Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 76, Issue 2
- COVID-19 pandemic and its impact on social relationships and health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1512-4471 Emily Long 1 ,
- Susan Patterson 1 ,
- Karen Maxwell 1 ,
- Carolyn Blake 1 ,
- http://orcid.org/0000-0001-7342-4566 Raquel Bosó Pérez 1 ,
- Ruth Lewis 1 ,
- Mark McCann 1 ,
- Julie Riddell 1 ,
- Kathryn Skivington 1 ,
- Rachel Wilson-Lowe 1 ,
- http://orcid.org/0000-0002-4409-6601 Kirstin R Mitchell 2
- 1 MRC/CSO Social and Public Health Sciences Unit , University of Glasgow , Glasgow , UK
- 2 MRC/CSO Social and Public Health Sciences Unit, Institute of Health & Wellbeing , University of Glasgow , Glasgow , UK
- Correspondence to Dr Emily Long, MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, Glasgow G3 7HR, UK; emily.long{at}glasgow.ac.uk
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the nature of the public health response. We then introduce four distinct domains of social relationships: social networks, social support, social interaction and intimacy, highlighting the mechanisms through which the pandemic and associated public health response drastically altered social interactions in each domain. Throughout the essay, the lens of health inequalities, and perspective of relationships as interconnecting elements in a broader system, is used to explore the varying impact of these disruptions. The essay concludes by providing recommendations for longer term recovery ensuring that the social relational cost of COVID-19 is adequately considered in efforts to rebuild.
- inequalities
Data availability statement
Data sharing not applicable as no data sets generated and/or analysed for this study. Data sharing not applicable as no data sets generated or analysed for this essay.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/jech-2021-216690
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Infectious disease pandemics, including SARS and COVID-19, demand intrapersonal behaviour change and present highly complex challenges for public health. 1 A pandemic of an airborne infection, spread easily through social contact, assails human relationships by drastically altering the ways through which humans interact. In this essay, we draw on theories of social relationships to examine specific ways in which relational mechanisms key to health and well-being were disrupted by the COVID-19 pandemic. Relational mechanisms refer to the processes between people that lead to change in health outcomes.
At the time of writing, the future surrounding COVID-19 was uncertain. Vaccine programmes were being rolled out in countries that could afford them, but new and more contagious variants of the virus were also being discovered. The recovery journey looked long, with continued disruption to social relationships. The social cost of COVID-19 was only just beginning to emerge, but the mental health impact was already considerable, 2 3 and the inequality of the health burden stark. 4 Knowledge of the epidemiology of COVID-19 accrued rapidly, but evidence of the most effective policy responses remained uncertain.
The initial response to COVID-19 in the UK was reactive and aimed at reducing mortality, with little time to consider the social implications, including for interpersonal and community relationships. The terminology of ‘social distancing’ quickly became entrenched both in public and policy discourse. This equation of physical distance with social distance was regrettable, since only physical proximity causes viral transmission, whereas many forms of social proximity (eg, conversations while walking outdoors) are minimal risk, and are crucial to maintaining relationships supportive of health and well-being.
The aim of this essay is to explore four key relational mechanisms that were impacted by the pandemic and associated restrictions: social networks, social support, social interaction and intimacy. We use relational theories and emerging research on the effects of the COVID-19 pandemic response to make three key recommendations: one regarding public health responses; and two regarding social recovery. Our understanding of these mechanisms stems from a ‘systems’ perspective which casts social relationships as interdependent elements within a connected whole. 5
Social networks
Social networks characterise the individuals and social connections that compose a system (such as a workplace, community or society). Social relationships range from spouses and partners, to coworkers, friends and acquaintances. They vary across many dimensions, including, for example, frequency of contact and emotional closeness. Social networks can be understood both in terms of the individuals and relationships that compose the network, as well as the overall network structure (eg, how many of your friends know each other).
Social networks show a tendency towards homophily, or a phenomenon of associating with individuals who are similar to self. 6 This is particularly true for ‘core’ network ties (eg, close friends), while more distant, sometimes called ‘weak’ ties tend to show more diversity. During the height of COVID-19 restrictions, face-to-face interactions were often reduced to core network members, such as partners, family members or, potentially, live-in roommates; some ‘weak’ ties were lost, and interactions became more limited to those closest. Given that peripheral, weaker social ties provide a diversity of resources, opinions and support, 7 COVID-19 likely resulted in networks that were smaller and more homogenous.
Such changes were not inevitable nor necessarily enduring, since social networks are also adaptive and responsive to change, in that a disruption to usual ways of interacting can be replaced by new ways of engaging (eg, Zoom). Yet, important inequalities exist, wherein networks and individual relationships within networks are not equally able to adapt to such changes. For example, individuals with a large number of newly established relationships (eg, university students) may have struggled to transfer these relationships online, resulting in lost contacts and a heightened risk of social isolation. This is consistent with research suggesting that young adults were the most likely to report a worsening of relationships during COVID-19, whereas older adults were the least likely to report a change. 8
Lastly, social connections give rise to emergent properties of social systems, 9 where a community-level phenomenon develops that cannot be attributed to any one member or portion of the network. For example, local area-based networks emerged due to geographic restrictions (eg, stay-at-home orders), resulting in increases in neighbourly support and local volunteering. 10 In fact, research suggests that relationships with neighbours displayed the largest net gain in ratings of relationship quality compared with a range of relationship types (eg, partner, colleague, friend). 8 Much of this was built from spontaneous individual interactions within local communities, which together contributed to the ‘community spirit’ that many experienced. 11 COVID-19 restrictions thus impacted the personal social networks and the structure of the larger networks within the society.
Social support
Social support, referring to the psychological and material resources provided through social interaction, is a critical mechanism through which social relationships benefit health. In fact, social support has been shown to be one of the most important resilience factors in the aftermath of stressful events. 12 In the context of COVID-19, the usual ways in which individuals interact and obtain social support have been severely disrupted.
One such disruption has been to opportunities for spontaneous social interactions. For example, conversations with colleagues in a break room offer an opportunity for socialising beyond one’s core social network, and these peripheral conversations can provide a form of social support. 13 14 A chance conversation may lead to advice helpful to coping with situations or seeking formal help. Thus, the absence of these spontaneous interactions may mean the reduction of indirect support-seeking opportunities. While direct support-seeking behaviour is more effective at eliciting support, it also requires significantly more effort and may be perceived as forceful and burdensome. 15 The shift to homeworking and closure of community venues reduced the number of opportunities for these spontaneous interactions to occur, and has, second, focused them locally. Consequently, individuals whose core networks are located elsewhere, or who live in communities where spontaneous interaction is less likely, have less opportunity to benefit from spontaneous in-person supportive interactions.
However, alongside this disruption, new opportunities to interact and obtain social support have arisen. The surge in community social support during the initial lockdown mirrored that often seen in response to adverse events (eg, natural disasters 16 ). COVID-19 restrictions that confined individuals to their local area also compelled them to focus their in-person efforts locally. Commentators on the initial lockdown in the UK remarked on extraordinary acts of generosity between individuals who belonged to the same community but were unknown to each other. However, research on adverse events also tells us that such community support is not necessarily maintained in the longer term. 16
Meanwhile, online forms of social support are not bound by geography, thus enabling interactions and social support to be received from a wider network of people. Formal online social support spaces (eg, support groups) existed well before COVID-19, but have vastly increased since. While online interactions can increase perceived social support, it is unclear whether remote communication technologies provide an effective substitute from in-person interaction during periods of social distancing. 17 18 It makes intuitive sense that the usefulness of online social support will vary by the type of support offered, degree of social interaction and ‘online communication skills’ of those taking part. Youth workers, for instance, have struggled to keep vulnerable youth engaged in online youth clubs, 19 despite others finding a positive association between amount of digital technology used by individuals during lockdown and perceived social support. 20 Other research has found that more frequent face-to-face contact and phone/video contact both related to lower levels of depression during the time period of March to August 2020, but the negative effect of a lack of contact was greater for those with higher levels of usual sociability. 21 Relatedly, important inequalities in social support exist, such that individuals who occupy more socially disadvantaged positions in society (eg, low socioeconomic status, older people) tend to have less access to social support, 22 potentially exacerbated by COVID-19.
Social and interactional norms
Interactional norms are key relational mechanisms which build trust, belonging and identity within and across groups in a system. Individuals in groups and societies apply meaning by ‘approving, arranging and redefining’ symbols of interaction. 23 A handshake, for instance, is a powerful symbol of trust and equality. Depending on context, not shaking hands may symbolise a failure to extend friendship, or a failure to reach agreement. The norms governing these symbols represent shared values and identity; and mutual understanding of these symbols enables individuals to achieve orderly interactions, establish supportive relationship accountability and connect socially. 24 25
Physical distancing measures to contain the spread of COVID-19 radically altered these norms of interaction, particularly those used to convey trust, affinity, empathy and respect (eg, hugging, physical comforting). 26 As epidemic waves rose and fell, the work to negotiate these norms required intense cognitive effort; previously taken-for-granted interactions were re-examined, factoring in current restriction levels, own and (assumed) others’ vulnerability and tolerance of risk. This created awkwardness, and uncertainty, for example, around how to bring closure to an in-person interaction or convey warmth. The instability in scripted ways of interacting created particular strain for individuals who already struggled to encode and decode interactions with others (eg, those who are deaf or have autism spectrum disorder); difficulties often intensified by mask wearing. 27
Large social gatherings—for example, weddings, school assemblies, sporting events—also present key opportunities for affirming and assimilating interactional norms, building cohesion and shared identity and facilitating cooperation across social groups. 28 Online ‘equivalents’ do not easily support ‘social-bonding’ activities such as singing and dancing, and rarely enable chance/spontaneous one-on-one conversations with peripheral/weaker network ties (see the Social networks section) which can help strengthen bonds across a larger network. The loss of large gatherings to celebrate rites of passage (eg, bar mitzvah, weddings) has additional relational costs since these events are performed by and for communities to reinforce belonging, and to assist in transitioning to new phases of life. 29 The loss of interaction with diverse others via community and large group gatherings also reduces intergroup contact, which may then tend towards more prejudiced outgroup attitudes. While online interaction can go some way to mimicking these interaction norms, there are key differences. A sense of anonymity, and lack of in-person emotional cues, tends to support norms of polarisation and aggression in expressing differences of opinion online. And while online platforms have potential to provide intergroup contact, the tendency of much social media to form homogeneous ‘echo chambers’ can serve to further reduce intergroup contact. 30 31
Intimacy relates to the feeling of emotional connection and closeness with other human beings. Emotional connection, through romantic, friendship or familial relationships, fulfils a basic human need 32 and strongly benefits health, including reduced stress levels, improved mental health, lowered blood pressure and reduced risk of heart disease. 32 33 Intimacy can be fostered through familiarity, feeling understood and feeling accepted by close others. 34
Intimacy via companionship and closeness is fundamental to mental well-being. Positively, the COVID-19 pandemic has offered opportunities for individuals to (re)connect and (re)strengthen close relationships within their household via quality time together, following closure of many usual external social activities. Research suggests that the first full UK lockdown period led to a net gain in the quality of steady relationships at a population level, 35 but amplified existing inequalities in relationship quality. 35 36 For some in single-person households, the absence of a companion became more conspicuous, leading to feelings of loneliness and lower mental well-being. 37 38 Additional pandemic-related relational strain 39 40 resulted, for some, in the initiation or intensification of domestic abuse. 41 42
Physical touch is another key aspect of intimacy, a fundamental human need crucial in maintaining and developing intimacy within close relationships. 34 Restrictions on social interactions severely restricted the number and range of people with whom physical affection was possible. The reduction in opportunity to give and receive affectionate physical touch was not experienced equally. Many of those living alone found themselves completely without physical contact for extended periods. The deprivation of physical touch is evidenced to take a heavy emotional toll. 43 Even in future, once physical expressions of affection can resume, new levels of anxiety over germs may introduce hesitancy into previously fluent blending of physical and verbal intimate social connections. 44
The pandemic also led to shifts in practices and norms around sexual relationship building and maintenance, as individuals adapted and sought alternative ways of enacting sexual intimacy. This too is important, given that intimate sexual activity has known benefits for health. 45 46 Given that social restrictions hinged on reducing household mixing, possibilities for partnered sexual activity were primarily guided by living arrangements. While those in cohabiting relationships could potentially continue as before, those who were single or in non-cohabiting relationships generally had restricted opportunities to maintain their sexual relationships. Pornography consumption and digital partners were reported to increase since lockdown. 47 However, online interactions are qualitatively different from in-person interactions and do not provide the same opportunities for physical intimacy.
Recommendations and conclusions
In the sections above we have outlined the ways in which COVID-19 has impacted social relationships, showing how relational mechanisms key to health have been undermined. While some of the damage might well self-repair after the pandemic, there are opportunities inherent in deliberative efforts to build back in ways that facilitate greater resilience in social and community relationships. We conclude by making three recommendations: one regarding public health responses to the pandemic; and two regarding social recovery.
Recommendation 1: explicitly count the relational cost of public health policies to control the pandemic
Effective handling of a pandemic recognises that social, economic and health concerns are intricately interwoven. It is clear that future research and policy attention must focus on the social consequences. As described above, policies which restrict physical mixing across households carry heavy and unequal relational costs. These include for individuals (eg, loss of intimate touch), dyads (eg, loss of warmth, comfort), networks (eg, restricted access to support) and communities (eg, loss of cohesion and identity). Such costs—and their unequal impact—should not be ignored in short-term efforts to control an epidemic. Some public health responses—restrictions on international holiday travel and highly efficient test and trace systems—have relatively small relational costs and should be prioritised. At a national level, an earlier move to proportionate restrictions, and investment in effective test and trace systems, may help prevent escalation of spread to the point where a national lockdown or tight restrictions became an inevitability. Where policies with relational costs are unavoidable, close attention should be paid to the unequal relational impact for those whose personal circumstances differ from normative assumptions of two adult families. This includes consideration of whether expectations are fair (eg, for those who live alone), whether restrictions on social events are equitable across age group, religious/ethnic groupings and social class, and also to ensure that the language promoted by such policies (eg, households; families) is not exclusionary. 48 49 Forethought to unequal impacts on social relationships should thus be integral to the work of epidemic preparedness teams.
Recommendation 2: intelligently balance online and offline ways of relating
A key ingredient for well-being is ‘getting together’ in a physical sense. This is fundamental to a human need for intimate touch, physical comfort, reinforcing interactional norms and providing practical support. Emerging evidence suggests that online ways of relating cannot simply replace physical interactions. But online interaction has many benefits and for some it offers connections that did not exist previously. In particular, online platforms provide new forms of support for those unable to access offline services because of mobility issues (eg, older people) or because they are geographically isolated from their support community (eg, lesbian, gay, bisexual, transgender and queer (LGBTQ) youth). Ultimately, multiple forms of online and offline social interactions are required to meet the needs of varying groups of people (eg, LGBTQ, older people). Future research and practice should aim to establish ways of using offline and online support in complementary and even synergistic ways, rather than veering between them as social restrictions expand and contract. Intelligent balancing of online and offline ways of relating also pertains to future policies on home and flexible working. A decision to switch to wholesale or obligatory homeworking should consider the risk to relational ‘group properties’ of the workplace community and their impact on employees’ well-being, focusing in particular on unequal impacts (eg, new vs established employees). Intelligent blending of online and in-person working is required to achieve flexibility while also nurturing supportive networks at work. Intelligent balance also implies strategies to build digital literacy and minimise digital exclusion, as well as coproducing solutions with intended beneficiaries.
Recommendation 3: build stronger and sustainable localised communities
In balancing offline and online ways of interacting, there is opportunity to capitalise on the potential for more localised, coherent communities due to scaled-down travel, homeworking and local focus that will ideally continue after restrictions end. There are potential economic benefits after the pandemic, such as increased trade as home workers use local resources (eg, coffee shops), but also relational benefits from stronger relationships around the orbit of the home and neighbourhood. Experience from previous crises shows that community volunteer efforts generated early on will wane over time in the absence of deliberate work to maintain them. Adequately funded partnerships between local government, third sector and community groups are required to sustain community assets that began as a direct response to the pandemic. Such partnerships could work to secure green spaces and indoor (non-commercial) meeting spaces that promote community interaction. Green spaces in particular provide a triple benefit in encouraging physical activity and mental health, as well as facilitating social bonding. 50 In building local communities, small community networks—that allow for diversity and break down ingroup/outgroup views—may be more helpful than the concept of ‘support bubbles’, which are exclusionary and less sustainable in the longer term. Rigorously designed intervention and evaluation—taking a systems approach—will be crucial in ensuring scale-up and sustainability.
The dramatic change to social interaction necessitated by efforts to control the spread of COVID-19 created stark challenges but also opportunities. Our essay highlights opportunities for learning, both to ensure the equity and humanity of physical restrictions, and to sustain the salutogenic effects of social relationships going forward. The starting point for capitalising on this learning is recognition of the disruption to relational mechanisms as a key part of the socioeconomic and health impact of the pandemic. In recovery planning, a general rule is that what is good for decreasing health inequalities (such as expanding social protection and public services and pursuing green inclusive growth strategies) 4 will also benefit relationships and safeguard relational mechanisms for future generations. Putting this into action will require political will.
Ethics statements
Patient consent for publication.
Not required.
- Office for National Statistics (ONS)
- Ford T , et al
- Riordan R ,
- Ford J , et al
- Glonti K , et al
- McPherson JM ,
- Smith-Lovin L
- Granovetter MS
- Fancourt D et al
- Stadtfeld C
- Office for Civil Society
- Cook J et al
- Rodriguez-Llanes JM ,
- Guha-Sapir D
- Patulny R et al
- Granovetter M
- Winkeler M ,
- Filipp S-H ,
- Kaniasty K ,
- de Terte I ,
- Guilaran J , et al
- Wright KB ,
- Martin J et al
- Gabbiadini A ,
- Baldissarri C ,
- Durante F , et al
- Sommerlad A ,
- Marston L ,
- Huntley J , et al
- Turner RJ ,
- Bicchieri C
- Brennan G et al
- Watson-Jones RE ,
- Amichai-Hamburger Y ,
- McKenna KYA
- Page-Gould E ,
- Aron A , et al
- Pietromonaco PR ,
- Timmerman GM
- Bradbury-Jones C ,
- Mikocka-Walus A ,
- Klas A , et al
- Marshall L ,
- Steptoe A ,
- Stanley SM ,
- Campbell AM
- ↵ (ONS), O.f.N.S., Domestic abuse during the coronavirus (COVID-19) pandemic, England and Wales . Available: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/domesticabuseduringthecoronaviruscovid19pandemicenglandandwales/november2020
- Rosenberg M ,
- Hensel D , et al
- Banerjee D ,
- Bruner DW , et al
- Bavel JJV ,
- Baicker K ,
- Boggio PS , et al
- van Barneveld K ,
- Quinlan M ,
- Kriesler P , et al
- Mitchell R ,
- de Vries S , et al
Twitter @karenmaxSPHSU, @Mark_McCann, @Rwilsonlowe, @KMitchinGlasgow
Contributors EL and KM led on the manuscript conceptualisation, review and editing. SP, KM, CB, RBP, RL, MM, JR, KS and RW-L contributed to drafting and revising the article. All authors assisted in revising the final draft.
Funding The research reported in this publication was supported by the Medical Research Council (MC_UU_00022/1, MC_UU_00022/3) and the Chief Scientist Office (SPHSU11, SPHSU14). EL is also supported by MRC Skills Development Fellowship Award (MR/S015078/1). KS and MM are also supported by a Medical Research Council Strategic Award (MC_PC_13027).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Physics Magazine
- Physical Review Journals
- Physics Today
- Other APS Publications
- March Meeting
- April Meeting
- Meeting Calendar
- Abstract Submission
- Meeting Archive
- Policies & Guidelines
- International Affairs
- Public Engagement
- Women in Physics
- Minorities in Physics
- LGBT Physicists
- Industrial Physics
- Renew Membership
- Member Directory
- My Member Profile
- Member Services
- APS Chapters
- Action Center
- Reports & Studies
- APS Statements
- Contact APS Government Affairs
- Physics Jobs
- Becoming a Physicist
- Career Guidance
- Tools for Career Advisors
- Statistical Data
- News & Announcements
- Press Releases
- Social Media
- Mission, Vision, Values
- Strategic Plan
- Society Governance
- Society History
- Donate to APS
- Become a Member
July/August 2020 (Volume 29, Number 7)
Defending my phd thesis in the time of the coronavirus.
By Danielle Sofferman
Ten years ago I attended the Conference for Undergraduate Women in Physics (CUWiP). Once I returned to my undergrad institution, at Adelphi University, I was ecstatic and eager to do research. This experience led me to become more involved in presenting at conferences and taking a Research Experience for Undergraduates (REU) at the University of Michigan (U of M) that ultimately led me to pursue a PhD at U of M. Little did I know how the completion of my degree would unfold. In March 2020 the entire country was brought into a chaotic state where the number of COVID-19 cases were beginning to spike, businesses were forced to close and people were scrambling to stock up with as many rolls of toilet paper as possible. In the middle of this mess, I only had two more months until my PhD defense.
During my PhD studies, I worked with a home-built femtosecond Ti-Sapphire laser system that was used to create ultrafast pulses for broadband transient absorption (TA) spectroscopy of molecules in the ultraviolet-visible region. This technique involves a two-pulse sequence, where one pulse (272 nm) optically excites and another pulse (250–650 nm) probes the dynamics of the molecules after certain time delays. More specifically my studies explored the initial dynamics involved in vitamin D3 formation in simple skin membrane models during the first 500 picoseconds after excitation. The ultimate goal was to investigate the photochemistry involved in vitamin D3 formation as a function of lipid membrane parameters, such as lipid tail length, hydrogen bonding, and van der Waals interactions.
After restless days and nights of trying to maintain a stable laser system and collect data, I wanted to make my defense day even more memorable. But I never expected that it would turn out like this: it was held in the middle of a pandemic that will forever trigger memories of writing and defending my thesis. Within the months prior to the pandemic, I imagined my defense to be in the fanciest room on campus and I would provide my audience with a chocolate fountain and marshmallows next to an ice sculpture of a vitamin D3 molecule. However, those ideas quickly vanished as the COVID-19 pandemic forced my defense to be held remotely.

