Childhood Obesity - Free Essay Samples And Topic Ideas
Childhood Obesity is a serious medical condition where excess body fat negatively affects a child’s health or well-being. Essays might discuss the causes, consequences, prevention and management of childhood obesity, as well as the role of parents, schools, and healthcare providers in addressing this issue. A vast selection of complimentary essay illustrations pertaining to Childhood Obesity you can find in Papersowl database. You can use our samples for inspiration to write your own essay, research paper, or just to explore a new topic for yourself.

Problem: Childhood Obesity in America
As you've probably heard, more children are becoming overweight today in America than ever before. Experts are calling this an "obesity epidemic." To first understand childhood obesity we must ask ourselves what is obesity? Obesity is a diet-related chronic disease involving excessive body fat that increases the risk of health problems. Many doctors have expressed obesity has an increasing problem in today's youth as obesity can lead to many health issues such as type 2 diabetes, high blood pressure, heart […]
Childhood Obesity Parents are the Blame
In current years, children becoming more obese in their entire childhood development has become common. Obesity in children could be due to various reasons such as family structure, busy family life experienced in the modern days, and insufficient knowledge of foods containing high calories. Parents ought to be accountable for what they do or fail to do that amounts to a negative influence on their children's weight and cause them to be overweight or obese during their childhood period. When […]
Childhood and Adolescents Obesity Prevention
Obesity in children and adolescents is a serious and growing problem in America. Overweight children are becoming overweight adults and that is causing life-threatening, chronic diseases such as diabetes and heart disease. There are multiple reasons for childhood obesity. The most common reasons are genetic factors, lack of physical activity, unhealthy eating patterns, or a combination of all three factors (“Obesity in Children,” 2018). Today, there are many children that spend a lot of time being inactive and eating junk […]
We will write an essay sample crafted to your needs.
Childhood Obesity – Causes and Potential Long-Term Effects
Abstract There is growing concern about the state of children’s health. Every year there is an increase in the number of overweight and obese children. What causes this and what does it mean for them long-term? There are many contributing factors to children’s weight issues. Some of these factors are limited access to healthy food, more time spent in front of a screen, and less physical activity. Long-term health affects include a rising risk of Type 2 diabetes, coronary heart […]
How are Fast Food Advertising and Childhood Obesity Related
By 1950s, fast food industry boom was in full swing. It was secured in 1951. In the 1950s, McDonald has become a staple of the American diet. Fast food restaurants have been grown more and more and by now, there are over one hundred and sixty thousands fast food restaurants in the United States, becoming a one hundred and ten billion dollar industry. One can’t deny that fast food has become really important in American life nowadays. Whether Americans are […]
Obesity in Childhood
There are numerous issues that society faces on a daily basis. One of the issues that society faces is obesity. It is one of the leading risks of death and has been ongoing since the 1960s and 1970s. Obesity is an issue that continues to grow not only in the United States but also in developing countries as well. Not only does obesity affect adults but it has become a serious issue for children. According to an article, "approximately 12.7 […]
Childhood Obesity a Serious Problem in the USA
Childhood obesity is a serious problem in the United States. Obesity is condition in which a child is significantly overweight for his or her age and height. It is a very common condition and is estimated to have around 3 million cases in the United States each year. Every day more children are getting diagnosed with obesity, and some as young as 4 years old. When a child gets diagnosed with obesity at a young age, it can be very […]
Childhood Obesity is an Epidemic in the USA
Introduction Childhood obesity has become an epidemic in the United States and other western industrialized societies. "Childhood obesity affects more than 18 percent of children in the United States, making it the most common chronic disease of childhood" (Obesity Action Coalition). According to the OAC, the percentage of children suffering from childhood obesity has tripled since 1980. A child is considered obese if their body mass index for their age is greater than 95 percent. Childhood obesity is both an […]
Obese Kids and Low Self-esteem
Those who are in poverty are predominately people of color and as you can see from the chart above there is a high percentage of children of color who were diagnosed with childhood obesity. According to Centers of Disease Control, "Overall, non-Hispanic black and Hispanic adults and youth had a higher prevalence of obesity compared with other race and Hispanic-origin groups. Obesity prevalence was lower among non-Hispanic Asian men and women compared with other race and Hispanic-origin groups. Among men, […]
Childhood Obesity Today
In America, childhood obesity is on a rise today. Children can gain obsessive weight because of environmental factors. Vending machines, low cost on snacks, and a increase in the fast food chain are contributing factors towards obesity. Genetics can also play a part in childhood obesity. Many children come from a generation of overweight families. Most parents don't see the harm in letting their children gain tons of weight. Obesity can cause many health problems. Childhood obesity affects the health […]
Childhood Obesity in the American Nation
Childhood obesity is still rising in this nation. One out of three Americans is obese. The outlook for children is not much better, as adolescent obesity has quadrupled over the last thirty years. "As of 2012, almost 18 percent of children aged 6-11 years were obese" (Newman, 1). Despite the considerable public awareness of the negative impacts of obesity, this challenge persists. The situation for youngsters is hardly brighter; over the last few decades, the rate of youth obesity has […]
Child and Adolescent Obesity in the United States
Child and adolescent obesity in the United States has nearly tripled sincethe 70s. About 1 out of every 5 children suffer from childhood obesity. It is the duty ofmothers and fathers to prevent and find solutions to child and adolescent obesity. Thispaper will seek to explain the many causes and current results which parents can execute.Child and adolescent obesity comprises of several likely causes such as poor diet and lowphysical activity including numerous adverse effects. Therefore, changes in familyhousehold structures […]
The Causes and Preventions of Childhood Obesity
When trying to find out if a child is considered for obesity, they need to have a body mass index that is between the ranges of the 85th percentile and the 95th percentile. When speaking about childhood obesity it is for children between the ages of infancy and early adulthood which is eighteen years of age. Obesity is one of the most preventable diseases especially if caught early enough. There are many different reasons for the cause of childhood obesity, […]
The Effects of the Epidemic Childhood Obesity
Childhood obesity has become a growing epidemic in more than just the U.S. However, over the past three decades, childhood obesity rates have tripled in the U.S. and today, the country has some of the highest obesity rates in the world: One out of six children is obese, and one out of three children is overweight. Chubby children were once thought of as cute, it was there baby fat and they would soon emerge into healthy adults, however this isn't […]
Tackling Childhood Obesity in Rural Mississippi
Childhood obesity is a growing health issue in the United States. Children with higher Body Mass Indexes than the recommended by the National Institutes of Health are more prone to adverse health effects later in life. Obesity in early age can translate into adulthood and increases the risk of developing cardiovascular diseases and diabetes (Franks 2010). The highest rates of childhood obesity can be observed in the southeastern corner of the United States, Mississippi, in particular, with the highest prevalence […]
Childhood Obesity, a Crisis that could be Cure
Obesity is a crisis that is affecting many countries, their most vulnerable citizens being children. Bad eating habits, high calorie intake, genetics, and lack of activity or exercise are some of the elements that, either combined or individually, are the cause for childhood obesity in America, Latin America, and many other nations. In the United States, rural areas have higher rates of childhood obesity, as do Hispanics and Blacks (Davis 2011). Keywords: Obesity, Childhood. Childhood Obesity, a Crisis that could […]
Childhood Obesity: Global Epidemic and Ethical Concerns
Abstract Numbers continue to climb for those who have childhood obesity. This serious issue has been brought to the attention of the public who have been taking preventative measures and action in hopes to reduce the number of cases. In a number of countries, public policies have been implemented to prevent obesity. However, in the U.S. efforts made are not enough or have not been effective to stop the obesity rate from increasing. Proposals for solutions to this health problem […]
Childhood Obesity and Unhealthy Diets
Over the years childhood obesity has become an epidemic. Working as a medical assistant in family practice for the past ten years, I have witnessed a lot of children struggling with being overweight and obese. Many children now in days lack whole foods that contain proper macronutrients for their bodies to use as energy adequately. Processed foods and sugary beverages can cause more complications over time when overconsumed. Along with lack of proper nutrition, a lot of children seem to […]
The Social Environment and Childhood Obesity
I, Marisol Nuñez, reside in South Gate the reason for this letter is that I am very concerned about the prevention of childhood obesity. Residents in our city lack the resources of acquiring healthy nutritious foods for their families, the resources in our city are very limited. The city has a farmer’s market once a week, and the likelihood of working families purchasing healthier foods is very limited. We need more resources for our families can eat highly nutritious foods. […]
Childhood Obesity and Physical Activity
Most children and teens have access to a tablet, smartphone, television, laptop or a video console. They are sitting around on-screen time more and more as the days go by. Research from the CDC states obesity has nearly doubled since the 1970s in the United States. It is estimated now that 20 percent of children and adolescents are affected by obesity. Too much screen time, the accessibility to the internet and not enough physical activity are the biggest reasons the […]
Childhood Obesity and Adolesence
Childhood obesity can be prevented in many ways. Parents are the main ones with a say so on obesity. They allow their children to digest all kinds of bad foods. Parents should introduce on a daily basis different kinds of healthy foods. They should also promote is by showing children how healthy food are good for the body. You have some children that won’t eat healthy things because of the color and the way it looks. Obesity is one of […]
Several Factors in Childhood Obesity
Childhood obesity is widely described as excess in body fat in children and teenagers. There is, however, no agreement about exactly how much body fat is excessive in relation to the group. The Center for Disease Control and Prevention on its part defined overweight as at or above the 95th percentile of body mass index (BMI) for age and "at risk for overweight" as between 85th to 95th percentile of BMI for age (Krushnapriya Sahoo). In general clinic environments, the […]
Factors that Influence Childhood Obesity
The cause of pediatric obesity is multifactorial (1). There is not a single cause, nor solution, found that leads to all cases of pediatric obesity. Parental discipline in regard to the child is not proven to lead to less adiposity or obesity in children. Parental feeding strategy may actually be a cause of obesity with restrictive approach to food by the parent shown to increase the proclivity for the restricted foods (2). Likewise, when parents allowed their children to have […]
Childhood Obesity, Disease Control and Prevention
According to the Centers for Disease Control and Prevention, identifying effective intervention strategies that can target both improvements in physical activity and providing a nutritious diet to reduce childhood obesity are important" (Karnik, 21). There has been a rising concern on whether or not the government needs to be involved in this childhood obesity epidemic. Sameera, Karnik, and Amar Kanekar give an amazing detailed article on how important it is to get involved with children through the government and through […]
The Impact of Childhood Obesity on Health
Childhood Obesity has become an ongoing problem across the United States. Obesity kills about 34 children every hour in the world, making it a serious issue. Many leaders and people have come together to attempt to prevent the issue, but some strategies have failed. Most people disregard the fact that what they feed their children can affect them in many ways, specifically become obese. Childhood obesity can lead to becoming obese in the future, being susceptible to different diseases and […]
What is Childhood Obesity?
Introduction Childhood obesity has become a widespread epidemic, especially in the United States. Twenty five percent of children in the United States are overweight and eleven percent are obese (Dehghan, et al, 2005). On top of that, about seventy percent of those children will grow up to be obese adults (Dehgan, et al, 2005). There are many different causes that can be attributed to the childhood obesity. Environmental factors, lifestyle preferences, and cultural environment play pivotal roles in the rising […]
Problem of Childhood Obesity in the United States
Among the many issues that the United States is facing, there is no doubt that Childhood Obesity is a timely and relevant debatable topic that has brought many consequences and health issues among our nation’s children. Many debates in regard to childhood obesity have formed. Because the prevalence of childhood obesity is on the rise, there have been varying opinions about what leading factors contribute to this issue. Although some health professionals and parents believe that childhood obesity stems from […]
A Big Problem – Bad Healthcare is Aiding Childhood Obesity
A study done in 2002 found that, almost 14 million children are obese, that is 24 percent of the U.S. population from ages 2 to 17. This number just keeps rising as the years go by. Some people would argue that the increasing numbers are due to sugary dinks and foods sold in vending machines at schools, or not enough healthy food options. Other parties can argue that this number keeps increasing because of bad healthcare and not enough opportunities […]
Childhood Obesity Rate Can be Decreased
Child obesity has become a major concern as it continues to increase every year in the US. Many parents are uneducated about the risks of childhood obesity. Parental awareness and increasing physical activity are steps towards making a change in the rates of childhood obesity. There are many side effects of childhood obesity that can obstruct a child’s future. However, positive changes to children’s health can be achieved through the influence of adults. Child obesity has become a more critical […]
Additional Example Essays
- The Mental Health Stigma
- Psychiatric Nurse Practitioner
- Substance Abuse and Mental Illnesses
- Homeschooling vs Public School
- Socioautobiography Choices and Experiences Growing up
- A Research Paper on Alzheimer's Disease
- The Effect of Alcohol on College Students
- Is Sexual Orientation Determined At Birth?
- Nursing Shortage: solutions of the problem
- End Of Life Ethical Issues
- Beauty Pageants for Children Should Be Banned: Protecting Child Well-being
- Live Free and Starve, by Chitra Divakaruni
How To Write an Essay About Childhood Obesity
Understanding childhood obesity.
Writing an essay about childhood obesity requires a comprehensive understanding of the topic. Childhood obesity is a serious public health issue that has grown significantly in recent years. It's characterized by children having a body mass index (BMI) at or above the 95th percentile for children of the same age and sex. Start by exploring the causes of childhood obesity, which can include genetic factors, poor dietary habits, lack of physical activity, and environmental influences. Also, consider the short and long-term health implications, such as an increased risk of chronic diseases like diabetes and heart disease. This foundational knowledge sets the stage for a deeper analysis in your essay.
Developing a Focused Thesis Statement
Your essay should be guided by a clear, focused thesis statement. This statement should present a specific angle or argument about childhood obesity. For instance, you might argue the importance of early intervention programs, the role of schools in promoting healthy lifestyles, or the impact of advertising and media on children’s eating habits. Your thesis will determine the direction of your essay, guiding your analysis and ensuring a structured approach to the topic.
Gathering and Analyzing Data
An effective essay on childhood obesity should be supported by relevant data and research. This includes statistics on the prevalence of obesity, studies on its causes and effects, and evaluations of intervention programs. Use this information to support your thesis, incorporating both national and global perspectives. Analyze the data critically, acknowledging any limitations and considering different viewpoints. This approach adds depth to your essay and strengthens your arguments.
Discussing Solutions and Interventions
A significant portion of your essay should be dedicated to discussing potential solutions and interventions for childhood obesity. This can include public health policies, educational programs, changes in food industry practices, or community-based initiatives. Evaluate the effectiveness of these solutions, drawing on case studies or research findings. Discussing both the successes and challenges in tackling childhood obesity will provide a balanced view and demonstrate a comprehensive understanding of the topic.
Concluding the Essay
Conclude your essay by summarizing the main points of your discussion and restating your thesis in light of the evidence presented. Your conclusion should tie together your analysis and emphasize the significance of addressing childhood obesity. This is also an opportunity to reflect on potential future developments in the field or to suggest areas for further research.
Reviewing and Refining the Essay
After completing your essay, it's important to review and refine it. Check for coherence in your arguments and clarity in your writing. Ensure that your essay is well-organized and free from grammatical errors. Consider seeking feedback from peers, teachers, or health professionals to further improve your work. A well-crafted essay on childhood obesity should not only inform but also engage readers in considering the complexities of this public health issue and the collective efforts required to address it.
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
Home — Essay Samples — Nursing & Health — Childhood Obesity — Child Obesity Essay Outline
Child Obesity Essay Outline
- Categories: Childhood Obesity
About this sample

Words: 681 |
Published: Mar 14, 2024
Words: 681 | Page: 1 | 4 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1163 words
5 pages / 2053 words
5 pages / 2799 words
13 pages / 5869 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Childhood Obesity
Buzzell, L. (2019, August 13). Benefits of a Healthy Lifestyle. Johns Hopkins Medicine. https://www.healthline.com/health/healthy-eating-on-a-budget#1.-Plan-meals-and-shop-for-groceries-in-advance
Obesity in children in the US and Canada is on the rise, and never ending because new parents or parents with experience, either way tend to ignore what is happening with their child. A study at UCSF tells us that “A child with [...]
In conclusion, while Zinczenko's analysis in "Don't Blame the Eater" offers valuable insights into the rise of childhood obesity and the role of the fast-food industry, it is necessary to critically examine his claims. While [...]
With obesity rates on the rise, and student MVPA time at an all time low, it is important, now more than ever, to provide students with tools and creative opportunities for a healthy and active lifestyle. A school following a [...]
In today's fast-paced world, where stress levels are high and unhealthy habits run rampant, the importance of good health cannot be overstated. From physical well-being to mental resilience, good health impacts every aspect of [...]
It is well known today that the obesity epidemic is claiming more and more victims each day. The Centers for Disease Control and Prevention writes “that nearly 1 in 5 school age children and young people (6 to 19 years) in the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Share full article
Advertisement
Supported by
Leave Fat Kids Alone
The “war on childhood obesity” has only caused shame.

By Aubrey Gordon
Ms. Gordon is the author of the forthcoming book “What We Don’t Talk About When We Talk About Fat.”
I was in the fourth grade, sitting in a doctor’s office, the first time my face flushed with shame. I was, I had just learned, overweight.
I will remember the pediatrician’s words forever: It’s probably from eating all that pizza and ice cream. It tastes good, doesn’t it? But it makes your body big and fat.
I felt my face sear with shame.
There was more: Just imagine that your body is made out of clay. If you can just stay the same weight, as you grow, you’ll stretch out. And once you grow up, you’ll be thin and beautiful. Won’t that be great?
I learned so much in that one moment: You’re not beautiful. You’re indulging too much. Your body is wrong. You must have done it. I’d failed a test I didn’t even know I’d taken, and the sense of failure and self-loathing it inspired planted the seeds of a depression I would live with for many years.
As the holiday season approaches, with its celebratory family meals and seasonal treats, I worry about the children across the country who will endure similar remarks, the kind that shatter their confidence, reject their bodies and usher them into a harsh new world of judgment.
For the rest of my childhood, I weathered the storm of conversations like the one I had at the doctor’s office. Well-meaning, supportive adults eagerly pointed out my perceived failings at every turn. As the years went on, more and more foods, I was told, were off limits.
It wasn’t just that I shouldn’t eat them; it was that they were sinful, bad, tempting . Many of those foods — eggs, nuts, avocados — would later fall back into the good graces of healthy eating. At the time, though, they were collateral damage in a crusade to cut calories at all costs. Fiber, vitamins, minerals, fatty acids, protein — they were all sacrificed at the altar of calories in, calories out. The focus was never on enjoying nutritious foods, just on deprivation, will and lack.
My life was filled with self-flagellation, forced performances to display my commitment to changing an unacceptable body. Adults asked openly about what I had eaten, when I had exercised and whether I knew how to do either correctly. After all, if I was still fat, it must be my fault.
My body wasn’t just a body, the way a thinner one might have been. It was perceived as a burden, an inconvenience, a bothersome problem to solve. Only thinness would allow me to forget my body, but despite my best efforts, thinness never came.
The more I and others tried to change my size, the deeper my depression became. Even at such a young age, I had been declared an enemy combatant in the nation’s war on childhood obesity, and I felt that fact deeply. Bodies like mine now represented an epidemic, and we were its virus, personified.
The war on obesity seemed to emerge, fully formed, near the turn of the millennium, but its roots run deeper than that. C. Everett Koop, surgeon general under President Ronald Reagan, made fatness a priority for his office in the 1980s. In 2004, nearly three years after the Sept. 11 attacks, Surgeon General Richard Carmona compared the war on obesity to the war on terror. Suddenly, fat people weren’t just neighbors, friends or family members — we were enemies to be feared.
The war on childhood obesity reached its zenith with the 2010 introduction of the national “Let’s Move!” campaign, “dedicated to solving the problem of obesity within a generation.” It was a campaign against “childhood obesity” — not specific health conditions or the behaviors that may contribute to those health conditions. It wasn’t a campaign against foods with little nutritional value, or against the unchecked poverty that called for such low-cost, shelf-stable foods. It was a campaign against a body type — specifically, children’s body types.
In 2012, Georgia began its Strong4Life campaign aimed at reducing children’s weight and lowering the state’s national ranking: second in childhood obesity. Run by the pediatric hospital Children’s Healthcare of Atlanta, it was inspired in part by a previous anti-meth campaign. Now, instead of targeting addiction in adults, the billboards targeted fatness in children. Somber black-and-white photographs of fat children stared at viewers, emblazoned with bold text. “WARNING: My fat may be funny to you but it’s killing me. Stop childhood obesity.” “WARNING: Fat prevention begins at home. And the buffet line.” “WARNING: Big bones didn’t make me this way. Big meals did.”
The billboards purported to warn parents of the danger of childhood fatness, but to many they appeared to be public ridicule of fat kids. Strong4Life became one of the nation’s highest-profile fat-shaming campaigns — and its targets were children.
These declarations of an obesity epidemic and a war on childhood obesity all doggedly pursued one question, and one question only: How do we make fat kids thin? In other words, how do we get rid of fat kids?
Overwhelmingly, childhood anti-obesity programs hinged on shame and fear, a scared-straight approach for fat children. As of 2017, fully half of the states required that schools track students’ body mass index. Many require “B.M.I. report cards” to be sent home to parents, despite the fact that 53 percent of parents don’t actually believe that the reports accurately categorize their child’s weight status. And observational studies in Arkansas and California have shown that the practice of parental notification doesn’t appear to lead to individual weight loss or an overall reduction in students’ B.M.I.s. One eating disorder treatment center called the report cards a “pathway to weight stigma” that would most likely contribute to the development of eating disorders in predisposed students.
Experiencing weight stigma has significant long-term effects, too. A 2012 study in the journal Obesity asked fat adults to indicate how often they had experienced various weight-stigmatizing events. Seventy-four percent of women and 70 percent of men of similar B.M.I. and age reported others’ making negative assumptions. Twenty-eight percent of women and 23 percent of men reported job discrimination. The effects of stigma were especially dire for young people, very fat people and those who started dieting early in life. To cope, 79 percent of all respondents reported eating, 74 percent isolated themselves, and 41 percent left the situation or avoided it in the future. Rather than motivating fat people to lose weight, weight stigma had led to more isolation, more avoidance and less support.
Despite ample federal and state funding, multiple national public health campaigns and a slew of television shows, the war on obesity does not appear to be lowering Americans’ B.M.I.s. According to the Centers for Disease Control and Prevention, since 1999 there has been a 39 percent increase in adult obesity and a 33.1 percent increase in obesity among children.
Weight stigma kick-starts what for many will become lifelong cycles of shame. And it sends a clear, heartbreaking message to fat children: The world would be a better place without you in it.
Yet, despite its demonstrated ineffectiveness, the so-called war on childhood obesity rages on. This holiday season, for the sake of children who are told You’re not beautiful. You’re indulging too much. Your body is wrong. You must have done it, I hope some parents will declare a cease-fire.
Aubrey Gordon, who has written under the pseudonym “Your Fat Friend,” is a columnist for Self magazine, a co-host of the podcast “Maintenance Phase” and the author of the forthcoming book “ What We Don’t Talk About When We Talk About Fat .”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow The New York Times Opinion section on Facebook , Twitter (@NYTopinion) and Instagram .
- IELTS Scores
- Life Skills Test
- Find a Test Centre
- Alternatives to IELTS
- General Training
- Academic Word List
- Topic Vocabulary
- Collocation
- Phrasal Verbs
- Writing eBooks
- Reading eBook
- All eBooks & Courses
IELTS Sample Task 2 Essay: Child Obesity
by Patel (Bolton)
“There is no doubt that overweight children’s percentages rose by twenty percent in western world.”
“overweight children’s percentages rose”
“Secondly, some advertisements that encourage children to eat unhealthy diet.”
Overweight children are prone to many problems.
Such as + noun For example + Subject Verb
to be concerned about
Click here to add your own comments
Return to Writing Submissions - Task 2.
Before you go...
Check out the ielts buddy band 7+ ebooks & courses.
Would you prefer to share this page with others by linking to it?
- Click on the HTML link code below.
- Copy and paste it, adding a note of your own, into your blog, a Web page, forums, a blog comment, your Facebook account, or anywhere that someone would find this page valuable.
Band 7+ eBooks
"I think these eBooks are FANTASTIC!!! I know that's not academic language, but it's the truth!"
Linda, from Italy, Scored Band 7.5
IELTS Modules:
Other resources:.
