Last updated 20/06/24: Online ordering is currently unavailable due to technical issues. We apologise for any delays responding to customers while we resolve this. For further updates please visit our website: https://www.cambridge.org/news-and-insights/technical-incident
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .

Login Alert

- > Journals
- > European Psychiatry
- > Volume 26 Issue S2: Abstracts of the 19th European...
- > Olfactory reference syndrome - A case report

Article contents
Olfactory reference syndrome - a case report.
Published online by Cambridge University Press: 16 April 2020
Olfactory reference syndrome (ORS), first described by Pryse-Phillips in 1971, is a rare psychiatric condition whose defining characteristic is a preoccupation with the belief that one emits a foul or offensive body odor, which is not perceived by others. Although the existence of ORS is now widely accepted, current classifications do not explicitly mention ORS as an independent category, but consider it as a delusional disorder, somatic type. Nonetheless, given this syndrome's consistent description along time and cultures, and the associated substancial distress and disability, many authors debate the possibility of a new classification in order to establish its nosological status.
The aim of this paper is to show and discuss some troublesome and complex issues of diagnosis and management of patients with ORS.
Herein we report a case of a 38-year-old woman who presented with ORS.
Improvement in ORS can take place, in some extent, with a variety of different modalities of treatment, with the disorder responding to antidepressants and psychotherapy more frequently than to neuroleptics. Data on ORS are still limited and more research in this field is needed. Awareness of this particular diagnosis allows appropriate treatment to be administered.

No CrossRef data available.
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 26, Issue S2
- D. Freitas (a1) , P. Ferreira (a1) and N. Fernandes (a1)
- DOI: https://doi.org/10.1016/S0924-9338(11)73423-X
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Olfactory reference syndrome: a still open nosological and treatment debate
Affiliations.
- 1 Botucatu Medical School, São Paulo State University-Univ Estadual Paulista (Unesp), Brazil.
- 2 Anxiety and Depression Research Program, Institute of Psychiatry, Federal University of Rio de Janeiro & D'Or Institute for Research and Education, Brazil.
- 3 Botucatu Medical School, São Paulo State University-Univ Estadual Paulista (Unesp), Brazil. Electronic address: [email protected].
- PMID: 25041636
- DOI: 10.1016/j.genhosppsych.2014.06.001
Objective: The objective was to report a case of olfactory reference syndrome (ORS) with several co-occurring disorders and to discuss ORS differential diagnoses, diagnostic criteria and classification.
Method: Case report.
Results: A 37-year-old married woman presented overvalued ideas of having bad breath since adolescence. She met current diagnostic criteria for social anxiety disorder, specific phobia, obsessive-compulsive disorder, generalized anxiety disorder, body dysmorphic disorder and major depressive disorder. ORS similarities and differences with some related disorders are discussed.
Conclusion: Further studies regarding symptoms, biomarkers and outcomes are needed to fully disentangle ORS from existing depressive, anxiety and obsessive-compulsive spectrum disorders.
Keywords: Diagnostic criteria; Differential diagnoses; Nosological classification; Obsessive–compulsive disorder; Olfactory reference syndrome.
Copyright © 2014 Elsevier Inc. All rights reserved.
PubMed Disclaimer
Similar articles
- Transdiagnostic Approach to Olfactory Reference Syndrome: Neurobiological Considerations. Skimming KA, Miller CWT. Skimming KA, et al. Harv Rev Psychiatry. 2019 May/Jun;27(3):193-200. doi: 10.1097/HRP.0000000000000215. Harv Rev Psychiatry. 2019. PMID: 31082994 Review.
- Unremitting body odour: A case of Olfactory Reference Syndrome. Tee CK, Suzaily W. Tee CK, et al. Clin Ter. 2015;166(2):72-3. doi: 10.7417/CT.2015.1819. Clin Ter. 2015. PMID: 25945434
- Obsessive-compulsive spectrum disorders in obsessive-compulsive disorder and other anxiety disorders. Lochner C, Stein DJ. Lochner C, et al. Psychopathology. 2010;43(6):389-96. doi: 10.1159/000321070. Epub 2010 Sep 16. Psychopathology. 2010. PMID: 20847586
- Body dysmorphic disorder and obsessive-compulsive disorder: similarities, differences and the classification debate. Chosak A, Marques L, Greenberg JL, Jenike E, Dougherty DD, Wilhelm S. Chosak A, et al. Expert Rev Neurother. 2008 Aug;8(8):1209-18. doi: 10.1586/14737175.8.8.1209. Expert Rev Neurother. 2008. PMID: 18671665 Review.
- Olfactory reference syndrome: diagnostic criteria and differential diagnosis. Lochner C, Stein DJ. Lochner C, et al. J Postgrad Med. 2003 Oct-Dec;49(4):328-31. J Postgrad Med. 2003. PMID: 14699232
- Psychosomatic problems in dentistry. Toyofuku A. Toyofuku A. Biopsychosoc Med. 2016 Apr 30;10:14. doi: 10.1186/s13030-016-0068-2. eCollection 2016. Biopsychosoc Med. 2016. PMID: 27134647 Free PMC article. Review.
- Olfactory Reference Disorder: Diagnosis, Epidemiology and Management. Thomas E, du Plessis S, Chiliza B, Lochner C, Stein D. Thomas E, et al. CNS Drugs. 2015 Dec;29(12):999-1007. doi: 10.1007/s40263-015-0292-5. CNS Drugs. 2015. PMID: 26563195 Review.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Elsevier Science
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Olfactory Reference Syndrome: A Case Report and Screening Tool
- Published: 29 April 2020
- Volume 28 , pages 344–348, ( 2021 )
Cite this article

- Yelena Chernyak ORCID: orcid.org/0000-0001-6925-1981 1 ,
- Kristine M. Chapleau 1 ,
- Shariff F. Tanious 1 ,
- Natalie C. Dattilo 2 ,
- David R. Diaz 1 &
- Sarah A. Landsberger 1
573 Accesses
3 Citations
1 Altmetric
Explore all metrics
Olfactory reference syndrome (ORS) is a lesser known disorder that is related to obsessive–compulsive disorder. ORS is the obsessional and inaccurate belief that one is emitting a foul odor leading to embarrassment or concern about offending others, excessive hygiene behaviors, and social avoidance that significantly interferes with daily functioning. Although ORS is rare, it is challenging to diagnose. ORS-sufferers first seek treatment from non-psychiatric providers (e.g., dermatologists, dentists.) to alleviate the perceived odor, which frequently leads to misdiagnosis and unnecessary treatments. Additionally, because ORS-sufferers can have limited insight and ideas of reference, they can be misdiagnosed as having a psychotic or delusional disorder. We present a case report of a 42-year-old woman with ORS, and how the correct diagnosis of ORS provided with psychiatric treatment led to significant improvement in her daily functioning. We provide a literature review on the disorder as well as a short screener to assess ORS.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Olfactory reference disorder—a review

Olfactory Reference Disorder: Diagnosis, Epidemiology and Management
Prevalence of olfactory reference disorder according to the icd-11 in a german university student sample.
Allen-Crooks, R., & Challacombe, F. (2017). Cognitive behavior therapy for olfactory reference disorder (ORD): A case study. Journal of Obsessive-Compulsive and Related Disorders, 13 , 7–13.
Article Google Scholar
American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR . Washington, DC: APA.
Google Scholar
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, DSM-5 . Washington, DC: APA.
Book Google Scholar
Asakura, S., Inoue, T., Kitagawa, N., Nasegama, M., Fujii, Y., Kako, Y., … Nakagawa, S. (2012). Social Anxiety/Taijin-Kyofu Scale (SATS): Development and psychometric evaluation of a new instrument. Psychopathology, 45 , 96–101.
Atmaca, M., Korkmaz, S., Namli, M. N., Kormaz, H., & Kuloglu, M. (2011). Olfactory reference syndrome treated with quetiapine: A case. Bull of Clinical Psychopharmacology, 21 , 246–248.
Begum, M., & McKenna, P. J. (2011). Olfactory reference syndrome: A systematic review of the world literature. Psychological Medicine, 41 , 453–461.
Article CAS Google Scholar
Bizamcer, A. N., Dubin, W. R., & Hayburn, B. (2008). Olfactory reference syndrome. Psychosomatics, 49 , 77–81.
Feusner, J. D., Phillips, K. A., & Stein, D. J. (2010). Olfactory reference syndrome: Issues for DSM-V. Depression & Anxiety, 27 , 592–599.
Greenberg, J. L., Shaw, A. M., Reuman, L., Schwarts, R., & Wilhelm, S. (2016). Clinical features of olfactory reference syndrome: An internet-based study. Journal of Psychosomatic Research, 80 , 11–16.
Kasahara, Y., & Kenji, S. (1971). Ereuthophobia and allied conditions: A contribution toward the psychopathological and cross cultural study of a borderline state. In S. Arieti (Ed.), The world biennial of psychiatry in psychotherapy . New York: Basic Books.
Kozak, M. J., & Foa, E. B. (1994). Obsessions, overvalued ideas, and delusions in obsessive-compulsive disorder. Behavior Research and Therapy, 32 , 343–353.
Lim, L., & Wan, Y. M. (2015). Jikoshu-kyofu in Singapore. Australasian Psychiatry, 23 , 300–302.
Lochner, C., & Stein, D. (2003). Olfactory reference syndrome: Diagnostic criteria and differential diagnosis. Journal of Postgraduate Medicine, 49 , 328–331.
CAS PubMed Google Scholar
Marks, I., & Mishan, J. (1988). Dysmorphophobic avoidance with disturbed bodily perception: A pilot study of exposure therapy. British Journal of Psychiatry, 152 , 674–678.
Muffatti, R., Scarone, S., & Gambini, O. (2008). An olfactory reference syndrome successfully treated by aripiprazole augmentation to antidepressant therapy. Cognitive and Behavioral Neurology, 21 , 258–260.
Phillips, K. A., Hollander, E., Rasmussen, S. A., Aronowitz, B. R., DeCaria, C., & Goodman, W. K. (1997). A severity rating scale or body dysmorphic disorder: Development, reliability, and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychopharmacology Bulletin, 33 , 17–22.
Phillips, K. A., & Menard, W. (2011). Olfactory reference syndrome: Demographic and clinical features of imagined body odor. General Hospital Psychiatry, 33 , 398–406.
Prazeres, A. M., Fontenelle, L. F., Medlowicz, M. V., De Mathis, M. A., Ferraro, Y. A., de Brito, N. F., … Miguel, E. C. (2010). Olfactory reference syndrome as a subtype of body dysmorphic disorder. Journal of Clinical Psychiatry, 71 , 87–89.
Pryse-Phillips, W. (1971). An olfactory reference syndrome. Acta Psychiatrica Scandinavica, 47 , 484–509.
Stein, D. J., Le Roux, L., Bouwer, C., & Van Heerdeen, B. (1998). Is olfactory reference syndrome an obsessive-compulsive spectrum disorder?: Two cases and a discussion. Journal of Neuropsychiatry and Clinical Neuroscience, 10 , 96–99.
Stein, D. J., Kogan, C. S., Atmaca, M., Fineberg, N. A., Fontenelle, L. F., Grant, J. E., … Van Den Heuvel, O. A. (2016). The classification of obsessive-compulsive and related disorders in the ICD-11. Journal of Affective Disorders, 190 , 663–674.
Suzuki, K., Takei, N., Iwata, Y., Sekine, Y., Toyoda, T., Nakamura, K., … Mori, N. (2004). Do olfactory reference syndrome and jiko-shu-kyofu (a subtype of taijin-kyofu) share a common entity? Acta Psychiatrica Scandinavica, 109 , 150–155.
Teraishi, T., Takahashi, T., Suda, T., Hirano, J., Ogawa, T., Kuwahara, T., … Nomura, S. (2012). Successful treatment of olfactory reference syndrome with paroxetine. Journal of Neuropsychiatry and Clinical Neuroscience, 24 , E24.
Download references
This article has no funding source.
Author information
Authors and affiliations.
Department of Psychiatry, Indiana University School of Medicine, 355 W. 16th St., Suite 2800, Indianapolis, IN, 46202, USA
Yelena Chernyak, Kristine M. Chapleau, Shariff F. Tanious, David R. Diaz & Sarah A. Landsberger
Department of Psychiatry, Brigham and Women’s Hospital, Boston, MA, USA
Natalie C. Dattilo
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yelena Chernyak .
Ethics declarations
Conflict of interest.
Yelena Chernyak, Kristine M. Chapleau, Shariff F. Tanious, Natalie C. Dattilo, David R. Diaz, and Sarah A. Landsberger declare that they have no conflict of interest.
Human and Animal Rights
All applicable human rights were honored during the writing of this manuscript.
Informed Consent
Informed consent was obtained from all individual participants included in this case report.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Chernyak, Y., Chapleau, K.M., Tanious, S.F. et al. Olfactory Reference Syndrome: A Case Report and Screening Tool. J Clin Psychol Med Settings 28 , 344–348 (2021). https://doi.org/10.1007/s10880-020-09721-9
Download citation
Published : 29 April 2020
Issue Date : June 2021
DOI : https://doi.org/10.1007/s10880-020-09721-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Olfactory reference syndrome
- Psychiatric disorders
- Anxiety disorders
- Delusional disorders
- Obsessive–compulsive disorder
- Jikoshu-kyofu
- Taijin-kyofu
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 04 December 2023
Olfactory reference disorder—a review
- Savitha Soman ORCID: orcid.org/0000-0003-4866-372X 1 &
- Rajesh Nair 2
Middle East Current Psychiatry volume 30 , Article number: 95 ( 2023 ) Cite this article
894 Accesses
Metrics details
Olfactory Reference Disorder (ORD) is a known clinical entity for several decades; however, it is only in ICD 11 that it has found its niche. Long considered a delusional disorder, it is currently classified as an obsessive–compulsive (OC) spectrum disorder.
ORD is characterised by an erroneous conviction that the body is emitting an unpleasant smell. Patients harbour referential thinking, practise rituals to eliminate or mask the perceived odour, and avoid social interactions. While the conviction can be at a delusional level in some patients, the preoccupation has an obsessive quality in others. The level of insight can be varied. Patients present to mental health settings after traversing a long pathway of care comprising of various specialists. Medical and psychiatric conditions which can present with ORD-like symptoms need to be ruled out. Establishing a therapeutic alliance is the first step in management. There are no randomised controlled trials comparing treatment options in ORD. Antidepressants, antipsychotics, and their combinations have been used with varying degrees of success, in addition to psychotherapy and electroconvulsive therapy. Data on prognosis is limited.
Introduction
Of the five senses that man is blessed with, smell, taste, and touch have always been accorded a backseat to sight and hearing. This applies to psychopathology as well where problems related to smell are often overlooked. A good example is that of olfactory reference disorder (ORD) or olfactory reference syndrome (ORS) as it used to be popularly called. Olfactory reference disorder is defined as a condition “in which one believes that his or her body emits a foul odour that makes people react in a negative way to their body” [ 1 ]. The presentation encompasses an overlapping phenomenology of overvalued ideas, delusions, somatic preoccupations, anxiety, and obsessive phenomena; hence, slotting it into a particular diagnostic category has been wrought with controversies. The theory that bodily odour is normal and that ORD may represent a higher intensity in its dimension has added to the confusion. ORD in its classical form or as an isolated body odour symptom of another disorder is a common clinical presentation. Though prevalence statistics for the disorder are available in literature, most studies also attach a disclaimer stating that these values are probably underestimated. Hence, the magnitude of this condition is presumably much higher than what is generally quoted. Patients suffer from intense embarrassment and personal distress and turn into social recluses because of ORD. There is also an associated risk of self-harm. Though the condition came to clinical attention several decades ago, our knowledge of the various treatment options remains restricted to case reports and case series. ORD has now been recognised as a prominent psychiatric condition and has found its niche in the recent versions of the classificatory systems.
The aim of this review is to provide an overview of olfactory reference disorder, covering the definition, evolution of the concept and classification, epidemiology, psychopathology and clinical features, comorbidities, diagnosis, differential diagnosis, assessment, treatment, and prognosis.
Evolution of the concept and classification
Descriptions of a clinical condition that resembles the current day ORS date to the 1800s, with cases being reported from Asia, Africa, the USA, Europe, and the Middle East. Several of these were then described as schizophrenia, though they did not meet the full criteria for the disorder. We owe the clinical description and the term olfactory reference syndrome to Pryse-Philips who proposed the same after analysing a large case series [ 1 ]. The condition has received several other monikers, chiefly, parosmia [ 2 ], hallucinations of smell [ 1 ], chronic olfactory paranoid syndrome [ 3 ], and monosymptomatic hypochondriacal psychosis [ 4 ]. It was predominantly conceptualised as a type of delusional disorder [ 5 ].