Danielle Sofferman
The defense took place through the BlueJeans video conference system. Instead of being in a room filled with curious eyes and chocolate covered mouths, I was in a video meeting where I felt as if I was just talking to my PowerPoint because the meeting screen was too small to display everyone that had their camera unblocked. My camera was also off until the end where I gave the acknowledgments and answered questions. I did this to narrow the connection bandwidth and to secretly refer to notes to each of the slides. The window that showed the meeting sat in the corner of my most current slide, and it blocked some of my figures. With only a single monitor, I was forced to minimize the meeting app while I spoke. My audience listened with their microphones muted to minimize the background noise and did not interrupt during the presentation. Since I wasn’t able to view my audience, the actual presentation felt more like a practice run and it wasn’t until the very last slide, where I gave my acknowledgments that the talk felt like the real thing. While my blocked camera didn’t prevent other computer glitches and new BlueJeans users from sending me permission notifications to switch who shared the screen, it did prevent showing my worried facial expressions when my PowerPoint, for some unknown reason froze multiple times. Since this was actually a real talk and not a practice, the multiple computer glitches made me feel like I was further being initiated into the world of professional physics research.
The grand finale, when I presented the most significant parts of my research also lined up with the time when the Blue Angels, honoring all the front line workers, flew directly over me on their way to Detroit. At the end of the talk, the smiles from friends, family and visual satisfactory nods from my PhD committee were lost as most people just sent “clap“ emojis and other appraisal messages through the chat window. My advisor then asked if there were any questions, the 15–30 seconds of silence felt like an eternity as I patiently waited for someone to ask anything they wanted about my research. My former labmate was the only one that asked a question. The back and forth felt similar to virtually teaching (due to the pandemic) the Math Methods discussion section that I was a Graduate Student Instructor (GSI) for during the past term: trying to answer a question as completely as possible while also trying to figure out who was asking the question. Now, while I didn’t get the room setup that I imagined and lost the visual interaction with my audience, the virtual setup did allow me to invite people from outside of Michigan who otherwise would have not been able to attend.
As I start to close another successful chapter in my career, my future is just as exciting as it terrifying. The COVID-19 pandemic has slowed down my job search and left behind a trail of canceled interviews. However, in these uncertain times I am confident that my future is brighter than the strongest pump laser that I have been working with, ~15 watts of 527 nm light, and that’s VERY bright!
Danielle Sofferman graduated Magna Cum Laude from Adelphi University in 2013. Historically Adelphi’s undergraduate population (~5,000 students) is mostly female (70% as of 2019), however the ratio of female to male students is dramatically switched in the physics department. During the 2013 graduation year, she was the only woman to graduate with a physics degree. She spent more than half of her undergraduate career studying the nonlinear optical properties of cadmium selenide (CdSe) quantum dots. She also collaborated with Eugene Hecht on writing Schaum’s Outline of College Physics, Eleventh edition, where she is acknowledged in the book. As a graduate student in the Applied Physics Program at The University of Michigan, Danielle continued with her passion for optics by working in an ultra-fast spectroscopy lab, researching how the human skin membrane influences the initial photochemistry involved in vitamin D3 formation, where the initial reactions occur on the timescale of picoseconds. She has now successfully completed her PhD in the Applied Physics Program and is searching for her next adventure. (Contact: [email protected] )
©1995 - 2024, AMERICAN PHYSICAL SOCIETY APS encourages the redistribution of the materials included in this newspaper provided that attribution to the source is noted and the materials are not truncated or changed.
Editor: David Voss Staff Science Writer: Leah Poffenberger Contributing Correspondent: Alaina G. Levine Publication Designer and Production: Nancy Bennett-Karasik
APS News Home
Issue Table of Contents
APS News Archives
Contact APS News Editor
Become an APS Member Submit a Meeting Abstract Submit a Manuscript Find a Journal Article Donate to APS
Renew Membership Join an APS Unit Update Contact Information
Information for
Librarians Authors Referees Media Students
The American Physical Society (APS) is a nonprofit membership organization working to advance the knowledge of physics.
© 2024 American Physical Society | Privacy Policy | Contact Us 1 Physics Ellipse, College Park, MD 20740-3844 | (301) 209-3200
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 10, Issue 12
- Impact of the COVID-19 pandemic on mental health and well-being of communities: an exploratory qualitative study protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-0180-0213 Anam Shahil Feroz 1 , 2 ,
- Naureen Akber Ali 3 ,
- Noshaba Akber Ali 1 ,
- Ridah Feroz 4 ,
- Salima Nazim Meghani 1 ,
- Sarah Saleem 1
- 1 Community Health Sciences , Aga Khan University , Karachi , Pakistan
- 2 Institute of Health Policy, Management and Evaluation , University of Toronto , Toronto , Ontario , Canada
- 3 School of Nursing and Midwifery , Aga Khan University , Karachi , Pakistan
- 4 Aga Khan University Institute for Educational Development , Karachi , Pakistan
- Correspondence to Ms Anam Shahil Feroz; anam.sahyl{at}gmail.com
Introduction The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. In addition, with the widespread use of social media, rumours, myths and inaccurate information about the virus are spreading rapidly, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes of community members towards COVID-19 and its impact on their daily lives and mental well-being.
Methods and analysis This formative research will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews with community members. The study will be conducted in the Karimabad Federal B Area and in the Garden (East and West) community settings in Karachi, Pakistan. The community members of these areas have been selected purposively for the interview. Study data will be analysed thematically using NVivo V.12 Plus software.
Ethics and dissemination Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The results of the study will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
- mental health
- public health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-041641
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The mental health impact of the COVID-19 pandemic is likely to last much longer than the physical health impact, and this study is positioned well to explore the perceptions and attitudes of community members towards the pandemic and its impact on their daily lives and mental well-being.
This study will guide the development of context-specific innovative mental health programmes to support communities in the future.
One limitation is that to minimise the risk of infection all study respondents will be interviewed online over Zoom and hence the authors will not have the opportunity to build rapport with the respondents or obtain non-verbal cues during interviews.
The COVID-19 pandemic has affected almost 180 countries since it was first detected in Wuhan, China in December 2019. 1 2 The COVID-19 outbreak has been declared a public health emergency of international concern by the WHO. 3 The WHO estimates the global mortality to be about 3.4% 4 ; however, death rates vary between countries and across age groups. 5 In Pakistan, a total of 10 880 cases and 228 deaths due to COVID-19 infection have been reported to date. 6
The worldwide COVID-19 pandemic has not only incurred massive challenges to the global supply chains and healthcare systems but also has a detrimental effect on the overall health of individuals. 7 The pandemic has led to lockdowns and has created destructive impact on the societies at large. Most company employees, including daily wage workers, have been prohibited from going to their workplaces or have been asked to work from home, which has caused job-related insecurities and financial crises in the communities. 8 Educational institutions and training centres have also been closed, which resulted in children losing their routine of going to schools, studying and socialising with their peers. Delay in examinations is likewise a huge stressor for students. 8 Alongside this, parents have been struggling with creating a structured milieu for their children. 9 COVID-19 has hindered the normal routine life of every individual, be it children, teenagers, adults or the elderly. The crisis is engendering burden throughout populations and communities, particularly in developing countries such as Pakistan which face major challenges due to fragile healthcare systems and poor economic structures. 10
The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. 8 Further, the highly contagious nature of COVID-19 has also escalated confusion, fear and panic among community residents. Moreover, social distancing is often an unpleasant experience for community members and for patients as it adds to mental suffering, particularly in the local setting where get-togethers with friends and families are a major source of entertainment. 9 Recent studies also showed that individuals who are following social distancing rules experience loneliness, causing a substantial level of distress in the form of anxiety, stress, anger, misperception and post-traumatic stress symptoms. 8 11 Separation from family members, loss of autonomy, insecurity over disease status, inadequate supplies, inadequate information, financial loss, frustration, stigma and boredom are all major stressors that can create drastic impact on an individual’s life. 11 Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. 12 With the widespread use of social media, 13 rumours, myths and inaccurate information about COVID-19 are also spreading rapidly, not only among adults but are also carried on to children, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. 9 The psychological symptoms associated with COVID-19 at the community level are also manifested as anxiety-driven panic buying, resulting in exhaustion of resources from the market. 14 Some level of panic also dwells in the community due to the unavailability of essential protective equipment, particularly masks and sanitisers. 15 Similarly, mental health issues, including depression, anxiety, panic attacks, psychotic symptoms and even suicide, were reported during the early severe acute respiratory syndrome outbreak. 16 17 COVID-19 is likely posing a similar risk throughout the world. 12
The fear of transmitting the disease or a family member falling ill is a probable mental function of human nature, but at some point the psychological fear of the disease generates more anxiety than the disease itself. Therefore, mental health problems are likely to increase among community residents during an epidemic situation. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes towards COVID-19 among community residents and the impact of these perceptions and attitude on their daily lives and mental well-being.
Methods and analysis
Study design.
This study will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews (IDIs) with community members. The IDIs aim to explore perceptions of community members towards COVID-19 and its impact on their mental well-being.
Study setting and study participants
The study will be conducted in two communities in Karachi City: Karimabad Federal B Area Block 3 Gulberg Town, and Garden East and Garden West. Karimabad is a neighbourhood in the Karachi Central District of Karachi, Pakistan, situated in the south of Gulberg Town bordering Liaquatabad, Gharibabad and Federal B Area. The population of this neighbourhood is predominantly Ismailis. People living here belong mostly to the middle class to the lower middle class. It is also known for its wholesale market of sports goods and stationery. Garden is an upmarket neighbourhood in the Karachi South District of Karachi, Pakistan, subdivided into two neighbourhoods: Garden East and Garden West. It is the residential area around the Karachi Zoological Gardens; hence, it is popularly known as the ‘Garden’ area. The population of Garden used to be primarily Ismailis and Goan Catholics but has seen an increasing number of Memons, Pashtuns and Baloch. These areas have been selected purposively because the few members of these communities are already known to one of the coinvestigators. The coinvestigator will serve as a gatekeeper for providing entrance to the community for the purpose of this study. Adult community members of different ages and both genders will be interviewed from both sites, as mentioned in table 1 . Interview participants will be selected following the eligibility criteria.
- View inline
Study participants for indepth interviews
IDIs with community members
We will conduct IDIs with community members to explore the perceptions and attitudes of community members towards COVID-19 and its effects on their daily lives and mental well-being. IDI participants will be identified via the community WhatsApp group, and will be invited for an interview via a WhatsApp message or email. Consent will be taken over email or WhatsApp before the interview begins, where they will agree that the interview can be audio-recorded and that written notes can be taken. The interviews will be conducted either in Urdu or in English language, and each interview will last around 40–50 min. Study participants will be assured that their information will remain confidential and that no identifying features will be mentioned on the transcript. The major themes will include a general discussion about participants’ knowledge and perceptions about the COVID-19 pandemic, perceptions on safety measures, and perceived challenges in the current situation and its impact on their mental well-being. We anticipate that 24–30 interviews will be conducted, but we will cease interviews once data saturation has been achieved. Data saturation is the point when no new themes emerge from the additional interviews. Data collection will occur concurrently with data analysis to determine data saturation point. The audio recordings will be transcribed by a transcriptionist within 24 hours of the interviews.
An interview guide for IDIs is shown in online supplemental annex 1 .
Supplemental material
Eligibility criteria.
The following are the criteria for inclusion and exclusion of study participants:
Inclusion criteria
Residents of Garden (East and West) and Karimabad Federal B Area of Karachi who have not contracted the disease.
Exclusion criteria
Those who refuse to participate in the study.
Those who have experienced COVID-19 and are undergoing treatment.
Those who are suspected for COVID-19 and have been isolated/quarantined.
Family members of COVID-19-positive cases.
Data collection procedure
A semistructured interview guide has been developed for community members. The initial questions on the guide will help to explore participants’ perceptions and attitudes towards COVID-19. Additional questions on the guide will assess the impact of these perceptions and attitude on the daily lives and mental health and well-being of community residents. All semistructured interviews will be conducted online via Zoom or WhatsApp. Interviews will be scheduled at the participant’s convenient day and time. Interviews are anticipated to begin on 1 December 2020.
Patient and public involvement
No patients were involved.
Data analysis
We will transcribe and translate collected data into English language by listening to the audio recordings in order to conduct a thematic analysis. NVivo V.12 Plus software will be used to import, organise and explore data for analysis. Two independent researchers will read the transcripts at various times to develop familiarity and clarification with the data. We will employ an iterative process which will help us to label data and generate new categories to identify emergent themes. The recorded text will be divided into shortened units and labelled as a ‘code’ without losing the main essence of the research study. Subsequently, codes will be analysed and merged into comparable categories. Lastly, the same categories will be grouped into subthemes and final themes. To ensure inter-rater reliability, two independent investigators will perform the coding, category creation and thematic analyses. Discrepancies between the two investigators will be resolved through consensus meetings to reduce researcher bias.
Ethics and dissemination
Study participants will be asked to provide informed, written consent prior to participation in the study. The informed consent form can be submitted by the participant via WhatsApp or email. Participants who are unable to write their names will be asked to provide a thumbprint to symbolise their consent to participate. Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The study results will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
The findings of this study will help us to explore the perceptions and attitudes towards the COVID-19 pandemic and its impact on the daily lives and mental well-being of individuals in the community. Besides, an indepth understanding of the needs of the community will be identified, which will help us develop context-specific innovative mental health programmes to support communities in the future. The study will provide insights into how communities are managing their lives under such a difficult situation.
- World Health Organization
- Nielsen-Saines K , et al
- Worldometer
- Ebrahim SH ,
- Gozzer E , et al
- Snoswell CL ,
- Harding LE , et al
- Nargis Asad
- van Weel C ,
- Qidwai W , et al
- Brooks SK ,
- Webster RK ,
- Smith LE , et al
- Tripathy S ,
- Kar SK , et al
- Schwartz J ,
- Maunder R ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
ASF and NAA are joint first authors.
Contributors ASF and NAA conceived the study. ASF, NAA, RF, NA, SNM and SS contributed to the development of the study design and final protocols for sample selection and interviews. ASF and NAA contributed to writing the manuscript. All authors reviewed and approved the final version of the paper.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- The role of COVID-19 vaccines in preventing post-COVID-19 thromboembolic and cardiovascular complications
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Núria Mercadé-Besora 1 , 2 , 3 ,
- Xintong Li 1 ,
- Raivo Kolde 4 ,
- Nhung TH Trinh 5 ,
- Maria T Sanchez-Santos 1 ,
- Wai Yi Man 1 ,
- Elena Roel 3 ,
- Carlen Reyes 3 ,
- http://orcid.org/0000-0003-0388-3403 Antonella Delmestri 1 ,
- Hedvig M E Nordeng 6 , 7 ,
- http://orcid.org/0000-0002-4036-3856 Anneli Uusküla 8 ,
- http://orcid.org/0000-0002-8274-0357 Talita Duarte-Salles 3 , 9 ,
- Clara Prats 2 ,
- http://orcid.org/0000-0002-3950-6346 Daniel Prieto-Alhambra 1 , 9 ,
- http://orcid.org/0000-0002-0000-0110 Annika M Jödicke 1 ,
- Martí Català 1
- 1 Pharmaco- and Device Epidemiology Group, Health Data Sciences, Botnar Research Centre, NDORMS , University of Oxford , Oxford , UK
- 2 Department of Physics , Universitat Politècnica de Catalunya , Barcelona , Spain
- 3 Fundació Institut Universitari per a la recerca a l'Atenció Primària de Salut Jordi Gol i Gurina (IDIAPJGol) , IDIAP Jordi Gol , Barcelona , Catalunya , Spain
- 4 Institute of Computer Science , University of Tartu , Tartu , Estonia
- 5 Pharmacoepidemiology and Drug Safety Research Group, Department of Pharmacy, Faculty of Mathematics and Natural Sciences , University of Oslo , Oslo , Norway
- 6 School of Pharmacy , University of Oslo , Oslo , Norway
- 7 Division of Mental Health , Norwegian Institute of Public Health , Oslo , Norway
- 8 Department of Family Medicine and Public Health , University of Tartu , Tartu , Estonia
- 9 Department of Medical Informatics, Erasmus University Medical Center , Erasmus University Rotterdam , Rotterdam , Zuid-Holland , Netherlands
- Correspondence to Prof Daniel Prieto-Alhambra, Pharmaco- and Device Epidemiology Group, Health Data Sciences, Botnar Research Centre, NDORMS, University of Oxford, Oxford, UK; daniel.prietoalhambra{at}ndorms.ox.ac.uk
Objective To study the association between COVID-19 vaccination and the risk of post-COVID-19 cardiac and thromboembolic complications.
Methods We conducted a staggered cohort study based on national vaccination campaigns using electronic health records from the UK, Spain and Estonia. Vaccine rollout was grouped into four stages with predefined enrolment periods. Each stage included all individuals eligible for vaccination, with no previous SARS-CoV-2 infection or COVID-19 vaccine at the start date. Vaccination status was used as a time-varying exposure. Outcomes included heart failure (HF), venous thromboembolism (VTE) and arterial thrombosis/thromboembolism (ATE) recorded in four time windows after SARS-CoV-2 infection: 0–30, 31–90, 91–180 and 181–365 days. Propensity score overlap weighting and empirical calibration were used to minimise observed and unobserved confounding, respectively.
Fine-Gray models estimated subdistribution hazard ratios (sHR). Random effect meta-analyses were conducted across staggered cohorts and databases.
Results The study included 10.17 million vaccinated and 10.39 million unvaccinated people. Vaccination was associated with reduced risks of acute (30-day) and post-acute COVID-19 VTE, ATE and HF: for example, meta-analytic sHR of 0.22 (95% CI 0.17 to 0.29), 0.53 (0.44 to 0.63) and 0.45 (0.38 to 0.53), respectively, for 0–30 days after SARS-CoV-2 infection, while in the 91–180 days sHR were 0.53 (0.40 to 0.70), 0.72 (0.58 to 0.88) and 0.61 (0.51 to 0.73), respectively.
Conclusions COVID-19 vaccination reduced the risk of post-COVID-19 cardiac and thromboembolic outcomes. These effects were more pronounced for acute COVID-19 outcomes, consistent with known reductions in disease severity following breakthrough versus unvaccinated SARS-CoV-2 infection.
- Epidemiology
- PUBLIC HEALTH
- Electronic Health Records
Data availability statement
Data may be obtained from a third party and are not publicly available. CPRD: CPRD data were obtained under the CPRD multi-study license held by the University of Oxford after Research Data Governance (RDG) approval. Direct data sharing is not allowed. SIDIAP: In accordance with current European and national law, the data used in this study is only available for the researchers participating in this study. Thus, we are not allowed to distribute or make publicly available the data to other parties. However, researchers from public institutions can request data from SIDIAP if they comply with certain requirements. Further information is available online ( https://www.sidiap.org/index.php/menu-solicitudesen/application-proccedure ) or by contacting SIDIAP ([email protected]). CORIVA: CORIVA data were obtained under the approval of Research Ethics Committee of the University of Tartu and the patient level data sharing is not allowed. All analyses in this study were conducted in a federated manner, where analytical code and aggregated (anonymised) results were shared, but no patient-level data was transferred across the collaborating institutions.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/heartjnl-2023-323483
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
COVID-19 vaccines proved to be highly effective in reducing the severity of acute SARS-CoV-2 infection.
