- Main Navigation
- Account Navigation
- Main Content

JavaScript is disabled on your browser
Please enable JavaScript or upgrade to a JavaScript-capable browser to use the ASH Image Bank.
- ASH Academy
- ABOUT IMAGE BANK
- PERMISSIONS
- COLLECTION Images of peripheral blood and/or bone marrow of blood disorders and normal hematopoiesis.
- ATLAS Normal and abnormal blood cells
- REFERENCE CASES Complete cases of common blood disorders (peripheral blood, bone marrow, and diagnostic studies).
- UPLOAD IMAGES
- Home / Reference Cases
Case history of a child with sickle cell anemia in India
A three years old male child, native of Jharkhand, Central India presented with mild pallor, icterus, and history of on and off abdominal and joint pains. On examination the child had mild splenomegaly. He had history of two prior hospital admissions. First at the age of 1 year, when he was diagnosed to have pneumonia and second, at the age of 3 years (3 months prior to coming to our institution) for fever, anemia and jaundice. He has had three transfusions till now, last transfusion was 3 months back. There is history of sibling death at 5 years of age due to fever and jaundice.
The hemogram showed anemia with leukocytosis. Red cell morphology (Figure 1) revealed severe anisopoikilocytosis with macrocytes, microcytic hypochromic red cells, target cells, many boat cells, sickled RBCs, polychromatic cells and occasional nucleated RBCs. Results of the automated blood cell counts showed Hb 7.7 g/dl, RBC 2.44 x 109/l, MCV 97.1 fl, MCH 31.4 pg, MCHC 32.3 g/dl, RDW 26.6%. There were occasional nucleated red cells and relative neutrophilia. Further to confirm HbS, a sickling test using freshly prepared 2% sodium meta-bisulphite was performed which was positive (Figure 2).
Hemoglobin HPLC on Bio-Rad Variant 2 showed raised fetal hemoglobin (HbF) and a variant peak in S window (71.9%) at retention time of 4.36 mins. Adult Hb (HbA) of 8.5% was noted (Figure 3). Figure 4 shows Cellulose acetate hemoglobin electrophoresis at alkaline pH (8.6), which showed a prominent band in S/D/G region and a faint band in F region. Investigations of the father showed also showed a variant peak in S window (32.9%) at retention time of 4.36 mins along with HbA (57.1%) on HPLC with Bio-Rad Variant II which is diagnostic of Sickle cell trait (Figure 5).
Sickle cell disease (SCD) is the most common symptomatic hemoglobinopathy caused as a result of inheritance of two copies of the sickle β-globin gene variant (βS). A single nucleotide substitution leading to replacement of glutamic acid by valine at position 6 of the β-globin polypeptide chain leads to formation of HbS which is responsible for disease manifestation. SCD has a wide geographical distribution throughout major parts of Africa, the Middle East, India and in some regions of Mediterranean countries. In India, it is mainly concentrated in the central region including parts of Madhya Pradesh, Chattisgarh, Orissa, Maharashtra, Gujrat and Jharkhand. HbS has carrier frequencies varying from 5 to 35% and are especially seen amongst the scheduled tribes, scheduled castes and other backward castes.
Sickle cell mutation is believed to be originated five times in history spontaneously. This can be elucidated by five βS-globin haplotypes. These haplotypes include Senegal (SEN), Benin (BEN), Bantu or the Central African Republic (CAR), Cameroon (CAM) and Arab-Indian (ARAB). They enable us to understand the origin, evolution, migration and natural selection of genetic defects. They can be identified by specific restriction sites within the β-globin gene cluster. Different haplotypes are known to have different HbF levels. Senegal and Arab-Indian haplotypes have higher HbF levels when compared to other haplotypes. However, recently a study has investigated the origins of the sickle mutation by using whole-genome-sequence data to conclude that there might be single origin of sickle allele.
LEARNING POINTS
1. Sickle cell disease (SCD) is the most common symptomatic hemoglobinopathy in the world, largely seen in parts of Africa, the Middle East, India and in some regions of Mediterranean countries.
2. SCA is a monogenic disorder with an autosomal recessive inheritance. The parents are clinically asymptomatic and have normal blood counts. They are usually diagnosed incidentally or as a result of family studies in SCA patients.
3. Neonates are asymptomatic due to high HbF, but symptoms begin to appear by six months of age. Many infants present with lethal complications at first presentation. This emphasizes the importance of newborn screening in these susceptible pre-symptomatic cases in endemic regions.
4. SCA has a variable clinical course amongst different individuals depending upon various genetic determinants like βs haplotype, factors affecting HbF levels and co-inheritance of other disease modifying factors.
5. Diagnosis mainly relies upon identification of HbS (by any of the following HPLC, Hb Electrophoresis, Iso-electric focusing or sickling test). Once HbS is identified, it has to be validated by alternative method.
6. Treatment of sickle cell disease generally aims at relieving symptoms and preventing infections, sickle cell crises and long-term complications. Stem cell transplant is the only potential cure available presently.
HPLC pattern of the index case with sickle cell anemia showing HbS and HbF peaks.
Hemoglobin electrophoresis at alkaline pH. Black arrow shows the index case with HbS and HbF bands.
Loading. Please wait.
Uploading files. please wait..
- ASH Foundation
- Log in or create an account
- Publications
- Diversity Equity and Inclusion
- Global Initiatives
- Resources for Hematology Fellows
- American Society of Hematology
- Hematopoiesis Case Studies
Case Study: Sickle Cell Disease A 25-Year-Old in Transition
- Agenda for Nematology Research
- Precision Medicine
- Genome Editing and Gene Therapy
- Immunologic Treatment
- Research Support and Funding
A 25-year-old woman with a history of sickle cell disease (SCD) presents to the clinic for follow-up after a hospitalization for a vaso-occlusive pain crisis complicated by influenza A. She has a history of an acute ischemic stroke at age 5 years and has received monthly, simple red cell transfusions since the stroke. Her last transfusion was approximately four months prior. She is taking deferasirox 20 mg/kg daily but occasionally misses doses.
Laboratory results show the following:
| Hemoglobin | 7.5 g/dL |
| Hematocrit | 24% |
| Leukocyte count | 9,300/mm |
| Platelet count | 202,000/m |
| Mean corpuscular volume | 105 fL |
| Hemoglobin electrophoresis | 92% HbS, 6% HbF, 2% HbA2 |
| Aspartate aminotransferase | 24 U/L |
| Alanine aminotransferase | 45 U/L |
| Ferritin | 1,300 ng/mL |
Which of the following is the next best step in diagnosis
- Restart scheduled red blood cell transfusions
- Start prophylactic penicillin
- Discontinue transfusions and start hydroxyurea
- Order transcranial doppler ultrasonography (TCD) to assess risk of stroke
- Increase dose of deferasirox to 25 mg/kg/day
Explanation
The incidence of primary stroke in children with SCD is 0.6 to 0.8 events per 100 patient-years, with a cumulative incidence of 7.8 percent by age 14 years in the Jamaican cohort and 11 percent by age 20 years in the U.S. Cooperative Study of Sickle Cell Disease. Once stroke has occurred, the incidence of recurrent (secondary) stroke ranges from 47 to 93 percent in patients not started on regular transfusions. The Stroke Prevention Trial in SCD (STOP) randomized 130 high-risk children with SCD to either transfusion therapy (to maintain HbS 30%) or observation. These high-risk children had an increased blood flow in the internal carotid or middle cerebral artery by TCD. This study showed a 92 percent reduction in incidence of first stroke in transfused high-risk patients. A follow-up study, STOP2, randomly assigned 72 children whose TCD had normalized after 30 months of transfusion therapy to either ongoing or discontinued transfusions. The study was closed early due to a significant increase in abnormal TCD velocity and stroke risk for those who halted transfusion therapy.
The multicenter phase III TWiTCH trial evaluated children with SCA and abnormal TCD velocities without a history of stroke on chronic transfusions. Data showed that hydroxyurea at maximal tolerated dose was noninferior to chronic transfusions for maintaining TCD velocities as primary stroke prophylaxis (choice C). This patient has a history of ischemic stroke, so the results of TWiTCH do not apply to her.
The Stroke with Transfusions Changing to Hydroxyurea (SWiTCH) study was designed as a phase III multicenter trial to determine the efficacy of hydroxyurea/phlebotomy, compared with transfusions/chelation for children with SCA, stroke, and iron overload in secondary stroke prophylaxis. The primary endpoint was a composite of noninferiority for stroke prevention and superiority for reduction of liver iron content. The trial was terminated at the first scheduled interim analysis for futility for the composite endpoint, which required superiority of phlebotomy over iron chelation for reducing excess iron stores. The incidence of stroke on the hydroxyurea plus phlebotomy arm was higher (7 of 67 patients; 10.4%) than in the transfusion plus chelation arm (1 of 66 patients; 1.5%). These results, though not powered for inferiority, showed a trend towars increased stroke risk with transition to hydroxyurea. In patients with prior stroke, cessation of transfusion therapy is currently not recommended.
Whether chronic transfusion therapy can be stopped after a longer period of transfusions in a patient with a prior stroke remains unclear even though risk of recurrent stroke remains high in adolescence and young adulthood. In patients older than 16 years, TCD velocity criteria to determine stroke risk is not reliable (choice D).
In the Prophylaxis with Oral Penicillin in Children with Sickle Cell Anemia trial, children with SCA were randomly assigned to receive oral prophylactic penicillin or placebo PROPS 1986 ). The trial ended eight months early after the occurrence of 15 cases of pneumococcal sepsis, 13 in the placebo group and two in the penicillin group, showing an 84 percent reduction in pneumococcal sepsis with penicillin prophylaxis. The follow-up study, PROPS II, did not show an increased risk in pneumococcal infections with discontinuation of prophylactic penicillin after age 5 years. Therefore, prophylactic penicillin is not recommended in adults with SCA (choice B).
The trajectory of ferritin in this patient has not been established and an increase in oral iron chelation is not indicated at this time.
Case Study submitted by Marquita Nelson, MD, of University of Chicago, Chicago, IL.
- Hirst C, Owusu-Ofori S Prophylactic antibiotics for preventing pneumococcal infection in children with sickle cell disease . Cochrane Database Syst Rev. 2014 6:CD003427.
- Valadi N, Silva GS, Bowman LS, et al Transcranial Doppler ultrasonography in adults with sickle cell disease . Neurology. 2006 22:572-574.
- Ware RE, Davis BR, Schultz WH, et al Stroke with transfusions changing to hydroxyurea (SWiTCH) . Blood. 2012 119:3925-3932.
- Kumar N, Gross JB Jr, Ahlskog JE TCD with transfusions changing to hydroxyurea (TWiTCH): hydroxyurea therapy as an alternative to transfusions for primary stroke prevention in children with sickle cell anemia . Blood. 2015 126:3.
American Society of Hematology. (1). Case Study: Sickle Cell Disease A 25-Year-Old in Transition. Retrieved from https://www.hematology.org/education/trainees/fellows/case-studies/sickle-cell-disease-a-25-year-old-in-transition .
American Society of Hematology. "Case Study: Sickle Cell Disease A 25-Year-Old in Transition." Hematology.org. https://www.hematology.org/education/trainees/fellows/case-studies/sickle-cell-disease-a-25-year-old-in-transition (label-accessed July 30, 2024).
"American Society of Hematology." Case Study: Sickle Cell Disease A 25-Year-Old in Transition, 30 Jul. 2024 , https://www.hematology.org/education/trainees/fellows/case-studies/sickle-cell-disease-a-25-year-old-in-transition .
Citation Manager Formats
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Sickle-Cell anemia (SCA).pptx
Related Papers
Hematology/Oncology Clinics of North America
Virgilio Lew
Biology of Blood and Marrow Transplantation
Shalini Shenoy
Pediatric Clinics of North America
JPMA. The Journal of the Pakistan Medical Association
Sickle Cell Disease (SCD) is a structural haemoglobinopathy which is extremely diverse in its presentation regarding disease severity and organ involved. The homozygous form if poorly managed gives rise to numerous life threatening conditions which are otherwise avoidable. Here we report the case of a male adolescent with homozygous SCD who presented with haemolytic anaemia, massive ascites, hepatomegaly and multiple fractures secondary to severe malnourishment associated with the disease.
The Pharma Innovation Journal
MADHURI SHENDE
Sickle cell disease (SCD) is a genetic disorder that affects erythrocytes (RBCs) causing them to become sickle or crescent shaped. The effects of this condition due to an abnormality of the hemoglobin molecules found in erythrocytes. The substitution of one amino acid in the hemoglobin molecule results in sickle hemoglobin. As a result RBCs sickle in low oxygen states causing occlusion of blood vessels, increased viscosity and inflammation. These RBCs are prematurely removed from the circulation, resulting in a chronic hemolytic anemia. With new born screening and early treatment, the death rate among children with SCD has declined. In addition, a variety of treatments are being introduced to help manage the various manifestations of disease. Transfusion, simple or exchange, is a mainstay of therapy, since it reduces the amount of Hgb S in circulation and suppresses erythropoiesis. Transfusion is indicated for symptomatic anemia and specifically to prevent stroke (first or recurrent...
Leonardo Lombardi
Andreas Chiabi
Current knowledge on the pathophysiology of sickle cell anemia is reviewed and potential therapeutic options are reviewed and discussed. It is hoped that better understanding of the pathophysiology will improve the care given to these patients as well as their quality of life. Keywords : sickle cell anemia, pathophysiology, treatment Clinics in Mother and Child Health Vol. 1(1) 2004: 30-36
Landmarks in Medical …
Titin Hamka
Clinical Medicine: Case Reports
John Olaniyi
Dr.shahid Raza
Sickle cell anemia is a genetic disorder resulting in irregularly regulating red blood cells also called as sickled cells leading to serious conditions like stroke, acute chest syndrome, pulmonary hypertension, organ damage, blindness and skin ulcers. Several mutations in HBB gene can cause sickle cell disease. Persons with sickle cell anemia can inherit infected genes from both parents. Despite a variable disease severity, individuals affected require regular health care from childhood all the way to adult age. This review, highlights the increased susceptibility to infections, the genetic factors and preventive measures to overcome various complications and challenges for sickle cell anemia.
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Journal of Pharmaceutical Research International
Madhuri Naik
Current Paediatrics
Kunle Adekile
The Internet Journal of Hematology
Hiren Dhanani
Journal of Blood Disorders & Transfusion
Varsha Wankhade
Charles Quinn
Jesus Rafael Moreno Piña
The American Journal of Medicine
Freda Boateng
International Journal of Neonatal Screening
Samsung Galaxy GT-S5312
Journal of Evolution of Medical and Dental Sciences
Sourya Acharya
Baillière's Clinical Haematology
Griffin Rodgers
Zenodo (CERN European Organization for Nuclear Research)
Dr. Gopal Krishna Purohit
The Indian journal of medical research
Ana Silva-Pinto
South African Medical Journal
ranjana sharma
Case Reports in Medicine
machiel van den akker
The Scientific World Journal
Carlton Dampier
American Journal of Hematology
Marilyn Telen
Clinical Pediatrics
Jose' Humphreys
Journal of Pediatric Hematology/Oncology
Mustapha Danesi
Clinical and Vaccine Immunology
Najat Qader
UKRAINIAN JOURNAL OF PERINATOLOGY AND PEDIATRICS
samira aggoune
abdullah alnajjar
Case Reports
Deepak Batura
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
SICKLE CELL DISEASE
Apr 18, 2013
1.63k likes | 3.02k Views
SICKLE CELL DISEASE. JOHN M KAUFFMAN JR DO ASSOCIATE DEAN FOR POSTGRADUATE AFFAIRS VIA COLLEGE OF OSTEOPATHIC MEDICINE. Goals and Objectives. At the conclusion of this program, the attendee will have a better understanding of: The genetics and transmission of Sickle Cell Disease
Share Presentation
- hemoglobin a s sickle
- single polypeptide chain
- better understanding
- gamma chains
- first office visit

