An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol

How Psychological Safety Affects Team Performance: Mediating Role of Efficacy and Learning Behavior
1 Department of Business Administration, Seoul School of Integrated Sciences & Technologies (aSSIST), Seoul, South Korea
2 Department of Education, Chung-Ang University, Seoul, South Korea
Timothy Paul Connerton
3 Business School Lausanne, Chavannes, Switzerland
Associated Data
The datasets generated for this study are available on request to the corresponding author.
This article examines the mechanisms that influence team-level performance. It investigates psychological safety, a shared belief that the team is safe for interpersonal risk taking and a causal model mediated by learning behavior and efficacy. This model hypothesizes that psychological safety and efficacy are related, which have been believed to be same-dimension constructs. It also explains the process of how learning behavior affects the team’s efficacy. In a study of 104 field sales and service teams in South Korea, psychological safety did not directly affect team effectiveness. However, when mediated by learning behavior and efficacy, a full-mediation effect was found. The results show (i) that psychological safety is the engine of performance, not the fuel, and (ii) how individuals contribute to group performance under a psychologically safe climate, enhancing team processes. Based on the findings, this article suggests theoretical and methodological implications for future research to maximize teams’ effectiveness.
Introduction
Teams play a crucial role in highly effective organizations. Teams perform better than individuals ( Glassop, 2002 ), becoming sources for firms’ sustainable competitive advantage. Through horizontal interaction, the knowledge gained by teams contributes to performance on an organizational level ( Edmondson, 2012 ). There is a growing concern about how to improve the performance of teams in organizations. Although a large body of literature has focused on individual motivation over decades, research to advance the understanding of team motivation processes is insufficient ( Kozlowski and Bell, 2003 ; Chen and Kanfer, 2006 ).
From the literature, physical factors such as team size and task attributes, personal factors such as member competencies and personality, and organizational–environmental factors were studied as antecedents of team effectiveness (TEF) ( Cohen and Bailey, 1997 ; Mathieu et al., 2008 ). However, organizations are gradually recognizing the value of psychological assets, the importance of synergy among individuals and groups for innovation and growth in highly competitive markets ( Donaldson et al., 2011 ).
The concept of psychological safety appeared half a century ago in the organizational science field, but in recent years, empirical research flourished ( Frazier et al., 2017 ). Previous literature has shown that psychological safety has a direct influence on work performance ( Baer and Frese, 2003 ; Schaubroeck et al., 2011 ). Besides, more authors insisted that organizational support, safety climate, and performance are unquestionably related, implying that psychological safety might involve benefits that extend its influence on work engagement ( Rich et al., 2010 ; Christian et al., 2011 ).
Team psychological safety (TPS) is a shared belief that people feel safe about the interpersonal risks that arise concerning their behaviors in a team context ( Edmondson, 2018 ). “Project Aristotle,” which explored over 250 team-level variables, found that successful Google teams have five elements in common: psychological safety, dependability, structure and clarity, meaning, and impact of work ( Google, 2015 ). The findings argue that psychological safety is the most critical factor and a prerequisite to enabling the other four elements. However, surprisingly, despite the importance of that psychological factor, only 47% of employees across the world described that their workplaces are psychologically safe and healthy ( Ipsos, 2012 ).
As Edmondson (2018) pointed out, TPS is the engine of performance, not fuel. Various factors affect the mechanism in the underlying process. What we need to understand is “how” psychological safety leads to team performance. What is necessary for identifying such mechanisms are (i) extended, sustained research at group level and (ii) expansion of the studies in various contexts (e.g., country and culture). Notably, research conducted at the group level is insufficient compared to those conducted at the individual level in psychological safety literature. If related work continues and data accumulate, the theoretical background to examine the incremental validity issue at the group level will be intensified ( Frazier et al., 2017 ).
In many cases, psychological safety has been studied in limited regions (i.e., advanced economies in the west), and now the research context needs to be expanded ( Abror, 2017 ). There is a need to verify the influence of psychological safety on group performance, enhancing its explanatory potential and applicability in the workplace. Additional research is needed to determine what factors mediate the relationship between psychological safety and group effectiveness.
Psychological safety could affect behavioral outcomes such as team’s creativity ( Madjar and Ortiz-Walters, 2009 ), and both individual learning ( Carmeli and Gittell, 2009 ; Carmeli et al., 2009 ) and team learning ( Edmondson, 1999 ; Wong et al., 2010 ). Team learning behavior (TLB) is a symbolic variable that affects TEF. TLB is the process by which members interact, acquire knowledge and skills needed for their work, and share information ( Argote et al., 1999 ), and it raises the team process level to generate performance-oriented ideas. When members learn and improve their problem-solving skills, they can create a competitive organization ( Dyer and Nobeoka, 2000 ). Despite the mediating role of learning that has been empirically demonstrated in previous literature, it still needs to be dealt with as a research subject when considering the significance of learning in modern organizations.
Psychological safety has been linked to several attitudinal outcomes as well. Another factor that drives TEF is efficacy. Team efficacy (TE) is a member’s assessment of team ability to perform job-related activities successfully ( Walumbwa et al., 2004 ). Confidence in the team’s abilities affects performance and aligns the members’ activities on the team level ( Gibson et al., 2000 ; Gully et al., 2002 ). However, few studies have reported the effects of psychological safety to efficacy to present ( Abror, 2017 ). Therefore, there is a theoretical implication to see how efficacy mediates the relationship between psychological safety and performance at the group level. We selected the team’s learning behavior and efficacy as mediating variables to understand the mechanism for creating TEF. Despite the extensive research and empirical support for the critical role of psychological safety, a few unclear questions remain: How does psychological safety affect TEF? How does it affect learning behavior and efficacy? How does learning behavior mediate the overall relationship, and how does it affect the team’s efficacy? Does TE mediate between psychological safety and TEF?
Our aim in this research is to contribute to the team and psychological safety literature in three ways: (i) bring team literature together with related theories by examining psychological safety and learning behavior as determinants of TE; (ii) extend the TEF model and the traditional input–process–output (I–P–O) framework ( Hackman, 1987 ; Cohen and Bailey, 1997 ) by integrating psychological safety (as contextual input), learning behavior, and efficacy (as process and team traits) that might stimulate TEF; and (iii) embrace TE as a possible mediator between psychological safety and TEF creation.
Literature Review and Research Model
Psychological safety is “a condition in which one feels (a) included, (b) safe to learn, (c) safe to contribute, and (d) safe to challenge the status quo , without fear of being embarrassed, marginalized or punished in some way” ( Clark, 2019 ). TPS is a group variable that describes team context. In the last decade, the concept of psychological safety started attracting attention as a primary factor in predicting TEF.
Results from several empirical studies conducted in various regions and countries show that psychological safety plays a vital role in workplace effectiveness ( Edmondson and Lei, 2014 ). The psychological safety of individuals and their teams’ psychological safety are different constructs ( Baer and Frese, 2003 ). The concept was first pioneered by Schein and Bennis (1965) in organizational phenomena and developed by Kahn (1990) as a representative definition of the psychological safety of an individual.
Creating a psychologically safe workplace is different from being undisciplined or being unconditionally generous to any process or outcome ( Edmondson, 2012 ). Two factors—psychological safety and accountability for performance—identify four types of teams. In this regard, the presence of TPS does not necessarily mean that TEF will increase automatically.
Prior research also focused on the relationship between psychological safety and outcomes such as innovation, employee attitudes, creativity, knowledge sharing, voice behaviors, and communication ( Newman et al., 2017 ). Overall, TPS is known to have a positive association with TEF ( Schaubroeck et al., 2011 ; Kessel et al., 2012 ; Newman et al., 2017 ).
Extant literature has found positive associations between psychological safety and learning behavior at different levels ( Newman et al., 2017 ). Several pieces of empirical evidence on such relationships were found in previous literature at the team level ( Roberto, 2002 ; Van den Bossche et al., 2006 ; Stalmeijer et al., 2007 ; Bstieler and Hemmert, 2010 ; Ortega et al., 2010 ; Wong et al., 2010 ) and individual level.
In addition to this, the relationship between TPS and efficacy should be confirmed. Abror (2017) argues that TPS affects group efficacy. The author criticized Edmondson (1999) for putting TPS and TE on the same level and argued for the need to identify the relationship between the two factors. Recent studies started arguing that TPS may affect group efficacy ( May et al., 2004 ; Roussin et al., 2016 ; Hernandez and Guarana, 2018 ). TPS appears to have a significant effect on team behavior and goal orientation and improves performance while affecting a team’s efficacy ( Roussin et al., 2016 ). The following hypotheses arise from the above background.
- H1: TPS positively affects TEF.
- H2: TPS positively affects TLB.
- H3: TPS positively affects TE.
Discussions on team learning arose since Argyris (1986) defined organizational learning and discussed it as a sub-element of a learning organization. Edmondson (1999) used the term “team learning behavior” to distinguish the learning process from learning outcomes.
Team learning behavior is defined as gaining and sharing skills, knowledge, and information about work through the interaction of members ( Argote et al., 1999 ), an iterative team process leading to a change ( van Offenbeek, 2001 ). Gibson and Vermeulen (2003) defined TLB as a process of experimentation, reflective communication, and codification. The three elements are interdependent and difficult to replace. Edmondson et al. (2007) divided the perspective on team learning research into three streams.
Previous literature has shown that there is a positive relationship between TLB and TEF. Zellmer-Bruhn and Gibson (2006) identified the factors that influence team learning, team learning’s effects on task performance, and interpersonal relationships. TLB had a positive effect on TE. Van den Bossche et al. (2006) studied how teams build shared beliefs in a collaborative learning environment and found that team learning improves the perceived performance of a team.
Team learning behavior is also known to be positively associated with the team’s efficacy (i.e., van Emmerik et al., 2011 ). However, further research is needed to verify the direction of the causal relationship between the two variables.
This study views TLB as a process variable and identifies the relationship between TPS and TEF. Also, TLB’s mediating role between TPS and TE would be identified to confirm its value as a useful predictive tool. This section raises the following hypotheses:
- H4: TLB positively affects TEF.
- H5: TLB positively affects TE.
TE has a vital role in team research ( Rico et al., 2011 ). As the importance of creating team-based outcomes has grown, TE has attracted the interest of researchers ( Day et al., 2009 ).
Efficacy is the belief that an individual’s ability or competency to perform a particular task will produce a successful outcome ( Bandura, 1986 , 1997 ). When expanded into a group level, it becomes group efficacy, which is the belief of group members that they can accomplish a given task. TE is unlikely to be the sum of individual competence and self-esteem ( Bandura, 2000 ).
The concept of TE, together with team resilience and team optimism, is a representative sub-construct of positive organizational behavior ( West et al., 2009 ). It is an essential antecedent predicting group performance ( Werner and Lester, 2001 ; Gully et al., 2002 ; Chen et al., 2005 ; Tasa et al., 2007 ; Porter et al., 2011 ; Zoogah et al., 2015 ). The literature supports that efficacy coordinates group processes, such as decision-making and team communication. The level of belief can lead to different outcomes, even under the same conditions. Several empirical works have proved the effect of TE on team performance ( Mathieu et al., 2008 ). In the TE literature, it appears to influence TEF.
As such, we predicted that TE would activate collective processes and impact group performance. Teams that believe they can succeed in a given task can perform better. TE is expected to play an indispensable role in achieving crucial tasks that require enhanced team performance.
- H6: TE positively affects TEF.
Concepts such as team performance, characteristics, and attitudes of team members define TEF in a comprehensive way ( Shen and Chen, 2007 ). It is difficult to measure or give TEF one single definition. In earlier literature of TEF, the majority of studies defined “effectiveness” as physical outcomes. However, it gradually expanded to the concept of team performance, characteristics, or member attitudes ( Shen and Chen, 2007 ). Lin et al. (2005) insist that researchers should pay attention to various factors simultaneously at the individual and organizational levels to maximize performance.
Rousseau et al. (2006) summarized studies dealing with individual-level variables that improve TEF. As noted, the effectiveness criteria for defining a team’s performance are not limited to the team’s physical output. In addition to productivity, most studies adopted team member satisfaction, attitudes, and perceived outcomes as essential measures. The most widely used are performance and attitude aspects. In this study, TEF is measured by a team’s perception of their performance. Team performance is the result of a dynamic process of member interaction. In-role behavior describes a state in which team members play a supportive role in achieving goals ( Williams and Anderson, 1991 ). Surveys are common ways to measure perceived team performance ( Pearce and Sims, 2002 ; Pearce and Herbik, 2004 ). In this study, in-role behavior will measure TEF.
Theoretical Framework and the Moderating Role of TLB and TE
The theoretical foundation can be put on the social cognitive theory ( Bandura, 1988 ). According to the theory, learning is a cognitive process taking place in a social context and could occur purely via observation or instruction, even without direct reinforcement. Also, one’s sense of efficacy can play a crucial role in approaching goals, tasks, and challenges ( Luszczynska and Schwarzer, 2005 ). The theory adequately describes the mechanism of how psychological safety leads to its outcome variables and the relationship between behavioral changes and cognitive beliefs.
Psychological safety at the group level as a model of TEF uses some forms of the input–process–output (I–P–O) model as a theoretical framework. The I–P–O model is an approach that explains the mechanism of team outcome creation. It was Gladstein (1984) and Hackman (1987) who introduced the I–P–O model to explore the mechanism, and Cohen and Bailey (1997) further expanded the model to the TEF model. This framework suits the structural mediation process that involves TLB and TE as process variables for the research. The framework is still valid in many effectiveness research ( Liu et al., 2010 ; Dulebohn and Hoch, 2017 ; Escribano et al., 2017 ; Mansikka et al., 2017 ).
Team learning behavior is known to mediate the relationship between psychological safety and performance ( Edmondson, 1999 ; Li and Yan, 2009 ; Brueller and Carmeli, 2011 ; Kostopoulos and Bozionelos, 2011 ; Hirak et al., 2012 ; Huang and Jiang, 2012 ; Li and Tan, 2013 ; Ortega et al., 2014 ). Sanner and Bunderson (2013) found in their meta-analysis that TLB was a significant mediator in a large body of literature. In this regard, we try to confirm TLB’s mediating role in the TEF creation mechanism.
Bandura (1988) identified factors that affect efficacy. Social persuasion is encouragement or discouragement from another person. Also, psychological factors alter the level of efficacy. As noted earlier in the literature review, the team’s efficacy affects the performance ( Luszczynska and Schwarzer, 2005 ), and TLB affects TE.
As such, this study investigates the following mediation effects. The hypothesized relationships of the research model (see Figure 2 ) are as follows:

Research model.

Psychological safety-accountability for performance framework. Source: Edmondson (2012 : 174).
- H7: TLB mediates the relationship between TPS and TE.
- H8: TE mediates the relationship between TPS and TEF.
- H9: TLB and TE jointly mediate the relationship between TPS and TEF.
Research Methodology
We collected samples from 16 local sales and service companies located in 98 outlets in South Korea. The survey targeted sales, service, and admin staff working at the front line. Under normal working conditions, field employees providing customer service have to work with a high level of customer orientation, with their service level evaluated continuously. Besides, they are exposed to complaints from dissatisfied customers and feel pressure about their performance, resulting in significant anxiety and stress. Therefore, fieldwork teams were considered appropriate for the research.
A mobile survey was sent to a total of 282 teams and 1,433 employees. Five hundred thirty-six questionnaires were recovered (37%), and 529 valid samples were analyzed. Frequency analysis was performed to examine the distribution of respondents (see Table 1 ).
Demographic characteristics of the participants.
| Attributes | Frequency | (%) | Attributes | Frequency | (%) | ||
| Gender | Male | 465 | 87.9 | Tenure in team (months) | Under 6 | 87 | 16.4 |
| Female | 64 | 12.1 | 6∼12 | 80 | 15.1 | ||
| Age | Under 30 | 120 | 22.7 | 13∼24 | 94 | 17.8 | |
| 30∼35 | 142 | 26.8 | 25∼36 | 59 | 11.2 | ||
| 35∼40 | 133 | 25.1 | Above 37 | 209 | 39.5 | ||
| 40∼50 | 132 | 25.0 | Team function | Admin | 55 | 10.4 | |
| Above 50 | 2 | 0.4 | Sales | 236 | 44.6 | ||
| Tenure in company (years) | Under 3 | 222 | 42.0 | Service | 238 | 45.0 | |
| 3∼5 | 132 | 25.0 | Team size | 5 | 149 | 28.2 | |
| 5∼10 | 121 | 22.9 | 5∼7 | 253 | 47.8 | ||
| 10∼15 | 41 | 7.8 | 8∼10 | 80 | 15.1 | ||
| Above 15 | 13 | 2.5 | 11∼14 | 22 | 4.2 | ||
| Title | Staff | 207 | 39.1 | Above 15 | 25 | 4.7 | |
| AM | 126 | 23.8 | Education | High school | 109 | 20.6 | |
| MGR | 96 | 18.1 | Associate degree | 200 | 37.8 | ||
| AGM | 73 | 13.8 | Bachelor’s degree | 206 | 38.9 | ||
| Above GM | 27 | 5.1 | Master’s degree | 11 | 2.1 | ||
| Total | 529 | 100.0 | Doctor’s degree | 3 | 0.6 | ||
| No. of members (mean) | 4.5 | Member’s age (mean) | 31 | ||||
Respondents had the following characteristics: gender, 465 male (87.9%) and 64 female (12.1%); age, 30s group highest (26.8% for 30–35 and 25.1% for 35–40), mean = 31; title, staff level highest (39.1%); tenure, under 3 years (42.0%); tenure in the team, 3 years or above (39.5%); team size, less than five members (28.2%), mean = 4.5; team function, admin (10.4%), sales (44.6%), and service (45.0%); and education, bachelor’s degree (38.9%).
Measurements
Original measurements developed in English were translated to Korean and reviewed by HRD professionals and a group of Ph.D. students to ensure accuracy in the delivery of the meaning. All 27 items adopted a Likert 7-point scale, from 1 = not at all to 7 = to a large extent. TPS consisted of seven questions by Edmondson (1999) . Sample items were as follows: “Members are criticized when making a mistake,” “Members often ignore individual’s opinion,” and “Members do not degrade other people’s efforts.”
Team learning behavior adopted nine items from Gibson and Vermeulen (2003) . Sample items were as follows: “The team’s ideas and practices are introduced to other teams,” “Members exchange ideas,” and “The team leaves documents about the details of work.”
For measuring TE, we adjusted six items by Riggs and Knight (1994) . Sample items were as follows: “Members have the best work skills,” “Members have above-average ability,” “The team has excellent performance compared to other teams.”
Team effectiveness was adapted from Williams and Anderson (1991) , with the following sample items: “Fulfilling responsibilities given by the organization,” “Achieving the level of task that we expect,” and “Meeting official performance requirements” (see Table 2 and Appendix 1 ).
Measurement items of the construct.
| Variable | No. | Scale | Source | ||
| Independent | Team psychological safety | 7 | Likert 7-point | ||
| Mediator | Team learning behavior | Experimentation | 3 | ||
| Reflective communication | 3 | ||||
| Codification | 3 | ||||
| Team efficacy | 6 | ||||
| Dependent | Team effectiveness (in-role behavior) | 5 | |||
Analytical Procedure
Process Macro 3.3 was used for the mediated regression model, and Jamovi 1.0.0.0 was used for other analytical procedures, including exploratory factor analysis (EFA) and CFA. First, the demographic distribution was confirmed by frequency analysis. Second, the normality of distribution was tested by descriptive analysis. Third, EFA was carried out to test the variance. Fourth, the confirmatory factor analysis (CFA) secured the validity and reliability of the measurement model. Fifth, we tested the reliability and validity of each team’s value through ICC and R wg tests to clear level issues. Sixth, the regression analysis confirmed the relationships between variables. Seventh, statistical significance was confirmed by bootstrap replications. It verified the mediating effects and effect size within the relationships.
There is a possibility of common method bias (CMB) when measuring constructs in the same survey. This issue can lead to the structural underestimation or overestimation of the coefficients ( Bido et al., 2017 ). As criticized by Guide and Ketokivi (2015) , researchers should be careful about claiming that the issue is cleared after conducting weak tests, such as Harman’s (1967) . In this case, EFA is considered a legitimate statistical procedure to test CMB that supplements the weaknesses of Harman’s, considering both the structural model and the measurement model ( Bido et al., 2017 ). Also, when trying to identify a potential structure or to ensure if the measurements reflected the construct accurately, an additional EFA procedure could be considered, regardless of existing theoretical backgrounds ( Fabrigar and Wegener, 2012 ).
In this study, the maximum likelihood method and oblimin rotation were applied to extract the factors. In the process, variables that did not meet the criteria were removed (factor loadings less than 0.50 and communality less than 0.40). The results of Cronbach’s α confirmed the reliability of measurement instruments (see Table 3 ).
Result of exploratory factor analysis.
| Item | Factor loading | Communality | Cronbach’s α | |||
| 1 | 2 | 3 | 4 | |||
| TPS_1 | – | – | – | 0.682 | 0.510 | 0.793 |
| TPS_2 | – | – | – | 0.361 | 0.324 | |
| TPS_3 | – | – | – | 0.689 | 0.622 | |
| TPS_5 | – | – | – | 0.600 | 0.568 | |
| TLB _ex_1 | 0.621 | – | – | – | 0.787 | 0.922 |
| TLB_ex_2 | 0.647 | – | – | – | 0.705 | |
| TLB_ex_3 | 0.641 | – | – | – | 0.543 | |
| TLB_com_3 | 0.519 | – | – | – | 0.791 | |
| TLB_cod_1 | 0.758 | – | – | – | 0.545 | |
| TLB_cod_2 | 0.847 | – | – | – | 0.696 | |
| TLB_cod_3 | 0.810 | – | – | – | 0.604 | |
| TE_1 | – | 0.885 | – | – | 0.787 | 0.925 |
| TE_2 | – | 0.755 | – | – | 0.742 | |
| TE_4 | – | 0.819 | – | – | 0.715 | |
| TE_5 | – | 0.608 | – | – | 0.704 | |
| TE_6 | – | 0.622 | – | – | 0.727 | |
| TEF_1 | – | – | 0.621 | – | 0.713 | 0.916 |
| TEF_3 | – | – | 0.864 | – | 0.813 | |
| TEF_4 | – | – | 0.886 | – | 0.728 | |
| TEF_5 | – | – | 0.618 | – | 0.760 | |
| Eigen value | 4.126 | 3.799 | 3.107 | 2.353 | – | – |
| Variance (%) | 20.631 | 18.996 | 15.533 | 11.767 | 66.927 | – |
It was confirmed that the measurements constituting the four theoretical constructs were grouped into factors without difficulty, and the factor loadings and construct reliability (CR) were also found to be significant. The Bartlett test result showed that the model had a good fit ( P < 0.001), and the KMO statistics were 0.960, which is also acceptable. TPS question 2 showed a low communality level and was further reviewed for use in the following CFA. Finally, the model was used for CFA after removing three questions from TPS, one from TE, two from TLB, and one from TEF.
CFA was conducted to confirm the fit of the measurement model. The criteria for model fit are a chi-square NC (CMIN/ df ) of 5.0 and below, an absolute fitness index (SRMR) below 0.08, an RMSEA below 0.10, and incremental fitness index, TLI, and CFI above 0.90.
The average variance extracted (AVE) value ranged from 0.519 to 0.735, indicating that all variables met the criteria of 0.50 ( Bagozzi and Yi, 1988 ). The internal consistency of Cronbach’s α coefficient was found to be reliable, with all variables above 0.70 or higher ( Murphy and Davidshofer, 1988 ). The standard factor loadings of most items except for one item from TPS and two from TLB were above the recommended level of 0.70 and were significant ( P < 0.001) ( Hair et al., 2017 ). All the items in CFA were adopted, considering overall AVE ( Bagozzi and Yi, 1988 ). From the above analysis results, the measurement model is acceptable, showing an appropriate level of reliability.
The model fit details are as follows. From the results of χ 2 = 650 ( P < 0.001), NC (CMIN/ df ) = 3.963, TLI = 0.933, CFI = 0.942, SRMR = 0.044, and RMSEA = 0.075, no item showed lack in model fit criteria. The reliability analysis results are as shown in Table 4 .
Result of confirmatory factor analysis.
| Factor | Indicator | Estimate | Std. estimate | SE | -value | CR | AVE | Cronbach’s α |
| TPS | TPS_1 | 1.000 | 0.705 | – | – | 0.809 | 0.519 | 0.793 |
| TPS_2 | 0.758 | 0.568 | 0.066 | 11.600*** | ||||
| TPS_3 | 0.956 | 0.812 | 0.056 | 17.000*** | ||||
| TPS_5 | 0.928 | 0.772 | 0.060 | 15.400*** | ||||
| TLB | TLB_ex_1 | 1.000 | 0.899 | – | – | 0.921 | 0.627 | 0.922 |
| TLB_ex_2 | 0.894 | 0.846 | 0.032 | 27.600*** | ||||
| TLB_ex_3 | 0.805 | 0.734 | 0.038 | 21.100*** | ||||
| TLB_com_3 | 0.934 | 0.892 | 0.030 | 31.400*** | ||||
| TLB_cod_1 | 0.769 | 0.682 | 0.041 | 18.600*** | ||||
| TLB_cod_2 | 0.921 | 0.780 | 0.040 | 23.300*** | ||||
| TLB_cod_3 | 0.824 | 0.675 | 0.045 | 18.200*** | ||||
| TE | TE_1 | 1.000 | 0.873 | – | – | 0.927 | 0.719 | 0.925 |
| TE_2 | 1.033 | 0.864 | 0.038 | 27.300*** | ||||
| TE_4 | 0.953 | 0.832 | 0.038 | 25.400*** | ||||
| TE_5 | 0.894 | 0.836 | 0.035 | 25.500*** | ||||
| TE_6 | 1.130 | 0.834 | 0.045 | 25.300*** | ||||
| TFE | TEF_1 | 1.000 | 0.844 | – | – | 0.917 | 0.735 | 0.916 |
| TEF_3 | 1.197 | 0.879 | 0.046 | 26.000*** | ||||
| TEF_4 | 1.168 | 0.823 | 0.050 | 23.300*** | ||||
| TEF_5 | 1.160 | 0.881 | 0.045 | 25.900*** | ||||
| Criteria | – | – | Under 5.0 | Above 0.90 | Above 0.90 | Under 0.08 | Under 0.10 | Interval |
| Result | 650 | 164 | 3.963 | 0.933 | 0.942 | 0.044 | 0.075 | 0.069∼0.081 |
Validity of the Constructs
Convergent validity and discriminant validity were verified to confirm the validity of the construct. Convergent validity is verified by factor loading, CR, and AVE. Convergent validity was confirmed from the measurement model as all the constructs were found to be higher than 0.50 in factor loading, 0.70 in CR, and 0.50 in AVE (see Table 5 ).
Test of convergent validity.
| Item | Factor loading | CR | AVE | |||
| Criteria | Above 0.50 | Above 0.70 | Above 0.50 | |||
| Accepted | Accepted | Accepted | ||||
| TPS | 0.714 | TPS | 0.809 | TPS | 0.519 | |
| TLB | 0.787 | TLB | 0.921 | TLB | 0.627 | |
| TE | 0.848 | TE | 0.927 | TE | 0.719 | |
| TEF | 0.857 | TEF | 0.917 | TEF | 0.735 | |
Discriminant validity means that latent variables are constructs that are independent of each other. If the correlation between factors is relatively high (above 0.80 or 0.85), the researcher can consider a more parsimonious model ( Brown, 2015 ). The results of correlation analysis among the factors are presented (see Table 6 ).
Correlations between dimensions.
| Mean | SD | 1 | 2 | 3 | 4 | |
| 1. TPS | 5.748 | 1.249 | 1 | – | – | – |
| 2. TLB | 5.044 | 1.177 | 0.728*** | 1 | – | – |
| 3. TE | 5.615 | 1.109 | 0.750*** | 0.769*** | 1 | – |
| 4. TEF | 5.669 | 1.069 | 0.630*** | 0.772*** | 0.857*** | 1 |
The r ± 2SE method was applied to verify discriminant validity. This method adds and subtracts two standard error range from the correlation values of each factor and checks whether the value includes 1 in the range. The absence of 1 in the calculation range verifies the discriminant validity ( Fornell and Larcker, 1981 ). The r ± 2SE range of correlations among all factors did not include 1 (see Table 7 ).
Test of discriminant validity by r ± 2SE method.
| SE | - (2 × SE) | + (2 × SE) | Including 1 | ||
| TPS ↔ TE | 0.750 | 0.026 | 0.698 | 0.802 | N |
| TPS ↔ TLB | 0.728 | 0.027 | 0.674 | 0.782 | N |
| TPS ↔ TEF | 0.630 | 0.033 | 0.564 | 0.696 | N |
| TLB ↔ TE | 0.769 | 0.021 | 0.727 | 0.811 | N |
| TE ↔ TEF | 0.857 | 0.016 | 0.826 | 0.888 | N |
| TLB ↔ TEF | 0.772 | 0.021 | 0.729 | 0.815 | N |
Level Issue
This study assumes a team-level analysis. Klein et al. (1994) collectively defined three “level issues” that arise in group-level research, which are the level of theory, level of measurement, and level of analysis ( Klein et al., 1994 ). In this study, all the questionnaires measure the team’s view based on a reference-shift model. In the case of using the results of summed or averaged individual responses as a team value, there are two additional requirements as follows.
First, the group members’ responses must be consistent and show homogeneity. Second, the variation or variance between teams should be higher than that within a team. To prove this, Klein and Kozlowski (2000) proposed R wg (within-group interrater reliability), intraclass correlation (ICC)(1), and ICC(2). These are the methodologies that support inference for aggregation of individually collected data. This study conducted essential statistical procedures to resolve the level issues before aggregating individual values into a team value.
Checking the consistency and consensus of each rater’s answer to the question solves the problem. ICC is a standard method used for reliability verification in multilevel studies ( James, 1982 ). Reliability refers to the degree of consistency that an individual rater’s evaluation has, and there are two kinds, ICC(1) and ICC(2). Both use analysis of variance to verify data consistency. The usual cutoff level for ICC(1) is 0.20. ICC(2) further supplements ICC(1). It analyzes each group’s composite rating to verify the reliability and is acceptable at 0.60 or higher. The ICC(1) result shows that TEF did not meet the criteria, and TLB and TEF were not acceptable by ICC(2) baseline (see Table 8 ).