Despite the clear existence of ORS, it had not been classified separately as a disorder in the earlier versions of the International Classification of Diseases (ICD) or Diagnostic and Statistical Manual (DSM).
In the DSM IIIR, it is described as a common presentation of a “delusional disorder, somatic type”. The DSM IV TR and ICD 10 continued this tradition; the term ORS is not included in either of them. DSM IV makes a reference to ORS in the section on social phobia as well as under its culture-bound syndrome section, with specific mention of the Taijin Kyofusho of Japan [ 5 ].
However, a seminal paper that published a systematic review of 84 cases reported in existing literature, while supporting the existence of ORS, questioned its validity as a delusional disorder. The authors put forth the argument that while the conviction held by some patients (57%) amounts to a delusional level, not all cases are delusional (43%). They posited that the position of the ORS needs to be reconsidered in future classificatory systems [ 6 ].
Despite there being a proposal to include ORD as a separate disorder in the DSM 5, it only achieved a mention under the category “other specified obsessive–compulsive and related disorders”, with a specific mention of the culture-bound variant (Taijin Kyofusho).
ORD has finally come into its own in the ICD 11. It has merited a separate category with a code (6B22) under obsessive–compulsive and related disorders. Furthermore, it has been granted additional insight specifiers (fair to good, poor to absent insight and unspecified).
Another debate that has ranged since long is whether ORD must be classified categorically as a separate entity or conceptualised as a dimensional construct, considering its boundary with normal body odour concerns. One study that attempted to make this distinction assessed a mixed sample of 757 individuals (both community and student participants). Three independent taxometric procedures were conducted on three indicators derived from the Yale-Brown Obsessive–Compulsive Scale Modified for olfactory reference syndrome, namely, ORD obsessions, ORD compulsions, and avoidance. Two of the three revealed a dimensional rather than a categorical structure of ORD. The researchers suggested that in clinical practice, it would be better to view ORD as a dimensional concept while assessing and planning treatment [ 7 ].
Besides, though the neurobiology of ORD as a separate disorder has been poorly researched, an integrated neurobiological approach has been proposed [ 8 ]. ORD incorporates symptoms of various phenomenological types, and it is known that an overlapping circuitry is implicated in the neurobiology of trauma reactions, OCD, and psychotic spectrum disorders. This model also lends credence to the viewing of the ORD phenomenology as dimensional rather than categorical.
The classification of ORD has been summarised in Table 1 .
Epidemiology
The community prevalence of olfactory reference disorder ranges from 0.5 to 2.1%; however, since most of these values are based on self-report of body odour concerns, it is probably a far from accurate value [ 5 ]. There appears to be underreporting from developing nations as well [ 9 ].
Women are affected more, in addition to single individuals. The onset is most often in the mid-twenties [ 6 , 10 ], with some case reports suggesting an earlier age of onset [ 11 ].
The most frequently seen personality traits in these individuals (67%) correspond to the cluster C of the DSM (anxious, perfectionistic, and dependent) [ 6 ]. There is limited evidence to show that some of these patients may have a family history of schizophrenia [ 12 ].
Most patients reach a mental health setting only through a long pathway of care encompassing dentists, dermatologists, gastroenterologists, and, sometimes, even the surgical specialties [ 13 , 14 ]. The delay in clinical care is due to the embarrassing nature of the symptom. If ORD is associated with poor or absent insight, it delays treatment seeking even further.
Psychopathology and clinical features
The core symptom in ORD is a preoccupation with the erroneous belief that one’s body is emitting an offensive smell. Phenomenologically, these beliefs range from overvalued ideas to delusions [ 15 ]. The constant preoccupation also has an obsessive quality to it. The patient describes the odour as foul. One or several body parts may be held responsible as the source of the odour, commonly reported ones being the mouth, axillae, feet, and genital regions. The source may change over time. Rarely, patients report of non-bodily odours such as that of ammonia [ 2 ] or detergent [ 16 ]. Sometimes, the patient may be unable to pinpoint an exact region as the source of smell. The odour is reported to be present all the time. Half of the patients complain of being able to smell the foul odour [ 6 ]. Insight may be varied. In the systematic review previously quoted, 49% of the reports mention a precipitating event/statement, which while appearing to be incongruous at the time seemed to set the patients on a morbid course. These were chiefly smell-related negative experiences (85%) and less often unrelated sources of stress (17%). Common examples reported by patients include “an older sibling quipping that his feet smelled, a colleague turning away once or twice during a conversation, housemates teasing her for breaking wind, had an episode of halitosis during a severe throat infection, etc.” [ 6 ].
In keeping with the name, the belief is also accompanied by referential ideas (74%) that are sometimes of a delusional intensity. They often misinterpret other peoples’ actions, e.g. a couple of colleagues sniffed or took their handkerchiefs out when he was nearby, she was gifted a perfume for her birthday by her classmates, a vacant seat next to her on a bus was not claimed by anybody though the bus was full, friends stopped talking soon as she appeared in the distance, hence they probably had been discussing that she stank, etc. [ 6 ].
As a result, these patients often suffer from intense social anxiety; they avoid close relationships and social contacts or endure them with high levels of embarrassment and distress. In severe cases, they may become house bound [ 6 ].
There are repeated behaviours aimed at checking for, camouflaging, or eliminating the odour that these patients perceive. These could include multiple baths, ritualistic grooming, using deodorants or powder excessively, chewing gum or mints, and making drastic changes in diet. These are often time consuming and add to the social and occupational dysfunction [ 12 ].
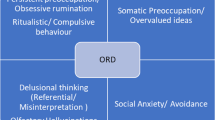
The range of psychopathology seen in ORD is summarised in Fig. 1 .
The range of psychopathology in ORD
A 2011 study of 20 patients diagnosed with ORD assessed them using semi structured measures to gather information about demographic and clinical features. Women constituted 60% of the sample, the mean age being 33.4 ± 14.1 years. The most common sources of the odour were reported from mouth (75%), armpits (60%), and genitals (35%). Delusional ORS beliefs and olfactory hallucinations were the most common (85%) followed by referential thinking (77%). Ninety-five percent of the patients reported repetitive behaviours. Fifty-three percent had undergone psychiatric hospitalisation for the symptoms, 68% reported suicidal ideation, while 32% had a history of attempts at self-harm. Forty-four percent had sought treatment from non-mental health specialists; the treatments received were reported as unhelpful in alleviation of symptoms [ 10 ].
Another Internet-based study that attempted to showcase the phenomenology of ORD obtained data from 253 subjects over a 3-month period in the year 2010. The participants were assessed using questionnaires that were specific to symptoms reported, along with the Depression Anxiety Stress Scales (DASS), Yale-Brown Obsessive–Compulsive Scale Modified for ORS (ORS-YBOCS), and Work and Social Adjustment Scale (WSAS). The age of onset of the illness was found to be an average of 21.1 years, more than half had a chronic course. The source of the odours were the armpits, feet, and breasts. The nature of the odours commonly reported related to stool, garbage, and ammonia. Eighteen percent had poor insight; 64% reported referential delusions. Almost all the patients spent time in repetitive rituals to reduce or hide the perceived odour. Women had greater illness severity. Severity was also associated with poor insight and impairment in work and social relationships [ 17 ].
Comorbidities
Major depression is frequently comorbid, both anxiety and depressive symptoms being prominent in about 40% of patients, often as a reaction to the ORD [ 10 ]. Up to 30% of the patients attempt self-harm, and more than half require hospitalization [ 6 ]. Other comorbid conditions include obsessive–compulsive disorder [ 18 ], social anxiety disorder [ 5 ], body dysmorphic disorder [ 10 ], and substance use disorders [ 10 ].
The frequency of occurrence of these comorbidities is depicted in Table 2 .
According to the ICD-11 criteria, the essential features required to diagnose olfactory reference disorder include the following:
“Persistent preoccupation about emitting a foul or offensive body odour or breath (i.e. halitosis) that is either unnoticeable or slightly noticeable to others such that the individual’s concerns are markedly disproportionate to the smell, if any is perceptible
Excessive self-consciousness about the perceived odour, often including ideas of self-reference (i.e. the conviction that people are taking notice, judging, or talking about the odour)
The preoccupation or self-consciousness is accompanied by any of the following: repetitive and excessive behaviours, such as repeatedly checking for body odour or checking the perceived source of the smell (e.g. clothing), or repeatedly seeking reassurance; excessive attempts to camouflage, alter, or prevent the perceived odour (e.g. using perfume or deodorant, repetitive bathing, brushing teeth, or changing clothing, avoidance of certain foods); marked avoidance of social or other situations or stimuli that increase distress about the perceived foul or offensive odour (e.g. public transportation or other situations of close proximity to other people)
The symptoms are not a manifestation of another medical condition and are not due to the effects of a substance or medication on the central nervous system, including withdrawal effects
The symptoms result in significant distress or significant impairment in personal, family, social, educational, occupational, or other important areas of functioning. If functioning is maintained, it is only through significant additional effort.”
Differential diagnosis
Several medical illnesses may present with a body odour that is objectively verifiable. Common ones include those related to the skin (hyperhidrosis), oral cavity (halitosis and dental abscesses), genital areas (rectal fistulae), and metabolic causes (trimethylaminuria). If the classical features of ORD are not met, then an underlying cause should be considered. Rarely, circumscribed ORD presentations may be a result of illnesses like temporal lobe epilepsy (TLE), arteriovenous malformations, and Parkinson’s disease. Associated olfactory hallucinations are rarely reported in ORD, and their presence must raise the suspicion of a TLE [ 19 ].
Psychiatric differentials include body dysmorphic disorder, obsessive–compulsive disorder, social anxiety disorder, and other delusional disorders of the somatic type. Rarely, a major depression with psychotic symptoms, bodily distress disorder, or an avoidant personality disorder can also present with ORD-like features [ 20 ].
A boundary with normality needs to be considered especially in cultures where fear of emitting offensive odours is a known entity. Both the ICD 11 and the DSM 5 allude to these cultural presentations. One such condition that is popularly described from Japan, Korea, and certain other cultures is the Taijin Kyofusho (Kyofu-fear and Taijin-interpersonal relationships). It is akin to social anxiety and is characterised by an extreme fear that one may offend, hurt, or embarrass others by awkward or unacceptable social behaviour, body movements, or appearance. These could include beliefs about blushing, eye contact, or offensive body odour. The one related to body odour is termed as Jikoshu-Kyofu (Jiko: oneself; Shu: odour, Kyofu: fear).
A study [ 21 ] undertaken in 2004 aimed to clarify the relationship between the Japanese Jikoshu-Kyofu and the Western ORD. A series of seven cases were analysed with specific emphasis on phenomenology and treatment. The researchers found that symptoms, insight, and drug response in the cultural variant were found to be identical to ORD, except when the onset of symptoms had been at a relatively younger age. They questioned the validity of the Jikoshu-Kyofu as a culturally distinctive disorder.
In yet another study from Japan [ 22 ], the authors attempted to trace a possible causal relationship among social anxiety, ORS, pathologic halitosis, and preoccupation with bodily smells. One thousand three hundred sixty female students (19.6 ± 1.1 years) were assessed using a self-administered questionnaire. Statistically significant differences in the results for ORS and social anxiety ( P < 0.001) were found among the various severity grades of pathologic subjective halitosis. Participants with greater severity of pathologic subjective halitosis were found to be more preoccupied with body and mouth odours ( P < 0.05). It was found that social anxiety has a direct influence on both pathologic subjective halitosis and ORS.
Olfactory reference disorder can be differentiated from regular or culture-bound concerns of body odour by the extent of preoccupation, frequency of related rituals carried out, and the severity of distress or interference the individual experiences because of his/her symptoms.
A recent paper [ 23 ] on a case series of four patients with ORS has presented some very interesting findings. The authors measured the olfactory function of the patients using a “University of Pennsylvania Smell Identification Test”. They found that all the patients had a genuine smell impairment, like that observed in patients who have dysosmia or phantosmia due to olfactory epithelium damage. Based on their novel findings, the authors speculated that patients with ORS may have an actual smell perception difficulty.
A detailed clinical history taking will yield the symptoms necessary to make a diagnosis of olfactory reference disorder. If the presentation is atypical, relevant investigations need to be done to rule out underlying medical causes, e.g. an EEG when temporal lobe epilepsy is suspected.
A set of simple screening questions [ 24 ] can help uncover symptoms of ORD. “1. Are you very much concerned about your body odour? 2. Do you spend a lot of time worrying about your body odour? 3. Do you believe that other people perceive the body odour and take special notice of it? 4. Do you have urges to repeatedly do something to reduce the body odour? 5. Do you avoid certain situations due to this body odour? 6. Do these concerns affect your mood or daily life activities?”.
Rating scales that have been commonly employed include the Brown Assessment of Beliefs Scale (BABS) [ 25 , 26 ] which is a seven item clinician administered instrument that assesses insight or delusional thinking across several psychiatric conditions, The Yale Brown Obsessive–Compulsive Scale modified for ORD [ 27 , 28 ] which is a 12-item clinician-rated scale that assesses the severity of the ORD, and the Structured Clinical Interview for identifying disorders of the Obsessive–Compulsive Spectrum (SCID-OCSD) [ 29 ].
The available literature on treatment of ORD is restricted mainly to case reports and case series. There are no randomised controlled trials on the use of psychotropics in ORD. There have been reports of specialists using antidepressants of various classes [ 30 , 31 , 32 , 33 ], both typical and atypical antipsychotics [ 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 ], as well as combinations of antipsychotics and antidepressants [ 42 , 43 , 44 ]. Various degrees of success have been reported with individual and combination therapy. However, there is no investigational proof of whether combined or sequential treatment leads to a more favourable outcome.
Regarding non-pharmacological treatment, case studies have documented response to various modalities, commonly behavioural techniques [ 45 ], eye movement desensitization and reprocessing [ 46 ], and cognitive behavioural therapy [ 47 , 48 , 49 ]. There have also been reports of patients improving with only psychotherapy [ 6 ].
There have also been case reports of patients showing improvement after a course of electroconvulsive therapy (ECT) was added to existing pharmacological management [ 50 ].
The systematic review [ 6 ] quoted in the article found that 33% of the patients improved with antipsychotic agents, while 55% responded well to antidepressant therapy. Only one in five cases showed symptom reduction with ECT, leucotomy did not have any effect on symptoms, and 78% improved with psychotherapy and 45% with varying combinations of treatment options. This lent further support to their argument that ORD must not be considered a delusional disorder.
Given the fact that the perception of the odour is considered a “physical” symptom by the sufferers, most of them may be reluctant to accept the need for psychiatric treatment. This is more pronounced when the ORS is associated with poor insight. However, most sufferers accept that the symptom is distressing and hampers their quality of life. Hence, the first step in offering treatment would be to establish a therapeutic rapport with the patient. The clinician needs to validate the patient’s symptom and, more importantly, the suffering endured. Patients are more likely to accept medications and therapy when offered to alleviate distress and anxiety rather than as a measure to stop the odour.
Data on prognosis of the condition is limited. Case reports and series have not measured treatment outcome or response in a uniform manner; some have relied on rating instruments, while others have simply commented on the symptoms that improved; each has used a different period from start of treatment to document response. Comorbidities have not been systematically examined while reporting response to treatment. In the 2011 systematic review [ 6 ], reduction in the olfactory symptoms was considered as recovery (complete or partial), while reduced preoccupation with the smell and interference in daily life activities was documented as improvement. Of the 84 cases assessed, 76 reported outcome data ranging from 2-week to 10-year follow-up period (average of 21 months). The authors found that 30% of the patients had recovered, 37% showed improvement, and 33% either continued to fare the same or worsened.
Olfactory reference syndrome is a commonly reported clinical condition which can present with varying degrees of insight. Sometimes, the severity of the conviction is almost delusional; at other times, it can present like an overvalued idea or with an associated obsessive component. Researchers have also attempted to view it as a dimensional concept, where concerns about normal body odour are intensified. Cultural variants have been described with components of associated social anxiety. Patients remain preoccupied with the perceived foul smell, often harbour ideas of reference, engage in repeated rituals to cleanse themselves of the odour, experience intense distress because of this condition, and suffer significant impairment in their social and occupational milieu. Like its nosological status, the treatment options also do not seem to be clear cut or conventionally defined. What appears to help the most is the establishment of a strong therapeutic alliance. Several classes of psychotropics alone and in combination have been tried with varying degrees of success, in addition to psychotherapy and electroconvulsive therapy. We need randomised controlled trials to get a clear understanding of effective treatment options.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were created or analysed in this review.
