Online ordering is currently unavailable due to technical issues. We apologise for any delays responding to customers while we resolve this. For further updates please visit our website: https://www.cambridge.org/news-and-insights/technical-incident
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .

Login Alert

- > Journals
- > BJPsych Advances
- > Volume 24 Issue 2
- > How to carry out a literature search for a systematic...

Article contents
- LEARNING OBJECTIVES
- DECLARATION OF INTEREST
Defining the clinical question
Scoping search, search strategy, sources to search, developing a search strategy, searching electronic databases, supplementary search techniques, obtaining unpublished literature, conclusions, how to carry out a literature search for a systematic review: a practical guide.
Published online by Cambridge University Press: 01 March 2018
Performing an effective literature search to obtain the best available evidence is the basis of any evidence-based discipline, in particular evidence-based medicine. However, with a vast and growing volume of published research available, searching the literature can be challenging. Even when journals are indexed in electronic databases, it can be difficult to identify all relevant studies without an effective search strategy. It is also important to search unpublished literature to reduce publication bias, which occurs from a tendency for authors and journals to preferentially publish statistically significant studies. This article is intended for clinicians and researchers who are approaching the field of evidence synthesis and would like to perform a literature search. It aims to provide advice on how to develop the search protocol and the strategy to identify the most relevant evidence for a given research or clinical question. It will also focus on how to search not only the published but also the unpublished literature using a number of online resources.
• Understand the purpose of conducting a literature search and its integral part of the literature review process
• Become aware of the range of sources that are available, including electronic databases of published data and trial registries to identify unpublished data
• Understand how to develop a search strategy and apply appropriate search terms to interrogate electronic databases or trial registries
A literature search is distinguished from, but integral to, a literature review. Literature reviews are conducted for the purpose of (a) locating information on a topic or identifying gaps in the literature for areas of future study, (b) synthesising conclusions in an area of ambiguity and (c) helping clinicians and researchers inform decision-making and practice guidelines. Literature reviews can be narrative or systematic, with narrative reviews aiming to provide a descriptive overview of selected literature, without undertaking a systematic literature search. By contrast, systematic reviews use explicit and replicable methods in order to retrieve all available literature pertaining to a specific topic to answer a defined question (Higgins Reference Higgins and Green 2011 ). Systematic reviews therefore require a priori strategies to search the literature, with predefined criteria for included and excluded studies that should be reported in full detail in a review protocol.
Performing an effective literature search to obtain the best available evidence is the basis of any evidence-based discipline, in particular evidence-based medicine (Sackett Reference Sackett 1997 ; McKeever Reference McKeever, Nguyen and Peterson 2015 ). However, with a vast and growing volume of published research available, searching the literature can be challenging. Even when journals are indexed in electronic databases, it can be difficult to identify all relevant studies without an effective search strategy (Hopewell Reference Hopewell, Clarke and Lefebvre 2007 ). In addition, unpublished data and ‘grey’ literature (informally published material such as conference abstracts) are now becoming more accessible to the public. It is important to search unpublished literature to reduce publication bias, which occurs because of a tendency for authors and journals to preferentially publish statistically significant studies (Dickersin Reference Dickersin and Min 1993 ). Efforts to locate unpublished and grey literature during the search process can help to reduce bias in the results of systematic reviews (Song Reference Song, Parekh and Hooper 2010 ). A paradigmatic example demonstrating the importance of capturing unpublished data is that of Turner et al ( Reference Turner, Matthews and Linardatos 2008 ), who showed that using only published data in their meta-analysis led to effect sizes for antidepressants that were one-third (32%) larger than effect sizes derived from combining both published and unpublished data. Such differences in findings from published and unpublished data can have real-life implications in clinical decision-making and treatment recommendation. In another relevant publication, Whittington et al ( Reference Whittington, Kendall and Fonagy 2004 ) compared the risks and benefits of selective serotonin reuptake inhibitors (SSRIs) in the treatment of depression in children. They found that published data suggested favourable risk–benefit profiles for SSRIs in this population, but the addition of unpublished data indicated that risk outweighed treatment benefits. The relative weight of drug efficacy to side-effects can be skewed if there has been a failure to search for, or include, unpublished data.
In this guide for clinicians and researchers on how to perform a literature search we use a working example about efficacy of an intervention for bipolar disorder to demonstrate the search techniques outlined. However, the overarching methods described are purposefully broad to make them accessible to all clinicians and researchers, regardless of their research or clinical question.
The review question will guide not only the search strategy, but also the conclusions that can be drawn from the review, as these will depend on which studies or other forms of evidence are included and excluded from the literature review. A narrow question will produce a narrow and precise search, perhaps resulting in too few studies on which to base a review, or be so focused that the results are not useful in wider clinical settings. Using an overly narrow search also increases the chances of missing important studies. A broad question may produce an imprecise search, with many false-positive search results. These search results may be too heterogeneous to evaluate in one review. Therefore from the outset, choices should be made about the remit of the review, which will in turn affect the search.
A number of frameworks can be used to break the review question into concepts. One such is the PICO (population, intervention, comparator and outcome) framework, developed to answer clinical questions such as the effectiveness of a clinical intervention (Richardson Reference Richardson, Wilson and Nishikawa 1995 ). It is noteworthy that ‘outcome’ concepts of the PICO framework are less often used in a search strategy as they are less well defined in the titles and abstracts of available literature (Higgins Reference Higgins and Green 2011 ). Although PICO is widely used, it is not a suitable framework for identifying key elements of all questions in the medical field, and minor adaptations are necessary to enable the structuring of different questions. Other frameworks exist that may be more appropriate for questions about health policy and management, such as ECLIPSE (expectation, client group, location, impact, professionals, service) (Wildridge Reference Wildridge and Bell 2002 ) or SPICE (setting, perspective, intervention, comparison, evaluation) for service evaluation (Booth Reference Booth 2006 ). A detailed overview of frameworks is provided in Davies ( Reference Davies 2011 ).
Before conducting a comprehensive literature search, a scoping search of the literature using just one or two databases (such as PubMed or MEDLINE) can provide valuable information as to how much literature for a given review question already exists. A scoping search may reveal whether systematic reviews have already been undertaken for a review question. Caution should be taken, however, as systematic reviews that may appear to ask the same question may have differing inclusion and exclusion criteria for studies included in the review. In addition, not all systematic reviews are of the same quality. If the original search strategy is of poor quality methodologically, original data are likely to have been missed and the search should not simply be updated (compare, for example, Naughton et al ( Reference Naughton, Clarke and O'Leary 2014 ) and Caddy et al ( Reference Caddy, Amit and McCloud 2015 ) on ketamine for treatment-resistant depression).
The first step in conducting a literature search should be to develop a search strategy. The search strategy should define how relevant literature will be identified. It should identify sources to be searched (list of databases and trial registries) and keywords used in the literature (list of keywords). The search strategy should be documented as an integral part of the systematic review protocol. Just as the rest of a well-conducted systematic review, the search strategy used needs to be explicit and detailed such that it could reproduced using the same methodology, with exactly the same results, or updated at a later time. This not only improves the reliability and accuracy of the review, but also means that if the review is replicated, the difference in reviewers should have little effect, as they will use an identical search strategy. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement was developed to standardise the reporting of systematic reviews (Moher Reference Moher, Liberati and Tetzlaff 2009 ). The PRISMA statement consists of a 27-item checklist to assess the quality of each element of a systematic review (items 6, 7 and 8 relate to the quality of literature searching) and also to guide authors when reporting their findings.
There are a number of databases that can be searched for literature, but the identification of relevant sources is dependent on the clinical or research question (different databases have different focuses, from more biology to more social science oriented) and the type of evidence that is sought (i.e. some databases report only randomised controlled trials).
• MEDLINE and Embase are the two main biomedical literature databases. MEDLINE contains more than 22 million references from more than 5600 journals worldwide. In addition, the MEDLINE In-Process & Other Non-Indexed Citations database holds references before they are published on MEDLINE. Embase has a strong coverage of drug and pharmaceutical research and provides over 30 million references from more than 8500 currently published journals, 2900 of which are not in MEDLINE. These two databases, however, are only available to either individual subscribers or through institutional access such as universities and hospitals. PubMed, developed by the National Center for Biotechnology Information of the US National Library of Medicine, provides access to a free version of MEDLINE and is accessible to researchers, clinicians and the public. PubMed comprises medical and biomedical literature indexed in MEDLINE, but provides additional access to life science journals and e-books.
In addition, there are a number of subject- and discipline-specific databases.
• PsycINFO covers a range of psychological, behavioural, social and health sciences research.
• The Cochrane Central Register of Controlled Trials (CENTRAL) hosts the most comprehensive source of randomised and quasi-randomised controlled trials. Although some of the evidence on this register is also included in Embase and MEDLINE, there are over 150 000 reports indexed from other sources, such as conference proceedings and trial registers, that would otherwise be less accessible (Dickersin Reference Dickersin, Manheimer and Wieland 2002 ).
• The Cumulative Index to Nursing and Allied Health Literature (CINAHL), British Nursing Index (BNI) and the British Nursing Database (formerly BNI with Full Text) are databases relevant to nursing, but they span literature across medical, allied health, community and health management journals.
• The Allied and Complementary Medicine Database (AMED) is a database specifically for alternative treatments in medicine.
The examples of specific databases given here are by no means exhaustive, but they are popular and likely to be used for literature searching in medicine, psychiatry and psychology. Website links for these databases are given in Box 1 , along with links to resources not mentioned above. Box 1 also provides a website link to a couple of video tutorials for searching electronic databases. Box 2 shows an example of the search sources chosen for a review of a pharmacological intervention of calcium channel antagonists in bipolar disorder, taken from a recent systematic review (Cipriani Reference Cipriani, Saunders and Attenburrow 2016a ).
BOX 1 Website links of search sources to obtain published and unpublished literature
Electronic databases
• MEDLINE/PubMed: www.ncbi.nlm.nih.gov/pubmed
• Embase: www.embase.com
• PsycINFO: www.apa.org/psycinfo
• Cochrane Central Register of Controlled Trials (CENTRAL): www.cochranelibrary.com
• Cumulative Index of Nursing and Allied Health Literature (CINAHL): www.cinahl.com
• British Nursing Index: www.bniplus.co.uk
• Allied and Complementary Medicine Database: https://www.ebsco.com/products/research-databases/amed-the-allied-and-complementary-medicine-database
Grey literature databases
• BIOSIS Previews (part of Thomson Reuters Web of Science): https://apps.webofknowledge.com
Trial registries
• ClinicalTrials.gov: www.clinicaltrials.gov
• Drugs@FDA: www.accessdata.fda.gov/scripts/cder/daf
• European Medicines Agency (EMA): www.ema.europa.eu
• World Health Organization International Clinical Trials Registry Platform (WHO ICTRP): www.who.int/ictrp
• GlaxoSmithKline Study Register: www.gsk-clinicalstudyregister.com
• Eli-Lilly clinical trial results: https://www.lilly.com/clinical-study-report-csr-synopses
Guides to further resources
• King's College London Library Services: http://libguides.kcl.ac.uk/ld.php?content_id=17678464
• Georgetown University Medical Center Dahlgren Memorial Library: https://dml.georgetown.edu/core
• University of Minnesota Biomedical Library: https://hsl.lib.umn.edu/biomed/help/nursing
Tutorial videos
• Searches in electronic databases: http://library.buffalo.edu/hsl/services/instruction/tutorials.html
• Using the Yale MeSH Analyzer tool: http://library.medicine.yale.edu/tutorials/1559
BOX 2 Example of search sources chosen for a review of calcium channel antagonists in bipolar disorder (Cipriani Reference Cipriani, Saunders and Attenburrow 2016a )
Electronic databases searched:
• MEDLINE In-Process and Other Non-Indexed Citations
For a comprehensive search of the literature it has been suggested that two or more electronic databases should be used (Suarez-Almazor Reference Suarez-Almazor, Belseck and Homik 2000 ). Suarez-Almazor and colleagues demonstrated that, in a search for controlled clinical trials (CCTs) for rheumatoid arthritis, osteoporosis and lower back pain, only 67% of available citations were found by both Embase and MEDLINE. Searching MEDLINE alone would have resulted in 25% of available CCTs being missed and searching Embase alone would have resulted in 15% of CCTs being missed. However, a balance between the sensitivity of a search (an attempt to retrieve all relevant literature in an extensive search) and the specificity of a search (an attempt to retrieve a more manageable number of relevant citations) is optimal. In addition, supplementing electronic database searches with unpublished literature searches (see ‘Obtaining unpublished literature’ below) is likely to reduce publication bias. The capacity of the individuals or review team is likely largely to determine the number of sources searched. In all cases, a clear rationale should be outlined in the review protocol for the sources chosen (the expertise of an information scientist is valuable in this process).
Important methodological considerations (such as study design) may also be included in the search strategy. Dependent on the databases and supplementary sources chosen, filters can be used to search the literature by study design (see ‘Searching electronic databases’). For instance, if the search strategy is confined to one study design term only (e.g. randomised controlled trial, RCT), only the articles labelled in this way will be selected. However, it is possible that in the database some RCTs are not labelled as such, so they will not be picked up by the filtered search. Filters can help reduce the number of references retrieved by the search, but using just one term is not 100% sensitive, especially if only one database is used (i.e. MEDLINE). It is important for systematic reviewers to know how reliable such a strategy can be and treat the results with caution.
Identifying search terms
Standardised search terms are thesaurus and indexing terms that are used by electronic databases as a convenient way to categorise articles, allowing for efficient searching. Individual database records may be assigned several different standardised search terms that describe the same or similar concepts (e.g. bipolar disorder, bipolar depression, manic–depressive psychosis, mania). This has the advantage that even if the original article did not use the standardised term, when the article is catalogued in a database it is allocated that term (Guaiana Reference Guaiana, Barbui and Cipriani 2010 ). For example, an older paper might refer to ‘manic depression’, but would be categorised under the term ‘bipolar disorder’ when catalogued in MEDLINE. These standardised search terms are called MeSH (medical subject headings) in MEDLINE and PubMed, and Emtree in Embase, and are organised in a hierarchal structure ( Fig. 1 ). In both MEDLINE and Embase an ‘explode’ command enables the database to search for a requested term, as well as specific related terms. Both narrow and broader search terms can be viewed and selected to be included in the search if appropriate to a topic. The Yale MeSH Analyzer tool ( mesh.med.yale.edu ) can be used to help identify potential terms and phrases to include in a search. It is also useful to understand why relevant articles may be missing from an initial search, as it produces a comparison grid of MeSH terms used to index each article (see Box 1 for a tutorial video link).
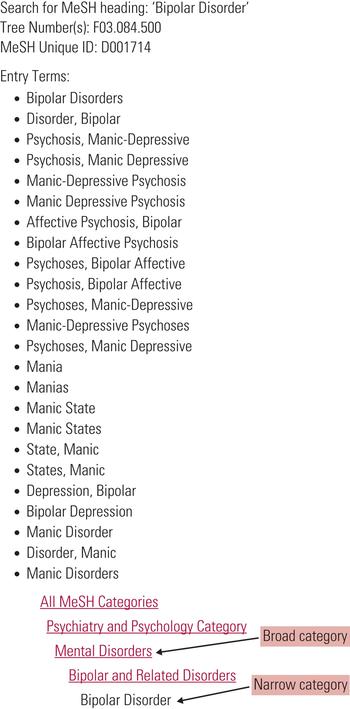
FIG 1 Search terms and hierarchical structure of MeSH (medical subject heading) in MEDLINE and PubMed.
In addition, MEDLINE also distinguishes between MeSH headings (MH) and publication type (PT) terms. Publication terms are less about the content of an article than about its type, specifying for example a review article, meta-analysis or RCT.
Both MeSH and Emtree have their own peculiarities, with variations in thesaurus and indexing terms. In addition, not all concepts are assigned standardised search terms, and not all databases use this method of indexing the literature. It is advisable to check the guidelines of selected databases before undertaking a search. In the absence of a MeSH heading for a particular term, free-text terms could be used.
Free-text terms are used in natural language and are not part of a database’s controlled vocabulary. Free-text terms can be used in addition to standardised search terms in order to identify as many relevant records as possible (Higgins Reference Higgins and Green 2011 ). Using free-text terms allows the reviewer to search using variations in language or spelling (e.g. hypomani* or mania* or manic* – see truncation and wildcard functions below and Fig. 2 ). A disadvantage of free-text terms is that they are only searched for in the title and abstracts of database records, and not in the full texts, meaning that when a free-text word is used only in the body of an article, it will not be retrieved in the search. Additionally, a number of specific considerations should be taken into account when selecting and using free-text terms:
• synonyms, related terms and alternative phrases (e.g. mood instability, affective instability, mood lability or emotion dysregulation)
• abbreviations or acronyms in medical and scientific research (e.g. magnetic resonance imaging or MRI)
• lay and medical terminology (e.g. high blood pressure or hypertension)
• brand and generic drug names (e.g. Prozac or fluoxetine)
• variants in spelling (e.g. UK English and American English: behaviour or behavior; paediatric or pediatric).

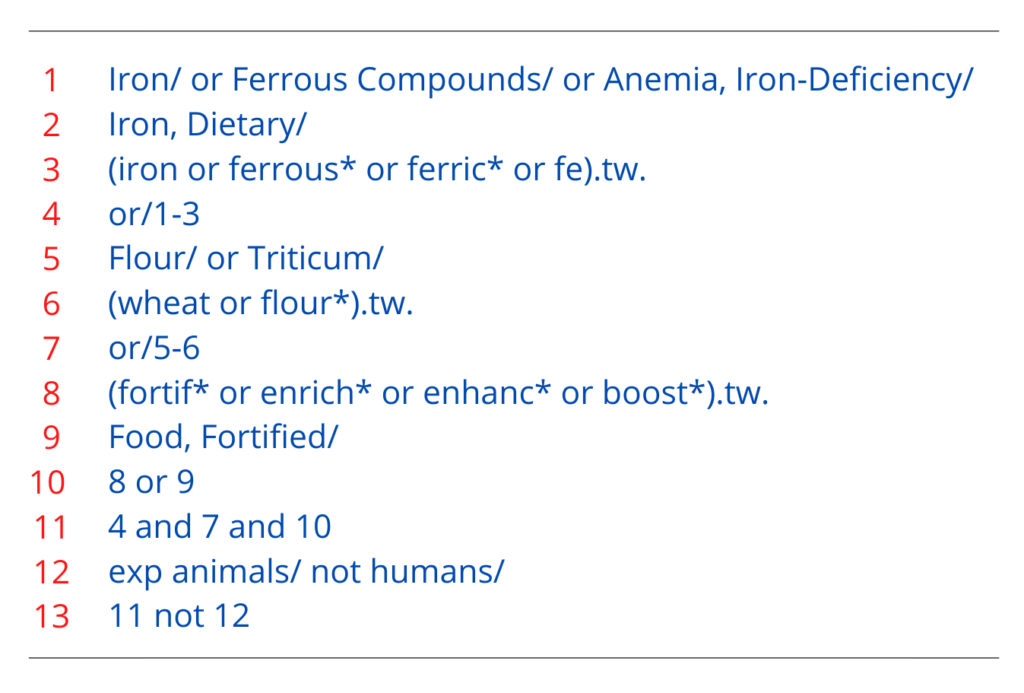
FIG 2 Example of a search strategy about bipolar disorder using MEDLINE (Cipriani Reference Cipriani, Saunders and Attenburrow 2016a ). The strategy follows the PICO framework and includes MeSH terms, free-text keywords and a number of other techniques, such as truncation, that have been outlined in this article. Numbers in bold give the number of citations retrieved by each search.
Truncation and wildcard functions can be used in most databases to capture variations in language:
• truncation allows the stem of a word that may have variant endings to be searched: for example, a search for depress* uses truncation to retrieve articles that mention both depression and depressive; truncation symbols may vary by database, but common symbols include: *, ! and #
• wild cards substitute one letter within a word to retrieve alternative spellings: for example, ‘wom?n’ would retrieve the terms ‘woman’ and ‘women’.
Combining search terms
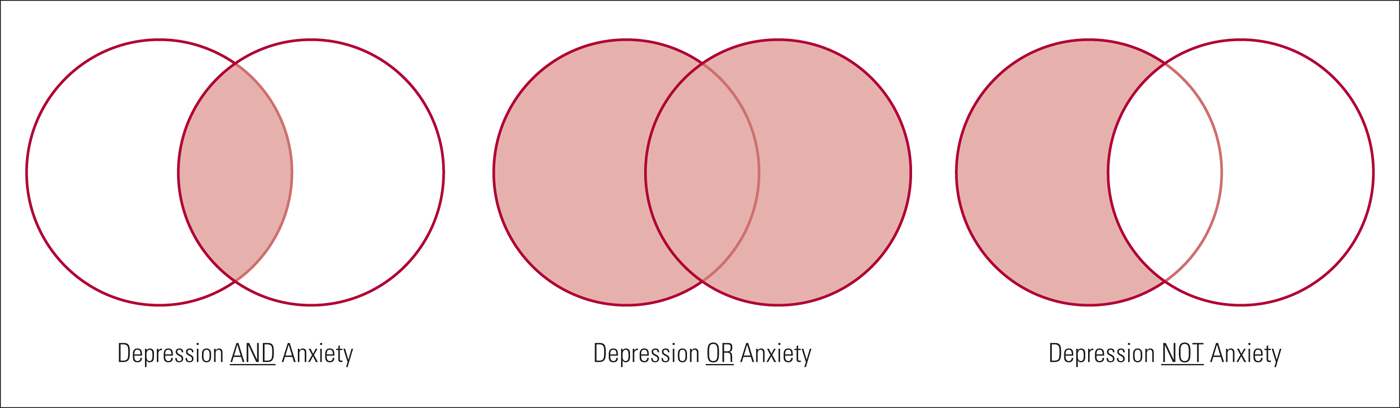
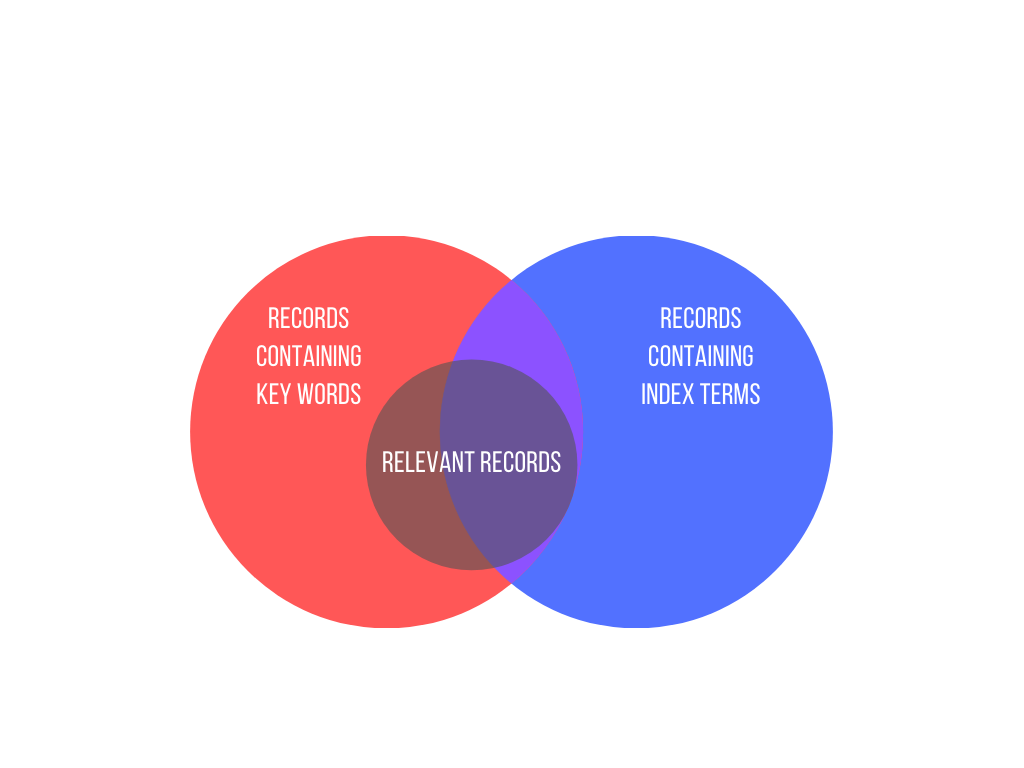
Search terms should be combined in the search strategy using Boolean operators. Boolean operators allow standardised search terms and free-text terms to be combined. There are three main Boolean operators – AND, OR and NOT ( Fig. 3 ).
• OR – this operator is used to broaden a search, finding articles that contain at least one of the search terms within a concept. Sets of terms can be created for each concept, for example the population of interest: (bipolar disorder OR bipolar depression). Parentheses are used to build up search terms, with words within parentheses treated as a unit.
• AND – this can be used to join sets of concepts together, narrowing the retrieved literature to articles that contain all concepts, for example the population or condition of interest and the intervention to be evaluated: (bipolar disorder OR bipolar depression) AND calcium channel blockers. However, if at least one term from each set of concepts is not identified from the title or abstract of an article, this article will not be identified by the search strategy. It is worth mentioning here that some databases can run the search also across the full texts. For example, ScienceDirect and most publishing houses allow this kind of search, which is much more comprehensive than abstract or title searches only.
• NOT – this operator, used less often, can focus a search strategy so that it does not retrieve specific literature, for example human studies NOT animal studies. However, in certain cases the NOT operator can be too restrictive, for example if excluding male gender from a population, using ‘NOT male’ would also mean that any articles about both males and females are not obtained by the search.
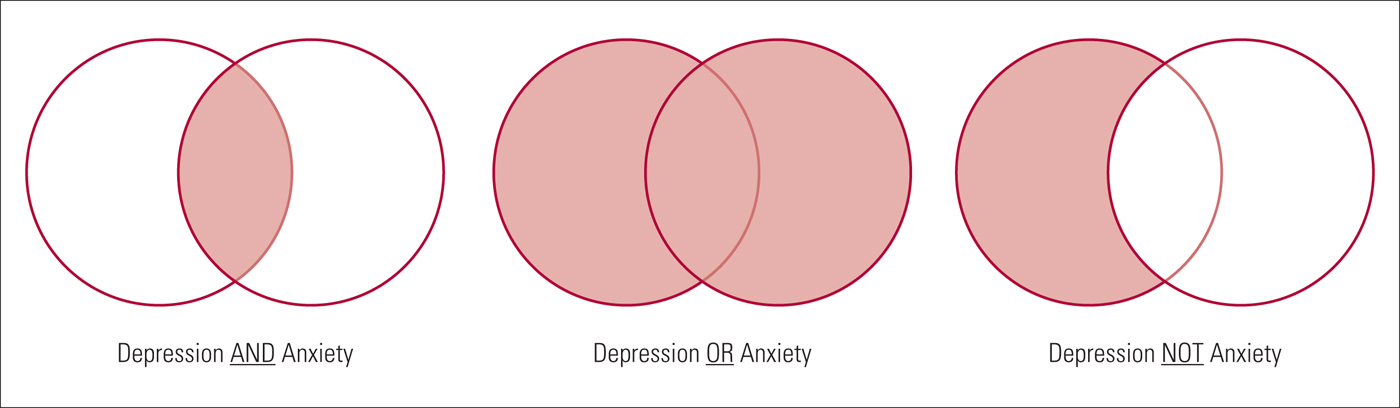
FIG 3 Example of Boolean operator concepts (the resulting search is the light red shaded area).
The conventions of each database should be checked before undertaking a literature search, as functions and operators may differ slightly between them (Cipriani Reference Cipriani, Saunders and Attenburrow 2016b ). This is particularly relevant when using limits and filters. Figure 2 shows an example search strategy incorporating many of the concepts described above. The search strategy is taken from Cipriani et al ( Reference Cipriani, Zhou and Del Giovane 2016a ), but simplified to include only one intervention.
Search filters
A number of filters exist to focus a search, including language, date and study design or study focus filters. Language filters can restrict retrieval of articles to the English language, although if language is not an inclusion criterion it should not be restricted, to avoid language bias. Date filters can be used to restrict the search to literature from a specified period, for example if an intervention was only made available after a certain date. In addition, if good systematic reviews exist that are likely to capture all relevant literature (as advised by an information specialist), date restrictions can be used to search additional literature published after the date of that included in the systematic review. In the same way, date filters can be used to update a literature search since the last time it was conducted. Reviewing the literature should be a timely process (new and potentially relevant evidence is produced constantly) and updating the search is an important step, especially if collecting evidence to inform clinical decision-making, as publications in the field of medicine are increasing at an impressive rate (Barber Reference Barber, Corsi and Furukawa 2016 ). The filters chosen will depend on the research question and nature of evidence that is sought through the literature search and the guidelines of the individual database that is used.
- Google Scholar
Google Scholar allows basic Boolean operators to be used in strings of search terms. However, the search engine does not use standardised search terms that have been tagged as in traditional databases and therefore variations of keywords should always be searched. There are advantages and disadvantages to using a web search engine such as Google Scholar. Google Scholar searches the full text of an article for keywords and also searches a wider range of sources, such as conference proceedings and books, that are not found in traditional databases, making it a good resource to search for grey literature (Haddaway Reference Haddaway, Collins and Coughlin 2015 ). In addition, Google Scholar finds articles cited by other relevant articles produced in the search. However, variable retrieval of content (due to regular updating of Google algorithms and the individual's search history and location) means that search results are not necessarily reproducible and are therefore not in keeping with replicable search methods required by systematic reviews. Google Scholar alone has not been shown to retrieve more literature than other traditional databases discussed in this article and therefore should be used in addition to other sources (Bramer Reference Bramer, Giustini and Kramer 2016 ).
Citation searching
Once the search strategy has identified relevant literature, the reference lists in these sources can be searched. This is called citation searching or backward searching, and it can be used to see where particular research topics led others. This method is particularly useful if the search identifies systematic reviews or meta-analyses of a similar topic.
Conference abstracts
Conference abstracts are considered ‘grey literature’, i.e. literature that is not formally published in journals or books (Alberani Reference Alberani, De Castro Pietrangeli and Mazza 1990 ). Scherer and colleagues found that only 52.6% of all conference abstracts go on to full publication of results, and factors associated with publication were studies that had RCT designs and the reporting of positive or significant results (Scherer Reference Scherer, Langenberg and von Elm 2007 ). Therefore, failure to search relevant grey literature might miss certain data and bias the results of a review. Although conference abstracts are not indexed in most major electronic databases, they are available in databases such as BIOSIS Previews ( Box 1 ). However, as with many unpublished studies, these data did not undergo the peer review process that is often a tool for assessing and possibly improving the quality of the publication.
Searching trial registers and pharmaceutical websites
For reviews of trial interventions, a number of trial registers exist. ClinicalTrials.gov ( clinicaltrials.gov ) provides access to information on public and privately conducted clinical trials in humans. Results for both published and unpublished studies can be found for many trials on the register, in addition to information about studies that are ongoing. Searching each trial register requires a slightly different search strategy, but many of the basic principles described above still apply. Basic searches on ClinicialTrials.gov include searching by condition, specific drugs or interventions and these can be linked using Boolean operators: for example, (bipolar disorder OR manic depressive disorder) AND lithium. As mentioned above, parentheses can be used to build up search terms. More advanced searches allow one to specify further search fields such as the status of studies, study type and age of participants. The US Food and Drug Administration (FDA) hosts a database providing information about FDA-approved drugs, therapeutic products and devices ( www.fda.gov ). The database (with open access to anyone, not only in the USA) can be searched by the drug name, its active ingredient or its approval application number and, for most drugs approved in the past 20 years or so, a review of clinical trial results (some of which remain unpublished) used as evidence in the approval process is available. The European Medicines Agency (EMA) hosts a similar register for medicines developed for use in the European Union ( www.ema.europa.eu ). An internet search will show that many other national and international trial registers exist that, depending on the review question, may be relevant search sources. The World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; www.who.int/ictrp ) provides access to a central database bringing a number of these national and international trial registers together. It can be searched in much the same way as ClinicalTrials.gov.
A number of pharmaceutical companies now share data from company-sponsored clinical trials. GlaxoSmithKline (GSK) is transparent in the sharing of its data from clinical studies and hosts its own clinical study register ( www.gsk-clinicalstudyregister.com ). Eli-Lilly provides clinical trial results both on its website ( www.lillytrialguide.com ) and in external registries. However, other pharmaceutical companies, such as Wyeth and Roche, divert users to clinical trial results in external registries. These registries include both published and previously unpublished studies. Searching techniques differ for each company and hand-searching through documents is often required to identify studies.
Communication with authors
Direct communication with authors of published papers could produce both additional data omitted from published studies and other unpublished studies. Contact details are usually available for the corresponding author of each paper. Although high-quality reviews do make efforts to obtain and include unpublished data, this does have potential disadvantages: the data may be incomplete and are likely not to have been peer-reviewed. It is also important to note that, although reviewers should make every effort to find unpublished data in an effort to minimise publication bias, there is still likely to remain a degree of this bias in the studies selected for a systematic review.
Developing a literature search strategy is a key part of the systematic review process, and the conclusions reached in a systematic review will depend on the quality of the evidence retrieved by the literature search. Sources should therefore be selected to minimise the possibility of bias, and supplementary search techniques should be used in addition to electronic database searching to ensure that an extensive review of the literature has been carried out. It is worth reminding that developing a search strategy should be an iterative and flexible process (Higgins Reference Higgins and Green 2011 ), and only by conducting a search oneself will one learn about the vast literature available and how best to capture it.
Acknowledgements
We thank Sarah Stockton for her help in drafting this article. Andrea Cipriani is supported by the NIHR Oxford cognitive health Clinical Research Facility.
Select the single best option for each question stem
a an explicit and replicable method used to retrieve all available literature pertaining to a specific topic to answer a defined question
b a descriptive overview of selected literature
c an initial impression of a topic which is understood more fully as a research study is conducted
d a method of gathering opinions of all clinicians or researchers in a given field
e a step-by-step process of identifying the earliest published literature through to the latest published literature.
a does not need to be specified in advance of a literature search
b does not need to be reported in a systematic literature review
c defines which sources of literature are to be searched, but not how a search is to be carried out
d defines how relevant literature will be identified and provides a basis for the search strategy
e provides a timeline for searching each electronic database or unpublished literature source.
a the Cochrane Central Register of Controlled Trials (CENTRAL)
d the Cumulative Index to Nursing and Allied Health Literature (CINAHL)
e the British Nursing Index.
a bipolar disorder OR treatment
b bipolar* OR treatment
c bipolar disorder AND treatment
d bipolar disorder NOT treatment
e (bipolar disorder) OR (treatment).
a publication bias
b funding bias
c language bias
d outcome reporting bias
e selection bias.
MCQ answers
1 a 2 d 3 b 4 c 5 a
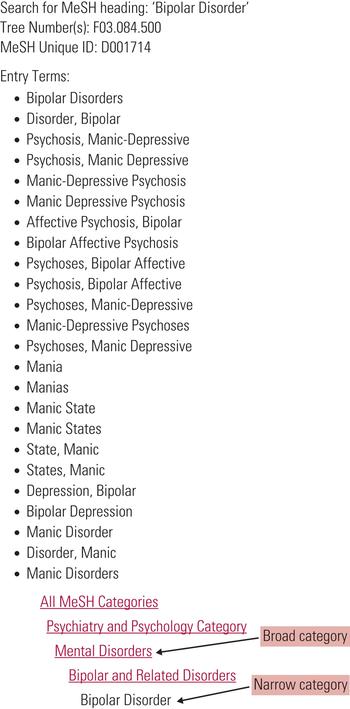
FIG 2 Example of a search strategy about bipolar disorder using MEDLINE (Cipriani 2016a). The strategy follows the PICO framework and includes MeSH terms, free-text keywords and a number of other techniques, such as truncation, that have been outlined in this article. Numbers in bold give the number of citations retrieved by each search.
This article has been cited by the following publications. This list is generated based on data provided by Crossref .
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 24, Issue 2
- Lauren Z. Atkinson and Andrea Cipriani
- DOI: https://doi.org/10.1192/bja.2017.3
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
Covidence website will be inaccessible as we upgrading our platform on Monday 23rd August at 10am AEST, / 2am CEST/1am BST (Sunday, 15th August 8pm EDT/5pm PDT)
How to write a search strategy for your systematic review
Home | Blog | How To | How to write a search strategy for your systematic review
Practical tips to write a search strategy for your systematic review
With a great review question and a clear set of eligibility criteria already mapped out, it’s now time to plan the search strategy. The medical literature is vast. Your team plans a thorough and methodical search, but you also know that resources and interest in the project are finite. At this stage it might feel like you have a mountain to climb.
The bottom line? You will have to sift through some irrelevant search results to find the studies that you need for your review. Capturing a proportion of irrelevant records in your search is necessary to ensure that it identifies as many relevant records as possible. This is the trade-off of precision versus sensitivity and, because systematic reviews aim to be as comprehensive as possible, it is best to favour sensitivity – more is more.
By now, the size of this task might be sounding alarm bells. The good news is that a range of techniques and web-based tools can help to make searching more efficient and save you time. We’ll look at some of them as we walk through the four main steps of searching for studies:
- Decide where to search
- Write and refine the search
- Run and record the search
- Manage the search results
Searching is a specialist discipline and the information given here is not intended to replace the advice of a skilled professional. Before we look at each of the steps in turn, the most important systematic reviewer pro-tip for searching is:
Pro Tip – Talk to your librarian and do it early!
1. decide where to search .
It’s important to come up with a comprehensive list of sources to search so that you don’t miss anything potentially relevant. In clinical medicine, your first stop will likely be the databases MEDLINE , Embase , and CENTRAL . Depending on the subject of the review, it might also be appropriate to run the search in databases that cover specific geographical regions or specialist areas, such as traditional Chinese medicine.
In addition to these databases, you’ll also search for grey literature (essentially, research that was not published in journals). That’s because your search of bibliographic databases will not find relevant information if it is part of, for example:
- a trials register
- a study that is ongoing
- a thesis or dissertation
- a conference abstract.
Over-reliance on published data introduces bias in favour of positive results. Studies with positive results are more likely to be submitted to journals, published in journals, and therefore indexed in databases. This is publication bias and systematic reviews seek to minimise its effects by searching for grey literature.
2. Write and refine the search
Search terms are derived from key concepts in the review question and from the inclusion and exclusion criteria that are specified in the protocol or research plan.
Keywords will be searched for in the title or abstract of the records in the database. They are often truncated (for example, a search for therap* to find therapy, therapies, therapist). They might also use wildcards to allow for spelling variants and plurals (for example, wom#n to find woman and women). The symbols used to perform truncation and wildcard searches vary by database.
Index terms
Using index terms such as MeSH and Emtree in a search can improve its performance. Indexers with subject area expertise work through databases and tag each record with subject terms from a prespecified controlled vocabulary.
This indexing can save review teams a lot of time that would otherwise be spent sifting through irrelevant records. Using index terms in your search, for example, can help you find the records that are actually about the topic of interest (tagged with the index term) but ignore those that contain only a brief mention of it (not tagged with the index term).
Indexers assign terms based on a careful read of each study, rather than whether or not the study contains certain words. So the index terms enable the retrieval of relevant records that cannot be captured by a simple search for the keyword or phrase.
Use a combination
Relying solely on index terms is not advisable. Doing so could miss a relevant record that for some reason (indexer’s judgment, time lag between a record being listed in a database and being indexed) has not been tagged with an index term that would enable you to retrieve it. Good search strategies include both index terms and keywords.
Let’s see how this works in a real review! Figure 2 shows the search strategy for the review ‘Wheat flour fortification with iron and other micronutrients for reducing anaemia and improving iron status in populations’. This strategy combines index terms and keywords using the Boolean operators AND, OR, and NOT. OR is used first to reach as many records as possible before AND and NOT are used to narrow them down.
- Lines 1 and 2: contain MeSH terms (denoted by the initial capitals and the slash at the end).
- Line 3: contains truncated keywords (‘tw’ in this context is an instruction to search the title and abstract fields of the record).
- Line 4: combines the three previous lines using Boolean OR to broaden the search.
- Line 11: combines previous lines using Boolean AND to narrow the search.
- Lines 12 and 13: further narrow the search using Boolean NOT to exclude records of studies with no human subjects.
Writing a search strategy is an iterative process. A good plan is to try out a new strategy and check that it has picked up the key studies that you would expect it to find based on your existing knowledge of the topic area. If it hasn’t, you can explore the reasons for this, revise the strategy, check it for errors, and try it again!
3. Run and record the search
Because of the different ways that individual databases are structured and indexed, a separate search strategy is needed for each database. This adds complexity to the search process, and it is important to keep a careful record of each search strategy as you run it. Search strategies can often be saved in the databases themselves, but it is a good idea to keep an offline copy as a back-up; Covidence allows you to store your search strategies online in your review settings.
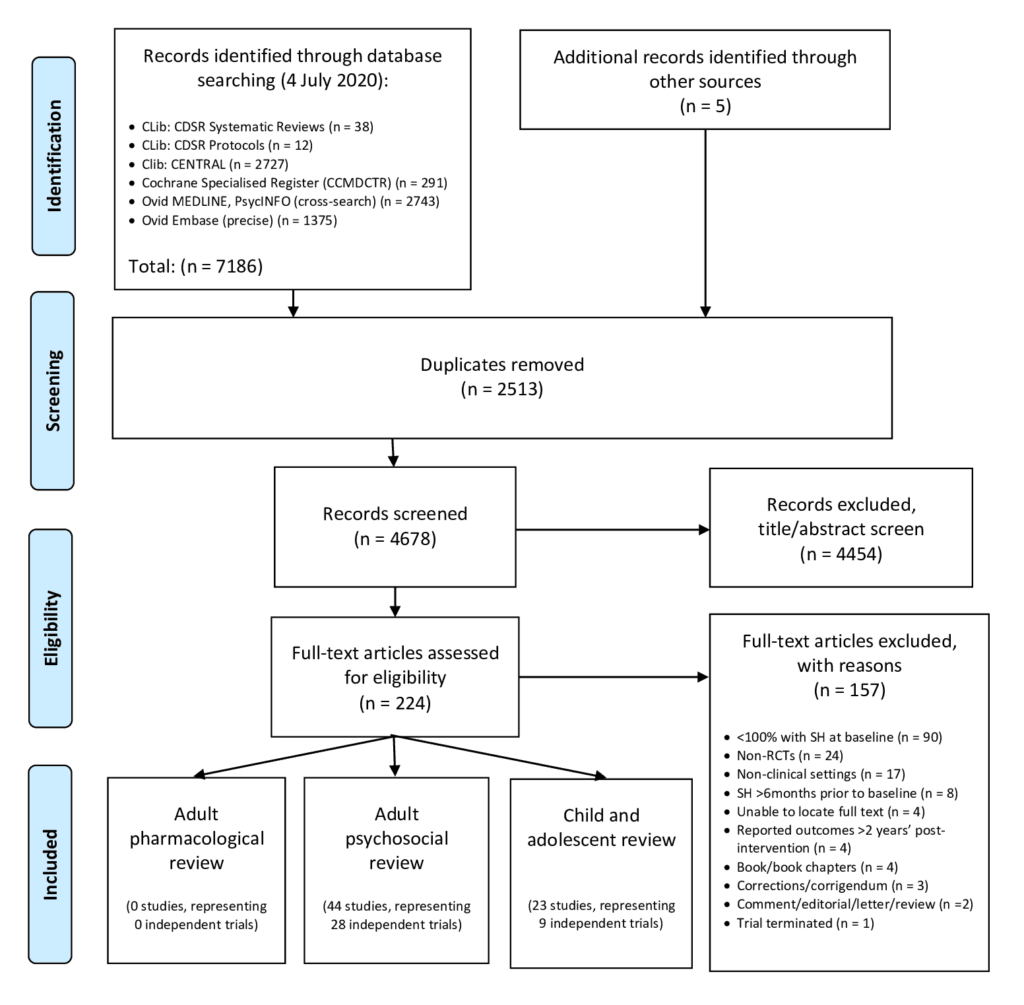
The reporting of the search will be included in the methods section of your review and should follow the PRISMA guidelines. You can download a flow diagram from PRISMA’s website to help you log the number of records retrieved from the search and the subsequent decisions about the inclusion or exclusion of studies. The PRISMA-S extension provides guidance on reporting literature searches.
It is very important that search strategies are reproduced in their entirety (preferably using copy and paste to avoid typos) as part of the published review so that they can be studied and replicated by other researchers. Search strategies are often made available as an appendix because they are long and might otherwise interrupt the flow of the text in the methods section.
4. Manage the search results
Once the search is done and you have recorded the process in enough detail to write up a thorough description in the methods section, you will move on to screening the results. This is an exciting stage in any review because it’s the first glimpse of what the search strategies have found. A large volume of results may be daunting but your search is very likely to have captured some irrelevant studies because of its high sensitivity, as we have already seen. Fortunately, it will be possible to exclude many of these irrelevant studies at the screening stage on the basis of the title and abstract alone 😅.
Search results from multiple databases can be collated in a single spreadsheet for screening. To benefit from process efficiencies, time-saving and easy collaboration with your team, you can import search results into a specialist tool such as Covidence. A key benefit of Covidence is that you can track decisions made about the inclusion or exclusion of studies in a simple workflow and resolve conflicting decisions quickly and transparently. Covidence currently supports three formats for file imports of search results:
- EndNote XML
- PubMed text format
- RIS text format
If you’d like to try this feature of Covidence but don’t have any data yet, you can download some ready-made sample data .
And you’re done!
There is a lot to think about when planning a search strategy. With practice, expert help, and the right tools your team can complete the search process with confidence.
This blog post is part of the Covidence series on how to write a systematic review.
Sign up for a free trial of Covidence today!
[1] Witt KG, Hetrick SE, Rajaram G, Hazell P, Taylor Salisbury TL, Townsend E, Hawton K. Pharmacological interventions for self‐harm in adults . Cochrane Database of Systematic Reviews 2020, Issue 12. Art. No.: CD013669. DOI: 10.1002/14651858.CD013669.pub2. Accessed 02 February 2021
Laura Mellor. Portsmouth, UK
Perhaps you'd also like....
Top 5 Tips for High-Quality Systematic Review Data Extraction
Data extraction can be a complex step in the systematic review process. Here are 5 top tips from our experts to help prepare and achieve high quality data extraction.
How to get through study quality assessment Systematic Review
Find out 5 tops tips to conducting quality assessment and why it’s an important step in the systematic review process.