While COVID-19 vaccines were associated with increased risk for cardiac and thromboembolic events, such as myocarditis and thrombosis, the risk of complications was substantially higher due to SARS-CoV-2 infection.
WHAT THIS STUDY ADDS
COVID-19 vaccination reduced the risk of heart failure, venous thromboembolism and arterial thrombosis/thromboembolism in the acute (30 days) and post-acute (31 to 365 days) phase following SARS-CoV-2 infection. This effect was stronger in the acute phase.
The overall additive effect of vaccination on the risk of post-vaccine and/or post-COVID thromboembolic and cardiac events needs further research.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
COVID-19 vaccines proved to be highly effective in reducing the risk of post-COVID cardiovascular and thromboembolic complications.
Introduction
COVID-19 vaccines were approved under emergency authorisation in December 2020 and showed high effectiveness against SARS-CoV-2 infection, COVID-19-related hospitalisation and death. 1 2 However, concerns were raised after spontaneous reports of unusual thromboembolic events following adenovirus-based COVID-19 vaccines, an association that was further assessed in observational studies. 3 4 More recently, mRNA-based vaccines were found to be associated with a risk of rare myocarditis events. 5 6
On the other hand, SARS-CoV-2 infection can trigger cardiac and thromboembolic complications. 7 8 Previous studies showed that, while slowly decreasing over time, the risk for serious complications remain high for up to a year after infection. 9 10 Although acute and post-acute cardiac and thromboembolic complications following COVID-19 are rare, they present a substantial burden to the affected patients, and the absolute number of cases globally could become substantial.
Recent studies suggest that COVID-19 vaccination could protect against cardiac and thromboembolic complications attributable to COVID-19. 11 12 However, most studies did not include long-term complications and were conducted among specific populations.
Evidence is still scarce as to whether the combined effects of COVID-19 vaccines protecting against SARS-CoV-2 infection and reducing post-COVID-19 cardiac and thromboembolic outcomes, outweigh any risks of these complications potentially associated with vaccination.
We therefore used large, representative data sources from three European countries to assess the overall effect of COVID-19 vaccines on the risk of acute and post-acute COVID-19 complications including venous thromboembolism (VTE), arterial thrombosis/thromboembolism (ATE) and other cardiac events. Additionally, we studied the comparative effects of ChAdOx1 versus BNT162b2 on the risk of these same outcomes.
Data sources
We used four routinely collected population-based healthcare datasets from three European countries: the UK, Spain and Estonia.
For the UK, we used data from two primary care databases—namely, Clinical Practice Research Datalink, CPRD Aurum 13 and CPRD Gold. 14 CPRD Aurum currently covers 13 million people from predominantly English practices, while CPRD Gold comprises 3.1 million active participants mostly from GP practices in Wales and Scotland. Spanish data were provided by the Information System for the Development of Research in Primary Care (SIDIAP), 15 which encompasses primary care records from 6 million active patients (around 75% of the population in the region of Catalonia) linked to hospital admissions data (Conjunt Mínim Bàsic de Dades d’Alta Hospitalària). Finally, the CORIVA dataset based on national health claims data from Estonia was used. It contains all COVID-19 cases from the first year of the pandemic and ~440 000 randomly selected controls. CORIVA was linked to the death registry and all COVID-19 testing from the national health information system.
Databases included sociodemographic information, diagnoses, measurements, prescriptions and secondary care referrals and were linked to vaccine registries, including records of all administered vaccines from all healthcare settings. Data availability for CPRD Gold ended in December 2021, CPRD Aurum in January 2022, SIDIAP in June 2022 and CORIVA in December 2022.
All databases were mapped to the Observational Medical Outcomes Partnership Common Data Model (OMOP CDM) 16 to facilitate federated analytics.
Multinational network staggered cohort study: study design and participants
The study design has been published in detail elsewhere. 17 Briefly, we used a staggered cohort design considering vaccination as a time-varying exposure. Four staggered cohorts were designed with each cohort representing a country-specific vaccination rollout phase (eg, dates when people became eligible for vaccination, and eligibility criteria).
The source population comprised all adults registered in the respective database for at least 180 days at the start of the study (4 January 2021 for CPRD Gold and Aurum, 20 February 2021 for SIDIAP and 28 January 2021 for CORIVA). Subsequently, each staggered cohort corresponded to an enrolment period: all people eligible for vaccination during this time were included in the cohort and people with a history of SARS-CoV-2 infection or COVID-19 vaccination before the start of the enrolment period were excluded. Across countries, cohort 1 comprised older age groups, whereas cohort 2 comprised individuals at risk for severe COVID-19. Cohort 3 included people aged ≥40 and cohort 4 enrolled people aged ≥18.
In each cohort, people receiving a first vaccine dose during the enrolment period were allocated to the vaccinated group, with their index date being the date of vaccination. Individuals who did not receive a vaccine dose comprised the unvaccinated group and their index date was assigned within the enrolment period, based on the distribution of index dates in the vaccinated group. People with COVID-19 before the index date were excluded.
Follow-up started from the index date until the earliest of end of available data, death, change in exposure status (first vaccine dose for those unvaccinated) or outcome of interest.
COVID-19 vaccination
All vaccines approved within the study period from January 2021 to July 2021—namely, ChAdOx1 (Oxford/AstraZeneca), BNT162b2 (BioNTech/Pfizer]) Ad26.COV2.S (Janssen) and mRNA-1273 (Moderna), were included for this study.
Post-COVID-19 outcomes of interest
Outcomes of interest were defined as SARS-CoV-2 infection followed by a predefined thromboembolic or cardiac event of interest within a year after infection, and with no record of the same clinical event in the 6 months before COVID-19. Outcome date was set as the corresponding SARS-CoV-2 infection date.
COVID-19 was identified from either a positive SARS-CoV-2 test (polymerase chain reaction (PCR) or antigen), or a clinical COVID-19 diagnosis, with no record of COVID-19 in the previous 6 weeks. This wash-out period was imposed to exclude re-recordings of the same COVID-19 episode.
Post-COVID-19 outcome events were selected based on previous studies. 11–13 Events comprised ischaemic stroke (IS), haemorrhagic stroke (HS), transient ischaemic attack (TIA), ventricular arrhythmia/cardiac arrest (VACA), myocarditis/pericarditis (MP), myocardial infarction (MI), heart failure (HF), pulmonary embolism (PE) and deep vein thrombosis (DVT). We used two composite outcomes: (1) VTE, as an aggregate of PE and DVT and (2) ATE, as a composite of IS, TIA and MI. To avoid re-recording of the same complication we imposed a wash-out period of 90 days between records. Phenotypes for these complications were based on previously published studies. 3 4 8 18
All outcomes were ascertained in four different time periods following SARS-CoV-2 infection: the first period described the acute infection phase—that is, 0–30 days after COVID-19, whereas the later periods - which are 31–90 days, 91–180 days and 181–365 days, illustrate the post-acute phase ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Study outcome design. Study outcomes of interest are defined as a COVID-19 infection followed by one of the complications in the figure, within a year after infection. Outcomes were ascertained in four different time windows after SARS-CoV-2 infection: 0–30 days (namely the acute phase), 31–90 days, 91–180 days and 181–365 days (these last three comprise the post-acute phase).
Negative control outcomes
Negative control outcomes (NCOs) were used to detect residual confounding. NCOs are outcomes which are not believed to be causally associated with the exposure, but share the same bias structure with the exposure and outcome of interest. Therefore, no significant association between exposure and NCO is to be expected. Our study used 43 different NCOs from previous work assessing vaccine effectiveness. 19
Statistical analysis
Federated network analyses.
A template for an analytical script was developed and subsequently tailored to include the country-specific aspects (eg, dates, priority groups) for the vaccination rollout. Analyses were conducted locally for each database. Only aggregated data were shared and person counts <5 were clouded.
Propensity score weighting
Large-scale propensity scores (PS) were calculated to estimate the likelihood of a person receiving the vaccine based on their demographic and health-related characteristics (eg, conditions, medications) prior to the index date. PS were then used to minimise observed confounding by creating a weighted population (overlap weighting 20 ), in which individuals contributed with a different weight based on their PS and vaccination status.
Prespecified key variables included in the PS comprised age, sex, location, index date, prior observation time in the database, number of previous outpatient visits and previous SARS-CoV-2 PCR/antigen tests. Regional vaccination, testing and COVID-19 incidence rates were also forced into the PS equation for the UK databases 21 and SIDIAP. 22 In addition, least absolute shrinkage and selection operator (LASSO) regression, a technique for variable selection, was used to identify additional variables from all recorded conditions and prescriptions within 0–30 days, 31–180 days and 181-any time (conditions only) before the index date that had a prevalence of >0.5% in the study population.
PS were then separately estimated for each staggered cohort and analysis. We considered covariate balance to be achieved if absolute standardised mean differences (ASMDs) were ≤0.1 after weighting. Baseline characteristics such as demographics and comorbidities were reported.
Effect estimation
To account for the competing risk of death associated with COVID-19, Fine-and-Grey models 23 were used to calculate subdistribution hazard ratios (sHRs). Subsequently, sHRs and confidence intervals were empirically calibrated from NCO estimates 24 to account for unmeasured confounding. To calibrate the estimates, the empirical null distribution was derived from NCO estimates and was used to compute calibrated confidence intervals. For each outcome, sHRs from the four staggered cohorts were pooled using random-effect meta-analysis, both separately for each database and across all four databases.
Sensitivity analysis
Sensitivity analyses comprised 1) censoring follow-up for vaccinated people at the time when they received their second vaccine dose and 2) considering only the first post-COVID-19 outcome within the year after infection ( online supplemental figure S1 ). In addition, comparative effectiveness analyses were conducted for BNT162b2 versus ChAdOx1.
Supplemental material
Data and code availability.
All analytic code for the study is available in GitHub ( https://github.com/oxford-pharmacoepi/vaccineEffectOnPostCovidCardiacThromboembolicEvents ), including code lists for vaccines, COVID-19 tests and diagnoses, cardiac and thromboembolic events, NCO and health conditions to prioritise patients for vaccination in each country. We used R version 4.2.3 and statistical packages survival (3.5–3), Empirical Calibration (3.1.1), glmnet (4.1-7), and Hmisc (5.0–1).
Patient and public involvement
Owing to the nature of the study and the limitations regarding data privacy, the study design, analysis, interpretation of data and revision of the manuscript did not involve any patients or members of the public.
All aggregated results are available in a web application ( https://dpa-pde-oxford.shinyapps.io/PostCovidComplications/ ).
We included over 10.17 million vaccinated individuals (1 618 395 from CPRD Gold; 5 729 800 from CPRD Aurum; 2 744 821 from SIDIAP and 77 603 from CORIVA) and 10.39 million unvaccinated individuals (1 640 371; 5 860 564; 2 588 518 and 302 267, respectively). Online supplemental figures S2-5 illustrate study inclusion for each database.
Adequate covariate balance was achieved after PS weighting in most studies: CORIVA (all cohorts) and SIDIAP (cohorts 1 and 4) did not contribute to ChAdOx1 subanalyses owing to sample size and covariate imbalance. ASMD results are accessible in the web application.
NCO analyses suggested residual bias after PS weighting, with a majority of NCOs associated positively with vaccination. Therefore, calibrated estimates are reported in this manuscript. Uncalibrated effect estimates and NCO analyses are available in the web interface.
Population characteristics
Table 1 presents baseline characteristics for the weighted populations in CPRD Aurum, for illustrative purposes. Online supplemental tables S1-25 summarise baseline characteristics for weighted and unweighted populations for each database and comparison. Across databases and cohorts, populations followed similar patterns: cohort 1 represented an older subpopulation (around 80 years old) with a high proportion of women (57%). Median age was lowest in cohort 4 ranging between 30 and 40 years.
- View inline
Characteristics of weighted populations in CPRD Aurum database, stratified by staggered cohort and exposure status. Exposure is any COVID-19 vaccine
COVID-19 vaccination and post-COVID-19 complications
Table 2 shows the incidence of post-COVID-19 VTE, ATE and HF, the three most common post-COVID-19 conditions among the studied outcomes. Outcome counts are presented separately for 0–30, 31–90, 91–180 and 181–365 days after SARS-CoV-2 infection. Online supplemental tables S26-36 include all studied complications, also for the sensitivity and subanalyses. Similar pattern for incidences were observed across all databases: higher outcome rates in the older populations (cohort 1) and decreasing frequency with increasing time after infection in all cohorts.
Number of records (and risk per 10 000 individuals) for acute and post-acute COVID-19 cardiac and thromboembolic complications, across cohorts and databases for any COVID-19 vaccination
Forest plots for the effect of COVID-19 vaccines on post-COVID-19 cardiac and thromboembolic complications; meta-analysis across cohorts and databases. Dashed line represents a level of heterogeneity I 2 >0.4. ATE, arterial thrombosis/thromboembolism; CD+HS, cardiac diseases and haemorrhagic stroke; VTE, venous thromboembolism.
Results from calibrated estimates pooled in meta-analysis across cohorts and databases are shown in figure 2 .
Reduced risk associated with vaccination is observed for acute and post-acute VTE, DVT, and PE: acute meta-analytic sHR are 0.22 (95% CI, 0.17–0.29); 0.36 (0.28–0.45); and 0.19 (0.15–0.25), respectively. For VTE in the post-acute phase, sHR estimates are 0.43 (0.34–0.53), 0.53 (0.40–0.70) and 0.50 (0.36–0.70) for 31–90, 91–180, and 181–365 days post COVID-19, respectively. Reduced risk of VTE outcomes was observed in vaccinated across databases and cohorts, see online supplemental figures S14–22 .
Similarly, the risk of ATE, IS and MI in the acute phase after infection was reduced for the vaccinated group, sHR of 0.53 (0.44–0.63), 0.55 (0.43–0.70) and 0.49 (0.38–0.62), respectively. Reduced risk associated with vaccination persisted for post-acute ATE, with sHR of 0.74 (0.60–0.92), 0.72 (0.58–0.88) and 0.62 (0.48–0.80) for 31–90, 91–180 and 181–365 days post-COVID-19, respectively. Risk of post-acute MI remained lower for vaccinated in the 31–90 and 91–180 days after COVID-19, with sHR of 0.64 (0.46–0.87) and 0.64 (0.45–0.90), respectively. Vaccination effect on post-COVID-19 TIA was seen only in the 181–365 days, with sHR of 0.51 (0.31–0.82). Online supplemental figures S23-31 show database-specific and cohort-specific estimates for ATE-related complications.
Risk of post-COVID-19 cardiac complications was reduced in vaccinated individuals. Meta-analytic estimates in the acute phase showed sHR of 0.45 (0.38–0.53) for HF, 0.41 (0.26–0.66) for MP and 0.41 (0.27–0.63) for VACA. Reduced risk persisted for post-acute COVID-19 HF: sHR 0.61 (0.51–0.73) for 31–90 days, 0.61 (0.51–0.73) for 91–180 days and 0.52 (0.43–0.63) for 181–365 days. For post-acute MP, risk was only lowered in the first post-acute window (31–90 days), with sHR of 0.43 (0.21–0.85). Vaccination showed no association with post-COVID-19 HS. Database-specific and cohort-specific results for these cardiac diseases are shown in online supplemental figures S32-40 .
Stratified analyses by vaccine showed similar associations, except for ChAdOx1 which was not associated with reduced VTE and ATE risk in the last post-acute window. Sensitivity analyses were consistent with main results ( online supplemental figures S6-13 ).
Figure 3 shows the results of comparative effects of BNT162b2 versus ChAdOx1, based on UK data. Meta-analytic estimates favoured BNT162b2 (sHR of 0.66 (0.46–0.93)) for VTE in the 0–30 days after infection, but no differences were seen for post-acute VTE or for any of the other outcomes. Results from sensitivity analyses, database-specific and cohort-specific estimates were in line with the main findings ( online supplemental figures S41-51 ).
Forest plots for comparative vaccine effect (BNT162b2 vs ChAdOx1); meta-analysis across cohorts and databases. ATE, arterial thrombosis/thromboembolism; CD+HS, cardiac diseases and haemorrhagic stroke; VTE, venous thromboembolism.
Key findings
Our analyses showed a substantial reduction of risk (45–81%) for thromboembolic and cardiac events in the acute phase of COVID-19 associated with vaccination. This finding was consistent across four databases and three different European countries. Risks for post-acute COVID-19 VTE, ATE and HF were reduced to a lesser extent (24–58%), whereas a reduced risk for post-COVID-19 MP and VACA in vaccinated people was seen only in the acute phase.
Results in context
The relationship between SARS-CoV-2 infection, COVID-19 vaccines and thromboembolic and/or cardiac complications is tangled. Some large studies report an increased risk of VTE and ATE following both ChAdOx1 and BNT162b2 vaccination, 7 whereas other studies have not identified such a risk. 25 Elevated risk of VTE has also been reported among patients with COVID-19 and its occurrence can lead to poor prognosis and mortality. 26 27 Similarly, several observational studies have found an association between COVID-19 mRNA vaccination and a short-term increased risk of myocarditis, particularly among younger male individuals. 5 6 For instance, a self-controlled case series study conducted in England revealed about 30% increased risk of hospital admission due to myocarditis within 28 days following both ChAdOx1 and BNT162b2 vaccines. However, this same study also found a ninefold higher risk for myocarditis following a positive SARS-CoV-2 test, clearly offsetting the observed post-vaccine risk.
COVID-19 vaccines have demonstrated high efficacy and effectiveness in preventing infection and reducing the severity of acute-phase infection. However, with the emergence of newer variants of the virus, such as omicron, and the waning protective effect of the vaccine over time, there is a growing interest in understanding whether the vaccine can also reduce the risk of complications after breakthrough infections. Recent studies suggested that COVID-19 vaccination could potentially protect against acute post-COVID-19 cardiac and thromboembolic events. 11 12 A large prospective cohort study 11 reports risk of VTE after SARS-CoV-2 infection to be substantially reduced in fully vaccinated ambulatory patients. Likewise, Al-Aly et al 12 suggest a reduced risk for post-acute COVID-19 conditions in breakthrough infection versus SARS-CoV-2 infection without prior vaccination. However, the populations were limited to SARS-CoV-2 infected individuals and estimates did not include the effect of the vaccine to prevent COVID-19 in the first place. Other studies on post-acute COVID-19 conditions and symptoms have been conducted, 28 29 but there has been limited reporting on the condition-specific risks associated with COVID-19, even though the prognosis for different complications can vary significantly.
In line with previous studies, our findings suggest a potential benefit of vaccination in reducing the risk of post-COVID-19 thromboembolic and cardiac complications. We included broader populations, estimated the risk in both acute and post-acute infection phases and replicated these using four large independent observational databases. By pooling results across different settings, we provided the most up-to-date and robust evidence on this topic.
Strengths and limitations
The study has several strengths. Our multinational study covering different healthcare systems and settings showed consistent results across all databases, which highlights the robustness and replicability of our findings. All databases had complete recordings of vaccination status (date and vaccine) and are representative of the respective general population. Algorithms to identify study outcomes were used in previous published network studies, including regulatory-funded research. 3 4 8 18 Other strengths are the staggered cohort design which minimises confounding by indication and immortal time bias. PS overlap weighting and NCO empirical calibration have been shown to adequately minimise bias in vaccine effectiveness studies. 19 Furthermore, our estimates include the vaccine effectiveness against COVID-19, which is crucial in the pathway to experience post-COVID-19 complications.
Our study has some limitations. The use of real-world data comes with inherent limitations including data quality concerns and risk of confounding. To deal with these limitations, we employed state-of-the-art methods, including large-scale propensity score weighting and calibration of effect estimates using NCO. 19 24 A recent study 30 has demonstrated that methodologically sound observational studies based on routinely collected data can produce results similar to those of clinical trials. We acknowledge that results from NCO were positively associated with vaccination, and estimates might still be influenced by residual bias despite using calibration. Another limitation is potential under-reporting of post-COVID-19 complications: some asymptomatic and mild COVID-19 infections might have not been recorded. Additionally, post-COVID-19 outcomes of interest might be under-recorded in primary care databases (CPRD Aurum and Gold) without hospital linkage, which represent a large proportion of the data in the study. However, results in SIDIAP and CORIVA, which include secondary care data, were similar. Also, our study included a small number of young men and male teenagers, who were the main population concerned with increased risks of myocarditis/pericarditis following vaccination.
Conclusions
Vaccination against SARS-CoV-2 substantially reduced the risk of acute post-COVID-19 thromboembolic and cardiac complications, probably through a reduction in the risk of SARS-CoV-2 infection and the severity of COVID-19 disease due to vaccine-induced immunity. Reduced risk in vaccinated people lasted for up to 1 year for post-COVID-19 VTE, ATE and HF, but not clearly for other complications. Findings from this study highlight yet another benefit of COVID-19 vaccination. However, further research is needed on the possible waning of the risk reduction over time and on the impact of booster vaccination.
Ethics statements
Patient consent for publication.
Not applicable.