Presentation Transcript
SICKLE CELL DISEASE JOHN M KAUFFMAN JR DO ASSOCIATE DEAN FOR POSTGRADUATE AFFAIRS VIA COLLEGE OF OSTEOPATHIC MEDICINE
Goals and Objectives • At the conclusion of this program, the attendee will have a better understanding of: • The genetics and transmission of Sickle Cell Disease • The Diagnosis and pathophysiology of Sickle Cell Disease • The management of the complications of Sickle Cell Disease • The current treatment of Sickle Cell Disease
Sickle Cell Disease: A Case • A 22yo AA woman is transferred to your hospital with respiratory failure. You are asked to see her in the emergency department. In the ED the patient is in obvious distress with a RR of 45 and an O2sat of 72%. Her ABG revealed 7.34/44/59/23/76% on 3 liters O2 by nasal canula.
Sickle Cell Disease: A Case • The patient had been diagnosed with Sickle Cell Anemia at age 6 and was hospitalized for a sickle cell crisis at age 12. 24 hours prior to admission in your hospital she was seen in another ED with severe pain (10/10) in her back thighs and knees. She was nauseated and had vomited once. She denied chest pain, SOB, fever, chills, abdominal pain, dysuria, constipation or diarrhea.
Sickle Cell Disease: A Case • Within 10 hours of admission to your hospital, the patients O2 sat dropped to 40% and she was intubated. Her ABG revealed: 7.35/44/80/22/94% on the vent with 100% O2 TV=350, and 22cm of peep. • What is your diagnosis?
Definitions • Sickle-Cell Disease: A group of blood disorders caused by a mutation in the hemoglobin gene. • Common Sickle Cell Diseases Include: • Sickle Cell Anemia • Hemoglobin SC Disease • Sickle Beta Thalasemia • Sickling and sickle cell disease also confer some resistance to malaria
Definitions • Sickle-Cell Anemia : Sickle-cell anemia is the name of a specific form of sickle-cell disease in which the individual is homozygous for the mutation that causes HbS. Normal hemoglobin is called hemoglobin A, but people with sickle cell anemia have only hemoglobin S, which in the homozygous form, turns normal, round red blood cells into abnormally curved (sickle) shapes. Sickling decreases the cells' flexibility and predisposes the carrier to potentially serious complications. Sickle-cell anemia is also referred to as "HbSS", "SS disease", "hemoglobin S" etc.
Sickle Cell Anemia
Definitions • Sickle Cell Trait: condition in which a person has one abnormal allele of the hemoglobin beta gene ( heterozygous), but does not display the severe symptoms of sickle cell disease that occur in individuals who have two copies of the abnormal Hb S allele ( homozygous) • About 2 million Americans have sickle cell trait. The condition occurs in about 1 in 12 African Americans.
Sickle Cell Disease • Sickle cell disease (SCD) is the most common genetic disorder identified in African Americans, • Also found in people from South and Central America, the Mediterranean and the Middle East.
Sickle Cell Disease • In the United States, it’s estimated that sickle cell anemia affects around 50,000 people, mainly African Americans. The disease occurs in about 1 out of every 700 African American births. • Before the era of Hydroxyurea, the average life expectancy was in the 40’s
Clinical Hallmarks of Sickle Cell Disease (SCD) • Vaso-occlusion • Hemolysis
Diagnostic Testing: • Cellulose acetate electrophoresis is a standard method of separating Hb S from other hemoglobin variants. However Hb S, G, and D have the same electrophoretic mobility with this method.
Diagnostic Testing: • Citrate agar electrophoresis seperates Hb S from Hb D and G • Thin-layer isoelectric focusing and high performance liquid chomatography (HPLC) are highly accurate tools for the diagnosis of sickle or other hemoglobin variants
Diagnostic Testing • In Summary: Cellulose acetate electrophoresis with either citrate agar electrophoresis or a solubility test allows a definitive diagnosis of sickle cell syndrome • Alternatively, thin layer isoelectric focusing will separate Hb S, D, and G and can replace the two electrophoretic methods. • However, thin-layer isoelectric focusing still requires a confirmatory solubility test for Hb S
Newborn Screening • Mandated in all 50 states and the District of Columbia. • Most states use either thin-layer isoelectric focusing (IEF) or high performance liquid chromatography (HPLC) as the initial screening test. • Both methods have extremely high sensitivity and specificity for sickle cell anemia. Specimens must be drawn prior to any blood transfusion (false negative) • Extremely premature infants may have false positive results when adult hemoglobin is undetectable
Screening Programs • Selective screening of infants of high-risk parents • Universal testing of newborns • Selective screening misses up to 20% of AA newborns with SCD • sickle cell diagnoses doubled when screening was changed from targeted to universal
Hemoglobin Patterns
Laboratory Findings in Sickle Cell Disease • Chronic Hemolysis with mild to moderate anemia (Hct 20-30%) • Reticulocytosis of 3-15% (.5-1.85% RBCs) • Unconjugatedhyperbilirubinemia • Sickled RBCs on peripheral smear • Low serum erythropoietin secondary to progressive renal disease • Folate and Iron deficiency secondary to increased utilizaton of folate and urinary excretion of iron
Peripheral Blood Smear • Sickled red cells • Polychromasia indicative of reticulocytosis • Howell-Jolly bodies secondary to splenic infarcts • Normochromic, normocytic RBCs
Findings in Sickle Cell Disease • The Cooperative Study of Sickle Cell Disease looked at Lab Data in 2600 people with SCD • Mean WBC counts elevated especially in children < age 10 • Thrombocytosis seen individuals < age 18 • Serum Alk Phos elevated until puberty
TIMING OF SCREENING • Test all newborns at the time of birth • Verify screening results at first office visit • Perform confirmatory tests no later than 2 months of age.
Most common types of sickle cell disease • Hemoglobin SS disease (also called Sickle Cell Anemia) • Hemoglobin Sickle-C disease • Sickle Beta-Thalassemia.
Hemoglobin • Hemoglobin: Definition and Structure • Hemoglobin carries oxygen from the lungs to tissues and CO2 from the tissues to the lungs for excretion. • Hemoglobin molecule consists of two parts: • Porphyrin group or heme • Protein or globin portion. • Globin is made up of four polypeptide chains attached to the porphyrin ring • Four types: alpha, beta, delta and gamma.
Hemoglobin Molecule
Sickle Cell Hemoglobin • In normal Hemoglobin A, glutamic acid is on the 6th position of the beta chain, while in sickle-cell disease, this glutamic acid is replaced by valine (point mutation) leading to the formation of sickle cells. • Polymerization: the two beta chains fit into each other forming a longitudinal polymer (or lock and key) causing the cell to become deformed and very rigid leading to vessel occlusion. • Polymerization: activated by infections, hypoxia, acidosis, physical exercise, vasoocclusion due to cold as well as dehydration.
Sickle Cell Hemoglobin In sickle cell hemoglobin (HbS) glutamic acid in position 6 (in beta chain) is mutated to valine. This change allows the deoxygenated form of the hemoglobin to stick to each other.
Normal Adult Hemoglobin • Primarily Hemoglobin A • 2 alpha chains and 2 beta chains • Beta chain synthesis begins early in fetal development • Sixth week of gestation, hemoglobin A composes about 7% of the total hemoglobin; the percentages slowly increase throughout the pregnancy • Thirtieth week there is a switch from gamma chain to beta chain production.
Fetal Hemoglobin • At birth babies have mostly fetal or F hemoglobin • falls to the normal level of less than 3 to 5% by the time the infant is 5-6 months of age • Adults have less than 2% fetal hemoglobin. • Fetal hemoglobin is made up of two alpha and two gamma chains.
STRUCTURAL FORMULA FOR NORMAL HEMOGLOBIN • A Major Adult Hemoglobin 2 Alpha Chains + 2 Beta Chains • F Fetal Hemoglobin 2 Alpha Chains + 2 Gamma Chains • A2 Minor Adult Hemoglobin 2 Alpha Chains + 2 Delta Chain
HEMOGLOBINOPATHIES • Hemoglobinopathy: disease or trait caused by a defect in the genetic code for hemoglobin synthesis • Over 600 known hemoglobin variants reported • Vast majority of abnormal hemoglobin result from the mutation of a single polypeptide chain.
Genetics of Sickle Cell Trait • Heterozygous subject (sickle cell trait (A/S), an abnormal gene is inherited from one parent and it directs the formation of abnormal hemoglobin. • A normal gene is inherited from the other parent and it directs the formation of normal hemoglobin.
Example of an Inheritance Pattern for Sickle Cell Trait
Genetics of Sickle Cell Disease • Homozygous subject, identical abnormal genes are inherited; one from each parent, and the majority of the hemoglobin is abnormal, such as in sickle cell anemia (S/S).
HEMOGLOBIN A/S SICKLE CELL TRAIT • GENOTYPE: AS • Beta chain variant • Each red cell contains a mixture of A (60%) and S (40%). • Amount of A in each cell is enough to prevent sickling under most physiological conditions.
POPULATIONS AFFECTED • African Americans: 8-10% • Hispanic Americans: 2% • Occurs frequently in Greeks, Italians, Saudi Arabians, East indians and Middle Easterners
CLINICAL SYMPTOMS of Sickle Cell Trait • NOT associated with anemia. • Offers some protection against malaria. • Occasional hematuria and hyposthenia (impaired renal concentrating ability) • Splenic infarction reported to occur at altitudes greater than 7,000 feet • Greater risk for sudden death under extreme conditions such as those that might occur during basic training in the military. • severe dehydration, malnutrition, physical overexertion and exhaustion. This risk though increased, is small.
PRECAUTIONS • Avoid hypoxic situations: deep sea diving, flying in unpressurized aircraft, strenuous physical activity over a prolonged period of time.
COUNSELING POINTS TO BE MADE • Person is a healthy carrier • Person is not sick. • Sickle cell trait is not a disease. • Sickle cell trait will not cause you to be anemic. • There is a small amount of hemoglobin S, but not enough to change the shape of the red blood cell. • The red blood cells of a person with sickle cell trait remain round and flexible.
SICKLE CELL ANEMIA • GENOTYPE: S/S • Hemoglobin S (90-100%) • Hemoglobin F may be slightly elevated
SICKLE CELL ANEMIA • Most common form of sickle cell disease identified in African Americans
SICKLE CELL ANEMIAClinical Symptoms • Most severe form of sickle cell disease • Clinical course variable • Severe anemia • Vaso-occlusion, pain episodes, organ damage • Aplastic episode, splenic sequestration, increased risk for infection • If HbF is greater than 10% there is a decreased risk of stroke
SICKLE CELL ANEMIAPRECAUTIONS • Genetic counseling and screening to clarify risk for child born with sickle cell disease • Referral to High Risk OB Clinic for pregnancy. • Avoid Hypoxia, dehydration
Clinical Manifestations of Sickle Cell Disease • Vasoocclusion and hemolysis are the hallmarks of sickle cell disease • Vasoocclusion results in recurrent painful episodes (sickle cell crisis) • Dactylitis (acute pain in the hands and feet) is the most common initial symptom
Most Common Complications of Sickle Cell Disease • Acute Painful Crisis (Sickle Cell Crisis) • Acute Chest Syndrome • Stroke • Chronic Lung Disease • Avascular Necrosis • Leg Ulcers
- More by User
Sickle Cell Disease
Sickle Cell Disease. Project Title: Building Sickle Cell Disease and Leadership Capacity of Nurses in Nigeria. Name of Proposers : Grace Ogiehor-Enoma, RN, MSN, MPH, CNA, BC; Victoria Odesina, CNM, MS, APRN, APNG, CCRP & Sandra Anyoha, RN, MSN, MPH.
481 views • 16 slides
Sickle Cell Disease. Sickle Cell Disease. Group of genetic disorders characterized by: Hemolytic anemia - not enough red blood cells in the blood Vasculopathy - disorder of blood vessels In US, predominantly with African-Americans (i.e., 1 in 400)
564 views • 17 slides
314 views • 8 slides

