- Search Menu
- Sign in through your institution
- Advance Articles
- Special Issues
- Supplements
- Virtual Collection
- Online Only Articles
- International Spotlight
- Free Editor's Choice
- Free Feature Articles
- Author Guidelines
- Submission Site
- Calls for Papers
- Why Submit to the GSA Portfolio?
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Journals Career Network
- About The Gerontologist
- About The Gerontological Society of America
- Editorial Board
- Self-Archiving Policy
- Dispatch Dates
- GSA Journals
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Intervention outcomes, types of interventions, moderators of caregiver intervention effectiveness.
- < Previous
How Effective Are Interventions With Caregivers? An Updated Meta-Analysis
- Article contents
- Figures & tables
- Supplementary Data
Silvia Sörensen, Martin Pinquart, Paul Duberstein, How Effective Are Interventions With Caregivers? An Updated Meta-Analysis, The Gerontologist , Volume 42, Issue 3, 1 June 2002, Pages 356–372, https://doi.org/10.1093/geront/42.3.356
- Permissions Icon Permissions
Purpose : The purpose of this study was to determine the effectiveness of interventions for family caregivers of older adults. Design and Methods: Meta-analysis was used to synthesize the effects of 78 caregiver intervention studies for six outcome variables and six types of interventions. Results: The combined interventions produced a significant improvement of 0.14 to 0.41 standard deviation units, on average, for caregiver burden, depression, subjective well-being, perceived caregiver satisfaction, ability/knowledge, and care receiver symptoms. Intervention effects were larger for increasing caregivers' ability/knowledge than for caregiver burden and depression. Psychoeducational and psychotherapeutic interventions showed the most consistent short-term effects on all outcome measures. Intervention effects for dementia caregivers were smaller than those for other groups. The number of sessions, the setting, care receiver age, caregiver age, gender, type of caregiver–care receiver relationship (spouse vs adult child), initial burden, and study characteristics moderated the observed effects. Implications: Caregiver interventions are effective, but some interventions have primarily domain-specific effects rather than global effects. The differences between intervention types and moderators suggest ways of optimizing interventions.
Decision Editor: Laurence G. Branch, PhD
Family caregivers of elderly persons with physical ailments and/or dementing illnesses often experience high levels of stress (Vitaliano, Russo, Young, Becker, and Maiuro 1991 ), which can lead to a lowered sense of well-being (Rose-Rego, Strauss, and Smyth 1998 ), feelings of being burdened (Dunkin and Anderson-Hanley 1998 ), depression (Bodnar and Kiecolt-Glaser 1994 ; Rose-Rego et al. 1998 ), compromised physical health (Loomis and Booth 1995 ; Rose-Rego et al. 1998 ), and even premature mortality (Schulz and Beach 1999 ). Although some caregivers derive benefits from caregiving (Kramer 1997 ), many are nonetheless in need of psychosocial and instrumental support. In this article, we report the findings of a meta-analysis examining the effects that psychoeducational, supportive, respite-based, psychotherapy, care receiver-focused, and multicomponent interventions have on caregivers.
Early studies of the effects of interventions relied on the clinical impressions of group leaders or satisfaction surveys of small, select samples of caregivers (see Toseland and Rossiter 1989 , for review). These interventions were, not surprisingly, judged to be effective. However, more recent studies using standard measures of change in emotional distress were less conclusive (for reviews, see Bourgeois, Schultz, & Burgio, 1996; Callahan 1989 ; Cooke, McNally, Mulligan, Harrison, and Newman 2001 ; Kennet, Burgio, and Schulz 2000 ; Pusey and Richards 2001 ).
In response to Callahan 1989 provocative suggestion that many interventions fail to produce desirable effects and the ensuing flurry of studies in the early 1990s, Knight, Lutzky, and Macofsky-Urban 1993 published a meta-analysis of studies on the effectiveness of caregiver intervention programs, focusing on caregiver distress. They observed that interventions had small to moderate effects but that results of individual studies were often inconsistent with each other, and many showed minimal or no effects. Callahan's critique of caregiver interventions was thus diminished but not invalidated.
In explaining the inconsistencies in intervention effectiveness, Knight and colleagues 1993 (see also George and Gwyther 1986 ; Zarit 1994 ) discussed three major limitations of the existing research. The first is the failure to examine multiple outcome variables. Some outcome measures may be more sensitive to change than others (George and Gwyther 1986 ). For example, measures of caregiver burden are often less modifiable than measures of well-being. Examining the effect of an intervention only on burden may underestimate its effectiveness.
The second major issue is the lack of attention to differences between types of interventions. Because interventions vary in their style of administration and content, some outcomes may be more responsive to certain types of interventions. For example, assuming that specific types of interventions yield specific effects, one might expect psychoeducational interventions to have a stronger effect on knowledge about the care receiver's condition or knowledge about effective ways to cope with stress, but not necessarily on burden. However, if it is assumed that the effects of interventions are nonspecific, then the effect of psychoeducational interventions on knowledge and burden may be roughly equivalent.
The third issue involves the need to identify moderators of intervention effectiveness, including the influence of (a) the intensity of interventions (individual or group, number of sessions), (b) the extent to which participants adhere to the intervention (regularity of attendance and dropout), (c) the type of relationship between caregiver and care recipient (spouses, adult children), (d) random assignment, and (e) reliability and validity of the outcome measures.
Since the publication of Knight and associates 1993 meta-analysis, the findings of new intervention studies have been reported. Many have used methodologically sophisticated designs and provided more complete descriptions of subjects, procedures, and outcomes than have earlier studies. The purpose of the present study was, therefore, to present an updated and expanded meta-analysis in which we estimate the effectiveness of interventions for caregivers and examine potential moderators.
The difference between efficacy and effectiveness has been highlighted in clinical and epidemiological research (Fletcher, Fletcher, and Wagner 1996 ). Efficacy refers to whether treatment has the desired effect under ideal conditions of implementation. In efficacy studies, participants are restricted to those who will adhere completely to the treatment as presented. In contrast, effectiveness is established by offering a program and allowing participants to accept or reject it as they would in a real-world implementation. Thus, it focuses more on generalizability than on internal validity. Because in meta-analysis treatment conditions cannot be controlled retrospectively and because most of the studies in this area have examined effectiveness, not efficacy, the results of this study bear on the effectiveness of interventions with caregivers.
Intervention studies have used a number of different outcome measures. Knight and colleagues 1993 distinguished two major categories: caregiver burden and dysphoria. However, there are a number of other outcome criteria that have not been investigated in a meta-analytic study. The availability of a large number of studies with diverse outcomes enables us to examine several effects of caregiver interventions in addition to those on depression and burden. These effects are subjective well-being, uplifts of caregiving, ability/knowledge, and symptoms of care receivers. We also test whether effect sizes are dependent on the measurement used for these outcomes.
Caregiver interventions can be divided into two major groups: (a) those aimed at reducing the objective amount of care provided by caregivers (respite, interventions to enhance the competence of the care receiver) and (b) those aimed at improving the caregiver's well-being and coping skills (e.g., psychoeducational interventions, support groups). Knight and associates 1993 suggested that a one-size-fits-all approach to assisting caregivers may not be useful because caregivers have vastly different needs. The data we have compiled allow us to conduct separate analyses to examine the effectiveness of six distinct types of caregiver intervention: pychoeducational interventions, supportive interventions, respite/adult day care, psychotherapy, interventions to improve care receiver competence, and multicomponent interventions. Classification into these types was based on the dominant approach used, as described in the original empirical article. When several approaches appeared to have equal weight, the intervention was classified as multicomponent.
Psychoeducational Interventions (38 Studies)
Psychoeducational interventions involve a structured program geared toward providing information about the care receiver's disease process and about resources and services and training caregivers to respond effectively to disease-related problems, such as memory and behavior problems in dementia patients or depression and anger in cancer patients(e.g., Chiverton and Caine 1989 ; Schultz, Smyrnios, Schultz, and Grbich 1994 ; Ostwald, Hepburn, Caron, Burns, and Mantell 1999 ). Intervention formats usually include lectures, group discussions, and written materials and are always led by a trained leader. Support may be part of a psychoeducational group, but it is secondary to the educational content.
Supportive Interventions (7 Studies)
This category subsumes both professionally led and peer-led unstructured support groups focused on building rapport among participants and creating a space in which to discuss problems, successes, and feelings regarding caregiving (e.g., Gonyea & Silverstein, 1991; Scharlach 1987 [Condition B]; Toseland, Rossiter, and Labrecque 1989 [self-help group]). Rather than using the principles of group therapy to explore deeper psychological conflicts or confront participants with problematic behaviors, support groups help the participants recognize that others have similar problems, and they provide an opportunity for participants to exchange ideas and strategies for coping with their shared difficulties. Support groups rely strongly on group members to provide mutual emotional support and to share concrete information on the nature of the care receiver's needs, how to manage problem behaviors, and where to obtain services. In contrast to psychoeducational programs, these interventions are rarely standardized or manualized, education is not their primary focus, and publications rarely provide much detail on the exact content or procedure (e.g., Gonyea and Silverstein 1991 ). Of the seven supportive interventions, one was peer led (Toseland et al., 1989 [self-help group only]) and the rest had professional leaders.
Respite/Adult Day Care (13 Studies)
Respite care is either in-home or site-specific supervision, assistance with activities of daily living, or skilled nursing care designed to give the caregiver time off. It does not imply that activities or programs are offered to the care recipient (e.g., Burdz, Easton, and Bond 1988 ). Adult day care programs provide a combination of respite and activity programs. The interventions often engage the care receiver away from home and offer stimulating programs tailored toward the patient population's specific needs (e.g., Guttman 1991 ; Zarit, Stephens, Townsend, and Greene 1998 ).
Psychotherapy (10 Studies)
This type of intervention involves a therapeutic relationship between the caregiver and a trained professional. Most psychotherapeutic interventions with caregivers follow a cognitive–behavioral approach ( N = 9), where therapists may teach self-monitoring, challenge negative thoughts and assumptions that maintain the caregiver's problematic behavior; help caregivers develop problem-solving abilities by focusing on time management, overload, and emotional reactivity management; and help the caregiver reengage in pleasant activities and positive experiences (e.g., Goldberg and Wool 1985 ; Lovett and Gallagher 1988 ).
Interventions to Improve Care Receiver Competence (6 Studies)
These interventions include memory clinics for patients with dementia and activity therapy programs designed to improve affect and everyday competence (LoGiudice et al. 1999 ; Zarit, Zarit, and Reever 1982 ). We included studies that report caregiver outcomes, even if they were otherwise focused on the patient.
Multicomponent Interventions (12 Studies)
Interventions in this group included various combinations of educational interventions, support, psychotherapy, and respite (e.g., Montgomery and Borgatta 1989 ).
Miscellaneous
Three studies could not be coded into one of the above categories because, although they offered more than one intervention component, there was evidence that some participants did not use or were not exposed to more than one component (e.g., Newcomer, Yordi, DuNah, Fox, and Wilkinson 1999 ; Weuve, Boult, and Morishita 2000 ).
Three groups of moderators of the effectiveness of caregiver interventions are analyzed here: (a) characteristics of the intervention, (b) characteristics of the caregiving situation, and (c) characteristics of the study. The moderators and their coding are described in Table 1 .
First, characteristics of the intervention—for example, whether the intervention is conducted with individuals or in a group setting—and also how many sessions the treatment involves may have an impact on its effectiveness (Toseland, Rossiter, Peak, and Smith 1990 ; Whitlatch, Zarit, and von Eye 1991 ; Zarit, Anthony, and Boutselis 1987 ). Treatment effectiveness may also be inflated or mitigated by participant dropout from the intervention group or from the waiting list.
Second, the nature of the caregiving situation and the caregiver population are important considerations. For example, caregivers for dementia patients have higher stress levels than other caregivers (Clipp and George 1993 ; Coen, Swanwick, O'Boyle, and Coakley 1997 ), suggesting that responses to interventions may also differ. Spouse caregivers have been shown to suffer more from providing care than adult children (Barber and Pasley 1994 ; Tennstedt, McKinlay, and Sullivan 1988 ), thus suggesting that they may differ in their needs and in how they benefit from interventions.
Third, characteristics of the study, including the design, may also moderate the findings of intervention studies. For example, nonrandom assignment of participants to intervention and nonintervention groups may lead the more distressed caregivers to self-select into the intervention groups. This may undermine attempts to unequivocally document the intervention's effectiveness. Another study characteristic that may moderate findings is when the study was published: Investigators who have implemented studies more recently have had access to more information about the validity of measures and potential pitfalls in caregiver intervention.
In sum, in this article we report the effectiveness of caregiver interventions in three major steps: (a) the averaged effect of all types of interventions on six outcome measures (caregiver burden, depression, subjective well-being, uplifts, ability/knowledge, and care receiver symptoms), (b) the effects of six types of interventions (psychoeducation, supportive interventions, psychotherapy respite/daycare, care receiver training, and multicomponent), and (c) the extent to which intervention effects are moderated by characteristics of the intervention, of the caregiving situation, and of the study. The coding of the variables is displayed in Table 1 .
Literature Search
A comprehensive sample of the available studies that investigate the effects of interventions with caregivers to older adults on caregiver outcomes was identified from the geriatric, gerontological, and clinical literature by searching electronic databases (Psycinfo, Medline, Psyndex; search terms: caregiver or carer or caregiving , intervention or support or training , and elderly or old age ) and using the ancestry method. In addition, suggestions from reviewers were included. Criteria for inclusion of the studies in the meta-analysis were the following:
The care recipients had a mean or median age of ≥60 years.
An intervention condition was compared with an untreated control condition. Comparisons of several treatments (e.g., Steffen, Futterman, and Gallagher-Thompson 1998 ) were not included because (a) the goal of the meta-analysis was to test whether greater improvements were found in caregivers who received treatment compared with caregivers who received no specific intervention; (b) if two interventions were compared, there would be no theoretical reason to label one as the experimental condition and the other as the control condition; and (c) comparing change in an intervention condition to change in a control condition that is also an intervention underestimates intervention effects when both interventions show some desired effects.
At least one of the following outcomes was reported: caregiver burden, depression, other measures of psychological well-being (e.g., life satisfaction, morale, self-esteem, happiness), uplifts of caregiving, caregivers' knowledge and/or coping abilities, and care receivers' symptoms.
Statistics could be converted into effect sizes (means, F or t values, correlations).
Studies were written in German, English, French, or Russian.
Studies were published in peer-reviewed journals.
The 78 eligible studies are listed in the References and marked with an asterisk. Fifteen additional studies had to be excluded because they provided insufficient information to calculate effect sizes, 32 were excluded because they did not include a no-treatment control group or did not provide comparative data on the no-treatment group, and 14 were excluded because they were not published in peer-reviewed journals (see Appendix>, Note 1). Most studies were in English (76); two German studies were included as well. The majority of articles were from The Gerontologist (12), the Journal of the American Geriatrics Society (6), Psychology and Aging (4), the Journal of Gerontology (3), International Journal of Geriatric Psychiatry (3), and Nursing Research (3). The studies were coded by two doctoral-level raters who had specialized training in gerontology. In addition, one rater had special training in behavior therapy and practical experience leading caregiver support and psychoeducational groups. The average observed agreement between the raters (Cohen's κ) was .91. Inconsistencies between the raters were resolved by discussion.
Outcome Measures
We used six main outcome variables. Of the 78 studies, 57 reported effects for caregiver burden; 40, for depression; 23, for other self-rated measures of subjective well-being; 3, for uplifts of caregiving; 33, for knowledge and coping abilities; and 31, care receiver symptoms as well as caregiver outcomes.
Caregiver burden was assessed using the Zarit Burden Scale (Zarit, Reever, & Bach-Peterson, 1980; 21 studies), Montgomery and Borgatta's Burden Scale (1989; 8 studies) and other scales (29 studies).
Self-rated depression was most often measured with the Centers for Epidemiologic Studies–Depression Scale (Radloff 1977 ; 8 studies), the Beck Depression Inventory (Beck and Steer 1987 ;8 studies), the Depression Subscale of the Brief Symptom Inventory (Derogatis and Melisaratos 1983 ; 7 studies), the Geriatric Depression Scale (Yesavage et al. 1983 ; 5 studies), and other measures (13 studies).
Subjective well-being was assessed with a broad variety of measures, including the Affect Balance Scale (Bradburn 1969 ; 6 studies), Life Satisfaction Scales (e.g., Neugarten, Havighurst, and Tobin 1961 ; 4 studies), the Philadelphia Geriatric Center Morale Scale (Lawton 1975 ; 4 studies), the Positive and Negative Affect Scale (Watson, Clark, and Tellegen 1988 ; 3 studies), the Profile of Mood States (McNair, Lorr, and Droppleman 1971 ; 2 studies), and other scales (8 studies).
Uplifts were measured as sources of satisfaction from caregiving or satisfaction with caregiving (three studies).
Ability and knowledge dealt with the necessary tools to cope competently with the caregiver role. It was most often assessed by questionnaires on knowledge about the care receiver's illness and available services (16 studies), coping abilities (10 studies), and self-efficacy specifically in dealing with caregiving tasks (11 studies). (Self-efficacy was included here rather than under well-being because it was specific to care-related abilities.)
Care receiver outcomes were assessed by the Memory and Behavior Problem Checklist (Teri et al. 1992 ; 17 studies), deficits in functional abilities (activities of daily living [ADL], instrumental ADL [IADL]; e.g., RPI Home Care Classification Project 1986 ; 8 studies), and others (9 studies).
Statistical Integration of Research Findings
We performed calculations for the meta-analysis in five steps mainly by using procedures outlined by Hedges and Olkin 1985 .
Effect sizes were computed for each study as the difference in the posttreatment measure between the experimental and control groups divided by the pooled standard deviation (Glass, McGaw, and Smith 1981 ; Hedges 1981 ). Effect sizes were also derived from t values, F values, exact p values, and alpha levels. The effect size estimates were adjusted for bias due to differences in pretests between the experimental and control groups on the basis of Mullen 1989 and for bias owing to overestimation of the population effect size (common for small samples), based on Hedges 1981 . Confidence intervals that include 95% of the effects were computed for each effect size.
Weighted mean effect sizes were computed.
The significance of the mean effect size was tested by dividing the mean effect size by the estimation of the standard deviation. Differences between two conditions were interpreted as significant when the 95% intervals did not overlap (Hedges and Olkin 1985 ).
The homogeneity of effect sizes was computed by use of the homogeneity statistic Q , which is distributed approximately as chi-square with k − 1 degrees of freedom, where k is the number of effect sizes.
To test the influence of moderator variables simultaneously, weighted multiple linear regression analyses were used, following the approach outlined by Hedges 1994 . The significance test from the weighted regressions was corrected because the standard errors for the regression coefficients are incorrect by a factor of the square root of the residual mean square. The effects of potential moderator variables were estimated in a multivariate analysis only if data on the moderator variable were available for 80% of the studies; otherwise, univariate weighted linear regression analyses were computed.
Descriptive Characteristics of the Studies
For intervention characteristics, the number of sessions ranged from 1 to 180 with a median of 8 sessions. Follow-ups were conducted in 22% of cases after an average of 7 months ( SD = 5.1 months). Group treatments were examined in 59% of the studies; 22% used individual treatments, 18% combined group and individual treatments, and 1% gave no information whether group or individual treatments were used. The average dropout rate across all studies was 19.6%. Dropout was highest for day care/respite interventions (35.9%) and for training of the care receiver (33.3%) and lowest for psychotherapy (11.7%). Dropout for psychoeducational interventions was 16.1%, 12.5% for supportive interventions, and 25.8% for multicomponent interventions.
The number of participants in the experimental (intervention) condition ranged from 4 to 2,268 ( M = 24). Mean age of the caregivers was 62.3 years ( SD = 3.7). The percentage of female caregivers varied between 40% and 100%, with a mean of 69%. Most of the caregivers (77%) coresided with the care receiver, 40% were adult children, 50% were spouses; the remaining 9% were siblings, nieces, nephews, grandchildren, and friends; 79% of the respondents were married, and 39% were employed. The median income of the caregivers was $17,000. Only 14% reported their ethnicity as non-White; 78% had more than 12 years of education (high school). The caregivers had been providing care for an average of 4.0 years, and they provided 30 hours/week of care. For care receivers, the mean age was 77.3 years ( SD = 2.9); 64% were female. More than half (61%) of the studies focused only on care for dementia patients; most of the other studies were conducted with heterogeneous samples, including seniors with physical disabilities or mental illness, stroke patients, and cancer patients. Many of the heterogeneous samples also included dementia patients, but not exclusively. Twenty-one were published before 1990. Sixty of the studies were conducted in North America, 11 in Europe, and 7 in Australia.
Effectiveness of Intervention on Different Outcomes
As shown in Table 2 , all caregiver interventions taken together produced a significant improvement of between 0.14 and 0.41 standard deviation units in the level of caregiver burden, depressive mood, subjective well-being, perceived caregiving satisfaction, ability/knowledge, and care receiver symptoms. The effects for the immediate pre–post tests on burden, depression, subjective well-being, ability/knowledge, and symptoms of the care receiver were significant ( p < .01), whereas the effect on uplifts of caregiving was only significant at the p < .10 level. Immediate posttest effects were significantly larger for ability/knowledge than for caregiver burden, depression, uplifts of caregiving, and symptoms of the care receiver. In addition, effects on subjective well-being were stronger than effects on burden and depression. For the follow-up, only the effects on caregiver burden, depression, subjective well-being, and ability/knowledge were significant. Follow-up effects for ability/knowledge were larger than for burden and depression; no other significant differences in magnitude of effects were found.
Effectiveness of Different Forms of Intervention
We computed average effects for the different types of interventions for each class of outcome variable. As shown in Table 3 , psychoeducational interventions and psychotherapy had a significant effect on all outcome variables. Multicomponent interventions had significant effects on caregiver burden, well-being, and ability/knowledge but not on depression and care receiver symptoms. Respite/daycare interventions were also effective for three outcomes: caregiver burden, caregiver depression, and caregiver well-being. In addition, supportive interventions reduced caregiver burden and increased ability/knowledge but had no effect on the other outcome variables. Furthermore, training care recipients was effective in increasing caregivers' subjective well-being and reducing care receivers' symptoms, but the effects on caregiver burden, depression, and ability/knowledge were not statistically significant. Miscellaneous interventions showed no significant effects on any outcome.
Next we calculated whether the effect sizes varied across treatments, within each outcome, by looking at the overlap of the 95% intervals. These comparisons should be interpreted with caution, given the nonrandom selection of treatment modalities. Few differences within outcomes were observed. For caregiver burden, the effect of multicomponent interventions was significantly larger than those of psychoeducation, respite/daycare, training of the care receiver, and miscellaneous interventions ( Table 3 ). In addition, the effect of miscellaneous interventions on caregiver burden was significantly smaller than those of other interventions, except psychoeducation. Similarly, the effect of miscellaneous interventions on depression was smaller than the effects of other interventions. Multicomponent interventions had larger effects on subjective well-being than on respite/daycare.There were no other significant differences between intervention types for depression, subjective well-being, ability/knowledge, and care receiver symptoms.
Influences of Moderator Variables
To answer our third research question, we tested for moderator variables. We conducted a weighted multiple regression analysis ( Table 4 ) with the moderator variables as predictors and the mean effect size ( g ) on five of the outcomes as dependent variables (see Appendix>, Note 2).
For several of the moderators, information was missing for more than 20% of the studies. For these studies, we calculated univariate weighted linear regression models ( Table 5 ). For organizational purposes, we report the results by topic, alternately referring to Table 4 and Table 5 .
Intervention Characteristics
As shown in Table 4 , intervention characteristics were strongly related to the effect sizes found. Interventions conducted in a group setting yielded smaller effects for improvement in caregiver burden and well-being than did individual or mixed interventions. However, with regard to the reduction of care receiver symptoms, group interventions had larger effects. That is, group interventions were less effective at improving burden and well-being but more effective at reducing care receiver symptoms than were nongroup interventions.
Because interventions in groups were compared against a combination of individual and group interventions, the preceding analysis does not allow a direct comparison of group and individual interventions. Thus, we created an additional "setting" variable (1 = interventions in an individual setting, 0 = others) that allowed us to compare the effectiveness of individual versus group or combined interventions in another multiple regression. For the individual interventions, improvements of caregiver burden ( B = .13, β = .15, p < .001), depression ( B = .08, β = .07, p < .001), and well-being ( B = .32, β = .28, p < .001) were greater than for nonindividual interventions. Effect sizes for individual interventions did not differ from other interventions with regard to ability/knowledge and symptoms of the care receiver. Because participants were not randomly assigned to an individual treatment or a group treatment, these results should be treated with caution.
To ascertain that the moderator effect for individual versus group intervention was not merely due to selection effects related to differences in the initial levels of objective burden (number of hours and years they provided care) and subjective burden (mean level of Zarit Caregiver Burden Inventory [ZCBI]), we compared the two groups with regard to these variables. No significant differences were found between caregivers who received individual treatments and those who received group treatments for number of caregiving hours( M ind = 46.58, SD = 42.40, N = 216, vs M group = 50.67, SD = 14.88, N = 168) and the levels of ZCBI at pretest ( M ind = 46.93, SD = 3.80, N = 73, vs M group = 43.94, SD = 6.88, N = 320).
To analyze for the moderating effect of the length of interventions, we first z -standardized the number of sessions within each type of intervention. This transformation was performed because the number of sessions varied systematically between the interventions, so that this variable would have been confounded with the effects of the type of intervention. The longer the intervention, the larger the effects for improving caregiver depression, but the smaller the effects for improving caregivers' ability/knowledge ( Table 4 ).
As shown in Table 5 , for intervention programs with higher dropout rates, caregiver burden, depression, and care receiver symptoms were reduced more effectively, but ability/knowledge increased less in response to the intervention than for programs with lower dropout rates.
Characteristics of the Caregiving Situation
Using a regression model, we compared studies in which all care receivers were suffering from dementia to those in which only a subset were dementia patients or in which there were no dementia patients. Table 4 shows that interventions were less effective at improving caregiver burden, depression, subjective well-being, and ability/knowledge when all care receivers had dementia than when care receivers did not have dementia or when the sample was mixed. Surprisingly, there was no association of patient diagnosis with the effect sizes for changes in care receiver symptoms. Note that because only seven studies specifically excluded caregivers of elders with dementia, we were not able to test whether interventions with these groups had a stronger effect than those that exclusively focused on dementia caregivers or on mixed groups of caregivers. In contrast to care receivers' diagnoses, their age was positively associated with intervention effectiveness for improvement of burden, depression, and subjective well-being ( Table 5 ).
