
- MJC Library & Learning Center
- Research Guides

Drug Abuse, Addiction, Substance Use Disorder
- Research Drug Abuse
Start Learning About Your Topic
Create research questions to focus your topic, find books in the library catalog, find articles in library databases, find web resources, cite your sources, key search words.
Use the words below to search for useful information in books and articles .
- substance use disorder
- substance abuse
- drug addiction
- substance addiction
- chemical dependency
- war on drugs
- names of specific drugs such as methamphetamine, cocaine, heroin
- opioid crisis
Background Reading:
It's important to begin your research learning something about your subject; in fact, you won't be able to create a focused, manageable thesis unless you already know something about your topic.
This step is important so that you will:
- Begin building your core knowledge about your topic
- Be able to put your topic in context
- Create research questions that drive your search for information
- Create a list of search terms that will help you find relevant information
- Know if the information you’re finding is relevant and useful
If you're working from off campus , you'll be prompted to log in just like you do for your MJC email or Canvas courses.
All of these resources are free for MJC students, faculty, & staff.
- Gale eBooks This link opens in a new window Use this database for preliminary reading as you start your research. Try searching these terms: addiction, substance abuse
Other eBooks from the MJC Library collection:
Use some of the questions below to help you narrow this broad topic. See "substance abuse" in our Developing Research Questions guide for an example of research questions on a focused study of drug abuse.
- In what ways is drug abuse a serious problem?
- What drugs are abused?
- Who abuses drugs?
- What causes people to abuse drugs?
- How do drug abusers' actions affect themselves, their families, and their communities?
- What resources and treatment are available to drug abusers?
- What are the laws pertaining to drug use?
- What are the arguments for legalizing drugs?
- What are the arguments against legalizing drugs?
- Is drug abuse best handled on a personal, local, state or federal level?
- Based on what I have learned from my research what do I think about the issue of drug abuse?
Why Use Books:
Use books to read broad overviews and detailed discussions of your topic. You can also use books to find primary sources , which are often published together in collections.
Where Do I Find Books?
You'll use the library catalog to search for books, ebooks, articles, and more.
What if MJC Doesn't Have What I Need?
If you need materials (books, articles, recordings, videos, etc.) that you cannot find in the library catalog , use our interlibrary loan service .
All of these resources are free for MJC students, faculty, & staff.
- EBSCOhost Databases This link opens in a new window Search 22 databases simultaneously that cover almost any topic you need to research at MJC. EBSCO databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Gale Databases This link opens in a new window Search over 35 databases simultaneously that cover almost any topic you need to research at MJC. Gale databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Psychology and Behavioral Sciences Collection This link opens in a new window Contains articles from nearly 560 scholarly journals, some dating as far back as 1965
- Access World News This link opens in a new window Search the full-text of editions of record for local, regional, and national U.S. newspapers as well as full-text content of key international sources. This is your source for The Modesto Bee from January 1989 to the present. Also includes in-depth special reports and hot topics from around the country. To access The Modesto Bee , limit your search to that publication. more... less... Watch this short video to learn how to find The Modesto Bee .
Use Google Scholar to find scholarly literature on the Web:

Browse Featured Web Sites:
- National Institute on Drug Abuse NIDA's mission is to lead the nation in bringing the power of science to bear on drug abuse and addiction. This charge has two critical components. The first is the strategic support and conduct of research across a broad range of disciplines. The second is ensuring the rapid and effective dissemination and use of the results of that research to significantly improve prevention and treatment and to inform policy as it relates to drug abuse and addiction.
- Drug Free America Foundation Drug Free America Foundation, Inc. is a drug prevention and policy organization committed to developing, promoting and sustaining national and international policies and laws that will reduce illegal drug use and drug addiction.
- Office of National Drug Control Policy A component of the Executive Office of the President, ONDCP was created by the Anti-Drug Abuse Act of 1988. ONDCP advises the President on drug-control issues, coordinates drug-control activities and related funding across the Federal government, and produces the annual National Drug Control Strategy, which outlines Administration efforts to reduce illicit drug use, manufacturing and trafficking, drug-related crime and violence, and drug-related health consequences.
- Drug Policy Alliance The Drug Policy Alliance (DPA) is the nation's leading organization promoting alternatives to current drug policy that are grounded in science, compassion, health and human rights.
Your instructor should tell you which citation style they want you to use. Click on the appropriate link below to learn how to format your paper and cite your sources according to a particular style.
- Chicago Style
- ASA & Other Citation Styles
- Last Updated: Sep 6, 2024 2:58 PM
- URL: https://libguides.mjc.edu/drugabuse
Except where otherwise noted, this work is licensed under CC BY-SA 4.0 and CC BY-NC 4.0 Licenses .
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
Information & authors, metrics & citations, view options, insights into mechanisms related to cocaine addiction using a novel imaging method for dopamine neurons, treatment implications of understanding brain function during early abstinence in patients with alcohol use disorder, relatively low amounts of alcohol intake during pregnancy are associated with subtle neurodevelopmental effects in preadolescent offspring, increased comorbidity between substance use and psychiatric disorders in sexual identity minorities, trends in nicotine use and dependence from 2001–2002 to 2012–2013, conclusions, information, published in.

- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
Competing Interests
Export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
NEXT ARTICLE
Request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