- All Lessons
- Band Score Calculator
- Writing Feedback
- Speaking Feedback
- Teacher Resources
- Free Downloads
- Recent Essay Exam Questions
- Books for IELTS Prep
- Useful Links
Recent Articles
Key Phrases for IELTS Speaking: Fluency and Coherence
May 26, 24 06:52 AM
Useful Language for IELTS Graphs
May 16, 24 04:44 AM
Taking a Gap Year
May 14, 24 03:00 PM
Important pages
IELTS Writing IELTS Speaking IELTS Listening IELTS Reading All Lessons Vocabulary Academic Task 1 Academic Task 2 Practice Tests
Connect with us
Copyright © 2022- IELTSbuddy All Rights Reserved
IELTS is a registered trademark of University of Cambridge, the British Council, and IDP Education Australia. This site and its owners are not affiliated, approved or endorsed by the University of Cambridge ESOL, the British Council, and IDP Education Australia.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Obesity in children and adolescents: epidemiology, causes, assessment, and management
Hiba jebeile.
a Sydney Medical School, The University of Sydney, Sydney, NSW, Australia
b Institute of Endocrinology and Diabetes, The Children's Hospital at Westmead, Westmead, NSW, Australia
Aaron S Kelly
d Department of Pediatrics and Center for Pediatric Obesity Medicine, University of Minnesota Medical School, Minneapolis, MN, USA
Grace O'Malley
e School of Physiotherapy, RCSI University of Medicine and Health Sciences, Dublin, Ireland
f Child and Adolescent Obesity Service, Children's Health Ireland at Temple Street, Dublin, Ireland
Louise A Baur
c Weight Management Services, The Children's Hospital at Westmead, Westmead, NSW, Australia
This Review describes current knowledge on the epidemiology and causes of child and adolescent obesity, considerations for assessment, and current management approaches. Before the COVID-19 pandemic, obesity prevalence in children and adolescents had plateaued in many high-income countries despite levels of severe obesity having increased. However, in low-income and middle-income countries, obesity prevalence had risen. During the pandemic, weight gain among children and adolescents has increased in several jurisdictions. Obesity is associated with cardiometabolic and psychosocial comorbidity as well as premature adult mortality. The development and perpetuation of obesity is largely explained by a bio-socioecological framework, whereby biological predisposition, socioeconomic, and environmental factors interact together to promote deposition and proliferation of adipose tissue. First-line treatment approaches include family-based behavioural obesity interventions addressing diet, physical activity, sedentary behaviours, and sleep quality, underpinned by behaviour change strategies. Evidence for intensive dietary approaches, pharmacotherapy, and metabolic and bariatric surgery as supplemental therapies are emerging; however, access to these therapies is scarce in most jurisdictions. Research is still needed to inform the personalisation of treatment approaches of obesity in children and adolescents and their translation to clinical practice.
Introduction
Obesity in children and adolescents is a global health issue with increasing prevalence in low-income and middle-income countries (LMICs) as well as a high prevalence in many high-income countries. 1 Obesity during childhood is likely to continue into adulthood and is associated with cardiometabolic and psychosocial comorbidity as well as premature mortality. 2 , 3 , 4 The provision of effective and compassionate care, tailored to the child and family, is vital. In this Review, we describe current knowledge on the epidemiology and causes of child and adolescent obesity, considerations for assessment, and current management approaches.
Epidemiology
Definitions of overweight and obesity in children and adolescents.
WHO defines overweight and obesity as an abnormal or excessive fat accumulation that presents a risk to health. For epidemiological purposes and routine clinical practice, simple anthropometric measures are generally used as screening tools. BMI (weight/height 2 ; kg/m 2 ) is used as an indirect measure of body fatness in children and adolescents 5 and should be compared with population growth references adjusted for sex and age. The WHO 2006 Growth Standard is recommended in many countries for children aged 0–5 years, and for children aged 0–2 years in the USA. 6 For older children and adolescents, other growth references are used, including the WHO 2007 Growth Reference, recommended for those aged 5–19 years (overweight defined as BMI ≥1SD and obesity as BMI ≥2SD of the median for age and sex), and the United States Centers for Disease Control and Prevention (CDC) Growth Reference for those aged 2 to 20 years (overweight is >85th to <95th percentile and obesity is ≥95th percentile based on CDC growth charts). 6 , 7 The International Obesity Task Force tables for children aged 2 to 18 years are used for epidemiological studies. 8
Abdominal or central obesity is associated with increased cardiometabolic risk in children and adolescents. 9 For waist circumference there are regional and international growth references allowing adjustment for age and sex. 10 , 11 , 12 A waist-to-height ratio of more than 0·5 is increasingly used as an indicator of abdominal adiposity in clinical and research studies, with no need for a comparison reference. 13
Various definitions have been suggested to identify more extreme values of BMI in children and adolescents. The International Obesity Task Force defined morbid obesity as equivalent to age-adjusted and sex-adjusted BMI of 35kg/m 2 or more at age 18 years, a definition specifically for epidemiological use. 14 The American Heart Association characterises severe obesity as a BMI of 120% or more of the 95th percentile of BMI for age and sex (based on CDC2000 growth charts), a definition that can be used in both clinical practice and research. 15 There are marked limitations in transforming very high BMI values to z-scores, particularly when using CDC2000 growth charts because reductions in BMI can be underestimated. 15
The prevalence of paediatric obesity 16 has increased worldwide over the past five decades. From 1975 to 2016, the global age-standardised prevalence of obesity in children and adolescents aged 5–19 years increased from 0·7% (95% credible interval [CrI] 0·4–1·2) to 5·6% (4·8–6·5) for girls and from 0·9% (0·5–1·3) to 7·8% (6·7–9·1) for boys. 17 Since 2000, the mean BMI has plateaued, usually at high levels, in many high-income countries but has continued to rise in LMICs. In 2016, obesity prevalence in this age group was highest (>30%) in many Pacific Island nations and was high (>20%) in several countries in the Middle East, north Africa, Micronesia (region of the western Pacific), Polynesia (subregion of Oceania), the Caribbean, as well as in the USA. 17
In 2019, the World Obesity Federation estimated there would be 206 million children and adolescents aged 5–19 years living with obesity in 2025, and 254 million in 2030. 1 Of the 42 countries each estimated to have more than 1 million children with obesity in 2030, the top ranked are China, followed by India, the USA, Indonesia, and Brazil, with only seven of the top 42 countries being high-income countries.
The prevalence of severe obesity in the paediatric population has grown in many high-income countries, even though overall prevalence of obesity has been stable. 18 , 19 , 20 , 21 In a survey of European countries, approximately a quarter of children with obesity were classified with severe obesity, a finding that has implications for delivery of obesity clinical services, because such children will need more specialised and intensive therapy. 19
There are socioeconomic disparities in paediatric obesity prevalence within countries. In lower-income to middle-income countries, children of higher socioeconomic status are at greater risk of being affected by overweight or obesity than children of a lower socioeconomic status, whereas in high-income countries, it is children living in socioeconomic disadvantage who are at higher risk. 22 , 23 , 24
Reports from China, Europe, and the USA have documented increased weight gain among children and adolescents during the COVID-19 pandemic compared with the rate before the pandemic, 25 , 26 , 27 , 28 , 29 an apparent consequence of decreases in physical activity, increased screen time, changes in dietary intake, food insecurity, and increased family and individual stress. 30
Development and perpetuation of obesity: a bio-socioecological framework
The development and perpetuation of obesity in modern society can largely be explained by a bio-socioecological framework that has created the conditions for a scenario in which biological predisposition, socioeconomic forces, and environmental factors together promote deposition and proliferation of adipose tissue and resistance to efforts of obesity management. A high degree of biological heterogeneity exists in bodyweight regulation and energy dynamics such that some individuals can maintain healthy levels of adipose tissue with little effort while others face a lifelong struggle with regulating levels. Further, adipose tissue is heterogeneous such that white, brown, and beige forms exist with a variety of physiological functions. 31 The anatomical sites where adipose tissue is stored can translate into varying health risks (eg, central accumulation of adipose tissue is associated with cardiometabolic disease compared to peripheral stores). 32 At a fundamental level, the relative function of the energy regulatory system (the complex interplay of central and peripheral pathways driving appetite, satiety, pleasure-seeking behaviours, and metabolic efficiency) strongly influences body composition. More specifically, the bodyweight set point theory posits the existence of a tightly regulated and complex biological control system, which drives a dynamic feedback loop aimed at defending a predetermined relative or absolute amount of adiposity. 33 Support for this theory comes from evidence in adults demonstrating immediate and sustained alterations in levels of hormones driving appetite and satiety, perceptions of food palatability, and resting energy expenditure following attempts at weight loss. 34 , 35 Other biobehavioural factors such as poor sleep quality, adversity, stress, and medications (causing iatrogenic weight gain) can also serve to exacerbate dysfunction of the energy regulatory system favouring weight gain.
Environmental and behavioural associations of obesity
Over the past few decades the rise in obesity prevalence has been profoundly influenced by changes in the broader obesogenic environment. 36 These changes operate at the level of the family (eg, family modelling of physical activity, food habits, sleep, screen use), local community (eg, child care and schools, parks, green space, public transport and food outlets), or the broader sociopolitical environment (eg, government policies, food industry, food marketing, transport systems, agricultural policies and subsidies). Such influences have been described as having the ability to exploit people's biological, psychological, social, and economic vulnerabilities. 37 Figure 1 depicts a socioecological model incorporating some of the personal and environmental factors influencing paediatric obesity. 38

A socioecological model for understanding the dynamic interrelationships between various personal and environmental factors influencing child and adolescent obesity.
Adapted from the Centers for Disease Control and Prevention social-ecological model framework for prevention. 38 *Defined as being traversable on foot, compact, physically enticing, and safe.
Dietary factors contributing to obesity risk in children and adolescents include excessive consumption of energy-dense, micronutrient-poor foods; a high intake of sugar-sweetened beverages; and the ubiquitous marketing of these and fast foods. 39 , 40 The relative effect of other factors such as specific eating patterns (eg, frequent snacking, skipping breakfast, not eating together as a family, the window of time from first to last daily meal), portion sizes, the speed of eating, macronutrient intake, and glycaemic load on obesity development remain unclear, although all might be important. 41 , 42
The link between screen time and obesity in childhood and adolescence was initially documented through cross-sectional and longitudinal studies of television viewing. 43 , 44 The past two decades have seen the increase of mobile and gaming devices. Screen exposure influences risk of obesity in children and adolescents via increased exposure to food marketing, increased mindless eating while watching screens, displacement of time spent in more physical activities, reinforcement of sedentary behaviours, and reduced sleep time. 44 , 45
Children's physical activity levels decline around the age of 6 years and again at age 13 years, with girls usually exhibiting more marked declines than boys. Overall, children with obesity tend to engage in lower levels of moderate-vigorous activity than leaner peers. 46 , 47 , 48 Sedentary time increases from the age of 6 years in general, although accelerometery studies report no differences between children with obesity compared with leaner peers. 48 Lower levels of physical activity and increasing sedentary behaviours throughout childhood in all children contribute to obesity development. 49 In most countries, children and adolescents are not sufficiently active due to the loss of public recreation space, the increase in motorised transport and decrease in active transport (eg, cycling, walking, public transport), perceptions of lack of safety in local neighbourhoods leading to less active behaviour, as well as an increase in passive entertainment. 39 , 49
There is growing evidence that short sleep duration, poor sleep quality and a late bedtime are associated with a higher obesity risk, sedentary behaviours, poor dietary patterns, and insulin resistance. In addition, there is a possible link with increased screen time, decreased physical activity, and changes in ghrelin and leptin levels. 50 Many of these obesity-conducive behaviours co-occur. For example, increased screen time is associated with delayed sleep onset and shortened sleep duration, and insufficient sleep is associated with increased food intake and lower levels of physical activity. 50
Early life factors
Several factors in early life put children at increased risk of developing obesity. These factors include maternal obesity before pregnancy, excessive gestational weight gain, and gestational diabetes, all associated with increased birth weight. 51 , 52 Infant and young child feeding practices have variable influences on childhood obesity. Meta-analyses from systematic reviews suggest that breastfeeding has a modest but protective effect against later child obesity. 53 , 54 There is some evidence suggesting that the very early introduction of complementary foods and beverages, before the age of 4 months, especially in formula-fed babies, is associated with higher odds of overweight and obesity. 55 Parental approaches to feeding, especially in the preschool age group (aged 1–4 years), might influence obesity risk, with a systematic review showing a small but significant association between controlling child feed practices (eg, restriction of specific foods or the overall amount of food) and higher child weight. 56 Studies of the role of responsive feeding, whereby the caregiver attends to the baby's cues of hunger and satiety, show that non-responsive feeding is associated with increased child BMI or overweight or obesity. 57 , 58 By contrast, a responsive feeding style that recognises the child's cues of hunger and satiety appears to support healthy weight gain trajectories. 58 , 59 However, in all such studies of infant and young child feeding, the effect of residual confounding on child weight status cannot be discounted.
Other environmental exposures in early life that influence child obesity risk include maternal smoking during pregnancy, 60 second-hand exposure to smoke, and air pollution. 61 Antibiotic exposure in infancy is associated with a slight increase in childhood overweight and obesity, especially if there are repeated treatments, an association that might be mediated by alterations in the gut microbiome. 62 Importantly, there is increased recognition that adverse childhood experiences, such as abuse, family dysfunction and neglect are associated with the development of childhood obesity. This association appears to be especially the case for sexual abuse and for co-occurrence of multiple adverse experiences. 63
Medical conditions associated with obesity
Obesity might occur secondary to a range of medical conditions including several endocrine disorders (eg, hypothyroidism, hypercortisolism, growth hormone deficiency), central nervous system damage (ie, hypothalamic-pituitary damage because of surgery or trauma) and post-malignancy (eg, acute leukaemia). Several pharmacological agents are associated with excess weight gain, including glucocorticoids, some anti-epileptics (eg, sodium valproate), insulin, and several atypical antipsychotics (eg, risperidone, olanzapine, clozapine). 64 The rapid and large weight gain associated with the latter class of drugs suggests that anticipatory weight management strategies should be formally used when commencing such therapy, although evidence is largely from adult studies. 65
Weight stigma
Weight stigma refers to the societal devaluation of a person because they have overweight or obesity, and includes negative stereotypes that individuals are lazy and lack motivation and willpower to improve health. 66 , 67 Higher body mass is associated with a greater degree of weight stigma, although longitudinal studies have shown associations between weight stigma and BMI to be bidirectional. 68 Stereotypes manifest in different ways, leading to discrimination and social rejection, often expressed as teasing, bullying and weight-based victimisation in children and adolescents. 66 , 67 Bodyweight is consistently reported to be the most frequent reason for teasing and bullying in children and adolescents, with a quarter to half of youth reporting being bullied based on their bodyweight. 69 Parents and health-care providers can also be sources of weight stigma. 69 , 70 Weight stigma is associated with poor mental health, impaired social development and education, and engagement in disordered eating behaviours including binge eating. 69 Of concern, youth who have experienced weight related teasing or bullying have higher rates of self-harm behaviours and suicidality compared with peers of the same weight who have not felt stigmatised. 67
Experience of weight stigma is a barrier to accessing health care. 67 Health professionals have a responsibility to help reduce weight stigma experienced by children, adolescents, and families through the use of supportive, compassionate, and non-stigmatising language while providing care. 69 In 2020, an international consensus statement was endorsed by more than 100 organisations pledging to reduce weight stigma. 66 Additionally, the American Academy of Paediatrics recommends paediatricians help mitigate weight stigma within clinical practice by role-modelling professional behaviours, using non-stigmatising language, using patient-centred behaviour change counselling, creating a safe and welcoming clinical environment accommodating of all body sizes, and conducting behavioural health screening for signs of weight-based bullying including emotional comorbidities. 67
Health complications
All body systems can be affected by obesity in the short, medium, or longer term, depending upon age and obesity severity. Figure 2 depicts the possible complications of obesity that can occur anywhere from childhood and adolescence to adulthood. It is important that complications are assessed in childhood and treated alongside obesity to prevent progression of both. Recent reviews provide additional detail regarding complications. 2 , 3 , 4 , 48 , 72 , 73 , 74 , 76 , 77 , 78 , 79 , 84 , 85 , 86 , 87 , 88 , 91 , 92 , 94 , 95

Short-term and long-term health complications and comorbidities associated with child and adolescent obesity
Health complications and comorbidities include neurological, 71 dental, 72 cardiovascular, 2 , 73 , 74 , 75 psychosocial, 2 , 4 , 76 , 77 , 78 respiratory, 79 , 80 , 81 , 82 , 83 endocrine, 73 , 84 , 85 musculoskeletal, 80 , 86 , 87 , 88 renal, 89 , 90 gastrointestinal, 90 , 91 skin, 92 function, and participation. 48 , 93
Clinical assessment
A detailed clinical examination screens for underlying causes of obesity, and assesses for possible obesity-related complications, risk of future disease, and whether potentially modifiable behavioural factors exist. Adapted from various national or regional level clinical practice guidelines, 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 summaries of the main aspects to be explored in history taking and physical examination are included in the panel and table . Laboratory tests can complement clinical assessment, looking for cardio-metabolic complications and some underlying causes of obesity. These tests are appropriate in most adolescents with obesity, and in all patients with severe obesity, with clinical signs or history suggestive of complications (eg, acanthosis nigricans), or with a family history of cardio-metabolic disease. Investigations would generally include liver function tests, lipid profile, fasting glucose, and glycated haemoglobin, and might include an oral glucose tolerance test and additional endocrine or genetic studies. 96 , 97 , 98 , 99 , 100 , 101 , 102
Elements of history taking
General history
- • Prenatal and birth history, including gestational obesity, gestational diabetes, maternal smoking, gestational age, birth weight, and neonatal concerns
- • General medical history, including psychiatric or behavioural diagnoses and previous malignancy
- • Developmental history, including any delays in motor, speech, or cognitive developmental, and therapy received
- • Infant feeding, including breastfeeding and duration and timing of introduction of complementary foods
- • Current medications, including glucocorticoids, anti-epileptics (eg, sodium valproate), and antipsychotics (eg, clozapine, risperidone, and olanzapine)
Growth history
- • Height and weight growth trajectories
- • Onset of obesity and timing of weight concerns of child or adolescent and family
- • Previous obesity management, whether supervised or self-initiated
- • Previous and current dieting and exercise behaviours or use of supplements
Complications history
- • Psychological impacts of obesity, including bullying, poor self-esteem, anxiety, depression, and disordered eating
- • Sleep routines, presence of snoring or possible sleep apnoea (eg, poor refreshment after sleep, daytime somnolence, and witnessed apnoea)
- • Exercise tolerance, exercise-induced bronchoconstriction, dyspnoea, hypertension, and fatigue levels
- • Specific symptoms including acne and hirsutism (girls), morning headache and visual disturbance, nocturnal enuresis, daytime dribbling, constipation, hip and knee joint pain, and gastrointestinal complaints (vomiting, abdominal pain, constipation, and gastrointestinal reflux)
- • Menstrual history (girls)
Family history
- • Ethnicity (high risk groups for cardiometabolic complications include First Nations peoples, Latin American, south Asian, east Asian, Mediterranean, and Middle Eastern)
- • Family members with a history of obesity; type 2 diabetes and gestational diabetes; hypertension, dyslipidaemia, and cardiovascular disease; obstructive sleep apnoea; polycystic ovary disease; bariatric surgery; eating disorders; and mental health disorders
- • Home environment including household members, parental relationship, parental employment, hours, and home supervision
Social history, including welfare, and safety
- • Housing or accommodation situation (stable or homeless) and residential care
- • Family income (or proxy) and food insecurity
- • Previous social services involvement
- • School attendance, additional educational assistance, learning difficulties, and behavioural difficulties
- • Hobbies and interests
- • Friends in school or neighbourhood
- • Use of tobacco, alcohol, or recreational drugs
- • Parenting style and child–parent interactions
Behavioural risk factors
- • Nutrition and eating behaviours: breakfast consumption; eating patterns including snacking, grazing, sneaking or hiding food, fast-food intake, binge-eating; beverage consumption (sodas, juices, other sugary drinks); family routines around food and eating; and active dieting
- • Physical activity: transport to and from school; participation in physical education class; participation in organised sport, dance, or martial arts; gym membership; after-school and weekend recreation; and family activities
- • Sedentary behaviours: time spent sitting each day; screen-time per day (television, video game, mobile phone, tablet, computer use); number of devices in the household and bedrooms; patterns of screen viewing (eg, during meals, at night); and use of social media
- • Sleep behaviours: bedtime routines; sleep and wake times on weekdays and weekends; and daytime napping
Clinical findings on examination by organ system
Obesity treatment in children and adolescents aims to reduce adiposity, improve related physical and psychosocial complications, and prevent the development of chronic diseases. The degree of BMI reduction needed to improve obesity related complications is currently unknown. However, some evidence suggests that BMI z-score reductions greater than 0·25 and 0·5 might represent clinically important thresholds. 104 Several high-quality clinical practice guidelines are in use internationally. 96 , 97 , 98 , 99 , 100 , 101 , 102 Treatment type and intensity depends upon obesity severity, the age and developmental stage of the child, needs and preferences of the patient and family, clinical competency and training of the clinician(s), and the health-care system in which treatment is offered. 105 Treatment integrates multiple components including nutrition, exercise and psychological therapy, pharmacotherapy, and surgical procedures. It should be delivered by suitably qualified paediatric health professionals who incorporate behavioural support and non-stigmatising child-focused and youth-focused communication into their practice. 69
Multicomponent behavioural interventions
Behavioural support strategies in obesity management include a combination of addressing dietary intake, physical activity, sedentary behaviours, sleep hygiene, and behavioural components within the context of a family-based and developmentally appropriate approach aiming for long-term behaviour modification. 106 , 107 , 108 Tailoring of interventions to various subgroups based on age, gender, and culture might be needed. For example, with young children the therapy might be largely parent-focussed 109 and for adolescents a greater degree of autonomy might be required. 107
Dietary intervention
Dietary interventions might include dietary education alone or combined with a moderate energy restriction, 110 with structured dietary plans or advice preferred over broad dietary principles, particularly for adolescents. 111 Principles of dietary education focus on adoption of dietary intake patterns consistent with local dietary guidelines—eg, increased intake of vegetables and fruit, reductions in energy-dense nutrient-poor foods and sugar sweetened beverages, and improvement in dietary behaviours such as encouraging mealtime routines and family meals. 110 , 112 One common approach, the traffic light diet, categorises foods by energy density, with green low-energy foods that can be eaten freely, yellow foods eaten moderately, and red foods eaten occasionally due to a higher energy-density. 107 Dietary approaches aim to be nutritionally complete and to address and prevent nutritional deficiencies. 113 , 114 However, children and adolescents might present for obesity treatment with relatively poor diet quality; 115 therefore, an initial goal of improving the baseline diet might be appropriate. Selection of dietary strategies should be informed by individual preference and circumstances, family environment, and available support.

Physical activity
Physical activity components might include provision of education or a structured exercise programme, or both, in line with local guidelines. The goals of exercise interventions should be to offer a safe, supportive, fun, and non-judgemental environment for children with obesity to engage in active play. It can also enable socialisation with peers and facilitate motor competence, confidence, and optimisation of fundamental motor skills. The aims of exercise itself are to increase physical fitness, reduce or attenuate obesity-related complications, improve quality of life, and support the child to reach age-appropriate physical activity levels. 116 , 117 Studies have found that the most effective exercise interventions consist of sessions lasting 60 min or more on at least 3 days per week for at least 12 weeks duration. 118 Training programmes should be tailored to the child's physical abilities and fitness level evaluated at baseline using standardised and age-appropriate outcome measures. Intervention should be fun, leverage the preferences of the child while following frequency, intensity, duration, type, volume, and progression principles. 119
Children with obesity often experience personal barriers to movement and exercise. Therefore tailoring and adapting paediatric exercise interventions will often be necessary, particularly for those that report musculoskeletal pain, high rates of fatigue, urinary incontinence, skin chafing, or have impaired motor skills. Additionally, the presence of intellectual or physical disabilities should be considered. As such, the type of exercise intervention offered will vary according to the child's clinical presentation and the desired outcome (eg, improvements in aerobic fitness, increased enjoyment, or reduction of fat-mass). The health professional might need to consider whether the intervention incorporates weight-bearing or non-weight bearing games, aerobic, proprioceptive and resistance exercises, individual or group-based work, or whether specific physiotherapy approaches might also need to be integrated to address underlying impairments. Appropriate monitoring and evaluation of the exercise intervention is recommended and should include the perspective of the child in addition to psychometrically robust outcome measurement. Additional guidance is available elsewhere. 120 , 121 , 122
Screen time and sedentary behaviours
Sedentary behaviours, including screen time, are distinct from physical activity and need to be addressed as part of a comprehensive behavioural change programme. Interventions that are successful in decreasing screen time in the short term include strong parental engagement, structural changes in the home environment (eg, removing or replacing home or bedroom electronic games access), and e-monitoring of time on digital devices. 123 These interventions tend to be more effective in young children.