Caregiver characteristics were less consistently associated with intervention effectiveness. The effects of interventions varied with the percentage of adult child versus spouse caregivers: The larger the proportion of adult children participating in the intervention, the greater were the improvements for burden, depression, subjective well-being, and ability/knowledge, but the smaller the improvements of care receiver symptoms. Similarly, smaller improvements for burden, depression, subjective well-being, and ability/knowledge, but greater improvements for care receiver symptoms, were found in studies with a higher percentage of spousal caregivers. Also, interventions with older caregivers yielded larger improvements of burden, subjective well-being, ability/knowledge, and care receiver symptoms than those with younger caregivers; no effects were found for depression ( Table 4 ). As shown in Table 4 , for studies with a higher percentage of female caregivers, the reduction in burden, the increase of ability/knowledge, and the improvement of care receiver symptoms was more pronounced than for studies with a higher proportion of male caregivers. However, no gender differences were found for changes in depression and subjective well-being .
Furthermore, we found that the effects of interventions varied by the levels of objective and subjective burden at the time of first measurement. With regard to objective burden, in studies where caregivers provided support for more hours, we found less improvement for burden, depression, and subjective well-being, but greater improvements for ability/knowledge. In addition, in studies where caregivers had been providing care over a longer period, a greater increase in well-being and ability/knowledge and a greater improvement of care receivers' symptoms but a smaller decrease in depression were observed. Greater subjective burden (as indicated by Zarit and colleagues' 1980 , burden interview) at pretest was associated with greater improvements during intervention for caregiver burden, depression, and well-being, but smaller improvements of ability/knowledge and symptoms of the care receiver ( Table 5 ).
Study Characteristics
The measurement of outcome variables was a concern in this study. We compared, first, the different measures of caregiver burden. Studies using Zarit and colleagues 1980 ZCBI had lower effect sizes ( g = − .04, confidence interval [CI] − .09, .01) than those using other measures ( g = − .29, CI = − .34, − .24). Interventions using the Geriatric Depression Scale showed lower effect sizes ( g = − .03, CI = − .09, .02) than studies using the Beck Depression Inventory ( g = − .43, CI = − .60, − .26). However, the intervention effects on other self-ratings on subjective well-being, ability/knowledge, and care receiver's symptoms did not vary by the method of assessing these variables. We also looked at whether earlier studies may have shown larger effects than later studies. This was the case for caregiver burden but not for other outcomes. In fact, for improvement of care receiver symptoms, later studies had larger effects.
Whether treatment and control group were randomly assigned significantly predicted the size of the effects for four out of five outcome variables. Depression, subjective well-being, ability/knowledge, and care receiver symptoms showed less improvement in randomized studies. For this reason, we also computed average effect sizes for each outcome measure and for each intervention type only for randomized studies. As shown in Table 6 , we found significant short-term effects of interventions for caregiver burden, depression, ability/knowledge, and symptoms of the care receiver, and, at the p < .10 level, for subjective well-being. Significant effects at follow-up were found for depression and ability/knowledge and, at the p < .10 level, for caregiver burden.
The comparison of different types of interventions using only randomized studies revealed that psychotherapy was effective with regard to all outcome measures. Psychoeducational interventions had significant effects for all but two outcomes (well-being and care receiver symptoms; Table 7 ). Multicomponent interventions were effective in improving caregiver burden, well-being, and ability/knowledge. Also, training of the care receiver improved caregivers' subjective well-being and care receiver symptoms. However, supportive interventions were effective only for improving caregiver burden and ability/knowledge. Furthermore, only one significant effect was found for respite/daycare: Caregiver ability/knowledge, surprisingly, actually decreased in the experimental condition. However, because this effect was based on only one small study, this might reflect an outlier rather than a valid result.
The purpose of this meta-analysis was to provide an updated estimate of the overall effectiveness of caregiver interventions. The study examined new outcome variables and types of interventions that had not been included in prior meta-analyses. It also tested the effect of moderator variables on the impact of interventions. Consistent with Knight and colleagues 1993 , we found that interventions with caregivers were, on average, of small to moderate effect size (on average, 0.14 to 0.41 standard deviation units) for all six outcome variables. Among different types of treatments, psychotherapeutic and psychoeducational interventions showed the most consistent effects on all outcome variables. The effect sizes varied by intervention characteristics, aspects of the caregiving situation, the initial level of objective and subjective burden, and general study characteristics. In the following, we discuss how our study compares with other meta-analyses of caregiver interventions, explain differences in the effects of particular interventions, and consider the implications of our findings for future research.
Comparison of Outcome Variables
When considering the whole sample, all outcome variables in this study were affected by at least one intervention. However, in the present study, the average effect sizes for depressive symptoms and burden were smaller ( g s = −.15 and −.14, respectively) than the effects found by Knight and associates 1993 for individual interventions ( d s = .58 and .41, respectively; see Appendix, Note 3). The differences are likely due to the fact that a larger variety of individual interventions was included in the present study and that some studies with small average effect sizes have been published recently. The analyses for types of intervention suggest that some interventions have effects on specific outcome variables (training of the care receiver, supportive interventions, respite care), whereas others are broader in their effects. In the breakdown, effect sizes comparable to Knight and associates' are found for the impact of multicomponent interventions ( g = −.62) on burden and for psychoeducational interventions ( g = −.43) on depression. Consistent with George and Gwyther 1986 suggestion that some outcome measures may be more sensitive to change than others, we found stronger effects of interventions on caregivers' ability/knowledge than on burden, depression, uplifts of caregiving, and care receiver symptoms. This may be due, first, to the fact that a large number of studies focused on psychoeducational interventions that aim to increase caregivers' ability and knowledge. Second, smaller effects of interventions on caregiver burden and care receiver symptoms than on ability/knowledge are not surprising because even the best interventions can reduce the impact of the care receiver's illness, but they do not eliminate the problem (Zarit and Leitsch 2001 ).
The most consistent positive effects of caregiver interventions were found for psychotherapy and psychoeducational interventions, which produced improvements across practically all outcome domains. Multicomponent interventions and respite/daycare were effective for three of the outcomes, and supportive interventions were effective for two. All of these interventions address salient caregiving stressors: being overburdened with the physical and temporal demands of care, feeling isolated, having difficulties managing and responding to the care recipient's behavior, and dealing with one's own negative emotions (e.g., Kosberg and Cairl 1986 ). Multicomponent interventions may have had a large effect on caregiver burden ( g = −.57) because they consist of multiple techniques and target multiple outcome domains. They are thus most able to address a variety of caregiver needs (e.g., Mittelman et al. 1995 ). However, the effect of multicomponent interventions on caregiver depression and care receiver symptoms was not significant—presumably because only a small number of studies were available in this category. Training of the care receiver had a specific effect primarily on care receiver symptoms and almost no effect on the caregiver. Thus, a combination of interventions directly targeted to the caregiver is recommended to reduce caregiver burden and depression.
One surprising finding was that one intervention that targeted caregivers exclusively (psychotherapy) also had a positive impact on care receiver symptoms. Psychotherapy may have taught the care receiver specific techniques to respond more effectively to care receivers' problem behaviors and emotional struggles (Teri 1999 ). However, the effect may also be due to the fact that care receiver symptoms in many studies were measured by caregiver reports and were thus subject to a halo effect.
It should be noted here that comparing different types of interventions with each other in a meta-analytic context can be inherently problematic because respondents in each study may nonrandomly elect to participate in particular types of interventions or intervention studies. As covarying baseline variables is not possible in the comparative analysis, the factors that may contribute to selective participation cannot be controlled. In addition, inclusion of specific interventions in particular categories is at times difficult because the interventions may not be described in sufficient detail, and there is no agreed-on taxonomy for classifying intervention types (Schulz 2001 ). Finally, the effectiveness of an intervention depends, to some degree, on the dropout rate. Because the different types of interventions did not have identical dropout rates, some reached fewer individuals (e.g., daycare/respite and care receiver interventions) and may therefore be considered less effective, regardless of their effect sizes. Thus, analyses comparing different interventions, while informative about the outcomes that these interventions affect, should not be construed as an exclusive evaluation of the overall quality of these intervention types.
Influence of Moderator Variables
Our finding that group interventions are less effective at improving caregiver burden and well-being than individual and mixed interventions (i.e., combinations of group and individual programs) replicates earlier findings (Knight et al. 1993 ; Whitlatch et al. 1991 ). Our reanalysis comparing individual versus group and mixed interventions confirms this finding. It is also consistent with Pinquart and Sorensen 2001 meta-analysis of the effectiveness of therapeutic interventions with older adults in general.
The smaller effect of group interventions on caregiver burden and well-being in the present study may be related to three methodological issues: First, the type of intervention may be confounded with the group versus individual format. That is, psychoeducational interventions are mostly done in groups, whereas psychotherapy is often done in an individual setting. However, psychoeducational interventions and supportive interventions, which are usually carried out in groups, did not significantly differ from psychotherapeutic interventions in their effects on caregiver burden and well-being. In fact, the only intervention type that was significantly different from others for burden was the multicomponent intervention, and only miscellaneous interventions were significantly different from other interventions in their effects on caregiver well-being. Because multicomponent and miscellaneous interventions usually combine individual interventions and group interventions, they are unlikely to have biased the comparison of interventions in groups with interventions in the individual setting.
Second, it is also possible that among the group approaches that were included, the less effective interventions of the early years dominated over later, more sophisticated programs. However, because we controlled for year of publication, the smaller effects of group interventions on burden and well-being cannot be explained by the fact that early studies were less effective than later studies. Finally, the results may have been influenced by a selection bias, because participants were not randomly assigned to individual treatment or group treatment. However, we found no significant differences in the levels of initial objective and subjective burden between the participants of the individual condition and those of the group condition. Although other differences between participants in the individual and group conditions may still have contributed to our results, a comparison to specific caregiver intervention studies that randomly assigned participants to group and individual conditions (e.g., Whitlatch et al. 1991 ) or that approached a true experimental design (e.g, Toseland et al. 1990 ) also shows that individual caregiver interventions look slightly more effective than group interventions in reducing depression and improving well-being. Thus it is relatively unlikely that our finding is an artifact of selection. The observed differences between individual and group interventions on depression and well-being may, rather, indicate that individual interventions are somewhat more effective at adapting the topics and methods of the intervention to individuals' specific caregiving concerns.
However, we found that interventions in groups are more effective than individual treatments with regard to improving care receiver symptoms. The group setting may promote the exchange of experiences and techniques in how to influence the care recipient's behavior, thus enabling mutual learning. In addition, previous studies have shown that interventions in groups have the added advantage of building up supportive social networks (Toseland and Rossiter 1989 ). Owing to the lack of sufficient data for different forms of intervention, social support outcomes were not a focus of the present meta-analysis. Thus, whether individual interventions or group interventions are of advantage depends on the selection of outcome measures.
The length of an intervention appears to be important in alleviating caregiver depression and care receiver symptoms. Change in other variables was unaffected by the length of the intervention. Caregivers may benefit more from longer interventions with regard to depression because of the supportive aspects of prolonged contact with a group or a professional. Care receivers may benefit more from longer interventions because it takes more time for caregivers to learn, place their trust in, and subsequently implement new response patterns that can effect change in care receivers' behavior and because multiple approaches are often needed to change care receivers' symptoms (Ostwald et al. 1999 ).
Aspects of the Caregiving Situation
The analyses of the caregiving situation suggest that care receiver characteristics are strongly related to intervention effectiveness. Because many of the diseases and disabilities leading to the need for care are progressive in nature, the caregivers of older care recipients are likely to encounter more stressors and limitations in their activities (Coen, Swanwick, O'Boyle, and Coakley 1997 ). They are thus more likely to benefit from an intervention that either frees up their time or provides them with emotional support. However, for four of the five dependent variables, interventions with caregivers of dementia patients are less successful than for other caregivers. This effect is probably underestimated in our study because even among studies that do not explicitly focus on dementia, there are often care receivers suffering from this disease. Dementia caregivers cope with unpredictable stressors, such as problem behaviors and personality changes. Because these may be more difficult to cope with and less modifiable than the stressors common to pure physical care (Birkel and Jones 1989 ), it may be more difficult to effect change through intervention with this population.
The findings regarding care receiver age and diagnosis are consistent with results regarding initial objective caregiver burden. The impact of objective burden (measured by number of care hours per week and number of years providing care) on effect sizes of interventions varies with the outcome variable that is investigated. Greater objective burden at pretest is associated with greater increases in knowledge and greater improvements of care receiver symptoms. However, greater objective burden is also related to less improvement of subjective burden and depression. Presumably, if levels of caregiving are relatively high and cannot be reduced, as might be the case for dementia caregivers, then burden and depression are less amenable to change as well. In contrast, a larger time commitment to caregiving may also preclude independent information gathering, such as about the care receiver's disease or available community services, and an intervention that provides this information may substantially increase knowledge for those who are more burdened. Surprisingly, this is even the case for individuals with a longer history of caregiving, even though one might expect them to have gathered much knowledge about caregiving from experience.
In contrast to objective burden, greater initial subjective burden is related to larger intervention effects for burden, depression, and well-being, probably because most interventions are geared toward reducing subjective burden, as measured by the ZCBI and other burden measures. Also, for those with already low levels of burden, interventions are less likely to produce improvements because of floor effects. However, caregivers with high subjective distress reported less improvement in ability/knowledge and care receiver symptoms, which may indicate that they were faced with severe care receiver symptoms that were not easily modifiable.
With regard to caregiver characteristics, spouse caregivers benefit less from interventions than do adult children. Adult children probably derive greater advantages from caregiver interventions because they are often less prepared for the strains of caregiving than spouses. Spouses are more likely to have already cared for their parents and have developed coping strategies or gathered information about community services and supports from their previous experience. The crucial information that interventions provide is more novel to adult children and, therefore, more effective at reducing their burden. Moreover, adult children often have several additional social roles (e.g., nuclear family responsibilities and work), which may lead to greater role strain (Reid and Hardy 1999 ; Stephens, Franks, and Townsend 1994 ). Learning to cope with role strain may be a particularly useful aspect of caregiver interventions.
Higher proportions of women in the sample are related to a more positive caregiver response to interventions with regard to burden, ability/knowledge, and care receiver symptoms. This effect may be related to higher levels of initial psychological distress in female than in male caregivers (Miller and Cafasso 1992 ).
Studies where caregivers were assigned randomly to the intervention or control group reported smaller improvements for depression, well-being, ability/knowledge, and care receiver symptoms when randomization was evaluated as a predictor of effect size. Random assignment does not guarantee that control groups remain pure "placebo" groups (Zarit et al. 1987 ); greater use of alternative services by those on a wait-list may lead to smaller intervention effects. In addition, individuals with lower subjective well-being and higher motivation are more likely to self-select into the intervention condition in nonrandom studies and are thus more likely to benefit from the intervention (Gonyea and Silverstein 1991 ), although selection factors may vary for different studies (Knight et al. 1993 ).
When analyzing only the randomized studies, we found positive short-term intervention effects for five out of six outcome variables and positive intervention effects at follow-up for three out of five outcome variables. However, because only one and four studies, respectively, were available for the short-term effects on caregiver uplifts and long-term effects on caregiver well-being, these nonsignificant effects must be interpreted with caution. The positive effects of psychotherapy and psychoeducational interventions and, in part, of supportive and multicomponent interventions were replicated. However, no positive effects of respite/daycare remained when only randomized studies were analyzed. Only a small number of randomized respite/daycare interventions were available, thus reducing the chance of finding significant effects. Also, caregivers seeking respite and being randomly assigned to the control condition may be very highly motivated to seek alternative support, thus reducing the difference to observed change in the experimental condition (Zarit 1994 ). Unfortunately, we were not able to rule out this explanation empirically. A third explanation may be that the positive effects of daycare/respite in the full sample are based primarily on sources of bias in the nonrandomized studies (e.g., influences of social desirability). Although there is no direct evidence for this in the analyzed publications, this explanation also cannot be completely ruled out.
Higher dropout rates are associated with greater reductions in burden, depression, and care receiver symptoms, but smaller improvements of caregivers' ability/knowledge. Individuals who do not benefit from the intervention are more likely to discontinue participation. In studies with high dropout rates, above average effects on burden and depression may be based on the highly motivated "stayers." Psychoeducational interventions, which were very effective at increasing knowledge and abilities, had low dropout rates, on average. This may explain the increase in knowledge in studies with low dropout rates.
A further study characteristic is the year of publication. In our study, more recent publication was related to smaller improvements for burden but larger improvements of care receiver symptoms than earlier publication. Callahan 1989 and others' criticism of the intervention literature may have initiated a trend toward more careful studies with control groups, higher quality outcome measures, and a greater likelihood for null results to be published. In addition, recent advances in methods for teaching caregivers how to respond more effectively to care receivers' memory and behavioral problems may have improved the effects of interventions on care receiver symptoms in more recent studies (e.g., Ostwald et al. 1999 ).
Limitations
The first limitation is that we were not able to disaggregate the multiple dimensions of the burden measures in this study, as has been suggested by George and Gwyther 1986 , primarily because burden is still reported as one score in most intervention studies. However, we were able to separate subjective and objective burden in our moderator analysis, which contributed to a more differentiated picture. Second, many studies had missing data for relevant variables (e.g., dropout rate), making it impossible to do multivariate analyses for these variables. Similarly, some of the outcome variables were addressed in very few studies. For example, no separate analyses for types of interventions or subgroups could be performed for uplifts because of the small number of studies in this category. Third, delivery characteristics (group or length) and intervention type are sometimes confounded. Thus, although we used multivariate methods of analysis when possible, it was impossible to specify the source of some of our effects. Fourth, although we analyzed for follow-up outcomes across all interventions, we were not able to disaggregate proximal and distal outcomes for specific types of interventions. Future research is needed to assess which interventions provide caregivers with coping strategies that facilitate long-term relief versus provide only short-term solutions (Schulz 2001 ). Fifth, it was not possible in this study to control for the timing of interventions, that is, to see whether interventions that focus on family members in the early and middle stages of a progressive disease are more effective than those that focus on late-stage caregivers (Zarit and Leitsch 2001 ). Sixth, in a meta-analysis it is not possible to control for the selection effects that may have led individuals to enroll in particular types of interventions. As suggested by one reviewer, the best way to determine whether one type of intervention is more effective than another is to design a randomized direct comparison. As there are relatively few such studies, future research should embrace this approach. In addition, further research is needed on how the individual's motivation to participate in specific forms of intervention influences effect sizes. Seventh, meta-analysis allows the researcher to control only some of the possible moderators that can affect an intervention's effectiveness. For example, we were unable to control for the effect of therapists' or group leaders' level of training. Eighth, the majority of studies reviewed here are studies of the interventions' effectiveness and not its efficacy. Thus, this meta-analytic method allows only an assessment of effectiveness. Finally, meta-analysis is often criticized for using primarily published studies, which tend to have higher effect sizes and are less likely to have null results (because null results are less likely to be published: file-drawer problem; Rosenthal 1991 ). Our analyses (see Appendix, Note 1) suggest that it is highly unlikely that we have overestimated our effects due to the file drawer problem, as unpublished studies had higher effect sizes than published studies.
Conclusions and Recommendations
Interventions are, on average, successful in alleviating burden and depression, increasing general subjective well-being, and increasing caregiving ability/knowledge. The majority of these effects persist after an average of 7 months postintervention. Providing psychoeducational interventions, psychotherapy, and a combination of several of these interventions, as is done in multicomponent approaches, is most effective for improving caregiver well-being in the short term. Although the lack of random assignment limits our conclusions, the results suggest that some interventions have broad, nonspecific effects across a range of outcomes (psychotherapy, psychoeducational interventions, multicomponent interventions), whereas others have more specific effects on targeted outcomes (care receiver training, supportive interventions).
Clinicians and interventionists should decide in advance whether specific targeted outcomes or general improvement of well-being is the goal of their intervention because each of these goals may require a different set of intervention techniques, implementation strategies, and attention to different potential moderators. For example, based on our findings, we recommend that the length of the intervention be matched to the goal of the program. Interventions of 7–9 sessions (the average across all interventions reviewed here except respite/daycare) should be adequate to increase ability/knowledge, but may be too limited to improve depression.
Spousal caregivers benefit less from existing interventions than adult children. This may be due to a ceiling effect because they have more knowledge of and experience with the caregiving process. In this case, interventions might focus more on trying to influence the affective aspects of caregiving. Also, spousal caregivers, due to their advanced age, often have more risk factors for distress, such as shrinking social networks, lower income, and health problems (Barber and Pasley 1994 ; Montgomery and Borgatta 1989 ) and may need assistance with building supportive social networks, access to low-cost respite care, and taking care of their own health. Further research is necessary to understand which factors are most responsible for spouses' smaller benefit from interventions so that interventions can take these factors into account.
Dementia caregivers also benefited less from the interventions than did caregivers of older adults without dementia and mixed samples. More efforts are needed to increase the effectiveness of interventions with dementia caregivers, for example, by combining respite/daycare with training to increase caregivers' abilities to cope with care receiver behavior problems. New initiatives of this kind are likely to be found in large, multicenter studies, such as the Resources for Enhancing Alzheimer's Caregiver Health project (REACH; Schulz and Ory 1999 ).
Individual interventions were more effective at improving caregiver well-being whereas interventions in groups were more effective at improving care receiver symptoms. Other studies have shown that group interventions are effective ways to build supportive networks. Thus, we recommend that choosing an intervention setting should depend on the main goals of the intervention. If the intervention aims to improve caregiver affect, build supportive networks, and alleviate care receiver symptoms, then a combination of individual and group intervention may be the best choice.
The data also suggest that more well-controlled randomized intervention studies are needed to study the effects of respite/daycare as well as the long-term or delayed effects of interventions with caregivers.
In sum, our findings suggest that it is both justifiable and recommended to implement interventions while maintaining realistic expectations with regard to outcomes. Objective caregiver burden can be reduced to some degree, but it is rarely possible to eliminate it completely. The present comparison of different intervention types and analysis of moderators of effectiveness provides an important foundation on which to develop more effective interventions.
Book Reviews
Practice Concepts
In an additional analysis, we checked whether unpublished studies would show different effect sizes than published studies. Surprisingly, we found larger effects for unpublished studies (e.g., doctoral dissertations) than for published studies. This may indicate that doctoral students are more motivated and have more time to plan and conduct a well-designed intervention study. However, we cannot rule out an alternative explanation, that unpublished studies that have not been subjected to peer scrutiny are, in some cases, more likely to contain biased, manipulated, or erroneous data. We therefore followed the recommendation of a reviewer to include in the meta-analysis only studies published in peer-reviewed journals.
Because for some outcomes a negative effect is more desirable (e.g., reduction of burden) whereas for some a positive effect is hoped for (e.g, ability/knowledge), the desired direction of the outcome variable is reflected in the column headings in Table 4 and Table 5 .
Our effect size measure g differs from the measure d that was used by Knight and colleagues 1993 in that g is corrected for a bias due to overestimation of the population effect size common for small samples. On the basis of Hedges 1981 , g is the product of d and a correction factor c(m) that equals 1 − [3/(4* df − 1)], with df = degrees of freedom ( n intervention + n control − 2). For an average n intervention = 24 and n control = 20, g is 1.8% smaller than d . Because this difference is much smaller than the observed differences in the overall effect size between Knight and colleagues 1993 and our meta-analysis, the latter differences cannot be interpreted as mainly reflecting a difference in the computation of effect sizes.
Moderators of Intervention Effects and Their Coding
Note : ZCBI = Zarit Caregiver Burden Inventory.
Intervention Effects on Caregivers' Burden, Depression, Subjective Well-Being, Uplifts, Abilities/Knowledge, and Symptoms of Care Recipients
Notes : t = test of significance of the mean. Homogeneity: Significant effects indicate heterogeneity of the effect sizes. Heterogeneous effects indicate that the effect sizes between studies vary and that there are likely to be moderators. Effect sizes for uplifts were not included for the follow-up because there was only one study in this category.
p < .10;
p < .05;
p < .01;
p < .001.
Effects of Different Types of Intervention on Caregiver and Care Receiver Outcomes (Pre–Post)
Notes : t = test of significance of the mean. Homogeneity: Significant effects indicate heterogeneity of the effect sizes. There were no studies on the effects of miscellaneous interventions on caregiver well-being and ability/knowledge. Dashes indicate that it was impossible to calculate a homogeneity coefficient because only one study was available for that category.
Influence of Moderator Variables on Positive Intervention Effects (Weighted Multiple Linear Regression)
Influence of Moderator Variables on Positive Intervention Effects (Univariate Multiple Linear Regression)
Intervention Effects on Caregiver Burden, Depression, Subjective Well-Being, Uplifts, Abilities/Knowledge, and Symptoms of Care Recipients: Randomized Studies Only
Notes : t = test of significance of the mean. Homogeneity: Significant effects indicate heterogeneity of the effect sizes. Heterogeneous effects indicate that the effect sizes between studies vary and that there are likely to be moderators. Effect sizes for uplifts were not included for the follow-up because there was only one study in this category. Also, because there was only one study for subjective well-being follow-up, no homogeneity coefficient could be calculated.