RANKING EVIDENCE IN SUBSTANCE USE AND ADDICTION
Hudson reddon.
1. British Columbia Centre on Substance Use, 1045 Howe Street, Vancouver, BC V6Z 2A9, Canada
2. CIHR Canadian HIV Trials Network, 588-1081 Burrard Street, Vancouver, BC V6B 3E6, Canada
Thomas Kerr
3. Department of Medicine, University of British Columbia, St. Paul’s Hospital, 1081 Burrard St, Vancouver, BC V6Z 1Y6, Canada
Hudson Reddon: Writing-Original draft, Writing-Review and Editing Thomas Kerr: Writing-Review and Editing M-J Milloy: Writing-Review and Editing
Evidence-based medicine has consistently prized the epistemological value of randomized-controlled trials (RCTs) owing to their methodological advantages over alternative designs such as observational studies. However, there are limitations to RCTs that hinder their ability to study chronic and dynamic conditions such as substance use and addiction. For these conditions, observational studies may provide superior evidence based on methodological and practical strengths. Assuming epistemic superiority of RCTs has led to an inappropriate devaluation of other study designs and the findings they support, including support for harm reduction services, especially needle exchange programs and supervised injection facilities. The value offered by observational studies should be reflected in evidence-based medicine by allowing more flexibility in evidence hierarchies that presume methodological superiority of RCTs. Despite the popularity of evidence ranking systems and hierarchies, nothing should replace critical appraisal of study methodology and examining the suitability of applying a given study design to a specific research question.
Long-regarded the gold standard of medical evidence, randomized-controlled trials (RCTs) have been given the paramount role in evaluating the safety and efficacy of new interventions to improve human health and wellbeing. Several ranking systems, including evidence hierarchies and the GRADE framework, consistently bestow superiority to the RCT and place limitations on the value that can be assigned to observational studies ( Guyatt, Oxman, Vist, et al., 2008 ; Rawlins, 2008 ; Schunemann, Fretheim, & Oxman, 2006 ). However, the limitations of RCTs are seldom acknowledged, nor is the fact that observational designs are often better suited to characterize certain health conditions, in particular, chronic diseases. Assuming epistemic superiority of RCTs has led to an inappropriate devaluation of other study designs and the findings they support. This trend is particularly important for fields that are less ethically or scientifically well-suited to RCTs, such as substance use and addiction.
Critique of current evidence ranking
The methodological strength from which RCTs draw their scientific credibility is the random allocation of the intervention among trial participants. Other primary strengths include, but are not limited to, blinding, the use of a control group and applying an intervention. Randomization is presumed to remove any between-group differences in prognostic factors associated with the development of the study outcome ( Sackett, 1996 ; Sackett, Strauss, Richardson, Rosenberg, & Haynes, 2000 ). Observational studies are able to control for known confounders, yet RCTs are the only design to address the distribution of unknown confounders through randomization. However, randomization is not a guarantee that known or unknown confounders will be balanced between groups at the outset of a given study. The distribution of covariates between the intervention and control group after randomization is typically assessed by the trialists, and if uneven distributions are observed the randomization is deemed to have failed and is repeated until balanced groups are produced. Most importantly, it is also possible that imbalances in unknown confounders exist post-randomization, which cannot be detected or corrected by study investigators. Therefore, the extent to which RCTs can remove baseline imbalances between study arms is limited, to some degree, by the existing knowledge of the disease under study (i.e., the number of known confounders that can be assessed by the study investigators post-randomization). Imbalances in confounders are also an issue for observational studies. While randomization is a more effective strategy to balance these factors than approaches used in observational studies (e.g., propensity scores), randomization does not guarantee that prognostic balance is achieved ( Austin, 2011 ; Han, Enas, & McEntegart, 2009 ; Worrall, 2010 ).
The ability to establish external validity and extrapolate a trial’s findings beyond the study protocol is a second issue—one particularly germane to RCTs in substance use and addiction. With the objective of restricting any change in study outcome to the treatment intervention, RCTs typically seek to recruit a select and specific group of participants undergoing a highly structured intervention for a brief period with limited follow-up ( Rawlins, 2008 ; Worrall, 2010 ). Patients living with comorbidities or receiving multiple medications tend to be excluded in order to minimize the heterogeneity among study participants and minimize the risk of randomizing an intervention to vulnerable patients. Among people who use illicit drugs and are living with substance use disorders, minimizing heterogeneity in the study sample is challenging due to the high prevalence of comorbid health conditions and engagement with diverse health and social services. For example, current estimates among people who inject drugs report that upwards of 50% have a lifetime diagnosis of depression, 50% are living with hepatitis C virus infection, 13% are living with HIV and the medications/treatments prescribed to these patients are highly personalized ( Conner, Pinquart, & Duberstein, 2008 ; Kessler et al., 1994 ; Lengauer, Pfeifer, & Kaiser, 2014 ; United Nations Office on Drugs and Crime, 2017 ). Notwithstanding the ethical challenges of placing restrictions on inclusion and exclusion criteria, identifying a homogeneous group of participants based on these complex comorbidities and co-interventions is often practically untenable. Administering a structured intervention to this population is further complicated by high rates of marginalization (e.g., homelessness, social instability, stigmatization) and criminalization ( Marshall et al., 2016 ; Stone et al., 2018 ). In consequence, the average treatment effect calculated from an RCT is only as valuable as the sample from which it was estimated ( Dahabreh, 2018 ; Deaton & Cartwright, 2018b ; Ioannidis, 2018 ). The superior internal validity of an RCT does not translate to invariance in the treatment effect across contexts if the sample is not representative of all the patients to which the study could be applied ( Deaton & Cartwright, 2018a , 2018b ). Nevertheless, the results of RCTs are often extrapolated generously despite the limitations imposed by selection criteria and artificial environments that do not reflect real-world applications of the target intervention ( Deaton & Cartwright, 2018a , 2018b ). As an alternative, some authors advocate for strategies such as propensity scores, instrumental variables and matching to strengthen the methodology of observational studies ( Concato & Horwitz, 2018 ; Deaton & Cartwright, 2018b ). Empirical comparisons between RCTs and well-designed observational studies have found similar summary measures of effect size with neither design producing a consistently greater effect ( Anglemyer, Horvath, & Bero, 2014 ; Benson & Hartz, 2000 ; Concato, Shah, & Horwitz, 2000 ; Sterne et al., 2002 ). Moreover, many treatments that continue to be used in clinical and non-clinical settings have been evaluated through observational methods have been found to be both safe and effective ( Concato & Horwitz, 2018 ; Deaton & Cartwright, 2018b ; Tsimberidou, Braiteh, Stewart, & Kurzrock, 2009 ). In these cases, conducting an RCT on the basis that the existing evidence is observational is unnecessary based on the long-term record of safety and effectiveness and RCTs may expose patients to unnecessary risk if patients are denied treatment shown to be beneficial ( Deaton & Cartwright, 2018b ; Vandenbroucke, 2008 ).
Some authors have also questioned the value of RCTs and evidence hierarchies for identifying unintended or adverse effects of new treatment interventions ( Osimani, 2013 ; Vandenbroucke, 2008 ). As the unintended or possibly adverse effects of novel treatments are typically unknown, the treatment allocation is masked with respect to the unintended effects even if the investigator is aware of who is receiving the treatment ( Vandenbroucke, 2004 ). These authors argue that this achieves the same separation between intervention allocation and prognosis that is accomplished through blinding ( Osimani, 2013 ). As a result, observational studies examining adverse events will not be as vulnerable to confounding and selection bias as observational studies evaluating intervention efficacy ( Vandenbroucke, 2004 , 2006 , 2008 ; Vandenbroucke & Psaty, 2008 ). This view is supported by empirical evidence that shows no systematic difference in risk estimation for adverse events between RCTs and observational studies ( Benson & Hartz, 2000 ; Concato et al., 2000 ; Papanikolaou, Christidi, & Ioannidis, 2006 ). A second critique is that the strict inclusion criteria of RCTs may exclude vulnerable participants with complex comorbidities at an increased risk of experiencing adverse events, which applies to many people who use drugs ( Conner et al., 2008 ; Rawlins, 2008 ). In these circumstances case reports or case series may be the most sensitive or only tool available to identify side effects ( Glasziou, Chalmers, Rawlins, & McCulloch, 2007 ; Stricker & Psaty, 2004 ). Based on these arguments, it has been suggested that the evidence hierarchy should be inverted when the objective is to identify unknown adverse events ( Vandenbroucke, 2008 ).
Although RCTs excel at investigating the safety and efficacy of novel pharmacological formulations, issues arise in testing harm reduction-based interventions to benefit people who inject drugs. The risk environments in which needle exchange programs (NEP) and supervised injection facilities (SIF) are implemented are highly variable between settings. For example, the criminalization of illicit drug use in North America has adjusted as policies legalizing and regulating non-medical cannabis continue to expand in the context of an opioid overdose crisis sparked by the contamination of the illicit drug supply. In these circumstances, long-term observational studies in real world or natural settings may be better suited to evaluate the evolving impacts of changes in substance use policy and criminalization than RCTs. While RCTs are not feasible or ethical in this situation, observational studies are advantageous in that they can often include more follow-up time than RCTs, which is needed to better evaluate the long-term effects of structural factors such as policy change and criminalization on the chronic and dynamic nature of substance use and addiction ( Kelly, Greene, & Bergman, 2018 ; Worrall, 2010 ). The utility of real world data has sparked calls for the integration of alternative data sources such as electronic health records and patient registries to study patient groups who may have been excluded from RCTs (e.g., elderly people living with comorbidities) ( Nabhan, Klink, & Prasad, 2019 ). Other alternatives that have been applied to evaluating substance use include pragmatic trials that blend the traits of observational studies with traditional RCTs ( Coulton et al., 2017 ; Henderson et al., 2017 ). Alternative trial designs including stepped wedge and crossover trials have been effectively applied to study diseases requiring extended follow-up evaluation ( Chotard et al., 1992 ; Hemming, Haines, Chilton, Girling, & Lilford, 2015 ). These designs have been used in diverse areas, including HIV and social policy, although they are challenging when the intervention is believed to be effective and receipt should not be denied or delayed, or there are complex contextual and patient factors that moderate the impact of the intervention on the study outcome ( Bonell et al., 2011 ; Brown & Lilford, 2006 ). Unfortunately, these challenges are common among interventions for people who use drugs. Blinding and providing a placebo are often not possible for these interventions and extrapolating the effects of the intervention beyond the study protocol must be done with caution given that substance use and addiction are chronic and relapsing conditions ( Kelly et al., 2018 ; Kelly, Greene, Bergman, White, & Hoeppner, 2019 ).
Perhaps the most significant unacknowledged weakness of RCTs is their typically limited periods for the intervention and follow-up. Due to their substantial expense, funding for post-study follow-up is typically limited to six to 24 months, which is often insufficient for chronic diseases ( Bluhm, 2010 ; Vlieland, 2002 ) such as substance use disorders, characterized as chronically relapsing conditions with recurring transitions between substance use, abstinence, treatment engagement and incarceration ( Dennis & Scott, 2007 ; Kelly et al., 2019 ). For example, the median time from first to final instance of substance use was estimated at 27 years among people admitted to publicly-funded treatment who were able to abstain for at least one year, and the average time between the first episode of substance use treatment and last instance of substance use was nine years ( Dennis, Scott, Funk, & Foss, 2005 ). A recent analyses from a national study of adults in recovery in the United States (N=39,809) found that an average of two to five attempts were required to resolve an alcohol or drug problem and the number of attempts varied by demographic characteristics, type of treatment and clinical history ( Kelly et al., 2019 ). African American ethnicity, previous use of treatment and mutual-help groups and psychiatric comorbidity were associated with a greater number of recovery attempts ( Kelly et al., 2019 ). Moreover, many patient-important outcomes including quality of life, happiness and self-esteem do not increase monotonically during recovery. These measures were found to decrease significantly in the first year following resolution of an alcohol or drug problem and then increase over subsequent years ( Kelly et al., 2018 ). As a result, the methodological strengths of RCTs are, to some extent, mitigated by the limitations of administering brief structured interventions to a heterogeneous population living with chronic and dynamic disorders. For conditions such as substance use and addiction, RCTs are often limited to providing a snapshot of the effectiveness of interventions in the short term and may fail to identify long-term effects among heterogeneous groups of participants living with chronic and dynamic disorders. In these circumstances, observational studies are often better suited to study interventions designed for a more representative sample of individuals who are often excluded from studies requiring randomization, and who require long-term follow to evaluate enduring changes in study outcomes ( Bluhm, 2010 ; Worrall, 2010 ). Rather than viewing observational designs as a next best option in situations where RCTs are perceived as practically or ethically unfeasible, it should be recognized that the methodological strengths of observational studies may provide the best available evidence to evaluate the course of chronic conditions and the effect of interventions to address them ( Bluhm, 2010 ; Worrall, 2010 ).
In contrast to the approach of evidence-based medicine that strives to identify the most accurate estimate of an average treatment effect, other researchers have proposed a framework that conceptualizes health interventions as “evidence-making” ( Rhodes & Lancaster, 2019 ). Rather than assuming a singular and universal effect of an intervention, the evidence-making framework posits that the variability of practice and patients produces multiple realities of the effects of an intervention and treats evidence, interventions and their effects as emergent, contingent and multiple ( Rhodes & Lancaster, 2019 ). By recognizing that the diversity of practices creates multiple realities of an intervention, evidence-making frameworks foster dialogue across diverse forms of knowledge and knowledge actors to recognize how the politics of intervention knowledge and the realities they create influence their effects across settings ( Rhodes & Lancaster, 2019 ). While it is beyond the scope of this paper to provide a detailed analysis of this framework, similar approaches have been raised by authors who advocate for a process of cumulative scientific understanding that is often challenged by the assumptions of evidence-based medicine and evidence hierarchies ( Deaton & Cartwright, 2018b ). The production of new scientific evidence should build upon and be integrated with existing knowledge to enhance collective scientific knowledge. Unfortunately, it is not uncommon for the findings from observational studies to be dismissed if more recent evidence from a randomized study contradicts the original results ( Deaton & Cartwright, 2018a , 2018b ). Some experts argue that new findings must be able to explain or be integrated with previous results as knowledge advances, even if previous results are believed to be invalid ( Deaton & Cartwright, 2018b ). Failure to integrate results from randomized and non-randomized studies undermines the responsibility of science to advance the cumulative understanding of health interventions and acknowledge the legitimate variability of intervention effects created by the diversity of practice and patients ( Concato et al., 2000 ; Rhodes & Lancaster, 2019 ).
The inappropriate devaluation of observational studies has slowed the implementation and scale-up of several harm reduction interventions for PWUD. The observational evidence supporting SIF and NEP includes many large-scale prospective cohort studies with several years of follow-up from multiple countries ( Aspinall et al., 2014 ; Potier, Laprevote, Dubois-Arber, Cottencin, & Rolland, 2014 ; Wood, Tyndall, Montaner, & Kerr, 2006 ). The advantages of being able to prospectively evaluate the health impacts of these interventions among heterogeneous samples of people who use drugs in real-world settings are unique methodological strengths that provide evidence into the long-term trajectories of this population. Existing evaluations of NEP and SIF have provided strong evidence for reducing HIV risk behaviours, overdose mortality and increasing engagement with addiction treatment services without adverse effects on broader public health and safety ( Aspinall et al., 2014 ; Marshall, Milloy, Wood, Montaner, & Kerr, 2011 ; Potier et al., 2014 ). In spite of this evidence, these services remain limited in many countries contending with the challenges of substance use harms ( Degenhardt et al., 2014 ).
Although ideological opposition to harm reduction-based interventions like NEP and SIF remains the primary barrier limiting their availability in many settings worldwide ( Nadelmann & LaSalle, 2017 ), their establishment and expansion has also been hindered by an ironic epistemic predicament regarding their scientific evaluation. As these services provide self-evident health and safety benefits to profoundly marginalized and vulnerable individuals, regulators and trialists have determined it would be unethical to evaluate them through RCTs as randomization would restrict the control group from accessing potentially life-saving interventions ( Bastos & Strathdee, 2000 ; Bluthenthal & Kral, 2010 ; Lurie, 1998 ). Yet, when observational evidence accumulates demonstrating the benefit of these interventions, the lack of RCTs is critiqued as a methodological weakness ( Bluthenthal & Kral, 2010 ). In effect, the anticipated benefit of these services limits the credibility of subsequent empirical evidence supporting these services ( Bluthenthal & Kral, 2010 ). Throughout the implementation of NEP and SIF, the use of observational methodologies to evaluate these services has often been referenced as a precaution against their expansion or a methodological limitation ( Palmateer et al., 2010 ; Wood et al., 2006 ).
In addition, the effectiveness of SIFs has been challenged based on uncertainty regarding the effect size of these services, despite the large evidence base that is nearly unanimous in support of SIF, with no SIF overdose deaths reported to date and no reported adverse effects ( Caulkins, Pardo, & Kilmer, 2019 ; May, Holloway, & Bennett, 2019 ). Criticism about effect heterogeneity relates to the EBM objective of estimating a singular treatment effect, whereas it is entirely possible, and we would argue likely, that the effect size of these interventions may vary across patient populations and contexts ( Deaton & Cartwright, 2018b ; Rhodes & Lancaster, 2019 ). Rather than this heterogeneity being perceived as a weakness of study methodology, we would argue that this variability is consistent with the evidence-making intervention framework whereby the diversity of practice and patients creates multiple realities of an intervention’s effects ( Rhodes & Lancaster, 2019 ). In fact, this variability should be expected based on the specific crisis situations in which these services are often implemented ( Caulkins et al., 2019 ). SIFs have been established in diverse countries experiencing different types of illicit substance use, patient populations, service models, local contexts, adjunct services and drug policy ( Caulkins et al., 2019 ). These situations are not well-suited to the evidence-based medicine perspective that attempts to minimize patient and intervention heterogeneity to estimate a precise and singular treatment effect ( Deaton & Cartwright, 2018b ; Rhodes & Lancaster, 2019 ). Instead, the existence of multiple contingent effects of an intervention that are adaptive is in keeping with the ontology of the evidence-making intervention framework ( Rhodes & Lancaster, 2019 ). While we acknowledge that randomizing participants to SIF participation (e.g., through community-randomized trials or wait-list studies) would be theoretically valuable, we contend that this is has become unethical and unnecessary given the evidence of benefit and absence of harm associated with these services ( Caulkins et al., 2019 ; Kennedy, Hayashi, Milloy, Wood, & Kerr, 2019 ). As previously mentioned, RCTs do not have the same benefits for assessing adverse outcomes and the risks associated with denying or delaying SIF use among vulnerable populations of PWUD through RCTs is difficult to justify ( May et al., 2019 ; Osimani, 2013 ; Vandenbroucke, 2006 ). Although RCTs are held as the gold-standard for identifying causal associations, observational and qualitative studies are able to provide valuable evidence about the causal mechanisms underlying these associations and contribute to advancing the cumulative understanding of an intervention without the need for experimental closure ( Deaton & Cartwright, 2018b ; Rhodes & Lancaster, 2019 ). The study design that provides the best evidence may therefore vary depending on the theory or research question being evaluated; this should be reflected in evidence ranking systems such as the GRADE framework and the Maryland Scientific Methods Scale that place limits on the value that can be assigned to non-randomized studies ( Alonso-Coello et al., 2016 ; Worrall, 2010 ).
There are examples where observational studies have been sufficient to demonstrate effectiveness and continue to be used clinically without the need for verification through RCTs. An analysis of oncology drugs approved by the United States Food and Drug Administration found that 31 of 68 drugs were approved without an RCT and 30 of these drugs remain fully approved ( Concato & Horwitz, 2018 ; Tsimberidou et al., 2009 ). Studies using objective endpoints were the most common among those approved and these drugs demonstrated a long-term record of efficacy and safety based on observational evidence ( Tsimberidou et al., 2009 ). There are also cases where the belief that RCTs are needed to confirm observational evidence has caused harm. The controversy surrounding the RCTs of extracorporeal membrane oxygenation (ECMO) therapy in newborns has been well described ( Bluhm, 2010 ; Truog, 1992 ). Both ECMO and the standard treatment were evolving rapidly and observational studies had already supported the benefit of ECMO ( Bartlett, 1984 ; Wung, James, Kilchevsky, & James, 1985 ). Yet, variability in the success rate of ECMO across centres prompted many researchers to call for RCTs before ECMO became an accepted therapy ( Bluhm, 2010 ). In the first trial, the one infant who received conventional therapy did not survive while all 11 who received ECMO survived ( Bartlett et al., 1985 ). In phase one of the second trial, four of the ten newborns receiving conventional therapy did not survive while all nine who received ECMO survived ( O’Rourke et al., 1989 ). In phase two, 20 patients received ECMO and 19 survived ( O’Rourke et al., 1989 ). These examples have led some experts to suggest that RCTs should not be used in cases where interventions are rapidly evolving and are potentially life saving ( Truog, 1992 ). In these cases, the interventions or their implementation may be out-dated by the time the RCT has concluded and observational studies of clinical practice (e.g., outcomes research) may provide better evidence of intervention effectiveness while avoiding some of the ethical challenges of withholding or delaying novel treatments in RCTs ( Truog, 1992 ; Worrall, 2010 ). This is particularly relevant to the situation of SIFs, which are often implemented in situations of crisis that are rapidly evolving as new challenges arise, such as the multiple waves of the opioid overdose crisis. Under these circumstances, variability in the effect should not detract from the fact the evidence is, even in the opinion of critics, “almost unanimous in its support” and is potentially life saving ( Caulkins et al., 2019 ; Kennedy et al., 2019 ; May et al., 2019 ). Performing RCTs of SIFs to ascertain a singular measure of effect should be viewed as unnecessary and unethical given the existing evidence and that observational studies may provide better information to evaluate these interventions based on the evolving context of their implementation and the potential for them to be life saving.
Future directions for addiction science and evidence ranking
An alternative observational design that has gained considerable attention, particularly for studying chronic diseases, is Mendelian randomization ( Lawlor, Harbord, Sterne, Timpson, & Davey Smith, 2008 ; Smith, 2006 ). These studies integrate genetic variants into observational epidemiology to enhance the causal inferences that can be drawn about modifiable risk factors and health outcomes ( Smith & Ebrahim, 2003 ; Youngman, Keavney, & Palmer, 2000 ). Rather than randomize participants to receive the exposure being studied, Mendelian randomization studies take advantage of the random assignment of an individual’s genotype from their parents to conduct a ‘natural’ RCT ( Davey Smith & Ebrahim, 2005 ; Hingorani & Humphries, 2005 ). If germline genetic variants for an environmental exposure (e.g., substance use) have been identified, these variants can be used as a proxy measure of the exposure in observational studies and be treated as randomly distributed ( Lawlor et al., 2008 ; Pasman et al., 2018 ). Mendelian randomization studies can also be performed in representative population samples without the need for exclusion criteria or randomizing participants as is necessary in traditional RCTs ( Lawlor et al., 2008 ; Smith & Ebrahim, 2003 ). In addition, the associations between these gene variants and health outcomes are not susceptible to reverse causality as germline genotypes are not affected by disease progression, and, if the gene variant is not pleiotropic, the risk of confounding is mitigated ( Smith & Ebrahim, 2004 ). Finally, genetic variants that predict an environmental exposure typically do so throughout the life span, a fact which minimizes regression dilution bias ( Smith & Ebrahim, 2004 ). As the cost of genome sequencing continues to decrease and more large-scale consortia are forming, integrating genetic data into observational designs is becoming increasingly feasible for studies of substance use and addiction ( Pasman et al., 2018 ; Phillips, Deverka, Hooker, & Douglas, 2018 ; Vaucher et al., 2018 ). For example, Mendelian randomization studies have been applied to investigate the longstanding debate surrounding the association between schizophrenia and cannabis use ( Gage et al., 2017 ; Pasman et al., 2018 ; Vaucher et al., 2018 ). The limitations of Mendelian randomization studies include population stratification, identifying a reliable genetic variant for the exposure of interest that does not have pleiotropic effects on the outcome and is not in linkage disequilibrium with other gene variants associated with the outcome ( Cardon & Palmer, 2003 ; Lawlor et al., 2008 ; Smith & Ebrahim, 2004 ). Additional challenges include developmental compensation, contextual influences on the exposures predicted by gene variants and non-linear associations ( Gibson & Wagner, 2000 ). Despite these limitations, Mendelian randomization studies retain the ability of traditional observational studies to study the development of chronic conditions over time with the advantage of studying gene variants for exposures that are randomly distributed ( Lawlor et al., 2008 ; Smith & Ebrahim, 2003 ). The ability to combine the strengths of observational studies while adding a component of randomization should challenge the assumed superiority of RCTs among policymakers and healthcare professionals. The evidence from these studies may also prevent the need to conduct RCTs to address certain research questions. For example, a Mendelian randomization study evaluating the effects of selenium supplementation on prostate cancer risk provided evidence of no effect, which was consistent with the largest ever prostate cancer prevention trial ( Yarmolinsky et al., 2018 ). This trial was stopped before completion based on a lack of efficacy and adverse events, at a cost of $114 million ( Yarmolinsky et al., 2018 ). As the efficacy and adverse events were predicted by this Mendelian randomization study, these designs may be an efficient and affordable means to study interventions traditionally assessed RCTs as big data resources for genetic information continue to expand ( Yarmolinsky et al., 2018 ).