There are few trials targeting sleep in the treatment of paediatric obesity, especially in older children and adolescents. Sleep interventions in preschool-aged children are associated with reduced weight gain. 124 Improvements in sleep hygiene, such as a consistent bedtime routine, regular sleep-wake times, and reduced screen times in the evening, are likely to have many co-benefits and positive effects on other weight-related behaviours.
Behavioural support strategies
Changes in dietary intake, physical activity, sedentary behaviours, and sleep are underpinned by strategies supporting behaviour change with the vast majority of interventions using a form of behavioural therapy. Common behaviour change techniques include goal setting, stimulus control (modifying the environment), and self-monitoring. 107 , 125 Motivational interviewing techniques such as reflective listening and shared decision making might also be used by healthcare workers to improve motivation for behaviour change. 126 , 127
The effectiveness of behaviour change interventions are well described, with modest reductions in weight-related outcomes 128 , 129 and improvements in cardiometabolic health. 130 The 2017 Cochrane reviews 128 , 129 found that behaviour changing interventions were more successful than no treatment or usual care comparators in reducing BMI (–0·53 kg/m 2 [95% CI –0·82 to –0·24], low-quality evidence in children; –1·18 kg/m 2 [–1·67 to –0·69], low-quality evidence in adolescents), and BMI z score (–0·06 units [–0·10 to –0·02], low-quality evidence in children; –0·13 [–0·21 to –0·05], low quality evidence in adolescents). 128 , 129 Effects were maintained at 18 to 24 months' follow-up for both BMI and BMI z-score in adolescents. 128 In children and adolescents aged 5–18 years, behavioural interventions are also associated with reductions in total cholesterol, triglycerides, fasting insulin, and HOMA-insulin resistance 130 as well as increased sleep duration and a reduced prevalence of obstructive sleep apnea. 131
A systematic review of 109 randomised controlled trials (RCTs) found that dietary interventions achieve a modest reduction in energy intake, reduced intake of sugar sweetened beverages, and increased intake of fruit and vegetables in children and adolescents aged 2–20 years. 132 The beneficial effects of supervised exercise in children and adolescents with obesity on measures of anthropometry and adiposity include reductions in BMI, bodyweight, waist circumference, and percent body fat. 133 Improvements in obesity-related complications are also observed, independent of changes in anthropometry including increased cardiorespiratory fitness, 134 improved muscle performance 80 and fundamental motor skills, 135 reductions in insulin resistance, reductions in fasting glucose and insulin levels, 136 improved lipid profile, 137 and reductions in blood pressure. 138 , 139 Exercise might also yield additional benefits related to appetite and response to food cues.
Behavioural obesity treatment is also associated with improved psychosocial health, including improved quality of life, 128 , 140 and body image 141 compared with no treatment or usual care comparators post-intervention and improvements in self-esteem at latest follow-up in those aged 4–19 years at baseline. 141 In assessing mental health, no difference between intervention and no-treatment comparator groups have been seen for the changes in symptoms of depression, 142 anxiety, 142 and eating disorders, 143 during the intervention period. However, symptoms of depression, anxiety, and eating disorders are reduced post-intervention or at follow-up in intervention arms, with no worsening of symptoms within groups. 142 , 143 , 144 , 145 Adverse effects of lifestyle interventions are poorly reported. 128 , 129 Where reported, no significant differences in adverse events between intervention and control groups are seen. 146
Psychological interventions
Psychological interventions, incorporated alongside traditional behavioural obesity treatment strategies, or as stand-alone interventions, target psychological factors that might contribute to eating behaviours and obesity, including distorted body image, negative mood, and stimulus control. 125 , 147 A core objective of psychological interventions is to reduce barriers for behaviour change. 147 Cognitive behavioural therapy (CBT) is the most frequently used approach, and addresses the relationship between cognitions, feelings, and behaviours using behavioural therapy techniques to modify behaviours and cognitive techniques to modify dysfunctional cognitions. 125 CBT-based interventions have been shown to result in healthier food habits, improved psychosocial health, quality of life, self-esteem, and anthropometric variables including BMI and waist circumference in children and adolescents. 125 Acceptance and commitment therapy (ACT), which encourage acceptance rather than avoidance of internal experiences (eg, food cravings), have shown to be effective in the management of obesity in adults and are an emerging area of research in adolescence. Pilot studies have found ACT-based interventions to be feasible and acceptable in adolescents with obesity, 148 , 149 with further research underway. Weight-neutral interventions, aiming to promote healthy behaviours and improve physical and psychosocial health without promoting weight loss, are an emerging area of practice in adults. There is currently insufficient evidence to guide the use of weight-neutral approaches in paediatrics.
Mode of intervention delivery
Evidence for behavioural change programmes encompass a variety of modes of delivery including group programmes, one-on-one therapist sessions, and various forms of e-health support. 128 , 129 , 150 , 151 No one form is necessarily superior to another, although a combination of such approaches might be used in a comprehensive integrated programme. Availability of resources; time constraints for health professionals, patients, and families; and appropriate health professional training will influence treatment provided alongside the child's developmental stage and patient or parent preferences. The COVID-19 pandemic has highlighted the need for effective interventions that can be delivered remotely without exacerbating existing social and technological disparities. 152 A 2021 review describes the considerations for successful implementation for such telemedicine approaches. 153
Eating disorders risk management
Children and adolescents with obesity are vulnerable to the development of eating disorders because obesity and eating disorders have several shared risk factors. 76 , 154 Disordered eating attitudes and behaviours, as precursors to eating disorders, are also elevated in children and adolescents with obesity. 155 Although obesity treatment helps improve eating disorder symptoms, including binge eating and loss of control in most youth with obesity, 143 , 144 a small number undergoing obesity treatment might develop an eating disorder during or after an intervention. 143 Although whether this low risk of developing eating disorders differs in youth who do not present for clinical treatment remains unclear, it is an important consideration for clinicians providing obesity care. For over a decade, it has been recommended that there be screening of disordered eating attitudes and behaviours before obesity treatment, 76 , 154 particularly with the use of dietary interventions, 112 to identify undiagnosed eating disorders. However, guidance on how this should occur in practice is scarce. Screening tools that assess for binge eating disorder specifically in children 156 and adolescents 157 with obesity are available but a self-report screening tool to assess for the broad spectrum of eating disorders for those with obesity and with adequate diagnostic accuracy is lacking. Eating disorder symptoms should not prevent the provision of obesity care; 158 rather, a combination of self-report questionnaires and clinical assessment might be needed to assess and monitor eating disorder risk in practice. 76
Intensive dietary interventions
Use of intensive dietary interventions is an emerging area of research and practice, particularly in post-pubertal adolescents with obesity related comorbidity or severe obesity. 110 , 159 Prescriptive dietary approaches may be delivered within the context of a multicomponent behavioural intervention, by experienced paediatric dietitians with medical supervision. 159 Very Low Energy Diets (VLEDs), consisting of an energy prescription of approximately 800 kcal/day or less than 50% of estimated energy requirements, often involving the use of nutritionally complete meal replacement products, are one such option. A meta-analysis of 20 studies found VLEDs to be effective at inducing rapid short term weight loss in children and adolescents with obesity (–10·1kg [95% CI 8·7 to 11·4] over 3 to 20 weeks), though follow-up beyond 12-months is scarce. 160 Data on VLEDs in the treatment of youth with early onset type 2 diabetes are limited to a small pilot study 161 and a medical chart review, 162 however, they have shown early short-term success and the possibility of reducing the requirement for medication, including insulin, and inducing remission of diabetes. 163 However, there is need for further research. 163 Variations in macronutrient distribution have been widely studied due to hypothesised effects on satiety, particularly higher protein (20–30% of energy intake from protein) approaches and very low carbohydrate diets (<50g per day or <10% energy from carbohydrate) aiming to induce ketosis. Although lower carbohydrate approaches show a significantly greater reduction in weight-related outcomes in the short-term (<6 months), dietary patterns with varied macronutrient distribution do not show superior effects in the longer term in children and adolescents. 164 Pilot studies on the use of various regimens of intermittent energy restriction in adolescents with obesity have shown these to be feasible and acceptable. 165 , 166 Larger trials are underway.
Anti-obesity medications
Anti-obesity medications are an important part of comprehensive obesity treatment. Pharmacotherapy, when combined with behavioural change interventions, can be particularly useful in patients for whom behavioural approaches alone have proven suboptimal or unsuccessful in reducing BMI and improving obesity-related complications. Although regulatory approval and availability varies by country and region, there is one anti-obesity medication that is approved by most regulatory agencies (including the United States Food and Drug Administration and the European Medicines Agency) for chronic obesity treatment in adolescents aged 12–18 years, which is liraglutide at 3 mg daily. Liraglutide, delivered via subcutaneous injection, belongs to the glucagon-like peptide-1 receptor agonist class, which acts on its receptors in the hypothalamus to reduce appetite, slow gastric motility, and act centrally on the hind brain to enhance satiety. 167 In the largest RCT of liraglutide 3 mg among adolescents (12 to <18 years old) with obesity, whereby all participants also received lifestyle therapy, the mean placebo-subtracted BMI reduction was approximately 5% with one year of treatment. 168 More participants in the liraglutide versus placebo group had a decline in BMI by 5% (43·3% liraglutide vs 18·7% placebo) and 10% (26·1% liraglutide vs 8·1% placebo). Importantly, no new safety signals were observed in the adolescent trial in relation to previous adult trials. The most reported adverse events were gastrointestinal and were more frequent in the liraglutide group (64·8% liraglutide vs 36·5% placebo). No statistically significant improvements in cardiometabolic risks factors or quality of life were observed between groups.
Other medications have been evaluated for the treatment of paediatric obesity yet are not approved in the EU and many other countries. These medications include orlistat (mean placebo-subtracted BMI reduction <3%), phentermine (no randomised, controlled trials conducted in children or adolescents), topiramate (mean placebo-subtracted BMI reduction <3%), and metformin (mean placebo-subtracted BMI reduction of around 3%). 169 , 170 , 171 , 172 Two anti-obesity medications are currently under evaluation for the treatment of adolescent obesity: semaglutide 2·4 mg weekly ( {"type":"clinical-trial","attrs":{"text":"NCT04102189","term_id":"NCT04102189"}} NCT04102189 ) and the combination of phentermine and topiramate ( {"type":"clinical-trial","attrs":{"text":"NCT03922945","term_id":"NCT03922945"}} NCT03922945 ). Results from these clinical trials are expected in 2022 with regulatory review and perhaps approval in 2022–23. Additional therapies are available for monogenic forms of obesity, 173 details of which are beyond the scope of the current Review.
Metabolic and bariatric surgery
Metabolic and bariatric surgery is the most effective and durable treatment for inducing weight loss in adolescents with obesity, with average BMI reductions in various longitudinal studies of the Roux-en-Y gastric bypass and vertical sleeve gastrectomy ranging from approximately 25–40% at 1–9 years post-surgery. 174 , 175 , 176 , 177 , 178 Beyond weight loss, metabolic and bariatric surgery leads to clinically meaningful improvements in obesity-related complications, cardiometabolic risk factors, musculoskeletal pain, and functional mobility. 174 , 178 , 179 , 180 Importantly, although the relative degree of weight loss with metabolic and bariatric surgery is similar between adults and adolescents, emerging data suggest that serious complications like type 2 diabetes and hypertension might be more likely to remit in adolescents than in adults. 177 Improved quality of life and reduced symptoms of depression are also seen following metabolic and bariatric surgery in the short term. 181 , 182 However, incidence and remission of mental health problems are highly variable following metabolic and bariatric surgery; a proportion of youth will continue to experience mental health concerns post-surgery that can persist long-term, with a subset experiencing suicidal ideations and behaviours. 183 , 184 , 185 , 186 Pre-surgical and post-surgical psychological support is recommended 187 and is associated with improved psychosocial health and weight loss maintenance. 188 Mortality rates 5 years following metabolic and bariatric surgery in adolescents (1·9%) appear to be similar to that of adults (1·8%) but adolescents tend to require abdominal reoperations more frequently than adults and have a higher incidence of low levels of ferritin, 177 requiring monitoring of nutritional status. 189 Until approximately 5 years ago, clinical practice guidelines for metabolic and bariatric surgery restricted eligibility to older adolescents having reached skeletal maturity. However, contemporary guidelines have now suggested that there need not be any lower age limit for consideration of metabolic and bariatric surgery as long as other medical eligibility requirements are met (detailed rationale and other considerations such as pubertal progression, linear growth, and pregnancy). 190 , 191 The uptake of metabolic and bariatric surgery has been extremely limited as surgery is typically reserved for the most severe forms of obesity and for patients with significant obesity-associated complications. 192 Other factors probably contributing to the low use of metabolic and bariatric surgery among adolescents include the perceived invasiveness and irreversibility of the procedures, lingering concerns regarding long-term safety, lack of access to surgical centres, poor insurance coverage, and referral bias.
Treatment selection
Treatment outcomes for paediatric obesity are highly variable 193 , 194 , 195 and a thorough baseline assessment guides the health professional on the appropriate treatment at a given time for a given patient. Baseline factors known to negatively predict weight-related outcomes with treatment include high levels of picky eating in preschool age children, 196 poor family functioning, or low self-concept 193 in the child and maternal psychological distress. 197 Positive predictors of treatment effect on weight include younger age, lower baseline BMI, higher global self-esteem, and adherence 198 to follow up. Predictors of treatment response represents a critically important area of future research as the ultimate goal is to match the appropriate patient to the treatment most likely to provide benefit and minimise potential risks from a non-suitable treatment plan.
Barriers to obesity treatment
Despite its growing evidence base, there remain many barriers to delivery of effective obesity treatment. For example, most RCTs have not been undertaken in culturally diverse populations, in people with complex health needs or disabilities, nor in those living with social disadvantage, all of which might make adherence to standard therapies more challenging. 199 Further, there are failures in implementing the known evidence into routine service delivery. An audit of adult and paediatric obesity services in 68 countries revealed poor resourcing and staffing of clinical services; a lack of integration of services across primary, secondary and tertiary level care; inadequate health professional training; widespread health system stigma towards people with obesity; and frequent unaffordability and inaccessibility of services. 200 Future research is needed to both develop the evidence base for obesity treatment in priority populations and in LMICs, as well as bring an implementation science perspective to obesity service delivery.
Conclusions
Structured, supported and life-long care for children and adolescents with obesity and their families is essential. The provision of care will change over time based on growth, development, life stage, and available support. More research is needed on management of obesity in disadvantaged communities and in those from LMICs, and on the real-world implementation of management approaches. Importantly, clinical care needs to be underscored by modifications to the social, commercial, and built environments which currently promote, rather than protect against, obesity, together with associated policy changes.
Search strategy and selection criteria
References for this Review were identified through searches of Medline (PubMed) and the Cochrane Database of Systematic Reviews for articles published up to Nov 1, 2021, using combinations of terms such as “child”, “adolescent”, “obesity”, “epidemiology”, “aetiology”, “complications”, “co-morbidity”, “treatment”, “behaviour change”, “prevention”, “bariatric surgery”, “metabolic surgery”, “pharmacotherapy”, and “BMI”. Articles published in English were included. We also reviewed reference lists of published manuscripts, clinical guidelines, and other relevant reviews and meta-analyses.
Declaration of interests
ASK serves as an unpaid consultant for Novo Nordisk, Vivus, Eli Lilly, and Boehringer Ingelheim; and receives donated drug and placebo from Vivus for a National Institutes of Health funded clinical trial. LAB serves on the Advisory Committee of the ACTION Teens study, sponsored by Novo Nordisk, for which an honorarium is paid to her hospital research cost centre. All other authors declare no competing interests.
Acknowledgements
HJ was supported by the Sydney University Medical Foundation. GO was supported by funding from the Royal College of Surgeons in Ireland StAR programme (grant number 2151).
Contributors
All authors contributed to the literature search, writing, reviewing, and editing of the manuscript.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 18 May 2023
Child and adolescent obesity
- Natalie B. Lister ORCID: orcid.org/0000-0002-9148-8632 1 , 2 ,
- Louise A. Baur ORCID: orcid.org/0000-0002-4521-9482 1 , 3 , 4 ,
- Janine F. Felix 5 , 6 ,
- Andrew J. Hill ORCID: orcid.org/0000-0003-3192-0427 7 ,
- Claude Marcus ORCID: orcid.org/0000-0003-0890-2650 8 ,
- Thomas Reinehr ORCID: orcid.org/0000-0002-4351-1834 9 ,
- Carolyn Summerbell 10 &
- Martin Wabitsch ORCID: orcid.org/0000-0001-6795-8430 11
Nature Reviews Disease Primers volume 9 , Article number: 24 ( 2023 ) Cite this article
52 Citations
247 Altmetric
Metrics details
- Paediatric research
The prevalence of child and adolescent obesity has plateaued at high levels in most high-income countries and is increasing in many low-income and middle-income countries. Obesity arises when a mix of genetic and epigenetic factors, behavioural risk patterns and broader environmental and sociocultural influences affect the two body weight regulation systems: energy homeostasis, including leptin and gastrointestinal tract signals, operating predominantly at an unconscious level, and cognitive–emotional control that is regulated by higher brain centres, operating at a conscious level. Health-related quality of life is reduced in those with obesity. Comorbidities of obesity, including type 2 diabetes mellitus, fatty liver disease and depression, are more likely in adolescents and in those with severe obesity. Treatment incorporates a respectful, stigma-free and family-based approach involving multiple components, and addresses dietary, physical activity, sedentary and sleep behaviours. In adolescents in particular, adjunctive therapies can be valuable, such as more intensive dietary therapies, pharmacotherapy and bariatric surgery. Prevention of obesity requires a whole-system approach and joined-up policy initiatives across government departments. Development and implementation of interventions to prevent paediatric obesity in children should focus on interventions that are feasible, effective and likely to reduce gaps in health inequalities.
Similar content being viewed by others

Associations of dietary patterns with brain health from behavioral, neuroimaging, biochemical and genetic analyses

Effects of a personalized nutrition program on cardiometabolic health: a randomized controlled trial
Investigating nutrient biomarkers of healthy brain aging: a multimodal brain imaging study
Introduction.
The prevalence of child and adolescent obesity remains high and continues to rise in low-income and middle-income countries (LMICs) at a time when these regions are also contending with under-nutrition in its various forms 1 , 2 . In addition, during the COVID-19 pandemic, children and adolescents with obesity have been more likely to have severe COVID-19 requiring hospitalization and mechanical ventilation 3 . At the same time, the pandemic was associated with rising levels of childhood obesity in many countries. These developments are concerning, considering that recognition is also growing that paediatric obesity is associated with a range of immediate and long-term negative health outcomes, a decreased quality of life 4 , 5 , an increased presentation to health services 6 and increased economic costs to individuals and society 7 .
Body weight is regulated by a range of energy homeostatic and cognitive–emotional processes and a multifactorial interplay of complex regulatory circuits 8 . Paediatric obesity arises when multiple environmental factors — covering preconception and prenatal exposures, as well as broader changes in the food and physical activity environments — disturb these regulatory processes; these influences are now widespread in most countries 9 .
The treatment of obesity includes management of obesity-associated complications, a developmentally sensitive approach, family engagement, and support for long-term behaviour changes in diet, physical activity, sedentary behaviours and sleep 10 . New evidence highlights the role, in adolescents with more severe obesity, of bariatric surgery 11 and pharmacotherapy, particularly the potential for glucagon-like peptide 1 (GLP1) receptor agonists 12 .
Obesity prevention requires a whole-system approach, with policies across all government and community sectors systematically taking health into account, avoiding harmful health impacts and decreasing inequity. Programmatic prevention interventions operating ‘downstream’ at the level of the child and family, as well as ‘upstream’ interventions at the level of the community and broader society, are required if a step change in tackling childhood obesity is to be realized 13 , 14 .
In this Primer, we provide an overview of the epidemiology, causes, pathophysiology and consequences of child and adolescent obesity. We discuss diagnostic considerations, as well as approaches to its prevention and management. Furthermore, we summarize effects of paediatric obesity on quality of life, and open research questions.
Epidemiology
Definition and prevalence.
The World Health Organization (WHO) defines obesity as “abnormal or excessive fat accumulation that presents a risk to health” 15 . Paediatric obesity is defined epidemiologically using BMI, which is adjusted for age and sex because of the physiological changes in BMI during growth 16 . Global prevalence of paediatric obesity has risen markedly over the past four decades, initially in high-income countries (HICs), but now also in many LMICs 1 .
Despite attempts to standardize the epidemiological classification, several definitions of paediatric obesity are in use; hence, care is needed when comparing prevalence rates. The 2006 WHO Child Growth Standard, for children aged 0 to 5 years, is based on longitudinal observations of multiethnic populations of children with optimal infant feeding and child-rearing conditions 17 . The 2007 WHO Growth Reference is used for the age group 5–19 years 18 , and the 2000 US Centers for Disease Control and Prevention (CDC) Growth Charts for the age group 2–20 years 19 . The WHO and CDC definitions based on BMI-for-age charts are widely used, including in clinical practice. By contrast, the International Obesity Task Force (IOTF) definition, developed from nationally representative BMI data for the age group 2–18 years from six countries, is used exclusively for epidemiological studies 20 .
For the age group 5–19 years, between 1975 and 2016, the global prevalence of obesity (BMI >2 standard deviations (SD) above the median of the WHO growth reference) increased around eightfold to 5.6% in girls and 7.8% in boys 1 . Rates have plateaued at high levels in many HICs but have accelerated in other regions, particularly in parts of Asia. For the age group 2–4 years, between 1980 and 2015, obesity prevalence (IOTF definition, equivalent to an adult BMI of ≥30 kg/m 2 ) increased from 3.9% to 7.2% in boys and from 3.7% to 6.4% in girls 21 . Obesity prevalence is highest in Polynesia and Micronesia, the Middle East and North Africa, the Caribbean and the USA (Fig. 1 ). Variations in prevalence probably reflect different background levels of obesogenic environments, or the sum total of the physical, economic, policy, social and cultural factors that promote obesity 22 . Obesogenic environments include those with decreased active transport options, a ubiquity of food marketing directed towards children, and reduced costs and increased availability of nutrient-poor, energy-dense foods. Particularly in LMICs, the growth of urbanization, new forms of technology and global trade have led to reduced physical activity at work and leisure, a shift towards Western diets, and the expansion of transnational food and beverage companies to shape local food systems 23 .
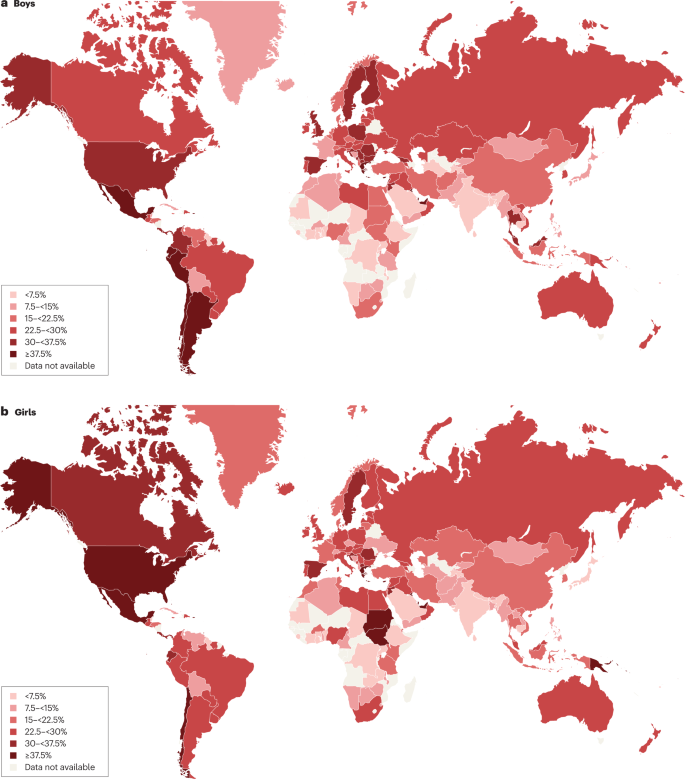
Maps showing the proportions of children and adolescents living with overweight or obesity (part a , boys; part b , girls) according to latest available data from the Global Obesity Observatory . Data might not be comparable between countries owing to differences in survey methodology.