Effects of Different Types of Interventions on Caregiver and Care Receiver Outcomes (Pre–Post):Randomized Studies Only
Notes : t = test of significance of the mean. Homogeneity: Significant effects indicate heterogeneity of the effect sizes. Dashes indicate that it was impossible to calculate a homogeneity coefficient because there was only one study available for that category.
Special thanks to Louise Dugan for help with literature search and format editing.
References marked with an asterisk indicate studies included in the meta-analysis.
Archbold P. G., Stewart B. J., Miller L. L., Harvath T. A., Greenlick M. R., Van Buren L., Kirschling J. M., Valanis B. G., Brody K. K., Schook J. E., Hagan J. M., 1995 . The PREP system of nursing interventions: A pilot test with families caring for older members. Research in Nursing and Health 18: 3 -16.
Baldwin B. A., Kleeman K. M., Stevens G. L., Rasin J., 1989 . Family caregiver stress: Clinical assessment and management. International Psychogeriatrics 1: 185 -194.
Barber C. E., Pasley B. K., 1994 . Family care of Alzheimer's patients: The role of gender and generational relationship on caregiver outcomes. Journal of Applied Gerontology 14: 172 -192.
Beck A. T., Steer R. A., 1987 . Beck Depression Inventory—Manual Psychological Corporation, San Antonio, TX.
Birkel R. C., Jones C. J., 1989 . A comparison of the caregiving networks of dependent elderly individuals who are lucid and those who are demented. The Gerontologist 29: 114 -119.
Bodnar J. C., Kiecolt-Glaser J. K., 1994 . Caregiver depression after bereavement: Chronic stress isn't over when it's over. Psychology and Aging 9: 372 -380.
Bourgeois M. S., Schulz R., Burgio L., 1996 . Interventions for caregivers of patients with Alzheimer's disease: A review and analysis of content, process, and outcomes. International Journal of Aging and Human Development 43: 35 -92.
Bourgeois, M. S., Schulz, R., Burgio, L., & Beach, S. (in press). Skills training for spouses of patients with Alzheimer's disease: Outcomes of an intervention study. Journal of Clinical Geropsychology .*
Bradburn N. M., 1969 . The structure of psychological well-being Aldine, Chicago.
Brennan P. F., Moore S. M., Smyth K. A., 1995 . The effects of a special computer network on caregivers of persons with Alzheimer's disease. Nursing Research 44: 166 -172.
Brodaty H., Gresham M., 1989 . Effect of a training programme to reduce stress in carers of patients with dementia. British Medical Journal 299: 1375 -1379.
Brodaty H., Gresham M., Luscombe G., 1997 . The Prince Henry Hospital dementia caregivers' training program. International Journal of Geriatric Psychiatry 12: 183 -192.
Brodaty H., Roberts K., Peters K., 1994 . Quasi-experimental evaluation of an educational model for dementia caregivers. International Journal of Geriatric Psychiatry 9: 195 -204.
Buckwaller K. C., Gerdner L., Kohout F., Hall G. R., Kelly A., Richards B., Sime M., 1999 . A nursing intervention to decrease depression in family caregivers of persons with dementia. Archives of Psychiatric Nursing 13: 80 -88.
Burdz M. P., Easton W. O., Bond J. B., 1988 . Effects of respite care on dementia and nondementia patients and their caregivers. Psychology and Aging 3: 38 -42.
Burgener S.C., Bakas T., Murray C., Dunahee J., Tossey S., 1998 . Effective caregiving approaches for patients with Alzheimer's disease. Geriatric Nursing 19: 121 -126.
Callahan J. J., 1989 . Play it again Sam—There is no impact. The Gerontologist 29: 5 -6.
Chang B. L., 1999 . Cognitive-behavioral intervention for homebound caregivers of persons with dementia. Nursing Research 48: 173 -182.
Chiverton P., Caine E. D., 1989 . Education to assist spouses in coping with Alzheimer's disease: A controlled trial. Journal of the American Geriatrics Society 37: 593 -598.
Chu P., Edwards J., Levin R., Thomson J., 2000 . The use of clinical case management for early stage Alzheimer's patients and their families. American Journal of Alzheimer's Disease and other Dementias 15: 284 -290.
Clipp E. C., George L. K., 1993 . Dementia and cancer: A comparison of spouse caregivers. The Gerontologist 33: 534 -541.
Coen R. F., Swanwick G. R., O'Boyle C. A., Coakley D., 1997 . Behavior disturbance and other predictors of carer burden in Alzheimer disease. International Journal of Geriatric Psychiatry 12: 331 -336.
Cooke D. D., McNally L., Mulligan K. T., Harrison M. J. G., Newman S. P., 2001 . Psychosocial interventions for caregivers of people with dementia: A systematic review. Aging and Mental Health 5: 120 -135.
Dellasega C., 1990 . Coping with caregiving: Stress management for caregivers of the elderly. Journal of Psychosocial Nursing 28: 15 -22.
Demers A., Lavoie J. P., 1996 . Effect of support groups on family caregivers to the frail elderly. Canadian Journal on Aging 15: 129 -144.
Derogatis L., Melisaratos N., 1983 . The Brief Symptom Inventory: An introductory report. Psychological Medicine 13: 595 -605.
Dunkin J., Anderson-Hanley C., 1998 . Dementia caregiver burden: A review of the literature and guidelines for assessment and intervention. Neurology 51: (Suppl. 1) S53 -S60.
Drummond M. F., Mohide E. A., Tew M., Streiner D. L., Pringle D. M., Gilbert J. R., 1991 . Economic evaluation of a support program for caregivers of demented elderly. International Journal of Technology Assessment in Health Care 7: 209 -218.
Dziegielewski S.F., 1991 . Social group work with the family member of elderly nursing home residents with dementia: A controlled evaluation. Research on Social Work Practice 1: 358 -370.
Fletcher R. H., Fletcher S. W., Wagner E. H., 1996 . Clinical epidemiology: The essentials 3rd Ed. Kluwer, New York.
Gallagher-Thompson D., Arean P., Rivera P., Thompson L. W., 2001 . A psychoeducational intervention to reduce distress in Hispanic family caregivers: Results of a pilot study. Clinical Gerontologist 23: 17 -32.
Gallagher-Thompson D., Lovett S., Rose J., McKibbin C., Coon D., Futterman A., Thompson L. W., 2000 . Impact of psychoeducational interventions on distressed family caregivers. Journal of Clinical Geropsychology 6: 91 -110.
Gendron C. E., Poitras L.-R., Engels M. L., Dastoor D. P., Sirota S. E., Barza S. L., Davis J. C., Levine N. B., 1986 . Skills training with supporters of the demented. Journal of the American Geriatrics Society 34: 875 -880.
George L. K., Gwyther L. P., 1986 . Caregiver well-being: A multidimensional examination of family caregivers of demented adults. The Gerontologist 26: 253 -259.
Gitlin L., Cocoran M., Winter L., Boyce A., Hauck W. W., 2001 . A randomized controlled trial of a home environmental intervention: Effect on efficacy and upset in caregivers and on daily function of persons with dementia. The Gerontologist 41: 4 -14.
Glass G. V., McGaw B., Smith M. L., 1981 . Meta-analysis in social research Sage, Beverly Hills, CA.
Goldberg R. J., Wool M. S., 1985 . Psychotherapy with spouses of lung cancer patients: Assessment of interventions. Psychotherapy and Psychosomatics 43: 141 -150.
Gonyea J. G., Silverstein N. M., 1991 . The role of Alzheimer's disease support groups in families' utilization of community services. Journal of Gerontological Social Work 16: (3/4) 43 -55.
Greene V. L., Monahan D. J., 1989 . The effect of a support and education program on stress and burden among family caregivers to frail elderly persons. The Gerontologist 29: 472 -477.
Guttman R. A., 1991 . Adult day care for Alzheimer's patients: Impact on family caregivers Garland, New York.
Haley W. H., Brown S. L., Levine E. G., 1987 . Experimental evaluation of the effectiveness of group intervention for dementia caregivers. The Gerontologist 27: 376 -382.
Hebert R., Leclerc G., Bravo G., Girouard D., 1994 . Efficacy of a support group programme for caregivers of demented patients in the community: A randomized controlled trial. Archives of Gerontology and Geriatrics 18: 1 -14.
Hedges L. V., 1981 . Distribution theory for Glass's estimator of effect size and related estimators. Journal of Educational Statistics 6: 107 -128.
Hedges L. V., 1994 . Fixed effect models. Cooper H., Hedges L. V., , ed. Handbook of research synthesis 285 -299. Sage, New York.
Hedges L. V., Olkin I., 1985 . Statistical methods for meta-analysis Academic Press, Orlando, FL.
Hepburn K. W., Tornatore J., Center B., Ostwald S. W., 2001 . Dementia family caregiver training: Affecting beliefs about caregiving and caregiver outcomes. Journal of the American Geriatrics Society 49: 450 -457.
Hincliffe A. C., Hyman I. L., Blizard B., Livingston G., 1995 . Behavioral complications of dementia—can they be treated?. International Journal of Geriatric Psychiatry 10: 839 -847.
Hughes S. L., Cummings J., Weaver F., Manheim L. M., Conrad K. J., Nash K., 1990 . A randomized trial of Veterans Administration home care for severely disabled veterans. Medical Care 28: 135 -145.
Kaasalainen S., Craig D., Wells D., 2000 . Impact of the caring for aging relatives group program: An evaluation. Public Health Nursing 17: 169 -177.
Kahan J., Kemp B., Staples F. R., Brummel-Smith K., 1985 . Decreasing the burden in families caring for a relative with dementing illness: A controlled study. Journal of the American Geriatrics Society 33: 664 -670.
Kennet J., Burgio L., Schulz R., 2000 . Interventions for in-home caregivers: A review of research 1990 to present. Schulz R., , ed. Handbook on dementia caregiving: Evidence-based interventions for family caregivers 61 -125. Springer, New York.
Knight B. G., Lutzky S. M., Macofsky-Urban F., 1993 . A meta-analytic review of interventions for caregiver distress: Recommendations for future research. The Gerontologist 33: 240 -248.
Kosberg J. I., Cairl R. E., 1986 . The Cost of Care Index: A case management tool for screening informal care providers. The Gerontologist 26: 273 -285.
Kosloski K., Montgomery R. J., 1993 . The effects of respite on caregivers of Alzheimer's patients: One-year evaluation of the Michigan Model Respite Programs. Journal of Applied Gerontology 12: 4 -17.
Kramer B. J., 1997 . Gain in the caregiving experience: Where are we? What next?. The Gerontologist 37: 218 -232.
Lawton M. P., 1975 . The Philadelphia Geriatric Center Morale Scale: A revision. Journal of Gerontology 30: 85 -89.
Lawton M. P., Brody E. M., Saperstein A. R., 1989 . A controlled study of respite service for caregivers of Alzheimer's patients. The Gerontologist 29: 8 -16.
LoGiudice D., Waltrowicz W., Brown K., Burrows C., Ames D., Flicker L., 1999 . Do memory clinics improve the quality of life of carers? A randomized pilot trial. International Journal of Geriatric Psychiatry 14: 626 -632.
Loomis L. S., Booth A., 1995 . Multigenerational caregiving and well-being: The myth of the beleaguered sandwich generation. Journal of Family Issues 16: 131 -148.
Lorensini S., Bates G. W., 1997 . The health, psychological and social consequences of caring for a person with dementia. Australian Journal on Aging 16: 198 -202.
Lovett S., Gallagher D., 1988 . Psychoeducational interventions for family caregivers: Preliminary efficacy data. Behavior Therapy 19: 321 -330.
Marks R., 1987 . The family dimension in long-term care: An assessment of stress and intervention. Journal of Long-Term Home Health Care 3: 18 -26.
Marriott A., Donaldson C., Tarrier N., Burns A., 2000 . Effectiveness of cognitive-behavioural family intervention in reducing the burden of carers of patients with Alzheimer's disease. British Journal of Psychiatry 176: 557 -562.
McCurry S. M., Logsdon R. G., Vitiello M. V., Teri L., 1998 . Successful behavioral treatment for reported sleep problems in elderly caregivers of dementia patients: A controlled study. Journal of Gerontology: Psychological Sciences 53B: P122 -P129.
McNair D. M., Lorr M., Droppleman L. F., 1971 . Manual for the Profile of Mood States Educational & Industrial Testing Service, San Diego, CA.
Miller B., Cafasso L., 1992 . Gender differences in caregiving: Fact or artifact?. The Gerontologist 32: 498 -507.
Milne D., Pitt I., Sabin N., 1993 . Evaluation of a carer support scheme for elderly people: The importance of coping. British Journal of Social Work 23: 157 -168.
Mittelman M.S., Ferris S.H., Shulman E., Steinberg G., Ambinder A., Mackell J., Cohen J., 1995 . A comprehensive support program: Effect on depression in spouse-caregivers of AD patients. The Gerontologist 35: 792 -802.
Mohide E. A., Pringle D. M., Streiner D. L., Gilbert J. R., Muir G., Tew M., 1990 . A randomized trial of family caregiver support in the home management of dementia. Journal of the American Geriatrics Society 38: 446 -454.
Moniz-Cook E., Agar S., Gibson G., Win T., Wang M., 1998 . A preliminary study of the effects of early intervention with people with dementia and their families in a memory clinic. Aging and Mental Health 2: 119 -211.
Montgomery R. J., Borgatta E. F., 1989 . The effect of alternative support strategies on family caregiving. The Gerontologist 29: 457 -464.
Mullen B., 1989 . Advanced basic meta-analysis Erlbaum, Hillsdale, NJ.
Neugarten B., Havighurst R. J., Tobin S. S., 1961 . The measurement of life satisfaction. Journal of Gerontology 16: 134 -143.
Newcomer R., Yordi C., DuNah R., Fox P., Wilkinson A., 1999 . Effects of the Medicare Alzheimer's disease demonstration on caregiver burden and depression. Health Services Research 34: 669 -689.
Oktay J. S., Volland P. J., 1990 . Post-hospital support program for frail elderly and their caregivers: A quasi-experimental evaluation. American Journal of Public Health 80: 39 -46.
Ostwald S. K., Hepburn K. W., Caron W., Burns T., Mantell R., 1999 . Reducing caregiver burden: A randomized psychoeducational intervention for caregivers of persons with dementia. The Gerontologist 39: 299 -309.
Pinquart M., Sörensen S., 2001 . How effective are psychotherapeutic and other psychosocial interventions with older adults? A meta-analysis. Journal of Mental Health and Aging 7: 207 -243.
Pusey H., Richards D., 2001 . A systematic review of the effectiveness of psychosocial interventions for carers of people with dementia. Aging and Mental Health 5: (2) 107 -119.
Quayhagen M. P., Quayhagen M., 1989 . Differential effects of family-based strategies on Alzheimer's disease. The Gerontologist 29: 150 -155.
Quayhagen M. P., Quayhagen M., Corbeil R. R., Hendrix R. C., Jackson J. E., Snyder L., Bower D., 2000 . Coping with dementia: Evaluation of four non-pharmacologic interventions. International Psychogeriatrics 12: 249 -265.
Radloff L. S., 1977 . The CES-D scale: A self-report depression scale for research in the general population. Journal of Applied Psychological Measurement 1: 385 -401.
Reid J., Hardy M., 1999 . Multiple roles and well-being among midlife women: Testing role strain and role enhancement theories. Journal of Gerontology: Social Sciences 54B: S329 -S338.
Riordan J. M., Bennett A.V., 1998 . An evaluation of an augmented domiciliary service to older people with dementia and their carers. Aging & Mental Health 2: 137 -143.
Ripich D. N., Ziol E., Lee M. M., 1998 . Longitudinal effects of communication training on caregivers of persons with Alzheimer's disease. Clinical Gerontologist 19: (2) 37 -55.
Roberts J., Browne G., Milne C., Spooner L., Gafni A., Drummond-Young M., LeGris J., Watt S., LeClair K., Beaumont L., Roberts J., 1999 . Problem-solving counseling for caregivers of the cognitively impaired: Effective for whom?. Nursing Research 48: 162 -172.
Robinson K. M., 1988 . A social skills training program for adult caregivers. Advanced Nursing Science 10: (2) 59 -72.
Robinson K. M., Yates K., 1994 . Effects of two caregiver-training programs on burden and attitude toward help. Archives of Psychiatric Nursing 8: 312 -319.
Rosenthal R., 1991 . Meta-analytic procedures for social research Sage, Beverly Hills, CA.
Rose-Rego S. K., Strauss M. E., Smyth K. A., 1998 . Differences in the perceived well-being of wives and husbands caring for persons with Alzheimer's disease. The Gerontologist 38: 224 -230.
RPI Home Care Classification Project 1986 . Development of a survey, case mix measurement system, and assessment instrument to rationalize the long-term care system Rensselaer Polytechnic Institute, Troy, NY.
Schacke, C., & Zank, S. (in press). Gerontopsychiatrische Tagespflege als Entlastungsmöglichkeit für die Angehörigen der demenzkranken Patienten: Eine Evaluationsstudie [Reducing caregiver burden by daycare for demented elderly: An evaluation study]. Zeitschrift für Verhaltenstherapie und Verhaltensmedizin .*
Scharlach A. E., 1987 . Relieving feelings of strain among women with elderly mothers. Psychology and Aging 2: 9 -13.
Schultz C. L., Schultz N. C., 1990 . Caring for family caregivers. Australian Journal of Marriage & Family 11: 84 -93.
Schultz C. L., Schultz N. C., Greenwood K. M., 1992 . Caring for family caregivers: A replication study. Australian Psychologist 27: 181 -185.
Schultz C. L., Schultz N. C., Smyrnios K. X., 1994 . Caring for family caregivers of dependent aging persons: Process and outcome evaluation. Australian Journal on Aging 13: 193 -196.
Schultz C. L., Smyrnios K. X., Grbich C. F., Schultz N. C., 1993 . Caring for family caregivers in Australia: A model of psychoeducational support. Aging and Society 13: 1 -25.
Schultz C. L., Smyrnios K. X., Schultz N. C., Grbich C. F., 1994 . Longitudinal outcomes of psychoeducational support for family caregivers of elderly dependent persons. Australian Psychologist 28: 21 -24.
Schulz R., 2001 . Some critical issues in caregiver intervention research. Aging and Mental Health 5: (Suppl. 1) S114 -S117.
Schulz R., Beach S., 1999 . Caregiving as a risk factor for mortality: Caregiver Health Effects Study. Journal of the American Medical Association 282: 2215 -2219.
Schulz R., Ory M., 1999 . REACHing out to dementia caregivers. Innovations in Aging 3: 8 -11.
Schwiebert V. L., Myers J. E., 1994 . Midlife care givers: Effectiveness of a psychoeducational intervention for midlife adults with parent-care responsibilities. Journal of Counseling and Development 72: 627 -632.
Silliman R., McGarvey S. T., Raymond P. M., Fretwell M. D., 1990 . The Senior Care Study: Does inpatient interdisciplinary geriatric assessment help the family caregivers of acutely ill older patients?. Journal of the American Geriatrics Society 38: 461 -466.
Smeenk, F. W., deWitte, L. P., vanHaastregt, J. C., Schipper, R. M., Biezemans, H. P., & Crebolder, H. F. (1998). Transmural care of terminal cancer patients: Effects on the quality of life of direct caregivers. Nursing Research, 1998 , 129–136.*
Steffen A. M., 2000 . Anger management for dementia caregivers: A preliminary study using video and telephone interviews. Behavior Therapy 31: 281 -299.
Steffen A. M., Futterman A., Gallagher-Thompson D., 1998 . Depressed caregivers: Comparative outcomes of two interventions. Clinical Gerontologist 19: (4) 3 -15.
Stephens M. A. P., Franks M. A., Townsend A. L., 1994 . Stress and rewards in women's multiple roles: The case of women in the middle. Psychology and Aging 9: 45 -52.
Sutcliffe C., Larner S., 1988 . Counselling carers of the elderly at home: A preliminary study. British Journal of Clinical Psychology 27: 177 -178.
Tennstedt, S. L., McKinlay, J. B., & Sullivan, L. M. (1988, November). Informal care for frail elders: The role of secondary characteristics . Paper presented at the 41st Annual Scientific Meeting of The Gerontological Society of America, San Francisco, CA.
Teri L., 1999 . Training families to provide care: Effects on people with dementia. International Journal of Geriatric Psychiatry 14: 110 -119.
Teri L., Logsdon R. G., Uomoto J., McCurry S. M., 1997 . Behavioral treatment of depression in dementia patients: A controlled clinical trial. Journal of Gerontology: Psychological Sciences 52B: P159 -P166.
Teri L., Truax P., Logsdon R., Uomoto J., Zarit S., Vitaliano P. P., 1992 . Assessment of behavioral problems in dementia: The revised Memory and Behavior Problems Checklist. Psychology and Aging 7: 622 -631.
Toseland R. W., Labrecque M. S., Goebel S. T., Whitney M. H., 1992 . An evaluation of a group program for spouses of frail elderly veterans. The Gerontologist 32: 383 -390.
Toseland R. W., McCallion P., Smith T., Huck S., Bourgeois P., Garstka T. A., 2001 . Health education groups for caregivers in an HMO. Journal of Clinical Psychology 57: 551 -570.
Toseland R. W., Rossiter C. M., 1989 . Group interventions to support family caregivers: A review and analysis. The Gerontologist 29: 438 -448.
Toseland R. W., Rossiter C. M., Labrecque M. S., 1989 . The effectiveness of peer-led and professionally led groups to support family caregivers. The Gerontologist 29: 465 -471.
Toseland R. W., Rossiter C. M., Peak T., Smith G., 1990 . Comparative effectiveness of individual and group interventions to support family caregivers. Social Work 35: 209 -217.
Toseland R. W., Smith G., 1990 . Effectiveness of individual counseling by professional and peer helpers for family caregivers of the elderly. Psychology and Aging 5: 256 -263.
Van den Heuvel E. T., deWitte L. P., Nooyen-Haazen I., Sanderman R., Meyboom-deJong B., 2000 . Short-term effects of a group support program and an individual support program for caregivers of stroke patients. Patient Education and Counseling 40: 109 -120.
Vitaliano P. P., Russo J., Young H. M., Becker J., Maiuro R. D., 1991 . The screen for caregiver burden. The Gerontologist 31: 76 -83.
Watson D., Clark L. A., Tellegen A., 1988 . Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology 54: 1063 -1070.
Weuve J. L., Boult C., Morishita L., 2000 . The effects of outpatient geriatric evaluation and management on caregiver burden. The Gerontologist 40: 429 -436.
Whitlatch C. J., Zarit S. H., von Eye A., 1991 . Efficacy of interventions with caregivers: A reanalysis. The Gerontologist 31: 9 -14.
Wilz G., Gunzelmann T., Adler C., Brähler E., 1998 . Gruppenprogramm für pflegende Angehörige von Demenzkranken. Zeitschrift für Gerontopsychologie und-psychiatrie 11: 97 -106.
Yesavage J. A., Brink T. L., Rose T. L., Lum O., Huang V., Adey M., Leirer V. O., 1983 . Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research 17: 37 -49.
Zanetti O., Metitieri T., Bianchetti A., Trabucchi M., 1998 . Effectiveness of an educational program for demented person's relatives. Archives of Gerontology and Geriatrics 6: (Suppl. 6) 531 -538.
Zarit S. H., 1994 . Methodological considerations in caregiver intervention and outcome research. Light E., Niederehe G., Lebowitz B. D., , ed. Stress effects on family caregivers of Alzheimer's patients: Research and interventions 351 -369. Springer, New York.
Zarit S. H., Anthony C. R., Boutselis M., 1987 . Interventions with caregivers of dementia patients: Comparison of two approaches. Psychology and Aging 2: 225 -232.
Zarit S. H., Leitsch S. A., 2001 . Developing and evaluating community based intervention programs for Alzheimer's patients and their caregivers. Aging and Mental Health 5: (Suppl. 1) S86 -S100.
Zarit S. H., Reever K. E., Bach-Petersen J., 1980 . Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist 20: 649 -655.
Zarit S. H., Stephens M. A. P., Townsend A., Greene R., 1998 . Stress reduction for family caregivers: Effects of adult day care use. Journal of Gerontology: Social Sciences 53B: S267 -S277.
Zarit S. H., Zarit J. M., Reever K. E., 1982 . Memory training for severe memory loss: Effects on senile dementia patients and their families. The Gerontologist 22: 373 -377.
Email alerts
Citing articles via, looking for your next opportunity.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1758-5341
- Copyright © 2024 The Gerontological Society of America
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Study protocol
- Open access
- Published: 17 March 2023
Study protocol of a telephone problem-solving intervention for Spanish-speaking caregivers of veterans post-stroke: an 8-session investigator-blinded, two-arm parallel (intervention vs usual care), randomized clinical trial
- I. Magaly Freytes ORCID: orcid.org/0000-0002-5928-3098 1 , 2 ,
- Magda K. Schmitzberger 1 ,
- Naiomi Rivera-Rivera 3 ,
- Janet Lopez 1 ,
- Keryl Motta-Valencia 4 ,
- Samuel S. Wu 5 ,
- Tatiana Orozco 1 ,
- Jennifer Hale-Gallardo 1 ,
- Nathaniel Eliazar-Macke 1 ,
- Jennifer H. LeLaurin 1 &
- Constance R. Uphold 2 , 6
BMC Primary Care volume 24 , Article number: 73 ( 2023 ) Cite this article
1730 Accesses
Metrics details
Stroke is one of the leading causes of death and the main cause of long-term disability in the United States. The significant risk factors of stroke among Hispanics are well-documented. The majority of stroke survivors return home following a stroke and are cared for by family caregivers. Due to the abrupt nature of strokes, caregivers experience unexpected changes and demands that oftentimes lead to caregiver burden and depression. Given the significant risk factors for stroke in Hispanics and the influence of culture in family norms and family management, we developed a telephone and online problem-solving intervention for Spanish-speaking stroke caregivers. This study tests the impact of a telephone and online problem-solving intervention for Spanish-speaking stroke caregivers on caregiver outcomes.
The design is a two-arm parallel randomized clinical trial with repeated measures. We will enroll 290 caregivers from 3 Veterans Affairs (VA) medical centers. Participants randomized into the intervention arm receive a problem-solving intervention that uses telephone and online education and care management tools on the previously developed and nationally available RESCUE en Español Caregiver website. In the usual care group, participants receive the information and/or support caregivers of veterans with stroke normally receive through existing VA resources (e.g., stroke-related information and support). The primary outcome is change in caregiver’s depressive symptoms at 1- and 12-weeks post-intervention. Secondary outcomes include changes in stroke caregivers’ burden, self-efficacy, problem-solving, and health-related quality of life (HRQOL) and veterans’ functional abilities. We will also determine the budgetary impact, the acceptability of the intervention and participation barriers and facilitators for Spanish-speaking stroke caregivers.
This is an ongoing study. It is the first known randomized controlled trial testing the effect of a telephone and online problem-solving intervention in Spanish for caregivers of veterans post-stroke. If successful, findings will support an evidence-based model that can be transported into clinical practice to improve the quality of caregiving post-stroke.
Trial registration
ClinicalTrials.gov: NCT03142841— Spanish Intervention for Caregivers of Veterans with Stroke (RESCUE Español). Registered on February 23, 2018. Protocol version 8. 08.11.2022.
Peer Review reports
Stroke is one of the leading causes of death and the main cause of long-term disability in the United States (U.S.) [ 1 ]. By 2030 there is a projected 20.5% increase in stroke prevalence compared to 2012; the largest increase (29%) is projected amongst Hispanic men [ 2 ]. Cardiovascular disease is a leading cause of mortality among Hispanics in the US, and Puerto Ricans have the highest hypertension-related death rate among all Hispanics [ 3 , 4 ]. A recent report from the American Heart Association and the American Stroke Association identified important issues that require the attention of researchers, such as culture and language barriers, accessibility issues, and bias among healthcare providers [ 5 ]. The economic burden of stroke on the healthcare system is also significant. The projected total cost of stroke from 2005 to 2050 (in 2005 dollars) for Hispanic individuals is $313 billion [ 2 ].
Due to the residual, and oftentimes debilitating, deficits of stroke, family caregivers become a major source of support for stroke survivors. Between 25 and 74% of stroke survivors have residual deficits and require some assistance, whereas other survivors are completely dependent on their caregivers to meet their daily living needs [ 6 ]. These unexpected changes experienced by family caregivers oftentimes result in high rates of caregiver depression [ 7 , 8 ] and burden [ 9 ]. Studies on stroke caregivers report rates of depressive symptoms in 11% to 42% of this population [ 8 ] and caregiving burden has been found to be a main reason for institutionalizing stroke survivors [ 10 ]. Consequently, national practice guidelines [ 11 , 12 ] underscore the importance of educating and supporting stroke survivors, and the family caregivers who manage their care.
Education and support programs for family caregivers have proven significant in facilitating the transition home following a stroke. Providing caregivers with information, support, and skills has the potential to reduce negative caregiver outcomes and increase the likelihood that stroke survivors can remain at home. Even though there is variation in the type and amount of information and support that caregivers need [ 13 ], multiple researchers found that individualized, tailored messages and support programs are more likely to improve caregiver outcomes than generic programs [ 14 , 15 , 16 , 17 , 18 ]. Offering education and support appropriate to the caregivers’ culture and preferred language is one way to tailor strategies and interventions for stroke caregivers. Further, interventions that include building skills to solve self-identified problems are more beneficial than other interventions [ 19 , 20 ].
Caregiver studies examining face-to-face sessions indicate that these individual or group sessions were burdensome to caregivers who had limited time and energy. Moreover, they were found to be costly and labor-intensive [ 20 ]. While some studies evaluating the effectiveness of telephone problem-solving interventions report promising findings [ 21 , 22 ], none have focused on Spanish-speaking caregivers. Therefore, it is uncertain if these telephone interventions would be equally effective within the Hispanic population.
The Internet is increasingly recognized as a cost-effective medium for disseminating up-to-date health information to large numbers of healthcare consumers. Research has shown that over 78% of Americans regularly use the Internet to obtain health information [ 23 ]. Adults 55 years and older (typical age range of stroke caregivers) are more likely to seek information on the Internet than adults in other age groups [ 24 ]. Over the last several years, the gap in Internet use between Hispanics and other groups has shrunk considerably, with Hispanics showing the highest increase in Internet usage (54% to 64%) [ 25 ]. The advantage of the Internet is that adults can receive health information at a convenient place and time.
Another gap in the stroke caregiving literature is that only a handful of studies have evaluated interventions and programs aimed at improving the lives of caregivers of veterans [ 26 ]. This is important because there are differences between veteran and non-veteran caregivers [ 26 ]. While caregivers of veterans face similar challenges as non-veteran caregivers, they also must contend with the issues related to combat-related injuries or disability, posttraumatic stress disorder (PTSD), depression, and greater health risks than the general population. Veteran care recipients also usually have lower incomes, higher rates of chronic disease, more comorbid conditions, and poorer health overall than their non-veteran counterparts [ 7 ].
Little is known about caregivers from cultural or minority groups, such as Hispanic caregivers of veterans. Studies show that in the general population, Hispanic caregivers exhibit more depression than white caregivers [ 27 ]. Other studies demonstrate that Hispanic dementia caregivers, who share similar challenges to stroke caregivers, have also been shown to have higher rates of depression compared to their non-Hispanic counterparts [ 28 ]. Given the importance of culture in affecting family norms and family management [ 29 , 30 , 31 , 32 ], it is critical that we expand our understanding of ways to enhance the important role that informal Hispanic caregivers play in the recovery and use of healthcare services by veterans post-stroke.
This study addresses an important and understudied area of caregiving research, Hispanic, Spanish-speaking caregivers of veterans who have suffered a stroke. We will focus on a Hispanic veteran population that geographically has been shown to have a high rate of strokes, Puerto Rican veterans. This study recognizes the important role that socio-cultural factors play in enhancing the skills of caregivers of stroke patients and addresses the need for culturally relevant caregiver programs. Although Hispanics are the fastest growing group in the military and the VA, there has been insufficient effort to reduce the health disparities in this population. All veterans are required to understand English, but many Hispanic family caregivers lack basic English-language skills and Spanish is their preferred language.
Methods/design
Advisory panel.
We established an advisory panel consisting of clinicians and VA leadership at the national and local level who are independent from the funding agency to obtain input in the planning and development phases of the study. The study team and the advisory panel meet quarterly to discuss progress and challenges. Once data collection is completed, members of the advisory panel will assist in the interpretation of the study findings and planning for the dissemination of results and strategies to sustain the intervention in practice if it is found to be successful. Upon approval and funding, this study was not assigned a data monitoring committee, thus, our independent advisory panel serves as our monitoring committee.
Objective and hypothesis