Abbreviations
Olfactory Reference Disorder
Olfactory Reference Syndrome
International Classification of Diseases
Diagnostic and Statistical Manual
Depression Anxiety Stress Scales
Yale-Brown Obsessive–Compulsive Scale Modified for ORS
Work and Social Adjustment Scale
Obsessive–Compulsive Disorder
Body Dysmorphic Disorder
Temporal Lobe Epilepsy
Electro-encephalogram
Brown Assessment of Beliefs Scale
Structured Clinical Interview for identifying disorders of the Obsessive–Compulsive Spectrum
Electroconvulsive therapy
Pryse-Phillips W (1971) An olfactory reference syndrome. Acta Psychiatr Scand 47:484–509
CAS PubMed Google Scholar
Tilley H (1895) Three cases of parosmia: causes, treatment, & C. The Lancet 146(3763):907–908
Google Scholar
Videbech T (1966) Chronic olfactory paranoid syndromes. Acta Psychiatr Scand 42(2):183–213
Munro A (1988) Monosymptomatic hypochondriacal psychosis. Br J Psychiatry 153:37–40
Feusner JD, Phillips KA, Stein DJ (2010) Olfactory reference syndrome: issues for DSM-V. Depress Anxiety 27(6):592–599
PubMed PubMed Central Google Scholar
Begum M, McKenna PJ (2011) Olfactory reference syndrome: a systematic review of the world literature. Psychol Med 41:453–461
Ren F, Zhou R, Zhou X, Schneider SC, Storch EA (2020) The latent structure of olfactory reference disorder symptoms: a taxometric analysis. J Obsessive Compuls Relat Disord 27:100583
Skimming KA, Miller CWT (2019) Transdiagnostic approach to olfactory reference syndrome: neurobiological considerations. Harv Rev Psychiatry 27(3):193–200
PubMed Google Scholar
Osman AA (1991) Monosymptomatic hypochondriacal psychosis in developing countries. Br J Psychiatry 159(3):428–431
Phillips KA, Menard W (2011) Olfactory reference syndrome: demographic and clinical features of imagined body odour. Gen Hosp Psychiatry 33(4):398–406
Ferreira JA, Dallaqua RP, Fontenelle LF, Torres AR (2014) Olfactory reference syndrome: a still open nosological and treatment debate. Gen Hosp Psychiatry 36(6):760–763
Cruzado L, Caceres-Taco E, Calizaya JR (2012) Apropos of an olfactory reference syndrome case. Actas Esp Psiquiatr 40(4):234–8
Miranda-Sivelo A, Bajo-Del Pozo C, Fructuoso-Castellar A (2013) Unnecessary surgical treatment in a case of olfactory reference syndrome. Gen Hosp Psychiatry 35(6):683–684
Aydin M, Harvey-Woodworth CN (2014) Halitosis: a new definition and classification. Br Dent J 217(1):1–10
Jesus G, Gama Marques J, Durval R (2014) EPA-0909 – a review of olfactory reference syndrome about a series of clinical cases. Eur Psychiatry 29:1
Ross CA, Siddiqui AR, Matas M (1987) DSM-III: problems in diagnosis of paranoia and obsessive-compulsive disorder. Can J Psychiatry 32(2):146–148
Greenberg JL, Shaw AM, Reuman L, Shwartz R, Wilhelm S (2016) Clinical features of olfactory reference syndrome: an Internet -based study. J Psychosom Res 80:11–16
Zerzinski M, Burdzik M, Zmuda R, Debski P, Witkowska- Berek A et al (2023) Olfactory obsessions: a study of prevalence and phenomenology in the course of obsessive - compulsive disorder. J Clin Med 12(9):3081
Chen C, Shih YH, Yen DJ, Lirng JF, Guo YC, Yu HY, Yiu CH (2003) Olfactory auras in patients with temporal lobe epilepsy. Epilepsia 44(2):257–260
Lochner C, Stein DJ (2003) Olfactory reference syndrome: diagnostic criteria & differential diagnosis. J Postgrad Med 49(4):328–331
Suzuki K, Takei N, Iwata Y, Sekine Y, Toyoda T, Nakamura K, Mori N (2004). Do olfactory reference syndrome and Jiko-shu-kyofu (a subtype of Taijin-kyofu) share a common entity? Acta Psychiatr Scand 109(2):150–155.
Tsuruta M, Takahashi T, Tokunaga M, Iwasaki M, Kataoka S, Kakuta S et al (2017) Relationships between pathologic subjective halitosis, olfactory reference syndrome, and social anxiety in young Japanese women. BMC Psychol 5:7
Tallab H, Sell EA, Bromley SM, Doty RL (2023) A novel perspective on olfactory reference syndrome and associated specified obsessive-compulsive disorders. Ann Case Rep 8(1):1137–1142
Phillips KA, Castle DJ (2007) How to help patients with olfactory reference syndrome. Curr Psychiatr 6(3):49–65
Eisen JL, Phillips KA, Baer L, Beer DA, la Ata KD, Rasmussen SA (1998) The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry 155:102
Phillips KA, Hart AS, Menard W, Eisen JL (2013) Psychometric evaluation of the Brown Assessment of Beliefs Scale in body dysmorphic disorder. J Nerv Ment 201(7):640–643
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL et al (1989) The Yale-Brown Obsessive-Compulsive Scale: I. Development, use, and reliability. Arch Gen Psychiatry 46:1006–1011
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR et al (1989) The Yale-Brown Obsessive-Compulsive Scale: II. Validity Arch Gen Psychiatry 46:1012–1016
Du Toit PL, van Kradenburg J, Niehaus D, Stein DJ (2001) Comparison of obsessive-compulsive disorder patients with and without comorbid putative obsessive-compulsive spectrum disorders using a structured clinical interview. Compr Psychiatry 42:291–300
Brotman AW, Jenike MA (1984) Monosymptomatic hypochondriasis treated with tricyclic antidepressants. Am J of Psychiatry 141(12):1608–1609
CAS Google Scholar
Balaban OD, BOZ G, Senyasar K, Yazar MS, Keyvan A, Eradamlar N (2015) The olfactory reference syndrome treated with escitalopram: a case report. Marmara Med. J 28:120–122
Alhadi AN, Almaghrebi AH (2018) Challenges in diagnosis and treatment of olfactory reference syndrome: a case study. J Obsessive Compuls Relat Disord 19:23–28
Yoshimura R, Konishi Y, Okamato N, Ikenouchi A (2021) Letter to the Editor: Vortioxetine improved olfactory reference syndrome in a patient with major depressive disorder: a case report. Arch Clin Psychiatry 48(2):128
Ulzen TPM (1993) Letters to the Editor: Pimozide- responsive monosymptomatic hypochondriacal psychosis in an adolescent. Can J Psychiatry 38(2):154–155
Basu D, Bhagat A, Giridhar C, Avasthi A, Kulhara P (1990) Monosymptomatic hypochondriacal psychosis: a clinico-descriptive analysis. Indian J Psychol Med 13(2):147–152
Weintraub E, Robinson C (2000) A case of monosymptomatic hypochondriacal psychosis treated with olanzapine. Ann Clin Psychiatry 12(4):247–249
Nakaya M (2004) Letters to the editor: Olanzapine treatment of monosymptomatic hypochondriacal psychosis. Gen Hosp Psychiatry 26:164–169
Albers AD, Amato I, Albers MW (2018) Olanzapine improved symptoms and olfactory function in an olfactory reference syndrome patient. J Neuropsychiatr Clin Neurosci 30(2):164–167
Ikenouchi A, Terao T, Nakamura J (2004) A male case of monosymptomatic hypochondriacal psychosis responding to olanzapine: a case report. Pharmacopsychiatry 37:240–241
Reddy B, Nocera A, de Filippis R, Das S (2022) Two cases of olfactory reference syndrome treated with risperidone. Neuropsychiatric Invest 60(2):49–51
Elmer KB, George RM, Peterson K, Yokota AB, Langley AFB (2000) Therapeutic update: use of risperidone for the treatment of monosymptomatic hypochondriacal psychosis. Journal Am Acad Dermatol 43:683–686
Karia S, Shrivastava S, DeSousa A, Shah N (2013) Olfactory reference syndrome: a case report. Int J Sci Res 2(9):261
Ozten E, Sayar GH, Tufan AE, Cerit C, Dogan O (2013) Olfactory reference syndrome: treated with sertraline and olanzapine. Sch J Med Case Rep 1(2):44–46
Jegede O, Virk I, Cherukupally K, Germain W, Fouron P, Olupona T, Jolayemi A (2018) Case Report: Olfactory reference syndrome with suicidal attempt treated with pimozide and fluvoxamine. Case Rep Psychiatry 2018:1–3. Article ID 7876497. https://doi.org/10.1155/2018/7876497 .
Milan MA, Kolko DJ (1982) Paradoxical intention in the treatment of obsessional flatulence ruminations. J Behav Ther Exp Psychiatry 13(2):167–172
McGoldrick T, Begum M, Brown KW (2008) EMDR & olfactory reference syndrome: a case series. J EMDR Pract Res 2(1):63–68
Haica C (2021) Olfactory reference syndrome: a case report. Mental Health Human Resilience Int J 5(2):1–7
Martin-Pinchora AL, Antony MM (2011) Successful treatment of olfactory reference syndrome with cognitive behavioral therapy: a case study. Cogn Behav Pract 18:545–554
Zantvoord JB, Vulink N, Denys D (2016) Cognitive behavioural therapy for olfactory reference syndrome: a case report. J Clin Psychiatry 77:9–10
Bhagat H, Bendre A, Dikshit R, DeSousa A, Shah N, Karia S (2017) Olfactory reference syndrome treated with electroconvulsive therapy. Annals Indian Psychiatry 1(2):129–131
Download references

Acknowledgements
Not applicable.
No funding.
Author information
Authors and affiliations.
Department of Psychiatry, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India
Savitha Soman
Sanjivani Multi-Speciality Hospital, Kollakadavu, Chengannur, Kerala, India
Rajesh Nair
You can also search for this author in PubMed Google Scholar
Contributions
Both authors have contributed to the literature review and compilation of the article. The manuscript has been read and approved by both the authors, the requirements for authorship have been met, and each author believes that the manuscript represents honest work.
Corresponding author
Correspondence to Savitha Soman .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Soman, S., Nair, R. Olfactory reference disorder—a review. Middle East Curr Psychiatry 30 , 95 (2023). https://doi.org/10.1186/s43045-023-00367-5
Download citation
Received : 26 July 2023
Accepted : 15 September 2023
Published : 04 December 2023
DOI : https://doi.org/10.1186/s43045-023-00367-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Olfactory Reference Syndrome
- Somatic preoccupation
- Ideas of reference

- From the Experts
These articles are about special topics related to OCD and related disorders. For more general information, please visit our "About OCD" section.
Olfactory Reference Syndrome: Problematic Preoccupation with Perceived Body Odor
by Katharine Phillips, MD
This article was initially published in the Winter 2018 edition of the OCD Newsletter .
Kyle is a 37-year-old single white male who believes that he has severe halitosis (bad breath) and flatulence, which makes him “stinky and smelly.” He states, “I know it’s true, because I can smell it, and why would people touch their face, sniff, and move away from me?” To minimize the awful odor that he is certain he emits, Kyle brushes his teeth for about an hour a day, which has damaged his gums and tooth enamel. He gargles with prescription-strength mouthwash about 20 times a day, wears lots of cologne, changes his underwear many times a day, and washes his clothes twice a day. Because he is embarrassed by the “horrible” odor he believes he emits, Kyle avoids most social situations. He does not date and has dropped out of college. Unable to work, he spends most of his time alone in his apartment. He states, “I have to stay alone, because I stink so much, and if I go out people will make fun of me.”
Kyle is experiencing olfactory reference syndrome (ORS), an underrecognized disorder characterized by preoccupation with the false belief that one emits a foul, unpleasant, or offensive body odor. This preoccupation causes significant distress or impairment in functioning (for example, avoidance of social situations). Although people with ORS believe that they really do smell bad, other people cannot detect the odor. ORS usually triggers excessive, repetitive behaviors such as repeatedly checking oneself for body odor, or excessive clothes laundering. As a result of these concerns, social anxiety and social avoidance are usually prominent, and the odor concerns are so distressing and impairing that suicidal thinking and suicide attempts are common (1-6).
ORS has many similarities to body dysmorphic disorder (BDD), which is characterized by distressing or impairing preoccupation with slight or nonexistent flaws in physical appearance, and obsessive-compulsive disorder (OCD) (2,3,6). Our understanding of ORS and its relationship to other disorders is limited by a lack of research studies. However, ORS is not a new phenomenon; it has been consistently described around the world since the 1800s as a distressing and often severely impairing disorder (2,3,7,8). The largest studies come from Japan, Canada, Nigeria, Saudi Arabia, Brazil, and the United States (1,6,9-13).
DIAGNOSTIC STATUS OF ORS
A Google search of ORS yields approximately 590,000 results, reflecting the public’s interest in this condition. Efforts were made to add ORS to the Diagnostic and Statistical Manual of Mental Disorders, 5 th Edition (DSM-5) (14), but research evidence was considered too limited to include ORS as its own disorder with full diagnostic criteria. Instead, DSM-5 lists ORS as an example of an “Other Specified Obsessive-Compulsive and Related Disorder” (14). DSM-5 provides a very brief description of ORS’s key clinical features, but does not include full diagnostic criteria or discussion of ORS in the text (14). However, the recently published International Classification of Diseases, 11 th Edition (ICD-11), did add ORS as a new, separate disorder in the chapter of Obsessive-Compulsive or Related Disorders, alongside BDD and OCD (see Box) (15). It is hoped that inclusion of ORS in ICD-11 will foster much-needed research studies and enhance understanding and recognition of this often severe and underrecognized condition.
CLINICAL PRESENTATION OF ORS
Preoccupation with Perceived Body Odor
Individuals with ORS are excessively preoccupied with the belief that they emit an unpleasant or foul body odor, most commonly bad breath or sweat (see Table 1). They believe that the foul odor emanates from body areas that correspond to the type of odor — for example, bad breath from the mouth or sweat from the armpits or skin. Occasionally, the perceived odor may smell like non-bodily odors, such as ammonia, detergent, or rotten onions. Most — but not all — people with ORS report actually smelling the odor.
Insight and Referential Thinking
Most people with ORS are completely convinced that they actually smell terrible, despite the fact that other people cannot detect an odor; very few recognize that their belief about the body odor is inaccurate (6). The likely explanation for this mistaken perception is that most people with ORS report that they actually smell the odor themselves (see Table 1) (6).
Alternatively, those who do not smell the odor base their belief on a misinterpretation of other people’s comments, gestures, or behaviors. For example, if someone opens a window, touches their nose, moves away, or says “It’s stuffy in here,” people with ORS typically — and mistakenly — believe that their unpleasant body odor is the reason for such behavior (see Table 1). This inaccurate belief that other people are taking special notice of them in a negative way because they smell bad is known as referential thinking (or as ideas or delusions of reference).
Excessive Repetitive Behaviors
People with ORS experience their preoccupation with body odor as highly distressing, and it triggers upsetting feelings such as depressed mood, anxiety, and self-consciousness. For this reason, nearly everyone with ORS feels compelled to perform repetitive behaviors intended to mitigate, check, mask, or reassure themselves about their perceived odor. The most common behaviors are smelling oneself, excessive showering, and frequent clothes changing (see Table 1).
Camouflaging the Perceived Odor
People with ORS attempt to mask the perceived body odor, most often with excessive perfume or powder, chewing gum, excessive or strong deodorant, or mints (see Table 1). This behavior can occur repeatedly throughout the day.
Functional Impairment
ORS typically impairs functioning, which can range from mild to extreme; on average, impairment is severe in clinical samples of individuals with ORS (6). Nearly three-quarters of people with ORS report periods during which they avoided most social interactions because of their ORS symptoms, and about 50% report periods during which they avoided most of their important occupational, academic, or life activities because of ORS symptoms (6) (see Table 1). Some people are completely housebound because they feel too distressed, self-conscious, and embarrassed about the perceived odor to be around other people, or because they fear offending others with their smell.
High rates of psychiatric hospitalization, suicidal thoughts, suicide attempts, and completed suicide have been reported, which many individuals attribute primarily to their ORS symptoms (see Table 1) (1,6).
Comorbidity
Commonly co-occurring disorders are a major depressive disorder, social anxiety disorder, drug or alcohol use disorders, obsessive-compulsive disorder, and body dysmorphic disorder (6).
PREVALENCE AND DEMOGRAPHIC CHARACTERISTICS
In one study, 60% of individuals with ORS were female, and most were single (6). The prevalence of ORS is not known, but it is certainly more common than generally recognized (2,3,16).