Test of level issue: ICC and r wg values.
| Factor | ICC(1) | ICC(2) | AVG. | -value |
| TPS | 4.340*** | |||
| TLB | 0.572 | 2.335*** | ||
| TE | 2.717*** | |||
| TEF | 0.144 | 0.431 | 1.757*** |
R wg is an additional verification procedure for the variables which did not meet baseline values. R wg , also referred to as the within-group agreement index, checks for consistency or reliability of lower-level data ( James et al., 1993 ). Its baseline is 0.70 or higher ( James et al., 1993 ; Klein and Kozlowski, 2000 ), but variables with R wg values higher than 0.50 can be aggregated as a team’s value ( James et al., 1993 ). Finally, a total of 104 team data were analyzed after excluding teams with less than three members and whose R wg values did not meet the requirements.
Hypothesis Test
Relationship between variables.
A process analysis was conducted to verify the effect size on direct and indirect effects simultaneously ( Hayes, 2013 ). By default, a thousand resampling of the percentile bootstrapping method is used to estimate the parameters. The absence of 0 in the 95% confidence interval identifies statistical significance ( Preacher et al., 2007 ; Hayes, 2013 ). The analysis was carried out based on the Hayes (2013) procedure to verify all the relationships and the direct and indirect effects.
The direct effect of TPS on TE was not significant (H1, β = 0.037). As expected, psychological safety activates team processes but may not direct driver of performance ( Edmondson, 2008 ). TPS had a positive effect on TLB (H2, β = 0.747) and had a significant positive effect on TE (H3, β = 0.596). The result was consistent with previous researches that a sense of safety has a significant impact on team behavior change and performance.
Also, TLB had a positive effect on TE (H4, β = 0.317). The learning process affected the team’s efficacy, which is the team’s emotional response. TLB had a positive effect on TEF (H5, β = 0.193) and was consistent with previous studies’ results that learning improves the quality of task performance.
Finally, the positive effect on TEF of TE was confirmed (H6, β = 0.694). In summary, TPS did not directly affect effectiveness but had a positive effect on other variables. In the other causal paths, positive causal relationships were identified (see Figure 3 and Table 9 ).
Result of main effect analysis.
| Hypothesis | Path | β | SE | LLCI | ULCI | Remarks | |
| H1 | TPS → TEF | 0.037 | 0.064 | 0.413 | (0.100) | 0.153 | Rejected |
| H2 | TPS → TLB | 0.747 | 0.060 | 11.349*** | 0.563 | 0.801 | Accepted |
| H3 | TPS → TE | 0.596 | 0.063 | 7.788*** | 0.367 | 0.618 | Accepted |
| H4 | TLB → TE | 0.317 | 0.069 | 4.149*** | 0.150 | 0.425 | Accepted |
| H5 | TLB → TEF | 0.193 | 0.060 | 2.513* | 0.032 | 0.268 | Accepted |
| H6 | TE → TEF | 0.694 | 0.079 | 7.520*** | 0.438 | 0.752 | Accepted |

Research model with regression coefficient values. ns: not significant.
Mediating Effect
For the mediating effects to be statistically significant, the indirect effect must show significance in the relationship of the independent variable to the dependent variable. If only the indirect effect is significant in a proposed model, it is a full-mediation effect. In a partial-mediation model, both indirect and direct effects are significant.
The mediating effect of TLB was identified between TPS and TEF (H7, β = 0.144). Also, the mediating role of TE was verified between TPS and TEF (H8, β = 0.413). The effect size was confirmed, and the upper and lower bounds of the 95% confidence interval did not contain 0. TLB and TE showed a double-mediation effect on the relationship between TPS and TEF (H9, β = 0.165).
The total effect of the research model was significant (β = 0.722). The applicability of the research model was supported, and TE was found to have the most substantial indirect effect. The results of the mediation effect analysis are presented (see Table 10 ).
Total, direct, indirect effect of research model.
| Hypothesis | Effect | Path | β | SE | LLCI | ULCI | Remarks |
| Total | TPS → TEF | 0.722 | 0.077 | 0.556 | 0.861 | Full mediation | |
| Direct | TPS → TEF | 0.037 | 0.064 | (0.100) | 0.153 | – | |
| H7 | Indirect 1 | TPS → TLB → TEF | 0.144 | 0.070 | 0.009 | 0.276 | Accepted |
| H8 | Indirect 2 | TPS → TE → TEF | 0.413 | 0.074 | 0.283 | 0.562 | Accepted |
| H9 | Indirect 3 | TPS → TLB → TE → TEF | 0.165 | 0.056 | 0.069 | 0.286 | Accepted |
In conclusion, TPS did not directly affect TEF, but TLB and TE indirectly influenced TEF. It also confirmed that TLB contributed to team performance through TE. From the above, the full-mediation and double-mediation effect were found in the research model.
This paper explored how psychological safety influences the team’s effectiveness through learning behavior and efficacy. We applied two mediators in the research design to examine causal relationships. In summary, the research model was found to have a full double-mediation effect. TPS did not have a direct effect on the dependent variable.
First, based on social cognitive theory, we have found the crucial roles of learning behavior and efficacy in connecting psychological safety and TEF. The finding of team learning’s mediation effect is consistent with previous studies (i.e., Kostopoulos and Bozionelos, 2011 ). Also, the mediating role of TE has been confirmed. To date, little research has been done on the mediating role of TE between psychological safety and TEF. As discussed earlier, psychological factors and climate could alter the level of efficacy. According to social cognitive theory, traits such as the team’s expectations and beliefs could be affected by the psychological factors (environment) and influencing behavior. When members believe that they can complete a given task, the team produces more positive results (e.g., Tasa et al., 2007 ; Porter et al., 2011 ).
Second, the results showed that learning behavior positively affects the team’s efficacy. The result was in line with van Emmerik et al. (2011) . This finding answers the request of Knapp (2016) for additional research to determine if efficacy is significantly related to learning behavior at the team level. Learning behavior is a process that leads to a shared result and is a link toward change in organizations. If the members recognize excellent communication in the team, they become more involved, and the belief in the team’s ability could be strengthened.
Third, the results did not support one of our hypotheses that psychological safety affects TEF. The research model supported full mediation. This result is consistent with the claims of Edmondson (2012 , 2018) . Psychological safety is the “engine,” not “fuel” for performance. If individuals are under an atmosphere that highly values their ideas and actions, employees can adapt themselves even to challenging tasks. A team’s psychological safety promotes team learning and consequently increases the team’s effectiveness. Also, the favorable climate promotes the team’s efficacy and contributes to the performance of the team.
Theoretical Implications
The findings of the study present important contributions to the present knowledge in the domain. First, the research contributes to psychological safety literature by unfolding its little-known relationship with TE, answering the theoretical call from Abror (2017) to examine the relationship between the two constructs. As discussed, we found a significant effect of TPS to TE, confirming the mechanism of how team performance is created through the path.
Today, there is only limited empirical evidence on the effect of psychological safety to efficacy ( Abror, 2017 ). The author criticized Edmondson (1999) for putting the two variables on the same level. Until recently, researchers have insisted that TPS and TE are both psychological factors on the same dimension. Therefore, the causal relationship between the two is rarely experimented. This paper aims to ignite debates on that theoretical discordance in the future based on the full-mediation effect identified.
Recent studies started arguing that psychological safety might affect group efficacy (e.g., Roussin et al., 2016 ; Hernandez and Guarana, 2018 ). In the field of education, researchers started reporting the relationship between psychological climate and efficacy. When there is a respectful, collaborative, and trusting school climate ( Bryk et al., 2010 ; Ronfeldt et al., 2013 ), teachers tend to report higher levels of efficacy and more likely to stay in the profession ( Allensworth et al., 2009 ; Johnson et al., 2012 ). The research hinted at the theoretical implications and discussions, moving a step forward under the workplace context.
Second, our research contributes to the current literature of TEF by developing and exploring the two different mediating paths, further broadening the boundaries of the studies in human behavior.
The study extends the prevailing framework for TEF ( Cohen and Bailey, 1997 ) by adding empirical data. In the research model, we added a less-proven relationship (i.e., TE as another mediator) to a “psychological safety–team learning–effectiveness” model, further contributing to the applicability and the expandability of the variables as valid predictors in future team studies. To our knowledge, little research has been conducted at a team level, incorporating TPS, TLB, TE, and TEF.
We approached from the aspects of social cognitive theory to explain the TEF creation mechanism that is affected by psychological factors. Prior literature also examined the relationship between psychological safety and other outcomes, integrating theoretical views from social learning theory, social identification theory, social information processing theory, or social exchange theory ( Carmeli, 2007 ; De clercq and Rius, 2007 ; Schaubroeck et al., 2011 ; Singh et al., 2013 ; Chen et al., 2014 ; Liu et al., 2014 ; Wang et al., 2018 ). Our study contributes to building concrete theoretical foundations, enriching various angles available to decipher the complicated phenomena under a team context.
The effect of TLB on TE also presents a new perspective. Previous research has demonstrated that efficacy affects learning behavior (i.e., van Emmerik et al., 2011 ). However, the studies that reported learning behavior’s effect on TE are limited. This study argues that learning behavior can be a catalyst for the efficacy of teams.
Furthermore, our research answers Frazier et al.’s (2017) call to continue research under the team context. Group-level research is insufficient compared to individual-level studies, and continued research would contribute to the robustness of related theories ( Frazier et al., 2017 ).
Third, the study extended the contexts where psychological safety research takes place. Most of the research was conducted in western countries and advanced economies ( Abror, 2017 ). Moreover, most of the literature dealt with limited work context (e.g., medical, healthcare, and nursing). This research paid attention to frontline sales and service employees in South Korea, broadening boundaries for future empirical work.
Implications for Practice
The research results may provide several implications for practice. First, the findings point to the vital role of safety climate as a performance enabler in an organization. Top management’s intense pressure can lead to extreme consequences ( Edmondson, 2018 ). Unconditional emphasis on psychological safety is also undesirable. Unrestrained psychological well-being could result in cheating and incompliance with the group’s social constraints ( Pearsall and Ellis, 2011 ). Leaders should pay close attention to establishing an equilibrium that might maximize team performance. Teams can move into a “learning zone” when accountability for performance interacts with psychological safety.
Second, the findings also suggest that energizing the team’s process should be considered for enhanced performance in teams. When a safe environment is ready, members facilitate learning from failures ( Hirak et al., 2012 ), and members’ feedback-seeking behavior and adaptability could be strengthened ( Gong and Li, 2019 ). Therefore, leaders can take a strategy that promotes a psychologically safe climate and stimulates interaction, regardless of external support at a team level. Raising the team’s efficacy would be a superior strategy, too. Regarding the limited resources and authority of team leaders, promoting the team process can be a reliable approach.
Third, the results shed light on the importance of team learning in an organizational context. There are limitations to a top-down approach and centralized training. Learning at a lower level should be stressed as a way of contributing to the firm’s sustainability. Leaders should pay attention to approaches that nurture the dynamic learning process that mediates psychological safety and efficacy, finally leading to performance.
Limitations and Future Research
In this study, we suggest several limitations as follows. First, as Wang et al. (2018) pointed out, it is still difficult for researchers to infer causal relationships when there is a possible underlying bias from research methodology. In any survey method, some form of bias may be present that leads to the overestimation or underestimation of coefficients or relations ( Bido et al., 2017 ). We collected data from multiple sources based on a single survey followed by a statistical procedure to test the CMB issue. We recommend future researchers of human behavior in business to consider the ex ante approach (i.e., the time difference in data collection) so that they can minimize the bias.
Second, longitudinal data collection would provide a stronger theoretical foundation than cross-sectional data. The mediation effect explained by cross-sectional data might not be fully adequate to reveal the hidden structural relationships ( Maxwell et al., 2011 ). Replication of this study based on longitudinal data collection would also be an option for future researchers, re-simulating the findings of the study.
Third, researchers can consider a new line of methodologies and other mediation variables. As Newman et al. (2017) suggested, a qualitative research approach would provide a more holistic and more profound understanding of how psychological safety influences the outcome. With more observational techniques, researches can provide descriptions of a vibrant and dynamic process of a TEF creation. Several factors can influence TEF as a mediator or a moderator. Including little known factors in a research model would provide precious evidence about teams in an era of rapid change.
Data Availability Statement
Ethics statement.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
SK devised the research idea, developed the research model, and performed the analytic calculations for the manuscript. HL and TC contributed to the final version of the manuscript and supervised the research. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Questionnaire and descriptive statistics.
| Author | Questionnaire | Mean | SD | Skewness | Kurtosis |
| Members criticized when making a mistake* | 5.254 | 1.045 | 0.682 | 0.536 | |
| Can bring up work problems and awkward stories | |||||
| Members often ignore other people’s opinions* | |||||
| Able to take risks | |||||
| Cannot ask for help from other members* | |||||
| Members do not degrade my efforts | |||||
| My own skills and talents appreciated and utilized | |||||
| Actively propose new ideas for tasks | 4.932 | 1.321 | 0.500 | 0.087 | |
| Creating a new way of doing things. | |||||
| Ideas and practices often introduced to other teams | |||||
| Mutual communication | 5.535 | 1.272 | 1.072 | 0.977 | |
| Chance to express own opinions | |||||
| Exchange ideas with each other | |||||
| Documents the details of work | 4.533 | 1.409 | 0.246 | 0.415 | |
| Records good ideas | |||||
| Records or manages best practice | |||||
| Total | 5.000 | 1.205 | 0.593 | 0.236 | |
| Has above-average ability | 5.562 | 1.080 | 0.781 | 0.572 | |
| Members have the best work skills | |||||
| Some members can’t do their job properly* | |||||
| Excellent performance compared to other teams | |||||
| Can achieve more than the team’s goal | |||||
| Very efficient | |||||
| Fulfilling responsibilities given by the organization | 5.678 | 1.030 | 0.702 | 0.228 | |
| Achieving the level of task that we expect | |||||
| Meeting official performance requirements | |||||
| Doing a key role that can improve team’s evaluation |
- Abror A. (2017). The Relationship Between Psychological Safety, Self-Efficacy and Organisational Performance: A Case in Indonesian Companies. Doctoral dissertation, University of Hull, Kingston upon Hull. [ Google Scholar ]
- Allensworth E., Ponisciak S., Mazzeo C. (2009). The Schools Teachers Leave: Teacher Mobility in Chicago Public Schools. Available online at: https://eric.ed.gov/?id=ED505882 (accessed June 2009). [ Google Scholar ]
- Argote L., Gruenfeld D., Naquin C. (1999). “ Group learning in organizations ,” in Groups at Work: Advances in Theory and Research , ed. Turner M. E. (Mahwah, NJ: Erlbaum; ), 369–411. [ Google Scholar ]
- Argyris C. (1986). Reinforcing organizational defensive routines: an unintended human resources activity. Hum. Resour. Manage. 25 541–555. 10.1002/hrm.3930250405 [ CrossRef ] [ Google Scholar ]
- Baer M., Frese M. (2003). Innovation is not enough: climates for initiative and psychological safety, process innovations, and firm performance. J. Organ. Behav. 24 45–68. 10.1002/job.179 [ CrossRef ] [ Google Scholar ]
- Bagozzi R. P., Yi Y. (1988). On the evaluation of structural equation models. J. Acad. Mark. Sci. 16 74–94. 10.1007/bf02723327 [ CrossRef ] [ Google Scholar ]
- Bandura A. (1986). “ Social foundations of thought and action ,” in The Health Psychology Reader , ed. Marks D. F. (London, UK: Sage Publications; ), 94–106. 10.4135/9781446221129.n6 [ CrossRef ] [ Google Scholar ]
- Bandura A. (1988). Organisational applications of social cognitive theory. Austr. J. Manage. 13 275–302. 10.1177/031289628801300210 [ CrossRef ] [ Google Scholar ]
- Bandura A. (1997). Self-Efficacy: The Exercise of Control. New York, NY: W.H. Freeman & Company. [ Google Scholar ]
- Bandura A. (2000). Exercise of human agency through collective efficacy. Curr. Dir. Psychol. Sci. 9 75–78. 10.1111/1467-8721.00064 [ CrossRef ] [ Google Scholar ]
- Bido D. S., Mantovani D. M. N., Cohen E. D. (2017). Destruction of measurement scale through exploratory factor analysis in production and operations research. Gestão Produção 25 384–397. 10.1590/0104-530x3391-16 [ CrossRef ] [ Google Scholar ]
- Brown T. A. (2015). Confirmatory Factor Analysis for Applied Research , 2nd Edn New York, NY: Guilford Press. [ Google Scholar ]
- Brueller D., Carmeli A. (2011). Linking capacities of high-quality relationships to team learning and performance in service organizations. Hum. Resour. Manage. 50 455–477. 10.1002/hrm.20435 [ CrossRef ] [ Google Scholar ]
- Bryk A., Sebring P., Allensworth E., Luppescu S., Easton J. (2010). Organizing Schools for Improvement: Lessons from Chicago. Chicago, IL: University of Chicago Press. [ Google Scholar ]
- Bstieler L., Hemmert M. (2010). Increasing learning and time efficiency in interorganizational new product development teams. J. Prod. Innov. Manage. 27 485–499. 10.1111/j.1540-5885.2010.00731.x [ CrossRef ] [ Google Scholar ]
- Carmeli A. (2007). Social capital, psychological safety and learning behaviours from failure in organisations. Long Range Plann. 40 30–44. 10.1016/j.lrp.2006.12.002 [ CrossRef ] [ Google Scholar ]
- Carmeli A., Brueller D., Dutton J. E. (2009). Learning behaviours in the workplace: the role of high-quality interpersonal relationships and psychological safety. Syst. Res. Behav. Sci. 26 81–98. 10.1002/sres.932 [ CrossRef ] [ Google Scholar ]
- Carmeli A., Gittell J. H. (2009). High-quality relationships, psychological safety, and learning from failures in work organizations. J. Organ. Behav. 30 709–729. 10.1002/job.565 [ CrossRef ] [ Google Scholar ]
- Chen C., Liao J., Wen P. (2014). Why does formal mentoring matter? The mediating role of psychological safety and the moderating role of power distance orientation in the Chinese context. Int. J. Hum. Resour. Manage. 25 1112–1130. 10.1080/09585192.2013.816861 [ CrossRef ] [ Google Scholar ]
- Chen G., Kanfer R. (2006). Toward a systems theory of motivated behavior in work teams. Res. Organ. Behav. 27 223–267. 10.1016/S0191-3085(06)27006-0 [ CrossRef ] [ Google Scholar ]
- Chen G., Thomas B., Wallace J. C. (2005). A multilevel examination of the relationships among training outcomes, mediating regulatory processes, and adaptive performance. J. Appl. Psychol. 90 827–841. 10.1037/0021-9010.90.5.827 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Christian M. S., Garza A. S., Slaughter J. E. (2011). Work engagement: a quantitative review and test of its relations with task and contextual performance. Pers. Psychol. 64 89–136. 10.1111/j.1744-6570.2010.01203.x [ CrossRef ] [ Google Scholar ]
- Clark T. R. (2019). The 4 Stages of Psychological Safety. Available online at: http://adigaskell.org/2019/11/17/the-4-stages-of-psychological-safety/ (accessed November 17, 2019. [ Google Scholar ]
- Cohen S. G., Bailey D. E. (1997). What makes teams work: group effectiveness research from the shop floor to the executive suite. J. Manage. 23 239–290. 10.1177/014920639702300303 [ CrossRef ] [ Google Scholar ]
- Day C., Hopkins D., Harris A., Ahtaridou E. (2009). The Impact of School Leadership on Pupil Outcomes. Available online at: https://dera.ioe.ac.uk/11329/1/DCSF-RR108.pdf (accessed June 2009). [ Google Scholar ]
- De clercq D., Rius I. B. (2007). Organizational commitment in Mexican small and medium-sized firms: the role of work status, organizational climate, and entrepreneurial orientation. J. Small Bus. Manage. 45 467–490. 10.1111/j.1540-627X.2007.00223.x [ CrossRef ] [ Google Scholar ]
- Donaldson S. I., Csikszentmihalyi M., Nakamura J. (2011). Applied Positive Psychology: Improving Everyday Life, Health, Schools, Work, and Society. New York, NY: Routledge. [ Google Scholar ]
- Dulebohn J. H., Hoch J. E. (2017). Virtual teams in organizations. Hum. Resour. Manage. Rev. 27 569–574. 10.1016/j.hrmr.2016.12.004 [ CrossRef ] [ Google Scholar ]
- Dyer J. H., Nobeoka K. (2000). Creating and managing a high-performance knowledge-sharing network: the Toyota case. Strateg. Manage. J. 21 345–367. 10.1002/(sici)1097-0266(200003)21:3<345::aid-smj96<3.0.co;2-n [ CrossRef ] [ Google Scholar ]
- Edmondson A. C. (1999). Psychological safety and learning behavior in work teams. Adm. Sci. Q. 44 350–383. 10.2307/2666999 [ CrossRef ] [ Google Scholar ]
- Edmondson A. C. (2008). The competitive imperative of learning . Harv. Bus. Rev. 86 , 60–67. [ PubMed ] [ Google Scholar ]
- Edmondson A. C. (2012). Teaming: How Organizations Learn, Innovate, and Compete in the Knowledge Economy. Hoboken, NJ: John Wiley & Sons. [ Google Scholar ]
- Edmondson A. C. (2018). The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth. Hoboken, NJ: John Wiley & Sons. [ Google Scholar ]
- Edmondson A. C., Dillon J. R., Roloff K. S. (2007). Three perspectives on team learning. Acad. Manage. Ann. 1 269–314. 10.1080/078559811 [ CrossRef ] [ Google Scholar ]
- Edmondson A. C., Lei Z. (2014). Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu. Rev. Organ. Psychol. Organ. Behav. 1 23–43. 10.1146/annurev-orgpsych-031413-091305 [ CrossRef ] [ Google Scholar ]
- Escribano P., Dufour L., Maoret M. (2017). “ Will I socialize you? An IPO model of supervisors’ involvement in newcomers’ socialization ,” in Proceedings of the Academy of Management Annual Meeting , At Atlanta, GA: 10.5465/AMBPP.2017.251 [ CrossRef ] [ Google Scholar ]
- Fabrigar L. R., Wegener D. T. (2012). Exploratory Factor Analysis. New York, NY: Oxford University Press. [ Google Scholar ]
- Fornell C., Larcker D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 18 39–50. 10.1177/002224378101800104 [ CrossRef ] [ Google Scholar ]
- Frazier M. L., Fainshmidt S., Klinger R. L., Pezeshkan A., Vracheva V. (2017). Psychological safety: a meta-analytic review and extension. Pers. Psychol. 70 113–165. 10.1111/peps.12183 [ CrossRef ] [ Google Scholar ]
- Gibson C., Vermeulen F. (2003). A healthy divide: subgroups as a stimulus for team learning behavior. Adm. Sci. Q. 48 202–239. 10.2307/3556657 [ CrossRef ] [ Google Scholar ]
- Gibson C. B., Randel A. E., Earley P. C. (2000). Understanding group efficacy: an empirical test of multiple assessment methods. Group Organ. Manage. 25 67–97. 10.1177/1059601100251005 [ CrossRef ] [ Google Scholar ]
- Gladstein D. L. (1984). Groups in context: a model of task group effectiveness. Adm. Sci. Q. 29 499–517. 10.2307/2392936 [ CrossRef ] [ Google Scholar ]
- Glassop L. I. (2002). The organizational benefits of teams. Hum. Relat. 55 225–249. 10.1177/0018726702055002184 [ CrossRef ] [ Google Scholar ]
- Gong Z., Li T. (2019). Relationship between feedback environment established by mentor and nurses’ career adaptability: a cross-sectional study. J. Nurs. Manage. 27 1568–1575. 10.1111/jonm.12847 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Google (2015). Five Keys to A Successful Google Team. Available online at: https://rework.withgoogle.com/blog/five-keys-to-a-successful-google-team (accessed November 17, 2015). [ Google Scholar ]
- Guide V. D. R., Ketokivi M. (2015). Notes from the editors: redefining some methodological criteria for the journal. J. Operat. Manage. 37 5–8. 10.1016/S0272-6963(15)00056-X [ CrossRef ] [ Google Scholar ]
- Gully S. M., Incalcaterra K. A., Joshi A., Beaubien J. M. (2002). A meta-analysis of team-efficacy, potency, and performance: interdependence and level of analysis as moderators of observed relationships. J. Appl. Psychol. 87 819–832. 10.1037/0021-9010.87.5.819 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hackman J. R. (1987). “ The design of work teams ,” in Handbook of Organizational Behavior , ed. Lorsch J. (New York, NY: Prentice Hall; ), 315–342. [ Google Scholar ]
- Hair J. F., Hult G. T. M., Ringle C. M., Sarstedt M. (2017). A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM) , 2nd Edn Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Harman D. (1967). A single factor test of common method variance. J. Psychol. 35 359–378. [ Google Scholar ]
- Hayes A. F. (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press. [ Google Scholar ]
- Hernandez M., Guarana C. L. (2018). An examination of the temporal intricacies of job engagement. J. Manage. 44 1711–1735. 10.1177/0149206315622573 [ CrossRef ] [ Google Scholar ]
- Hirak R., Peng A. C., Carmeli A., Schaubroeck J. M. (2012). Linking leader inclusiveness to work unit performance: the importance of psychological safety and learning from failures. Leadersh. Q. 23 107–117. 10.1016/j.leaqua.2011.11.009 [ CrossRef ] [ Google Scholar ]
- Huang C.-C., Jiang P.-C. (2012). Exploring the psychological safety of R&D teams: an empirical analysis in Taiwan. J. Manage. Organ. 18 175–192. 10.1017/S1833367200000948 [ CrossRef ] [ Google Scholar ]
- Ipsos (2012). Half (47%) of Global Employees Agree Their Workplace is Psychologically Safe and Healthy: Three in Ten (27%) Say Not. Available online at: https://www.ipsos.com/en-us/half-47-global-employees-agree-their-workplace-psychologically-safe-and-healthy-three-ten-27-say (accessed March 14, 2012). [ Google Scholar ]
- James L. R. (1982). Aggregation bias in estimates of perceptual agreement . J. Appl. Psychol. 67 , 219–229. 10.1037/0021-9010.67.2.219 [ CrossRef ] [ Google Scholar ]
- James L. R., Demaree R. G., Wolf G. (1993). rwg: An assessment of within-group interrater agreement. J. Appl. Psychol. 78 306–309. 10.1037/0021-9010.78.2.306 [ CrossRef ] [ Google Scholar ]
- Johnson S. M., Kraft M. A., Papay J. P. (2012). How context matters in high-need schools: the effects of teachers’ working conditions on their professional satisfaction and their students’ achievement. Teach. Coll. Rec. 114 1–39. [ Google Scholar ]
- Kahn W. A. (1990). Psychological conditions of personal engagement and disengagement at work. Acad. Manage. J. 33 692–724. 10.5465/256287 [ CrossRef ] [ Google Scholar ]
- Kessel M., Kratzer J., Schultz C. (2012). Psychological safety, knowledge sharing, and creative performance in healthcare teams. Creat. Innovat. Manage. 21 147–157. 10.1111/j.1467-8691.2012.00635.x [ CrossRef ] [ Google Scholar ]
- Klein K. J., Dansereau F., Hall R. J. (1994). Levels issues in theory development, data collection, and analysis. Acad. Manage. Rev. 19 195–229. 10.5465/amr.1994.9410210745 [ CrossRef ] [ Google Scholar ]
- Klein K. J., Kozlowski S. W. (2000). From micro to meso: critical steps in conceptualizing and conducting multilevel research. Organ. Res. Methods 3 211–236. 10.1177/109442810033001 [ CrossRef ] [ Google Scholar ]
- Knapp R. J. (2016). The Effects of Psychological Safety, Team Efficacy, and Transactive Memory System Development on Team Learning Behavior in Virtual Work Teams. Doctoral dissertation, University of Minnesota, Minneapolis, MN. [ Google Scholar ]
- Kostopoulos K. C., Bozionelos N. (2011). Team exploratory and exploitative learning: psychological safety, task conflict, and team performance. Group Organ. Manage. 36 385–415. 10.1177/1059601111405985 [ CrossRef ] [ Google Scholar ]
- Kozlowski S. W. J., Bell B. S. (2003). “ Work groups and teams in organizations ,” in Handbook of Psychology: Industrial and Organizational Psychology , Vol. 12 eds Borman W. C., Ilgen D. R., Klimoski R. J. (Hoboken, NJ: John Wiley & Sons Inc; ), 333–375. [ Google Scholar ]
- Li A. N., Tan H. H. (2013). What happens when you trust your supervisor? Mediators of individual performance in trust relationships. J. Organ. Behav. 34 407–425. 10.1002/job.1812 [ CrossRef ] [ Google Scholar ]
- Li N., Yan J. (2009). The effects of trust climate on individual performance. Front. Bus. Res. China 3 :27–49. 10.1007/s11782-009-0002-6 [ CrossRef ] [ Google Scholar ]
- Lin Z., Yang H., Arya B., Huang Z., Li D. (2005). Structural versus individual perspectives on the dynamics of group performance: theoretical exploration and empirical investigation. J. Manage. 31 354–380. 10.1177/0149206304272150 [ CrossRef ] [ Google Scholar ]
- Liu S., Hu J., Li Y., Wang Z., Lin X. (2014). Examining the cross-level relationship between shared leadership and learning in teams: evidence from China. Leadersh. Q. 25 282–295. 10.1016/j.leaqua.2013.08.006 [ CrossRef ] [ Google Scholar ]
- Liu Y., Yan X., Sun Y. (2010). “ A meta-analysis of virtual team communication based on IPO model ,” in Proceedings of the 1st International Conference on E-Business Intelligence (ICEBI2010) , Kunming, 10.2991/icebi.2010.3 [ CrossRef ] [ Google Scholar ]
- Luszczynska A., Schwarzer R. (2005). “ Social cognitive theory ,” in Predicting Health Behaviour , eds Connor M., Norman P. (New York: NY: Open University Press; ), 127–169. [ Google Scholar ]
- Madjar N., Ortiz-Walters R. (2009). Trust in supervisors and trust in customers: their independent, relative, and joint effects on employee performance and creativity . Hum. Perform. 22 , 128–142. 10.1080/08959280902743501 [ CrossRef ] [ Google Scholar ]
- Mansikka H., Harris D., Virtanen K. (2017). An input-process-output model of pilot core competencies. Aviat. Psychol. Appl. Hum. Fact. 7 78–85. 10.1027/2192-0923/a000120 [ CrossRef ] [ Google Scholar ]
- Mathieu J., Maynard M. T., Rapp T., Gilson L. (2008). Team effectiveness 1997-2007: a review of recent advancements and a glimpse into the future. J. Manage. 34 410–476. 10.1177/0149206308316061 [ CrossRef ] [ Google Scholar ]
- Maxwell S. E., Cole D. A., Mitchell M. A. (2011). Bias in cross-sectional analyses of longitudinal mediation: partial and complete mediation under an autoregressive model. Multivariate Behav. Res. 46 816–841. 10.1080/00273171.2011.606716 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- May D. R., Gilson R. L., Harter L. M. (2004). The psychological conditions of meaningfulness, safety and availability and the engagement of the human spirit at work. J. Occup. Organ. Psychol. 77 11–37. 10.1348/096317904322915892 [ CrossRef ] [ Google Scholar ]
- Murphy K. R., Davidshofer C. O. (1988). Psychological Testing: Principles, and Applications. Englewood Cliffs, NJ: Prentice-Hall. [ Google Scholar ]
- Newman A., Donohue R., Eva N. (2017). Psychological safety: a systematic review of the literature. Hum. Resour. Manage. Rev. 27 521–535. 10.1016/j.hrmr.2017.01.001 [ CrossRef ] [ Google Scholar ]
- Ortega A., Sánchez-Manzanares M., Gil F., Rico R. (2010). Team learning and effectiveness in virtual project teams: the role of beliefs about interpersonal context. Span. J. Psychol. 13 267–276. 10.1017/s113874160000384x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ortega A., Van den Bossche P., Sánchez-Manzanares M., Rico R., Gil F. (2014). The influence of change-oriented leadership and psychological safety on team learning in healthcare teams. J. Bus. Psychol. 29 311–321. 10.1007/s10869-013-9315-8 [ CrossRef ] [ Google Scholar ]
- Pearce C. L., Herbik P. A. (2004). Citizenship behavior at the team level of analysis: the effects of team leadership, team commitment, perceived team support, and team size. J. Soc. Psychol. 144 293–310. 10.3200/SOCP.144.3.293-310 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pearce C. L., Sims H. P., Jr. (2002). Vertical versus shared leadership as predictors of the effectiveness of change management teams: an examination of aversive, directive, transactional, transformational, and empowering leader behaviors. Group Dyn. Theor. Res. Pract. 6 172–197. 10.1037/1089-2699.6.2.172 [ CrossRef ] [ Google Scholar ]
- Pearsall M. J., Ellis A. P. (2011). Thick as thieves: the effects of ethical orientation and psychological safety on unethical team behavior. J. Appl. Psychol. 96 401–411. 10.1037/a0021503 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Porter C. O. L. H., Itir Gogus C., Yu R. C.-F. (2011). Does backing up behavior explain the efficacy–performance relationship in teams? Small Group Res. 42 458–474. 10.1177/1046496410390964 [ CrossRef ] [ Google Scholar ]
- Preacher K. J., Rucker D. D., Hayes A. F. (2007). Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivariate Behav. Res. 42 185–227. 10.1080/00273170701341316 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rich B. L., Lepine J. A., Crawford E. R. (2010). Job engagement: antecedents and effects on job performance. Acad. Manage. J. 53 617–635. 10.5465/AMJ.2010.51468988 [ CrossRef ] [ Google Scholar ]
- Rico R., de la Hera C. M. A., Tabernero C. (2011). Work team effectiveness, a review of research from the last decade (1999-2009). Psychol. Spain 15 57–79. [ Google Scholar ]
- Riggs M. L., Knight P. A. (1994). The impact of perceived group success-failure on motivational beliefs and attitudes: a causal model. J. Appl. Psychol. 79 755–766. 10.1037/0021-9010.79.5.755 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberto M. A. (2002). Lessons from Everest: the interaction of cognitive bias, psychological safety, and system complexity. Calif. Manage. Rev. 45 136–158. 10.2307/41166157 [ CrossRef ] [ Google Scholar ]
- Ronfeldt M., Loeb S., Wyckoff J. (2013). How teacher turnover harms student achievement. Am. Educ. Res. J. 50 4–36. 10.3102/0002831212463813 [ CrossRef ] [ Google Scholar ]
- Rousseau V., Aubé C., Savoie A. (2006). Teamwork behaviors: a review and an integration of frameworks. Small Group Res. 37 540–570. 10.1177/1046496406293125 [ CrossRef ] [ Google Scholar ]
- Roussin C. J., MacLean T. L., Rudolph J. W. (2016). The safety in unsafe teams: a multilevel approach to team psychological safety. J. Manage. 42 1409–1433. 10.1177/0149206314525204 [ CrossRef ] [ Google Scholar ]
- Sanner B., Bunderson J. S. (2013). Psychological safety, learning, and performance: a comparison of direct and contingent effects. Acad. Manage. Proc. 2013 : 10198 10.5465/ambpp.2013.10198abstract [ CrossRef ] [ Google Scholar ]
- Schaubroeck J., Lam S. S. K., Peng A. C. (2011). Cognition-based and affect-based trust as mediators of leader behavior influences on team performance. J. Appl. Psychol. 96 863–871. 10.1037/a0022625 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schein E. H., Bennis W. G. (1965). Personal and Organizational Change Through Group Methods: The Laboratory Approach. New York, NY: Wiley. [ Google Scholar ]
- Shen M. J., Chen M. C. (2007). The relationship of leadership, team trust and team performance: a comparison of the service and manufacturing industries. Soc. Behav. Pers. 35 643–658. 10.2224/sbp.2007.35.5.643 [ CrossRef ] [ Google Scholar ]
- Singh B., Winkel D. E., Selvarajan T. T. (2013). Managing diversity at work: does psychological safety hold the key to racial differences in employee performance? J. Occup. Organ. Psychol. 86 242–263. 10.1111/joop.12015 [ CrossRef ] [ Google Scholar ]
- Stalmeijer R. E., Gijselaers W. H., Wolfhagen I. H., Harendza S., Scherpbier A. J. (2007). How interdisciplinary teams can create multi-disciplinary education: the interplay between team processes and educational quality. Med. Educ. 41 1059–1066. 10.1111/j.1365-2923.2007.02898.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tasa K., Taggar S., Seijts G. H. (2007). The development of collective efficacy in teams: a multilevel and longitudinal perspective. J. Appl. Psychol. 92 17–27. 10.1037/0021-9010.92.1.17 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van den Bossche P., Gijselaers W. H., Segers M., Kirschner P. A. (2006). Social and cognitive factors driving teamwork in collaborative learning environments: team learning beliefs and behaviors. Small Group Res. 37 490–521. 10.1177/1046496406292938 [ CrossRef ] [ Google Scholar ]
- van Emmerik H., Jawahar I. M., Schreurs B., De Cuyper N. (2011). Social capital, team efficacy and team potency: the mediating role of team learning behaviors. Career Dev. Int. 16 82–99. 10.1108/13620431111107829 [ CrossRef ] [ Google Scholar ]
- van Offenbeek M. (2001). Processes and outcomes of team learning. Eur. J. Work Organ. Psychol. 10 303–317. 10.1080/13594320143000690 [ CrossRef ] [ Google Scholar ]
- Walumbwa F. O., Wang P., Lawler J. J., Shi K. (2004). The role of collective efficacy in the relations between transformational leadership and work outcomes. J. Occup. Organ. Psychol. 77 515–530. 10.1348/0963179042596441 [ CrossRef ] [ Google Scholar ]
- Wang Y., Liu J., Zhu Y. (2018). Humble leadership, psychological safety, knowledge sharing, and follower creativity: a cross-level investigation. Front. Psychol. 9 : 1727 . 10.3389/fpsyg.2018.01727 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Werner J. M., Lester S. W. (2001). Applying a team effectiveness framework to the performance of student case teams. Hum. Resour. Dev. Q. 12 385–402. 10.1002/hrdq.1004 [ CrossRef ] [ Google Scholar ]
- West B. J., Patera J. L., Carsten M. K. (2009). Team level positivity: investigating positive psychological capacities and team level outcomes. J. Organ. Behav. 30 249–267. 10.1002/job.593 [ CrossRef ] [ Google Scholar ]
- Williams L. J., Anderson S. E. (1991). Job satisfaction and organizational commitment as predictors of organizational citizenship and in-role behaviors. J. Manage. 17 601–617. 10.1177/014920639101700305 [ CrossRef ] [ Google Scholar ]
- Wong A., Tjosvold D., Lu J. (2010). Leadership values and learning in China: the mediating role of psychological safety. Asia Pac. J. Hum. Resour. 48 86–107. 10.1177/1038411109355374 [ CrossRef ] [ Google Scholar ]
- Zellmer-Bruhn M., Gibson C. (2006). Multinational organization context: implications for team learning and performance. Acad. Manage. J. 49 501–518. 10.5465/amj.2006.21794668 [ CrossRef ] [ Google Scholar ]
- Zoogah D. B., Noe R. A., Shenkar O. (2015). Shared mental model, team communication and collective self-efficacy: an investigation of strategic alliance team effectiveness. Int. J. Strateg. Bus. Alliances 4 244–270. 10.1504/IJSBA.2015.075383 [ CrossRef ] [ Google Scholar ]
- A-Z Publications
Annual Review of Organizational Psychology and Organizational Behavior
Volume 10, 2023, review article, open access, psychological safety comes of age: observed themes in an established literature.