The reasons for varying sex differences in prevalence in different countries are unclear but may relate to cultural variations in parental feeding practices for boys and girls and societal ideals of body size 24 . In 2016, obesity in the age group 5–19 years was more prevalent in girls than in boys in sub-Saharan Africa, Oceania and some middle-income countries in other regions, whereas it was more prevalent in boys than in girls in all HICs, and in East and South-East Asia 21 . Ethnic and racial differences in obesity prevalence within countries are often assumed to mirror variations in social deprivation and other social determinants of obesity. However, an independent effect of ethnicity even after adjustment for socioeconomic status has been documented in the UK, with Black and Asian boys in primary school having higher prevalence of obesity than white boys 25 .
Among individuals with obesity, very high BMI values have become more common in the past 15 years. The prevalence of severe obesity (BMI ≥120% of the 95th percentile (CDC definition), or ≥35 kg/m 2 at any age 26 , 27 ) has increased in many HICs, accounting for one-quarter to one-third of those with obesity 28 , 29 . Future health risks of paediatric obesity in adulthood are well documented. For example, in a data linkage prospective study in Israel with 2.3 million participants who had BMI measured at age 17 years, those with obesity (≥95th percentile BMI for age) had a much higher risk of death from coronary heart disease (HR 4.9, 95% CI 3.9–6.1), stroke (HR 2.6, 95% CI 1.7–4.1) and sudden death (HR 2.1, 95% CI 1.5–2.9) compared with those whose BMI fell between the 5th and 24th percentiles 30 .
Causes and risk factors
Early life is a critical period for childhood obesity development 9 , 31 , 32 , 33 . According to the Developmental Origins of Health and Disease framework, the early life environment may affect organ structure and function and influence health in later life 34 , 35 . Meta-analyses have shown that preconception and prenatal environmental exposures, including high maternal pre-pregnancy BMI and, to a lesser extent, gestational weight gain, as well as gestational diabetes and maternal smoking, are associated with childhood obesity, potentially through effects on the in utero environment 33 , 36 , 37 , 38 . Paternal obesity is also associated with childhood obesity 33 . Birthweight, reflecting fetal growth, is a proxy for in utero exposures. Both low and high birthweights are associated with later adiposity, with high birthweight linked to increased BMI and low birthweight to central obesity 33 , 39 .
Growth trajectories in early life are important determinants of later adiposity. Rapid weight gain in early childhood is associated with obesity in adolescence 32 . Also, later age and higher BMI at adiposity peak (the usual peak in BMI around 9 months of age), as well as earlier age at adiposity rebound (the lowest BMI reached between 4 and 7 years of age), are associated with increased adolescent and adult BMI 40 , 41 . Specific early life nutritional factors, including a lower protein content in formula food, are consistently associated with a lower risk of childhood obesity 42 , 43 . These also include longer breastfeeding duration, which is generally associated with a lower risk of childhood obesity 42 . However, some controversy exists, as these effects are affected by multiple sociodemographic confounding factors and their underlying mechanisms remain uncertain 44 . Some studies comparing higher and lower infant formula protein content have reported that the higher protein group have a greater risk of subsequent obesity, especially in early childhood 41 , 42 ; however, one study with a follow-up period until age 11 years found no significant difference in the risk of obesity, but an increased risk of overweight in the high protein group was still observed 42 , 43 , 45 . A high intake of sugar-sweetened beverages is associated with childhood obesity 33 , 46 .
Many other behavioural factors are associated with an increased risk of childhood obesity, including increased screen time, short sleep duration and poor sleep quality 33 , 47 , reductions in physical activity 48 and increased intake of energy-dense micronutrient-poor foods 49 . These have been influenced by multiple changes in the past few decades in the broader social, economic, political and physical environments, including the widespread marketing of food and beverages to children, the loss of walkable green spaces in many urban environments, the rise in motorized transport, rapid changes in the use of technology, and the move away from traditional foods to ultraprocessed foods.
Obesity prevalence is inextricably linked to relative social inequality, with data suggesting a shift in prevalence over time towards those living with socioeconomic disadvantage, and thus contributes to social inequalities. In HICs, being in lower social strata is associated with a higher risk of obesity, even in infants and young children 50 , whereas the opposite relationship occurs in middle-income countries 51 . In low-income countries, the relationship is variable, and the obesity burden seems to be across socioeconomic groups 52 , 53 .
Overall, many environmental, lifestyle, behavioural and social factors in early life are associated with childhood obesity. These factors cannot be seen in isolation but are part of a complex interplay of exposures that jointly contribute to increased obesity risk. In addition to multiple prenatal and postnatal environmental factors, genetic variants also have a role in the development of childhood obesity (see section Mechanisms/pathophysiology).
Comorbidities and complications
Childhood obesity is associated with a wide range of short-term comorbidities (Fig. 2 ). In addition, childhood obesity tracks into adolescence and adulthood and is associated with complications across the life course 32 , 41 , 54 , 55 .
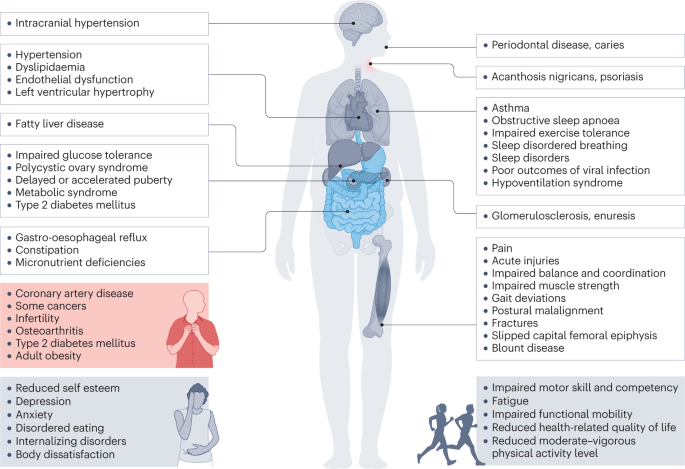
Obesity in children and adolescents can be accompanied by various other pathologies. In addition, childhood obesity is associated with complications and disorders that manifest in adulthood (red box).
Increased BMI, especially in adolescence, is linked to a higher risk of many health outcomes, including metabolic disorders, such as raised fasting glucose, impaired glucose tolerance, type 2 diabetes mellitus (T2DM), metabolic syndrome and fatty liver disease 56 , 57 , 58 , 59 . Other well-recognized obesity-associated complications include coronary heart disease, asthma, obstructive sleep apnoea syndrome (itself associated with metabolic dysfunction and inflammation) 60 , orthopaedic complications and a range of mental health outcomes including depression and low self-esteem 27 , 55 , 57 , 61 , 62 , 63 .
A 2019 systematic review showed that children and adolescents with obesity are 1.4 times more likely to have prediabetes, 1.7 times more likely to have asthma, 4.4 times more likely to have high blood pressure and 26.1 times more likely to have fatty liver disease than those with a healthy weight 64 . In 2016, it was estimated that, at a global level by 2025, childhood obesity would lead to 12 million children aged 5–17 years with glucose intolerance, 4 million with T2DM, 27 million with hypertension and 38 million with fatty liver disease 65 . These high prevalence rates have implications for both paediatric and adult health services.
Mechanisms/pathophysiology
Body weight regulation.
Body weight is regulated within narrow limits by homeostatic and cognitive–emotional processes and a multifactorial interplay of hormones and messenger substances in complex regulatory circuits (Fig. 3 ). When these regulatory circuits are disturbed, an imbalance between energy intake and expenditure leads to obesity or to poor weight gain. As weight loss is much harder to achieve than weight gain in the long term due to the regulation circuits discussed below, the development of obesity is encouraged by modern living conditions, which enable underlying predispositions for obesity to become manifest 8 , 66 .
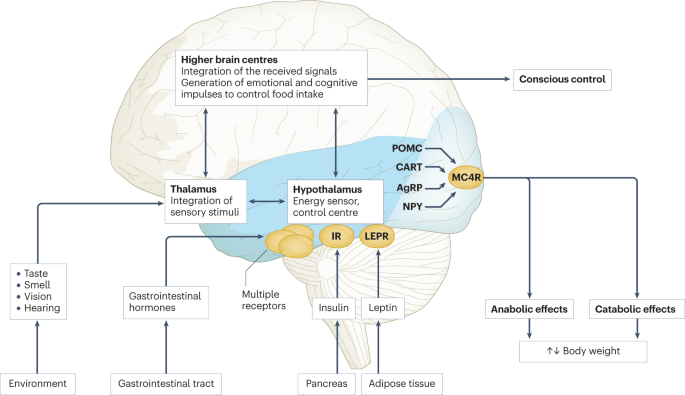
Body weight is predominantly regulated by two systems: energy homeostasis and cognitive–emotional control. Both homeostatic and non-homeostatic signals are processed in the brain, involving multiple hormone and receptor cascades 217 , 218 , 219 . This overview depicts the best-known regulatory pathways. The homeostatic system, which is mainly regulated by brain centres in the hypothalamus and brainstem, operates on an unconscious level. Both long-term signals from the energy store in adipose tissue (for example, leptin) and short-term hunger and satiety signals from the gastrointestinal tract signal the current nutrient status. During gastric distension or after the release of gastrointestinal hormones (multiple receptors are involved) and insulin, a temporary feeling of fullness is induced. The non-homeostatic or hedonic system is regulated by higher-level brain centres and operates at the conscious level. After integration in the thalamus, homeostatic signals are combined with stimuli from the environment, experiences and emotions; emotional and cognitive impulses are then induced to control food intake. Regulation of energy homeostasis in the hypothalamus involves two neuron types of the arcuate nucleus: neurons producing neuropeptide Y (NPY) and agouti-related peptide (AgRP) and neurons producing pro-opiomelanocortin (POMC). Leptin stimulates these neurons via specific leptin receptors (LEPR) inducing anabolic effects in case of decreasing leptin levels and catabolic effects in case of increasing leptin levels. Leptin inhibits the production of NPY and AgRP, whereas low leptin levels stimulate AgRP and NPY production resulting in the feeling of hunger. Leptin directly stimulates POMC production in POMC neurons. POMC is cleaved into different hormone polypeptides including α-melanocyte-stimulating hormone which in turn activates melanocortin 4 receptors (MC4R) of cells in the nucleus paraventricularis of the hypothalamus, leading to the feeling of satiety. CART, cocaine and amphetamine responsive transcript; IR, insulin receptor.
In principle, there are two main systems in the brain which regulate body weight 8 , 66 (Fig. 3 ): energy homeostasis and cognitive–emotional control. Energy homeostasis is predominantly regulated by brain centres in the hypothalamus and brainstem and operates at an unconscious level. Both long-term signals from the adipose tissue energy stores and short-term hunger and satiety signals from the gastrointestinal tract signal the current nutrient status 8 , 66 . For example, negative energy balance leading to reduced fat mass results in reduced leptin levels, a permanently reduced urge to exercise and an increased feeling of hunger. During gastric distension or after the release of gastrointestinal hormones and insulin, a temporary feeling of fullness is induced 8 , 66 . Cognitive–emotional control is regulated by higher brain centres and operates at a conscious level. Here, the homeostatic signals are combined with stimuli from the environment (sight, smell and taste of food), experiences and emotions 8 , 66 . Disorders at the level of cognitive–emotional control mechanisms include emotional eating as well as eating disorders. For example, the reward areas in the brain of people with overweight are more strongly activated by high-calorie foods than those in the brain of people with normal weight 67 . Both systems interact with each other, and the cognitive–emotional system is strongly influenced by the homeostatic control circuits.
Disturbances in the regulatory circuits of energy homeostasis can be genetically determined, can result from disease or injury to the regulatory centres involved, or can be caused by prenatal programming 8 , 66 . If the target value of body weight has been shifted, the organism tries by all means (hunger, drive) to reach the desired higher weight. These disturbed signals of the homeostatic system can have an imperative, irresistible character, so that a conscious influence on food intake is no longer effectively possible 8 , 66 . The most important disturbances of energy homeostasis are listed in Table 1 .
The leptin pathway
The peptide hormone leptin is primarily produced by fat cells. Its production depends on the amount of adipose tissue and the energy balance. A negative energy balance during fasting results in a reduction of circulating leptin levels by 50% after 24 h (ref. 68 ). In a state of weight loss, leptin production is reduced 69 . In the brain, leptin stimulates two neuron types of the arcuate nucleus in the hypothalamus via specific leptin receptors: neurons producing neuropeptide Y (NPY) and agouti-related peptide (AgRP) and neurons producing pro-opiomelanocortin (POMC). High leptin levels inhibit the production of NPY and AgRP, whereas low leptin levels stimulate AgRP and NPY production. By contrast, leptin directly stimulates POMC production in POMC neurons (Fig. 3 ). POMC is a hormone precursor that is cleaved into different hormone polypeptides by specific enzymes, such as prohormone convertase 1 (PCSK1). This releases α-melanocyte-stimulating hormone (α-MSH) which in turn activates melanocortin 4 receptors (MC4R) of cells in the nucleus paraventricularis of the hypothalamus, leading to the feeling of satiety. Rare, functionally relevant mutations in the genes for leptin and leptin receptor, POMC , PCSK1/3 or MC4R lead to extreme obesity in early childhood. These forms of obesity are potential indications for specific pharmacological treatments, for example setmelanotide 70 , 71 . MC4R mutations are the most common cause of monogenic obesity, as heterozygous mutations can be symptomatic depending on the functional impairment and with variable penetrance and expression. Other genes have been identified, in which rare heterozygous pathological variants are also associated with early onset obesity (Table 1 ).
Pathological changes in adipose tissue
Adipose tissue can be classified into two types, white and brown adipose tissue. White adipose tissue comprises unilocular fat cells and brown adipose tissue contains multilocular fat cells, which are rich in mitochondria 72 . A third type of adipocyte, beige adipocytes, within the white adipose tissue are induced by prolonged exposure to cold or adrenergic signalling, and show a brown adipocyte-like morphology 72 . White adipose tissue has a large potential to change its volume to store energy and meet the metabolic demands of the body. The storage capacity and metabolic function of adipose tissue depend on the anatomical location of the adipose tissue depot. Predominant enlargement of white adipose tissue in the visceral, intra-abdominal area (central obesity) is associated with insulin resistance and an increased risk of metabolic disease development before puberty. Accumulation of adipose tissue in the hips and flanks has no adverse effect and may be protective against metabolic syndrome. In those with obesity, adipose tissue is characterized by an increased number of adipocytes (hyperplasia), which originate from tissue-resident mesenchymal stem cells, and by enlarged adipocytes (hypertrophy) 73 . Adipocytes with a very large diameter reach the limit of the maximal oxygen diffusion distance, resulting in hypoxia, the development of an inflammatory expression profile (characterized by, for example, leptin, TNF and IL-6) and adipocyte necrosis, triggering the recruitment of leukocytes. Resident macrophages switch from the anti-inflammatory M2 phenotype to a pro-inflammatory M1 phenotype, which is associated with insulin resistance, further promoting local sterile inflammation and the development of fibrotic adipose tissue. This process limits the expandability of the adipose tissue for further storage of triglycerides. In the patient, the increase in fat mass in obesity is associated with insulin resistance and systemic low-grade inflammation characterized by elevated serum levels of C-reactive protein and pro-inflammatory cytokines. The limitation of adipose tissue expandability results in storage of triglycerides in other organs, such as the liver, muscle and pancreas 74 .
Genetics and epigenetics in the general population
Twin studies have found heritability estimates for BMI of up to 70% 75 , 76 . In contrast to rare monogenic forms of obesity, which are often caused by a single genetic defect with a large effect, the genetic background of childhood obesity in the general population is shaped by the joint effects of many common genetic variants, each of which individually makes a small contribution to the phenotype. For adult BMI, genome-wide association studies, which examine associations of millions of such variants across the genome at the same time, have identified around 1,000 genetic loci 77 . The largest genome-wide association studies in children, which include much smaller sample sizes of up to 60,000 children, have identified 25 genetic loci for childhood BMI and 18 for childhood obesity, the majority of which overlap 78 , 79 . There is also a clear overlap with genetic loci identified in adults, for example for FTO , MC4R and TMEM18 , but this overlap is not complete, some loci are specific to early life BMI, or have a relatively larger contribution in childhood 78 , 79 , 80 . These findings suggest that biological mechanisms underlying obesity in childhood are mostly similar to those in adulthood, but the relative influence of these mechanisms may differ at different phases of life.
The role of epigenetic processes in childhood and adolescent obesity has gained increasing attention. In children, several studies found associations between DNA methylation and BMI 81 , 82 , 83 , 84 , but a meta-analysis including data from >4,000 children identified only minimal associations 85 . Most studies support the hypothesis that DNA methylation changes are predominantly a consequence rather than a cause of obesity, which may explain the lower number of identified (up to 12) associations in children, in whom duration of exposure to a higher BMI is shorter than in adults, in whom associations with DNA methylation at hundreds of sites have been identified 85 , 86 , 87 . In addition to DNA methylation, some specific circulating microRNAs have been found to be associated with obesity in childhood 84 .
The field of epigenetic studies in childhood obesity is relatively young and evolving quickly. Future studies will need to focus on defining robust associations in blood as well as other tissues and on identifying cause-and-effect relationships. In addition, other omics, such as metabolomics and proteomics, are promising areas that may contribute to an improved aetiological understanding or may provide biological signatures that can be used as predictive or prognostic markers of childhood obesity and its comorbidities.
Parental obesity and childhood obesity
There is an established link between increased parental BMI and increased childhood BMI 88 , 89 . This link may be due to shared genetics, shared environment, a direct intrauterine effect of maternal BMI or a combination of these factors. In the case of shared genetics, the child inherits BMI-increasing genetic variants from one or both parents. Shared environmental factors, such as diet or lifestyle, may also contribute to an increased BMI in both parents and child. In addition, maternal obesity might create an intrauterine environment that programmes metabolic processes in the fetus, which increases the risk of childhood obesity. Some studies show larger effects of maternal than paternal BMI, indicating a potential causal intrauterine mechanism of maternal obesity, but evidence showing similar maternal and paternal effects is increasing. The data may indicate that there is only a limited direct intrauterine effect of maternal obesity on childhood obesity; rather, genetic effects inherited from the mother or father, or both, and/or shared environmental factors may contribute to childhood obesity risk 90 , 91 , 92 , 93 , 94 , 95 .
Diagnosis, screening and prevention
Diagnostic work-up.
The extent of overweight in clinical practice is estimated using BMI based on national charts 96 , 97 , 98 , 99 , 100 . Of note, the clinical classification of overweight or obesity differ depending on the BMI charts used and national recommendations; hence, local guidelines should be referred to. For example, the US CDC Growth Charts and several others use the 85th and 95th centile cut-points to denote overweight and obesity, respectively 19 . The WHO Growth Reference for children aged 5–19 years defines cut-points for overweight and obesity as a BMI-for-age greater than +1 and +2 SDs for BMI for age, respectively 18 . For children <5 years of age, overweight and obesity are defined as weight-for-height greater than +2 and +3 SDs, respectively, above the WHO Child Growth Standards median 17 . The IOTF and many countries in Europe use cut-points of 85th, 90th and 97th to define overweight, obesity and extreme obesity 26 .
BMI as an indirect measurement of body fat has some limitations; for example, pronounced muscle tissue leads to an increase in BMI, and BMI is not independent of height. In addition, people of different ethnicities may have different cut-points for obesity risk; for example, cardiometabolic risk occurs at lower BMI values in individuals with south Asian than in those with European ancestry 101 . Thus, BMI is best seen as a convenient screening tool that is supplemented by clinical assessment and investigations.
Other measures of body fat may help differentiate between fat mass and other tissues. Some of these tools are prone to low reliability, such as body impedance analyses (high day-to-day variation and dependent on level of fluid consumption) or skinfold thickness (high inter-observer variation), or are more expensive or invasive, such as MRI, CT or dual-energy X-ray absorptiometry, than simpler measures of body composition or BMI assessment.
Primary diseases rarely cause obesity in children and adolescents (<2%) 102 . However, treatable diseases should be excluded in those with obesity. A suggested diagnostic work-up is summarized in Fig. 4 . Routine measurement of thyroid-stimulating hormone (TSH) is not recommended 96 . Moderately elevated TSH levels (usually <10 IU/l) are frequently observed in obesity and are a consequence, and not a cause, of obesity 103 . In a growing child with normal height velocity, a normal BMI at the age of 2 years and normal cognitive development, no further diagnostic steps are necessary to exclude primary diseases 96 , 104 .
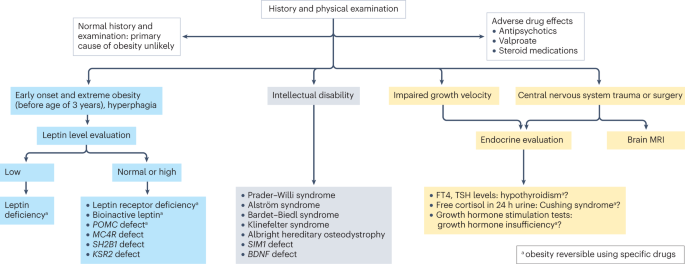
Concerning findings from a detailed medical history and physical examination will lead to further examinations. In individuals with early onset, extreme obesity (before age 3 years) and signs of hyperphagia, serum leptin level should be measured to rule out the extremely rare condition of congenital leptin deficiency. In individuals with normal or high leptin levels, genetic testing is indicated to search for monogenetic obesity. In individuals with intellectual disability, a syndromic disease may be present. Signs of impaired growth velocity or the history of central nervous system trauma or surgery will result in deeper endocrine evaluation and/or brain MRI. BDNF , brain-derived neurotropic factor; FT4, free thyroxin; KSR2 , kinase suppressor of ras 2; MC4R , melanocortin 4 receptor; POMC , pro-opiomelanocortin; SH2B1 , Src-homology 2 (SH2) B adapter protein 1; SIM1 , single-minded homologue 1; TSH, thyroid-stimulating hormone.
Clinical findings which need no further examination include pseudogynaecomastia (adipose tissue mimicking breast development; differentiated from breast tissue by ultrasonography), striae (caused by rapid weight increase) and a hidden penis in suprapubic adipose tissue (differentiated from micropenis by measurement of stretched penis length while pressing down on the suprapubic adipose tissue) 96 , 105 . Girls with obesity tend to have an earlier puberty onset (usually at around 8–9 years of age) and boys with severe obesity may have a delayed puberty onset (usually at around 13–14 years of age) 106 . Thus, if pubertal onset is slightly premature in girls or slightly delayed in boys, no further endocrine assessment is necessary.
Assessment of obesity-associated comorbidities
A waist to height ratio of >0.5 is a simple tool to identify central obesity 107 , 108 . Screening for cardiometabolic risk factors and fatty liver disease is recommended, especially in adolescents, and in those with more severe obesity or central adiposity, a strong family history of T2DM or premature heart disease, or relevant clinical symptoms, such as high blood pressure or acanthosis nigricans 96 , 97 , 98 , 99 , 109 . Investigations generally include fasting glucose levels, lipid profile, liver function and glycated haemoglobin, and might include an oral glucose tolerance test, polysomnography, and additional endocrine tests for polycystic ovary syndrome 96 , 97 , 98 , 99 .
T2DM in children and adolescents often occurs in the presence of a strong family history and may not be related to obesity severity 110 . T2DM onset usually occurs during puberty, a physiological state associated with increased insulin resistance 111 and, therefore, screening for T2DM should be considered in children and adolescents with obesity and at least one risk factor (family history of T2DM or features of metabolic syndrome) starting at pubertal onset 112 . As maturity-onset diabetes of the young (MODY) type II and type III are more frequent than T2DM in children and adolescents in many ethnicities, genetic screening for MODY may be appropriate 112 . Furthermore, type 1 diabetes mellitus (T1DM) should be excluded by measurement of autoantibodies in any individual with suspected diabetes with obesity. The differentiation of T2DM from MODY and T1DM is important as the diabetes treatment approaches differ 112 .