How to extract study data for your systematic review
Learn the basic process and some tips to build data extraction forms for your systematic review with Covidence.
Better systematic review management
Head office, working for an institution or organisation.
Find out why over 350 of the world’s leading institutions are seeing a surge in publications since using Covidence!
Request a consultation with one of our team members and start empowering your researchers:
By using our site you consent to our use of cookies to measure and improve our site’s performance. Please see our Privacy Policy for more information.
Search Strategies for [Systematic] Literature Reviews
- First Online: 11 August 2022
Cite this chapter

- Rob Dekkers 4 ,
- Lindsey Carey 5 &
- Peter Langhorne 6
2112 Accesses
3 Citations
After setting review questions as discussed in the previous chapter, the search for relevant publications is the next step of a literature review.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
JEL is the abbreviation of the ‘Journal of Economics Literature’, published by the American Economic Association, which launched this coding system.
Actually, Schlosser et al. ( 2006 , p. 571 ff.) call it ‘traditional pearl growing.’ The term ‘classical’ pearl growing has been adopted to ensure consistency throughout the book.
The wording ‘topical bibliography’ by Schlosser et al. ( 2006 , p. 574) has been replaced with ‘topical survey’ in order to connect better to the terminology in this book.
Webster and Watson ( 2002 , p. xvi) call it forward searching and backward searching rather than snowballing. See Table 5.3 for the nomenclature used in the book for search strategies.
Aguillo IF (2012) Is Google Scholar useful for bibliometrics? A webometric analysis. Scientometrics 91(2):343–351. https://doi.org/10.1007/s11192-011-0582-8
Bardia A, Wahner-Roedler DL, Erwin PL, Sood A (2006) Search strategies for retrieving complementary and alternative medicine clinical trials in oncology. Integr Cancer Ther 5(3):202–205. https://doi.org/10.1177/1534735406292146
Bates MJ (1989) The design of browsing and berrypicking techniques for the online search interface. Online Rev 13(5):407–424
Google Scholar
Bates MJ (2007) What is browsing—really? A model drawing from behavioural science research. Inform Res 20(4). http://informationr.net/ir/12-4/paper330.html
Benzies KM, Premji S, Hayden KA, Serrett K (2006) State-of-the-evidence reviews: advantages and challenges of including grey literature. Worldviews Evid Based Nurs 3(2):55–61. https://doi.org/10.1111/j.1741-6787.2006.00051.x
Bernardo M, Simon A, Tarí JJ, Molina-Azorín JF (2015) Benefits of management systems integration: a literature review. J Clean Prod 94:260–267. https://doi.org/10.1016/j.jclepro.2015.01.075
Beynon R, Leeflang MM, McDonald S, Eisinga A, Mitchell RL, Whiting P, Glanville JM (2013) Search strategies to identify diagnostic accuracy studies in MEDLINE and EMBASE. Cochrane Database Syst Rev (9). https://doi.org/10.1002/14651858.MR000022.pub3
Bolton JE (1971) Small firms—report of the committee of inquiry on small firms (4811). London
Boluyt N, Tjosvold L, Lefebvre C, Klassen TP, Offringa M (2008) Usefulness of systematic review search strategies in finding child health systematic reviews in MEDLINE. Arch Pediatr Adolesc Med 162(2):111–116. https://doi.org/10.1001/archpediatrics.2007.40
Booth A, Noyes J, Flemming K, Gerhardus A, Wahlster P, van der Wilt GJ, Rehfuess E (2018) Structured methodology review identified seven (RETREAT) criteria for selecting qualitative evidence synthesis approaches. J Clinic Epidemiol 99:41–52. https://doi.org/10.1016/j.jclinepi.2018.03.003
Chesbrough H (2012) Open innovation: where we’ve been and where we’re going. Res Technol Manag 55(4):20–27. https://doi.org/10.5437/08956308X5504085
Chesbrough HW (2003) Open innovation: the new imperative for creating and profiting from technology. Harvard Business School Press, Boston
Conn VS, Valentine JC, Cooper HM, Rantz MJ (2003) Grey literature in meta-analyses. Nurs Res 52(4):256–261
de la Torre Díez I, Cosgaya HM, Garcia-Zapirain B, López-Coronado M (2016) Big data in health: a literature review from the year 2005. J Med Syst 40(9):209. https://doi.org/10.1007/s10916-016-0565-7
Dekkers R, Hicks C (2019) How many cases do you need for studies into operations management? Guidance based on saturation. In: Paper presented at the 26th EurOMA conference, Helsinki
Dekkers R, Koukou MI, Mitchell S, Sinclair S (2019) Engaging with open innovation: a Scottish perspective on its opportunities, challenges and risks. J Innov Econ Manag 28(1):193–226. https://doi.org/10.3917/jie.028.0187
Dieste O, Grimán A, Juristo N (2009) Developing search strategies for detecting relevant experiments. Empir Softw Eng 14(5):513–539. https://doi.org/10.1007/s10664-008-9091-7
Eady AM, Wilczynski NL, Haynes RB (2008) PsycINFO search strategies identified methodologically sound therapy studies and review articles for use by clinicians and researchers. J Clin Epidemiol 61(1):34–40. https://doi.org/10.1016/j.jclinepi.2006.09.016
Egger M, Zellweger-Zähner T, Schneider M, Junker C, Lengeler C, Antes G (1997) Language bias in randomised controlled trials published in English and German. The Lancet 350(9074):326–329. https://doi.org/10.1016/S0140-6736(97)02419-7
Eisenhardt KM (1989) Agency theory: an assessment and review. Acad Manag Rev 14(1):57–74. https://doi.org/10.5465/AMR.1989.4279003
Finfgeld-Connett D, Johnson ED (2013) Literature search strategies for conducting knowledge-building and theory-generating qualitative systematic reviews. J Adv Nurs 69(1):194–204. https://doi.org/10.1111/j.1365-2648.2012.06037.x
Frederick JT, Steinman LE, Prohaska T, Satariano WA, Bruce M, Bryant L, Snowden M (2007) Community-based treatment of late life depression: an expert panel-informed literature review. Am J Prev Med 33(3):222–249. https://doi.org/10.1016/j.amepre.2007.04.035
Glanville J, Kaunelis D, Mensinkai S (2009) How well do search filters perform in identifying economic evaluations in MEDLINE and EMBASE. Int J Technol Assess Health Care 25(4):522–529. https://doi.org/10.1017/S0266462309990523
Godin K, Stapleton J, Kirkpatrick SI, Hanning RM, Leatherdale ST (2015) Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Rev 4(1):138. https://doi.org/10.1186/s13643-015-0125-0
Green BN, Johnson CD, Adams A (2006) Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med 5(3):101–117. https://doi.org/10.1016/S0899-3467(07)60142-6
Greenhalgh T, Peacock R (2005) Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 331(7524):1064–1065. https://doi.org/10.1136/bmj.38636.593461.68
Grégoire G, Derderian F, le Lorier J (1995) Selecting the language of the publications included in a meta-analysis: is there a Tower of Babel bias? J Clin Epidemiol 48(1):159–163
Gross T, Taylor AG, Joudrey DN (2015) Still a lot to lose: the role of controlled vocabulary in keyword searching. Catalog Classific Q 53(1):1–39. https://doi.org/10.1080/01639374.2014.917447
Grosso G, Godos J, Galvano F, Giovannucci EL (2017) Coffee, caffeine, and health outcomes: an umbrella review. Annu Rev Nutr 37(1):131–156. https://doi.org/10.1146/annurev-nutr-071816-064941
Gusenbauer M, Haddaway NR (2020) Which academic search systems are suitable for systematic reviews or meta-analyses? Evaluating retrieval qualities of Google Scholar, PubMed, and 26 other resources. Res Synthesis Methods 11(2):181–217. https://doi.org/10.1002/jrsm.1378
Haddaway NR, Bayliss HR (2015) Shades of grey: two forms of grey literature important for reviews in conservation. Biol Cons 191:827–829. https://doi.org/10.1016/j.biocon.2015.08.018
Haddaway NR, Collins AM, Coughlin D, Kirk S (2015) The role of Google Scholar in evidence reviews and its applicability to grey literature searching. PLoS One 10(9):e0138237. https://doi.org/10.1371/journal.pone.0138237
Harari MB, Parola HR, Hartwell CJ, Riegelman A (2020) Literature searches in systematic reviews and meta-analyses: a review, evaluation, and recommendations. J Vocat Behav 118:103377. https://doi.org/10.1016/j.jvb.2020.103377
Harzing A-WK, van der Wal R (2008) Google Scholar as a new source for citation analysis. Ethics Sci Environ Politics 8(1):61–73. https://doi.org/10.3354/esep00076
Hausner E, Guddat C, Hermanns T, Lampert U, Waffenschmidt S (2016) Prospective comparison of search strategies for systematic reviews: an objective approach yielded higher sensitivity than a conceptual one. J Clin Epidemiol 77:118–124. https://doi.org/10.1016/j.jclinepi.2016.05.002
Hausner E, Waffenschmidt S, Kaiser T, Simon M (2012) Routine development of objectively derived search strategies. Syst Rev 1(1):19. https://doi.org/10.1186/2046-4053-1-19
Havill NL, Leeman J, Shaw-Kokot J, Knafl K, Crandell J, Sandelowski M (2014) Managing large-volume literature searches in research synthesis studies. Nurs Outlook 62(2):112–118. https://doi.org/10.1016/j.outlook.2013.11.002
Hildebrand AM, Iansavichus AV, Haynes RB, Wilczynski NL, Mehta RL, Parikh CR, Garg AX (2014) High-performance information search filters for acute kidney injury content in PubMed, Ovid Medline and Embase. Nephrol Dial Transplant 29(4):823–832. https://doi.org/10.1093/ndt/gft531
Hinckeldeyn J, Dekkers R, Kreutzfeldt J (2015) Productivity of product design and engineering processes—unexplored territory for production management techniques? Int J Oper Prod Manag 35(4):458–486. https://doi.org/10.1108/IJOPM-03-2013-0101
Hopewell S, Clarke M, Lefebvre C, Scherer R (2007) Handsearching versus electronic searching to identify reports of randomized trials. Cochrane Database Syst Rev (2):MR000001. https://doi.org/10.1002/14651858.mr000001.pub2
Isckia T, Lescop D (2011) Une analyse critique des fondements de l’innovation ouverte. Rev Fr Gest 210(1):87–98
Jackson JL, Kuriyama A (2019) How often do systematic reviews exclude articles not published in English? J Gen Intern Med 34(8):1388–1389. https://doi.org/10.1007/s11606-019-04976-x
Jennex ME (2015) Literature reviews and the review process: an editor-in-chief’s perspective. Commun Assoc Inf Syst 36:139–146. https://doi.org/10.17705/1CAIS.03608
Jensen MC, Meckling WH (1976) Theory of the firm: managerial behavior, agency costs and ownership structure. J Financ Econ 3(4):305–360. https://doi.org/10.1016/0304-405X(76)90026-X
Jüni P, Holenstein F, Sterne J, Bartlett C, Egger M (2002) Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol 31(1):115–123. https://doi.org/10.1093/ije/31.1.115
Kennedy MM (2007) Defining a literature. Educ Res 36(3):139. https://doi.org/10.3102/0013189x07299197
Koffel JB (2015) Use of recommended search strategies in systematic reviews and the impact of librarian involvement: a cross-sectional survey of recent authors. PLoS One 10(5):e0125931. https://doi.org/10.1371/journal.pone.0125931
Koffel JB, Rethlefsen ML (2016) Reproducibility of search strategies is poor in systematic reviews published in high-impact pediatrics, cardiology and surgery journals: a cross-sectional study. PLoS One 11(9):e0163309. https://doi.org/10.1371/journal.pone.0163309
Lawal AK, Rotter T, Kinsman L, Sari N, Harrison L, Jeffery C, Flynn R (2014) Lean management in health care: definition, concepts, methodology and effects reported (systematic review protocol). Syst Rev 3(1):103. https://doi.org/10.1186/2046-4053-3-103
Levay P, Ainsworth N, Kettle R, Morgan A (2016) Identifying evidence for public health guidance: a comparison of citation searching with Web of Science and Google Scholar. Res Synthesis Methods 7(1):34–45. https://doi.org/10.1002/jrsm.1158
Li L, Smith HE, Atun R, Tudor Car L (2019) Search strategies to identify observational studies in MEDLINE and Embase. Cochrane Database Syst Rev (3). https://doi.org/10.1002/14651858.MR000041.pub2
Linton JD, Thongpapanl NT (2004) Ranking the technology innovation management journals. J Prod Innov Manag 21(2):123–139. https://doi.org/10.1111/j.0737-6782.2004.00062.x
Lokker C, McKibbon KA, Wilczynski NL, Haynes RB, Ciliska D, Dobbins M, Straus SE (2010) Finding knowledge translation articles in CINAHL. Studies Health Technol Inform 160(2):1179–1183
Lu Z (2011) PubMed and beyond: a survey of web tools for searching biomedical literature. Database. https://doi.org/10.1093/database/baq036
MacSuga-Gage AS, Simonsen B (2015) Examining the effects of teacher—directed opportunities to respond on student outcomes: a systematic review of the literature. Educ Treat Child 38(2):211–239. https://doi.org/10.1353/etc.2015.0009
Mahood Q, Van Eerd D, Irvin E (2014) Searching for grey literature for systematic reviews: challenges and benefits. Res Synthesis Methods 5(3):221–234. https://doi.org/10.1002/jrsm.1106
Marangunić N, Granić A (2015) Technology acceptance model: a literature review from 1986 to 2013. Univ Access Inf Soc 14(1):81–95. https://doi.org/10.1007/s10209-014-0348-1
Mc Elhinney H, Taylor B, Sinclair M, Holman MR (2016) Sensitivity and specificity of electronic databases: the example of searching for evidence on child protection issues related to pregnant women. Evid Based Midwifery 14(1):29–34
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C (2016) PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 75:40–46. https://doi.org/10.1016/j.jclinepi.2016.01.021
McManus RJ, Wilson S, Delaney BC, Fitzmaurice DA, Hyde CJ, Tobias S, Hobbs FDR (1998) Review of the usefulness of contacting other experts when conducting a literature search for systematic reviews. Br Med J 317(7172):1562–1563 https://doi.org/10.1136/bmj.317.7172.1562
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi (2014) PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14(1):579. https://doi.org/10.1186/s12913-014-0579-0
Mitnick BM (1973) Fiduciary rationality and public policy: the theory of agency and some consequences. In: Paper presented at the annual meeting of the American political science association, New Orleans, LA
Morrison A, Polisena J, Husereau D, Moulton K, Clark M, Fiander M, Rabb D (2012) The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care 28(2):138–144. https://doi.org/10.1017/S0266462312000086
Neuhaus C, Daniel HD (2008) Data sources for performing citation analysis: an overview. J Document 64(2):193–210. https://doi.org/10.1108/00220410810858010
O’Mara-Eves A, Thomas J, McNaught J, Miwa M, Ananiadou S (2015) Using text mining for study identification in systematic reviews: a systematic review of current approaches. Syst Rev 4(1):5. https://doi.org/10.1186/2046-4053-4-5
Ogilvie D, Foster CE, Rothnie H, Cavill N, Hamilton V, Fitzsimons CF, Mutrie N (2007) Interventions to promote walking: systematic review. BMJ 334(7605):1204. https://doi.org/10.1136/bmj.39198.722720.BE
Onetti A (2019) Turning open innovation into practice: trends in European corporates. J Bus Strateg 42(1):51–58. https://doi.org/10.1108/JBS-07-2019-0138
Papaioannou D, Sutton A, Carroll C, Booth A, Wong R (2010) Literature searching for social science systematic reviews: consideration of a range of search techniques. Health Info Libr J 27(2):114–122. https://doi.org/10.1111/j.1471-1842.2009.00863.x
Pappas C, Williams I (2011) Grey literature: its emerging importance. J Hosp Librariansh 11(3):228–234. https://doi.org/10.1080/15323269.2011.587100
Pearson M, Moxham T, Ashton K (2011) Effectiveness of search strategies for qualitative research about barriers and facilitators of program delivery. Eval Health Prof 34(3):297–308. https://doi.org/10.1177/0163278710388029
Piggott-McKellar AE, McNamara KE, Nunn PD, Watson JEM (2019) What are the barriers to successful community-based climate change adaptation? A review of grey literature. Local Environ 24(4):374–390. https://doi.org/10.1080/13549839.2019.1580688
Piller F, West J (2014) Firms, users, and innovations: an interactive model of coupled innovation. In: Chesbrough HW, Vanhaverbeke W, West J (eds) New frontiers in open innovation. Oxford University Press, Oxford, pp 29–49
Poole R, Kennedy OJ, Roderick P, Fallowfield JA, Hayes PC, Parkes J (2017) Coffee consumption and health: umbrella review of meta-analyses of multiple health outcomes. BMJ 359:j5024. https://doi.org/10.1136/bmj.j5024
Priem RL, Butler JE (2001) Is the resource-based “view” a useful perspective for strategic management research? Acad Manag Rev 26(1):22–40. https://doi.org/10.5465/amr.2001.4011928
Relevo R (2012) Effective search strategies for systematic reviews of medical tests. J Gener Internal Med 27(1):S28–S32. https://doi.org/10.1007/s11606-011-1873-8
Rethlefsen ML, Farrell AM, Osterhaus Trzasko LC, Brigham TJ (2015) Librarian co-authors correlated with higher quality reported search strategies in general internal medicine systematic reviews. J Clin Epidemiol 68(6):617–626. https://doi.org/10.1016/j.jclinepi.2014.11.025
Rewhorn S (2018) Writing your successful literature review. J Geogr High Educ 42(1):143–147. https://doi.org/10.1080/03098265.2017.1337732
Rietjens JA, Bramer WM, Geijteman EC, van der Heide A, Oldenmenger WH (2019) Development and validation of search filters to find articles on palliative care in bibliographic databases. Palliat Med 33(4):470–474. https://doi.org/10.1177/0269216318824275
Rogers M, Bethel A, Abbott R (2018) Locating qualitative studies in dementia on MEDLINE, EMBASE, CINAHL, and PsycINFO: a comparison of search strategies. Res Synthesis Methods 9(4):579–586. https://doi.org/10.1002/jrsm.1280
Rosenstock TS, Lamanna C, Chesterman S, Bell P, Arslan A, Richards M, Zhou W (2016) The scientific basis of climate-smart agriculture: a systematic review protocol. CGIAR, Copenhagen
Ross SA (1973) The economic theory of agency: the principal’s problem. Am Econ Rev 63(2):134–139
Rosumeck S, Wagner M, Wallraf S, Euler U (2020) A validation study revealed differences in design and performance of search filters for qualitative research in PsycINFO and CINAHL. J Clin Epidemiol 128:101–108. https://doi.org/10.1016/j.jclinepi.2020.09.031
Rowley J, Slack F (2004) Conducting a literature review. Manag Res News 27(6):31–39. https://doi.org/10.1108/01409170410784185
Rudestam K, Newton R (1992) Surviving your dissertation: a comprehensive guide to content and process. Sage, London
Salgado EG, Dekkers R (2018) Lean product development: nothing new under the sun? Int J Manag Rev 20(4):903–933. https://doi.org/10.1111/ijmr.12169
Savoie I, Helmer D, Green CJ, Kazanjian A (2003) BEYOND MEDLINE: reducing bias through extended systematic review search. Int J Technol Assess Health Care 19(1):168–178. https://doi.org/10.1017/S0266462303000163
Schlosser RW, Wendt O, Bhavnani S et al (2006) Use of information-seeking strategies for developing systematic reviews and engaging in evidence-based practice: the application of traditional and comprehensive Pearl growing. A review. Int J Language Commun Disorders 41(5):567–582. https://doi.org/10.1080/13682820600742190
Schryen G (2015) Writing qualitative IS literature reviews—guidelines for synthesis, interpretation, and guidance of research. Commun Assoc Inf Syst 34:286–325. https://doi.org/10.17705/1CAIS.03712
Shishank S, Dekkers R (2013) Outsourcing: decision-making methods and criteria during design and engineering. Product Plan Control Manage Oper 24(4–5):318–336. https://doi.org/10.1080/09537287.2011.648544
Silagy CA, Middleton P, Hopewell S (2002) Publishing protocols of systematic reviews comparing what was done to what was planned. JAMA 287(21):2831–2834. https://doi.org/10.1001/jama.287.21.2831
Soldani J, Tamburri DA, Van Den Heuvel W-J (2018) The pains and gains of microservices: a systematic grey literature review. J Syst Softw 146:215–232. https://doi.org/10.1016/j.jss.2018.09.082
Stevinson C, Lawlor DA (2004) Searching multiple databases for systematic reviews: added value or diminishing returns? Complement Ther Med 12(4):228–232. https://doi.org/10.1016/j.ctim.2004.09.003
Swift JK, Wampold BE (2018) Inclusion and exclusion strategies for conducting meta-analyses. Psychother Res 28(3):356–366. https://doi.org/10.1080/10503307.2017.1405169
Swift JK, Callahan JL, Cooper M, Parkin SR (2018) The impact of accommodating client preference in psychotherapy: a meta-analysis. J Clin Psychol 74(11):1924–1937. https://doi.org/10.1002/jclp.22680
Tanon AA, Champagne F, Contandriopoulos A-P, Pomey M-P, Vadeboncoeur A, Nguyen H (2010) Patient safety and systematic reviews: finding papers indexed in MEDLINE, EMBASE and CINAHL. Qual Saf Health Care 19(5):452–461. https://doi.org/10.1136/qshc.2008.031401
Tillett S, Newbold E (2006) Grey literature at the British library: revealing a hidden resource. Interlend Document Supply 34(2):70–73. https://doi.org/10.1108/02641610610669769
Trott P, Hartmann D (2009) Why ‘open innovation’ is old wine in new bottles. Int J Innov Manag 13(4):715–736. https://doi.org/10.1142/S1363919609002509
vom Brocke J, Simons A, Riemer K, Niehaves B, Plattfaut R, Cleven A (2015) Standing on the shoulders of giants: challenges and recommendations of literature search in information systems research. Commun Assoc Inf Syst 37:205–224. https://doi.org/10.17705/1CAIS.03709
Webster J, Watson RT (2002) Analyzing the past to prepare for the future: writing a literature review. MIS Q 26(2):xiii–xxiii
Wellington JJ, Bathmaker A, Hunt C, McCulloch G, Sikes P (2005) Succeeding with your doctorate. Sage, Thousand Oaks
Wilczynski NL, Haynes RB (2007) EMBASE search strategies achieved high sensitivity and specificity for retrieving methodologically sound systematic reviews. J Clin Epidemiol 60(1):29–33. https://doi.org/10.1016/j.jclinepi.2006.04.001
Wilczynski NL, Marks S, Haynes RB (2007) Search strategies for identifying qualitative studies in CINAHL. Qual Health Res 17(5):705–710. https://doi.org/10.1177/1049732306294515
Wohlin C, Prikladnicki R (2013) Systematic literature reviews in software engineering. Inf Softw Technol 55(6):919–920. https://doi.org/10.1016/j.infsof.2013.02.002
Wong SS-L, Wilczynski NL, Haynes RB (2006) Optimal CINAHL search strategies for identifying therapy studies and review articles. J Nurs Scholarsh 38(2):194–199. https://doi.org/10.1111/j.1547-5069.2006.00100.x
Zhang L, Ajiferuke I, Sampson M (2006) Optimizing search strategies to identify randomized controlled trials in MEDLINE. BMC Med Res Methodol 6(1):23. https://doi.org/10.1186/1471-2288-6-23
Download references
Author information
Authors and affiliations.
University of Glasgow, Glasgow, UK
Rob Dekkers
Glasgow Caledonian University, Glasgow, UK
Lindsey Carey
Prof. Peter Langhorne
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Dekkers, R., Carey, L., Langhorne, P. (2022). Search Strategies for [Systematic] Literature Reviews. In: Making Literature Reviews Work: A Multidisciplinary Guide to Systematic Approaches. Springer, Cham. https://doi.org/10.1007/978-3-030-90025-0_5
Download citation
DOI : https://doi.org/10.1007/978-3-030-90025-0_5
Published : 11 August 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-90024-3
Online ISBN : 978-3-030-90025-0
eBook Packages : Education Education (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

Literature Reviews: systematic searching at various levels
- for assignments
- for dissertations / theses
- Search strategy and searching
- Boolean Operators
Search strategy template
- Screening & critiquing
- Citation Searching
- Google Scholar (with Lean Library)
- Resources for literature reviews
- Adding a referencing style to EndNote
- Exporting from different databases
- PRISMA Flow Diagram
- Grey Literature
You can map out your search strategy in whatever way works for you.
Some people like lists and so plan their search strategy out in a grid-box or table format. Some people are more visual and like to draw their strategy out using a mind-map approach (either on paper or using mind-mapping software). Some people use sticky notes or Trello or a spreadsheet.
If it works for you then as long as it enables you to search systematically and thoroughly there's no need to change the way you work.
If your search strategies are not very developed, the method you use doesn't lead to a good search, then consider using one of the other methods to see if changing your approach helps.
- Search Strategy Document
- << Previous: Boolean Operators
- Next: Screening & critiquing >>
- Last Updated: Jun 11, 2024 9:55 AM
- URL: https://libguides.derby.ac.uk/literature-reviews

Literature Review: Developing a search strategy
- Traditional or narrative literature reviews
- Scoping Reviews
- Systematic literature reviews
- Annotated bibliography
- Keeping up to date with literature
- Finding a thesis
- Evaluating sources and critical appraisal of literature
- Managing and analysing your literature
- Further reading and resources
From research question to search strategy
Keeping a record of your search activity
Good search practice could involve keeping a search diary or document detailing your search activities (Phelps et. al. 2007, pp. 128-149), so that you can keep track of effective search terms, or to help others to reproduce your steps and get the same results.
This record could be a document, table or spreadsheet with:
- The names of the sources you search and which provider you accessed them through - eg Medline (Ovid), Web of Science (Thomson Reuters). You should also include any other literature sources you used.
- how you searched (keyword and/or subject headings)
- which search terms you used (which words and phrases)
- any search techniques you employed (truncation, adjacency, etc)
- how you combined your search terms (AND/OR). Check out the Database Help guide for more tips on Boolean Searching.
- The number of search results from each source and each strategy used. This can be the evidence you need to prove a gap in the literature, and confirms the importance of your research question.
| you will be doing a number of searches as your initial search evolves. As your thesis, discussions and argument develops you will search for further evidence and support from the literature. Each search should be included in your search record. |
A search planner may help you to organise you thoughts prior to conducting your search. If you have any problems with organising your thoughts prior, during and after searching please contact your Library Faculty Team for individual help.
- Literature search - a librarian's handout to introduce tools, terms and techniques Created by Elsevier librarian, Katy Kavanagh Web, this document outlines tools, terms and techniques to think about when conducting a literature search.
- Search planner
Literature search cycle

Diagram text description
This diagram illustrates the literature search cycle. It shows a circle in quarters. Top left quarter is identify main concepts with rectangle describing how to do this by identifying:controlled vocabulary terms, synonyms, keywords and spelling. Top right quarter select library resources to search and rectangle describing resources to search library catalogue relevant journal articles and other resource. Bottom right corner of circle search resources and in rectangle consider using boolean searching proximity searching and truncated searching techniques. Bottom left quarter of circle review and refine results. In rectangle evaluate results, rethink keywords and create alerts.
Have a search framework
Search frameworks are mnemonics which can help you focus your research question. They are also useful in helping you to identify the concepts and terms you will use in your literature search.
PICO is a search framework commonly used in the health sciences to focus clinical questions. As an example, you work in an aged care facility and are interested in whether cranberry juice might help reduce the common occurrence of urinary tract infections. The PICO framework would look like this:
| opulation/ atient/ roblem | People living in aged care facilities |
| ntervention | Cranberry juice |
| omparison | No cranberry juice (status quo) |
| utcome | Prevention of UTIs |
Now that the issue has been broken up to its elements, it is easier to turn it into an answerable research question: “Does cranberry juice help reduce urinary tract infections in people living in aged care facilities?”
Other frameworks may be helpful, depending on your question and your field of interest. PICO can be adapted to PICOT (which adds T ime) or PICOS (which adds S tudy design), or PICOC (adding C ontext).
For qualitative questions you could use
- SPIDER : S ample, P henomenon of I nterest, D esign, E valuation, R esearch type
For questions about causes or risk,
- PEO : P opulation, E xposure, O utcomes
For evaluations of interventions or policies,
- SPICE: S etting, P opulation or P erspective, I ntervention, C omparison, E valuation or
- ECLIPSE: E xpectation, C lient group, L ocation, I mpact, P rofessionals, SE rvice
See the University of Notre Dame Australia’s examples of some of these frameworks.
You can also try some PICO examples in the National Library of Medicine's PubMed training site: Using PICO to frame clinical questions.
| If you use the elements of your search framework to combine terms, you may find you have narrowed the search too much and will struggle to find relevant studies. Try using only the most critical elements from the mnemonic for concepts to search. For example, in a PICO search, you would sometimes exclude the O (outcome) terms in your search strategy as the outcomes may come from combining the other terms. If the C (comparison) is the status quo, you wouldn't use those terms either. Try to avoid concepts that have vague or broad meanings, such as benefits or health effects. Ask your for help and advice! |
Contact Your Faculty Team Librarian
Faculty librarians are here to provide assistance to students, researchers and academic staff by providing expert searching advice, research and curriculum support.
- Faculty of Arts & Education team
- Faculty of Business, Justice & Behavioural Science team
- Faculty of Science team
Further reading
- << Previous: Annotated bibliography
- Next: Keeping up to date with literature >>
- Last Updated: Jun 3, 2024 9:25 AM
- URL: https://libguides.csu.edu.au/review