The objective of this study is to evaluate the impact of a telephone and online, problem-solving intervention on caregiver outcomes. Our primary aim is to reduce caregiver depression. Secondary aims are to: reduce caregiver burden, improve caregivers’ problem-solving abilities, self-efficacy, and quality of life, improve veterans’ functional abilities and determine the intervention’s impact on veterans’ healthcare utilization. Additionally, we will determine the intervention’s budgetary impact, and caregivers’ perceptions of the intervention. The primary hypothesis is that stroke caregivers in the intervention group will have fewer depressive symptoms compared to those in the usual care group. The secondary hypotheses are that caregivers of stroke survivors in the intervention will have less burden, better problem-solving abilities, higher self-efficacy, and higher quality of life compared to caregivers assigned to usual care and veterans will have better functional abilities and lower healthcare utilization.
Study design
This is a blinded, two-arm parallel (intervention vs usual care), randomized clinical trial with repeated measures. The trial started recruitment in March 2018 and is still actively recruiting participants. The original protocol was to recruit study participants from the VA Caribbean Healthcare System (VACHS) in San Juan, PR and all study procedures were to be conducted over the phone from either the North/Florida South Georgia Veterans Healthcare System (NF/SG VHS) in Gainesville, FL or the VACHS in San Juan. Within a year from the initiation of the study, we submitted and obtain approval for a project modification to add two additional sites with the sole purpose of identifying potential study participants. Data collection is currently on going in Puerto Rico and Gainesville, Florida, USA.
Study setting
The main study site is the North Florida/South Georgia Veterans Health System which coordinates all study activities and lead all research procedures. Originally, the secondary site was the VA Caribbean Healthcare System, which continues to be the main recruitment site. Due to slow recruitment as a result of the impact of hurricane Maria in PR and in an effort to capture Puerto Rican families that migrated to the mainland, we added two additional VA, the Orlando VA Medical Center and the James A. Haley Veterans Hospital. All other study procedures (recruitment, data collection, etc.) are conducted from the North Florida/South Georgia Veterans Health System, in Gainesville, FL or the VA Caribbean Healthcare System, in San Juan, PR. A flow chart of the study design is shown below in Fig. 1 .
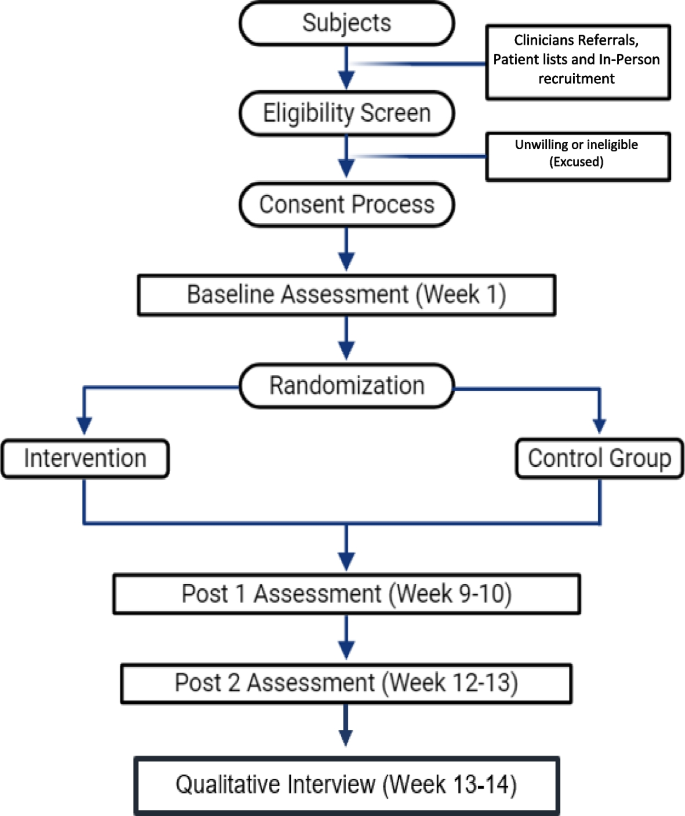
Flow chart of the study design
Eligibility criteria
All Hispanic caregivers of veterans with a primary diagnosis of stroke are eligible for participation if they meet the following criteria: 1) are the primary caregiver and provide the majority of care for a veteran who has a diagnosis of stroke (ICD9 codes for stroke: 430–438 or ICD 10 codes 160.0 through 169.998) within the last year and who have at least two activity of daily living (ADL) deficits or a new or worsening neurological problem as measured by a score of 74 or lower in the Stroke Impact Scale (SIS-16), 2) have Internet access and ability, (either themselves or via a relative or friend) 3) are reachable by cell or home phone, 4) Spanish is their preferred language, 5) have moderate to severe stress as measured by a score of 1 or higher on the Perceived Stress Scale (PSS-10), 6) self-identify as Hispanic, and 7) agree to random assignment to the intervention or usual care group. We determine caregiver status using previous research guidelines that indicate that one individual is typically identified as the primary caregiver and is responsible for the majority of caregiving tasks. We determine time since stroke by reviewing the veterans’ electronic health record (EHR). Deficits in activities of daily living [ADL] are assessed by asking caregivers if the Veteran is unable to complete any of the ADLs on the Stroke Impact Scale 16 (SIS-16). Caregivers of Veterans who had either embolic or thrombotic strokes are included because there are no previous studies that indicate a differential impact of stroke type on caregiver outcomes. We do not limit the study to caregivers of first-time stroke survivors. Hispanic/Hispanic ethnicity and Internet access and ability to use are determined by caregiver self-report. We exclude caregivers who are managing end-of-life issues (stroke survivors who are likely to die within five months following discharge). Life expectancy is determined by reviewing the EHRs and conferring with our physician team members.
Since the intervention is conducted over the phone and to reduce participation burden, we obtained a Waiver Documentation of Informed Consent. However, members of the research team trained in informed consent procedures utilize an Informed Consent Written Statement to inform interested and eligible participants about the purpose of the study, study procedures including that some sessions may be recorded, risks, volunteer nature of their participation, potential benefits, and who to contact in case of questions or concerns, etc. The written statement is also used to inform and obtain oral permission to record the interventions. A copy of the written statement is mailed to participants prior to reviewing the Informed Consent Written Statement. All informed consent procedures are conducted over the telephone by trained and experienced members of the research team from either the NF/SG VHS or the VACHS. To collect veteran healthcare utilization data, we ask caregivers to self-report.
Intervention
The intervention is based on the relational/problem-solving model of stress.
developed by D-Zurilla and Nezu [ 33 ] and integrates concepts from Lazarus’ stress appraisal and coping theory [ 34 ]. The model can be summarized by the acronym COPE (Creativity, Optimism, Planning, and Expert Information) [ 35 ] and has been translated into Spanish.
Session 1. Tour of the Spanish RESCUE Website and orientation to the problem-solving approach. During this session the interventionist builds rapport with the study participant, discusses the purpose, goals and scope of the intervention, and discusses his/her role in the intervention and the expectations for study participants. The interventionist reviews the content in the RESCUE workbook that the caregivers receive in the mail and ensures that the caregiver can access the RESCUE website. The interventionist then gives a tour of the various features on the RESCUE website as the participant simultaneously navigates and explores the website. Next, the interventionist directs the participant to the problem-solving module (either online or in the workbook) to teach the COPE problem-solving approach which involves the following steps: 1) identifying & defining problems; 2) prioritizing problems; 3) selecting the highest priority problem; 4) gathering expert information; 5) setting realistic goals; 6) listing all possible solutions; 7) choosing the best solution; and 8) evaluating the plan. The interventionist assesses participant’s understanding before discussing an illustrative example on how to apply the problem-solving approach to caregiver problems, and to use of the problem-solving diary and the materials in the RESCUE website. Session one concludes with a summary of caregiver stress and depression, assignment on the next topics for discussion, and scheduling session two with the caregiver.
Session 2. The interventionist and study participant discusses assigned topics and use the problem-solving diary and RESCUE website to work through the caregiver problems. The interventionist begins the session assessing any changes in the caregiver and veteran. Next, the interventionist discusses the content on the pre-assigned topics and addresses any questions. The study participant and the interventionist then collaborate to develop a personalized problem-solving plan to address participant’s caregiving problems using the problem-solving diary which can be accessed and printed from the RESCUE website. The interventionist uses motivational interviewing [ 36 ] and encourages the participant to talk about their caregiver challenges. The interventionist can also review the list of topics/factsheets that are on the RESCUE website to trigger identification of problems. The study participant uses the diary to write down and prioritize their caregiving problems, identifying the most troublesome. The interventionist then empowers the participant to identify realistic goal(s), possible solutions, best solution, and evaluation plans, which are recorded in the problem-solving diary. At the conclusion of session two, the interventionist addresses any questions and highlights the major points of discussion. The next session is also scheduled and three fact sheets from the RESCUE website are assigned for the following session.
Sessions 3–7. The interventionist and study participant continue to discuss assigned topics and use the problem-solving diary and RESCUE website to work through the caregiver problems. These sessions are very similar to the previous one. The assigned readings for sessions 4—7, are chosen based on the caregiver problems and priorities identified in the previous session. In session seven, the interventionist also alerts the participant that the next session will be their last.
Session 8. Summary of the problem-solving approach. The interventionist begins by assessing any changes in the participant and veteran. Next, they review and discuss the assigned topics for the session. The interventionist then works with the study participant to review and finalize the personalized problem-solving plan using the problem-solving diary and, identify information related to newly identified caregiver problems on the RESCUE website. The session ends with a summary of what they learned throughout the intervention and motivational message to empower the participant to continue using the RESCUE website and to regularly evaluate their personalized problem-solving plan.
To reflect the current real-world experience of caregivers, we selected usual care as the control condition in this study to determine if the intervention is superior to usual care. Participants in the standard care group receive the care that is normally provided to stroke caregivers of Veterans. Caregivers do not normally receive any follow-up telephone or transitional care unless they are enrolled in the telehealth or home-based primary care programs (study exclusionary criteria). Stroke caregivers may only receive contact information for stroke clinicians, and some may receive informational brochures or an invitation to participate in an open support group led by the psychologist in the rehabilitation clinic. At the end of the study, we will ask caregivers in the standard care group about resources used throughout the study.
Fidelity considerations
We make special effort to enhance, maintain and track treatment fidelity. Study personnel use a study manual that provides step-by-step guidelines for recruitment, enrollment, informed consent, intervention and data collection procedures. All members of the study team receive extensive training on all pertinent study procedures. In addition, ten percent of the intervention sessions are observed either in-person or from a digital recording by the study PI using a fidelity checklist developed by the study team to measure adherence to the protocol, therapeutic communication skills, delivery of intervention content, integration of the COPE model, decision-making skills, and response to caregiver problems. This tool is used to document deviation from study protocols and give feedback to the interventionists to ensure fidelity.
To improve subject adherence, study staff provide reminder phone calls one day prior to the weekly session. The interventionists also emphasize the importance of following study procedures during the first intervention session and have staggered schedules to offer participants a wide variety of availability including early morning and early evening.
At the final session we make sure there is a smooth transition and hand-off by re-iterating where the study participants can find additional resources once the intervention is over. This includes making sure they have contact information for their VA primary care provider, social worker, and the VA Caregiver Support Line. We also remind them about the online availability of the entire RESCUE website and we give participants in the usual care group the address for the RESCUE en Español website.
Participants who are unable to be contacted or unable to adhere to the intervention schedule are administratively withdrawn. Participants whose care recipient dies or are institutionalized are withdrawn. If the subject experiences worsening or severe stress or burden that prevents them from fully participating in the study, we re-assess their current situation and if it is determined to be in their best interest, they are withdrawn.
The primary outcome is caregiver’s depressive symptoms. Secondary caregiver outcomes are stroke caregivers’ burden, self-efficacy, problem-solving, and health-related quality of life (HRQOL). Secondary stroke survivor outcomes are change in functional abilities. All outcomes are measures three times, pre-intervention (week 1 for participants assigned to the usual care group) and at 1- and 12-weeks post-intervention (9 and 21 weeks after baseline for participants assigned to the usual care group).
Depressive symptoms is assessed using the Center for Epidemiologic Studies Depression [ 37 ] (CES-D 20, Spanish Version) The CES-D is a 20-item, 4-point Likert scale ranging from never (0) to most of the time (3). It assesses depressive symptoms and is not a clinical measure of depression [ 37 ]. The total score of the CES-D 20 is obtained by adding all the items. Scores range from 0–60 with higher scores indicating greater depressive symptoms. If more than 4 items are missing, the CES-D is not scored. This tool has been used in numerous studies with caregivers and has good reliability and validity [ 38 ].
Caregiver burden is assessed using the Zarit Burden Interview (S-ZBI, Spanish Version)[ 39 ]. This is a 22-item instrument with good validity and reliability. The ZBI uses Likert items on a 5-point scale to measure the degree of burden felt by caregivers. Items fall into five categories (health, well-being, finances, social life, relationship with impaired person). The total score of the ZBI is obtained by adding all the items. High scores indicate greater burden. We selected this tool above other burden instruments because it is brief, easy-to-answer, measures both subjective and objective burden, and is a widely-used [ 39 ].
Self-efficacy is assessed using the Caregiver Self-Efficacy (Spanish Version) [ 40 ]. This is a 15-item measure of caregivers’ judgments regarding their ability to perform effectively in specific, caregiving settings. The measure is composed of three domains: obtaining respite, responding to disruptive patient behaviors, and controlling upsetting thoughts. Respondents rate their level of confidence for each item on a scale from 0 to 100, with higher scores corresponding to greater confidence. The item scores within each domain are averaged to obtain subscale ratings ranging between 0 and 100. The tool has established reliability and validity. We selected this self-efficacy tool because it was developed specifically for caregivers and has two subscales that are related to our problem-solving framework.
Problem-solving abilities are assessed using the Social Problem-Solving Inventory Revised—Short Form (SPSI-R:SF) [ 41 ] (Spanish Version). The SPSI-R-SF is a 25-item tool consisting of five subscales (positive problem-solving orientation, rational problem-solving orientation, negative problem-solving orientation, impulsivity or carelessness style problem solving, avoidance style problem solving). Items on the SPSI-R are rated on a 5-point Likert-type scale (0 = not at all true of me to 4 = extremely true of me) with higher scores on each factor indicating greater intensity on a particular dimension. Each subscale is scored individually by summing the items and converting to age-normed scores, and a total standardized score is obtained by reverse-scoring the appropriate subdomains (NPO, ICS, and ACS), summing the subscale scores, and converting to an age-normed total score. Thus, both total score and separate domain scores can be obtained. We chose this tool because it has been used in previous, stroke caregiver studies, it has good psychometric properties, and it is briefer than the original 52-item tool [ 42 ].
Quality of life is assessed using the VR-12 RAND 12-Item Health Survey [ 43 ] (Spanish Version). The VR-12 is a multi-use, health survey comprised of 12 items. The instrument is primarily used to measure health-related quality of life, to estimate disease burden and to evaluate disease-specific benchmarks with other populations. The VR-12 items are scored on a 3-point, 5-point or 6-point Likert scale consisting of two scales: “Physical Health Summary Measure” and “Mental Health Summary” Measure”. Scale scores are obtained by running the scoring algorithm provided by Kazis et al. [ 44 ] The VR-12 has good psychometric properties [ 45 ].
Veterans’ function ability is assessed using the Stroke Impact Scale-16 [ 45 ] (Spanish Version), It is comprised of 16 short questions on a 5-point scale and is used to assess physical function of patients with stroke. Appropriate items are reverse-scored, and the total score is transformed to be on a scale of 0–100, with higher scores corresponding to higher physical function abilities. The scale has good psychometric properties and has been used extensively in studies of outcomes of care in rehabilitation settings [ 46 ]. We screen caregivers by asking them if their stroke survivor needs assistance performing the tasks.
Veterans’ healthcare utilization data (i.e., unintended hospital bed days of care, number of emergency room visits, number of unscheduled clinic visits) during the study period time are obtained by caregivers’ self-report. We record the number, dates, and the reasons for all healthcare visits.
Other measures
For caregivers we use the Problem Checklist [ 47 ], as a screening tool. This instrument developed via consensus by members of the research team with expertise in nursing, psychology, and public health based on published caregiving literature [ 48 , 49 ] and items in the World Health Organization’s (WHO) International Classification of Functioning (ICF) [ 50 ]. This 20-item tool measures common caregiving problems (and stroke survivors’ problems and is only administered during the baseline data collection. Study participants respond “yes” or “no” to indicate whether the problem had occurred in the past month. This tool is used to obtain a better understanding about the challenges participants were experiencing at the beginning of the study. If later during the intervention participants have trouble identifying caregiving related problems, the interventionists use this data to help them generate ideas. We also use the Perceived Stress Scale – PSS10 (Spanish) [ 51 ] as a screening tool for caregiver. This is a 10-item 5-point Likert scale ranging from never (0) to very often (5) used to evaluates level of perceived stress. It is ideal to be used It has been used in numerous studies with caregivers and has good reliability and validity [ 51 ]. Both tools are used stress prior to study enrolment. The Stroke Impact Scale-16, one of the Veterans secondary outcomes, is also used as a screening tool for caregivers prior to enrolment to determine how much assistance stroke survivor needs to perform these tasks.
Budgetary impact. To determine the cost of the intervention itself, we will obtain Veterans’ health care utilization data at the end of the study. We will use the average elapsed time of intervention sessions along with an estimate of the average national wage of the type of interventionist most likely to deliver the intervention in the field. Data on VA-funded use costs will be obtained from Managerial Cost Accounting System (MCAS) and the Non-VA Medical Care files.
Enactment Tool (Translated). We used experienced translators to adapt and translate the Bakas, et al.,[ 52 ] enactment tool. Translations were then verified by native Spanish-speaking members of the research team who met to discuss and finalize the Spanish adaptation. This tool evaluates treatment acceptability and enactment by asking caregivers who complete the intervention to rate the amount of information and contact they received during the 8-sesssion intervention, how much they used the problem-solving strategies and the RESCUE en Español website, how helpful the intervention was and whether their caregiver problems were resolved. It consists of 8 closed-ended questions with a 5-point scale and three open-ended questions for participants to elaborate on what they like best about the intervention and how it can be improved. Participant timeline including enrollment, interventions, and assessments is show in Fig. 2 .
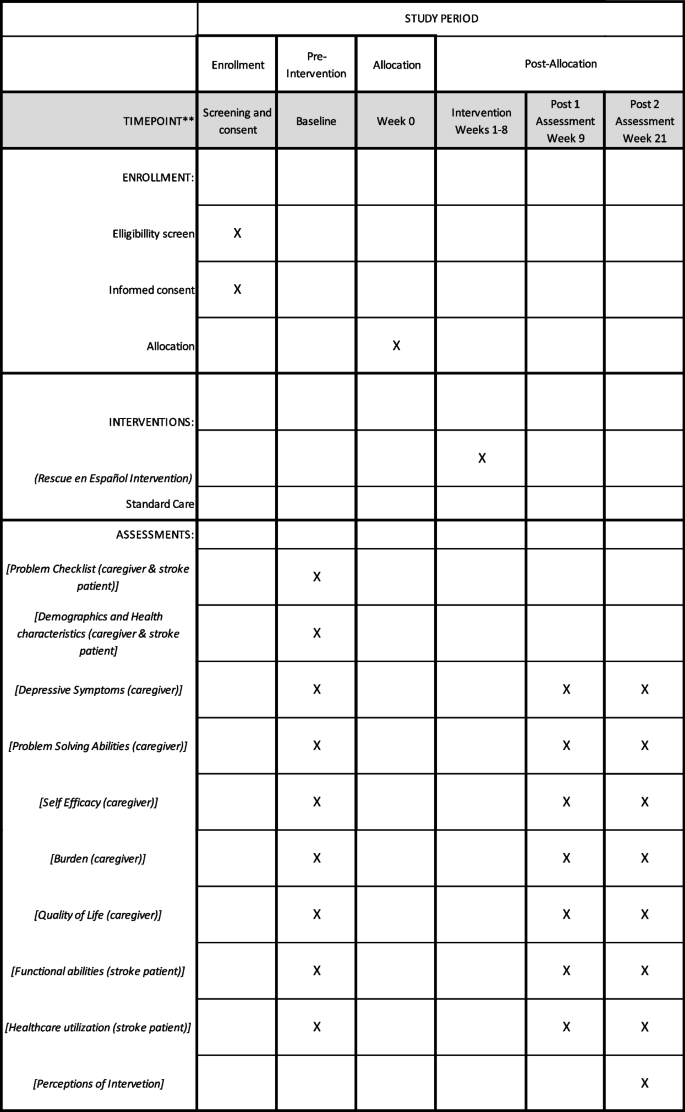
Schedule of enrollment, interventions, and assessments
Sample size
Quantitative methods.
The sample will consist of 290 caregivers. Pilot data from a previous study showed 3.1 points reduction in CES-D with a within group standard deviation of 8.9. Assuming such an intervention effect size on depression, 145 subjects per group would achieve 80% power to detect the difference at a 5% significance level. The sample size of 145 per group (intervention vs. standard care) was selected to account for the occurrence of a 10% dropout rate. The 10% drop-out rate is based on a one of a previous stroke caregivers study conducted by members of the team. The assumed effect size and variability were deemed reasonable based on a number of other sources. Radloff [ 37 ] described large changes pre and post treatment in a clinical setting, with depression from time of admission to 4 weeks post decreasing 20 points for “recovered” patients and 12 points for “still ill” patients. Grant et al. [ 22 ] in a study of a telephone intervention to family caregivers of stroke caregivers, found an estimated 1-month treatment effect of 3.1.
Qualitative methods
Sample size considerations in qualitative studies include the purpose/goal of the study and the depth of data needed to reach theoretical saturation and adequately answer the study question [ 53 ]. Typically, 8–12 participants are needed to reach theoretical sample [ 54 ]. We will select a purposive subsample of 8–12 caregivers who participated in the intervention arm of the project. We will sequentially enroll every sixth caregiver who completes the intervention until we have the desired sample size or theoretical saturation.
Recruitment and enrollment procedures are guided by procedures that have been used successfully to enrol caregivers in our pilot project and other caregiver studies. VACHS recruitment site procedures: We have three methods for identifying potential study participants. 1) Patients List. Each month, we obtain a list of stoke patients with ICD9 codes (430.00—438.99) and/or ICD10 codes (160.0—169.98) from the Health Administration Service (HAS) to review patient EHR to develop a list of potential subjects. We have a full Health Insurance Portability and Accountability Act (HIPAA) Waiver for patient screening and record review to verify diagnosis and identify next of kin. We mail invitation letters explaining the purpose of the study to potential study participants (caregivers of veterans post-stroke) and contact number to call to decline to participate in the study. If we do not receive a response, we contact them in 7–10 days. 2) Clinicians Referrals. Clinicians will inform potential participants about the study and refer them to the study team if interested. 3) Referrals from Another Study. We also receive referrals from a similar study testing a similar English-language version of our intervention if potential participants prefer to receive the intervention in Spanish.
At the James A. Haley Veteran’s Hospital site we use clinician referral recruitment procedures (these recruitment procedures were approved by the University of South Florida IRB (IRB#: Pro00039920) and in the Orlando VAMC, we use patient list and clinician referral in our recruitment procedures (these recruitment procedures were approved by the Orlando VA IRB (Study #1,400,648–1). Recruitment calls to potential participants identified from any of the three sites through the procedures described above are conducted by trained, Spanish speaking study staff in either Gainesville or PR. In addition to explaining study purpose and procedures, during the recruitment phone calls we will screen potential participants for study eligibility. All study procedures will be conducted over the telephone.
Randomization
The study statistician implements the Pocock-Simon covariate adaptive randomization procedure [ 55 ] so that an approximately equal number of caregivers are assigned to the two groups within each covariate level. To conceal the sequence until participants are assigned to the study arm, we use opaque, sealed envelopes. The envelopes are opened by an unblinded member of the study team who conducts the baseline data collection at completion of baseline assessment while participant is on the phone. The data collector notifies participants of their assignment and advises on next steps.
The data collector who conducts all the post-intervention assessments and the study PI will be blinded to the participants’ group assignments. The study database is secured with a two-way accessibility in which study team members who are not blinded have a password to access any information that may reveal participant’s assignment.
Safety considerations
In the event of a safety concern (e.g., abuse, suicidality), the PI will be notified of the situation immediately after the safety concern arises to address the situation and determine participants continuation or need for withdrawal from the trial. In the event a data collector’s blinding was compromised for an individual participant they are not permitted to do future data collections for that participant. This can occur because of the format of the data collections (e.g., participant mentions doing intervention sessions).
Data collection and management
Quantitative data.
All data collectors in the study are experienced data collectors and were trained specifically on the data collection tools used in this study. Baseline data collection is scheduled shortly after informed consent procedures are completed over the telephone at a day and time convenient to the participant. Data collectors record participant responses on paper and then enter them into an online database and data quality checks are conducted and entered by staff. A study member who did not enter or collect the data checks paper data collection forms against database entries to assure that that information is accurate and no data are missing. The two data collectors do not know participants’ group assignment.
Qualitative data
In-depth qualitative interviews are conducted using a semi-structured interview guide consisting of 22 questions developed by the research team for this study. These in-depth interviews about participants’ perception of the intervention address three main topics: feedback about the components of the intervention, the usefulness of the intervention, and the study procedures. Interview questions ranged from asking participants to share their thoughts about the quantity and breadth of the stroke related topics covered during the intervention to what they would change about the intervention and what barriers, if any, they face throughout the study.
Qualitative interviews are conducted by experienced fluent Spanish-speaking interviewers using an interview script over the telephone. Interviewers receive training on the study interview scrip. Interviews are digitally recorded, transcribed verbatim, and validated by another Spanish-speaking member of the research team.
Participants retention
TO promote participant retention and completion of follow-up, we conduct reminder calls before sessions or data collections and have expanded scheduling hours to accommodate participants busy schedules. We do not collect any additional data on participants who withdraw from the study, but we do track reasons for withdrawing.
Confidentiality
We conduct intervention and data collection sessions in a private and secured area. We use encrypted voice recorders to record intervention sessions for fidelity checks and qualitative interviews. The audio sessions are downloaded and stored on a protected, secure VA research server, and then deleted from the portable device. Digital recordings use first names only and any identifying information is be removed during the transcription. All data files are kept in secured spaces and stored on a secure VA serve that has limited access to only study personnel.
Data analysis
The primary analysis is to examine the effect of the intervention on caregiver depression based on “intention to treat.” Data from all the participants will be part of the primary analyses regardless of actual number of completed sessions. As an exploratory study element, we will assess compliance and attempt to determine its effect on study results. For the primary analysis, the general linear mixed model for repeated measures will be used to model the follow-up depression times (1- and 12-weeks post-intervention or 9 and 21 weeks for usual care), adjusted for baseline scores as fixed effects. Let yij be the depression score for person i at time j, then basic fixed effects model will be:
with covariates for baseline depression (Baseline), time (Time = 0 for 1 week, 1 for 12 weeks post-intervention or 9 and 21 weeks for usual care), and group (0 if active control, 1 if intervention). In order to control for possible chance sample imbalances resulting from randomization, the model will include covariates for baseline prognostic factors (e.g., caregivers’ relationship to veteran; number of previous strokes among veterans, location, etc.), deemed to have significant relationships with response and groupwise imbalances. Thus, analyses will be able to compare the groups on the measure of interest while controlling for these factors. The primary outcome of interest will be the immediate post-intervention effect at 1-week postintervention with the 12-week post-intervention as a secondary outcome. This will be tested based on linear contrast β3 + β4 at two-sided 0.05 level. All tests will be performed at the α = 0.05 significance level. The correlation among observations from the same person will be accounted for through the inclusion of a random person effect into the mixed model analysis. Data analysis for the secondary outcomes (i.e., burden, problem solving skills, self-efficacy, and HRQOL) will follow the plan for our primary outcome. No data analysis will take place until all data has been collected.
The analysis to determine the intervention’s budgetary impact consists of two parts: (1) the incremental cost of the intervention itself over and above usual care, and (2) the impact of the intervention on healthcare utilization. Micro-costing techniques [ 56 ] combined with average costing [ 57 ] will be used to determine the average staff time, wage, space, and equipment costs associated with the intervention. The micro-cost estimate for the telephone sessions will use the average elapsed time of such sessions along with an estimate of the average national wage of the type of nurse most likely to deliver the intervention in the field. To determine the intervention’s impact on the costs of healthcare utilization, the team will rely on the Professional Society for Health Economics and Outcomes Research ISPOR 2014 budgetary impact analysis guidelines [ 58 ]. Data on VA-funded utilization costs will be obtained from Managerial Cost Accounting System (MCAS) and the Non-VA Medical Care files. The team will tabulate all costs from these sources for study enrollees throughout the study, calculate the difference between intervention and usual care average costs, and test for the statistical significance of this difference using the Z-score method proposed by Zhou [ 59 ]. The final step in determining the budgetary impact of the intervention will combine parts 1 and 2 to determine the complete impact of the intervention on the VA budget.
The qualitative data analysis will consist semi-structure interviews to investigate the caregivers’ perceptions of barriers and facilitators and the acceptability of the intervention. We will invite every 6th study participant assigned to the intervention who completes the study to participate in a semi-structured interview. Once all the interviews have been conducted, study team members will begin the analysis by reading the first two caregiver transcripts and use template analysis to organize and analyse qualitative data using a priori themes based on the qualitative interview guide [ 60 ]. We will apply this framework to the first two interviews and add or revise themes as needed. Team members will independently code each transcript and l and meet to discuss coding decisions and resolve discrepancies. Data analysts will meet regularly with other team members to discuss the findings and search for alternative explanations in the data continuing this iterative process until no new themes are identified. To ensure rigor we keep an audit trail containing a log of all decisions and changes, along with the reason for the decision or change. Data will be analysed using NVIVO (QSR International) software.