WHAT CAUSES ORS?
The cause of ORS has not been studied and thus is not known. Like other psychiatric disorders, its cause likely has many genetic and environmental determinants. ORS has similarities to BDD, OCD, and social anxiety disorder, and thus it may share some etiologic and pathophysiologic characteristics with these disorders. For example, ORS may involve abnormalities in the brain’s olfactory system that cause olfactory hallucinations or extreme sensitivity to odors. However, this theory has not been studied, and it likely is not relevant to the minority of those with ORS who do not actually smell the odor.
TREATMENT FOR ORS
No prospective medication studies have been done (either controlled or open-label studies). Case reports and small case series describe improvement with serotonin reuptake inhibitor (SRI) monotherapy, neuroleptic (antipsychotic) monotherapy, non-SRI antidepressants (such as tricyclic antidepressants), or a combination of a neuroleptic and antidepressant medication (2-4). In the author’s clinical experience, SRIs at high doses often effectively treat ORS.
Psychotherapy
Reports on psychotherapy are similarly limited to single case reports and small case series, which report improvement with behavioral therapy, cognitive behavioral therapy, and paradoxical intention (2-4). In the author’s experience, cognitive behavioral therapy – consisting of cognitive restructuring and advanced cognitive strategies for core beliefs, including self-esteem work and self-compassion; ritual prevention; and exposure-based exercises along with behavioral experiments that are tailored to ORS symptoms – can be effective. ORS’s clinical features appear most similar to those of BDD, and an evidence-based CBT treatment manual for BDD can be easily adapted to treat ORS symptoms (17).
Non-Mental Health Medical Treatment
Nearly half of people with ORS seek non-mental health medical treatment for their perceived body odor (6), many before seeking mental health care (18); in one study, one third of people actually received such treatment (6). Patients may consult dentists, surgeons, and ear, nose, and throat specialists for supposed halitosis; proctologists, surgeons, and gastroenterologists for supposed anal odors; and other physicians such as dermatologists and gynecologists. Treatments such as a tonsillectomy for perceived bad breath or electrolysis of sweat glands for a perceived sweaty smell may be received. Such treatment does not appear to be effective for ORS symptoms and often leaves patients dissatisfied (6).
A neurologic workup, which may include an EEG, may sometimes be warranted to rule out a neurologic explanation (such as temporal lobe epilepsy or migraine aura) for perception of an odor that others cannot detect. This kind of evaluation is more relevant when concerns focus on nonbodily odors and occur only intermittently.
RECOMMENDATIONS FOR CLINICAL CARE
Current understanding of ORS is substantially limited by the very small number of published research studies on this condition. Nonetheless, it is important for clinicians and the public to be aware of ORS. Table 2 provides some clinical recommendations, based on current research-based knowledge about ORS and the author’s clinical experience. More research studies on all aspects of ORS are greatly needed to advance the understanding and treatment of this condition.
TABLE 1: Key Clinical Features of Olfactory Reference Syndrome
| Clinical Feature | % of Patients, or Mean ± Standard Deviation |
|---|---|
| Mouth | 75.00% |
| Armpits | 60.00% |
| Genitalia | 35.00% |
| Anus | 30.00% |
| Feet | 30.00% |
| Skin | 25.00% |
| Groin | 10.00% |
| Hands | 10.00% |
| Head/Scalp | 10.00% |
| Under Breasts | 5.00% |
| Total different # of sources | 2.9 ± 1.4 |
| Bad breath | 75.00% |
| Sweat | 65.00% |
| Other smell | 65.00% |
| Flatulence/Fecal | 30.00% |
| Urine | 20.00% |
| Vaginal | 10.00% |
| Olfactory hallucinations | 85.00% |
| Level of insight (Brown Assessment of Beliefs Scale [BABS]) | 20.6 ± 3.7 (delusional/absent insight range) |
| Insight (% with delusional/absent insight on BABS) | 84.60% |
| Referential thinking (ideas or delusions of reference; lifetime) | 88.30% |
| Smelling self | 80.00% |
| Showering | 68.40% |
| Changing clothes | 50.00% |
| Seeking reassurance | 45.00% |
| Dieting/unusual food intake | 45.00% |
| Brushing teeth | 40.00% |
| Laundering clothes | 30.00% |
| Comparing to other people | 30.00% |
| Other behavior | 30.00% |
| At least one compulsive behavior | 95.00% |
| Total # of compulsive behaviors | 4.2 ± 2.0 |
| Perfume/Fragrance/Powder | 70.00% |
| Gum | 60.00% |
| Deodorant | 55.00% |
| Mints | 55.00% |
| Mouthwash | 50.00% |
| Toothpaste | 30.00% |
| Clothes | 25.00% |
| Other6 | 25.00% |
| At least one item used to mask odor | 100.00% |
| Total # of items used to mask odor | 4.0 ± 2.2 |
| Age of ORS onset | 15.6 ± 5.7 |
| ORS onset | |
| One set of odor(s) that started at same time and did not change | 38.90% |
| New odors added to ongoing previous odors | 44.40% |
| Complex additions and remissions of odors | 16.70% |
| Functional Impairment Attributed to ORS (lifetime) | |
| Avoidance of social interactions | 73.70% |
| Avoidance of occupational/academic/role activities | 47.40% |
| Housebound for at least 1 week | 40.00% |
| GAF (Global Assessment of Functioning) (current) | 47.5 ± 13.2 |
| History of suicidal ideation | 68.40% |
| History of suicidal ideation attributed primarily to ORS | 47.40% |
| Attempted suicide | 31.60% |
| Attempted suicide primarily due to ORS | 15.80% |
| History of physical violence | 50.00% |
| History of physical violence attributed primarily to ORS | 21.40% |
| Psychiatric hospitalization | 52.60% |
| Psychiatric hospitalization attributed primarily to ORS | 31.60% |
Table Notes
- Table is adapted from Phillips KA, Menard W. Olfactory reference syndrome: demographic and clinical features of imagined body odor. General Hospital Psychiatry 2011;33:398-406
- Total is greater than 100% because some patients reported multiple odors, odors that emanated from multiple body areas, multiple repetitive behaviors, or multiple masking strategies.
- Other smells were (n=1 for each): “like wearing sanitary napkins too long,” “unpleasant vaginal odor,” ammonia, “bad,” “body odor/mucus/post nasal drip,” “body odor/rotten odor/morning breath,” “hard/unpleasant smell,” “like 5 day-old food and cigarette smoke,” oily-fishy smell,” and “vegetable soup/putrid body (odor).”
- The Brown Assessment of Beliefs Scale (BABS) classifies false beliefs as characterized by excellent, good, fair, poor, or absent insight/delusional belief (19,20). On the BABS, mean scores for ORS are in the absent insight/delusional range, for BDD are in the poor insight range, and for OCD are in the good insight range.
- Other excessive behaviors were as follows; scrapes tongue/coughs to remove bacteria on tonsils/talks softly/uses feminine wash, scrapes back of tongue/checks tonsils to pull mucous off them, uses spoon to scrape skin on tongue and inside of mouth, checks breath by blowing into nose/drinking water, frequent haircuts/avoids hats, drinks lots of fluids.
- Other items/behaviors used to mask the odor were as follows (n=1 for each); spraying alcohol on self and furniture/wearing heavy underwear, putting cornstarch under feet, putting toilet paper in underwear, crossing legs/putting toilet paper in underwear, using air fresheners.
- The mean GAF score reflects serious symptoms or serious functional impairment.
- Physical violence was defined as motor behavior that physically injured another person or caused significant property damage.
TABLE 2: Key Recommendations for Clinical Practice 1
| Be familiar with ORS and its clinical features; it is more common than generally recognized. |
| Do not assume that ORS is simply a symptom of another psychiatric condition, such as depression, a psychotic disorder, BDD, or OCD; focus specifically on ORS when providing treatment. |
| Screen patients for ORS, especially those with high levels of social anxiety or social avoidance, referential thinking, or performance of the repetitive or camouflaging behaviors in Table 1. |
| For selected patients, consider a neurologic workup to rule out a neurologic explanation for olfactory hallucinations, such as temporal lobe epilepsy. |
| Medication is strongly recommended for patients with more severe ORS symptoms, especially those who are very impaired in terms of functioning, are severely depressed, or are more highly suicidal. Medication is also a good option when symptoms are mild or moderate in severity, especially if co-occurring disorders are present that may respond to similar medication (such as BDD, OCD, social anxiety disorder, or depression). |
| Serotonin-reuptake inhibitors — at high doses if lower doses are not effective — are recommended as the first-line medication for ORS (similar to BDD and OCD). |
| Atypical neuroleptics (such as aripiprazole or risperidone) may potentially be helpful in combination with an SRI (similar to BDD and OCD). These medications should especially be considered if an adequate trial with an SRI is not sufficiently helpful or if problematic agitation, very severe depression, marked impairment in functioning, worrisome suicidal thinking, or suicidal behavior are present. |
| Cognitive-behavioral therapy that is tailored to ORS is also recommended, especially for more severe ORS symptoms. It is also a good option when symptoms are mild or moderate in severity. Core components of CBT appear to consist of cognitive therapy, exposure with behavioral experiments, and ritual prevention. |
| Given the presence of obsessions, repetitive behaviors (rituals), poor or absent ORS-related insight, depressive symptoms (usually present), and often-prominent social anxiety and avoidance, CBT for ORS appears most similar to that for BDD. In the author’s experience, an evidence-based treatment manual for BDD can easily be modified to effectively treat ORS17. |
| Many individuals with ORS desire non-mental health medical treatment for ORS concerns, such as removal of sweat glands or a tonsillectomy, which does not appear to be effective. |
| Because ORS-related insight is usually absent (i.e., ORS beliefs are usually delusional in nature), and because many individuals with ORS desire non-mental health medical treatment for ORS concerns, motivational interviewing is often needed to engage and retain patients in mental health treatment. |
Because research evidence on ORS is very limited, these recommendations are also based on the author’s clinical experience with ORS and may change as research studies are done.
Katharine A. Phillips, MD is Professor of Psychiatry at Weill Cornell Medical College, Cornell University; an Attending Psychiatrist at New York-Presbyterian Hospital; and an Adjunct Professor of Psychiatry and Human Behavior at the Alpert Medical School of Brown University. Dr. Phillips is also a member of the IOCDF Scientific and Clinical Advisory Board, a contributing member to the IOCDF www.HelpforBDD.org website, and a regular presenter at the Annual OCD Conference. Please address correspondence to: Katharine Phillips, MD, Weill Cornell Psychiatry Specialty Center, 315 East 62nd Street, New York, NY 10065; Telephone: 646-962-2820; Fax: 646-962-0175; email: [email protected]
- Pryse-Phillips W. (1971). An olfactory reference syndrome. Acta Psychiatr Scand, 47:484–509.
- Phillips KA, Gunderson C, Gruber U, Castle DJ. (2006). Delusions of body malodor: the olfactory reference syndrome. In: Brewer W, Castle D, Pantelis C, editors. Olfaction and the Brain. Cambridge: Cambridge University Press; pp. 334–353.
- Feusner JD, Phillips KA, Stein DJ. (2010). Olfactory reference syndrome: issues for DSM-V. Depress Anxiety, 27:592–599.
- Phillips KA, Castle DJ. (2007). How to help patients with olfactory reference syndrome. Curr Psychiatr, 6:49–65.
- Begum M, McKenna PJ. (2010). Olfactory reference syndrome: a systematic review of the world literature. Psychol Med, 1–9.
- Phillips KA, Menard W. (2011). Olfactory reference syndrome: demographic and clinical features of imagined body odor. Gen Hosp Psychiatry, 33:398-406.
- Potts CS. (1891). Two cases of hallucination of smell. U Penn Med Mag, 226.
- Tilley H. (1895). Three cases of parosmia: causes and treatment. Lancet, 907–908.
- Yamada M, Shigemoto T, Kashiwamura KI, Nakamura Y, Ota T. (1977). Fear of emitting bad odors. Bull Yam Med School, 24:141–161.
- Prazeres AM, Fontenelle LF, Mendlowicz MV, de Mathis MA, Ferrão YA, de Brito NF, et al. (2010). Olfactory reference syndrome as a subtype of body dysmorphic disorder. J Clin Psychiatry, 71:87–89.
- Iwu CO, Akpata O. (1990). Delusional halitosis. Review of the literature and analysis of 32 cases. Br Dent J, 168:294–296.
- Osman AA. (1991). Monosymptomatic hypochondriacal psychosis in developing countries. Br J Psychiatry, 159:428–431
- Greenberg J, Shaw AM, Reuman L, Schwartz R, Wilhelm S. (2016). Clinical features of olfactory reference syndrome: an internet-based study. J Psychosom Res, 80:11-6.
- Diagnostic and Statistical Manual for Mental Disorders, 5 th Edition. (2013). Arlington, VA; American Psychiatric Association.
- https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1119008568
16. Zhou X, Schneider SC, Cepeda SL, Storch EA. (2018). Olfactory reference syndrome symptoms in Chinese university students: Phenomenology, associated impairment, and clinical correlates. Compr Psychiatry, 86:91-95.
17. Wilhelm S, Phillips KA, Steketee G. (2013). Cognitive-Behavioral Therapy for Body Dysmorphic Disorder: A Treatment Manual. New York, NY: Guilford Press.
- Greenberg JL, Berman NC, Braddick V, Schwartz R, Mothi SS, Wilhelm S. (2018). Treatment utilization and barriers to treatment among individuals with olfactory reference syndrome (ORS). J Psychosom Res, 105:31-36.
- Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA. (1998). The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry, 155:102-108.
- Phillips KA, Hart A, Menard W, Eisen JL. (2013). Psychometric evaluation of the Brown Assessment of Beliefs Scale in body dysmorphic disorder. J Nerv Ment Dis, 201:640-643.
In This Section
More resources.
- Fact Sheets & Brochures
- Books About OCD
- Educational Resources
Search iocdf.org
Your gift has the power to change the life of someone living with ocd..
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Olfactory Reference Syndrome: Issues for DSM-V
Jamie d. feusner.
1 Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine at University of California, Los Angeles, USA
Katharine A. Phillips
2 Butler Hospital and the Department of Psychiatry and Human Behavior, Alpert Medical School of Brown University, USA
Dan J. Stein
3 Department of Psychiatry, University of Cape Town, South Africa
The published literature on olfactory reference syndrome (ORS) spans more than a century and provides consistent descriptions of its clinical features. The core symptom is preoccupation with the belief that one emits a foul or offensive body odor, which is not perceived by others. This syndrome is associated with substantial distress and disability. DSM-IV and ICD-10 do not explicitly mention ORS but note convictions about emitting a foul body odor in their description of delusional disorder, somatic type. However, the fact that such symptoms can be non-delusional poses a diagnostic conundrum. Indeed, DSM-IV also mentions fears about the offensiveness of one’s body odor in the social phobia text (as a symptom of taijin kyofusho). There also appears to be phenomenological overlap with body dysmorphic disorder, obsessive-compulsive disorder, and hypochondriasis. This paper provides a focused review of the literature to address issues for DSM-V, including whether ORS should continue to be mentioned as an example of another disorder or should be included as a separate diagnosis. We present a number of options and preliminary recommendations for consideration for DSM-V. Because research is still very limited, it is unclear how ORS should best be classified. Nonetheless, classifying ORS as a type of delusional disorder appears problematic. Given this syndrome’s consistent clinical description across cultures for more than a century, substantial morbidity, and a small but growing research literature, we make the preliminary recommendation that ORS be included in DSM-V’s Appendix of Criteria Sets Provided for Further Study, and we suggest diagnostic criteria.
INTRODUCTION
This paper focuses on some key issues pertaining to the classification of olfactory reference syndrome (ORS), a condition in which individuals erroneously believe that they emit an unpleasant, foul, or offensive body odor. Odors include almost anything foul-smelling and are often believed to originate from the mouth, genitals, rectum, or skin [ 1 ]. Common specific concerns include halitosis, genital odor, flatulence or anal odor, or sweat [ 2 ]. Occasional patients report emitting non-bodily odors such as ammonia [ 3 ], detergent [ 4 ], or rotten onions [ 5 ]. This belief is often accompanied by ideas or delusions of reference – i.e., the belief that other people take special notice of the odor in a negative way (for example, rub their nose in reference to the odor or turn away in disgust). In addition, many patients perform repetitive behaviors, such as smelling themselves, showering excessively, and attempting to mask the odor [ 6 ].