Ethics approval
The study was approved by the CPRD’s Research Data Governance Process, Protocol No 21_000557 and the Clinical Research Ethics committee of Fundació Institut Universitari per a la recerca a l’Atenció Primària de Salut Jordi Gol i Gurina (IDIAPJGol) (approval number 4R22/133) and the Research Ethics Committee of the University of Tartu (approval No. 330/T-10).
Acknowledgments
This study is based in part on data from the Clinical Practice Research Datalink (CPRD) obtained under licence from the UK Medicines and Healthcare products Regulatory Agency. We thank the patients who provided these data, and the NHS who collected the data as part of their care and support. All interpretations, conclusions and views expressed in this publication are those of the authors alone and not necessarily those of CPRD. We would also like to thank the healthcare professionals in the Catalan healthcare system involved in the management of COVID-19 during these challenging times, from primary care to intensive care units; the Institut de Català de la Salut and the Program d’Analítica de Dades per a la Recerca i la Innovació en Salut for providing access to the different data sources accessible through The System for the Development of Research in Primary Care (SIDIAP).
- Pritchard E ,
- Matthews PC ,
- Stoesser N , et al
- Lauring AS ,
- Tenforde MW ,
- Chappell JD , et al
- Pistillo A , et al
- Duarte-Salles T , et al
- Hansen JV ,
- Fosbøl E , et al
- Chen A , et al
- Hippisley-Cox J ,
- Mei XW , et al
- Duarte-Salles T ,
- Fernandez-Bertolin S , et al
- Ip S , et al
- Bowe B , et al
- Prats-Uribe A ,
- Feng Q , et al
- Campbell J , et al
- Herrett E ,
- Gallagher AM ,
- Bhaskaran K , et al
- Raventós B ,
- Fernández-Bertolín S ,
- Aragón M , et al
- Makadia R ,
- Matcho A , et al
- Mercadé-Besora N ,
- Kolde R , et al
- Ostropolets A ,
- Makadia R , et al
- Rathod-Mistry T , et al
- Thomas LE ,
- ↵ Coronavirus (COVID-19) in the UK . 2022 . Available : https://coronavirus.data.gov.uk/
- Generalitat de Catalunya
- Schuemie MJ ,
- Hripcsak G ,
- Ryan PB , et al
- Houghton DE ,
- Wysokinski W ,
- Casanegra AI , et al
- Katsoularis I ,
- Fonseca-Rodríguez O ,
- Farrington P , et al
- Jehangir Q ,
- Li P , et al
- Byambasuren O ,
- Stehlik P ,
- Clark J , et al
- Brannock MD ,
- Preiss AJ , et al
- Schneeweiss S , RCT-DUPLICATE Initiative , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
AMJ and MC are joint senior authors.
Contributors DPA and AMJ led the conceptualisation of the study with contributions from MC and NM-B. AMJ, TD-S, ER, AU and NTHT adapted the study design with respect to the local vaccine rollouts. AD and WYM mapped and curated CPRD data. MC and NM-B developed code with methodological contributions advice from MTS-S and CP. DPA, MC, NTHT, TD-S, HMEN, XL, CR and AMJ clinically interpreted the results. NM-B, XL, AMJ and DPA wrote the first draft of the manuscript, and all authors read, revised and approved the final version. DPA and AMJ obtained the funding for this research. DPA is responsible for the overall content as guarantor: he accepts full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish.
Funding The research was supported by the National Institute for Health and Care Research (NIHR) Oxford Biomedical Research Centre (BRC). DPA is funded through a NIHR Senior Research Fellowship (Grant number SRF-2018–11-ST2-004). Funding to perform the study in the SIDIAP database was provided by the Real World Epidemiology (RWEpi) research group at IDIAPJGol. Costs of databases mapping to OMOP CDM were covered by the European Health Data and Evidence Network (EHDEN).
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Open access
- Published: 21 March 2024
Stressors, emotions, and social support systems among respiratory nurses during the Omicron outbreak in China: a qualitative study
- Wenzhen Yu 1 ,
- Ying Zhang 1 ,
- Yunyan Xianyu 1 &
- Dan Cheng 1
BMC Nursing volume 23 , Article number: 188 ( 2024 ) Cite this article
36 Accesses
Metrics details
Respiratory nurses faced tremendous challenges when the Omicron variant spread rapidly in China from late 2022 to early 2023. An in-depth understanding of respiratory nurses’ experiences during challenging times can help to develop better management and support strategies. The present study was conducted to explore and describe the work experiences of nurses working in the Department of Pulmonary and Critical Care Medicine (PCCM) during the Omicron outbreak in China.
This study utilized a descriptive phenomenological method. Between January 9 and 22, 2023, semistructured and individual in-depth interviews were conducted with 11 respiratory nurses at a tertiary hospital in Wuhan, Hubei Province. A purposive sampling method was used to select the participants, and the sample size was determined based on data saturation. The data analysis was carried out using Colaizzi’s method.
Three themes with ten subthemes emerged: (a) multiple stressors (intense workload due to high variability in COVID patients; worry about not having enough ability and energy to care for critically ill patients; fighting for anxious clients, colleagues, and selves); (b) mixed emotions (feelings of loss and responsibility; feelings of frustration and achievement; feelings of nervousness and security); and (c) a perceived social support system (team cohesion; family support; head nurse leadership; and the impact of social media).
Nursing managers should be attentive to frontline nurses’ needs and occupational stress during novel coronavirus disease 2019 (COVID-19) outbreaks. Management should strengthen psychological and social support systems, optimize nursing leadership styles, and proactively consider the application of artificial intelligence (AI) technologies and products in clinical care to improve the ability of nurses to effectively respond to future public health crises.
Peer Review reports
Introduction
As of January 29, 2023, more than 753 million confirmed cases of COVID-19 have been reported globally, with more than 6.8 million deaths [ 1 ]. The Omicron variant (Omicron, B.1.1.529) is one of the five World Health Organization (WHO) variants of concern (VOCs). Compared with other VOCs, the Omicron variant has significantly increased transmission and immune escape [ 2 ]. An analysis by the Chinese Center for Disease Control and Prevention (CCDC) revealed that from December 1, 2022, to early January 2023, Omicron BA.5.2 and BF.7 were the prevalent strains in China, with these two lineages accounting for 97.5% of all indigenous cases [ 3 ]. At the press conference of the Joint COVID-19 Prevention and Control Mechanism of the State Council on January 14, 2023, the number of hospitalizations due to COVID-19 reached a peak of 1.63 million on January 5, and from December 8, 2022, to January 12, 2023, a total of 59,938 deaths related to hospitalizations due to COVID-19 occurred in medical institutions across the country. There were 5,503 deaths due to respiratory failure [ 4 ].
Nurses play a vital role in rescuing and treating COVID-19 patients. Nurses are at the forefront of the fight against disease, facing enormous physical and mental pressure while adopting effective strategies to overcome unprecedented challenges [ 5 – 6 ]. Research has shown that frontline nurses faced numerous challenges during the COVID-19 pandemic. A systematic review and meta-analysis exploring the impact of the COVID-19 pandemic on the prevalence of psychological symptoms among nurses showed that the pooled prevalence of anxiety, depression, and sleep disturbance was 37%, 35% and 43%, respectively [ 7 ]. During the COVID-19 pandemic, the workload of frontline nurses also increased significantly due to multiple factors, such as increased patient requirements and work content, longer work hours, and a shortage of staff and personal protective equipment [ 8 – 9 ]. In addition, nurses also expressed feelings of helplessness and inadequacy because, despite hard work, they were unable to provide dignified and acceptable-quality care [ 10 ]. Therefore, it is necessary to emphasize the significance of support for nurses from governments, policy-makers, and nursing organizations to reduce the negative impacts on nurses’ well-being during and after a pandemic or epidemic [ 11 ]. Otherwise, nurses may feel burnout, leading to turnover [ 12 – 13 ].
Nevertheless, existing studies on frontline nurses’ work experiences have been conducted predominantly in the context of nurses as physically healthy individuals providing health care services to COVID-19 patients. With the rapid spread of the Omicron BA.5.2 and BF.7 variants, it was estimated that most of the Chinese population was infected in December 2023 [ 14 ]. It has been reported that the number of clinic visits due to fever in China peaked on December 23, 2023. Two weeks later, the number of critical hospitalizations for COVID-19 also peaked [ 4 ]. During that period, the challenges faced by nurses in China were unprecedented and vastly different from those of other nurses worldwide. Most nurses were both health care providers and infected patients. The present qualitative study aimed to explore the work experiences of frontline respiratory nurses during the Omicron epidemic, develop better nursing countermeasures and management strategies for managers and promote better support for frontline nurses to provide patients with higher-quality care in possible future outbreaks.
Study design
The present study adopted a qualitative descriptive phenomenological design to conduct in-depth interviews. This design is suitable for providing detailed descriptions of participants’ emotions, opinions, and experiences and interpreting the meaning of their behaviours [ 15 ].
Participants and setting
All participants were recruited from a tertiary hospital in Wuhan, Hubei Province, China. A purposive sampling method was used in the present study. To obtain a wide range of experiences, we considered a diverse range of personal details, including age, sex, education level, marital status, years of nursing experience, professional title, type of employment, and workplace type, during the selection of participants. The sample size was determined based on data saturation [ 16 ].
The inclusion criteria were registered nurses working at the PCCM who provided direct care to COVID-19 patients between December 8, 2022, and January 8, 2023, and those who expressed willingness to participate in the study and share their experience. Nurse managers and nurses working less than two weeks during the abovementioned period were excluded.
Data collection
The data were collected through individual and face-to-face, in-depth interviews from January 9 to 22, 2023.
After a literature review and panel discussion, an interview guide was developed. Two pilot interviews were also conducted to investigate the appropriateness of the interview questions, and the guide remained the same. The data from the pilot interviews were not included in the analysis. All interviews were conducted by one researcher (first author), who completed a thorough and systematic study of qualitative research methods and reviewing skills before the start of the study. The final semistructured interview guide consisted of nine open-ended questions (see Supplementary file 1 ).
The interviewer and the participants had been colleagues for 3–7 years and trusted each other. The interviewer informed the participants about the purpose, voluntariness, anonymity, and confidentiality of the study one day before the interview and scheduled the time of the interview. Interviews were usually conducted on an afternoon when the participants were off duty, or an alternative time was arranged if the participants could not leave work on time. The interviews were conducted in a one-room office to ensure that the environment was quiet and undisturbed so that the participants could express their inner feelings to the interviewer with an open mind. With the participants’ permission, all interviews were audio-recorded using a digital voice recorder. The duration of the interviews varied between 30 and 60 min. Within 24 h of each interview, the audio-recorded data were fully transcribed, and two researchers independently evaluated the data saturation. Any disagreements were resolved through a panel discussion. Behavioural data (laughing, crying, sighing, silence or pausing, etc.) were also recorded during transcription for data analysis. Data saturation was reached at the 10th interview, but an additional interview was also conducted to ensure that no new information emerged. Therefore, a total of 11 respiratory nurses were recruited. None of the nurses dropped out of the study.
Data analysis
Colaizzi’s method was used to analyse the data [ 17 ]. This method involved the following steps: (a) Familiarization: rereading the transcripts verbatim multiple times to become familiar with the data; (b) Identifying significant statements: identifying and extracting meaningful statements relevant to the phenomenon; (c) Formulating meanings: formulating and encoding meanings from important statements; (d) Clustering themes: aggregating the encoded meanings into preliminary themes; (e) Developing an exhaustive description: providing a detailed description of each of the themes generated in step d with the addition of participants’ original statements; (f) Producing the fundamental structure: generating themes to reveal the basic structure of the phenomenon using short and condensed phrases; and (g) Verifying the fundamental structure: presenting the transcripts of the interviews, codes, and themes to the participants for feedback on whether their experience of the phenomenon had been accurately represented. Two independent researchers analysed the data simultaneously.
In this study, Lincoln and Guba’s criteria of credibility, transferability, dependability, and confirmability were utilized to ensure rigor [ 18 ]. The following strategies were implemented to achieve credible study findings: conducting semistructured, in-depth interviews with open-ended questions and field notes; transcribing audio-recorded data word-for-word and independently analysing the raw data by two researchers; and asking participants to provide feedback on the transcripts, codes, and themes. Transferability was established by considering maximum variations in participant characteristics and presenting appropriate participant quotes. To facilitate dependability and confirmability, several meetings were held among the researchers to discuss and identify codes, subthemes, and themes.
Ethical considerations
This study was approved by the research and ethics committees of Renmin Hospital of Wuhan University (Approval NO: WDRY2023-K031). Before the interviews, the details of the study, the expected risks and benefits, and the right to withdraw at any time was verbally explained to all participants, and written informed consent was obtained. After the interviews were transcribed, the participants’ names were deleted instead of their identities (A‒K). To ensure confidentiality and privacy, the text data were stored in a locked cabinet, and the audio data were stored on a password-protected computer.
Participant characteristics
A total of 11 nurses, including 10 females (90.9%) and 1 male (9.1%), were included. The mean age was 32.09 ± 5.45 years (range = 24–43 years), and the mean number of years of nursing experience was 10.36 ± 5.50 years (range = 3–21 years). The sociodemographic data are displayed in Table 1 .
Thematic results
Three major themes emerged: multiple stressors, mixed emotions, and a perceived social support system. Ten subthemes were identified. The findings are described in Fig. 1 .
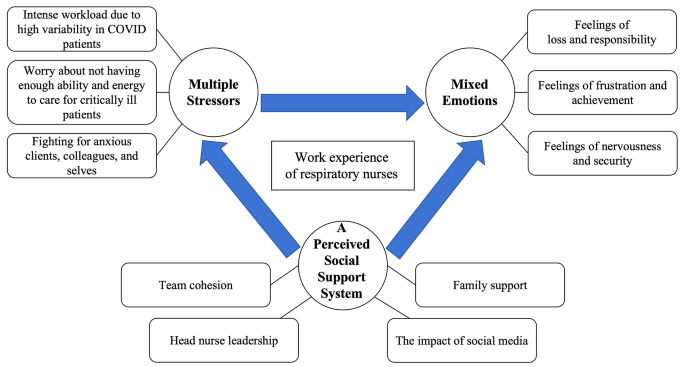
Themes and sub-themes of work experience for respiratory nurses during Omicron outbreak
Theme 1: Multiple Stressors
This theme focused on the workplace stressors experienced by respiratory nurses during the Omicron outbreak. Three subthemes were identified in this theme: intense workload due to high variability in COVID patients; worry about not having enough ability and energy to care for critically ill patients; and fighting for anxious clients, colleagues, and selves.
Intense workload due to high variability in COVID patients
Most participants reported a high level of work pressure, such as a high number of admissions, a high percentage of critical patients, rapid changes in patient conditions, and frequent resuscitations. As one participant said,
“For some time now, the RICU has been particularly busy. Every shift is filled with resuscitation cases and the admission of new critically ill patients, usually those who need to be intubated. We borrowed much equipment from the Equipment Division, such as ventilators and high-flow nasal cannula oxygen therapy devices. We usually have enough equipment in our Department, but now we do not.” (Participant G)
Almost all participants stated that the workload of nursing care associated with COVID-19 had significantly increased, and nurses often had to work overtime to complete their work. As two participants said,
“Almost all newly admitted patients are given nebulizers and oxygen and undergo urgent arterial blood gas analysis. I could not leave work on time almost daily (bitter smile).” (Participant C)
“There are many patients on oral corticosteroids, which is different than usual. I have to talk to the patients about the use and the dosage, tell them when to taper, and talk to the doctor before I give the medication. It all takes time.” (Participant I)
Another participant said the following:
“Except for nursing records, I get things done during working hours. Then, I spend off-duty time writing the records.” (Participant E)
Some participants reported working at an accelerated pace during the work period. One of the participants described their experience as follows:
“Patients ask me questions, and maybe I am fast in my speech and, well, fast enough in my steps.” (Participant D)
Most participants reported returning to work after taking a short break from their infections. However, they were still symptomatic when they returned to work. One participant said the following:
“I had three days of rest and came back to work when my fever was down, and my cough has not gone away yet.” (Participant A)
Worry about not having enough ability and energy to care for critically ill patients
Some of the participants in this study reported significant psychological distress from worrying about not having enough ability and energy to care for critically ill patients. The following excerpts illustrate this subtheme:
“There are many patients on invasive mechanical ventilation, and the biggest worry is accidental extubation. It is nerve-wracking.” (Participant F)
“Some patients are ventilated in the prone position; some are intubated, and some are not. Although the therapeutic efficacy was quite good, at least four colleagues were needed to change the position. It is a big risk at night when we are short-staffed, especially in a resuscitation situation.” (Participant G)
“I was worried about making mistakes. During that time, I had night sweats, did not sleep well, often felt weak and dizzy during the day, and was afraid that I would make a mistake while providing care because of my lack of concentration.” (Participant K)
Fighting for anxious clients, colleagues, and selves
In this study, most participants said that patients and their family members, doctors, other nurses, and themselves were experiencing negative emotions such as anxiety. Some participants expressed this as follows:
“In my communication with patients, I have noticed that many patients are anxious, so I do more explaining than before when I give patients medication. Many patients ask me if their disease is serious…” (Participant I)
“Some patients are transferred to the RICU when their condition deteriorates, and their families have no sight of them and are very anxious every day. There is also much pressure on the doctors.” (Participant G)
“For us young nurses who are faced with so many critically ill patients who experience rapid changes in their conditions, we often have to communicate with doctors, especially senior doctors. If (we are) inexperienced, communication is slightly difficult. Additionally, because everyone has been working for a long time, it is difficult to know whether (the staff) are irritated or can communicate well with their colleagues. Because after a long shift, they may all be experiencing negative emotions.” (Participant F)
“I am not sure if it is because of my illness or because of my work. I often dream about saving patients, probably for both reasons… I hope the hospital will open a free psychiatric and sleep disorder clinic for us.” (Participant K)
Some participants mentioned maintaining a positive mindset through self-regulation and psychological suggestions as a stress management strategy and expressed the hope that managers would pay attention to the psychological states of frontline nurses and provide psychological support. One participant said,
“It is important to keep thinking positively. We are all in the same boat now (laughs). The other thing is to learn some relaxation techniques. Leaders should be aware of the psychological dynamics of nurses on the front line and provide psychological comfort.” (Participant F)
Theme 2: Mixed emotions
This theme focused on mixed emotional states, that is, the co-occurrence of positive and negative emotions in respiratory nurses during the Omicron outbreak. Within this theme, three subthemes were identified: feelings of loss and responsibility, feelings of frustration and achievement, and feelings of nervousness and security.
Feelings of loss and responsibility
Some of the participants in this study expressed a certain sense of loss. This feeling stemmed from nurses caring for patients, uncertain about when they might become infected, and their lack of a role in taking care of family. One of the participants said,
“There could still be a psychological setback. I went through the 2020 pandemic in Wuhan, and then I went to another city (to offer support) and witnessed another outbreak. Previously, we thought about how to protect ourselves while helping others. This time, it is unclear how to protect ourselves while treating others.” (Participant H)
Another participant said,
“My family members were infected. I was working hard and very busy, and I did not have the extra time or energy to care for them. My parents did not live with me, and I wanted to have time to get them some medicine and check on them. During that time, I was worried about their health because the risks for older people were high. I was worried that their health conditions would become more serious, and I was not caring for them.” (Participant I)
The majority of the participants in this study stated that they stayed in their jobs despite experiencing substantial and multiple pressures because of a sense of responsibility. One participant, who was asymptomatic and not sure if he was infected, said the following:
“I think we have to work and stick to the job. First, we have to go to work according to the schedule, which is the most important point, the duty. I cannot stay away from work just because I haven’t been infected. At this most critical point, running away at the first sign of difficulty is impossible. That is certainly not the right thing to do. The main thing is duty because that is one of the most fundamental qualities of an employee.” (Participant F)
Some participants who had symptoms indicated that their intention in returning to work without fully recovering was to allow other nurses to also have breaks. One participant mentioned,
“At the time, I had been off for 3 days. Some of my colleagues were just showing symptoms and had no breaks. I thought I should go to work so those colleagues could have breaks, so I picked myself up and came to work.” (Participant A)
Feelings of frustration and achievement
Some of the participants in this study reported that patient blaming made them feel frustrated. Some participants claimed that their frustration stemmed from not seeing a significant improvement in patient outcomes in the short term. Participants described their experiences as follows:
“When I came back to work after being sick, I had not fully recovered, and occasionally I moved a little slower. Some patients did not understand my situation. I felt despondent at that moment (tears).” (Participant A)
“It is very depressing. Intubated patients are difficult to wean from mechanical ventilation for an extended period, and even less severe patients still have symptoms.” (Participant G)
Most of the participants in this study reported feeling a sense of achievement. The reasons included receiving affirmation from patients or their families; noticing gradual improvement in patient conditions; being helpful to families, friends, or colleagues; and enhancing professional competence. The participants described their experiences as follows:
“Many patients expressed admiration for my hard work and understood the challenges I faced, some even telling me to take a break. Their empathy motivated me to continue making contributions.” (Participant D)
“When the patients were admitted, they were extremely unwell, struggling with speech and reluctant to move. Following treatment, they could eat independently, move about independently, and express gratitude for feeling better. Moments like this bring great happiness to me!” (Participant H)
“During this period, I received more calls from acquaintances for counselling and felt fulfilled. They asked questions, such as if azvudine was effective, and I could advise them on the optimal stage for taking medication. Consequently, I felt that I was valued and was motivated to be a respiratory nurse. We are also confident that the mortality rate in our ward is very low, and many patients have been discharged.” (Participant I)
“This experience can be considered a form of training, helping us develop specialized skills and gain personal insights. If we face a similar emergency in the future, we will possess greater knowledge and skills regarding how to tackle it.” (Participant F)
Feelings of nervousness and security
