysis of semi-structured interviews with hospice palliative care providers.
The Canadian law permits both "clinician-administered medical assistance in dying" in which a physician or nurse practitioner "directly administers a substance that causes death" and "self-administered medical assistance in dying," in which a physician or nurse practitioner "provides or prescribes a drug that the eligible person ...
This thesis explores the Government of Canada's legislative response to the . Carter v. Canada (Attorney General) ruling. More specifically, this thesis analyzes the major issues that afflicted Bill C-14, or . An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying), as it
The legal criteria for medical assistance in dying (MAiD) for adults with a grievous and irremediable medical condition were established in Canada in 2016. There has been concern that potentially reversible states of depression or demoralization may contribute to the desire for death (DD) and requests for MAiD. However, little is known about the emergence of the DD in patients, its impact on ...
The term medical assistance in dying includes both physician-assisted suicide (a patient self-administers a prescribed lethal medication) and voluntary euthanasia (a medical practitioner administers a lethal medication), both of which are now legal in Canada. 3, 4 Patients must be competent to make medical decisions, must be 18 years of age or ...
The aim of this thesis is to reflect the role of care in response to requests for assistance to die. This thesis will seek to illustrate that it is fundamental that regulatory frameworks concerning assisted dying should attend to the reality of care. In the first chapter, this thesis will establish a care-based ethic which reflects assisted dying.
A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy ... Since the 2015 legalization of medical assistance in dying (MAiD), healthcare professionals across the interdisciplinary spectrum have been exploring their roles within this practice, and a
Medical Assistance in Dying (MAiD) can bring out positive and negative emotions in nurses. Nurses must feel comfortable with their role, be knowledgeable, and practice their skills according to the laws and regulations. Literature shows that education positively impacts nursing students' knowledge, beliefs, and comfort about MAiD.
medical assistance in dying (MAiD) if they lost decision-making capacity while awaiting MAiD. Little is known about healthcare providers' experiences of patients' loss of capacity to consent and subsequent ineligibility for MAiD. The enactment of Bill C-7 in 2021 has allowed eligible
Background: In June 2016, the Parliament of Canada passed federal legislation allowing eligible adults to request Medical Assistance in Dying (MAID). Since its implementation, there likely exists a degree of hesitancy among some healthcare providers due to the law being inconsistent with personal beliefs and values.
This is to certify that the thesis prepared By: Glenn Shewchuk Entitled: Medical Assistance in Dying: Exploring an Evangelical Approach to the Laws Surrounding MAID in Canada and an Application of Scripture to MAID and Suicide and submitted in partial fulfillment of the requirements for the degree of Master of Arts (Theology)
New York is one of 19 states where lawmakers are considering bills that would legalize medical aid in dying, a practice that is legal in 10 states and Washington, D.C. The bill in New York would ...
A Calgary woman whose access to medical assistance in dying (MAID) is currently blocked by the courts is starving herself to death and expects to die within a few weeks, according to court documents.
Physician aid in dying is a controversial subject raising issues central to the role of physicians. According to the American Medical Association, it occurs when a physician provides "the necessary means and/or information" to facilitate a patient's choice to end his or her life [].This essay's authors hold varying views on the ethics of aid in dying; thus, the essay explores the ...
Lawyers and judges are scrambling to expedite the case of a Calgary woman who was approved for medical assistance in dying (MAID) but is, instead, starving herself to death. The 27-year-old woman ...
The Calgary Court of King's Bench judge said he had to weigh the potential harm an injunction would cause the 27-year-old woman, who has autism, against the harm her parents would suffer if the ...
The autistic Calgary woman whose access to Medical Assistance in Dying was blocked is now starving herself to death and a stay preventing her from utilizing MAiD should be lifted, her lawyer says.
HARRISBURG — Attorney General Michelle Henry announced the parents of a newborn baby who died in Sullivan County in 2022 have pleaded guilty. The baby boy died two days after birth, and the parents and a third person were charged based upon failures to take reasonable action to summon medical assistance.