In this paper, we first summarize the history of ORS’s classification to provide a context for the issues discussed. We then address several key issues that are specifically relevant to DSM-V. This paper was commissioned by the DSM-V Anxiety, Obsessive-Compulsive Spectrum, Post-Traumatic, and Dissociative Disorders Work Group. It represents the work of the authors for consideration by the work group. Recommendations provided in this paper should be considered preliminary at this time; they do not necessarily reflect the final recommendations or decisions that will be made for DSM-V, as the DSM-V development process is still ongoing. It is possible that this paper’s recommendations will be revised as additional data and input from experts and the field are obtained.
HISTORY OF THE CLASSIFICATION OF ORS
Published descriptions of ORS date back to the late 1800s [ 2 , 3 , 7 – 11 ]. Several hundred cases from around the world have been reported, including Europe, the U.S., Asia, the Middle East, and Africa. Between 1891 and 1966 multiple cases consistent with this syndrome appear in the literature [ 3 , 7 , 10 – 14 ]. Many of these were described as schizophrenia, although the clinical descriptions did not contain signs and symptoms sufficient to meet criteria. In 1971 Pryse-Phillips noticed this, and after characterizing a large case series and carefully considering the differential diagnosis, coined the term olfactory reference syndrome for a separate group with consistent phenomenology [ 6 ]. Other terms that have appeared in the literature include delusions of bromosis, hallucinations of smell, chronic olfactory paranoid syndrome, and olfactory delusional syndrome, among others [ 2 ]. It has also been referred to as a type of monosymptomatic hypochondriacal psychosis based on the observation that it involves a single delusional belief [ 15 – 19 ].
ORS has never been classified as a separate disorder in DSM or the International Classification of Disease (ICD). DSM-III-R mentioned ORS in the text, stating that “convictions that the person emits a foul odor…are one of the most common types of delusional disorder, somatic type” [ 20 ]. Similarly, DSM-IV considers ORS a type of delusional disorder, somatic type, although the term “olfactory reference syndrome” is not mentioned. The DSM-IV text states: “Somatic delusions can occur in several forms. Most common are the person’s conviction that he or she emits a foul odor from the skin, mouth, rectum, or vagina….” [ 1 ]. Similarly, in its section on persistent delusional disorders, ICD-10 does not use the term “olfactory reference syndrome,” but the text notes that delusions may “express a conviction that…others think that he or she smells….” [ 21 ].
DSM-IV also implicitly refers to ORS in the text for social phobia, in the section on “specific culture, age, and gender features.” Here the text states: “In certain cultures (e.g., Japan and Korea), individuals with Social Phobia may develop persistent and excessive fears of giving offense to others in social situations….These fears may take the form of extreme anxiety that blushing, eye-to-eye contact, or one’s body odor will be offensive to others ( taijin kyofusho in Japan).” Similarly, the DSM-IV section on culture-bound syndromes implicitly refers to ORS, again under the rubric of taijin kyofusho , which is included in the official Japanese diagnostic system for mental disorders [ 1 ].
STATEMENT OF THE ISSUES
- Should ORS continue to be mentioned as an example of another disorder, such as delusional disorder, social phobia, or another disorder? Or should it instead be included as a separate diagnosis in DSM-V?
- If ORS is included as a separate disorder, what should its diagnostic criteria consist of?
SIGNIFICANCE OF THE ISSUES
ORS has been described as a discrete syndrome across many cultures for more than a century. However, its clinical features are confusingly mentioned in three different sections of DSM-IV, and they are not adequately described. Furthermore, the term ORS (currently the most widely used term for this syndrome) is not explicitly mentioned. Given the suffering and impairment associated with ORS, it is important to examine its classification in DSM-V.
SEARCH METHODS
To identify published articles on ORS, we used PubMed, WebofScience, and PsychInfo databases with the keywords “olfactory reference syndrome”; “olfactory paranoid syndrome”; “monosymptomatic hypochondriasis” and “olfactory”; “taijin kyofu” and “olfactory”; “taijin kyofusho” and “olfactory”; “jiko-shu-kyofu”; “delusional halitosis”; “psychosomatic halitosis”; “olfactory hallucination”; “hallucinations of smell”; “olfactory delusional syndrome”; “olfactory delusional disorder”; “olfactory paranoia”; “olfactory hypochondriasis”; “monosymptomatic hypochondriacal psychosis” and “olfactory”; “delusion” and “smell”; “delusions of bromosis”; and “bromidrosiphobia.” Additional relevant articles identified from reference lists were also included [ 2 – 4 , 7 , 11 – 13 , 17 , 19 , 22 – 28 ]. Only peer-reviewed manuscripts published in the English language were included. Articles that appeared in these searches but did not provide any data or clinical description of ORS were excluded (n=7). Two recently published reviews on ORS, one from a book [ 2 ] and one from a professional journal [ 8 ], were also included. The DSM-IV Sourcebook and DSM-IV Options Book were also reviewed.
Sixty journal articles [ 2 – 8 , 11 – 16 , 19 – 69 ], and 4 book chapters [ 2 , 12 , 25 , 26 ] fit the inclusion criteria. Fifty-nine of the journal articles were case reports or case series, some in combination with reviews of the literature, and one was a literature review without a case report [ 29 ]. The four largest published reports contain systematically described patients from Japan (N=38), Canada (N=36), Nigeria (N=32), and Saudi Arabia (N=15) [ 6 , 18 , 28 , 30 ]. Recently analyzed data from a series of 20 cases of ORS (primarily outpatients) in the U.S. are also included (Phillips KA, unpublished data), because cases were systematically assessed with the Structured Clinical Interview for DSM and certain other standard measures that were not used in previously published studies.
1) Should ORS continue to be mentioned as an example of another disorder, such as delusional disorder, social phobia, or another disorder, or should it instead be included as a separate diagnosis in DSM-V?
To examine whether or not a syndrome is distinct from other disorders, the DSM-V process has focused on validators such as symptom profile; familial aggregation; environmental risk factors; cognitive, emotional, temperament, and personality correlates; biological markers; patterns of comorbidity; course of illness: and response to treatment. Unfortunately, for ORS, there is a lack of empirical data for most of these validators. However, there are some early data to suggest that ORS does appear to differ in important ways from other disorders in terms of its symptom profile, comorbidity, and response to treatment.
We will first consider whether ORS should be classified as a type of delusional disorder, as in DSM-IV. This requires consideration of whether ORS beliefs are delusional in nature. Data on this issue are limited. Most published case reports include patients with delusional beliefs (i.e., complete conviction of emitting a foul or offensive body odor). However, the literature contains reports of patients whose beliefs were not delusional – that is, the person recognized that he/she might not actually be emitting a noticeable odor. Osman (1991) noted that overvalued ideation may occur rather than delusions, and Suzuki et al. (2004) reported that 3 of 7 patients in their series had good insight [ 31 ]. Other authors have also commented on the existence of non-delusional forms of ORS [ 16 , 18 , 32 ]. In a recently analyzed data set, which used the reliable and valid Brown Assessment of Beliefs Scale [ 33 ] to assess delusionality/insight of ORS beliefs, 84.6% of patients with current ORS currently had delusional ORS beliefs; 15.4% had nondelusional ORS beliefs (good to poor insight) [Phillips, unpublished data]. Thus, ORS beliefs may not always be delusional and in such cases would not meet criteria for delusional disorder.
An additional consideration is that the DSM-IV definition of delusional disorder requires the total duration of any concurrent mood episodes to be brief relative to the duration of the delusional periods [ 2 ]. Depression is the most commonly reported comorbid disorder or symptom [Phillips, unpublished data], and it is often considered secondary to ORS [ 6 , 32 ]. Data are lacking on the duration of delusional ORS symptoms versus duration of concurrent mood episodes. However, clinical experience suggests that patients with ORS often have prolonged depressive episodes. In the majority of cases, these episodes appear after the development of odor concerns [ 6 ] [Phillips, unpublished data] and may be secondary to the distress and suffering that ORS causes. Thus, this delusional disorder criterion may not be suitable for ORS.
Although controlled studies are lacking, patterns of response to pharmacotherapy reported in the literature also suggest that ORS is probably not simply a type of delusional disorder. Several case reports and series describe response to antipsychotic monotherapy, particularly pimozide [ 18 , 34 ], but multiple case reports and series describe improvement with serotonin reuptake inhibitor (SRI) monotherapy [ 35 – 38 ]. Some individuals did not respond to an antipsychotic but did respond to an SRI [ 35 ]. Other reports describe response to non-SRI antidepressants, such as tricyclic antidepressants [ 39 , 40 ]. And yet others describe improvement with a combination of an antipsychotic and antidepressant medication [ 18 , 32 , 41 ].
Might ORS be a form of a disorder other than delusional disorder? Available data on this issue are also very limited. Some published reports included individuals with comorbid Axis I conditions, with the authors providing evidence as to how the ORS symptoms were phenomenologically and/or temporally distinct from the other conditions [ 41 – 45 ].
ORS appears to have some features in common with social phobia, and is considered a form of taijin kyofusho in Japan and Korea. Taijin kyofusho is considered a culturally bound syndrome in which individuals fear that their body or bodily functions may displease, embarrass, or be offensive to others in terms of appearance, odor, facial expressions, or movements [ 1 ]. An estimated 17% of individuals with taijin kyofusho have fears of emitting body odor [ 46 ], although this is one of only several fears in this syndrome (see also the review for DSM-V of culture and anxiety disorders, [Lewis-Fernández et al., under review]). The literature suggests that most individuals with ORS are concerned about the social implications of emitting a foul odor, with patients commonly experiencing shame, embarrassment, and anxiety in social situations, as well as avoidance of social situations [ 36 ]. Some fear offending others with their odor [ 47 ]. One small study that directly compared individuals with ORS symptoms to those with social phobia found similarities in demographics, comorbidity with depression, and symptom scores on social phobia ratings scales (although the study was underpowered to detect differences between groups). However, the key characteristic of social phobia is the fear that one will act in a way that will be embarrassing or humiliating; thus, patients are typically primarily concerned about how they speak (or eat, write, etc.) rather than how they smell. Another apparent difference between ORS and social phobia is the often-delusional nature of the core belief in ORS. In addition, it appears that most individuals with ORS perform excessive, repetitive behaviors that are compulsive in nature. The intent of these behaviors is usually to check or eliminate the perceived odor, obtain reassurance about it, or prevent others from smelling it. Examples include checking their body for odor; excessive showering or other washing; or repetitive use of deodorant, mouthwash, or perfume [ 6 , 16 , 32 , 48 ]. In the above-noted sample, 95% of subjects performed at least one such behavior (Phillips, unpublished data).
These behaviors raise the question of whether ORS may be related to OCD. Another similarity with OCD is that individuals with ORS usually report troubling, repetitive, and intrusive thoughts about their “odor,” which some describe as obsessive [ 12 , 18 , 49 ]. Indeed, sufferers may spend many hours per day preoccupied with these thoughts [ 49 ], [Phillips, unpublished data]. These symptoms, in addition to case reports of ORS symptoms responding to SRIs [ 35 , 38 , 50 ], has led some to posit a relationship between ORS and OCD [ 2 ]. However, ORS appears to differ from OCD in that OCD beliefs are delusional in fewer than 5% of cases, and ideas/delusions of reference appear less common in OCD than in ORS [ 51 – 53 ]. In addition, available data, while very preliminary, suggest that comorbidity patterns may differ, with comorbid major depressive disorder and social phobia more common in ORS [Phillips, unpublished data] [ 54 ].
More than 20 years ago, Isaac Marks noted that ORS’s clinical features have many similarities to body dysmorphic disorder (BDD); the primary symptoms of both disorders involve a belief of a bodily defect which leads to anxious avoidance of relevant (often social) situations [ 36 ]. Other similarities include preoccupation and repetitive behaviors to check or remediate the perceived problem [ 2 , 15 , 16 , 40 , 42 , 48 , 55 ]. In addition, both disorders are characterized by frequent seeking of non-mental health medical treatment in an attempt to alleviate the symptoms. Examples include surgery and dermatologic treatment in BDD, and treatment from dentists and gastroenterologists in ORS [ 16 , 18 , 30 , 32 , 42 ]. However, BDD and ORS have some apparent differences. The content of the core beliefs, many of the repetitive behaviors, and treatment response may all differ [ 2 ]. In addition, available preliminary data (while very limited) suggest that ORS is more often characterized by current delusional beliefs (about odor in ORS [85%] and appearance in BDD [36–60%]), current ideas or delusions of reference (77% in ORS vs 38% in BDD), and more frequent lifetime comorbidity with DSM-IV social phobia (65% in ORS vs 37%–39% in BDD) [ 56 – 58 ] [Phillips KA, unpublished data].
Finally, there are apparent similarities with other somatoform disorders, primarily hypochondriasis. Both disorders involve preoccupation with the body, are often marked by obsessional thinking, and include repetitive behaviors such as checking and seeking medical diagnoses and treatments [ 1 ]. However, unlike ORS, in hypochondriasis the core fear is about having a serious disease. Moreover, unlike hypochondriasis, ORS is typically characterized by prominent ideas/delusions of reference and social avoidance.
We will now address issue #1 from a different perspective, which is whether ORS should be included as a diagnosis in DSM-V, separate from delusional disorder or another mental disorder. First, we draw in part on recent considerations for what constitutes a mental disorder, while also considering ongoing discussion in the literature on this topic [e.g., [ 59 , 60 ]. We then address several additional considerations for adding a disorder to the nomenclature [ 61 ].
1) The condition is a behavioral or psychological syndrome or pattern that occurs in an individual
As detailed above, ORS has long been recognized in the psychiatric literature as a syndrome that occurs in individuals, and it has been described in multiple regions of the world.
2) The consequences of which are clinically significant distress or disability
The literature consistently indicates that ORS causes clinically significant limitations in functioning or distress. A number of authors have noted significant social disability associated with ORS. In Pryse-Phillips’ case series, only 3% of patients were “socially active” [ 6 ]. Prominent social avoidance and isolation appears common, which is usually attributed to shame, embarrassment, and/or concern about offending others with the odor [ 6 , 16 , 32 , 42 ]. Impairment of work or school functioning is also common [ 6 , 16 , 32 , 42 ]. This, too, is often noted to be due to avoidance of other people because of shame, embarrassment, or concern about offending others with the perceived odor, or it may result from time spent preoccupied with thoughts about the odor and engaging in behaviors to check or minimize it [ 2 ]. In a small recently analyzed data set, ORS symptoms had caused 74% of subjects to avoid social situations, and 47% to avoid occupational, academic, or other important role activities [Phillips, unpublished data]. Forty percent reported that they had been completely housebound for at least one week because of ORS symptoms. The mean score on the Global Assessment of Functioning Scale among those with current ORS was 47.5 (SD=13.2). A majority of subjects (52.6%) reported a history of psychiatric hospitalization, with 31.6% of the sample reporting that they had been psychiatrically hospitalized primarily because of ORS symptoms. Furthermore, 68% of subjects had a history of suicidal ideation, 47% reported lifetime suicidal ideation that they attributed primarily to the distress caused by ORS symptoms, 32% had attempted suicide, and 16% had made at least one suicide attempt that they attributed primarily to ORS [Phillips, unpublished data]. Of Pryse-Phillips’ 36 subjects, 43% experienced “suicidal ideas or action” and 5.6% committed suicide over the follow-up period (the duration of the follow-up period is unclear but appears to have been 1–2 years), with the author implying that the suicides were attributable to ORS [ 6 ].
3) The proposed syndrome is not merely an expectable response to common stressors or losses or a culturally sanctioned response to a particular event
The literature provides no evidence or suggestion that ORS is merely an expectable response to common stressors or losses, or a culturally sanctioned response to a particular event.
4) The proposed syndrome reflects an underlying psychobiological dysfunction
To our knowledge, disturbances in biological and psychological processes in ORS have not been studied, although preliminary (uncontrolled) reports of improvement in ORS with pharmacotherapy or psychosocial treatment (behavioral therapy [ 15 , 48 ], cognitive-behavioral therapy [ 62 ], and paradoxical intention [ 63 ]) indirectly support the presence of such underlying mechanisms. In addition, excessive grooming behaviors in animals offer a possible ethological model for human ORS [ 64 ]. One purpose of grooming across species is to clean in order to maintain health – for example, by improving predation or avoiding predators via removal of odors [ 65 ]. While the relationship between evolutionary function/dysfunction and disorders remains controversial [ 66 , 67 ], conceivably such processes can go awry and result in disorders.
5) The syndrome is not primarily a result of social deviance or conflicts with society
There is no evidence or suggestion in the literature that ORS is solely a result of social deviance, other conflicts with society, or “eccentricity.” ORS has many features of an “internalizing” disorder rather than reflecting social deviance or conflict. Responsiveness (in many cases) to psychotropic agents or behavioral therapy (as noted above) is consistent with such a view.