- Amy C. Edmondson 1 , and Derrick P. Bransby 1
- View Affiliations Hide Affiliations Affiliations: Harvard Business School, Harvard University, Boston, Massachusetts, USA; email: [email protected] [email protected]
- Vol. 10:55-78 (Volume publication date January 2023) https://doi.org/10.1146/annurev-orgpsych-120920-055217
- First published as a Review in Advance on November 14, 2022
- Copyright © 2023 by the author(s). This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. See credit lines of images or other third-party material in this article for license information
Since its renaissance in the 1990s, psychological safety research has flourished—a boom motivated by recognition of the challenge of navigating uncertainty and change. Today, its theoretical and practical significance is amplified by the increasingly complex and interdependent nature of the work in organizations. Conceptual and empirical research on psychological safety—a state of reduced interpersonal risk—is thus timely, relevant, and extensive. In this article, we review contemporary psychological safety research by describing its various content areas, assessing what has been learned in recent years, and suggesting directions for future research. We identify four dominant themes relating to psychological safety: getting things done, learning behaviors, improving the work experience, and leadership. Overall, psychological safety plays important roles in enabling organizations to learn and perform in dynamic environments, becoming particularly relevant in a world altered by a global pandemic.
Article metrics loading...
Full text loading...
Literature Cited
- Agarwal P , Farndale E. 2017 . High-performance work systems and creativity implementation: the role of psychological capital and psychological safety. Hum. Resour. Manag. J. 27 : 3 440 – 58 [Google Scholar]
- Ahmad I , Umrani WA 2019 . The impact of ethical leadership style on job satisfaction: mediating role of perception of Green HRM and psychological safety. Leadersh. Organ. Dev. J. 40 : 5 534 – 47 [Google Scholar]
- Ahmed F , Zhao F , Faraz NA , Qin YJ. 2021 . How inclusive leadership paves way for psychological well-being of employees during trauma and crisis: a three-wave longitudinal mediation study. J. Adv. Nurs. 77 : 2 819 – 31 [Google Scholar]
- Andersson M , Moen O , Brett PO. 2020 . The organizational climate for psychological safety: associations with SMEs’ innovation capabilities and innovation performance. J. Eng. Technol. Manag. 55 : 101554 [Google Scholar]
- Appelbaum NP , Dow A , Mazmanian PE , Jundt DK , Appelbaum EN. 2016 . The effects of power, leadership and psychological safety on resident event reporting. Med. Educ. 50 : 3 343 – 50 [Google Scholar]
- Arnetz JE , Sudan S , Fitzpatrick L , Cotten SR , Jodoin C et al. 2019 . Organizational determinants of bullying and work disengagement among hospital nurses. J. Adv. Nurs. 75 : 6 1229 – 38 [Google Scholar]
- Baer M , Frese M. 2003 . Innovation is not enough: climates for initiative and psychological safety, process innovations, and firm performance. J. Organ. Behav. 24 : 1 45 – 68 [Google Scholar]
- Baik D , Zierler B. 2019 . Clinical nurses’ experiences and perceptions after the implementation of an interprofessional team intervention: a qualitative study. J. Clin. Nurs. 28 : 3–4 430 – 43 [Google Scholar]
- Bani-Melhem S , Shamsudin FM , Abukhait RM , Quratulain S. 2021 . Paranoid personality and frontline employee's proactive work behaviours: a moderated mediation model of empathetic leadership and perceived psychological safety. J. Serv. Theory Pract. 31 : 1 113 – 35 [Google Scholar]
- Basit AA. 2017 . Trust in supervisor and job engagement: mediating effects of psychological safety and felt obligation. J. Psychol. 151 : 8 701 – 21 [Google Scholar]
- Bienefeld N , Grote G. 2014 . Speaking up in ad hoc multiteam systems: individual-level effects of psychological safety, status, and leadership within and across teams. Eur. J. Work Organ. Psychol. 23 : 6 930 – 45 [Google Scholar]
- Binyamin G , Friedman A , Carmeli A. 2018 . Reciprocal care in hierarchical exchange: implications for psychological safety and innovative behaviors at work. Psychol. Aesthet. Creat. Arts 12 : 1 79 – 88 [Google Scholar]
- Bresman H , Zellmer-Bruhn M. 2013 . The structural context of team learning: effects of organizational and team structure on internal and external learning. Organ. Sci. 24 : 4 1120 – 39 [Google Scholar]
- Brinsfield CT. 2013 . Employee silence motives: investigation of dimensionality and development of measures. J. Organ. Behav. 34 : 5 671 – 97 [Google Scholar]
- Cajiao J , Burke MJ. 2016 . How instructional methods influence skill development in management education. Acad. Manag. Learn. Educ. 15 : 3 508 – 24 [Google Scholar]
- Carmeli A , Reiter-Palmon R , Ziv E. 2010 . Inclusive leadership and employee involvement in creative tasks in the workplace: the mediating role of psychological safety. Creat. Res. J. 22 : 3 250 – 60 [Google Scholar]
- Carmeli A , Sheaffer Z , Binyamin G , Reiter-Palmon R , Shimoni T. 2014 . Transformational leadership and creative problem-solving: the mediating role of psychological safety and reflexivity. J. Creat. Behav. 48 : 2 115 – 35 [Google Scholar]
- Castro DR , Anseel F , Kluger AN , Lloyd KJ , Turjeman-Levi Y. 2018 . Mere listening effect on creativity and the mediating role of psychological safety. Psychol. Aesthet. Creat. Arts. 12 : 4 489 – 502 [Google Scholar]
- Cauwelier P , Ribiere VM , Bennet A 2019 . The influence of team psychological safety on team knowledge creation: a study with French and American engineering teams. J. Knowl. Manag. 23 : 6 1157 – 75 [Google Scholar]
- Chen C , Liao J , Wen P. 2014 . Why does formal mentoring matter? The mediating role of psychological safety and the moderating role of power distance orientation in the Chinese context. Int. J. Hum. Resour. Manag. 25 : 8 1112 – 30 [Google Scholar]
- Chen L , Wadei KA , Bai S , Liu J. 2020 . Participative leadership and employee creativity: a sequential mediation model of psychological safety and creative process engagement. Leadersh. Organ. Dev. J. 41 : 6 741 – 59 [Google Scholar]
- Chen S , Wang D , Zhou Y , Chen Z , Wu D. 2017 . When too little or too much hurts: evidence for a curvilinear relationship between team faultlines and performance. Asia Pac. J. Manag. 34 : 4 931 – 50 [Google Scholar]
- Chughtai AA. 2016 . Servant leadership and follower outcomes: mediating effects of organizational identification and psychological safety. J. Psychol. 150 : 7 866 – 80 [Google Scholar]
- Coutifaris CGV , Grant AM. 2021 . Taking your team behind the curtain: the effects of leader feedback-sharing and feedback-seeking on team psychological safety. Organ. Sci. 33 : 4 1574 – 98 [Google Scholar]
- Creon LE , Schermuly CC. 2019 . Training group diversity and training transfer: a psychological safety perspective. Hum. Resour. Dev. Q. 30 : 4 583 – 603 [Google Scholar]
- De Hoogh AHB , Greer LL , Den Hartog DN. 2015 . Diabolical dictators or capable commanders? An investigation of the differential effects of autocratic leadership on team performance. Leadersh. Q. 26 : 5 687 – 701 [Google Scholar]
- De Stobbeleir K , Ashford S , Zhang C. 2020 . Shifting focus: antecedents and outcomes of proactive feedback seeking from peers. Hum. Relat. 73 : 3 303 – 25 [Google Scholar]
- Deng H , Leung K , Lam CK , Huang X. 2019 . Slacking off in comfort: a dual-pathway model for psychological safety climate. J. Manag. 45 : 3 1114 – 44 [Google Scholar]
- Edmondson AC. 1999 . Psychological safety and learning behavior in work teams. Adm. Sci. Q. 44 : 2 350 – 83 [Google Scholar]
- Edmondson AC 2003 . Managing the risk of learning: psychological safety in work teams. International Handbook of Organizational Teamwork and Cooperative Working MA West 255 – 76 . London: Blackwell [Google Scholar]
- Edmondson AC. 2019 . The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth Hoboken, NJ: Wiley [Google Scholar]
- Edmondson AC , Lei Z. 2014 . Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu. Rev. Organ. Psychol. Organ. Behav. 1 : 23 – 43 [Google Scholar]
- Edmondson AC , McManus SE. 2007 . Methodological fit in management field research. Acad. Manag. Rev. 32 : 4 1246 – 64 [Google Scholar]
- Edwards ST , Marino M , Solberg LI , Damschroder L , Stange KC et al. 2021 . Cultural and structural features of zero-burnout primary care practices. Health Aff. 40 : 6 928 – 29 [Google Scholar]
- Erkutlu H , Chafra J. 2016 . Benevolent leadership and psychological well-being: the moderating effects of psychological safety and psychological contract breach. Leadersh. Organ. Dev. J. 37 : 3 369 – 86 [Google Scholar]
- Espedido A , Searle BJ. 2021 . Proactivity, stress appraisals, and problem-solving: a cross-level moderated mediation model. Work Stress 35 : 2 132 – 52 [Google Scholar]
- Fleştea AM , Curşeu PL , Fodor OC. 2017 . The bittersweet effect of power disparity. J. Manag. Psychol. 32 : 5 401 – 16 [Google Scholar]
- Frazier LM , Tupper C. 2018 . Supervisor prosocial motivation, employee thriving, and helping behavior: a trickle-down model of psychological safety. Group Organ. Manag. 43 : 4 561 – 93 [Google Scholar]
- Frazier ML , Fainshmidt S , Klinger RL , Pezeshkan A , Vracheva V. 2017 . Psychological safety: a meta-analytic review and extension. Pers. Psychol. 70 : 1 113 – 65 [Google Scholar]
- Gerpott FH , Lehmann-Willenbrock N , Wenzel R , Voelpel SC. 2019 . Age diversity and learning outcomes in organizational training groups: the role of knowledge sharing and psychological safety. Int. J. Hum. Resour. Manag. 32 : 18 3777 – 3804 [Google Scholar]
- Gonzalez K , Tillman CJ , Holmes JJ. 2020 . Coming home: why veterans with disabilities withhold workplace accommodation requests. Hum. Relat. 73 : 10 1439 – 66 [Google Scholar]
- Grant AM , Berg JM , Cable DM. 2014 . Job titles as identity badges: how self-reflective titles can reduce emotional exhaustion. Acad. Manag. J. 57 : 4 1201 – 25 [Google Scholar]
- Greenbaum RL , Bonner JM , Mawritz MB , Butts MM , Smith MB. 2020 . It is all about the bottom line: group bottom-line mentality, psychological safety, and group creativity. J. Organ. Behav. 41 : 6 503 – 17 [Google Scholar]
- Gu Q , Wang GG , Wang L. 2013 . Social capital and innovation in R&D teams: the mediating roles of psychological safety and learning from mistakes. R&D Manag . 43 : 2 89 – 102 [Google Scholar]
- Guchait P , Madera J , Dawson M. 2016 . Learning in the service environment: the influence of diversity climate. J. Serv. Theory Pract. 26 : 4 448 – 70 [Google Scholar]
- Han Y , Hao P , Yang B , Liu W. 2017 . How leaders’ transparent behavior influences employee creativity: the mediating roles of psychological safety and ability to focus attention. J. Leadersh. Organ. Stud. 24 : 3 335 – 44 [Google Scholar]
- Harms R. 2015 . Self-regulated learning, team learning and project performance in entrepreneurship education: learning in a lean startup environment. Technol. Forecast. Soc. Change 100 : 21 – 28 [Google Scholar]
- Harvey J-F , Johnson KJ , Roloff KS , Edmondson AC. 2019 . From orientation to behavior: the interplay between learning orientation, open-mindedness, and psychological safety in team learning. Hum. Relat. 72 : 11 1726 – 51 [Google Scholar]
- Hassan S , Jiang Z. 2021 . Facilitating learning to improve performance of law enforcement workgroups: the role of inclusive leadership behavior. Int. Public Manag. J. 24 : 1 106 – 30 [Google Scholar]
- He AS , Lizano EL , Stahlschmidt MJ. 2021 . When doing the right thing feels wrong: moral distress among child welfare caseworkers. Child. Youth Serv. Rev. 122 : 105914 [Google Scholar]
- Heath C , Sitkin SB. 2001 . Big-B versus Big-O: What is organizational about organizational behavior?. J. Organ. Behav. 22 : 43 – 58 [Google Scholar]
- Hood AC , Bachrach DG , Zivnuska S , Bendoly E. 2016 . Mediating effects of psychological safety in the relationship between team affectivity and transactive memory systems. J. Organ. Behav. 37 : 3 416 – 35 [Google Scholar]
- Hora S , Lemoine GJ , Xu N , Shalley CE. 2021 . Unlocking and closing the gender gap in creative performance: a multilevel model. J. Organ. Behav. 42 : 3 297 – 312 [Google Scholar]
- Hu J , Erdogan B , Jiang K , Bauer TN , Liu S. 2018 . Leader humility and team creativity: the role of team information sharing, psychological safety, and power distance. J. Appl. Psychol. 103 : 3 313 – 23 [Google Scholar]
- Huang C-C , Chen P-K. 2018 . Exploring the antecedents and consequences of the transactive memory system: an empirical analysis. J. Knowl. Manag. 22 : 1 92 – 118 [Google Scholar]
- Iqbal A , Latif KF , Ahmad MS. 2020 . Servant leadership and employee innovative behaviour: exploring psychological pathways. Leadersh. Organ. Dev. J. 41 : 6 813 – 27 [Google Scholar]
- Jiang Z , Hu X , Wang Z , Jiang X 2019 . Knowledge hiding as a barrier to thriving: the mediating role of psychological safety and moderating role of organizational cynicism. J. Organ. Behav. 40 : 7 800 – 818 [Google Scholar]
- Johnson HH , Avolio BJ. 2019 . Team psychological safety and conflict trajectories’ effect on individual's team identification and satisfaction. Group Organ. Manag. 44 : 5 843 – 73 [Google Scholar]
- Kahn WA. 1990 . Psychological conditions of personal engagement and disengagement at work. Acad. Manag. J. 33 : 4 692 – 724 [Google Scholar]
- Kerrissey MJ , Satterstrom P , Edmondson AC. 2020 . Into the fray: adaptive approaches to studying novel teamwork forms. Organ. Psychol. Rev. 10 : 2 62 – 86 [Google Scholar]
- Kirkman BL , Cordery JL , Mathieu J , Rosen B , Kukenberger M. 2013 . Global organizational communities of practice: the effects of nationality diversity, psychological safety, and media richness on community performance. Hum. Relat. 66 : 3 333 – 62 [Google Scholar]
- Klingberg K , Gadelhak K , Jegerlehner SN , Brown AD , Exadaktylos AK , Srivastava DS. 2018 . Bad manners in the Emergency Department: incivility among doctors. PLOS ONE 13 : 3 e0194933 [Google Scholar]
- Kong F , Liu P , Weng J. 2020 . How and when group cohesion influences employee voice: a conservation of resources perspective. J. Manag. Psychol. 35 : 3 142 – 54 [Google Scholar]
- Koopmann J , Lanaj K , Wang M , Zhou L , Shi J. 2016 . Nonlinear effects of team tenure on team psychological safety climate and climate strength: implications for average team member performance. J. Appl. Psychol. 101 : 7 940 – 57 [Google Scholar]
- Li AN , Tan HH. 2013 . What happens when you trust your supervisor? Mediators of individual performance in trust relationships. J. Organ. Behav. 34 : 3 407 – 25 [Google Scholar]
- Li J , Wu L , Liu D , Kwan HK , Liu J. 2014 . Insiders maintain voice: a psychological safety model of organizational politics. Asia Pac. J. Manag. 31 : 3 853 – 74 [Google Scholar]
- Li Y , Li N , Guo J , Li J , Harris TB 2018 . A network view of advice-giving and individual creativity in teams: a brokerage-driven, socially perpetuated phenomenon. Acad. Manag. J. 61 : 6 2210 – 29 [Google Scholar]
- Liang J , Farh CIC , Farh J-L. 2012 . Psychological antecedents of promotive and prohibitive voice: a two-wave examination. Acad. Manag. J. 55 : 1 71 – 92 [Google Scholar]
- Lin W , Koopmann J , Wang M. 2020 . How does workplace helping behavior step up or slack off? integrating enrichment-based and depletion-based perspectives. J. Manag. 46 : 3 385 – 413 [Google Scholar]
- Liu S , Hu J , Li Y , Wang Z , Lin X 2014 . Examining the cross-level relationship between shared leadership and learning in teams: evidence from China. Leadersh. Q. 25 : 2 282 – 95 [Google Scholar]
- Liu S , Liao J , Wei H. 2015 . Authentic leadership and whistleblowing: mediating roles of psychological safety and personal identification. J. Bus. Ethics 131 : 1 107 – 19 [Google Scholar]
- Liu W , Song Z , Li X , Liao 2017 . Why and when leaders’ affective states influence employee upward voice. Acad. Manag. J. 60 : 1 238 – 63 [Google Scholar]
- Liu W , Tangirala S , Lam W , Chen Z , Jia RT , Huang X. 2015 . How and when peers’ positive mood influences employees’ voice. J. Appl. Psychol. 100 : 3 976 – 89 [Google Scholar]
- Liu Y , Keller RT. 2021 . How psychological safety impacts R&D project teams’ performance: In a psychologically safe workplace, R&D project teams perform better, more readily share knowledge and engage in organizational citizenship behavior, and are less likely to leave. Res. Technol. Manag. 64 : 2 39 – 45 [Google Scholar]
- Liu Y , Keller RT , Bartlett KR. 2021 . Initiative climate, psychological safety and knowledge sharing as predictors of team creativity: a multilevel study of research and development project teams. Creat. Innov. Manag. 30 : 3 498 – 510 [Google Scholar]
- Lyman B , Biddulph ME , Hopper VG , Brogan JL. 2020a . Nurses’ experiences of organisational learning: a qualitative descriptive study. J. Nurs. Manag. 28 : 6 1241 – 49 [Google Scholar]
- Lyman B , Gunn MM , Mendon CR. 2020b . New graduate registered nurses’ experiences with psychological safety. J. Nurs. Manag. 28 : 4 831 – 39 [Google Scholar]
- MacCurtain S , Murphy C , O'Sullivan M , MacMahon J , Turner T 2018 . To stand back or step in? Exploring the responses of employees who observe workplace bullying. Nurs. Inq. 25 : 1 e12207 [Google Scholar]
- Malhotra MK , Ahire S , Shang G. 2017 . Mitigating the impact of functional dominance in cross-functional process improvement teams. Decis. Sci. 48 : 1 39 – 70 [Google Scholar]
- Mao J , Chiang JT , Chen L , Wu Y , Wang J. 2019 . Feeling safe? A conservation of resources perspective examining the interactive effect of leader competence and leader self-serving behaviour on team performance. J. Occup. Organ. Psychol. 92 : 1 52 – 73 [Google Scholar]
- Martins LL , Schilpzand MC , Kirkman BL , Ivanaj S , Ivanaj V. 2013 . A contingency view of the effects of cognitive diversity on team performance: the moderating roles of team psychological safety and relationship conflict. Small Group Res . 44 : 2 96 – 126 [Google Scholar]
- Miao Q , Eva N , Newman A , Cooper B. 2019 . CEO entrepreneurial leadership and performance outcomes of top management teams in entrepreneurial ventures: the mediating effects of psychological safety. J. Small Bus. Manag. 57 : 3 1119 – 35 [Google Scholar]
- Moake TR , Nahyun O , Steele CR. 2019 . The importance of team psychological safety climate for enhancing younger team members’ innovation-related behaviors in South Korea. Int. J. Cross Cult. Manag. 19 : 3 353 – 68 [Google Scholar]
- Mura M , Lettieri E , Radaelli G , Spiller N. 2016 . Behavioural operations in healthcare: a knowledge sharing perspective. Int. J. Oper. Prod. Manag. 36 : 10 1222 – 46 [Google Scholar]
- Najafi-Tavani Z , Robson MJ , Zaefarian G , Andersson U , Yu C. 2018 . Building subsidiary local responsiveness: (When) does the directionality of intrafirm knowledge transfers matter?. J. World Bus. 53 : 4 475 – 92 [Google Scholar]
- Newman A , Donohue R , Eva N. 2017 . Psychological safety: a systematic review of the literature. Hum. Resour. Manag. Rev. 27 : 3 521 – 35 [Google Scholar]
- O'Donovan R , De Brún A , McAuliffe E. 2021 . Healthcare professionals experience of psychological safety, voice, and silence. Front. Psychol. 12 : 626689 [Google Scholar]
- O'Donovan R , McAuliffe E. 2020a . A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour. BMC Health Serv. Res. 20 : 101 [Google Scholar]
- O'Donovan R , McAuliffe E. 2020b . A systematic review of factors that enable psychological safety in healthcare teams. Int. J. Qual. Health Care. 32 : 4 240 – 50 [Google Scholar]
- Ortega A , Bossche P , Sánchez-Manzanares M , Rico R , Gil F 2014 . The influence of change-oriented leadership and psychological safety on team learning in healthcare teams. J. Bus. Psychol. 29 : 2 311 – 21 [Google Scholar]
- Pan Y , Shang Y , Malika R 2020 . Enhancing creativity in organizations: the role of the need for cognition. Manag. Decis. 59 : 9 2057 – 76 [Google Scholar]
- Peng J , Wang Z , Chen X 2019 . Does self-serving leadership hinder team creativity? A moderated dual-path model. J. Bus. Ethics. 159 : 2 419 – 33 [Google Scholar]
- Rabbanee FK , Haque MM , Banik S , Islam MM. 2019 . Managing engagement in an emerging economy service. J. Serv. Theory Pract. 29 : 5–6 610 – 38 [Google Scholar]
- Remtulla R , Hagana A , Houbby N , Ruparell K , Aojula N et al. 2021 . Exploring the barriers and facilitators of psychological safety in primary care teams: a qualitative study. BMC Health Serv. Res. 21 : 269 [Google Scholar]
- Rivera AE , Rodríguez-Aceves L , Mojarro-Duran BI. 2021 . Enabling knowledge sharing through psychological safety in inter-organisational arrangements. J. Knowl. Manag. 25 : 5 1170 – 93 [Google Scholar]
- Romney AC. 2020 . It's not just what you say, it's how you say it: How callings influence constructive voice delivery. Hum. Relat. 74 : 12 2021 – 50 [Google Scholar]
- Sanner B , Bunderson JS. 2015 . When feeling safe isn't enough: contextualizing models of safety and learning in teams. Organ. Psychol. Rev. 5 : 3 224 – 43 [Google Scholar]
- Schein EH. 1993 . How can organizations learn faster? The challenge of entering the green room. MIT Sloan Management Review Magazine Jan. 15. https://sloanreview.mit.edu/article/how-can-organizations-learn-faster-the-challenge-of-entering-the-green-room/ [Google Scholar]
- Schein EH , Bennis WG. 1965 . Personal and Organizational Change through Group Methods: The Laboratory Approach New York: Wiley [Google Scholar]
- Shea T , Cooper B , De Cieri H , Sheehan C , Donohue R , Lindsay S 2018 . Postincident support for healthcare workers experiencing occupational violence and aggression. J. Nurs. Scholarsh. 50 : 4 344 – 52 [Google Scholar]
- Sherf EN , Parke MR , Isaakyan S. 2021 . Distinguishing voice and silence at work: unique relationships with perceived impact, psychological safety, and burnout. Acad. Manag. J. 64 : 1 114 – 48 [Google Scholar]
- Singer SJ , Hayes JE , Gray GC , Kiang MV. 2015 . Making time for learning-oriented leadership in multidisciplinary hospital management groups. Health Care Manag. Rev. 40 : 4 300 – 12 [Google Scholar]
- Singh B , Winkel DE , Selvarajan TT. 2013 . Managing diversity at work: Does psychological safety hold the key to racial differences in employee performance?. J. Occup. Organ. Psychol. 86 : 2 242 – 63 [Google Scholar]
- Smith ME , Wells EE , Friese CR , Krein SL , Ghaferi AA. 2018 . Interpersonal and organizational dynamics are key drivers of failure to rescue. Health Aff. 37 : 11 1870 – 76 [Google Scholar]
- Spoelma TM , Ellis APJ. 2017 . Fuse or fracture? Threat as a moderator of the effects of diversity faultlines in teams. J. Appl. Psychol. 102 : 9 1344 – 59 [Google Scholar]
- Starzyk A , Sonnentag S. 2019 . When do low-initiative employees feel responsible for change and speak up to managers?. J. Vocat. Behav. 115 : 1033 – 42 [Google Scholar]
- Stühlinger M , Schmutz JB , Gudela G , Dunja N , Domenica F 2021 . To get vaccinated or not? Psychological safety as a catalyst for the alignment between individual beliefs and behavior. Group Organ. Manag. 46 : 1 38 – 69 [Google Scholar]
- Tangirala S , Kamdar D , Venkataramani V , Parke MR. 2013 . Doing right versus getting ahead: The effects of duty and achievement orientations on employees’ voice. J. Appl. Psychol. 98 : 6 1040 – 50 [Google Scholar]
- True G , Stewart GL , Lampman M , Pelak M , Solimeo SL. 2014 . Teamwork and delegation in medical homes: primary care staff perspectives in the Veterans Health Administration. J. Gen. Intern. Med. 29 : Suppl. 2 632 – 39 [Google Scholar]
- Tu Y , Lu X , Choi JN , Guo W. 2019 . Ethical leadership and team-level creativity: mediation of psychological safety climate and moderation of supervisor support for creativity. J. Bus. Ethics 159 : 2 551 – 65 [Google Scholar]
- Ulusoy N , Mölders C , Fischer S , Bayur H , Deveci S et al. 2016 . A matter of psychological safety: commitment and mental health in Turkish immigrant employees in Germany. J. Cross-Cult. Psychol. 47 : 4 626 – 45 [Google Scholar]
- Unler E , Caliskan S. 2019 . Individual and managerial predictors of the different forms of employee voice. J. Manag. Dev. 38 : 7 582 – 603 [Google Scholar]
- van den Berg J , Alblas A , Le Blanc P , Romme AGL 2022 . How structural empowerment boosts organizational resilience: a case study in the Dutch home care industry. Organ. Stud. 43 : 9 1425 – 51 [Google Scholar]
- Vogus TJ , Cull MJ , Hengelbrok NE , Modell SJ , Epstein RA. 2016 . Assessing safety culture in child welfare: evidence from Tennessee. Child. Youth Serv. Rev. 65 : 94 – 103 [Google Scholar]
- Wang X , Guchait P , Paşamehmetoğlu A. 2020 . Tolerating errors in hospitality organizations: relationships with learning behavior, error reporting and service recovery performance. Int. J. Contemp. Hosp. Manag. 32 : 8 2635 – 55 [Google Scholar]
- Wilhelm H , Richter AW , Semrau T. 2019 . Employee learning from failure: a team-as-resource perspective. Organ. Sci. 30 : 4 694 – 714 [Google Scholar]
- Yeo R , Marquardt M. 2015 . To share or not to share? Self-perception and knowledge-sharing intent. Knowl. Manag. Res. Pract. 13 : 3 311 – 28 [Google Scholar]
- Yoon J , Solomon GT. 2017 . A curvilinear relationship between entrepreneurial orientation and firm performance: the moderating role of employees’ psychological safety. Int. Entrep. Manag. J. 13 : 4 1139 – 56 [Google Scholar]
Data & Media loading...