Sickle Cell Disease. www.nursing.oman-face.com. Done by: nursing institutes fourms Evaluated by: prince of nursing.
969 views • 43 slides
Sickle Cell Disease. www.nursing.oman-face.com. Done by: nursing institutes fourms Evaluated by: prince of nursing. Introduction.
508 views • 31 slides
Sickle Cell Disease. Maggie Marsh. Causes. It is an inherited disease Sickle hemoglobin causes the cell to become crescent shaped A person inherits two genes, one from each parent and if both have sickle cell gene then you will get it. Signs. Shortness of breath Dizziness Headaches
429 views • 6 slides
Sickle Cell Disease. Taeron Burrell. What Is Sickle Cell Anemia? Sickle cell Anemia is a serious disorder in which the body makes sickle shape blood cells instead of regular ones.
652 views • 16 slides
Sickle Cell Disease. Yohan Kim. Sickle Cell. First to described in 1904 by James B. Herrick. Found “elongated and sickle-shaped” red blood cells (RBCs) from a patient suffering from anemia
862 views • 23 slides
Sickle Cell Disease. Mason Clark Max Smith Neil Towery Leslie Probus. Cardiovascular System Effects. Misshapen RBCs lead to impaired blood flow Needed nutrients can’t be transported effectively Can lead to blood clots . Nervous System Effects. Can lead to: stroke ischemic attack
197 views • 7 slides
Sickle Cell Disease. Sickle Cell Anemia. Sickle Cell anemia is an inherited red blood cell disorder. Normal red blood cells are biconcave discs, and they move through small blood tubes in the body to deliver oxygen.
523 views • 16 slides
Sickle Cell Disease. Project done by: Alexis Ferguson. About this disease:. Sickle Cell Disease is passed down through families. It is where the red blood cells that normally are shaped like a disk, take on a sickle or crescent shape.
297 views • 5 slides
Sickle Cell Disease. James Everett, LaCasha Gordon, Richard Lucas, Eboni Taylor. What is Sickle Cell Disease?. An Inherited Group of Red Blood Cell Disorders. Sickle Cell Anemia, Sickle Cell Disease, and Sickle beta-thalassemia.
493 views • 11 slides
Sickle Cell Disease. Kelsey Jarzembowski. I f your red blood cells don't contain enough hemoglobin . Your blood has a lower than normal number of red blood cells.
184 views • 7 slides
Sickle Cell Disease. Sickle C ell Disease:.
161 views • 4 slides
Sickle Cell Disease. Martin H. Steinberg. Department of Medicine, Boston University School of Medicine, Boston, MA. (07/18/13). Sickle Cell Disease: General Points. Globin Gene Mutations are Autosomal Co-dominant (Recessive) Traits.
995 views • 30 slides
* For Best Viewing: Open in Slide Show Mode Click on icon or From the View menu, select the Slide Show option. * To help you as you prepare a talk, we have included the relevant text from ITC in the notes pages of each slide. Sickle Cell Disease.
599 views • 32 slides
Sickle-cell disease
Sickle-cell disease. By: Adam Clark and Stephanie Fuqua. Inheritance. Recessive in parents Two copies are altered They combine. Symptoms. Painful episodes Chronic anemia Serious infections Damage to organs. Punnet Square. Sickle-cell anemia in children. Both parents affected
349 views • 12 slides
Sickle Cell Disease. Hemoglobin. Protein made of many amino acids The sequence of amino acids is genetic coded by DNA Function to carry oxygen and other compounds. Genetic Process. DNA contains compounds called bases– adenine, thymine, guanine and cytosine– in a genetic coded sequence
186 views • 11 slides
Sickle Cell Disease. Blaze Mowatt. SBI 3U. http://www.unm.edu/~mpachman/Blood/sicle.htm. Definition. Disorder of the red blood cells that carry oxygen to body tissue Normal red blood cells are round and soft
522 views • 14 slides
Sickle cell disease
Sickle cell disease. This is an inherited multisystem disorder caused by abnormal properties of RBCs containing HbS. This results from mutation in the β-globin gene that changes the 6th amino acid from glutamic acid to valine. Pathophysiology.
613 views • 37 slides
Sickle Cell Disease. Introduction. Vaso-occlusive phenomena and hemolysis are the clinical hallmarks of Sickle Cell Disease (SCD) Inherited disorder due to homozygosity for the abnormal hemoglobin, hemoglobin S (HbS).
657 views • 34 slides
Sickle Cell Disease. Paolo Aquino, M.D., M.P.H., PGY I Combined Internal Medicine/Pediatrics. Outline. What is sickle cell disease? Epidemiology Manifestations Approach Treatment. What is it?.
460 views • 22 slides
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

90 templates
classroom rules
5 templates

meet the teacher
31 templates

95 templates
earth science
84 templates
38 templates
Sickle Cell Anemia
It seems that you like this template, sickle cell anemia presentation, free google slides theme, powerpoint template, and canva presentation template.
There was a French cartoon that was very popular in Spain many years ago, and it told kids how the human body works, in a way that they can understand. The main characters were red blood cells, and we wouldn't be able to picture them in a sickle-like shape, which is what would happen in the case of sickle cell anemia. This disease can be the topic of your informative presentation, and this template can be your starting point! Be sure to add things such as risk factors, diagnosis, recommendations and prevalence!
Features of this template
- 100% editable and easy to modify
- 28 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the free resources used
How can I use the template?
Am I free to use the templates?
How to attribute?

Combines with:
This template can be combined with this other one to create the perfect presentation:

Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Register for free and start downloading now
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access


- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
SICKLE CELL ANEMIA.
Published by Dakota Channon Modified over 9 years ago
Similar presentations
Presentation on theme: "SICKLE CELL ANEMIA."— Presentation transcript:
SICKLE CELL DISEASE Sickle cell anemia.
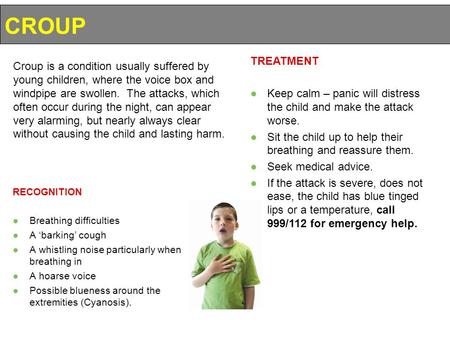
RECOGNITION ●Breathing difficulties ●A ‘barking’ cough ●A whistling noise particularly when breathing in ●A hoarse voice ●Possible blueness around the.
SICKLE CELL ANEMIA Adeline Olaniran.
Sickle Cell Anemia. Sickle cell anemia - abnormally shaped red blood cells that are shaped like a sickle (or crescent). Hard and sticky, sickle cells.
S ICKLE C ELL A NEMIA Muna Abubaker & Christina Fry 4 th Period.
Sickle Cell Anemia By Alex Lange & Roy Darrah. Inheritance Pattern Parents can be carriers and show no symptoms of the disease. Sickle Cell Anemia is.
By: Alejandra Arellano
Sickle Cell Anemia By: Jazzalyn Williams, Ashley Townsell & Makarios Ngure.
Sickle Cell Anemia By: Daniel Lee, Matt Milan, and Min-ki Kim.

cell trait.doc.
Sickle Cell Anemia.
By: Kyle Wislinsky Bryce Peterson
Sickle Cell Anemia Columbia County Medical Assistant Association.
Sickle- Cell Anemia Lulu Liu Meghan Ha AP BIO- 7TH Genetic Disorders:
Sickle Cell Anemia. What Is It? Sickle Cell Anemia is……. A Genetic disease body produces abnormally shaped red blood cells. Red blood cells shaped like.
Sickle Cell Anemia - basics (? #1) O Sickle cell anemia (or sickle-cell disease) is an inherited disorder of the red blood cells– it causes blood cells.