6) The syndrome has diagnostic validity on the basis of various diagnostic validators
For ORS, there is a lack of empirical data for most of these validators (mentioned above) and only minimal data for others. As noted above, however, ORS does appear to differ in important ways from other disorders in terms of its symptom profile and possibly comorbidity. Furthermore, it appears to differ from delusional disorder on the basis of preliminary observations that some patients appear to respond to antidepressant monotherapy [ 6 , 18 , 32 , 34 – 40 ]. However, the fact that some patients appear to respond to antipsychotics alone [ 6 , 32 , 43 ] suggests that ORS also differs from social phobia, BDD [ 68 ], and OCD [ 69 ].
7) The syndrome has clinical utility
In our clinical experience, many patients with ORS receive no diagnosis or an inaccurate diagnosis, such as schizophrenia, OCD, or major depressive disorder. This in turn may lead to treatment for another disorder. Such misidentification may occur because DSM-IV only very briefly mentions ORS symptoms in the text, does not include the specific term “olfactory reference syndrome,” and lacks diagnostic criteria. Alternatively, patients present to non-mental health professionals, such as dentists, gastroenterologists, dermatologists, and gynecologists, who may not be aware that ORS is a known form of mental illness. Many patients do not seek treatment at all, which may in part be due to lack of public awareness that the symptoms represent a treatable entity.
Taken together, then, the potential benefits of creating a new diagnosis (e.g. identifying individuals who require appropriate clinical attention) appear to outweigh any potential harm. However, research data on this syndrome are still limited. Therefore, we propose that ORS be included in an Appendix of Criteria Sets Provided for Further Study rather than in the main part of the manual. The following are additional considerations that may arise when proposing a new disorder for the nomenclature (including research diagnostic criteria):
- Is there a need for the category; for example, is the syndrome sufficiently common in clinical or population samples that it merits an independent category as opposed to being one example in an NOS category? Prevalence studies using the proposed diagnostic criteria below have not been done. However, in a tertiary referral unit for the behavioral treatment of psychiatric disorders (the Psychological Treatment Unit at the Maudsley Hospital in London), 9 of 2000 patients (0.5%) spontaneously reported ORS symptoms [ 48 ]. This figure is likely an underestimate, given the shame and secrecy that often characterizes ORS. A self-report survey of 2,481 university students in Japan found that 2.1% had been concerned with emitting a strange bodily odor during the previous year [ 70 ]. While this symptom is not necessarily equivalent to a clinical diagnosis of ORS, the authors nonetheless imply that ORS is relatively common in Japan and conclude that in Japan "fears of …bodily odor are…encountered almost every day." Several other authors have suggested that ORS is more common than usually recognized [ 13 ]. Iwu noted that delusional halitosis (one form of ORS) "may be frequently encountered by the dental surgeon" [ 30 ]. Osman concluded that the monosymptomatic hypochondriacal psychoses are likely to be underreported and "form an important and not uncommon cause of psychiatric morbidity in [developing countries]" [ 18 ].
- What is the relationship of the proposed disorder with other DSM-IV diagnoses; for example, is the diagnosis sufficiently distinct from other diagnoses? As noted, ORS appears to differ from diagnostic near neighbors in several ways, although further research is needed.
- Are there proposed diagnostic criteria with clinical face validity, reliability, and adequate sensitivity and specificity for the proposed construct? As discussed below, available criteria exist. Nevertheless, further work is needed to test their reliability.
- Can the criteria be easily implemented in a typical clinical interview and reliably operationalized/assessed for research purposes? Suggested criteria are provided below, but have not yet been rigorously studied.
2) If ORS is included as a separate disorder, what should its diagnostic criteria consist of?
Two different sets of criteria have been proposed for ORS [ 8 , 36 ]. The research diagnostic criteria proposed below reflect features of each criteria set, with further minor modifications; in addition, we propose the addition of insight specifiers:
- Preoccupation with the belief that one emits a foul or offensive body odor, which is not perceived by others.
- The preoccupation causes clinically significant distress (for example, depressed mood, anxiety, shame) or impairment in social, occupational, or other important areas of functioning.
- The symptoms are not a symptom of schizophrenia or another psychotic disorder, and are not due to the direct physiological effects of a substance (e.g., a drug of abuse or medication) or a general medical condition.
Specify whether ORS beliefs are currently characterized by:
- Good or fair insight: Recognizes that ORS beliefs are definitely or probably not true, or that they may or may not be true
- Poor insight: Thinks ORS beliefs are probably true
- Delusional beliefs about body odor: Completely convinced ORS beliefs are true
We suggest the phrase “which is not perceived by others” in criterion A rather than a phrase such as “false belief” because it may be more patient-friendly and thus perhaps less likely to deter patients with ORS, whose insight is usually absent or poor, from seeking treatment. Criterion B is based on the DSM-IV clinical significance criterion and will ultimately need to be consistent with language used throughout DSM-V. We considered adding a phrase about “associated avoidance” to this criterion; although possibly open to somewhat different interpretations by clinicians, it seems clear that avoidance contributes to the clinical distress and impairment associated with ORS. However, in the absence of adequate data on the prevalence of avoidant behavior in ORS, and whether it is characteristic of all patients with ORS, avoidance may be better in the text than in the criteria. Furthermore, impairment in functioning should cover clinically significant avoidance. The diagnostic hierarchy criterion (criterion C) specifically emphasizes psychotic disorders. We considered including social phobia in the exclusion criterion, given the relationship between taijin kyofusho and concerns about body odor, but concluded that insufficient data are available to support this. We suggest a dimensional approach to insight, consistent with the emphasis in DSM-V on dimensional constructs, and given that there appears to be a range of insight in ORS. We considered whether these criteria are appropriate for both genders, for patients throughout the course of development, and for all cultures, and are not aware of a compelling reason for modifying the proposed criteria for any of these reasons.
SUMMARY AND PRELIMINARY RECOMMENDATIONS
Considering ORS a type of delusional disorder poses a number of diagnostic problems, as discussed above. In addition, available data suggest that ORS differs from other “near-neighbor” disorders. One possibility is that ORS might represent variable presentations of several different disorders, such as BDD, social phobia, or others, rather than being a distinct syndrome. While this possibility requires investigation, studies and case descriptions of ORS over the past century provide a consistent description of its clinical features, suggesting that ORS is likely a distinct entity, although one that shares some features with other disorders. In addition, ORS appears to meet many of the above considerations for what constitutes a mental disorder and for adding a disorder to the nomenclature. In particular, ORS appears to characterize a distinct and suffering group of people who need clinical attention; in our experience, its near absence in DSM has led to underdiagnosis and under-treatment of a severe mental illness. Also of clinical importance, there is limited but emerging literature on its treatment, which appears to differ in some ways from that of other disorders [ 2 , 8 ] – in particular, delusional disorder, under which ORS is currently classified.
Nevertheless, data on ORS are still limited, and research on the above criteria is needed. For example, reliability data are not available on the proposed diagnostic criteria, many of the above-noted validators have not been examined, and ORS’s prevalence and the nature of its relationship to other disorders have been only minimally examined. Thus, it is probably premature to include ORS in the main body of DSM as a separate diagnostic category.
Taken together, we recommend including a criteria set for ORS in an Appendix of Criteria Sets Provided for Further Study. ORS has been clinically observed and reported for more than a century around the world, with the literature consistently underscoring the suffering of these individuals. ORS’s current classification is problematic, causing it to be confused with other disorders, missed in clinical settings, or unsuccessfully treated. Including ORS in an Appendix would also have the advantage of stimulating further systematic research on ORS, using specified diagnostic criteria.
Acknowledgements
We wish to thank Drs. Hisato Matsunaga, Harrison Pope, and Susan Bogels for their comments on drafts of this review.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Spring 2024 | VOL. 36, NO. 2 CURRENT ISSUE pp.A4-174
- Winter 2024 | VOL. 36, NO. 1 pp.A5-81
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Is Olfactory Reference Syndrome an Obsessive-Compulsive Spectrum Disorder?
- Dan J. Stein , M.B. ,
- Leon Le Roux , M.B. ,
- Colin Bouwer , M.B. , and
- Ben Van Heerden , M.B.
Search for more papers by this author
A number of disorders characterized by intrusive repetitive symptoms and varying degrees of insight may overlap phenomenologically and neurobiologically with obsessive-compulsive disorder (OCD). There is a question as to whether olfactory reference syndrome, a disorder characterized by persistent preoccupations about body odor accompanied by shame and embarrassment, is also an OCD spectrum disorder. Two cases of olfactory reference syndrome, with accompanying phenomenological and neurobiological data, are presented in order to discuss the possible overlap with OCD. A number of phenomenological and neurobiological features in these patients were at least partially reminiscent of OCD. In particular, despite having poor insight, both patients demonstrated significant improvement upon treatment with a serotonin reuptake inhibitor.
Several authors have described psychiatric patients with persistent preoccupations with personal odor. 1 – 4 Although these olfactory symptoms can be seen in a number of disorders, including schizophrenia, depression, and medical conditions, there also seems to be a specific clinical entity characterized by such preoccupations. An early case series in the Western literature used the term olfactory paranoid syndrome . 5 Japanese patients with similar symptoms have, however, been characterized as having an anxiety condition known as taijin kyofusho or anthropophobia , 6 , 7 a term that emphasizes the avoidance of social situations typically seen in such patients.
In perhaps the most extensive investigation of the syndrome to date, Pryse-Phillips 8 introduced the term olfactory reference syndrome (ORS) to differentiate the olfactory symptoms seen in this entity from those of schizophrenia, depression, and temporal lobe epilepsy. Patients with ORS held themselves responsible for the odor, and therefore experienced a “contrite reaction,” characterized by shame and embarrassment. Such patients “tended to wash themselves excessively, to change their clothes with more than usual frequency, to hide themselves away, and to restrict their social and domestic excursions.” 8
In DSM-IV, 9 delusions about personal odor are described as an example of the somatic subtype of delusional disorder. However, it is conceivable that ORS might also be diagnosed as obsessive-compulsive disorder (OCD) with poor insight. Indeed, a number of so-called obsessive-compulsive spectrum disorders, 10 – 12 such as body dysmorphic disorder, 13 , 14 hypochondriasis, 15 , 16 and pathological jealousy, 17 have been described as having both obsessional and delusional variants. This spectrum of disorders has been defined in terms of a commonality of important phenomenological and neurobiological features, such as preferential response to selective serotonin reuptake inhibitors (SSRIs). 13 , 15 , 18
An immediate question is whether it is also useful to conceptualize ORS as lying on an OCD spectrum. In this article we present two cases of patients with ORS, with accompanying phenomenological and neurobiological data, in order to address the possible overlap of this condition with OCD. Both patients had a Western (rather than Eastern or African) cultural background and were seen in our Obsessive-Compulsive Disorders Clinic, where they were interviewed with the Structured Clinical Interview for the Diagnosis of Axis I Disorders 19 on presentation.
CASE REPORTS
Case 1. Mr. A. was a 17-year-old male who described a persistent preoccupation, which had begun about 6 months previously, with the idea that he smelled of urine. Each time he urinated, for example, he worried that he had wet his underwear, and that consequently people would think that he smelled of urine. He stated that these thoughts occupied most of his waking time. As a result of the thoughts he would repeatedly check his underwear for urine stains, would change his clothing excessively often, and would use more deodorant than usual. In addition, shame and embarrassment about the perceived odor gradually led him to avoid more and more social interactions, and he even began to miss days at school. He became increasingly demoralized and at the time of presentation exhibited a number of symptoms of depression, although he did not meet DSM-IV criteria for a major depressive episode. On close questioning, the patient said that he was 95% certain that he did in fact smell of urine, although on occasion he felt that his preoccupations about odor were excessive and unreasonable. There was no history of classic obsessions or compulsions or of definite hallucinations or delusions. There was no history of substance abuse or of an underlying general medical disorder.
The patient consented to SPECT imaging of the brain before beginning a trial of an SSRI. Five minutes prior to injection of 555 MBq (15 mCi) [ 99m Tc]hexamethylpropyleneamine oxime (HMPAO), the patient was instructed to allow himself to focus on the idea that he might in fact be smelling of urine, in the same way that he usually did when preoccupied with this concern. He continued with these thoughts and actions for 5 minutes after injection.
SPECT data were acquired by use of a dual detector gamma camera (Elscint, Helix) equipped with fanbeam collimators, using the step-and-shoot mode and a circular orbit. A 128×128 image matrix was used, acquiring data in 3-degree steps, for 15 seconds per step, through 360 degrees. Data were reconstructed by using a Metz filter (power 5, FWHM 14mm) to provide tomographic images in the transaxial (parallel to the orbitomeatal line), coronal, and sagittal planes. Each image set was normalized to the mean cerebellar counts.
Pretreatment SPECT revealed multiple perfusion defects, including perfusion defects anteriorly in the right and left inferior frontal lobes (higher on the left) and in the left frontoparietal area; irregular perfusion in the parietooccipital regions; and diminished perfusion of both temporal lobes and the left occipital area.
The patient was then treated with citalopram 40 mg daily. He showed a gradual reduction in his preoccupation with odors. Ratings of symptoms related to his odor on the Yale-Brown Obsessive-Compulsive Rating Scale 20 fell from 29 at week 0 to 25 at week 4, 17 at week 8, and 8 at week 12. Ratings of depressive symptoms on the Montgomery-Åsberg Depression Scale fell from 11 at week 0 to 6 at week 4, 5 at week 8, and 1 at week 12. Symptoms remained significantly improved throughout the subsequent course of treatment in our clinic (8 months).
Case 2. A 54-year-old woman presented with a persistent preoccupation that she had a foul body odor. The smell emanated from her armpits, breast folds, feet, and anal region and was reminiscent of rotting fruit. This particular symptom had begun about 30 years earlier. A more recent concern was that drains from her house emitted a similar foul smell. Although the patient was able to admit that these concerns were perhaps unrealistic, she was often concerned about embarrassing herself, and this had led to excessive handwashing, frequent changes of clothing, and repeated cleansing of drains. Furthermore, at times these concerns resulted in marked depressive symptoms that met DSM-IV criteria for a major depressive episode. The patient also suffered at times from checking (of lights, stove, taps) and counting rituals. There was no history of definite hallucinations or delusions. There was no history of substance abuse or of an underlying general medical disorder.
Electroencephalography and computed tomography of the brain revealed no abnormalities. The patient was initially treated with amitriptyline 150 mg daily, which improved mood but not olfactory symptoms. When the patient discontinued medication after 12 weeks, depressive symptoms worsened, and she submitted to a course of electroconvulsive therapy (18 bilateral treatments). This again improved mood but not olfactory symptoms. A 12-week course of fluoxetine, reaching a maximum dose of 80 mg daily, had no further effect on olfactory symptoms. Treatment with pimozide 4 mg daily for 8 weeks was similarly unsuccessful. A combination of clomipramine 250 mg daily and perphenazine 4 mg thrice daily for 12 weeks also had little positive effect. However, after increase of the clomipramine to 300 mg daily and discontinuation of the perphenazine, the patient showed a gradual, partial, but definite improvement in both her preoccupation with foul odors and her depressive symptoms. A retrospective Clinician's Global Impression change score would be 2 (much improved).
The two case reports of olfactory reference syndrome (ORS) presented here can be used as a basis for a discussion of the relationship between this entity and OCD. Phenomenologic, neurobiologic, and pharmacologic issues will be considered in turn.