- Article Type: Review Article
Most Read This Month
Most cited most cited rss feed, conservation of resources in the organizational context: the reality of resources and their consequences, self-determination theory in work organizations: the state of a science, burnout and work engagement: the jd–r approach, psychological safety: the history, renaissance, and future of an interpersonal construct, employee voice and silence, psychological capital: an evidence-based positive approach, how technology is changing work and organizations, research on workplace creativity: a review and redirection, the psychology of entrepreneurship, abusive supervision.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Psychological safety: A systematic review of the literature

2017, Human Resource Management Review
Related Papers
Rafael Ireneo
Psychological safety [PS] was introduced in the 90s, and is a term popularized by Harvard Business School professor Amy Edmonson in a study conducted among medical teams in hospitals. PS is an environment of being able to express one’s self without fear of negative consequences such as embarrassment, and ridicule on self image, status or even career (Kahn 1990 as cited in Edmonson 2003). PS enhances sense of self-worth because it overpowers feelings of rejection and negative impacts on self-image whenever self-expression is exercised in the workplace. PS increases morale and self-confidence of members of a team, without having to be personally close to one another. Subsequent researches concluded that greater trust and respect were developed among teams in workplaces of varied settings. This paper is a literature review on various studies and applications of psychological safety. Using literatures published in scholarly journals from 2009 to 2010, the review revealed that many indus...
Academy of Management Discoveries
jennie weiner
Journal of Applied Psychology
Kho Michael Christian Kosasih
Asia Pacific Journal of Human Resources
Gemma Hicks
Journal of Occupational and Organizational Psychology
Sharon Clarke
Safety Science
Libby Brook
Work & Stress
Maureen Dollard
Jan Visagie , Wilfred Ukpere
The aim of this article was to investigate the psychosocial risk environment influencing employee behaviour, and subsequently the trust relationship between employer and employee. The unique nature and commonness of negative acts, such as unsafe behaviour, human errors, poor performance and negligence (also referred to as unsafe practices) are explored in this article. Pertinent literatures were reviewed on the nature of negative acts or unsafe behaviour. The findings of this study were used to draw comparisons between unsafe behaviour/misconduct and accidents in the workplace and finally recommendations were made on how the problem can be addressed from a labour relations perspective. The results indicate that a relationship between unsafe practice/misconduct and occupational injuries and accidents exist, owing to system flaws, human error or psychosocial risk.
BMC Health Services Research
Simon Tulloch
Background Emergency medicine is a complex setting for healthcare delivery which relies on communication, negotiation, teamwork, trust, and shared dialog. The nature of the work comprises dealing with emotionally challenging situations and acting under uncertainty. For healthcare staff this poses the need to be adaptive and open to change. Psychological safety is an important component of productive teamwork and learning in such contexts. Edmondson’s model of team psychological safety highlights factors which contribute to the development of psychological safety for staff groups and the mediating role this has for team performance. Aim The aim of the study was explore the link between psychological safety and improvement work. The research question was: Do the aspects covered in the Edmondson model fully describe healthcare workers’ perceptions of psychological safety and are all aspects in the model needed to describe these perceptions during testing of new work procedures in an em...
2007 IEEE 8th Human Factors and Power Plants and HPRCT 13th Annual Meeting
Teemu Reiman
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Arnold Bakker
Papeles del Psicologo
Begoña Urien
The Journal of applied psychology
David Hofmann
Journal of Safety Research
Geoff Willis
Journal of Management Sciences
Shabana Gul
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

File(s) under permanent embargo
Psychological safety: a systematic review of the literature, publisher doi.
- https://doi.org/10.1016/j.hrmr.2017.01.001
Publication classification
Copyright notice, usage metrics.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
A systematic review of factors that enable psychological safety in healthcare teams
Affiliation.
- 1 School of Nursing, Midwifery & Health Systems, Health Sciences Centre, University College Dublin, Dublin 4, Ireland.
- PMID: 32232323
- DOI: 10.1093/intqhc/mzaa025
Purpose: The current systematic review will identify enablers of psychological safety within the literature in order to produce a comprehensive list of factors that enable psychological safety specific to healthcare teams.
Data sources: A keyword search strategy was developed and used to search the following electronic databases PsycINFO, ABI/INFORM, Academic search complete and PubMed and grey literature databases OpenGrey, OCLC WorldCAT and Espace.
Study selection: Peer-reviewed studies relevant to enablers of psychological safety in healthcare setting that were published between 1999 and 2019 were eligible for inclusion. Covidence, an online specialized systematic review website, was used to screen records. Data extraction, quality appraisal and narrative synthesis were conducted on identified papers.
Data extraction: Thirty-six relevant studies were identified for full review and data extraction. A data extraction template was developed and included sections for the study methodology and the specific enablers identified within each study.
Results of data synthesis: Identified studies were reviewed using a narrative synthesis. Within the 36 articles reviewed, 13 enablers from across organizational, team and individual levels were identified. These enablers were grouped according to five broader themes: priority for patient safety, improvement or learning orientation, support, familiarity with colleagues, status, hierarchy and inclusiveness and individual differences.
Conclusion: This systematic review of psychological safety literature identifies a list of enablers of psychological safety within healthcare teams. This list can be used as a first step in developing observational measures and interventions to improve psychological safety in healthcare teams.
Keywords: Enablers; Healthcare teams; Psychological safety.
© The Author(s) 2020. Published by Oxford University Press in association with the International Society for Quality in Health Care. All rights reserved. For permissions, please e-mail: [email protected].
PubMed Disclaimer
Similar articles
- A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour. O'Donovan R, McAuliffe E. O'Donovan R, et al. BMC Health Serv Res. 2020 Feb 10;20(1):101. doi: 10.1186/s12913-020-4931-2. BMC Health Serv Res. 2020. PMID: 32041595 Free PMC article.
- Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. Eddy K, Jordan Z, Stephenson M. Eddy K, et al. JBI Database System Rev Implement Rep. 2016 Apr;14(4):96-137. doi: 10.11124/JBISRIR-2016-1843. JBI Database System Rev Implement Rep. 2016. PMID: 27532314 Review.
- The measurement of collaboration within healthcare settings: a systematic review of measurement properties of instruments. Walters SJ, Stern C, Robertson-Malt S. Walters SJ, et al. JBI Database System Rev Implement Rep. 2016 Apr;14(4):138-97. doi: 10.11124/JBISRIR-2016-2159. JBI Database System Rev Implement Rep. 2016. PMID: 27532315 Review.
- Measuring psychological safety in healthcare teams: developing an observational measure to complement survey methods. O'Donovan R, Van Dun D, McAuliffe E. O'Donovan R, et al. BMC Med Res Methodol. 2020 Jul 29;20(1):203. doi: 10.1186/s12874-020-01066-z. BMC Med Res Methodol. 2020. PMID: 32727374 Free PMC article.
- Team interventions in acute hospital contexts: a systematic search of the literature using realist synthesis. Cunningham U, Ward ME, De Brún A, McAuliffe E. Cunningham U, et al. BMC Health Serv Res. 2018 Jul 11;18(1):536. doi: 10.1186/s12913-018-3331-3. BMC Health Serv Res. 2018. PMID: 29996820 Free PMC article. Review.
- Psychological safety in an ECMO retrieval team: a qualitative study to inform improvement. Passariello M, Tarrant C. Passariello M, et al. BMJ Open Qual. 2024 May 23;13(2):e002706. doi: 10.1136/bmjoq-2023-002706. BMJ Open Qual. 2024. PMID: 38782489 Free PMC article.
- Wellbeing Convene during COVID-19: A pilot intervention for improving wellbeing and social connectedness for staff, students, residents, and faculty. Shroff FM, Mehta DH. Shroff FM, et al. J Clin Transl Sci. 2023 Nov 8;7(1):e269. doi: 10.1017/cts.2023.677. eCollection 2023. J Clin Transl Sci. 2023. PMID: 38380389 Free PMC article.
- The anatomy of safe surgical teams: an interview-based qualitative study among members of surgical teams at tertiary referral hospitals in Norway. Vikan M, Deilkås EC, Valeberg BT, Bjørnnes AK, Husby VS, Haugen AS, Danielsen SO. Vikan M, et al. Patient Saf Surg. 2024 Feb 19;18(1):7. doi: 10.1186/s13037-024-00389-w. Patient Saf Surg. 2024. PMID: 38374077 Free PMC article.
- Should the existing science of teams be applied to fluid teams? An exploration of fluid team effectiveness within the context of healthcare simulation. Grossman R, Billotti BM, Ha JJ, Cassara M. Grossman R, et al. Front Psychol. 2024 Feb 1;15:1323469. doi: 10.3389/fpsyg.2024.1323469. eCollection 2024. Front Psychol. 2024. PMID: 38362245 Free PMC article.
- Identifying and developing strategies for implementation of a guided internet- and mobile-based infant sleep intervention in well-baby and community mental health clinics using group concept mapping. Drozd F, Pettersen Sandtrø H, Leksbø TS, Haga SM, Jacobsen H, Størksen HT. Drozd F, et al. BMC Health Serv Res. 2024 Feb 7;24(1):175. doi: 10.1186/s12913-024-10632-w. BMC Health Serv Res. 2024. PMID: 38326797 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Silverchair Information Systems
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Harvard Business School →
- Faculty & Research →
- January 2023
- Annual Review of Organizational Psychology and Organizational Behavior
Psychological Safety Comes of Age: Observed Themes in an Established Literature
- Format: Print
- | Pages: 24
- Find it at Harvard
About The Author
Amy C. Edmondson
More from the authors.
- Faculty Research
Leading Culture Change at Microsoft Western Europe
Right kind of wrong: the science of failing well.
- September 2023
- Administrative Science Quarterly
The Dynamics of Team Learning: Harmony and Rhythm in Teamwork Arrangements for Innovation
- Leading Culture Change at Microsoft Western Europe By: Amy C. Edmondson and Cat Huang
- Right Kind of Wrong: The Science of Failing Well By: Amy Edmondson
- The Dynamics of Team Learning: Harmony and Rhythm in Teamwork Arrangements for Innovation By: Jean-François Harvey, Johnathan R. Cromwell, Kevin J. Johnson and Amy C. Edmondson
- Open access
- Published: 14 April 2021
Enhancing psychological safety in mental health services
- D. F. Hunt ORCID: orcid.org/0000-0002-8802-7368 1 , 2 ,
- J. Bailey 4 ,
- B. R. Lennox 2 , 3 ,
- M. Crofts 2 &
- C. Vincent 1 , 2
International Journal of Mental Health Systems volume 15 , Article number: 33 ( 2021 ) Cite this article
25k Accesses
25 Citations
12 Altmetric
Metrics details
Psychological safety—speaking up about ideas and concerns, free from interpersonal risk—are essential to the high-risk environment, such as healthcare settings. Psychologically safe working is particularly important in mental health where recovery-oriented approaches rely on collaborative efforts of interprofessional teams to make complex decisions. Much research focuses on antecedents and outcomes associated with psychological safety, but little focus on the practical steps for how to increase psychological safety across and at different levels of a healthcare organisation.
We explore how a mental health organisation creates an organisation-wide plan for building the foundations of mental health and how to enhance psychological safety.
This review encompasses strategies across psychological safety and organisational culture change to increase psychological safety at an individual, team and organisational level.
We set out a comprehensive overview of the types of strategies and interventions for increasing the ethos of psychological safety and setting the foundations for delivering an organisation-wide programme on this topic. We also provide a list of key targeted areas in mental health that would maximally benefit from increasing psychological safety—both in clinical and non-clinical settings.
Conclusions
Psychological safety is a crucial determinant of safe and effective patient care in mental health services. This paper provides the key steps and considerations, creating a large-scale programme in psychological safety with a focus on mental health and drawing from the current literature, providing concrete steps for how our current understanding of psychological safety into practice.
Psychological safety is the shared belief that it is safe to engage in interpersonal risk-taking in the workplace and is vital to team learning and performance, and facilitates willingness for workers to contribute towards a shared goal [ 1 , 2 ]. Ideally, staff are free from the fear of being rejected for speaking up with suggestions and will be treated fairly and compassionately when discussing concerns, errors, or identifying problems. Not only to feel free from fear but also free from interpersonal, professional and social threats that could unfairly threaten their work status and future professional and occupational progression.
Psychological safety is particularly important in high-risk environments, such as healthcare, that rely on staff working in interprofessional and interdisciplinary environments where errors can result in significant harm or even death [ 3 , 4 , 5 , 6 ]. Despite the benefits of psychological safety, a culture of blame and fear is still prevalent in healthcare organisations, which is detrimental to patient safety, staff morale and organisational performance, leading to unreported errors and decreased patient safety [ 7 , 8 , 9 , 10 ]. This culture of blame and fear possibly compounded in countries that strictly adhere to hierarchical structures, where structure and control are paramount, with little to no opportunity for candid conversations across different organisation levels. Countries with market cultures may place competitiveness over the importance of discussing failures, creating a potentially toxic environment.
Psychological safety has an additional resonance and importance in mental health in empowering patients and families to voice their suggestions, concerns and anxieties. Many mental healthcare organisations adopt a recovery-oriented approach, focusing on empowering patients with the help of support structures (i.e., family and carers) to build on their strengths, make informed choices and play a central role in their health and other aspects of life [ 11 ].
This paper will discuss the benefits of creating a psychologically safe culture and then tackle the more difficult task of how psychological safety can be implemented organisation-wide. We first consider the challenges of cultural change of any kind, before addressing the particular challenge of enhancing psychological safety in mental health services. We set out a range of practical proposals to both support a broader organisational ethos of psychological safety and complementary initiatives which target settings that could benefit most from this approach. The design simultaneously considers building an ethos of psychological safety as well as targeted interventions that can have a measurable and impactful change.
The challenges of cultural change
Organisational culture is the personality or spirit of an organisation. It is critical to the engagement and wellbeing of its workforce. More specifically, it is the collective manifestation of the shared beliefs, behaviours, thoughts, attitudes and norms that permeate throughout the workplace [ 12 ]. Schein describes culture as “the pattern of shared basic assumption—invented, discovered or developed by a given group” that new members receive as the “way we do things around here” [ 13 , 14 ]. Importantly, this interpretation encompasses the observable socio-cognitive, interpersonal and symbolic manifestations of culture [ 15 ]. In this sense, organisational culture acts as the collective and is the potential driver of wider organisational innovation and change [ 16 ].
Despite the clear benefits of a positive organisational culture in healthcare, it has proved very difficult to achieve in practice and even more difficult to demonstrate. Recent systematic reviews investigating organisational cultural change on healthcare performance have not shown reliable results on its effectiveness [ 15 , 17 ]. This is echoed in other research, with many attempts failing immediately or not sustaining over a long period [ 18 ]. Underlying these challenges is a longstanding debate whether it is possible to influence culture directly or whether it simply has to be taken into account, like the weather, when planning interventions and change [ 19 ].
Culture change in healthcare poses additional challenges. Healthcare needs and behaviours change over time to reflect the complex and diverse nature of patient needs, as well as increasing complexities in healthcare delivery. Typically, healthcare consists of different nested structures, some clinical and others non-clinical, with an executive core. Any team may deal with a different population, provide a different service or be part of several different services, and be placed within a particular location and form part of a particular site or be spread across multiple sites [ 20 ]. As well as team heterogeneity, healthcare organisations have multiple stakeholders’ interests and differing levels of interest that can present challenges to implementing consistent change. All of this has particular resonance and relevance when fostering a culture of psychological safety in a healthcare organisation.
On an international scale, the prevailing national culture will significantly influence whether cultural change is possible in any healthcare organisation in any given country. Factors such as individualistic vs collectivist ideologies, patriarchal vs matriarchal cultures, levels of tolerance of uncertainty will undoubtedly influence navigating cultural change in terms of what is achievable.
Psychological safety in mental health
Creating a psychologically safe culture offers direct benefits to staff and the healthcare it provides, as well as making the foundations required for any future cultural changes. In healthcare, these benefits can be seen both in the day-to-day management and clinical practice and in providing the necessary foundations for longer-term improvement and innovation. In this section, we briefly set out areas which have particular relevance in mental health services.
Speaking up and error management
Psychological safety plays a central role in detecting errors and near misses [ 1 , 2 , 21 ]. Speaking up is potentially particularly challenging in situations where there are intra-organisational (e.g., issues around patient safety and bed capacity) and inter-organisational (e.g., regulatory pressures from healthcare inspectorates) pressures.
The importance of speaking up is recognised internationally, with concerted efforts to remove barriers in healthcare organisations [ 22 , 23 ]. Across countries and cultures, there are common barriers such as power and hierarchy, leadership influence, and concerns regarding the negative consequences of speaking up [ 23 ]. Most studies of psychological safety have been carried out in the United States and Europe, but the importance of speaking up to prevent errors has been recognised in diverse clinical settings across the world [ 22 , 24 , 25 ]. Patient safety teaching programmes and the World Health Organisation curriculum guide also recognise the critical role played by open communication within teams [ 26 , 27 ].
In mental health, open and candid discussions are crucial as many clinical decisions are complex and ambiguous, and are a collection of subjective observations of a patient [ 28 , 29 ]. Staff should not only be encouraged to discuss errors, but it should be an organisational cultural expectation. In return, staff should receive fair treatment and investigations into error will consider all contributing factors (e.g., staffing levels, patient acuity). Rather than error management just serving as an assurance tool for safe care, psychologically safe organisations use it as an opportunity to learn, to improve, and to calibrate expectations across its workforce.
The confidence to voice concerns is especially critical for patients, carers and families in mental health services. However, not all patients and loved ones feel able to discuss the difficulties that they have with their mental health issues or experiences of care. This is especially important as carers and families form an integral part of mental healthcare in the community. Psychologically safe organisations give patients, family, and carers the opportunities and space to have candid discussions and care pathways to be adapted to accommodate these discussions.
Foundations of safety and quality improvement
Studies in other industries indicate a relationship between psychological safety and a capacity for rapid learning and innovation [ 30 , 31 ]. Innovation and quality improvement (QI) rely on the workforce having the opportunity to feedback on problem areas that may require attention or that could be improved. Engaged staff who feel a collective responsibility provide intelligence on local need and effort in embedding change. Psychological safety is vital throughout all QI stages, from candid discussions when identifying problems, to taking controlled risks when experimenting and being free from fear of failure.
Psychological safety and its implications to QI are important in all countries. It is crucial in lower-income countries seeking to build and mature an effective healthcare workforce [ 32 ]. Both psychological safety and learning behaviours are key factors for the success of newly-formed QI teams in these settings [ 23 , 32 ].
There has been a strong focus on QI in mental health, with many healthcare organisations shifting from away from assurance-based reporting. This approach has been reflected in healthcare inspectorates and regulators, such as the CQC’s evaluation of mental health in the UK, emphasising QI approaches [ 33 ].
Teams characterised by interpersonal trust and respect are more likely to engage in QI projects [ 21 , 34 , 35 ]. A psychologically safe organisation will understand the importance of learning from failure, and that as organisational changes are difficult, its workforce will understand the part they play in its success.
Psychological safety and wellbeing
Promoting work-based wellbeing requires individuals to be able to recognise and report when they need help and are struggling with current work demands. Being able to admit that you need help can be viewed as a weakness with some being fearful that it may affect their reputation, job stability and future career prospects. However, not being able to speak up can lead to work-related stress, which can incubate this problem and lead to more significant health problems further down the line [ 36 ]. In mental health, speaking up about wellbeing may be incredibly difficult for staff as they may support people with similar challenges. Moreover, some staff may feel that speaking up about these issues will affect their perceived competence in carrying out their duties.
Confidence for healthcare staff to speak up is especially crucial during the COVID-19 pandemic, when many staff could be at risk of post-traumatic stress disorder or forms of moral injury, subsequently affecting their health and the care they provide (i.e., feelings of guilt in not being able to cope with current work conditions [ 37 ]).
Principles of psychological safety
Studies of organisational change in general, and culture change in particular, suggest that several essential principles underlie any successful programme. To note, a recent systematic review discuss factors that enable psychological safety [ 4 ]. These principles focus on a whole system approach, considering behavioural change towards staff taking interpersonal risks in speaking up, leadership support to model and enable these changes and facilitating environmental and organisational changes. We summarise the main principles and success factors here, before turning to the practicalities of mapping and intervention.
Psychological safety at every level
Psychological safety must be lived and experienced at every level of the organisation. This is clearly an ambitious and idealistic proposition but is vital as a principle even if it is hard to achieve in practice. Psychological safety will, however, be experienced and expressed in different ways according to the work context (Table 1 ).
Executive leadership is essential for any large-scale change [ 38 , 39 ]. Any organisation-wide programme requires engagement from the extended executive to simultaneously engage stakeholders from different directorates and core operations (i.e., HR, Governance). Executive buy-in is necessary at an early stage by discussing the research literature, options available, and developing an initial work plan with multiple streams. Furthermore, it increases the likelihood of obtaining an adequate level of investment at an early stage.
Cultures and sub-cultures
Healthcare organisations are likely to be comprised of many subcultures [ 19 ]. The extent to which each subculture is psychologically safe will vary. Some teams may champion speaking up and open discussion, while others may be less psychologically safe. Staff may fear the risk of punishment or damage to their job security, engagement, and future job prospects. Some teams may be more willing to make changes that increase psychological safety. In contrast, some may feel resistant to change and hold on to current practice.
Creating a flexible psychological safety programme, refined to meet local need is crucial to the success of an organisation-wide programme. Indeed, teams vary in terms of their beliefs related to psychological safety. These can be influenced by variance in local manager styles and the known consequences in taking an interpersonal risk to speak up [ 2 , 40 ]. Research underpins the importance of local leadership behaviours to enhance psychological safety; these behaviours include transformational leadership, leadership inclusiveness, managerial openness, trustworthiness and behavioural integrity [ 21 , 41 , 42 , 43 , 44 ]. Furthermore, teams might vary in terms of the operational processes in place that facilitate psychological safety (e.g., meeting structures, content and frequency).
As well as recognising positive leadership styles, leadership values and behaviours should align with psychologically safe practice modelling throughout the organisation at an executive and local level. This approach requires a balance between not promoting direct and combative altercations within and between teams, but equally, not allowing unspoken issues and differences to fester and incubate into much larger problems in the future. As such, leaders at all levels must provide opportunities for subordinates to speak up, but equally to manage contributions positively and collaboratively. Moreover, leaders must also have the courage to temper or even thwart contributions that undermine psychologically safe practice. In other words, psychological safety is to promote collaborative and candid focused discussions and not a carte blanche approach, accepting any contributions. As well as the role of leaders in fostering psychological safety, it is also vital that they feel psychologically safe in their managerial duties and have HR practices that support them.
Collaboration, co-design and co-production
Co-production demonstrates and utilises the value of experiential knowledge of staff, patients and their carers and families. This approach is a core practice that is commonly applied in health-related research [ 45 , 46 ]. There are several connotations to the meaning of co-design/production in different contexts. For psychological safety, it is the collective responsibility in contributing to innovation and change that may lead to safer patient care. This includes contributing to suggestions for change, experimentation and providing feedback, and making efforts to implement changes into practice.
There are several reasons why this is important for the development of psychological safety interventions. First, it provides an opportunity for staff to participate in collaborating and co-designing interventions to apply their understanding of the local nuances to organisational plans, maximising chances of success [ 47 ]. Second, the experience of collaboration in itself can foster an experience of psychological safety and persuade staff of the sincerity of the intentions of executive leadership. Thirdly, co-design/production also increases the intrinsic motivation of staff and increases engagement in these changes and further promotes sustainability [ 48 ]. Finally, and related to the role of executive-level leadership support, co-design/production also places value in the involvement of staff, providing them with the opportunity to have the authority and feel empowered in supporting in increasing psychological safety.
Understanding the current experience and practice of psychological safety
The first step in developing a programme is to assess the current state of psychological safety in the organisation, in terms of overall understanding and practice. Most organisations will also have other plans and initiatives already running, for instance, on staff well-being, which will overlap with the proposed programme on psychological safety. Mapping existing initiatives reduce the risk of duplicating work and, subsequently, maximises investment in changes related to improve psychological safety. This landscape mapping and scoping require a few key foundation steps (Box 1 ).
Box 1 First steps in psychological safety
Assemble a small team to conduct the mapping exercise and will have access to key contacts within the organisation | |
Establish a small steering group to guide the parameters of this mapping exercise, the ambitions and criteria for success | |
Agree on an operational definition to identify what is a psychologically safe practice and what is not | |
Establish a series of workshops, focus groups and interviews to explore current experience and perceptions of psychological safety with patients, families and staff | |
Review relevant documents and procedures which may either support or detract from psychological safety | |
Review training programmes, induction and other initiative both in terms of their ethos and content concerning psychological safety | |
To establish a baseline measurement of psychological safety across the organisation |
Understanding the patient and family/carer experience
It is important to explore patient understanding of speaking up and their family/carer experience, who often form part delivering informal care. Unlike staff surveys, there is unlikely to be any large-scale surveys to formally capture the climate of psychological safety across all family members and carers involved in care. This is for several reasons. First, not all informal support is visible to the healthcare system (e.g., the sibling who supports their brother or sister when arriving home from school or work). Secondly, not all family/carers have access to the same methods of communication (e.g., email). Finally, this population is typically geographically disparate when compared to a healthcare workforce. The first step is to reach out to all active patients in the organisation to ask for participation. For particular groups, there may be gatekeepers that play an integral role in representing their population. Gatekeepers can include formal organisations such as large charities or local initiatives, or virtual social media support groups. Any focus groups or interviews should be at the convenience of patients and family/carers and should provide confidentiality. Messaging around these approaches is particularly important, clearly articulating that these experiences will inform mental healthcare delivery.