Several comorbidities of obesity should be considered if specific symptoms occur 96 , 109 . For polycystic ovary syndrome in hirsute adolescent girls with oligomenorrhoea or amenorrhoea, moderately increased testosterone levels and decreased sex hormone binding globulin levels are typical laboratory findings 113 . Obstructive sleep apnoea can occur in those with more severe obesity and who snore, have daytime somnolence or witnessed apnoeas. Diagnosis is made by polysomnography 114 . Minor orthopaedic disorders, such as flat feet and genu valgum, are frequent in children and adolescents with obesity and may cause pain. Major orthopaedic complications include slipped capital femoral epiphyses (acute and chronic), which manifest with hip and knee pain in young adolescents and are characterized by reduced range of hip rotation and waddling gait; and Blount disease (tibia vara), typically occurring in children aged 2–5 years 105 , 115 . In addition, children and adolescents with extreme obesity frequently have increased dyspnoea and decreased exercise capacity. A heightened demand for ventilation, elevated work of breathing, respiratory muscle inefficiency and diminished respiratory compliance are caused by increased truncal fat mass. This may result in a decreased functional residual capacity and expiratory reserve volume, ventilation to perfusion ratio abnormalities and hypoxaemia, especially when supine. However, conventional respiratory function tests are only mildly affected by obesity except in extreme cases 116 . Furthermore, gallstones should be suspected in the context of abdominal pain after rapid weight loss, which can be readily diagnosed via abdominal ultrasonography 105 . Finally, pseudotumor cerebri may present with chronic headache, and depression may present with flat affect, chronic fatigue and sleep problems 105 .
Obesity in adolescents can also be associated with disordered eating, eating disorders and other psychological disorders 117 , 118 . If suspected, assessment by a mental health professional is recommended.
A comprehensive approach
The 2016 report of the WHO Commission on Ending Childhood Obesity stated that progress in tackling childhood obesity has been slow and inconsistent, with obesity prevention requiring a whole-of-government approach in which policies across all sectors systematically take health into account, avoiding harmful health impacts and, therefore, improving population health and health equity 13 , 119 . The focus in developing and implementing interventions to prevent obesity in children should be on interventions that are feasible, effective and likely to reduce health inequalities 14 . Importantly, the voices of children and adolescents living with social disadvantage and those from minority groups must be heard if such interventions are to be effective and reduce inequalities 120 .
Figure 5 presents a system for the prevention of childhood obesity within different domains of the socioecological model 121 and highlights opportunities for interventions. These domains can be described on a continuum, from (most downstream) individual and interpersonal (including parents, peers and wider family) through to organizational (including health care and schools), community (including food, activity and environment), society (including media and finally cultural norms) and (most upstream) public policy (from local to national level). Interventions to prevent childhood obesity can be classified on the Nuffield intervention ladder 122 . This framework was proposed by the Nuffield Council on Bioethics in 2007 (ref. 122 ) and distributes interventions on the ladder steps depending on the degree of agency required by the individual to make the behavioural changes that are the aim of the intervention. The bottom step of the ladder includes interventions that provide information, which requires the highest agency and relies on a child, adolescent and/or family choosing (and their ability to choose) to act on that information and change behaviour. The next steps of the ladder are interventions that enable choice, guide choice through changing the default policy, guide choice through incentives, guide choice through disincentives, or restrict choice. On the top-most step of the ladder (lowest agency required) are interventions that eliminate choice.
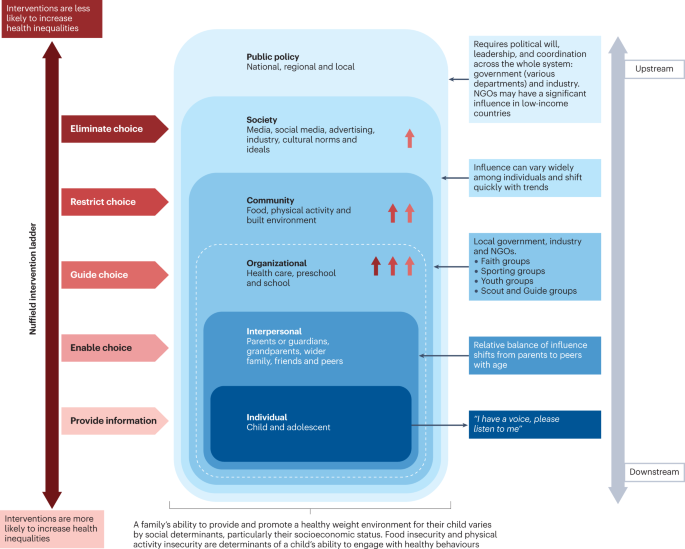
This schematic integrates interventions that were included in a Cochrane review 127 of 153 randomized controlled trials of interventions to prevent obesity in children and are high on the Nuffield intervention ladder 122 . The Nuffield intervention ladder distributes interventions depending on the degree of agency required for the behavioural changes that are the aim of the intervention. The socioecological model 121 comprises different domains (or levels) from the individual up to public policy. Interventions targeting the individual and interpersonal domains can be described as downstream interventions, and interventions within public policy can be described as the highest level of upstream interventions. Within each of these domains, arrow symbols with colours corresponding to the Nuffield intervention ladder category are used to show interventions that were both included in the Cochrane review 127 and that guide, restrict or eliminate choice as defined by the Nuffield intervention ladder 122 . Upstream interventions, and interventions on the top steps of the Nuffield ladder, are more likely to reduce inequalities. NGO, non-governmental organization.
Downstream and high-agency interventions (on the bottom steps of the Nuffield ladder) are more likely to result in intervention-generated inequalities 123 . This has been elegantly described and evidenced, with examples from the obesity prevention literature 124 , 125 . A particularly strong example is a systematic review of 38 interventions to promote healthy eating that showed that food price (an upstream and low-agency intervention) seemed to decrease inequalities, all interventions that combined taxes and subsidies consistently decreased inequalities, and downstream high-agency interventions, especially dietary counselling, seemed to increase inequalities 126 .
Effectiveness of prevention interventions
A 2019 Cochrane review of interventions to prevent obesity in children 127 included 153 randomized controlled trials (RCTs), mainly in HICs (12% were from middle-income countries). Of these RCTs, 56% tested interventions in children aged 6–12 years, 24% in children aged 0–5 years, and 20% in adolescents aged 13–18 years. The review showed that diet-only interventions to prevent obesity in children were generally ineffective across all ages. Interventions combining diet and physical activity resulted in modest benefits in children aged 0–12 years but not in adolescents. However, physical activity-only interventions to prevent obesity were effective in school-age children (aged 5–18 years). Whether the interventions were likely to work equitably in all children was investigated in 13 RCTs. These RCTs did not indicate that the strategies increased inequalities, although most of the 13 RCTs included relatively homogeneous groups of children from disadvantaged backgrounds.
The potential for negative unintended consequences of obesity prevention interventions has received much attention 128 . The Cochrane review 127 investigated whether children were harmed by any of the strategies; for example, by having injuries, losing too much weight or developing damaging views about themselves and their weight. Of the few RCTs that did monitor these outcomes, none found any harms in participants.
Intervention levels
Most interventions (58%) of RCTs in the Cochrane review aimed to change individual lifestyle factors via education-based approaches (that is, simply provide information) 129 . In relation to the socioecological model, only 11 RCTs were set in the food and physical activity environment domain, and child care, preschools and schools were the most common targets for interventions. Of note, no RCTs were conducted in a faith-based setting 130 . Table 2 highlights examples of upstream interventions that involve more than simply providing information and their classification on the Nuffield intervention ladder.
Different settings for interventions to prevent childhood obesity, including preschools and schools, primary health care, community settings and national policy, offer different opportunities for reach and effectiveness, and a reduction in inequalities.
Preschools and schools are key settings for public policy interventions for childhood obesity prevention, and mandatory and voluntary food standards and guidance on physical education are in place in many countries. Individual schools are tasked with translating and implementing these standards and guidance for their local context. Successful implementation of a whole-school approach, such as that used in the WHO Nutrition-Friendly Schools Initiative 131 , is a key factor in the effectiveness of interventions. Careful consideration should be given to how school culture can, and needs to, be shifted by working with schools to tailor the approach and manage possible staff capacity issues, and by building relationships within and outside the school gates to enhance sustainability 132 , 133 .
Primary health care offers opportunities for guidance for obesity prevention, especially from early childhood to puberty. Parent-targeted interventions conducted by clinicians in health-care or community settings have the strongest level of evidence for their effectiveness in reducing BMI z -score at age 2 years 134 . These interventions include group programmes, clinic nurse consultations, mobile phone text support or nurse home visiting, and focusing on healthy infant feeding, healthy childhood feeding behaviours and screen time.
A prospective individual participant data meta-analysis of four RCTs involving 2,196 mother–baby dyads, and involving nurse home visiting or group programmes, resulted in a small but significant reduction in BMI in infants in the intervention groups compared with control infants at age 18–24 months 134 . Improvements were also seen in television viewing time, breastfeeding duration and feeding practices. Interventions were more effective in settings with limited provision of maternal and child health services in the community. However, effectiveness diminished by age 5 years without further intervention, highlighting the need for ongoing interventions at each life stage 135 . Evidence exists that short-duration interventions targeting sleep in very early childhood may be more effective than nutrition-targeted interventions in influencing child BMI at age 5 years 136 .
Primary care clinicians can provide anticipatory guidance, as a form of primary prevention, to older children, adolescents and their families, aiming to support healthy weight and weight-related behaviours. Clinical guidelines recommend that clinicians monitor growth regularly, and provide guidance on healthy eating patterns, physical activity, sedentary behaviours and sleep patterns 97 , 100 . Very few paediatric trials have investigated whether this opportunistic screening and advice is effective in obesity prevention 100 . A 2021 review of registered RCTs for the prevention of obesity in infancy found 29 trials 137 , of which most were delivered, or were planned to be delivered, in community health-care settings, such as nurse-led clinics. At the time of publication, 11 trials had reported child weight-related outcomes, two of which showed a small but significant beneficial effect on BMI at age 2 years, and one found significant improvements in the prevalence of obesity but not BMI. Many of the trials showed improvements in practices, such as breastfeeding and screen time.
At the community level, local public policy should be mindful of the geography of the area (such as urban or rural) and population demographics. Adolescents usually have more freedom in food and beverage choices made outside the home than younger children. In addition, physical activity levels usually decline and sedentary behaviours rise during adolescence, particularly in girls 138 , 139 . These behavioural changes offer both opportunities and barriers for those developing community interventions. On a national societal level, public policies for interventions to prevent obesity in children include the control of advertising of foods and beverages high in fat, sugar and/or salt in some countries. Industry and the media, including social media, can have a considerable influence on the food and physical activity behaviours of children 13 , 119 .
Public policy may target interventions at all domains from the individual to the societal level. The main focus of interventions in most national public policies relies on the ability of individuals to make the behavioural changes that are the aim of the intervention (high-agency interventions) at the individual level (downstream interventions). An equal focus on low-agency and upstream interventions is required if a step change in tackling childhood obesity is to be realized 140 , 141 .
COVID-19 and obesity
Early indications in several countries show rising levels of childhood obesity, and an increase in inequalities in childhood obesity during the COVID-19 pandemic 142 . The substantial disruptions in nutrition and lifestyle habits of children during and since the pandemic include social isolation and addiction to screens 143 . Under-nutrition is expected to worsen in poor countries, but obesity rates could increase in middle-income countries and HICs, especially among vulnerable groups, widening the gap in health and social inequalities 143 . Public health approaches at national, regional and local levels should include strategies that not only prevent obesity and under-nutrition, but also reduce health inequalities.
In summary, although most trials of obesity prevention have occurred at the level of the individual, the immediate family, school or community, effective prevention of obesity will require greater investment in upstream, low-agency interventions.
Treatment goals
Treatment should be centred on the individual and stigma-free (Box 1 ) and may aim for a reduction in overweight and improvement in associated comorbidities and health behaviours. Clinical considerations when determining a treatment approach should include age, severity of overweight and the presence of associated complications 144 , 145 .
Box 1 Strategies for minimizing weight stigma in health care 220 , 221 , 222
Minimizing weight bias in the education of health-care professionals
Improved education of health professionals:
pay attention to the implicit and explicit communication of social norms
include coverage of the broader determinants of obesity
include discussion of harms caused by social and cultural norms and messages concerning body weight
provide opportunities to practise non-stigmatizing care throughout education
Provide causal information focusing on the genetic and/or socioenvironmental determinants of weight.
Provide empathy-invoking interventions, emphasizing size acceptance, respect and human dignity.
Provide a weight-inclusive approach, by emphasizing that all individuals, regardless of size, have the right to equal health care.
Addressing health facility infrastructure and processes
Provide appropriately sized chairs, blood pressure cuffs, weight scales, beds, toilets, showers and gowns.
Use non-stigmatizing language in signage, descriptions of clinical services and other documentation.
Providing clinical leadership and using appropriate language within health-care settings
Senior clinicians and managers should role-model supportive and non-biased behaviours towards people with obesity and indicate that they do not tolerate weight-based discrimination in any form.
Staff should identify the language that individuals prefer in referring to obesity.
Use person-first language, for example a ‘person with obesity’ rather than ‘an obese person’.
Treatment guidelines
Clinical guidelines advise that first-line management incorporates a family-based multicomponent approach that addresses dietary, physical activity, sedentary and sleep behaviours 97 , 99 , 109 , 146 . This approach is foundational, with adjunctive therapies, especially pharmacotherapy and bariatric surgery, indicated under specific circumstances, usually in adolescents with more severe obesity 144 , 145 . Guideline recommendations vary greatly among countries and are influenced by current evidence, and functionality and resourcing of local health systems. Hence, availability and feasibility of therapies differs internationally. In usual clinical practice, interventions may have poorer outcomes than is observed in original studies or anticipated in evidence-based guidelines 147 because implementation of guidelines is more challenging in resource-constrained environments 148 . In addition, clinical trials are less likely to include patients with specialized needs, such as children from culturally diverse populations, those living with social disadvantage, children with complex health problems, and those with severe obesity 149 , 150 .
Behavioural interventions
There are marked differences in individual responses to behavioural interventions, and overall weight change outcomes are often modest. In children aged 6–11 years, a 2017 Cochrane review 150 found that mean BMI z -scores were reduced in those involved in behaviour-changing interventions compared with those receiving usual care or no treatment by only 0.06 units (37 trials; 4,019 participants; low-quality evidence) at the latest follow-up (median 10 months after the end of active intervention). In adolescents aged 12–17 years, another 2017 Cochrane review 149 found that multicomponent behavioural interventions resulted in a mean reduction in weight of 3.67 kg (20 trials; 1,993 participants) and reduction in BMI of 1.18 kg/m 2 (28 trials; 2,774 participants). These effects were maintained at the 24-month follow-up. A 2012 systematic review found significant improvements in LDL cholesterol triglycerides and blood pressure up to 1 year from baseline following lifestyle interventions in children and adolescents 151 .
Family-based behavioural interventions are recommended in national level clinical practice guidelines 97 , 100 , 146 , 152 . They are an important element of intensive health behaviour and lifestyle treatments (IHBLTs) 109 . Family-based approaches use behavioural techniques, such as goal setting, parental monitoring or modelling, taught in family sessions or in individual sessions separately to children and care givers, depending on the child’s developmental level. The priority is to encourage the whole family to engage in healthier behaviours that result in dietary improvement, greater physical activity, and less sedentariness. This includes making changes to the family food environment and requires parental monitoring.
Family-based interventions differ in philosophy and implementation from those based on family systems theory and therapy 153 . All are intensive interventions that require multiple contact hours (26 or more) with trained specialists delivered over an extended period of time (6–12 months) 10 . Changing family lifestyle habits is challenging and expensive, and the therapeutic expertise is not widely available. Moving interventions to primary care settings, delivered by trained health coaches, and supplemented by remote contact (for example by phone), will improve access and equity 154 .
Very few interventions use single psychological approaches. Most effective IHBLTs are multicomponent and intensive (many sessions), and include face-to-face contact. There has been interest in motivational interviewing as an approach to delivery 155 . As client-centred counselling, this places the young person at the centre of their behaviour change. Fundamental to motivational interviewing is the practitioner partnership that helps the young person and/or parents to explore ambivalence to change, consolidate commitment to change, and develop a plan based on their own insights and expertise. Evidence reviews generally support the view that motivational interviewing reduces BMI. Longer interventions (>4 months), those that assess and report on intervention fidelity, and those that target both diet and physical activity are most effective 155 , 156 .
More intensive dietary interventions
Some individuals benefit from more intensive interventions 98 , 144 , 157 , 158 , which include very low-energy diets, very low-carbohydrate diets and intermittent energy restriction 159 . These interventions usually aim for weight loss and are only recommended for adolescents who have reached their final height. These diets are not recommended for long periods of time due to challenges in achieving nutritional adequacy 158 , 160 , and lack of long-term safety data 158 , 161 . However, intensive dietary interventions may be considered when conventional treatment is unsuccessful, or when adolescents with comorbidities or severe obesity require rapid or substantial weight loss 98 . A 2019 systematic review of very low-energy diets in children and adolescents found a mean reduction in body weight of −5.3 kg (seven studies) at the latest follow‐up, ranging from 5 to 14.5 months from baseline 161 .
Pharmacological treatment
Until the early 2020s the only drug approved in many jurisdictions for the treatment of obesity in adolescents was orlistat, a gastrointestinal lipase inhibitor resulting in reduced uptake of lipids and, thereby, a reduced total energy intake 162 . However, the modest effect on weight in combination with gastrointestinal adverse effects limit its usefulness overall 163 .
A new generation of drugs has been developed for the treatment of both T2DM and obesity. These drugs are based on gastrointestinal peptides with effects both locally and in the central nervous system. GLP1 is an incretin that reduces appetite and slows gastric motility. The GLP1 receptor agonist liraglutide is approved for the treatment of obesity in those aged 12 years and older both in the USA and Europe 164 , 165 . Liraglutide, delivered subcutaneously daily at a higher dose than used for T2DM resulted in a 5% better BMI reduction than placebo after 12 months 166 . A 2022 trial of semaglutide, another GLP1 receptor agonist, delivered subcutaneously weekly in adolescents demonstrated 16% weight loss after 68 weeks of treatment, with modest adverse events and a low drop-out rate 12 . Tirzepatide, an agonist of both GLP1 and glucose-dependent insulinotropic polypeptide (GIP), is approved by the FDA for the treatment of T2DM in adults 167 . Subcutaneous tirzepatide weekly in adults with obesity resulted in ~20% weight loss over 72 weeks 168 . Of note, GIP alone increases appetite, but the complex receptor–agonist interaction results in downregulation of the GIP receptors 169 , illustrating why slightly modified agonists exert different effects. A study of the use of tirzepatide in adolescents with T2DM has been initiated but results are not expected before 2027 (ref. 170 ). No trials of tirzepatide are currently underway in adolescents with obesity but without T2DM.
Hypothalamic obesity is difficult to treat. Setmelanotide is a MC4R agonist that reduces weight and improves quality of life in most people with LEPR and POMC mutations 71 . In trials of setmelanotide, 8 of 10 participants with POMC deficiency and 5 of 11 with LEPR deficiency had weight loss of at least 10% at ~1 year. The mean percentage change in most hunger score from baseline was −27.1% and −43.7% in those with POMC deficiency and leptin receptor deficiency, respectively 71 .
In the near future, effective new drugs with, hopefully, an acceptable safety profile will be available that will change the way we treat and set goals for paediatric obesity treatment 171 .
Bariatric surgery
Bariatric surgery is the most potent treatment for obesity in adolescents with severe obesity. The types of surgery most frequently used are sleeve gastrectomy and gastric bypass, both of which reduce appetite 172 . Mechanisms of action are complex, involving changes in gastrointestinal hormones, neural signalling, bile acid metabolism and gut microbiota 173 . Sleeve gastrectomy is a more straightforward procedure and the need for vitamin supplementation is lower than with gastric bypass. However, long-term weight loss may be greater after gastric bypass surgery 174 .
Prospective long-term studies demonstrate beneficial effects of both sleeve gastrectomy and gastric bypass on weight loss and comorbidities in adolescents with severe obesity 175 , 176 . In a 5-year follow-up period, in 161 participants in the US TEEN-LABS study who underwent gastric bypass, mean BMI declined from 50 to 37 kg/m 2 (ref. 11 ). In a Swedish prospective study in 81 adolescents who underwent gastric bypass, the mean decrease in BMI at 5 years was 13.1 kg/m 2 (baseline BMI 45.5 kg/m 2 ) compared with a BMI increase of 3.1 kg/m 2 in the control group 176 . Both studies showed marked inter-individual variations. Negative adverse effects, including gastrointestinal problems, vitamin deficits and reduction in lean body mass, are similar in adults and adolescents. Most surgical complications following bariatric surgery in the paediatric population are minor, occurring in the early postoperative time frame, but 8% of patients may have major perioperative complications 177 . Up to one-quarter of patients may require subsequent related procedures within 5 years 109 . However, many adolescents with severe obesity also have social and psychological problems, highlighting the need for routine and long-term monitoring 109 , 178 .
Recommendations for bariatric surgery in adolescents differ considerably among countries, with information on long-term outcomes emerging rapidly. In many countries, bariatric surgery is recommended only from Tanner pubertal stage 3–4 and beyond, and only in children with severe obesity and cardiometabolic comorbidities 177 . The 2023 American Academy of Pediatrics clinical practice guidelines recommend that bariatric surgery be considered in adolescents ≥13 years of age with a BMI of ≥35 kg/m 2 or 120% of the 95th percentile for age and sex, whichever is lower, as well as clinically significant disease, such as T2DM, non-alcoholic fatty liver disease, major orthopaedic complications, obstructive sleep apnoea, the presence of cardiometabolic risk, or depressed quality of life 109 . For those with a BMI of ≥40 kg/m 2 or 140% of the 95th percentile for age and sex, bariatric surgery is indicated regardless of the presence of comorbidities. Potential contraindications to surgery include correctable causes of obesity, pregnancy and ongoing substance use disorder. The guidelines comment that further evaluation, undertaken by multidisciplinary centres that offer bariatric surgery for adolescents, should determine the capacity of the patient and family to understand the risks and benefits of surgery and to adhere to the required lifestyle changes before and after surgery.
Long-term weight outcomes
Few paediatric studies have investigated long-term weight maintenance after the initial, more intensive, weight loss phase. A 2018 systematic review of 11 studies in children and adolescents showed that a diverse range of maintenance interventions, including support via face-to-face psychobehavioural therapies, individual physician consultations, or adjunctive therapeutic contact via newsletters, mobile phone text or e-mail, led to stabilization of BMI z -score compared with control participants, who had increases in BMI z -score 179 . Interventions that are web-based or use mobile devices may be particularly useful in young people 180 .
One concern is weight regain which occurs after bariatric surgery in general 181 but may be more prevalent in adolescents 176 . For example, in a Swedish prospective study, after 5 years, 25–30% of participants fulfilled the definitions of low surgical treatment effectiveness, which was associated with poorer metabolic outcomes 176 . As with adults, prevention of weight regain for most at-risk individuals might be possible with the combination of lifestyle support and pharmacological treatment 182 . Further weight maintenance strategies and long-term outcomes are discussed in the 2023 American Academy of Pediatrics clinical practice guidelines 109 . The appropriate role and timing of other therapies for long-term weight loss maintenance, such as anti-obesity medications, more intensive dietary interventions and bariatric surgery, are areas for future research.
In summary, management of obesity in childhood and adolescence requires intensive interventions. Emerging pharmacological therapies demonstrate greater short-term effectiveness than behavioural interventions; however, long-term outcomes at ≥2 years remain an important area for future research.
Quality of life
Weight bias describes the negative attitudes to, beliefs about and behaviour towards people with obesity 183 . It can lead to stigma causing exclusion, and discrimination in work, school and health care, and contributes to the inequities common in people with obesity 184 . Weight bias also affects social engagement and psychological well-being of children.
Children and adolescents with obesity score lower overall on health-related quality of life (HRQoL) 4 , 5 . In measures that assess domains of functioning, most score lower in physical functioning, physical/general health and psychosocial areas, such as appearance, and social acceptance and functioning. HRQoL is lowest in treatment-seeking children and in those with more extreme obesity 185 . Weight loss interventions generally increase HRQoL independent of the extent of weight loss 186 , especially in the domains most affected. However, changes in weight and HRQoL are often not strongly correlated. This may reflect a lag in the physical and/or psychosocial benefit from weight change, or the extent of change that is needed to drive change in a child’s self-perception.
Similar observations apply to the literature on self-esteem. Global self-worth is reduced in children and adolescents with obesity, as is satisfaction with physical appearance, athletic competence and social acceptance 187 . Data from intensive interventions suggest the psychological benefit of weight loss may be as dependent on some feature of the treatment environment or supportive social network as the weight loss itself 188 . This may include the daily company of others with obesity, making new friendships, and experienced improvements in newly prioritized competences.
There is a bidirectional relationship between HRQoL and obesity 189 , something also accepted in the relationship with mood disorder. Obesity increases the risk of depression and vice versa, albeit over a longer period of time and which may only become apparent in adulthood 190 . Obesity also presents an increased risk of anxiety 191 .