Some of the participants in this study expressed nervousness due to the fear of being infected and of passing the virus on to their family members. One participant who tested negative for SARS-CoV-2 antibodies described her feelings as follows:
“My workmates falling ill affected me. I did not know what the symptoms would be if I got it. It was that uncertainty. Therefore, going to work caused anxiety at the beginning of the outbreak. It is that feeling of not knowing if you will go down next… It is like there’s no escape.” (Participant H)
Another participant stated the following:
“I am feeling nervous. I am in daily contact with patients who have tested positive, and since I have elderly relatives and young children at home, I am more concerned about bringing the virus back with me. That is why, when I return home from work, I leave my clothes and shoes outside, and the first thing I do upon entering my home is shower. When I returned home, my children used to hug me, but I would say, “Stay back, stay back.” I had to take a shower before I embraced them. Will there be a second or third wave? Can elderly people and children withstand this? Will my health worsen over time?” (Participant B)
Some of the participants expressed that their work in the PCCM made them feel reassured:
“I feel that working in a hospital makes it easier to get help if I become infected. As a respiratory staff member, I feel safe.” (Participant K)
“ It is not really that worrying. I think I was in the PCCM, and if anything happened to me, everyone would save me. I’m in this department, and the backup is strong. ” (Participant C)
Theme 3: Perceived social support systems
The vast majority of participants talked about the social support systems they perceived and how these social support systems impacted them. Within this theme, four subthemes were identified: team cohesion, family support, head nurse leadership, and the impact of social media
Team cohesion
Most participants in this study reported that coworkers helped each other at work, comforted each other psychologically, and were more unified than before the epidemic. The following descriptions represented this subtheme:
“During that time, even though almost everyone was sick and very busy at work, the atmosphere in our department was amiable. Every time you were busy, others would come to help you, and so would I. No one slacked off or hid from work, and everyone worked hard. It was a positive boost because no one was dragging their feet.” (Participant B)
“In such a busy situation, our colleagues are more united. We help each other. It is more cohesive. Busier, but more in touch (smile).” (Participant C)
“After my colleagues got infected, they shared some of their feelings with me. It was not really that uncomfortable, so my mind quickly relaxed. When people’s symptoms subsided, their temperature dropped, or the pain in their bodies eased, you could sense their happiness. I also felt happy when I heard such news. I feel that this kind of happiness is different from usual.” (Participant H)
Family support
Some participants in this study indicated that the health and support of their families strongly supported them in focusing on fighting against the outbreak:
“My family was very supportive (laughs). Everyone was very supportive. They were trying to minimize my burden. Because I did not know if I was infected, but when they were infected, they drank water, took their own medicine, and took their temperature. They wore masks, and they disinfected at home. I think that this was also a kind of support. They did not delay buying food or cooking every day and did not stop cooking or eating just because they were lethargic after the infection. Therefore, I think that is a kind of support (laughs).” (Participant H)
“I think my family… my support system is stable (grin), so I think I would be fine (to work).” (Participant C)
Head nurse leadership
Some of the participants in this study indicated that the head nurses’ leadership had a significant impact on the nurses’ work experiences:
“Rational scheduling and decision-making by the nurse managers is important. Pairing senior nurses with junior nurses during scheduling can avoid several risks. It is also important to try to ensure that everyone gets enough rest while maximizing the potential of the frontline nurses.” (Participant F)
“One day, the on-call shift started. Zhang was on it, and she did not get a moment’s rest until the end of the shift, and neither did we. She came to help us. She helped everyone. Where we were busy, where she was, arranging that shift helped our whole team and individuals a lot.” (Participant B)
“Any shortage of supplies or equipment or emergency, just talk to the head nurse, and it all gets resolved, so it is not so draining to work.” (Participant D)
Impact of social media
In this study, some participants mentioned that social media use impacted their psychological feelings, as follows:
“There are some very positive short videos online. One of our colleagues and some well-known people have shared their personal experiences fighting the outbreak, and it has been helpful to see others actively confronting it.” (Participant H)
Some participants expressed the opposite view:
“It worries me a little bit because the reinfections that are rumoured online can be scary.” (Participant C).
This study describes the challenges faced by respiratory nurses caring for COVID-19 patients during the Omicron outbreak in China from late 2022 to early 2023. Specifically, the findings interpreted these experiences as multiple stressors, mixed emotions, and perceived social support systems.
Like in the study by Al Maqbali M [ 7 ], a significant proportion of participants in our study reported that they had psychological problems such as stress, anxiety, frustration, or sleep disturbance and expressed a need for psychological support. Falatah’s [ 12 ] study showed that nurses’ turnover intentions increased significantly during the COVID-19 pandemic compared with that before the pandemic, and stress, anxiety, and fear of disease were predictors of nurses’ turnover intentions. In contrast to those in other studies, the participants in our study expressed their sense of security, which stemmed from confidence in their own professional background and trust in their colleagues. A previous study emphasized that understanding the psychological needs of frontline nurses and providing them with tailored psychological support can improve their mental health status and promote quality responses to clinical nursing and public health emergencies [ 19 ]. In addition, a cross-sectional correlation study conducted by Hoşgör [ 20 ] revealed that there was a significant positive correlation between nurses’ psychological resilience and job performance during the COVID-19 pandemic. These findings show that adopting strategies to improve the psychological resilience of nurses is helpful for optimizing the efficiency of nursing work and improving the quality of patient care. Therefore, during a public health crisis, nurse managers should assess the mental health status of frontline nurses in a timely manner, understand in depth the sources of pressure experienced by nurses, and establish psychological treatment teams to provide offline or online psychological support in the form of one-on-one or group support to improve the mental resilience and physical health of nurses.
In our study, participants described their sources of perceived social support, such as support from their teams, family members, head nurses, and social media. This social support helped them cope with the challenges during this difficult time and encouraged them to provide nursing care to the best of their ability. The participants had positive expressions and emotions when discussing their perceived social support systems. These findings are consistent with the findings of the Shen study [ 21 ], which revealed that the greater the level of social support, the better the psychological condition of nurses during the COVID-19 pandemic. Therefore, we strongly recommend that hospital managers regularly visit clinics, interact with frontline nurses, praise their vital role in dealing with the outbreak, and take comprehensive measures to increase value awareness, including compensation, honorary certificates, and publicly recognizing nurses’ contributions. In addition, visiting nurses on the frontline will help address difficulties such as shortages of equipment and human resources in the early stages of outbreaks.
Conversely, some participants in our study reported that rumours on social media about the serious consequences of reinfection negatively affected them. This may be related to the fact that most of the study participants were both patients and caregivers at the beginning of the outbreak. This points to the importance of leading public health experts being organized by the executive branch to provide evidence-based information to the public through social media.
Consistent with the findings of previous research [ 22 ], some participants described concerns not only about their own health but also about the health of their family members. This highlights the necessity of extending support for frontline nurses to their family members, including providing medicine and medical counselling. In addition, developing contingency plans to ensure the timeliness and accessibility of social support systems is an issue that managers must address.
The results of this study showed that flexible shift scheduling, active communication, timely resolution of problems, and close working cooperation with nurses played crucial roles in facilitating frontline nurses’ responses to the outbreak. Nursing managers are critical in maximizing the retention of nursing human resources and maintaining productivity and efficiency in health care organizations. Nursing leadership styles strongly influence nurses’ happiness and work environments. Niinihuhta [ 23 ] suggested that nurse leaders should use a supportive and relationship-focused leadership style. Another systematic review conducted by Cummings [ 24 ] provided robust evidence that relational leadership styles, such as transformational and authentic leadership styles, are significantly associated with improved outcomes, including outcomes regarding job satisfaction, employee-work relationships, employee health and well-being, the organizational environment and productivity.
In contrast, leadership focusing only on task completion is insufficient for achieving positive nursing health and workforce outcomes. As revealed in the scoping review conducted by Sihvola [ 25 ], nurse leaders should adopt a relational leadership style and positive communication to support nurse resilience during the COVID-19 pandemic. Furthermore, as an extension of the relational leadership style, inclusive leadership could increase the psychological ownership of nurses and reduce turnover intentions [ 26 ].
Unlike in previous situations, most participants in our study had symptoms, such as coughing or weakness, while caring for their clients. Therefore, as the bellwether of frontline nursing caregivers, head nurses should consider the overall situation of hospital management when public health emergencies occur, pay attention to the needs of frontline nurses, consider nurses’ advice, tolerate nurses’ shortcomings and mistakes, and construct an organizational relationship with clear and transparent communication, updated information, flexible shift arrangements, and mutual trust among colleagues to achieve the common goals of organizations and individuals to defeat the pandemic.
According to the results of the present study, respiratory nurses generally work longer hours in the event of an outbreak. At the beginning of the outbreak, the care workload surged as a large number of patients flooded hospitals. As a result, the amount of time to required complete nursing records increased. Consequently, bedside care was commonly provided to patients during normal business hours, and care notes were commonly completed during off hours. In addition, staff shortages were exacerbated by the infection of most logistics staff, and nurses had to take over delivering meals to patients and transporting medical and living supplies.
To alleviate the acute shortage of nursing staff and improve the quality and efficiency of nursing care, attempts are being made worldwide to apply AI technology to care, including COVID-19 care. Kagiyama [ 27 ] reported that a telemedicine-based self-vital sign examination system could quickly and accurately obtain vital sign information by measuring and uploading COVID-19 patient data without the risk of spreading infections. Mairittha [ 28 ] integrated a spoken conversation system into a smartphone application for care records. They found that the method increased the documentation speed by approximately 58.3% compared to the traditional keyboard-based method. Alderden [ 29 ] explored an AI-based transparent machine learning model that could predict the risk of hospital-acquired pressure injuries in ICU patients with COVID-19. Other studies have shown that nurses already use AI to perform various tasks across multiple patient populations, such as assisting elderly patients or recovering patients with exercise and in pain management, communication, interviewing, and patient education [ 30 ]. Nurses should recognize the need using AI in care. Nurses should increase their awareness of AI development; actively communicate and collaborate with experts in related fields; and advocate for patient and nurse involvement in the design, implementation, and evaluation of all aspects of AI health technology to prepare for possible future public health events.
Limitations
All participants in this study were from a tertiary hospital in Wuhan, China. Therefore, the results of the current study may not be generalizable to other settings. Despite we utilized purposive sampling method to ensure diversity of opinions, the majority of participants were female, which was due to the relatively small proportion of male nurse in China. In addition, although our interviews began one month after the start of the outbreak, they took place for two weeks, which may have influenced the views and expressions of the participants over time.
Respiratory department nurses provided insight into their work experiences during the Omicron outbreak in China from late 2022 to early 2023. Despite experiencing exhaustion, nurses continued to take care of COVID-19 patients with the sense of responsibility of “angels without wings.” Respiratory nurses also experienced a sense of accomplishment from helping patients and a sense of security from their professional backgrounds. The mutual help of team members, support from family members, leadership by head nurses, and influence of social media are essential factors supporting frontline respiratory nurses in the fight against COVID-19. Hospital administrators should pay attention to the pressure and needs of frontline nurses during epidemics, improve psychosocial support systems, optimize the leadership styles of nurse managers, and actively explore the use of AI in the field of clinical nursing to improve nurses’ abilities to respond to public health emergencies.
Implications
The findings of this study reveal the multiple stressors and mixed emotions encountered by frontline respiratory nurses in combating COVID-19, which is helpful for nurse managers to develop comprehensive strategies that mitigate the adverse impact of these stressors and the negative emotions on nurses’ well-being and augment the positive emotions’ influence on nurses’ work engagement. Moreover, the identification of the nurses perceived social support system would assist policy-makers and hospital administrators in formulating more tailored polices to enhance their support for frontline nurses. Additionally, the design and implementation of training programs focusing on respiratory intensive care for nurses and leadership skills for charge nurse, will play a crucial role in effectively responding to extreme pandemic events. Furthermore, the researchers recommend that more qualitative research be carried out in different medical institutions and that more male nurses be included to improve understanding of the phenomenon. It is also suggested that further research be conducted to explore the psychosocial support needs of frontline nurses and ultimately improve their mental and physical health and quality of care for COVID-19 patients.
Data availability
The datasets generated and/or analyzed in this study are not publicly available because the data contain individual participant information, but are available from the corresponding author on reasonable request.
Abbreviations
Department of Pulmonary and Critical Care Medicine
Novel coronavirus disease 2019
Artificial intelligence
World Health Organization
Variants of concern
Chinese Center for Disease Control and Prevention
Respiratory intensive care unit
World Health Organization. Weekly epidemiological update on COVID-19 - Feb 1. 2023. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---1-february-2023 . Accessed 2 Feb 2023.
Joint COVID-19 Prevention and Control Mechanism of State Council. Diagnosis and treatment protocol for COVID-19 (10th edition). http://www.nhc.gov.cn/xcs/zhengcwj/202301/bdc1ff75feb94934ae1dade176d30936.shtml . Accessed 2 Feb 2023.
World Health Organization. TAG-VE statement on the meeting of Jan 3 on the COVID-19 situation in China. https://www.who.int/news/item/04-01-2023-tag-ve-statement-on-the-3rd-january-meeting-on-the-covid-19-situation-in-china . Accessed 2 Feb 2023.
National Health Commission of the People’s Republic of China. Transcript of the State Council Joint Prevention and Control Mechanism press conference on Jan 14, 2023. http://www.nhc.gov.cn/xcs/yqfkdt/202301/a68301ee500b436b989ec5be2a35cad2.shtml . Accessed 2 Feb 2023.
Gu L, Chang J, Wang J, Feng P, Xu H. Stress load of Chinese nurses in Fangcang Shelter Hospitals during the COVID-19 pandemic: a latent profile analysis. Front Public Health. 2023;10:1048358. https://doi.org/10.3389/fpubh.2022.1048358 .
Article PubMed PubMed Central Google Scholar
Podgorica N, Zenzmaier C, Rungg C, Bertini B, Perkhofer S. Facing the unknown COVID-19 pandemic: a qualitative study with nurses and nursing assistants in three European countries. Front Public Health. 2022;10:985702. https://doi.org/10.3389/fpubh.2022.985702 .
Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J Psychosom Res. 2021;141:110343. https://doi.org/10.1016/j.jpsychores.2020.110343 .
Article PubMed Google Scholar
Yuan Z, Wang J, Feng F, Jin M, Xie W, He H, et al. The levels and related factors of mental workload among nurses: a systematic review and meta-analysis. Int J Nurs Pract. 2023;29(5):e13148. https://doi.org/10.1111/ijn.13148 .
Doleman G, De Leo A, Bloxsome D. The impact of pandemics on healthcare providers’ workloads: a scoping review. J Adv Nurs. 2023;79(12):4434–54. https://doi.org/10.1111/jan.15690 .
Slettmyr A, Arman M, Andermo S, Malmberg C, Hällström Å, Hugelius K, et al. Intensive care nurses’ lived experience of altruism and sacrifices during the Covid-19 pandemic: a phenomenological study. J Adv Nurs. 2023;79(1):244–53. https://doi.org/10.1111/jan.15467 .
Fernandez R, Lord H, Halcomb E, Moxham L, Middleton R, Alananzeh I, et al. Implications for COVID-19: a systematic review of nurses’ experiences of working in acute care hospital settings during a respiratory pandemic. Int J Nurs Stud. 2020;111:103637. https://doi.org/10.1016/j.ijnurstu.2020.103637 .
Falatah R. The impact of the Coronavirus Disease (COVID-19) pandemic on nurses’ turnover intention: an integrative review. Nurs Rep. 2021;11(4):787–810. https://doi.org/10.3390/nursrep11040075 .
Wan Z, Lian M, Ma H, Cai Z, Xianyu Y. Factors associated with burnout among Chinese nurses during COVID-19 epidemic: a cross-sectional study. BMC Nurs. 2022;21(1):51. https://doi.org/10.1186/s12912-022-00831-3 .
Goldberg EE, Lin Q, Romero-Severson EO, Ke R. Swift and extensive Omicron outbreak in China after sudden exit from ‘zero-COVID’ policy. Nat Commun. 2023;14(1):3888. https://doi.org/10.1038/s41467-023-39638-4 .
Article ADS CAS PubMed PubMed Central Google Scholar
Bradshaw C, Atkinson S, Doody O. Employing a qualitative description Approach in Health Care Research. Glob Qual Nurs Res. 2017;4:2333393617742282. https://doi.org/10.1177/2333393617742282 .
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. https://doi.org/10.1097/ACM.0000000000000388 .
Colaizzi P. Psychological research as the phenomenologist views it. In: Vale RS, KingM, editors. Existential-phenomenological Alternatives for psychology. Oxford, England: Oxford University Press; 1978.
Google Scholar
Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir Program Evaluation. 1986;30:73–84. https://doi.org/10.1002/ev.1427 .
Article Google Scholar
Ding C, Wang L, Guo Z, Chen Y, Jin J. Psychological care needs for frontline nurses during the COVID-19 pandemic: a qualitative study. Front Public Health. 2022;10:1043515. https://doi.org/10.3389/fpubh.2022.1043515 .
Hoşgör H, Yaman M. Investigation of the relationship between psychological resilience and job performance in Turkish nurses during the Covid-19 pandemic in terms of descriptive characteristics. J Nurs Manag. 2022;30(1):44–52. https://doi.org/10.1111/jonm.13477 .
Shen YJ, Wei L, Li Q, Li LQ, Zhang XH. Mental health and social support among nurses during the COVID-19 pandemic. Psychol Health Med. 2022;27(2):444–52. https://doi.org/10.1080/13548506.2021.1944653 .
Thobane KF, Mulaudzi FM, Moagi MM. Improvement of the psychosocial support for frontline nurses in public hospitals during COVID-19 pandemic. J Nurs Manag. 2022;30(7):2461–9. https://doi.org/10.1111/jonm.13761 .
Niinihuhta M, Häggman-Laitila A. A systematic review of the relationships between nurse leaders’ leadership styles and nurses’ work-related well-being. Int J Nurs Pract. 2022;28(5):e13040. https://doi.org/10.1111/ijn.13040 .
Cummings GG, Tate K, Lee S, Wong CA, Paananen T, Micaroni SPM, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud. 2018;85:19–60. https://doi.org/10.1016/j.ijnurstu.2018.04.016 .
Sihvola S, Kvist T, Nurmeksela A. Nurse leaders’ resilience and their role in supporting nurses’ resilience during the COVID-19 pandemic: a scoping review. J Nurs Manag. 2022;30(6):1869–80. https://doi.org/10.1111/jonm.13640 .
Zeng D, Wang B, Chen W. Inclusive leadership can improve nurses’ psychological ownership and reduce their turnover intention under the normalization of COVID-19 prevention. Front Psychol. 2023;13:1100172. https://doi.org/10.3389/fpsyg.2022.1100172 .
Kagiyama N, Hiki M, Matsue Y, Dohi T, Matsuzawa W, Daida H, et al. Validation of telemedicine-based self-assessment of vital signs for patients with COVID-19: a pilot study. J Telemed Telecare. 2023;29(8):600–6. https://doi.org/10.1177/1357633X211011825 .
Mairittha T, Mairittha N, Inoue S. Integrating a spoken dialogue system, nursing records, and activity data collection based on smartphones. Comput Methods Programs Biomed. 2021;210:106364. https://doi.org/10.1016/j.cmpb.2021.106364 .
Alderden J, Kennerly SM, Wilson A, Dimas J, McFarland C, Yap DY, et al. Explainable artificial intelligence for predicting hospital-acquired pressure injuries in COVID-19-positive critical care patients. Comput Inf Nurs. 2022;40(10):659–65. https://doi.org/10.1097/CIN.0000000000000943 .
Buchanan C, Howitt ML, Wilson R, Booth RG, Risling T, Bamford M. Predicted influences of Artificial Intelligence on the domains of nursing: scoping review. JMIR Nurs. 2020;3(1):e23939. https://doi.org/10.2196/23939 .
Download references
Acknowledgements
The authors thank the participants in this study for sharing their experiences.
This study was supported by the Hubei key laboratory opening project of Health Commission of Hubei Province (2022KFH002) and general project of Health Commission of Hubei Province (WJ2021M150).
Author information
Authors and affiliations.
Department of Respiratory and Critical Care Medicine, Renmin Hospital of Wuhan University, No. 238, Jiefang Road, 430060, Wuhan, China
Wenzhen Yu, Ying Zhang, Yunyan Xianyu & Dan Cheng
You can also search for this author in PubMed Google Scholar
Contributions
W.Y., Y.Z., and D.C. conceptualized and designed the study. W.Y. collected the data. W.Y. and Y.Z. analyzed and interpreted the data. Y.X. acquired the funding and administered the projects. W.Y. wrote the original draft. W.Y., Y.Z., Y.X., and D.C. reviewed and edited the draft manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Dan Cheng .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the research and ethics committees of Renmin Hospital of Wuhan University (Approval NO: WDRY2023-K031). Before the interviews, all participants were verbally explained the details of the study, expected risks and benefits, and their right to withdraw at any time, and written informed consents were obtained. All the methods and procedures in this study are in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yu, W., Zhang, Y., Xianyu, Y. et al. Stressors, emotions, and social support systems among respiratory nurses during the Omicron outbreak in China: a qualitative study. BMC Nurs 23 , 188 (2024). https://doi.org/10.1186/s12912-024-01856-6
Download citation
Received : 23 November 2023
Accepted : 10 March 2024
Published : 21 March 2024
DOI : https://doi.org/10.1186/s12912-024-01856-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Working experience
- Pulmonary medicine
- Qualitative research
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Kerstin Emily Frailey - “PRACTICAL DATA QUALITY FOR MODERN DATA & MODERN USES, WITH APPLICATIONS TO AMERICA’S COVID-19 DATA"
Dissertation Advisor: Martin Wells
Initial job placement: Co-Founder & CEO
David Kent - “Smoothness-Penalized Deconvolution: Rates of Convergence, Choice of Tuning Parameter, and Inference"
Dissertation Advisor: David Ruppert
Initial job placement: VISITING ASSISTANT PROFESSOR - Cornell University
Yuchen Xu - “Dynamic Atomic Column Detection in Transmission Electron Microscopy Videos via Ridge Estimation”
Dissertation Advisor: David Matteson
Initial job placement: Postdoctoral Fellow - UCLA
Siyi Deng - “Optimal and Safe Semi-supervised Estimation and Inference for High-dimensional Linear Regression"
Dissertation Advisor: Yang Ning
Initial job placement: Data Scientist - TikTok