Charles Sturt University is an Australian University, TEQSA Provider Identification: PRV12018. CRICOS Provider: 00005F.
- University of Wisconsin–Madison
- University of Wisconsin-Madison
- Research Guides
- Evidence Synthesis, Systematic Review Services
- Write a Search Strategy
Evidence Synthesis, Systematic Review Services : Write a Search Strategy
- Literature Review Types, Taxonomies
- Develop a Protocol
- Develop Your Research Question
- Select Databases
- Select Gray Literature Sources
- Manage Your Search Process
- Register Your Protocol
- Citation Management
- Article Screening
- Risk of Bias Assessment
- Synthesize, Map, or Describe the Results
- Find Guidance by Discipline
- Manage Your Research Data
- Browse Evidence Portals by Discipline
- Automate the Process, Tools & Technologies
- Additional Resources
Searching Strategies, Search Syntax
While constructing a precise and productive search for the literature will take time and testing (or scoping), here are some useful tips on the mechanics for constructing search expressions that can be interpreted by database search engines. Search terms (keywords), operators, wildcards, and more!
- Be sure to visit the database "Help" files to learn about the special features, operators and wildcard characters that a database may uniquely use.
See also sections 3 and 4 from the CEE Guidelines for Authors. ( Guidelines and Standards for Environmental Synthesis in Environmental Management , Version 5.1, 2022) Section 3: Planning the conduct of an Evidence Synthesis Section 4: Conducting a Search
A few fundamentals and tips:
Make a list of your search terms (keywords) and the alternative, like or similar concepts. You may find it helpful to consult a thesaurus (for example, see NAL's Thesaurus and Glossary )
- As you run a search, review "subject headings" or "descriptors" to identify essential vocabulary.
Use AND to combine search terms; retrieve records with those terms, in any order: friends AND communication
Use OR to combine similar search terms or synonyms: friends OR peers
Use quotation marks ( " ") to search a required phrase: "interpersonal communication"
- Note: In many instances, the adjacency of your search terms may be sufficient to retrieve a phrase. Unless specific phrasing is necessary for meaning (or to assist if retrieving too many erroneous results), enclosing your search phrases within quotation marks may be too limiting.
Use an asterisk ( * ) to retrieve singular and plural forms or suffixes for search terms: friend* = friend, friend s , friend ly or friend ship
- Consult the Help files provided within the database to determine the correct symbol used for this function.
Apply field limits or filters to your results, if necessary (by date, document type, or other).
Using the examples, above, and putting it all together as a simple search expression, you would have: (friend* OR peer*) AND "interpersonal communication"
Tools for Translating Your Search Syntax
- Database Syntax Guide (PDF), Cochrane Effective Practice and Organisation of Care Chart of commonly used syntax (operators, wildcard characters, field codes) and their behavior across several database products.
- Medline Transpose (project) Translate a search expression between Ovid MEDLINE and PubMed.
- Polyglot Search, SR-Accelerator Tool for translating search syntax across several database products.
Why Perform an Exploratory Search
In preparing for your review, you will begin with an exploratory or preliminary search of the literature.
This search will help you:
- Identify existing reviews (so as not to duplicate work),
- Assess the quantity and quality of relevant, primary research studies (so as to be sufficiently abundant and productive for your work), and
- Identify key (benchmark) articles/publications with which to inform your subsequent searching.
Hedges, Search Filters
- ISSG Search Filter Resource (InterTASC Information Specialists' Sub-Group) Collaborative venture to identify, assess and test search filters designed to retrieve research by study design or focus.
- searchRxiv Resource created to support researchers by reporting, storing and sharing their searches to review and re-use.
How to Work with Sensitive Search Terms
- Addressing antiquated, non-standard, exclusionary, and potentially offensive terms in evidence syntheses and systematic searches Suggested wording provided is intended to be a template only, and should be adapted as appropriate for a given topic or project.
- AGROVOC, Multilingual Thesaurus, FAO
- CABI/CAB Thesaurus Stand-alone edition. Thesaurus can also be accessed from within the CAB Abstracts database.
- NAL Thesaurus (National Agricultural Library)
- << Previous: Select Gray Literature Sources
- Next: Manage Your Search Process >>
- Last Updated: May 30, 2024 2:53 PM
- URL: https://researchguides.library.wisc.edu/literature_review
- Open access
- Published: 14 August 2018
Defining the process to literature searching in systematic reviews: a literature review of guidance and supporting studies
- Chris Cooper ORCID: orcid.org/0000-0003-0864-5607 1 ,
- Andrew Booth 2 ,
- Jo Varley-Campbell 1 ,
- Nicky Britten 3 &
- Ruth Garside 4
BMC Medical Research Methodology volume 18 , Article number: 85 ( 2018 ) Cite this article
206k Accesses
205 Citations
117 Altmetric
Metrics details
Systematic literature searching is recognised as a critical component of the systematic review process. It involves a systematic search for studies and aims for a transparent report of study identification, leaving readers clear about what was done to identify studies, and how the findings of the review are situated in the relevant evidence.
Information specialists and review teams appear to work from a shared and tacit model of the literature search process. How this tacit model has developed and evolved is unclear, and it has not been explicitly examined before.
The purpose of this review is to determine if a shared model of the literature searching process can be detected across systematic review guidance documents and, if so, how this process is reported in the guidance and supported by published studies.
A literature review.
Two types of literature were reviewed: guidance and published studies. Nine guidance documents were identified, including: The Cochrane and Campbell Handbooks. Published studies were identified through ‘pearl growing’, citation chasing, a search of PubMed using the systematic review methods filter, and the authors’ topic knowledge.
The relevant sections within each guidance document were then read and re-read, with the aim of determining key methodological stages. Methodological stages were identified and defined. This data was reviewed to identify agreements and areas of unique guidance between guidance documents. Consensus across multiple guidance documents was used to inform selection of ‘key stages’ in the process of literature searching.
Eight key stages were determined relating specifically to literature searching in systematic reviews. They were: who should literature search, aims and purpose of literature searching, preparation, the search strategy, searching databases, supplementary searching, managing references and reporting the search process.
Conclusions
Eight key stages to the process of literature searching in systematic reviews were identified. These key stages are consistently reported in the nine guidance documents, suggesting consensus on the key stages of literature searching, and therefore the process of literature searching as a whole, in systematic reviews. Further research to determine the suitability of using the same process of literature searching for all types of systematic review is indicated.
Peer Review reports
Systematic literature searching is recognised as a critical component of the systematic review process. It involves a systematic search for studies and aims for a transparent report of study identification, leaving review stakeholders clear about what was done to identify studies, and how the findings of the review are situated in the relevant evidence.
Information specialists and review teams appear to work from a shared and tacit model of the literature search process. How this tacit model has developed and evolved is unclear, and it has not been explicitly examined before. This is in contrast to the information science literature, which has developed information processing models as an explicit basis for dialogue and empirical testing. Without an explicit model, research in the process of systematic literature searching will remain immature and potentially uneven, and the development of shared information models will be assumed but never articulated.
One way of developing such a conceptual model is by formally examining the implicit “programme theory” as embodied in key methodological texts. The aim of this review is therefore to determine if a shared model of the literature searching process in systematic reviews can be detected across guidance documents and, if so, how this process is reported and supported.
Identifying guidance
Key texts (henceforth referred to as “guidance”) were identified based upon their accessibility to, and prominence within, United Kingdom systematic reviewing practice. The United Kingdom occupies a prominent position in the science of health information retrieval, as quantified by such objective measures as the authorship of papers, the number of Cochrane groups based in the UK, membership and leadership of groups such as the Cochrane Information Retrieval Methods Group, the HTA-I Information Specialists’ Group and historic association with such centres as the UK Cochrane Centre, the NHS Centre for Reviews and Dissemination, the Centre for Evidence Based Medicine and the National Institute for Clinical Excellence (NICE). Coupled with the linguistic dominance of English within medical and health science and the science of systematic reviews more generally, this offers a justification for a purposive sample that favours UK, European and Australian guidance documents.
Nine guidance documents were identified. These documents provide guidance for different types of reviews, namely: reviews of interventions, reviews of health technologies, reviews of qualitative research studies, reviews of social science topics, and reviews to inform guidance.
Whilst these guidance documents occasionally offer additional guidance on other types of systematic reviews, we have focused on the core and stated aims of these documents as they relate to literature searching. Table 1 sets out: the guidance document, the version audited, their core stated focus, and a bibliographical pointer to the main guidance relating to literature searching.
Once a list of key guidance documents was determined, it was checked by six senior information professionals based in the UK for relevance to current literature searching in systematic reviews.
Identifying supporting studies
In addition to identifying guidance, the authors sought to populate an evidence base of supporting studies (henceforth referred to as “studies”) that contribute to existing search practice. Studies were first identified by the authors from their knowledge on this topic area and, subsequently, through systematic citation chasing key studies (‘pearls’ [ 1 ]) located within each key stage of the search process. These studies are identified in Additional file 1 : Appendix Table 1. Citation chasing was conducted by analysing the bibliography of references for each study (backwards citation chasing) and through Google Scholar (forward citation chasing). A search of PubMed using the systematic review methods filter was undertaken in August 2017 (see Additional file 1 ). The search terms used were: (literature search*[Title/Abstract]) AND sysrev_methods[sb] and 586 results were returned. These results were sifted for relevance to the key stages in Fig. 1 by CC.
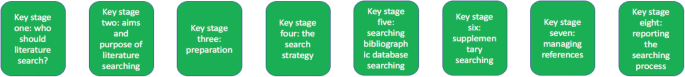
The key stages of literature search guidance as identified from nine key texts
Extracting the data
To reveal the implicit process of literature searching within each guidance document, the relevant sections (chapters) on literature searching were read and re-read, with the aim of determining key methodological stages. We defined a key methodological stage as a distinct step in the overall process for which specific guidance is reported, and action is taken, that collectively would result in a completed literature search.
The chapter or section sub-heading for each methodological stage was extracted into a table using the exact language as reported in each guidance document. The lead author (CC) then read and re-read these data, and the paragraphs of the document to which the headings referred, summarising section details. This table was then reviewed, using comparison and contrast to identify agreements and areas of unique guidance. Consensus across multiple guidelines was used to inform selection of ‘key stages’ in the process of literature searching.
Having determined the key stages to literature searching, we then read and re-read the sections relating to literature searching again, extracting specific detail relating to the methodological process of literature searching within each key stage. Again, the guidance was then read and re-read, first on a document-by-document-basis and, secondly, across all the documents above, to identify both commonalities and areas of unique guidance.
Results and discussion
Our findings.
We were able to identify consensus across the guidance on literature searching for systematic reviews suggesting a shared implicit model within the information retrieval community. Whilst the structure of the guidance varies between documents, the same key stages are reported, even where the core focus of each document is different. We were able to identify specific areas of unique guidance, where a document reported guidance not summarised in other documents, together with areas of consensus across guidance.
Unique guidance
Only one document provided guidance on the topic of when to stop searching [ 2 ]. This guidance from 2005 anticipates a topic of increasing importance with the current interest in time-limited (i.e. “rapid”) reviews. Quality assurance (or peer review) of literature searches was only covered in two guidance documents [ 3 , 4 ]. This topic has emerged as increasingly important as indicated by the development of the PRESS instrument [ 5 ]. Text mining was discussed in four guidance documents [ 4 , 6 , 7 , 8 ] where the automation of some manual review work may offer efficiencies in literature searching [ 8 ].
Agreement between guidance: Defining the key stages of literature searching
Where there was agreement on the process, we determined that this constituted a key stage in the process of literature searching to inform systematic reviews.
From the guidance, we determined eight key stages that relate specifically to literature searching in systematic reviews. These are summarised at Fig. 1 . The data extraction table to inform Fig. 1 is reported in Table 2 . Table 2 reports the areas of common agreement and it demonstrates that the language used to describe key stages and processes varies significantly between guidance documents.
For each key stage, we set out the specific guidance, followed by discussion on how this guidance is situated within the wider literature.
Key stage one: Deciding who should undertake the literature search
The guidance.
Eight documents provided guidance on who should undertake literature searching in systematic reviews [ 2 , 4 , 6 , 7 , 8 , 9 , 10 , 11 ]. The guidance affirms that people with relevant expertise of literature searching should ‘ideally’ be included within the review team [ 6 ]. Information specialists (or information scientists), librarians or trial search co-ordinators (TSCs) are indicated as appropriate researchers in six guidance documents [ 2 , 7 , 8 , 9 , 10 , 11 ].
How the guidance corresponds to the published studies
The guidance is consistent with studies that call for the involvement of information specialists and librarians in systematic reviews [ 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 ] and which demonstrate how their training as ‘expert searchers’ and ‘analysers and organisers of data’ can be put to good use [ 13 ] in a variety of roles [ 12 , 16 , 20 , 21 , 24 , 25 , 26 ]. These arguments make sense in the context of the aims and purposes of literature searching in systematic reviews, explored below. The need for ‘thorough’ and ‘replicable’ literature searches was fundamental to the guidance and recurs in key stage two. Studies have found poor reporting, and a lack of replicable literature searches, to be a weakness in systematic reviews [ 17 , 18 , 27 , 28 ] and they argue that involvement of information specialists/ librarians would be associated with better reporting and better quality literature searching. Indeed, Meert et al. [ 29 ] demonstrated that involving a librarian as a co-author to a systematic review correlated with a higher score in the literature searching component of a systematic review [ 29 ]. As ‘new styles’ of rapid and scoping reviews emerge, where decisions on how to search are more iterative and creative, a clear role is made here too [ 30 ].
Knowing where to search for studies was noted as important in the guidance, with no agreement as to the appropriate number of databases to be searched [ 2 , 6 ]. Database (and resource selection more broadly) is acknowledged as a relevant key skill of information specialists and librarians [ 12 , 15 , 16 , 31 ].
Whilst arguments for including information specialists and librarians in the process of systematic review might be considered self-evident, Koffel and Rethlefsen [ 31 ] have questioned if the necessary involvement is actually happening [ 31 ].
Key stage two: Determining the aim and purpose of a literature search
The aim: Five of the nine guidance documents use adjectives such as ‘thorough’, ‘comprehensive’, ‘transparent’ and ‘reproducible’ to define the aim of literature searching [ 6 , 7 , 8 , 9 , 10 ]. Analogous phrases were present in a further three guidance documents, namely: ‘to identify the best available evidence’ [ 4 ] or ‘the aim of the literature search is not to retrieve everything. It is to retrieve everything of relevance’ [ 2 ] or ‘A systematic literature search aims to identify all publications relevant to the particular research question’ [ 3 ]. The Joanna Briggs Institute reviewers’ manual was the only guidance document where a clear statement on the aim of literature searching could not be identified. The purpose of literature searching was defined in three guidance documents, namely to minimise bias in the resultant review [ 6 , 8 , 10 ]. Accordingly, eight of nine documents clearly asserted that thorough and comprehensive literature searches are required as a potential mechanism for minimising bias.
The need for thorough and comprehensive literature searches appears as uniform within the eight guidance documents that describe approaches to literature searching in systematic reviews of effectiveness. Reviews of effectiveness (of intervention or cost), accuracy and prognosis, require thorough and comprehensive literature searches to transparently produce a reliable estimate of intervention effect. The belief that all relevant studies have been ‘comprehensively’ identified, and that this process has been ‘transparently’ reported, increases confidence in the estimate of effect and the conclusions that can be drawn [ 32 ]. The supporting literature exploring the need for comprehensive literature searches focuses almost exclusively on reviews of intervention effectiveness and meta-analysis. Different ‘styles’ of review may have different standards however; the alternative, offered by purposive sampling, has been suggested in the specific context of qualitative evidence syntheses [ 33 ].
What is a comprehensive literature search?
Whilst the guidance calls for thorough and comprehensive literature searches, it lacks clarity on what constitutes a thorough and comprehensive literature search, beyond the implication that all of the literature search methods in Table 2 should be used to identify studies. Egger et al. [ 34 ], in an empirical study evaluating the importance of comprehensive literature searches for trials in systematic reviews, defined a comprehensive search for trials as:
a search not restricted to English language;
where Cochrane CENTRAL or at least two other electronic databases had been searched (such as MEDLINE or EMBASE); and
at least one of the following search methods has been used to identify unpublished trials: searches for (I) conference abstracts, (ii) theses, (iii) trials registers; and (iv) contacts with experts in the field [ 34 ].
Tricco et al. (2008) used a similar threshold of bibliographic database searching AND a supplementary search method in a review when examining the risk of bias in systematic reviews. Their criteria were: one database (limited using the Cochrane Highly Sensitive Search Strategy (HSSS)) and handsearching [ 35 ].
Together with the guidance, this would suggest that comprehensive literature searching requires the use of BOTH bibliographic database searching AND supplementary search methods.
Comprehensiveness in literature searching, in the sense of how much searching should be undertaken, remains unclear. Egger et al. recommend that ‘investigators should consider the type of literature search and degree of comprehension that is appropriate for the review in question, taking into account budget and time constraints’ [ 34 ]. This view tallies with the Cochrane Handbook, which stipulates clearly, that study identification should be undertaken ‘within resource limits’ [ 9 ]. This would suggest that the limitations to comprehension are recognised but it raises questions on how this is decided and reported [ 36 ].
What is the point of comprehensive literature searching?
The purpose of thorough and comprehensive literature searches is to avoid missing key studies and to minimize bias [ 6 , 8 , 10 , 34 , 37 , 38 , 39 ] since a systematic review based only on published (or easily accessible) studies may have an exaggerated effect size [ 35 ]. Felson (1992) sets out potential biases that could affect the estimate of effect in a meta-analysis [ 40 ] and Tricco et al. summarize the evidence concerning bias and confounding in systematic reviews [ 35 ]. Egger et al. point to non-publication of studies, publication bias, language bias and MEDLINE bias, as key biases [ 34 , 35 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ]. Comprehensive searches are not the sole factor to mitigate these biases but their contribution is thought to be significant [ 2 , 32 , 34 ]. Fehrmann (2011) suggests that ‘the search process being described in detail’ and that, where standard comprehensive search techniques have been applied, increases confidence in the search results [ 32 ].
Does comprehensive literature searching work?
Egger et al., and other study authors, have demonstrated a change in the estimate of intervention effectiveness where relevant studies were excluded from meta-analysis [ 34 , 47 ]. This would suggest that missing studies in literature searching alters the reliability of effectiveness estimates. This is an argument for comprehensive literature searching. Conversely, Egger et al. found that ‘comprehensive’ searches still missed studies and that comprehensive searches could, in fact, introduce bias into a review rather than preventing it, through the identification of low quality studies then being included in the meta-analysis [ 34 ]. Studies query if identifying and including low quality or grey literature studies changes the estimate of effect [ 43 , 48 ] and question if time is better invested updating systematic reviews rather than searching for unpublished studies [ 49 ], or mapping studies for review as opposed to aiming for high sensitivity in literature searching [ 50 ].
Aim and purpose beyond reviews of effectiveness
The need for comprehensive literature searches is less certain in reviews of qualitative studies, and for reviews where a comprehensive identification of studies is difficult to achieve (for example, in Public health) [ 33 , 51 , 52 , 53 , 54 , 55 ]. Literature searching for qualitative studies, and in public health topics, typically generates a greater number of studies to sift than in reviews of effectiveness [ 39 ] and demonstrating the ‘value’ of studies identified or missed is harder [ 56 ], since the study data do not typically support meta-analysis. Nussbaumer-Streit et al. (2016) have registered a review protocol to assess whether abbreviated literature searches (as opposed to comprehensive literature searches) has an impact on conclusions across multiple bodies of evidence, not only on effect estimates [ 57 ] which may develop this understanding. It may be that decision makers and users of systematic reviews are willing to trade the certainty from a comprehensive literature search and systematic review in exchange for different approaches to evidence synthesis [ 58 ], and that comprehensive literature searches are not necessarily a marker of literature search quality, as previously thought [ 36 ]. Different approaches to literature searching [ 37 , 38 , 59 , 60 , 61 , 62 ] and developing the concept of when to stop searching are important areas for further study [ 36 , 59 ].
The study by Nussbaumer-Streit et al. has been published since the submission of this literature review [ 63 ]. Nussbaumer-Streit et al. (2018) conclude that abbreviated literature searches are viable options for rapid evidence syntheses, if decision-makers are willing to trade the certainty from a comprehensive literature search and systematic review, but that decision-making which demands detailed scrutiny should still be based on comprehensive literature searches [ 63 ].
Key stage three: Preparing for the literature search
Six documents provided guidance on preparing for a literature search [ 2 , 3 , 6 , 7 , 9 , 10 ]. The Cochrane Handbook clearly stated that Cochrane authors (i.e. researchers) should seek advice from a trial search co-ordinator (i.e. a person with specific skills in literature searching) ‘before’ starting a literature search [ 9 ].
Two key tasks were perceptible in preparing for a literature searching [ 2 , 6 , 7 , 10 , 11 ]. First, to determine if there are any existing or on-going reviews, or if a new review is justified [ 6 , 11 ]; and, secondly, to develop an initial literature search strategy to estimate the volume of relevant literature (and quality of a small sample of relevant studies [ 10 ]) and indicate the resources required for literature searching and the review of the studies that follows [ 7 , 10 ].
Three documents summarised guidance on where to search to determine if a new review was justified [ 2 , 6 , 11 ]. These focused on searching databases of systematic reviews (The Cochrane Database of Systematic Reviews (CDSR) and the Database of Abstracts of Reviews of Effects (DARE)), institutional registries (including PROSPERO), and MEDLINE [ 6 , 11 ]. It is worth noting, however, that as of 2015, DARE (and NHS EEDs) are no longer being updated and so the relevance of this (these) resource(s) will diminish over-time [ 64 ]. One guidance document, ‘Systematic reviews in the Social Sciences’, noted, however, that databases are not the only source of information and unpublished reports, conference proceeding and grey literature may also be required, depending on the nature of the review question [ 2 ].
Two documents reported clearly that this preparation (or ‘scoping’) exercise should be undertaken before the actual search strategy is developed [ 7 , 10 ]).
The guidance offers the best available source on preparing the literature search with the published studies not typically reporting how their scoping informed the development of their search strategies nor how their search approaches were developed. Text mining has been proposed as a technique to develop search strategies in the scoping stages of a review although this work is still exploratory [ 65 ]. ‘Clustering documents’ and word frequency analysis have also been tested to identify search terms and studies for review [ 66 , 67 ]. Preparing for literature searches and scoping constitutes an area for future research.
Key stage four: Designing the search strategy
The Population, Intervention, Comparator, Outcome (PICO) structure was the commonly reported structure promoted to design a literature search strategy. Five documents suggested that the eligibility criteria or review question will determine which concepts of PICO will be populated to develop the search strategy [ 1 , 4 , 7 , 8 , 9 ]. The NICE handbook promoted multiple structures, namely PICO, SPICE (Setting, Perspective, Intervention, Comparison, Evaluation) and multi-stranded approaches [ 4 ].
With the exclusion of The Joanna Briggs Institute reviewers’ manual, the guidance offered detail on selecting key search terms, synonyms, Boolean language, selecting database indexing terms and combining search terms. The CEE handbook suggested that ‘search terms may be compiled with the help of the commissioning organisation and stakeholders’ [ 10 ].
The use of limits, such as language or date limits, were discussed in all documents [ 2 , 3 , 4 , 6 , 7 , 8 , 9 , 10 , 11 ].
Search strategy structure
The guidance typically relates to reviews of intervention effectiveness so PICO – with its focus on intervention and comparator - is the dominant model used to structure literature search strategies [ 68 ]. PICOs – where the S denotes study design - is also commonly used in effectiveness reviews [ 6 , 68 ]. As the NICE handbook notes, alternative models to structure literature search strategies have been developed and tested. Booth provides an overview on formulating questions for evidence based practice [ 69 ] and has developed a number of alternatives to the PICO structure, namely: BeHEMoTh (Behaviour of interest; Health context; Exclusions; Models or Theories) for use when systematically identifying theory [ 55 ]; SPICE (Setting, Perspective, Intervention, Comparison, Evaluation) for identification of social science and evaluation studies [ 69 ] and, working with Cooke and colleagues, SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type) [ 70 ]. SPIDER has been compared to PICO and PICOs in a study by Methley et al. [ 68 ].
The NICE handbook also suggests the use of multi-stranded approaches to developing literature search strategies [ 4 ]. Glanville developed this idea in a study by Whitting et al. [ 71 ] and a worked example of this approach is included in the development of a search filter by Cooper et al. [ 72 ].
Writing search strategies: Conceptual and objective approaches
Hausner et al. [ 73 ] provide guidance on writing literature search strategies, delineating between conceptually and objectively derived approaches. The conceptual approach, advocated by and explained in the guidance documents, relies on the expertise of the literature searcher to identify key search terms and then develop key terms to include synonyms and controlled syntax. Hausner and colleagues set out the objective approach [ 73 ] and describe what may be done to validate it [ 74 ].
The use of limits
The guidance documents offer direction on the use of limits within a literature search. Limits can be used to focus literature searching to specific study designs or by other markers (such as by date) which limits the number of studies returned by a literature search. The use of limits should be described and the implications explored [ 34 ] since limiting literature searching can introduce bias (explored above). Craven et al. have suggested the use of a supporting narrative to explain decisions made in the process of developing literature searches and this advice would usefully capture decisions on the use of search limits [ 75 ].
Key stage five: Determining the process of literature searching and deciding where to search (bibliographic database searching)
Table 2 summarises the process of literature searching as reported in each guidance document. Searching bibliographic databases was consistently reported as the ‘first step’ to literature searching in all nine guidance documents.
Three documents reported specific guidance on where to search, in each case specific to the type of review their guidance informed, and as a minimum requirement [ 4 , 9 , 11 ]. Seven of the key guidance documents suggest that the selection of bibliographic databases depends on the topic of review [ 2 , 3 , 4 , 6 , 7 , 8 , 10 ], with two documents noting the absence of an agreed standard on what constitutes an acceptable number of databases searched [ 2 , 6 ].
The guidance documents summarise ‘how to’ search bibliographic databases in detail and this guidance is further contextualised above in terms of developing the search strategy. The documents provide guidance of selecting bibliographic databases, in some cases stating acceptable minima (i.e. The Cochrane Handbook states Cochrane CENTRAL, MEDLINE and EMBASE), and in other cases simply listing bibliographic database available to search. Studies have explored the value in searching specific bibliographic databases, with Wright et al. (2015) noting the contribution of CINAHL in identifying qualitative studies [ 76 ], Beckles et al. (2013) questioning the contribution of CINAHL to identifying clinical studies for guideline development [ 77 ], and Cooper et al. (2015) exploring the role of UK-focused bibliographic databases to identify UK-relevant studies [ 78 ]. The host of the database (e.g. OVID or ProQuest) has been shown to alter the search returns offered. Younger and Boddy [ 79 ] report differing search returns from the same database (AMED) but where the ‘host’ was different [ 79 ].
The average number of bibliographic database searched in systematic reviews has risen in the period 1994–2014 (from 1 to 4) [ 80 ] but there remains (as attested to by the guidance) no consensus on what constitutes an acceptable number of databases searched [ 48 ]. This is perhaps because thinking about the number of databases searched is the wrong question, researchers should be focused on which databases were searched and why, and which databases were not searched and why. The discussion should re-orientate to the differential value of sources but researchers need to think about how to report this in studies to allow findings to be generalised. Bethel (2017) has proposed ‘search summaries’, completed by the literature searcher, to record where included studies were identified, whether from database (and which databases specifically) or supplementary search methods [ 81 ]. Search summaries document both yield and accuracy of searches, which could prospectively inform resource use and decisions to search or not to search specific databases in topic areas. The prospective use of such data presupposes, however, that past searches are a potential predictor of future search performance (i.e. that each topic is to be considered representative and not unique). In offering a body of practice, this data would be of greater practicable use than current studies which are considered as little more than individual case studies [ 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 ].
When to database search is another question posed in the literature. Beyer et al. [ 91 ] report that databases can be prioritised for literature searching which, whilst not addressing the question of which databases to search, may at least bring clarity as to which databases to search first [ 91 ]. Paradoxically, this links to studies that suggest PubMed should be searched in addition to MEDLINE (OVID interface) since this improves the currency of systematic reviews [ 92 , 93 ]. Cooper et al. (2017) have tested the idea of database searching not as a primary search method (as suggested in the guidance) but as a supplementary search method in order to manage the volume of studies identified for an environmental effectiveness systematic review. Their case study compared the effectiveness of database searching versus a protocol using supplementary search methods and found that the latter identified more relevant studies for review than searching bibliographic databases [ 94 ].
Key stage six: Determining the process of literature searching and deciding where to search (supplementary search methods)
Table 2 also summaries the process of literature searching which follows bibliographic database searching. As Table 2 sets out, guidance that supplementary literature search methods should be used in systematic reviews recurs across documents, but the order in which these methods are used, and the extent to which they are used, varies. We noted inconsistency in the labelling of supplementary search methods between guidance documents.
Rather than focus on the guidance on how to use the methods (which has been summarised in a recent review [ 95 ]), we focus on the aim or purpose of supplementary search methods.
The Cochrane Handbook reported that ‘efforts’ to identify unpublished studies should be made [ 9 ]. Four guidance documents [ 2 , 3 , 6 , 9 ] acknowledged that searching beyond bibliographic databases was necessary since ‘databases are not the only source of literature’ [ 2 ]. Only one document reported any guidance on determining when to use supplementary methods. The IQWiG handbook reported that the use of handsearching (in their example) could be determined on a ‘case-by-case basis’ which implies that the use of these methods is optional rather than mandatory. This is in contrast to the guidance (above) on bibliographic database searching.
The issue for supplementary search methods is similar in many ways to the issue of searching bibliographic databases: demonstrating value. The purpose and contribution of supplementary search methods in systematic reviews is increasingly acknowledged [ 37 , 61 , 62 , 96 , 97 , 98 , 99 , 100 , 101 ] but understanding the value of the search methods to identify studies and data is unclear. In a recently published review, Cooper et al. (2017) reviewed the literature on supplementary search methods looking to determine the advantages, disadvantages and resource implications of using supplementary search methods [ 95 ]. This review also summarises the key guidance and empirical studies and seeks to address the question on when to use these search methods and when not to [ 95 ]. The guidance is limited in this regard and, as Table 2 demonstrates, offers conflicting advice on the order of searching, and the extent to which these search methods should be used in systematic reviews.
Key stage seven: Managing the references
Five of the documents provided guidance on managing references, for example downloading, de-duplicating and managing the output of literature searches [ 2 , 4 , 6 , 8 , 10 ]. This guidance typically itemised available bibliographic management tools rather than offering guidance on how to use them specifically [ 2 , 4 , 6 , 8 ]. The CEE handbook provided guidance on importing data where no direct export option is available (e.g. web-searching) [ 10 ].
The literature on using bibliographic management tools is not large relative to the number of ‘how to’ videos on platforms such as YouTube (see for example [ 102 ]). These YouTube videos confirm the overall lack of ‘how to’ guidance identified in this study and offer useful instruction on managing references. Bramer et al. set out methods for de-duplicating data and reviewing references in Endnote [ 103 , 104 ] and Gall tests the direct search function within Endnote to access databases such as PubMed, finding a number of limitations [ 105 ]. Coar et al. and Ahmed et al. consider the role of the free-source tool, Zotero [ 106 , 107 ]. Managing references is a key administrative function in the process of review particularly for documenting searches in PRISMA guidance.
Key stage eight: Documenting the search
The Cochrane Handbook was the only guidance document to recommend a specific reporting guideline: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 9 ]. Six documents provided guidance on reporting the process of literature searching with specific criteria to report [ 3 , 4 , 6 , 8 , 9 , 10 ]. There was consensus on reporting: the databases searched (and the host searched by), the search strategies used, and any use of limits (e.g. date, language, search filters (The CRD handbook called for these limits to be justified [ 6 ])). Three guidance documents reported that the number of studies identified should be recorded [ 3 , 6 , 10 ]. The number of duplicates identified [ 10 ], the screening decisions [ 3 ], a comprehensive list of grey literature sources searched (and full detail for other supplementary search methods) [ 8 ], and an annotation of search terms tested but not used [ 4 ] were identified as unique items in four documents.
The Cochrane Handbook was the only guidance document to note that the full search strategies for each database should be included in the Additional file 1 of the review [ 9 ].
All guidance documents should ultimately deliver completed systematic reviews that fulfil the requirements of the PRISMA reporting guidelines [ 108 ]. The guidance broadly requires the reporting of data that corresponds with the requirements of the PRISMA statement although documents typically ask for diverse and additional items [ 108 ]. In 2008, Sampson et al. observed a lack of consensus on reporting search methods in systematic reviews [ 109 ] and this remains the case as of 2017, as evidenced in the guidance documents, and in spite of the publication of the PRISMA guidelines in 2009 [ 110 ]. It is unclear why the collective guidance does not more explicitly endorse adherence to the PRISMA guidance.
Reporting of literature searching is a key area in systematic reviews since it sets out clearly what was done and how the conclusions of the review can be believed [ 52 , 109 ]. Despite strong endorsement in the guidance documents, specifically supported in PRISMA guidance, and other related reporting standards too (such as ENTREQ for qualitative evidence synthesis, STROBE for reviews of observational studies), authors still highlight the prevalence of poor standards of literature search reporting [ 31 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 ]. To explore issues experienced by authors in reporting literature searches, and look at uptake of PRISMA, Radar et al. [ 120 ] surveyed over 260 review authors to determine common problems and their work summaries the practical aspects of reporting literature searching [ 120 ]. Atkinson et al. [ 121 ] have also analysed reporting standards for literature searching, summarising recommendations and gaps for reporting search strategies [ 121 ].
One area that is less well covered by the guidance, but nevertheless appears in this literature, is the quality appraisal or peer review of literature search strategies. The PRESS checklist is the most prominent and it aims to develop evidence-based guidelines to peer review of electronic search strategies [ 5 , 122 , 123 ]. A corresponding guideline for documentation of supplementary search methods does not yet exist although this idea is currently being explored.
How the reporting of the literature searching process corresponds to critical appraisal tools is an area for further research. In the survey undertaken by Radar et al. (2014), 86% of survey respondents (153/178) identified a need for further guidance on what aspects of the literature search process to report [ 120 ]. The PRISMA statement offers a brief summary of what to report but little practical guidance on how to report it [ 108 ]. Critical appraisal tools for systematic reviews, such as AMSTAR 2 (Shea et al. [ 124 ]) and ROBIS (Whiting et al. [ 125 ]), can usefully be read alongside PRISMA guidance, since they offer greater detail on how the reporting of the literature search will be appraised and, therefore, they offer a proxy on what to report [ 124 , 125 ]. Further research in the form of a study which undertakes a comparison between PRISMA and quality appraisal checklists for systematic reviews would seem to begin addressing the call, identified by Radar et al., for further guidance on what to report [ 120 ].
Limitations
Other handbooks exist.
A potential limitation of this literature review is the focus on guidance produced in Europe (the UK specifically) and Australia. We justify the decision for our selection of the nine guidance documents reviewed in this literature review in section “ Identifying guidance ”. In brief, these nine guidance documents were selected as the most relevant health care guidance that inform UK systematic reviewing practice, given that the UK occupies a prominent position in the science of health information retrieval. We acknowledge the existence of other guidance documents, such as those from North America (e.g. the Agency for Healthcare Research and Quality (AHRQ) [ 126 ], The Institute of Medicine [ 127 ] and the guidance and resources produced by the Canadian Agency for Drugs and Technologies in Health (CADTH) [ 128 ]). We comment further on this directly below.
The handbooks are potentially linked to one another
What is not clear is the extent to which the guidance documents inter-relate or provide guidance uniquely. The Cochrane Handbook, first published in 1994, is notably a key source of reference in guidance and systematic reviews beyond Cochrane reviews. It is not clear to what extent broadening the sample of guidance handbooks to include North American handbooks, and guidance handbooks from other relevant countries too, would alter the findings of this literature review or develop further support for the process model. Since we cannot be clear, we raise this as a potential limitation of this literature review. On our initial review of a sample of North American, and other, guidance documents (before selecting the guidance documents considered in this review), however, we do not consider that the inclusion of these further handbooks would alter significantly the findings of this literature review.
This is a literature review
A further limitation of this review was that the review of published studies is not a systematic review of the evidence for each key stage. It is possible that other relevant studies could help contribute to the exploration and development of the key stages identified in this review.
This literature review would appear to demonstrate the existence of a shared model of the literature searching process in systematic reviews. We call this model ‘the conventional approach’, since it appears to be common convention in nine different guidance documents.
The findings reported above reveal eight key stages in the process of literature searching for systematic reviews. These key stages are consistently reported in the nine guidance documents which suggests consensus on the key stages of literature searching, and therefore the process of literature searching as a whole, in systematic reviews.
In Table 2 , we demonstrate consensus regarding the application of literature search methods. All guidance documents distinguish between primary and supplementary search methods. Bibliographic database searching is consistently the first method of literature searching referenced in each guidance document. Whilst the guidance uniformly supports the use of supplementary search methods, there is little evidence for a consistent process with diverse guidance across documents. This may reflect differences in the core focus across each document, linked to differences in identifying effectiveness studies or qualitative studies, for instance.
Eight of the nine guidance documents reported on the aims of literature searching. The shared understanding was that literature searching should be thorough and comprehensive in its aim and that this process should be reported transparently so that that it could be reproduced. Whilst only three documents explicitly link this understanding to minimising bias, it is clear that comprehensive literature searching is implicitly linked to ‘not missing relevant studies’ which is approximately the same point.
Defining the key stages in this review helps categorise the scholarship available, and it prioritises areas for development or further study. The supporting studies on preparing for literature searching (key stage three, ‘preparation’) were, for example, comparatively few, and yet this key stage represents a decisive moment in literature searching for systematic reviews. It is where search strategy structure is determined, search terms are chosen or discarded, and the resources to be searched are selected. Information specialists, librarians and researchers, are well placed to develop these and other areas within the key stages we identify.
This review calls for further research to determine the suitability of using the conventional approach. The publication dates of the guidance documents which underpin the conventional approach may raise questions as to whether the process which they each report remains valid for current systematic literature searching. In addition, it may be useful to test whether it is desirable to use the same process model of literature searching for qualitative evidence synthesis as that for reviews of intervention effectiveness, which this literature review demonstrates is presently recommended best practice.
Abbreviations
Behaviour of interest; Health context; Exclusions; Models or Theories
Cochrane Database of Systematic Reviews
The Cochrane Central Register of Controlled Trials
Database of Abstracts of Reviews of Effects
Enhancing transparency in reporting the synthesis of qualitative research
Institute for Quality and Efficiency in Healthcare
National Institute for Clinical Excellence
Population, Intervention, Comparator, Outcome
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Setting, Perspective, Intervention, Comparison, Evaluation
Sample, Phenomenon of Interest, Design, Evaluation, Research type
STrengthening the Reporting of OBservational studies in Epidemiology
Trial Search Co-ordinators
Booth A. Unpacking your literature search toolbox: on search styles and tactics. Health Information & Libraries Journal. 2008;25(4):313–7.
Article Google Scholar
Petticrew M, Roberts H. Systematic reviews in the social sciences: a practical guide. Oxford: Blackwell Publishing Ltd; 2006.
Book Google Scholar
Institute for Quality and Efficiency in Health Care (IQWiG). IQWiG Methods Resources. 7 Information retrieval 2014 [Available from: https://www.ncbi.nlm.nih.gov/books/NBK385787/ .
NICE: National Institute for Health and Care Excellence. Developing NICE guidelines: the manual 2014. Available from: https://www.nice.org.uk/media/default/about/what-we-do/our-programmes/developing-nice-guidelines-the-manual.pdf .
Sampson M. MJ, Lefebvre C, Moher D, Grimshaw J. Peer Review of Electronic Search Strategies: PRESS; 2008.
Google Scholar
Centre for Reviews & Dissemination. Systematic reviews – CRD’s guidance for undertaking reviews in healthcare. York: Centre for Reviews and Dissemination, University of York; 2009.
eunetha: European Network for Health Technology Assesment Process of information retrieval for systematic reviews and health technology assessments on clinical effectiveness 2016. Available from: http://www.eunethta.eu/sites/default/files/Guideline_Information_Retrieval_V1-1.pdf .
Kugley SWA, Thomas J, Mahood Q, Jørgensen AMK, Hammerstrøm K, Sathe N. Searching for studies: a guide to information retrieval for Campbell systematic reviews. Oslo: Campbell Collaboration. 2017; Available from: https://www.campbellcollaboration.org/library/searching-for-studies-information-retrieval-guide-campbell-reviews.html
Lefebvre C, Manheimer E, Glanville J. Chapter 6: searching for studies. In: JPT H, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions; 2011.
Collaboration for Environmental Evidence. Guidelines for Systematic Review and Evidence Synthesis in Environmental Management.: Environmental Evidence:; 2013. Available from: http://www.environmentalevidence.org/wp-content/uploads/2017/01/Review-guidelines-version-4.2-final-update.pdf .
The Joanna Briggs Institute. Joanna Briggs institute reviewers’ manual. 2014th ed: the Joanna Briggs institute; 2014. Available from: https://joannabriggs.org/assets/docs/sumari/ReviewersManual-2014.pdf
Beverley CA, Booth A, Bath PA. The role of the information specialist in the systematic review process: a health information case study. Health Inf Libr J. 2003;20(2):65–74.
Article CAS Google Scholar
Harris MR. The librarian's roles in the systematic review process: a case study. Journal of the Medical Library Association. 2005;93(1):81–7.
PubMed PubMed Central Google Scholar
Egger JB. Use of recommended search strategies in systematic reviews and the impact of librarian involvement: a cross-sectional survey of recent authors. PLoS One. 2015;10(5):e0125931.
Li L, Tian J, Tian H, Moher D, Liang F, Jiang T, et al. Network meta-analyses could be improved by searching more sources and by involving a librarian. J Clin Epidemiol. 2014;67(9):1001–7.
Article PubMed Google Scholar
McGowan J, Sampson M. Systematic reviews need systematic searchers. J Med Libr Assoc. 2005;93(1):74–80.
Rethlefsen ML, Farrell AM, Osterhaus Trzasko LC, Brigham TJ. Librarian co-authors correlated with higher quality reported search strategies in general internal medicine systematic reviews. J Clin Epidemiol. 2015;68(6):617–26.
Weller AC. Mounting evidence that librarians are essential for comprehensive literature searches for meta-analyses and Cochrane reports. J Med Libr Assoc. 2004;92(2):163–4.
Swinkels A, Briddon J, Hall J. Two physiotherapists, one librarian and a systematic literature review: collaboration in action. Health Info Libr J. 2006;23(4):248–56.
Foster M. An overview of the role of librarians in systematic reviews: from expert search to project manager. EAHIL. 2015;11(3):3–7.
Lawson L. OPERATING OUTSIDE LIBRARY WALLS 2004.
Vassar M, Yerokhin V, Sinnett PM, Weiher M, Muckelrath H, Carr B, et al. Database selection in systematic reviews: an insight through clinical neurology. Health Inf Libr J. 2017;34(2):156–64.
Townsend WA, Anderson PF, Ginier EC, MacEachern MP, Saylor KM, Shipman BL, et al. A competency framework for librarians involved in systematic reviews. Journal of the Medical Library Association : JMLA. 2017;105(3):268–75.
Cooper ID, Crum JA. New activities and changing roles of health sciences librarians: a systematic review, 1990-2012. Journal of the Medical Library Association : JMLA. 2013;101(4):268–77.
Crum JA, Cooper ID. Emerging roles for biomedical librarians: a survey of current practice, challenges, and changes. Journal of the Medical Library Association : JMLA. 2013;101(4):278–86.
Dudden RF, Protzko SL. The systematic review team: contributions of the health sciences librarian. Med Ref Serv Q. 2011;30(3):301–15.
Golder S, Loke Y, McIntosh HM. Poor reporting and inadequate searches were apparent in systematic reviews of adverse effects. J Clin Epidemiol. 2008;61(5):440–8.
Maggio LA, Tannery NH, Kanter SL. Reproducibility of literature search reporting in medical education reviews. Academic medicine : journal of the Association of American Medical Colleges. 2011;86(8):1049–54.
Meert D, Torabi N, Costella J. Impact of librarians on reporting of the literature searching component of pediatric systematic reviews. Journal of the Medical Library Association : JMLA. 2016;104(4):267–77.
Morris M, Boruff JT, Gore GC. Scoping reviews: establishing the role of the librarian. Journal of the Medical Library Association : JMLA. 2016;104(4):346–54.
Koffel JB, Rethlefsen ML. Reproducibility of search strategies is poor in systematic reviews published in high-impact pediatrics, cardiology and surgery journals: a cross-sectional study. PLoS One. 2016;11(9):e0163309.
Article PubMed PubMed Central CAS Google Scholar
Fehrmann P, Thomas J. Comprehensive computer searches and reporting in systematic reviews. Research Synthesis Methods. 2011;2(1):15–32.
Booth A. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Systematic Reviews. 2016;5(1):74.
Article PubMed PubMed Central Google Scholar
Egger M, Juni P, Bartlett C, Holenstein F, Sterne J. How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study. Health technology assessment (Winchester, England). 2003;7(1):1–76.
Tricco AC, Tetzlaff J, Sampson M, Fergusson D, Cogo E, Horsley T, et al. Few systematic reviews exist documenting the extent of bias: a systematic review. J Clin Epidemiol. 2008;61(5):422–34.
Booth A. How much searching is enough? Comprehensive versus optimal retrieval for technology assessments. Int J Technol Assess Health Care. 2010;26(4):431–5.
Papaioannou D, Sutton A, Carroll C, Booth A, Wong R. Literature searching for social science systematic reviews: consideration of a range of search techniques. Health Inf Libr J. 2010;27(2):114–22.
Petticrew M. Time to rethink the systematic review catechism? Moving from ‘what works’ to ‘what happens’. Systematic Reviews. 2015;4(1):36.
Betrán AP, Say L, Gülmezoglu AM, Allen T, Hampson L. Effectiveness of different databases in identifying studies for systematic reviews: experience from the WHO systematic review of maternal morbidity and mortality. BMC Med Res Methodol. 2005;5
Felson DT. Bias in meta-analytic research. J Clin Epidemiol. 1992;45(8):885–92.
Article PubMed CAS Google Scholar
Franco A, Malhotra N, Simonovits G. Publication bias in the social sciences: unlocking the file drawer. Science. 2014;345(6203):1502–5.
Hartling L, Featherstone R, Nuspl M, Shave K, Dryden DM, Vandermeer B. Grey literature in systematic reviews: a cross-sectional study of the contribution of non-English reports, unpublished studies and dissertations to the results of meta-analyses in child-relevant reviews. BMC Med Res Methodol. 2017;17(1):64.
Schmucker CM, Blümle A, Schell LK, Schwarzer G, Oeller P, Cabrera L, et al. Systematic review finds that study data not published in full text articles have unclear impact on meta-analyses results in medical research. PLoS One. 2017;12(4):e0176210.
Egger M, Zellweger-Zahner T, Schneider M, Junker C, Lengeler C, Antes G. Language bias in randomised controlled trials published in English and German. Lancet (London, England). 1997;350(9074):326–9.
Moher D, Pham B, Lawson ML, Klassen TP. The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health technology assessment (Winchester, England). 2003;7(41):1–90.
Pham B, Klassen TP, Lawson ML, Moher D. Language of publication restrictions in systematic reviews gave different results depending on whether the intervention was conventional or complementary. J Clin Epidemiol. 2005;58(8):769–76.
Mills EJ, Kanters S, Thorlund K, Chaimani A, Veroniki A-A, Ioannidis JPA. The effects of excluding treatments from network meta-analyses: survey. BMJ : British Medical Journal. 2013;347
Hartling L, Featherstone R, Nuspl M, Shave K, Dryden DM, Vandermeer B. The contribution of databases to the results of systematic reviews: a cross-sectional study. BMC Med Res Methodol. 2016;16(1):127.
van Driel ML, De Sutter A, De Maeseneer J, Christiaens T. Searching for unpublished trials in Cochrane reviews may not be worth the effort. J Clin Epidemiol. 2009;62(8):838–44.e3.
Buchberger B, Krabbe L, Lux B, Mattivi JT. Evidence mapping for decision making: feasibility versus accuracy - when to abandon high sensitivity in electronic searches. German medical science : GMS e-journal. 2016;14:Doc09.
Lorenc T, Pearson M, Jamal F, Cooper C, Garside R. The role of systematic reviews of qualitative evidence in evaluating interventions: a case study. Research Synthesis Methods. 2012;3(1):1–10.
Gough D. Weight of evidence: a framework for the appraisal of the quality and relevance of evidence. Res Pap Educ. 2007;22(2):213–28.
Barroso J, Gollop CJ, Sandelowski M, Meynell J, Pearce PF, Collins LJ. The challenges of searching for and retrieving qualitative studies. West J Nurs Res. 2003;25(2):153–78.
Britten N, Garside R, Pope C, Frost J, Cooper C. Asking more of qualitative synthesis: a response to Sally Thorne. Qual Health Res. 2017;27(9):1370–6.
Booth A, Carroll C. Systematic searching for theory to inform systematic reviews: is it feasible? Is it desirable? Health Info Libr J. 2015;32(3):220–35.
Kwon Y, Powelson SE, Wong H, Ghali WA, Conly JM. An assessment of the efficacy of searching in biomedical databases beyond MEDLINE in identifying studies for a systematic review on ward closures as an infection control intervention to control outbreaks. Syst Rev. 2014;3:135.
Nussbaumer-Streit B, Klerings I, Wagner G, Titscher V, Gartlehner G. Assessing the validity of abbreviated literature searches for rapid reviews: protocol of a non-inferiority and meta-epidemiologic study. Systematic Reviews. 2016;5:197.
Wagner G, Nussbaumer-Streit B, Greimel J, Ciapponi A, Gartlehner G. Trading certainty for speed - how much uncertainty are decisionmakers and guideline developers willing to accept when using rapid reviews: an international survey. BMC Med Res Methodol. 2017;17(1):121.
Ogilvie D, Hamilton V, Egan M, Petticrew M. Systematic reviews of health effects of social interventions: 1. Finding the evidence: how far should you go? J Epidemiol Community Health. 2005;59(9):804–8.
Royle P, Milne R. Literature searching for randomized controlled trials used in Cochrane reviews: rapid versus exhaustive searches. Int J Technol Assess Health Care. 2003;19(4):591–603.
Pearson M, Moxham T, Ashton K. Effectiveness of search strategies for qualitative research about barriers and facilitators of program delivery. Eval Health Prof. 2011;34(3):297–308.
Levay P, Raynor M, Tuvey D. The Contributions of MEDLINE, Other Bibliographic Databases and Various Search Techniques to NICE Public Health Guidance. 2015. 2015;10(1):19.
Nussbaumer-Streit B, Klerings I, Wagner G, Heise TL, Dobrescu AI, Armijo-Olivo S, et al. Abbreviated literature searches were viable alternatives to comprehensive searches: a meta-epidemiological study. J Clin Epidemiol. 2018;102:1–11.
Briscoe S, Cooper C, Glanville J, Lefebvre C. The loss of the NHS EED and DARE databases and the effect on evidence synthesis and evaluation. Res Synth Methods. 2017;8(3):256–7.
Stansfield C, O'Mara-Eves A, Thomas J. Text mining for search term development in systematic reviewing: A discussion of some methods and challenges. Research Synthesis Methods.n/a-n/a.
Petrova M, Sutcliffe P, Fulford KW, Dale J. Search terms and a validated brief search filter to retrieve publications on health-related values in Medline: a word frequency analysis study. Journal of the American Medical Informatics Association : JAMIA. 2012;19(3):479–88.
Stansfield C, Thomas J, Kavanagh J. 'Clustering' documents automatically to support scoping reviews of research: a case study. Res Synth Methods. 2013;4(3):230–41.
PubMed Google Scholar
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14:579.
Andrew B. Clear and present questions: formulating questions for evidence based practice. Library Hi Tech. 2006;24(3):355–68.
Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–43.
Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al. Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model. Health technology assessment (Winchester, England). 2006;10(36):iii-iv, xi-xiii, 1–154.
Cooper C, Levay P, Lorenc T, Craig GM. A population search filter for hard-to-reach populations increased search efficiency for a systematic review. J Clin Epidemiol. 2014;67(5):554–9.
Hausner E, Waffenschmidt S, Kaiser T, Simon M. Routine development of objectively derived search strategies. Systematic Reviews. 2012;1(1):19.
Hausner E, Guddat C, Hermanns T, Lampert U, Waffenschmidt S. Prospective comparison of search strategies for systematic reviews: an objective approach yielded higher sensitivity than a conceptual one. J Clin Epidemiol. 2016;77:118–24.
Craven J, Levay P. Recording database searches for systematic reviews - what is the value of adding a narrative to peer-review checklists? A case study of nice interventional procedures guidance. Evid Based Libr Inf Pract. 2011;6(4):72–87.
Wright K, Golder S, Lewis-Light K. What value is the CINAHL database when searching for systematic reviews of qualitative studies? Syst Rev. 2015;4:104.
Beckles Z, Glover S, Ashe J, Stockton S, Boynton J, Lai R, et al. Searching CINAHL did not add value to clinical questions posed in NICE guidelines. J Clin Epidemiol. 2013;66(9):1051–7.
Cooper C, Rogers M, Bethel A, Briscoe S, Lowe J. A mapping review of the literature on UK-focused health and social care databases. Health Inf Libr J. 2015;32(1):5–22.
Younger P, Boddy K. When is a search not a search? A comparison of searching the AMED complementary health database via EBSCOhost, OVID and DIALOG. Health Inf Libr J. 2009;26(2):126–35.
Lam MT, McDiarmid M. Increasing number of databases searched in systematic reviews and meta-analyses between 1994 and 2014. Journal of the Medical Library Association : JMLA. 2016;104(4):284–9.
Bethel A, editor Search summary tables for systematic reviews: results and findings. HLC Conference 2017a.
Aagaard T, Lund H, Juhl C. Optimizing literature search in systematic reviews - are MEDLINE, EMBASE and CENTRAL enough for identifying effect studies within the area of musculoskeletal disorders? BMC Med Res Methodol. 2016;16(1):161.
Adams CE, Frederick K. An investigation of the adequacy of MEDLINE searches for randomized controlled trials (RCTs) of the effects of mental health care. Psychol Med. 1994;24(3):741–8.
Kelly L, St Pierre-Hansen N. So many databases, such little clarity: searching the literature for the topic aboriginal. Canadian family physician Medecin de famille canadien. 2008;54(11):1572–3.
Lawrence DW. What is lost when searching only one literature database for articles relevant to injury prevention and safety promotion? Injury Prevention. 2008;14(6):401–4.
Lemeshow AR, Blum RE, Berlin JA, Stoto MA, Colditz GA. Searching one or two databases was insufficient for meta-analysis of observational studies. J Clin Epidemiol. 2005;58(9):867–73.
Sampson M, Barrowman NJ, Moher D, Klassen TP, Pham B, Platt R, et al. Should meta-analysts search Embase in addition to Medline? J Clin Epidemiol. 2003;56(10):943–55.
Stevinson C, Lawlor DA. Searching multiple databases for systematic reviews: added value or diminishing returns? Complementary Therapies in Medicine. 2004;12(4):228–32.
Suarez-Almazor ME, Belseck E, Homik J, Dorgan M, Ramos-Remus C. Identifying clinical trials in the medical literature with electronic databases: MEDLINE alone is not enough. Control Clin Trials. 2000;21(5):476–87.
Taylor B, Wylie E, Dempster M, Donnelly M. Systematically retrieving research: a case study evaluating seven databases. Res Soc Work Pract. 2007;17(6):697–706.
Beyer FR, Wright K. Can we prioritise which databases to search? A case study using a systematic review of frozen shoulder management. Health Info Libr J. 2013;30(1):49–58.
Duffy S, de Kock S, Misso K, Noake C, Ross J, Stirk L. Supplementary searches of PubMed to improve currency of MEDLINE and MEDLINE in-process searches via Ovid. Journal of the Medical Library Association : JMLA. 2016;104(4):309–12.
Katchamart W, Faulkner A, Feldman B, Tomlinson G, Bombardier C. PubMed had a higher sensitivity than Ovid-MEDLINE in the search for systematic reviews. J Clin Epidemiol. 2011;64(7):805–7.
Cooper C, Lovell R, Husk K, Booth A, Garside R. Supplementary search methods were more effective and offered better value than bibliographic database searching: a case study from public health and environmental enhancement (in Press). Research Synthesis Methods. 2017;
Cooper C, Booth, A., Britten, N., Garside, R. A comparison of results of empirical studies of supplementary search techniques and recommendations in review methodology handbooks: A methodological review. (In Press). BMC Systematic Reviews. 2017.
Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ (Clinical research ed). 2005;331(7524):1064–5.
Article PubMed Central Google Scholar
Hinde S, Spackman E. Bidirectional citation searching to completion: an exploration of literature searching methods. PharmacoEconomics. 2015;33(1):5–11.
Levay P, Ainsworth N, Kettle R, Morgan A. Identifying evidence for public health guidance: a comparison of citation searching with web of science and Google scholar. Res Synth Methods. 2016;7(1):34–45.
McManus RJ, Wilson S, Delaney BC, Fitzmaurice DA, Hyde CJ, Tobias RS, et al. Review of the usefulness of contacting other experts when conducting a literature search for systematic reviews. BMJ (Clinical research ed). 1998;317(7172):1562–3.
Westphal A, Kriston L, Holzel LP, Harter M, von Wolff A. Efficiency and contribution of strategies for finding randomized controlled trials: a case study from a systematic review on therapeutic interventions of chronic depression. Journal of public health research. 2014;3(2):177.
Matthews EJ, Edwards AG, Barker J, Bloor M, Covey J, Hood K, et al. Efficient literature searching in diffuse topics: lessons from a systematic review of research on communicating risk to patients in primary care. Health Libr Rev. 1999;16(2):112–20.
Bethel A. Endnote Training (YouTube Videos) 2017b [Available from: http://medicine.exeter.ac.uk/esmi/workstreams/informationscience/is_resources,_guidance_&_advice/ .
Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association : JMLA. 2016;104(3):240–3.
Bramer WM, Milic J, Mast F. Reviewing retrieved references for inclusion in systematic reviews using EndNote. Journal of the Medical Library Association : JMLA. 2017;105(1):84–7.
Gall C, Brahmi FA. Retrieval comparison of EndNote to search MEDLINE (Ovid and PubMed) versus searching them directly. Medical reference services quarterly. 2004;23(3):25–32.
Ahmed KK, Al Dhubaib BE. Zotero: a bibliographic assistant to researcher. J Pharmacol Pharmacother. 2011;2(4):303–5.
Coar JT, Sewell JP. Zotero: harnessing the power of a personal bibliographic manager. Nurse Educ. 2010;35(5):205–7.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Sampson M, McGowan J, Tetzlaff J, Cogo E, Moher D. No consensus exists on search reporting methods for systematic reviews. J Clin Epidemiol. 2008;61(8):748–54.
Toews LC. Compliance of systematic reviews in veterinary journals with preferred reporting items for systematic reviews and meta-analysis (PRISMA) literature search reporting guidelines. Journal of the Medical Library Association : JMLA. 2017;105(3):233–9.
Booth A. "brimful of STARLITE": toward standards for reporting literature searches. Journal of the Medical Library Association : JMLA. 2006;94(4):421–9. e205
Faggion CM Jr, Wu YC, Tu YK, Wasiak J. Quality of search strategies reported in systematic reviews published in stereotactic radiosurgery. Br J Radiol. 2016;89(1062):20150878.
Mullins MM, DeLuca JB, Crepaz N, Lyles CM. Reporting quality of search methods in systematic reviews of HIV behavioral interventions (2000–2010): are the searches clearly explained, systematic and reproducible? Research Synthesis Methods. 2014;5(2):116–30.
Yoshii A, Plaut DA, McGraw KA, Anderson MJ, Wellik KE. Analysis of the reporting of search strategies in Cochrane systematic reviews. Journal of the Medical Library Association : JMLA. 2009;97(1):21–9.
Bigna JJ, Um LN, Nansseu JR. A comparison of quality of abstracts of systematic reviews including meta-analysis of randomized controlled trials in high-impact general medicine journals before and after the publication of PRISMA extension for abstracts: a systematic review and meta-analysis. Syst Rev. 2016;5(1):174.
Akhigbe T, Zolnourian A, Bulters D. Compliance of systematic reviews articles in brain arteriovenous malformation with PRISMA statement guidelines: review of literature. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2017;39:45–8.
Tao KM, Li XQ, Zhou QH, Moher D, Ling CQ, Yu WF. From QUOROM to PRISMA: a survey of high-impact medical journals' instructions to authors and a review of systematic reviews in anesthesia literature. PLoS One. 2011;6(11):e27611.
Wasiak J, Tyack Z, Ware R. Goodwin N. Jr. Poor methodological quality and reporting standards of systematic reviews in burn care management. International wound journal: Faggion CM; 2016.
Tam WW, Lo KK, Khalechelvam P. Endorsement of PRISMA statement and quality of systematic reviews and meta-analyses published in nursing journals: a cross-sectional study. BMJ Open. 2017;7(2):e013905.
Rader T, Mann M, Stansfield C, Cooper C, Sampson M. Methods for documenting systematic review searches: a discussion of common issues. Res Synth Methods. 2014;5(2):98–115.
Atkinson KM, Koenka AC, Sanchez CE, Moshontz H, Cooper H. Reporting standards for literature searches and report inclusion criteria: making research syntheses more transparent and easy to replicate. Res Synth Methods. 2015;6(1):87–95.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
Sampson M, McGowan J, Cogo E, Grimshaw J, Moher D, Lefebvre C. An evidence-based practice guideline for the peer review of electronic search strategies. J Clin Epidemiol. 2009;62(9):944–52.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical research ed). 2017;358.
Whiting P, Savović J, Higgins JPT, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Relevo R, Balshem H. Finding evidence for comparing medical interventions: AHRQ and the effective health care program. J Clin Epidemiol. 2011;64(11):1168–77.
Medicine Io. Standards for Systematic Reviews 2011 [Available from: http://www.nationalacademies.org/hmd/Reports/2011/Finding-What-Works-in-Health-Care-Standards-for-Systematic-Reviews/Standards.aspx .
CADTH: Resources 2018.
Download references
Acknowledgements
CC acknowledges the supervision offered by Professor Chris Hyde.
This publication forms a part of CC’s PhD. CC’s PhD was funded through the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) Programme (Project Number 16/54/11). The open access fee for this publication was paid for by Exeter Medical School.
RG and NB were partially supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South West Peninsula.
The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and affiliations.
Institute of Health Research, University of Exeter Medical School, Exeter, UK
Chris Cooper & Jo Varley-Campbell
HEDS, School of Health and Related Research (ScHARR), University of Sheffield, Sheffield, UK
Andrew Booth
Nicky Britten
European Centre for Environment and Human Health, University of Exeter Medical School, Truro, UK
Ruth Garside
You can also search for this author in PubMed Google Scholar
Contributions
CC conceived the idea for this study and wrote the first draft of the manuscript. CC discussed this publication in PhD supervision with AB and separately with JVC. CC revised the publication with input and comments from AB, JVC, RG and NB. All authors revised the manuscript prior to submission. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chris Cooper .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Appendix tables and PubMed search strategy. Key studies used for pearl growing per key stage, working data extraction tables and the PubMed search strategy. (DOCX 30 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Cooper, C., Booth, A., Varley-Campbell, J. et al. Defining the process to literature searching in systematic reviews: a literature review of guidance and supporting studies. BMC Med Res Methodol 18 , 85 (2018). https://doi.org/10.1186/s12874-018-0545-3
Download citation
Received : 20 September 2017
Accepted : 06 August 2018
Published : 14 August 2018
DOI : https://doi.org/10.1186/s12874-018-0545-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Literature Search Process
- Citation Chasing
- Tacit Models
- Unique Guidance
- Information Specialists
BMC Medical Research Methodology
ISSN: 1471-2288
- General enquiries: [email protected]