Your body makes three types of blood cells: red blood cells, white blood cells, and platelets (PLATE-lets). Red blood cells contain hemoglobin, an iron-rich.
The Disease Lesson 3.1 Review.
SICKLE CELL DISEASE -Monica. Sickle Cell is inherited, and it affects the shape of red blood cells. Genetic: Caused by a Hemoglobin S (sickle) molecule.
Anemia Dr Gihan Gawish.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Sickle cell anemia.
Ankit Mangla ; Moavia Ehsan ; Nikki Agarwal ; Smita Maruvada .
Affiliations
Last Update: September 4, 2023 .
- Continuing Education Activity
Sickle cell anemia is an inherited disorder of the globin chains that causes hemolysis and chronic organ damage. Sickle cell anemia is the most common form of sickle cell disease (SCD), with a lifelong affliction of hemolytic anemia requiring blood transfusions, pain crises, and organ damage. Since the first description of the irregular sickle-shaped red blood cells (RBC) more than 100 years ago, our understanding of the disease has evolved tremendously. Recent advances in the field, more so within the last three decades, have alleviated symptoms for countless patients, especially in high-income countries. This activity reviews the pathophysiology, presentation, complications, diagnosis, and treatment of sickle cell anemia and also highlights the role of the interprofessional team in the management of these patients.
- Describe the pathophysiology of sickle cell anemia.
- Summarize the epidemiology of sickle-cell anemia.
- List the management options for sickle cell anemia.
- Outline the importance of cooperation among healthcare professionals to educate the patients on getting vaccinated, remaining hydrated, and timely follow-up to prevent the development of complications in those with sickle cell disease.
- Introduction
Sickle cell disease (SCD) refers to a group of hemoglobinopathies that include mutations in the gene encoding the beta subunit of hemoglobin. The first description of SCA 'like' disorder was provided by Dr. Africanus Horton in his book The Disease of Tropical Climates and their treatment (1872). However, it was not until 1910 when Dr. James B Herrick and Dr. Ernest Irons reported noticing 'sickle-shaped' red cells in a dental student (Walter Clement Noel from Grenada). [1] In 1949, independent reports from Dr. James V Neel and Col. E. A. Beet described the patterns of inheritance in patients with SCD. In the same year, Dr. Linus Pauling described the molecular nature of sickle hemoglobin (HbS) in his paper 'Sickle Cell Anemia Hemoglobin.' Ingram Vernon, in 1956, used a fingerprinting technique to describe the replacement of negatively charged glutamine with neutral valine and validated the findings of Linus Pauling. [2]
Within the umbrella of SCD, many subgroups exist, namely sickle cell anemia (SCA), hemoglobin SC disease (HbSC), and hemoglobin sickle-beta-thalassemia (beta-thalassemia positive or beta-thalassemia negative). Several other minor variants within the group of SCDs also, albeit not as common as the varieties mentioned above. Lastly, it is essential to mention the sickle cell trait (HbAS), which carries a heterozygous mutation and seldom presents clinical signs or symptoms. Sickle cell anemia is the most common form of SCD, with a lifelong affliction of hemolytic anemia requiring blood transfusions, pain crises, and organ damage. [3]
Since the first description of the irregular sickle-shaped red blood cells (RBC) more than 100 years ago, our understanding of the disease has evolved tremendously. Recent advances in the field, more so within the last three decades, have alleviated symptoms for countless patients, especially in high-income countries. In 1984, Platt et al. first reported the use of hydroxyurea in increasing the levels of HbF. [4] Since then, the treatment of sickle cell has taken to new heights by introducing several new agents (voxelotor, crinzalizumab, L-glutamine) and, most recently, gene therapy.
Hemoglobin (Hb) is a significant protein within the red blood cell (RBC). It comprises four globin chains, two derived from alpha-globin (locus on chromosome 16) and two from beta-globin (locus on chromosome 11). There are many subtypes of Hb. The most common ones that are found in adults without hemoglobinopathies are listed here:
- HbA1- comprises two chains of the alpha-globin and two chains of the beta-globin (a2b2) - This constitutes 95% of the adult hemoglobin.
- HbA2- comprises two chains of the alpha-globin and two chains of the delta-globin (a2d2) - This constitutes less than 4% of the adult hemoglobin.
- HbF- comprises two chains of the alpha-globin and two chains of the gamma-globin (a2g2) - This Hb is more prevalent in the fetus (due to the high oxygen binding affinity that helps extract oxygen from maternal circulation).
The sickle cell mutation occurs when negatively charged glutamine is replaced by a neutral valine at the sixth position of the beta-globin chain. The mutation is transmitted via Mendelian genetics and is inherited in an autosomal codominant fashion. [5] A homozygous mutation leads to the severest form of SCD, i.e., SCA- also called HBSS disease. The coinheritance of beta-naught thalassemia and sickle cell mutation leads to HBS-Beta-0 disease, which phenotypically behaves like HBSS disease.
A heterozygous inheritance leads to HbAS. Patients with HbAS are not considered within the spectrum of SCD as most of them never present with typical symptoms of SCA. They might only be detected during childbirth, blood donation, or screening procedures.
Several other compound heterozygotes exist where a single copy of the mutated beta-globin gene is coinherited with a single copy of another mutated gene. The second most common variant of SCD is the HbSC disease, where the sickle cell gene is coinherited with a single copy of the mutated hemoglobin C gene. HbC is formed when lysine replaces glutamine at the sixth position on the beta-globin chain. HbSC disease accounts for 30% of patients in the United States.
- Epidemiology
The epidemiological data on SCD is scarce. It is well known that SCD and HbAS are more prevalent in sub-Saharan Africa, where the carrier of HbAS is afforded natural protection against severe Plasmodium falciparum malaria. It is estimated that ~230,000 children were born with SCA, and more than 3.5 million neonates were born with HbAS in sub-Saharan Africa in 2010. an estimated 75% of SCD-related births take place in sub-Saharan Africa. West Africa is home to the largest population of individuals with HbSC disease. [3]
The United States (US) Center for Disease Control (CDC) estimates that approximately 100,000 Americans have SCD. The CDC also estimates that 1 in 13 babies born to African-American parents have sickle cell trait, and 1 in 365 African-Americans have SCD. The estimated ratio of Hispanic Americans with SCD is 1 in 16,300. Children and adolescents make up to 40% of all SCD patients in the US. The incidence varies by state and geographical concentration of ethnicities. Besides, migration within the country and immigration from foreign countries alter the prevalence of SCD and HbAS. This is true for several countries where patients with SCD and SCA are living. Genetic studies in Brazil have also tied the origin of such patients to the slave trade originating from West Africa (Mina Coast and Angola). [6] With the improvement in technology and ease of international migration, the incidence of SCA is predicted to rise. It is estimated that the annual number of newborns with SCA will exceed 400,000 by 2050.
There is also a stark difference in mortality and morbidity in high-income and low-income countries. Adopting vaccination guidelines for children with SCD and intensive screening procedures has sharply reduced the mortality of kids with SCD between 0 to 4 years (68% drop noted from 1999 to 2002 compared to 1983 to 1986). On the other hand, in sub-Saharan Africa, 50 to 90% of children born with SCD will die before their fifth birthday. Improving the care afforded in high-income countries and targeted training of healthcare providers have improved life expectancy. However, it still lags by decades compared to matched non-SCD cohorts (54 versus 76 years - projected life expectancy, and 33 years versus 67 years- quality-adjusted life expectancy). [7]
HbSC disease accounts for 30% of all patients with SCD in the US. As with HbAS, patients with the Hb C trait (heterozygous mutation) also remain asymptomatic for most of their lives. Although considered a milder variant of SCD, HbSC disease may present with severe morbidities. [8]
- Pathophysiology
Sickle cell anemia is characterized by two major components: Hemolysis and vaso-occlusive crises (VOC). The defect in the beta-globin gene makes the sickle hemoglobin (HbS) molecule susceptible to converting into rigid, elongated polymers in a deoxygenated state. The sickling process is cyclical initially, where sickle erythrocytes oscillate between the normal biconcave shape and the abnormal crescent shape (acquired under low oxygen pressure). However, there comes a time when the change becomes irreversible, and the sickle erythrocytes develop a permanent sickle shape increasing the risk for hemolysis and VOC. All variants of SCD share the same pathophysiology leading to polymerization of the HbS component. [3]
Multiple factors inherent to sickle erythrocytes, like low affinity of HbS to oxygen, physiologically high 2,3-diphosphoglycerate, and increased sphingokinase-1 activity, lead to deoxygenation, which promotes polymerization of HbS. In addition to this, high concentration of HbS, abnormal activity of Gados channel leading to dehydration, and repeated damage to red blood cell (RBC) membrane also increase the risk of polymerization of HbS.
Oxidative stress contributes to hemolysis by auto-oxidation of HbS, leading to erythrocyte cell membrane damage. The increased expression of xanthine dehydrogenase, xanthine oxidase, and decreased expression of NADPH oxidase increase the oxidative stress within sickle RBC. A hemolyzed cell releases free hemoglobin (scavenges nitrous oxide) and arginase 1 (competes for L-arginine) that prevent the action and formation of nitrous oxide and contribute to oxidative stress and vascular remodeling (arginase-1 converts arginine to ornithine). [3]
Besides the polymerization of the HbS and intravascular hemolysis, several other factors also contribute to vaso-occlusion. For example, the sickle RBC (expresses several adhesion molecules on the surface), free heme and Hb, reactive oxygen species, and endothelium interact with each other and with neutrophils and platelets to promote vaso-occlusion and thrombosis.
- Histopathology
In patients with SCA, peripheral blood smear shows elongated RBC with tapering ends that look like a sickle (also called drepanocytes). Additional findings are present in a few patients.
- Howell-Jolly bodies- Remnants of DNA are seen in the RBC and commonly seen in patients in whom the spleen has been removed. Therefore, patients with SCA have auto-splenectomy.
- Target cells (Leptocytes)- Most commonly seen in patients with Thalassemia. They are seen frequently in sickle-thalassemia syndromes and are sometimes noted in patients with SCA.
- Polychromatic cells - these are reticulocytes that signify marrow response to hemolysis.
- Nucleated red blood cells can sometimes be visible on the peripheral smear.
None of these findings are confirmatory. Confirmation is obtained only through hemoglobin electrophoresis, high-performance liquid chromatography, or isoelectric focusing. DNA-based techniques are not used routinely. Instead, they are used in patients with uncertain diagnoses. Pre-natal fetal testing involves using fetal DNA obtained through amniocentesis. Techniques to capture the fetal DNA in maternal blood remain investigational.
- History and Physical
Most patients with HbSS phenotype do not present with classical 'sickle cell crises' soon after birth. HbF is still present in the blood, helping maintain adequate tissue oxygenation, and it takes around 6-9 months to wean off completely. Not all SCA have the same phenotype, and multiple phenotypes exist that can either co-exist or present as a spectrum of the disease. [3]
- Vaso-occlusive subphenotype - Distinguished by higher hematocrit (Hct) compared to other SCA. A higher Hct leads to higher viscosity that promotes frequent vaso-occlusive crises and acute chest syndrome.
- Higher risk of gallstones, pulmonary hypertension, ischemic stroke, priapism, and nephropathy
- Severe anemia increases cardiac workload and blood flow through organs, making them susceptible to damage
- Higher free heme and Hb in blood vessels cause oxidative damage
- High Hb F subtype- A 10 to 15% level of HbF alleviates the symptoms of SCA. However, the distribution of HbF is not consistent throughout the body.
- Pain-sensitive subphenotype- Altered neurophysiology amongst various individuals make them susceptible to pain. Some individuals are more susceptible to pain compared to others with SCA.
The patients with SCA present wither with acute or chronic complications associated with the disease. The most common acute complication of SCA is Vaso-occlusive crisis (VOC). The treatment section below discusses the management of acute and chronic issues.
Important points to be noted in the history of patients with SCA
- All patients with SCA will experience VOC during their lives. The earliest presentation is dactylitis in kids as young as six months of age.
- Any body organ can develop VOC (head, eyes, etc.), although extremities and the chest are most commonly involved. If a VOC pain sounds atypical, obtain a history to rule out other causes.
- When was the last pain crisis, and how many times in the previous year have they been admitted to the hospital with pain crises?
- If they take analgesics daily, it is prudent to know the type and quantity of the analgesic (opioid or non-opioid), the last use of analgesics, and whether they take the analgesics before coming to the ER/office
- History of taking disease-modifying drugs (hydroxyurea, voxelotor, crinzalizumab, etc.)
- A history of substance abuse, psychiatric disorders, and use of psychotropic medications must be obtained.
- History of receiving blood transfusions and exchange transfusions- helps assess the risk of iron overload, presence of alloantibodies (multiple transfusions in the past can lead to the development of alloantibodies, which will help assess the risk of transfusion reactions), and previous transfusion reactions.
- History of any other diseases that may or may not be associated with SCA - previous history of stroke, thrombosis, priapism, etc.
- It is also advised to get in touch with the primary hematologist taking care of the patient- it is valuable to have their input in understanding the patient's normal physiology.
- History of previous surgeries.
- History of life-threatening crises in the past- if present, should alert the clinician to ensure that a similar event is not occurring again. For example, fat embolism may occur more frequently in patients with SCA.
The physical exam should focus on the general system exam to determine the need for oxygen requirements, pain management, and blood/exchange transfusion. However, a focused exam is also necessary to rule out any organ-specific problem. For example, a rapidly enlarging liver or spleen should alert the physician about sequestration crises.
Patients with SCA are usually diagnosed in childhood. Intensive newborn screening programs in developed countries can identify patients in the neonatal stage. In the US, universal screening for SCA was implemented in all states by 2007. High-performance liquid chromatography and isoelectric focusing are the methods used in the US. In Europe, most countries deploy targeted screening in high-risk areas (where SCA is more common) and not a universal screen. In sub-Saharan Africa, no country has adopted a screening program. In India, the solubility test is used as the first step- if positive, then high-performance liquid chromatography is used to confirm at the reference center. [3]
Acute Complications in Patients with SCA
Acute Chest Syndrome (ACS): ACS is the most common complication of SCA. It is also the most common cause of death and the second most common cause of hospital admission. A patient can either present with ACS or may develop it during hospitalization for any other reason. Hence, it is prudent to monitor all patients with SCA admitted to the hospital for ACS. It is important to recognize ACS early and act upon it to prevent respiratory failure.
- The risk factors for ACS include a previous history of ACS, asthma, or recent events like recent surgical procedures, pulmonary embolism, fluid overload, infection, etc.
- The clinical features include sudden onset of cough and shortness of breath. Fever may or may not be a part of the spectrum of presentation. If present, then it usually points towards infection.
- Laboratory evaluation includes a complete blood count with differential chemistries, including liver and kidney evaluation, blood cultures, and sputum cultures.
- Chest X-ray shows a new pulmonary infiltrate- this is a quintessential feature of defining ACS. CT and perfusion mismatch scans are only used if there is a strong clinical suspicion of pulmonary embolism or fat embolism. Therefore, they are not usually helpful in acute settings.
Sequestration Crises: This can either be hepatic or splenic sequestration.
- Patients experience rapid spleen enlargement associated with pain in the left upper quadrant. In children with SCA, it is common in children between 1 to 4 years of age, as the spleen is still intact.
- Patients with non-SCA variants (HbSC, HbS-beta+ thalassemia) are not prone to 'auto-splenectomy' commonly seen in patients with SCA. Hence they can develop splenic sequestration later in life. Such patients may have baseline splenomegaly, causing hypersplenism. Parents and patients must receive counseling regarding the signs and symptoms of an enlarging spleen.
- Younger patients present with acute anemia and hypovolemic shock due to smaller circulating volumes, whereas adults may present with a more insidious onset.
- Pain occurs due to stretching of the splenic capsule and new infarcts.
- Blood count shows a drop in Hb by more than 2gm/dL, increased reticulocyte count, and nucleated red blood cells.
- Hepatic sequestration: Hepatic sequestration can occur across all phenotypes of SCA. Like the spleen, patients may have a baseline enlargement of the liver. Hepatic sequestration is also defined as rapid enlargement of the liver with stretching of the capsule. The hemoglobin shows a drop of more than 2gm/dL. Liver enzymes may not get elevated.
Acute Stroke: Stroke is the most devastating complication of SCA. Since the advent of transcranial doppler (TCD) and the institution of primary prevention programs, the incidence of stroke has gone down in patients with SCA. In the absence of primary prevention, ~10% of children suffer from overt stroke, and approximately 20 to 35% have silent cerebral infarcts. TCD is not useful for adults.
- Severe headache, altered mental status, slurred speech, seizures, and paralysis- are signs of stroke.
- Urgent neurological consultation and CT scan followed by MRI/MRA must be done.
Aplastic crises: It is usually precipitated by parvovirus B-19 and is defined as a rapid drop in Hb at least 3 to 6 gm/dL below the baseline. Patients present with severe fatigue, anemia, shortness of breath, and even syncope. Blood counts show severely low hemoglobin with near-absent reticulocytes. Bone marrow biopsy shows arrest in the pro-normoblast stage in patients with acute parvovirus infections. [9]
Acute intrahepatic cholestasis (AIC): Presents with sudden onset right upper quadrant pain. Physical exam shows worsening jaundice, enlarging and tender liver, and clay-colored stools. Labs show very high bilirubin levels, elevated alkaline phosphatase, and coagulopathy. The hemolysis parameters may be normal. AIC is a medical emergency.