The phenomenology of the symptoms in the two patients is reminiscent of OCD in a number of respects. Although all symptoms were related to body odor, these met the DSM-IV 9 criteria for obsessions (intrusive thoughts about body odor) and compulsions (repetitive cleansing behaviors). Although symptoms were often not recognized to be unreasonable or excessive, they were accompanied by significant shame and distress. Thus, on SCID-I interview, the patients were diagnosed as having OCD with poor insight. Both patients experienced onset of the disorder in adolescence, as well as secondary depressive symptoms, features that are common in OCD. 21 Nevertheless, only Patient 2 described obsessions and compulsions that did not directly relate to complaints about her own body odor (concerns about other odors, checking, counting), whereas OCD patients tend to have a number of different kinds of symptoms over time. 22
Pryse-Phillips' pioneering report 8 described 36 patients with ORS and documented extensive support for the existence of this entity in previously published case material. The report emphasized that ORS is characterized by a “contrite” reaction to the perception of odor. That is, the patients are “deeply ashamed, embarrassed, self-abasing.” In this series there was common use of deodorant or excessive washing (82%) and excessive changing of clothes (68%). Patients were able to construct a hierarchy of feared situations, and avoidance behavior was typical (97%). Fifty-two percent had developed continuous depression, and 50% had obsessional features. Although many patients continued to work and did not meet criteria for schizophrenia, there was often marked functional impairment. They had frequently presented to medical specialists but had rarely received psychiatric treatment. These findings of psychosocial dysfunction are consistent with our cases and with an overlap between ORS and OCD. 23
On the other hand, Pryse-Phillips 8 found that average age at onset of ORS was 25.4 years, 78% of patients were males, 60% had lost insight, and 75% had olfactory “hallucinations.” This age at onset and male:female ratio were higher than is typical for OCD, and psychotic symptoms are uncommon in OCD. However, demographic discrepancies may reflect the fact that Pryse-Phillips drew many subjects from inpatient settings. Furthermore, degree of insight varies in OCD and related disorders, and patients with poor insight have been classified as psychotic by early authors. Indeed, given the focused nature of these patients' symptoms, with no evidence of obsessions and compulsions unrelated to odor, the entity is particularly reminiscent of disorders such as body dysmorphic disorder, hypochondriasis, and obsessional jealousy, where there is frequently limited insight about a single obsessional focus.
SPECT findings in Case 1 described here differed partially from the classic findings of increased prefrontal/orbitofrontal cortex activity often seen in OCD. 24 However, a number of SPECT studies have also noted reduced blood flow in patients with OCD. 25 Furthermore, the behavioral challenge used during our SPECT procedure differed from the resting scan methodology used in most OCD studies. Unfortunately, it was not possible to obtain a repeat SPECT scan after treatment to determine whether the medication had led to improvement in perfusion deficits.
There is little in the literature on the neurobiology of ORS. Alliez and Dongiers 26 described one patient with right temporal spike activity, but the phenomenology of olfactory hallucinations in temporal lobe epilepsy appears rather different from that seen in ORS. 8 Certainly it has been suggested that central mechanisms in psychiatric disorders such as depression and schizophrenia result in alterations to olfactory threshold. However, once again the phenomenology of olfactory symptoms in these disorders differs from that in ORS, 8 and it is not clear that the latter actually involves alterations in perceptual rather than cognitive-affective processes.
Both patients reported here showed a gradual but significant response to treatment with an SSRI. The SSRIs, including clomipramine 27 and citalopram, 28 are well known to be effective in OCD. 29 , 30 There are a number of previous reports of pharmacotherapy for olfactory reference syndrome, with Videbech 5 describing patients who failed to respond to neuroleptics and Pryse-Phillips 8 noting that one patient did not respond to treatment with tranquilizers and a monoamine oxidase inhibitor. Pryse-Phillips 8 does indicate, without providing more details, that there may be fair reduction in symptoms after treatment with psychotherapy and tricyclic antidepressants. Monosymptomatic hypochondriasis, which includes some patients with ORS, 31 , 32 has been linked with response to pimozide, 33 and a number of authors have also noted that this condition may respond to tricyclics. 32 , 34 Finally, there are reports of ORS responding to clomipramine. 35
Although connections between olfactory and obsessive-compulsive symptoms have long been drawn, 36 there is little in the contemporary literature about this topic. However, the cases of ORS described here provide tentative evidence of at least a partial overlap with other patients with obsessive-compulsive spectrum disorders such as body dysmorphic disorder, hypochondriasis, and obsessional jealousy. Given the separate classifications of ORS and possibly related conditions in our current nosology, perhaps further changes to the DSM-IV are necessary to emphasize that a number of conditions previously conceptualized as psychotic in nature may have similarities with OCD. In addition, given the similarities between ORS and entities that have been conceptualized as “culture-bound,” 6 , 7 such nosological changes should perhaps reflect the possible universality of these conditions.
Systematic study of a larger sample of patients may be helpful in determining whether ORS is best viewed as an OCD spectrum disorder, as part of a social phobia spectrum, or as a delusional disorder. A putative overlap between ORS and OCD would suggest that ORS patients might also respond to SSRIs and behavioral therapies; further basic and clinical work to determine the selectivity of the serotonergic mediation of ORS and similar symptoms would thus be of particular interest. 37 , 38
ACKNOWLEDGMENTS
Dr. Stein is supported in his work by a grant from the Medical Research Council of South Africa and by the Lundbeck Fellowship.
1. Souchanoff S: Les représentations obsédantes hallucinatoires et les hallucinations obsédantes. Rev Med 1906 ; 26:336–350 Google Scholar
2. Birnbaum K: Pathologische Überwertigkeit und Wahnbidung. Mschr Psychiat Neurol 1915 ; 37:39–80 Crossref , Google Scholar
3. Reichart M: Allgemeine und Spezielle Psychiatrie, 2nd edition. Jena, G Fischer, 1918 Google Scholar
4. Mayer-Gross W: Die Sinnesanomalien, in Bumkes Handbuch der Geisteskrankheiten, vol 9. Berlin, Springer-Verlag, 1932 Google Scholar
5. Videbech T: Chronic olfactory paranoid syndromes. Acta Psychiatr Scand 1967 ; 42:182–213 Google Scholar
6. Tanaka-Matsumi J: Taijin kyofusho: diagnostic and cultural issues in Japanese psychiatry. Cult Med Psychiatry 1979 ; 3:231–245 Crossref , Medline , Google Scholar
7. Takahashi T: A social club spontaneously formed by ex-patients who had suffered from anthrophobia (taijin kyofu (sho)). Int J Soc Psychiatry 1975 ; 21:137–140 Crossref , Medline , Google Scholar
8. Pryse-Phillips W: An olfactory reference syndrome. Acta Psychiatr Scand 1971 ; 47:484–509 Crossref , Medline , Google Scholar
9. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th edition. Washington, DC, American Psychiatric Association, 1994 Google Scholar
10. Jenike MA: Obsessive-compulsive related disorders: a hidden epidemic. N Engl J Med 1989 ; 321:539–541 Crossref , Medline , Google Scholar
11. Stein DJ, Hollander E: The spectrum of obsessive-compulsive–related disorders, in Obsessive-Compulsive Related Disorders, edited by Hollander E. Washington, DC, American Psychiatric Press, 1993, pp 241–271 Google Scholar
12. Hollander E (ed): Obsessive-Compulsive Related Disorders. Washington, DC, American Psychiatric Press, 1993 Google Scholar
13. Hollander E, Liebowitz MR, Winchel R, et al: Treatment of body dysmorphic disorder with serotonin reuptake blockers. Am J Psychiatry 1989 ; 146:768–770 Crossref , Medline , Google Scholar
14. McElroy SL, Phillips KA, Keck PE Jr, et al: Body dysmorphic disorder: does it have a psychotic subtype? J Clin Psychiatry 1993 ; 54:389–395 Google Scholar
15. Fallon BA, Javitch J, Liebowitz MR: Hypochondriasis and OCD: overlaps in diagnosis and treatment. J Clin Psychiatry 1991 ; 52:457–460 Medline , Google Scholar
16. Bishop ER: Monosymptomatic hypochondriasis. Psychosomatics 1980 ; 21:731–747 Crossref , Medline , Google Scholar
17. Stein DJ, Hollander E: Serotonin reuptake blockers for the treatment of obsessional jealousy. J Clin Psychiatry 1994 ; 55:30–33 Medline , Google Scholar
18. Zohar J, Insel TR: Obsessive-compulsive disorder: psychobiological approaches to diagnosis, treatment, and pathophysiology. Biol Psychiatry 1987 ; 22:667–687 Crossref , Medline , Google Scholar
19. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for Axis I DSM-IV Disorders. New York, Biometrics Research Department, New York State Psychiatric Institute, 1994 Google Scholar
20. Goodman WK, Price LH, Rasmussen SA, et al: The Yale-Brown Obsessive Compulsive Scale, I: development, use, and reliability. Arch Gen Psychiatry 1989 ; 46:1006–1011 Crossref , Medline , Google Scholar
21. Rassmussen SA, Tsuang MT: Clinical characteristics and family history in DSM-III obsessive-compulsive disorder. Am J Psychiatry 1986 ; 143:317–322 Crossref , Medline , Google Scholar
22. Swedo S, Rapoport J, Leonard H, et al: Obsessive compulsive disorder in children and adolescents, I: clinical phenomenology of 70 consecutive cases. Arch Gen Psychiatry 1989 ; 46:335–349 Crossref , Medline , Google Scholar
23. Hollander E, Stein DJ, Rowland CR, et al: Pharmaco-economic and quality of life study of OCD. Presented at the American Psychiatric Association annual meeting, New York, May, 1996 Google Scholar
24. Insel TR: Toward a neuroanatomy of obsessive-compulsive disorder. Arch Gen Psychiatry 1992 ; 49:739–744 Crossref , Medline , Google Scholar
25. Lucey JV, Costa DC, Blanes T, et al: Regional cerebral blood flow in obsessive-compulsive disordered patients at rest: differential correlates with obsessive-compulsive and anxious-avoidant dimensions. Br J Psychiatry 1995 ; 167:629–634 Crossref , Medline , Google Scholar
26. Alliez J, Dongiers S: EEG correlations of olfactory hallucinations. Ann Med Psychol 1955 ; 110:665–667 Google Scholar
27. DeVaugh-Geiss J, Katz R, Landau P, et al: Clomipramine in the treatment of patients with obsessive-compulsive disorder: the clomipramine collaborative study group. Arch Gen Psychiatry 1991 ; 48:730–738 Crossref , Medline , Google Scholar
28. Stein DJ, Maud CM, Bouwer C: Use of citalopram a selective serotonin reuptake inhibitor in obsessive-compulsive disorder. Journal of Serotonin Research 1996 ; 1:29–33 Google Scholar
29. Greist JH, Jefferson JW, Kobak KA, et al: Efficacy and tolerability of serotonin transport inhibitors in obsessive-compulsive disorder. Arch Gen Psychiatry 1995 ; 52:53–60 Crossref , Medline , Google Scholar
30. Stein DJ, Spadaccini E, Hollander E: Meta-analysis of pharmacotherapy trials for obsessive compulsive disorder. Int Clin Psychopharmacol 1995 ; 10:11–18 Crossref , Medline , Google Scholar
31. Bishop ER: An olfactory reference syndrome: monosymptomatic hypochondriasis. J Clin Psychiatry 1980 ; 41:57–59 Medline , Google Scholar
32. Brotman AW, Jenike MA: Monosymptomatic hypochondriasis treated with tricyclic antidepressants. Am J Psychiatry 1984 ; 141:1608–1609 Crossref , Medline , Google Scholar
33. Riding J, Munro A: Pimozide in the treatment of monosymptomatic hypochondriacal psychosis. Acta Psychiatr Scand 1975 ; 52:23–30 Crossref , Medline , Google Scholar
34. Fernando N: Monosymptomatic hypochondriasis treated with a tricyclic antidepressant. Br J Psychiatry 1988 ; 152:851–852 Crossref , Medline , Google Scholar
35. Kizu A, Miyoshi N, Yoshida Y, et al: A case with fear of emitting body odour resulted in successful treatment with clomipramine. Hokkaido Igaku Zasshi 1994 ; 69:1477–1480 Medline , Google Scholar
36. Freud S: Notes upon a case of obsessional neurosis (1909), in The Standard Edition of the Complete Psychological Works of Sigmund Freud, vol 10, translated and edited by Strachey J. London, Hogarth Press, 1955, pp 221–249 Google Scholar
37. King BH: Hypothesis: involvement of the serotonergic system in the clinical expression of monosymptomatic hypochondriasis. Pharmacopsychiatry 1990 ; 23:85–89 Crossref , Medline , Google Scholar
38. Dykman RA, Murphree OD, Reen WG: Familial anthrophobia in pointer dogs. Arch Gen Psychiatry 1979 ; 36:988–993 Crossref , Medline , Google Scholar
- Prevalence of olfactory reference disorder according to the ICD-11 in a German university student sample 1 December 2023 | Current Psychology, Vol. 43, No. 17
- Associations between olfactory reference disorder and social phobia – results of an internet-based study 7 March 2024 | Frontiers in Psychology, Vol. 15
- Olfactory Reference Syndrome Journal of Nervous & Mental Disease, Vol. 211, No. 9
- Effect of Oral Health and Toothbrushing Performance on Halitosis among People with Intellectual Disabilities American Journal of Health Behavior, Vol. 47, No. 4
- Olfactory Obsessions: A Study of Prevalence and Phenomenology in the Course of Obsessive-Compulsive Disorder 24 April 2023 | Journal of Clinical Medicine, Vol. 12, No. 9
- Psychopathological symptoms in dermatology: A basic approach toward psychocutaneous disorders 11 July 2022 | International Journal of Dermatology, Vol. 62, No. 3
- Anthropophobia (Taijin Kyofusho) beyond the Boundaries of a Culture-Bound Syndrome: A Case Series from India 1 December 2021 | Indian Journal of Psychological Medicine, Vol. 44, No. 6
- Olfactory Reference Syndrome: A Case Report and Screening Tool 29 April 2020 | Journal of Clinical Psychology in Medical Settings, Vol. 28, No. 2
- “Would you tell me If i smelled bad?,” 14‐year‐old Dylan diagnosed with olfactory reference syndrome: A case report 7 April 2020 | Journal of Child and Adolescent Psychiatric Nursing, Vol. 33, No. 2
- Diagnosis and phenotypic assessment of trimethylaminuria, and its treatment with riboflavin: 1H NMR spectroscopy and genetic testing 18 September 2019 | Orphanet Journal of Rare Diseases, Vol. 14, No. 1
- Transdiagnostic Approach to Olfactory Reference Syndrome: Neurobiological Considerations Harvard Review of Psychiatry, Vol. 27, No. 3
- Alefiya Dhilla Albers , Ph.D. ,
- Ilaria Amato , B.S. ,
- Mark W. Albers , M.D., Ph.D.
- Comprehensive Psychiatry, Vol. 86
- Journal of Obsessive-Compulsive and Related Disorders, Vol. 19
- Journal of Psychosomatic Research, Vol. 105
- Psiquiatría Biológica, Vol. 25, No. 1
- Journal of Obsessive-Compulsive and Related Disorders, Vol. 13
- Journal of Psychosomatic Research, Vol. 80
- Clinical Disorders of Olfaction 4 June 2015
- Sex‐related and non‐sex‐related comorbidity subtypes of tic disorders: a latent class approach 7 October 2013 | European Journal of Neurology, Vol. 21, No. 5
- Psiquiatría Biológica, Vol. 21, No. 3
- British Dental Journal, Vol. 217, No. 1
- Olfactory delusional syndrome 11 February 2013 | Australian & New Zealand Journal of Psychiatry, Vol. 47, No. 7
- BMC Research Notes, Vol. 6, No. 1
- Open Journal of Psychiatry, Vol. 03, No. 04
- Descriptive psychopathology
- L'Encéphale, Vol. 38, No. 1
- La Presse Médicale, Vol. 41, No. 1
- Acta Neuropsychiatrica, Vol. 24, No. 5
- Psychopathology, Vol. 45, No. 2
- Successful Treatment of Olfactory Reference Syndrome With Cognitive Behavioral Therapy: A Case Study Cognitive and Behavioral Practice, Vol. 18, No. 4
- Olfactory reference syndrome: demographic and clinical features of imagined body odor General Hospital Psychiatry, Vol. 33, No. 4
- Psychological Medicine, Vol. 41, No. 3
- Jornal Brasileiro de Psiquiatria, Vol. 60, No. 4
- Depression and Anxiety, Vol. 27, No. 6
- CNS Spectrums, Vol. 14, No. 9
- An Olfactory Reference Syndrome Successfully Treated by Aripiprazole Augmentation of Antidepressant Therapy Cognitive and Behavioral Neurology, Vol. 21, No. 4
- Psiquiatría Biológica, Vol. 15, No. 4
- CNS Spectrums, Vol. 13, No. 2
- Psychosomatics, Vol. 49, No. 1
- Expert Review of Neurotherapeutics, Vol. 8, No. 2
- PSN, Vol. 5, No. 3
- Delusions of Body Malodour: The Olfactory Reference Syndrome
- General Hospital Psychiatry, Vol. 28, No. 2
- The World Journal of Biological Psychiatry, Vol. 7, No. 2
- Senile depression with olfactory reference syndrome: a psychopathological review 17 August 2005 | Psychogeriatrics, Vol. 5, No. 2
- Psychiatry Research: Neuroimaging, Vol. 140, No. 2
- On phenomenology and classification of hoarding: a review 29 September 2004 | Acta Psychiatrica Scandinavica, Vol. 110, No. 5
- Do olfactory reference syndrome and Jiko‐shu‐kyofu (a subtype of Taijin‐kyofu ) share a common entity? 16 January 2004 | Acta Psychiatrica Scandinavica, Vol. 109, No. 2
- International Journal of Psychiatry in Clinical Practice, Vol. 7, No. 1
- Social Anxiety Disorder 26 October 2007
- Psychosomatic Medicine, Vol. 64, No. 2
- Psychiatric Clinics of North America, Vol. 24, No. 4
- Psychiatric Clinics of North America, Vol. 23, No. 3
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Advertisement
- Register for Free
- My account Orders Downloads Address Payment methods Account details
- About About Psychiatrist.com About JCP About PCC About CME Institute
Error: Search field were incomplete.