A second area for improvement in substance use and addiction research is the further integration of patient-important outcomes. The underrepresentation of patient-reported outcomes has been highlighted in several study designs yet is more pronounced in RCTs ( Pardo-Hernandez & Alonso-Coello, 2017 ; Saldanha et al., 2017 ). Previous field-specific systematic reviews of RCTs have found that less than 25% include a patient-important outcome as a primary outcome ( Gaudry et al., 2017 ; Rahimi, Malhotra, Banning, & Jenkinson, 2010 ). The lack of patient-important outcomes is highly germane to substance use research and a systematic review is currently ongoing to identify patient-important outcomes to assess the effectiveness of opioid use disorder in the context of the overdose epidemic ( Dennis et al., 2015 ; Sanger et al., 2018 ). Increased recognition of the value of patient-important data is reflected in the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system, which recommends their inclusion at two different stages (the outset of study design and when ranking the importance of study outcomes) ( Guyatt, Oxman, Kunz, et al., 2008 ). Other frameworks designed to help stakeholders translate scientific evidence to healthcare decisions prioritize the inclusion of patient-important outcomes and considers the degree to which patients value each outcome ( Alonso-Coello et al., 2016 ). The Core Outcome Measures in Effectiveness Trials (COMET) initiative extends this view by promoting the selection of a standardized set of outcomes for each health condition to compare effectiveness across studies (“ The COMET Initiative,” 2010 ; Gorst et al., 2016 ; Williamson et al., 2012 ). The lack of patient-important outcomes in addiction literature, and the fact that these measures vary significantly in different stages of addiction, calls for further integration of these outcomes in future research ( Kelly et al., 2018 ; Sanger et al., 2018 ). Given the value of patient-important outcomes—and that they are prioritized in stakeholder frameworks including GRADE and COMET—further evaluation of these outcomes will be important to promote the uptake of observational evidence on substance use and addiction among policymakers and healthcare officials ( Gorst et al., 2016 ; Guyatt, Oxman, Kunz, et al., 2008 ; Pardo-Hernandez & Alonso-Coello, 2017 ; Williamson et al., 2012 ).
There are, without question, important limitations to studies with non-randomized designs. However, the value offered by observational studies should be reflected in evidence-based medicine by allowing more flexibility in evidence hierarchies that presume methodological superiority of RCTs. Observational designs may provide the best evidence to evaluate interventions to address chronic conditions such as substance use and addiction. Unfortunately, assuming epistemic superiority of RCTs has unnecessarily slowed the uptake of substance use research and harm reduction services for people who use drugs. Despite the popularity of evidence ranking systems and hierarchies, nothing should replace critical appraisal of study methodology and examining the suitability of applying a given study design to a specific clinical question.
Acknowledgments:
This work was supported by the CIHR Canadian HIV Trials Network (CTN 222). Dr. Hudson Reddon is supported by a Sponsor/CTN Postdoctoral Fellowship Award and a Michael Smith Research Trainee Award. Dr. M-J Milloy is supported in part by the United States National Institutes of Health (U01-DA021525), a New Investigator Award from CIHR and a Scholar Award from MSFHR. His institution has received an unstructured gift to support him from NG Biomed, Ltd., a private firm applying for a government license to produce cannabis. The Canopy Growth professorship in cannabis science was established through unstructured gifts to the University of British Columbia from Canopy Growth, a licensed producer of cannabis, and the Ministry of Mental Health and Addictions of the Government of British Columbia.
Competing Interests: None to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
- Alonso-Coello P, Schunemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, … Group, G. W. (2016). GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction . BMJ , 353 , i2016. doi: 10.1136/bmj.i2016 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Anglemyer A, Horvath HT, & Bero L. (2014). Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials . Cochrane Database Syst Rev ( 4 ), MR000034. doi: 10.1002/14651858.MR000034.pub2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aspinall EJ, Nambiar D, Goldberg DJ, Hickman M, Weir A, Van Velzen E, … Hutchinson SJ (2014). Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis . Int J Epidemiol , 43 ( 1 ), 235–248. doi: 10.1093/ije/dyt243 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Austin PC (2011). An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies . Multivariate Behav Res , 46 ( 3 ), 399–424. doi: 10.1080/00273171.2011.568786 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bartlett RH (1984). Extracorporeal oxygenation in neonates . Hosp Pract (Off Ed) , 19 ( 4 ), 139–143, 146, 151. doi: 10.1080/21548331.1984.11702803 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bartlett RH, Roloff DW, Cornell RG, Andrews AF, Dillon PW, & Zwischenberger JB (1985). Extracorporeal circulation in neonatal respiratory failure: a prospective randomized study . Pediatrics , 76 ( 4 ), 479–487. [ PubMed ] [ Google Scholar ]
- Bastos FI, & Strathdee SA (2000). Evaluating effectiveness of syringe exchange programmes: current issues and future prospects . Soc Sci Med , 51 , 1771–1782. [ PubMed ] [ Google Scholar ]
- Benson K, & Hartz AJ (2000). A comparison of observational studies and randomized, controlled trials . Am J Ophthalmol , 130 ( 5 ), 688. doi: 10.1016/s0002-9394(00)00754-6 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bluhm R. (2010). The epistemology and ethics of chronic disease research: Further lessons from ECMO . Theory of Medical Bioethics , 31 , 107–122. doi: 10.1007/s11017-010-9139-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bluthenthal R, & Kral A. (2010). Commentary on Palmateer et al. (2010): next steps in the global research agenda on syringe access for injection drug users . Addiction , 105 ( 5 ), 860–861. doi: 10.1111/j.1360-0443.2010.02942.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bonell CP, Hargreaves J, Cousens S, Ross D, Hayes R, Petticrew M, & Kirkwood BR (2011). Alternatives to randomisation in the evaluation of public health interventions: design challenges and solutions . J Epidemiol Community Health , 65 ( 7 ), 582–587. doi: 10.1136/jech.2008.082602 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown CA, & Lilford RJ (2006). The stepped wedge trial design: a systematic review . BMC Med Res Methodol , 6 , 54. doi: 10.1186/1471-2288-6-54 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cardon LR, & Palmer LJ (2003). Population stratification and spurious allelic association . Lancet , 361 ( 9357 ), 598–604. doi: 10.1016/S0140-6736(03)12520-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Caulkins JP, Pardo B, & Kilmer B. (2019). Supervised consumption sites: a nuanced assessment of the causal evidence . Addiction , 114 ( 12 ), 2109–2115. doi: 10.1111/add.14747 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chotard J, Inskip HM, Hall AJ, Loik F, Mendy M, Whittle H, … Lowe Y. (1992). The Gambia Hepatitis Intervention Study: follow-up of a cohort of children vaccinated against hepatitis B . J Infect Dis , 166 ( 4 ), 764–768. doi: 10.1093/infdis/166.4.764 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- The COMET Initiative . (2010). [ Google Scholar ]
- Concato J, & Horwitz RI (2018). Randomized trials and evidence in medicine: A commentary on Deaton and Cartwright . Soc Sci Med , 210 , 32–36. doi: 10.1016/j.socscimed.2018.04.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Concato J, Shah N, & Horwitz RI (2000). Randomized, controlled trials, observational studies, and the hierarchy of research designs . N Engl J Med , 342 ( 25 ), 1887–1892. doi: 10.1056/NEJM200006223422507 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Conner KR, Pinquart M, & Duberstein PR (2008). Meta-analysis of depression and substance use and impairment among intravenous drug users (IDUs) . Addiction , 103 ( 4 ), 524–534. doi: 10.1111/j.1360-0443.2007.02118.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coulton S, Stockdale K, Marchand C, Hendrie N, Billings J, Boniface S, … Wilson E. (2017). Pragmatic randomised controlled trial to evaluate the effectiveness and cost effectiveness of a multi-component intervention to reduce substance use and risk-taking behaviour in adolescents involved in the criminal justice system: A trial protocol (RISKIT-CJS) . BMC Public Health , 17 ( 1 ), 246. doi: 10.1186/s12889-017-4170-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dahabreh IJ (2018). Randomization, randomized trials, and analyses using observational data: A commentary on Deaton and Cartwright . Soc Sci Med , 210 , 41–44. doi: 10.1016/j.socscimed.2018.05.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davey Smith G, & Ebrahim S. (2005). What can mendelian randomisation tell us about modifiable behavioural and environmental exposures? BMJ , 330 ( 7499 ), 1076–1079. doi: 10.1136/bmj.330.7499.1076 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Deaton A, & Cartwright N. (2018a). Reflections on Randomized Control Trials . Soc Sci Med , 210 , 86–90. doi: 10.1016/j.socscimed.2018.04.046 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Deaton A, & Cartwright N. (2018b). Understanding and misunderstanding randomized controlled trials . Soc Sci Med , 210 , 2–21. doi: 10.1016/j.socscimed.2017.12.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Degenhardt L, Mathers BM, Wirtz AL, Wolfe D, Kamarulzaman A, Carrieri MP, … Beyrer C. (2014). What has been achieved in HIV prevention, treatment and care for people who inject drugs, 2010–2012? A review of the six highest burden countries . International Journal of Drug Policy , 25 ( 1 ), 53–60. doi: 10.1016/j.drugpo.2013.08.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dennis BB, Roshanov PS, Naji L, Bawor M, Paul J, Plater C, … Thabane L. (2015). Opioid substitution and antagonist therapy trials exclude the common addiction patient: a systematic review and analysis of eligibility criteria . Trials , 16 , 475. doi: 10.1186/s13063-015-0942-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dennis M, Scott C, Funk R, & Foss M. (2005). The duration and correlates of addiction and treatment careers . J Subst Abuse Treat , 28 ( 1 ), S61–S62. [ PubMed ] [ Google Scholar ]
- Dennis M, & Scott CK (2007). Managing addiction as a chronic condition . Addict Sci Clin Pract , 4 ( 1 ), 45–55. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gage SH, Jones HJ, Burgess S, Bowden J, Davey Smith G, Zammit S, & Munafo MR (2017). Assessing causality in associations between cannabis use and schizophrenia risk: a two-sample Mendelian randomization study . Psychol Med , 47 ( 5 ), 971–980. doi: 10.1017/S0033291716003172 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gaudry S, Messika J, Ricard JD, Guillo S, Pasquet B, Dubief E, … Tubach F. (2017). Patient-important outcomes in randomized controlled trials in critically ill patients: a systematic review . Ann Intensive Care , 7 ( 1 ), 28. doi: 10.1186/s13613-017-0243-z [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gibson G, & Wagner G. (2000). Canalization in evolutionary genetics: a stabilizing theory? Bioessays , 22 ( 4 ), 372–380. doi: 10.1002/(SICI)1521-1878(200004)22:4<372::AID-BIES7>3.0.CO;2-J [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Glasziou P, Chalmers I, Rawlins M, & McCulloch P. (2007). When are randomised trials unnecessary? Picking signal from noise . BMJ , 334 ( 7589 ), 349–351. doi: 10.1136/bmj.39070.527986.68 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gorst SL, Gargon E, Clarke M, Blazeby JM, Altman DG, & Williamson PR (2016). Choosing Important Health Outcomes for Comparative Effectiveness Research: An Updated Review and User Survey . PLoS One , 11 ( 1 ), e0146444. doi: 10.1371/journal.pone.0146444 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schunemann HJ, & Group GW (2008). What is “quality of evidence” and why is it important to clinicians? BMJ , 336 ( 7651 ), 995–998. doi: 10.1136/bmj.39490.551019.BE [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, … Group, G. W. (2008). GRADE: an emerging consensus on rating quality of evidence and strength of recommendations . BMJ , 336 ( 7650 ), 924–926. doi: 10.1136/bmj.39489.470347.AD [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Han B, Enas NH, & McEntegart D. (2009). Randomization by minimization for unbalanced treatment allocation . Stat Med , 28 ( 27 ), 3329–3346. doi: 10.1002/sim.3710 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hemming K, Haines TP, Chilton PJ, Girling AJ, & Lilford RJ (2015). The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting . BMJ , 350 , h391. doi: 10.1136/bmj.h391 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Henderson JL, Cheung A, Cleverley K, Chaim G, Moretti ME, de Oliveira C, … Szatmari P. (2017). Integrated collaborative care teams to enhance service delivery to youth with mental health and substance use challenges: protocol for a pragmatic randomised controlled trial . BMJ Open , 7 ( 2 ), e014080. doi: 10.1136/bmjopen-2016-014080 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hingorani A, & Humphries S. (2005). Nature’s randomised trials . Lancet , 366 ( 9501 ), 1906–1908. doi: 10.1016/S0140-6736(05)67767-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ioannidis JPA (2018). Randomized controlled trials: Often flawed, mostly useless, clearly indispensable: A commentary on Deaton and Cartwright . Soc Sci Med , 210 , 53–56. doi: 10.1016/j.socscimed.2018.04.029 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kelly J, Greene C, & Bergman B. (2018). Beyond abstinence: Changes in indices of quality of lifewith time in recovery in a nationally-representative sample of US adults . Alcohol Clin Exp Res , 42 ( 4 ), 770–780. doi: 10.1111/acer.13604 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kelly JF, Greene MC, Bergman BG, White WL, & Hoeppner BB (2019). How Many Recovery Attempts Does it Take to Successfully Resolve an Alcohol or Drug Problem? Estimates and Correlates From a National Study of Recovering U.S. Adults . Alcohol Clin Exp Res , 43 ( 7 ), 1533–1544. doi: 10.1111/acer.14067 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kennedy MC, Hayashi K, Milloy MJ, Wood E, & Kerr T. (2019). Supervised injection facility use and all-cause mortality among people who inject drugs in Vancouver, Canada: A cohort study . PLoS Med , 16 ( 11 ), e1002964. doi: 10.1371/journal.pmed.1002964 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, … Kendler KS (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey . Arch Gen Psychiatry , 51 ( 1 ), 8–19. doi: 10.1001/archpsyc.1994.03950010008002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lawlor DA, Harbord RM, Sterne JA, Timpson N, & Davey Smith G. (2008). Mendelian randomization: using genes as instruments for making causal inferences in epidemiology . Stat Med , 27 ( 8 ), 1133–1163. doi: 10.1002/sim.3034 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lengauer T, Pfeifer N, & Kaiser R. (2014). Personalized HIV therapy to control drug resistance . Drug Discov Today Technol , 11 , 57–64. doi: 10.1016/j.ddtec.2014.02.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lurie P. (1998). Re: ‘Invited commentary: le mystere de Montreal’ . Am J Epidemiol , 148 , 715–716. [ PubMed ] [ Google Scholar ]
- Marshall BD, Elston B, Dobrer S, Parashar S, Hogg RS, Montaner JS, … Milloy MJ (2016). The population impact of eliminating homelessness on HIV viral suppression among people who use drugs . AIDS , 30 ( 6 ), 933–942. doi: 10.1097/qad.0000000000000990 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marshall BD, Milloy MJ, Wood E, Montaner JS, & Kerr T. (2011). Reduction in overdose mortality after the opening of North America’s first medically supervised safer injecting facility: a retrospective population-based study . Lancet , 377 ( 9775 ), 1429–1437. doi: 10.1016/S0140-6736(10)62353-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- May T, Bennett T, & Holloway K. (2018). RETRACTED: The impact of medically supervised injection centres on drug-related harms: a meta-analysis . Int J Drug Policy , 59 , 98–107. doi: 10.1016/j.drugpo.2018.06.018 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- May T, Holloway K, & Bennett T. (2019). The need to broaden and strengthen the evidence base for supervised consumption sites . Addiction , 114 ( 12 ), 2117–2118. doi: 10.1111/add.14789 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nabhan C, Klink A, & Prasad V. (2019). Real-world Evidence-What Does It Really Mean? JAMA Oncol , 5 ( 6 ), 781–783. doi: 10.1001/jamaoncol.2019.0450 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nadelmann E, & LaSalle L. (2017). Two steps forward, one step back: current harm reduction policy and politics in the United States . Harm Reduct J , 14 ( 1 ), 37. doi: 10.1186/s12954-017-0157-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O’Rourke PP, Crone RK, Vacanti JP, Ware JH, Lillehei CW, Parad RB, & Epstein MF (1989). Extracorporeal membrane oxygenation and conventional medical therapy in neonates with persistent pulmonary hypertension of the newborn: a prospective randomized study . Pediatrics , 84 ( 6 ), 957–963. [ PubMed ] [ Google Scholar ]
- Osimani B. (2013). Until RCT proven? On the asymmetry of evidence requirements for risk assessment . J Eval Clin Pract , 19 ( 3 ), 454–462. doi: 10.1111/jep.12039 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Palmateer N, Kimber J, Hickman M, Hutchinson S, Rhodes T, & Goldberg D. (2010). Evidence for the effectiveness of sterile injecting equipment provision in preventing hepatitis C and human immunodeficiency virus transmission among injecting drug users: a review of reviews . Addiction , 105 ( 5 ), 844–859. doi: 10.1111/j.1360-0443.2009.02888.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Papanikolaou PN, Christidi GD, & Ioannidis JP (2006). Comparison of evidence on harms of medical interventions in randomized and nonrandomized studies . CMAJ , 174 ( 5 ), 635–641. doi: 10.1503/cmaj.050873 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pardo-Hernandez H, & Alonso-Coello P. (2017). Patient-important outcomes in decision-making: a point of no return . J Clin Epidemiol , 88 , 4–6. doi: 10.1016/j.jclinepi.2017.05.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pasman JA, Verweij KJH, Gerring Z, Stringer S, Sanchez-Roige S, Treur JL, … Vink JM (2018). GWAS of lifetime cannabis use reveals new risk loci, genetic overlap with psychiatric traits, and a causal influence of schizophrenia . Nat Neurosci , 21 ( 9 ), 1161–1170. doi: 10.1038/s41593-018-0206-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Phillips KA, Deverka PA, Hooker GW, & Douglas MP (2018). Genetic Test Availability And Spending: Where Are We Now? Where Are We Going? Health Aff (Millwood) , 37 ( 5 ), 710–716. doi: 10.1377/hlthaff.2017.1427 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Potier C, Laprevote V, Dubois-Arber F, Cottencin O, & Rolland B. (2014). Supervised injection services: what has been demonstrated? A systematic literature review . Drug Alcohol Depend , 145 , 48–68. doi: 10.1016/j.drugalcdep.2014.10.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rahimi K, Malhotra A, Banning AP, & Jenkinson C. (2010). Outcome selection and role of patient reported outcomes in contemporary cardiovascular trials: systematic review . BMJ , 341 , c5707. doi: 10.1136/bmj.c5707 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rawlins MD (2008). De Testimonio: On the Evidence for Decisions about the use of Therapeutic Interventions The Harveian Oration . London: Royal College of Physicians. [ Google Scholar ]
- Rhodes T, & Lancaster K. (2019). Evidence-making interventions in health: A conceptual framing . Soc Sci Med , 238 , 112488. doi: 10.1016/j.socscimed.2019.112488 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- ackett DL (1996). Evidence based medicine. What it is and what it isn’t . British Medical Journal , 312 , 71–72. [ Google Scholar ]
- Sackett DL, Strauss SE, Richardson WS, Rosenberg W, & Haynes RB (2000). Evidence Based Medicine. How to Practice and Teach EBM (2 ed.). Edinburgh and London: Churchill Livingston. [ Google Scholar ]
- Saldanha IJ, Li T, Yang C, Owczarzak J, Williamson PR, & Dickersin K. (2017). Clinical trials and systematic reviews addressing similar interventions for the same condition do not consider similar outcomes to be important: a case study in HIV/AIDS . J Clin Epidemiol , 84 , 85–94. doi: 10.1016/j.jclinepi.2017.02.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sanger N, Shahid H, Dennis BB, Hudson J, Marsh D, Sanger S, … Samaan Z. (2018). Identifying patient-important outcomes in medication-assisted treatment for opioid use disorder patients: a systematic review protocol . BMJ Open , 8 ( 12 ), e025059. doi: 10.1136/bmjopen-2018-025059 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schunemann HJ, Fretheim A, & Oxman AD (2006). Improving the use of research evidence in guideline development: 9. Grading evidence and recommendations . Health Res Policy Syst , 4 ( 21 ). [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith GD (2006). Capitalising on Mendelian randomisation to assess the effects of treatment . James Lind Library . [ Google Scholar ]
- Smith GD, & Ebrahim S. (2003). ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol , 32 ( 1 ), 1–22. doi: 10.1093/ije/dyg070 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith GD, & Ebrahim S. (2004). Mendelian randomization: prospects, potentials, and limitations . Int J Epidemiol , 33 ( 1 ), 30–42. doi: 10.1093/ije/dyh132 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sterne JA, Juni P, Schulz KF, Altman DG, Bartlett C, & Egger M. (2002). Statistical methods for assessing the influence of study characteristics on treatment effects in ‘meta-epidemiological’ research . Stat Med , 21 ( 11 ), 1513–1524. doi: 10.1002/sim.1184 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stone J, Fraser H, Lim AG, Walker JG, Ward Z, MacGregor L, … Vickerman P. (2018). Incarceration history and risk of HIV and hepatitis C virus acquisition among people who inject drugs: a systematic review and meta-analysis . Lancet Infect Dis , 18 ( 12 ), 1397–1409. doi: 10.1016/S1473-3099(18)30469-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stricker BH, & Psaty BM (2004). Detection, verification, and quantification of adverse drug reactions . BMJ , 329 ( 7456 ), 44–47. doi: 10.1136/bmj.329.7456.44 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Truog RD (1992). Randomized controlled trials: lessons from ECMO . Clin Res , 40 ( 3 ), 519–527. [ PubMed ] [ Google Scholar ]
- Tsimberidou AM, Braiteh F, Stewart DJ, & Kurzrock R. (2009). Ultimate fate of oncology drugs approved by the us food and drug administration without a randomized Trial . J Clin Oncol , 27 ( 36 ), 6243–6250. doi: 10.1200/JCO.2009.23.6018 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- United Nations Office on Drugs and Crime. (2017). World Drug Report, United Nations publication (ISBN: 978–92-1–148291-1, eISBN:978–92-1–060623-3, Sales No. E.17.XI.6 ). [ Google Scholar ]
- Vandenbroucke JP (2004). When are observational studies as credible as randomised trials? Lancet , 363 ( 9422 ), 1728–1731. doi: 10.1016/S0140-6736(04)16261-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vandenbroucke JP (2006). What is the best evidence for determining harms of medical treatment? CMAJ , 174 ( 5 ), 645–646. doi: 10.1503/cmaj.051484 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vandenbroucke JP (2008). Observational research, randomised trials, and two views of medical science . PLoS Med , 5 ( 3 ), e67. doi: 10.1371/journal.pmed.0050067 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vandenbroucke JP, & Psaty BM (2008). Benefits and risks of drug treatments: how to combine the best evidence on benefits with the best data about adverse effects . JAMA , 300 ( 20 ), 2417–2419. doi: 10.1001/jama.2008.723 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vaucher J, Keating BJ, Lasserre AM, Gan W, Lyall DM, Ward J, … Holmes MV (2018). Cannabis use and risk of schizophrenia: a Mendelian randomization study . Mol Psychiatry , 23 ( 5 ), 1287–1292. doi: 10.1038/mp.2016.252 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vlieland T. (2002). Managing chronic disease: Evidence-based medicine or patient centred medicine? Health Care Analysis , 10 ( 3 ), 289–298. [ PubMed ] [ Google Scholar ]
- Williamson PR, Altman DG, Blazeby JM, Clarke M, Devane D, Gargon E, & Tugwell P. (2012). Developing core outcome sets for clinical trials: issues to consider . Trials , 13 , 132. doi: 10.1186/1745-6215-13-132 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wood E, Tyndall MW, Montaner JS, & Kerr T. (2006). Summary of findings from the evaluation of a pilot medically supervised safer injecting facility . CMAJ , 175 ( 11 ), 1399–1404. doi: 10.1503/cmaj.060863 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Worrall J. (2010). Evidence: philosophy of science meets medicine . J Eval Clin Pract , 16 ( 2 ), 356–362. doi: 10.1111/j.1365-2753.2010.01400.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wung JT, James LS, Kilchevsky E, & James E. (1985). Management of infants with severe respiratory failure and persistence of the fetal circulation, without hyperventilation . Pediatrics , 76 ( 4 ), 488–494. [ PubMed ] [ Google Scholar ]
- Yarmolinsky J, Bonilla C, Haycock PC, Langdon RJQ, Lotta LA, Langenberg C, … Martin RM (2018). Circulating Selenium and Prostate Cancer Risk: A Mendelian Randomization Analysis . J Natl Cancer Inst , 110 ( 9 ), 1035–1038. doi: 10.1093/jnci/djy081 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Youngman LD, Keavney BD, & Palmer A. (2000). Plasma fibrinogen and fibrinogen genotypes in 4685 cases of myocardial infarction and in 6002 controls: test of causality by ‘Mendelian randomization’ . Circulation , 102 ( Suppl. II ), 31–32. [ Google Scholar ]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Addiction articles from across Nature Portfolio
Addiction involves loss of control over use of a substance, often in the presence of physiological and psychological dependence on a substance and compulsion to continue seeking and using the substance despite possible negative consequences.
Latest Research and Reviews
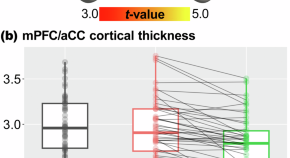
Medial prefrontal neuroplasticity during extended-release naltrexone treatment of opioid use disorder – a longitudinal structural magnetic resonance imaging study
- Zhenhao Shi
- Corinde E. Wiers
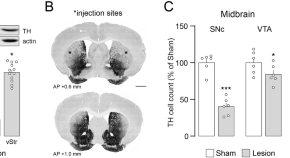
Rewarding properties of L-Dopa in experimental parkinsonism are mediated by sensitized dopamine D1 receptors in the dorsal striatum
- Carina Plewnia
- Débora Masini
- Gilberto Fisone
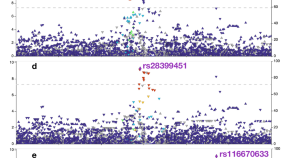
Fine-mapping the CYP2A6 regional association with nicotine metabolism among African American smokers
- Jennie G. Pouget
- Haidy Giratallah
- Rachel F. Tyndale
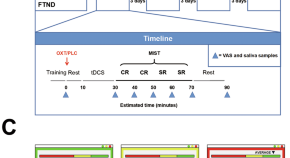
The interaction of oxytocin and nicotine addiction on psychosocial stress: an fMRI study
- Jiecheng Ren
- Yuting Zhang
- Zhengde Wei
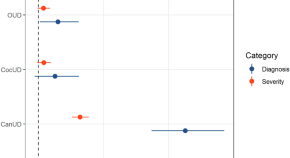
Association patterns of antisocial personality disorder across substance use disorders
- Aislinn Low
- Brendan Stiltner
- Renato Polimanti
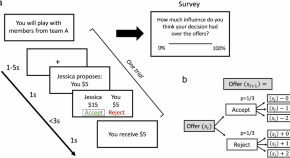
Aberrant neural computation of social controllability in nicotine-dependent humans
A neurocomputational model of social forward thinking shows that smokers under-estimate the influence of their actions on future interactions, a cognitive deficit associated with aberrant prefrontal and midbrain activities.
- Caroline McLaughlin
News and Comment
Morphine maladaptively modulates myelination.
- Leonie Welberg
Wrapping up reward
The maladaptive reward learning associated with morphine administration is shown here to be mediated by changes in dopamine-release dynamics in reward circuitry resulting from increased myelination specifically in the ventral tegmental area.
Cracking the chicken and egg problem of schizophrenia and substance use: Genetic interplay between schizophrenia, cannabis use disorder, and tobacco smoking
- Meghan J. Chenoweth
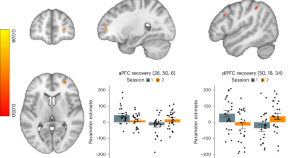
Prefrontal cortex activity increases after inpatient treatment for heroin addiction
Using task-based functional MRI, we examined inpatients with heroin use disorder. We found that 15 weeks of medication-assisted treatment (including supplemental group therapy) improved impaired anterior and dorsolateral prefrontal cortex function during an inhibitory control task. Inhibitory control, a core deficit in drug addiction, may be amenable to targeted prefrontal cortex interventions.
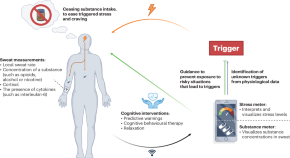
Towards on-skin analysis of sweat for managing disorders of substance abuse
A patient-centred system that leverages the analysis of sweat via wearable sensors may better support the management of patients with substance-use disorders.
- Noe Brasier
- Juliane R. Sempionatto
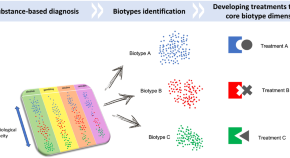
Addiction biotypes: a paradigm shift for future treatment strategies?
- Mauro Pettorruso
- Giorgio Di Lorenzo
- Giovanni Martinotti
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
We use cookies to give you the best experience possible. By continuing we’ll assume you’re on board with our cookie policy