Infections in patients with SCA can be a harbinger of infection with Streptococcus pneumoniae infection or osteomyelitis.
- The use of prophylactic antibiotics and pneumococcal vaccinations has reduced their incidence. However, loss of splenic function in SCA patients puts them at risk of invasive bacterial species.
- Osteomyelitis can be unifocal or multifocal- Staphylococcus aureus , Salmonella , and other enteric organisms can cause osteomyelitis in SCA patients.
Priapism is defined as a sustained, unwanted painful erection lasting more than 4 hours. It is a common condition among patients with SCA, affecting 35% of all men/boys.
Acute Ocular Complications
- The complication presents similarly in patients with SCA and sickle cell trait.
- The low oxygen pressure and acidotic nature of the aqueous humor promote sickling of the RBC, leading to blockage of the trabecular network leading to an acute rise in intraocular pressure (IOP).
- High IOP is poorly handled in patients with SCA - which can lead to CRAO and secondary hemorrhages.
- Central Retinal Artery Occlusion (CRAO)- Results from thrombus formation in the retinal artery leading to infarction of the retina, macular ischemia, or macular infarction. CRAO can occur spontaneously or secondary to increased IOP (from hyphema), Moyamoya syndrome, or ACS in patients with SCA.
- Patients present with proptosis, local pain, and edema of the lid or orbit.
- The exam shows reduced extraocular motility and decreased visual acuity.
- CT scan helps in distinguishing this from orbital cellulitis/ infection.
- Orbital Compression Syndrome (OCS) - also called orbital apex syndrome, is characterized by ophthalmoplegia and vision loss secondary to events occurring at the orbital apex. Cranial nerves II, III, IV, VI, and the first division of CN V can be involved. MRI of the orbits is the best modality for diagnosis.
Chronic Complications in Patients with SCA
Iron Overload: Iron (Fe) overload is a common problem in SCA patients due to repeated transfusions and chronic hemolysis. Each unit of packed RBC contains 200 to 250 mg of iron. Excessive iron mainly affects the heart, lungs, and endocrine glands. [10] Hepatic cirrhosis from excessive iron is a major cause of death in patients with SCA. Clinical trials in patients with thalassemia have shown that systemic iron load correlates directly with survival and cardiac incidents. [11]
Avascular Necrosis (AVN) of Joints: AVN of the femoral head is a common cause of chronic pain and disability in SCA patients. Although the hip joint is the most common joint to be involved, other joints can also be affected. AVN occurs at the distal portion of the bone, where collateral circulation is poor. The capillaries get occluded by sickle RBCs leading to hypoxia and bone death. Risk factors for AVN of the femoral head include age, frequency of painful episodes, hemoglobin level, and alpha-gene deletion. In patients with HbSS, the overall prevalence is 50 percent by age 33. HbSS-alpha thalassemia and HbSS-Beta-0 thalassemia are at higher risk of developing AVN early in life.
Leg Ulcers : More common in SCA compared to other SCD genotypes. Approximately 2.5% of patients with SCA above ten years of age have leg ulcers. Leg ulcers are more common in men and older people and less common in people with high total hemoglobin, alpha-gene deletion, and high levels of HbF. Trauma, infections, and severe anemia also increase the risk of leg ulcers. The ulcers occur more commonly on the medial and lateral surfaces of the ankles. They vary in size and depth, and chronic ulcers may lead to osteomyelitis, especially if they are deep enough to expose the bone.
Pulmonary Artery Hypertension (PAH) : Affects 6 to 11% of patients with SCA. PAH in SCA is classified under World Health Organization (WHO) group V. However; chronic hemolysis leads to pulmonary vascular changes classified under WHO group 1 in up to 10% of all SCA patients. PAH in SCA can also occur due to left heart dysfunction (Group II), chronic lung disease from SCA (Group III), chronic thromboembolism (Group IV), or extrathoracic causes (Group V).
The patient may complain of dyspnea on exertion, swelling in the legs, or present with symptoms of underlying disease (like a history of thrombosis, heart failure, etc.). An echocardiogram helps in estimating the tricuspid regurgitant jet velocity (TRV). Elevated TRV is associated with increased mortality in adults. However, TRV can be transiently elevated during acute chest syndrome. Serum NT-pro-BNP is directly correlated with mortality as well. The final diagnosis is made with a right heart catheterization.
Renal complications: Chronic kidney disease (CKD) occurs in approximately 30% of adult patients with SCA. The acidotic, osmotic, and hypoxic environment of the kidney increases the risk of polymerization of HbS, leading to the sickling of RBC. SCA patients secrete excessive creatinine in their proximal tubules. Hence, it becomes challenging to identify early signs of kidney disease, as creatinine takes a longer time to rise. Microalbuminuria (30-300mg albumin in 24-hour urine collection) is often the first manifestation of CKD. Spot urine-creatinine ratio is not validated in SCA patients due to hypersecretion of creatinine.
- Hypoesthenuria- Inability to concentrate urine due to loss of deep juxtamedullary nephrons. It is the most common complication in SCA patients. It leads to frequent urination and increases the risk of dehydration. It also increases the risk of enuresis in children.
- Renal papillary necrosis occurs due to obstruction of the vessels supplying the vasa recta resulting in medullary infarction. It presents with hematuria. It is more common in patients with HbSC disease.
- Asymptomatic Proteinuria: It is present in 15 to 50% of patients. It develops early in life due to hyperfiltration and loss of selectivity for albumin.
Ophthalmologic Complications: Chronic eye complications are more common in patients with HbSC and HbSS disease. They are found in up to 50% of patients.
- Proliferative Sickle Retinopathy occurs due to vaso-occlusion of vitreal arterioles leading to ischemia which leads to neovascularization. Neovascular tissue is predisposed to hemorrhage and vitreal traction forces resulting in vitreal hemorrhage (the most severe complication of proliferative sickle retinopathy).
- Treatment / Management
Patients with SCA present with acute and chronic complications.
Management of Acute Complications
Pain management is a critical part of SCA. It is challenging for clinicians to accurately assess patients' needs, especially if they meet them for the first time. Patients with SCA often suffer from the stigma of requiring high doses of opioids for pain control, which leads to them being labeled as 'opioid abusers,' 'manipulators,' or even' drug seekers.' [12]
- Analgesic administration starts simultaneous with evaluating the cause, ideally within 30 minutes of triage and 60 minutes of registration.
- Develop individualized pain management plans - this should be made available to the emergency room and should be implemented each time the patient presents with VOC and pain.
- NSAIDs are used in patients with mild to moderate pain who report prior episodes of relief with NSAIDs
- Any patient presenting with severe pain- preferably used parenteral opioids. An intravenous route is preferred; however, if access is difficult, use the subcutaneous route.
- The dose of parenteral opioids is calculated based on the total dose of short-acting oral opioids taken at home.
- Pain should be reassessed every 15 to 30 minutes, and readminister opioids if needed. The escalation of opioids is done in 25% increments.
- Patient-controlled analgesia (PCA) is preferred. If an "on-demand" setting is used in PCA, then continue long-acting analgesia.
- When pain control is achieved, "wean off" parenteral opioids before converting to oral medications.
- Calculate the inpatient analgesic requirement at discharge and adjust home doses of short and long-acting opioids accordingly.
- Meperidine is not used in managing VOC-related pain unless this is the only medication that controls the pain.
- Antihistamines only help in controlling opioid-related itching. When required, use oral formulations only—readminister every 4 to 6 hours as needed.
- Incentive spirometry
- Intravenous hydration
- Supplemental oxygen is needed only if saturation drops below 95% on the room air.
Management of Chronic Pain
Chronic pain management in SCA patients focuses on the safe and adequate use of pain medications, particularly opioids. A comprehensive assessment of the patient's ailment, the kind and doses of pain medicine required to control pain, and the functional outcomes of using these medications are made at each encounter. The process involves collaboration with multiple specialties, like psychiatry, social work, etc., to administer the right pain medicine in the proper doses.
The strategy adopted in the clinic to prescribe pain medicine involves:
- One person must be assigned to prescribe long-term opioids. They should document all encounters extensively involving the physical exam, lab work, etc.
- Assess each patient for non-SCA-related pain and treat/refer to the appropriate specialty for managing this pain.
- Limit prescribing pain medicines without meeting the patient- every patient must be physically assessed every 2 to 3 months or sooner.
- Develop an individualized pain management plan for each patient, reassess this plan annually, and modify it accordingly.
- Encourage patients to explore alternative methods of controlling pain, like direct massage, self-hypnosis, and music therapy.
Acute Chest Syndrome (ACS): It is an emergency regardless of the sickle cell disease phenotype. It can lead to respiratory failure and death if not managed as an emergency.
- All patients must be hospitalized-
- Upon admission, start treatment with antibiotics, including coverage for atypical bacteria.
- Supplemental oxygen is provided to those with oxygen saturation of less than 95% at room air.
- "Early" administration of simple blood transfusion is recommended for hypoxic patients. However, exchange transfusion is recommended at the earliest opportunity.
- Close monitoring for worsening respiratory status, increasing oxygen requirement, worsening anemia, and bronchospasm (use of beta-adrenergic dilators is encouraged in asthmatics) must be done. Intensive care units must be on standby to receive such patients who experience worsening respiratory status.
- Closely monitor predictors of severity- increasing respiratory rate, worsening hypoxia, decreasing hemoglobin or platelet count, multilobar involvement on chest X-ray, and developing neurological complications.
- Incentive spirometry and hydration (intravenous or oral) must always be encouraged.
- ACS is a strong indicator for initiating disease-modifying therapy (hydroxyurea, etc.) or starting the patient on a chronic blood transfusion program.
Sequestration Crises
- Intravenous fluids for hydration, pain control, and simple/exchange blood transfusion are central to managing sequestration crises.
- Never correct anemia completely- when the crises resolve, and the organs shrink, the sequestered blood re-enters the circulation, leading to increased hematocrit and viscosity, increasing the risk of thrombotic and ischemic events.
- Splenectomy is recommended for patients with life-threatening episode splenic sequestration crises or with recurrent splenic sequestration. It is also offered to those who have baseline hypersplenism.
- Instruct patients and parents in monitoring the size of the liver and spleen regularly.
Acute Stroke: Urgent neurology and transfusion medicine consultation are needed to provide optimal care and prevent long-term damage.
- Simple or exchange blood transfusion emergently.
- Start a program of chronic exchanges or blood transfusion.
- Where blood transfusion cannot be used (iron overload, excessive alloantibodies) or is unavailable, start on long-term disease-modifying therapy. SWiTCH trial demonstrated that chronic transfusions are a better way to manage patients with stroke.
Aplastic Crises: Parvovirus infections cause a transient drop in hemoglobin. Humoral immunity develops within 7 to 10 days that stays for life. The patient is extremely susceptible to developing ACS or stroke during the acute period. Initiate exchange/simple transfusion to bring Hb to a safe level, not necessarily to normal/baseline level.
Infections presenting with fever: Oral empiric antibiotics are given promptly while evaluating the reason for the fever. For ill-appearing patients, admit them and administer intravenous antibiotics.
Priapism: Early recognition is the key to management. Delayed management can lead to impotence. Urologists need to be involved early on in the care of such patients.
- Conservative measures include using analgesics, hydration, and sedation - which usually leads to detumescence and retains potency. Most experts would call for upfront urologic management rather than losing time trying conservative measures. [13]
- Urologists can perform penile aspiration or irrigation of corpora cavernosa with alpha-adrenergic drugs.
- Blood transfusion/ exchange transfusion is not useful - few authors have reported neurological complications with the use of blood transfusion (ASPEN syndrome). Hence it is best to avoid blood transfusion.
Acute ocular Complications: All ocular complications must be managed in consultation with ophthalmologists and hematologists to prevent vision loss.
- Hyphema- Anterior chamber paracentesis or surgical intervention to manage the thrombus must be done promptly.
- Reducing intraocular pressure helps prevent CRAO and other compression issues.
- Infections are managed with prompt administration of antibiotics.
- Corticosteroids are used to relieve excessive pressure in patients with OCS.
Chronic Complications
Avascular Necrosis: About 40 to 80% of cases of hip joint AVN are bilateral; therefore, both joints should be investigated simultaneously. Pain management and physical therapy are to be initiated as early as possible. Advanced cases may require hip arthroplasty.
Leg Ulcer: Conservative measures involve wound care, wet-to-dry dressings, and pain control. Hydroxyurea is avoided in patients with open leg ulcers, as it may prevent healing. Frequent evaluation for the stage of healing or lack of infection, osteomyelitis must be done. Local and systemic antibiotics are used for infected ulcers.
Pulmonary Hypertension: Patients with higher TRV are referred to pulmonologists for management. Small studies have shown increased mortality with sildenafil.
Renal Complications: Refer SCA patients with micro- or microalbuminuria to nephrologists for detailed workup and consideration of angiotensin-converting enzyme inhibitor (ACE-inhibitor). Follow patients closely who have modest elevation in creatinine (>0.7 mg/dL in children, >1.0 mg/dL in adults), and refer to a nephrologist at the earliest sign of worsening creatinine.
Ophthalmologic Complications: Refer SCA patients regularly for ophthalmologic evaluation, especially if they complain of slow vision changes. Direct and indirect ophthalmoscopy, slit-lamp biomicroscopy, and fluorescein angiography are used to evaluate SCA patients. Laser photocoagulation therapy is used to manage proliferative sickle retinopathy. A vitrectomy or retinal repair may be needed in the rare event of vitreal hemorrhage or retinal detachment.
Iron Overload
Unlike hemochromatosis, phlebotomy is not an option in patients with SCA. Preventing iron overload with good transfusion practices is the best way to deal with iron overload. Patients with SCA need not follow the rule of having hemoglobin close to 7gm/dL. Packed RBC transfusion should be restricted to the management of symptoms. Choosing exchange transfusion over simple transfusion also helps to reduce/prevent iron overload.
Indications to start iron chelation therapy
- A liver iron concentration (LIC) greater than 3 mg iron (Fe)/gm dry weight
- Cardiac T2* < 20 milliseconds
- Serum ferritin greater than 1000 on two different occasions 15 days apart
- Age greater than two years
- Expected survival beyond one year
- Number of transfusion of Packed RBC in 1 year- > 10 in pediatric patients OR > 20 in adults.
Goals of therapy
- Serum ferritin < 1000 mcg/L,
- LIC <7mg Fe/gm dry weight
- Cardiac T2* > 20 milliseconds
When do patients need modification of treatment?
- Treatment needs to be intensified if LIC > 15 mg Fe/gm dry weight and deescalated when LIC < 3 mg Fe/gm dry weight.
- Treatment needs to be intensified if serum ferritin > 2500 IU/L and deescalated when serum ferritin < 300 IU/L
- Treatment needs to be intensified when cardiac MRI shows T2* < 15 milliseconds or when cardiac symptoms occur (like heart failure, arrhythmias)
Iron Chelators
- Disperse tab formulation: Initial dose: 10mg/kg/day. Maximum dose: 20mg/kg/day
- Tablet or granule formulation: Initial dose: 7mg/kg/day. Maximum dose: 14mg/kg/day
- It does not interfere with the pharmacodynamics of hydroxyurea; hence it can be used simultaneously.
- Adverse effects- gastrointestinal intolerance, dose-dependent rise in serum creatinine, liver dysfunction.
- Daily subcutaneous infusions via portable infusion pump given over 8 to 24 hours; 1 to 2 gm/day
- It can be given as a daily IV infusion also. 40 to 50 mg/kg/day (max dose 60 mg/kg/day) over 8 to 12 hours (max rate 15 mg/kg/hour)
- IM route is acceptable for children but not preferred for adults. 0.5 to 1mg/day
- Adverse effects- Injection site reactions, cardiovascular shock (if administered too fast), blood dyscrasias, growth retardation.
- Adverse effects - agranulocytosis, hepatotoxicity, gastrointestinal symptoms, and arthralgia.
Blood transfusion: Blood transfusions form an integral part of the management of SCA. The goal of transfusion is to increase the oxygen-carrying capacity of blood and reduce the HbS component. A blood transfusion (simple or exchange) is given to keep the HbS level below 30% (STOP 1 and 2 trials). [14] In patients receiving regular exchange transfusions (history of stroke, intolerance, or contraindication to hydroxyurea), a more practical target for HbS is 25% to prevent a rise of HbS beyond 30%.
What types of blood transfusion are used in SCA?
- Simple transfusion: Transfusion of matched packed red blood cells (PRBC)
- Exchange transfusion: Transfusion of PRBC while removing blood from the patient at the same time.
Who should receive blood transfusions?
- Hb < 7gm/dL or drop of >2 gm/dL from baseline- consider simple or exchange transfusion.
- Twin pregnancy- consider prophylactic exchange transfusion
- Hb less than 9 gm/dL- Simple transfusion
- Hb more than 9gm/dL- Partial exchange transfusion
What kind of transfusion practice should be followed?
- Severe ACS - oxygen saturation less than 90% even when started on supplemental oxygen.
- Multiorgan Failure
- Acute ischemic stroke
- Splenic sequestration - never corrects the anemia completely.
- Acute anemia
Complications from Chronic Transfusions
- Alloimmunization- increases the risk of transfusion reactions, especially delayed hemolytic transfusion reactions.
- Iron overload
- Transmission of blood-borne diseases like hepatitis B, C, and HIV; extremely low risk due to intensive screening of donors and blood products.
- Differential Diagnosis
In general, globin gene mutations affecting hemoglobin are common and affect 7% of the entire world population. [15] Over 1000 variations of hemoglobin exist. However, only a handful of variations are significant clinically.
Common Variants of SCA or HbSS Disease
- Hemoglobin S-beta-0 thalassemia (Clinically behaves exactly like HbSS disease)
- Hemoglobin SC (a milder variant of SCD) - can have a phenotypic presentation of sickle cell anemia
- Hemoglobin S-beta+ thalassemia (a milder variant of SCD)