Understanding the staff experience
Staff surveys (discussed below) will give a general picture of psychological safety across an organisation, but it is essential to complement this with a more nuanced understanding of staff views and experience of psychological safety. For example, a series of focus groups could be run with junior staff to explore their perceptions of speaking up. The experience of staff needs to be understood at all levels and sampled across all settings in the organisation. To fully engage with the workforce, it is essential that an accurate representation of perceptions of psychological safety, including barriers and opportunities. Those staff who feel trust in an organisation will be relatively easy to recruit, thus potentially biasing the findings. It is therefore critical to reach out to other individuals and groups who may be warier of speaking about their experiences. For example, introverted people, who may be less likely to speak up, but have equally valuable ideas than more assertive extroverts. It is therefore essential to gather feedback from those who do not typically speak up to gather the quiet power they bring in increasing psychological safety.
One way is to establish trusted gatekeepers who can serve to champion these initial discussions and facilitate in increasing confidence in speaking up, such as clinical leaders who may represent the protection of standards and quality. Engaging union representatives is a suitable method of reaching disenfranchised groups as well as provided reassurance of the confidential nature of such discussions. To further bolster confidentiality, focus groups can be held outside of regular working hours and at a neutral venue, so their participation remains confidential. Facilitators can be from an independent organisation or be a trusted person from the current organisation. For example, a chaplain from the organisation or union representatives are potentially ideal for facilitating these discussions. Telephone interviews also offer an alternative method of discussing this topic without the need to attend a venue and be recognised by others in the group.
Review of core organisational policies and procedures
Organisational culture is primarily determined by the behaviour of people, particularly leaders, in that organisation. However, documents, procedures and symbols used by the organisation also express organisational culture. There are specific policies that would benefit from having a psychologically safe focus. For example, whistleblowing policies should embed psychologically safe practices to enable candid and fair dialogue between the whistle blower, those potentially implicated and the organisation. Encouraging staff to speak up is the first step, and organisational practices that support what happens after someone has spoken up is essential to sustaining these behaviours amongst the workforce. Policies relating to near misses should shift from being an assurance-based tool to encouraging and even rewarding staff that speak up, as well as promoting transparency, to show what learning and improvement are looped back into the organisation. Those policies enacting organisational change should take a similar approach, setting out an engagement approach to utilise local intelligence and gain buy-in from the workforce.
Review induction and training programmes
Healthcare organisations provide different forms of education, both formal and informal, to all levels of the workforce. Many of the induction programmes include essential training on governance and information security, but other courses can consist of methods of care. For some roles (e.g., nurses, allied healthcare roles, and doctors), years of formal education has been completed as well as several placements. Local and organisation-wide induction training should focus on antecedents of psychological safety, such as team working, voice behaviours, and respectful listening [ 6 ]. Leadership programmes should have a strong focus on leadership behaviours such as inclusive, compassionate and collaborative leadership are integral to psychological safety [ 6 , 31 ].
Measuring psychological safety
Psychological safety is a complex multi-faceted concept and, subsequently, understanding the extent to which it has been a success and how this can be measured is a challenge. The most common form of measure for psychological safety is a team-level survey [ 1 ]. Others have adapted this survey to measure psychological safety at an individual- and organisation-level [ 42 , 49 ].
Healthcare organisations typically send out staff surveys that are focused on different aspects of work experiences from their workforce. These surveys tend to cover categories that can serve as indicators for psychological safety (perceived managerial and organisational support, perceived compassion), so teams or services that may score low in these areas may also feel psychologically unsafe. For a major programme, however, it would be preferable to mount a specific survey of psychological safety at baseline and defined intervals as the programme unfolds. Burdening staff with additional surveys is of course, always a concern, but these are short and take only a few minutes to complete. Careful sampling strategies will also reduce the number of staff recruited to complete a new survey or adding questions to existing surveys. As well as producing longitudinal data, surveys can be useful in identifying groups of people who have scored low on psychological safety or who do not even feel able to complete a survey. These individuals and groups need particular support as executive leaders seek to gain trust across the whole organisation.
Objective measures of psychological safety will be beneficial for future research in this area. For example, observational frameworks relating to the verbal and non-verbal indicators of psychologically safe and unsafe practices might be particularly helpful in simulation interventions around speaking up and decision making. Once behaviours of psychological safety are agreed, behavioural markers provide ways to measure what is good or poor practice. Indeed, simulation-based education uses these frameworks to measure speaking up and assessing non-technical skills amongst medical teams [ 50 , 51 ]. As such, observational frameworks behaviours provide an opportunity to measure behaviours reflective of psychological safety. In particular, to measure psychologically safe practice in some of the targeted interventions discussed below.
In the longer term, the fostering and enhancement of psychological safety should influence healthcare outcomes, such as improvements in patient safety and staff engagement. However, psychological safety is only one of many influences on such indices, and, therefore, it is challenging to measure a direct effect reliably. Assessing more immediate impacts, such as increased speaking up or reporting of near misses, maybe a more realistic earlier target. Furthermore, these targets can create a pathway to link the effects of psychological safety on ultimate outcomes such as safe patient care. Implementing a cultural change and increasing psychological safety will take a considerable amount of time, both in terms of a cultural shift with the existing workforce and inducting new staff. Staff surveys and evaluation of current practices over a long period offer an opportunity to realise the longer-term outcomes of a programme such as the one described.
Enhancing psychological safety
Psychological safety is an intuitively straightforward and persuasive concept, though on reflection more complicated than it immediately appears. However, making meaningful, concrete steps to enhance psychological safety in an organisation is challenging for several reasons. First, psychological safety is multi-faceted, meaning that it requires a multi-faceted approach to change. Second, enhancing psychological safety requires a cultural shift, and any cultural initiative involves engagement and commitment from the majority of the workforce at all levels. Third, measuring psychological safety is especially challenging, in terms of how it influences ultimate outcomes such as patient safety, healthcare improvement and wellbeing. Finally, and most importantly, it is difficult to identify what concrete steps to take to enhance psychological safety, in what order and over what timescale. While there are many inspiring descriptions of organisations, who have embraced psychological safety, very little research provides any kind of defined set of steps or interventions. The journey of each organisation will be different, but it would be beneficial to define the essential components of a programme to enhance psychological safety.
Most psychological safety interventions aim to produce a broad change in attitudes, values and trust across the whole organisation. We refer to this generic approach as building an ethos of psychological safety. Targeted interventions, addressing settings and activities in which psychological safety is particularly critical, provide a complementary approach. Promoting a psychologically safe ethos should focus particularly on being a person-centred organisation, and a listening and learning organisation. A person-centred organisation will facilitate staff participating in creating an engaging workplace that focuses on safe patient care. A listening and learning organisation will make sure that they hear staff voices to discuss ideas for improvements, mistakes and errors, and contribute to failure-based learning.
The wider literature on psychological safety and organisational change suggest that there are a number of potentially useful means of exploring and influencing the experience of psychological safety. In Box 2 we set out the target actions for increasing an ethos of psychological safety, and in Table 2 we set out methods for implementing these actions, based on literature relating to psychological safety interventions and organisational change interventions [ 4 , 15 , 17 , 52 , 53 ].
Box 2 Areas of action to increase a culture of psychological safety
1. Select and engage a core group of key influencers in the organisation to lay out a strategic plan with the core columns of psychologically safe practice. Pillars for ultimate outcomes and cross-cutting themes for the requirements to achieve these outcomes. A visual representation of this is below: | |
| |
2. Support and commitment to psychologically safe practice from the organisation to their workforce. This approach includes communicating this commitment to the workforce and the wider community, solidifying the organisational commitment to psychological safety to the proposed strategic plan | |
3. Leadership messaging to model psychological safety and focus on the following topics: (a) Discussing the importance of reporting failures and benefits from focusing on quality improvement. Providing empirical substantiation to create an impetus for change (b) Discuss the collective responsibility of staff to speak up when delivering safe patient care and areas that can be improved, including plans to make the process of reporting fair and straightforward. This can also include actively congratulating and even rewarding these actions, where appropriate (c) Discuss personal experiences of occupational failure and what learned lessons from these experiences. This will serve to make failure an acceptable and model that it is acceptable and is part of occupational development (d) Discuss previous difficulties in speaking up to senior colleagues, lessons learned and the importance of speaking up and shared decision-making within and between teams and professions | |
4. Create a code of conduct to set expectations for how people should act with each other and instil the values of psychological safety, including open and candid discussions, balanced with compassion and fairness: respectful listening and collaborative debate, all with the focus on providing safe and optimum patient care | |
5. Forums and structured discussions for intra- and inter-professional groups to discuss challenges and opportunities in mental health practice. These could provide opportunities to: (a) Create a series of groups that target particular professions, services or problems related to psychological safety. Each group should include an appropriate sponsor who will commit to championing actions arising from these discussions (b) Discuss the collective responsibility of staff to speak up when delivering safe patient care and areas that can be improved. Crucially, these discussions should directly feedback into the organisation and take an action research approach to create improvements from these discussions (c) Provide opportunities to discuss complex decision-making and inform action research that involves staff in co-designing interventions to enhance behaviours relating to psychologically safe practice | |
6. Provide training that focuses on psychologically safe behaviours and practice. These include speaking up and voice behaviours, autonomy, respectful listening, collaborative working, advocacy enquiry and collaborative debate | |
7. Create medical, educational interventions that allow teams to practice psychologically safe practice in clinical and non-clinical situations. These can include simulating high-pressured situations such as aggressive and violent patients |
Targeted interventions
Psychological safety culture change requires a broad approach to instil the ethos through all layers of the organisation, creating a consistent message and support for this approach. However, alongside this, targeted interventions provide an opportunity to create test beds where psychological safety is vitally important. There are ‘pinch points’ when it is particularly important for patient, family and staff engagement and the delivery of care. Psychological safety is particularly important, when coercive measures have to be used to protect the patient from harming themselves or other people. The trauma and distress that such measures may provoke can be eased by open and compassionate communication at the time and by careful debriefing and explanation afterwards when the crisis has passed. Whilst debriefs tend to be a statutory requirement, they provide an opportunity for increased staff reflexivity, empower patients to contribute to their care (e.g., discuss future ways of using alternative options to restrictive practice) and enhance patient outcomes [ 72 ].
In the broadest sense, targeted interventions fall into two categories. The first is structured situations such as meetings that provide an opportunity to speak up about areas of concern or possible improvement. The second is where decisions are made in situ and take place on an ad hoc basis and require a group discussion. When a decision is complex, and there is no obviously correct course of action, it is particularly critical that patients, families and staff all feel able to speak openly and contribute to the decision-making process. Table 3 provides some key target areas for psychological safety, both in a clinical and non-clinical setting.
In the targeted interventions discussed, three common themes emerge in mental healthcare practice. The first is the importance of empowering patients by keeping them informed at every stage of their care and providing patient choice wherever possible. The second is the importance respecting and encouraging the contributions of all healthcare staff that help deliver patient-centered and recovery-oriented care. The third is understanding that in difficult situations, such as disputes or grievance procedures, there should be an expectation of candid, open, and fair conversations that are collaborative in nature and not combative, focusing on individual development and team development.
Psychologically safe practice is essential in mental health to innovative practice and safe patient care, provided by a healthy and engaged workforce. Despite psychological safety, being an intuitive concept to understand, operationalising it at scale is particularly challenging. It has a particular resonance in mental health for two reasons. First, many mental health organisations focus on recovery-oriented practice which requires substantial patient and family involvement. Second, decision making in mental health is often complex and ambiguous, based on subjective observations that require whole team input. As such, assuring all parties feel free to speak up and have maximum involvement is vital to safe and optimum mental health patient care.
This overview and proposed plan for enhancing psychological safety largely focuses on the UK mental healthcare system and may not be applicable to healthcare settings in different countries. Indeed, healthcare organisations will differ in terms of their structures, levels of investment and prevailing cultures, meaning that not all aspects of this plan are applicable in different countries or cultures. Despite these differences, many of the challenges and suggested approaches will translate on across countries and cultures. For example, the importance of speaking up about errors or ideas for improvements, the barriers are common across different countries and cultures.
As well as staff engagement, establishing a council of patients and actively encouraging family/carer participation is possible in all settings, even if this is more challenging in some cultures. As such, whilst the plan itself may not be applicable to different and more disparate healthcare organisations, many of the suggestions can be applied individually or tailored to be applicable to different settings.
Future studies may explore methods for implementing psychological safety in non-traditional organisational research settings, and factor in the recognised differences in culture and existing structures. For example, one might envisage healthcare organisations may differ in societies strong in collectivist vs individualistic ideologies.
In this paper, we discuss how to create the foundations of psychological safety and the importance of preparatory stages from a structural and cultural perspective. Following this, we propose a practical guide that split psychological safety into two categories: building an ethos across an organisation and target areas, including some specific to mental health. This paper seeks to provide two advancements. First, it can serve as a ‘blueprint’ for healthcare organisations to approach enhancing psychological safety in a meaningful way. Second, it provides suggestions for research to be advanced in psychological safety, with a particular focus on what possible routes for development. This paper, therefore, serves as a primer for approaching psychological safety and forms a bedrock for further development on this topic, from a mental health perspective.
Availability of data and materials
Not applicable.
Edmondson A. Psychological safety and learning behavior in work teams. Adm Sci Q. 1999;44(2):350–83. https://doi.org/10.2307/2666999 .
Article Google Scholar
Edmondson AC. Speaking up in the operating room: how team leaders promote learning in interdisciplinary action teams. J Manage Stud. 2003;40(6):1419–52. https://doi.org/10.1111/1467-6486.00386 .
Leroy H, Dierynck B, Anseel F, Simons T, Halbesleben JR, McCaughey D, Savage GT, Sels L. Behavioral integrity for safety, priority of safety, psychological safety, and patient safety: a team-level study. J Appl Psychol. 2012;97(6):1273. https://doi.org/10.1037/a0030076 .
Article PubMed Google Scholar
O'donovan R, Mcauliffe E. A systematic review of factors that enable psychological safety in healthcare teams. Int J Qual Health Care. 2020;32(4):240–50. https://doi.org/10.1093/intqhc/mzaa025 .
O’donovan R, McAuliffe E. A systematic review exploring the content and outcomes of interventions to improve psychological safety speaking up and voice behaviour. BMC Health Serv Res. 2020;20(1):1–1. https://doi.org/10.1186/s12913-020-4931-2 .
Newman A, Donohue R, Eva N. Psychological safety: a systematic review of the literature. Human Resour Manage Rev. 2017;27(3):521–35. https://doi.org/10.1016/j.hrmr.2017.01.001 .
Alnaqi H, McIntosh B, Lancaster A. Cultures of fear: perspectives on whistleblowing. Br J Mental Health Nurs. 2017;6(3):134–7. https://doi.org/10.12968/bjmh.2017.6.3.134 .
Moore L, McAuliffe E. To report or not to report? Why some nurses are reluctant to whistleblow. Clin Gov Int J. 2012. https://doi.org/10.1108/14777271211273215 .
Moore L, McAuliffe E. Is inadequate response to whistleblowing perpetuating a culture of silence in hospitals? Clin Gov Int J. 2010. https://doi.org/10.1108/14777271011063805 .
Patrick K. Barriers to whistleblowing in the NHS. https://doi.org/10.1136/bmj.e6840
Slade M, Amering M, Farkas M, Hamilton B, O’Hagan M, Panther G, Perkins R, Shepherd G, Tse S, Whitley R. Uses and abuses of recovery: implementing recovery-oriented practices in mental health systems. World Psychiatry. 2014;13(1):12–20. https://doi.org/10.1002/wps.20084 .
Article PubMed PubMed Central Google Scholar
Reason J. Managing the risks of organizational accidents. Routledge; 2016.
Schein EH. Organizational culture and leadership San Francisco. San Francisco: Jossey-Basss; 1985.
Google Scholar
Balogun J, Hailey VH. Exploring strategic change. Pearson Education; 2008.
Parmelli E, Flodgren G, Beyer F, Baillie N, Schaafsma ME, Eccles MP. The effectiveness of strategies to change organisational culture to improve healthcare performance: a systematic review. Implementat Sci. 2011;6(1):33. https://doi.org/10.1186/1748-5908-6-33 .
Konteh FH, Mannion R, Davies HT. Clinical governance views on culture and quality improvement. Clin Gov Int J. 2008. https://doi.org/10.1108/14777270810892610 .
Parmelli E, Flodgren G, Schaafsma ME, Baillie N, Beyer FR, Eccles MP. The effectiveness of strategies to change organisational culture to improve healthcare performance. Cochrane Database Syst Rev. 2011;1. https://doi.org/10.1002/14651858.CD008315.pub2 .
Smith ME. Changing an organisation’s culture: correlates of success and failure. Leadership Organ Dev J. 2003. https://doi.org/10.1108/01437730310485752 .
Mannion R, Davies H. Understanding organisational culture for healthcare quality improvement. BMJ. 2018;28:363. https://doi.org/10.1136/bmj.k4907 .
Edmondson AC, Higgins M, Singer S, Weiner J. Understanding psychological safety in health care and education organizations: a comparative perspective. Res Human Dev. 2016;13(1):65–83. https://doi.org/10.1080/15427609.2016.1141280 .
Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav Intern J Indus Occup Organ Psychol Behav. 2006;27(7):941–66. https://doi.org/10.1002/job.413 .
Edrees HH, Ismail MN, Kelly B, Goeschel CA, Berenholtz SM, Pronovost PJ, Al Obaidli AA, Weaver SJ. Examining influences on speaking up among critical care healthcare providers in the United Arab Emirates. Int J Qual Health Care. 2017;29(7):948–60. https://doi.org/10.1093/intqhc/mzx144 .
Morrow KJ, Gustavson AM, Jones J. Speaking up behaviours (safety voices) of healthcare workers: a metasynthesis of qualitative research studies. Int J Nurs Stud. 2016;1(64):42–51. https://doi.org/10.1016/j.ijnurstu.2016.09.014 .
English M, Ogola M, Aluvaala J, Gicheha E, Irimu G, McKnight J, Vincent CA. First do no harm: practitioners’ ability to ‘diagnose’system weaknesses and improve safety is a critical initial step in improving care quality. Arch Dis Child. 2020. https://doi.org/10.1136/archdischild-2020-320630 .
Hurley J, Hutchinson M. Hierarchy and medical error: speaking up when witnessing an error. Saf Sci. 2020;1(125):104648. https://doi.org/10.1016/j.ssci.2020.104648 .
World Health Organization. WHO patient safety curriculum guide for medical schools. 2009.
Johnston BE, Lou-Meda R, Mendez S, Frush K, Milne J, Fitzgerald T, Sexton JB, Rice H. Teaching patient safety in global health: lessons from the Duke Global Health Patient Safety Fellowship. BMJ Global Health. 2019;4(1). https://doi.org/10.1136/bmjgh-2018-001220 .
Marangos-Frost S, Wells D. Psychiatric nurses’ thoughts and feelings about restraint use: a decision dilemma. J Adv Nurs. 2000;31(2):362–9. https://doi.org/10.1046/j.1365-2648.2000.01290.x .
Article CAS PubMed Google Scholar
Wynaden D, Chapman R, McGowan S, Holmes C, Ash P, Boschman A. Through the eye of the beholder: to seclude or not to seclude. Intern J Mental Health Nurs. 2002;11(4):260–8. https://doi.org/10.1046/j.1440-0979.2002.00257.x .
Carmeli A, Gittell JH. High-quality relationships, psychological safety, and learning from failures in work organizations. J Organ Behav Intern J Indus Occup Organ Psychol Behav. 2009;30(6):709–29. https://doi.org/10.1002/job.565 .
Edmondson AC, Lei Z. Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23–43. https://doi.org/10.1146/annurev-orgpsych-031413-091305 .
Albritton JA, Fried B, Singh K, Weiner BJ, Reeve B, Edwards JR. The role of psychological safety and learning behavior in the development of effective quality improvement teams in Ghana: an observational study. BMC Health Serv Res. 2019;19(1):385. https://doi.org/10.1186/s12913-019-4234-7 .
Care Quality Commission. Quality improvement in hospital trusts: Sharing learning from trusts on a journey of QI. Newcastle-upon-Tyne: Care Quality Commission; 2018.
Aranzamendez G, James D, Toms R. Finding antecedents of psychological safety: a step toward quality improvement. Nurs Forum. 2015;50(3):171–8. https://doi.org/10.1111/nuf.12084 .
Rathert C, Ishqaidef G, May DR. Improving work environments in health care: test of a theoretical framework. Health Care Manage Rev. 2009;34(4):334–43. https://doi.org/10.1097/HMR.0b013e3181abce2b .
Ilies R, Dimotakis N, De Pater IE. Psychological and physiological reactions to high workloads: implications for well-being. Pers Psychol. 2010;63(2):407–36. https://doi.org/10.1111/j.1744-6570.2010.01175.x .
Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368. https://doi.org/10.1136/bmj.m1211.
Cohen MB, Hyde CA, editors. Empowering workers and clients for organizational change. Oxford: Oxford University Press; 2013.
Schmid H. The contingencies of non-profit leadership. In: Kane et al.(eds). 2009; pp. 193–210.
Edmondson AC. The local and variegated nature of learning in organizations: a group-level perspective. Organ Sci. 2002;13(2):128–46. https://doi.org/10.1287/orsc.13.2.128.530 .
Carmeli A, Reiter-Palmon R, Ziv E. Inclusive leadership and employee involvement in creative tasks in the workplace: the mediating role of psychological safety. Creativ Res J. 2010;22(3):250–60. https://doi.org/10.1080/10400419.2010.504654 .
Detert JR, Burris ER. Leadership behavior and employee voice: is the door really open? Acad Manag J. 2007;50(4):869–84. https://doi.org/10.5465/amj.2007.26279183 .
Madjar N, Ortiz-Walters R. Trust in supervisors and trust in customers: their independent, relative, and joint effects on employee performance and creativity. Human Perform. 2009;22(2):128–42. https://doi.org/10.1080/08959280902743501 .
Palanski ME, Vogelgesang GR. Virtuous creativity: The effects of leader behavioural integrity on follower creative thinking and risk taking. Can J Admin Sci Revue. 2011;28(3):259–69. https://doi.org/10.1002/cjas.219 .
Elliott H, Popay J. How are policy makers using evidence? Models of research utilisation and local NHS policy making. J Epidemiol Commun Health. 2000;54(6):461–8. https://doi.org/10.1136/jech.54.6.461 .
Article CAS Google Scholar
Filipe A, Renedo A, Marston C. The co-production of what? Knowledge, values, and social relations in health care. PLoS Biol. 2017;15(5):e2001403. https://doi.org/10.1371/journal.pbio.2001403 .
Article CAS PubMed PubMed Central Google Scholar
Maybin J. How proximity and trust are key factors in getting research to feed into policymaking. British Politics and Policy at LSE. 2016.
Vennik FD, van de Bovenkamp HM, Putters K, Grit KJ. Co-production in healthcare: rhetoric and practice. Intern Rev Admin Sci. 2016;82(1):150–68. https://doi.org/10.1177/2F0020852315570553 .
Baer M, Frese M. Innovation is not enough: climates for initiative and psychological safety, process innovations, and firm performance. J Organ Behav Intern J Indus Occup Organ Psychol Behav. 2003;24(1):45–68. https://doi.org/10.1002/job.179 .
Flin R, Maran N. Identifying and training non-technical skills for teams in acute medicine. BMJ Qual Saf. 2004;13(suppl 1):i80–4. https://doi.org/10.1136/qshc.2004.009993 .
Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, Raemer D. Teaching residents the two-challenge rule: a simulation-based approach to improve education and patient safety. Simul Healthcare. 2009;4(2):84–91. https://doi.org/10.1097/SIH.0b013e31818cffd3 .
Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G. Association between organisational and workplace cultures, and patient outcomes: systematic review. BMJ Open. 2017;7(11). https://doi.org/10.1136/bmjopen-2017-017708 .
Johnson A, Nguyen H, Groth M, Wang K, Ng JL. Time to change: a review of organisational culture change in health care organisations. J Organ Effect People Perform. 2016. https://doi.org/10.1108/JOEPP-06-2016-0040 .
Larson EL, Early E, Cloonan P, Sugrue S, Parides M. An organizational climate intervention associated with increased handwashing and decreased nosocomial infections. Behav Med. 2000;26(1):14–22. https://doi.org/10.1080/08964280009595749 .
O’Connor P, Byrne D, O’Dea A, McVeigh TP, Kerin MJ. “Excuse me:” teaching interns to speak up. Joint Comm J Qual Patient Saf. 2013;39(9):426–31. https://doi.org/10.1016/S1553-7250(13)39056-4 .
Costello J, Clarke C, Gravely G, D’Agostino-Rose D, Puopolo R. Working together to build a respectful workplace: transforming OR culture. AORN J. 2011;93(1):115–26. https://doi.org/10.1016/j.aorn.2010.05.030 .
Mulcahy C, Betts L. Transforming culture: an exploration of unit culture and nursing retention within a neonatal unit. J Nurs Manag. 2005;13(6):519–23. https://doi.org/10.1111/j.1365-2934.2005.00588.x .
Syse I, Førde R, Pedersen R. Clinical ethics committees—also for mental health care? The Norwegian experience. Clin Ethics. 2016;11(2–3):81–6. https://doi.org/10.1177/2F1477750916657656 .
Thomas JT. The ethics of supervision and consultation: practical guidance for mental health professionals. American Psychological Association; 2010.
Mikkelsen EG, Hogh A, Puggaard LB. Prevention of bullying and conflicts at work: process factors influencing the implementation and effects of interventions. Intern J Workplace Health Manage. 2011;4(1):84–100. https://doi.org/10.1108/17538351111118617 .
Marcus BS, Shank G, Carlson JN, Venkat A. Qualitative analysis of healthcare professionals’ viewpoints on the role of ethics committees and hospitals in the resolution of clinical ethical dilemmas. HEC Forum (Springer, The Netherlands). 2015;27(1):11–34. https://doi.org/10.1007/s10730-014-9258-0 .
Farr M, Barker R. Can staff be supported to deliver compassionate care through implementing Schwartz Rounds in community and mental health services? Qual Health Res. 2017;27(11):1652–63. https://doi.org/10.1177/1049732317702101 .
Glisson C. Assessing and changing organizational culture and climate for effective services. Res Soc Work Pract. 2007;17(6):736–47. https://doi.org/10.1177/1049731507301659 .
Brown D, McCormack B. Exploring psychological safety as a component of facilitation within the promoting action on research Implementation in Health Services framework. J Clin Nurs. 2016;25(19–20):2921–32. https://doi.org/10.1111/jocn.13348 .
O’Leary DF. Exploring the importance of team psychological safety in the development of two interprofessional teams. J Interprof Care. 2016;30(1):29–34. https://doi.org/10.3109/13561820.2015.1072142 .
Haesebaert J, Samson I, Lee-Gosselin H, Guay-Bélanger S, Proteau JF, Drouin G, Guimont C, Vigneault L, Poirier A, Sanon PN, Roch G. “They heard our voice!” patient engagement councils in community-based primary care practices: a participatory action research pilot study. Res Invol Engag. 2020;6(1):1–4. https://doi.org/10.1186/s40900-020-00232-3 .
Cave D, Pearson H, Whitehead P, Rahim-Jamal S. CENTRE: creating psychological safety in groups. Clin Teach. 2016;13(6):427–31. https://doi.org/10.1111/tct.12465 .
Kinjerski V, Skrypnek BJ. The promise of spirit at work increasing job satisfaction and organizational commitment and reducing turnover and absenteeism in long-term care. J Gerontolog Nurs. 2008;34(10):17–25. https://doi.org/10.3928/00989134-20081001-03 .
Swahnberg K, Wijma B. Staff’s perception of abuse in healthcare: a Swedish qualitative study. BMJ Open. 2012;2(5). https://doi.org/10.1136/bmjopen-2012-001111 .
Coyle YM, Mercer SQ, Murphy-Cullen CL, Schneider GW, Hynan LS. Effectiveness of a graduate medical education program for improving medical event reporting attitude and behavior. BMJ Qual Saf. 2005;14(5):383–8. https://doi.org/10.1136/qshc.2005.013979 .
Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Joint Comm J Qual Patient Saf. 2014;40(4):168-AP1. https://doi.org/10.1016/S1553-7250(14)40022-9 .
Hammervold UE, Norvoll R, Aas RW, Sagvaag H. Post-incident review after restraint in mental health care-a potential for knowledge development, recovery promotion and restraint prevention. A scoping review. BMC Health Serv Res. 2019;19(1):1–3. https://doi.org/10.1186/s12913-019-4060-y .
Download references
Acknowledgements
We would like to thank the Oxford Healthcare Improvement Team and the Risk and Safety Group at the Department of Experimental Psychology, University of Oxford for their helpful feedback when developing this article.
There are no funding declarations.
Author information
Authors and affiliations.
Department of Experimental Psychology, Radcliffe Observatory, University of Oxford, Anna Watts Building, Woodstock Road, Oxford, OX2 6GG, UK
D. F. Hunt & C. Vincent
Oxford Health NHS Foundation Trust, Warneford Hospital, Warneford Lane, Headington, Oxford, OX3 7JX, UK
D. F. Hunt, B. R. Lennox, M. Crofts & C. Vincent
Department of Psychiatry, University of Oxford, Warneford Hospital, Warneford Lane, Headington, Oxford, OX3 7JX, UK
B. R. Lennox
Oxford School of Nursing and Midwifery, Oxford Brookes University, Headington Campus, Oxford, OX3 0BP, UK
You can also search for this author in PubMed Google Scholar
Contributions
DFH, JB, and CV contributed to idea formation and drafting the manuscript.
BL and MC contributed to idea refinement and proofreading. All authors read and approved the final manuscript.