Four of the biggest problems facing education—and four trends that could make a difference
Eduardo velez bustillo, harry a. patrinos.

In 2022, we published, Lessons for the education sector from the COVID-19 pandemic , which was a follow up to, Four Education Trends that Countries Everywhere Should Know About , which summarized views of education experts around the world on how to handle the most pressing issues facing the education sector then. We focused on neuroscience, the role of the private sector, education technology, inequality, and pedagogy.
Unfortunately, we think the four biggest problems facing education today in developing countries are the same ones we have identified in the last decades .
1. The learning crisis was made worse by COVID-19 school closures
Low quality instruction is a major constraint and prior to COVID-19, the learning poverty rate in low- and middle-income countries was 57% (6 out of 10 children could not read and understand basic texts by age 10). More dramatic is the case of Sub-Saharan Africa with a rate even higher at 86%. Several analyses show that the impact of the pandemic on student learning was significant, leaving students in low- and middle-income countries way behind in mathematics, reading and other subjects. Some argue that learning poverty may be close to 70% after the pandemic , with a substantial long-term negative effect in future earnings. This generation could lose around $21 trillion in future salaries, with the vulnerable students affected the most.
2. Countries are not paying enough attention to early childhood care and education (ECCE)
At the pre-school level about two-thirds of countries do not have a proper legal framework to provide free and compulsory pre-primary education. According to UNESCO, only a minority of countries, mostly high-income, were making timely progress towards SDG4 benchmarks on early childhood indicators prior to the onset of COVID-19. And remember that ECCE is not only preparation for primary school. It can be the foundation for emotional wellbeing and learning throughout life; one of the best investments a country can make.
3. There is an inadequate supply of high-quality teachers
Low quality teaching is a huge problem and getting worse in many low- and middle-income countries. In Sub-Saharan Africa, for example, the percentage of trained teachers fell from 84% in 2000 to 69% in 2019 . In addition, in many countries teachers are formally trained and as such qualified, but do not have the minimum pedagogical training. Globally, teachers for science, technology, engineering, and mathematics (STEM) subjects are the biggest shortfalls.
4. Decision-makers are not implementing evidence-based or pro-equity policies that guarantee solid foundations
It is difficult to understand the continued focus on non-evidence-based policies when there is so much that we know now about what works. Two factors contribute to this problem. One is the short tenure that top officials have when leading education systems. Examples of countries where ministers last less than one year on average are plentiful. The second and more worrisome deals with the fact that there is little attention given to empirical evidence when designing education policies.
To help improve on these four fronts, we see four supporting trends:
1. Neuroscience should be integrated into education policies
Policies considering neuroscience can help ensure that students get proper attention early to support brain development in the first 2-3 years of life. It can also help ensure that children learn to read at the proper age so that they will be able to acquire foundational skills to learn during the primary education cycle and from there on. Inputs like micronutrients, early child stimulation for gross and fine motor skills, speech and language and playing with other children before the age of three are cost-effective ways to get proper development. Early grade reading, using the pedagogical suggestion by the Early Grade Reading Assessment model, has improved learning outcomes in many low- and middle-income countries. We now have the tools to incorporate these advances into the teaching and learning system with AI , ChatGPT , MOOCs and online tutoring.
2. Reversing learning losses at home and at school
There is a real need to address the remaining and lingering losses due to school closures because of COVID-19. Most students living in households with incomes under the poverty line in the developing world, roughly the bottom 80% in low-income countries and the bottom 50% in middle-income countries, do not have the minimum conditions to learn at home . These students do not have access to the internet, and, often, their parents or guardians do not have the necessary schooling level or the time to help them in their learning process. Connectivity for poor households is a priority. But learning continuity also requires the presence of an adult as a facilitator—a parent, guardian, instructor, or community worker assisting the student during the learning process while schools are closed or e-learning is used.
To recover from the negative impact of the pandemic, the school system will need to develop at the student level: (i) active and reflective learning; (ii) analytical and applied skills; (iii) strong self-esteem; (iv) attitudes supportive of cooperation and solidarity; and (v) a good knowledge of the curriculum areas. At the teacher (instructor, facilitator, parent) level, the system should aim to develop a new disposition toward the role of teacher as a guide and facilitator. And finally, the system also needs to increase parental involvement in the education of their children and be active part in the solution of the children’s problems. The Escuela Nueva Learning Circles or the Pratham Teaching at the Right Level (TaRL) are models that can be used.
3. Use of evidence to improve teaching and learning
We now know more about what works at scale to address the learning crisis. To help countries improve teaching and learning and make teaching an attractive profession, based on available empirical world-wide evidence , we need to improve its status, compensation policies and career progression structures; ensure pre-service education includes a strong practicum component so teachers are well equipped to transition and perform effectively in the classroom; and provide high-quality in-service professional development to ensure they keep teaching in an effective way. We also have the tools to address learning issues cost-effectively. The returns to schooling are high and increasing post-pandemic. But we also have the cost-benefit tools to make good decisions, and these suggest that structured pedagogy, teaching according to learning levels (with and without technology use) are proven effective and cost-effective .
4. The role of the private sector
When properly regulated the private sector can be an effective education provider, and it can help address the specific needs of countries. Most of the pedagogical models that have received international recognition come from the private sector. For example, the recipients of the Yidan Prize on education development are from the non-state sector experiences (Escuela Nueva, BRAC, edX, Pratham, CAMFED and New Education Initiative). In the context of the Artificial Intelligence movement, most of the tools that will revolutionize teaching and learning come from the private sector (i.e., big data, machine learning, electronic pedagogies like OER-Open Educational Resources, MOOCs, etc.). Around the world education technology start-ups are developing AI tools that may have a good potential to help improve quality of education .
After decades asking the same questions on how to improve the education systems of countries, we, finally, are finding answers that are very promising. Governments need to be aware of this fact.
To receive weekly articles, sign-up here