Several other hemoglobin variants are present that can mimic SCA if they are inherited along with HbS.
- Hemoglobin Jamaica-Plain (beta-68 [E12] Leu -> Phe)
- Hemoglobin Quebec-Chori (beta-87 [F3] Thr > Ile)
- Hemoglobin D-Punjab (beta-globin, codon 121, glutamine to glutamic acid)
- Hemoglobin O-Arab
- Hemoglobin E
Other conditions that can present with hemolysis, where SCA can be ruled out with history, examination, hemoglobin electrophoresis, and study of the peripheral smear
- Antibody-mediated autoimmune hemolytic anemia (both warm and cold antibodies)
- Other hemoglobinopathies- alpha or beta-thalassemia
- Paroxysmal nocturnal hemoglobinuria
- RBC-membrane defects (hereditary spherocytosis, hereditary elliptocytosis)
- Enzyme defects (pyruvate kinase deficiency, glucose-6-phosphate deficiency)
- Drug-induced hemolysis
- Transfusion-related hemolysis (acute or delayed hemolytic reaction)
- Microangiopathic hemolytic anemia (atypical or typical hemolytic uremic syndrome, thrombotic thrombocytopenic purpura)
- Infectious causes (malaria, babesiosis, Rickettsia , Clostridia , Bartonella )
- Vasculitis-induced hemolysis
- Medical Oncology
The goal of disease-modifying therapy in sickle cell anemia is to reduce the frequency of vaso-occlusive crises (VOC) and pain crises and prevent organ damage. These medications usually do not have a role "during" acute crises. Hydroxycarbamide, or hydroxyurea, was the first drug approved by the FDA for use in patients with SCA. However, the USFDA approved hydroxyurea for pediatric patients two years and above only in 2017 (based on the ESCORT HU trial).
Disease-Modifying Drugs/Therapy
The goal of disease-modifying therapy in patients with SCA is to alter the kinetics of sickle erythrocytes. Hydroxyurea does this by increasing the concentration of fetal hemoglobin (HbF).
Hydroxyurea: This is a ribonucleotide reductase inhibitor that increases the concentration of HbF in patients with SCD. It not only increases the intracellular concentration of HbF but also increases the number of erythrocytes containing HbF. In addition to this, hydroxyurea also reduces the number of circulating reticulocytes and leukocytes, raises the volume of an RBC (high MCV is noted in patients receiving hydroxyurea), reduces the deformability of RBC, improves the flow of blood through capillaries, and alters the expression of adhesion molecules hence preventing vaso-occlusive crises. The initial trials with hydroxyurea (Phase-III Multicenter Study of Hydroxyurea in Sickle Cell Anemia (MSH)) demonstrated a clear benefit over placebo in reducing the incidence of pain crises and the cost of care. Long term, the MSH study also showed a mortality benefit. In the pediatric age group, two seminal trials (HUG-KIDS-Phase I/II and BABY HUG-phase III) demonstrated good tolerability and led to the drug's approval. [16] [17]
- Having three or more sickle cell-associated moderate to severe pain crises within a 12-month period; treat with hydroxyurea
- Those with sickle cell-associated pain that interferes with daily activities of living and quality of life
- History of severe and/or recurrent ACS
- Severe symptomatic chronic anemia that interferes with daily activities or quality of life
- Infants 9 months of age and older, children, and adolescents with SCA, offer hydroxyurea regardless of clinical severity to reduce SCA-related complications (e.g., pain, dactylitis, ACS, anemia)
- For those with chronic kidney disease taking erythropoietin and hydroxyurea can be added to improve anemia
- DO NOT give hydroxyurea to pregnant women and lactating mothers who choose to breastfeed their babies
- Dosing for adults: Start with 15 mg/kg/day. Round up to the closest 500 mg. For patients with CKD- start at 5 to 10 mg/kg/day.
- Dosing for infants and children: start at 20 mg/kg/day
- Target absolute neutrophil count (ANC) of above 2000/microL and platelet count above 80,000/microL. In younger patients, an ANC of 1250/microL is allowed if baseline counts are low.
- Monitor blood counts every four weeks when increasing the dose of hydroxyurea.
- Clinical response takes 3 to 6 months to come. Hence a minimal trial of 6 months of daily continued use of hydroxyurea is done before considering alternative therapies.
- Daily adherence is a must. It must be emphasized to the patient.
- If a positive response is seen, then hydroxyurea must be continued indefinitely.
- Myelotoxicity is the most common and most substantiated adverse effect of hydroxyurea. The rest of the adverse effects reported in the literature, especially carcinogenesis and leukemia, have never been demonstrated in large studies.
- Avoid the use of hydroxyurea in patients with leg ulcers.
Voxelotor: Voxelotor acts by inhibiting the polymerization of HbS and increasing the affinity for oxygen. It is dosed at 1500 mg by mouth daily and is approved for SCA treatment in patients 12 years of age and older. Voxelotor can be given with or without hydroxyurea. USFDA approved it in 2019 based on the results of the phase 3 HOPE trial (Hemoglobin Oxygen Affinity Modulation to Inhibit HbS Polymerization) evaluating voxelotor (1500 mg versus 900 mg versus placebo in 1:1:1 design). [18] [19]
The most common adverse reactions are headache, diarrhea, abdominal pain, nausea, fatigue, rash, and pyrexia. Voxelotor interferes with high-performance liquid chromatography (HPLC). Hence the hemoglobin quantification is not accurate when the patient is on voxelotor. HPLC should be done when the patient is off therapy. Also, the use of voxelotor may increase the Hb, but there is no evidence to suggest discontinuation of exchange transfusion in patients receiving this for stroke prophylaxis.
Crizanlizumab: A humanized immunoglobulin G2-Kappa monoclonal antibody inhibits P-selectin, thereby blocking its interaction with P-selecting glycoprotein-1. This leads to reduced interaction between activated endothelium, platelets, leukocytes, and sickled RBCs, leading to reduced VOC. [20] The phase II SUSTAIN trial demonstrated a clinical benefit of Crizanlizumab by demonstrating a reduction in pain crises, VOC, emergency room visits, and increased median time to first crises. Although the hospitalization rate was numerically lower in the intervention group, the difference was not statistically significant compared to the placebo group. [21]
It is approved for the treatment of SCA in patients 16 years of age and older. It is dosed as a 5mg/kg intravenous infusion administered over 30 minutes at weeks 0, 2, and then every four weeks. The most common adverse reactions are nausea, arthralgia, back pain, and pyrexia. Infusion-related reactions can occur. Crizanlizumab can interfere with platelet counts; send the blood immediately before administration or send blood in citrated tubes.
L-Glutamine: Glutamine is the most abundant amino acid in the body. It is not an essential amino acid under normal circumstances, but in patients with SCA, a high hemolysis rate increases the demand for glutamine. L-glutamine is available in a medical formulation. The exact mechanism of action of L-glutamine remains anecdotal. It is believed to work by scavenging for reactive oxygen species and acting as a substrate for the regeneration of nitrous oxide, NAD, and NADH. [22] The USFDA approved L-glutamine in 2017 after positive results from the phase III trial. The authors demonstrated a statistically lower number of pain crises, fewer hospitalizations, fewer cumulative days in the hospital, prolonged time to first and second pain crises, and a reduced number of ACS. [23] Adverse events include constipation, nausea, headache, abdominal pain, cough, extremity pain, back pain, and chest pain. There is an additional concern that L-glutamine may increase mortality and the rate of multiorgan failure. However, these are yet exploratory.
Hematopoietic Stem Cell Transplant
Allogeneic hematopoietic stem cell transplant (HSCT) is a potentially curative option in SCA patients where cure rates approach approximately 90%. Improving the quality of life and reducing the cost of managing long-term complications trumps the cost of performing allogeneic HSC. Pre-school age is considered the best time to perform HSCT, with increased mortality recorded in older patients. A myeloablative or a non-myeloablative regimen can be used; however, myeloablative regimens are not recommended for adults. Matched sibling donor is preferred for performing allogeneic HSCT. Due to the lack of matched sibling donors, other approaches like a matched unrelated donor, umbilical cord blood transplant, and haploidentical transplant are also being explored. [24] [25]
Potential barriers to performing allogeneic HSCT
- Alloimmunization due to repetitive transfusions (exchange of blood)
- Organ dysfunction due to SCA (possibly a reason why younger patients do better)
- Lack of matched sibling donors/ insurance.
Indications for performing allogeneic HSCT
- Stroke (most common and strongest indication to perform allogeneic HSCT.
- Abnormal transcranial doppler
- Acute chest syndrome
- Recurrent VOC not controlled with medical therapy or chronic transfusions
The complications with allogeneic HSCT:
- Transplant-related mortality approaches 7 to 10%, comparable with SCD-related mortality
- Graft rejection OR graft failure - less with myeloablative regimens (7 to 11%) compared to non-myeloablative regimens (11 to 50%)
- Graft-versus-host disease and related morbidity
- Transplant-related complications like lung injury, endocrine, and metabolic adverse events
The recent approvals of newer agents and the emergence of gene-editing techniques have expanded the options for SCA patients. Also, extending the benefit of HSCT to low-income countries remains a significant challenge.
Future Perspectives
Gene editing is a new therapy focus whereby researchers attempt to increase the HbF level in patients with SCA. This technique is being developed alongside HSCT. Many approaches to gene editing are in clinical trials right now. [26] [27]
- Viral gene addition using lentivirus: The technique aims to add a modified beta or gamma-globin gene to reduce the HbS component and increase the HbA (beta-globin gene) or the HbF (gamma-globin gene).
- CRISPR (Clustered regularly interspaced short palindromic repeats): Targets the expression of BCL11A, which normally downregulates gamma-globin expression. By introducing insertions and deletions in the BCL11A erythroid lineage-specific enhancer on chromosome 2, BCL11A is downregulated, resulting in increased expression of the gamma-globin gene, which subsequently increases HbF.
Cost Factor
The annual cost of the voxelotor is approximately $125,000. Each vial of crizanlizumab costs approximately $2400, with a yearly cost of $84,852 and $113,136 per year for most patients. The monthly cost of the L-glutamine formulation is $3000 for adults and up to $1000 for the pediatric age group. A myeloablative regimen for HSCT can lead to a cost of approximately $280,000 at 100 days of care/admission. [28] In addition, the advanced level of expertise and dedicated infrastructure required to deliver such care also comes at a considerably high cost. Considering such high costs for the newer therapies, bringing them to lower-income regions like sub-Saharan Africa is a challenge, where approximately 6 million suffer from sickle cell anemia.
Most of the survival data in patients with SCA does not factor in the advent of new medications. The Cooperative Study of Sickle Cell Disease (CSSCD) (between 1978-88) reported the median age of death for women and men as 42 and 48 years, respectively. This study also showed that acute chest syndrome, renal failure, seizures, high leukocyte count, and low levels of HbF were associated with an increased risk of early death in patients with SCA. [29] More recent studies have shown that elevated tricuspid regurgitant jet velocity on echocardiography, prolonged QTc interval, pulmonary hypertension, high N-terminal pro-brain natriuretic peptide, history of asthma and/or wheezing, history of end-stage renal disease requiring dialysis, and the severity of hemolysis are independent risk factors towards early death in patients with SCA. [30]
More recent data combining nine studies from Europe and North America (evaluating 3257 patients) listed the following as predictors of mortality:
- Age (per 10-year increase in age)
- Tricuspid regurgitant jet velocity 2.5 m/s or more
- Reticulocyte count
- Log(N-terminal-pro-brain natriuretic peptide)
- Fetal hemoglobin [30]
With the approval of newer drugs in 2019 (voxelotor and crizanlizumab), increased use of hematopoietic stem cell transplant, and exploring newer techniques like gene therapy, survival is bound to increase along with the quality of life.
- Complications
SCA can lead to acute complications and chronic complications
Acute complications: Most acute complications are associated with occlusion of the small to medium-sized vessels (sometimes large-sized vessels) due to polymerization of HbS and hemolysis.
- Sequestration crises: splenic or hepatic sequestration
- Fat embolism
- Bone infarction/necrosis
- Coagulopathy: increases the risk of both arterial and venous clots- stroke, myocardial infarction, venous thrombosis
- Ophthalmic: vitreous hemorrhage, retinal detachment, retinal artery/vein occlusion
- Aplastic crises: in association with parvovirus infection
- Papillary necrosis
- Delayed growth and development and growth retardation
- Cardiac: cardiomegaly, cardiomyopathy, left ventricular hypertrophy, arrhythmia, congestive heart failure
- Pulmonary: pulmonary edema, sickle cell lung disease, pulmonary hypertension
- Hepatobiliary: Hepatomegaly, intrahepatic cholestasis, cholelithiasis, viral hepatitis
- Splenic complications: splenomegaly, hyposplenia, asplenia
- Renal: acute and chronic renal failure, pyelonephritis, renal medullary carcinoma
- Musculoskeletal: degenerative changes, osteomyelitis, septic arthritis, osteonecrosis, osteopenia/osteoporosis
- Neurologic: aneurysm, mental retardation
- Ophthalmic: proliferative sickle retinopathy, vitreous hemorrhage, retinal detachment, nonproliferative retinal changes
- Endocrine: primary hypogonadism, hypopituitarism, hypothalamic insufficiency
- Iron overload due to repeated transfusions and chronic hemolysis
- Deterrence and Patient Education
SCA is a debilitating disease that affects a patient physically and has significant emotional and psychiatric consequences. The stigma of being diagnosed with SCA has been well documented. Many SCA patients are inaccurately labeled as drug seekers and opioid abusers due to the need for an inordinately high amount of opioids for pain control. In addition, frequent interactions with different providers (in the emergency rooms, hospital admissions, etc.) can lead to inconsistent care. In such a scenario, the patients need to be an advocate for themselves. The following points can act as a guide for patient education.
- Show consistency in outpatient clinics and show up for your appointments. Regularity in visits to your providers helps to build trust within the system.
- Discuss pain requirements for pain medications with your provider with an open mindset- They may appear restrictive in prescribing pain medications, especially opioids. Still, they are trying to help you by protecting you against overdosing.
- Try and use the same emergency room, or at least the ER within the same hospital system. It is useful and helps in developing familiarity with the people who work in that ER. It also allows easy access to your individualized plan of care, which your provider develops for such situations.
- Adherence to disease-modifying therapy will help reduce the events of pain crises and prevent long-term organ damage.
- Always be receptive to alternative ways of getting control over pain - including music therapy, self-hypnosis, and deep muscle relaxation.
- Patients can adopt protective measures- stay warm and avoid exposure to extreme temperatures, adequate hydration, and breathing exercises at home.
- Enhancing Healthcare Team Outcomes
SCA is a systemic disorder that affects the entire body. The disease not only manifests with physical symptoms (pain crises, organ damage, etc.) but also has numerous psycho-social implications. Most patients with SCA belong to the African-American community and a minority to Hispanic and other communities, which makes them prone to certain prejudices. Besides, the high demand for opioids to manage chronic pain makes the situation even more challenging. [31] All providers must keep aside their inherent prejudice when caring for a patient with SCA, working collaboratively as an interprofessional team. Almost all specialties need to be involved in managing patients with SCA. However, the hematology team dedicated to taking care of SCA patients must be the primary physicians for these patients.
Specialties like ophthalmology, orthopedics, psychiatry, gastroenterology, and cardiovascular medicine interact closely with SCA patients. However, this does not diminish the importance of other specialties. Pharmacy and nursing also play a vital role. With the advent of newer drugs and infusions and SCA affecting liver and kidney function, pharmacists and nursing experts are required to ensure safe dosage and medication delivery to the patient.
The data presented here is derived mostly from large and small randomized clinical trials. [Level 1 and 2] Few aspects of care presented here are from cohort and case-control studies. [Level 3]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Sickle Cell Anemia, Hemoglobin C Contributed by Ed Uthman (CC BY 2.0 https://creativecommons.org/licenses/by/2.0)
Disclosure: Ankit Mangla declares no relevant financial relationships with ineligible companies.
Disclosure: Moavia Ehsan declares no relevant financial relationships with ineligible companies.
Disclosure: Nikki Agarwal declares no relevant financial relationships with ineligible companies.
Disclosure: Smita Maruvada declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Mangla A, Ehsan M, Agarwal N, et al. Sickle Cell Anemia. [Updated 2023 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Sickle Cell Trait. [StatPearls. 2024] Sickle Cell Trait. Ashorobi D, Ramsey A, Killeen RB, Bhatt R. StatPearls. 2024 Jan
- Review Potential role of LSD1 inhibitors in the treatment of sickle cell disease: a review of preclinical animal model data. [Am J Physiol Regul Integr Comp...] Review Potential role of LSD1 inhibitors in the treatment of sickle cell disease: a review of preclinical animal model data. Rivers A, Jagadeeswaran R, Lavelle D. Am J Physiol Regul Integr Comp Physiol. 2018 Oct 1; 315(4):R840-R847. Epub 2018 Aug 1.
- Hematopoietic Stem Cell Transplantation in Sickle Cell Disease. [StatPearls. 2024] Hematopoietic Stem Cell Transplantation in Sickle Cell Disease. Ashorobi D, Naha K, Bhatt R. StatPearls. 2024 Jan
- Rheological properties of sickle erythrocytes in patients with sickle-cell anemia: The effect of hydroxyurea, fetal hemoglobin, and α-thalassemia. [Eur J Haematol. 2018] Rheological properties of sickle erythrocytes in patients with sickle-cell anemia: The effect of hydroxyurea, fetal hemoglobin, and α-thalassemia. Ballas SK, Connes P, Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia. Eur J Haematol. 2018 Dec; 101(6):798-803. Epub 2018 Oct 9.
- Review Therapeutic perspective for children and young adults living with thalassemia and sickle cell disease. [Eur J Pediatr. 2023] Review Therapeutic perspective for children and young adults living with thalassemia and sickle cell disease. Ferraresi M, Panzieri DL, Leoni S, Cappellini MD, Kattamis A, Motta I. Eur J Pediatr. 2023 Jun; 182(6):2509-2519. Epub 2023 Mar 31.
Recent Activity
- Sickle Cell Anemia - StatPearls Sickle Cell Anemia - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Carl Zeiss Case Studies
- High-Frequency Deep Sclerotomy A MIGS Procedure for Mild-to-Moderate Glaucoma
- iCare COMPASS Automated Perimeter