Corresponding author
Correspondence to D. F. Hunt .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hunt, D.F., Bailey, J., Lennox, B.R. et al. Enhancing psychological safety in mental health services. Int J Ment Health Syst 15 , 33 (2021). https://doi.org/10.1186/s13033-021-00439-1
Download citation
Received : 20 October 2020
Accepted : 01 February 2021
Published : 14 April 2021
DOI : https://doi.org/10.1186/s13033-021-00439-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
International Journal of Mental Health Systems
ISSN: 1752-4458
- Submission enquiries: [email protected]
- Research article
- Open access
- Published: 10 February 2020
A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour
- Róisín O’Donovan ORCID: orcid.org/0000-0003-1993-5319 1 &
- Eilish McAuliffe 1
BMC Health Services Research volume 20 , Article number: 101 ( 2020 ) Cite this article
30k Accesses
63 Citations
50 Altmetric
Metrics details
Having psychologically safe teams can improve learning, creativity and performance within organisations. Within a healthcare context, psychological safety supports patient safety by enabling engagement in quality improvement and encouraging staff to speak up about errors. Despite the low levels of psychological safety in healthcare teams and the important role it plays in supporting patient safety, there is a dearth of research on interventions that can be used to improve psychological safety or its related constructs. This review synthesises the content, theoretical underpinnings and outcomes of interventions which have targeted psychological safety, speaking up, and voice behaviour within a healthcare setting. It aims to identify successful interventions and inform the development of more effective interventions.
A key word search strategy was developed and used to search electronic databases (PsycINFO, ABI/Inform, Academic search complete and PubMed) and grey literature databases (OpenGrey, OCLC WorldCat, Espace). Covidence, an online specialised systematic review website, was used to screen records. Data extraction, quality appraisal and narrative synthesis were conducted on identified papers.
Fourteen interventions were reviewed. These interventions fell into five categories. Educational interventions used simulation, video presentations, case studies and workshops while interventions which did not include an educational component used holistic facilitation, forum play and action research meetings. Mixed results were found for the efficacy or effectiveness of these interventions. While some interventions showed improvement in outcomes related to psychological safety, speaking up and voice, this was not consistently demonstrated across interventions. Included interventions’ ability to demonstrate improvements in these outcomes were limited by a lack of objective outcome measures and the ability of educational interventions alone to change deeply rooted speaking up behaviours.
To improve our understanding of the efficacy or effectiveness of interventions targeting psychological safety, speaking up and voice behaviour, longitudinal and multifaceted interventions are needed. In order to understand whether these interventions are successful, more objective measures should be developed. It is recommended that future research involves end users in the design phase of interventions, target both group and organisational levels, ensure visible leader support and work across and within interdisciplinary teams.
Prospero registration number
CRD42018100659.
Peer Review reports
When teams are psychologically safe, there is a shared belief that members are safe to take interpersonal risks, such as speaking up and engaging in voice behaviour. This definition of psychological safety was proposed by Amy Edmondson [ 1 ] in 1999 and began research on psychological safety as a phenomenon that exists at a group level and is built through workplace interactions. Psychological safety is a key determinant of high-quality communication, trust and decision making which improves team performance and, therefore, plays an important role within workplace teams [ 2 , 3 , 4 ]. Psychological safety plays a particularly vital role in high-risk work contexts, such as healthcare [ 3 ]. When healthcare teams are psychologically safe they are more likely to engage in quality improvement and team learning initiatives [ 5 , 6 ]. This engagement allows healthcare teams to deal with the increased knowledge they need to absorb, the specialisation of healthcare professionals and the resulting interdependence between these professionals [ 5 ]. Therefore, having psychologically safe teams is critical to the delivery of safe and effective care within a complex, dynamic and high stakes work environment. However, a culture of fear and low psychological safety still exists within healthcare organisations [ 7 , 8 , 9 ]. Given the important outcomes associated with psychological safety, there is a need to develop and implement interventions to improve psychological safety within healthcare teams. This article will build on previous reviews of psychological safety literature [ 2 , 3 ] by examining interventions which specifically aimed to improve psychological safety, or its related constructs, speaking up and voice behaviour. It is hoped that the findings of this synthesis will inform the development of future interventions.
Although research to date has illustrated the beneficial outcomes of psychological safety, there is little guidance on how teams can introduce, improve and maintain psychological safety. In their cross-industry comparison study examining psychological safety in both healthcare and educational contexts, Edmondson and colleagues [ 10 ] acknowledge that there is limited research on interventions to promote psychological safety. They argue that psychological safety would be a useful focus for interventions and provide suggestive avenues for research into such interventions. However, given the dearth of interventions targeting psychological safety, this review will take a broader view by including interventions targeting speaking up and voice behaviour, which are closely related to psychological safety.
Speaking up and voice are interpersonally risky behaviours which are facilitated by psychological safety [ 5 , 11 , 12 , 13 ]. Lack of psychological safety has been associated with silence [ 14 ]. Even when employees believe they have something useful to say, lack of psychological safety often leads them to choose silence over voice [ 9 , 15 , 16 , 17 ]. It is necessary to encourage an organisational climate where it is safe to speak up and voice ideas or concerns, as this enables organisational learning and organisational safety [ 9 , 17 , 18 ].
This review aims to identify team building interventions which have focused on psychological safety and its related components, speaking up, voice and silence behaviours. Team development interventions have been broadly defined as intentional actions which attempt to improve or support teams that may be struggling or adequately performing or maximise the capacities of teams ready to advance to a higher level of performance [ 19 ]. These interventions are relevant to this review, because they are suited to targeting psychological safety, speaking up and voice behaviours. They focus on interpersonal relations in order to increase teamwork process and emergent states such as mutual support and communication [ 20 ]. Team development interventions can also focus on problem solving which promotes synergy through encouraging team members to practice setting goals, developing interpersonal relations, clarifying team roles and working to improve organisational characteristics through participating in problem solving tasks. These types of team development interventions have the strongest and most consistent effects on affectively driven states that are critical to teams, such as psychological safety [ 20 ].
This systematic review of the literature will synthesise the content, theoretical underpinnings and outcomes of interventions which have been conducted to date to improve psychological safety and its related components, speaking up and voice behaviour, within a healthcare setting. Both efficacy and effectiveness outcomes will be considered. This review aims to answer the research questions: What interventions have been conducted to improve psychological safety, speaking up and voice behaviour within a healthcare setting? What are the underlying theoretical approaches in these interventions? How have these interventions been evaluated? Which interventions have been most effective for encouraging a climate of psychological safety? This will enable future research to build on what has been done before to create a reliable intervention for improving psychological safety in workplace teams.
A systematic review was used to explore the above research questions. Systematic reviews are an essential tool for synthesising the evidence from available studies to answer a specific research questions [ 21 , 22 , 23 , 24 ]. The Cochrane and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 23 , 24 , 25 ] have been followed in this review.
The protocol for this review has been published on Prospero (registration number: CRD42018100659). Since publishing this protocol, the following changes were made to the reivew:
The terms Speaking Up and Voice Behaviour were added to the title of the review in order to accurately capture the interventions reviewed. Originally, this review intended to examine interventions targeting psychological safety alone. However, given the limited number of interventions targeting psychological safety, the inclusion criteria were widened to include interventions targeting speaking up and voice behaviour.
After conducting the search, a large number of interventions conducted within a healthcare setting were identified. In addition, the literature highlighted the import role played by psychological safety, speaking up and voice in a healthcare setting. Therefore, the inclusion criteria for the setting of the interventions was narrowed from “no defined setting” to “within a healthcare setting”. As well as reflecting the body of literature found by this review, narrowing the setting allowed the review to explore the identified interventions in more detail and to consider their impact within a specific work setting.
The research question “how have these interventions been evaluated?” was added to the final version of this review in order to explore the ways in which each study assessed the impact of the intervention on psychological safety, speaking up and voice.
The inclusion criteria of the final review were updated to reflect the above changes.
Inclusion and exclusion criteria
Studies eligible for inclusion were peer reviewed, from any country, published between 1999 and 2018 and explored the development, implementation and/or evaluation of interventions relevant to psychological safety in healthcare settings. Given the limited number of interventions targeting psychological safety, the inclusion criteria were widened to include interventions targeting speaking up and voice behaviour.
Studies were excluded if they were not available in English or if they reported on interventions conducted outside healthcare settings.
Search strategy
The search strategy used key words identified through a scoping review of the literature. They were grouped together using the OR Boolean term. The resulting search strategy was reviewed by a researcher with extensive systematic review experience. The final search strategy was: “Psychological* safe*” OR “Speak* up” OR voic* OR silen*. The term “intervention” had been included in an earlier iteration but was excluded because it narrowed the search too much. A full search strategy can be found in Additional file 1 .
Information sources
Electronic databases were searched between the 19th of March 2018 and the 8th of June 2018 to find relevant studies (See search strings in online supplementary material). Electronic databases searched were: PsycINFO, ABI/Inform, Academic search complete and PubMed.
A grey literature search was conducted to supplement the above searches. Grey literature was identified by searching electronic databases which had a broad scope and the ability to conduct specific searches [ 26 , 27 ]. The databases searched were; OpenGrey, OCLC WorldCAT, Espace (Curtin’s institutional repository). In addition, the authors hand-searched the reference lists of included studies and contacted experts in the field to identify any eligible studies.
Study screening
Covidence, an online specialised systematic review website, was used to screen records. One reviewer screened titles and abstracts based on the eligibility criteria. When the eligible papers were identified, two reviewers independently reviewed each text. The reviewers met to discuss and resolve any conflicts or disagreements. An option to involve a third reviewer if agreement could not be reached was put in place but proved unnecessary, as following discussion, the original two reviewers reached agreement on all papers for inclusion.
Data extraction process
A data extraction template was developed to capture the relevant information from included studies. This template was based on the third version of guidelines produced by Cochrane in 2014 for data collection for intervention reviews of randomised control trials and non-randomised control trials and recommendations from Hoffmann and colleagues [ 28 ]. Information was collected for: aims, design, theoretical underpinnings, details of the intervention, participant information and outcomes. The final template can be seen in Additional file 2 .
Quality assessment
Depending on the study design, the Critical Appraisal Skills Programme [ 29 ] Qualitative Checklist, Cohort Study Checklist, or the Mixed Methods Appraisal Tool [ 30 ] were used to assess the quality of included studies.
Study synthesis
Given the heterogeneity in interventions and measures used in this review, a narrative approach to synthesis was deemed most appropriate [ 31 ]. Narrative synthesis relies on words and text to ‘tell the story’ of the included studies [ 31 ]. Based on guideline from Popay and colleagues [ 31 ], the narrative synthesis followed three iterative steps: organising studies into logical categories by becoming familiar with them, comparing them to one another and synthesising their findings; analysing the findings within each category by exploring relationships within and between the studies and synthesising data under the relevant themes.
Search result
The database search yielded 8947 studies and 11 grey literature studies were identified. After 5614 duplicates were removed, 3344 were screened. Three thousand one hundred forty-eight studies were excluded based on title and abstract screening, leaving 196 studies for full text screening. One hundred eighty-two full text articles were excluded, leaving 14 studies included in the review.
Figure 1 shows the PRISMA flow chart which summarises the screening stage of this review.
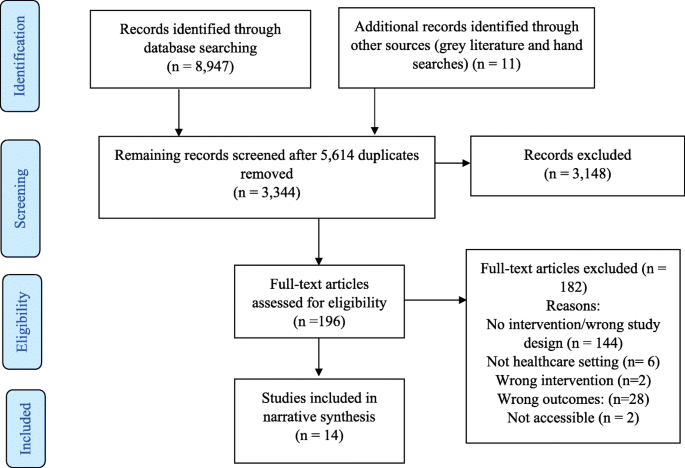
PRISMA flow diagram. This PRISMA flow diagram illustrates the inclusion and exclusion of identified studies
No study was excluded from the review based on quality assessment (see Additional file 3 ).
Included studies
A summary of included studies can be found in Additional file 4 : Tables S1, S2, S3, S4 and S5. They were divided into interventions using education and simulation ( n = 5), interventions using education and leadership videos ( n = 2), interventions using education and case studies ( n = 3), interventions using educational workshops alone ( n = 1) and non-educational interventions ( n = 3). All interventions are synthesised below.
Narrative synthesis
Interventions conducted to improve psychological safety or its related components.
Educational interventions and simulation exercises
Simulation exercises offer opportunities for developing skills without endangering the health of patients through placing them in situations that replicate real clinical practice [ 32 , 33 , 34 ]. The simulation exercises included in five educational interventions presented participants with opportunities to practice speaking up behaviour and were followed by group reflection and debriefing.
Both Pian-Smith and colleagues [ 35 ] and Raemer and colleagues [ 36 ] used simulation-based scenarios to present anaesthesiologists with opportunities to speak up to healthcare professionals (nurses, surgeons and anaesthesiologists). Both conducted educational workshops which introduced participants to tools for speaking-up (see Additional file 4 : Table S1). Pian-Smith and colleagues [ 35 ] found improvements in anaesthesiologists speaking up behaviours, however, Raemer and colleagues [ 36 ] found no statistically significant changes. Given that Pian-Smith and colleagues [ 35 ] explicitly told participants that there would be opportunities to practice speaking up, they had expected their scores to be much higher. Participants in both studies were less likely to speak up to a circulating nurse, suggesting a lack of appreciation of the role of circulating nurses. However, low levels of speaking up were also identified within the anaesthesiologist discipline, with only 25% of participants speaking up to their anaesthesiologist colleague [ 36 ].
Dufresne [ 37 ] simulated a critical incident for anaesthesia teams. They found that the debriefing leaders’ behaviour had a significant impact on the development of psychological safety. Specifically, when leaders balanced advocacy and inquiry language in the first 10 minutes of the debriefing, the team had lower psychological safety. There were also lower levels of psychological safety when the leader used negative evaluative statements. This suggests that, to cultivate psychological safety, leaders should avoid making early evaluative statements about team or individual performance. Further analysis also suggested when leaders showed they were willing to share their own insights, the team felt more psychologically safe. However, this finding did not reach significance.
Ginsburg and Bain [ 38 ] used simulation as part of their multifaceted intervention to promote speaking up behaviour and teamwork in an emergency department (ED). This intervention took place within the context of the hospital’s new Accountability Framework, which holds staff accountable to speak up in the face of unsafe or unprofessional behaviour. Participants were given the opportunity to practice speaking up techniques during role playing simulations and to take part in debriefing sessions, staff huddles and one to one meetings. While there was no significant difference between the ED and Intensive Care Unit (control group) at baseline, the teamwork climate score in the ED was significantly higher post intervention. This score included measures of “speaking up”, but these results were not reported separately.
Thomas and colleagues [ 39 ] used simulation to assess changes in team behaviours following an educational intervention. While the intervention focused on a variety of team behaviours, speaking up and voice inquiry, information sharing, and assertion were most relevant to this review. Participants completed a simulated resuscitation where they could use the behaviours they had been taught. Compared to the control group, the intervention group showed more incidents of inquiry, information sharing and assertion.
Leaders video presentations
Two educational interventions used video presentations to communicate leaders support for speaking up. O’Connor et al. [ 40 ] presented videos of attending physicians discussing situations they faced as interns where their communication and assertiveness skills were challenged. While their intervention had no significant effect on interns’ attitudes towards speaking up about stress or to seniors, the post-training group had significantly more positive attitudes towards speaking up to seniors than the pre-training group. Participants’ speaking behaviour was measured using standardised patient exercises, which showed no significant improvement.
Sayre and colleagues [ 41 ] used videos of senior staff expressing their expectation and support for nurses to speak up to remove any implicit sanctions against nurses speaking up. After the videos, participants discussed barriers to speaking up and developed action plans. The intervention group showed a significant improvement in speaking up survey scores and individual lists of nurse behaviours (see Additional file 4 : Table S2). There was no difference found in the control group.
Video presentations and case studies
Johnson & Kimsey [ 42 ] used video presentations of scenarios where there was a risk or an error to spark discussion. Like Pian-Smith [ 35 ] and Raemer [ 36 ] they introduced tools for speaking up. After the course, the majority (78%) of participants reported believing that they were better able to question decisions or actions of those in authority and were no longer afraid to ask questions (75%). As an objective measure, they found a marked decrease in the number of near misses or sentinel events requiring root cause analysis post training.
Coyle et al. [ 43 ] used video dramatization of a medical event and case studies of medical events that occurred in the study clinic to improve attitudes and behaviour related to medical event reporting. They also conducted educational conferences (see Additional file 4 : Table S3). According to questionnaires completed post intervention, there was no significant change in participants’ attitude and behaviour towards medical event reporting. However, those who participated in more conferences showed a more positive change in medical event reporting attitudes and behaviour.
Shapiro et al. [ 44 ] used video vignettes to encourage clinicians to discuss professional behaviour and the responsibility of bystanders to speak up. Participants were taught specific strategies for managing conflict and speaking up to colleagues who have behaved unprofessionally (see Additional file 4 : Table S3). Following this intervention, the number of reported concerns regarding professional behaviour increased across 3 years. Participants also reported that they were aware of their personal role in ensuring a culture of professionalism.
Educational workshops
Cave et al. [ 45 ] was the only intervention to educational workshops alone. They introduced the CENTRE tool to teams by providing education on the use of the guidelines. CENTRE is a tool which establishes guidelines to promote psychological safety by focusing on confidentiality, equal airtime and non-judgemental listening (see Additional file 4 : Table S4). While 17 health care group leaders have said that they found using CENTRE helpful, no formal assessment of this tool has been published to date. Further research is needed to test the effectiveness of this tool in promoting psychological safety.
Interventions without educational component
The studies which did not include an educational component all used different interventions and are discussed separately below.
Swahnberg and Wijma [ 46 ] used an intervention based on “forum play” (see Additional file 4 : Table S5) to understand staffs perceptions of Abuse in Health Care (AHC). Findings were particularly relevant to psychological safety as the intervention created an open climate where all staff felt comfortable discussing AHC. Staff shifted from being detached to having an emotional engagement with AHC. They saw acting against or speaking up about AHC as their responsibility and emphasised the critical role played by bystanders.
Brown and McCormack [ 47 ] used holistic facilitation to create psychologically safe spaces where nurses could explore their oppressed behaviours, helping them to discuss differences in opinions more openly within a multidisciplinary team. The facilitation sessions made ward leaders more aware of the role they played in creating a culture of psychological safety in their unit. This enabled the leaders to build trusting partnerships that permitted information and knowledge sharing which could help solve problems.
O’Leary [ 48 ] conducted action research meetings with two newly-formed interprofessional project teams. The supportive leadership style used by the author encouraged psychological safety within team meetings. However, psychological safety developed differently in each team. In the first team, a psychologically safe space developed, allowing them to share power and to co-generate knowledge. In the other team, psychological safety did not fully develop. The differences between the teams in this study were explained by the impact of organisational norms and stability in team membership, with organisational norms of shared decision making and a stable core group of team members supporting the development of psychological safety.
Interventions most effective at improving psychological safety and its related components
The diagram presented in Fig. 2 maps the relationships between the five categories of interventions and outcomes which are relevant to psychological safety.

Map of interventions categories, individual interventions review and relevant outcomes. This diagram maps the intervention categories, the studies grouped within them and the relationship between each intervention and key outcomes
As can be seen in Fig. 2 , mixed results were found for the impact of the interventions on outcomes related to psychological safety, speaking up and voice. Five studies [ 38 , 39 , 41 , 43 , 44 ] reported improved and three studies [ 35 , 40 , 43 ] found mixed results for “questioning, challenging, reporting or speaking up”. One further study [ 36 ] found no significant relationship. Three studies [ 39 , 46 , 47 ] reported improved and one study [ 48 ] found mixed results for “communication and collaboration” following interventions. Five studies [ 38 , 40 , 42 , 44 , 45 ] reported positive evaluations by participants post-interventions. Three studies had “Psychological safety” as an outcome, with one of these reporting mixed results for the impact of the intervention on psychological safety [ 48 ] and the other two reporting improvement [ 37 , 47 ]. Mixed results were found for the impact of one intervention on “power sharing” [ 48 ]. Lastly, one study [ 46 ] showed a positive impact of the intervention on creating an “open climate” and another showed improvement in “trusting relationships” [ 47 ].
This review examined educational and non-educational interventions which targeted psychological safety, speaking up and voice behaviour. The outcomes from these studies were mixed. These mixed results limit our ability to accurately answer the research question: “Which interventions have been most effective for encouraging a climate of psychological safety?”. However, the results of this review highlight areas where further research is needed to improve our understanding of the efficacy or effectiveness of interventions targeting psychological safety, speaking up and voice.
Emerging themes and issues for future research
Limitations of educational interventions.
Educational interventions identified challenges related to changing deeply rooted speaking up behaviours and questioned whether education alone is sufficient [ 35 , 36 ]. Implementation science literature suggests that education alone is insufficient for changing behaviour and that it is necessary to have a context which is receptive to change and appropriate facilitation [ 47 , 49 ]. The limitations associated with educational interventions may explain the mixed outcomes from studies in this review. Some educational studies suggested that there would have been more improvement if interventions had been conducted over a longer period of time [ 38 , 41 ] and O’Leary [ 48 ] highlights how having core team members who are meeting regularly supported the development of psychological safety. These findings suggest that educational interventions may benefit from more regular, longitudinal and multifaceted interventions for improving psychological safety, speaking up and voice.

Measuring outcomes
This review identified issues with outcome measurement. Although the simulated scenarios used were as close as possible to reality, they are limited by participants’ awareness that they are not in a real clinical environment. This perception of scenarios realism may affect participants’ behaviour particularly within a healthcare context, when issues of patient safety arise. However, the results from the simulated scenarios made an important contribution to the evidence in this review by providing behavioural evidence of changes relevant to psychological safety, speaking up and voice. This evidence was missing from studies which used questionnaire and survey measures, which were limited by the potential for self-report bias.
According to Shuffler et al. [ 19 ] team building interventions, such as the ones reviewed here, are often judged subjectively by collecting data on participants perceptions of the interventions value. However, in order to fully understand if interventions are successful, more objective measures are needed. This is particularly true for interventions targeting psychological safety. Only three interventions reviewed here evaluated psychological safety as an outcome. While other interventions may have been effective in improving psychological safety, no measure was taken to verify this. There is a need to develop more objective ways of assessing the effectiveness of interventions targeting psychological safety. For example, the observational scheme developed by Hoenderdos et al. [ 50 ] provides a more objective measure of psychological safety. However, this measure has not yet been adapted for a healthcare context and further validation is needed. Future research should focus on developing more objective measures for assessing changes in psychological safety and its related behaviours in order to fully understand the effects of interventions.
Levels of intervention
Many of the interventions reviewed here were team level interventions, however, O’Leary [ 48 ] demonstrated the impact of factors at the organisational level by showing that it is difficult to develop psychological safety within organisations where shared decision making is not an organisational norm. In order for future research to develop effective interventions, they should target the organisational level, as well as the team level.
Who should participate in the intervention?
Studies in this review highlighted the importance and relevance of psychological safety, speaking up and voice behaviour within interdisciplinary teams [ 35 , 36 , 44 , 47 , 48 ]. This highlights the need for future interventions to address psychological safety, speaking up and voice behaviour across and between all disciplines. Studies also illustrated the need to involve team members in the development of interventions. Effective team building interventions ensure that team members contribute their knowledge of the team’s needs to inform the design of the intervention [ 19 ]. Four interventions in this review engaged with participants as part of the development stage of their intervention to ensure the intervention was grounded in reality of the participants work environment [ 43 , 46 , 47 , 48 ]. However, other studies delivered pre-designed interventions that were not based on the needs of the participants. Adopting a co-design approach, where researchers and end-users collaborate in designing the intervention, can ensure that future interventions are tailored to teams needs. A study protocol published by Ward et al. outlines plans to work with key stakeholders, staff and patient representatives to co-design an intervention to create a culture of medical professionalism in relation to patient safety. Future research should ensure that participants are involved in the development stages on interventions, to ensure that the intervention is grounded in the team’s needs.
Lastly, team leaders play a key role in creating psychologically safe teams and should be involved in interventions [ 1 ]. In line with this, key stakeholders and leaders were involved in many of the studies reviewed here, either as a participant in the study or in facilitating the interventions. Leaders were involved in interventions through their behaviour facilitating psychological safety [ 37 , 48 ] or through showing their support and commitment to the intervention [ 38 , 40 , 41 , 47 ]. Since the search for this systematic review was conducted, a case study intervention focused on understanding voice and improving the response to disruptive behaviours has been published by Dixon-Woods et al. Leaders played a key role within this case study by becoming more open and willing to listen and to take staff concerns on board and by completing training in skills for encouraging voice and having difficult conversations. The interventions reviewed here, along with the recent paper by Dixon-Woods et al., highlight the important role leaders play in the success of interventions. This suggests that future research should ensure that key stakeholders and leaders are engaged with interventions in order to create a supportive environment that facilitates change.
Strengths and limitations
In order to minimise the risk of publication bias, searches were conducted on academic and grey literature databases as well as through contacting experts. In addition, the eligibility of the included papers were independently screened by two reviewers.
Given the lack of interventions focused on psychological safety, the scope of this review was widened to included speaking up and voice behaviour. This allowed the review to gain a broader view of how interventions could be used to improve behaviours related to psychological safety. While these behaviours are strongly associated with psychological safety, the phenomenon of psychological safety is also associated with a variety of other concepts, including communication, decision making, team performance, team learning and divergent thinking. However, examining interventions which targeted each of these related concepts was beyond the scope of this review.
This review is the first systematic review to examine interventions to improve psychological safety, speaking up and voice behaviour in healthcare teams. The mixed results found suggest a need to improve the effectiveness or efficacy, and measurement of these interventions. Longitudinal and multifaceted interventions may allow future studies to further investigate the efficacy or effectiveness of these interventions. In addition, the development and use of more objective measures may allow future studies to understand whether interventions are successful in improving psychological safety. Based on the identification of the successful elements of the interventions reviewed here, it is suggested that future intervention studies test the impact of these elements by involving end users in the design phase, target both group and organisational levels, ensure visible leader support and work across and within interdisciplinary teams.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
Abuse in Health Care
Audience Response System
Confidentiality, Equal airtime, Non-Judgemental (respectful) listening, Timeliness, Right to pass, Engaged
Chief Nursing Officer
Centre for Professionalism and Peer Support
Crew Resource Model
Concerned, Uncomfortable, Stop
Describe, Express, Suggest, Consequences
Emergency Department
Neonatal Resuscitation Program
Obstetrics/gynocology
Online Computer Library Center
Promoting Action of Research Implementation in Health Service
Preferred Reporting of Items for Systematic Reviews and Meta-Analysis
Situation, Background, Assessment, Recommendation
Team Strategies and Tools to Enhance Performance and Patient Safety
World Health Organisation
Edmondson A. Psychological safety and learning behavior in work teams. Adm Sci Q. 1999;44(2):350–83.
Article Google Scholar
Edmondson AC, Lei Z. Psychological safety: The history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23–43.
Newman A, Donohue R, Eva N. Psychological safety: A systematic review of the literature. Hum Res Manag Rev. 2017;27(3):521–35.
Google Scholar
Singer S, Edmondson A. Confronting the tension between learning and performance. Reflect The SoL J. 2012;11(4):34–43.
Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav. 2006;27(7):941–66.
Rathert C, Ishqaidef G, May DR. Improving work environments in health care: test of a theoretical framework. Health Care Manag Rev. 2009;34(4):334–43.
Moore L, McAuliffe E. To report or not to report? Why some nurses are reluctant to whistleblow. Clin Gov. 2012;17(4):332–42.
Moore L, McAuliffe E. Is inadequate response to whistleblowing perpetuating a culture of silence in hospitals? Clin Gov. 2010;15(3):166–78.
Edmondson AC. Speaking up in the operating room: how team leaders promote learning in interdisciplinary action teams. J Manag Stud. 2003;40(6):1419–52.
Edmondson AC, Higgins M, Singer S, et al. Understanding psychological safety in health care and education organizations: a comparative perspective. Res Hum Dev. 2016;13(1):65–83.
Pearsall MJ, Ellis AP. Thick as thieves: the effects of ethical orientation and psychological safety on unethical team behavior. J Appl Psychol. 2011;96(2):401.
Article PubMed Google Scholar
Bienefeld N, Grote G. Speaking up in ad hoc multiteam systems: Individual-level effects of psychological safety, status, and leadership within and across teams. Eur J Work Organ Psychol. 2014;23(6):930–45.
Leroy H, Dierynck B, Anseel F, et al. Behavioral integrity for safety, priority of safety, psychological safety, and patient safety: a team-level study. J Appl Psychol. 2012;97(6):1273.
Brinsfield CT. Employee silence motives: investigation of dimensionality and development of measures. J Organ Behav. 2013;34(5):671–97.
Detert JR, Edmondson AC. Implicit voice theories: taken-for-granted rules of self censorship at work. Acad Manag J. 2011;54:461–88.
Kish-Gephart JJ, Detert JR, Treviño LK, et al. Silenced by fear: The nature, sources, and consequences of fear at work. Res Organ Behav. 2009;29:163–93.
Morrison EW, Milliken FJ. Organizational silence: a barrier to change and development in a pluralistic world. Acad Manag Rev. 2000;25(4):706–25.
Beer M, Eisenstat RA. The silent killers of strategy implementation and learning. Sloan Manage Rev. 2000;41(4):29.
Shuffler ML, Diazgranados D, Maynard MT, et al. Developing, sustaining, and maximizing team effectiveness: an integrative, dynamic perspective of team development interventions. Acad Manag Ann. 2018;12(2):688–724.
Article PubMed PubMed Central Google Scholar
Tannenbaum SI, Beard RL, Salas E. Team building and its influence on team effectiveness: an examination of conceptual and empirical developments. North Holland Adv Psychol. 1992;82:117–53.
Khan K, Kunz R, Kleijnen J., et al. Systematic reviews to support evidence-based medicine: Crc press 2011.
Kitchenham B. Procedures for performing systematic reviews, vol. 33. Keele: Keele University; 2004. p. 1–26.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Moher D, Liberati A, Tetzlaff J, et al. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Wiley Online Library; 2008.
Book Google Scholar
Godin K, Stapleton J, Kirkpatrick SI, et al. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Rev. 2015;4(1):138.
Oliver KB, Swain R. Directories of institutional repositories: research results & recommendations. 72nd IFLA general conference and council; 2006. p. 20–4.
Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Critical Appraisal Skills Programme. CASP Qualitative, Cohort Study and Randomised Controlled trial Checklist. 2018. Available at: https://casp uk.net/casptools-checklists/ Accessed: 20/03/2018.
Pluye P, Robert E, Cargo M, Bartlett G, O’Cathain A, Griffiths F, Boardman F, Gagnon MP, & Rousseau MC. Proposal: A mixed methods appraisal tool for systematic mixed studies reviews. 2011. Retrieved on [20/03/2018] from http://mixedmethodsappraisaltoolpublic.pbworks.com . Archived by WebCite ® at http://www.webcitation.org/5tTRTc9yJ
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version, vol. 1; 2006. p. b92.
Hovancsek MT. Using simulation in nursing education. Simulation in nursing education: From conceptualization to evaluation; 2007. p. 1–9.
Murray DJ, Boulet JR, Kras JF, Woodhouse JA, Cox T, McAllister JD. Acute care skills in anesthesia PracticeA simulation-based resident performance assessment. Anesthesiology. 2004;101(5):1084–95.
Issenberg SB, McGaghie WC, Hart IR, Mayer JW, Felner JM, Petrusa ER, Waugh RA, Brown DD, Safford RR, Gessner IH, Gordon DL. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282(9):861–6.
Article CAS PubMed Google Scholar
Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, Raemer D. Teaching residents the two-challenge rule: a simulation-based approach to improve education and patient safety. Simul Healthc. 2009;4(2):84–91.
Raemer DB, Kolbe M, Minehart RD, et al. Improving anesthesiologists’ ability to speak up in the operating room: a randomized controlled experiment of a simulation based intervention and a qualitative analysis of hurdles and enablers. Acad Med. 2016;91(4):530–9.
Dufresne RL. Learning from critical incidents by ad hoc teams: the impacts of team debriefing leader behaviors and psychological safety: Unpublished dissertation. Boston: Boston College; 2007.
Ginsburg L, Bain L. The evaluation of a multifaceted intervention to promote “speaking up” and strengthen interprofessional teamwork climate perceptions. J Interprof Care. 2017;31(2):207–17.
Thomas EJ, Taggart B, Crandell S, et al. Teaching teamwork during the Neonatal Resuscitation Program: a randomized trial. J Perinatol. 2007;27(7):409.
O’Connor P, Byrne D, O’Dea A, et al. “Excuse me:” teaching interns to speak up. Jt Comm J Qual Patient Saf. 2013;39(9):426–31.
Sayre MM, McNeese-Smith D, Leach LS, et al. An educational intervention to increase “speaking-up” behaviors in nurses and improve patient safety. J Nurs Care Qual. 2012;27(2):154–60.
Johnson HL, Kimsey D. Patient safety: break the silence. AORN J. 2012;95(5):591–601.
Coyle YM, Mercer SQ, Murphy-Cullen CL, et al. Effectiveness of a graduate medical education program for improving medical event reporting attitude and behavior. BMJ Qual Saf. 2005;14(5):83–8.
Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf. 2014;40(4):168–AP1.
Cave D, Pearson H, Whitehead P, Rahim-Jamal S. CENTRE: creating psychological safety in groups. Clin Teach. 2016;13(6):427–31.
Swahnberg K, Wijma B. Staff’s perception of abuse in healthcare: a Swedish qualitative study. BMJ Open. 2012;2(5):e001111.
Brown D, McCormack B. Exploring psychological safety as a component of facilitation within the promoting action on research implementation in health services framework. J Clin Nurs. 2016;25(19–20):2921–32.
O’Leary DF. Exploring the importance of team psychological safety in the development of two interprofessional teams. J Interprof Care. 2016;30(1):29–34.
Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–5.
Hoenderdos JW. Towards an observational measure for team psychological safety: Unpublished thesis. Enschede: University of Twente; 2013.
Download references
Acknowledgements
Not applicable.
This research is funded by the Irish Research Council and the Ireland East Hospital Group under the Employment Based Partnership Scholarship. The funding body did not play a role in the study design, data collection, analysis and interpretation of data or in the writing of the manuscript.
Author information
Authors and affiliations.
UCD School of Nursing, Midwifery & Health Systems, UCD Health Sciences Centre, University College Dublin, Dublin 4, Ireland
Róisín O’Donovan & Eilish McAuliffe
You can also search for this author in PubMed Google Scholar
Contributions
Both authors were involved in the design and planning of this systematic review. ROD completed title and abstract screening. Both authors completed full text screening. ROD completed data extraction. ROD drafted the manuscript and EMcA contributed to writing and revising the paper. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Róisín O’Donovan .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Search Strategy. Search strategies presented for each database searched.
Additional file 2.
Data Extraction Template. The categories by which data was extracted from excluded studies are presented in the final template.
Additional file 3.
Quality Assessment. The results of the quality assessment conducted are presented according to study design. The Critical Appraisal Skills Programme Qualitative Checklist, Cohort Study Checklist, or the Mixed Methods Appraisal Tool are presented.
Additional file 4.
Summaries of included studies. Each table includes summary details of all interventions included in the review. Details are listed under the following titles: Author, Aims, Participants, Intervention Duration, Intervention Content, Methods of Evaluation, Key Findings.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
O’Donovan, R., McAuliffe, E. A systematic review exploring the content and outcomes of interventions to improve psychological safety, speaking up and voice behaviour. BMC Health Serv Res 20 , 101 (2020). https://doi.org/10.1186/s12913-020-4931-2
Download citation
Received : 02 May 2019
Accepted : 27 January 2020
Published : 10 February 2020
DOI : https://doi.org/10.1186/s12913-020-4931-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological safety
- Speaking up
- Voice behaviour
- Interventions
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
What Is Psychological Safety?

A culture of trust and belonging doesn’t just happen. Here’s how you make one.
What exactly is psychological safety? It’s a term that’s used a lot but is often misunderstood. In this piece, the author answers the following questions with input from Harvard Business School professor Amy Edmondson, who coined the phrase “team psychological safety”: 1) What is psychological safety? 2) Why is psychological safety important? 3) How has the idea evolved? 4) How do you know if your team has it? 5) How do you create psychological safety? 6) What are common misconceptions?
No one likes to deliver bad news to their boss. But that’s exactly what I had to do when a project I’d been working on wasn’t delivering the results we expected. I’d been a big advocate for our team taking on the initiative and, personally, I’d invested a lot of time into it — and convinced others to do the same.
- Amy Gallo is a contributing editor at Harvard Business Review, cohost of the Women at Work podcast , and the author of two books: Getting Along: How to Work with Anyone (Even Difficult People) and the HBR Guide to Dealing with Conflict . She writes and speaks about workplace dynamics. Watch her TEDx talk on conflict and follow her on LinkedIn . amyegallo
Partner Center
- Open access
- Published: 06 June 2024
How does psychosocial safety climate cross-level influence work engagement and job burnout: the roles of organization-based self-esteem and psychological detachment
- Tongshuang Yuan 1 na1 ,
- Hui Ren 2 na1 ,
- Xin Yin 2 ,
- Leilei Liang 1 ,
- Junsong Fei 1 ,
- Xiaoying Liu 1 ,
- Chengbin Zheng 1 ,
- Huimin Wang 1 ,
- Jiaying Gao 1 ,
- Songli Mei ORCID: orcid.org/0000-0003-1815-8255 1 &
- Hongyan Li 3
BMC Nursing volume 23 , Article number: 389 ( 2024 ) Cite this article
120 Accesses
Metrics details
Existing researches on nurses’ work engagement and job burnout have mostly stayed at the individual level, and limited researches test the cross-level effects of psychosocial safety climate (PSC). The study aimed to explore the cross-level mediating effect of organization-based self-esteem (OBSE) and the moderating effect of psychological detachment between the relationship of PSC and work engagement and job burnout in nurses.
The cross-sectional study was conducted during November to December 2022 at a tertiary hospital in a northeastern province of China. Data was collected from 1832 nurses through an online questionnaire. Correlation analyses and hierarchical linear modeling were used to test study hypotheses.
The results showed that PSC was positively associated with work engagement, and negatively associated with job burnout. OBSE mediated the effect of PSC on work engagement, as well as job burnout. Additionally, psychological detachment played a moderating role between PSC and work engagement, but no moderating effect was found between PSC and job burnout.
Conclusions
PSC at the organizational level increases work engagement and reduces job burnout by stimulating nurses’ high levels of OBSE. Psychological detachment, as a situational factor, enhances the positive influence of PSC on work engagement. The implementation of measures to improve the PSC levels of the organization, and the levels of OBSE and psychological detachment among nurses could help to promote their good work performance.
Peer Review reports
Introduction
As the largest group of health care professionals, nurses are essential participants in achieving high quality care and positive health outcomes in patients [ 1 ]. Safeguarding the quality of care and increasing the nurses’ willingness to stay in the workforce are important to support people’s health and well-being, and to safeguard the stability and growth of health care systems. Work engagement has grown in prevalence over the past 25 years as an important predictor of job performance and outcomes [ 2 ]. Work engagement is a state of individuals’ continuous, positive emotional activation related to work, characterized by three aspects: vitality, dedication and concentration [ 3 ]. Previous studies results point out that work engagement is closely related to nurses’ psychological, physical, behavioral and organizational outcomes, such as reducing psychological disorders, reducing work errors, improving nursing services, reducing their tendency of leaving, and increasing the economic benefits of hospitals [ 4 ].
Simultaneously, increased work demands and inadequate work resources cause nurses to be negatively affected by work-related stressors for long duration and increase the incidence of job burnout [ 5 ]. A meta-analysis showed that the global incidence of nurses’ burnout is high and on an upward trend, and that the COVID-19 pandemic has led to an increase in the upward trend [ 6 ]. Job burnout refers to a syndrome involving emotional exhaustion, dehumanization and diminished accomplishment under prolonged work stress [ 7 ]. Higher levels of burnout could lead to various mental and physical health problems in nurses such as anxiety, depression, insomnia, headaches, and chest pain. Meanwhile, when nurses suffer from high level of burnout, patient safety and quality of care decline and the intention of leaving increases [ 8 , 9 ]. Given the significant impacts of work engagement and job burnout on individual and organizational outcomes, it is critical to explore the factors that promote work engagement and reduce job burnout among nurses in healthcare settings.
However, existing researches on nurses’ work engagement and job burnout have mostly stayed at the individual level. Kacey Keyko et al. proposed the Nursing Job Demands-Resources for nursing practice, which emphasized the vital influence of organizational-level factors on nurses’ physical and psychological health, job performance and nursing outcomes [ 10 ]. Psychosocial safety climate (PSC), as a key resource at the organizational level, has attracted a lot of attentions. PSC refers to policies, practices and procedures established by the organization regarding employees’ psychological health and safety in the course of their work [ 11 ]. PSC has been shown to be strongly associated with employees’ physical and mental health, work attitudes, and job performance, and is more strongly correlated with psychological health outcomes such as burnout than other organizational measures [ 12 , 13 ]. Given the challenges and stresses nurses face in their work environments, our study aimed to better understand how to promote work engagement and prevent job burnout, and to use the PSC as an important organizational resource to achieve this goal in order to further consider promoting positive work outcomes by focusing on the mental health and safety of nurses. However, limited researches test the cross-level effects of PSC on work engagement and job burnout, and there are also unknown factors in the mediating mechanisms of the above relationship, such as from the perspective of individuals’ resources, i.e., organization-based self-esteem (OBSE). Furthermore, the influence of PSC on work engagement and job burnout may have boundary conditions. It is necessary to explore in depth the moderating effect of individual characteristics (psychological detachment) in the PSC’s influence mechanism from the perspective of human-environmental interaction. Based on this, the present study constructed a cross-level model of PSC at the organizational level affecting nurses’ work engagement and job burnout, used OBSE as a mediator to further clarify its mechanism, and focused on the moderating effect of psychological detachment in the above relationships. In order to provide theoretical guidance for the implementation of measures to promote PSC in organizations to enhance nurses’ mental health and work performance. In summary, the model for this study is shown in Fig. 1 .

Theoretical model
PSC and work engagement, as well as job burnout
PSC was included in the Job Demands-Resources (JD-R) model as an antecedent variable that affected job characteristics and it was considered as an active organizational variable acting on health-impairment process and motivational process [ 14 ]. In a high PSC context, people’s mental health goals are valued, supported, committed and prioritized by senior managers [ 15 , 16 ]. Correspondingly, multiple resources are provided to employees, thus facilitating them access to more conditional, individual, and workplace resources. Individuals can use these resources to regulate their own emotional responses, thereby alleviating the negative impact of various stressors in the work environment. Consequently, the prevalence of job burnout and mental health problems will be reduced, and individuals’ work engagement would be increased. In addition, according to social exchange theory (SET) [ 17 ], when an organization cares for members’ mental health and well-being through rational allocation of resources and priority management, members would fully perceive the organization’s support. Based on the reciprocity’s principle, individuals will have a sense of obligation to reciprocate. In exchange, they will reward the organization with more positive attitudes and behaviors, which could elevate organizational commitment and work engagement. Taken together, we propose the hypotheses that:
H1a. PSC at the organizational level is positively related to work engagement.
H1b. PSC at the organizational level is negatively related to job burnout.
PSC and OBSE
Self-esteem, as a component of the self-concept, reflects the perception of the self and encompasses both evaluation and cognitive orientation. People with high self-esteem generally have more positive views and feelings about themselves and have a higher sense of “self-liking” [ 18 ]. OBSE reflects individual’s self-esteem in the specific area of work and organizational environment, and is the self-judgement on one’s own value, ability, and importance in the organization [ 19 ]. OBSE is highly situational in nature, and it has been shown that that performance feedback, organizational climate, managerial roles and related behaviors can all affect OBSE [ 20 ]. When the health and well-being of employees is a priority for the organization, that is, in the case of a high level of PSC, managers usually keep work demands within limits and increase work resources to reduce the negative impact of factors such as work stress on employees [ 12 ]. As a result, nurses perceive that they are valued by the organization and may make judgments that their work behaviors and outcomes are affirmed by the organization. Such information is incorporated into their self-perceptions, allowing them to form their own positive evaluations of the organization as having value and competence. Therefore, we hypothesize that:
H2: PSC at organizational level is positively related to OBSE.
Mediating effect of OBSE
Combined with H2, when nurses perceive high levels of PSC, their OBSE levels increase. When nurses perceive that their mental health and safety is important to management and the organization, their positive emotions and motivation increase. And PSC plays a role in reducing work demands and improving work resources [ 12 ], as a result, nurses perceive that the organization values and recognizes them and tend to positively evaluate their value in the organization, and their OBSE levels are enhanced. When people actively evaluate their values in the organization, the organizational identity becomes the content of the constructed self-concept and an important component of the self-concept system [ 21 ]. The consistency theory assumes that people are motivated to achieve conjunctions that are consistent with their self-concept [ 22 ]. Nurses with high OBSE levels maintain consistency in self-evaluation through a series of positive behaviors and responses, which in turn could maintain or even increase them self-esteem levels in the organization and achieve the maintenance of positive self-concept [ 23 , 24 ]. Based on this, nurses tend to be more willing to put in work and demonstrate more positive efforts and enthusiasm to strengthen their self-perception and value. Conversely, nurses would align their self-perception by exhibiting pessimistic work-related attitudes and behaviors. Eventually, nurses’ work commitment would be undermined and the risk of job burnout would increase. In addition, according to Conservation of Resource Theory (COR) [ 24 ], OBSE, as an individual resource, can motivate individuals to work and thus increase their levels of work engagement. The higher levels of OBSE, the higher quality sense of meaning, security, and access they experience in their work role engagement, which in turn shows higher levels of work engagement and lower levels of job burnout. And, high levels of OBSE would help nurses build and access more resources that would further contribute to their positive psychological experiences at work and reduce job burnout levels. Accordingly, we propose the hypotheses that:
H3a. OBSE mediates the relationship between PSC and work engagement.
H3b. OBSE mediates the relationship between PSC and job burnout.
Moderating effect of psychological detachment
Psychological detachment refers to a state in which people is temporally, spatially, and psychologically detached from work after work time, is not disturbed by work-related matters, and stops thinking about work-related issues [ 25 ]. Work engagement is a positive emotional state that lasts for a long time and requires the consumption physical and psychological resources. The effort-recovery model revealed that people responded to work demands through effortful behaviors which depleted their resources, so that short breaks allow their physical and mental systems to recover properly. Psychological detachment has been found to reduce energy expenditure and allow people to acquire new resources and perspectives form other activities, so they can return to work with better state [ 26 ]. Conversely, nurses who cannot detach from work and continue to devote time and energy to work-related tasks after working hours. This will lead to further depletion of personal resources and elevated emotional exhaustion, and harder to adequate recovery [ 25 ]. On this basis, we propose that,
H4a. Psychological detachment moderates the relationship between PSC and work engagement.
H4b. Psychological detachment moderates the relationship between PSC and job burnout.
Study design
The study data was collected from a tertiary hospital in a northeastern province of China during November to December 2022, collected through cluster sampling procedures. 1,832 nurses from 17 departments (such as obstetrics and gynecology, oncology, pediatrics, and intensive care unit) participated in the survey.
Participants and procedure
First, we contacted the head of the nursing department and relevant administrators to illustrate the purpose and procedures of the investigation. After obtaining their consent, electronic questionnaires were created and distributed through the ‘Questionnaire Star platform’. The platform enables online survey for data collection and download. Once the online questionnaire was created, the head of nursing department forwarded the information and the QR code of the investigation to chief nurses via the WeChat group, who then distributed the questionnaire to the WeChat groups of nurses in each department. Nurses were fully aware of study purpose and procedures and chose to participate voluntarily. The survey was conducted anonymously to fully protect the privacy of the participants. Online informed consent was obtained from all participants.
A total of 1868 questionnaires were received in the current study, and 1832 questionnaires were collected ultimately after deleting those with missing key variables, obvious regular answers or repeated answers, with a valid recovery rate of 98.07%. The survey collected more than half of the hospital’s nurse population and the basic demographic characteristics of the nurses surveyed were similar to those of the total population. The average age of participants was 35.11 (SD = 6.10) years old. The study was carried out in accordance with the Helsinki Declaration as revised 1989, and the study protocol was approved by the Institutional Review Board of the School of Public Health, Jilin University.
Measurements
PSC was assessed by the 12-item psychosocial safety climate scale (PSC-12), which contains four subscales: management commitment, organizational communication, management priority, and organizational participation [ 27 ]. The Chinese version PSC-12 had good reliability and validity [ 28 ]. Each item was rated on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The total score was the sum of four subscales, with higher score values indicating higher levels of PSC. The Cronbach’s α coefficient in this study was 0.97.
The Organization-Based Self-Esteem (OBSE) Scale developed by Pierce was used to measure the level of self-esteem at work [ 29 ]. An example item was “I am valuable around here”. The total four items were rated on a 5-point Likert scale, from 1 (strongly disagree) to 5 (strongly agree). The OBSE scale was proved to be a reliable and valid instrument [ 30 ]. The Cronbach’s α coefficient in this study was 0.88.
- Work engagement
The 3-item short version scale developed by Christian et al. was utilized to measure work engagement [ 31 ]. Three items were as follows: “I was enthusiastic in my job today” (emotional engagement), “I was absorbed by my job today” (cognitive engagement), and “I exerted my full effort on my job today” (physical engagement). The answers to each item were rated on a 5-point Likert scale varying from 1 (strongly disagree) to 5 (strongly agree). The Cronbach’s α coefficient in this study was 0.89.
- Job burnout
Job burnout was measured by the 10-item burnout subscale from the Professional Quality of Life (ProQOL) Scale developed by Stamm [ 32 ]. An example question was “I have happy thoughts and feelings about the people I help and how I can help them”. Items were rated on a 5-point Likert scale ranging from 1 (no) to 5 (always). The scale has shown good validity and reliability in previous research [ 33 ]. The Cronbach’s α coefficient in this study was 0.71.
Psychological detachment
Four items associating with psychological detachment derived from the recovery experience questionnaire were used to assess the psychological detachment [ 34 ]. The scale was widely used to measure the degree of psychological detachment [ 35 ]. Each item was responded with a 5-point Likert scale, ranging from1 (strongly disagree) to 5 (strongly agree). The Cronbach’s α coefficient in this study was 0.85.
Control variables
Demographic information, including gender (1 = “male”; 2 = “female”), age (1 = “≤30”; 2 = “31–40”; 3 = “>40”), education level (1 = “junior college or below”; 2 = “bachelor degree”; 3 = “master degree or above”), and monthly income (yuan) (1 = “≤6000”; 2 = “6001–8000”; 3 = “8001-10,000”; 4 = “>10,000”), and work-related variables, including technical title (1 = “none”; 2 = “nurse”; 3 = “senior nurse”; 4 = “supervisor nurse”; 5 = “co-chief nurse”; 6 = “chief nurse”), working years (1 = “≤4”; 2 = “5–9”; 3 = “10–14”; 4 = “≥15”), working time (hours)/week (1 = “≤40”; 2 = “41–45”; 3 = “>45”), and night shift (times)/week (1 = “0”; 2 = “1–2”; 3 = “3–4”; 4 = “≥5”) were measured as control variables. This is because these variables have been shown to potentially influence the hypothesized relationships in this study [ 36 , 37 ]. Therefore, the inclusion of these variables helps to control for external factors that may have an impact on the results, thus allowing for a more accurate examination of the relationship between the study variables.
Statistical analysis
In this study, the data analyses and hypotheses testing were conducted using the SPSS 24.0, Hierarchical Liner Modeling 6.08 and R 4.1.0. First, descriptive statistics and Pearson correlations were used to analyze the characteristics of the sample and the relationship between all study variables. Second, considering the study variables involve both individual level and organizational level, hierarchical linear modeling was used for hypothesis testing. Hierarchical linear modeling is a linear statistical analysis method for multi-layer nested structured data, capable of processing data from different levels simultaneously. In the present study, the level 2 represented data at the organizational level and the level 1 represented data at the individual level. The study used R-Mediation to calculate the 95% confidence interval (CI) of the mediating effect [ 38 ]. Statistical significance was defined as a two-tailed p -value smaller than 0.05.
Common method bias test
The results showed that six factors with eigenvalues greater than 1 were extracted. The variance explained by the first factor was 39.45%, which was below the threshold of 50% [ 39 ]. The result indicated no serious common method bias in the measurements.
Results of descriptive statistics and correlations
Table 1 displays the means, standard deviation, and correlation coefficients of the studied variables. The results showed that all the control variables were significantly associated with work engagement and job burnout ( p <0.05). PSC was significantly and positively correlated with OBSE and work engagement ( r = 0.499, 0.512, p <0.001), and negatively correlated with job burnout ( r =-0.477, p <0.001). OBSE was significantly and positively correlated with work engagement ( r = 0.812, p <0.001), and negatively correlated with job burnout ( r =-0.566, p <0.001). Psychological detachment was significantly and positively correlated with work engagement ( r = 0.092, p <0.001), and negatively correlated with job burnout ( r =-0.081, p <0.01).
Aggregation statistics
PSC, an organizational-level variable derived from multiple evaluations on nurses at the individual level, should be aggregated to the organizational level in the actual analysis. R wg and two intraclass correlation coefficients (ICC) were calculated, and used to determine the aggregation’s reasonableness of individual-level data to organization-level data. R wg was used to confirm whether the data of each department has high intraclass consistency [ 40 ], and in general, R wg value should be greater than 0.70 [ 41 ]. ICC(1) examines whether there is sufficient between-group variation in the variable, with a larger value representing greater variation between groups, and ICC(1) is usually required to be greater than 0.059 [ 42 ]. ICC(2) indicates the organizational variables’ reliability after aggregation of individual variables to the organizational level, and ICC(2) should be greater than 0.70 [ 42 ]. In this study, the mean and median R wg of PSC were 0.78 and 0.76, respectively, indicating a high intraclass consistency of the survey data. ICC(1) and ICC(2) were 0.06 and 0.87, respectively, indicating that the survey data had good intraclass stability and variability, thus supporting the effective aggregation of PSC from the individual level to the organizational level.
Hypotheses testing
The direct effects of PSC on OBSE, work engagement, and job burnout at the individual level all involved cross-level relationships, so three null models needed to be construct. ICCs were 0.066, 0.104 and 0.082 of OBSE, work engagement and job burnout, respectively, in accordance with the judgment criteria of ICC (1) greater than 0.059 (see supplementary material table S1 ). The between-group differences in OBSE (F = 5.018, p < 0.001), work engagement (F = 6.108, p < 0. 001), and job burnout (F = 6.422, p < 0.001) were significant, thus requiring a cross-level analysis to examine the between-group differences in the above variables.
The study used hierarchical linear modeling to verify the cross-level mediating effect, and the variables other than the dependent variables were group-mean centered. The results are shown in Table 2 . After controlling for demographic information and work-related variables, there was a positive relationship between PSC and work engagement (M3, γ = 0.828, p <0.001). Thus, H1a was supported. PSC was positively associated with OBSE (M1, γ = 0.630, p <0.001). Thus, H2 was supported. OBSE was positively correlated with work engagement (M2, γ = 0.858, p <0.01). OBSE had a significant positive effect on work engagement when it entered M4 (M4, γ = 0.845, p < 0.001), while the coefficient of significant effect of PSC on work engagement decreased from 0.828 to 0.259, with OBSE partially mediated the relationship between PSC and work engagement. Furthermore, the result of the Monte Carlo method (5,000 replications) showed that the coefficient of indirect effect was significant (indirect effect = 0.491, 95%CI=[0.443, 0.623]). The 95%CI did not contain zero, which confirmed that OBSE played a mediating role in the association between PSC and work engagement. Thus, H3a was supported.
The same procedure was adopted to verify the mediating role of OBSE in the relationship between PSC and job burnout. There was a negative relationship between PSC and job burnout (M6, γ=-0.518, p <0.001). Thus, H1b was supported. OBSE was negatively correlated with job burnout (M5, γ=-0.449, p <0.001). OBSE had a significant negative effect on burnout when it entered M7 (M7, γ=-0.443, p <0.001), while the coefficient of significant effect of PSC on job burnout decreased from − 0.518 to -0.259, with OBSE partially mediated the effect between PSC and job burnout. Further, the Monte Carlo method (5,000 replications) results showed that coefficient of indirect effect was significant (indirect effect − 0.279, 95%CI=[-0.326, -0.232]). The 95%CI did not contain zero, which confirmed that OBSE mediated the association between PSC and job burnout. Thus, H3b was supported.
In this study, when validating the cross-level interaction effect, the data of organizational-level PSC (as the independent variable) was grand-mean centered, and the psychological detachment at the individual level (as the moderator) was group-mean centered [ 43 ]. The moderating effects of psychological detachment in the relationship between PSC and work engagement, as well as job burnout are shown in Table 3 . The results indicated that the interaction between PSC and psychological detachment was positively and significantly related to work engagement (γ = 0.158, p <0.05), but the interaction was insignificantly related to job burnout (γ=-0.135, p >0.05). To better visualize the moderating role of psychological detachment, the simple slope test as recommended by Aiken et al. was utilized [ 44 ]. Figure 2 presents a plot of the interaction effect between psychological detachment (M ± 1SD) and PSC at different levels. As shown in Fig. 2 , the relationship between PSC and work engagement was stronger for higher level psychological detachment than lower level.

The interactive effect of PSC and PD on work engagement. (Note: PSC: psychosocial safety climate, PD: psychological detachment)
To the knowledge of the authors, this is the first study to reveal the influence of PSC on work engagement and job burnout in Chinese nurses and to examine the mediating role of OBSE and the moderating role of psychological detachment based on a large sample. The results showed that the effect of PSC differs from person to person and enriched the situational analysis of PSC’s mechanism. And relative to the moderators incorporated in previous studies (such as individual fixed characteristics and external resources), psychological detachment has developable, actionable characteristics and significant value. The findings provide theoretical support and guidance for the organization and manager to improve nurses’ work engagement and reduce job burnout.
First, this study found that PSC had a positive effect on work engagement and a negative effect on job burnout, which is consistent with previous research findings [ 16 ]. At a high level of PSC, the organization’s senior management takes mental health and safety seriously and endeavors to ensure job requirements are reasonable. By creating good working conditions, nurses are protected from mental health problems and their work engagement can be improved [ 45 ]. Meanwhile, PSC acts as ‘resource caravan passageways’ to promote motivational process of the JD-R model through the organization at all levels of management or the organization’s resources, thus producing a spiral gain effect of resources [ 16 ]. Nurses’ existing resources are protected and more new resources are developed, generating a resource caravan phenomenon [ 46 ]. Hence, in a high-level PSC scenario, nurses are more likely to have access to work-related psychological resources to reduce the negative effects of work-related stress and demands. Moreover, when nurses perceive higher level of PSC, it means that they perceive that the organization values and supports their mental health. Nurses are more likely to develop a ‘perceived obligation’ to repay the organization with more positive work attitudes and work behaviors. This finding is also supported by SET.
Second, this study confirmed that OBSE mediated the relationship between PSC and work engagement, as well as job burnout. Specifically, PSC positively predicted OBSE, and OBSE positively predicted work engagement, and negatively predicted job burnout. Similar findings pointed to a mediating role of OBSE between environmental resources and job crafting behaviors [ 47 ]. The positive organizational climate has a motivating effect on the spirit of individuals and stimulates their intrinsic motivation. Therefore, high PSC increases nurses’ perception of their own values in the organization, which in turn raises their OBSE. Based on the self-consistency theory, nurses maintain and strengthen their self-perceptions by developing more positive work attitudes and behaviors [ 48 ]. This finding is also supported by COR theory. OBSE reflects nurses’ sense of self-worth as members of the organization, which acts as a valuable workplace resource and can stimulates nurses’ loyalty and commitment to the organization. When nurses feel respected and recognized by the organization, they are motivated to participate in their work and devote more time and experience to their tasks. And they are better able to face challenges at work and face problems with a more positive attitude, which reduces burnout levels [ 49 ].
Finally, psychological detachment significantly moderated the relationship between PSC and work engagement. Previous studies have similar confirmations. For instance, Yu et al. revealed that psychological detachment moderated the relationship between stressors and innovative work behavior [ 50 ]. This may be because that when nurses achieve a state of physical and mental separation from work during non-working time, they would recover and acquire new resources from leisure activities. When they return to work again, they could deal with their work in a better condition, which promotes the positive impact of PSC on work engagement. However, psychological detachment did not have a significant moderating effect in the association between PSC and job burnout. This may be due to the fact that high levels of PSC provide nurses with abundant resources, and even nurses with lower levels of psychological detachment still have access to relatively adequate resources to maintain their good emotional state. This suggests that a lack of psychological detachment does not necessarily increase job burnout. Lack of psychological detachment only becomes a problem when work resources are inadequate, because it means that individuals will be continually and negatively affected by work-related stressors. Notably, previous studies suggested that high level of psychological detachment could lead to more severe burnout and depression when work resources were insufficient [ 51 ]. These findings emphasize that the psychological detachment does not always produce positive outcomes and that work resources still are a key factor in reducing burnout and the risk of mental health problems.