Structured and professionally delivered weight management interventions ameliorate mood disorder symptoms 192 and improve self-esteem 193 . Regular and extended support are important components beyond losing weight. Such interventions do not increase the risk of eating disorders 194 . This is despite a recognition that binge eating disorder is present in up to 5% of adolescents with overweight or obesity 195 . They are five times more likely to have binge eating symptoms than those with average weight. Importantly, adolescents who do not have access to professionally delivered weight management may be more likely to engage in self-directed dieting, which is implicated in eating disorder development 196 .
The literature linking childhood obesity with either attention deficit hyperactivity disorder or autism spectrum disorder is complex and the relationship is uncertain. The association seems to be clearer in adults but the mechanisms and their causal directions remain unclear 109 , 197 . Young children with obesity, especially boys, are more likely to be parent-rated as having behavioural problems 198 . This may be a response to the behaviour of others rather than reflect clinical diagnoses such as attention deficit hyperactivity disorder or autism spectrum disorder. Conduct and peer relationship problems co-occur in children, regardless of their weight.
Children with obesity experience more social rejection. They receive fewer friendship nominations and more peer rejections, most pronounced in those with severe obesity 199 . This continues through adolescence and beyond. Children with obesity are more likely to report being victimized 200 . Younger children may respond by being perpetrators themselves. While it is assumed that children are victimized because of their weight, very few studies have looked at the nature or reason behind victimization. A substantial proportion of children with obesity fail to identify themselves as being fat-teased 187 . Although the stigma associated with obesity should be anticipated in children, especially in those most overweight, it would be inappropriate to see all as victims. A better understanding of children’s resilience is needed.
Many gaps remain in basic, translational and clinical research in child and adolescent obesity. The mechanisms (genetic, epigenetic, environmental and social) behind the overwhelming association between parental obesity and child and adolescent obesity are still unclear given the paradoxically weak association in BMI between adopted children and their parents in combination with the modest effect size of known genetic loci associated with obesity 201 .
Early manifestation of extreme obesity in childhood suggests a strong biological basis for disturbances of homeostatic weight regulation. Deep genotyping (including next-generation sequencing) and epigenetic analyses in these patients will reveal new genetic causes and causal pathways as a basis for the development of mechanism-based treatments. Future work aiming to understand the mechanisms underlying the development of childhood obesity should consider the complex biopsychosocial interactions and take a systems approach to understanding causal pathways leading to childhood obesity to contribute to evidence-based prevention and treatment strategies.
Long-term outcome data to better determine the risks of eating disorders are required. Although symptoms improve during obesity treatment in most adolescents, screening and monitoring for disordered eating is recommended in those presenting for treatment 202 and effective tools for use in clinical practice are required. A limited number of tools are validated to identify binge eating disorder in youth with obesity 203 but further research is needed to screen appropriately for the full spectrum of eating disorder diagnoses in obesity treatment seeking youth 203 . Recent reviews provide additional detail regarding eating disorder risk in child and adolescent obesity 117 , 202 , 204 .
Most studies of paediatric obesity treatment have been undertaken in HICs and predominantly middle-class populations. However, research is needed to determine which strategies are best suited for those in LMICs and low-resource settings, for priority population groups including indigenous peoples, migrant populations and those living with social disadvantage, and for children with neurobehavioural and psychiatric disorders. We currently have a limited understanding of how best to target treatment pathways for different levels of genetic risk, age, developmental level, obesity severity, and cardiometabolic and psychological risk. Current outcomes for behavioural interventions are relatively modest and improved treatment outcomes are needed to address the potentially severe long-term health outcomes of paediatric obesity. Studies also need to include longer follow-up periods after an intervention, record all adverse events, incorporate cost-effectiveness analyses and have improved process evaluation.
Other areas in need of research include the role of new anti-obesity medications especially in adolescents, long-term outcomes following bariatric surgery and implementation of digital support systems to optimize outcomes and reduce costs of behavioural change interventions 205 . We must also better understand and tackle the barriers to implementation of treatment in real-life clinical settings, including the role of training of health professionals. Importantly, treatment studies of all kinds must engage people with lived experience — adolescents, parents and families — to understand what outcomes and elements of treatment are most valued.
Obesity prevention is challenging because it requires a multilevel, multisectoral approach that addresses inequity, involves many stakeholders and addresses both the upstream and the downstream factors influencing obesity risk. Some evidence exists of effectiveness of prevention interventions operating at the level of the child, family and school, but the very poor progress overall in modifying obesity prevalence globally highlights many areas in need of research and evidence implementation. Studies are needed especially in LMICs, particularly in the context of the nutrition transition and the double burden of malnutrition. A focus on intergenerational research, rather than the age-based focus of current work, is also needed. Systems research approaches should be used, addressing the broader food and physical activity environments, and links to climate change 206 . In all studies, strategies are needed that enable co-production with relevant communities, long-term follow-up, process evaluation and cost-effectiveness analyses. In the next few years, research and practice priorities must include a focus on intervention strategies in the earliest phases of life, including during pregnancy. The effects of COVID-19 and cost of living crises in many countries are leading to widening health inequalities 207 and this will further challenge obesity prevention interventions. Available resourcing for prevention interventions may become further constrained, requiring innovative solutions across agendas, with clear identification of co-benefits. For example, public health interventions for other diseases, such as dental caries or depression, or other societal concerns, such as urban congestion or climate change, may also act as obesity prevention strategies. Ultimately, to implement obesity prevention, societal changes are needed in terms of urban planning, social structures and health-care access.
Future high-quality paediatric obesity research can be enabled through strategies that support data sharing, which avoids research waste and bias, and enables new research questions to be addressed. Such approaches require leadership, careful engagement of multiple research teams, and resourcing. Four national or regional level paediatric weight registries exist 208 , 209 , 210 , 211 , which are all based in North America or Europe. Such registries should be established in other countries, especially in low-resource settings, even if challenging 208 . Another data-sharing approach is through individual participant data meta-analyses of intervention trials, which can include prospectively collected data 212 and are quite distinct from systematic reviews of aggregate data. Two recent examples are the Transforming Obesity Prevention in Childhood (TOPCHILD) Collaboration, which includes early interventions to prevent obesity in the first 2 years of life 213 , and the Eating Disorders in Weight-Related Therapy (EDIT) Collaboration, which aims to identify characteristics of individuals or trials that increase or protect against eating disorder risk following obesity treatment 214 . Formal data linkage studies, especially those joining up routine administrative datasets, enable longer-term and broader outcome measures to be assessed than is possible with standard clinical or public health intervention studies.
Collaborative research will also be enhanced through the use of agreed core outcome sets, supporting data harmonization. The Edmonton Obesity Staging System – Paediatric 215 is one option for paediatric obesity treatment. A core outcome set for early intervention trials to prevent obesity in childhood (COS-EPOCH) has been recently established 216 . These efforts incorporate a balance between wanting and needing to share data and adhering to privacy protection regulations. Objective end points are ideal, including directly measured physical activity and body composition.
Collaborative efforts and a systems approach are paramount to understand, prevent and manage child and adolescent obesity. Research funding and health policies should focus on feasible, effective and equitable interventions.
NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet https://doi.org/10.1016/S0140-6736(17)32129-3 (2017).
Article Google Scholar
Popkin, B. M., Corvalan, C. & Grummer-Strawn, L. M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 395 , 65–74 (2020).
Article PubMed Google Scholar
Kompaniyets, L. et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw. Open 4 , e2111182 (2021).
Article PubMed PubMed Central Google Scholar
Griffiths, L. J., Parsons, T. J. & Hill, A. J. Self‐esteem and quality of life in obese children and adolescents: a systematic review. Int. J. Pediatr. Obes. 5 , 282–304 (2010).
Buttitta, M., Iliescu, C., Rousseau, A. & Guerrien, A. Quality of life in overweight and obese children and adolescents: a literature review. Qual. Life Res. 23 , 1117–1139 (2014).
Hayes, A. et al. Early childhood obesity: association with healthcare expenditure in Australia. Obesity 24 , 1752–1758 (2016).
Marcus, C., Danielsson, P. & Hagman, E. Pediatric obesity – long-term consequences and effect of weight loss. J. Intern. Med. 292 , 870–891 (2022).
Berthoud, H. R., Morrison, C. D. & Münzberg, H. The obesity epidemic in the face of homeostatic body weight regulation: what went wrong and how can it be fixed? Physiol. Behav. 222 , 112959 (2020).
Article CAS PubMed PubMed Central Google Scholar
World Health Organization. Report of the commission on ending childhood obesity. WHO https://www.who.int/publications/i/item/9789241510066 (2016). This report from the WHO on approaches to childhood and adolescent obesity has six main recommendations for governments, covering food and physical activity, age-based settings and provision of weight management for those with obesity.
O’Connor, E. A. et al. Screening for obesity and intervention for weight management in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA 317 , 2427–2444 (2017).
Inge, T. H. et al. Five-year outcomes of gastric bypass in adolescents as compared with adults. N. Engl. J. Med. 380 , 2136–2145 (2019).
Weghuber, D. et al. Once-weekly semaglutide in adolescents with obesity. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2208601 (2022). To our knowledge, the first RCT of semaglutide 2.4 mg, administered weekly by subcutaneous injection, in adolescents with obesity.
World Health Organization. Report of the Commission on Ending Childhood Obesity: Implementation Plan: Executive Summary (WHO, 2017).
Hillier-Brown, F. C. et al. A systematic review of the effectiveness of individual, community and societal level interventions at reducing socioeconomic inequalities in obesity amongst children. BMC Public Health 14 , 834 (2014).
World Health Organization. Obesity. WHO https://www.who.int/health-topics/obesity#tab=tab_1 (2023).
Mei, Z. et al. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am. J. Clin. Nutr. 75 , 978–985 (2002).
Article CAS PubMed Google Scholar
World Health Organization. Child growth standards. WHO https://www.who.int/tools/child-growth-standards/standards (2006).
World Health Organization. Growth reference data for 5–19 years. WHO https://www.who.int/tools/growth-reference-data-for-5to19-years (2007).
National Center for Health Statistics. CDC growth charts. Centers for Disease Control and Prevention http://www.cdc.gov/growthcharts/ (2022).
Cole, T. J., Bellizzi, M. C., Flegal, K. M. & Dietz, W. H. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320 , 1240 (2000).
Di Cesare, M. et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. 17 , 212 (2019).
Swinburn, B., Egger, G. & Raza, F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev. Med. 29 , 563–570 (1999).
Ford, N. D., Patel, S. A. & Narayan, K. V. Obesity in low-and middle-income countries: burden, drivers, and emerging challenges. Annu. Rev. Public Health 38 , 145–164 (2017).
Shah, B., Tombeau Cost, K., Fuller, A., Birken, C. S. & Anderson, L. N. Sex and gender differences in childhood obesity: contributing to the research agenda. BMJ Nutr. Prev. Health 3 , 387–390 (2020).
Public Health England. Research and analysis: differences in child obesity by ethnic group. GOV.UK https://www.gov.uk/government/publications/differences-in-child-obesity-by-ethnic-group/differences-in-child-obesity-by-ethnic-group#data (2019).
Cole, T. J. & Lobstein, T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr. Obes. 7 , 284–294 (2012).
Kelly, A. S. et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation 128 , 1689–1712 (2013).
Garnett, S. P., Baur, L. A., Jones, A. M. & Hardy, L. L. Trends in the prevalence of morbid and severe obesity in Australian children aged 7–15 years, 1985-2012. PLoS ONE 11 , e0154879 (2016).
Spinelli, A. et al. Prevalence of severe obesity among primary school children in 21 European countries. Obes. Facts 12 , 244–258 (2019).
Twig, G. et al. Body-Mass Index in 2.3 million adolescents and cardiovascular death in adulthood. N. Engl. J. Med. 374 , 2430–2440 (2016).
González-Muniesa, P. et al. Obesity. Nat. Rev. Dis. Primers 3 , 17034 (2017).
Geserick, M. et al. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl. J. Med. 379 , 1303–1312 (2018).
Larqué, E. et al. From conception to infancy – early risk factors for childhood obesity. Nat. Rev. Endocrinol. 15 , 456–478 (2019).
Barker, D. J. Fetal origins of coronary heart disease. Br. Med. J. 311 , 171–174 (1995).
Article CAS Google Scholar
Gluckman, P. D., Hanson, M. A., Cooper, C. & Thornburg, K. L. Effect of in utero and early-life conditions on adult health and disease. N. Engl. J. Med. 359 , 61–73 (2008).
Philips, E. M. et al. Changes in parental smoking during pregnancy and risks of adverse birth outcomes and childhood overweight in Europe and North America: an individual participant data meta-analysis of 229,000 singleton births. PLoS Med. 17 , e1003182 (2020).
Voerman, E. et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. 16 , e1002744 (2019). Individual participant data meta-analysis of >160,000 mothers and their children on the associations of maternal BMI and gestational weight gain and childhood overweight or obesity.
McIntyre, H. D. et al. Gestational diabetes mellitus. Nat. Rev. Dis. Primers 5 , 47 (2019).
Oken, E. & Gillman, M. W. Fetal origins of obesity. Obes. Res. 11 , 496–506 (2003).
Hughes, A. R., Sherriff, A., Ness, A. R. & Reilly, J. J. Timing of adiposity rebound and adiposity in adolescence. Pediatrics 134 , e1354–e1361 (2014).
Rolland-Cachera, M. F. et al. Tracking the development of adiposity from one month of age to adulthood. Ann. Hum. Biol. 14 , 219–229 (1987).
Koletzko, B. et al. Prevention of childhood obesity: a position paper of the Global Federation of International Societies of Paediatric Gastroenterology, Hepatology and Nutrition (FISPGHAN). J. Pediatr. Gastroenterol. Nutr. 70 , 702–710 (2020).
Weber, M. et al. Lower protein content in infant formula reduces BMI and obesity risk at school age: follow-up of a randomized trial. Am. J. Clin. Nutr. 99 , 1041–1051 (2014).
Cope, M. B. & Allison, D. B. Critical review of the World Health Organization’s (WHO) 2007 report on ‘evidence of the long‐term effects of breastfeeding: systematic reviews and meta‐analysis’ with respect to obesity. Obes. Rev. 9 , 594–605 (2008).
Totzauer, M. et al. Different protein intake in the first year and its effects on adiposity rebound and obesity throughout childhood: 11 years follow‐up of a randomized controlled trial. Pediatr. Obes. 17 , e12961 (2022).
Deren, K. et al. Consumption of sugar-sweetened beverages in paediatric age: a position paper of the European academy of paediatrics and the European Childhood Obesity Group. Ann. Nutr. Metab. 74 , 296–302 (2019).
Felső, R., Lohner, S., Hollódy, K., Erhardt, É. & Molnár, D. Relationship between sleep duration and childhood obesity: systematic review including the potential underlying mechanisms. Nutr. Metab. Cardiovasc. Dis. 27 , 751–761 (2017).
Farooq, A. et al. Longitudinal changes in moderate‐to‐vigorous‐intensity physical activity in children and adolescents: a systematic review and meta‐analysis. Obes. Rev. 21 , e12953 (2020).
Mahumud, R. A. et al. Association of dietary intake, physical activity, and sedentary behaviours with overweight and obesity among 282,213 adolescents in 89 low and middle income to high-income countries. Int. J. Obes. 45 , 2404–2418 (2021).
Ballon, M. et al. Socioeconomic inequalities in weight, height and body mass index from birth to 5 years. Int. J. Obes. 42 , 1671–1679 (2018).
Buoncristiano, M. et al. Socioeconomic inequalities in overweight and obesity among 6- to 9-year-old children in 24 countries from the World Health Organization European region. Obes. Rev. 22 , e13213 (2021).
Jiwani, S. S. et al. The shift of obesity burden by socioeconomic status between 1998 and 2017 in Latin America and the Caribbean: a cross-sectional series study. Lancet Glob. Health 7 , e1644–e1654 (2019).
Monteiro, C. A., Conde, W. L., Lu, B. & Popkin, B. M. Obesity and inequities in health in the developing world. Int. J. Obes. 28 , 1181–1186 (2004).
Guo, S. S. & Chumlea, W. C. Tracking of body mass index in children in relation to overweight in adulthood. Am. J. Clin. Nutr. 70 , 145S–148S (1999).
Aarestrup, J. et al. Birthweight, childhood overweight, height and growth and adult cancer risks: a review of studies using the Copenhagen School Health Records Register. Int. J. Obes. 44 , 1546–1560 (2020).
Eslam, M. et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: an international expert consensus statement. Lancet Gastroenterol. Hepatol. 6 , 864–873 (2021).
Daniels, S. R. et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 111 , 1999–2012 (2005).
Cioana, M. et al. The prevalence of obesity among children with type 2 diabetes: a systematic review and meta-analysis. JAMA Netw. Open 5 , e2247186 (2022).
Gepstein, V. & Weiss, R. Obesity as the main risk factor for metabolic syndrome in children. Front. Endocrinol. 10 , 568 (2019).
Kuvat, N., Tanriverdi, H. & Armutcu, F. The relationship between obstructive sleep apnea syndrome and obesity: a new perspective on the pathogenesis in terms of organ crosstalk. Clin. Respir. J. 14 , 595–604 (2020).
Baker, J. L., Olsen, L. W. & Sorensen, T. I. Childhood body-mass index and the risk of coronary heart disease in adulthood. N. Engl. J. Med. 357 , 2329–2337 (2007).
Bjerregaard, L. G. et al. Change in overweight from childhood to early adulthood and risk of type 2 diabetes. N. Engl. J. Med. 378 , 1302–1312 (2018).
Kelsey, M. M., Zaepfel, A., Bjornstad, P. & Nadeau, K. J. Age-related consequences of childhood obesity. Gerontology 60 , 222–228 (2014).
Sharma, V. et al. A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes. Rev. 20 , 1341–1349 (2019).
Lobstein, T. & Jackson-Leach, R. Planning for the worst: estimates of obesity and comorbidities in school-age children in 2025. Pediatr. Obes. 11 , 321–325 (2016).
Berthoud, H. R., Münzberg, H. & Morrison, C. D. Blaming the brain for obesity: integration of hedonic and homeostatic mechanisms. Gastroenterology 152 , 1728–1738 (2017).
Devoto, F. et al. Hungry brains: a meta-analytical review of brain activation imaging studies on food perception and appetite in obese individuals. Neurosci. Biobehav. Rev. 94 , 271–285 (2018).
Blum, W. F., Englaro, P., Attanasio, A. M., Kiess, W. & Rascher, W. Human and clinical perspectives on leptin. Proc. Nutr. Soc. 57 , 477–485 (1998).
Friedman, J. M. Leptin and the endocrine control of energy balance. Nat. Metab. 1 , 754–764 (2019).
Kühnen, P. et al. Proopiomelanocortin deficiency treated with a melanocortin-4 receptor agonist. N. Engl. J. Med. 375 , 240–246 (2016).
Clément, K. et al. Efficacy and safety of setmelanotide, an MC4R agonist, in individuals with severe obesity due to LEPR or POMC deficiency: single-arm, open-label, multicentre, phase 3 trials. Lancet Diabetes Endocrinol. 8 , 960–970 (2020).
Rosen, E. D. & Spiegelman, B. M. What we talk about when we talk about fat. Cell 156 , 20–44 (2014).
Fischer-Posovszky, P., Roos, J., Zoller, V. & Wabitsch, M. in Pediatric Obesity: Etiology, Pathogenesis and Treatment (ed. Freemark, M. S.) 81–93 (Springer, 2018).
Hammarstedt, A., Gogg, S., Hedjazifar, S., Nerstedt, A. & Smith, U. Impaired adipogenesis and dysfunctional adipose tissue in human hypertrophic obesity. Physiol. Rev. 98 , 1911–1941 (2018).
Silventoinen, K. et al. Genetic and environmental effects on body mass index from infancy to the onset of adulthood: an individual-based pooled analysis of 45 twin cohorts participating in the collaborative project of development of anthropometrical measures in twins (CODATwins) study. Am. J. Clin. Nutr. 104 , 371–379 (2016).
Silventoinen, K. et al. Differences in genetic and environmental variation in adult BMI by sex, age, time period, and region: an individual-based pooled analysis of 40 twin cohorts. Am. J. Clin. Nutr. 106 , 457–466 (2017).
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in approximately 700000 individuals of European ancestry. Hum. Mol. Genet. 27 , 3641–3649 (2018).
Vogelezang, S. et al. Novel loci for childhood body mass index and shared heritability with adult cardiometabolic traits. PLoS Genet. 16 , e1008718 (2020).
Bradfield, J. P. et al. A trans-ancestral meta-analysis of genome-wide association studies reveals loci associated with childhood obesity. Hum. Mol. Genet. 28 , 3327–3338 (2019). To our knowledge, currently the largest genome-wide association study meta-analysis on childhood obesity in >13,000 individuals with obesity and >15,500 controls.
Couto Alves, A. et al. GWAS on longitudinal growth traits reveals different genetic factors influencing infant, child, and adult BMI. Sci. Adv. 5 , eaaw3095 (2019).
Ding, X. et al. Genome-wide screen of DNA methylation identifies novel markers in childhood obesity. Gene 566 , 74–83 (2015).
Huang, R. C. et al. Genome-wide methylation analysis identifies differentially methylated CpG loci associated with severe obesity in childhood. Epigenetics 10 , 995–1005 (2015).
Rzehak, P. et al. DNA-methylation and body composition in preschool children: epigenome-wide-analysis in the European Childhood Obesity Project (CHOP)-Study. Sci. Rep. 7 , 14349 (2017).
Alfano, R. et al. Perspectives and challenges of epigenetic determinants of childhood obesity: a systematic review. Obes. Rev. 23 , e13389 (2022).
Vehmeijer, F. O. L. et al. DNA methylation and body mass index from birth to adolescence: meta-analyses of epigenome-wide association studies. Genome Med. 12 , 105 (2020). Meta-analysis of epigenome-wide association studies of childhood BMI in >4,000 children.
Richmond, R. C. et al. DNA methylation and BMI: investigating identified methylation sites at HIF3A in a causal framework. Diabetes 65 , 1231–1244 (2016).
Wahl, S. et al. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature 541 , 81–86 (2017).
Kivimäki, M. et al. Substantial intergenerational increases in body mass index are not explained by the fetal overnutrition hypothesis: the Cardiovascular Risk in Young Finns Study. Am. J. Clin. Nutr. 86 , 1509–1514 (2007).
Whitaker, R. C., Wright, J. A., Pepe, M. S., Seidel, K. D. & Dietz, W. H. Predicting obesity in young adulthood from childhood and parental obesity. N. Engl. J. Med. 337 , 869–873 (1997).
Davey Smith, G., Steer, C., Leary, S. & Ness, A. Is there an intrauterine influence on obesity? Evidence from parent child associations in the Avon Longitudinal Study of Parents and Children (ALSPAC). Arch. Dis. Child. 92 , 876–880 (2007).
Fleten, C. et al. Parent-offspring body mass index associations in the Norwegian Mother and Child Cohort Study: a family-based approach to studying the role of the intrauterine environment in childhood adiposity. Am. J. Epidemiol. 176 , 83–92 (2012).
Gaillard, R. et al. Childhood cardiometabolic outcomes of maternal obesity during pregnancy: the Generation R Study. Hypertension 63 , 683–691 (2014).
Lawlor, D. A. et al. Exploring the developmental overnutrition hypothesis using parental-offspring associations and FTO as an instrumental variable. PLoS Med. 5 , e33 (2008).
Patro, B. et al. Maternal and paternal body mass index and offspring obesity: a systematic review. Ann. Nutr. Metab. 63 , 32–41 (2013).
Sorensen, T. et al. Comparison of associations of maternal peri-pregnancy and paternal anthropometrics with child anthropometrics from birth through age 7 y assessed in the Danish National Birth Cohort. Am. J. Clin. Nutr. 104 , 389–396 (2016).
Styne, D. M. et al. Pediatric obesity – assessment, treatment, and prevention: an Endocrine Society Clinical Practice guideline. J. Clin. Endocrinol. Metab. 102 , 709–757 (2017).
National Institute for Health and Care Excellence. Obesity: identification, assessment and managenent: clinical guideline [CG189]. NICE https://www.nice.org.uk/guidance/cg189 (2022). A high quality clinical practice guideline for obesity management.
Barlow, S. E. Expert Committee Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 120 (Suppl. 4), S164–S192 (2007).