Quantitative data obtained from the Enactment Tool (Bakas) [ 52 ] in which the caregiver rates aspects of the intervention, combined with qualitative data, will help us understand which aspects of the website and intervention were most beneficial and how the perceptions about the strengths and weaknesses of the various parts of the intervention varied between caregivers with different depression levels. We will use simple descriptive statistics to analyse quantitative data and thematic analysis for the qualitative data. Findings will provide data to help refine methods for future testing and roll-outs.
The measures for problem-solving and quality of life have methods for imputing missing scores on individual items. In the event of participant withdrawals, the missingness mechanism will be explored. If the assumption of Missing Completely at Random (MCAR) or the common assumption of Missing at Random (MAR) are plausible, then little change to the analysis plan is necessary. The mixed models analysis using direct-likelihood approaches will be unbiased and appropriate. Mixed effects modeling requires large samples but does not require full data on each subject.
Study efficiency (power) will of course be affected by the smaller amount of available information, thus we have inflated the planned recruitment sample size [ 61 , 62 ]. It is important to note however, that it is rarely the case for missing data to be truly and purely MCAR; missingness may be multifaceted and portions of data may be missing at random vs missing systematically, in a way related to outcome of interest. Thus, even if missingness and attrition is not completely random (i.e., the cause of missingness or dropout is not related to the outcome of interest), missing data handling techniques will still be valuable, and we will employ one of a few options available. We may choose to use either multiple imputation (MI) or full-information maximum likelihood (FIML) estimation with the mixed effects regression models proposed. If there is a portion of missingness that is missing not at random, then parameter estimates may still be biased and should interpreted cautiously, but power will be less affected. Ultimately, even if there are data missing not entirely at random, these techniques are better alternatives than the default of listwise deletion of participants with missing data (which would introduce both bias and loss of power).
Stroke caregiving has been associated with higher rates of caregiver burden and depression [ 7 8 ]. Because majority of stroke survivors return home after a stroke, family members take on the roles of caregiver, oftentimes with little knowledge or skills to handle the sequalae of stroke survivors and the negative toll on their own physical and mental health. Thus, it is imperative to provide stroke caregivers with resources in order to adequately prepare them for their caregiver role and help alleviate the negative impact of caregiving.
The RESCUE intervention offers an alternative to traditional face to face interventions and if found to be successful, easily implemented in clinical setting. The ability to receive the intervention over the telephone minimizes caregiver burden and requires less healthcare system resources compared to in-person interventions. It is also especially relevant to the Hispanic population’s preferences for more direct contact with healthcare providers [ 63 ].
This is the first study that uses a culturally-adapted intervention specifically for Hispanic stroke caregiver. Unlike most intervention studies, this study includes an evaluation of the budgetary impact of the intervention and an advisory panel to collaborate throughout all the study phases and guide future plans for wider implementation. Once the study is completed, findings will be disseminated via professional publications and conferences, and reports to sponsor agency and programs. We will collaborate with stakeholders and members of our Advisory Panel to find additional venues for disseminating findings.
We have experienced some operational issues with this study. Lower recruitment than expected, due to natural disasters affecting our target population and negatively impacting the communication infrastructure in Puerto Rico, led to a revision in study procedures to add additional recruitment sites where many Puerto Ricans migrated to after these natural events. Issues with broad-band and telecommunications have also negatively impacted our ability to reach study participants in a timely manner.
This study addresses an important and understudied area of caregiving research, Hispanic, Spanish-speaking caregivers of veterans who have suffered a stroke. This is the first known to evaluate a telephone and online problem-solving intervention combined with the nationally available Spanish- language, evidence-based RESCUE website. The intervention has the potential to reduce stroke caregiver depression, improve the recovery of veterans post-stroke, enable veterans to remain in their homes, and reduce healthcare costs. Another outcome will be a state-of-the art, nationally available culturally relevant website that both, family caregivers and health care providers can use for patient and caregiver education.
This trial is ongoing and is using protocol version #8 dated 08. 011.2022. Recruitment procedures started March 2018 and are expected to end in March 2023.
Availability of data and materials
Currently, only investigators associated with this study will have access to the final dataset. Final de-identified will be disclosed upon request per VA rules and regulations. Dissemination of findings and final study data will be available without restriction, in accordance with VHA directive 1200.19.
Abbreviations
Activity of daily living
Center for Epidemiologic Studies Depression
Creativity, Optimism, Planning, and Expert Information
Electronic Health Record
Full-information maximum likelihood
Health Administration Service
Health Related Quality of life
International Classification of Disease
International Classification of Functioning
Professional Society for Health Economics and Outcomes Research (formerly known as the International Society for Pharmaeconomics and Outcomes Research)
Institutional Review Board
Missing at Random
Missing Completely at Random
Managerial Cost Accounting System
Medical Doctor
Multiple Imputation
North Florida/ South Georgia Veterans Healthcare System
Principal Investigator
Patient Satisfaction Questionnaire
Perceived Stress Scale
Post-Traumatic stress disorder
Research and Development
Resources and Education for Stroke Caregivers’ Understanding and Empowerment
Stroke Impact Scale
Social Problem-Solving Inventory Revised – Short Form
Short Version of Zarit Burden Interview
United States
Department of Veteran Affairs
Veteran Affairs Caribbean Healthcare System
World Health Organization
Gutierrez J, Williams OA. A decade of racial and ethnic stroke disparities in the United States. Neurol. 2014;82(12):1080–2. https://doi.org/10.1212/WNL.0000000000000237 .
Article Google Scholar
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38-60. https://doi.org/10.1161/CIR.0000000000000350 .
Article PubMed Google Scholar
Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, Criqui MH, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–84. https://doi.org/10.1001/jama.2012.14517 .
Article CAS PubMed PubMed Central Google Scholar
Mozaffarian D, Benjamin EJ, Go AS, Arnett D, Blaha M, Cushman M, et al. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29-322. https://doi.org/10.1161/CIR.000000000000015 .
Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, et al. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(7):2091–116. https://doi.org/10.1161/STR.0b013e3182213e24 .
Dewey HM, Thrift AG, Mihalopoulos C, Carter R, Macdonell RA, McNeil JJ, et al. Informal care for stroke survivors: results from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke. 2002;33(4):1028–33. https://doi.org/10.1161/01.str.0000013067.24300.b0 .
Article CAS PubMed Google Scholar
Haley WE, Roth DL, Hovater M, Clay OJ. Long-term impact of stroke on family caregiver well-being: a population-based case-control study. Neurol. 2015;84(13):1323–9. https://doi.org/10.1212/WNL.0000000000001418 .
Berg A, Palomäki H, Lönnqvist J, Lehtihalmes M, Kaste M. Depression among caregivers of stroke survivors. Stroke. 2005;36(3):639–43. https://doi.org/10.1161/01.STR.0000155690.04697.c0 .
McCullagh E, Brigstocke G, Donaldson N, Kalra L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke. 2005;36(10):2181–6. https://doi.org/10.1161/01.STR.0000181755.23914.53 .
Camak DJ. Addressing the burden of stroke caregivers: a literature review. J Clin Nurs. 2015;24(17–18):2376–82. https://doi.org/10.1111/jocn.12884 .
Miller EL, Murray L, Richards L, Zorowitz RD, Bakas T, Clark P, et al. Comprehensive overview of nursing and interdisciplinary rehabilitation care of the stroke patient: a scientific statement from the American Heart Association. Stroke. 2010;41(10):2402–48. https://doi.org/10.1161/STR.0b013e3181e7512b .
Management of Stroke Rehabilitation Work Group. This is a guideline providing recommendations on the assessment, treatment, and follow-up of stroke in the Department of Veteran Affairs (VA) and Department of Defense (DoD). Washington, D.C.: Department of Defense, Department of Veterans Affairs; 2019. p. 1–170. Available from: https://www.healthquality.va.gov/guidelines/Rehab/stroke/VADoDStrokeRehabCPGFinal8292019.pdf .
Hoffmann T, Russell T, McKenna K. Producing computer-generated tailored written information for stroke patients and their carers: system development and preliminary evaluation. Int J Med Inform. 2004;73(11–12):751–8. https://doi.org/10.1016/j.ijmedinf.2004.07.001 .
Lui MH, Ross FM, Thompson DR. Supporting family caregivers in stroke care: a review of the evidence for problem solving. Stroke. 2005;36(11):2514–22. https://doi.org/10.1161/01.STR.0000185743.41231.85 .
Demiris G, Parker Oliver D, Washington K, Fruehling LT, Haggarty-Robbins D, Doorenbos A, et al. A problem solving intervention for hospice caregivers: a pilot study. J Palliat Med. 2010;13(8):1005–11. https://doi.org/10.1089/jpm.2010.0022 .
Article PubMed PubMed Central Google Scholar
Elliott TR, Brossart D, Berry JW, Fine PR. Problem-solving training via videoconferencing for family caregivers of persons with spinal cord injuries: A randomized controlled trial. Behav Res Ther. 2008;46(11):1220–9. https://doi.org/10.1016/j.brat.2008.08.004 .
Kurylo MF, Elliott TR, Shewchuk RM. FOCUS on the family caregiver: A problem-solving training intervention. J Couns Dev. 2001;79(3):275–81. https://doi.org/10.1002/j.1556-6676.2001.tb01972.x .
Rivera PA, Elliott TR, Berry JW, Grant JS. Problem-solving training for family caregivers of persons with traumatic brain injuries: a randomized controlled trial. Arch Phys Med Rehabil. 2008;89(5):931–41. https://doi.org/10.1016/j.apmr.2007.12.032 .
Forster A, Brown L, Smith J, House A, Knapp P, Wright J, et al. Information provision for stroke patients and their caregivers. Cochrane Database Syst Rev. 2012;11(11):CD001919. https://doi.org/10.1002/14651858.CD001919.PUB3 .
Sorensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? An updated meta-analysis. Gerontol. 2002;42(3):356–72. https://doi.org/10.1093/geront/42.3.356 .
Bakas T, Clark PC, Kelly-Hayes M, King RB, Lutz BJ, Miller EL. Evidence for stroke family caregiver and dyad interventions: a statement for healthcare professionals from the American Heart Association and American Stroke Association. Stroke. 2014;45(9):2836–52. https://doi.org/10.1161/STR.0000000000000033 .
Grant JS, Elliott TR, Weaver M, Bartolucci AA, Giger JN. Telephone intervention with family caregivers of stroke survivors after rehabilitation. Stroke. 2002;33(8):2060–5. https://doi.org/10.1161/01.str.0000020711.38824.e3 .
Zickuhr K, Smith A. Digital differences [Internet]. Washington, D.C.: Pew Research Center’s Internet & American Life Project; 2012. Available from: https://www.pewinternet.org/wp/content/uploads/sites/9/media/Files/Reports/2012/PIP_Digital_differences_041312.pdf .
Computer and Internet Use in the United States: 2013 [Internet] Washington, D.C.: American Community Survey Reports, ACS-28, U.S. Census Bureau; 2014. Available from: http://www.census.gov/history/pdf/2013computeruse.pdf .
“Digital Divide Is Shrinking for America’s Hispanic Population, NTIA Data Show | National Telecommunications and Information Administration,” n.d. https://www.ntia.doc.gov/blog/2019/digital-divide-shrinking-america-s-hispanic-population-ntia-data-show .
Uphold CR, Jordan M, Freytes M. Chapter 8 family caregivers of veterans: a critical review of the empirical literature and recommendations for future research. Annu Rev Nurs Res. 2014;32:155–202. https://doi.org/10.1891/0739-6686.32.155 .
National Alliance for Caregiving and AARP. Caregiving in the U.S . 2004, Washington D.C.: National Alliance for Caregiving and AARP.
Gelman CR. Familismo and its impact on the family caregiving of Latinos with Alzheimer's disease: a complex narrative. Res Aging. 2014;36(1):40–71. https://doi.org/10.1177/0164027512469213 .
Hinojosa MS, Rittman MR. Stroke caregiver information needs: comparison of mainland and Puerto Rican caregivers. J rehabil res dev. 2007;44(5):649–58. https://doi.org/10.1682/jrrd.2006.10.0131 .
Hinojosa MS, Rittman M, Hinojosa R, Rodriguez W. Racial/ethnic variation in recovery of motor function in stroke survivors: role of informal caregivers. J Rehabil Res Dev. 2009;46(2):223–32.
Perrin PB, Heesacker M, Hinojosa MS, Uthe CE, Rittman MR. Identifying at-risk, ethnically diverse stroke caregivers for counseling: A longitudinal study of mental health. Rehabil Psychol. 2009;54(2):138–49. https://doi.org/10.1037/a0015964 .
Perrin PB, Johnston A, Bsot MV. A culturally sensitive Transition Assistance Program for stroke caregivers: examining caregiver mental health and stroke rehabilitation. J Rehabil Res Dev. 2010;47(7):605–17. https://doi.org/10.1682/jrrd.2009.10.0170 .
D'Zurilla T, Nezu A. Problem-solving therapy. New York, NY: Springer Pub.; 1999.
Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer publishing company; 1984.
Houts PS, Nezu AM, Nezu CM, Bucher JA. The prepared family caregiver: a problem-solving approach to family caregiver education. Patient Educ Couns. 1996;27(1):63–73. https://doi.org/10.1016/0738-3991(95)00790-3 .
Hecht J, Borrelli B, Breger RK, Defrancesco C, Ernst D, Resnicow K. Motivational interviewing in community-based research: experiences from the field. Ann Behav Med. 2005;29 Suppl:29-34. https://doi.org/10.1207/s15324796abm2902s_6 .
Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl psychol meas. 1977;1(3):385–401. https://doi.org/10.1177/014662167700100306 .
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med. 1994;10(2):77–84.
Martin-Carrasco M, Otermin P, Pérez-Camo V, Pujol J, Agüera L, Martín MJ, et al. EDUCA study: Psychometric properties of the Spanish version of the Zarit caregiver burden scale. Aging ment health. 2010;14(6):705–11.
Márquez-González M, Losada A, López J, Peñacoba C. Reliability and validity of the Spanish version of the revised scale for caregiving self-efficacy. Clin gerontol. 2009;32(4):347–57. https://doi.org/10.1080/07317110903110419 .
D'Zurilla TJ, Nezu AM, Maydeu-Olivares A. Social problem-solving inventory--revised (SPSI-R). Multi-Health Systems; 2002.
Cameron JI, Shin JL, Williams D, Stewart DE. A brief problem-solving intervention for family caregivers to individuals with advanced cancer. J Psychosom Res. 2004;57(2):137–43. https://doi.org/10.1016/s0022-3999(03)00609-3 .
Selim AJ, Rogers W, Fleishman JA, Qian SX, Fincke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-item Health Survey (VR-12). Qual Life Res. 2009;18(1):43–52. https://doi.org/10.1007/s11136-008-9418-2 .
Kazis LE, Nethercot VA, Ren XS, Lee A, Selim A, Miller DR. Medication effectiveness studies in the United States Veterans Administration health care system: a model for large integrated delivery systems. Drug dev res. 2006;67(3):217–26. https://doi.org/10.1002/ddr.20080 .
Article CAS Google Scholar
Duncan PW, Lai SM, Bode RK, Perera S, DeRosa J. GAIN Americas Investigators. Stroke Impact Scale-16. A brief assessment of physical function. Neurol. 2003;60(2):291–6. https://doi.org/10.1212/01.wnl.0000041493.65665.d6 .
Aguado BP. Contribución de la adaptación y validación de la escala sis-16 (stroke impact scale) en el manejo de la rehabilitación de pacientes con ictus. Servicio de Publicaciones: Universidad Complutense de Madrid; 2010.
Google Scholar
Freytes IM, Sullivan M, Schmitzberger M, LeLaurin J, Orozco T, Eliazar-Macke N, et al. Types of stroke-related deficits and their impact on family caregiver’s depressive symptoms, burden, and quality of life. Disabil health j. 2020;14(2):101019. https://doi.org/10.1016/j.dhjo.2020.101019 .
Vanhook P. The domains of stroke recovery: a synopsis of the literature. J neurosci nurs. 2009;41(1):6–17. https://doi.org/10.1097/jnn.0b013e31819345e4 .
Hillis AE, Tippett DC. Stroke recovery Surprising influences and residual consequences. Adv Med. 2014;2014:378263. https://doi.org/10.1155/2014/378263 .
Who.int. 2021 [cited 9 April 2021]. Available from: https://www.who.int/classifications/icf/icfbeginnersguide.pdf
Patton MQ. Qualitative evaluation and research methods. SAGE Publications, inc; 1990.
Bakas T, Farran CJ, Austin JK, Given BA, Johnson EA, Williams LS. Stroke caregiver outcomes from the telephone assessment and skill-building kit (TASK). Top Stroke Rehabil. 2009;16(2):105–21. https://doi.org/10.1310/tsr1602-105 .
Creswell JW, Fetters MD, Ivankova NV. Designing a mixed methods study in primary care. Ann Fam Med. 2004;2(1):7–12. https://doi.org/10.1370/afm.104 .
Zagoraiou M. Choosing a covariate-adaptive randomization procedure in practice. J Biopharm Stat. 2017;27(5):845–57. https://doi.org/10.1080/10543406.2017.1289944 .
Remor E. Psychometric properties of a European Spanish version of the perceived stress scale (PSS). Span J Psychol. 2006;9(1):86–93. https://doi.org/10.1017/s1138741600006004 .
Smith MW, Barnett PG, Phibbs CS, Wagner TH. Microcost methods for determining VA healthcare costs. Menlow Park, CA: Health Economics Resource Center, 2010.
Smith MW, Barnett PG. Direct measurement of health care costs. Med Care Res Rev. 2003;60(3 Suppl):74S–91S. https://doi.org/10.1177/1077558703257001 .
Sullivan SD, Mauskopf JA, Augustovski F, Caro JJ, Lee KM, Minchin M, Orlewska E, Penna P, Barrios JM, Shau WY. Budget impact analysis—principles of good practice: report of the ISPOR 2012 budget impact analysis good practice II task force. Value health. 2014;17(1):5–14. https://doi.org/10.1016/j.jval.2013.08.2291 .
Zhou XH, Melfi CA, Hui SL. Methods for comparison of cost data. Ann Intern Med. 1997;127(8 Part 2):752–6. https://doi.org/10.7326/0003-4819-127-8_part_2-199710151-00063 .
J Brooks N King 2014 Doing template analysis: evaluating an end of life care service Sage Res Methods Cases https://doi.org/10.4135/978144627305013512755 .
Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. London: Oxford University Press; 2003.
Book Google Scholar
Tabachnick BG, Fidell LS. Using multivariate statistics, Vol. 5th ed. Boston: Pearson/Allyn & Bacon; 2007.
Quality Health Services for Hispanics: The Cultural Competency Component. 2000. Department of Health and Human Services. Washington, D.C. 2001. Available from: https://www.hrsa.gov/sites/default/files/culturalcompetence/servicesforhispanics.pdf .
Download references
Acknowledgements
We would like to acknowledge the contributions of Melanie Orejuela, Daniella Mylott, Casey Bopp, Kimberly Findley, Jason Rogers, Adam Golden, MD; Linda Cowan, PhD; Angelina S. Klanchar, Jorge Martinez-Martino, Lisette Jimenez-Rodriguez, Bruce Vogel, and Xinping Wang to this project.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of VA or the United States government.
VA Office of Research and Development, Health Services Research & Development; IIR 15–117.
Funding agency cover all costs associated with this trial including all meetings, organizational and operational costs of the study, study personnel, analysis and reporting of study findings throughout the duration of the study.
This is an investigator initiated clinical trial. Therefore, the funders played no role in the design of the study and collection, analysis, and interpretation of data and writing of this manuscript.
Author information
Authors and affiliations.
Research Service, North Florida/South Georgia Veterans Health System, 1601 SW Archer Rd #151B, Gainesville, FL, 32608, USA
I. Magaly Freytes, Magda K. Schmitzberger, Janet Lopez, Tatiana Orozco, Jennifer Hale-Gallardo, Nathaniel Eliazar-Macke & Jennifer H. LeLaurin
Geriatric Research Education and Clinical Center, North Florida/South Georgia Veterans Health System, 1601 SW Archer Rd #151B, Gainesville, FL, 32608, USA
I. Magaly Freytes & Constance R. Uphold
Research Service, VA Caribbean Healthcare System, 10 Casia St, San Juan, PR, 00921, USA
Naiomi Rivera-Rivera
Physical Medicine and Rehabilitation Service, VA Caribbean Healthcare System, 10 Casia St, San Juan, PR, 00921, USA
Keryl Motta-Valencia
College of Medicine, Department of Biostatistics, University of Florida, CTRB Room 5243, 2004 Mowry Road, Gainesville, FL, 32610, USA
Samuel S. Wu
College of Medicine, Department of Aging and Geriatric Research, University of Florida, 2004 Mowry Rd, Gainesville, FL, 32603, USA
Constance R. Uphold
You can also search for this author in PubMed Google Scholar
Contributions
IMF & CRU developed the study protocol; IMF and MKS wrote the initial draft of the manuscript. NR-R created tables and figures and revised the manuscript. JL, JH-G, KM-V and CRU helped write and revise manuscript. SW and TO wrote and revised quantitative data analysis plan. NE-M revised manuscript and updated citations. JHL revised introduction section, verified SPIRIT guidelines compliance, and revised manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to I. Magaly Freytes .
Ethics declarations
Ethics approval and consent to participate.
Approvals were obtained from the IRB affiliated with each participating site and the local VA Rehabilitation and Development committees: the University of Florida Institutional Review Board and the North Florida/South Georgia Veterans Health Systems, Research & Development Committee in Gainesville, FL.; the VA Caribbean Healthcare System’s Institutional Review Board and the VA Caribbean Healthcare System’s Research & Development Committee in San Juan, PR; the Orlando VA Medical Center’s Institutional Review Board and the Orlando VA Medical Center’s Research & Development Committee in Orlando, FL.; the University of South Florida, Research Integrity & Compliance, Institutional Review Board and the James A Haley Veterans' Hospital, Research & Development Committee in Tampa, FL. The protocol is registered in clinicaltrials.gov (NCT03142841).
Tracking and reporting of unanticipated or adverse events is done following IRB guidelines and both are tracked and, logged in a tracking form and reported on yearly review, unless it is an adverse event involving harm to participants which are reported within 24 h of occurrence to the IRB and research compliance officer.
This study is audited. Triennial regulatory compliance audits and research safety audits are conducted independently, (one per site) once every three years by the VA medical centers’ compliance officers in Gainesville, Fl., and San Juan, PR who are independent from the funding agency. Audit procedures involve reviewing that informed consent documentation waiver criteria is documented on IRB records and verifying whether continuing review requirements are completed as required. The main study PI conducts yearly visits to all the study sites to ensure proper study procedures are properly followed.
All major modifications to the research plan have been submitted for approval from the funding agency. Once approved, modifications are submitted to the IRB and the VA local R&D for approval. No changes are implemented before approvals are obtained unless there is harm to study participants.
While we obtained a Waiver Documentation of Informed Consent, members of the research team trained in informed consent procedures utilize an Informed Consent Written Statement to inform interested and eligible participants about the purpose of the study, study procedures including that some sessions may be recorded, risks, volunteer nature of their participation, potential benefits, and who to contact in case of questions or concerns, etc. The written statement is also used to inform and obtain oral permission to record the interventions. A copy of the written statement is mailed to participants prior to reviewing the Informed Consent Written Statement. All informed consent procedures are conducted over the telephone by trained and experienced members of the research team from either the NF/SG VHS or the VACHS. To collect veteran healthcare utilization data, we ask caregivers to self-report.
Consent for publication
Competing interests.
The authors have no conflicts of interest to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Freytes, I.M., Schmitzberger, M.K., Rivera-Rivera, N. et al. Study protocol of a telephone problem-solving intervention for Spanish-speaking caregivers of veterans post-stroke: an 8-session investigator-blinded, two-arm parallel (intervention vs usual care), randomized clinical trial. BMC Prim. Care 24 , 73 (2023). https://doi.org/10.1186/s12875-022-01929-y
Download citation
Received : 19 October 2022
Accepted : 25 November 2022
Published : 17 March 2023
DOI : https://doi.org/10.1186/s12875-022-01929-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hispanic Americans
- Caregiver Burden
- Stroke Caregiving
- Problem-solving
- Culturally-relevant Intervention
- Health Education
- Quality of Life
- Minority Health
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
- Help & FAQ
A Problem-Solving Intervention for Hospice Family Caregivers: A Randomized Clinical Trial
- Institute of Clinical and Translational Sciences (ICTS)
- Siteman Cancer Center
- Division of Palliative Medicine
Research output : Contribution to journal › Article › peer-review
OBJECTIVES: Family caregivers of hospice patients have multiple needs as they try to cope during a stressful time. Translatable interventions effective in improving caregiver outcomes are greatly needed. Our objective was to assess the impact of a problem-solving intervention (called Problem-Solving Intervention to Support Caregivers in End-of-Life Care Settings [PISCES]) to support hospice caregivers on caregiver quality of life and anxiety, and compare its effectiveness delivered face to face and via videoconferencing. DESIGN: In this 4-year randomized clinical trial, caregivers were randomly assigned to a group receiving standard care with added “friendly calls” (attention control [AC] group), a group receiving standard care and PISCES delivered face to face (F2F), or a group receiving standard care and PISCES delivered via videoconferencing (VC). SETTING: Home hospice. PARTICIPANTS: A total of 514 caregivers participated (172 in AC, 171 in F2F, and 171 in VC). Caregivers were predominantly female (75%); mean age was 60.3 years. INTERVENTION: PISCES includes a structured curriculum delivered in three sessions and motivates caregivers to adopt a positive attitude, define problems by obtaining facts, set goals, and generate and evaluate solutions. MEASUREMENTS: Quality of life was measured by the Caregiver Quality of Life Index-Revised; anxiety was measured by the Generalized Anxiety Disorder 7-Item. Other measures included the Caregiver Reaction Assessment scale, demographic data, and an exit interview. RESULTS: Compared with AC, caregivers in the F2F condition had postintervention reduced anxiety (−1.31 [95% confidence interval [CI] = −2.11 to.50]; p =.004) and improved social (.57 [95% CI =.19-.95]; p =.01), financial (.57 [95% CI =.21-.93]; p =.004), and physical quality of life (.53 [95% CI =.19-.87]; p =.01). There were no differences in caregivers in the VC condition compared with the AC condition. CONCLUSION: The PISCES intervention improves caregiver outcomes and is effective when delivered in person. How to integrate technology to reduce the intervention delivery cost warrants further investigation.
- Problem-Solving Therapy
Access to Document
- 10.1111/jgs.15894
Other files and links
- Link to publication in Scopus
Fingerprint
- Hospices Medicine & Life Sciences 100%
- Caregivers Medicine & Life Sciences 69%
- Randomized Controlled Trials Medicine & Life Sciences 54%
- Videoconferencing Medicine & Life Sciences 33%
- Quality of Life Medicine & Life Sciences 14%
- Confidence Intervals Medicine & Life Sciences 13%
- Anxiety Medicine & Life Sciences 12%
- Terminal Care Medicine & Life Sciences 6%
T1 - A Problem-Solving Intervention for Hospice Family Caregivers
T2 - A Randomized Clinical Trial
AU - Demiris, George
AU - Oliver, Debra Parker
AU - Washington, Karla
AU - Pike, Kenneth
N1 - Publisher Copyright: © 2019 The American Geriatrics Society
N2 - OBJECTIVES: Family caregivers of hospice patients have multiple needs as they try to cope during a stressful time. Translatable interventions effective in improving caregiver outcomes are greatly needed. Our objective was to assess the impact of a problem-solving intervention (called Problem-Solving Intervention to Support Caregivers in End-of-Life Care Settings [PISCES]) to support hospice caregivers on caregiver quality of life and anxiety, and compare its effectiveness delivered face to face and via videoconferencing. DESIGN: In this 4-year randomized clinical trial, caregivers were randomly assigned to a group receiving standard care with added “friendly calls” (attention control [AC] group), a group receiving standard care and PISCES delivered face to face (F2F), or a group receiving standard care and PISCES delivered via videoconferencing (VC). SETTING: Home hospice. PARTICIPANTS: A total of 514 caregivers participated (172 in AC, 171 in F2F, and 171 in VC). Caregivers were predominantly female (75%); mean age was 60.3 years. INTERVENTION: PISCES includes a structured curriculum delivered in three sessions and motivates caregivers to adopt a positive attitude, define problems by obtaining facts, set goals, and generate and evaluate solutions. MEASUREMENTS: Quality of life was measured by the Caregiver Quality of Life Index-Revised; anxiety was measured by the Generalized Anxiety Disorder 7-Item. Other measures included the Caregiver Reaction Assessment scale, demographic data, and an exit interview. RESULTS: Compared with AC, caregivers in the F2F condition had postintervention reduced anxiety (−1.31 [95% confidence interval [CI] = −2.11 to.50]; p =.004) and improved social (.57 [95% CI =.19-.95]; p =.01), financial (.57 [95% CI =.21-.93]; p =.004), and physical quality of life (.53 [95% CI =.19-.87]; p =.01). There were no differences in caregivers in the VC condition compared with the AC condition. CONCLUSION: The PISCES intervention improves caregiver outcomes and is effective when delivered in person. How to integrate technology to reduce the intervention delivery cost warrants further investigation.
AB - OBJECTIVES: Family caregivers of hospice patients have multiple needs as they try to cope during a stressful time. Translatable interventions effective in improving caregiver outcomes are greatly needed. Our objective was to assess the impact of a problem-solving intervention (called Problem-Solving Intervention to Support Caregivers in End-of-Life Care Settings [PISCES]) to support hospice caregivers on caregiver quality of life and anxiety, and compare its effectiveness delivered face to face and via videoconferencing. DESIGN: In this 4-year randomized clinical trial, caregivers were randomly assigned to a group receiving standard care with added “friendly calls” (attention control [AC] group), a group receiving standard care and PISCES delivered face to face (F2F), or a group receiving standard care and PISCES delivered via videoconferencing (VC). SETTING: Home hospice. PARTICIPANTS: A total of 514 caregivers participated (172 in AC, 171 in F2F, and 171 in VC). Caregivers were predominantly female (75%); mean age was 60.3 years. INTERVENTION: PISCES includes a structured curriculum delivered in three sessions and motivates caregivers to adopt a positive attitude, define problems by obtaining facts, set goals, and generate and evaluate solutions. MEASUREMENTS: Quality of life was measured by the Caregiver Quality of Life Index-Revised; anxiety was measured by the Generalized Anxiety Disorder 7-Item. Other measures included the Caregiver Reaction Assessment scale, demographic data, and an exit interview. RESULTS: Compared with AC, caregivers in the F2F condition had postintervention reduced anxiety (−1.31 [95% confidence interval [CI] = −2.11 to.50]; p =.004) and improved social (.57 [95% CI =.19-.95]; p =.01), financial (.57 [95% CI =.21-.93]; p =.004), and physical quality of life (.53 [95% CI =.19-.87]; p =.01). There were no differences in caregivers in the VC condition compared with the AC condition. CONCLUSION: The PISCES intervention improves caregiver outcomes and is effective when delivered in person. How to integrate technology to reduce the intervention delivery cost warrants further investigation.
KW - Problem-Solving Therapy
KW - caregiving
KW - hospice
UR - http://www.scopus.com/inward/record.url?scp=85063882651&partnerID=8YFLogxK
U2 - 10.1111/jgs.15894
DO - 10.1111/jgs.15894
M3 - Article
C2 - 30946495
AN - SCOPUS:85063882651
SN - 0002-8614
JO - Journal of the American Geriatrics Society
JF - Journal of the American Geriatrics Society
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 29, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Study: CARES intervention reduces stress for family caregivers of older adults with dementia
by George Mason University