- A Research Guide
- Research Paper Topics
- 40 Drug Abuse & Addiction Research Paper Topics
40 Drug Abuse & Addiction Research Paper Topics
Drug Abuse and Sociology
Drug abuse and medicine, drug abuse and psychology.
- Drug abuse and the degradation of neuron cells
- The social aspects of the drug abuse. The most vulnerable categories of people
- Drugs and religion. Drug abuse as the part of the sacred rituals
- Chronic Lymphocytic Leukemia
- Drug abuse as the part of human trafficking and as psychological defence of victims
- Reversible and irreversible consequences of drug abuse
- Drug abuse and minors
- Ethnic and cultural traditions that may lead to drug abuse
- Medical marijuana. Can legalizing it lead to drug abuse?
- The ethical questions of abusing painkiller drugs or other drugs that ease the state of a person
- The “club culture”. May it enhance the danger of drug abuse?
- Preventing drug abuse. Mandatory examination or voluntary learning: what will help most?
- The abstinence after the drug abuse. Rehabilitation and resocialization of the victims of it
- The harm done by drug abuse to the family and social relations
- The types of drugs and the impact of their abuse to the human body
- The positive effects of drugs. May they be reached without drawbacks of drug abuse?
- Alcoholics Anonymous, similar organisations and their role in overcoming the dependency
- Is constant smoking a drug abuse? Quitting smoking: government and social decisions
- Exotic addictions: game addiction, porn addiction etc. Do they have the effects similar to drug abuse?
- Substance abuse during pregnancy and before conceiving. What additional harm it causes?
- The correlation between drugs and spreading of HIV/AIDS
- Drug abuse and crime rates
- History of drug abuse. Opium houses, heroin cough syrup and others
- Drunk driving and drunk violence. The indirect victims of alcohol abuse
- The social rejection of the former drug abusers and the way to overcome it
- The main causes of drug abuse in the different social groups
- Drug abuse and mental health
- LGBTQ+ and drug abuse
- The development of drug testing. The governmental implementation of it
- Geniuses and drug abuse. Did drugs really helped them to create their masterpieces?
- Shall the laws about drug abuse be changed?
- Health Care Information Technology
- Drug abuse and global health throughout the 20-21 centuries
- Personal freedom or the safety of society: can drugs be allowed for personal use?
- Legal drinking age in different countries and its connection to the cultural diversity
- The different attitude to drugs and drug abuse in the different countries. Why it differs so much?
- Teenage and college culture. Why substance abuse is considered to be cool?
- Drugs, rape and robbery. Drugging people intentionally as the way to prevent them defending themselves
- 12-Step Programs and their impact on healing the drug addiction
- Alcohol, tobacco and sleeping pills advertising. Can it lead to more drug abuse?
By clicking "Log In", you agree to our terms of service and privacy policy . We'll occasionally send you account related and promo emails.
Sign Up for your FREE account