Canadian Task Force on Preventive Health Care. Recommendations for growth monitoring, and prevention and management of overweight and obesity in children and youth in primary care. Can. Med. Assoc. J. 187 , 411–421 (2015).
US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA 317 , 2417–2426 (2017).
McConnell-Nzunga, J. et al. Classification of obesity varies between body mass index and direct measures of body fat in boys and girls of Asian and European ancestry. Meas. Phys. Educ. Exerc. Sci. 22 , 154–166 (2018).
Reinehr, T. et al. Definable somatic disorders in overweight children and adolescents. J. Pediatr. 150 , 618–622.e5 (2007).
Reinehr, T. Thyroid function in the nutritionally obese child and adolescent. Curr. Opin. Pediatr. 23 , 415–420 (2011).
Kohlsdorf, K. et al. Early childhood BMI trajectories in monogenic obesity due to leptin, leptin receptor, and melanocortin 4 receptor deficiency. Int. J. Obes. 42 , 1602–1609 (2018).
Armstrong, S. et al. Physical examination findings among children and adolescents with obesity: an evidence-based review. Pediatrics 137 , e20151766 (2016).
Reinehr, T. & Roth, C. L. Is there a causal relationship between obesity and puberty? Lancet Child Adolesc. Health 3 , 44–54 (2019).
Garnett, S. P., Baur, L. A. & Cowell, C. T. Waist-to-height ratio: a simple option for determining excess central adiposity in young people. Int. J. Obes. 32 , 1028–1030 (2008).
Maffeis, C., Banzato, C., Talamini, G. & Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J. Pediatr. 152 , 207–213.e2 (2008).
Hampl, S. E. et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics 151 , e2022060640 (2023). A new, comprehensive clinical practice guideline outlining current recommendations on assessment and treatment of children and adolescents with obesity.
Reinehr, T. et al. Comparison of cardiovascular risk factors between children and adolescents with classes III and IV obesity: findings from the APV cohort. Int. J. Obes. 45 , 1061–1073 (2021).
Reinehr, T. Metabolic syndrome in children and adolescents: a critical approach considering the interaction between pubertal stage and insulin resistance. Curr. Diabetes Rep. 16 , 8 (2016).
Zeitler, P. et al. ISPAD Clinical Practice Consensus Guidelines 2018: type 2 diabetes mellitus in youth. Pediatr. Diabetes 19 , 28–46 (2018).
Ibáñez, L. et al. An International Consortium update: pathophysiology, diagnosis, and treatment of polycystic ovarian syndrome in adolescence. Horm. Res. Paediatr. 88 , 371–395 (2017).
Brockmann, P. E., Schaefer, C., Poets, A., Poets, C. F. & Urschitz, M. S. Diagnosis of obstructive sleep apnea in children: a systematic review. Sleep Med. Rev. 17 , 331–340 (2013).
Taylor, E. D. et al. Orthopedic complications of overweight in children and adolescents. Pediatrics 117 , 2167–2174 (2006).
Winck, A. D. et al. Effects of obesity on lung volume and capacity in children and adolescents: a systematic review. Rev. Paul. Pediatr. 34 , 510–517 (2016).
PubMed PubMed Central Google Scholar
Jebeile, H., Lister, N., Baur, L., Garnett, S. & Paxton, S. J. Eating disorder risk in adolescents with obesity. Obes. Rev. 22 , e13173 (2021).
Quek, Y. H., Tam, W. W. S., Zhang, M. W. B. & Ho, R. C. M. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes. Rev. 18 , 742–754 (2017).
World Health Organization. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity . Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity (WHO, 2016).
Pickett, K. et al. The Child of the North: building a fairer future after COVID-19. The Northern Health Science Alliance and N8 Research Partnership https://www.thenhsa.co.uk/app/uploads/2022/01/Child-of-the-North-Report-FINAL-1.pdf (2021).
Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 32 , 513–531 (1977).
Nuffield Council on Bioethics. Public Health: Ethical Issues (Nuffield Council on Bioethics, 2007).
Lorenc, T., Petticrew, M., Welch, V. & Tugwell, P. What types of interventions generate inequalities? Evidence from systematic reviews. J. Epidemiol. Community Health 67 , 190–193 (2013).
Adams, J., Mytton, O., White, M. & Monsivais, P. Why are some population interventions for diet and obesity more equitable and effective than others? The role of individual agency. PLoS Med. 13 , e1001990 (2016).
Backholer, K. et al. A framework for evaluating the impact of obesity prevention strategies on socioeconomic inequalities in weight. Am. J. Public Health 104 , e43–e50 (2014).
McGill, R. et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 15 , 457 (2015).
Brown, T. et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 7 , Cd001871 (2019). A Cochrane review involving 153 RCTs of diet and/or physical activity interventions to prevent obesity in children and adolescents, highlighting varying effectiveness of interventions in different age groups.
PubMed Google Scholar
Le, L. K.-D. et al. Prevention of high body mass index and eating disorders: a systematic review and meta-analysis. Eat. Weight Disord. 27 , 2989–3003 (2022).
Nobles, J., Summerbell, C., Brown, T., Jago, R. & Moore, T. A secondary analysis of the childhood obesity prevention Cochrane Review through a wider determinants of health lens: implications for research funders, researchers, policymakers and practitioners. Int. J. Behav. Nutr. Phys. Act. 18 , 22 (2021).
Rai, K. K., Dogra, S. A., Barber, S., Adab, P. & Summerbell, C. A scoping review and systematic mapping of health promotion interventions associated with obesity in Islamic religious settings in the UK. Obes. Rev. 20 , 1231–1261 (2019).
World Health Organization. Nutrition Action in Schools: A Review of Evidence Related to the Nutrition-Friendly Schools Initiative (WHO, 2021).
Daly-Smith, A. et al. Using a multi-stakeholder experience-based design process to co-develop the Creating Active Schools Framework. Int. J. Behav. Nutr. Phys. Act. 17 , 13 (2020).
Tibbitts, B. et al. Considerations for individual-level versus whole-school physical activity interventions: stakeholder perspectives. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph18147628 (2021).
Askie, L. M. et al. Interventions commenced by early infancy to prevent childhood obesity-The EPOCH Collaboration: an individual participant data prospective meta-analysis of four randomized controlled trials. Pediatr. Obes. 15 , e12618 (2020). To our knowledge, the first prospective individual participant data meta-analysis showing that interventions commencing in late pregnancy or very early childhood are associated with healthier BMI z -score at age 18–24 months.
Seidler, A. L. et al. Examining the sustainability of effects of early childhood obesity prevention interventions: follow-up of the EPOCH individual participant data prospective meta-analysis. Pediatr. Obes. 17 , e12919 (2022).
Taylor, R. W. et al. Sleep, nutrition, and physical activity interventions to prevent obesity in infancy: follow-up of the prevention of overweight in infancy (POI) randomized controlled trial at ages 3.5 and 5 y. Am. J. Clin. Nutr. 108 , 228–236 (2018).
Mihrshahi, S. et al. A review of registered randomized controlled trials for the prevention of obesity in infancy. Int. J. Environ. Res. Public Health 18 , 2444 (2021).
Farooq, M. A. et al. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. Br. J. Sports Med. 52 , 1002–1006 (2018).
van Sluijs, E. M. F. et al. Physical activity behaviours in adolescence: current evidence and opportunities for intervention. Lancet 398 , 429–442 (2021).
Griffin, N. et al. A critique of the English national policy from a social determinants of health perspective using a realist and problem representation approach: the ‘Childhood Obesity: a plan for action’ (2016, 2018, 2019). BMC Public Health 21 , 2284 (2021).
Knai, C., Lobstein, T., Petticrew, M., Rutter, H. & Savona, N. England’s childhood obesity action plan II. Br. Med. J. 362 , k3098 (2018).
World Health Organization. WHO European Regional Obesity Report 2022 (WHO, 2022).
Zemrani, B., Gehri, M., Masserey, E., Knob, C. & Pellaton, R. A hidden side of the COVID-19 pandemic in children: the double burden of undernutrition and overnutrition. Int. J. Equity Health 20 , 44 (2021).
Alman, K. L. et al. Dietetic management of obesity and severe obesity in children and adolescents: a scoping review of guidelines. Obes. Rev. https://doi.org/10.1111/obr.13132 (2020).
Pfeiffle, S. et al. Current recommendations for nutritional management of overweight and obesity in children and adolescents: a structured framework. Nutrients https://doi.org/10.3390/nu11020362 (2019).
Scottish Intercollegiate Guidelines Network. Management of obesity. A National Clinical Guideline . SIGN 115 (SIGN, 2010).
Reinehr, T. et al. Two-year follow-up in 21,784 overweight children and adolescents with lifestyle intervention. Obesity 17 , 1196–1199 (2009).
Ells, L. J. et al. Interventions for treating children and adolescents with overweight and obesity: an overview of Cochrane reviews. Int. J. Obes. 42 , 1823–1833 (2018).
Al‐Khudairy, L. et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst. Rev. 6 , CD012691 (2017). One of three Cochrane reviews looking at lifestyle treatment of paediatric obesity, in this case in adolescents, which identified 44 completed trials, finding low quality evidence of improvements in BMI and moderate quality evidence of improvements in weight.
Mead, E. et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst. Rev. 6 , CD012651 (2017). A Cochrane Review, involving 70 RCTs, showing that multicomponent behavioural interventions can lead to small, short-term reductions in BMI and related measures in children aged 6–11 years with obesity.
Ho, M. et al. Effectiveness of lifestyle interventions in child obesity: systematic review with meta-analysis. Pediatrics 130 , e1647–e1671 (2012). To our knowledge, the first systematic review of lifestyle interventions in children and adolescents with obesity to show improvements in cardiometabolic outcomes (LDL cholesterol, triglycerides, fasting insulin and blood pressure), as well as weight.
Clinical Practice Guideline Panel. Clinical practice guideline for multicomponent behavioral treatment of obesity and overweight in children and adolescents: current state of the evidence and research needs. American Psychological Association https://www.apa.org/obesity-guideline/clinical-practice-guideline.pdf (2018).
Nowicka, P. & Flodmark, C. E. Family therapy as a model for treating childhood obesity: useful tools for clinicians. Clin. Child. Psychol. Psychiatry 16 , 129–145 (2011).
Wilfley, D. E. et al. Improving access and systems of care for evidence-based childhood obesity treatment: conference key findings and next steps. Obesity 25 , 16–29 (2017).
Amiri, P. et al. Does motivational interviewing improve the weight management process in adolescents? A systematic review and meta-analysis. Int. J. Behav. Med. 29 , 78–103 (2022).
Kao, T. A., Ling, J., Hawn, R. & Vu, C. The effects of motivational interviewing on children’s body mass index and fat distributions: a systematic review and meta-analysis. Obes. Rev. 22 , e13308 (2021).
Hassapidou, M. et al. European Association for the Study of Obesity (EASO) position statement on medical nutrition therapy for the management of overweight and obesity in children and adolescents developed in collaboration with the European Federation of the Associations of Dietitians (EFAD). Obes. Facts https://doi.org/10.1159/000527540 (2022).
Hoelscher, D. M., Kirk, S., Ritchie, L. & Cunningham-Sabo, L. Position of the Academy of Nutrition and Dietetics: interventions for the prevention and treatment of pediatric overweight and obesity. J. Acad. Nutr. Diet. 113 , 1375–1394 (2013).
Hoare, J. K., Jebeile, H., Garnett, S. P. & Lister, N. B. Novel dietary interventions for adolescents with obesity: a narrative review. Pediatr. Obes. 16 , e12798 (2021).
Lister, N. et al. Nutritional adequacy of diets for adolescents with overweight and obesity: considerations for dietetic practice. Eur. J. Clin. Nutr. 71 , 646–651 (2017).
Andela, S. et al. Efficacy of very low-energy diet programs for weight loss: a systematic review with meta-analysis of intervention studies in children and adolescents with obesity. Obes. Rev. 20 , 871–882 (2019).
Srivastava, G. & Apovian, C. M. Current pharmacotherapy for obesity. Nat. Rev. Endocrinol. 14 , 12–24 (2018).
Apperley, L. J. et al. Childhood obesity: a review of current and future management options. Clin. Endocrinol. 96 , 288–301 (2022).
European Medicines Agency. Saxenda. European Medicines Agency https://www.ema.europa.eu/en/medicines/human/EPAR/saxenda (2022).
US Food and Drug Administration. FDA approves weight management drug for patients aged 12 and older. FDA https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-weight-management-drug-patients-aged-12-and-older (2021).
Kelly, A. S. et al. A randomized, controlled trial of liraglutide for adolescents with obesity. N. Engl. J. Med. 382 , 2117–2128 (2020). To our knowledge, the first RCT of liraglutide, administered daily via subcutaneous injection, in adolescents with obesity.
US Food and Drug Administration. FDA approves novel, dual-targeted treatment for type 2 iabetes. FDA https://www.fda.gov/news-events/press-announcements/fda-approves-novel-dual-targeted-treatment-type-2-diabetes (2022).
Jastreboff, A. M. et al. Tirzepatide once weekly for the treatment of obesity. N. Engl. J. Med. 387 , 205–216 (2022).
Holst, J. J. & Rosenkilde, M. M. GIP as a therapeutic target in diabetes and obesity: insight from incretin co-agonists. J. Clin. Endocrinol. Metab. https://doi.org/10.1210/clinem/dgaa327 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/study/NCT05260021 (2023).
Müller, T. D., Blüher, M., Tschöp, M. H. & DiMarchi, R. D. Anti-obesity drug discovery: advances and challenges. Nat. Rev. Drug Discov. 21 , 201–223 (2022).
Chalklin, C. G., Ryan Harper, E. G. & Beamish, A. J. Metabolic and bariatric surgery in adolescents. Curr. Obes. Rep. 10 , 61–69 (2021).
Albaugh, V. L. et al. Regulation of body weight: lessons learned from bariatric surgery. Mol. Metab. https://doi.org/10.1016/j.molmet.2022.101517 (2022).
Uhe, I. et al. Roux-en-Y gastric bypass, sleeve gastrectomy, or one-anastomosis gastric bypass? A systematic review and meta-analysis of randomized-controlled trials. Obesity 30 , 614–627 (2022).
Inge, T. H. et al. Long-term outcomes of bariatric surgery in adolescents with severe obesity (FABS-5+): a prospective follow-up analysis. Lancet Diabetes Endocrinol. 5 , 165–173 (2017).
Olbers, T. et al. Laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity (AMOS): a prospective, 5-year, Swedish nationwide study. Lancet Diabetes Endocrinol. https://doi.org/10.1016/S2213-8587(16)30424-7 (2017).
Pratt, J. S. et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg. Obes. Relat. Dis. 14 , 882–901 (2018).
Jarvholm, K. et al. 5-year mental health and eating pattern outcomes following bariatric surgery in adolescents: a prospective cohort study. Lancet Child Adolesc. Health 4 , 210–219 (2020).
Van Der Heijden, L., Feskens, E. & Janse, A. Maintenance interventions for overweight or obesity in children: a systematic review and meta‐analysis. Obes. Rev. 19 , 798–809 (2018).
Park, J., Park, M.-J. & Seo, Y.-G. Effectiveness of information and communication technology on obesity in childhood and adolescence: systematic review and meta-analysis. J. Med. Internet Res. 23 , e29003 (2021).
Brissman, M., Beamish, A. J., Olbers, T. & Marcus, C. Prevalence of insufficient weight loss 5 years after Roux-en-Y gastric bypass: metabolic consequences and prediction estimates: a prospective registry study. BMJ Open 11 , e046407 (2021).
El Ansari, W. & Elhag, W. Weight regain and insufficient weight loss after bariatric surgery: definitions, prevalence, mechanisms, predictors, prevention and management strategies, and knowledge gaps – a scoping review. Obes. Surg. 31 , 1755–1766 (2021).
World Health Organization Regional Office for Europe. Weight Bias and Obesity Stigma: Considerations for the WHO European Region (WHO, 2017).
Puhl, R. M. & Latner, J. D. Stigma, obesity, and the health of the nation’s children. Psychol. Bull. 133 , 557–580 (2007).
Black, W. R. et al. Health-related quality of life across recent pediatric obesity classification recommendations. Children 8 , 303 (2021).
Finne, E., Reinehr, T., Schaefer, A., Winkel, K. & Kolip, P. Changes in self-reported and parent-reported health-related quality of life in overweight children and adolescents participating in an outpatient training: findings from a 12-month follow-up study. Health Qual. Life Outcomes 11 , 1 (2013).
Hill, A. J. Obesity in children and the ‘myth of psychological maladjustment’: self-esteem in the spotlight. Curr. Obes. Rep. 6 , 63–70 (2017).
McGregor, S., McKenna, J., Gately, P. & Hill, A. J. Self‐esteem outcomes over a summer camp for obese youth. Pediatr. Obes. 11 , 500–505 (2016).
Jansen, P., Mensah, F., Clifford, S., Nicholson, J. & Wake, M. Bidirectional associations between overweight and health-related quality of life from 4–11 years: longitudinal study of Australian children. Int. J. Obes. 37 , 1307–1313 (2013).
Mannan, M., Mamun, A., Doi, S. & Clavarino, A. Is there a bi-directional relationship between depression and obesity among adult men and women? Systematic review and bias-adjusted meta analysis. Asian J. Psychiatr. 21 , 51–66 (2016).
Lindberg, L., Hagman, E., Danielsson, P., Marcus, C. & Persson, M. Anxiety and depression in children and adolescents with obesity: a nationwide study in Sweden. BMC Med. 18 , 30 (2020).
Jebeile, H. et al. Association of pediatric obesity treatment, including a dietary component, with change in depression and anxiety: a systematic review and meta-analysis. JAMA Pediatr. 173 , e192841 (2019).
Gow, M. L. et al. Pediatric obesity treatment, self‐esteem, and body image: a systematic review with meta‐analysis. Pediatr. Obes. 15 , e12600 (2020).
Jebeile, H. et al. Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: a systematic review with meta-analysis. Obes. Rev. 20 , 1287–1298 (2019). To our knowledge, the first systematic review to show that structured and professionally led weight management interventions in children and adolescents with obesity are associated with reductions in eating disorder risk and symptoms.
Kjeldbjerg, M. L. & Clausen, L. Prevalence of binge-eating disorder among children and adolescents: a systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-021-01850-2 (2021).
Patton, G. C., Selzer, R., Coffey, C., Carlin, J. B. & Wolfe, R. Onset of adolescent eating disorders: population based cohort study over 3 years. BMJ 318 , 765–768 (1999).
Cortese, S. The association between ADHD and obesity: intriguing, progressively more investigated, but still puzzling. Brain Sci. 9 , 256 (2019).
Griffiths, L. J., Dezateux, C. & Hill, A. Is obesity associated with emotional and behavioural problems in children? Findings from the Millennium Cohort Study. Int. J. Pediatr. Obes. 6 , e423–e432 (2011).
Harrist, A. W. et al. The social and emotional lives of overweight, obese, and severely obese children. Child. Dev. 87 , 1564–1580 (2016).
Van Geel, M., Vedder, P. & Tanilon, J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the relation between weight status and bullying. Int. J. Obes. 38 , 1263–1267 (2014).
Albuquerque, D., Nóbrega, C., Manco, L. & Padez, C. The contribution of genetics and environment to obesity. Br. Med. Bull. 123 , 159–173 (2017).
Rancourt, D. & McCullough, M. B. Overlap in eating disorders and obesity in adolescence. Curr. Diabetes Rep. 15 , 78 (2015).
House, E. T. et al. Identifying eating disorders in adolescents and adults with overweight or obesity: a systematic review of screening questionnaires. Int. J. Eat. Disord. 55 , 1171–1193 (2022).
Lister, N. B., Baur, L. A., Paxton, S. J. & Jebeile, H. Contextualising eating disorder concerns for paediatric obesity treatment. Curr. Obes. Rep. 10 , 322–331 (2021).
Hagman, E. et al. Effect of an interactive mobile health support system and daily weight measurements for pediatric obesity treatment, a 1-year pragmatical clinical trial. Int. J. Obes. 46 , 1527–1533 (2022).
Swinburn, B. A. et al. The global syndemic of obesity, undernutrition, and climate change: The Lancet commission report. Lancet 393 , 791–846 (2019).
Whitehead, M., Taylor-Robinson, D. & Barr, B. Poverty, health, and covid-19. Br. Med. J. 372 , n376 (2021).
Morrison, K. M. et al. The CANadian Pediatric Weight Management Registry (CANPWR): lessons learned from developing and initiating a national, multi-centre study embedded in pediatric clinical practice. BMC Pediatr. 18 , 237 (2018).
Kirk, S. et al. Establishment of the pediatric obesity weight evaluation registry: a national research collaborative for identifying the optimal assessment and treatment of pediatric obesity. Child. Obes. 13 , 9–17 (2017).
Hagman, E., Danielsson, P., Lindberg, L. & Marcus, C., BORIS Steering Committee. Paediatric obesity treatment during 14 years in Sweden: lessons from the Swedish Childhood Obesity Treatment Register – BORIS. Pediatr. Obes. 15 , e12626 (2020).
Bohn, B. et al. Changing characteristics of obese children and adolescents entering pediatric lifestyle intervention programs in Germany over the last 11 years: an adiposity patients registry multicenter analysis of 65,453 children and adolescents. Obes. Facts 10 , 517–530 (2017).
Seidler, A. L. et al. A guide to prospective meta-analysis. BMJ 367 , l5342 (2019).
Hunter, K. E. et al. Transforming obesity prevention for children (TOPCHILD) collaboration: protocol for a systematic review with individual participant data meta-analysis of behavioural interventions for the prevention of early childhood obesity. BMJ Open 12 , e048166 (2022).
Lister, N. B. et al. Eating disorders in weight-related therapy (EDIT) collaboration: rationale and study design. Nutr. Res. Rev. https://doi.org/10.1017/S0954422423000045 (2023).
Hadjiyannakis, S. et al. Obesity class versus the Edmonton Obesity Staging System for Pediatrics to define health risk in childhood obesity: results from the CANPWR cross-sectional study. Lancet Child Adolesc. Health 3 , 398–407 (2019).
Brown, V. et al. Core outcome set for early intervention trials to prevent obesity in childhood (COS-EPOCH): agreement on “what” to measure. Int. J. Obes. 46 , 1867–1874 (2022). A stakeholder-informed study that identified the minimum outcomes recommended for collecting and reporting in obesity prevention trials in early childhood.
Han, J. C., Lawlor, D. A. & Kimm, S. Y. Childhood obesity. Lancet 375 , 1737–1748 (2010).
Shin, A. C., Zheng, H. & Berthoud, H. R. An expanded view of energy homeostasis: neural integration of metabolic, cognitive, and emotional drives to eat. Physiol. Behav. 97 , 572–580 (2009).
Lennerz, B., Wabitsch, M. & Eser, K. Ätiologie und genese [German]. Berufl. Rehabil. 1 , 14 (2014).
Google Scholar
Pont, S. J., Puhl, R., Cook, S. R. & Slusser, W. Stigma experienced by children and adolescents with obesity. Pediatrics 140 , e20173034 (2017).
Talumaa, B., Brown, A., Batterham, R. L. & Kalea, A. Z. Effective strategies in ending weight stigma in healthcare. Obes. Rev. 23 , e13494 (2022).
Rubino, F. et al. Joint international consensus statement for ending stigma of obesity. Nat. Med. 26 , 485–497 (2020).
Download references
Author information
Authors and affiliations.
Children’s Hospital Westmead Clinical School, Sydney Medical School, The University of Sydney, Sydney, New South Wales, Australia
Natalie B. Lister & Louise A. Baur
Institute of Endocrinology and Diabetes, The Children’s Hospital at Westmead, Sydney, New South Wales, Australia
Natalie B. Lister
Sydney School of Public Health, The University of Sydney, Sydney, New South Wales, Australia
Louise A. Baur
Weight Management Services, The Children’s Hospital at Westmead, Sydney, New South Wales, Australia
The Generation R Study Group, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
Janine F. Felix
Department of Paediatrics, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
Institute of Health Sciences, School of Medicine, University of Leeds, Leeds, UK
Andrew J. Hill
Division of Paediatrics, Department of Clinical Science Intervention and Technology, Karolinska Institutet and Karolinska University Hospital, Stockholm, Sweden
Claude Marcus
Vestische Hospital for Children and Adolescents Datteln, University of Witten/Herdecke, Datteln, Germany
Thomas Reinehr
Department of Sport and Exercise Sciences, Durham University, Durham, UK
- Carolyn Summerbell
Division of Paediatric Endocrinology and Diabetes, Department of Paediatrics and Adolescent Medicine, Ulm University Medical Centre, Ulm, Germany
Martin Wabitsch
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (L.A.B., J.F.F. and N.B.L.); Epidemiology (L.A.B. and J.F.F.); Mechanisms/pathophysiology (L.A.B., J.F.F., T.R. and M.W.); Diagnosis, screening and prevention (L.A.B., N.B.L., T.R., C.S. and M.W.); Management (L.A.B., N.B.L., A.J.H., C.M. and T.R.); Quality of life (L.A.B., N.B.L. and A.J.H.); Outlook (L.A.B., N.B.L., J.F.F., A.J.H., C.M., T.R., C.S. and M.W.); Overview of the Primer (L.A.B. and N.B.L.).