According to the U.S. Centers for Disease Control and Prevention , 80% of those living with dementia receive informal care from family members or friends. This equates to 16 million family caregivers in the U.S. However, caring for family members with dementia is often associated with increased caregiver burden (which includes emotional, physical, and financial strain), stress, and worse physical health for the caregiver.
A recent study published in the Journal of Applied Gerontology , led by George Mason University researchers, found that a 9-week online stress management intervention program for family caregivers reduced burden scores by 15% for 97 family caregivers of older adults living with dementia . The Stress-Busting Program for Family Caregivers TM, intervention was specifically designed to help family caregivers with managing their own stress when caring for older adults living with dementia or a chronic illness
"In this study, we found evidence of a range in average caregiver burden levels based on the dementia severity category of care recipients. The findings show that an online Zoom intervention in a peer group setting can be beneficial for family caregivers of older adults with mild, moderate, or severe dementia," said Catherine Tompkins, principal investigator, professor of social work, and associate dean of faculty and staff affairs in the College of Public Health.
The intervention provided family caregivers with education and strategies to manage stress when caring for someone living with dementia. Examples of self-care techniques included breathing and meditation; troubleshooting behaviors associated with dementia; and peer-to- peer support within a virtual group setting.
"Reducing caregiver burden and managing stress are critical to the well-being of families. These findings show that effective stress management interventions for family caregivers can be facilitated through online peer groups," said Gilbert Gimm, first author and associate professor of health administration and policy.
Co-authors include George Mason Associate Professor Megumi Inoue, Professor Emily Ihara, Mason CARES Project Manager Shannon Layman, and Master of Social Work alumna graduate Harveen Pantleay. This study was supported by a grant (#2021048) from the Retirement Research Foundation (RRF).
The study is part of a larger project, entitled Mason CARES (Caregivers Aiming for Resilience, Empowerment, and Support), that implemented and assessed interventions for family caregivers.
Explore further
Feedback to editors