Substance use, abuse, and addiction

Substance use disorder is a cluster of physiological, behavioral, and cognitive symptoms associated with the continued use of substances despite substance-related problems, distress, and/or impairment, such as impaired control and risky use.
Addiction is a state of psychological and/or physical dependence on the use of drugs or other substances, such as alcohol, or on activities or behaviors, such as sex, exercise, and gambling.
Adapted from the APA Dictionary of Psychology
Resources from APA

Science-backed interventions for problematic gaming
Evidence-based psychological interventions can help people with an excessive drive to play

Reclassification of cannabis is a win for researchers
Now deemed a less dangerous drug, scientists are optimistic that more studies on the benefits and risks of cannabis will be possible.

Substance use disorders in people with serious mental illness
Psychologists help these patients kick nicotine and other addictions

The emergence of psychedelics as medicine
Research confirms the potential of these drugs to help people with treatment-resistant mental health conditions
What APA is doing

Substance use disorders
APA Services advocates for policies, programs, and funding to improve the prevention and treatment of opioid and other substance use disorders, including nonpharmacological interventions for pain management.

Society for Psychopharmacology and Substance Use
APA’s Division 28 promotes teaching, research, and dissemination of information regarding the effects of drugs on behavior.

Society of Addiction Psychology
APA’s Division 50 promotes advances in research, professional training, and clinical practice within the broad range of addictive behaviors including problematic use of alcohol, nicotine, and other drugs and disorders involving gambling, eating, sexual behavior, or spending.
Addictive Behaviors
Alcohol and Illicit Drug Use in the Workforce and Workplace
Designing Interventions to Promote Community Health
Methamphetamine Addiction
Trauma and Substance Abuse, 2nd Edition
Magination Press children’s books

All the Pieces
Journal special issues
Combined Use of Alcohol and Cannabis
Brief Alcohol Interventions for Young Adults
Neuroimaging Mechanisms of Change in Psychotherapy for Addictive Behaviors
Sex Differences in Drug Abuse
Substance Use Disorders and Addictions
APA journals
Journal of Consulting and Clinical Psychology
Journal of Psychopathology and Clinical Science
Psychology of Addictive Behaviors
Experimental and Clinical Psychopharmacology
- Signs of Addiction
Addiction Research
Discover the latest in addiction research, from the neuroscience of substance use disorders to evidence-based treatment practices. reports, updates, case studies and white papers are available to you at hazelden betty ford’s butler center for research..

Why do people become addicted to alcohol and other drugs? How effective is addiction treatment? What makes certain substances so addictive? The Butler Center for Research at the Hazelden Betty Ford Foundation investigates these and other questions and publishes its scientific findings in a variety of alcohol and drug addiction research papers and reports. Research topics include:
- Evidence-based treatment practices
- Addiction treatment outcomes
- Addiction, psychiatry and the brain
- Addictive substances such as prescription opioids and heroin
- Substance abuse in youth/teens, older adults and other demographic groups such as health care or legal professionals
These research queries and findings are presented in the form of updates, white papers and case studies. In addition, the Butler Center for Research collaborates with the Recovery Advocacy team to study special-focus addiction research topics, summarized in monthly Emerging Drug Trends reports. Altogether, these studies provide the latest in addiction research for anyone interested in learning more about the neuroscience of addiction and how addiction affects individuals, families and society in general. The research also helps clinicians and health care professionals further understand, diagnose and treat drug and alcohol addiction. Learn more about each of the Butler Center's addiction research studies below.
Research Updates
Written by Butler Center for Research staff, our one-page, topic-specific summaries discuss current research on topics of interest within the drug abuse and addiction treatment field.
View our most recent updates, or view the archive at the bottom of the page.
Patient Outcomes Study Results at Hazelden Betty Ford
Trends and Patterns in Cannabis Use across Different Age Groups
Alcohol and Tobacco Harm Reduction Interventions
Harm Reduction: History and Context
Racial and Ethnic Health Disparities and Addiction
Psychedelics as Therapeutic Treatment
Sexual and Gender Minority Youth and SUDs
Health Care Professionals and Mental Health
Grief and Addiction
Helping Families Cope with Addiction
Emerging Drug Trends Report and National Surveys
Shedding New Light on America’s No. 1 Health Problem
In collaboration with the University of Maryland School of Public Health and with support from the Butler Center for Research, the Recovery Advocacy team routinely issues research reports on emerging drug trends in America. Recovery Advocacy also commissions national surveys on attitudes, behaviors and perspectives related to substance use. From binge drinking and excessive alcohol use on college campuses, to marijuana potency concerns in an age of legalized marijuana, deeper analysis and understanding of emerging drug trends allows for greater opportunities to educate, inform and prevent misuse and deaths.
Each drug trends report explores the topic at hand, documenting the prevalence of the problem, relevant demographics, prevention and treatment options available, as well as providing insight and perspectives from thought leaders throughout the Hazelden Betty Ford Foundation.
View the latest Emerging Drug Trends Report:
Pediatricians First Responders for Preventing Substance Use
- Clearing Away the Confusion: Marijuana Is Not a Public Health Solution to the Opioid Crisis
- Does Socioeconomic Advantage Lessen the Risk of Adolescent Substance Use?
- The Collegiate Recovery Movement Is Gaining Strength
- Considerations for Policymakers Regarding Involuntary Commitment for Substance Use Disorders
- Widening the Lens on the Opioid Crisis
- Concerns Rising Over High-Potency Marijuana Use
- Beyond Binging: “High-Intensity Drinking”
View the latest National Surveys :
- College Administrators See Problems As More Students View Marijuana As Safe
College Parents See Serious Problems From Campus Alcohol Use
- Youth Opioid Study: Attitudes and Usage
About Recovery Advocacy
Our mission is to provide a trusted national voice on all issues related to addiction prevention, treatment and recovery, and to facilitate conversation among those in recovery, those still suffering and society at large. We are committed to smashing stigma, shaping public policy and educating people everywhere about the problems of addiction and the promise of recovery. Learn more about recovery advocacy and how you can make a difference.
Evidence-Based Treatment Series
To help get consumers and clinicians on the same page, the Butler Center for Research has created a series of informational summaries describing:
- Evidence-based addiction treatment modalities
- Distinctive levels of substance use disorder treatment
- Specialized drug and alcohol treatment programs
Each evidence-based treatment series summary includes:
- A definition of the therapeutic approach, level of care or specialized program
- A discussion of applicability, usage and practice
- A description of outcomes and efficacy
- Research citations and related resources for more information
View the latest in this series:
Motivational Interviewing
Cognitive Behavioral Therapy