This work may not be copied, distributed, displayed, published, reproduced, transmitted, modified, posted, sold, licensed, or used for commercial purposes. By downloading this file, you are agreeing to the publisher’s Terms & Conditions.
Case Report
Cognitive Behavioral Therapy for Olfactory Reference Syndrome: A Case Report
Jasper B. Zantvoord, MD a,b, *; Nienke Vulink, MD, PhD a ; and Damiaan Denys, MD, PhD a,c
Published: September 28, 2016
O lfactory reference syndrome (ORS) is a psychiatric condition characterized by concerns about perceived body odor, which may be accompanied by repetitive behaviors to mask body odor and avoidance of social situations. 1 ORS has been proposed as an obsessive-compulsive and related disorder in the DSM-5 . 2 There is no established standard treatment for ORS. Some case studies have reported (partial) response with clomipramine, 1 , 3 , 4 while others have reported nonresponse. 5-7 The interpretation of previous case reports on behavioral therapy and eye movement desensitization and reprocessing (EMDR) is impeded by the paucity of objective outcome assessments. 5 , 7-9 To date, no report on cognitive behavioral therapy (CBT) has been published. We present a case of ORS in a woman who was successfully treated with CBT.
Case report. Ms A, a 23-year-old Creole woman with no history of physical disease, had been suffering from ORS symptoms for 10 years. She was diagnosed ( DSM-IV criteria) with generalized anxiety disorder (GAD), which developed after the onset of ORS symptoms. She had an overvalued idea that she emitted a sweaty body odor that disgusted people around her. She interpreted other people’s frowning or distancing themselves as proof for her beliefs. She experienced severe distress in confined spaces (classroom and public transport) where people could smell her presumed odor. She regularly checked her odor, showered every time she left home, and used excessive amounts of deodorant. She repeatedly sought consultation with dermatologists. Due to avoidance and distress, her study performance and social life were impaired. She had received supportive psychotherapy, which was associated with limited improvement. Ms A was therefore referred for assessment and further treatment.
Pretreatment physical, neurologic, and laboratory evaluation showed no abnormalities. Her pretreatment score on the Body Dysmorphic Disorder Modification of the Yale-Brown Obsessive Compulsive Scale (BDD-YBOCS) 10 was 28 out of 48, indicating moderate symptoms ( Table 1 ). CBT was carried out with 8 fellow group members who were all suffering from body dysmorphic disorder (BDD). Treatment consisted of twice-weekly sessions with a total duration of 16 weeks. CBT was based on a previously published manual, 13 which was adapted to facilitate group-based treatment. The first session entailed psychoeducation and establishment of treatment goals. In the second session, an exposure hierarchy was composed. During and between sessions, gradual and repetitive in vivo exposure with task concentration and response prevention were performed. The treatment manual was adapted specifically for Ms A to include tailored exposure exercises to evoke fear-inducing stimuli related to her emitting an offensive body odor. Examples included approaching someone on the street for small talk and, subsequently, standing close and talking to someone in a confined space and then doing so without using deodorant or showering beforehand. Cognitive restructuring was introduced to identify and adjust dysfunctional beliefs. In the final sessions, relapse prevention strategies were discussed. Apart from body-oriented therapy elements, such as progressive muscle relaxation (Jacobson technique) and breathing exercises, no concurrent treatments were performed.
Following treatment, Ms A’s ORS symptoms fully remitted. For residual GAD symptoms, paroxetine 20 mg/d was initiated after CBT termination. Two months thereafter, GAD symptoms remitted ( Table 1 ). In the following months, ORS and GAD symptoms remained in remission. Ms A resumed her studies and group fitness classes.
Click figure to enlarge
The present case is the first report of successful treatment of ORS combining cognitive and behavioral techniques. ORS and comorbid symptoms were assessed using objective rating scales, elaborating on previous reports on behavioral therapy and EMDR in ORS. 5 , 7-9 After CBT group treatment, ORS symptoms fully remitted and improvement was maintained for 6 months. Paroxetine treatment initiated after CBT could have contributed to maintenance of remission. Our findings are promising, because a standard treatment for ORS has not been established. 2 , 6 The classification of ORS as an obsessive-compulsive spectrum disorder is a point of ongoing debate. 2 The group CBT in which our patient enrolled was designed for treatment of BDD. Nevertheless, ORS remitted, which gives some support for the classification of ORS as an obsessive-compulsive spectrum disorder. However, our observations should be interpreted with caution, as the effects noted could be based on nonspecific therapeutic factors and were limited to a single case. Therefore, further research, particularly a randomized controlled trial of the efficacy of CBT in ORS, is warranted.
a Department of Psychiatry, Academic Medical Center, Amsterdam, The Netherlands b The Bascule Academic Centre for Child and Adolescent Psychiatry, Amsterdam, The Netherlands c Netherlands Institute for Neuroscience, Royal Netherlands Academy of Arts and Sciences, Amsterdam, The Netherlands. * Corresponding author: Jasper B. Zantvoord, MD, Department of Psychiatry, Academic Medical Centre, Meibergdreef 5, Room PA2-226, 1105 AZ, Amsterdam, The Netherlands ( [email protected] ) .
J Clin Psychiatry 2016;77(9):e1144
dx.doi.org/ 10.4088/JCP.15cr10451
© Copyright 2016 Physicians Postgraduate Press, Inc.
Submitted: October 12, 2015; accepted December 21, 2015. Online first: July 19, 2016. Drug names: clomipramine (Anafranil and others), paroxetine (Paxil, Pexeva, and others). Potential conflicts of interest: None. Funding/support: None.
1. Lochner C, Stein DJ. Olfactory reference syndrome: diagnostic criteria and differential diagnosis. J Postgrad M ed . 2003;49(4):328-331. PubMed
2. Feusner JD, Phillips KA, Stein DJ. Olfactory reference syndrome: issues for DSM-V . D epress Anxiety . 2010;27(6):592-599. PubMed doi: 10.1002/da.20688
3. Dominguez RA, Puig A. Olfactory reference syndrome responds to clomipramine but not fluoxetine: a case report. J Clin Psychiatry . 1997;58(11):497-498. PubMed doi:10.4088/JCP.v58n1106 e
4. Stein DJ, Le Roux L, Bouwer C, et al. Is olfactory reference syndrome an obsessive-compulsive spectrum disorder? two cases and a discussion. J Neu ropsychiatry Clin Ne urosci . 1998;10(1):96-99. PubMed doi:10.1176/jn p.10.1.96
5. McGoldrick T, Begum M, Brown KW. EMDR and Olfactory Reference Syndrome. J EMDR Pract Res . 2008;2(1):63-68. doi:10.1891 /1933-3196.2.1.63
6. Lochner C, Stein DJ. Prevalence of olfactory reference syndrome in obsessive-compulsive disorder and social anxiety disorder. J Clin Psyc hiatry . 2014;75(11):1266. PubMed doi:10.4088/JC P.14l08987
7. Beary MD, Cobb JP. Solitary psychosis—three cases of monosymptomatic delusion of alimentary stench treated with behavioural psychotherapy. Br J Psychiat ry . 1981;138(1):64-66. PubMed doi:10.1192/bjp.1 38.1.64
8. Gomez-Perez JC, Marks IM, Gutierrez-Fisac JL. Dysmorphophobia: clinical features and outcome with behavior therapy. Eur Psychiatry . 1994;9(5):229-235.
9. Marks I, Mishan J. Dysmorphophobic avoidance with disturbed bodily perception: a pilot study of exposure therapy. Br J Psych iatry . 1988;152(5):674-678. PubMed doi:10.1192/ bjp.152.5.674
10. Phillips KA, Hollander E, Rasmussen SA, et al. A severity rating scale for body dysmorphic disorder: development, reliability, and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychop harmacol Bull . 1997;33(1):17-22. PubMed
11. Domen AC, Borsboom D, Vullink NC. Psychometric Pro perties o f t he Dutch Dimensional Obsessi ve Compulsive Scale [master’s thesis]. http://dare.uva.nl/cgi/arno/show.cgi?fid=509444 . Amsterdam, The Netherlands: University of Amsterdam; 2013.
12. Maier W, Buller R, Philipp M, et al. The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord . 1988;14(1):61-68. PubMed doi :10.1016/0165-0327(8 8)90072-9
13. Wilhelm S, Phillips KA, Fama JM, et al. Modular cognitive-behavioral therapy for body dysmorphic disorder. Behav Ther . 2011;42(4):624-633. PubMed doi:10.1016/j.beth.2 011.02.002
Quick Links:
Hide Abstract
CTE Presenting as Psychogenic Nonepileptic Seizures
This case of a 14-year-old boy with a history of tbis highlights the evolution of neuropsy..., balancing psychiatric stability and cardiometabolic health in bipolar i disorder, dr goldberg takes viewers through two case profiles of patients with bipolar i disorder, including assessment, diagnosis, and treatment, with a focus on cardiometabolic safety., pharmacogenetic phenotypes in a perinatal mental health clinic, in patients of childbearing age who have had atypical responses or side effects to antidep..., impact of disability on medical care, given that many people have disabilities, physicians should develop skills that assess the..., why ask patients to cut into quarters 10 mg thc gummies from a dispensary when 2.5 mg thc is available by prescription, the authors discuss a study by sawicki et al of dementia patients for whom 2.5 mg of thc w....
Search Articles
Related articles, table of contents.

IMAGES
VIDEO
COMMENTS
Olfactory reference syndrome (ORS) is a lesser known disorder that is related to obsessive-compulsive disorder. ORS is the obsessional and inaccurate belief that one is emitting a foul odor leading to embarrassment or concern about offending others, excessive hygiene behaviors, and social avoidance that significantly interferes with daily functioning.
Olfactory reference syndrome (ORS) is a lesser known disorder that is related to obsessive-compulsive disorder. ORS is the obsessional and inaccurate belief that one is emitting a foul odor leading to embarrassment or concern about offending others, excessive hygiene behaviors, and social avoidance that significantly interferes with daily functioning. Although ORS is rare, it is challenging ...
Olfactory reference syndrome - A case report - Volume 26 Issue S2. Introduction. Olfactory reference syndrome (ORS), first described by Pryse-Phillips in 1971, is a rare psychiatric condition whose defining characteristic is a preoccupation with the belief that one emits a foul or offensive body odor, which is not perceived by others.
Introduction. Olfactory Reference Syndrome (ORS) is a psychiatric condition characterized by an erroneous belief that one is exuding a false body odor, that brings significant distress and socio-functional impairment to the patient, albeit, is undetectable to others. 1 Described as a disorder in a case series of 36 patients for the first time in 1971, the literature since then is permeated ...
1. Introduction. The symptoms of Olfactory Reference Syndrome (ORS) were first described in a case series of 36 patients by Pryse-Phillips in 1971 [].Although published literature on the subject spans more than a century, areas of controversies persist in terms of the nosology and treatment of the disease [].The core symptomatology of ORS is characterized by a preoccupation with the belief ...
O lfactory reference syndrome (ORS) is an ill-. ness that has been the subject of debate since. its fi rst description more than a century ago. (Potts, 1891). In a comprehensive study of 137 pa ...
Olfactory Reference Syndrome (ORS) is understudied. • ORS shares manifestations in some psychiatric disorders. It is unique in the idea of having a bad smell. • Combining CBT with SSRIs can be a good treatment plan for OSR. • Having a good presenting problem understanding will yield a correct case conceptualization and effective intervention.
the term olfactory reference syndrome to Pryse-Philips who proposed the same after analysing a large case series [1]. e condition has received several other monikers, chiey, parosmia [2], hallucinations of smell [1], chronic olfactory paranoid syndrome [3], and monosymptomatic hypochondriacal psychosis [4]. It was predominantly
Cognitive Behavioral Therapy for Olfactory Reference Syndrome: A Case Report J Clin Psychiatry. 2016 Sep;77(9):e1144. doi: 10.4088/JCP.15cr10451. Authors Jasper B Zantvoord 1 2 3 , Nienke Vulink 2 , Damiaan Denys 2 4 Affiliations 1 Department of Psychiatry, Academic Medical Centre ...
Olfactory reference syndrome (ORS) is a distressing clinical condition characterized by the belief that one's body emits a foul odor which disturbs others though others are unable to perceive the ...
Objective: The objective was to report a case of olfactory reference syndrome (ORS) with several co-occurring disorders and to discuss ORS differential diagnoses, diagnostic criteria and classification. Method: Case report. Results: A 37-year-old married woman presented overvalued ideas of having bad breath since adolescence. . She met current diagnostic criteria for social anxiety disorder ...
In olfactory reference syndrome, concerns about perceived body odor cause distress and may impair functioning. ... Some case studies have reported (partial) response with clomipramine, 1,3,4 while others have reported nonresponse. 5-7 The interpretation of previous case reports on behavioral therapy and eye movement desensitization and ...
Olfactory Reference Disorder (ORD), also referred to as Olfactory Reference Syndrome, is a persistent preoccupation with the belief that the sufferer emits a foul and unpleasant body odour despite lack of evidence to the contrary. ... The current case study adds to the literature by guiding the reader in detail through treatment using these ...
Olfactory reference syndrome (ORS) is a lesser known disorder that is related to obsessive-compulsive disorder. ORS is the obsessional and inaccurate belief that one is emitting a foul odor leading to embarrassment or concern about ofending others, excessive hygiene behaviors, and social avoidance that significantly interferes with daily ...
and treatment of olfactory reference syndrome: a case study. J Obsessive Compuls Relat Disord. 2018;19:23-28. CrossRef 5. Das S, Sekharan L, Prasad S, et al. Olfactory reference syndrome treated with lurasidone and cognitive behavioral therapy: a case report. Clin Med Insights Case Rep. 2022;15:11795476221139396. PubMed CrossRef
INTRODUCTION. Olfactory reference syndrome (ORS) -- preoccupation with a false belief that one emits a foul or offensive body odor -- has been described for over a century [1-3].Cases have been reported around the world, including Africa, Japan, Europe, South America, Canada, the Middle East, and the United States [3,4].However, ORS's clinical features have received little systematic study.
We owe the clinical description and the term olfactory reference syndrome to Pryse-Philips who proposed the same after analysing a large case series . The condition has received several other monikers, chiefly, parosmia [ 2 ], hallucinations of smell [ 1 ], chronic olfactory paranoid syndrome [ 3 ], and monosymptomatic hypochondriacal psychosis ...
Olfactory Reference Syndrome: Problematic Preoccupation with Perceived Body Odor. ... No prospective medication studies have been done (either controlled or open-label studies). Case reports and small case series describe improvement with serotonin reuptake inhibitor (SRI) monotherapy, neuroleptic (antipsychotic) monotherapy, non-SRI ...
The published literature on olfactory reference syndrome (ORS) spans more than a century and provides consistent descriptions of its clinical features. ... While this possibility requires investigation, studies and case descriptions of ORS over the past century provide a consistent description of its clinical features, suggesting that ORS is ...
The two case reports of olfactory reference syndrome (ORS) presented here can be used as a basis for a discussion of the relationship between this entity and OCD. Phenomenologic, neurobiologic, and pharmacologic issues will be considered in turn. The phenomenology of the symptoms in the two patients is reminiscent of OCD in a number of respects.
The published literature on olfactory reference syndrome (ORS) spans more than a century and provides consistent descriptions of its clinical features. ... While this possibility requires investigation, studies and case descriptions of ORS over the past century provide a consistent description of its clinical features, suggesting that ORS is ...
In olfactory reference syndrome, concerns about perceived body odor cause distress and may impair functioning. ... Some case studies have reported (partial) response with clomipramine, 1,3,4 while others have reported nonresponse. 5-7 The interpretation of previous case reports on behavioral therapy and eye movement desensitization and ...
Olfactory Reference syndrome (ORS) is a rare syndrome and is quite challenging to diagnose. It is characterised ... Case-1:A 28 years old graduate male employed in a private company belonging to Middle Socioeconomic Status ... In a largest study by Greenberg et al. (2016) (N=253), the most commonly reported symptom ...