Corresponding author
Correspondence to Louise A. Baur .
Ethics declarations
Competing interests.
A.J.H. reports receiving payment for consultancy advice for Slimming World (UK). L.A.B. reports receiving honoraria for speaking in forums organized by Novo Nordisk in relation to management of adolescent obesity and the ACTION-Teens study, which is sponsored by Novo Nordisk. L.A.B. is the Australian lead of the study. T.R. received funding from the German Federal Ministry of Education and Research (BMBF; 01GI1120A/B) as part of the German Competence Network Obesity (Consortium ‘Youth with Extreme Obesity’). T.R. receives payment for consultancy advice related to pharmacological treatment of obesity from Novo Nordisk and Lilly, as well as honoraria for lectures in symposia organized by Novo Nordisk, Novartis and Merck. C.M. receives payments for consultancy advice and advisory board participation from Novo Nordisk, Oriflame Wellness, DeFaire AB and Itrim AB. C.M. also receives honoraria for speaking at meetings organized by Novo Nordisk and Astra Zeneca. C.M. is a shareholder and founder of Evira AB, a company that develops and sells systems for digital support for weight loss, and receives grants from Novo Nordisk for epidemiological studies of the effects of weight loss on future heath. M.W. received funding from the German Federal Ministry of Education and Research (BMBF; 01GI1120A/B) as part of the German Competence Network Obesity (Consortium ‘Youth with Extreme Obesity’). M.W. receives payment for consultancy advice related to pharmacological treatment of obesity from Novo Nordisk, Regeneron, Boehringer Ingelheim and LG Chem, as well as honoraria for speaking in symposia organized by Novo Nordisk, Rhythm Pharmaceuticals and Infectopharm. M.W. is principal investigator in phase II and phase III studies of setmelanotide sponsored by Rhythm Pharmaceuticals. N.B.L., J.F.F. and C.S. declare no competing interests.
Peer review
Peer review information.
Nature Reviews Disease Primers thanks C. Maffeis, L. Moreno, R, Weiss and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Lister, N.B., Baur, L.A., Felix, J.F. et al. Child and adolescent obesity. Nat Rev Dis Primers 9 , 24 (2023). https://doi.org/10.1038/s41572-023-00435-4
Download citation
Accepted : 12 April 2023
Published : 18 May 2023
DOI : https://doi.org/10.1038/s41572-023-00435-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Relationship between 24-h activity behavior and body fat percentage in preschool children: based on compositional data and isotemporal substitution analysis.
BMC Public Health (2024)
Young people's experiences of physical activity insecurity: a qualitative study highlighting intersectional disadvantage in the UK
- Caroline Dodd-Reynolds
- Naomi Griffin
Enough with simplifying: “eat less and move more”: at what point are we with the treatment of excess weight in paediatrics?
- Giovanni Corsello
- Sergio Bernasconi
Italian Journal of Pediatrics (2024)
Association between watching eating broadcast “Mukbang and Cookbang” and body mass index status in South Korean adolescents stratified by gender
- Sang-yeon Park
- Jeongha Eom
- Eun-Cheol Park
Nutrition Journal (2024)
Waist-circumference-to-height-ratio had better longitudinal agreement with DEXA-measured fat mass than BMI in 7237 children
- Andrew O. Agbaje
Pediatric Research (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

- China Daily PDF
- China Daily E-paper
- Global Lens
- Global Views
- Chinese Perspectives
- Opinion Line

Obese children, parental responsiblity and economic burden

Child obesity is a global issue, and while this article will focus on China, many of the points discussed are relevant worldwide, transcending geographical boundaries.
Overweight children are more prone to issues like poor cardiovascular health, asthma, and non-alcoholic fatty liver disease compared to their non-overweight peers. Additionally, these children are more likely to become obese adults, significantly burdening even the most robust healthcare systems. A 2021 study in The Lancet projected that the number of obese children in China would reach 58 million by 2030. In the same year, the Chinese Centre for Disease Control and Prevention estimated that, without preventive measures, adult chronic diseases resulting from being overweight or obese would cost 49 billion yuan annually. Furthermore, a 2023 Lancet study revealed that mortality associated with overweight and obesity among children and adolescents would lead to economic losses of CNY 211.4 trillion between 2025 and 2092. To clarify, when I refer to overweight children, I mean those who are visibly overweight and clearly need to lose a few pounds. While I could distinguish between being overweight and being obese, I believe that both conditions can have significant repercussions. Since the Chinese days of famine and scarcity are well-behind us, it's become apparent that the number of overweight children has increased substantially. Of course, several factors contribute to this issue, including the increase in sedentary lifestyles, excessive screen time, and changing dietary habits. However, attributing the problem solely to these factors can sometimes be an evasion of responsibility. I agree that all stakeholders are accountable for combating this tragic epidemic affecting not only China, but the world. However, since this article centres primarily on China, that will be our geographic focus. The government should certainly play a role in addressing the rising incidence of childhood obesity, such as by restricting internet access for children, taxing sugary drinks, and creating regulations for healthy school meals. However, why is there always so much emphasis on policy and interventions by authorities? Are caregivers of children truly so incapable that they need others to control what they feed their kids? Parents and caregivers must act and not shirk their responsibility. Some argue that we need to educate people on what constitutes a healthy diet. While I partially agree, I also see this as an excuse to virtue signal and defend the 'downtrodden.' Seriously, what parent doesn't understand that giving their child an apple is healthier than a Snickers bar? Some claim that past famines have influenced parents and other caregivers, especially grandparents, to overfeed their children. I believe this can largely be overcome with some simple intervention. My wife and I have constantly emphasized to my mother-in-law the importance of providing our daughter with a healthy diet, and by limiting the amount of junk food in the house, we've been successful so far. If my daughter eats a bowl of noodles and is still hungry, I offer her some chopped fruit or a sugar free yoghurt—she certainly doesn't need a second bowl of noodles. That's just common sense! As a pastoral worker in a secondary school, I have occasionally been concerned about some children's weight. At one point, I even considered speaking to a parent about their child's blatant obesity, but my wife advised me against it, saying, "No, Gary, don't do that. Their parents will get upset." Of course, I would approach this issue in a caring and supportive manner, driven by genuine concern for the child's health and long-term well-being. I understand it would be difficult for parents to hear, but my role sometimes requires having difficult conversations with parents. I recall a commentary a few years ago from Russia Today, and despite criticisms of this media outlet, I wholeheartedly agreed with their analysis of obesity and the UK's National Health Service (NHS). The video report argued that doctors in the UK need to stop avoiding difficult conversations with obese patients due to fear of causing 'offense'. As many know, obesity—a largely preventable ailment—is now placing a tremendous strain on the NHS, the British public's most beloved institution. I understand that some individuals are genetically predisposed to certain conditions and there is also the consideration of 'Food deserts', but does this apply to every overweight child? I doubt it! Parents and caregivers are the ultimate authority in guiding children towards a healthy lifestyle. No one ever said parenting was easy, and I, like all parents, find it challenging. However, if you are unable to make small adjustments to help your child achieve good health, you are failing both yourself and your family.
Gary Wood is a student pastoral worker at an international school and he has lived in China for 12 years. The views don't necessarily reflect those of China Daily. The article was first published on the Beautiful China website.
If you have a specific expertise, or would like to share your thought about our stories, then send us your writings at [email protected], and [email protected].
Childhood Obesity: Causes/Solutions Research Paper
Thesis statement, introduction, statistics about the problem, causes of childhood obesity, steps the government should take to eliminate the problem, works cited, note card i, note card ii.
Childhood obesity is one of the biggest developing health problems associated with the things such as types of foods that children consume, genetic factors, addiction to highly pleasurable foods, and diminished physical activities.
Therefore, failure of the government to take precautionary measures such as controlling the foods served to children, introduction of BMI checking to schoolchildren, and planning of anti-obesity campaigns amongst others will automatically threaten the health of children and that of the population of the nation at large.
Obesity is the development of more weight than the body of an individual is supposed to carry. Ideally, the body of a person should carry weight within a certain range according to the height of the given individual. Much weight for a specific height is deemed overweight and consequently underweight for a much less weight for a specific height.
Therefore, childhood obesity is the development of more weight, which is mostly fats, more than the height can accommodate. It is usually 20% more body fat weight in a child. Childhood obesity is a serious health problem to society due to the frequency of obesity cases that are being reported of late.
The greatest concern brought about by childhood obesity is that it has been identified as a precursor to certain adulthood ailments if not controlled. Thus, controlling it is a way of eliminating some adulthood ailments. As Riley reveals, childhood obesity leads to such ailments as; “hypertension, respiratory ailments, orthopedic problems, depression, type two diabetes, and high cholesterol among others” (395).
According to Green and Riley, childhood obesity has increased threefold since the year 1981. Sixteen per cent percentage of the population of children between the ages of 6 and 19 years suffer from obesity (917).
In the United States, 23% of children coming from poor families are likely to suffer from obesity compared to 14% of those who come from families that are doing well socially and economically (Riley 395). Obesity has led to a rise in the cost of healthcare for the national government with obesity cases consuming up to 71million dollars in terms of treatment between the years 2008-2009.
According to statistics, there has been a 50% increase in obese cases among children of 7-12 years during the years 1991-1998. Eyler finds that the United States of America government has had to come up with policies and legislation that would reverse the trend by the year 2015 (2294). This effort is an indicator to the seriousness of the problem and the concern that the government has towards it. What causes childhood obesity?
The Foods in the Market
One of the biggest causes of childhood obesity is the type of food a child eats. Following the increase in populations and the decrease in the land for agricultural production, scientists have come up with ways of producing high yields of crops on remarkably small pieces of land for feeding the populations. Most of these foods are produced using biotechnology and bioengineering, which lead to high crop yields. Most crops produced using the methods have been cited as sources of obesity upon producing food from them.
High yield crop production involves altering of the genetic makeup of the crops. When consumed by children and or other people, the effects are directly transferred to them. Animals that used as food to human beings are usually fed on foods with high hormones to spur quick growth of the animals. When children feed on products from these animals, the hormones are directly transferred to them thus triggering a faster development of their cells and body tissues hence leading to obesity.
Genetic Factors
Genetic factors can also be attributed to be a cause of childhood obesity that happens when a child grows bigger than the actual size, and then it is cited as a family trend. Some people are naturally grown. This condition sometimes inherited and passes from one generation to the other.
The study further revealed that there is a 75% chance of children being obese if their parents were obese and a 75% chance of children being thin or slim if their parents were thin. This fact is a sure indicator that obesity is a genetic factor that is passed on from parents to their children. The situation can be controlled if the children engage in activities that can enable them burn the extra calories and fats.
Addiction to highly pleasurable foods
According to Pretlow, addiction to highly pleasurable foods can be one of the biggest causes of obesity in children between the age of 5years to 19years (297). Most of these highly pleasurable foods are extraordinarily high in calories thus leading to extremely fast weight gain in children and young adults.
The advent of fast food outlets has exacerbated the problem because most of the foods sold in fast food outlets are highly pleasurable besides containing excess calories. Addiction to these kinds of foods can be equated to some extent to the addiction found in substances like drugs. Addiction to highly pleasurable foods thus leads the child eating more and more of the food. Because they are not in a position to burn the loads of calories gained by their bodies, they tend to begin piling more and more fats in their bodies.
Diminished physical activities
Childhood obesity can be attributed to diminished physical activities among children. Most children nowadays do not engage in physical activities as compared to the past. In the past, most parents would engage their children in physical activities like doing household chores while going out to play at the same time as a way of engaging in fun. That trend has changed dramatically in the recent past with most children engaging in activities that are not energy sapping.
The trend has changed with the introduction of computer games in society. Most children have ended up becoming couch potatoes because they spend almost all of their playing time playing computer games, which are addictive in nature. The increase in television programs has also led to children getting addicted to watching television. Reilly finds that television companies have come up with tailor-made programs for children thus leading to television addiction (395).
Controlling the food served in schools
The government should come up with a policy guideline on what types of food can be served in school kitchens. Nutritionists should recommend the foods because they have the right calorie contents for children at specific ages.
This campaign will see the government prepare a school feeding diet program that is based on healthy eating habits, which are aimed at reducing obesity and hence eliminating it in the end. An observation by Wojcicki and Heyman contends that an awareness program starting from schools is a sure way of controlling obesity (1630).
Introduction of BMI check in schools
The government should introduce a regular body mass index check to all children in schools as a way of checking and regulating the problem. A regular body mass index check will make the children aware of their weight status and the need to keep healthy bodies and lifestyles.
Such checks can also be used for recommending specific physical activity programs to the children as a way of enabling them burn the excess fats that have accumulated in their bodies. Children growing up with the awareness of the right body mass index will be able to control overweight problems when they occur in the future thus ensuring a healthy nation.
Develop a nationwide anti obesity campaign
The government should develop a nationwide campaign that will see the awareness levels of the population increased to such an extent that everyone in society is aware of the problem. Huang observes that a nationwide campaign to eliminate obesity will enable parents bring up their children with awareness of the obesity problem (148).
Most parents are usually unaware of the obesity problem in their children thus ending up not taking the right steps to stop it. The society today is made up of parents who spend a lot of their time chasing their careers than taking care of their children and hence the need to remind them of their responsibility.
Childhood obesity is a complex problem that cannot be easily wished away due to the many different elements that cause to it. It needs a multipronged approach that will control it. The problem with obesity is that it cannot be eliminated. Thus, there is a need for the government to put measures as discussed above to minimize it as much as possible.
Eyler, Army et al. “Patterns and predictions of state childhood obesity legislation in United States: 2006-2009.” American Journal of Public health 102.12 (2012): 2294- 2302. Print.
Green, Gregory, and Riley Clarence. “Physical activity and childhood obesity: Strategies and solutions for schools and parents.” Education 132.4 (2012): 915-920. Print.
Huang, Terry. “Prevention and treatment: Solutions beyond the individual.” Journal of Law, Medicine & Ethics 35 (2007): 148-149. Print.
Pretlow, Robert. Addiction to highly pleasurable food as a cause of the childhood obesity epidemic: A qualitative internet study . Washington D.C: Routledge, 2008. Print.
Riley, John. “Childhood obesity: An overview.” Children & Society 21.5 (2007): 390-396. Print.
Wojcicki, Janet, and Melvin Heyman. “Reducing childhood obesity by eliminating 100% fruit juice.” American Journal of Public Health 102.9 (2012): 1630-1633. Print.
Summary Note Card:
Following the rising impacts that obesity has had on the US citizens, leave alone the children, there has been a call to the government to pass bills that emphasize the need to reduce the danger caused by this fatal disease. Patterns and Predictors of Enactment of State Childhood Obesity Legislation in the United States: 2006-2009 points out the efforts that the US is making to curb the rising trend by 2015. The article reveals how the US has made it a priority to pass bills that address needs of the obese people as a way of ensuring that they are not left to die of the disease when measures can actually be implemented to rescue them and the US at large.
Quotation Note Card:
Eyler et al state, “…the number of bills introduced from 2006 to 2009 with obesity prevention content is encouraging, as is the enactment rate of these bills.”
Eyler, Army et al. “Patterns and predictions of state childhood obesity legislation in United States: 2006-2009.” American Journal of Public health 102.12 (2012): 2298. Print.
Paraphrase Note Card:
According to Eyler et al, the period 2006-2008 has been characterized by tremendous efforts by the US government to publish many bills that specifically touch on the issue of obesity. The findings indicate that the earlier on observed obesity trend in the US will be changing with time with fewer reports of obesity cases.
Despite the many efforts put in place to fight obesity, it is alarming to find out how obesity prevalence is rising in the UK and the US specifically among children and adolescents.
This revelation indicates that the current strategies used to fight the disease do not have a well-crafted message to persuade the children and adolescents to change their eating habits and or engage in strenuous activities to help rid themselves of the many useless calories whose accumulation has led to their obese nature. Hence, there is room for more studies on the best strategies to use to reach the affected children and adolescent if at all eliminating obesity is the goal of both the UK and the US.
“Successful prevention of obesity in future will require good examples or models of interventions which have achieved objectively measured and sustained behavior change”
Riley, John. “Childhood obesity: An overview.” Children & Society 21.5 (2007): 395. Print.
Due to the observed failure of the current strategies to help the obese children and adolescents, there has been a call for future research to incorporate interventions that will have the capacity to alter the observed high rates of obesity among the US and the UK children and adolescents.
- Fats, Carbohydrates, and Proteins
- Television Plus Junk Foods Equal Childhood Obesity
- How meth affects women and their children
- Human Digestion
- Definitions of Obesity and Criteria for Diagnosing It
- Obesity Could Be Catching
- White Wines vs. Red Wines
- Increased Nutrition Regulations on Fast Food Restaurants
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, December 11). Childhood Obesity: Causes/Solutions. https://ivypanda.com/essays/childhood-obesity-causes-solutions/
"Childhood Obesity: Causes/Solutions." IvyPanda , 11 Dec. 2018, ivypanda.com/essays/childhood-obesity-causes-solutions/.
IvyPanda . (2018) 'Childhood Obesity: Causes/Solutions'. 11 December.
IvyPanda . 2018. "Childhood Obesity: Causes/Solutions." December 11, 2018. https://ivypanda.com/essays/childhood-obesity-causes-solutions/.
1. IvyPanda . "Childhood Obesity: Causes/Solutions." December 11, 2018. https://ivypanda.com/essays/childhood-obesity-causes-solutions/.
Bibliography
IvyPanda . "Childhood Obesity: Causes/Solutions." December 11, 2018. https://ivypanda.com/essays/childhood-obesity-causes-solutions/.

COMMENTS
134 Childhood Obesity Essay Topics & Examples. Updated: Mar 2nd, 2024. 17 min. If you're writing an academic paper or speech on kids' nutrition or weight loss, you will benefit greatly from our childhood obesity essay examples. Besides, our experts have prepared a list of original topics for your work. We will write.
29 essay samples found. Childhood Obesity is a serious medical condition where excess body fat negatively affects a child's health or well-being. Essays might discuss the causes, consequences, prevention and management of childhood obesity, as well as the role of parents, schools, and healthcare providers in addressing this issue.
Long Essay on Childhood Obesity 500 Words in English. Long Essay on Childhood Obesity is usually given to classes 7, 8, 9, and 10. Obesity is a severe threat to children's health today. Childhood obesity is increasing year of year. A survey by The American Heart Association shows that obesity in children has more than tripled from 1971 to 2011.
Introduction. Childhood and adolescent obesity have reached epidemic levels in the United States, affecting the lives of millions of people. In the past 3 decades, the prevalence of childhood obesity has more than doubled in children and tripled in adolescents. 1 The latest data from the National Health and Nutrition Examination Survey show that the prevalence of obesity among US children and ...
Childhood Obesity 2 Abstract Obesity is a chronic health condition that is increasing at alarming rates in the United States, particularly among low-income children. This literature review examines several of the factors that place low-income children at risk for developing obesity: environmental (i.e., lack of access
Childhood obesity rates have increased substantially over the past year in the UK, according to a new report from the UK Government's National Child Measurement Programme. This rise in prevalence is the largest single-year increase since the programme began 15 years ago and highlights the worldwide rising trend for obesity among children and adolescents. Once considered a problem mainly in ...
Child Obesity Essay Outline. Childhood obesity is a growing epidemic that has raised significant concerns among health professionals, parents, and policymakers alike. With the rise of sedentary lifestyles, increased consumption of processed foods, and lack of access to healthy options, children are facing unprecedented challenges when it comes ...
Extraneous Variables. Confounding factors in childhood obesity largely revolve around the parental variable. Parents' socioeconomic level and body mass index (BMI) should be considered independent variables. Such extraneous variables are part of the category of participant factors; thus, a strategic approach will aid in regulating them ...
Childhood obesity: Current and novel approaches. Best Practice & Research Clinical endocrinology & Metabolism, 29, 327-338. This essay, "Children Health. Childhood Obesity" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper.
Suddenly, fat people weren't just neighbors, friends or family members — we were enemies to be feared. The war on childhood obesity reached its zenith with the 2010 introduction of the ...
This Review describes current knowledge on the epidemiology and causes of child and adolescent obesity, considerations for assessment, and current management approaches. Before the COVID-19 pandemic, obesity prevalence in children and adolescents had plateaued in many high-income countries despite levels of severe obesity having increased. However, in low-income and middle-income countries ...
IELTS Sample Task 2 Essay: Child Obesity. by Patel. (Bolton) The percentage of overweight children in western society has increased by almost 20% in the last ten years. Discuss the causes and effects of this disturbing trend. There is no doubt that overweight children's percentages rose by twenty percent in western world.
Prevalence. The prevalence of paediatric obesity 16 has increased worldwide over the past five decades. From 1975 to 2016, the global age-standardised prevalence of obesity in children and adolescents aged 5-19 years increased from 0·7% (95% credible interval [CrI] 0·4-1·2) to 5·6% (4·8-6·5) for girls and from 0·9% (0·5-1·3) to 7·8% (6·7-9·1) for boys. 17 Since 2000, the ...
Introduction. The prevalence of child and adolescent obesity remains high and continues to rise in low-income and middle-income countries (LMICs) at a time when these regions are also contending ...
Epidemiology is used in multiple instances in this article to make a compelling case for the advocacy and prevention of childhood obesity. Primarily, the authors examine the relatively high childhood obesity rates making a connection with its effects on health. The article provides that pediatric obesity has been on an upward spiral recently ...
February 12, 2024 by Prasanna. Obesity Essay: Obesity is a condition that occurs when a person puts on excess body fat. It is a sudden and unusual increase in body fat. It can lead to heart-related diseases, blood pressure, hypertension, cholesterol, and various other health issues. The main cause of obesity is over-eating.
This updated synthesis of obesity prevention interventions for children aged 6-18 years, found a small beneficial impact on child BMI for school-based obesity prevention interventions. A more comprehensive assessment of interventions is required to identify mechanisms of effective interventions to inform future obesity prevention public health policy, which may be particularly salient in for ...
The prevalence of childhood obesity continues to rise despite decades of clinical and public health efforts. Early identification of children at risk of developing obesity is essential using newer electronic health systems, which move beyond traditional growth charts to provide a wealth of information about body mass index and other relevant parameters such as social determinants of health and ...
The effect of obesity in children is vital. Self-esteem and confidence of the yout are usually affected. Overweight children have experienced being bullied by other kids. Consequently, depression ...
GB sentence 2: In the United States, the percentage of children and adolescents affected by obesity has more than tripled since the 1970s Data from 2015- 2016 show that nearly 1 in 5 school-age children and young people aged 6 to 19 years in the United States has obesity (Center for Disease Control and Prevention, 2018) iii.
We will write a custom essay on your topic. Meyers (2009) confirms the claim that child obesity has increasingly become prevalent among children aged between 6 and11 years. According to research evidences, it is apparent that the pediatric complications associated with obesity prolongs from childhood to adulthood.
Furthermore, a 2023 Lancet study revealed that mortality associated with overweight and obesity among children and adolescents would lead to economic losses of CNY 211.4 trillion between 2025 and ...
Childhood Obesity (Health - Essay the following are general comments about the structure and content of an academic essay written for university they are not. Skip to document. ... English Literature To 1800 ENG 493 Written Assignment Unit 4. English Literature To 1800. Assignments. None. 2. Resume 2021 Leah Loveless.
Addiction to highly pleasurable foods. According to Pretlow, addiction to highly pleasurable foods can be one of the biggest causes of obesity in children between the age of 5years to 19years (297). Most of these highly pleasurable foods are extraordinarily high in calories thus leading to extremely fast weight gain in children and young adults.
Position: Fall 2024 Public Health Fieldwork Placement Organization: NYC Health + Hospitals/Elmhurst Program Description: NYC Health + Hospitals/Elmhurst is the second oldest municipal hospital in New York City. Recently, Elmhurst was ranked by US News & World Report as a High Performing Hospital in 6 areas: Chronic Obstructive Pulmonary Disease, Heart Failure, Kidney Failure, Orthopedics ...