Case Studies and White Papers
Written by Hazelden Betty Ford Foundation researchers and clinicians, case studies and white papers presented by the Butler Center for Research provide invaluable insight into clinical processes and complex issues related to addiction prevention, treatment and recovery. These in-depth reports examine and chronicle clinical activities, initiatives and developments as a means of informing practitioners and continually improving the quality and delivery of substance use disorder services and related resources and initiatives.
- What does it really mean to be providing medication-assisted treatment for opioid addiction?
Adolescent Motivational Interviewing
Peer Recovery Support: Walking the Path Together
Addiction and Violence During COVID-19
The Brain Disease Model of Addiction
Healthcare Professionals and Compassion Fatigue
Moving to Trauma-Responsive Care
Virtual Intensive Outpatient Outcomes: Preliminary Findings
Driving Under the Influence of Cannabis
Vaping and E-Cigarettes
Using Telehealth for Addiction Treatment
Grandparents Raising Grandchildren
Substance Use Disorders Among Military Populations
Co-Occurring Mental Health and Substance Use Disorders
Women and Alcohol
Prescription Rates of Opioid Analgesics in Medical Treatment Settings
Applications of Positive Psychology to Substance Use Disorder
Substance Use Disorders Among Legal Professionals
Factors Impacting Early Alcohol and Drug Use Among Youths
Animal-Assisted Therapy for Substance Use Disorders
Prevalence of Adolescent Substance Misuse
Problem Drinking Behaviors Among College Students
The Importance of Recovery Management
Substance Use Factors Among LGBTQ individuals
Prescription Opioids and Dependence
Alcohol Abuse Among Law Enforcement Officers
Helping Families Cope with Substance Dependence
The Social Norms Approach to Student Substance Abuse Prevention
Drug Abuse, Dopamine and the Brain's Reward System
Women and Substance Abuse
Substance Use in the Workplace
Health Care Professionals: Addiction and Treatment
Cognitive Improvement and Alcohol Recovery
Drug Use, Misuse and Dependence Among Older Adults
Emerging Drug Trends
Does Socioeconomic Advantage Lessen the Risk of Adolescent Substance Use
The Collegiate Recovery Movement is Gaining Strength
Involuntary Commitment for Substance Use Disorders
Widening the Lens of the Opioid Crisis
Beyond Binge Drinking: High Intensity Drinking
High Potency Marijuana
National Surveys
College Administrators See Problems as More Students View Marijuana as Safe
Risky Opioid Use Among College-Age Youth
Case Studies/ White Papers
What does it really mean to be providing medication-assisted treatment for opioid addiction
Are you or a loved one struggling with alcohol or other drugs? Call today to speak confidentially with a recovery expert. Most insurance accepted.
Harnessing science, love and the wisdom of lived experience, we are a force of healing and hope for individuals, families and communities affected by substance use and mental health conditions..
Search Issues
Vol. XXVIII, No. 4, Summer 2012
Eight Questions for Drug Policy Research
By Mark A. R. Kleiman , Jonathan P. Caulkins , Angela Hawken , Beau Kilmer
The current research agenda has only limited capacity to shrink the damage caused by drug abuse. Some promising alternative approaches could lead to improved results.
Drug abuse—of licit and illicit drugs alike—is a big medical and social problem and attracts a substantial amount of research attention. But the most attractive and most easily fundable research topics are not always those with the most to contribute to improved social outcomes. If the scientific effort paid more attention to the substantial opportunities for improved policies, its contribution to the public welfare might be greater.
The current research agenda around drug policy concentrates on the biology, psychology, and sociology of drugtaking and on the existing repertoire of drug-control interventions. But that repertoire has only limited capacity to shrink the damage that drug users do to themselves and others or the harms associated with drug dealing, drug enforcement, and drug-related incarceration; and the current research effort pays little attention to some innovative policies with substantial apparent promise of providing improved results.
At the same time, public opinion on marijuana has shifted so much that legalization has moved from the dreams of enthusiasts to the realm of practical possibility. Yet voters looking to science for guidance on the practicalities of legalization in various forms find little direct help.
All of this suggests the potential of a research effort less focused on current approaches and more attentive to alternatives.
The standard set of drug policies largely consists of:
- Prohibiting the production, sale, and possession of drugs
- Seizing illicit drugs
- Arresting and imprisoning dealers
- Preventing the diversion of pharmaceuticals to nonmedical use
- Persuading children not to begin drug use
- Offering treatment to people with drug-abuse disorders or imposing it on those whose behavior has brought them into conflict with the law
- Making alcohol and nicotine more expensive and harder to get with taxes and regulations
- Suspending the drivers’ licenses of those who drive while drunk and threatening them with jail if they keep doing it
With respect to alcohol and tobacco, there is great room or improvement even within the existing policy repertoire for example, by raising taxes), even before more-innovaive approaches are considered. With respect to the currently illicit drugs, it is much harder to see how increasing or slightly modifying standard-issue efforts will measurably shrink the size of the problems.
The costs—fiscal, personal, and social—of keeping half a million drug offenders (mostly dealers) behind bars are sufficiently great to raise the question of whether less comprehensive but more targeted drug enforcement might be the better course. Various forms of focused enforcement offer the promise of greatly reduced drug abuse, nondrug crime, and incarceration. These include testing and sanctions programs, interventions to shrink flagrant retail drug markets, collective deterrence directed at violent drug-dealing organizations, and drug-law enforcement aimed at deterring and incapacitating unusually violent individual dealers. Substantial increases in alcohol taxes might also greatly reduce abuse, as might developing more- effective treatments for stimulant abusers or improving the actual evidence base underlying the movement toward “evidence-based policies.”
These opportunities and changes ought to influence the research agenda. Surely what we try to find out should bear some relationship to the practical choices we face. Below we list eight research questions that we think would be worth answering. We have selected them primarily for policy relevance rather than for purely scientific interest.
1) How responsive is drug use to changes in price, risk, availability, and “normalcy”?
The fundamental policy question concerning any drug is whether to make it legal or prohibited. Although the choice s not merely binary, a fairly sharp line divides the spectrum of options. A substance is legal if a large segment of he population can purchase and possess it for unsupervised “recreational” use, and if there are no restrictions on who can produce and sell the drug beyond licensing and routine regulations.
Accepting that binary simplification, the choice becomes what kind of problem one prefers. Use and use-related problems will be more prevalent if the substance is legal. Prohibition will reduce, not eliminate, use and abuse, but with three principal costs: black markets that can be violent and corrupting, enforcement costs that exceed those of regulating a legal market, and increased damage per unit of consumption among those who use despite the ban. (Total use related harm could go up or down depending on the extent to which the reduction in use offsets the increase in harmfulness per unit of use.)
The costs of prohibition are easier to observe than are its benefits in the form of averted use and use-related problems. In that sense, prohibition is like investments in prevention, such as improving roads; it’s easier to identify the costs than to identify lives saved in accidents that did not happen.
We would like to know the long-run effect on consumption of changes in both price and the nonprice aspects of availability, including legal risks and stigma. There is now a literature estimating the price elasticity of demand for illegal drugs, but the estimates vary widely from one study to the next and many studies are based on surveys that may not give adequate weight to the heavy users who dominate consumption. Moreover, legalization would probably involve price declines that go far beyond the support of historical data.
Furthermore, as Mark Moore pointed out many years ago, the nonprice terms of availability, which he conceptualized as “search cost,” may match price effects in terms of their impact on consumption. Ye t those effects have never been quantitatively estimated for a change as profound as that from illegality to legality. The decision not to enforce laws against small cannabis transactions in the Netherlands did not cause an explosion in use; whether and how much it increased consumption and whether the establishment of retail shops mattered remain controversial questions.
This ignorance about the effect on consumption hamstrings attempts to be objective and analytical when discussing the question of whether to legalize any of the currently illicit drugs, and if so, under what conditions.
2) How responsive is the use of drug Y to changes in policy toward drug X?
Polydrug use is the norm, particularly among frequent and compulsive users. (Most users do not fall in that category, but the minority who do account for the bulk of consumption and harms.) Therefore, “scoring” policy interventions by considering only effects on the target substance is potentially misleading.
For example, driving up the price of one drug, say cocaine, might reduce its use, but victory celebrations should be tempered if the reduction stemmed from users switching to methamphetamine or heroin. On the other hand, school based drug-prevention efforts may generate greater benefits through effects on alcohol and tobacco abuse than via their effects on illegal drug use. Comparing them to other drug-control interventions, such as mandatory minimum sentences for drug dealers, in terms of ability to control illegal drugs alone is a mistake; those school-based prevention interventions are not (just) illicit-drug–control programs.
But policy is largely made one substance at a time. Drugs are added to schedules of prohibited substances based on their potential for abuse and for use as medicine. Reformers clamor for evidence-based policies that rank individual drugs’ harmfulness, as attempted recently by David Nutt, and ban only the most dangerous. Ye t it makes little practical sense to allow powder cocaine while banning crack, because anyone with baking soda and a microwave oven can convert powder to crack.
Considerations of substitution or complementarity ought to arise in making policy toward some of the so-called designer drugs. Mephedrone looks relatively good if most of its users would otherwise have been abusing methamphetamine; it looks terrible if in fact it acts as a stepping stone to methamphetamine use. But no one knows which is the case.
Marijuana legalization is in play in a way it has not been since the 1970s. Various authors have produced social-welfare analyses of marijuana legalization, toting up the benefits of reduced enforcement costs and the costs of greater need for treatment, accounting for potential tax revenues and the like.
Yet the marijuana-specific gains and losses from legalization would be swamped by the uncertainties concerning its effects on alcohol consumption. The damage from alcohol is a large multiple of the damage from cannabis; thus a 10% change, up or down, in alcohol abuse could outweigh any changes in marijuana-related outcomes.
There is conflicting evidence as to whether marijuana and alcohol are complements or substitutes; no one can rule out even larger increases or decreases in alcohol use as a result of marijuana legalization, especially in the long run.
Marijuana legalization might also influence heavy use of cocaine or cigarette smoking. But again, no one knows whether that effect would be to drive cocaine or cigarette use up or down, let alone by how much. If doubling marijuana use led to even a 1% increase or decrease in tobacco use, it could produce 4,000 more or 4,000 fewer tobacco related deaths per year, far more than the (quite small) number of deaths associated with marijuana.
This uncertainty makes it impossible to produce a solid benefit/cost analysis of marijuana legalization with existing data. That suggests both caution in drawing policy conclusions and aggressive efforts to learn more about cross-elasticities among drugs prone to abuse.
3) Can we stop large numbers of drug-involved criminal offenders from using illicit drugs?
Many county, state, and federal initiatives target drug use among criminal offenders. Ye t most do little to curtail drug use or crime. An exception is the drug courts process; some implementations of that idea have been shown to reduce drug use and other illegal behavior. Unfortunately, the resource intensity of drug courts limits their potential scope. The requirement that every participant must appear regularly before a judge for a status hearing means that a drug court judge can oversee fewer than 100 offenders at any time.
The HOPE approach to enforcing conditions of probation and parole, named after Hawaii’s Opportunity Probation with Enforcement, offers the potential for reducing use among drug-involved offenders at a larger scale. Like drug courts, HOPE provides swift and certain sanctions for probation violations, including drug use. HOPE starts with a formal warning that any violation of probation conditions will lead to an immediate but brief stay in jail. Probationers are then subject to regular random drug testing: six times a month at first, diminishing in frequency with sustained compliance. A positive drug test leads to an immediate arrest and a brief jail stay (usually a few days but in some jurisdictions as little as a few hours in a holding cell). Probationers appear before the judge only if they have violated a rule; in contrast, a drug court judge participates in every status review. Thus HOPE sites can supervise large numbers of offenders; a single judge in Hawaii now supervises more than 2,000 HOPE probationers.
In a large randomized controlled trial (RCT), Hawaii’s HOPE program greatly outperformed standard probation in reducing drug use, new crimes, and incarceration among a population of mostly methamphetamine-using felony probationers. A similar program in Tarrant County, Texas (encompassing Arlington and Fort Worth), appears to produce similar results, although this has not yet been verified by an RCT, as has a smaller-scale program (verified by an RCT) among parolees in Seattle. Reductions in drug use of 80%, in new arrests of 30 to 50%, and in days behind bars of 50% appear to be achievable at scale. The last result is the most striking; get-tough automatic-incarceration policies can reduce incarceration rather than increasing it, if the emphasis is on certainty and celerity rather than severity.
The Department of Justice is funding four additional RCTs; those results should help clarify how generalizable the HOPE outcomes are. But to date there has been no systematic experimentation to test how variations in program parameters lead to variations in results.
Hawaii’s HOPE program uses two days in jail as its typical first sanction. Penalties escalate for repeated violations, and the 15% or so of participants who violate a fourth time face a choice between residential treatment and prison. No one is mandated to undergo treatment except after repeated failures. The results suggest that this is an effective design, but is it optimal? Would some sanction short of jail for the first violation—a curfew, home confinement, or community service—work as well? Are escalating penalties necessary and if so, what is the optimal pattern of escalation? Is there a subset of offenders who ought to be mandated to treatment immediately rather than waiting for failures to accumulate? Should cannabis be included in the list of drugs tested for, as it is in Hawaii, or excluded? How about synthetically produced cannabinoids (sold as “Spice”) and cathinones (sold as “bath salts”), which require more complex and costly screening? Would adding other services to the mix improve outcomes? How can HOPE be integrated with existing treatment-diversion programs and drug courts? How can HOPE principles best be applied to parole, pretrial release, and juvenile offenders?
Answering these questions would require measuring the results of systematic variation in program conditions. There is no strong reason to think that the optimal program design will be the same in every jurisdiction or for every offender population. But it’s time to move beyond the question “Does HOPE work?” to consider how to optimize the design of testing-and-sanctions programs.
4) Can we stop alcohol-abusing criminal offenders from getting drunk?
Under current law, state governments effectively give every adult a license to purchase and consume alcohol in unlimited quantities. Judges in some jurisdictions can temporarily revoke that license for those with an alcohol-related offense by prohibiting drinking and going to bars as conditions of bail or probation. However, because alcohol passes through the body quickly, a typical random-but-infrequent testing regiment would miss most violations, making the revocation toothless.
In 2005, South Dakota embraced an innovative approach to this problem, called 24/7 Sobriety. As a condition of bail, repeat drunk drivers who were ordered to abstain from alcohol were now subject to twice-a-day breathalyzer tests, every day. Those testing positive or missing the test were immediately subject to a short stay in jail, typically a night or two. What started as a five-county pilot program expanded throughout the state, and judges began applying the program to offenders with all types of alcohol-related criminal behavior, not just drunk driving. Some jurisdictions even started using continuous alcohol-monitoring bracelets, which can remotely test for alcohol consumption every 30 minutes. Approximately 20,000 South Dakotans have participated in 24/7—an astounding figure for a state with a population of 825,000.
The anecdotal evidence about the program is spectacular; fewer than 1% of the 4.8 million breathalyzer tests ordered since 2005 were failed or missed. That is not because the offenders have no interest in drinking. About half of the participants miss or fail at least one test, but very few do so more than once or twice. 24/7 is now up and running in other states, and will soon be operating in the United Kingdom. As of yet there are no peer-reviewed studies of 24/7, but preliminary results from a rigorous quasi-experimental evaluation suggest that the program did reduce repeat drunk driving in South Dakota. Furthermore, as with HOPE, there remains a need to better understand for whom the program works, how long the effects last, the mechanism(s) by which it works, and whether it can be effective in a more urban environment.
Programs such as HOPE and 24/7 can complement traditional treatment by providing “behavioral triage.” Identifying which subset of substance abusers cannot stop drinking on their own, even under the threat of sanctions, allows the system to direct scarce treatment resources specifically to that minority.
Another way to take away someone’s drinking license would be to require that bars and package stores card every would be to require that bars and package stores card every buyer and to issue modified driver’s licenses with nondrinker markings on them to those convicted of alcohol-related crimes. This approach would probably face legal and political challenges, but that should not discourage serious analysis of the idea.
There is also strong evidence that increasing the excise tax on alcohol could reduce alcohol-related crime. Duke University economist Philip Cook estimates that doubling the federal tax, leading to a price increase of about 10%, would reduce violent crime and auto fatalities by about 3%, a striking saving in deaths for a relatively minor and easy-to-administer policy change. There is also evidence that formal treatment, both psychological and pharmacological, can yield improvements in outcomes for those who accept it.
There is also strong evidence that increasing the excise linked. Among people with drug problems who are also crimtax on alcohol could reduce alcohol-related crime. Duke Uni- inally active, criminal activity tends to rise and fall with drug versity economist Philip Cook estimates that doubling the consumption. Reductions in crime constitute a major benfederal tax, leading to a price increase of about 10%, would efit of providing drug treatment for the offender population, reduce violent crime and auto fatalities by about 3%, a strik- or of imposing HOPE-style community supervision. ing saving in deaths for a relatively minor and easy-to-ad- Reducing drug use among active offenders could also minister policy change. There is also evidence that formal shrink illicit drug markets, producing benefits everywhere, treatment, both psychological and pharmacological, can yield from inner-city neighborhoods wracked by flagrant drug improvements in outcomes for those who accept it.
5) How concentrated is hard-drug use among active criminals?
Literally hundreds of substances have been prohibited, but the big three expensive drugs (sometimes called the “hard” drugs)—cocaine, including crack; heroin; and methamphetamine— account for most of the societal harm. The serious criminal activity and other harms associated with those substances are further highly concentrated among a minority of their users. Many people commit a little bit of crime or use hard drugs a handful of times, but relatively few make a habit of either one. Despite their relatively small numbers, those frequent users and their suppliers account for a large share of all drug-related crime and violence.
The populations overlap; an astonishing proportion of those committing income-generating crimes, such as robbery, as opposed to arson, are drug-dependent and/or intoxicated at the time of their offense, and a large proportion of frequent users of expensive drugs commit income-generating crime. Moreover, the two sets of behaviors are causally linked. Among people with drug problems who are also criminally active, criminal activity tends to rise and fall with drug consumption. Reductions in crime constitute a major benefit of providing drug treatment for the offender population, or of imposing HOPE-style community supervision.
Reducing drug use among active offenders could also shrink illicit drug markets, producing benefits everywhere, from inner-city neighborhoods wracked by flagrant drug dealing to source and transit countries such as Colombia and Mexico.
A back-of-the envelope calculation suggests the potential size of these effects. The National Survey on Drug Use and Health estimates users in the household population. The Arrestee Drug Abuse Monitoring Program measures the rate of active substance use among active offenders (by self-report and urinalysis). Two decades ago, an author of this article (Kleiman) and Chris Putala, then on the Senate Judiciary Committee staff, used the predecessors of those surveys to estimate that about three-quarters of all heavy (morethan-weekly) cocaine users had been arrested for a nondrug felony in the previous year.
Applying the Pareto Law’s rule of thumb that 80% of the volume of any activity is likely to be accounted for by about 20% of those who engage in it—true, for example, about the distribution of alcohol consumption—suggests that something like three-fifths of all the cocaine is used by people who get arrested in the course of a typical year and who are therefore likely to be on probation, parole, or pretrial release if not behind bars.
Combining that calculation with the result from HOPE that frequent testing with swift and certain sanctions can shrink (in the Hawaii case) methamphetamine use among heavily drug-involved felony probationers by 80%, suggests that total hard-drug volume might be reduced by something like 50% if HOPE-style supervision were applied to all heavy users of hard drugs under criminal-justice supervision. No known drug-enforcement program has any comparable capability to shrink illicit-market volumes.
By the same token, HOPE seems to reduce criminal activity, as measured by felony arrests, by 30 to 50%. If frequent offenders commit 80% of income-generating crime, and half of those frequent offenders also have serious harddrug problems, such a reduction in offending within that group could reduce total income-generating crime by approximately 15 to 20%, while also decreasing the number of jail and prison inmates.
The Kleiman and Putala estimate was necessarily crude because it was based on studies that weren’t designed to measure the concentration of hard-drug use among offenders. Unfortunately, no one in the interim has attempted to refine that estimate with more precise methods (for example, stochastic-process modeling) or more recent data.
6) What is the evidence for evidence-based practices?
Many agencies now recommend (and some states and federal grant programs mandate) adoption of prevention and treatment programs that are evidence-based. But the move toward evidence-based practices has one serious limitation: the quality of the evidence base. It is important to ask what qualifies as evidence and who gets to produce it. Many programs are expanded and replicated on the basis of weak evidence. Study design matters. A review by George Mason University Criminologist David Weisburd and colleagues showed that the effect size of offender programs is negatively related to study quality: The more rigorous the study is, the smaller its reported effects.
Who does the evaluation can also make a difference. Texas A&M Epidemiologist Dennis Gorman found that evaluations authored by program developers report much larger effect sizes than those authored by independent researchers. Yet Benjamin Wright and colleagues reported that more than half of the substance-abuse programs targeting criminal-justice programs that were designated as evidence-based on the Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) National Registry of Evidence Based Programs and Practices (NREPP) include the program developer as evaluator. Consequently, we may be spending large sums of money on ineffective programs. Many jurisdictions, secure in their illusory evidence base, could become complacent about searching for alternative programs that really do work.
We need to get better at identifying effective strategies and helping practitioners sort through the evidence. Requiring that publicly funded programs be evaluated and show improved outcomes using strong research designs—experimental designs where feasible, well-designed historicalcontrol strategies where experiments can’t be done, and “intent-to-treat” analyses rather than cherry-picking success by studying program completers only—would cut the number of programs designated as promising or evidence-based by more than 75%. Not only would this relieve taxpayers of the burden of supporting ineffective programs, it would also help researchers identify more promising directions for future intervention research.
The potential for selection biases when studying druginvolved people is substantial and thus makes experimental designs much more valuable. Small is key. It avoids expense, and equally important, it avoids champions with bruised egos. It is difficult to scale back a program once an agency becomes invested in the project. Small pilot evaluations that do show positive outcomes can then be replicated and expanded if the replications show similarly positive results.
7) What treats stimulant abuse?
Science can alleviate social problems not only by guiding policy but also by inventing better tools. The holy grail of such innovations would be a technology that addresses stimulant dependence.
The ubiquitous “treatment works” mantra masks a sharp disparity in technologies available for treating opiates (heroin and oxycodone) as opposed to stimulants (notably cocaine, crack, and meth). A variety of so-called opiate-substitute therapies (OSTs) exist that essentially substitute supervised use of legal, pure, and cheap opiates for unsupervised use of street opiates. Methadone is the first and best-known OST, but there are others. A number of countries even use clinically supplied heroin to substitute for street heroin.
OST stabilizes dependent individuals’ chaotic lives, with positive effects on a wide range of life outcomes, such as increased employment and reduced criminality and rates of overdose. Sometimes stabilization is a first step toward abstinence, but for better and for worse the dominant thinking since the 1980s has been to view substitution therapy as an open-ended therapy, akin to insulin for diabetics. Either way, OST consistently fares very well in evaluations that quantify social benefits produced relative to program costs.
There is no comparable technology for treating stimulant dependence. This is not for lack of trying. The National Institute on Drug Abuse has invested hundreds of millions of dollars in the quest for pharmacotherapies for stimulants. Decades of work have produced many promising advances in basic science, but with comparatively little effect on clinical practice. The gap between opiate and stimulant treatment technologies matters more in the United States and the rest of the Western Hemisphere, where stimulants have a large market, than in the rest of the world, where opiates remain predominant.
There are two reactions to this zero-for-very-many batting average. One is to redouble efforts; after all, Edison tried a lot of filament materials before hitting on carbonized bamboo. The other is to give up on the quest for a chemical that can offset, undo, or modulate stimulants’ effects in the brain and pursue other approaches. For example, immunotherapies are a fundamentally different technology inasmuch as the active introduced agent does not cross the blood-brain barrier. Rather, the antibodies act almost more like interdiction agents, but interdicting the drug molecules between ingestion and their crossing the blood-brain barrier rather than interdicting at the nation’s border.
There is evidence from clinical trials showing that some cognitive-behavioral therapies can reduce stimulant consumption for some individuals. Contingency management also takes a behavioral rather than a chemical approach, essentially incentivizing dependent users to remain abstinent. The stunning finding is that, properly deployed, very small incentives (for example, vouchers for everyday items) can induce much greater behavioral change than can conventional treatment methods alone.
The ability of contingency management to reduce consumption, and the finding that even the heaviest users respond to price increases by consuming less, profoundly challenge conventional thinking about the meaning of addiction. They seem superficially at odds with the clear evidence that addiction is a brain disease with a physiological basis. Brainimaging studies let us see literally how chronic use changes the brain in ways that are not reversed by mere withdrawal of the drugs. So just as light simultaneously displays characteristics of a particle and a wave, so too addiction simultaneously has characteristics of a physiological disease and a behavior over which the person has (at least limited) control.
8) What reduces drug-market violence?
Drug dealers can be very violent. Some use violence to settle disputes about territory or transactions; others use violence to climb the organizational ladder or intimidate witnesses or enforcement officials. Because many dealers have guns or have easy access to them, they also sometimes use these weapons to address conflicts that have nothing to do with drugs. Because the market tends to replace drug dealers who are incarcerated, there is little reason to think that routine drug-law enforcement can reduce violence; the opposite might even be true if greater enforcement pressure makes violence more advantageous to those most willing to use it.
That raises the question of whether drug-law enforcement can be designed specifically to reduce violence. One set of strategies toward this end is known as focused deterrence or pulling-levers policing. These approaches involve lawenforcement officials directly communicating a credible threat to violent individuals or groups, with the goal of reducing the violence level, even if the level of drug dealing or gang activity remains the same. Such interventions aim to tip situations from high-violence to low-violence equilibria by changing the actual and perceived probability of punishment; for example, by making violent drug dealing riskier, in enforcement terms, than less violent drug dealing.
The seminal effort was the Boston gun project Ceasefire, which focused on reducing juvenile homicides in the mid-1990s. Recognizing that many of the homicides stemmed from clashes between juvenile gangs, the strategy focused on telling members of each gang that if anyone in the gang shot someone (usually a member of a rival gang) police and prosecutors would pull every lever legally available against the entire gang, regardless of which individual had pulled the trigger. Instead of receiving praise from colleagues for increasing the group’s prestige, the potential shooter now had to deal with the fact that killing put the entire group at risk. Thus the social power of the gang was enlisted on the side of violence reduction. The results were dramatic: Youth gun homicides in Boston fell from two a month before the intervention to zero while the intervention lasted. Variants of Ceasefire have been implemented across the country, some with impressive results.
An alternative to the Ceasefire group-focused strategy is a focus on specific drug markets where flagrant dealing leads to violence and disorder. Police and prosecutors in High Point, North Carolina, adopted a focused-deterrence approach, which involved strong collaborations with community members. Their model, referred to as the Drug Market Intervention, involved identifying all of the dealers in the targeted market, making undercover buys from them (often on film), arresting the most violent dealers, and not arresting the others. Instead, the latter were invited to a community meeting where they were told that, although cases were made against them, they were going to get another chance as long as they stopped dealing. The flagrant drug market in that neighborhood, as David Kennedy reports, vanished literally overnight and has not reappeared for the subsequent seven years. The program has been replicated in dozens of jurisdictions, and there is a growing evidence base showing that it can reduce crime.
A third approach recognizes the heterogeneity in violence among individual drug dealers. By focusing enforcement on those identified as the most violent, police can create both Darwinian and incentive pressures to reduce the overall violence level. This technique has yet to be systematically evaluated. This seems like an attractive research opportunity if a jurisdiction wants to try out such an approach.
An especially challenging problem is dealing-related violence in Mexico, now claiming more than 1,000 lives per month. It is worth considering whether a Ceasefire-style strategy might start a tipping process toward a less violent market. Such a strategy could exploit two features of the current situation: The Mexican groups make most of their money selling drugs for distribution in the United States, and the United States has much greater drug enforcement capacity than does Mexico. If the Mexican government were to select one of the major organizations and target it for destruction after a transparent process based on relative violence levels, U.S. drug-law enforcement might be able to put the target group out of business by focusing attention on the U.S. distributors that buy their drugs from the target Mexican organization, thereby pressuring them to find an alternative source. If that happened, the target organization would find itself without a market for its product.
If one organization could be destroyed in this fashion, the remaining groups might respond to an announcement that a second selection process was underway by competitively reducing their violence levels, each hoping that one of its rivals would be chosen as the second target. The result might be—with the emphasis on might—a dramatic reduction in bloodshed.
Whatever the technical details of violence-minimizing drug-law enforcement, its conceptual basis is the understanding that in established markets enforcement pressure can have a greater effect on how drugs are sold than on how much is sold. So violence reduction is potentially more feasible than is greatly reducing drug dealing generally.
Drug policy involves contested questions of value as well as of fact; that limits the proper role of science in policymaking. And many of the factual questions are too hard to be solved with the current state of the art: The mechanisms of price and quantity determination in illicit markets, for example, have remained largely impervious to investigation. Conversely, research on drug abuse can provide insight into a variety of scientifically interesting questions about the nature of human motivation and self-regulation, complicated by imperfect information, intoxication, and impairment, and engaging group dynamics and tipping phenomena; not every study needs to be justified in terms of its potential contribution to making better policy. However, good theory is often developed in response to practical challenges, and policymakers need the guidance of scientists. Broadening the current research agenda away from biomedical studies and evaluations of the existing policy repertoire could produce both more interesting science and more successful policies.
Join the Conversation
Sign up for the Issues in Science and Technology newsletter to get the latest policy insights delivered direct to your inbox. When you do, you'll receive a special offer for nearly 50% off a one-year subscription to the magazine—or simply subscribe now at this special rate .
- Name * First Last
- Name This field is for validation purposes and should be left unchanged.
- Media Center
- Events & Webinars
- Healthy Minds TV
- Email Signup
- Get Involved
- Anxiety Disorders
- Attention-Deficit Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder (ASD)
- Bipolar Disorder
- Borderline Personality Disorder (BPD)
- Eating Disorders
- Mental Illness (General)
- Inaccessible
- Obsessive-Compulsive Disorder (OCD)
- Post-Traumatic Stress Disorder (PTSD)
- Schizophrenia
- Suicide Prevention
- Other Brain-Related Illnesses
- Basic Research
- New Technologies
- Early Intervention/ Diagnostic Tools
- Next Generation Therapies
- Donate Today
- Make a Memorial/Tribute Gift
- Create an Event/Memorial Page
- Find an Event/Memorial Page
- Make a Stock/Securities Gift/IRA Charitable Rollover Gift
- Donate Cryptocurrency
- Other Giving Opportunities
- Monthly Giving
- Planned Giving
- Research Partners
- Donor Advised Funds
- Workplace Giving
- Team Up for Research!
- Sponsorship Opportunities
Frequently Asked Questions About Addiction
Scientists say no single factor can predict whether a person might become addicted to drugs. But they think about half of the risk of addiction may come from a person’s biology and the other half from his or her environment. Some of the environmental factors that could make addiction more likely, especially among teens, include a lack of family involvement, the availability of drugs at school or in the home, or spending time with friends or family who use drugs. Smoking or injecting a drug also increases the risk of addiction, possibly because these methods have the quickest impact on the brain and body. The earlier a person begins using a drug, the more likely he or she is to become addicted. People with anxiety, depression or other mental health disorders such as attention-deficit hyperactivity disorder (ADHD) and post-traumatic stress disorder (PTSD) also have a higher risk of drug addiction.
More recently, researchers have identified specific genes that influence a person’s risk of addiction. For instance, Scientific Council member Wade Berrettini of the University of Pennsylvania led a research team in 2014 that uncovered rare variations of a gene that reduced the risk of heroin and cocaine addiction among some people.
It’s not uncommon for a person with a drug addiction to have another mental illness, but scientists say it’s difficult to know whether addiction is the cause of the mental illness, or whether people with mental illnesses turn to drug use to “self-medicate.” It’s also likely that some of the same genes and brain regions involved in addiction are also involved in other brain and behavior disorders, such as schizophrenia and depression.
Several studies show that in some cases marijuana can produce psychotic symptoms similar to those experienced by people with schizophrenia .
No. Although marijuana is not as addictive as alcohol or nicotine, nine percent of those who have tried marijuana at least once will become addicted to the drug. Researchers who analyzed 20 years’ worth of marijuana studies concluded that one in ten people worldwide who try the drug will become addicted. Marijuana was the illicit drug with the largest number of persons with past-year dependence or abuse in 2013, followed by pain relievers and cocaine. Of the almost seven million persons aged 12 or older who were classified with illicit drug dependence or abuse in 2013, more than four million had marijuana dependence or abuse (representing 1.6 percent of the total population aged 12 or older).
The past 15 years of imaging studies have shown that there are more types of brain circuitry involved in addiction than researchers previously thought. For instance, these studies have shown that drugs such as cocaine can impair parts of the brain involved in problem solving, reasoning, and planning. As a result, scientists have looked for ways to strengthen these circuits in people at risk for addiction—for instance, through behavioral methods aimed at improving executive function and decision-making. Imaging studies also show that some of the brain circuits involved in addiction are impaired in mental illnesses such as depression and schizophrenia. Saleem M. Nicola, Ph.D., of Albert Einstein College of Medicine, a NARSAD Young Investigator Grantee, and NARSAD Independent Investigator Alan I. Green, M.D., of Dartmouth Medical School are among the researchers using this information to explore whether medications used to treat these mental illnesses could aid the development of new treatments for addiction.
Opioids are a class of drugs most often used to reduce pain, by acting on opioid-sensitive receptors or chemical “docking ports” in the nervous system. These drugs can also produce a feeling of euphoria. Prescription opioids include medicines such as morphine, oxycodone (OxyContin), and hydrocodone (Vicodin), and the synthetic drug Fentanyl, which is most often prescribed for severe pain such as that experienced by terminal cancer patients. Heroin is an example of an illegal opioid drug.
The U.S Department of Health and Human Services estimates that in 2016, 11.5 million Americans misused prescription opioids and 948,000 Americans used heroin. There were 17,087 deaths resulting from prescription opioid misuse and 15,469 heroin overdose deaths in that same year.
The connection between prescription opioid and heroin addiction has changed over time, according to several studies. In the 1960s, more than 80 percent of patients who sought treatment for an opioid addiction began their drug use with heroin. Today, nearly 80 percent of heroin users say that their first opioid use was a prescription drug.
There are several possible reasons for the recent increase in prescription opioid abuse, according to National Institute of Drug Abuse Director and BBRF Scientific Council Member Nora D. Volkow, M.D. In her 2014 testimony before Congress, Dr. Volkow cited a drastic increase in opioid prescriptions filled; greater acceptability among the public for opioid medications being used for several purposes; and aggressive marketing of opioid drugs by pharmaceutical companies as reasons for crisis levels of opioid abuse. The number of prescriptions has increased from 76 million in 1991 to almost 207 million in 2013, she testified.
According to an annual survey of 8th, 10th and 12th –graders nationwide, pain medication misuse has dropped from 9.5 percent in 2004 to 4.2 percent in 2017. 35.8 percent of 12th-graders in 2017 said that the drugs were “easily available” to them, compared to more than 54 percent in 2010.
There is a growing consensus that opioid addiction should be treated with medications along with counseling, and that counseling alone may not be effective in preventing drug overdose and death. Medication treatment uses drugs, such as methadone, buprenorphine (Suboxone, Subutex), and naltrexone (Vivitrol). In essence these drugs substitute for the opioid and are prescribed to reduce opioid dependency and to prevent death by overdose. The length of the treatment course varies depending on how well a patient tolerates the medication, the type of substitute medication, and whether the patient relapses during treatment, but can run from 90 days to several years.
News and Events