Pharma firm urged to share new 'game-changer' HIV drug
14 minutes ago

Improving cell therapy by creating T-cell 'super soldiers'
12 hours ago

Study shows more than just social media use may be causing depression in young adults

More out-of-state patients seek abortions in Washington state


Researchers develop microneedle patch that can detect skin cancer early

Blood flow makes waves across the surface of the mouse brain

Study finds that memory complaints can predict biological changes in the brain

Research team creates mice that better reflect human genetic variation
13 hours ago

Research shows robotic ultrasound systems can aid doctors during surgery
14 hours ago

Researchers uncover surprising role of opioid receptors in gut development
Related stories.

Most caregivers are ill-prepared for their own hospitalization
May 2, 2024

Caring for the Alzheimer's caregivers
Feb 28, 2024

Research highlights importance of support reciprocity during early-stage dementia care
Mar 23, 2024

'Rare positive result' in trial of new support intervention for people with dementia and their family caregivers
Feb 1, 2024

Family caregivers who receive a high level of care from a family doctor found to have lower stress levels
Jun 26, 2023

Caregivers of people living with dementia experience discrimination, says study
Jan 9, 2023
Recommended for you

Dementia fighter: Orienteering helps brain and body alike, with greater benefits for those who move quickest
17 hours ago

A protein-based risk score for hip-fracture using an aptamer-based proteomic platform

Scientists identify key protein that preserves motor ability during aging
19 hours ago

Study finds older adults hospitalized for heart failure had high risk of kidney complications

Investigating hyperactivation of memory circuits and Alzheimer's disease risk
May 28, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Telephone-based problem-solving intervention for family caregivers of stroke survivors: a randomized controlled trial
Affiliations.
- 1 Clinic for Geriatric Rehabilitation, Robert-Bosch-Hospital.
- 2 Department of Psychology, Clinical Psychology and Psychotherapy, Eberhard Karls University.
- 3 Department of Psychology, Samford University.
- 4 Center for Neurorehabilitation, Schmieder Hospitals.
- 5 Department of Educational Psychology, Texas A&M University.
- PMID: 24911421
- DOI: 10.1037/a0036987
Objective: Intervention trials for stroke caregivers after the early poststroke period are lacking. To address this gap, we examined the effectiveness of a problem-solving intervention (PSI) for stroke caregivers who provided care for at least 6 months and who experienced significant strain in their role.
Method: One hundred twenty-two family caregivers (age = 66.2 years, 77.9% female) were randomly allocated to a PSI or control group. The PSI was composed of 2 home visits and 18 telephone calls delivered over a 3-month intensive intervention and a 9-month maintenance period. PSI and control groups received monthly information letters in addition to usual care. Primary caregiver outcomes were depressive symptoms (measure: Center for Epidemiologic Studies-Depression Scale) and sense of competence (measure: Sense of Competence Questionnaire).
Results: In covariance analyses, caregivers of the PSI group showed significantly lower levels of depressive symptoms after 3 months (p < .01, d = -.48) and after 12 months (p < .05, d = -.37), but no better sense of competence compared with the control group. Latent growth curve analyses revealed positive significant (p < .05) linear and quadratic effects of PSI on both primary outcomes. No effects, however, were found on caregiver social-problem-solving abilities.
Conclusions: Although beneficial effects were observed among caregivers in the PSI group, the lack of effects on problem-solving abilities implies other characteristics of the intervention might account for these benefits. The relative intensity and therapeutic contact during the first 3 months of the intervention may be particularly helpful to caregivers of stroke survivors.
PsycINFO Database Record (c) 2014 APA, all rights reserved.
Publication types
- Randomized Controlled Trial
- Research Support, Non-U.S. Gov't
- Caregivers*
- Depression / etiology
- Depression / prevention & control*
- Middle Aged
- Problem Solving*
- Stroke / nursing*
- Time Factors
When dementia becomes too much to handle, this tool offers guidance
A first-of-its-kind website offers caregivers a comprehensive approach to managing combativeness and other neuropsychiatric symptoms of dementia.
Caring for older adults with dementia is stressful, especially when they become physically or verbally aggressive, engage in other inappropriate or repetitive behaviors, or refuse to let caregivers help them.
Over 95 percent of patients experience these and other neuropsychiatric symptoms of dementia, which tend to fluctuate over time and vary in intensity. They’re often the reason people with dementia end up in assisted-living facilities or nursing homes, according to the Alzheimer’s Association. At some point, families and friends trying to help at home simply can’t manage.
“When people think about dementia, they usually think about forgetfulness and memory impairment,” said Mary Blazek, director of the Geriatric Psychiatry Clinic at the University of Michigan. “But it’s behavioral and psychological disturbances that are most disruptive to patients’ and caregivers’ lives.”
Now, help is available from a first-of-its-kind website created by prominent experts in the field. It offers free training in a comprehensive approach to managing neuropsychiatric symptoms of dementia — a method known as DICE, based on decades of scientific research as well as extensive clinical practice. DICE stands for Describe, Investigate, Create and Evaluate, the four pillars of the approach.
The website’s goal is to “give people tools to better manage often-distressing situations,” said Helen Kales, chair of the Department of Psychiatry and Behavioral Sciences at UC Davis Health in Sacramento and one of DICE’s creators. Users learn that neuropsychiatric symptoms are caused by changes in the brain that increase people’s vulnerability. Nine video modules and two simulations provide comprehensive information and problem-solving techniques. Although DICE training is free, people can pay for a written manual.
Moving beyond prescription drugs
More than 16 million unpaid caregivers — primarily family members and friends — help people with dementia live at home. (An estimated 20 percent of patients live in institutional settings, according to data from the Centers for Disease Control and Prevention.) The most common form of dementia, Alzheimer’s disease, affects nearly 7 million Americans 65 and older.
DICE is also designed to help “avoid the knee-jerk prescribing of psychoactive medications” that have potentially serious side effects, Kales said. Several medical organizations recommend that non-pharmaceutical approaches to troublesome behaviors be tried before drug therapy, but, in practice, this doesn’t routinely happen.
Drugs prescribed for dementia include antipsychotic medications, such as risperidone , that carry black-box warnings noting a higher risk of early death in elderly patients; anticonvulsants, such as gabapentin, whose use has been on the rise despite safety concerns; benzodiazepines, such as Ativan, which are associated with an increased risk of falls and, thus, fractures; and Celexa and other such antidepressants that have limited data supporting their effectiveness in easing dementia symptoms.
At DICE’s core is an assumption that people with dementia engage in disturbing behaviors for often-unrecognized reasons that can be addressed once they are understood.
Take an example on the website featuring Jennifer, a 55-year-old caregiver for her mother, Betty, 85, whom she tries to bathe daily in the late afternoon. When Betty resists getting into the tub, Jennifer insists, “Let’s go! I have things to do.” Betty responds by smacking her and shouting, “Leave me alone. It hurts.”
Look for underlying causes
DICE asks caregivers to step back from the heat of the moment and examine issues from three perspectives: the person with dementia, the caregiver and the environment. All can contribute to distressing situations, and all need to be considered in fashioning a response.
Examining the problem by using a “who, what, when, how, why” prompt can reveal several potential issues:
· The patient. Betty has arthritis and may experience pain getting in and out of the tub. She may feel tired and overwhelmed in the late afternoon.
· The caregiver. Jennifer may become easily frustrated when she encounters resistance — adopting a scolding and commanding tone rather than breaking down what Betty needs to do in simple steps.
· The environment. The bathroom tends to be cold, with overly bright lights, tepid bathwater and no grab bars around the tub.
Some possible solutions discussed on the website: Offer Betty an over-the-counter pain reliever before her bath. Try baths in the morning, not the afternoon. Relax expectations that she’ll have a daily bath and offer sponge baths several times a week. Install grab bars around the tub, and make sure the water temperature is comfortable. Use a nicely scented soap and play music to help Betty relax. Speak calmly, making simple statements.
These embody strategies shown to improve neuropsychiatric symptoms associated with dementia: recognizing and addressing underlying medical issues such as pain, infections or delirium; simplifying the tasks a person with dementia is expected to perform; and establishing daily routines that give structure to the day.
A new tool for family caregivers
Other important steps: Engage the person in activities that are meaningful to them, including social interactions. Reduce clutter and the potential for overstimulation in the environment. Make sure the person is using hearing or vision aids, if needed. Get them outside and exposed to light.
If safety, psychosis or major depression are urgent concerns, then consider using psychoactive medications after consulting a physician.
Of course, this isn’t a comprehensive list of recommendations. Nor is the method prescriptive. What works for one person with dementia may not work for another.
Using DICE requires creativity and frequent evaluation to assess whether strategies are working, Kales said. If not, it’s time to try new interventions.
Although the DICE tool kit is new to family caregivers, the program has been available to health-care professionals for a while. Notably, all of Wisconsin’s dementia-care specialists have been trained in DICE (every county in that state has a specialist who helps families with dementia).
“It’s a really pragmatic approach that’s put together in a very thoughtful fashion,” said Art Walaszek, a professor of psychiatry and medicine at the University of Wisconsin School of Medicine and Public Health who has been involved in that effort.
Other dementia training programs are available, some of which review behavioral and psychiatric symptoms in less depth, and they, too, are increasingly available online. Another valuable resource, Best Programs for Caregiving , launched in March, lists evidence-based programs across the country and their availability. Enter a Zip code to find information that previously hasn’t been assembled in one place. This site, too, is very much worth consulting.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

A Problem-Solving Intervention for Hospice Family Caregivers: A Randomized Clinical Trial
George demiris.
* School of Nursing, University of Pennsylvania, Philadelphia, Pennsylvania;
Debra Parker Oliver
† School of Medicine, University of Missouri, Columbia, Missouri;
Karla Washington
Kenneth pike.
‡ School of Nursing, University of Washington, Seattle, Washington.
Author Contributions: George Demiris conceptualized and designed the study, oversaw data collection, analysis, and interpretation of data. Debra Parker Oliver and Karla Washington contributed to study design, data analysis, and interpretation of data. Kenneth Pike oversaw data analysis, data management, and contributed to interpretation of data.
Associated Data
Objectives:.
Family caregivers of hospice patients have multiple needs as they try to cope during a stressful time. Translatable interventions effective in improving caregiver outcomes are greatly needed. Our objective was to assess the impact of a problem-solving intervention (called Problem-Solving Intervention to Support Caregivers in End-of-Life Care Settings [PISCES]) to support hospice caregivers on caregiver quality of life and anxiety, and compare its effectiveness delivered face to face and via videoconferencing.
In this 4-year randomized clinical trial, caregivers were randomly assigned to a group receiving standard care with added “friendly calls” (attention control [AC] group), a group receiving standard care and PISCES delivered face to face (F2F), or a group receiving standard care and PISCES delivered via videoconferencing (VC).
Home hospice.
PARTICIPANTS:
A total of 514 caregivers participated (172 in AC, 171 in F2F, and 171 in VC). Caregivers were predominantly female (75%); mean age was 60.3 years.
INTERVENTION:
PISCES includes a structured curriculum delivered in three sessions and motivates caregivers to adopt a positive attitude, define problems by obtaining facts, set goals, and generate and evaluate solutions.
MEASUREMENTS:
Quality of life was measured by the Caregiver Quality of Life Index-Revised; anxiety was measured by the Generalized Anxiety Disorder 7-Item. Other measures included the Caregiver Reaction Assessment scale, demographic data, and an exit interview.
Compared with AC, caregivers in the F2F condition had postintervention reduced anxiety (−1.31 [95% confidence interval [CI] = −2.11 to .50]; p = .004) and improved social (.57 [95% CI = .19-.95]; p = .01), financial (.57 [95% CI = .21-.93]; p = .004), and physical quality of life (.53 [95% CI = .19-.87]; p = .01). There were no differences in caregivers in the VC condition compared with the AC condition.
CONCLUSION:
The PISCES intervention improves caregiver outcomes and is effective when delivered in person. How to integrate technology to reduce the intervention delivery cost warrants further investigation.
Recent scientific evidence highlights the importance of understanding the risks and unmet needs of informal caregivers who care for patients at the end of life. 1 A plethora of research has shown informal family caregivers are at greater risk for depression, deteriorating physical health, financial difficulties, and premature death compared with noncaregivers. 2 , 3 These health risks are compounded by the fact that caregivers are less likely to engage in preventive health behaviors or otherwise attend to their own health needs.
A 2015 Institute of Medicine report identified challenges that hinder high-quality care near the end of life including a mismatch between the services patients and families need and the services they obtain, and a lack of social services for families. 4 Caregivers seek regular contact with hospice providers. 5 Nearly 25% of hospice patients and families report the need for improved communication and emotional support. 6 A systematic literature review 7 identified very few interventions specifically targeting caregivers in end-of-life care, and only two were tested within a randomized control trial. 7 Translatable interventions effective in supporting coping and improving the caregiving experience are greatly needed.
One intervention that has shown potential to support individuals during stressful times is Problem-Solving Therapy (PST). It is a brief, structured cognitive-behavioral treatment that teaches people problem-solving coping skills to help them deal with major negative life events as well as daily problems that are making them anxious or depressed. 8
PST is based on the relational/problem-solving model of stress by D’Zurilla and Nezu. 9 This model integrates Lazarus’s relational model of stress 10 whereby a person in a stressful situation significantly influences the quality and intensity of stress responses through two major processes: cognitive appraisal and coping. 11 PST focuses on behavioral change principles by addressing skills such as problem definition and formulation, and decision making. 9 Researchers have applied PST to various patient populations (eg, adolescents with human immunodeficiency virus, 12 impaired mobility patients, 13 and adolescents after traumatic brain injury [TBI] 14 ). When it comes to family caregivers, PST has been found effective in decreasing anxiety and/or depressive symptoms for caregivers of physically or cognitively impaired adults 15 and patients with dementia, 16 and caregivers of children with TBI. 17
We tailored a brief PST intervention for hospice caregivers called Problem-Solving Intervention to Support Caregivers in End-of-Life Care Settings (PISCES). Customization included development of a hospice-focused curriculum in a three-visit protocol to address the short length of hospice enrollment. In recognition of the geographic barriers in home hospice, we sought a translational delivery platform using web-based videoconferencing technology. This approach recognized the importance of nonverbal communication while bridging geographic distance and reducing cost. Feasibility of videoconferencing for the delivery of PISCES had been found acceptable, easy to use, and convenient for caregivers. 18 – 22 Untested was if the video-conferencing platform preserves the effectiveness of the intervention.
In this study we assessed the impact of the PISCES intervention on caregiver quality of life and anxiety while comparing the effectiveness of the intervention delivered face to face and via videoconferencing. The underlying hypotheses are (1) caregivers having received the PISCES intervention (in person or via videoconferencing) will report higher levels of (covariate-adjusted) postintervention quality of life and lower levels of anxiety compared with caregivers in an attention control (AC) group; and (2) caregivers in the videoconferencing PISCES group will report similar levels of (covariate-adjusted) postintervention quality of life and anxiety as compared with caregivers in the face-to-face PISCES group.
The study was designed as a three-arm randomized clinical trial. Hospice caregivers were randomly assigned to (1) a group receiving standard hospice care plus “friendly calls” (AC), (2) a group receiving standard hospice care with PISCES delivered face to face (F2F), or (3) a group receiving standard hospice care with PISCES delivered via videoconferencing (VC).
Setting and Participants
Two large hospice agencies in the Pacific Northwest participated in the project. Inclusion criteria for caregivers were the following:
- A family/informal caregiver of a hospice patient of one of the participating hospice agencies
- 18 years or older
- Access to a standard phone line or computer with Internet access
- Sufficient hearing for telephone or Internet conversations as assessed by the research staff
- Short Portable Mental Status scores greater than 7 (ie, less than three errors) 23
- Proficient in English with at least a sixth-grade education
Caregivers were asked by the admissions hospice staff if they were interested in being contacted by the team to learn about the study. A researcher contacted caregivers to screen for eligibility and schedule an in-person consent visit.
Intervention
Two interventionists (one psychologist and one social worker) employed by our team received 25 hours of PST training.
Attention Control Group
The AC group received standard hospice services and the same psychometric assessment and number of calls as subjects in the intervention groups. During these calls, caregivers were encouraged to discuss any concerns, and the interventionists refrained from giving advice, teaching skills, or providing solutions. This “friendly visit” intervention was designed to control for the nonspecific aspects of treatment, that is, passage of time, amount of contact, and general support of an empathic and skilled professional.
Intervention Groups F2F and VC
The three-session protocol for PISCES, detailed elsewhere, 18 involves five steps: adopting a positive attitude, defining the problem, creating alternatives, predicting consequences, and trying a solution. Session 1 (initiated near 5 days following hospice admission) focuses on the first two steps, the second session (day 11) the next two, and the last session (day 18) covers the final step. Each session lasts approximately 45 minutes. Caregivers in the F2F group interacted with the interventionist in person; the VC group interacted via videoconferencing.
This timeline was calculated based on average length of stay for our participating hospice agencies and at the national level, PST recommendations 9 and previous work on cognitive-behavioral interventions in hospice. 24 However, this was only a guideline, and the actual timing was tailored to the individual caregiver schedule.
Data Collection and Outcomes
The following sections describe the instruments administered to study subjects.
Caregiver Quality of Life Index-Revised
The Caregiver Quality of Life Index-Revised (CQLI-R), a measure of caregivers’ quality of life (QOL), includes four dimensions: emotional, social, financial, and physical. 25 This four-item instrument was designed specifically for hospice caregivers, and its reliability and validity have been established. 25 Cronbach α for the CQLI-R was .769.
Generalized Anxiety Disorder
The Generalized Anxiety Disorder 7-Item (GAD-7) is a brief, valid, and efficient tool for screening for anxiety and assessing its severity in clinical practice and research. 26 The GAD-7 was tested and demonstrated high levels of reliability and validity (with Cronbach α of .92). 26 The total score is calculated by assigning scores of 0 to 3 for each of the seven items. This instrument was used widely to assess anxiety of informal caregivers in hospice 27 , 28 and serves as a valid screening and continuous assessment tool given its brevity that reduces respondent burden. 26
Problem-Solving Inventory
The Problem Solving Inventory (PSI) is a 35-item Likert-type inventory that serves as a measure of an individual’s perceptions of their problem-solving behavior and attitudes. 29 The total score is used as an overall index of problem-solving ability. Reliability and validity of this instrument have been documented extensively (Cronbach α reported at .85).
The Caregiver Reaction Assessment Scale
The Caregiver Reaction Assessment (CRA) scale is a 24-item instrument designed to assess specific aspects of the caregiving situation, including both negative and positive dimensions of caregiving reactions. 30 Cronbach α varies between .62 and .83 for the separate subscales, indicating sufficient internal consistencies. 30
Demographic Data
Standard demographic data were collected on caregivers including age, sex, nativity, education level, marital status, occupation, and diagnosis of patient. Furthermore, if the patient died during the subject’s participation, date of death was recorded (to allow for calculation of timing of death in the context of subject’s days in the study).
An exit interview was conducted to assess participants’ perceptions of the intervention and its utility, and of videoconferencing for those in the VC group ( Supplementary Table S1 ). Exit interviews were conducted by another member of the team to reduce bias and audio-recorded with a random subset (30% of interviews) transcribed. Two members conducted a deductive thematic analysis to identify perceived benefits and challenges with the intervention and with videoconferencing (for those in the VC group).
Figure 1 demonstrates the timeline for data collection. One last follow-up assessment over the phone took place approximately 40 days after the exit interview. Most caregivers were in the bereavement phase at that point in time (and this is why assessment focuses at that follow-up on problem-solving inventory, anxiety, and QOL but not the caregiving-related experience); however, the purpose was to assess the long-term impact of the intervention.