Consultant, Education Sector, World Bank

Senior Adviser, Education
Join the Conversation
- Share on mail
- comments added
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

A quantitative and qualitative analysis of the COVID–19 pandemic model
Sarbaz h.a. khoshnaw.
a Department of Mathematics, University of Raparin, Ranya, Sulaimani, Iraq
Muhammad Shahzad
b Department of Mathematics and Statistics, Hazara University, Mansehra 21300, Pakistan
Mehboob Ali
Faisal sultan.
Global efforts around the world are focused on to discuss several health care strategies for minimizing the impact of the new coronavirus (COVID-19) on the community. As it is clear that this virus becomes a public health threat and spreading easily among individuals. Mathematical models with computational simulations are effective tools that help global efforts to estimate key transmission parameters and further improvements for controlling this disease. This is an infectious disease and can be modeled as a system of non-linear differential equations with reaction rates.
This work reviews and develops some suggested models for the COVID-19 that can address important questions about global health care and suggest important notes. Then, we suggest an updated model that includes a system of differential equations with transmission parameters. Some key computational simulations and sensitivity analysis are investigated. Also, the local sensitivities for each model state concerning the model parameters are computed using three different techniques: non-normalizations, half normalizations, and full normalizations.
Results based on the computational simulations show that the model dynamics are significantly changed for different key model parameters. Interestingly, we identify that transition rates between asymptomatic infected with both reported and unreported symptomatic infected individuals are very sensitive parameters concerning model variables in spreading this disease. This helps international efforts to reduce the number of infected individuals from the disease and to prevent the propagation of new coronavirus more widely on the community. Another novelty of this paper is the identification of the critical model parameters, which makes it easy to be used by biologists with less knowledge of mathematical modeling and also facilitates the improvement of the model for future development theoretically and practically.
1. Introduction
The history of the coronaviruses started from the 1930s when the infectious bronchitis virus (IBV) infection was caused by the domesticated chickens. In humans, it was firstly reported in the 1960s [1] . To avoid stigmatizing the virus's origins in terms of populations, geography, or animal associations the WHO termed as COVID-19 in December 2019. This virus involves serious respiratory tract infections [ 2 , 3 ]. Detected in Wuhan City, Hubei Province of China, this virus might be transferred to the seafood market [ 4 , 5 ] and then internationally via domestic/commercial air traveler carriers [6] . After that, an emergency has been declared in infected areas of the world and a serious public health concern has been paid at a global level. While to stop the impact of this infection and to avoid further spreading some mathematical estimations are also being performed at each level [7] .
Spreading the novel coronavirus (COVID-19) has become a very difficult global issue. For May 15th, 2020, there were 4609,787 confirmed cases, 307, 528 deaths, and 1742,813 recovered cases around the world [8] . This virus has been spread more quickly around the world, it is very important to know its dynamics and predications. Although there were several proposed studies based on mathematical tools, computational simulations, clinical, and examination tests for controlling the disease, there are still different dimensions about this issue that can be further improved.
Recently, mathematical modeling of the COVID-19 disease has been investigated by several mathematical and computational researchers for the prediction of the disease dynamics. One of the well-known concepts in epidemiology is the basic reproduction number (or it sometimes is called the basic reproductive ratio). This ratio is a quantity and it is denoted by R 0 . This is the average number of secondary infections produced by a single primary infection in a population where everyone is susceptible. Based on the developed approaches of mathematical epidemiology models, this quantity becomes an essential tool to understand epidemiological concepts and identify key critical parameters for such models. The value of this quantity has been changed for the confirmed cases of Coronavirus. According to a study published recently, the median value of R 0 was about 2.28 during the early stage experienced [9] . Based on another study, this quantity is about 2.489. They suggested a discrete-time stochastic epidemic model with binomial distributions to study the transmission of the disease [10] . There is also a developed compartmental model based on the clinical progression of the disease, the epidemiological status of the individuals, and intervention measures [11] . According to this study, the estimation of the basic reproduction number is very high and it was about 6.47. The idea of the next-generation matrix approach was used to calculate the basic reproduction number for the COVID-19 models, this is presented in [12] . According to their study, this ratio is bout 3.58. Furthermore, an updated model was proposed to estimate the transmission risk of the novel coronavirus, their calculations relate to a time-dependent dynamic model of contact and diagnosis rate. This helps us to re-estimated the daily reproduction number [13] .
One of the key parameters that can be accumulated from the confirmed cases is the serial interval. The serial interval is a time interval between primary patients (infecters) and the second patient (infectees). This parameter helps investigators to find epidemic transmission links between confirmed cases and uses for design healthcare program strategies [14] . The serial interval is widely used for describing models dynamics of infectious disease. This may help us to understand the effect of contact among individuals and how transmits the virus more quickly. Recently, the serial interval has been calculated for the COVID-19, this estimates by 4.6 days [15] . A reported study mentioned that the mean serial interval for COVID-19 was calculated as 3.96 days. This considerably shorter than the mean serial interval calculated for SARS 8.4 days and MERS 14.6 days [16] .
Although, there is a variety of modeling approaches that have been proposed so far for prediction and evaluation of the COVID-19 disease, there are more questions that can still be answered. There are some related works that sensitivity analysis used in their studies [ 13 , 17 ]. They used this technique only for special variables and parameters. More recently, mathematical modeling has been used to describe this disease in different views. Transmission and mitigation strategies for COVID-19 presented in [18] , response strategies for COVID-19 epidemics in African settings shown in [19] , the effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic explained in [20] , mathematical recommendations to fight against COVID-19 investigated in [21] , the feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts presented in [22] , a mathematical modeling approach in the Spread of the COVID-19 described in [23] , the reproductive number of COVID-19 is higher compared to SARS coronavirus presented in [24] .
Defining such proposed models based on the mass action law with transmission parameters and identify some critical model elements could improve the outcomes further. An issue that has not been explained very well for this new virus is identifying the local sensitivities for non-normalizations, half normalizations, and full normalization techniques in commotional simulations. Here, we are proposing a mathematical model to estimate the transmissibility with the dynamical view of the virus transmission. For the complex model of COVID-19 given in this paper, it is vital to pay more attention to identify critical model elements based on sensitivity analysis and computational results more widely and accurately. Another contribution of this paper is analyzing the suggested model based on different values of the model parameters in commotional simulations. This is also an important step forward to understand how changing the model dynamics and predicting the spread of this virus in the future. The main contribution here is to understand the impact of each model parameter on the model states, this is given in our computational simulations and calculating the local sensitivities. This will help to quantify possible disease control strategies with further improvements and recommendations. Results in this study provide effective roles in further suggestions and preventions theoretically and practically. On possible theoretical suggestion is that these results could help biologists to understand the model dynamics and parameter transmissions. This may give further improvements and analyze the complex models in computational simulations. While the results here could also give practical suggestions. One practical improvement for controlling this disease could be reducing the contact between asymptomatic infected, reported, and unreported infected classes because their transmission parameters are very sensitive based on our computational simulations.
The idea of chemical kinetic theory is an important approach for understanding and representing the biological process in terms of model equations. The important assumptions to build such models are model states, parameters, and equations. This is because it helps the investigation of mathematical modeling effectively and easily [25] , [26] , [27] , [28] , [29] , [30] , [31] , [32] , [33] , [34] , [35] . Therefore, we present here the basics of our calculations. We consider n irreversible chemical reactions and m chemical components with a stoichiometric equation given below
where x j for j = 1 , 2 , … , m are chemical species, a ij and b ij are stoichiometric coefficients (non-negative integers), α i > 0 , i = 1 , 2 , … , n are chemical interaction parameters. The model reaction rates are simply defined based on the classical theory of mass-action law
The chemical reactions can be expressed as a system of differential equations with initial components
where π i = b i j − a i j , for i = 1 , 2 , … , n and j = 1 , 2 , … , m . Therefore, Eq. (3) takes the form
where x ∈ R m and α ∈ R n . The functions h j , j = 1 , 2 , … , m are often non-linear therefore model differential equations may not solve analytically. The more details and descriptions about chemical reactions and their differential equations with some applications in system biology can be found in [ 25 , 36 , 37 ]. An important technique to analyze system 4 is the idea of sensitivity analysis. According to this approach, the sensitivity of each variable concerning parameters can be calculated. The main equation of sensitivity is given below
The first order derivatives given in Eq. (5) represent the time-dependent sensitivities of all variables { x j , j = 1 , 2 , … , m } concerning each parameter value { α p , p = 1 , 2 , … , n }
Furthermore, the differential equations can be solved for sensitivity coefficients as below
Using the chain rule of differentiation, Eq. (6) can be further driven and the sensitivity equations take the Jacobian matrix as follows
where the matrices S , H α p and J are defined by
For more details and applications of sensitivity analysis in the field systems biology, the reader can see in [ 25 , [38] , [39] , [40] , [41] , [42] , [43] , [44] , [45] ]. The local sensitivity values are given in Eq. (7) can be computed using SimBiology Toolbox in MATLAB with three different techniques: non-normalizations, half normalizations, and full normalizations. Accordingly, in a complicated modeling case like new coronavirus dynamics, it is necessary to pay attention to sensitivity analysis more accurately and widely. This provides one to identify the key critical model parameters and to improve model dynamics.
3. An updated model for coronavirus disease
The classical models of epidemic diseases normally include components (individuals) and interaction changes among components in the population. In other words, for an epidemic network model, nodes are individuals, and edges are contacted among individuals. This representation helps us to understand infectious disease models in terms of a graphical network. There are some recently proposed models for presenting the dynamical equations of COVID-19 [26] , [46] , [47] , [48] , [49] , [50] , [51] , [52] , [53] , [54] . The model initial populations and interaction parameters are mainly obtained for the confirmed cases in China. The main idea of the models is based on clinical progression, epidemiological individuals, and intervention measures. In this paper, we develop the previous model presented in [55] . We then extend the suggested model structure by including the recovered individuals (R), the unreported symptomatic death rate ( α 1 U ) and reported symptomatic death rate ( α 2 W ). The model network diagram and the interaction individual components demonstrated in Fig. 1 . The COVID-19 model digraph can be expressed as a graph G = ( N , L ) , where G is the model graph, N = ( S , I , U , W , R ) is the set of nodes (states), L = { v 1 , v 2 , v 3 , v 4 , v 5 , v 6 , v 7 } is the set of links (reactions).

The model interaction individuals for the COVID–19 epidemic outbreak with reaction rates.
Thus, let us consider the human groups separated into 5 different groups.
- 1 Susceptible group (S). This group presents a healthy individual.
- 2 Asymptomatic group (I). This group presents an infected individual in the early stage of infection. They do not show any symptoms, but capable to infect through droplets or direct contact with the susceptible individual.
- 3 Symptomatic unreported group (U). This group presents an individual who gets infected, had symptoms of COVID-19 but did not detect by the government as a COVID-19 suspect.
- 4 Symptomatic reported group (W). This group presents an individual who gets infected, shows symptoms of COVID-19, and detected by the government, either from a rapid test or from voluntary action to report to the hospital. We assume that all individuals in this class will get a specific treatment and supervision, whether it's through monitored isolation or treatment in the hospital.
- 5 Recovered group (R). This group present individual who get recovered from COVID-19, and had a temporal immunity.
The transmission diagram which illustrates the interaction between each group described in Fig. 1 . The developed model here has six parameters that can be analyzed in computational simulations. They are defined as interactions rate constants between individual groups. The contacts between different states (individuals) are as follows. Susceptible people ( S ) move into the infected people ( I ) when they are asymptomatic infected at the transition rate β S ( I + U ) . After that, the asymptomatic infected individuals ( I ) either move into the reported symptomatic infected individuals ( W ) with the transition rate γI or turn into the unreported symptomatic infected individuals ( U ) with transition rate δI . Both groups W and U move into the recovered individuals ( R ) with the transition rates ηW and ηU , respectively. In addition to that some unreported and reported infected individuals may die with transition rates α 1 U and α 2 W , respectively.
The model reactions with their rats are shown below:
where v 1 = β S ( I + U ) , v 2 = γ I , v 3 = δ I , v 4 = η W , v 5 = η U , v 6 = α 1 U ,
Furthermore, the model's constant parameters and initial states with their definitions are described in Table 1 . Using Eqs. (2) – (4) , the model dynamics are described by the following system of non-linear ordinary differential equations
The model reaction constants (parameters) and initial individual populations for COVID–19 epidemic outbreak with their biological definitions, all data are confirmed cases in China presented in [55] .
The model initial populations are expressed in the following equation
6. Computational results
Analyzing epidemic disease models with a high number of elements sometimes cannot be well understood only by biological tools. This is why mathematical models are used, such models help and provide a good environment to analyze infectious diseases more widely and easily. Theoretical studies may help biologists to predict future model dynamics and identify critical model parameters. In the case of COVID-19, the suggested mathematical models are effective tools that give estimations and suggestions about controlling the virus and further preventions more effectively.
The values of parameters and initial populations in this study are obtained from the WHO situation report (the National Health Commission of the Republic of China) presented in [55] . We calculate the numerical approximate solutions of the model equations (9) for different parameters and initial populations using System Biology Toolbox (SBedit) for MATLAB; see Fig. 2 , Fig. 3 , Fig. 4 , Fig. 5 , Fig. 6 . Accordingly, there are different model dynamics for initial population model states and estimated parameters. Computational numerical simulations are calculated in two-dimensional planes for model parameters and initial populations. Results in this study provide a good step forward in predicting the model dynamics in the future for development programs, interventions, and health care strategies.

Computational simulations for the model states given in system (9) of the COVID–19 using MATLAB; there are model dynamics of (a) susceptible individuals, (b) asymptomatic infected individuals, (c) unreported symptomatic infected individuals, (d) reported symptomatic infected individuals, (e) recovered individuals.