Intergenerational Effects of Adversity on Mind-Body Health: Pathways Through the Gut-Brain Axis
Toward Brain-Based Prediction of Recovery: How Neuroimaging Can Help Combat the Substance-Use Epidemic.

New Diagnostic Tools to Predict Symptom Improvements in Personality Disorders

ADVICE ON MENTAL HEALTH: Warning Signs & What to Look For: Anxiety and Depression in Childhood

‘Brains Within Brains’: Organoid Experiments Show How Pathologies Emerge in the Developing Brain

A RESEARCHER’S PERSPECTIVE: What Can We Do When Medicine is Not Enough in the Treatment of Schizophrenia?
What We Are Learning About Brain Biology and Borderline Personality Disorder

How to Deal with Holiday Stress during Covid-19

How Brain Circuits Function in Health and Disease: Understanding Brain-wide Current Flow

An Update on Treatment of Bipolar Depression

How to Get a Good Night Sleep When Stressed

Using Neuroscience to Evaluate and Guide Treatment for Pediatric Mood Disorders
Donations are welcome
100% of every dollar donated for research is invested in our research grants. Our operating expenses are covered by separate foundation grants.
The Brain & Behavior Research Foundation is a 501(c)(3) nonprofit organization, our Tax ID # is 31-1020010.
The 10 Most Common Questions About Addiction