Literature Reviews & Search Strategies
- Defining the Literature Review
- Types of Literature Reviews
- Choosing Databases
Overview of Search Strategies
Search strategies, subject searching, example: iteratively developing + using keywords, demonstration: developing keywords from a question, demonstration: an advanced search.
- Organizing Your Literature
- Books: Research Design & Scholarly Writing
- Recommended Tutorials
There are many ways to find literature for your review, and we recommend that you use a combination of strategies - keeping in mind that you're going to be searching multiple times in a variety of ways, using different databases and resources. Searching the literature is not a straightforward, linear process - it's iterative (translation: you'll search multiple times, modifying your strategies as you go, and sometimes it'll be frustrating).
- Known Item Searching
- Citation Jumping
Some form of a keyword search is the way most of us get at scholarly articles in database - it's a great approach! Make sure you're familiar with these librarian strategies to get the most out of your searches.
Figuring out the best keywords for your research topic/question is a process - you'll start with one or a few words and then shift, adapt, and expand them as you start finding source that describe the topic using other words. Your search terms are the bridge between known topics and the unknowns of your research question - so sometimes one specific word will be enough, sometimes you'll need several different words to describe a concept AND you'll need to connect that concept to a second (and/or third) concept.
The number and specificity of your search terms depend on your topic and the scope of your literature review.
Connect Keywords Using Boolean
| Boolean Connector | Purpose |
|---|---|
| Connects different concepts (keywords). Narrows down the number of results. | |
| Connects synonyms. Expands the number of results. | |
| Excludes a concept. Use with extreme caution (even librarians don't use this one much). |
Make the Database Work More
...uses the asterisk (*) to end a word at its core, allowing you to retrieve many more documents containing variations of the search term. Example: educat* will find educate, educates, education, educators, educating and more.
Phrase Searching
...is when you put quotations marks around two or more words, so that the database looks for those words in that exact order. Examples: "higher education," "public health" and "pharmaceutical industry."
Controlled Vocabulary
... is when you use the terms the database uses to describe what each article is about as search terms. Searching using controlled vocabularies is a great way to get at everything on a topic in a database.
Databases and search engines are probably going to bring back a lot of results - more than a human can realistically go through. Instead of trying to manually read and sort them all, use the filters in each database to remove the stuff you wouldn't use anyway (ie it's outside the scope of your project).
To make sure you're consistent between searches and databases, write down the filters you're using.
A Few Filters to Try
| Filter | How it's Useful |
|---|---|
| This a filter you'll see in MCPHS Smart Search and the Catalog, and it's way narrow your results to things immediately available through the MCPHS collections, or (when removed) means you'll also see previews of results that we'll get for you through Interlibrary Loan. If you're doing graduate-level or more advanced work, you'll want to removed any location limiters, because relevance to your topic is more important. | |
| You may want to limit the search results you're seeing based on when they were published. For example, evidence-based medicine often involves looking at research from the last five years, while a project taking a historical perspective will want to include work going further back in time. | |
| The Library collects resources in English, but various databases index (include the abstract) of articles in a variety of languages. Consider limiting your search results to just those published in languages that you can read research in. (Note: your professor/advisor may have additional language restrictions, so if you're including research in multiple languages make sure that works for them too.) | |
| Literature reviews usually rely rather narrowly on various scholarly or academic sources, rather than the full spectrum of sources available to you in the world. Consider limiting your results to Academic or Scholarly articles. | |
| Sometimes you just need a systematic review, empirical study, or some other form of research. Subject specific databases will almost always offer a way to narrow down your results by methodology (article type). When the filter isn't available you can add your method of choice as an additional keyword! | |
| These are just a start! When you get to a new database, pause and take a look around. Figure out how the database can do some of the work for you - you can always turn off a filter if you don't like what it does. |
Once you know you have a good article , there are a lot of useful parts to it - far beyond the content.
Not sure where to start? Try course readings and other required materials.
Useful Parts of a Good Article
| Useful Part | Explanation |
|---|---|
| Look at the author-generated keywords, the database subject headings, the title, abstract and introduction for words that may be great additional/alternative search terms. You don't have to know everything about a topic before you start searching - let what you find introduce you to the language of the field. | |
| Author(s) | If they're written one article on this topic, they may have written more. Click on the author names to see what else they have in the database, or use their names (individually) as a search term elsewhere. |
| Journal | They may have published other articles on your topic; sometimes there's even a special issue wholly focused on a single topic. Consider browsing or searching within a specific publication. Oftentimes you'll end up searching in the journal's website. |
| Instruments | If authors have already created and validated an instrument (survey, tests, and measures), consider if you can use/adapt it for your own work. Look for details in the methods section, an original citation in the reference, and/or a copy in the appendix. |
| Experts on this topic have gathered and evaluated these sources, make sure you look through them for potential sources for your own work. |
Ways to Use Citations
| By using the references from the end of an article you'll move backwards and laterally in time to connected literature in the field. This is a great way to find other relevant articles as well as foundational research in the field. | |
| By using a citation searching database (eg Scopus or Google Scholar) you can more forward and laterally in time to connect to newer literature in the field. This is a great way to find more relevant articles in a fields as well as get as sense of how significant the article you're starting from is to the field as a whole. |
- Interactive Tutorial: Searching Cited and Citing Practice starting your search at an article and using the references to gather additional sources.

Your search results don't have to be frozen in the moment you search! There are a few things you can set up to keep your search going automatically.
| Alerts | What it Does for You | Example |
|---|---|---|
| Receive an email each time a new issue is published. This is a great way to read the most current research being published in leading journals in your field. Or consider following journals on social media, via an RSS feed, or app like If This Then That - these tools are great ways to stay up on the new research out there. | Set up an account with the to receive eAlerts. | |
| You can create a personal account in most databases so that once you've fine-tuned your search terms and filters on a topic, you can easily rerun the search manually (going back to the database), or set it so the database automatically runs the search on a schedule and emails you any results. Make those tools work for you! | In PubMed, set up to start saving your searching and creating alerts. | |
| Similar to the database alerts, you can tell Google Scholar to email you whenever certain words or phrases (including authors, institutions, methods, keywords, etc.) appear in new search results. | In settings, and then enter the word/phrase you want them to email you about. |
Searching using subject headings is a comprehensive search strategy that requires some planning and topic knowledge. Work through this PubMed tutorial for an introduction to this important approach to searching.

Through these videos and the accompanying PDF, you'll see an example of starting with a potential research question and developing search terms through brainstorming and keyword searching.
- Slidedeck: Keywords and Advanced Search PowerPoint slides to accompany the two demonstration videos on developing keywords from a question, and doing an advanced search.
- << Previous: Choosing Databases
- Next: Organizing Your Literature >>
- Last Updated: Jun 14, 2023 11:18 AM
- URL: https://mcphs.libguides.com/litreviews
- Interlibrary Loan
Ask an Expert
Ask an expert about access to resources, publishing, grants, and more.
MD Anderson faculty and staff can also request a one-on-one consultation with a librarian or scientific editor.
- Library Calendar
Log in to the Library's remote access system using your MyID account.
- Library Home
- Research Guides
Literature Search Basics
Develop a search strategy.
- Define your search
- Decide where to search
What is a search strategy
Advanced search tips.
- Track and save your search
- Class Recording: Writing an Effective Narrative Review
- A search strategy includes a combination of keywords, subject headings, and limiters (language, date, publication type, etc.)
- A search strategy should be planned out and practiced before executing the final search in a database.
- A search strategy and search results should be documented throughout the searching process.
What is a search strategy?
A search strategy is an organized combination of keywords, phrases, subject headings, and limiters used to search a database.
Your search strategy will include:
- keywords
- boolean operators
- variations of search terms (synonyms, suffixes)
- subject headings
Your search strategy may include:
- truncation (where applicable)
- phrases (where applicable)
- limiters (date, language, age, publication type, etc.)
A search strategy usually requires several iterations. You will need to test the strategy along the way to ensure that you are finding relevant articles. It's also a good idea to review your search strategy with your co-authors. They may have ideas about terms or concepts you may have missed.
Additionally, each database you search is developed differently. You will need to adjust your strategy for each database your search. For instance, Embase is a European database, many of the medical terms are slightly different than those used in MEDLINE and PubMed.
Choose search terms
Start by writing down as many terms as you can think of that relate to your question. You might try cited reference searching to find a few good articles that you can review for relevant terms.
Remember than most terms or concepts can be expressed in different ways. A few things to consider:
- synonyms: "cancer" may be referred to as "neoplasms", "tumors", or "malignancy"
- abbreviations: spell out the word instead of abbreviating
- generic vs. trade names of drugs
Search for the exact phrase
If you want words to appear next to each other in an exact phrase, use quotation marks, eg “self-esteem”.
Phrase searching decreases the number of results you get. Most databases allow you to search for phrases, but check the database guide if you are unsure.
Truncation and wildcards
Many databases use an asterisk (*) as their truncation symbol to find various word endings like singulars and plurals. Check the database help section if you are not sure which symbol to use.
"Therap*"
retrieves: therapy, therapies, therapist or therapists.
Use a wildcard (?) to find different spellings like British and American spellings.
"Behavio?r" retrieves behaviour and behavior.
Searching with subject headings
Database subject headings are controlled vocabulary terms that a database uses to describe what an article is about.
Using appropriate subject headings enhances your search and will help you to find more results on your topic. This is because subject headings find articles according to their subject, even if the article does not use your chosen key words.
You should combine both subject headings and keywords in your search strategy for each of the concepts you identify. This is particularly important if you are undertaking a systematic review or an in-depth piece of work
Subject headings may vary between databases, so you need to investigate each database separately to find the subject headings they use. For example, for MEDLINE you can use MeSH (Medical Subject Headings) and for Embase you can use the EMTREE thesaurus.
SEARCH TIP: In Ovid databases, search for a known key paper by title, select the "complete reference" button to see which subject headings the database indexers have given that article, and consider adding relevant ones to your own search strategy.
Use Boolean logic to combine search terms

Boolean operators (AND, OR and NOT) allow you to try different combinations of search terms or subject headings.
Databases often show Boolean operators as buttons or drop-down menus that you can click to combine your search terms or results.
The main Boolean operators are:
OR is used to find articles that mention either of the topics you search for.
AND is used to find articles that mention both of the searched topics.
NOT excludes a search term or concept. It should be used with caution as you may inadvertently exclude relevant references.
For example, searching for “self-esteem NOT eating disorders” finds articles that mention self-esteem but removes any articles that mention eating disorders.
Adjacency searching
Use adjacency operators to search by phrase or with two or more words in relation to one another. A djacency searching commands differ among databases. Check the database help section if you are not sure which searching commands to use.
In Ovid Medline
"breast ADJ3 cancer" finds the word breast within three words of cancer, in any order.
This includes breast cancer or cancer of the breast.
Cited Reference Searching
Cited reference searching is a method to find articles that have been cited by other publications.
Use cited reference searching to:
- find keywords or terms you may need to include in your search strategy
- find pivotal papers the same or similar subject area
- find pivotal authors in the same or similar subject area
- track how a topic has developed over time
Cited reference searching is available through these tools:
- Web of Science
- GoogleScholar
- << Previous: Decide where to search
- Next: Track and save your search >>
- Last Updated: Nov 29, 2022 3:34 PM
- URL: https://mdanderson.libguides.com/literaturesearchbasics
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Guideline Centre (UK). Evidence review for targets: Hypertension in adults: diagnosis and management: Evidence review D. London: National Institute for Health and Care Excellence (NICE); 2019 Aug. (NICE Guideline, No. 136.)
Evidence review for targets: Hypertension in adults: diagnosis and management: Evidence review D.
Appendix b literature search strategies.
The literature searches for this review are detailed below and complied with the methodology outlined in Developing NICE guidelines: the manual 2014, updated 2017 .
For more detailed information, please see the Methodology Review.
B.1. Clinical search literature search strategy
Searches were constructed using a PICO framework where population (P) terms were combined with Intervention (I) and in some cases Comparison (C) terms. Outcomes (O) are rarely used in search strategies for interventions as these concepts may not be well described in title, abstract or indexes and therefore difficult to retrieve. Search filters were applied to the search where appropriate.
Table 10 Database date parameters and filters used
View in own window
| Database | Dates searched | Search filter used |
|---|---|---|
| Medline (OVID) | 2000–02 October 2018 | Exclusions Randomised controlled trials Systematic review studies |
| Embase (OVID) | 2000–02 October 2018 | Exclusions Randomised controlled trials Systematic review studies |
| The Cochrane Library (Wiley) | Cochrane Reviews to Issue 8 of 12, August 2018 CENTRAL to Issue 7 of 12, July 2018 DARE and NHS EED to Issue 2 of 4, April 2015 HTA to Issue 4 of 4, October 2016 | None |
Table 11: Medline (Ovid) search terms
| 1. | exp Hypertension/ |
| 2. | hypertens*.ti,ab. |
| 3. | (elevat* adj2 blood adj pressur*).ti,ab. |
| 4. | (high adj blood adj pressur*).ti,ab. |
| 5. | (increase* adj2 blood pressur*).ti,ab. |
| 6. | ((systolic or diastolic or arterial) adj2 pressur*).ti,ab. |
| 7. | or/1–6 |
| 8. | exp pregnancy/ |
| 9. | exp Hypertension, Pregnancy-Induced/ not exp Hypertension/ |
| 10. | (pre eclampsia or pre-eclampsia or preeclampsia).ti,ab. |
| 11. | exp Hypertension, Portal/ not exp Hypertension/ |
| 12. | exp Hypertension, Pulmonary/ not exp Hypertension/ |
| 13. | exp Intracranial Hypertension/ not exp Hypertension/ |
| 14. | exp Ocular Hypertension/ not exp Hypertension/ |
| 15. | exp Diabetes Mellitus, Type 1/ not exp Diabetes Mellitus, Type 2/ |
| 16. | or/8–15 |
| 17. | 7 not 16 |
| 18. | letter/ |
| 19. | editorial/ |
| 20. | news/ |
| 21. | exp historical article/ |
| 22. | Anecdotes as Topic/ |
| 23. | comment/ |
| 24. | case report/ |
| 25. | (letter or comment*).ti. |
| 26. | or/18–25 |
| 27. | randomized controlled trial/ or random*.ti,ab. |
| 28. | 26 not 27 |
| 29. | animals/ not humans/ |
| 30. | exp Animals, Laboratory/ |
| 31. | exp Animal Experimentation/ |
| 32. | exp Models, Animal/ |
| 33. | exp Rodentia/ |
| 34. | (rat or rats or mouse or mice).ti. |
| 35. | or/28–34 |
| 36. | 17 not 35 |
| 37. | (exp child/ or exp pediatrics/ or exp infant/) not (exp adolescent/ or exp adult/ or exp middle age/ or exp aged/) |
| 38. | 36 not 37 |
| 39. | limit 38 to English language |
| 40. | ((target* or level* or optimum or optimal or control* or tight* or strict*) adj2 (blood pressure or BP)).ti,ab. |
| 41. | (normotensive* or normotension).ti,ab. |
| 42. | ((target* or level* or optimum or optimal) adj3 (QRISK* or Framingham or FHS or SCORE or ASSIGN or Interheart)).ti,ab. |
| 43. | ((target* or level* or optimum or optimal) adj3 ((Cardiovascular or CVD) adj3 (risk* or tool*))).ti,ab. |
| 44. | or/40–43 |
| 45. | 39 and 44 |
| 46. | randomized controlled trial.pt. |
| 47. | controlled clinical trial.pt. |
| 48. | randomi#ed.ti,ab. |
| 49. | placebo.ab. |
| 50. | randomly.ti,ab. |
| 51. | Clinical Trials as topic.sh. |
| 52. | trial.ti. |
| 53. | or/46–52 |
| 54. | Meta-Analysis/ |
| 55. | exp Meta-Analysis as Topic/ |
| 56. | (meta analy* or metanaly* or metaanaly* or meta regression).ti,ab. |
| 57. | ((systematic* or evidence*) adj3 (review* or overview*)).ti,ab. |
| 58. | (reference list* or bibliograph* or hand search* or manual search* or relevant journals).ab. |
| 59. | (search strategy or search criteria or systematic search or study selection or data extraction).ab. |
| 60. | (search* adj4 literature).ab. |
| 61. | (medline or pubmed or cochrane or embase or psychlit or psyclit or psychinfo or psycinfo or cinahl or science citation index or bids or cancerlit).ab. |
| 62. | cochrane.jw. |
| 63. | ((multiple treatment* or indirect or mixed) adj2 comparison*).ti,ab. |
| 64. | or/54–63 |
| 65. | 45 and (53 or 64) |
Table 12 Embase (Ovid) search terms
| 1. | exp Hypertension/ |
| 2. | hypertens*.ti,ab. |
| 3. | (elevat* adj2 blood adj pressur*).ti,ab. |
| 4. | (high adj blood adj pressur*).ti,ab. |
| 5. | (increase* adj2 blood pressur*).ti,ab. |
| 6. | ((systolic or diastolic or arterial) adj2 pressur*).ti,ab. |
| 7. | or/1–6 |
| 8. | exp pregnancy/ |
| 9. | exp Maternal Hypertension/ |
| 10. | (pre eclampsia or pre-eclampsia or preeclampsia).ti,ab. |
| 11. | exp Hypertension, Portal/ not exp Hypertension/ |
| 12. | exp Hypertension, Pulmonary/ not exp Hypertension/ |
| 13. | exp Intracranial Hypertension/ |
| 14. | exp Ocular Hypertension/ not exp Hypertension/ |
| 15. | exp Diabetes Mellitus, Type 1/ not exp Diabetes Mellitus, Type 2/ |
| 16. | or/8–15 |
| 17. | 7 not 16 |
| 18. | letter.pt. or letter/ |
| 19. | note.pt. |
| 20. | editorial.pt. |
| 21. | case report/ or case study/ |
| 22. | (letter or comment*).ti. |
| 23. | or/18–22 |
| 24. | randomized controlled trial/ or random*.ti,ab. |
| 25. | 23 not 24 |
| 26. | animal/ not human/ |
| 27. | nonhuman/ |
| 28. | exp Animal Experiment/ |
| 29. | exp Experimental Animal/ |
| 30. | animal model/ |
| 31. | exp Rodent/ |
| 32. | (rat or rats or mouse or mice).ti. |
| 33. | or/25–32 |
| 34. | 17 not 33 |
| 35. | (exp child/ or exp pediatrics/) not (exp adult/ or exp adolescent/) |
| 36. | 34 not 35 |
| 37. | limit 36 to English language |
| 38. | ((target* or level* or optimum or optimal or control* or tight* or strict*) adj2 (blood pressure or BP)).ti,ab. |
| 39. | (normotensive* or normotension).ti,ab. |
| 40. | ((target* or level* or optimum or optimal) adj3 (QRISK* or Framingham or FHS or SCORE or ASSIGN or Interheart)).ti,ab. |
| 41. | ((target* or level* or optimum or optimal) adj3 ((Cardiovascular or CVD) adj3 (risk* or tool*))).ti,ab. |
| 42. | or/38–41 |
| 43. | 37 and 42 |
| 44. | random*.ti,ab. |
| 45. | factorial*.ti,ab. |
| 46. | (crossover* or cross over*).ti,ab. |
| 47. | ((doubl* or singl*) adj blind*).ti,ab. |
| 48. | (assign* or allocat* or volunteer* or placebo*).ti,ab. |
| 49. | crossover procedure/ |
| 50. | single blind procedure/ |
| 51. | randomized controlled trial/ |
| 52. | double blind procedure/ |
| 53. | or/44–52 |
| 54. | systematic review/ |
| 55. | meta-analysis/ |
| 56. | (meta analy* or metanaly* or metaanaly* or meta regression).ti,ab. |
| 57. | ((systematic* or evidence*) adj3 (review* or overview*)).ti,ab. |
| 58. | (reference list* or bibliograph* or hand search* or manual search* or relevant journals).ab. |
| 59. | (search strategy or search criteria or systematic search or study selection or data extraction).ab. |
| 60. | (search* adj4 literature).ab. |
| 61. | (medline or pubmed or cochrane or embase or psychlit or psyclit or psychinfo or psycinfo or cinahl or science citation index or bids or cancerlit).ab. |
| 62. | cochrane.jw. |
| 63. | ((multiple treatment* or indirect or mixed) adj2 comparison*).ti,ab. |
| 64. | or/54–63 |
| 65. | 43 and (53 or 64) |
Table 13 Cochrane Library (Wiley) search terms
| #1. | MeSH descriptor: [Hypertension] explode all trees |
| #2. | hypertens*:ti,ab |
| #3. | (elevat* near/2 blood next pressur*):ti,ab |
| #4. | (high near/1 blood near/1 pressur*):ti,ab |
| #5. | (increase* near/2 blood pressur*):ti,ab |
| #6. | ((systolic or diastolic or arterial) near/2 pressur*):ti,ab |
| #7. | (or #1-#6) |
| #8. | ((target* or level* or optimum or optimal or control* or tight* or strict*) near/2 (blood pressure or BP)):ti,ab |
| #9. | (normotensive* or normotension):ti,ab |
| #10. | ((target* or level* or optimum or optimal) near/3 (QRISK* or Framingham or FHS or SCORE or ASSIGN or Interheart)):ti,ab |
| #11. | ((target* or level* or optimum or optimal) near/3 ((Cardiovascular or CVD) near/3 (risk* or tool*))):ti,ab |
| #12. | (or #8-#11) |
| #13. | #7 and #12 |
B.2. Health Economics literature search strategy
Health economic evidence was identified by conducting a broad search relating hypertension in adults population in NHS Economic Evaluation Database (NHS EED – this ceased to be updated after March 2015) and the Health Technology Assessment database (HTA) with no date restrictions. NHS EED and HTA databases are hosted by the Centre for Research and Dissemination (CRD). Additional searches were run on Medline and Embase for health economics, economic modelling and quality of life studies.
Table 14 Database date parameters and filters used
| Database | Dates searched | Search filter used |
|---|---|---|
| Medline | 2014–28 August 2018 | Exclusions Health economics studies |
| Embase | 2014–28 August 2018 | Exclusions Health economics studies |
| Centre for Research and Dissemination (CRD) | HTA - Inception–28 August 2018 NHS EED - Inception to March 2015 | None |
Table 15 Medline (Ovid) search terms
| 1. | exp Hypertension/ |
| 2. | hypertens*.ti,ab. |
| 3. | (elevat* adj2 blood adj pressur*).ti,ab. |
| 4. | (high adj blood adj pressur*).ti,ab. |
| 5. | (increase* adj2 blood pressur*).ti,ab. |
| 6. | ((systolic or diastolic or arterial) adj2 pressur*).ti,ab. |
| 7. | or/1–6 |
| 8. | letter/ |
| 9. | editorial/ |
| 10. | news/ |
| 11. | exp historical article/ |
| 12. | Anecdotes as Topic/ |
| 13. | comment/ |
| 14. | case report/ |
| 15. | (letter or comment*).ti. |
| 16. | or/8–15 |
| 17. | randomized controlled trial/ or random*.ti,ab. |
| 18. | 16 not 17 |
| 19. | animals/ not humans/ |
| 20. | exp Animals, Laboratory/ |
| 21. | exp Animal Experimentation/ |
| 22. | exp Models, Animal/ |
| 23. | exp Rodentia/ |
| 24. | (rat or rats or mouse or mice).ti. |
| 25. | or/18–24 |
| 26. | 7 not 25 |
| 27. | limit 26 to English language |
| 28. | Economics/ |
| 29. | Value of life/ |
| 30. | exp “Costs and Cost Analysis”/ |
| 31. | exp Economics, Hospital/ |
| 32. | exp Economics, Medical/ |
| 33. | Economics, Nursing/ |
| 34. | Economics, Pharmaceutical/ |
| 35. | exp “Fees and Charges”/ |
| 36. | exp Budgets/ |
| 37. | budget*.ti,ab. |
| 38. | cost*.ti. |
| 39. | (economic* or pharmaco?economic*).ti. |
| 40. | (price* or pricing*).ti,ab. |
| 41. | (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab. |
| 42. | (financ* or fee or fees).ti,ab. |
| 43. | (value adj2 (money or monetary)).ti,ab. |
| 44. | or/28–43 |
| 45. | 27 and 44 |
Table 16 Embase (Ovid) search terms
| 1. | exp Hypertension/ |
| 2. | hypertens*.ti,ab. |
| 3. | (elevat* adj2 blood adj pressur*).ti,ab. |
| 4. | (high adj blood adj pressur*).ti,ab. |
| 5. | (increase* adj2 blood pressur*).ti,ab. |
| 6. | ((systolic or diastolic or arterial) adj2 pressur*).ti,ab. |
| 7. | or/1–6 |
| 8. | letter.pt. or letter/ |
| 9. | note.pt. |
| 10. | editorial.pt. |
| 11. | case report/ or case study/ |
| 12. | (letter or comment*).ti. |
| 13. | or/8–12 |
| 14. | randomized controlled trial/ or random*.ti,ab. |
| 15. | 13 not 14 |
| 16. | animal/ not human/ |
| 17. | nonhuman/ |
| 18. | exp Animal Experiment/ |
| 19. | exp Experimental Animal/ |
| 20. | animal model/ |
| 21. | exp Rodent/ |
| 22. | (rat or rats or mouse or mice).ti. |
| 23. | or/15–22 |
| 24. | 7 not 23 |
| 25. | limit 24 to English language |
| 26. | health economics/ |
| 27. | exp economic evaluation/ |
| 28. | exp health care cost/ |
| 29. | exp fee/ |
| 30. | budget/ |
| 31. | funding/ |
| 32. | budget*.ti,ab. |
| 33. | cost*.ti. |
| 34. | (economic* or pharmaco?economic*).ti. |
| 35. | (price* or pricing*).ti,ab. |
| 36. | (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab. |
| 37. | (financ* or fee or fees).ti,ab. |
| 38. | (value adj2 (money or monetary)).ti,ab. |
| 39. | or/26–38 |
| 40. | 25 and 39 |
Table 17 NHS EED and HTA (CRD) search terms
| #1. | MeSH DESCRIPTOR Hypertension EXPLODE ALL TREES IN NHSEED,HTA |
| #2. | (Hypertens*) IN NHSEED, HTA |
| #3. | (elevat* adj2 blood adj pressur*) IN NHSEED, HTA |
| #4. | (high adj blood adj pressur*) IN NHSEED, HTA |
| #5. | (increase* adj2 blood pressur*) IN NHSEED, HTA |
| #6. | ((systolic or diastolic or arterial) adj2 pressur*) IN NHSEED, HTA |
| #7. | #1 OR #2 OR #3 OR #4 OR #5 OR #6 |
- Cite this Page National Guideline Centre (UK). Evidence review for targets: Hypertension in adults: diagnosis and management: Evidence review D. London: National Institute for Health and Care Excellence (NICE); 2019 Aug. (NICE Guideline, No. 136.) Appendix B, Literature search strategies.
- PDF version of this title (1.3M)
In this Page
- Clinical search literature search strategy
- Health Economics literature search strategy
Other titles in this collection
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 136: Hypertension in adults: diagnosis and management
Supplemental NICE documents
- Methods (PDF)
- Cost-effectiveness analysis: Treatment initiation threshold for people with stage 1 hypertension (PDF)
Recent Activity
- Literature search strategies - Evidence review for targets Literature search strategies - Evidence review for targets
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- Study and research support
- Literature searching
Literature searching explained
Develop a search strategy.
A search strategy is an organised structure of key terms used to search a database. The search strategy combines the key concepts of your search question in order to retrieve accurate results.
Your search strategy will account for all:
- possible search terms
- keywords and phrases
- truncated and wildcard variations of search terms
- subject headings (where applicable)
Each database works differently so you need to adapt your search strategy for each database. You may wish to develop a number of separate search strategies if your research covers several different areas.
It is a good idea to test your strategies and refine them after you have reviewed the search results.
How a search strategy looks in practice
Take a look at this example literature search in PsycINFO (PDF) about self-esteem.
The example shows the subject heading and keyword searches that have been carried out for each concept within our research question and how they have been combined using Boolean operators. It also shows where keyword techniques like truncation, wildcards and adjacency searching have been used.
Search strategy techniques
The next sections show some techniques you can use to develop your search strategy.
Skip straight to:
- Choosing search terms
- Searching with keywords
- Searching for exact phrases
- Using truncated and wildcard searches
Searching with subject headings
- Using Boolean logic
Citation searching
Choose search terms.
Concepts can be expressed in different ways eg “self-esteem” might be referred to as “self-worth”. Your aim is to consider each of your concepts and come up with a list of the different ways they could be expressed.
To find alternative keywords or phrases for your concepts try the following:
- Use a thesaurus to identify synonyms.
- Search for your concepts on a search engine like Google Scholar, scanning the results for alternative words and phrases.
- Examine relevant abstracts or articles for alternative words, phrases and subject headings (if the database uses subject headings).
When you've done this, you should have lists of words and phrases for each concept as in this completed PICO model (PDF) or this example concept map (PDF).
As you search and scan articles and abstracts, you may discover different key terms to enhance your search strategy.
Using truncation and wildcards can save you time and effort by finding alternative keywords.
Search with keywords
Keywords are free text words and phrases. Database search strategies use a combination of free text and subject headings (where applicable).
A keyword search usually looks for your search terms in the title and abstract of a reference. You may wish to search in title fields only if you want a small number of specific results.
Some databases will find the exact word or phrase, so make sure your spelling is accurate or you will miss references.
Search for the exact phrase
If you want words to appear next to each other in an exact phrase, use quotation marks, eg “self-esteem”.
Phrase searching decreases the number of results you get and makes your results more relevant. Most databases allow you to search for phrases, but check the database guide if you are unsure.
Truncation and wildcard searches
You can use truncated and wildcard searches to find variations of your search term. Truncation is useful for finding singular and plural forms of words and variant endings.
Many databases use an asterisk (*) as their truncation symbol. Check the database help section if you are not sure which symbol to use. For example, “therap*” will find therapy, therapies, therapist or therapists. A wildcard finds variant spellings of words. Use it to search for a single character, or no character.
Check the database help section to see which symbol to use as a wildcard.
Wildcards are useful for finding British and American spellings, for example: “behavio?r” in Medline will find both behaviour and behavior.
There are sometimes different symbols to find a variable single character. For example, in the Medline database, “wom#n” will find woman and also women.
Use adjacency searching for more accurate results
You can specify how close two words appear together in your search strategy. This can make your results more relevant; generally the closer two words appear to each other, the closer the relationship is between them.
Commands for adjacency searching differ among databases, so make sure you consult database guides.
In OvidSP databases (like Medline), searching for “physician ADJ3 relationship” will find both physician and relationship within two major words of each other, in any order. This finds more papers than "physician relationship".
Using this adjacency retrieves papers with phrases like "physician patient relationship", "patient physician relationship", "relationship of the physician to the patient" and so on.
Database subject headings are controlled vocabulary terms that a database uses to describe what an article is about.
Watch our 3-minute introduction to subject headings video . You can also View the video using Microsoft Stream (link opens in a new window, available for University members only).
Using appropriate subject headings enhances your search and will help you to find more results on your topic. This is because subject headings find articles according to their subject, even if the article does not use your chosen key words.
You should combine both subject headings and keywords in your search strategy for each of the concepts you identify. This is particularly important if you are undertaking a systematic review or an in-depth piece of work
Subject headings may vary between databases, so you need to investigate each database separately to find the subject headings they use. For example, for Medline you can use MeSH (Medical Subject Headings) and for Embase you can use the EMTREE thesaurus.
SEARCH TIP: In Ovid databases, search for a known key paper by title, select the "complete reference" button to see which subject headings the database indexers have given that article, and consider adding relevant ones to your own search strategy.
Use Boolean logic to combine search terms
Boolean operators (AND, OR and NOT) allow you to try different combinations of search terms or subject headings.
Databases often show Boolean operators as buttons or drop-down menus that you can click to combine your search terms or results.
The main Boolean operators are:
OR is used to find articles that mention either of the topics you search for.
AND is used to find articles that mention both of the searched topics.
NOT excludes a search term or concept. It should be used with caution as you may inadvertently exclude relevant references.
For example, searching for “self-esteem NOT eating disorders” finds articles that mention self-esteem but removes any articles that mention eating disorders.
Citation searching is a method to find articles that have been cited by other publications.
Use citation searching (or cited reference searching) to:
- find out whether articles have been cited by other authors
- find more recent papers on the same or similar subject
- discover how a known idea or innovation has been confirmed, applied, improved, extended, or corrected
- help make your literature review more comprehensive.
You can use cited reference searching in:
- OvidSP databases
- Google Scholar
- Web of Science
Cited reference searching can complement your literature search. However be careful not to just look at papers that have been cited in isolation. A robust literature search is also needed to limit publication bias.
- University of Michigan Library
- Research Guides
Systematic Reviews
- Search Strategy
- Work with a Search Expert
- Covidence Review Software
- Types of Reviews
- Evidence in a Systematic Review
- Information Sources
Developing an Answerable Question
Creating a search strategy, identifying synonyms & related terms, keywords vs. index terms, combining search terms using boolean operators, a sr search strategy, search limits.
- Managing Records
- Selection Process
- Data Collection Process
- Study Risk of Bias Assessment
- Reporting Results
- For Search Professionals
Validated Search Filters
Depending on your topic, you may be able to save time in constructing your search by using specific search filters (also called "hedges") developed & validated by researchers in the Health Information Research Unit (HiRU) of McMaster University, under contract from the National Library of Medicine. These filters can be found on
- PubMed’s Clinical Queries & Health Services Research Queries pages
- Ovid Medline’s Clinical Queries filters or here
- Embase & PsycINFO
- EBSCOhost’s main search page for CINAHL (Clinical Queries category)
- HiRU’s Nephrology Filters page
- American U of Beirut, esp. for " humans" filters .
- Countway Library of Medicine methodology filters
- InterTASC Information Specialists' Sub-Group Search Filter Resource
- SIGN (Scottish Intercollegiate Guidelines Network) filters page
Why Create a Sensitive Search?
In many literature reviews, you try to balance the sensitivity of the search (how many potentially relevant articles you find) & specificit y (how many definitely relevant articles you find ), realizing that you will miss some. In a systematic review, you want a very sensitive search: you are trying to find any potentially relevant article. A systematic review search will:
- contain many synonyms & variants of search terms
- use care in adding search filters
- search multiple resources, databases & grey literature, such as reports & clinical trials
PICO is a good framework to help clarify your systematic review question.
P - Patient, Population or Problem: What are the important characteristics of the patients &/or problem?
I - Intervention: What you plan to do for the patient or problem?
C - Comparison: What, if anything, is the alternative to the intervention?
O - Outcome: What is the outcome that you would like to measure?
Beyond PICO: the SPIDER tool for qualitative evidence synthesis.
5-SPICE: the application of an original framework for community health worker program design, quality improvement and research agenda setting.
A well constructed search strategy is the core of your systematic review and will be reported on in the methods section of your paper. The search strategy retrieves the majority of the studies you will assess for eligibility & inclusion. The quality of the search strategy also affects what items may have been missed. Informationists can be partners in this process.
For a systematic review, it is important to broaden your search to maximize the retrieval of relevant results.
Use keywords: How other people might describe a topic?
Identify the appropriate index terms (subject headings) for your topic.
- Index terms differ by database (MeSH, or Medical Subject Headings , Emtree terms , Subject headings) are assigned by experts based on the article's content.
- Check the indexing of sentinel articles (3-6 articles that are fundamental to your topic). Sentinel articles can also be used to test your search results.
Include spelling variations (e.g., behavior, behaviour ).
Both types of search terms are useful & both should be used in your search.
Keywords help to broaden your results. They will be searched for at least in journal titles, author names, article titles, & article abstracts. They can also be tagged to search all text.
Index/subject terms help to focus your search appropriately, looking for items that have had a specific term applied by an indexer.
Boolean operators let you combine search terms in specific ways to broaden or narrow your results.