Computational simulations for the model states given in system (9) of the COVID–19 using MATLAB; there is the relationship between the asymptomatic infected people and (a) susceptible individuals, (b) unreported symptomatic infected individuals, (c) reported symptomatic infected individuals, (d) recovered individuals.

The effect of transition rate δ on (a) asymptomatic infected individuals, (b) unreported symptomatic infected individuals, (c) reported symptomatic infected individuals, in computational simulations using MATLAB parameters used δ = 0.0285 , 0.15 , 0.6 .

The effect of transition rate γ on (a) asymptomatic infected people, (b) unreported symptomatic infected people, (c) reported symptomatic infected people, in computational simulations using MATLAB parameters used γ = 0.1142, 0.26, 0.32.

The effect of parameter η on (a) unreported symptomatic infected people, (b) reported symptomatic infected people, (c) recovered people, in computational simulations using MATLAB parameters used η = 0.1428, 0.05, 0.02.
Fig. 2 shows the model dynamics of susceptible, asymptomatic infected, reported symptomatic, and unreported symptomatic individuals. The number of susceptible populations decreases gradually and becomes stable after 60 days while the dynamics of recovered people increase and get flat again after 60 days. Interestingly, the number of infected individuals in both asymptomatic and symptomatic groups is dramatically changed between 40 days to 80 days. Furthermore, Fig. 3 explains the relationship between infected people with the other groups in the COVID-19. It can be seen that there are the same dynamical relations for reported and unreported symptomatic states whereas there are slightly different model dynamics for susceptible and recovered groups.
Fig. 4 shows that the impact of transition rate δ on asymptomatic infected reported symptomatic infected and unreported symptomatic infected individuals. The effect of this parameter can easily occur on the variables I, U , and W . For example, if the value of δ is increased from 0.0285 to 0.6 then the number of unreported symptomatic infected people is dramatically increased, see Fig. 4 (b). On the other hand, there will be more asymptomatic infected and reported symptomatic infected cases when the values of transition rate δ become smaller and smaller, see Figs. 4 (a) and 4(c).
Fig. 5 shows that the impact of transition rate γ on asymptomatic infected people reported symptomatic infected people and unreported symptomatic infected people. The effect of this parameter can easily occur on the variables I , U , and W . It can be seen that the model dynamics for such states become more flat when the value of γ is increased. This is an important key element for controlling this disease.
Fig. 6 shows that the impact of parameter η (average time that infected people have symptoms) on the dynamics of unreported symptomatic, reported symptomatic, and recovered individuals. The number of both unreported and reported infected people are significantly increased when the value of η becomes smaller, see Figs. 6 (a) and 6(b). Conversely, the dynamics of recovered people dramatically grow and become stable very quickly when the value of η gets bigger and bigger, see Fig. 6 (c)
Another important step of parameter analysis is using the idea of local sensitivity analysis presented in Eq. (7) . We use SimBiology Toolbox for MATLAB to calculate the local sensitivity of each model state concerning model parameters for the model equations (9) . We compute the model sensitivities using three different techniques: non-normalizations, half normalizations, and full normalizations; see Figs. 7 . Interestingly, results provide us further understanding of the model and give one to identify the key critical model parameters. For example, it generally seems that the communication rate between asymptomatic infected and unreported symptomatic infected, transition rate between asymptomatic infected and reported symptomatic infected, the average time that infected people have symptoms are very sensitive parameters concerning model variables in spreading this disease among people. On the other hand, the other parameters are less sensitive to the model dynamics, they are unreported symptomatic death rate, reported symptomatic death rate and transition rate between susceptible and asymptomatic infected people. As a result, identifying critical model parameters in this study based on computational simulations is an effective way to further study the model practically and theoretically and give some suggestions for future improvements of the novel coronavirus vaccination programs, interventions, and controlling the spread of disease.

The sensitivity of each model state concerning model parameters in computational simulations for the coronavirus disease (COVID–19); (a) non-normalization sensitivity, (b) half normalization sensitivity, (c) full normalization sensitivity.
Accordingly, some findings and computational results are given based on the suggested approaches for the updated model of the COVID-19. We can mainly summarize them as the points given below:
- 1 The model dynamics of susceptible, asymptomatic infected, both reported and unreported symptomatic individuals, recovered individuals are computed using System Biology Toolbox (SBedit) in MATLAB. It can be seen that the relationship between infected people with the other groups in the COVID-19 model. There are the same dynamical relations for reported and unreported symptomatic states whereas there are slightly different model dynamics for susceptible and recovered groups.
- 2 The impact of transition rate δ on asymptomatic infected reported symptomatic infected and unreported symptomatic infected individuals is investigated. This parameter has an effective role in the dynamics of I, U , and W .
- 3 The transition rate γ has also affected asymptomatic infected people, reported symptomatic infected people, and unreported symptomatic infected people. It can be seen that the model dynamics for such states become more flat when the value of γ is increased. This is an important key element for controlling this disease.
- 4 The number of both unreported and reported infected people are significantly increased when the value of η becomes smaller whereas the dynamics of recovered people dramatically grow and become stable very quickly when the value of η becomes large.
- 5 The local sensitivity of each model state concerning the model parameters computed using three different techniques: non-normalizations, half normalizations, and full normalizations. Interestingly, results provide us further understanding and identifying the key critical model parameters. It can be concluded that the transmission parameters between asymptomatic infected and both reported and unreported symptomatic infected, the average time that infected people have symptoms are very sensitive parameters concerning model variables in computational simulations.
7. Discussions
Several healthcare strategies and preventions have been discussed and suggested as global efforts to reduce the impact of the new COVID-19 around the world. Although, this virus still spreads quickly and millions of people have been infected so far, but all scientific attempts give a great step forward to control this disease and minimizing the impact of such threats on the community. Currently, there are a variety of studies both theoretically and practically discussed and investigated in this area. One of the effective tools that could be used to describe such diseases is mathematical modeling. Mathematical modeling with computational simulations provides estimations and predictions about the dynamics of model states and parameters. However, having many suggested models in different countries makes the parameter estimations, predictions, and understandings of the disease remain unclear.
An issue that has not been well discussed and explained for this new virus is identifying the model critical elements. In this study, we computed the model dynamics for the different model parameter values. This provides us how the number of each model class changes concerning to the model parameters. Based on the results obtained here, we can simply understand the model critical parameters. For instance, the transmission parameter between asymptomatic class and the unreported symptomatic class becomes a key critical element and it has a great role in speeding this disease. However, the key critical model parameters may slightly change if we use different data reported for another country. Therefore, it can be argued that computational results and simulations based on the suggested models may give good approximations and predictions.
Another issue that can be discussed for the COVID-19 is the identification of the model sensitive parameters. This has also not well explained recently. In this work, we have used the idea of local sensitivities for non-normalizations, half normalizations, and full normalizations techniques in commotional simulations. For the complex model of COVID-19 given in this paper, it is vital to pay more attention to identify critical model elements based on sensitivity analysis and computational results more widely and accurately. Results in this paper become an important step forward to understand the model dynamics more widely. This provides to identify critical model parameters and how each model individual can be affected by the other model individuals. For example, results here show that almost all model states are sensitive to the critical model parameters { γ , δ , η } . On the other hand, such critical model parameters can be changed to the other model parameters when we use another set of initial states and parameters. Interestingly, the suggested approach here can be further developed and applied to a wide range of complex models of the COVID-19. It can work more effectively for identifying the model key elements. This provides us the suggested approaches here work very well for the COVID-19 models compared to the recently suggested techniques.
8. Conclusions
Global efforts and preventions of the speeding COVID-19 cannot be well understood only by biological and healthcare tools. Some mathematical models have been investigated for further improvements and give estimations for such model parameters. An issue that can be further studied is identifying key critical model parameters. This helps international efforts to pay more attention to the sensitive elements. The suggested coronavirus disease (COVID–19) model here is a complicated one, and it requires some mathematical tools to have improvements in interventions and healthcare programs.
The used model in this paper has further improved based on the computational results using MATLAB for different initial populations and parameters. Some main results can help in understanding the suggested model more widely and effectively. By using computational simulation, we identify some key critical parameters that have a great role in spreading this virus among the model classes. One of the identified key parameters is the transmission rate between asymptomatic infected and reported symptomatic individuals. This is an important finding in the understanding of the COVID-19 and how this virus spreads more quickly. Some other critical model parameters have investigated in this paper. For example, the transmission parameter between asymptomatic infected and unreported symptomatic individuals has a great impact on the dynamics of the model states. Besides these findings provide additional information about estimations and predictions for the number of infected individuals. Accordingly, our results in identifying key parameters are broadly consistent with clinical and biological findings.
Remaining issues are subject to sensitivity analysis. This is also an important issue that can be further studied. We have applied the idea of local sensitivity to calculate the sensitivity of each model state concerning model parameters for the updated model of the COVID-19. Three different techniques are investigated which are non-normalizations, half normalizations, and full normalizations. These provide us an important step forward to identify critical model elements. By using local sensitivity approaches we concluded that almost all model states are sensitive to the critical model parameters { γ , δ , η } . This becomes a great step forward and helps international attempts regarding the COVID-19 pandemic outbreak. This may help to reduce the number of infected individuals from the disease and to prevent the coronavirus more widely in the community. It can be concluded that the identified factors can be controlled to reduce the number of infected individuals. Overall, our results demonstrate a strong effect of the key critical parameters on the spreading COVID-19.
Therefore, based on the effect of each involved parameters over the model states, more suggestions and interventions can be proposed for controlling the COVID-19 disease. That will be useful for any interventions and vaccination programs. Accordingly, the healthcare communities should pay more attention to the quarantine places for controlling this disease more effectively. It can be strongly suggested that anyone in the quarantine places should be separated from the others and should use only their separate equipment, bedroom, and toilet to prevent the transmission of the virus through the touching of shared surfaces. Another suggestion is that reducing the contact between asymptomatic-symptomatic groups and susceptible groups, this is effectively minimizing the number of infected people. It seems necessary to plan a certain strategy to put the asymptomatic infected individuals on quarantine places sooner rather than later. Future research on identifying key critical elements might extend the explanations of the new COVID-19 more widely. It will be important that future research investigates more suggested transmissions between the model groups. For example, the model will further improve by adding two transmission paths, one of them is between unreported symptomatic infected and reported symptomatic infected, the other one is between asymptomatic infected and recovered individuals.
Declaration of Competing Interest
The authors declare that there are no competing interests.

IMAGES
VIDEO
COMMENTS
Additionally, apart from the physical effects of. COVID-19, significant psychological effects such as anxiety, depression, and loneliness. are shown to affect individuals of all ages including the older adult population, individuals aged 65 years and older (Wang et al., 2020). In a prevalence study of the rates.
As of March 2022, the United States has experienced 79.6 million cases of. COVID-19, and of those cases, 968,839, or 1.2%, resulted in death (Elflein, 2022). The South Dakota Department of Health recorded its first case of COVID-19 in South. Dakota on March 30, 2020 (Haskins, 2020).
The COVID-19 pandemic has caused widespread infection, school closures, and high rates of job loss. Much of the current research has focused on the clinical features of COVID-19 infection, but the family well-being consequences of COVID-19 are less well documented. The goal of the current study is to describe parent and child well-being
A caring teacher- student relationship helps students feel accepted, liked, and connected to others (OECD, 2019). The COVID-19 pandemic has threatened to exacerbate the problem of school connectedness between students as evidence has suggested that this has been at a decline over the past 15 years (OECD, 2017).
determining students' COVID-19 experiences. For example, the expected probability of delaying graduation due to COVID-19 increases by approximately 25% if either a student's subjective probability of being late on a debt payment in the following 90 days (a measure of nancial fragility) or subjective probability of requiring
Thinking about COVID-19 and your introduction The personal and professional context of your thesis is likely to have changed as a result of COVID-19. The changes implied are immediate and short-term, but there will also be long term implications (for example, online teaching, the role of the state, levels of unemployment, return to deepened
environment during the COVID-19 pandemic. Data were collected from semistructured interviews with 10 middle managers who were responsible for managing employees during the shift to remote work during the COVID-19 pandemic. The critical event approach was used to analyze the data and four conceptual categories emerged: (a)
An Abstract of the Thesis of. Lucy Hudson for the degree of Bachelor of Science in the Department of Economics to be taken June 2021. Title: Pandemic Economics: A Case Study of the Economic Effects of COVID-19 Mitigation Strategies in the United States and the European Union. Approved: Assistant Professor Keaton Miller, Ph.D.
Keywords: dissertation writers, COVID-19, anxiety, productivity, dissertation writing anxiety, doctoral student ... For example, many students experienced lab closures that could potentially delay the completion of their research (Elmer & Durocher, 2020), while others had to adapt and change their ...
A thesis submitted to the faculty of The University of Mississippi in partial fulfillment of the requirements of the Sally McDonnell Barksdale Honors College. ... for COVID-19, but the physician assured me I didn't have it. I packed up my bags and left to stay at my boyfriend's family house just outside of Oxford. I .
emotional exhaustion while 556 (27.6%) nurses marked high depersonalization while working. caring for COVID-19 patients (Hu, et al, 2020). A majority of participating nurses also disclosed. that they were experiencing moderate (28%) and high (36.2%) levels of fear when delivering.
The sample includes graduate students who began dissertation writing in Taiwan during the COVID-19 pandemic period. The majority of the respondents are female and from South East Asia. Table 1 provides background information of these interviewees.
The novel COVID-19 pandemic's impact on college students is unprecedented. College students are a priority population for health promotion and disease prevention [], and universities are unique settings that can affect the health of a larger segment of the population.College campuses are densely populated, with students living in close proximity to others; this means that college students can ...
A thesis submitted to the Johns Hopkins University in conformity with the requirements for the degree of Master of Science ... COVID‐19 such as drug overdoses and suicide surpassed the deaths from the disease itself (4). ... For example, the heart must work harder when epinephrine is released, leading to an increase in heart rate, breathing ...
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the ...
This article provides a comprehensive literature review on coronavirus disease 2019 (COVID-19), the infectious disease caused by a new strain of coronavirus that emerged in China in late 2019. It covers the epidemiology, clinical features, diagnosis, treatment, and prevention of COVID-19, as well as the current challenges and future perspectives.
All Theses And Dissertations Theses and Dissertations 12-2020 COVID-19: Descriptive Case Study Of A K-8 School District's Abrupt Transition To Remote Learning From A Traditional In-Person Model ... COVID-19 symptoms include cough, fatigue, loss of taste and smell, muscle pains,
July/August 2020 (Volume 29, Number 7) Defending My PhD Thesis in the Time of the Coronavirus. By Danielle Sofferman. Ten years ago I attended the Conference for Undergraduate Women in Physics (CUWiP). Once I returned to my undergrad institution, at Adelphi University, I was ecstatic and eager to do research.
Introduction The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. In addition, with the widespread use of social media, rumours ...
Content of a COVID-19 Thesis Impact Statement. Following is some examples and advice of what and what not to include in your COVID-19 Thesis Impact Statement. How your planned research activities such as topic, research question, methods and data collection and/or the scope of your research were disrupted or changed due the pandemic.
Graduate Theses, Dissertations, and Problem Reports 2021 COVID-19 vaccine rollout: Examining COVID-19 vaccination perceptions and intention among nurses Emilee T. Austin ... an online survey with a convenience sample recruited through the WV Nurses Association. Specifically, there were 328 nurses recruited, then screened for fully vaccinated ...
frontline nurses who reported not having attended for example a Coronavirus related training had increased fears of getting the Coronavirus. However, the study discovered that addressing the fear of Coronavirus led to improved job outcomes in frontline nurses, such as increased job satisfaction, decreased stress levels and lower intent to leave the
Objective To study the association between COVID-19 vaccination and the risk of post-COVID-19 cardiac and thromboembolic complications. Methods We conducted a staggered cohort study based on national vaccination campaigns using electronic health records from the UK, Spain and Estonia. Vaccine rollout was grouped into four stages with predefined enrolment periods. Each stage included all ...
The COVID-19 pandemic highlighted the fragility of health systems worldwide, with more than 90% of countries reporting interruptions to essential health service delivery. ... Some regions and countries are publishing more research papers than others (for example, a large proportion of the articles are published in China, Korea, and Iran, among ...
Abstract. Coronavirus (COVID-19) endemic is growing exponentially in the whole world. Researchers, technologists, doctors and other healthcare workers are working day and night on the development of vaccine and medicinesto control and treat this virus. SARS-CoV-2 is the name of the virus responsible for causing COVID-19 disease, which is highly ...
At the press conference of the Joint COVID-19 Prevention and Control Mechanism of the State Council on January 14, 2023, the number of hospitalizations due to COVID-19 reached a peak of 1.63 million on January 5, and from December 8, 2022, to January 12, 2023, a total of 59,938 deaths related to hospitalizations due to COVID-19 occurred in ...
Kerstin Emily Frailey - "PRACTICAL DATA QUALITY FOR MODERN DATA & MODERN USES, WITH APPLICATIONS TO AMERICA'S COVID-19 DATA" Dissertation Advisor: Martin Wells Initial job placement: Co-Founder & CEO David Kent - "Smoothness-Penalized Deconvolution: Rates of Convergence, Choice of Tuning Parameter, and Inference" Dissertation Advisor: David Ruppert Initial job placement: VISITING ...
In 2022, we published, Lessons for the education sector from the COVID-19 pandemic, which was a follow up to, Four Education Trends that Countries Everywhere Should Know About, which summarized views of education experts around the world on how to handle the most pressing issues facing the education sector then.We focused on neuroscience, the role of the private sector, education technology ...
OHSU has committed its entire organization to deploying COVID-19 vaccines, starting with difficult-to-reach community members and underserved communities. The university has also engaged students and trainees to vaccinate Oregonians.. After federal and state authorities recommended two COVID vaccines for children as young as 6 months old in June 2022, OHSU organized appointment-only ...
The COVID-19 model digraph can be expressed as a graph G = ( N, L), where G is the model graph, N = ( S, I, U, W, R) is the set of nodes (states), L = { v 1, v 2, v 3, v 4, v 5, v 6, v 7 } is the set of links (reactions). The model interaction individuals for the COVID-19 epidemic outbreak with reaction rates.