It is estimated that 1 in 10 individuals experience an alcohol or drug addiction at some point in their life. When other addictions such as gambling addiction, technology addiction, food addiction, or other common forms of addiction are taken into account the statistic of those suffering from an addiction increases substantially. Although someone you know likely experiences some form of an addiction, addictions continue to be stigmatized and are a seldom discussed topic among family and friends. Addiction all too often lacks basic understanding and education in our soceity, and common myths continue to circulate. Below are some of the most common questions and answers about addiction.
What is Addiction?
Addiction occurs when an individual continues to engage in a behavior with difficulty stopping or moderating. Addiction involves compulsive engagement in the behavior, such as drinking alcohol or gambling. The compulsive nature of an addiction surfaces as a result of rewarding stimulation in the brain, and a subsequent desire for the brain to crave that stimulation in order to induce pleasure. Addiction also often involves obsessive psychological preoccupation with getting, using, and recovering from the addictive substance or behavior.
A common cornerstone of addiction is continued engagement in the addictive behavior despite adverse consequences such as career problems, deterioration of relationships, legal issues, financial troubles, or health concerns, among many other negative impacts. Another common component of addiction involves tolerance, meaning that over time an individual requires more of the substance or behavior in order to produce the same desired pleasurable effects. Addiction also often involves withdrawal, meaning that when an individual is not engaged in their substance use or behavioral addiction they experience psychological or physiological withdrawal symptoms. Such symptoms vary from person to person as well as between various forms of addiction.
What is a Substance Use Disorder and What is the Difference Between an Addiction and a Dependence?
In the field of substance use and addiction there are many terms that are commonly used. For example, among addiction therapists and other addiction specialists the term regularly used to classify someone with an addiction to alcohol or drugs is “substance use disorder,” or more specifically may be “alcohol use disorder” if the addiction is to alcohol or “stimulant use disorder” if the addiction is to Adderall, etc. The term “substance use disorder” was updated from older terms such as “substance abuse” and “substance dependence.
The term used by addiction professionals for gambling addiction is “gambling disorder.” Other addictions, such as gaming addiction, cryptocurrency addiction, social media addiction and other addictions are not officially recognized as a disorder by the American Psychiatric Association and are currently left out of the Diagnostic Statistical Manual that is used by addiction professionals to render a clinical diagnosis. This is not to say that such behaviors are not problematic nor that individuals with such addictions are not deserving of treatment, but rather serves as a continued area of research among medical and addiction professionals.
Nonetheless, addictions are widespread and have a far-reaching impact beyond substance use disorder and gambling disorder. Two terms commonly used to discuss various problematic behaviors are addiction and dependence. The difference between addiction and dependence can be difficult to understand, and some may even use the words interchangeably. The term dependence is most notably used to refer to a physical dependence or physical reliance, most notably characterized by tolerance and withdrawal.
The term addiction is usually used to also include a psychological component, such as a mental obsession or preoccupation with a behavior. An individual can be physically dependent to a substance, such as opiates for example, but may not have breached the mental component of addiction. Such individuals are able to detox from their substance and not think about it thereafter once the substance is out of their body.
Why Do People Become Addicted?
There is not one reason why an individual becomes addicted, and anyone can become addicted to anything. However, two primary factors that may make someone vulnerable to become addicted are environmental factors and genetic factors. Environmental variables include a home environment in which there is trauma, abuse, or addictive behaviors occurring; a living environment in which drugs, alcohol or other addictions are readily available and taking place; friends, family members or other peer influences of individuals who are addicted or regularly engage in problematic behaviors; social acceptance of problematic behaviors; or a culture that generally accepts addiction. Genetic variables include a family history of mental health or addiction.
Aside from genetic and environmental risk factors, there are other variables that may make someone at higher risk of developing an addiction. Underlying mental health issues such as anxiety or depression certainly can make individuals at higher risk of developing an addiction. A history of physical, sexual, or emotional abuse or other trauma can also be a risk factor for addiction. Also, the earlier someone begins to engage in a problematic behavior the more likely they are to develop an addiction to that behavior.
What Is The Worst Addiction?
The term addiction is most commonly used in relation to substance dependence such as alcohol addiction, cocaine addiction, Adderall addiction, and other such drug addictions, but it is also used in regard to behavioral addictions such as gambling addiction, technology addiction, porn addiction, sex addiction, food addiction and other such addictions. Furthermore, there are subcategories of addictions, so for example types of gambling addiction may involve sports betting, poker, cryptocurrency addiction, or day trading addiction. A technology addiction may involve social media addiction, internet addiction, phone addiction or gaming addiction.
Addiction comes in many different forms, and there is no “worse” addiction. Yes, there are more deadly addictions. For example, an addiction to alcohol or heroin is more deadly and dangerous than an addiction to video games. However, all addictions can have a substantial negative impact on the individual suffering from the addiction, and impact them and their loved ones in a variety of ways from their mental health to physical health to spiritual health to financial health to relational health and every which way in-between. Instead of asking what type of addiction is the worst, one should be asking how the addiction is negatively impacting their life and the life of their loved ones.
Can You Get Addicted if You Do It Just Once?
This question is often posed for drug addiction. While just one use of a substance contributes to chemical changes in the brain, one does not become addicted or dependent after one use. However, after one use an individual may experience a sense of pleasure that they want to feel again, and the habitual nature of addiction can begin to take effect after continued use. Some individuals may also be at higher risk of addiction, for example, if they have an underlying mental health issue or if there is a history of addiction in their family.
This question is also often posed with the question, “Is marijuana addictive?” The answer is yes. Although marijuana is a natural substance, it does not mean that it is harmless nor does it mean that it is not addictive. Marijuana can change brain chemistry and take over the pleasure center of the brain in the same way as other drugs, and is especially dangerous for the development of the adolescent and young adult brain.
Another common question in this line of questioning is, “Are prescription drugs safe?” Before answering this question, it is important to always discuss your medication regiment with your prescribing doctor and to take medication safely as prescribed. That being said, prescription drugs can be highly addictive, especially Opioids such as Oxycodone or Oxycontin, Benzodiazepines such as Xanax, Klonopin or Ativan, and Amphetamines such as Adderall.
How Do You Know If Someone Is Addicted?
Addiction comes in many different severities, and can be classified as mild, moderate or severe. An individual may not fit into the box of having an alcohol use disorder or an addiction to alcohol, but they may be a binge drinker or problem drinker. In other words, they may on occasion be unable to control their alcohol use or their alcohol use may occasionally cause problems in their life. If alcohol, drugs, gambling, TikTok, gaming or other behaviors are causing a problem in your life or a loved one’s life then it should be enough to recognize that there is a problem that needs to be addressed.
If you answer yes to any of the below questions, your relationship with an addictive substance or addictive behavior is something you should take a closer look at.
- Have you had times when you ended up engaging in your behavior more, or longer, than you intended?
- Have you more than once wanted to cut down or stop your behavior, or tried to, but couldn’t?
- Have you spent a lot of time engaging in your behavior or spent time recovering from the aftereffects of your behavior?
- Have you wanted to engage in your behavior so badly you couldn’t think of anything else?
- Have you found that engaging in your behavior often interfered with taking care of your home or family? Or caused career troubles? Or Financial Problems?
- Have you continued to engage in your behavior even though it was causing trouble with your family or friends?
- Have you given up or cut back on activities that were important or interesting to you, or gave you pleasure, in order to engage in your behavior?
- Have you continued to engage in your behavior even though it was making you feel depressed or anxious or adding to another health problem?
- Have you had to engage in your behavior much more than you once did to get the effect you want? Have you increased the frequency, duration or quantity of use or engagement in the behavior?
- Have you found that when you stopped engaging in your behavior for hours or days you had withdrawal symptoms, such as trouble sleeping, shakiness, restlessness, irritability, agitation, depression, sweating, or other unwanted psychological or physiological symptoms?
Can Addiction Lead to Mental Health Disorders?
Yes. Addiction can lead to a variety of mental health concerns including depression and anxiety as well as other psychological problems. In some instances, such as with alcohol or drugs, mental health issues can be induced while under the influence of the substance or in other cases the mental health issues may continue to persist long-term.
Mental health issues can also serve as an underlying issue that existed prior to the addiction, and therefore can sometimes be a “chicken or the egg” scenario in which one is not certain if the mental health issue contributed to the addiction or if the addiction contributed to the mental health issue. In both cases it is important that the addiction and the mental health concerns are both addressed in treatment.
Is Addiction Treatable?
There is no cure for addiction, but addictions are treatable. In other words, an addiction can go into remission when an individual has abstained from their addictive behavior for some time, but there can be a recurrence. Individuals with a history of addiction will always be vulnerable to relapse, and unfortunately relapse rates for addictive disorders are quite high. Depending on the type of addiction, the severity of the addiction, and the history of the individual’s relationship with their addiction there are moderation management approaches, and many individuals are able to live a thriving life while moderating their addictive behavior. In other cases, and more widely accepted by the addiction recovery community and addiction specialists, are abstinence-based approaches to recovery involving complete abstinence from the addictive behavior.
Addictions are treated in various settings such as medical detox clinics, inpatient rehabilitation centers, and outpatient rehabilitation centers. Some individuals choose to work privately with an addiction therapist, addiction psychiatrist, or addiction recovery coach (sober coach). Common methods of treatment involve various behavioral therapeutic approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), Motivational Interviewing (MI), or Rational Emotive Behavior Therapy (REBT), among many other forms of therapy. Medication can also play an important role in recovery in curbing withdrawal symptoms, curbing cravings, and addressing underlying mental health concerns. There are also mutual help groups available such as Alcoholics Anonymous, SMART Recovery, Refuge Recovery, Gamblers Anonymous and many other twelve-step programs that are specific to the addiction.
What Do I Do If My Loved One Is Addicted?
Addictions are chronic, progressive and can be fatal, so it is always recommended that individuals encourage their loved ones to get help for their addiction if they are unable to stop on their own. If your loved one is in denial about their addiction or if they are unwilling to get help, then an intervention may be needed. There are different forms of intervention, but most commonly involve gathering loved ones to help encourage the addicted individual to seek out some form of help for their addiction. During the intervention process loved ones may be expected to express their love and concern for the individual and set boundaries that they are going to hold with the addicted individual should that individual choose not to get help. Lastly, it is also important for loved ones to seek out their own source of support regardless of if the addicted individual seeks out help or not. Such forms of help for loved ones can be with a family therapist who specializes in addiction, family therapy, or mutual help groups such as Al-Anon, Gam-Anon, or SMART Recovery Family & Friends.
To learn more about the impact of addiction on loved ones, please read “ The Impact of Alcoholism and Addiction on Family, and How to Protect Yourself .”
How Can I Support Someone with an Addiction?
It is not your job to get a person sober or to get them to stop destroying their life via their addictive behavior; your job is to take care of yourself. If your loved one is ready and willing to receive help or is in recovery, you can serve as a great source of strength and support. Some healthy behaviors you can implement are to actively listen, express empathy, set healthy boundaries, reduce environmental triggers, encourage healthy habits, role-model healthy behaviors, and educate yourself about addiction. For more information on supporting someone struggling with addiction, please read “ 10 Tips For How To Support Someone In Recovery From Addiction .”
For more information on New York City addiction treatment and to find the best addiction counselor in NYC, or for general therapy and mental health counseling, or to inquire about Family Addiction Specialist’s private concierge sober coach Manhattan, recovery coach Manhattan, sober companion Manhattan, Manhattan addiction therapy services and/or our Manhattan teletherapy services (online therapy/virtual therapy) for drug addiction, alcohol addiction, gambling addiction, or digital addiction and technology addiction, as well as our Manhattan hypnosis services in New York City please contact our undisclosed therapy office location in the Upper East Side of NYC today at (929) 220-2912.
You Might Also Enjoy...

Recognizing the Signs: Early Indicators of Addiction in College-Aged Children

Hidden Dangers of Alcohol Addiction in High-Functioning Individuals

The Rise of Cryptocurrency Addiction: Understanding the Phenomenon

Navigating the Challenges of High-Functioning Addiction: A Guide for Executives

A Guide To Supporting a Loved One Struggling with Day Trading Addiction

Understanding Marijuana Addiction: Risks, Symptoms, and Treatment Options

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Drugs, Brains, and Behavior: The Science of Addiction Treatment and Recovery
Can addiction be treated successfully.
Yes, addiction is a treatable disorder. Research on the science of addiction and the treatment of substance use disorders has led to the development of research-based methods that help people to stop using drugs and resume productive lives, also known as being in recovery.
Can addiction be cured?
Like treatment for other chronic diseases such as heart disease or asthma, addiction treatment is not a cure, but a way of managing the condition. Treatment enables people to counteract addiction's disruptive effects on their brain and behavior and regain control of their lives.
Does relapse to drug use mean treatment has failed?
No. The chronic nature of addiction means that for some people relapse, or a return to drug use after an attempt to stop, can be part of the process, but newer treatments are designed to help with relapse prevention. Relapse rates for drug use are similar to rates for other chronic medical illnesses. If people stop following their medical treatment plan, they are likely to relapse.
Treatment of chronic diseases involves changing deeply rooted behaviors, and relapse doesn’t mean treatment has failed. When a person recovering from an addiction relapses, it indicates that the person needs to speak with their doctor to resume treatment, modify it, or try another treatment. 52
While relapse is a normal part of recovery, for some drugs, it can be very dangerous—even deadly. If a person uses as much of the drug as they did before quitting, they can easily overdose because their bodies are no longer adapted to their previous level of drug exposure. An overdose happens when the person uses enough of a drug to produce uncomfortable feelings, life-threatening symptoms, or death.
What are the principles of effective treatment?
Research shows that when treating addictions to opioids (prescription pain relievers or drugs like heroin or fentanyl), medication should be the first line of treatment, usually combined with some form of behavioral therapy or counseling. Medications are also available to help treat addiction to alcohol and nicotine.
Additionally, medications are used to help people detoxify from drugs, although detoxification is not the same as treatment and is not sufficient to help a person recover. Detoxification alone without subsequent treatment generally leads to resumption of drug use.
For people with addictions to drugs like stimulants or cannabis, no medications are currently available to assist in treatment, so treatment consists of behavioral therapies. Treatment should be tailored to address each patient's drug use patterns and drug-related medical, mental, and social problems.
What medications and devices help treat drug addiction?
Different types of medications may be useful at different stages of treatment to help a patient stop abusing drugs, stay in treatment, and avoid relapse.
- Treating withdrawal. When patients first stop using drugs, they can experience various physical and emotional symptoms, including restlessness or sleeplessness, as well as depression, anxiety, and other mental health conditions. Certain treatment medications and devices reduce these symptoms, which makes it easier to stop the drug use.
- Staying in treatment. Some treatment medications and mobile applications are used to help the brain adapt gradually to the absence of the drug. These treatments act slowly to help prevent drug cravings and have a calming effect on body systems. They can help patients focus on counseling and other psychotherapies related to their drug treatment.
- Preventing relapse. Science has taught us that stress cues linked to the drug use (such as people, places, things, and moods), and contact with drugs are the most common triggers for relapse. Scientists have been developing therapies to interfere with these triggers to help patients stay in recovery.
Common medications used to treat drug addiction and withdrawal
- Buprenorphine
- Extended-release naltrexone
- Nicotine replacement therapies (available as a patch, inhaler, or gum)
- Varenicline
- Acamprosate
How do behavioral therapies treat drug addiction?
Behavioral therapies help people in drug addiction treatment modify their attitudes and behaviors related to drug use. As a result, patients are able to handle stressful situations and various triggers that might cause another relapse. Behavioral therapies can also enhance the effectiveness of medications and help people remain in treatment longer.
- Cognitive-behavioral therapy seeks to help patients recognize, avoid, and cope with the situations in which they're most likely to use drugs.
- Contingency management uses positive reinforcement such as providing rewards or privileges for remaining drugfree, for attending and participating in counseling sessions, or for taking treatment medications as prescribed.
- Motivational enhancement therapy uses strategies to make the most of people's readiness to change their behavior and enter treatment.
- Family therapy helps people (especially young people) with drug use problems, as well as their families, address influences on drug use patterns and improve overall family functioning.
- Twelve-step facilitation (TSF) is an individual therapy typically delivered in 12 weekly session to prepare people to become engaged in 12-step mutual support programs. 12-step programs, like Alcoholic Anonymous, are not medical treatments, but provide social and complementary support to those treatments. TSF follows the 12-step themes of acceptance, surrender, and active involvement in recovery.
How do the best treatment programs help patients recover from addiction?

Stopping drug use is just one part of a long and complex recovery process. When people enter treatment, addiction has often caused serious consequences in their lives, possibly disrupting their health and how they function in their family lives, at work, and in the community.
Because addiction can affect so many aspects of a person's life, treatment should address the needs of the whole person to be successful. Counselors may select from a menu of services that meet the specific medical, mental, social, occupational, family, and legal needs of their patients to help in their recovery.
For more information on drug treatment , see Principles of Drug Addiction Treatment: A Research-Based Guide , and Principles of Adolescent Substance Use Disorder Treatment: A Research-Based Guide .

IMAGES
VIDEO
COMMENTS
Research Topics | National Institute on Drug Abuse (NIDA)
Drugs, Brains, and Behavior: The Science of Addiction
Answers the questions people have about addiction and addictive behaviors of all kinds, including drugs, alcohol, gambling, sex, Internet usage, and more. Addiction surveys both the science of addiction and its history in the United States.
Addiction as a brain disease revised: why it still matters, ...
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
This Special Collection on Addiction focuses on scientific advances in the treatment and recovery mechanisms of addiction related to four widely misused substances: alcohol, nicotine, cocaine, and opioids. Although the opioid crisis has taken center stage across public policy and scientific forums, all of these substances continue to have a profound global impact on health and well-being and ...
Early exposure to drugs of abuse may further impair the development of the prefrontal cortex, ... There is a scarcity of research on the effects of adverse social environments on adult brain function. 60 ... Gianoulakis C Endogenous opioids and addiction to alcohol and other drugs of abuse. Current topics in medicinal chemistry 2004; 4 (1): 39 ...
Addiction Science | National Institute on Drug Abuse (NIDA)
The characterisation of the role of glia and the extracellular matrix (ECM) in drug-induced synaptic plasticity is an exciting emerging field of drug addiction research as it comes with promising ...
Observational designs may provide the best evidence to evaluate interventions to address chronic conditions such as substance use and addiction. Unfortunately, assuming epistemic superiority of RCTs has unnecessarily slowed the uptake of substance use research and harm reduction services for people who use drugs.
Addiction - Latest research and news
Neuroscience of Addiction: Relevance to Prevention and ...
Drug abuse and Medicine. The obvious topic for a medical research paper. The impact of drugs on the human body, the changes in its physiology and the nature of addiction are well studied also, but, unfortunately, the drugs evolve along with the science, so the new synthetic drugs that are sometimes considered harmless "energy club pills" emerge almost every year.
Understanding Drug Use and Addiction DrugFacts. | En español. | Provides an overview of drug use and addiction, including what happens in the brain during drug use, why some people become addicted while others don't, and the importance of prevention. DrugFacts.
Substance use, abuse, and addiction
These research queries and findings are presented in the form of updates, white papers and case studies. In addition, the Butler Center for Research collaborates with the Recovery Advocacy team to study special-focus addiction research topics, summarized in monthly Emerging Drug Trends reports. Altogether, these studies provide the latest in ...
Eight Questions for Drug Policy Research
Drug Misuse and Addiction
The connection between prescription opioid and heroin addiction has changed over time, according to several studies. In the 1960s, more than 80 percent of patients who sought treatment for an opioid addiction began their drug use with heroin. Today, nearly 80 percent of heroin users say that their first opioid use was a prescription drug.
The 10 Most Common Questions About Addiction
Understanding Drug Use and Addiction DrugFacts
The Science of Addiction Treatment and Recovery