An example of a search string for one concept in a systematic review.
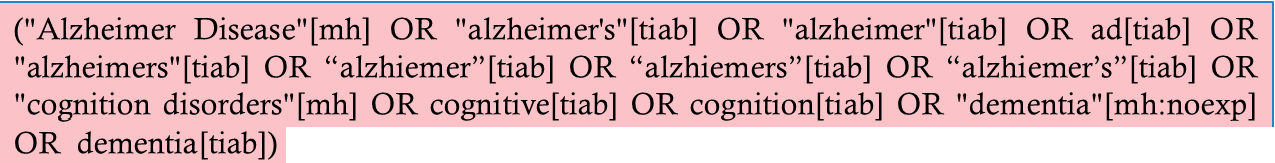
In this example from a PubMed search, [mh] = MeSH & [tiab] = Title/Abstract, a more focused version of a keyword search.
A typical database search limit allows you to narrow results so that you retrieve articles that are most relevant to your research question. Limit types vary by database & include:
- Article/publication type
- Publication dates
In a systematic review search, you should use care when applying limits, as you may lose articles inadvertently. For more information, see, particularly regarding language & format limits. Cochrane 2008 6.4.9
- Subject guides
- Researching for your literature review
- Develop a search strategy
Researching for your literature review: Develop a search strategy
- Literature reviews
- Literature sources
- Before you start
- Keyword search activity
- Subject search activity
- Combined keyword and subject searching
- Online tutorials
- Apply search limits
- Run a search in different databases
- Supplementary searching
- Save your searches
- Manage results

Identify key terms and concepts
Start developing a search strategy by identifying the key words and concepts within your research question. The aim is to identify the words likely to have been used in the published literature on this topic.
For example: What are the key infection control strategies for preventing the transmission of Meticillin-resistant Staphylococcus aureus (MRSA) in aged care homes .
Treat each component as a separate concept so that your topic is organised into separate blocks (concepts).
For each concept block, list the key words derived from your research question, as well as any other relevant terms or synonyms that you have found in your preliminary searches. Also consider singular and plural forms of words, variant spellings, acronyms and relevant index terms (subject headings).
| Search concept 1 | Search concept 2 | Search concept 3 |
|---|---|---|
| infection control | meticillin resistant staphylococcus aureus | aged care homes |
| infection prevention | methicillin resistant staphylococcus aureus | nursing homes |
| MRSA | ||
| exp Infection Control/ | Methicillin-resistant Staphylococcus aureus/ | homes for the aged/ |
| nursing homes/ |
As part of the process of developing a search strategy, it is recommended that you keep a master list of search terms for each key concept. This will make it easier when it comes to translating your search strategy across multiple database platforms.
Concept map template for documenting search terms
Combine search terms and concepts
Boolean operators are used to combine the different concepts in your topic to form a search strategy. The main operators used to connect your terms are AND and OR . See an explanation below:
- Link keywords related to a single concept with OR
- Linking with OR broadens a search (increases the number of results) by searching for any of the alternative keywords
Example: nursing home OR aged care home
- Link different concepts with AND
- Linking with AND narrows a search (reduces the number of results) by retrieving only those records that include all of your specified keywords
Example: nursing home AND infection control
- using NOT narrows a search by excluding results that contain certain search terms
- Most searches do not require the use of the NOT operator
Example: aged care homes NOT residential homes will retrieve all the results that include the words aged care homes but don't include the words residential homes . So if an article discussed both concepts this article would not be retrieved as it would be excluded on the basis of the words residential homes .
See the website for venn diagrams demonstrating the function of AND/OR/NOT:
Combine the search terms using Boolean
Advanced search operators - truncation and wildcards
By using a truncation symbol you can capture all of the various endings possible for a particular word. This may increase the number of results and reduce the likelihood of missing something relevant. Some tips about truncation:
- The truncation symbol is generally an asterisk symbol * and is added at the end of a word.
- It may be added to the root of a word that is a word in itself. Example: prevent * will retrieve prevent, prevent ing , prevent ion prevent ative etc. It may also be added to the root of a word that is not a word in itself. Example: strateg * will retrieve strateg y , strateg ies , strateg ic , strateg ize etc.
- If you don't want to retrieve all possible variations, an easy alternative is to utilise the OR operator instead e.g. strategy OR strategies. Always use OR instead of truncation where the root word is too small e.g. ill OR illness instead of ill*
There are also wildcard symbols that function like truncation but are often used in the middle of a word to replace zero, one or more characters.
- Unlike the truncator which is usually an asterisk, wildcards vary across database platforms
- Common wildcards symbols are the question mark ? and hash #.
- Example: wom # n finds woman or women, p ? ediatric finds pediatric or paediatric.
See the Database search tips for details of these operators, or check the Help link in any database.
Phrase searching
For words that you want to keep as a phrase, place two or more words in "inverted commas" or "quote marks". This will ensure word order is maintained and that you only retrieve results that have those words appearing together.
Example: “nursing homes”
There are a few databases that don't require the use of quote marks such as Ovid Medline and other databases in the Ovid suite. The Database search tips provides details on phrase searching in key databases, or you can check the Help link in any database.
Subject headings (index terms)
Identify appropriate subject headings (index terms).
Many databases use subject headings to index content. These are selected from a controlled list and describe what the article is about.
A comprehensive search strategy is often best achieved by using a combination of keywords and subject headings where possible.
In-depth knowledge of subject headings is not required for users to benefit from improved search performance using them in their searches.
Advantages of subject searching:
- Helps locate articles that use synonyms, variant spellings, plurals
- Search terms don’t have to appear in the title or abstract
Note: Subject headings are often unique to a particular database, so you will need to look for appropriate subject headings in each database you intend to use.
Subject headings are not available for every topic, and it is best to only select them if they relate closely to your area of interest.
MeSH (Medical Subject Headings)
The MeSH thesaurus provides standard terminology, imposing uniformity and consistency on the indexing of biomedical literature. In Pubmed/Medline each record is tagged with MeSH (Medical Subject Headings).
The MeSH vocabulary includes:
- Represent concepts found in the biomedical literature
- Some headings are commonly considered for every article (eg. Species (including humans), Sex, Age groups (for humans), Historical time periods)
- attached to MeSH headings to describe a specific aspect of a concept
- describe the type of publication being indexed; i.e., what the item is, not what the article is about (eg. Letter, Review, Randomized Controlled Trial)
- Terms in a separate thesaurus, primarily substance terms
Create a 'gold set'
It is useful to build a ‘sample set’ or ‘gold set’ of relevant references before you develop your search strategy..
Sources for a 'gold set' may include:
- key papers recommended by subject experts or supervisors
- citation searching - looking at a reference list to see who has been cited, or using a citation database (eg. Scopus, Web of Science) to see who has cited a known relevant article
- results of preliminary scoping searches.
The papers in your 'gold set' can then be used to help you identify relevant search terms
- Look up your 'gold set' articles in a database that you will use for your literature review. For the articles indexed in the database, look at the records to see what keywords and/or subject headings are listed.
The 'gold set' will also provide a means of testing your search strategy
- When an article in the sample set that is also indexed in the database is not retrieved, your search strategy can be revised in order to include it (see what concepts or keywords can be incorporated into your search strategy so that the article is retrieved).
- If your search strategy is retrieving a lot of irrelevant results, look at the irrelevant records to determine why they are being retrieved. What keywords or subject headings are causing them to appear? Can you change these without losing any relevant articles from your results?
- Information on the process of testing your search strategy using a gold set can be found in the systematic review guide
Example search strategy
A search strategy is the planned and structured organisation of terms used to search a database.
An example of a search strategy incorporating all three concepts, that could be applied to different databases is shown below:

You will use a combination of search operators to construct a search strategy, so it’s important to keep your concepts grouped together correctly. This can be done with parentheses (round brackets), or by searching for each concept separately or on a separate line.
The above search strategy in a nested format (combined into a single line using parentheses) would look like:
("infection control*" OR "infection prevention") AND ("methicillin resistant staphylococcus aureus" OR "meticillin resistant staphylococcus aureus" OR MRSA) AND ( "aged care home*" OR "nursing home*")
- << Previous: Search strategies - Health/Medical topic example
- Next: Keyword search activity >>
- Systematic Review
- Open access
- Published: 30 May 2024
Patient experiences: a qualitative systematic review of chemotherapy adherence
- Amineh Rashidi 1 ,
- Susma Thapa 1 ,
- Wasana Sandamali Kahawaththa Palliya Guruge 1 &
- Shubhpreet Kaur 1
BMC Cancer volume 24 , Article number: 658 ( 2024 ) Cite this article
263 Accesses
Metrics details
Adherence to chemotherapy treatment is recognized as a crucial health concern, especially in managing cancer patients. Chemotherapy presents challenges for patients, as it can lead to potential side effects that may adversely affect their mobility and overall function. Patients may sometimes neglect to communicate these side effects to health professionals, which can impact treatment management and leave their unresolved needs unaddressed. However, there is limited understanding of how patients’ experiences contribute to improving adherence to chemotherapy treatment and the provision of appropriate support. Therefore, gaining insights into patients’ experiences is crucial for enhancing the accompaniment and support provided during chemotherapy.
This review synthesizes qualitative literature on chemotherapy adherence within the context of patients’ experiences. Data were collected from Medline, Web of Science, CINAHL, PsychINFO, Embase, Scopus, and the Cochrane Library, systematically searched from 2006 to 2023. Keywords and MeSH terms were utilized to identify relevant research published in English. Thirteen articles were included in this review. Five key themes were synthesized from the findings, including positive outlook, receiving support, side effects, concerns about efficacy, and unmet information needs. The review underscores the importance for healthcare providers, particularly nurses, to focus on providing comprehensive information about chemotherapy treatment to patients. Adopting recommended strategies may assist patients in clinical practice settings in enhancing adherence to chemotherapy treatment and improving health outcomes for individuals living with cancer.
Peer Review reports
Introduction
Cancer can affect anyone and is recognized as a chronic disease characterized by abnormal cell multiplication in the body [ 1 ]. While cancer is prevalent worldwide, approximately 70% of cancer-related deaths occur in low- to middle-income nations [ 1 ]. Disparities in cancer outcomes are primarily attributed to variations in the accessibility of comprehensive diagnosis and treatment among countries [ 1 , 2 ]. Cancer treatment comes in various forms; however, chemotherapy is the most widely used approach [ 3 ]. Patients undergoing chemotherapy experience both disease-related and treatment-related adverse effects, significantly impacting their quality of life [ 4 ]. Despite these challenges, many cancer patients adhere to treatment in the hope of survival [ 5 ]. However, some studies have shown that concerns about treatment efficacy may hinder treatment adherence [ 6 ]. Adherence is defined as “the extent to which a person’s behaviour aligns with the recommendations of healthcare providers“ [ 7 ]. Additionally, treatment adherence is influenced by the information provided by healthcare professionals following a cancer diagnosis [ 8 ]. Patient experiences suggest that the decision to adhere to treatment is often influenced by personal factors, with family support playing a crucial role [ 8 ]. Furthermore, providing adequate information about chemotherapy, including its benefits and consequences, can help individuals living with cancer gain a better understanding of the advantages associated with adhering to chemotherapy treatment [ 9 ].
Recognizing the importance of adhering to chemotherapy treatment and understanding the impact of individual experiences of chemotherapy adherence would aid in identifying determinants of adherence and non-adherence that are modifiable through effective interventions [ 10 ]. Recently, systematic reviews have focused on experiences and adherence in breast cancer [ 11 ], self-management of chemotherapy in cancer patients [ 12 ], and the influence of medication side effects on adherence [ 13 ]. However, these reviews were narrow in scope, and to date, no review has integrated the findings of qualitative studies designed to explore both positive and negative experiences regarding chemotherapy treatment adherence. This review aims to synthesize the qualitative literature on chemotherapy adherence within the context of patients’ experiences.
This review was conducted in accordance with the Joanna Briggs Institute [ 14 ] guidelines for systemic review involving meta-aggregation. This review was registered in PROSPERO (CRD42021270459).
Search methods
The searches for peer reviewed publications in English from January 2006-September 2023 were conducted by using keywords, medical subject headings (MeSH) terms and Boolean operators ‘AND’ and ‘OR’, which are presented in the table in Appendix 1 . The searches were performed in a systematic manner in core databases such including Embase, Medline, PsycINFO, CINAHL, Web of Science, Cochrane Library, Scopus and the Joanna Briggs Institute (JBI). The search strategy was developed from keywords and medical subject headings (MeSH) terms. Librarian’s support and advice were sought in forming of the search strategies.
Study selection and inclusion criteria
The systematic search was conducted on each database and all articles were exported to Endnote and duplicates records were removed. Then, title and abstract of the full text was screened by two independent reviewers against the inclusion criteria. For this review, populations were patients aged 18 and over with cancer, the phenomenon of interest was experiences on chemotherapy adherence and context was considered as hospitals, communities, rehabilitation centres, outpatient clinics, and residential aged care. All peer-reviewed qualitative study design were also considered for inclusion. Studies included in this review were classified as primary research, published in English since 2006, some intervention implemented to improve adherence to treatment. This review excluded any studies that related to with cancer and mental health condition, animal studies and grey literature.
Quality appraisal and data extraction
The JBI Qualitative Assessment and Review Instrument for qualitative studies was used to assess the methodological quality of the included studies, which was conducted by the primary and second reviewers independently. There was no disagreement between the reviews. The qualitative data on objectives, study population, context, study methods, and the phenomena of interest and findings form the included studies were extracted.
Data synthesis
The meta-aggregation approach was used to combine the results with similar meaning. The primary and secondary reviewers created categories based on the meanings and concept. These categories were supported by direct quotations from participants. The findings were assess based on three levels of evidence, including unequivocal, credible, and unsupported [ 15 , 16 ]. Findings with no quotation were not considered for synthesis in this review. The categories and findings were also discussed by the third and fourth reviewers until a consensus was reached. The review was approved by the Edith Cowan University Human Research Ethics Committee (2021–02896).
Study inclusion
A total of 4145 records were identified through a systematic search. Duplicates ( n = 647) were excluded. Two independent reviewers conducted screening process. The remaining articles ( n = 3498) were examined for title and abstract screening. Then, the full text screening conducted, yielded 13 articles to be included in the final synthesis see Appendix 2 .
Methodological quality of included studies
All included qualitative studies scored between 7 and 9, which is displayed in Appendix 3 . The congruity between the research methodology and the research question or objectives, followed by applying appropriate data collection and data analysis were observed in all included studies. Only one study [ 17 ] indicated the researcher’s statement regarding cultural or theoretical perspectives. Three studies [ 18 , 19 , 20 ] identified the influence of the researcher on the research and vice-versa.
Characteristics of included studies
Most of studies conducted semi-structured and in-depth interviews, one study used narrative stories [ 19 ], one study used focus group discussion [ 21 ], and one study combined focus group and interview [ 22 ] to collect data. All studies conducted outpatient’s clinic, community, or hospital settings [ 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 ]. The study characteristics presented in Appendix 4 .
Review findings
Eighteen findings were extracted and synthesised into five categories: positive outlook, support, side effects, concern about efficacy and unmet information needs.
Positive outlook
Five studies discussed the link between positivity and hope and chemotherapy adherence [ 19 , 20 , 23 , 27 , 28 ]. Five studies commented that feeling positive and avoid the negativity and worry could encourage people to adhere in their mindset chemotherapy: “ I think the main thing for me was just keeping a positive attitude and not worrying, not letting myself worry about it ” [ 20 ]. Participants also considered the positive thoughts as a coping mechanism, that would help them to adhere and complete chemotherapy: “ I’m just real positive on how everything is going. I’m confident in the chemo, and I’m hoping to get out of her soon ” [ 23 ]. Viewing chemotherapy as part of their treatment regimen and having awareness of negative consequences of non-adherence to chemotherapy encouraged them to adhere chemotherapy: “ If I do not take medicine, I do not think I will be able to live ” [ 28 ]. Adhering chemotherapy was described as a survivor tool which helped people to control cancer-related symptoms: “ it is what is going to restore me. If it wasn’t this treatment, maybe I wasn’t here talking to you. So, I have to focus in what he is going to give me, life !” [ 27 ]. Similarly, people accepted the medical facts and prevent their life from worsening; “ without the treatment, it goes the wrong way. It is hard, but I have accepted it from the beginning, yes. This is how it is. I cannot do anything about it. Just have to accept it ” [ 19 ].
Finding from six studies contributed to this category [ 20 , 21 , 23 , 24 , 25 , 29 ]. Providing support from families and friends most important to the people. Receiving support from family members enhanced a sense responsibility towards their families, as they believed to survive for their family even if suffered: “ yes, I just thought that if something comes back again and I say no, then I have to look my family and friends in the eye and say I could have prevented it, perhaps. Now, if something comes back again, I can say I did everything I could. Cancer is bad enough without someone saying: It’s your own fault!!” [ 29 ]. Also, emotional support from family was described as important in helping and meeting their needs, and through facilitation helped people to adhere chemotherapy: “ people who genuinely mean the support that they’re giving […] just the pure joy on my daughter’s face for helping me. she was there day and night for me if I needed it, and that I think is the main thing not to have someone begrudgingly looking after you ” [ 20 ]. Another study discussed the role family, friends and social media as the best source of support during their treatment to adhere and continue “ I have tons of friends on Facebook, believe it or not, and it’s amazing how many people are supportive in that way, you know, just sending get-well wishes. I can’t imagine going through this like 10 years ago whenever stuff like that wasn’t around ” [ 23 ]. Receiving support from social workers was particularly helpful during chemotherapy in encouraging adherence to the chemotherapy: “ the social worker told me that love is courage. That was a huge encouragement, and I began to encourage myself ” [ 25 ].
Side effects
Findings from five studies informed this category [ 17 , 21 , 22 , 25 , 26 ]. Physical side effects were described by some as the most unpleasure experience: “ the side effects were very uncomfortable. I felt pain, fatigue, nausea, and dizziness that limited my daily activities. Sometimes, I was thinking about not keeping to my chemotherapy schedule due to those side effect ” [ 17 ]. The impact of side effects affected peoples’ ability to maintain their independence and self-care: “ I couldn’t walk because I didn’t have the energy, but I wouldn’t have dared to go out because the diarrhoea was so bad. Sometimes I couldn’t even get to the toilet; that’s very embarrassing because you feel like you’re a baby ” [ 26 ]. Some perceived that this resulted in being unable to perform independently: “ I was incredibly weak and then you still have to do things and you can’t manage it ” [ 22 ]. These side effect also decreased their quality of life “ I felt nauseated whenever I smelled food. I simply had no appetite when food was placed in front of me. I lost my sense of taste. Food had no taste anymore ” [ 25 ]. Although, the side effects impacted on patients´ leisure and free-time activities, they continued to undertake treatment: “ I had to give up doing the things I liked the most, such as going for walks or going to the beach. Routines, daily life in general were affected ” [ 21 ].
Concern about efficacy
Findings form four studies informed this category [ 17 , 18 , 24 , 28 ]. Although being concerned about the efficacy of the chemotherapy and whether or not chemotherapy treatment would be successful, one participant who undertook treatment described: “the efficacy is not so great. It is said to expect about 10% improvement, but I assume that it declines over time ” [ 28 ]. People were worried that such treatment could not cure their cancer and that their body suffered more due to the disease: “ I was really worried about my treatment effectiveness, and I will die shortly ” [ 17 ]. There were doubts expressed about remaining the cancer in the body after chemotherapy: “ there’s always sort of hidden worries in there that whilst they’re not actually taking the tumour away, then you’re wondering whether it’s getting bigger or what’s happening to it, whether it’s spreading or whatever, you know ” [ 24 ]. Uncertainty around the outcome of such treatment, or whether recovering from cancer or not was described as: “it makes you feel confused. You don’t know whether you are going to get better or else whether the illness is going to drag along further” [ 18 ].
Unmet information needs
Five studies contributed to this category [ 17 , 21 , 22 , 23 , 26 ]. The need for adequate information to assimilate information and provide more clarity when discussing complex information were described. Providing information from clinicians was described as minimal: “they explain everything to you and show you the statistics, then you’re supposed to take it all on-board. You could probably go a little bit slower with the different kinds of chemo and grappling with these statistics” [ 26 ]. People also used the internet search to gain information about their cancer or treatments, “I’ve done it (consult google), but I stopped right away because there’s so much information and you don’t know whether it’s true or not ” [ 21 ]. The need to receive from their clinicians to obtain clearer information was described as” I look a lot of stuff up online because it is not explained to me by the team here at the hospital ” [ 23 ]. Feeling overwhelmed with the volume of information could inhibit people to gain a better understanding of chemotherapy treatment and its relevant information: “ you don’t absorb everything that’s being said and an awful lot of information is given to you ” [ 22 ]. People stated that the need to know more information about their cancer, as they were never dared to ask from their clinicians: “ I am a low educated person and come from a rural area; I just follow the doctor’s advice for my health, and I do not dare to ask anything” [ 17 ].
The purpose of this review was to explore patient’s experiences about the chemotherapy adherence. After finalizing the searches, thirteen papers were included in this review that met the inclusion criteria.
The findings of the present review suggest that social support is a crucial element in people’s positive experiences of adhering to chemotherapy. Such support can lead to positive outcomes by providing consistent and timely assistance from family members or healthcare professionals, who play vital roles in maintaining chemotherapy adherence [ 30 ]. Consistent with our study, previous research has highlighted the significant role of family members in offering emotional and physical support, which helps individuals cope better with chemotherapy treatment [ 31 , 32 ]. However, while receiving support from family members reinforces individuals’ sense of responsibility in managing their treatment and their family, it also instils a desire to survive cancer and undergo chemotherapy. One study found that assuming self-responsibility empowers patients undergoing chemotherapy, as they feel a sense of control over their therapy and are less dependent on family members or healthcare professionals [ 33 ]. A qualitative systematic review reported that support from family members enables patients to become more proactive and effective in adhering to their treatment plan [ 34 ]. This review highlights the importance of maintaining a positive outlook and rational beliefs as essential components of chemotherapy adherence. Positive thinking helps individuals recognize their role in chemotherapy treatment and cope more effectively with their illness by accepting it as part of their treatment regimen and viewing it as a tool for survival. This finding is supported by previous studies indicating that positivity and positive affirmations play critical roles in helping individuals adapt to their reality and construct attitudes conducive to chemotherapy adherence [ 35 , 36 ]. Similarly, maintaining a positive mindset can foster more favourable thoughts regarding chemotherapy adherence, ultimately enhancing adherence and overall well-being [ 37 ].
This review identified side effects as a significant negative aspect of the chemotherapy experience, with individuals expressing concerns about how these side effects affected their ability to perform personal self-care tasks and maintain independent living in their daily lives. Previous studies have shown that participants with a history of chemotherapy drug side effects were less likely to adhere to their treatment regimen due to worsening symptoms, which increased the burden of medication side effects [ 38 , 39 ]. For instance, cancer patients who experienced minimal side effects from chemotherapy were at least 3.5 times more likely to adhere to their treatment plan compared to those who experienced side effects [ 40 ]. Despite experiencing side effects, patients were generally willing to accept and adhere to their treatment program, although one study in this review indicated that side effects made some patients unable to maintain treatment adherence. Side effects also decreased quality of life and imposed restrictions on lifestyle, as seen in another study where adverse effects limited individuals in fulfilling daily commitments and returning to normal levels of functioning [ 41 ]. Additionally, unmet needs regarding information on patients’ needs and expectations were common. Healthcare professionals were considered the most important source of information, followed by consultation with the internet. Providing information from healthcare professionals, particularly nurses, can support patients effectively and reinforce treatment adherence [ 42 , 43 ]. Chemotherapy patients often preferred to base their decisions on the recommendations of their care providers and required adequate information retention. Related studies have highlighted that unmet needs among cancer patients are known factors associated with chemotherapy adherence, emphasizing the importance of providing precise information and delivering it by healthcare professionals to improve adherence [ 44 , 45 ]. Doubts about the efficacy of chemotherapy treatment, as the disease may remain latent, were considered negative experiences. Despite these doubts, patients continued their treatment, echoing findings from a study where doubts regarding efficacy were identified as a main concern for chemotherapy adherence. Further research is needed to understand how doubts about treatment efficacy can still encourage patients to adhere to chemotherapy treatment.
Strengths and limitation
The strength of this review lies in its comprehensive search strategy across databases to select appropriate articles. Additionally, the use of JBI guidelines provided a comprehensive and rigorous methodological approach in conducting this review. However, the exclusion of non-English studies, quantitative studies, and studies involving adolescents and children may limit the generalizability of the findings. Furthermore, this review focuses solely on chemotherapy treatment and does not encompass other types of cancer treatment.
Conclusion and practical implications
Based on the discussion of the findings, it is evident that maintaining a positive mentality and receiving social support can enhance chemotherapy adherence. Conversely, experiencing treatment side effects, concerns about efficacy, and unmet information needs may lead to lower adherence. These findings present an opportunity for healthcare professionals, particularly nurses, to develop standardized approaches aimed at facilitating chemotherapy treatment adherence, with a focus on providing comprehensive information. By assessing patients’ needs, healthcare professionals can tailor approaches to promote chemotherapy adherence and improve the survival rates of people living with cancer. Raising awareness and providing education about cancer and chemotherapy treatment can enhance patients’ understanding of the disease and its treatment options. Utilizing videos and reading materials in outpatient clinics and pharmacy settings can broaden the reach of educational efforts. Policy makers and healthcare providers can collaborate to develop sustainable patient education models to optimize patient outcomes in the context of cancer care. A deeper understanding of individual processes related to chemotherapy adherence is necessary to plan the implementation of interventions effectively. Further research examining the experiences of both adherent and non-adherent patients is essential to gain a comprehensive understanding of this topic.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request. on our submission system as well.
World Health Organization. Cancer 2021 [ https://www.who.int/news-room/fact-sheets/detail/cancer .
Klapheke A, Yap SA, Pan K, Cress RDDHSDCA. Sociodemographic disparities in chemotherapy treatment and impact on survival among patients with metastatic bladder cancer. Urologic Oncology: Seminars Original Investigations. 2018;36(6):19–308.
Article Google Scholar
Moth EB, Kiely BE, Naganathan V, Martin A, Blinman P. How do oncologists make decisions about chemotherapy for their older patients with cancer? A survey of Australian oncologists. Support Care Cancer. 2018;26(2):451–60.
Article CAS PubMed Google Scholar
Khamboon T, Pakanta I. Intervention for symptom cluster management of fatigue, loss of appetite, and anxiety among patients with lung cancer undergoing chemotherapy. Asia-Pacific J Oncol Nurs. 2021;8(3):267–75.
Garcia ACM, Camargos Junior JB, Sarto KK, Silva Marcelo CAd, Paiva EMC, Nogueira DA, Mills J. Quality of life, self-compassion and mindfulness in cancer patients undergoing chemotherapy: a cross-sectional study. Eur J Oncol Nurs. 2021;51:N.PAG-N.PAG.
Horne R, Chapman SCE, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about Medicines prescribed for long-term conditions: a Meta-Analytic Review of the necessity-concerns Framework. PLoS ONE. 2013;8(12):e80633.
Article PubMed PubMed Central Google Scholar
WHO. Adherence to long-term therapies: evidence for action. Geneva, Switzerland: World Health Organisation; 2003.
Google Scholar
Warby A, Dhillon HM, Kao S, Vardy JL. A survey of patient and caregiver experience with malignant pleural mesothelioma. Support Care Cancer. 2019;27(12):4675–86.
Article PubMed Google Scholar
Arunachalam SS, Shetty AP, Panniyadi N, Meena C, Kumari J, Rani B, et al. Study on knowledge of chemotherapy’s adverse effects and their self-care ability to manage - the cancer survivors impact. Clin Epidemiol Global Health. 2021;11:100765.
Article CAS Google Scholar
Nizet P, Touchefeu Y, Pecout S, Cauchin E, Beaudouin E, Mayol S, et al. Exploring the factors influencing adherence to oral anticancer drugs in patients with digestive cancer: a qualitative study. Support Care Cancer. 2022;30(3):2591–604.
Clancy C, Lynch J, Oconnor P, Dowling M. Breast cancer patients’ experiences of adherence and persistence to oral endocrine therapy: a qualitative evidence synthesis. Eur J Oncol Nurs. 2020;44.
Magalhães B, Fernandes C, Lima L, Martinez-Galiano JM, Santos C. Cancer patients’ experiences on self-management of chemotherapy treatment-related symptoms: A systematic review and thematic synthesis. Eur J Oncol Nurs. 2020;49.
Peddie N, Agnew S, Crawford M, Dixon D, MacPherson I, Fleming L. The impact of medication side effects on adherence and persistence to hormone therapy in breast cancer survivors: a qualitative systematic review and thematic synthesis. Breast. 2021;58:147–59.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ: Br Med J. 2009;339(7716):332–6.
Joanna Briggs Institute. The Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews. Checklist for qualitative research. 2017.
Zachary M, Kylie P, Craig L, Edoardo A, Alan P. Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol [Internet]. 2014;14(1):108.
Iskandarsyah A, de Klerk C, Suardi DR, Soemitro MP, Sadarjoen SS, Passchier J. Psychosocial and cultural reasons for Delay in seeking help and Nonadherence to treatment in Indonesian women with breast Cancer: a qualitative study. Health Psychol. 2014;33(3):214–21.
Chircop D, Scerri J. The lived experience of patients with Non-hodgkin’s lymphoma undergoing chemotherapy. Eur J Oncol Nurs. 2018;35:117–21.
Kvåle K, Synnes O. Living with life-prolonging chemotherapy—control and meaning‐making in the tension between life and death. Eur J Cancer Care. 2018;27(1):1.
Staneva AA, Beesley VL, Niranjan N, Gibson AF, Rowlands I, Webb PM. I wasn’t gonna let it stop me: exploring women’s experiences of getting through chemotherapy for ovarian cancer. Cancer Nurs. 2019;42(2):E31–8.
Talens A, Guilabert M, Lumbreras B, Aznar MT, López-Pintor E. Medication Experience and Adherence to Oral Chemotherapy: A Qualitative Study of Patients’ and Health Professionals’ Perspectives. Int J Environ Res Public Health. 2021;18(8).
Dumas L, Lidington E, Appadu L, Jupp P, Husson O, Banerjee S, et al. Exploring older women’s attitudes to and experience of treatment for advanced ovarian cancer: a qualitative phenomenological study. Cancers. 2021;13(6):1207.
Albrecht TA, Keim-Malpass J, Boyiadzis M, Rosenzweig M. Psychosocial experiences of young adults diagnosed with acute leukemia during hospitalization for induction chemotherapy treatment. J Hospice Palliat Nurs. 2019;21(2):167–73.
Beaver K, Williamson S, Briggs J. Exploring patient experiences of neo-adjuvant chemotherapy for breast cancer. Eur J Oncol Nurs. 2016;20:77–86.
Chou J-F, Lu YY. Intraperitoneal chemotherapy: the lived experiences of Taiwanese patients with ovarian cancer. Clin J Oncol Nurs. 2019;23(6):E100–6.
Farrell C, Heaven C. Understanding the impact of chemotherapy on dignity for older people and their partners. Eur J Oncol Nurs. 2018;36:82–8.
Wakiuchi J, Silva Marcon S, de Oliveira DC, Aparecida Sales C. Rebuilding subjectivity from the experience of cancer and its treatment. Revista Brasileira De Enfermagem. 2019;72(1):125–33.
Yagasaki K, Komatsu H, Takahashi T. Inner conflict in patients receiving oral anticancer agents: a qualitative study. BMJ Open [Internet]. 2015; 5(4).
Gassmann C, Kolbe N, Brenner A. Experiences and coping strategies of oncology patients undergoing oral chemotherapy: first steps of a grounded theory study. Eur J Oncol Nurs. 2016;23:106–14.
Tang GX, Yan PP, Yan CL, Fu B, Zhu SJ, Zhou LQ, et al. Determinants of suicidal ideation in gynecological cancer patients. Psycho-oncology. 2016;25(1):97–103.
Oven Ustaalioglu B, Acar E, Caliskan M. The predictive factors for perceived social support among cancer patients and caregiver burden of their family caregivers in Turkish population. Int J Psychiatry Clin Pract. 2018;22(1):63–9.
Levkovich I, Cohen M, Karkabi K. The experience of fatigue in breast Cancer patients 1–12 Month Post-chemotherapy: a qualitative study. Behav Med. 2019;45(1):7–18.
Simchowitz B, Shiman L, Spencer J, Brouillard D, Gross A, Connor M, Weingart SN. Perceptions and experiences of patients receiving oral chemotherapy. Clin J Oncol Nurs. 2010;14(4):447–53.
Rashidi A, Kaistha P, Whitehead L, Robinson S. Factors that influence adherence to treatment plans amongst people living with cardiovascular disease: a review of published qualitative research studies. Int J Nurs Stud 2020;110(103727).
Aydogan U, Doganer YC, Komurcu S, Ozturk B, Ozet A, Saglam K. Coping attitudes of cancer patients and their caregivers and quality of life of caregivers. Indian J Palliat Care. 2016;22(2):150–6.
Langford DJ, Morgan S, Cooper B, Paul S, Kober K, Wright F, et al. Association of personality profiles with coping and adjustment to cancer among patients undergoing chemotherapy. Psycho-oncology. 2020;29(6):1060–7.
Jamie MJ, Pensak NA, Sporn NJ, MacDonald JJ, Lennes IT, Safren SA et al. Treatment satisfaction and adherence to oral chemotherapy in patients with Cancer. J Oncol Pract. 2017;13(2).
Tsai Y-F, Huang W-C, Cho S-F, Hsiao H-H, Liu Y-C, Lin S-F, et al. Side effects and medication adherence of tyrosine kinase inhibitors for patients with chronic myeloid leukemia in Taiwan. Medicine. 2018;97(26):415.
D S, M P, G R, S H. Importance of medication adherence and factors affecting it. IP Int J Compr Adv Pharmacolog. 2020;3(2):69–77.
Bekalu YE, Wudu MA, Gashu AW. Adherence to Chemotherapy and Associated factors among patients with Cancer in Amhara Region, Northeastern Ethiopia, 2022. A cross-sectional study. Cancer Control. 2023;30.
Hsu H-C, Liou W-S, Chiang A-J, Tsai S-Y, Jeang S-R, Wu S-L, et al. Longitudinal perceptions of the side effects of chemotherapy in patients with gynecological cancer. Support Care Cancer. 2017;25(11):3457–64.
Gow K, Rashidi A, Whithead L. Factors influencing medication adherence among adults living with diabetes and comorbidities: a qualitative systematic review. Curr Diab Rep. 2023:1–7.
Rashidi A, Whitehead L, Kaistha P. Nurses’ perceptions of factors influencing treatment engagement among patients with cardiovascular diseases: a systematic review. BMC Nurs. 2021;20(1):251.
Zebrack BJ, Block R, Hayes-Lattin B, Embry L, Aguilar C, Meeske KA, et al. Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer. 2013;119(1):201–14.
Timmers L, Boons CCLM, van den Verbrugghe M, Van Hecke A, Hugtenburg JG. Supporting adherence to oral anticancer agents: clinical practice and clues to improve care provided by physicians, nurse practitioners, nurses and pharmacists. BMC Cancer. 2017;17(1).
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
School of Nursing and Midwifery, Edith Cowan University, 270 Joondalup Drive, Joondalup, Perth, WA, 6027, Australia
Amineh Rashidi, Susma Thapa, Wasana Sandamali Kahawaththa Palliya Guruge & Shubhpreet Kaur
You can also search for this author in PubMed Google Scholar
Contributions
First author (AR) and second author (ST) conceived the review and the second author oversight for all stages of the review provided by the second author. All authors (AR), (ST), (WG) and (SK) undertook the literature search. Data extraction, screening the included papers and quality appraisal were undertaken by all authors (AR), (ST), (WG) and (SK). First and second authors (AR) and (ST) analysed the data and wrote the first draft of the manuscript and revised the manuscript and all authors (AR), (ST), (WG) and (SK) approved the final version of the manuscript.
Corresponding author
Correspondence to Amineh Rashidi .
Ethics declarations
Ethics approval and consent to participate.
The review was approved by the Edith Cowan University Human Research Ethics Committee (2021–02896). A proposal for the systematic review was assessed by the Edith Cowan University Human Research Ethics Committee and deemed not appropriate for full ethical review. However, a Data Management Plan (2021-02896-RASHIDI) was approved and monitored as part of this procedure. Raw data was extracted from the published manuscripts and authors could not identify individual participants during or after this process.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, supplementary material 5, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rashidi, A., Thapa, S., Kahawaththa Palliya Guruge, W. et al. Patient experiences: a qualitative systematic review of chemotherapy adherence. BMC Cancer 24 , 658 (2024). https://doi.org/10.1186/s12885-024-12353-z
Download citation
Received : 17 November 2023
Accepted : 07 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s12885-024-12353-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chemotherapy treatment
- Medication adherence
- Qualitative research
- Patients experiences
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 30 May 2024
Barriers and facilitators to mental health treatment access and engagement for LGBTQA+ people with psychosis: a scoping review protocol
- Cláudia C. Gonçalves ORCID: orcid.org/0000-0001-6767-0920 1 ,
- Zoe Waters 2 ,
- Shae E. Quirk 1 ,
- Peter M. Haddad 1 , 3 ,
- Ashleigh Lin 4 ,
- Lana J. Williams 1 &
- Alison R. Yung 1 , 5
Systematic Reviews volume 13 , Article number: 143 ( 2024 ) Cite this article
262 Accesses
Metrics details
The prevalence of psychosis has been shown to be disproportionately high amongst sexual and gender minority individuals. However, there is currently little consideration of the unique needs of this population in mental health treatment, with LGBTQA+ individuals facing barriers in accessing timely and non-stigmatising support for psychotic experiences. This issue deserves attention as delays to help-seeking and poor engagement with treatment predict worsened clinical and functional outcomes for people with psychosis. The present protocol describes the methodology for a scoping review which will aim to identify barriers and facilitators faced by LGBTQA+ individuals across the psychosis spectrum in help-seeking and accessing mental health support.
A comprehensive search strategy will be used to search Medline, PsycINFO, Embase, Scopus, LGBTQ+ Source, and grey literature. Original studies of any design, setting, and publication date will be included if they discuss barriers and facilitators to mental health treatment access and engagement for LGBTQA+ people with experiences of psychosis. Two reviewers will independently screen titles/abstracts and full-text articles for inclusion in the review. Both reviewers will then extract the relevant data according to pre-determined criteria, and study quality will be assessed using the Joanna Briggs Institute (JBI) critical appraisal checklists. Key data from included studies will be synthesised in narrative form according to the Guidance on the Conduct of Narrative Synthesis in Systematic Reviews.
The results of this review will provide a comprehensive account of the current and historical barriers and facilitators to mental healthcare faced by LGBTQA+ people with psychotic symptoms and experiences. It is anticipated that the findings from this review will be relevant to clinical and community services and inform future research. Findings will be disseminated through publication in a peer-reviewed journal and presented at conferences.
Scoping review registration
This protocol is registered in Open Science Framework Registries ( https://doi.org/10.17605/OSF.IO/AT6FC ).
Peer Review reports
The prevalence of psychotic disorders in the general population has been estimated to be around 0.27–0.75% [ 1 , 2 ], with the lifetime prevalence of ever having a psychotic experience being estimated at 5.8% [ 3 ]. However, rates of psychotic symptoms and experiences are disproportionately high amongst LGBTQA+ populations, with non-heterosexual individuals estimated to be 1.99–3.75 times more likely to experience psychosis than their heterosexual peers [ 4 , 5 , 6 , 7 ]. Additionally, it has been estimated that transgender or gender non-conforming (henceforth trans) individuals are 2.46–49.7 times more likely than their cisgender peers (i.e. individuals whose gender identity is the same as their birth registered sex) to receive a psychotic disorder diagnosis [ 8 , 9 ]. The increased rates of psychotic experiences noted amongst gender and sexual minorities may be explained by evidence indicating that LGBTQA+ people are also exposed to risk factors for psychosis at a far greater rate than members of the general population, such as childhood adversity [ 10 , 11 , 12 ], minority stress [ 13 ], discrimination [ 14 ], and stigma [ 15 , 16 ]. Furthermore, there is added potential for diagnostic biases leading to over-diagnosing psychosis in gender diverse individuals, whose gender expression and dysphoria may be pathologized by mental health service providers [ 8 ].
Despite these concerning statistics, there is very little research examining the experiences of LGBTQA+ people with psychosis, and limited consideration of the unique needs these individuals may have in accessing and engaging with mental health services. While timely access to treatment has consistently been associated with better symptomatic and functional outcomes for people with psychosis [ 17 , 18 ], there are often delays to treatment initiation which are worsened for LGBTQA+ individuals [ 19 , 20 ]. These individuals face additional barriers to accessing adequate mental health support compared to cisgender/heterosexual people [ 19 ] and may need to experiment with several mental health services before finding culturally competent care [ 20 ]. This in turn may lead to longer duration of untreated psychosis. Additionally, there seems to be a lack of targeted support for this population from healthcare providers, with LGBTQA+ individuals with serious mental health concerns reporting higher rates of dissatisfaction with psychiatric services than their cisgender and heterosexual counterparts [ 7 , 14 , 21 ]. However, the extent of these differences varies across contexts [ 22 ], potentially due to improved education around stigma and LGBTQA+ issues within a subset of mental health services.
Nonetheless, stigma remains one of the highest cited barriers to help-seeking for mental health problems, particularly with regard to concerns around disclosure [ 23 ], which can be particularly challenging for people experiencing psychosis [ 24 , 25 ]. Stigma stress in young people at risk for psychosis is associated with less positive attitudes towards help-seeking regarding both psychiatric medication and psychotherapy [ 26 ], potentially partly due to fears of judgement and being treated differently by service providers [ 27 ]. This issue may be compounded for people who also belong to minoritized groups [ 23 , 28 ], particularly as LGBTQA+ individuals have reported experiencing frequent stigma and encountering uninformed staff when accessing mental healthcare [ 7 , 29 ]. Furthermore, stigma-fuelled hesitance to access services may be heightened for trans people [ 30 ] whose identities have historically been pathologized and conflated with experiences of psychosis [ 31 ].
Even when individuals manage to overcome barriers to access support, there are added challenges to maintaining adequate treatment engagement. In a large online study, half of trans and nearly one third of LGB participants reported having stopped using mental health services in the past because of negative experiences related to their gender identity or sexuality [ 20 ]. This can be particularly problematic as experiences of stigma predict poorer medication adherence in psychosis [ 32 ] which subsequently multiplies the risk for relapse and suicide [ 33 ]. While no research to date has explored non-adherence rates in people with psychosis who are LGBTQA+, concerns around suicidality are heightened for individuals who are gender and sexuality diverse [ 34 , 35 , 36 ].
Generally, there is rising demand for mental healthcare that specifically addresses the needs of gender and sexual minority individuals and promotes respect for diversity, equity, and inclusion [ 29 , 37 ]. This is particularly salient as positive relationships with staff are associated with better medication adherence for people with psychosis [ 38 ] and healthcare providers with LGBTQA+-specific mandates have demonstrated higher satisfaction rates for LGBTQA+ individuals [ 20 ]. Mental health services need to adapt treatment options to acknowledge minority stress factors for those with stigmatised identities and, perhaps more importantly, how these intersect and interact to increase inequalities in people from minoritized groups accessing and benefiting from treatment [ 37 , 39 ].
Additionally, gender affirming care needs to be recognised as an important facet of mental health treatment for many trans individuals, as it is associated with positive outcomes such as improvements in quality of life and psychological functioning [ 40 , 41 , 42 ] and reductions in psychiatric symptom severity and need for subsequent mental health treatment [ 8 , 43 ]. While there are additional barriers in access to gender affirming care for individuals with psychosis, this treatment has shown success in parallel with treatment to address psychosis symptom stabilisation [ 19 , 44 ]. The importance of affirmation is echoed by the finding that many negative experiences of LGBTQA+ participants with mental health services could be avoided simply by respecting people’s pronouns and using gender-neutral language [ 20 ].
To ensure timely access to appropriate treatment for LGBTQA+ people with psychosis, there is a need for improved understanding of the factors which challenge and facilitate help-seeking and engagement with mental health support. A preliminary search of Google Scholar, Medline, the Cochrane Database of Systematic Reviews, and PROSPERO was conducted and revealed no existing or planned reviews exploring benefits and/or obstacles to mental health treatment specific to this population. Therefore, the proposed review seeks to comprehensively search and appraise the existing literature to identify and summarise a range of barriers and facilitators to adequate mental health support faced by LGBTQA+ people with experiences of psychosis. This will allow for the mapping of the types of evidence available and identification of any knowledge gaps. Moreover, we hope to guide future decision-making in mental healthcare to improve service accessibility for LGBTQA+ individuals with psychosis and to set the foundations for future research that centres this marginalised population. Based on published guidance [ 45 , 46 , 47 ], a scoping review methodology was identified as the most appropriate approach to address these aims.
Selection criteria
This scoping review protocol has been developed in compliance with the JBI Manual for Evidence Synthesis [ 48 ] and, where relevant, the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) checklist [ 49 ] (see Additional file 1). In the event of protocol amendments, the date, justification, and description for each amendment will be provided.
Due to the limited literature around the topic of this review, any primary original study design, setting, and publication date will be considered for inclusion. Publications written in English will be included, and articles in other languages may be considered pending time and cost constraints around translation. Publications will be excluded if the full text is not available upon request from authors.
The PCC (Population, Concept, Context) framework was used to develop the inclusion criteria for this scoping review:
This review will include individuals of any age who are LGBTQA+ and have had experiences of psychosis. For the purposes of this review, ‘LGBTQA+ individuals’ will be broadly defined as any individual that is not heterosexual and/or cisgender or anyone who engages in same-gender sexual behaviour. Studies may include participants who are cisgender and heterosexual if they separately report outcomes for LGBTQA+ individuals. Within this review, the term ‘psychosis’ includes (i) any diagnosis of a psychotic disorder, such as schizophrenia spectrum disorders, mood disorders with psychotic features, delusional disorders, and drug-induced psychotic disorders, (ii) sub-threshold psychotic symptoms, such as those present in ultra-high risk (UHR), clinical high risk (CHR), or at risk mental state (ARMS) individuals, and (iii) any psychotic-like symptoms or experiences. Studies may include participants with multiple diagnoses if they separately report outcomes for individuals on the psychosis spectrum.
This review will include publications which discuss potential barriers and/or facilitators to mental health help-seeking and/or engagement with mental health treatment. ‘Barriers’ will be operationalised as any factors which may delay or prevent individuals from accessing and engaging with appropriate mental health support. These may include lack of mental health education, experienced or internalised stigma, experiences of discrimination from health services, and lack of inclusivity in health services. ‘Facilitators’ will be operationalised as any factors which may promote timely help-seeking and engagement with sources of support. These may include improved access to mental health education, positive sources of social support, and welcoming and inclusive services. Mental health help-seeking will be broadly defined as any attempt to seek and access formal or informal support to address a mental health concern related to experiences of psychosis (e.g. making an initial appointment with a service provider, seeking help from a friend). Mental health treatment engagement will be broadly defined as adherence and active participation in the treatment that is offered by a source of support (e.g. attending scheduled appointments, taking medication as prescribed, openly communicating with service providers).
This review may include research encompassing any setting in which mental healthcare is provided. This is likely to include formal healthcare settings such as community mental health teams or inpatient clinics as well as informal settings such as LGBTQA+ spaces or informal peer support. Studies will be excluded if they focus exclusively on physical health treatment.
Search strategy
Database searches will be conducted in Medline, PsycINFO, Embase, Scopus, and LGBTQ+ Source. The full search strategy for this protocol is available (see Additional file 2). This strategy has been collaboratively developed and evaluated by a scholarly services health librarian. Searches will include subject headings relevant to each database and title/abstract keywords relating to three main concepts: (i) LGBTQA+ identity, (ii) experiences of psychosis, and (iii) mental health treatment. Keywords for each concept will be combined using the Boolean operator ‘OR’, and the three concepts will be combined using ‘AND’. This search strategy was appropriately translated for each of the selected databases. There will be no limitations on language or publication date at this stage to maximise the breadth of the literature captured. Publications returned from these searches will be exported to EndNote. Searches will be re-run prior to the final analysis to capture any newly published studies.
The database searches will be supplemented by searching the grey literature as per the eligibility criteria detailed above. These may include theses and dissertations, conference proceedings, reports from mental health services, and policy documents from LGBTQA+ groups. Google and Google Scholar will be searched using a combination of clauses for psychosis (Psychosis OR psychotic OR schizophrenia OR schizoaffective), treatment (treatment or “help-seeking”), and queer identity. The latter concept will have three clauses for three separate searches, with one including broad queer identity (LGBT), one specific to non-heterosexual individuals (gay OR lesbian OR homosexual OR bisexual OR queer OR asexual), and one specific to trans individuals (transgender OR transsexual OR transexual OR “non-binary” OR “gender minority”). Additionally, reference lists and citing literature will be manually searched for each paper included in the review to capture any articles and policy documents not previously identified.
Data selection
Search results will be imported into Covidence using EndNote, and duplicates will be eliminated. Titles and abstracts will be screened by the first and second authors according to pre-defined screening criteria, which will be discussed by the authors and piloted prior to screening. These criteria will consider whether the articles included LGBTQA+ participants with experiences of psychosis (as operationalised above) in relation to mental health help-seeking and/or treatment. Full texts of relevant articles will then be obtained and screened by the first and second reviewer in accordance with the full inclusion and exclusion criteria after initial piloting to maximise inter-rater reliability. Decisions on inclusion and exclusion will be blinded and recorded on Covidence. Potential discrepancies will be resolved through discussion, and when consensus cannot be reached, these will be resolved by the supervising author. The process of study selection will be documented using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram [ 50 ].
Data extraction
Data extraction will be performed independently by two reviewers using Covidence. Prior to beginning final extraction, both reviewers will independently pilot the extraction tool using a sample of five included studies and discuss any necessary changes. Information extracted is planned to include the following: title, author name(s), year of publication, country in which the study was conducted, study design, sample size, population of focus (i.e. sexual minorities, gender minorities, or both), sample demographics (i.e. age, gender identity, and sexual orientation), setting (e.g. early intervention service, community mental health team, etc.), psychosis characteristics (e.g. diagnoses included, severity of symptoms, etc.), type of treatment (e.g. cognitive behavioural therapy, antipsychotic medication, etc.), and any barriers and/or facilitators identified according to the aforementioned operationalised definitions. Disagreements will be resolved through discussion between the two reviewers and, when necessary, final decisions will be made by a senior supervisor. Once extracted, information will be recorded in Excel. Lead authors of papers will be contacted by the primary review author in cases where there is missing or insufficient data.
Quality assessment
Due to the expected heterogeneity in the types of studies that may be included in this review (e.g. qualitative studies, randomised controlled trials, case control studies, case reports), the relevant revised Joanna Briggs Institute (JBI) critical appraisal checklists [ 51 ] will be used to assess risk of bias and study quality for each study design. Two reviewers will independently use these checklists to assess each paper that is included following the full-text screening. If there are discrepancies in article ratings, these will be resolved through discussion between the two authors. If no consensus is reached, discrepancies will be resolved by a senior supervisor. In line with the scoping nature of this review, low-quality studies will not be excluded from the synthesis.
Evidence synthesis
Data from included studies will be synthesised using a narrative synthesis approach in accordance with the Guidance on the Conduct of Narrative Synthesis in Systematic Reviews [ 52 ]. A preliminary descriptive synthesis will be conducted by tabulating the extracted data elements from each study alongside quality assessment results and developing an initial description of the barriers and facilitators to (1) accessing and (2) engaging with mental health support that are identified in the literature. This initial synthesis will then be interrogated and refined to contextualise these barriers and facilitators in the setting, population, and methodology of each study to form the basis for an interpretative synthesis.
This review will not use a pre-existing thematic framework to categorise barriers and facilitators as it is expected that the factors identified will not neatly fit into existing criteria. Instead, these will be conceptualised according to overarching themes as interrelated factors, so that potentially complex interactions between barriers and facilitators within and across relevant studies may be explored through concept mapping. If most of the studies included are qualitative, there may also be scope for a partial meta-synthesis. To avoid oversimplifying the concept of ‘barriers and facilitators’ (see criticism by Bach-Mortensen & Verboom [ 53 ]), this data synthesis will be followed by a critical reflection of the findings through the lens of the socio-political contexts which may give rise to the barriers and facilitators identified, exploring the complexities necessary for any changes to be implemented in mental health services.
If the extracted data indicate that gender minority and sexual minority individuals experience unique or different barriers and/or facilitators to each other, these population groups will be analysed separately as opposed to findings being generalised across the LGBTQA+ spectrum. Furthermore, if there is scope to do so, analyses may be conducted to investigate how perceived barriers and facilitators for this population may have changed over time (i.e. according to publication date) as definitions of psychosis evolve and LGBTQA+ individuals gain visibility in clinical services.
The proposed review will add to the literature around mental health treatment for LGBTQA+ people with psychosis. It will provide a thorough account of the barriers and facilitators to accessing and engaging with support faced by this population and may inform future research and clinical practice.
In terms of limitations, this review will be constrained by the existing literature and may therefore not be sufficiently comprehensive in reflecting the barriers and facilitators experienced by subgroups within the broader LGBTQA+ community. Additionally, although broad inclusion criteria are necessary to capture the full breadth of research conducted in this topic, included studies are likely to be heterogeneous and varied in terms of their methodology and population which may complicate data synthesis.
Nonetheless, it is anticipated that the findings from this review will provide the most comprehensive synthesis to date of the issues driving low help-seeking and treatment engagement in people across the psychosis spectrum who are LGBTQA+. This review will likely also identify gaps in the literature which may inform avenues for future research, and the factors identified in this review will be considered in subsequent research by the authors.
Additionally, findings will be relevant to healthcare providers that offer support to people with psychosis who may have intersecting LGBTQA+ identities as well as LGBTQA+ organisations which offer support to LGBTQA+ people who may be experiencing distressing psychotic experiences. These services are likely to benefit from an increased awareness of the factors which may improve or hinder accessibility for these subsets of their target populations. Therefore, results from this review may inform decision-making around the implementation of service-wide policy changes.
The findings of this review will be disseminated through the publication of an article in a peer-reviewed journal and presented at relevant conferences in Australia and/or internationally. Additionally, the completed review will form part of the lead author’s doctoral thesis.
Availability of data and materials
Not applicable for this protocol.
Abbreviations
- At risk mental state
Clinical high risk for psychosis
Joanna Briggs Institute
Lesbian, gay, and bisexual
Lesbian, gay, bisexual, transgender, queer or questioning, asexual or aromantic, and more
Population, Concept, Context
Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols
Ultra-high risk for psychosis
Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Study (GBD) Results. Seattle, WA: IHME, University of Washington. 2020. https://vizhub.healthdata.org/gbd-results/ . Accessed 26 May 2023
Moreno-Kustner B, Martin C, Pastor L. Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PLoS One. 2018;13(4):e0195687. https://doi.org/10.1371/journal.pone.0195687 .
Article CAS PubMed PubMed Central Google Scholar
McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, et al. Psychotic experiences in the general population: a cross-national analysis based on 31 261 respondents from 18 countries. JAMA Psychiatry. 2015;72(7):697–705. https://doi.org/10.1001/jamapsychiatry.2015.0575 .
Article PubMed PubMed Central Google Scholar
Chakraborty A, McManus S, Brugha TS, Bebbington P, King M. Mental health of the non-heterosexual population of England. Br J Psychiatry. 2011;198(2):143–8. https://doi.org/10.1192/bjp.bp.110.082271 .
Article PubMed Google Scholar
Gevonden M, Selten J, Myin-Germeys I, De Graaf R, Ten Have M, Van Dorsselaer S, et al. Sexual minority status and psychotic symptoms: findings from the Netherlands Mental Health Survey and Incidence Studies (NEMESIS). Psychol Med. 2014;44(2):421–33. https://doi.org/10.1017/S0033291713000718 .
Article CAS PubMed Google Scholar
Jacob L, Smith L, McDermott D, Haro JM, Stickley A, Koyanagi A. Relationship between sexual orientation and psychotic experiences in the general population in England. Psychol Med. 2021;51(1):138–46. https://doi.org/10.1017/S003329171900309X .
Welch S, Collings SCD, Howden-Chapman P. Lesbians in New Zealand: their mental health and satisfaction with mental health services. Aust N Z J Psychiatry. 2000;34(2):256–63. https://doi.org/10.1080/j.1440-1614.2000.00710.x .
Barr SM, Roberts D, Thakkar KN. Psychosis in transgender and gender non-conforming individuals: a review of the literature and a call for more research. Psychiatry Res. 2021;306:114272. https://doi.org/10.1016/j.psychres.2021.114272 .
Hanna B, Desai R, Parekh T, Guirguis E, Kumar G, Sachdeva R. Psychiatric disorders in the U.S. transgender population. Ann Epidemiol. 2019;39:1–7. https://doi.org/10.1016/j.annepidem.2019.09.009 .
Schneeberger AR, Dietl MF, Muenzenmaier KH, Huber CG, Lang UE. Stressful childhood experiences and health outcomes in sexual minority populations: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1427–45. https://doi.org/10.1007/s00127-014-0854-8 .
Stanton KJ, Denietolis B, Goodwin BJ, Dvir Y. Childhood trauma and psychosis: an updated review. Child Adolesc Psychiatr Clin N Am. 2020;29(1):115–29. https://doi.org/10.1016/j.chc.2019.08.004 .
Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–71. https://doi.org/10.1093/schbul/sbs050 .
Mongelli F, Perrone D, Balducci J, Saccheti A, Ferrari S, Mattei G, et al. Minority stress and mental health among LGBT populations: an update on the evidence. Minerva Psichiatr. 2019;60(1):27–50. https://doi.org/10.23736/S0391-1772.18.01995-7 .
Article Google Scholar
Kidd SA, Howison M, Pilling M, Ross LE, McKenzie K. Severe mental illness in LGBT populations: a scoping review. Psychiatr Serv. 2016;67(7):779–83. https://doi.org/10.1176/appi.ps.201500209 .
Hatzenbuehler ML, Pachankis JE. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth. Pediatr Clin North Am. 2016;63(6):985–97. https://doi.org/10.1016/j.pcl.2016.07.003 .
Rüsch N, Heekeren K, Theodoridou A, Müller M, Corrigan PW, Mayer B, et al. Stigma as a stressor and transition to schizophrenia after one year among young people at risk of psychosis. Schizophr Res. 2015;166(1–3):43–8. https://doi.org/10.1016/j.schres.2015.05.027 .
Howes OD, Whitehurst T, Shatalina E, Townsend L, Onwordi EC, Mak TLA, et al. The clinical significance of duration of untreated psychosis: an umbrella review and random-effects meta-analysis. World Psychiatry. 2021;20(1):75–95. https://doi.org/10.1002/wps.20822 .
McGorry PD. Early intervention in psychosis: obvious, effective, overdue. J Nerv Ment Dis. 2015;203(5):310–308. https://doi.org/10.1097/NMD.0000000000000284 .
Peta JL. The Oxford Handbook of Sexual and Gender Minority Mental Health. Oxford (GB): Oxford University Press; 2020. Chapter 11, Schizophrenia spectrum and other psychotic disorders among sexual and gender minority populations; 125-134. Available from: The Oxford Handbook of Sexual and Gender Minority Mental Health - Google Books. Accessed 01 Jun 2023
Simeonov D, Steele LS, Anderson S, Ross LE. Perceived satisfaction with mental health services in the lesbian, gay, bisexual, transgender, and transsexual communities in Ontario, Canada: an internet-based survey. Can J Commun Ment Health. 2015;34(1):31–44. https://doi.org/10.7870/cjcmh-2014-037 .
Avery AM, Hellman RE, Sudderth LK. Satisfaction with mental health services among sexual minorities with major mental illness. Am J Public Health. 2001;91(6):990–1. https://doi.org/10.2105/AJPH.91.6.990 .
Plöderl M, Mestel R, Fartacek C. Differences by sexual orientation in treatment outcome and satisfaction with treatment among inpatients of a German psychiatric clinic. PLoS ONE. 2022;17(1):e0262928. https://doi.org/10.1371/journal.pone.0262928 .
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27. https://doi.org/10.1017/S0033291714000129 .
Pyle M, Morrison AP. “It’s just a very taboo and secretive kind of thing”: making sense of living with stigma and discrimination from accounts of people with psychosis. Psychosis. 2014;6(3):195–205. https://doi.org/10.1080/17522439.2013.834458 .
Wood L, Burke E, Byrne R, Pyle M, Chapman N, Morrison AP. Stigma in psychosis: a thematic synthesis of current qualitative evidence. Psychosis. 2015;7(2):152–65. https://doi.org/10.1080/17522439.2014.926561 .
Rüsch N, Heekeren K, Theodoridou A, Dvorsky D, Müller M, Paust T, et al. Attitudes towards help-seeking and stigma among young people at risk for psychosis. Psychiatry Res. 2013;210(3):1313–5. https://doi.org/10.1016/j.psychres.2013.08.028 .
Gronholm PC, Thornicroft G, Laurens KR, Evans-Lacko S. Mental health-related stigma and pathways to care for people at risk of psychotic disorders or experiencing first-episode psychosis: a systematic review. Psychol Med. 2017;47(11):1867–79. https://doi.org/10.1017/S0033291717000344 .
Rossman K, Salamanca P, Macapagal K. A qualitative study examining young adults’ experiences of disclosure and nondisclosure of LGBTQ identity to health care providers. J Homosex. 2017;64(10):1390–410. https://doi.org/10.1080/00918369.2017.1321379 .
Rees SM, Crowe M, Harris S. The lesbian, gay, bisexual and transgender communities’ mental health care needs and experiences of mental health services: an integrative review of qualitative studies. J Psychiat Mental Health Nurs. 2020;28(4):578–89. https://doi.org/10.1111/jpm.12720 .
Shipherd JC, Green KE, Abramovitz A. Transgender clients: identifying and minimizing barriers to mental health treatment. J Gay Lesbian Ment Health. 2010;14(2):94–108. https://doi.org/10.1080/19359701003622875 .
Hoening J, Kenna JC. The nosological position of transsexualism. Arch Sex Behav. 1974;3:273–87. https://doi.org/10.1007/BF01541490 .
Eliasson ET, McNamee L, Swanson L, Lawrie SM, Schwannauer M. Unpacking stigma: meta-analyses of correlates and moderators of personal stigma in psychosis. Clin Psychol Rev. 2021;89:102077. https://doi.org/10.1016/j.cpr.2021.102077 .
Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull. 2015;114(1):169–79. https://doi.org/10.1093/bmb/ldv017 .
De Lange J, Baams L, van Bergen D, Bos HMW, Bosker RJ. Minority stress and suicidal ideation and suicide attempts among LGBT adolescents and young adults: a meta-analysis. LGBT Health. 2022;9(4):222–37. https://doi.org/10.1089/lgbt.2021.0106 .
Skerrett DM, Kolves K, De Leo D. Are LGBT populations at higher risk for suicidal behaviours in Australia? Research findings and implications. J Homosex. 2015;62(7):883–901. https://doi.org/10.1080/00918369.2014.1003009 .
Strauss P, Cook A, Winter S, Watson V, Toussaint DW, Lin A. Trans Pathways: the mental health experiences and care pathways of trans young people: summary of results. Perth, Australia: Telethon Kids Institute. 2017. trans-pathways-report.pdf (telethonkids.org.au). Accessed 16 June 2023
DeLuca JS, Novacek DM, Adery LH, Herrera SN, Landa Y, Corcoran CM, et al. Equity in mental health services for youth at clinical high risk for psychosis: considering marginalized identities and stressors. Evid Based Pract Child Adolesc Ment Health. 2022;7(2):176–97. https://doi.org/10.1080/23794925.2022.2042874 .
Day JC, Bentall RP, Roberts C, Randall F, Rogers A, Cattell D, et al. Attitudes toward antipsychotic medication: the impact of clinical variables and relationships with health professionals. Arch Gen Psychiatry. 2005;62(7):717–24. https://doi.org/10.1001/archpsyc.62.7.717 .
Coyne CA, Poquiz JL, Janssen A, Chen D. Evidence-based psychological practice for transgender and non-binary youth: defining the need, framework for treatment adaptation, and future directions. Evid Based Pract Child Adolesc Ment Health. 2020;5(3):340–53. https://doi.org/10.1080/23794925.2020.1765433 .
Baker KE, Wilson LM, Sharma R, Dukhanin V, McArthur K, Robinson KA. Hormone therapy, mental health, and quality of life among transgender people: a systematic review. J Endocr Soc. 2021;5(4):bvab011. https://doi.org/10.1210/jendso/bvab011 .
Hughto JMW, Reisner SL. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgend Health. 2016;1(1):21–31. https://doi.org/10.1089/trgh.2015.0008 .
Wernick JA, Busa S, Matouk K, Nicholson J, Janssen A. A systematic review of the psychological benefits of gender-affirming surgery. Urol Clin North Am. 2019;46(4):475–86. https://doi.org/10.1016/j.ucl.2019.07.002 .
Bränström R, Packanhkis JE. Reductions in mental health treatment utilization among transgender individuals after gender-affirming surgeries: a total population study. Am J Psychiatry. 2019;177(8):727–34. https://doi.org/10.1176/appi.ajp.2019.19010080 .
Meijer JH, Eeckhout GM, van Vlerken RHT, de Vries ALC. Gender dysphoria and co-existing psychosis: review and four case examples of successful gender affirmative treatment. LGBT Health. 2017;4(2):106–14. https://doi.org/10.1089/lgbt.2016.0133 .
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. https://doi.org/10.1186/s12874-018-0611-x .
Munn Z, Pollock D, Khalil H, Alexander L, McInerney P, Godfrey CM, et al. What are scoping reviews? Providing a formal definition of scoping reviews as a type of evidence synthesis. JBI Evid Synth. 2022;20(4):950–2. https://doi.org/10.11124/JBIES-21-00483 .
Peters MDJ, Marnie C, Colquhoun H, Garritty CM, Hempel S, Horsley T, et al. Scoping reviews: reinforcing and advancing the methodology and application. Syst Rev. 2021;10(1):263. https://doi.org/10.1186/s13643-021-01821-3 .
Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z, editors. JBI Manual for Evidence Synthesis. JBI; 2024. https://synthesismanual.jbi.global . https://doi.org/10.46658/JBIMES-24-01
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350: g7647. https://doi.org/10.1136/bmj.g7647 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Barker TH, Stone JC, Sears K, Klugar M, Leonardi-Bee J, Tufanaru C, et al. Revising the JBI quantitative critical appraisal tools to improve their applicability: an overview of methods and the development process. JBI Evid Synth. 2023;21(3):478–93. https://doi.org/10.11124/JBIES-22-00125 .
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods programme. Lancaster University; 2006. https://doi.org/10.13140/2.1.1018.4643
Bach-Mortensen AM, Verboom B. Barriers and facilitators systematic reviews in health: a methodological review and recommendations for reviewers. Res Synth Methods. 2020;11(6):743–59. https://doi.org/10.1002/jrsm.1447 .
Download references
Acknowledgements
The authors would like to acknowledge the support of Ms Olivia Larobina, Scholarly Services Librarian (STEMM) at Deakin University, in the development of the search strategy.
CCG is funded by a Deakin University Postgraduate Research (DUPR) Scholarship. ZW is funded by a University of Western Australia Research Training Program (RTP) Scholarship. AL is supported by a National Health and Medical Research Council (NHMRC) Emerging Leaders Fellowship (2010063). LJW is supported by a NHMRC Emerging Leaders Fellowship (1174060). ARY is supported by a NHMRC Principal Research Fellowship (1136829). The funding providers had no role in the design and conduct of the study, or in the preparation, review, or approval of this manuscript.
Author information
Authors and affiliations.
Institute for Mental and Physical Health and Clinical Translation, Deakin University, Geelong, VIC, 3220, Australia
Cláudia C. Gonçalves, Shae E. Quirk, Peter M. Haddad, Lana J. Williams & Alison R. Yung
Telethon Kids Institute, University of Western Australia, Perth, WA, 6009, Australia
University Hospital Geelong, Barwon Health, Geelong, VIC, 3220, Australia
Peter M. Haddad
School of Population and Global Health, University of Western Australia, Perth, WA, 6009, Australia
Ashleigh Lin
School of Health Sciences, University of Manchester, Manchester, M13 9PL, UK
Alison R. Yung
You can also search for this author in PubMed Google Scholar
Contributions
CCG is the guarantor. CCG conceptualised the review, developed the study design, and drafted the manuscript. CCG, ZW, and SQ collaborated with OL (Scholarly Services Librarian) to develop the search strategy. All authors critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Cláudia C. Gonçalves .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
In the last 3 years, PMH has received honoraria for lecturing from Janssen, NewBridge Pharmaceuticals, and Otsuka and royalties from edited textbooks (Cambridge University Press, Oxford University Press).
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. prisma-p 2015 checklist. completed prisma-p checklist for this systematic review protocol., 13643_2024_2566_moesm2_esm.docx.
Additional file 2. Search Strategy. Detailed search strategy for this systematic review, including search terms and relevant controlled vocabulary terms for each included database.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gonçalves, C.C., Waters, Z., Quirk, S.E. et al. Barriers and facilitators to mental health treatment access and engagement for LGBTQA+ people with psychosis: a scoping review protocol. Syst Rev 13 , 143 (2024). https://doi.org/10.1186/s13643-024-02566-5
Download citation
Received : 04 July 2023
Accepted : 17 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s13643-024-02566-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Treatment access
- Treatment engagement
- Facilitators
- Clinical high risk
- Ultra-high risk
- Psychotic experiences
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 01 December 2022
The psychological impact, risk factors and coping strategies to COVID-19 pandemic on healthcare workers in the sub-Saharan Africa: a narrative review of existing literature
- Freddy Wathum Drinkwater Oyat 1 ,
- Johnson Nyeko Oloya 1 , 2 ,
- Pamela Atim 1 , 3 ,
- Eric Nzirakaindi Ikoona 4 ,
- Judith Aloyo 1 , 5 &
- David Lagoro Kitara ORCID: orcid.org/0000-0001-7282-5026 1 , 6 , 7
BMC Psychology volume 10 , Article number: 284 ( 2022 ) Cite this article
6038 Accesses
9 Citations
1 Altmetric
Metrics details
The ongoing COVID-19 pandemic has significantly impacted the physical and mental health of the general population worldwide, with healthcare workers at particular risk. The pandemic's effect on healthcare workers' mental well-being has been characterized by depression, anxiety, work-related stress, sleep disturbances, and post-traumatic stress disorder. Hence, protecting the mental well-being of healthcare workers (HCWs) is a considerable priority. This review aimed to determine risk factors for adverse mental health outcomes and protective or coping measures to mitigate the harmful effects of the COVID-19 crisis among HCWs in sub-Saharan Africa.
We performed a literature search using PubMed, Google Scholar, Cochrane Library, and Embase for relevant materials. We obtained all articles published between March 2020 and April 2022 relevant to the subject of review and met pre-defined eligibility criteria. We selected 23 articles for initial screening and included 12 in the final review.
A total of 5,323 participants in twelve studies, predominantly from Ethiopia (eight studies), one from Uganda, Cameroon, Mali, and Togo, fulfilled the eligibility criteria. Investigators found 16.3–71.9% of HCWs with depressive symptoms, 21.9–73.5% with anxiety symptoms, 15.5–63.7% experienced work-related stress symptoms, 12.4–77% experienced sleep disturbances, and 51.6–56.8% reported PTSD symptoms. Healthcare workers, working in emergency, intensive care units, pharmacies, and laboratories were at higher risk of adverse mental health impacts. HCWs had deep fear, anxious and stressed with the high transmission rate of the virus, high death rates, and lived in fear of infecting themselves and families. Other sources of fear and work-related stress were the lack of PPEs, availability of treatment and vaccines to protect themselves against the virus. HCWs faced stigma, abuse, financial problems, and lack of support from employers and communities.
The prevalence of depression, anxiety, insomnia, and PTSD in HCWs in sub-Saharan Africa during the COVID-19 pandemic has been high. Several organizational, community, and work-related challenges and interventions were identified, including improvement of workplace infrastructures, adoption of correct and shared infection control measures, provision of PPEs, social support, and implementation of resilience training programs. Setting up permanent multidisciplinary mental health teams at regional and national levels to deal with mental health and providing psychological support to HCWs, supported with long-term surveillance, are recommended.
Peer Review reports
Introduction
When coronavirus disease 2019 (COVID-19) was declared a pandemic in March 2020, healthcare workers (HCWs) globally and in sub-Saharan Africa (SSA) were unprepared for the scale of the physical and mental health devastation that was to follow [ 1 ]. The impact of the COVID-19 pandemic on healthcare workers has been profound, characterized by death, disability, and untenable burden on mental health and well-being [ 2 ]. Factors impacting their mental health include high risks of exposure and infection, financial insecurity, separation from loved ones, stigma, difficult triage decisions, stressful work environment, scarcity of supplies including personal protective equipment (PPEs), exhaustion, traumatic experiences due to regular witnessing of deaths among patients and colleagues [ 2 , 3 ]. Greenberg et al. [ 4 ] observed that the COVID-19 pandemic put healthcare professionals worldwide in an unprecedented situation, making difficult decisions to provide care for many severely ill patients with constrained or inadequate resources.
In almost all WHO regions, data indicates that infection rates among healthcare workers are higher than in the general population [ 5 ]. Scholars suggest that the end of the COVID-19 pandemic is not yet in sight. Neither are they sure about the virulence of the following variant when it appears as caseloads are still rising, with more than 621 million infections and 6.5 million deaths reported worldwide by 19th October 2022 [ 6 ]; mainly driven by the newer omicron variants. However, recently in October 2022, we received with gratitude a reassuring message from US President Biden declaring the end of the COVID-19 pandemic in the United States of America.
Meanwhile, previous studies found high levels of depression, anxiety, and PTSD in survivors among the general population and healthcare workers (HCWs) one-to-three years after the control of the SARS epidemic [ 7 ] and the 2014–2016 Ebola epidemic in West Africa [ 8 ]. In addition, recent surveys [ 9 , 10 , 11 , 12 , 13 , 14 ], reviews, and meta-analyses [ 15 , 16 , 17 , 18 ] are pointing to early evidence that a considerable proportion of healthcare workers have experienced stress, anxiety, depression, and sleep disturbances during the COVID-19 pandemic, raising concerns about risks to their long-term mental health.
Studies from the global north countries [ 19 , 20 ], UK [ 21 ], USA [ 22 ], and in India [ 23 ], and China [ 24 , 25 ] have shed light on the vulnerability that characterizes frontline healthcare workers during this pandemic, especially regarding their mental health and well-being. However, evidence in sub-Saharan Africa is scanty, and the pattern and prevalence of psychological disorders are not well understood.
Evidence from a systematic review by Pappa S et al. on 33,062 Chinese HCWs in April 2020 found a pooled prevalence rate of mental health problems among respondents; anxiety 23.2%, depression 22.8%, and insomnia 38.9% [ 26 ]. Similarly, Singapore study, Tan et al . [ 27 ], Li et al . [ 28 ], BMA [ 29 ] and in China [ 31 ] found high levels of psychological disorders among health workers.
Since the beginning of the pandemic, we found one systematic review involving 919 frontline HCWs, 3928 general HCWs, and 2979 medical students conducted in Africa from December 2019 to April 2020 [ 31 ]. The study by Chen J et al . reported a high prevalence of depression, anxiety, and insomnia among frontline HCWs in sub-Saharan Africa (SSA) at 45%, 51%, and 28%, respectively. In comparison, the prevalence of depression, anxiety, and insomnia among the general population was much lower at 30%, 31%, and 24%, respectively [ 31 ]. Furthermore, we found that only a few studies investigated protective and coping measures, given the many uncertainties surrounding the evolution of the COVID-19 pandemic [ 32 ]. Adequate data are needed to equip frontline HCWs and healthcare managers in sub-Saharan Africa to mitigate the medium and long-term adverse effects of the COVID-19 pandemic [ 33 ].
This review aimed to answer three questions (1) What is the psychological impact of the COVID-19 pandemic on HCWs in Sub-Saharan Africa?
(2) What are the associated risk factors during the COVID-19 pandemic?
(3) What interventions (mitigating and coping strategies) protect and support the mental health and well-being of HCWs during the ongoing crises and after the pandemic?
Methodology
Search methodology and article selection.
This current article is a mixed-method narrative review of existing literature on mental health disorders, risk factors, and interventions relevant to the COVID-19 pandemic on HCWs in sub-Saharan. A search on the PubMed electronic database was undertaken using the search terms "novel coronavirus", "COVID-19", "nCoV", "mental health", "psychiatry", "psychology", "anxiety", "depression" and "stress" in various permutations and combinations.
Search processes
We conducted a comprehensive literature search on original articles published from March 2020 to 30 April 2022 in electronic databases of Embase, PubMed, Google Scholar, and the daily updated WHO COVID-19 database. Our search terms included but were not limited to ('COVID-19'/exp OR COVID-19 OR 'coronavirus'/exp OR coronavirus) AND ('psychological'/exp OR psychological OR 'mental'/exp OR mental OR 'stress'/exp OR stress OR 'anxiety' OR anxiety OR 'depression' OR depression OR 'post-traumatic' OR 'post-traumatic'/exp OR 'trauma' OR 'trauma'/exp) OR Health care workers, medical workers of health care professionals, sub-Saharan Africa, for Embase. ("COVID-19" [All Fields] OR "coronavirus" [All Fields]) AND ("Stress, Psychological" [Mesh] OR "mental" OR "anxiety" OR "depression" OR "stress" OR "post-traumatic" OR "trauma") for PubMed, for the WHO COVID-19 database, and ("COVID-19" OR "coronavirus") AND ("Psychological" OR "mental" OR "anxiety" OR "depression" OR "stress" OR "post-traumatic" OR "trauma") for Google Scholar. On reviewing the above citations, twelve articles met the inclusion criteria relevant for this review and are in Table 1 . All twelve articles were cross-sectional, with one qualitative and the others quantitative observational studies.
Eligibility criteria
We included original qualitative and quantitative studies examining the risk factors, psychological impact of COVID-19 and coping strategies of healthcare workers (HCWs) in sub-Saharan Africa during the COVID-19 pandemic. We excluded studies if they were.
1. Not reported in the English language 2. Studies which were not primary research 3. Studies that had not been published in a peer-reviewed journal 4. Studies that did not include data on HCWs’ mental health or psychological well-being 5. Duplicate studies 6. not using validated instruments to measure the risks and psychological impact.
FWDO performed the search of articles. DLK reviewed the articles involving screening of titles, followed by examination of abstracts. The potential articles identified were further reviewed in full text to examine their eligibility. In addition, four of the authors independently reviewed the full articles to abstract the relevant data required for the review. Thereafter, a meeting to harmonise findings were done and presented in a report.
Data extraction and appraisal of the study
We extracted information from each study, including author, study population, year of publication, country, socio-demographic characteristics, sample size, response rate, gender proportion, age, and study time, areas assessed, the validated instrument used and the prevalence. The appraisal involved assessing the research design, recruitment of respondents, inclusion and exclusion criteria, reliability of outcome determination, statistical analyses, ethical compliance, strengths, limitations, and clinical implications of the articles.
Our review protocol was not registered on PROSPERO because of the significant variation in the methodologies of the articles used in the review. The results precluded using a meta-analytic approach and made a narrative review the most suitable for this work. In addition, we did not use the Cochrane Collaboration GRADE method to assess the quality of evidence of outcomes included in this narrative review. Instead, we used the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) 22 items checklist to gauge the quality of the twelve articles included in this review. We qualitatively validated the articles based on additional considerations namely study design, sample sizes, sampling procedures, response rates, statistical methods used, measures taken by the authors to deal with bias and confounding factors and ethical consideration.
Definition of healthcare worker (HCW)
For this narrative review, we adhered to the Centres for Disease Control and Prevention (CDC) definition of HCWs, which includes physicians, nurses, emergency medical personnel, dental professionals and students, medical and nursing students, laboratory technicians, pharmacists, hospital volunteers, and administrative staff [ 34 ].
Search results
The search found twenty-three studies of interest. Full texts of potentially relevant studies underwent eligibility assessment, and twelve articles met the inclusion criteria for this narrative review.
Study characteristics
The twelve articles comprised eleven quantitative and one qualitative study. The common mental health conditions assessed were depression, anxiety, perceived stress, and post-traumatic stress disorder (PTSD). The coping strategy, perceived health status, health distress (including burnout), insomnia, and perceived stigma were also assessed [ 35 , 36 ]. The total number of respondents in these studies was 5,323. The qualitative study had fifty respondents [ 35 ], while the most significant number of participants, 420 was recorded in one of the quantitative studies from Ethiopia [ 37 ]. The questionnaire response rates varied between 90%-100%, with most studies dominated by male respondents at 51.9%-69.2% [ 38 ]. Nurses were the commonest study population, followed by doctors, pharmacists, and laboratory technicians, and no study involved non-HCWs of facilities. Most papers utilized probability sampling procedures, and four quantitative studies used non-random sampling procedures limiting generalizability of their findings and increasing the risk of selection bias. Eight studies were from Ethiopia, and one was from Cameroon, Uganda, Mali, and Togo, respectively (Table 1 ). Most studies were conducted in urban tertiary public hospitals, university teaching hospitals, and rural and urban general hospitals, including primary care facilities operated by Non-Governmental Organizations (NGOs) for example in Mali [ 39 ]. Several validated tools assessed depression, anxiety, insomnia, stress, and PTSD (Table 1 ).
Table 1 provides an overview of the studies selected and validated instruments used to measure psychological disorders.
Table 2 provides comparisons with studies conducted outside of sub-Saharan Africa.
Table 3 provides information on studies showing the classification of psychological outcomes.
Table 4 are studies showing risk factors associated with psychological disorders.
Table 5 are studies that identified protective factors for psychological disorders.
Risks of bias and confounding factors
Most articles selected were cross-sectional studies that employed probability sampling procedures (Table 1 ). Cross-sectional study design minimized selection biases, but many used structured questionnaires, including online self-administered questionnaires, which increased bias due to social desirability. It was not clear how confounding variables were controlled in five papers reviewed [ 38 , 39 , 40 , 43 , 45 ] leading to excessive and perhaps inappropriate determination of associations.
Socio-demographic factors
In this review, the mean age of the respondents ranged between 23 and 35 years, and predominantly males. Age was associated with anxiety, and stress symptoms in 6(50%) of all the studies reviewed [ 35 , 37 , 40 , 41 , 42 , 44 ]. An age of over 40 years was associated with moderate to severe symptoms of PTSD. Two studies concluded that respondents aged over 40 years were more likely to develop PTSD symptoms than their younger counterparts [ 37 , 41 ].
Female gender was significantly associated with depression, anxiety, and stress symptoms among HCWs in seven studies reviewed [ 36 , 37 , 38 , 41 , 42 , 43 ]. Many studies found that being female, married, and a nurse were independent predictors of stress symptoms. Moreover, sex, age, marital status, type of profession, and working environment were significant factors for PTSD symptoms [ 37 , 41 ]. However, one study in Ethiopia found that the odds of depression were twice higher among male healthcare providers than among female healthcare providers [ 35 ].
Psychological impact on healthcare workers
Most studies reviewed directly assessed the prevalence of depression, anxiety, stress, insomnia, and PTSD in HCWs. Common causes of anxiety, fear, or psychological distress that health professionals reported were: lack of access to PPEs and other equipment, being exposed to COVID-19 at work and taking the infection home to their families, uncertainties that their organization will support/take care of their personal and family needs if they got infection, long working hours, death of colleagues, lack of social support, stigmatization, high rates of transmission and poor income [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. However, the prevalence of mental health symptoms exhibited great variations for example depressive symptoms were examined in nine studies [ 35 , 36 , 37 , 39 , 43 , 44 , 45 , 46 ], and varied between 16.3% and 71.9% among HCWs [ 38 , 39 ].
In addition, nine other studies reported high prevalence of anxiety symptoms among HCWs [ 35 , 36 , 37 , 40 , 43 , 44 , 45 , 46 , 47 ] which varied between 21.9% and 73.5% [ 36 , 39 ]. Five studies investigated HCWs' perceived stress during the pandemic; 15.5%-63.7% of HCWs reported high levels of work-related stress [ 35 , 36 , 37 , 43 , 45 ]. Three studies reported 12.4–77% of HCWs experienced sleep disturbances during the COVID-19 pandemic [ 37 , 39 , 40 ].
Post-traumatic stress disorder (PTSD) was in three studies [ 38 , 41 , 42 ], and the prevalence of PTSD-like symptoms varied between 51.6 and 56.8% in HCWs [ 38 , 41 ]. A qualitative study from Uganda reported high symptoms of depression, anxiety, and PTSD among HCWs [ 35 ]. Additionally, factors that increased the risk of PTSD symptoms were for example, working in emergency units and being frontline workers. Furthermore, many studies found that frontline HCWs had increased symptoms of mental disorders and being a frontline worker was an independent risk factor for depression, anxiety, and PTSD [ 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ].
Risk factors associated with adverse mental health outcomes
The qualitative study from Uganda reported the factors associated with mental disorder symptoms among HCWs. These were long working hours, lack of equipment (PPEs, testing kits), lack of sleep, exhaustion, high death rates, death of colleagues, and a high COVID-19 transmission rate among HCWs [ 35 ]. Lack of equipment (PPEs, ventilators, and testing kits), overworking, and lack of logistic support were in Ethiopian studies [ 36 , 37 , 38 , 39 , 40 , 41 , 42 , 45 ]. Most studies identified several risk factors for adverse mental health outcomes among respondents for example those with medical and mental illnesses, contacts with confirmed COVID-19 patients, and poor social support which were significantly associated with depression [ 42 , 43 ]. Other factors were females, nurses, married, frontline workers, ICU, emergency units, living alone, and lack of social support [ 35 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. Too, participants’ families with chronic illnesses, had contacts with confirmed COVID-19 cases, and poor social support were significantly associated with anxiety. Other risk factors associated with anxiety include exhaustion, long working hours, frontline workers, emergencies, nurses, pharmacists, laboratory technicians, married, older, younger, living alone, being female, working at general and referral hospitals, and perceived stigma. In addition, participants’ families with chronic illnesses, those who had contacts with confirmed COVID-19 cases, and those with poor social support were predictors of stress during the COVID-19 pandemic [ 37 , 38 , 40 , 41 , 42 , 43 , 45 ]. Other stress symptoms include having a medical illness, a mental illness, being a frontline worker, married, nurse, female, pharmacist, laboratory technician, physician, older age, lack of standardized PPE supply, low incomes, and living with a family [ 36 , 37 , 40 , 41 , 42 , 43 , 44 , 45 ]. Healthcare providers with low monthly incomes were significantly more likely to develop stress than those with high monthly incomes [ 38 ]. In addition, participants living alone, living with a family, and being married were associated with symptoms of psychological disorders among HCWs [ 36 , 37 , 38 , 45 ]. Overall, the risk factors for adverse psychological impacts are categorized in three thematic areas (i) occupational, (ii) psychosocial, and (iii) environmental aspects.
Occupational factors
Most studies showed that frontline HCWs, nurses, doctors, pharmacists, and laboratory technicians had significantly higher levels of mental health risks compared to non-frontline HCWs [ 35 , 36 , 37 , 38 , 40 , 42 , 43 , 45 ]. They experienced higher frequency of insomnia, anxiety, depression, and somatization than non-frontline medical HCWs. In contrast, Mali [ 39 ] and Cameroon [ 46 ] studies found a higher prevalence of depression, anxiety, and PTSD in non-frontline HCWs [ 39 , 46 ]. However, among HCWs, physicians were 20% less likely to develop mental health disorders than nurses, pharmacists, and laboratory technicians [ 39 ]. In addition, healthcare workers with low monthly incomes had higher symptoms of depression, anxiety, stress, and insomnia [ 37 ].
Healthcare groups
Five studies found that being a nurse was associated with worse mental disorders than doctors [ 36 , 37 , 40 , 44 , 45 ].
Frontline staff with direct contact with COVID-19
Most papers in the review found that being in a “frontline” position or having direct contact with COVID-19 patients was associated with higher level of psychological distress [ 35 , 36 , 37 , 38 , 40 , 42 , 43 , 45 ]. In addition, studies found that contact with COVID-19 patients was independently associated with an increased risk of sleep disturbances [ 40 , 46 ]. Moreover, HCWs who had contact with confirmed COVID-19 cases were more likely to develop depression, anxiety, and stress symptoms than those who had no contact with COVID-19 patients [ 36 , 37 , 38 , 43 , 45 ].
Lack of personal protective equipment (PPEs)
Most studies reported that the lack of PPEs was associated with higher symptoms of depression, anxiety, stress, and insomnia, while its availability was associated with fewer mental disorder symptoms [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ]. In Mali, workers from centres that provided facemasks were 51% less likely to suffer from depression, 62% less likely to develop anxiety, and 45% less likely to develop insomnia [ 39 ]. In Ethiopia, the odds of developing post-traumatic stress disorder were much higher among HCWs who did not receive standardized PPEs supplies than those who had [ 38 , 41 , 42 ]. In Uganda, the lack of PPEs was associated with depression, anxiety, and PTSD [ 35 ].
Heavy workload
Longer working hours, increased work intensity, increased patient load, and exhaustion were risk factors in Ugandan [ 35 ] and Ethiopian studies [ 36 ].
Psychosocial factors: perceived stigma and fear of infection
The fear of infection was in the qualitative study from Uganda [ 35 ], one quantitative study from Cameroon [ 47 ] and seven cross-sectional studies from Ethiopia [ 36 , 37 , 38 , 41 , 42 , 43 , 44 ]. Poor social support was associated with PTSD symptoms, depression, anxiety, and stress [ 35 , 36 , 37 , 38 , 42 , 43 ]. Two studies reported that HCWs with perceived stigmatization were more likely to suffer from depression, anxiety, stress, and PTSD [ 37 , 42 ].
family concerns
This came up as one of the main risk factors of stress in almost all studies, especially among those HCWs in direct contact with confirmed COVID-19 cases [ 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 ]. A family member suffering from COVID-19 was associated with poor mental health outcomes in HCWs [ 36 , 37 ].
Protective psychosocial factors
Two studies suggest a reduction of perceived stigma can be achieved by sensitization of communities about COVID-19 [ 37 , 42 ], and four studies recommend solid social support [ 36 , 37 , 42 , 43 ].
Safety of family
Family safety had the most significant impact in reducing stress. Safety from COVID-19 infection and financial protection of families were essential coping strategies for HCWs [ 35 , 36 ].
Underlying illnesses
We found three studies that reported an underlying medical and mental illness as an independent risk factor for poor psychological outcomes [ 42 , 43 , 45 ].
Protective factors against adverse mental health outcomes
The review identified protective factors to adverse mental health outcomes during COVID-19. The qualitative study from Uganda and four quantitative cross-sectional studies from Ethiopia identified some protective factors [ 35 , 38 , 41 , 42 , 45 ]. The protective factors are grouped under three thematic areas (i) occupational, (ii) psychosocial, and (iii) environmental aspects.
The qualitative study identified many social coping strategies among respondents, including family networks, community networks, help from family, responsibility to society, assistance from community members, availability of assistance from strangers, and the symbiotic nature of assistance in the community [ 35 ].
Protective occupational factors
Studies suggest that physicians suffered fewer mental health disorders partly because of their experience with previous epidemics [ 37 , 42 , 45 ].
Some necessary coping measures include good hospital guidance and ongoing training of frontline HCWs [ 37 , 42 , 45 ].
Adequate supply of PPEs
As mentioned above, PPE was a protective factor when adequate and a risk factor for poor mental health outcomes when deemed inadequate [ 35 , 36 , 37 , 42 , 43 ].
The COVID-19 pandemic has been an ongoing global public health emergency that has burdened healthcare workers' physical and mental well-being (HCWs) [ 1 , 5 ]. Our review confirms the enormous magnitude of mental health impact of COVID-19 on healthcare workers in sub-Saharan Africa, and it is widespread, with significant levels of depression, anxiety, distress, and insomnia; especially those working directly with COVID-19 patients at particular risk [ 34 , 35 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. Out of the twelve articles reviewed, eight studies (66%) came from Ethiopia, and this has implications on the results (Table 1 ). This finding indicates few research published to date on the psychological impact of the pandemic on the mental health of HCWs in sub-Saharan Africa; a subregion that the COVID-19 pandemic has severely impacted.
Overview of the study sites
Studies in this review were conducted predominantly in hospital settings. We found only one study relating to primary healthcare workers or facilities [ 38 ]. This finding is of concern, as there is increasing evidence that many non-frontline HCWs continue to suffer psychological symptoms long after the conclusion of infectious disease epidemics [ 7 , 8 ]. In addition, a significant mortality due to COVID-19 was due to excess morbidity, some of which were from primary care facilities. Given that this study is the first narrative review in sub-Saharan Africa, it would be helpful to briefly compare our findings with some published reviews and surveys from other regions (Table 2 ).
High prevalence of psychological disorders among participants
Investigators in this review found 16.3–71.9% HCWs with depressive symptoms, 21.9–73.5% had anxiety symptoms, 15.5–63.7% experienced work-related stress symptoms, 12.4–77% experienced sleep disturbances, and 51.6–56.8% PTSD symptoms [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. This high prevalence of mental health symptoms among HCWs in our review is consistent with previous reviews conducted early in the pandemic in sub-Saharan Africa [ 31 ], Asia [ 17 , 18 , 26 , 28 ], USA & Europe [ 15 , 16 ], and supported by a batch of cross-sectional studies globally [ 11 , 12 , 13 , 14 , 19 , 27 , 30 ]. We found mixed results with significant variations within and among regions and countries, as depicted in Tables 1 and 2 .
Risk factors of psychological disorders among participants
Studies established that HCWs responding to the COVID-19 pandemic in sub-Saharan Africa were exposed to long working hours, overworking, exhaustion, high risk of infection, and shortage of personal protective equipment (Tables 3 and 4 ). In addition, HCWs had deep fear, were anxious and stressed with the high transmission rate of the virus among themselves, high death rates among themselves and their patients, and lived under constant fear of infecting themselves and their families with obvious consequences [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. Some HCWs were deeply worried about the lack of standardized PPEs, known treatments and vaccines to protect against the virus. Many health workers had financial problems, lacked support from families and employers if they contracted the virus [ 34 , 35 , 36 , 37 , 39 , 40 , 41 , 42 , 44 ]. An additional source of fear and anxiety was the perceived stigma attached to being infected with COVID-19 by the public [ 36 , 41 ]. Studies found that HCWs, especially those working in emergency, intensive care units, infectious disease wards, pharmacies, and laboratories, were at higher risk of developing adverse mental health impacts compared to others [ 34 , 35 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 44 ]. This is supported by previous reviews [ 15 , 16 , 17 , 18 , 26 , 28 ] and cross-sectional studies [ 10 , 11 , 12 , 13 , 14 , 20 , 21 , 23 , 25 , 30 ]. However, findings were inconsistent on the impact of COVID-19 on frontline health workers, with ten studies [ 35 , 36 , 37 , 39 , 40 , 41 , 42 , 44 , 45 ] suggesting they are at higher risk than peers and two studies showing no significant difference in psychological disorders relating to the departments [ 38 , 43 ].
The Mali’s study was conducted exclusively in primary care facilities among HCWs not involved in treating COVID-19 cases but still registered a very high prevalence of depression 71.9%, anxiety 73.6%, and insomnia 77.0% [ 39 ]. In contrast, two studies conducted among HCWs at COVID-19 treatment facilities in Ethiopia [ 36 , 38 ] registered much lower prevalence of depression 20.2%, anxiety 21.0%, and insomnia12.4% [ 36 ], and 16.3%, 30.7% and 15.9% respectively, in the second study [ 38 ]. These findings show that not only frontline HCWs experienced mental health disorders during this pandemic but highlight the need for direct interventions for all HCWs regardless of occupation or workstation during this and future pandemics. The significant disparity in the studies could be due to structural, occupational, and environmental issues for example challenges faced by Mali's healthcare systems, characterized by acute equipment shortages, lack of PPEs, human resources, lack of trained and experienced HCWs, ongoing nationwide insecurity, and terrorism compared to Ethiopia. Therefore, local context needs to be considered as contributing factor to mental health disorders among HCWs.
Regional variations of psychological disorders
Tan et al . found a higher prevalence of anxiety among non-medical HCWs in Singapore [ 27 ]. As previously noted, the prevalence of poor psychological outcomes varied between countries. Compared to sub-Saharan Africa and China, data from India [ 23 ] and Singapore [ 27 ] revealed an overall lower prevalence of anxiety and depression than similar cross-sectional data from sub-Saharan Africa [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ] and China [ 9 , 25 , 30 ]. This finding suggests that different contexts and cultures may reveal different psychological findings and that, it is possible that being at different countries’ outbreak curve may play a part, as there is evidence that it is influential.
Tan et al . suggests that medical HCWs in Singapore had experienced a SARS outbreak and thus were well prepared for COVID-19 psychologically and infection control measures [ 27 ]. What can be deduced is that context and cultural factors play a role, not just the cadre or role of healthcare workers [ 16 ]. It also highlights the importance of reviewing evidence regularly as more data emerge from other countries.
One hospital in Ethiopia found that the thought of resignation was associated with higher chances of mental health disorders and that pharmacists and laboratory technicians who did not receive prior training exhibited higher symptoms of mental health disorders compared to others [ 36 ]. Work shift arrangement, considering a dangerous atmosphere presented by working in COVID-19 wards, was one which exacerbated or relieved mental health symptoms among HCWs, with shorter exposure periods being most beneficial [ 36 ]. Meanwhile, studies found that financial worries caused by severe lockdowns and erratic payment of salaries and allowances were also major stressors [ 35 ]. This finding is like studies in Pakistan [ 13 ] and China [ 30 , 32 ].
In this review, HCWs who had contact with confirmed COVID-19 patients were more affected by depression, anxiety, and stress than their counterparts who had not [ 35 , 36 , 37 , 40 , 41 , 43 , 45 ]. This finding is like previous reviews [ 15 , 16 , 17 , 18 , 26 , 28 , 31 ] and cross-sectional studies [ 9 , 10 , 11 , 12 , 13 , 14 , 21 , 23 , 24 , 25 , 27 , 30 ], which reported higher depression, anxiety, and psychological symptoms of distress in HCWs who were in direct contact with confirmed or suspected COVID-19 patients.
A study in Pakistan showed that 80% of participants expected the provision of PPE from authority [ 13 ], and 86% were anxious. Some respondents alluded to forced deployment, while in Mali, 73.3% were anxious, with the majority worrying about the shortage of nurses [ 39 ]. Therefore, prospects of being deployed at a workstation where one had not been trained or oriented contributed to fear among health workers. In the sub-Saharan African context, this scenario can best be represented in HCWs involved in internship who must endure hard work during their training. Tan et al . found that junior doctors were more stressed than nurses in Singapore [ 27 ].
Socio-demographic characteristics
Nearly all studies in our review suggest that socio-demographic variables for example age, gender, marital status, and living alone or with families contribute to the high mental disorder symptoms [ 35 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 44 ]. We, the authors suggest that these observations are handled cautiously as several investigators of these reviewed articles did not entirely control the influence of confounding variables. An alternative explanation for this study's findings may be the more significant risks of frontline exposure amongst women and junior HCWs, predominantly employed in lower-status roles, many of whom lacked experience and appropriate training within healthcare system globally. It is also important to note that respondents to all studies, when disaggregated by gender, and age, were predominantly younger or female, which may have impacted the outcomes of these findings [ 16 ]. In addition, the consistently higher mortality rates, and risk of severe COVID-19 disease amongst men would suggest that the complete picture regarding gender and mental health during this pandemic is still incomplete [ 16 ]. Moreover, in several studies, both younger and older age groups were equally affected by mental health symptoms but for different reasons. Cai et al . [ 32 ] in a Chinese study on HCWs for example observed that irrespective of age, colleagues' safety, self and families' safety, the lack of treatment for COVID-19 was a factor that induced stress in HCWs. Similarly, in our review, the lack of PPEs, high infection transmission rates, high death rates among HCWs, and the fear of infecting their families were the factors that induced stress in all HCWs [ 34 , 35 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ].
We, the authors propose that paying close attention to concerns of HCWs by employers would greatly relieve some stressors and contribute to increased mental well-being of participants. Compared with physicians, our review showed that nurses were more likely to suffer from depression, anxiety, insomnia, PTSD, and stress [ 35 , 37 , 39 , 40 , 41 , 44 , 45 ]. Workloads and night shifts in healthcare facilities, as well as contacts with risky patients, enhanced nurses' mental distress risks [ 15 , 16 , 17 , 18 , 26 , 27 , 28 ]. In addition, nursing staff have more extended physical contacts and closer interactions with patients than other professionals, providing round-the-clock care required by patients with COVID-19 and thus the increased risk [ 15 ]. On the one hand, we posit that most senior physicians are experienced and always keep well-informed with emerging medical emergencies. The majority become aware of emerging epidemic early and actively protect themselves from infections through regular scientific literature updates compared to their junior counterparts. Senior physicians also spend less time in emergency wards unless there is a need to conduct specific procedures which cannot be undertaken by senior housemen or general medical officers. Cai et al . [ 32 ] concluded that it is essential to have a high level of training and professional experience for healthcare workers engaging in public health emergencies, especially for the new staff. As a result, these findings highlight the importance of focusing on all the frontline HCWs sacrificing to contain the COVID-19 pandemic.
Regular monitoring of high-risk groups
There is a need to continue monitoring the high-at-risk groups, including nursing staff, interns, support staff, and all deployed in emergency wards. These high-at-risk groups should be encouraged to undertake screening, treatment, and vaccination to avoid the medium and long-term consequences of such epidemics [ 15 , 16 , 35 , 37 , 40 , 44 ].
Social support and coping mechanisms
The effect of social support and coping measures is in the qualitative study [ 34 ] and three other quantitative studies [ 36 , 41 , 42 ] which concluded that respondents with good social support were less likely to suffer from severe depression, anxiety, work-related stress, and PTSD. The qualitative study identified several coping measures, including community and organizational support, family, and community networks, help from family, responsibility to society, and assistance from community members and strangers, including the symbiotic nature of assistance in the community [ 35 ]. Other measures include providing accommodation and food to employees [ 35 ].
Interestingly, no study examined the association of resilience and self-efficacy with sleep quality, degrees of anxiety, depression, PTSD, and stress. However, a Chinese study by Cai et al. [ 32 ] suggests that the social support given to HCWs causes a reduction in anxiety and stress levels and increases their self-efficacy. In divergence, Xiao et al . [ 46 ] found no relationship between social support and sleep quality.
Only two studies in our review examined the effects of stigma on the mental health of HCWs [ 36 , 41 ] and found that HCWs with perceived stigma were more likely to be depressed, anxious, stressed, and prone to poor sleep quality [ 36 , 41 ]. We, the authors suggest that better community sensitization by creating public awareness involving appropriate local community structures and networks are essential. The broader community in sub-Saharan Africa may have suffered severely from infodemics with severe consequences on their mental health, especially during the difficult lockdowns. In addition, removing discrimination/inequalities at the workplace based on race and other social standings have a powerful influence on the mental health outcomes of HCWs. Also, because emotional exhaustion is long associated with depression, anxiety, and sleep disturbances, none of the studies in our review examined burnout as an essential component of mental health disorders in HCWs in sub-Saharan Africa.
Protective and coping measures
In this review we have provided evidence about personal, occupational, and environmental factors that were important protective and coping measures against psychological disorders. Based on these factors we suggest some protective and coping measures which can help to reduce the negative effects of the pandemic on mental health of HCWs in sub-Saharan Africa. Organizations and healthcare managers need to be aware that primary prevention is key to any successful interventions to contain and control any epidemic. This should take the form of planned regular training, orientation and continuing medical education grounded on proven infection control measures. These measures need to be backed up by timely provision of protective equipment, drugs, testing facilities, vaccines, isolation facilities, clinical and mental health support, and personal welfare of HCWs [ 35 , 36 , 37 , 42 , 45 ]. The effect of community and organizational support and coping measures was shown by the qualitative study [ 35 ] and five other quantitative studies [ 36 , 37 , 41 , 42 , 43 ] indicating that respondents who had good social and organizational support were less likely to suffer from severe depression, anxiety, work related stress and PTSD. Prior experience with comparable pandemics and training are suggested as beneficial coping strategies for healthcare workers during this pandemic but also local social structural and geopolitical conditions appear to determine the pattern and evolution of mental health symptoms among HCWs [ 14 , 15 , 31 , 32 , 47 ]. In our case the high prevalence of all mental health symptoms in non-frontline primary health care facilities in Mali [ 39 ] which was already plagued with instability and weak healthcare systems prior to the pandemic is a case in point. Results are particularly consistent in showing that provision of PPEs, testing kits, orientation training of workers, work shift arrangements, provision of online counselling, provision of food and accommodation and prompt payment of allowances by employers were important protective measures [ 35 , 36 , 37 , 38 , 39 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. The feeling of being protected is associated with higher work motivation with implication for staff turnover [ 35 , 38 , 43 , 45 ]. Hence, physical protective materials [ 14 ], together with frequent provision of information, should be the cornerstone of any interventions to prevent deterioration in mental health of HCWs (Table 5 ). Finally, provision of rest rooms, online consultation with psychologists/psychiatrists, protection from financial hardships, access to social amenities and religious activities are some important coping measures [ 35 , 36 , 38 , 42 , 45 ]. In this era of digital health care with plentiful internet and smartphones, organization can conduct online trainings, online mental health education, online psychological counselling services, and online psychological self-help intervention tailored to the needs of their HCWs [ 35 , 37 , 42 ]. In addition, it is essential to understand and address the sources of anxiety among healthcare professionals during this COVID-19 pandemic, as this has been one of the most experienced mental health symptoms [ 48 ]. Adequate protective equipment provided by health facilities is one of the most important motivational factors for encouraging continuation of work in future outbreaks. Furthermore, availability of strict infection control guidelines, specialized equipment, recognition of their efforts by facility management, government, and reduction in reported cases of COVID-19 provide psychological benefits [ 15 , 32 ]. Finally, we call upon Governments (the largest employers of HCWs) in sub-Saharan Africa to do what it takes to improve investments in the mental health of HCWs and plan proactively in anticipation of managing infectious disease epidemics, including other expected and unexpected disasters.
Future research direction
There was no study that examined the association of resilience and self-efficacy with sleep quality, degrees of anxiety, depression, PTSD, and stress. Although emotional exhaustion has long been associated with depression, anxiety, and sleep disturbances, no study in our review examined burnout as an important component of mental health disorders in HCWs in sub-Saharan Africa. The impacts of infodemics, stringent lockdown measures, discrimination/inequalities at workplaces based on race, and other social standings on mental health outcomes of HCWs need to be investigated.
Future studies are needed on the above including other critical areas like suicidality, suicidal ideations, and substance abuse during the COVID-19 pandemic. In addition, there is a significant variation of related literature calling for more rigorous research in future. More systematic studies will be required to clarify the full impact of the pandemic so that meaningful interventions can be planned and executed at institutional and national levels in the Sub-Saharan Africa.
Limitations of this study
There are some limitations to this study. First, most of the studies are from one country, limiting the generalizability of the results to the whole African continent. Second, all the studies were cross-sectional and only looked at associations and correlations. There is a need for prospective or retrospective cohort or case–control studies on this subject matter. Longitudinal research studies on the prevalence of mental disorders in the COVID-19 pandemic in the sub-Saharan Africa are urgently required. Third, most studies reviewed did not adequately examine protective factors or coping measures of the health workers in their settings. In addition, most studies did not pay strict attention to confounding variables which could have led to inappropriate results and conclusions. Fourth, most sample sizes were small and unlikely representative of the population and yet larger sample sizes would better identify the extent of mental health problems among health workers in the region. Fifth, depression, anxiety, and stress were assessed solely through self-administered questionnaires rather than face-to-face psychiatric interviews. Sixth, these studies employed various instruments and different cut-off thresholds to assess severity. Notably, the magnitude and severity of reported mental health outcomes may vary based on the validity and sensitivity of the measurement tools. Seventh, there was no mention of mental baseline information among the studied population and therefore it was unknown if the studied population had pre-existing mental health illnesses that decompensated during the pandemic crisis. Eight, investigators did not give much attention to stigma, burnout, resilience, and self-efficacy among study participants.
Furthermore, our review did not employ systematic reviews or meta-analyses methods for the information generated. This narrative review paper precluded deeper insight into the quality of reviewed articles for this paper. Still, our observation was that investigators did not consider the strict lockdown measures, quarantine, and isolation imposed by many countries in sub-Saharan Africa as possible risk factors for mental health disorders among HCWs.
Based on the articles reviewed, the prevalence of depression, anxiety, insomnia, and PTSD in HCWs in the sub-Saharan Africa during the COVID-19 pandemic is high. We implore health authorities to consider setting up permanent multidisciplinary mental health teams at regional and national levels to deal with mental health issues and provide psychological support to patients and HCWs, always supported with sufficient budgetary allocations.
Long-term surveillance is essential to keep track of insidiously rising mental health crises among community members. There is a significant variation of related literature thus calling for more rigorous research in the future. More systematic studies will be needed to clarify the full impact of the pandemic so that meaningful interventions can be planned better and executed at institutional and national levels in sub-Saharan Africa.
Availability of data and materials
Datasets analysed in the current study are available from the corresponding author at a reasonable request.
Abbreviations
Coronavirus disease 2019
Healthcare workers.
Mental health
Public health emergency
Personal protective equipment
World Health Organisation
World Health Organization. Coronavirus disease (COVID-19) outbreak. 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (Accessed 1 March 2020).
Veenema TG, Closser S, Thrul J. Mental Health, and Social Support for Healthcare and Hospital Workers During the COVID-19 Pandemic. Baltimore, MD: Johns Hopkins Center for Health Security; 2021.
Chersich MF, Gray G, Fairlie L. COVID-19 in Africa: care and protection for frontline healthcare workers. Global Health. 2020;16:46. https://doi.org/10.1186/s12992-020-00574-3Interventions .
Article PubMed PubMed Central Google Scholar
Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during a COVID-19 pandemic. BMJ. 2020;368: m1211. https://doi.org/10.1136/bmj.m1211 .
Article PubMed Google Scholar
WHO. Keep health workers safe to keep patients safe: WHO. 2020. https:// www.who.int/news/item/17-09-2020-keep-health-workers-safe-to-keep - patients-safe-who. Accessed 21 October 2020.
WHO. Weekly epidemiological update on COVID-19- 19 th October 2022. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---19-october-2022 .
Maunder R, Lancee W, Balderson K, Bennett J, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infect Dis. 2006;12(12):1924–32. https://doi.org/10.3201/eid1212.060584 .
Article Google Scholar
Jalloh MF, Li W, Bunnell RE. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. 2018;3: e000471. https://doi.org/10.1136/bmjgh-2017-000471 .
Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3): e14.
Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua lao dong wei sheng zhi ye bing za zhi = Zhonghua laodong weisheng zhiyebing zazhi. Chinese J Indus Hygiene Occup Dis. 2020;38:E001.
Google Scholar
Cai W, Lian B, Song X, Hou T, Deng G, Li H. A cross-sectional study on mental health among health care workers during the outbreak of coronavirus disease. Asian J Psychiatr. 2020. https://doi.org/10.1016/j.ajp.2020.102111 .
Elhadi M, Msherghi A, Elgzairi M, Alhashimi A, Bouhuwaish A, Biala M, Abuelmeda S, et al. Psychological status of healthcare workers during the civil war and COVID-19 pandemic: a cross-sectional study. J Psychosom Res. 2020;137: 110221.
Urooj U, Ansari A, Siraj A, Khan S, Tariq H. Expectations, fears, and perceptions of doctors during COVID-19 pandemic. Pak J Med Sci. 2020;36:S37–42. https://doi.org/10.12669/pjms.36.COVID19-S4.2643 .
Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Global Health. 2020;16(1):89. https://doi.org/10.1186/s12992-020-00621-z .
Preti E, Di Mattei V, Perego G. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. 2020;22(8):43. https://doi.org/10.1007/s11920-020-01166-z .
De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz SA, Ellis L, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. https://doi.org/10.1186/s12889-020-10070-3 .
Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and the general public. A systematic review and meta-analysis. Psychiatry Res. 2020;291:113190. https://doi.org/10.1016/j.psychres.2020.113190 .
Bareeqa SB, Ahmed SI, Samar SS, Yasin W, Zehra S, Monese GM, et al. Prevalence of depression, anxiety, and stress in china during COVID-19 pandemic: a systematic review with meta-analysis. Int J Psychiatry Med. 2021;56:210–27.
Søvold LE, Naslund JA, Kousoulis AA. Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front Public Health. 2021;9: 679397. https://doi.org/10.3389/fpubh.2021.679397 .
Consolo U, Bellini P, Bencivenni D, Iani C, Checchi V. Epidemiological aspects, and psychological reactions to COVID-19 of dental practitioners in the Northern Italy districts of Modena and Reggio Emilia. Int J Environ Res Public Health. 2020;17(10):3459. https://doi.org/10.3390/ijerph17103459 .
Gilleen J, Santaolalla A, Valdearenas L, Salice C, Fusté M. Impact of the COVID-19 pandemic on the mental health and well-being of UK healthcare workers. BJPsych Open. 2021;7(3): e88. https://doi.org/10.1192/bjo.2021.42 .
Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S, et al. psychological distress, coping behaviours, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1–8. https://doi.org/10.1016/j.genhosppsych.2020.06.007 .
Wilson W, Raj JP, Rao S, Ghiya M, Nedungalaparambil NM, Mundra H, et al. Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: a nationwide observational study. Indian J Psychol Med. 2020;42(4):353–8. https://doi.org/10.1177/0253717620933992 .
Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med. 2020. https://doi.org/10.1093/occmed/kqaa074 .
Kang L, Ma S, Chen M, Yang J, Wang Y, Li R. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020. https://doi.org/10.1016/j.bbi.2020.03.028 .
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behavi Immun. 2020. https://doi.org/10.1016/j.bbi.2020.05.026 .
Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020. https://doi.org/10.7326/M20-1083 .
Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety, and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PLoS One. 2021;16(3): e0246454. https://doi.org/10.1371/journal.pone.0246454 .
British Medical Association. The mental health and well-being of the medical workforce – now and beyond COVID-19. 2020. Available from URL: https://www.bma.org.uk/media/2475/bma-covid-19-and-nhs-staff-mental-healthwellbeing-report-may-2020.pdf .
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3): e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 .
Chen J, Farah N, Dong RK, Chen RZ, Xu W, Yin J, et al. Mental health during the COVID-19 crisis in Africa: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18:10604. https://doi.org/10.3390/ijerph182010604 .
Gupta S, Sahoo S. Pandemic, and mental health of the frontline healthcare workers: a review and implications in the Indian context amidst COVID-19. Gen Psychiatr. 2020;33(5): e100284. https://doi.org/10.1136/gpsych-2020-100284 .
Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. psychological impact, and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit. 2020;26:924171. https://doi.org/10.12659/MSM.924171 .
CDC. National Center for Immunization and Respiratory Diseases. CDC (2020) Available online at: https://www.cdc.gov/vaccines/adults/rec-vac/hcw.html .
Muzyamba C, Makova O, Mushibi GS. Exploring health workers’ experiences of mental health challenges during care of patients with COVID-19 in Uganda: a qualitative study. BMC Res Notes. 2021;14(1):286. https://doi.org/10.1186/s13104-021-05707-4 .
GebreEyesus FA, Tarekegn TT, Amlak BT, Shiferaw BZ, Emeria MS, Geleta OT, et al. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020: a multicentre cross-sectional study. PLoS One. 2021;16(11): e0259906. https://doi.org/10.1371/journal.pone.0259906 .
Mulatu HA, Tesfaye M, Woldeyes E. The prevalence of common mental disorders among health care professionals during the COVID-19 pandemic at a tertiary Hospital in East Africa. Med Rxiv. 2020. https://doi.org/10.1101/2020.10.29.20222430 .
Ayalew M, Deribe B, Abraham Y, Reta Y, Tadesse F, Defar S. Post-traumatic stress disorder symptoms and its predictors among healthcare workers following COVID-19 pandemic in Southern Ethiopia: a cross-sectional study. Front Psychiatry. 2021. https://doi.org/10.3389/fpsyt.2021.818910 .
Sagaon-Teyssier L, Kamissoko A, Yattassaye A, Diallo F, Castro DR, Delabre R, et al. Assessment of mental health outcomes and associated factors among workers in community-based HIV care centers in the early stage of the COVID-19 outbreak in Mali. Health Policy Open. 2020. https://doi.org/10.1016/j.hpopen.2020.100017 .
Kemal J. Psychological distress, early behavioral response, and perception toward the COVID-19 pandemic among health care workers in North Shoa Zone, Oromiya region. Front Psychiatry. 2020. https://doi.org/10.3389/fpsyt.2021.628898 .
Chekole YA, Minaye SY, Abate SM, Mekuriaw B. Perceived stress, and its associated factors during COVID-19 among healthcare providers in Ethiopia: a cross-sectional study. Adv Public Heal. 2020. https://doi.org/10.1155/2020/5036861 .
Asnakew S. Prevalence of post-traumatic stress disorder on health professionals in the era of COVID-19 pandemic, Northwest Ethiopia 2020: a multi-centred cross-sectional study. PLoS One. 2021;16(9):e0255340.
Asnakew S, Amha H, Kassew T. Mental health adverse effects of COVID-19 pandemic on health care workers in Northwest Ethiopia: a multicenter cross-sectional study. Neuropsychiatr Dis Treat. 2021;17:1375–84. https://doi.org/10.2147/NDT.S306300 .
Kounou KB, Guédénon KM, Foli AAD, Gnassounou-Akpa E. Mental health of medical professionals during the COVID-19 pandemic in Togo. Psychiatry Clin Neurosci. 2020;74:559–60.
Ayalew MB. Prevalence and determinant factors of mental health problems among healthcare professionals during COVID-19 pandemic in southern Ethiopia: a multicentre cross-sectional study. BMJ Open. 2021. https://doi.org/10.1136/bmjopen-2021-057708 .
Keubo FRN, Mboua PC, Tadongfack TD, Tchoffo EF, Tatang CT, Zeuna JI, et al. psychological distress among health care professionals of the three COVID-19 most affected Regions in Cameroon: Prevalence and associated factors. In: Annales Médico-Psychologiques, Revue Psychiatrique; Elsevier Masson: Paris, France. 2021;179:141–146.
Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. https://doi.org/10.12659/MSM.923549 .
Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among healthcare professionals during the COVID-19 pandemic. JAMA. 2020. https://doi.org/10.1001/jama.2020.5893 .
Download references
Acknowledgements
We thank Uganda Medical Association Acholi-branch members for the financial assistance which enabled the team to conduct this study successfully.
Author information
Authors and affiliations.
Uganda Medical Association (UMA), UMA-Acholi Branch, Gulu City, Uganda
Freddy Wathum Drinkwater Oyat, Johnson Nyeko Oloya, Pamela Atim, Judith Aloyo & David Lagoro Kitara
Moroto Regional Referral Hospital, Moroto, Uganda
Johnson Nyeko Oloya
St. Joseph’s Hospital, Kitgum District, Uganda
Pamela Atim
ICAP at Columbia University, Freetown, Sierra Leone
Eric Nzirakaindi Ikoona
Rhites-N, Acholi, Gulu City, Uganda
Judith Aloyo
Faculty of Medicine, Department of Surgery, Gulu University, P.O. Box 166, Gulu City, Uganda
David Lagoro Kitara
Harvard University, Cambridge, USA
You can also search for this author in PubMed Google Scholar
Contributions
FWDO, JA, JNO, ENI and DLK searched and screened studies and extracted data from selected articles. FWDO wrote the first draft of the manuscript, and all authors reviewed and edited the final draft. All authors approved the final version of the manuscript.
Corresponding author
Correspondence to David Lagoro Kitara .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
All authors declare no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Oyat, F.W.D., Oloya, J.N., Atim, P. et al. The psychological impact, risk factors and coping strategies to COVID-19 pandemic on healthcare workers in the sub-Saharan Africa: a narrative review of existing literature. BMC Psychol 10 , 284 (2022). https://doi.org/10.1186/s40359-022-00998-z
Download citation
Received : 03 September 2022
Accepted : 22 November 2022
Published : 01 December 2022
DOI : https://doi.org/10.1186/s40359-022-00998-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- COVID-19 pandemic
- Social support
- Occupational health and safety
- Mental health surveillance
- Workplace organization
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Splenic Embolism in Infective Endocarditis: A Systematic Review of the Literature with an Emphasis on Radiological and Histopathological Diagnoses
Affiliations.
- 1 Department of Medicine, Universidade do Grande Rio/Afya (UNIGRANRIO/Afya), Barra da Tijuca, Rio de Janeiro 22775-003, Rio de Janeiro, Brazil.
- 2 Instituto Nacional de Cardiologia, Rio de Janeiro 22240-006, Rio de Janeiro, Brazil.
- 3 Instituto Nacional de Infectologia Evandro Chagas, Fiocruz, Rio de Janeiro 21040-360, Rio de Janeiro, Brazil.
- PMID: 38668544
- PMCID: PMC11053958
- DOI: 10.3390/tropicalmed9040083
Infective endocarditis (IE) is characterised by fever, heart murmurs, and emboli. Splenic emboli are frequent in left-sided IE. A systematic review of the literature published on splenic embolism (SE) between 2000 and 2023 was conducted. Search strategies in electronic databases identified 2751 studies published between 1 January 2000 and 4 October 2023, of which 29 were finally included. The results showed that the imaging tests predominantly used to detect embolisms were computed tomography (CT), magnetic resonance imaging, positron emission tomography (PET)/CT, single-photon emission computed tomography/CT, ultrasound, and contrast-enhanced ultrasound. More recent studies typically used 18 F-FDG PET-CT. The proportion of SE ranged from 1.4% to 71.7%. Only seven studies performed systematic conventional CT screening for intra-abdominal emboli, and the weighted mean frequency of SE was 22% (range: 8-34.8%). 18 F-FDG PET-CT was performed systematically in seven studies, and splenic uptake was found in a weighted mean of 4.5%. There was a lack of uniformity in the published literature regarding the frequency and management of splenic embolisation. CT scans were the most frequently used method, until recently, when 18 F-FDG PET-CT scans began to predominate. More data are necessary regarding the frequency of SE, especially focusing on their impact on IE management and prognosis.
Keywords: computed tomography; embolism; endocarditis; histopathology; imaging; pathology; positron emission tomography; spleen; splenic emboli; tomography.
PubMed Disclaimer
Conflict of interest statement
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Peripheral splenic embolus on non-contrasted…
Peripheral splenic embolus on non-contrasted CT scan, wedge-shaped, subcapsular, from a patient with…
Large splenic abscesses in a…
Large splenic abscesses in a patient on chronic haemodialysis with Enterococcus faecalis aortic…
Flowchart for selecting publications based…
Flowchart for selecting publications based on search strategies 1 and 2; years 2000–2021.
Flowchart for selecting publications based on search strategies 1 and 2; years 2021–2023.
Similar articles
- Diagnostic value of 18 F-FDG PET/CT in infective endocarditis. Anton-Vazquez V, Cannata A, Amin-Youssef G, Watson S, Fife A, Mulholland N, Gunning M, Papachristidis A, MacCarthy P, Baghai M, Deshpande R, Khan H, Byrne J, Dworakowski R. Anton-Vazquez V, et al. Clin Res Cardiol. 2022 Jun;111(6):673-679. doi: 10.1007/s00392-021-01975-z. Epub 2021 Nov 25. Clin Res Cardiol. 2022. PMID: 34821999
- Diagnosis of Infective Endocarditis by Subtype Using 18 F-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography: A Contemporary Meta-Analysis. Wang TKM, Sánchez-Nadales A, Igbinomwanhia E, Cremer P, Griffin B, Xu B. Wang TKM, et al. Circ Cardiovasc Imaging. 2020 Jun;13(6):e010600. doi: 10.1161/CIRCIMAGING.120.010600. Epub 2020 Jun 8. Circ Cardiovasc Imaging. 2020. PMID: 32507019
- 18 F-fluorodeoxyglucose positron emission tomography/computed tomography for the diagnosis of native valve infective endocarditis: A prospective study. Philip M, Delcourt S, Mancini J, Tessonnier L, Cammilleri S, Arregle F, Martel H, Oliver L, Hubert S, Renard S, Camoin L, Casalta AC, Casalta JP, Gouriet F, Riberi A, Lepidi H, Collart F, Raoult D, Drancourt M, Habib G. Philip M, et al. Arch Cardiovasc Dis. 2021 Mar;114(3):211-220. doi: 10.1016/j.acvd.2020.10.005. Epub 2021 Jan 22. Arch Cardiovasc Dis. 2021. PMID: 33495137
- Diagnostic Accuracy of 18F-FDG PET/CT in Infective Endocarditis and Implantable Cardiac Electronic Device Infection: A Cross-Sectional Study. Granados U, Fuster D, Pericas JM, Llopis JL, Ninot S, Quintana E, Almela M, Paré C, Tolosana JM, Falces C, Moreno A, Pons F, Lomeña F, Miro JM; Hospital Clinic Endocarditis Study Group. Granados U, et al. J Nucl Med. 2016 Nov;57(11):1726-1732. doi: 10.2967/jnumed.116.173690. Epub 2016 Jun 3. J Nucl Med. 2016. PMID: 27261514 Review.
- 18 F-FDG-PET/CT Imaging to Diagnose Septic Emboli and Mycotic Aneurysms in Patients with Endocarditis and Cardiac Device Infections. Mikail N, Benali K, Mahida B, Vigne J, Hyafil F, Rouzet F, Le Guludec D. Mikail N, et al. Curr Cardiol Rep. 2018 Mar 6;20(3):14. doi: 10.1007/s11886-018-0956-0. Curr Cardiol Rep. 2018. PMID: 29511975 Review.
- Habib G., Hoen B., Tornos P., Thuny F., Prendergast B., Vilacosta I., Moreillon P., Antunes M.d.J., Thilen U., Lekakis J., et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): The Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC) Eur. Heart J. 2009;30:2369–2413. - PubMed
- Baddour L.M., Wilson W.R., Bayer A.S., Fowler V.G., Jr., Tleyjeh I.M., Rybak M.J., Barsic B., Lockhart P.B., Gewitz M.H., Levison M.E., et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals from the American Heart Association. Circulation. 2015;132:1435–1486. doi: 10.1161/CIR.0000000000000296. - DOI - PubMed
- Holland T.L., Baddour L.M., Bayer A.S., Hoen B., Miro J.M., Fowler V.G. Infective endocarditis. Nat. Rev. Dis. Primers. 2016;2:16059. doi: 10.1038/nrdp.2016.59. - DOI - PMC - PubMed
- Delgado V., Ajmone Marsan N., de Waha S., Bonaros N., Brida M., Burri H., Caselli S., Doenst T., Ederhy S., Erba P.A., et al. 2023 ESC Guidelines for the management of endocarditis. Eur. Heart J. 2023;44:3948–4042. doi: 10.1093/eurheartj/ehad193. - DOI - PubMed
- Habib G., Lancellotti P., Antunes M.J., Bongiorni M.G., Casalta J.-P., Del Zotti F., Dulgheru R., El Khoury G., Erba P.A., Iung B., et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC) Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM) Eur. Heart J. 2015;36:3075–3128. - PubMed
Publication types
- Search in MeSH
Related information
Grants and funding.
- 2023-2025/Fundação Pró Coração/FUNDACOR
LinkOut - more resources
Full text sources.
- PubMed Central