- Publications
- Conferences
ASRS 2024: Sickle cell retinopathy and measurements with dynamic OCT angiography
Richard B. Rosen, MD, recipient of the ASRS Founders Award for 2024, discusses his presentation at the meeting
Richard B. Rosen, MD, from the New York Eye and Ear Infirmary of Mount Sinai, received the American Society of Retina Specialists (ASRS) Founders Award at this year's meeting in Stockholm, Sweden. Rosen was given the award for his significant contributions to the advancement of vitreoretinal surgery, treatment, research and patient care.
During the conference, he met with the Eye Care Network to discuss his Founders Lecture, which focused on sickle cell retinopathy, measurement with dynamic OCT angiography and quad-fusion adaptive optics imaging.
Editor's note: The below transcript has been lightly edited for clarity.
Richard B. Rosen, MD, DSc(Hon), FACS, FASRS, FARVO: I'm Richard Rosen from the New York Eye and Ear Infirmary of Mount Sinai. And I presented on sickle cell retinopathy, which we measured with dynamic OCT angiography and quad-fusion adaptive optics imaging. We've developed a technique using dynamic OCT angiography that looks at intermittent perfusion changes in the retina in patients who have sickle cell disease. So, we can actually measure, not only the intensity of the disease, but response to therapy from an individual. So we can see [and] assess exactly how an individual responds to any particular therapy, and what the immediate status of their disease is. And we showed examples using hydroxyurea and also CRISPR stem cell therapy.
In the study that I reported, we looked at approximately 74 patients, 54 of them were patients with various types of sickle cell disease. There were patients who had different varieties, genotypes from sickle traits to sickle SC and sickle cell anemia SS. And we compare that to age match-race match controls, to see what was the incidence of these intermittent occlusive events that occur very commonly with sickle cell disease. Particular outcomes were in terms of the number of these events that would occur within a particular area, looking both around the fovea and temporal to the fovea.
I think the takeaway is, using dynamic OCT angiography we can assess non-invasively what the impact of therapy is in patients. We're currently doing a large study sponsored by the National Institute of Health looking at what is the impact of–first in patients who are asymptomatic what their particular condition is, then what is the impact for various therapies that we're giving these patients to see how they respond, particularly now that a lot of new therapies for sickle cell disease have become available. Most recently, the FDA has approved stem cell therapy. So we'll be looking at those patients as well.