Timeline for data collection. CQLI-R, Caregiver Quality of Life Index-Revised; CRA, Caregiver Reaction Assessment; F2F, face to face; GAD-7, Generalized Anxiety Disorder 7-Item; PISCES, Problem-Solving Intervention to Support Caregivers in End-of-Life Care Settings; VC, videoconferencing.
Randomization and Blinding
A block randomization approach was used to ensure that treatment groups were not imbalanced with respect to time of the year as season (eg, holidays) could have an effect on some of the measures. Randomization was stratified by hospice agency. Group assignment was revealed following the identification of problems and challenges, and consent for participation was obtained. Instruments were administered over the phone by a separate research assistant who was blinded to the assignment.
Sample Size
The study was designed to have 80% power (α = .05, two sided) to detect effect sizes of .5 standard deviations, equivalent to 3 points on the CQLI-R, the minimal difference of clinical significance, for the F2F and VC treatment effects. Recruitment greatly exceeded our expectations, so there was greater than 90% power for this effect size at exit and 40-day follow-up.
Statistical Analysis
The purpose of this study was to compare differences between treatment groups in terms of caregiver anxiety and QOL over the course of the intervention. Differences between groups in baseline characteristics were compared using one-way analysis of variances for continuous variables and χ 2 tests for categorical variables. We also compared attrition among caregivers using t tests and χ 2 tests. Specifically, analyses were conducted on baseline demographic characteristics, as well as baseline outcome measures, to determine whether participants who completed all phases of data collection were initially different when compared with persons who did not complete the entire longitudinal follow-up. For the study outcomes, we used multivariate linear regression models with robust standard errors. For each of the study outcomes, the corresponding preintervention score, hospice agency, a factor indicating assessment type (baseline, exit interview, or follow-up assessment), patient diagnosis, and whether the caregiver’s patient had died were used as primary adjustment covariates. The possibility of a change over time in the difference in effectiveness between treatments was explored by including a time by group interaction in the models. The primary goal of the analyses was pairwise comparisons between the three treatment groups. A Bonferroni adjustment was used to account for the three pairwise comparisons. Data were analyzed using the Stata statistical package, v.13.
Study Participants
A total of 2048 caregiver referrals were received by the study team; of these, 186 caregivers were ineligible for the study, 317 unable to contact, and 1031 declined to participate. This led to a total number of 514 caregivers who participated in the study (AC, n = 172; VC, n = 171; and F2F, n = 171). Figure 2 displays the study’s Consolidated Standards of Reporting Trials (CONSORT) diagram. Caregivers ranged in age from 19 to 100 (mean age = 60.3 y), were predominantly female (75%), and mostly adult children (55%) or spouses/partners (27%) of hospice patients. Table 1 includes the characteristics of caregivers and patients.

Consolidated Standards of Reporting Trials (CONSORT) diagram.
Caregiver and Patient Characteristics
Abbreviations: CQLI-R, Caregiver Quality of Life Index-Revised; GAD-7, Generalized Anxiety Disorder 7-Item; SD, standard deviation.
Caregivers assigned to the three intervention groups were similar in sex, age, race/ethnicity, relationship to patient, residing with patient, bereavement at consent, referring agency, employment, caregiving amount and duration, QOL, and anxiety. There were more patients with diagnoses of cancer and cardiovascular disease in the AC group, and dementia patients were more prevalent in the F2F group (P = .005). At baseline, 225 (44%) of the caregivers were bereaved as were the majority (79%) for whom data were available (n = 444) at the 40-day follow-up.
Of the 514 caregivers, 460 (89%) completed the exit assessment, and 416 (81%) completed the 40-day follow-up telephone survey. Attrition during active treatment (0–1 mo) was significantly lower for caregivers in the F2F (7.0% [12/171] and AC 7.0% [12/172] groups compared with the VC group 17.5% [30/171], P = .001, primarily because caregivers could not be contacted or their loved one had died. Total attrition over 3 months did not differ significantly between groups (AC, 17.4% [30/172]; F2F, 17.5% [30/171]; VC, 22.2% [38/171]; P = .44. When demographic characteristics were compared, those without follow-up data were slightly younger (57.7 y [95% confidence interval [CI] = 54.7–60.6] vs 60.9 [95% CI = 59.8–62.1]; P = .02); more likely to reside with their loved one (58.2% [57/98] vs 45.5% [189/416]; P = .02); were less likely to have been providing care longer than 1 year (56.1% [55/98] vs 74.0% [308/416]; P < .001); and were more likely to have been caregiving more than 20 hours/week (66.3 [65/98] vs 54.3% [226/416]; P = .03).
Primary Outcome
Compared with AC, caregivers in the F2F condition had postintervention reduced anxiety (−1.3 [95% CI = −2.1 to −.5]; P = .004), and improved social (.6 [95% CI = .2–1.0]; P = .01), financial (.6 [95% CI = .2-.9], P = .004), and physical QOL (.5 [95% CI = .2-.9]; P = .01). Results were adjusted for referral agency, patient diagnosis, and bereaved status. There were no differences in caregivers in the VC condition compared with the AC condition. Table 2 provides the anxiety and caregiver QOL values at baseline and exit from the intervention. Effect sizes for preintervention to follow-up were moderate to large (Anxiety .24 [.16-.30 CI]; QoL-physical .29 [.21-.35 CI]; QoL-social .17 [.10-.22 CI]; QoL-emotional .31 [.23-.37 CI]; QoL-financial .29 [.21-.30 CI]).
GAD-7 and CQLI-R Scores at Baseline and Exit by Treatment Group
Abbreviations: AC, attention control; CQLI-R, Caregiver Quality of Life Index-Revised; F2F, face to face; GAD-7, Generalized Anxiety Disorder 7-Item; VC, videoconferencing.
Sample sizes for AC, F2F, and VC, respectively, are 172, 171, and 171 at baseline; 160, 159, and 141 at 1 month.
Internal consistency for the measures was high (Cronbach α for CQLI-R = .75, GAD-7 = .88, PSI = .78, and CRA = .83). Caregivers took about 1 month (mean = 34.6 d; standard deviation = 18.2; median 28) to complete the intervention. Intervention duration in the F2F group (mean = 36.8 d) and the VC group (mean = 37.5 d) were comparable and slightly higher than in the AC group (mean = 29.9 d); time to complete the intervention was not related to outcomes.
Secondary Outcomes
A total of 300 exit interviews were conducted with participants in the intervention groups (159 in the F2F group, 141 in the VC group). A random set of 100 interviews were transcribed (53 in the F2F group, 47 in the V2C group). Average duration of the interviews was 22 minutes. Participants embraced the intervention, describing it as a “structured guide” to navigate challenges and brainstorm for effective solutions. Identified benefits included the availability of tools and templates necessary to brainstorm and the opportunity to reflect on challenges. Several participants commented on the intervention as a way to combat feelings of isolation. All participants agreed that PISCES should become a standard service of hospice care, and some commented on the value of getting exposed to it earlier in the caregiving trajectory to fully maximize benefits. Subjects in the VC group found videoconferencing an appropriate platform. In many cases (62% of transcribed interviews), participants felt that they would not have benefited more had they interacted with the interventionist in person, with some (16%) even stating a preference for videoconferencing because of their busy schedule.
To our knowledge this is the largest clinical trial with hospice caregivers to date. PISCES was found very effective when delivered in person. Compared with AC, caregivers in the F2F condition had postintervention reduced anxiety and improved QOL. These findings are statistically but also clinically significant (for GAD-7 a reduction of more than 1 point on the 7-point scale is clinically meaningful 31 ; the same for a reduction of .5 or more on each of the subscales of the CQLI-R 32 ). The intervention for the VC group was as effective as the AC group. Participants at the exit interview appreciated the convenience and ease of use of the videoconferencing delivery, and caregivers commented on the benefit of having a meaningful conversation, hearing and seeing each other “without yet another visitor in the home.”
However, even though the videoconferencing platform was embraced by participants at exit interviews, it is noteworthy that the videoconferencing mediated intervention was not as effective as the F2F group. Although a direct comparison of in-person and videoconferencing sessions has not been examined extensively in hospice, there are studies comparing these two modalities for other populations. Two randomized studies 33 , 34 reported no significant differences for symptoms of anxiety and depression between psychotherapy patients receiving in-person and videoconferencing sessions. Mitchell et al 35 found in a comparison of in-person and videoconferencing treatment for patients with eating disorders that the in-person group experienced greater reduction in depressive symptoms. Backhaus et al 36 conducted a systematic review of videoconferencing psychotherapy and identified challenges in the sample size of comparison studies calling for more studies with experimental design. In our study we hypothesize that findings for the videoconferencing group may be due to the lack of initial personal rapport and intimate F2F contact with the interventionist. Although overall the technical quality of the videoconferencing sessions was very good or excellent, in some instances there were technical difficulties.
The use of an AC group with a vulnerable population like hospice caregivers may not be ideal because the introduction of “friendly calls” to this population may be an intervention in and of itself, which could further explain why the AC group performed comparably with the VC group. A combination of platforms whereby a hybrid approach is pursued (eg, first session in person, follow-up sessions via video-conferencing) needs to be investigated as a cost-effective solution (especially in remote and rural areas). Study limitations include recruitment in only one geographic region (the Pacific Northwest) and a sample with limited racial diversity (although comparable with national hospice census data).
Translation of this study into practice requires an organization to consider available resources, costs, and adjustments to clinicians’ workflow. All aspects of the intervention have been standardized, and training manuals have been developed for hospice staff.
This study addresses a current gap in scientific evidence because there is a lack of evaluations of supportive interventions for family caregivers in hospice. A systematic review in 2016 of behavioral and educational interventions to support family caregivers in end-of-life care 37 identified only 14 studies; most of them were pilot trials. Hospice caregivers can benefit from structured cognitive-behavioral interventions designed to address their unique needs during the challenging time of taking care of a loved one at the end of life.
Supplementary Material
Supplementary Table S1: Exit interview questions.
ACKNOWLEDGMENTS
Sponsor’s Role: Research reported in this article was supported by the National Institute of Nursing Research of the National Institutes of Health (NIH) under Award Number R01NR012213. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Trial Registration: Trial registered with ClinicalTrials.gov has ID (Protocol ID: RNR012213A). The registry URL is https://clinicaltrials.gov/ct2/show/ {"type":"clinical-trial","attrs":{"text":"NCT01444027","term_id":"NCT01444027"}} NCT01444027 .
Conflict of Interest: The authors have no conflicts of interest.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.

- Bahasa Indonesia
- Eastern Europe
- Moscow Oblast
Elektrostal
Elektrostal Localisation : Country Russia , Oblast Moscow Oblast . Available Information : Geographical coordinates , Population, Area, Altitude, Weather and Hotel . Nearby cities and villages : Noginsk , Pavlovsky Posad and Staraya Kupavna .
Information
Find all the information of Elektrostal or click on the section of your choice in the left menu.
- Update data
Elektrostal Demography
Information on the people and the population of Elektrostal.
Elektrostal Geography
Geographic Information regarding City of Elektrostal .
Elektrostal Distance
Distance (in kilometers) between Elektrostal and the biggest cities of Russia.
Elektrostal Map
Locate simply the city of Elektrostal through the card, map and satellite image of the city.
Elektrostal Nearby cities and villages
Elektrostal weather.
Weather forecast for the next coming days and current time of Elektrostal.
Elektrostal Sunrise and sunset
Find below the times of sunrise and sunset calculated 7 days to Elektrostal.
Elektrostal Hotel
Our team has selected for you a list of hotel in Elektrostal classified by value for money. Book your hotel room at the best price.
Elektrostal Nearby
Below is a list of activities and point of interest in Elektrostal and its surroundings.
Elektrostal Page

- Information /Russian-Federation--Moscow-Oblast--Elektrostal#info
- Demography /Russian-Federation--Moscow-Oblast--Elektrostal#demo
- Geography /Russian-Federation--Moscow-Oblast--Elektrostal#geo
- Distance /Russian-Federation--Moscow-Oblast--Elektrostal#dist1
- Map /Russian-Federation--Moscow-Oblast--Elektrostal#map
- Nearby cities and villages /Russian-Federation--Moscow-Oblast--Elektrostal#dist2
- Weather /Russian-Federation--Moscow-Oblast--Elektrostal#weather
- Sunrise and sunset /Russian-Federation--Moscow-Oblast--Elektrostal#sun
- Hotel /Russian-Federation--Moscow-Oblast--Elektrostal#hotel
- Nearby /Russian-Federation--Moscow-Oblast--Elektrostal#around
- Page /Russian-Federation--Moscow-Oblast--Elektrostal#page
- Terms of Use
- Copyright © 2024 DB-City - All rights reserved
- Change Ad Consent Do not sell my data
Current time by city
For example, New York
Current time by country
For example, Japan
Time difference
For example, London
For example, Dubai
Coordinates
For example, Hong Kong
For example, Delhi
For example, Sydney
Geographic coordinates of Elektrostal, Moscow Oblast, Russia
City coordinates
Coordinates of Elektrostal in decimal degrees
Coordinates of elektrostal in degrees and decimal minutes, utm coordinates of elektrostal, geographic coordinate systems.
WGS 84 coordinate reference system is the latest revision of the World Geodetic System, which is used in mapping and navigation, including GPS satellite navigation system (the Global Positioning System).
Geographic coordinates (latitude and longitude) define a position on the Earth’s surface. Coordinates are angular units. The canonical form of latitude and longitude representation uses degrees (°), minutes (′), and seconds (″). GPS systems widely use coordinates in degrees and decimal minutes, or in decimal degrees.
Latitude varies from −90° to 90°. The latitude of the Equator is 0°; the latitude of the South Pole is −90°; the latitude of the North Pole is 90°. Positive latitude values correspond to the geographic locations north of the Equator (abbrev. N). Negative latitude values correspond to the geographic locations south of the Equator (abbrev. S).
Longitude is counted from the prime meridian ( IERS Reference Meridian for WGS 84) and varies from −180° to 180°. Positive longitude values correspond to the geographic locations east of the prime meridian (abbrev. E). Negative longitude values correspond to the geographic locations west of the prime meridian (abbrev. W).
UTM or Universal Transverse Mercator coordinate system divides the Earth’s surface into 60 longitudinal zones. The coordinates of a location within each zone are defined as a planar coordinate pair related to the intersection of the equator and the zone’s central meridian, and measured in meters.
Elevation above sea level is a measure of a geographic location’s height. We are using the global digital elevation model GTOPO30 .
Elektrostal , Moscow Oblast, Russia

COMMENTS
Most psychotherapeutic interventions with caregivers follow a cognitive-behavioral approach (N = 9), where therapists may teach self-monitoring, challenge negative thoughts and assumptions that maintain the caregiver's problematic behavior; help caregivers develop problem-solving abilities by focusing on time management, overload, and ...
Designed to empower family caregivers by applying the principles of problem-solving training to problems and stressors experienced by the caregiver. ... Weitzner, M., Schonwetter, R. S., Tittle, M., Moody, L., & Haley, W. E. (2006). Impact of coping skills intervention with family caregivers of hospice patients with cancer: A randomized ...
With respect to interventions for these caregivers, the literature generally suggests that psychosocial interventions such as problem-solving therapy, family psychoeducational and dyadic multicomponent psychosocial interventions (e.g., those that combine skills training, stress management techniques) can be beneficial to family caregivers.
This stud y reviewed the growing body of intervention describing the details of. problem -solving intervention, effects on caregiver outcomes. Most of the prob-. lem- solving intervention ...
Introduction. Powerful Tools for Caregivers (PTC) is a national program sustained by extensive collaborations with community-based organizations. 1 PTC is a train-the-trainer model program with a detailed, scripted curriculum. The PTC course is a group psychoeducational skill-building intervention that aims to empower caregivers to better care for themselves and enhance their self-efficacy.
Intervention: A registered nurse guided caregivers in using problem-solving strategies emphasizing creative thinking, optimism, planning, and expert information to address challenges associated with caregiving. Caregivers in the intervention completed one telephone orientation session followed by eight online, asynchronous messaging center ...
Translatable interventions effective in improving caregiver outcomes are greatly needed. Our objective was to assess the impact of a problem-solving intervention (called Problem-Solving Intervention to Support Caregivers in End-of-Life Care Settings [PISCES]) to support hospice caregivers on caregiver quality of life and anxiety, and compare ...
Problem-solving intervention is promising in caregiver intervention which could reduce caregiver depression, anxiety and burden. Background: Caregiving for someone is a huge task for informal caregivers. The caregiving role is often challenging and overwhelming for them. Stress, burden, and depression have been frequently identified as the negative caregiving experiences.
The BOSC intervention is a cognitive-behavioral problem-solving intervention (PSI) that was adapted from the Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) Program (Hegel & Arean, 2003).The BOSC intervention identifies primary caregivers' depressive symptoms and feelings of burden and links them to problems in living.
Problem-solving abilities and health-related quality of life showed no change. Seventy-eight percent of caregivers rated the intervention sessions with the nurses as very helpful or extremely helpful, and 76% reported using the problem-solving strategies a moderate amount to extremely often.
The Problem Solving Intervention (PSI) is a structured, cognitive-behavioral intervention that provides people with problem-solving coping skills to help them face major negative life events and daily challenges. PSI has been applied to numerous settings but remains largely unexplored in the hospice setting. The aim of this pilot study was to ...
The study purposes were to assess the efficacy of a caregiver problem-solving intervention (CPSI) on stroke caregiver physical and psychosocial adaptation compared with a wait-list control (WLC) treatment, and to assess the mediation effects of coping on outcomes. Methods. A stress and coping model guided the study design.
The objective of this study is to evaluate the impact of a telephone and online, problem-solving intervention on caregiver outcomes. Our primary aim is to reduce caregiver depression. Secondary aims are to: reduce caregiver burden, improve caregivers' problem-solving abilities, self-efficacy, and quality of life, improve veterans ...
Our objective was to assess the impact of a problem-solving intervention (called Problem-Solving Intervention to Support Caregivers in End-of-Life Care Settings [PISCES]) to support hospice caregivers on caregiver quality of life and anxiety, and compare its effectiveness delivered face to face and via videoconferencing.
PSI is a brief, structured, cognitive-behavioral intervention that teaches people problem-solving coping skills to help them deal with major negative life events as well as daily problems that are making them anxious or depressed. 12 Researchers have applied PSI to a wide variety of patient populations and program goals. Specifically, when it comes to family caregivers, PSI has been tested ...
1) (a) Systematic family caregiver distress screening and problem assessment, (b) plan tailed problem-solving strategies, (c) liaison by the oncology nurse. 1) Usual care: Family caregivers' distress decreased over time, but this reduction was observed in both groups. Similar results were found for secondary outcomes. 2) 9 months: 2)— 3) n = 54
According to the U.S. Centers for Disease Control and Prevention, 80% of those living with dementia receive informal care from family members or friends. This equates to 16 million family ...
To address this gap, we examined the effectiveness of a problem-solving intervention (PSI) for stroke caregivers who provided care for at least 6 months and who experienced significant strain in their role. Method: One hundred twenty-two family caregivers (age = 66.2 years, 77.9% female) were randomly allocated to a PSI or control group. The ...
A first-of-its-kind website offers caregivers a comprehensive approach to managing combativeness and other neuropsychiatric symptoms of dementia. By Judith Graham May 26, 2024 at 7:00 a.m. EDT
Elektrostal is a city in Moscow Oblast, Russia, located 58 kilometers east of Moscow. Elektrostal has about 158,000 residents. Mapcarta, the open map.
Abstract. OBJECTIVES: Family caregivers of hospice patients have multiple needs as they try to cope during a stressful time. Translatable interventions effective in improving caregiver outcomes are greatly needed. Our objective was to assess the impact of a problem-solving intervention (called Problem-Solving Intervention to Support Caregivers ...
Elektrostal Geography. Geographic Information regarding City of Elektrostal. Elektrostal Geographical coordinates. Latitude: 55.8, Longitude: 38.45. 55° 48′ 0″ North, 38° 27′ 0″ East. Elektrostal Area. 4,951 hectares. 49.51 km² (19.12 sq mi) Elektrostal Altitude.
March 17, 2011. Pavel Oderov was appointed as Head of the International Business Department pursuant to a Gazprom order. Pavel Oderov was born in June 1979 in the town of Elektrostal, Moscow Oblast. He graduated from Gubkin Russian State University of Oil and Gas with an Economics degree in 2000 and a Management degree in 2002.
Geographic coordinates of Elektrostal, Moscow Oblast, Russia in WGS 84 coordinate system which is a standard in cartography, geodesy, and navigation, including Global Positioning System (GPS). Latitude of Elektrostal, longitude of Elektrostal, elevation above sea level of Elektrostal.