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Systematic Review
- Open access
- Published: 11 June 2024
The effectiveness of visual-based interventions on health literacy in health care: a systematic review and meta-analysis
- Elisa Galmarini ORCID: orcid.org/0009-0002-7083-7896 1 ,
- Laura Marciano ORCID: orcid.org/0000-0002-8034-3227 2 &
- Peter Johannes Schulz ORCID: orcid.org/0000-0003-4281-489X 1 , 3
BMC Health Services Research volume 24 , Article number: 718 ( 2024 ) Cite this article
Metrics details
Limited Health Literacy (HL) is an obstacle to accessing and receiving optimal health care and negatively impacts patients’ quality of life, thus making it an urgent issue in the health care system. Visual-based interventions are a promising strategy to improve HL through the use of visual aids and pictorial materials to explain health-related concepts. However, a comprehensive summary of the literature on the topic is still scarce.
To fill this gap, we carried out a systematic review and meta-analysis with the aim to determine the effectiveness of visual-based interventions in improving comprehension of health related material in the clinical population. Independent studies evaluating the effectiveness of visual-based interventions on adults (> 18 years) and whose primary outcome was either health literacy (HL) or comprehension were eligible for the review. After a systematic literature search was carried out in five databases, 28 studies met the inclusion criteria and thus were included. Most of the studies were randomized controlled trials and they focused on HL and health knowledge as outcomes.
The review and meta-analysis showed that visual-based interventions were most effective in enhancing the comprehension of health-related material compared to traditional methods. According to meta-analytic results, videos are more effective than traditional methods (Z = 5.45, 95% CI [0.35, 0.75], p < 0.00001) and than the employment of written material (Z = 7.59, 95% CI [0.48, 0.82], p < 0.00001). Despite this, no significant difference was found between video and oral discussion (Z = 1.70, 95% CI [-0.46, 0.53], p = 0.09).
Conclusions
We conclude that visual-based interventions, particularly the ones using videos, are effective for improving HL and the comprehension of health-related material.
Peer Review reports
Health literacy (HL) is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [ 1 ]. Limited HL has been described as an obstacle to accessing healthcare [ 2 ] and it negatively impacts the patient’s quality of life and health outcomes. Hence, it represents an urgent issue in the health care system. Prevalence of low HL levels are still high in Europe where 33% to 50% of people cannot comprehend basic health information [ 3 ]. This percentage increases in the United States, where only 12% of people shows a proficient level of HL [ 4 , 5 ]. On the other hand, the prevalence of limited HL in Southeast Asian countries floats from 35.1% to 75.6%, with an average of 55.3% [ 6 ]. Limited HL negatively affects the healthcare system as a whole, including the use of resources and the economic burden. For example, limited HL is associated with non-adherence to pre-operative guidance and leads to detrimental health behaviors, including unhealthy lifestyles, drug abuse, and tobacco smoking [ 7 , 8 ]. Berkman and colleagues [ 9 ] summarized the results of 96 studies and reported that limited HL is consistently associated with higher hospitalization rates, indiscriminate usage of the emergency department, low medication adherence, and failure to use preventive medicine services (i.e., cancer screening and vaccines). Limited HL often results in the misuse of resources and, consequently, wastes economic assets. For example, in the systematic review by Eichler and colleagues [ 10 ], summarizing ten studies, the costs associated with limited HL represented 3–5% of the overall expenditure covered by the healthcare systems in Switzerland and the United States. According to the authors, an individual with poor HL incurs an additional health expense ranging between $143 and $7.798 each year compared to a person with adequate HL. Hence, due to the high prevalence of limited HL in the population and its impact on societies and healthcare costs at large, there is an increasing need to address this gap by using more efficient methods to adapt medical materials to patients’ needs and abilities and, hence, to improve their knowledge.
In this regard, visual-based interventions are encouraging approaches to address limited HL due to their applicability and promising results [ 11 ]. The Centers for Disease Control and Prevention defines these interventions as “images, videos, and similar tools used to communicate information about a specific topic and to simplify the comprehension process” [ 12 ]. The advantages of using visual-based tools have already been documented in 1971, when Allan Paivio elaborated the Dual Coding Theory [ 13 , 14 ] according to which the double encoding procedures reinforce the stimulus generated by visual cues. Images are encoded via multiple pathways, as they are simultaneously processed by the sensory and the verbal systems. In contrast, written words are only encoded by the verbal system. Since multiple systems are involved in elaborating visual materials, the “picture superiority effect” has been a key in facilitating comprehension and understanding [ 13 , 14 ]. A qualitative synthesis performed in 2006 revealed that pictorial aids effectively enhanced patients’ comprehension of medications and treatments [ 15 ].
Furthermore, a systematic review of 52 studies reported significant improvements in understanding health-related materials among patients provided with audio-visual cues compared to standard methods like written information sheets or oral discussions with physicians [ 16 ]. However, this latter review focused on a broad range of interventions rather than visual-based ones. Furthermore, Lee and colleagues [ 17 ] reported that using icons, color codes, and larger font sizes improved health outcomes regarding hypertension, heart failure, and hypercholesterolemia among patients with limited HL. More recently, a scoping review was mapped the existing studies on digital video interventions for mental health literacy among young people, underlying the importance of studying these interventions and the initial stage in mapping the literature [ 18 ].
Although the literature provides a consistent number of independent studies on the effectiveness of visual-based intervention in improving the comprehension of health-related materials, systematic reviews on this topic are still scarce, while a meta-analysis is entirely lacking. Hence, the present study aims to systematically and meta-analytically summarize the scientific literature on the effectiveness of visual-based interventions in improving HL and the comprehension of health-related information in the adult population. Based on this contextual information, EG, LM and PS, formulated the research question in PICO format: In an adult population (P), composed of either healthy or not impaired individuals (P), what is the effect of the usage of visual-based intervention (I) in improving comprehension of health related materials (O) compared to standard methods of information delivery (C), through a systematic review and metanalysis investigating the effectiveness of these intervention (S). In doing so, we hypothesized that (i) visual-based interventions would effectively improve HL and the comprehension of health-related materials among adult patients. Also, we expect that (ii) patients who receive health information through more interactive material (e.g., videos) would report higher levels of comprehension than standard methods of information delivery (e.g., oral discussion or written information).
The systematic review and meta-analysis was performed according to current PRISMA guidelines [ 19 ]. EG, LM and PS determined the most appropriate databases to conduct the literature search. Various databases were evaluated in order to ensure comprehensive coverage of relevant literature. As a result, five databases were used to perform a literature search on March 22nd: Behavioral Science Collection, CINHAL, Communication and Mass Media Complete, MEDLINE, and PsychInfo. EG and LM developed the list of keywords tailored to the research objectives. PS revised and approved them ensuring alignment with the study’s aim. The search terms covered two key topics: “visual intervention” and “health literacy”. The Boolean Operators “OR” and “AND” were used to divide keyterms within and between the two categories, respectively (see Table S 1 in the Appendix for the complete list of keywords). Additionally, EG carried out a handsearch in Google Scholar on April 14th by entering selected keywords and reviewing the first 100 entries of each combination. EG performed the selection procedure between March 23rd and April 20th.
Eligibility criteria
Studies were included in the systematic review and meta-analysis according to inclusion criteria previously defined by the authors. In particular, a study has to (1) be written in English and published in a peer-reviewed journal, (2) focus on visual-based intervention within the health-care setting, (3) include an adult population (≥ 18 years), (4) include either healthy or individuals from a clinical setting, and (5) use a measure of HL or comprehension of health related material as the outcome. No restriction was applied to the visual type or to the disease or healthcare area under investigation. Additionally, studies reporting a result convertible into an effect size were further included in the meta-analysis. A study was excluded if: (1) it investigated other interventions than visual aids, (2) the study population was composed of individuals under 18 years, (3) the study population consisted of adults on behalf of minors or impaired individuals, (4) HL or comprehension was not explicitly stated as outcomes, and (5) if the language differed from English. Duplicates, dissertations, books, magazines, reviews, editorial material, letters, and retracted publications were also excluded.
Data collection
For each included publication, EG extrapolated the following information: title, author(s)’s name, year of publication, health-care area (that was further divided into health promotion, health prevention, disease management, and consent or risk management), disease under investigation, study design, geographical location, description of the setting, the final number of participants, sample characteristics (i.e., age, gender, ethnic group), type of visual-based intervention, comparators such as standard methods of information delivery (written information sheet, oral discussion with doctor), outcome measure, the definition of HL (if present), and a brief description of the results.
Risk of bias assessment
The quality of the included studies was evaluated according to a selection of items from the Cochrane Risk of Bias assessment (RoB2) [ 20 ]. In particular, each article was evaluated for the procedure under which subjects were assigned to study arms (selection bias), the extent to which participants and researchers were aware of the allocation process (performance bias), the management of missing data (attrition bias) and the methods employed for measuring the outcome (detection bias) [ 20 ]. A single coder (EG) performed this assessment on Review Manager 5 (RevMan 5.4.1).
Data analysis
The meta-analysis was performed on RevMan 5.4.1. EG, LM, and PS contributed to the analysis and interpretation of data. The team used a standardized mean difference to calculate the effect size. Cut-off levels of Hedge’s g were set at 0.2, 0.5, and 0.8 for small, medium, and large effect sizes, respectively [ 21 ]. The inconsistency index (I 2 ) was used to measure heterogeneity across studies [ 21 ]. In order to interpret the results of the I 2 , the following standard cut-off values were set: an I 2 comprised between 0 and 40% (low) represented no significant difference across studies, whereas an I 2 greater than 75% indicated considerable heterogeneity; the interval in between was interpreted as either moderate or substantial differences between studies [ 21 ].
Characteristics of included studies
The literature search in the databases and hand search returned 3060 results. Out of these, 442 were duplicates, dissertations, books, and reviews and hence were excluded. Then, titles and abstracts of 2592 entries were screened, ending in 68 records eligible for full-text screening. Throughout the screening of titles and abstracts, a significant number of studies were deemed ineligible for inclusion. The predominant reasons for exclusion were the lack of measurement of the outcome of our interest, namely the comprehension of health related material and, more frequently, a predominant focus on ophthalmologic conditions or pathologies related to the visual system, a bias likely introduced by specific keywords within the search string pertaining to the domain of visual interventions. Among these, 28 studies met the inclusion criteria and were then included in the systematic review. Out of these, ten studies reported data convertible into effect sizes and were then included in the meta-analysis. The selection process is represented in the PRISMA flowchart (see Fig. 1 ).