Kiora Pharmaceuticals receives Orphan Medicinal Product Designation for KIO-301
The EMA issued a designation for the small molecule photoswitch, which targets inherited retinal diseases including retinitis pigmentosa

PHOTON Results and Their Relation to DME Patients in Your Practice
John Kitchens, MD, is joined by Diana Do, MD, to discuss the PHOTON trial results and their relation to patients with diabetic macular oedema in clinical practice.

Novaliq receives positive CHMP opinion for Vevizye in treatment of dry eye disease
The positive opinion comes with the recommendation that ciclosporin 0.1% be granted marketing authorisation in the European Union

PULSAR Results and Their Relation to nAMD Patients in Your Practice
John Kitchens, MD, is joined by David Brown, MD, to discuss the PULSAR study results and their relation to patients with neovascular age-related macular degeneration in clinical practice.

Alopecia areata and underlying corneal pathologies
Investigators conducted a case-control study to investigate the corneal topography parameters and biomechanics in patients with alopecia areata

Impact report highlights outcomes of Moorfields Eye Charity programmes
The organisation has secured £72.75 million for its new eye health centre
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

IMAGES
VIDEO
COMMENTS
Dactylitis, often referred to as hand-foot syndrome, is frequently the 1st manifestation of pain in children with sickle cell anemia, occurring in 50% of children by 2 years of age. [ 5] A 3.5-year-old girl from race of Arab reffered to Shafa Hospital with severe anemia, thrombocytopenia, leucocytosis and elevated ESR and LDH.
On examination the child had mild splenomegaly. He had history of two prior hospital admissions. First at the age of 1 year, when he was diagnosed to have pneumonia and second, at the age of 3 years (3 months prior to coming to our institution) for fever, anemia and jaundice. He has had three transfusions till now, last transfusion was 3 months ...
Explanation. The incidence of primary stroke in children with SCD is 0.6 to 0.8 events per 100 patient-years, with a cumulative incidence of 7.8 percent by age 14 years in the Jamaican cohort and 11 percent by age 20 years in the U.S. Cooperative Study of Sickle Cell Disease. Once stroke has occurred, the incidence of recurrent (secondary ...
Sickle cell disease (SCD) is a common group of life-threatening, genetic disorders caused by the synthesis of abnormal hemoglobin (sickle hemoglobin), which when deoxygenated, polymerizes and causes sickling of red blood cells. SCD is characterized by chronic hemolytic anemia, vasoocclusion, and progressive vascular injury causing multiorgan ...
Sickle cell disease (SCD) refers to a group of hereditary disorders that result in faulty hemoglobin carriage by the red blood cells. This paper discusses an atypical presentation of SCD in early infancy. Despite current literature suggesting protection by fetal hemoglobin in the first few months of life, we report a diagnosis of SCD at 2 ...
Nurse Maggie works in a pediatric hematology unit and is caring for Marcus, a 9-year-old with a history of sickle cell disease who was admitted for a vaso-occlusive crisis, or VOC. After settling Marcus in his room, Nurse Maggie goes through the steps of the Clinical Judgment Measurement Model to make clinical decisions about Marcus' care by ...
Sickle Cell Anemia Case Study. Case Presentation. Dominique Jones is a 17-year-old young woman who was diagnosed with sickle cell disease after she was born. Her siblings, George (15) and Sadie (10), also have the disease but neither of her parents do.
MADHURI SHENDE. Sickle cell disease (SCD) is a genetic disorder that affects erythrocytes (RBCs) causing them to become sickle or crescent shaped. The effects of this condition due to an abnormality of the hemoglobin molecules found in erythrocytes. The substitution of one amino acid in the hemoglobin molecule results in sickle hemoglobin.
Sickle Cell Disease • In the United States, it's estimated that sickle cell anemia affects around 50,000 people, mainly African Americans. The disease occurs in about 1 out of every 700 African American births. • Before the era of Hydroxyurea, the average life expectancy was in the 40's.
Sickle cell disease (SCD) is a monogenetic disorder due to a single base-pair point mutation in the β-globin gene resulting in the substitution of the amino acid valine for glutamic acid in the β-globin chain. Phenotypic variation in the clinical presentation and disease outcome is a characteristic feature of the disorder.
Blood and stool cultures remained negative. Hemoglobin electrophoresis confirmed the diagnosis of sickle cell disease (HbA2 2.7%, HbF 24.1%, and HbS 73%). The initial wrong diagnosis (doctor's delays) by not recognizing sickle cell disease despite high risk based on ethnicity and VOC and the high HbF were responsible for the late diagnosis. 2.3.
Sickle Cell Anemia Presentation. Free Google Slides theme, PowerPoint template, and Canva presentation template. There was a French cartoon that was very popular in Spain many years ago, and it told kids how the human body works, in a way that they can understand. The main characters were red blood cells, and we wouldn't be able to picture them ...
In sickle cell anemia, a lower-than-normal number of red blood cells occurs because sickle cells don't last very long. Sickle cells die faster than normal red blood cells, usually after only about 10 to 20 days. The bone marrow can't make new red blood cells fast enough to replace the dying ones. The result is anemia.
The case explores the initial presentation of sickle cell symptoms in a heterozygote, the assembly of a pedigree and calculation of genetic risk for transmission of the mutation, and the biochemical and genetic testing options that are available for diagnostic and preconception genetic testing in sickle cell disease. This case also covers the ...
Sickle cell disease (SCD) refers to a group of hemoglobinopathies that include mutations in the gene encoding the beta subunit of hemoglobin. The first description of SCA 'like' disorder was provided by Dr. Africanus Horton in his book The Disease of Tropical Climates and their treatment (1872). However, it was not until 1910 when Dr. James B Herrick and Dr. Ernest Irons reported noticing ...
We report the first documented case of a 9-year-old boy with sickle cell disease, presenting with fever, cough, and shortness of breath, diagnosed to have acute chest syndrome and coronavirus disease 2019 (COVID-19) pneumonia with inflammatory storm requiring ventilation, exchange blood transfusion, immunomodulatory agents, and prophylactic ...
And we showed examples using hydroxyurea and also CRISPR stem cell therapy. In the study that I reported, we looked at approximately 74 patients, 54 of them were patients with various types of sickle cell disease. There were patients who had different varieties, genotypes from sickle traits to sickle SC and sickle cell anemia SS.