PRISMA flowchart
Description and design of included studies
The current systematic review is based on 28 studies [ 11 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 ]. The characteristics of the included studies are reported in the Appendix (Table S2).
The total number of participants included in the studies was 5347, with sample sizes of individual studies ranging from 31 to 821 participants (Fig. S 1 ). Included studies reported an equal distribution in terms of males (53.36%) and females (45.46%), whereas one study did not report gender information [ 45 ] (Fig. S2). The mean age of participants in the included studies was 53.8 ± 12.1 years, ranging from a minimum of 33.7 to a maximum of 74 years (Figs. S3 and S4). Only few studies provided information regarding participants’ educational level ( n = 19) or ethnic group ( n = 9). Among these, 50.7% had less than a high school degree, whereas 22.25% and 27.04% had a high school diploma or more, respectively (Fig. S5). Information regarding the ethnic group was available for 1451 participants, among which 50.52% were Caucasian, 17.44% were Hispanic, 25.78% were African-American, and 0.83% were Asian. The remaining 5.44% represented study participants for whom the ethnic group differed from those mentioned above (Fig. S6).
All the studies were randomized clinical trials (RCTs) except for three. Among the RCTs, two adopted a randomized cross-over study design [ 32 , 48 ]. Whereas, within non-RCTs, two adopted a quasi-experimental design [ 29 , 40 ] and one a pre-post study design [ 25 ] (Fig. S7).
The majority of the studies ( n = 14) were conducted in North America (U.S. and Canada) and Oceania ( n = 6). In contrast, fewer studies were conducted in Europe ( n = 4), Asia ( n = 3), and Africa ( n = 1) (Figs. S8 and S9). The effectiveness of the visual-based intervention was evaluated on context-specific material; evaluated information covered topics such as informed consent ( n = 18), health prevention ( n = 8), and disease management ( n = 2). Medical areas of interest were equally distributed among the following categories: “surgery” ( n = 8) [ 28 , 32 , 36 , 38 , 41 , 42 , 44 , 45 ], “cancer” ( n = 8) [ 11 , 25 , 27 , 29 , 30 , 34 , 46 ] and “procedure” ( n = 8) [ 22 , 23 , 26 , 33 , 37 , 43 , 47 , 48 ]. The latter included colonoscopy, contrast administration, prostate vaporization, and urological and laser treatment, whereas cardiovascular diseases were investigated in four studies [ 24 , 31 , 35 , 39 ].
Description of visual-based interventions
The preferred format for visual-based intervention was the video ( n = 20), followed by multimedia-based presentations ( n = 3), graphs ( n = 1), and a booklet combined with either a video ( n = 2), a multimedia-based presentation ( n = 1), or a mind map ( n = 1). The types of visual cues and their frequencies are summarized in the Appendix (Table S3). The average length of the video, calculated on 17 studies, was 10.88 ± 7.347 min (ranging from 2 to 30 min). Information regarding the language used in the videos was provided only in two studies, including English, Spanish, and Kiswahili [ 25 ]. If not reported, a local or national language was likely used.
The reading level of the video material was provided in three studies, and it was equal to 8th [ 26 , 43 ] or 7th grade [ 41 ]. Concerning the multimedia-based presentation of material, it was impossible to determine the material’s average length: two studies reported data with different units of measurement, minutes [ 28 ] or just the number of slides [ 32 ] whereas the others did not disclose any information regarding the length of the material. Similarly, the reading level was provided only in one study, which was 7th grade [ 32 ].
Likewise, it was not possible to provide aggregated data on the length and reading level of the booklet format. The units of measurement, reported only in two studies, were not homogeneous: 18 min [ 46 ], 12 pages [ 11 ], and 2407 words [ 30 ]. Eventually, a mind map ( n = 1) and a graph ( n = 1) were the least represented formats. However, there was a lack of informative data concerning these strategies.
Description of outcome measures
Comprehension of health related material was the primary investigated outcome. However, this variable was measured differently across studies and included studies usually assessed patients’ level of comprehension through questionnaires explicitly developed for the study. Questionnaires were in the format of multiple choice ( n = 10), true/false questions ( n = 9), combined approach (multiple choice + true/false) ( n = 2), and in some cases, computational questions, which required individuals to perform basic mathematical tasks regarding the health-related topic. However, it is worth noting that some studies ( n = 6) did not disclose any information concerning the type of assessment. The individual’s level of comprehension was generally obtained by summing up the scores attributed to each correct answer. Occasionally, the final score was converted into a percentage. Furthermore, besides comprehension, three studies [ 11 , 27 , 47 ] measured participants’ level of HL with validated instruments: Test of Functional Health Literacy Ability – shortened (S-TOFHLA), Brief Health Literacy Scale (BHLS), Newest Vital Sign (NVS) and Rapid Estimate of Adult Literacy in Medicine (REALM) (Table S4).
Results of the systematic review
Overall, visual-based interventions were generally described as an effective instrument for enhancing the comprehension of health-related material compared to traditional methods (e.g., written material). In particular, in fourteen studies out of 22 (20 video-only + 2 videos combined with booklet) that adopted video material, participants in the intervention group (video format) had significantly higher comprehension levels than those in the control group (traditional method). Among the remaining six studies, two reported improvements in the level of comprehension after exposure to both video and standard material. However, the difference between the study arms was still not significant.
Among the studies that adopted multimedia-based presentation ( n = 3), two registered a significant difference between study arms and showed a higher comprehension level than the control group. Instead, no significant difference was found in a study evaluating the effectiveness of charts (bar graph). Eventually, among the studies evaluating the effectiveness of booklets ( n = 4), only one reported that participants provided with such format had higher comprehension levels than those provided with either leaflets or videos.
Meta-analytic results
Different meta-analyses were performed to compare video effectiveness to traditional information delivery methods. Due to the paucity of available data, studies including formats like multimedia-based presentations, charts, booklets, and mind maps were excluded. Also, among the studies adopting videos as a visual intervention tool ( n = 20), some were removed due to the lack of data regarding mean and standard deviation ( n = 9) or the study design ( n = 1). As a result, ten studies were included in the meta-analyses for a total of 1784 participants. Three meta-analyses were performed in order to compare videos with (1) traditional methods, (2) written communication, and (3) verbal discussion with the doctor.
The comprehension level was significantly higher among participants who received a video than those provided with traditional methods. In particular, a medium effect size was found when comparing video materials with the standard method of information delivery (without discrimination of the type) (k = 10, Hedge’s g = 0.55, 95% CI [0.35, 0.75], p < 0.001, see Fig. 2 ).

Meta-analysis: video vs traditional methods
Similarly, a medium effect size was also found in the case of videos compared to written information (k = 5, Hedge’s g = 0.65, 95% CI, [0.48, 0.82], p < 0.001, see Fig. 3 ).

Meta-analysis: video vs. written information
Conversely, no significant difference was found when videos were compared only to oral discussion with the doctor (k = 6, Hedge’s g = 0.36, 95% CI, [-0.06, 0.77], p = 0.09, see Fig. 4 ).
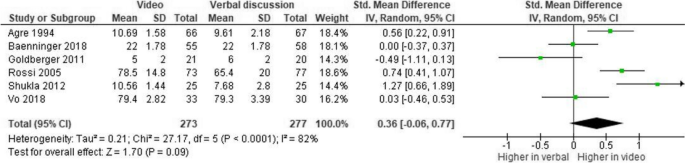
Meta-analysis: video vs. oral discussion
The level of heterogeneity was considerably high across the three meta-analyses. The former and the last meta-analysis reported high levels of inconsistency ( I 2 = 69%, p = 0.0006 and I 2 = 82%, p < 0.0001). Instead, the inconsistency index was not significant in the second meta-analysis ( I 2 = 33%, p = 0.20). These results could be due to substantial differences in sample sizes, study design, the material used for the intervention, topic of interest, medical area investigated, and the use of different measures to assess patients’ levels of comprehension.
Risk of bias
In general studies showed a low risk of bias, except for the selection bias, for which a small proportion of studies ( n = 4) is stated to be unclear. This result is mainly due to the study design: two studies [ 29 , 34 ] adopted a quasi-experimental approach and one a pre-post study design [ 25 ]. The remaining study was evaluated as medium risk of bias because of significant baseline differences between the study arms, which may indicate failure in the randomisation process. The good quality of the studies is mainly related to homogenous setting, the possibility to immediately assess the outcome soon after the intervention and the objectivity in the measurement, which avoided outcome assessors to provide a personal and subjective evaluation.
The current systematic review aims to evaluate the effectiveness of visual-based interventions to improve patients’ HL and levels of comprehension of health related material. To our knowledge, this is the first attempt to systematically and meta-analytically summarize evidence on the performance of these tools in the context of HL and knowledge of health information. According to qualitative results, visual-based interventions generally represented an effective way to improve comprehension of health-related information. However, their effectiveness mainly depends on the format employed. In particular, out of the 28 included studies, the most favorable evidence is provided by the studies that used videos as intervention tools ( n = 20). More than half reported a significant increase in participants’ levels of comprehension.
Compared with traditional methods, participants provided with video material showed higher comprehension levels, with medium effect size, than those with standard oral or written material. In line with the Dual Coding Theory [ 14 ], the effectiveness of visual-based interventions is mainly due to their increased interactivity [ 49 ] and reduced reading efforts [ 50 ]. Indeed, conversely to traditional communication strategies, visual tools involve greater patient participation [ 51 ]. For instance, more interactivity is conveyed by quizzes and short games embedded in some visual tools, thus augmenting comprehension [ 52 ]. This is in line with previous research on the effect of interactivity on comprehension and attitude in the healthcare context [ 53 ], according to which the level of interactivity predicted patient comprehension. Even the absence of words, either partial or total, may have contributed to significant improvements in the outcome. Functional HL, a basic component of HL which includes basic skills of reading and numeracy [ 54 ], dramatically impacts an individual’s ability to understand and appraise health-related material. Indeed, visual cues require less effort to be processed and recalled than written information; this may make information more accessible and comprehensible to those with limited HL [ 50 ]. Eventually, the effectiveness of these instruments could be explained by referring to the Dual Coding Theory [ 14 ]. Our results further show that the “picture superiority effect” owned by visual cues allows distinguishing these tools from more traditional methods (i.e., written communication) since the multimedia content embedded into these tools (i.e., video, images, audio) was subjected to a double encoding process [ 14 ], which in turn allowed the stimulus to be consolidated, thus improving the comprehension and recall of the information.
However, the difference was no longer significant when the video format was confronted with an oral discussion with a physician. The lack of a significant difference between video and verbal discussion could be attributed to the benefits of face-to-face consultations, such as the possibility to interpret non-verbal messages [ 55 ] and directly assess patient’s comprehension level [ 56 ]. Non-verbal communication is essential in the doctor-patient interaction [ 57 ]. Thanks to the possibility of perceiving patients’ emotional states through the analysis of gestures, postures, and mimics, the physician can adjust the conversation to make the patient feel more confident with the information received in terms of content and form. In practice, the doctor may avoid complex medical terminology to reduce cognitive efforts on behalf of the patient and simplify the comprehension process [ 56 , 58 ]. Similar strategies, like the “teach-back method” [ 56 ], involve the immediate assessment of the patient’s level of comprehension. Adopting such solutions might have noticeably reduced the gap in comprehension between the intervention (video) and control group (oral discussion), which eventually resulted in a non-significant difference. Hence, oral discussion with a doctor may represent a valuable and complementary intervention to be implemented for patients with low health literacy.
Finally, some remaining studies reported increases between pre-and post-intervention, though not significant. In particular, concerning multimedia-based presentations, two studies out of three registered a significant difference between the intervention and control groups. However, due to the low number of studies included in this category, it is not accurate to conclude that multimedia-based presentations are valuable tools for improving comprehension of medical material. Conversely, charts were ineffective. However, their use was investigated by only one study. Hence, future studies are needed to better explore the effectiveness of multimedia material in addition to the video.
Based on these findings, we encourage the adoption of visual tools for medical information purposes to set up innovative, effective, and fair communication. Nevertheless, we call for more research reporting more details on these interventions' characteristics, graphical layouts, and designs. Also, more research is needed regarding different medical areas and contexts, chronic and acute illnesses, and mental health problems.
Limitations
The present study has some limitations. First, the lack of validated scales for measuring comprehension of medical material might have introduced biases in the analyses and augmented the heterogeneity of the meta-analytic results. Indeed, each of the included studies measured the outcome through different scales. The heterogeneity found could also be attributed to variations in sample size and participants’ characteristics, including age, gender, ethnicity, and educational level. Second, included studies were not equally distributed across the different types of visual interventions. As a result, we could not draw robust conclusions on the effectiveness of some tools (i.e., charts, booklets, and mind maps). Third, included studies were mainly from limited geographical regions. Only a few were conducted in low- and middle-income countries, where adopting such instruments may represent an effective tool to improve people’s well-being and state of health [ 59 ]. Moreover, the absence of studies from South America may represent a methodological and research bias, that may have significantly limited the landscape of the included studies. Additionally, our study might be limited due to the lack of consideration of specific terms related to interactive visual resources (e.g., video). Hence, we suggest that future studies should include detailed descriptions of visual- and video- based interventions.
Finally, we call for future research to develop specific comprehension scales to increase and facilitate comparability across studies. Moreover, more data are needed to compare the mere use of videos with the combination of video and oral discussion, since adopting this mixed approach is a promising strategy for improving, even more, the comprehension of medical material. Finally, it would be useful to investigate the effectiveness of visual-based intervention in different clinical settings and populations, including young people. Antelo and colleagues [ 60 ] investigated the health literacy of women in Argentina regarding Human Papilloma Virus (HPV) after using a mobile counseling app and found that a mobile app is a good tool to help HPV-positive women by providing information and reducing fears [ 60 ]. Lee and colleagues [ 61 ] analyzed the effect of user-centered mHealth intervention apps (e.g., Click to Connect , PLANET MassCONECT, and SmartPhone App for Public Health ) to inform future work regarding app designing in Massachusetts and found that one of the critical features that increase HL among underserved communities is to design apps with usability, readability, and navigability in mind. Indeed, the vast majority of the studies in the review regarded the informed consent process, whereas publications on disease management and health prevention are still scarce. Regarding the need to investigate the effectiveness of similar instrument in other domains and population, Ito-Jaeger and collegues, in their scoping review on 17 studies, illuminated the effectiveness of digital video interventions as powerful tool in enhancing mental health literacy among young individuals [ 18 ].
Visual-based interventions are effective tools for improving patients’ levels of comprehension. In particular, the adoption of video formats significantly augments comprehension compared to more traditional methods. However, no additional benefits were found compared to the oral discussion with a physician. Future studies should investigate whether the combination of these methods (visual-based intervention + oral discussions with a physician) is more effective than the simple provision of the video format.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
Health Literacy
Test of Functional Health Literacy Ability Shortened
Brief Health Literacy Scale
Newest Vital Sign
Rapid Estimate of Adult Literacy in Medicine
*=articles included in the systematic review
Ratzan S, Parker R, Selden C, Zorn M. National library of medicine current bibliographies in medicine: health literacy. Bethesda: National Institutes of Health; 2000.
Google Scholar
Levy H, Janke A. Health literacy and access to care. J Health Commun. 2016;21(Suppl 1):43–50. https://doi.org/10.1080/10810730.2015.1131776 .
Article PubMed PubMed Central Google Scholar
Baccolini V, Rosso A, Di Paolo C, Isonne C, Salerno C, Migliara G, Prencipe GP, Massimi A, Marzuillo C, De Vito C, Villari P, Romano F. What is the prevalence of low health literacy in European Union Member States? A systematic review and meta-analysis. J Gen Intern Med. 2021;36(3):753–61. https://doi.org/10.1007/s11606-020-06407-8 .
Article CAS PubMed PubMed Central Google Scholar
Kutner M, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006–483. In National Center for Education Statistics. ED Pubs, P. 2006. https://eric.ed.gov/?id=ED493284 .
Lopez C, Kim B, Sacks K. Health literacy in the United States: enhancing assessments and reducing disparities. SSRN. 2022. https://doi.org/10.2139/ssrn.4182046 .
Article Google Scholar
Rajah R, Hassali MAA, Murugiah MK. A systematic review of the prevalence of limited health literacy in Southeast Asian countries. Public Health. 2019;167:8–15. https://doi.org/10.1016/j.puhe.2018.09.028 .
Article CAS PubMed Google Scholar
Chew LD, Bradley KA, Flum DR, Cornia PB, Koepsell TD. The impact of low health literacy on surgical practice. Am J Surg. 2004;188(3):250–3. https://doi.org/10.1016/j.amjsurg.2004.04.005 .
Article PubMed Google Scholar
Cho YI, Lee SYD, Arozullah AM, Crittenden KS. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med. 2008;66(8):1809–16. https://doi.org/10.1016/j.socscimed.2008.01.003 .
Berkman N, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011 https://www.acpjournals.org/doi/10.7326/0003-4819-155-2-201107190-00005 .
Eichler K, Wieser S, Brügger U. The costs of limited health literacy: A systematic review. Int J Public Health. 2009;54(5):313. https://doi.org/10.1007/s00038-009-0058-2 .
Housten AJ, Kamath GR, Bevers TB, Cantor SB, Dixon N, Hite A, Kallen MA, Leal VB, Li L, Volk RJ. Does animation improve comprehension of risk information in patients with low health literacy? A randomized trial. Med Decis Making. 2020;40(1):17–28. https://doi.org/10.1177/0272989X19890296 .
CDC. Visual Communication resources for health-related materials. Centers for disease control and prevention. https://www.cdc.gov/healthliteracy/developmaterials/visual-communication.html . Accessed 29 April 2021.
Crutcher RJ, Beer JM. An auditory analog of the picture superiority effect. Mem Cognit. 2011;39(1):63–74. https://doi.org/10.3758/s13421-010-0015-6 .
Paivio A. Imagery and verbal processes. Psychology Press. 2013. https://doi.org/10.4324/9781315798868 .
Katz MG, Kripalani S, Weiss BD. Use of pictorial aids in medication instructions: A review of the literature. Am J Health Syst Pharm. 2006;63(23):2391–7. https://doi.org/10.2146/ajhp060162 .
Glaser J, Nouri S, Fernandez A, Sudore RL, Schillinger D, Klein-Fedyshin M, Schenker Y. Interventions to improve patient comprehension in informed consent for medical and surgical procedures: an updated systematic review. Med Decis Making. 2020;40(2):119–43. https://doi.org/10.1177/0272989X19896348 .
Lee TW, Lee SH, Kim HH, Kang SJ. Effective intervention strategies to improve health outcomes for cardiovascular disease patients with low health literacy skills: a systematic review. Asian Nurs Res. 2012;6(4):128–36. https://doi.org/10.1016/j.anr.2012.09.001 .
Ito-Jaeger S, Perez Vallejos E, Curran T, Spors V, Long Y, Liguori A, ... & Crawford P. Digital video interventions and mental health literacy among young people: a scoping review. J Ment Health. 2022;31(6):873–883.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, … Moher D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021; 372: n71. https://doi.org/10.1136/bmj.n71
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions. 2019; 205–228. John Wiley & Sons, Ltd. https://doi.org/10.1002/9781119536604.ch8 .
Deeks JJ, Higgins JP, Altman DG, & Group, on behalf of the C. S. M. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions. 2019;241–284. John Wiley & Sons, Ltd https://doi.org/10.1002/9781119536604.ch10 .
* Agre P, Kurtz RC, Krauss BJ. A randomized trial using videotape to present consent information for colonoscopy. Gastrointest Endosc. 1994;40(3):271–6. https://doi.org/10.1016/s0016-5107(94)70054-0 .
* Baenninger PB, Faes L, Kaufmann C, Reichmuth V, Bachmann LM, Thiel MA. Efficiency of video-presented information about excimer laser treatment on ametropic patients’ knowledge and satisfaction with the informed consent process. J Cataract Refract Surg. 2018;44(12):1426–30. https://doi.org/10.1016/j.jcrs.2018.07.052 .
Bowers N, Eisenberg E, Montbriand J, Jaskolka J, Roche-Nagle G. Using a multimedia presentation to improve patient understanding and satisfaction with informed consent for minimally invasive vascular procedures. Surgeon. 2017;15(1):7–11. https://doi.org/10.1016/j.surge.2015.09.001 .
Cooper EC, Maher JA, Naaseh A, Crawford EW, Chinn JO, Runge AS, Lucas AN, Zezoff DC, Bera KR, Dinicu AI, White KM, Tewari SE, Hari A, Bernstein M, Chang J, Ziogas A, Pearre DC, Tewari KS. Implementation of human papillomavirus video education for women participating in mass cervical cancer screening in Tanzania. Am J Obstet Gynecol. 2021;224(1):105.e1–105.e9. https://doi.org/10.1016/j.ajog.2020.07.018 .
Cowan EA, Calderon Y, Gennis P, Macklin R, Ortiz C, Wall SP. Spanish and English video-assisted informed consent for intravenous contrast administration in the emergency department: A randomized controlled trial. Ann Emerg Med. 2007; 49(2):221–230, 230.e1–3. https://doi.org/10.1016/j.annemergmed.2006.07.934 .
Donelle L, Hoffman-Goetz L, Gatobu S, Arocha JF. Comprehension of Internet-based numeric cancer information by older adults. Inform Health Soc Care. 2009;34(4):209–24. https://doi.org/10.3109/17538150903358552 .
Ellett L, Villegas R, Beischer A, Ong N, Maher P. Use of a multimedia module to aid the informed consent process in patients undergoing gynecologic laparoscopy for pelvic pain: Randomized controlled trial. J Minim Invasive Gynecol. 2014;21(4):602–11. https://doi.org/10.1016/j.jmig.2014.01.002 .
Frosch DL, Légaré F, Mangione CM. Using decision aids in community-based primary care: A theory-driven evaluation with ethnically diverse patients. Patient Educ Couns. 2008;73(3):490–6. https://doi.org/10.1016/j.pec.2008.07.040 .
Gattellari M, Ward JE. A community-based randomised controlled trial of three different educational resources for men about prostate cancer screening. Patient Educ Couns. 2005;57(2):168–82. https://doi.org/10.1016/j.pec.2004.05.011 .
* Goldberger JJ, Kruse J, Kadish AH, Passman R, Bergner DW. Effect of informed consent format on patient anxiety, knowledge, and satisfaction. Am Heart J. 2011;162(4):780-785.e1. https://doi.org/10.1016/j.ahj.2011.07.006 .
Gyomber D, Lawrentschuk N, Wong P, Parker F, Bolton DM. Improving informed consent for patients undergoing radical prostatectomy using multimedia techniques: A prospective randomized crossover study. BJU Int. 2010;106(8):1152–6. https://doi.org/10.1111/j.1464-410X.2010.09309.x .
Ham DY, Choi WS, Song SH, Ahn YJ, Park HK, Kim HG, Son H. Prospective randomized controlled study on the efficacy of multimedia informed consent for patients scheduled to undergo green-light high-performance system photoselective vaporization of the prostate. World J Mens Health. 2016;34(1):47–55. https://doi.org/10.5534/wjmh.2016.34.1.47 .
* Ilic D, Egberts K, McKenzie JE, Risbridger G, Green S. Informing men about prostate cancer screening: A randomized controlled trial of patient education materials. J Gen Intern Med. 2008;23(4):466–71. https://doi.org/10.1007/s11606-007-0466-z .
* Lattuca B, Barber-Chamoux N, Alos B, Sfaxi A, Mulliez A, Miton N, Levasseur T, Servoz C, Derimay F, Hachet O, Motreff P, Metz D, Lairez O, Mewton N, Belle L, Akodad M, Mathivet T, Ecarnot F, Pollet J, … INFOCORO investigators. Impact of video on the understanding and satisfaction of patients receiving informed consent before elective inpatient coronary angiography: A randomized trial. Am Heart J. 2018; 200:67–74. https://doi.org/10.1016/j.ahj.2018.03.006 .
* Lin YK, Chen CW, Lee WC, Cheng YC, Lin TY, Lin CJ, Shi L, Tien YC, Kuo LC. Educational video-assisted versus conventional informed consent for trauma-related debridement surgery: A parallel group randomized controlled trial. BMC Med Ethics. 2018;19(1):23. https://doi.org/10.1186/s12910-018-0264-7 .
Luck A, Pearson S, Maddern G, Hewett P. Effects of video information on precolonoscopy anxiety and knowledge: A randomised trial. Lancet (London, England). 1999;354(9195):2032–5. https://doi.org/10.1016/s0140-6736(98)10495-6 .
Mason V, McEwan A, Walker D, Barrett S, James D. The use of video information in obtaining consent for female sterilisation: A randomised study. BJOG. 2003;110(12):1062–71.
* Mazor KM, Baril J, Dugan E, Spencer F, Burgwinkle P, Gurwitz JH. Patient education about anticoagulant medication: Is narrative evidence or statistical evidence more effective? Patient Educ Couns. 2007;69(1–3):145–57. https://doi.org/10.1016/j.pec.2007.08.010 .
Nagamma T, Ashok L, Konuri A, Chandrasekaran V. Effectiveness of audio-visual and print media intervention on knowledge of cervical health among rural women in Southern India. Niger Postgrad Med J. 2020;27(4):343–7. https://doi.org/10.4103/npmj.npmj_148_20 .
Rossi M, McClellan R, Chou L, Davis K. Informed consent for ankle fracture surgery: Patient comprehension of verbal and videotaped information. Foot Ankle Int. 2004;25(10):756–62. https://doi.org/10.1177/107110070402501011 .
* Rossi MJ, Guttmann D, MacLennan MJ, Lubowitz JH. Video informed consent improves knee arthroscopy patient comprehension. Arthroscopy. 2005;21(6):739–743 https://doi.org/10.1016/j.arthro.2005.02.015 .
Shaw MJ, Beebe TJ, Tomshine PA, Adlis SA, Cass OW. A randomized, controlled trial of interactive, multimedia software for patient colonoscopy education. J Clin Gastroenterol. 2001;32(2):142–7. https://doi.org/10.1097/00004836-200102000-00010 .
* Shukla AN, Daly MK, Legutko P. Informed consent for cataract surgery: Patient understanding of verbal, written, and videotaped information. J Cataract Refract Surg. 2012;38(1):80–4. https://doi.org/10.1016/j.jcrs.2011.07.030 .
* Vo TA, Ngai P, Tao JP. A randomized trial of multimedia-facilitated informed consent for cataract surgery. Clinical Ophthalmology (Auckland, N.Z.). 2018; 12, 1427–1432. https://doi.org/10.2147/OPTH.S150670 .
Volk RJ, Jibaja-Weiss ML, Hawley ST, Kneuper S, Spann SJ, Miles BJ, Hyman DJ. Entertainment education for prostate cancer screening: A randomized trial among primary care patients with low health literacy. Patient Educ Couns. 2008;73(3):482–9. https://doi.org/10.1016/j.pec.2008.07.033 .
Walker D, Adebajo A, Heslop P, Hill J, Firth J, Bishop P, Helliwell PS. Patient education in rheumatoid arthritis: The effectiveness of the ARC booklet and the mind map. Rheumatology (Oxford). 2007;46(10):1593–6. https://doi.org/10.1093/rheumatology/kem171 .
Winter M, Kam J, Nalavenkata S, Hardy E, Handmer M, Ainsworth H, Lee WG, Louie-Johnsun M. The use of portable video media vs standard verbal communication in the urological consent process: A multicentre, randomised controlled, crossover trial. BJU Int. 2016;118(5):823–8. https://doi.org/10.1111/bju.13595 .
Patwardhan M, Murthy S. When does higher degree of interaction lead to higher learning in visualizations? Exploring the role of ‘Interactivity Enriching Features.’ Comput Educ. 2015;82:292–305. https://doi.org/10.1016/j.compedu.2014.11.018 .
Dewan P. Words versus pictures: leveraging the research on visual communication. Partnership Can J Lib Info Pract Res. 2015;10(1). https://doi.org/10.21083/partnership.v10i1.3137
Lajoie SP, Azevedo R. Teaching and learning in technology-rich environments. In: Handbook of educational psychology. Mahwah (New Jersey): Lawrence Erlbaum Associates Publishers; 2006. p. 803–21.
Chou C. Interactivity and interactive functions in web-based learning systems: A technical framework for designers. Br J Edu Technol. 2003;34(3):265–79. https://doi.org/10.1111/1467-8535.00326 .
Lustria MLA. Can interactivity make a difference? Effects of interactivity on the comprehension of and attitudes toward online health content. J Am Soc Inform Sci Technol. 2007;58(6):766–76. https://doi.org/10.1002/asi.20557 .
Schulz PJ, Nakamoto K. Health literacy and patient empowerment in health communication: The importance of separating conjoined twins. Patient Educ Couns. 2013;90(1):4–11. https://doi.org/10.1016/j.pec.2012.09.006 .
Roter DL, Frankel RM, Hall JA, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. J Gen Intern Med. 2006;21(1):28–34. https://doi.org/10.1111/j.1525-1497.2006.00306.x .
Oates DJ, Paasche-Orlow MK. Health literacy: Communication strategies to improve patient comprehension of cardiovascular health. Circulation. 2009;119(7):1049–51. https://doi.org/10.1161/CIRCULATIONAHA.108.818468 .
Silverman J, Kinnersley P. Doctors’non-verbal behaviour in consultations: Look at the patient before you look at the computer. Br J Gen Pract. 2010;60(571):76–8. https://doi.org/10.3399/bjgp10X482293 .
Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61(2):173–90. https://doi.org/10.1016/j.pec.2005.05.004 .
McCool J, Dobson R, Whittaker R, Paton C. Mobile health (mHealth) in low- and middle-income countries. Annu Rev Public Health. 2022;43(1):525–39. https://doi.org/10.1146/annurev-publhealth-052620-093850 .
Sanchez Antelo V, Szwarc L, Paolino M, Saimovici D, Massaccesi S, Viswanath K, Arrossi S. A Counseling mobile app to reduce the psychosocial impact of human papillomavirus testing: formative research using a user-centered design approach in a low-middle-income setting in Argentina. JMIR Form Res. 2022;6(1):e32610. https://doi.org/10.2196/32610 .
Lee EW, McCloud RF, Viswanath K. Designing effective eHealth interventions for underserved groups: five lessons from a decade of eHealth intervention design and deployment. J Med Internet Res. 2022;24(1):e25419. https://doi.org/10.2196/25419 .
Download references
Acknowledgements
Not applicable.
This work was partially supported by the Swiss National Science Foundation under Grant P500PS_202974.
Author information
Authors and affiliations.
Faculty of Communication, Culture & Society, Università Della Svizzera Italiana (University of Lugano), Lab, Office 201 (Level 2), Via Buffi 13, 6900, Lugano, Switzerland
Elisa Galmarini & Peter Johannes Schulz
Harvard T.H. Chan School of Public Health and Dana Farber Cancer Institute, Boston, MA, USA
Laura Marciano
Department of Communication & Media, Ewha Womans University, Seoul, South Korea
Peter Johannes Schulz
You can also search for this author in PubMed Google Scholar
Contributions
EG, LM, and PJS contributed to the conception of the work; EG contributed to the acquisition and analysis of data. EG, LM, and PJS contributed to the interpretation of data. EG wrote the first draft of the manuscript. LM and PJS substantively revised it. All authors have approved the submitted version.
Authors’ information
Peter J. Schulz is Director of the Institute of Communication and Health at the University of Lugano, Switzerland and Professor of Communication Theories and Health Communication.
Laura Marciano is a post-doctoral research fellow at the Harvard Chan T.H. School of Public Health, Boston (USA). Her research is focused on digital media use and well-being.
Elisa Galmarini is, at the time of the draft of the manuscript, a student in the master course “Communication, Management and Health” at the University of Lugano, Switzerland.
Corresponding author
Correspondence to Peter Johannes Schulz .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Galmarini, E., Marciano, L. & Schulz, P.J. The effectiveness of visual-based interventions on health literacy in health care: a systematic review and meta-analysis. BMC Health Serv Res 24 , 718 (2024). https://doi.org/10.1186/s12913-024-11138-1
Download citation
Received : 22 December 2023
Accepted : 22 May 2024
Published : 11 June 2024
DOI : https://doi.org/10.1186/s12913-024-11138-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health literacy
- Visual-based intervention
- Health knowledge
- Meta-analysis
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
In Defense of Degrowth
- Christopher Marquis

Deconstructing the myth that infinite economic growth could ever be truly sustainable.
There is a critical need to reassess the focus on continuous growth in the global economic system. The concept of “degrowth” challenges the necessity of perpetual economic expansion for human prosperity, suggesting it contradicts ecological sustainability on a planet with finite resources. Despite some resistance, especially from the business sector, the arguments supporting degrowth underscore the inextricable link between economic growth and environmental degradation, proposing a shift toward more sustainable business practices and a reevaluation of the myths surrounding “sustainable growth,” such as the effectiveness of energy transitions and efficiency improvements, which often overlook significant environmental impacts and dependencies on existing energy infrastructures. The article advocates for a societal movement toward reducing consumption and over-production, while embracing values of care and redistribution, challenging traditional market-first ideologies.
In May 2023, the Beyond Growth conference was held at the EU Parliament in Brussels. Headlined by government leaders and academics, its agenda was the urgent need to change the current economic system. The culmination was a manifesto that stated: “Our world is facing an eco-social crisis…driven by the global capitalist system, centered around perpetual economic expansion (growth) and accumulation. Our obsession with economic expansion clashes with finite planetary boundaries.”
- Christopher Marquis is Sinyi Professor of Chinese Management at Cambridge Judge Business School.
Partner Center
- DOI: 10.52403/ijrr.20240412
- Corpus ID: 269117859
Analysis of Coca Cola Company's Global Marketing Strategy: Literature Review
- Gabelas Makmur Simamora , Agus Putra , Risky Rahmawati Pinardi
- Published in International journal of… 11 April 2024
Related Papers
Showing 1 through 3 of 0 Related Papers

IMAGES
VIDEO
COMMENTS
The preliminary search is the point in the research process where you can identify a gap in the literature. Use the search strategies above to help you get started. If you have any questions or need help with developing your search strategy, please schedule an appointment with a librarian. We are available to meet online and in-person.
The search strategy should define how relevant literature will be identified. It should identify sources to be searched (list of databases and trial registries) and keywords used in the literature (list of keywords). The search strategy should be documented as an integral part of the systematic review protocol.
Ideally, search strategies should be checked by other information specialists . The Peer Review of Electronic Search Strategies (PRESS) checklist offers good guidance for this process . Apart from the syntax (especially Boolean operators and field codes) of the search strategy, it is wise to have the search terms checked by the clinician or ...
4. Manage the search results. Once the search is done and you have recorded the process in enough detail to write up a thorough description in the methods section, you will move on to screening the results. This is an exciting stage in any review because it's the first glimpse of what the search strategies have found.
In this review, we focus on literature searching, specifically the development of the search strategies used in systematic reviews. This is a complex process ( Cooper et al., 2018 ; Lefebvre et al., 2020 ), in which the search methods and choice of databases to be used to identify literature for the systematic review are specified and peer ...
A search strategy is the method by which relevant sources are found, usually by searching selected databases and search engines using a mix of keywords, controlled vocabulary and search operators. Relevance is determined by a review question for which guidelines can be found in Sections 4.2 and 4.3.
If your search strategies are not very developed, the method you use doesn't lead to a good search, then consider using one of the other methods to see if changing your approach helps. ... Tags: dissertation, grey literature, literature review, literature reviews, postgraduate, prisma, prisma flow diagram, rapid evidence reviews, undergraduate ...
Have a search framework. Search frameworks are mnemonics which can help you focus your research question. They are also useful in helping you to identify the concepts and terms you will use in your literature search. PICO is a search framework commonly used in the health sciences to focus clinical questions. As an example, you work in an aged ...
Developing a search strategy is a balance between needing a very precise search that yields fewer highly relevant results or a comprehensive search (high retrieval) with lower precision. The focus of a narrative literature review for a dissertation or thesis is thoroughness, so you should aim for high retrieval.
In preparing for your review, you will begin with an exploratory or preliminary search of the literature. This search will help you: Identify existing reviews (so as not to duplicate work), Assess the quantity and quality of relevant, primary research studies (so as to be sufficiently abundant and productive for your work), and
One area that is less well covered by the guidance, but nevertheless appears in this literature, is the quality appraisal or peer review of literature search strategies. The PRESS checklist is the most prominent and it aims to develop evidence-based guidelines to peer review of electronic search strategies [5, 122, 123]. A corresponding ...
Overview of Search Strategies. There are many ways to find literature for your review, and we recommend that you use a combination of strategies - keeping in mind that you're going to be searching multiple times in a variety of ways, using different databases and resources. Searching the literature is not a straightforward, linear process - it ...
When you decide to update a systematic review search, there are two ways of identifying new articles: 1. Rerun the original search strategy without any changes. Rerun the original search strategy without making any changes. Import the results into your citation manager, and remove all articles duplicated from the original set of search results. 2.
Abstract. Undertaking a literature search can be a daunting prospect. Breaking the exercise down into smaller steps will make the process more manageable. This article suggests 10 steps that will help readers complete this task, from identifying key concepts to choosing databases for the search and saving the results and search strategy.
A search strategy should be planned out and practiced before executing the final search in a database. A search strategy and search results should be documented throughout the searching process. What is a search strategy? A search strategy is an organized combination of keywords, phrases, subject headings, and limiters used to search a database ...
draft the search template and table (see below) for the review team to comment on. Once the search strategy has been finalized, the authors can add it to the Revman version of their protocol. Alternatively, the authors can prepare the search strategy and send it to Vittoria Lutje for her comments before finalizing the protocol. 1.1. Search terms
Exemplar articles can be used to test your search strategy and ensure that your search strategy is retrieving the kinds of literature you want to include in the review. In addition, citation chasing from exemplar articles is a great way to identify additional relevant literature.
Look up your 'sample set' articles in a database that you will use for your literature review. For the articles indexed in the database, look at the records to see what keywords and/or subject headings are listed. The 'gold set' will also provide a means of testing your search strategy
B.1. Clinical search literature search strategy. Searches were constructed using a PICO framework where population (P) terms were combined with Intervention (I) and in some cases Comparison (C) terms. Outcomes (O) are rarely used in search strategies for interventions as these concepts may not be well described in title, abstract or indexes and ...
A search strategy is an organised structure of key terms used to search a database. The search strategy combines the key concepts of your search question in order to retrieve accurate results. Your search strategy will account for all: possible search terms. keywords and phrases. truncated and wildcard variations of search terms.
Creating a Search Strategy. A well constructed search strategy is the core of your systematic review and will be reported on in the methods section of your paper. The search strategy retrieves the majority of the studies you will assess for eligibility & inclusion. The quality of the search strategy also affects what items may have been missed.
By using a truncation symbol you can capture all of the various endings possible for a particular word. This may increase the number of results and reduce the likelihood of missing something relevant. Some tips about truncation: The truncation symbol is generally an asterisk symbol * and is added at the end of a word.; It may be added to the root of a word that is a word in itself.
The search strategy was developed from keywords and medical subject headings (MeSH) terms. Librarian's support and advice were sought in forming of the search strategies. Study selection and inclusion criteria. The systematic search was conducted on each database and all articles were exported to Endnote and duplicates records were removed.
A comprehensive search strategy will be used to search Medline, PsycINFO, Embase, Scopus, LGBTQ+ Source, and grey literature. Original studies of any design, setting, and publication date will be included if they discuss barriers and facilitators to mental health treatment access and engagement for LGBTQA+ people with experiences of psychosis.
We performed a literature search using PubMed, Google Scholar, Cochrane Library, and Embase for relevant materials. We obtained all articles published between March 2020 and April 2022 relevant to the subject of review and met pre-defined eligibility criteria. We selected 23 articles for initial screening and included 12 in the final review.
A systematic review of the literature published on splenic embolism (SE) between 2000 and 2023 was conducted. Search strategies in electronic databases identified 2751 studies published between 1 January 2000 and 4 October 2023, of which 29 were finally included.
Background Limited Health Literacy (HL) is an obstacle to accessing and receiving optimal health care and negatively impacts patients' quality of life, thus making it an urgent issue in the health care system. Visual-based interventions are a promising strategy to improve HL through the use of visual aids and pictorial materials to explain health-related concepts. However, a comprehensive ...
In Defense of Degrowth. Summary. There is a critical need to reassess the focus on continuous growth in the global economic system. The concept of "degrowth" challenges the necessity of ...
Coca-Cola Company is headquartered in Atlanta, Georgia, America. 70% of the company's volume and 80% of the company's profits come from outside the United States. The main idea behind Coca Cola's marketing strategy is the ability to read consumers' minds across geographic boundaries. Coca Cola began to establish relationships with various food ...
Literature Reviews; Narrative Review. Developing a Search Strategy ; Systematic Reviews This link opens in a new window; Scoping Reviews This link opens in a new window; ... You can export your search strategy in addition to the results, to use in your search documentation. A search string will generally look like: (Topic A term 1 OR Topic A ...