Implication
In summary, the study expands the pathway mechanisms and boundary conditions of PSC affecting nurses’ work engagement and job burnout. These findings emphasize the significant value of interventions at the organizational level. Managers should consider nurse psychological safety as one of the key organizational goals. The attention and behavioral practices of managers to nurses’ mental health could be enhanced through leadership styles’ training and development. Furthermore, the findings indicate that OBSE may act as a potential intervention target to increase work engagement and reduce job burnout through the implementation of programs that promote OBSE. Finally, the importance of appropriate detachment from work should be given full attention. Accordingly, organizations and managers should reduce communication with nurses during non-working time and rationalize work demands accordingly to allow and support nurses to detach during that time. At the meanwhile, nurses should be offered psychological detachment interventions, guidance, and training to enable them to better detach from their busy and stressful work. This would contribute to positive work performance and quality of care for nurses.
There were some limitations to consider in this study. Firstly, the cross-sectional design limited the ability to draw causal conclusions, and made it difficult to examine the dynamic processes by which PSC influenced work engagement and job burnout. The present study tried to control variables that may have an impact on the research hypotheses in order to minimize the influence of confounding factors on the results. To address the issue of common method bias arising from the cross-sectional design, this study collected nurses with different characteristics (including age, monthly income, technical title, working years, etc.), and the hierarchical linear modeling addressed common method bias in the individual-level data to some extent by modeling organization-level PSC and estimating between-team effects [ 52 ]. However, given the limitations of the cross-sectional study design, future studies may try to add consideration of the temporal dimension based on a multilevel design, while using methods such as scenario-based experiments. And it can be combined with qualitative research in order to explore in depth the mechanisms and reasons behind the relationships between the research variables. Secondly, we recruited participants from only one hospital, and the context of the present study should be considered when summarizing our findings. Despite the relatively large sample size collected, the generalizability of the findings to other populations and countries should be carefully assessed. Future studies are encouraged to be conducted in a wider range of populations as well as other cultures to increase the external validity of the findings. Thirdly, the data were measured by self-report approach, which may have introduced common method bias [ 39 ]. Future research could take the form of collecting data at multiple points in time. Also, where possible, objective indicators are used to verify the veracity of the data, for example, by using field or behavioral observations, assessments by others, and so on.
By constructing a cross-level theoretical model, this study provided a better understanding of “through what mechanisms” and “in what contexts” PSC at organizational level influences work engagement and job burnout among nurses. The study results showed that PSC was positively associated with work engagement and negatively associated with job burnout through OBSE. Our analysis also showed that high level of psychological detachment enhanced the positive effect of PSC on work engagement, but not the negative effect of PSC on job burnout. From the perspective of PSC, the study identified the influential mechanisms and situational characteristic of nurses’ work engagement and job burnout. The findings provide important insights in the management and practice for hospital managers and organizations to promote positive work engagement and psychological well-being among nurses.
Data availability
The data used or analyzed during the current study are available from the corresponding author upon reasonable request.
Chen C, Meier ST. Burnout and depression in nurses: a systematic review and meta-analysis. Int J Nurs Stud. 2021;124:104099. https://doi.org/10.1016/j.ijnurstu.2021.104099 .
Article PubMed Google Scholar
Bakker AB. The social psychology of work engagement: state of the field. Career Dev Int. 2022;27(1):36–53. https://doi.org/10.1108/cdi-08-2021-0213 .
Article Google Scholar
Zhu W, Avolio BJ, Walumbwa FOJG, Management O. Moderating role of follower characteristics with transformational Leadership and Follower Work Engagement. Group Organ Manage. 2009;34(5):590–619. https://doi.org/10.1177/1059601108331242 .
Zhang N, Xu D, Li J, Xu Z. Effects of role overload, work engagement and perceived organisational support on nurses’ job performance during the COVID-19 pandemic. J Nurs Manag. 2022;30(4):901–12. https://doi.org/10.1111/jonm.13598 .
Article PubMed PubMed Central Google Scholar
Alshamsi AI, Santos A, Thomson L. Psychosocial Safety Climate moderates the effect of demands of Hospital Accreditation on Healthcare professionals: a longitudinal study. Front Health Serv. 2022;2:824619–824619. https://doi.org/10.3389/frhs.2022.824619 .
Ge MW, Hu FH, Jia YJ, Tang W, Zhang WQ, Zhao DY, et al. COVID-19 pandemic increases the occurrence of nursing burnout syndrome: an interrupted time-series analysis of preliminary data from 38 countries. Nurse Educ Pract. 2023;69. https://doi.org/10.1016/j.nepr.2023.103643 .
Maslach C, Schaufeli WB, Leiter MP. Job burnout. Ann Rev Psychol. 2001;52:397–422. https://doi.org/10.1146/annurev.psych.52.1.397 .
Article CAS Google Scholar
Jun J, Ojemeni MM, Kalamani R, Tong J, Crecelius ML. Relationship between nurse burnout, patient and organizational outcomes: systematic review. Int J Nurs Stud. 2021;119. https://doi.org/10.1016/j.ijnurstu.2021.103933 .
Garcia CD, de Abreu LC, Ramos JLS, de Castro CFD, Smiderle FRN, dos Santos JA, et al. Influence of Burnout on Patient Safety: systematic review and Meta-analysis. Medicina-Lithuania. 2019;55(9). https://doi.org/10.3390/medicina55090553 .
Keyko K, Cummings GG, Yonge O, Wong CA. Work engagement in professional nursing practice: a systematic review. Int J Nurs Stud. 2016;61:142–64. https://doi.org/10.1016/j.ijnurstu.2016.06.003 .
Reichers AE. Climate and culture: an evolution of constructs. Organizational Culture & Climate. 1990.
Abdi F, Jahangiri M, Kamalinia M, Cousins R, Mokarami H. Developing a model for predicting safety performance of nurses based on psychosocial safety climate and role of job demands and resources, job satisfaction, and emotional exhaustion as mediators. BMC Psychol. 2023;11(1):187. https://doi.org/10.1186/s40359-023-01223-1 .
Huyghebaert T, Gillet N, Fernet C, Lahiani F-J, Fouquereau E. Leveraging psychosocial safety climate to prevent ill-being: the mediating role of psychological need thwarting. J Vocat Behav. 2018;107:111–25. https://doi.org/10.1016/j.jvb.2018.03.010 .
Dollard MF, Bakker AB. Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement. J Occup Organizational Psychol. 2010;83(3):579–99. https://doi.org/10.1348/096317909x470690 .
Loh MY, Idris MA, Dollard MF, Isahak M. Psychosocial safety climate as a moderator of the moderators: contextualizing JDR models and emotional demands effects. J Occup Organizational Psychol. 2018;91(3):620–44. https://doi.org/10.1111/joop.12211 .
Mansour S, Tremblay DGJPR. How can we decrease burnout and safety workaround behaviors in health care organizations? The role of psychosocial safety climate. Pers Rev. 2019;48(2):528–50. https://doi.org/10.1108/PR-07-2017-0224 .
Cropanzano R, Anthony EL, Daniels SR, Hall AV, SOCIAL EXCHANGE THEORY:, A CRITICAL REVIEW WITH THEORETICAL REMEDIES. Acad Manag Ann. 2017;11(1):479–516. https://doi.org/10.5465/annals.2015.0099 .
Norman SM, Gardner DG, Pierce JL. Leader roles, organization-based self-esteem, and employee outcomes. Leadersh Organ Dev J. 2015;36(3):253–70. https://doi.org/10.1108/lodj-06-2013-0072 .
Pierce JL, Gardner DG. Self-esteem within the work and organizational context: a review of the organization-based self-esteem literature. J Manag. 2004;30(5):591–622. https://doi.org/10.1016/j.jm.2003.10.001 .
Kim M, Beehr TA. Organization-based self-esteem and meaningful work Mediate effects of Empowering Leadership on Employee behaviors and well-being. 2018; 25(4):385–98. https://doi.org/10.1177/1548051818762337 .
Haider S, de Pablos Heredero C, Ahmed M. A three-wave time-lagged study of mediation between positive feedback and organizational citizenship behavior: the role of organization-based self-esteem. Psychol Res Behav Manag. 2019;12:241–53. https://doi.org/10.2147/prbm.S192515 .
Korman AK, ORGANIZATIONAL ACHIEVEMENT, AGGRESSION AND CREATIVITY - SOME SUGGESTIONS TOWARD AN INTEGRATED THEORY. Organizational Behav Hum Perform. 1971;6(5):593–613. https://doi.org/10.1016/s0030-5073(71)80009-0 .
Korman AK, TOWARD AN HYPOTHESIS OF, WORK BEHAVIOR. J Appl Psychol. 1970;54(1):31–. https://doi.org/10.1037/h0028656 .
Hobfoll SE, CONSERVATION OF RESOURCES - A NEW ATTEMPT AT, CONCEPTUALIZING STRESS. Am Psychol. 1989;44(3):513–24. https://doi.org/10.1037/0003-066x.44.3.513 .
Article CAS PubMed Google Scholar
Sonnentag S, Fritz C. Recovery from job stress: the stressor-detachment model as an integrative framework. J Organizational Behav. 2015;36:S72–103. https://doi.org/10.1002/job.1924 .
Wang H, Xu G, Liang C, Li Z. Coping with job stress for hospital nurses during the COVID-19 crisis: the joint roles of micro-breaks and psychological detachment. J Nurs Manag. 2022;30(7):2116–25. https://doi.org/10.1111/jonm.13431 .
Hall GB, Dollard MF, Coward J. Psychosocial Safety Climate: development of the PSC-12. Int J Stress Manage. 2010;17(4):353–83. https://doi.org/10.1037/a0021320 .
Pien LC, Cheng YW, Cheng WJ. Psychosocial safety climate, workplace violence and self-rated health: a multi-level study among hospital nurses. J Nurs Adm Manag. 2019;27(3):584–91. https://doi.org/10.1111/jonm.12715 .
Pierce JL, Gardner DG, Cummings LL, Dunham RB, ORGANIZATION-BASED SELF-ESTEEM -. CONSTRUCT DEFINITION, MEASUREMENT, AND VALIDATION. Acad Manag J. 1989;32(3):622–48. https://doi.org/10.2307/256437 .
De Cremer D, van Knippenberg B, van Knippenberg D, Mullenders D, Stinglhamber F. Rewarding leadership and fair procedures as determinants of self-esteem. J Appl Psychol. 2005;90(1):3–12. https://doi.org/10.1037/0021-9010.90.1.3 .
Christian MS, Eisenkraft N, Kapadia C. Dynamic associations among somatic complaints, Human Energy, and discretionary behaviors: experiences with Pain fluctuations at work. Adm Sci Q. 2015;60(1):66–102. https://doi.org/10.1177/0001839214553655 .
Stamm B. The Concise Manual for the Professional Quality of Life Scale. 2010.
Kartsonaki MG, Georgopoulos D, Kondili E, Nieri AS, Alevizaki A, Nyktari V, et al. Prevalence and factors associated with compassion fatigue, compassion satisfaction, burnout in health professionals. Nurs Crit Care. 2023;28(2):225–35. https://doi.org/10.1111/nicc.12769 .
Sonnentag S, Fritz C. The recovery experience questionnaire: development and validation of a measure for assessing recuperation and unwinding from work. J Occup Health Psychol. 2007;12(3):204–21. https://doi.org/10.1037/1076-8998.12.3.204 .
Shi Y, Xie J, Zhou ZE, Ma H, Tang Y. How parents’ psychological detachment from work affects their children via fatigue: the moderating role of gender. Stress Health. 2022;38(3):463–76. https://doi.org/10.1002/smi.3107 .
Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286–302. https://doi.org/10.1111/jan.14839 .
Tang P, Zhang X, Feng F, Li J, Zeng L, Xie W et al. The relationship between organizational commitment and work engagement among clinical nurses in China: a cross-sectional study. 2022; 30(8):4354–63. https://doi.org/10.1111/jonm.13847 .
Tofighi D, MacKinnon DP. RMediation: an R package for mediation analysis confidence intervals. Behav Res Methods. 2011;43(3):692–700. https://doi.org/10.3758/s13428-011-0076-x .
Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879–903. https://doi.org/10.1037/0021-9010.88.5.879 .
James LR, AGGREGATION BIAS IN ESTIMATES OF PERCEPTUAL AGREEMENT. J Appl Psychol. 1982;67(2):219–29. https://doi.org/10.1037/0021-9010.67.2.219 .
James LR, Demaree RG, Wolf G, ESTIMATING WITHIN-GROUP INTERRATER RELIABILITY WITH, AND WITHOUT RESPONSE BIAS. J Appl Psychol. 1984;69(1):85–98. https://doi.org/10.1037/0021-9010.69.1.85 .
Glick WH, CONCEPTUALIZING AND MEASURING ORGANIZATIONAL AND PSYCHOLOGICAL CLIMATE -, PITFALLS IN MULTILEVEL RESEARCH. Acad Manage Rev. 1985;10(3):601–16. https://doi.org/10.2307/258140 .
Hofmann DA. An overview of the logic and rationale of hierarchical linear models. J Manag. 1997;23(6):723–44. https://doi.org/10.1177/014920639702300602 .
Toothmaker LE. MULTIPLE-REGRESSION - TESTING AND INTERPRETING, INTERACTIONS - AIKEN. LS, WEST,SG. J Oper Res Soc. 1994;45(1):119–20.
Google Scholar
Dollard MF, Bailey T. Building Psychosocial Safety Climate in turbulent Times: the case of COVID-19. J Appl Psychol. 2021;106(7):951–64. https://doi.org/10.1037/apl0000939 .
Hobfoll SE. Conservation of resource caravans and engaged settings. J Occup Organizational Psychol. 2011;84(1):116–22. https://doi.org/10.1111/j.2044-8325.2010.02016.x .
Kim M, Beehr TA. The role of organization-based self-esteem and job resources in promoting employees’ job crafting behaviors. Int J Hum Resource Manage. 2022;33(19):3822–49. https://doi.org/10.1080/09585192.2021.1934711 .
Gardner DG, Pierce JL. Organization-based self-esteem in work teams. Group Processes Intergroup Relations. 2016;19(3):394–408. https://doi.org/10.1177/1368430215590491 .
Lapalme M, Guerrero S. How do I stand compared to agency workers? Justice perceptions and employees’ counterproductive work behaviours. J Nurs Manag. 2019;27(7):1471–8. https://doi.org/10.1111/jonm.12832 .
Yu J, Liu J, Lin S, Chi X. The relationship between stressors and Chinese employees’ innovative work behavior: the role of task crafting and psychological detachment. Eur J Innov Manage. 2023. https://doi.org/10.1108/ejim-08-2022-0417 .
Muhamad Nasharudin NA, Idris MA, Loh MY, Tuckey M. The role of psychological detachment in burnout and depression: a longitudinal study of Malaysian workers. Scand J Psychol. 2020;61(3):423–35. https://doi.org/10.1111/sjop.12622 .
Siami S, Gorji M, Martin A. Psychosocial safety climate and supportive leadership as vital enhancers of personal hope and resilience during the COVID-19 pandemic. 2023; 39(2):404–13. https://doi.org/10.1002/smi.3192 .
Download references
Acknowledgements
The authors thank all nurses, hospital directors and administrators for their support and assistance for this project. In addition, thanks for all members of the research group for their selfless help.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Tongshuang Yuan, Hui Ren contributed equally to this work and should be considered co-first authors.
Authors and Affiliations
School of Public Health, Jilin University, No. 1163 Xinmin Street, Changchun, Jilin, 130021, China
Tongshuang Yuan, Leilei Liang, Junsong Fei, Xiaoying Liu, Chengbin Zheng, Huimin Wang, Jiaying Gao & Songli Mei
Department of Nursing, The First Hospital of Jilin University, Changchun, Jilin, 130021, China
Hui Ren & Xin Yin
The First Hospital of Jilin University, No. 71 Xinmin Street, Changchun, Jilin, 130021, China
You can also search for this author in PubMed Google Scholar
Contributions
Tongshuang Yuan: Conceptualization, Writing-original draft, Formal analysis. Hui Ren: Investigation, Project administration. Xin Yin: Resources, Writing-review & editing. Leilei liang: Resources, Writing-review & editing. Junsong Fei: Writing-review & editing, Validation. Xiaoying Liu: Writing-review & editing, Validation. Chengbin Zheng: Methodology, Visualization. Huimin Wang: Data curation, Software. Jiaying Gao: Methodology, Visualization. Songli Mei: Data curation, Supervision. Hongyan Li: Resources, Data curation.
Corresponding authors
Correspondence to Songli Mei or Hongyan Li .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
The investigation was carried out in accordance with the latest version of the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board of the School of Public Health, Jilin University. And online informed consent was obtained from all participants.
Consent for publication
All authors have read and approved the final version for publication.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yuan, T., Ren, H., Yin, X. et al. How does psychosocial safety climate cross-level influence work engagement and job burnout: the roles of organization-based self-esteem and psychological detachment. BMC Nurs 23 , 389 (2024). https://doi.org/10.1186/s12912-024-01935-8
Download citation
Received : 13 December 2023
Accepted : 12 April 2024
Published : 06 June 2024
DOI : https://doi.org/10.1186/s12912-024-01935-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychosocial safety climate
- Cross-level model
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Ensuring Patient and Workforce Safety Culture in Healthcare
Introduction.
In 2020, the Institute for Healthcare Improvement (IHI) and the Agency for Healthcare Research and Quality (AHRQ) unveiled the National Action Plan to Advance Patient Safety. 1 Within this framework, four pillars were identified as critical to fostering a safer health care environment: Culture, Leadership and Governance; Patient and Family Engagement; Learning Systems; and Workforce Safety. This 2023 Year in Review Perspective highlights some of the research posted on PSNet in 2023 related to two of these elements: patient safety culture and workforce safety culture.
At a high level, organizational culture is the aggregated attitudes, norms, and perceptions of a team of workers. Although organizational policies certainly influence aspects of culture, the daily interactions that staff members have with each other and with managers are the lifeblood of an organization's culture. In healthcare organizations, patient and workforce safety culture are founded on how well teams work together, how supportive leadership and managers are of patient and workforce safety, how staff report events and near misses, and how teams and leaders respond to events. 2
A positive patient and workforce safety culture has been shown to significantly improve a number of patient outcomes, including lower rates of surgical site infections , falls, and medication errors . In addition to specific health outcomes, patients report having better experiences with their care when the culture of patient safety is strong.
Although most organizations and healthcare workers (HCWs) agree on the importance of safety culture, research this year focused heavily on the psychological factors surrounding culture, such as psychological safety, how to support HCWs after an adverse event, and burnout. There was also a smaller focus on safety culture in nonacute care settings. Methodologically, the year's research predominantly centers on surveys capturing health care workers' perceptions of culture, with less emphasis on interventions to improve safety culture. Researchers reviewed all relevant articles on PSNet in 2023 and consulted with Dr. John Murray, PhD, RN and Dr. Joann Sorra, PhD, subject matter experts in safety culture.
Psychological Safety and Employee Voice
The most prominent focus within the area of safety culture in 2023, based on the number of articles published on PSNet, was on the concepts of psychological safety and employee voice. These concepts are both related to how respected and comfortable employees feel speaking up and expressing their ideas, opinions, and concerns without fear of retribution. In a patient safety–specific context, this might entail a HCW raising a concern about a patient’s safety (such as an HCW missing a contraindication when prescribing a medication or not washing their hands prior to a procedure) to their peers or leaders. The concern may be raised preemptively before an incident occurs, or after, and it may involve either the actions of the individual who is raising the issue or the actions of their teammates. If an organization or a team has a culture of blame and retribution, then HCWs may stay silent about concerns or safety events. Psychologically safe cultures focus more on learning and how system failures lead to safety events rather than on individual actions. However, a culture focused on system failures does not preclude individual accountability where appropriate. The concept of just culture seeks to balance this systems-based approach to safety events with appropriate individual accountability if the events are negligent or repeated regularly.
Various tools have been developed to measure psychological safety and employee voice, primarily through Likert scale–based surveys to rate items such as “If you make a mistake on this team, it is often held against you,” “It is difficult to ask other members of this team for help,” and “Working with members of this team, my unique skills and talents are valued and utilized.” 3 However, objectively assessing these psychological concepts remains challenging. This reliance on self-reported data was listed as an evidence gap by a systematic review this year.
After reviewing the research on psychological safety and employee voice from the past year, we categorized the influencing factors into individual, team, and leadership factors. Although these factors are not mutually exclusive, this is a useful model for understanding what motivates an HCW to feel safe enough to speak up.
Individual Factors
At the most basic level, an individual’s personality traits could make it more likely for them to speak up, regardless of the environment. For example, someone who is extroverted may be more likely to speak up than someone who is introverted. Research linking specific personality traits to psychological safety and employee voice is currently limited but starting to be explored. A systematic review this past year found that prosocial motivations, dominant traits, level of competence, and level of self-efficacy affected speaking-up behavior. Another qualitative study found significant but weak correlations between participants’ emotional stability and level of abstract thinking and their feelings of psychological safety.
Despite the lack of evidence linking personality traits to psychological safety and employee voice, some studies in 2023 focused on improving individual psychological safety and speaking-up behavior. One pre-post study found that a four-hour communication training did not increase psychological safety or communication, but it should be noted that there was no control group in that study and the sample size was relatively low (N = 137). However, a meta-analysis found that assertive communication training for nurses improved speaking-up behavior related to safety events. This difference may speak to the variance in quality of each training, but the meta-analysis results suggest that a well-designed training could improve employee voice and psychological safety.
Team Factors
The team that an HCW interacts with every day can impact their psychological safety and willingness to speak up. For example, seeing others on the team speak up and receive a negative reaction, a peer discouraging them from speaking up to the manager, or experiencing retribution after a mistake could all potentially negatively affect HCWs’ psychological safety and suppress employee voice going forward. One large survey study in 2023 found the main factors that affected employee voice were the person’s social capital within the team, such as rank or seniority; their exposure to unprofessional behaviors; and demographic features such as age and gender (with older and male respondents more likely to speak up). The authors concluded that healthcare organizations should combine interventions to improve culture with efforts to reduce hierarchical structures, reduce inequalities, and increase protection for staff who speak up.
Several studies in 2023 found that when psychological safety is high, event reporting rates and teamwork improve. One survey of 526 nurses found that those who report high psychological safety are more likely to share important information about patient safety, actively engage in teamwork behaviors, and report safety events and near misses. 4 Similarly, another study with nurses found a correlation between high psychological safety and willingness to report safety events. A study using vignettes demonstrated that when an HCW has high personal psychological safety, they perceive colleagues who speak up as more helpful to the team. This finding suggests that high psychological safety can not only impact individual behavior but also improve teamwork and cohesiveness through increased positive affect. This observation is echoed by another study on psychological safety that found the more a team agrees on the level of psychological safety, the better their overall performance. 5
Some intervention studies this past year on improving team safety culture, centered on the use of in situ simulation. This type of simulation takes place in the same clinical environment with the same equipment and with the same team members as a real clinical situation. One systematic review found that in situ simulation training increased ICU staff perceptions of safety culture and teamwork climate post training. This is reinforced by a qualitative study on anesthesia personnel , where participants reported that the realism of the in situ training helped clarify team roles and improve clarity in communication.
Leadership and Organizational Factors
Finally, the last set of factors shown to affect psychological safety and employee voice come from leadership and the organization as a whole. The importance of this aspect was delineated in the National Action Plan to Advance Patient Safety, which called for governing boards to understand importance of safety, get involved in safety, and promote a culture of safety. 1 Studies on this topic on PSNet in 2023 covered many levels of leadership, from unit managers to executives.
A few studies this past year showed that when employees rate their leaders highly, employees’ perceptions of safety culture and psychological safety improve, such as a study of infection preventionists during the COVID-19 pandemic. Another large survey study found that rating leadership highly on items like “provides useful feedback about my performance” and “is available at predictable times” correlates with a higher perception of safety climate and teamwork climate.
Other studies focused on what attributes and techniques leaders can have or use to improve their role in psychological safety and safety culture. A systematic review of employee’s perceived ability to speak up found that leadership attributes (such as higher levels of inclusion, mediation, humility, and lower levels of narcissism), higher supervisor job security, and less top-down decision making were associated with more speaking up behaviors among employees. Another integrative review on Just Culture showed that leaders can demonstrate full commitment to Just Culture by being “visible, accessible, approachable and committed to providing the support and resources needed.” One smaller survey study concluded that leaders should understand employees’ unique skills and needs, express confidence in their abilities, and encourage them to share their ideas (safety related or otherwise) to create an inclusive and trusting work environment that facilitates psychological safety and ultimately reduces safety events. A qualitative study echoed that leaders should get to know the personalities of their employees.
Leaders can encourage psychological safety and employee voice in their responses to staff who bring up safety concerns. One qualitative study reported that nurses who tried to speak up about concerns during the COVID-19 pandemic often felt unheard, were treated with hostility, or experienced a lack of meaningful change. One reason for this may be that leaders and workers have different perceptions of how strong the safety culture is, as illustrated in one study of radiologist managers and staff. In an effort to address this, a qualitative study using simulation videos reported on various barriers to and enablers of receiving a safety message. These studies suggest it is important to train leaders on how to best receive a safety concern in addition to training staff members to speak up more often.
Few intervention studies posted on PSNet in 2023 related to leadership and psychological safety. One study demonstrated that when leaders capture and highlight proactive safety behaviors of staff daily, it can improve behaviors related to patient safety. This finding implies that a leader’s role in building a culture of safety is not only responding to events but also regularly highlighting their employees’ successes.
Supporting HCWs Who Are Involved in Adverse Events
In addition to fostering an environment of psychological safety, a strong safety culture creates an environment where HCWs feel support from their colleagues and leaders following an adverse safety event that may have caused preventable harm. Strong support of HCWs may decrease negative psychological symptoms, increase the safety awareness of that staff member and others they share the event with, and decrease staff turnover. Research posted on PSNet in 2023 examined how adverse events affect HCWs psychologically and how they hoped to be supported.
On the most recent AHRQ Hospital Survey on Patient Safety Culture (SOPS) report , 64% of respondents said a lack of support exists for staff involved in patient safety events. This finding is significant because of the serious effects an adverse event can have on HCWs. One scoping review on nurses who were involved in adverse events indicated that nurses most commonly reported feeling a loss of confidence, anxiety, shame, guilt, exhaustion, depression, and fear of lost trust from colleagues and managers after adverse events. Some coped with these symptoms by becoming hypervigilant, sharing their experience with others, and taking leave. All studies included in the review identified a lack of emotional support after a safety event. Many nurses yearned for empathy from their peers, opportunities to debrief about the incident, and follow-up check-ins on their mental health. These findings were echoed in studies with other professions in 2023, such as surgeons , respiratory therapists , and pediatric ICU staff . The latter study quantified that 42% of pediatric ICU staff who had experienced an adverse event felt psychological distress, 22% reported absenteeism, and 23% considered leaving the ICU. The most commonly sought form of support was a respected peer with whom to discuss the details of what happened (86%), followed by taking time off of the unit (73%). In response to these findings, the authors suggested creating and maintaining a supportive, empathetic, and nonpunitive workplace culture, establishing a peer support program with debriefs and regular check-ins, and using near misses and adverse events to improve safety awareness and skills among all staff.
Stress and Burnout Among HCWs
The final psychological factor of safety culture explored in research posted on PSNet in 2023 was HCW stress and burnout. The healthcare profession is inherently demanding, and HCWs may be prone to burnout due to issues including a heavy workload, responsibility for the wellbeing of others, irregular hours, experiences of workplace violence, and high administrative burden. This feeling of burnout can be worsened if organizations don’t provide adequate staffing, resources, and a positive workplace culture. A large hospital survey study in 2023 found that employees’ ratings of safety culture are negatively correlated with stress and burnout. A systematic review of research among nurses also found a negative relationship between safety culture and job-related stress. Although it is important to note that the theoretical relationship between these two concepts is unclear and may not be unidirectional, a poor workplace safety culture can worsen stress, and stress and burnout can also worsen safety culture.
Burnout was shown to affect a significant proportion of clinicians in 2023. Two recent large survey studies, one on the AHRQ Workplace Safety Supplemental Item Set for Hospitals and one in military hospitals , reported the rate of HCW burnout at 34% and 35%, respectively. This high HCW burnout rate has a compounding effect: It negatively affects individual HCWs and it also potentially leads to more adverse events. The majority of studies in one systematic review on physicians found a link between burnout and clinically significant safety events. In addition to burnout increasing the risk of adverse events, the number of adverse events in a unit can cause burnout , leading to a downward cycle in HCWs’ mental health and patient safety.
Several studies this year discussed factors that were associated with decreased stress and burnout. Strong teamwork, adequate staffing, and high-quality leadership were the most common themes. One study on military hospitals found that higher ratings of within- and across-unit teamwork significantly reduced the odds of burnout across all clinical areas studied. Another study in large academic medical centers found the same correlation. In addition, that study found a significant correlation between staffing levels and reported burnout. High ratings of leadership were also shown to be negatively correlated to burnout, such as in a study among infection preventionists. A systematic review found that high scores of nurse leaders on leadership metrics (such as coaching, informing, and interacting) was correlated with higher job satisfaction and improved performance among employees. 6 Finally, another study found the strongest correlation between leadership and reduced burnout came from leaders providing regular useful feedback on performance. The authors posit that this regular feedback may be increasing psychological safety in employees, which, as previously noted, correlates with improved safety culture.
Safety Culture in Nonacute Settings
Historically, the majority of safety culture research has focused on hospital safety culture. However, some research in non-acute settings (specifically, nursing homes) was posted on PSNet in 2023. Very little research in 2023 focused on safety culture in other non-acute settings, such as primary care or medical offices.
Research into patient safety in nursing homes and long-term care settings has increased in the last decade. Research in 2023 built on this by focusing on safety culture in nursing homes. The most recent AHRQ SOPS Nursing Home Survey found that 54% of nursing home employees rated resident safety as very good or excellent, compared to 67% of employees in hospitals . While respondents rated nursing home culture highly on some measures, such as communication about incidents, only 39% of respondents agreed there were enough staff to handle the workload, meet residents’ needs during shift changes, and keep residents safe. In addition, only 54% of respondents agreed that nonpunitive responses to mistakes were used. Interestingly, a different survey study focusing exclusively on licensed practical nurses (LPNs) compared their results with the AHRQ SOPS Nursing Home Survey (LPNs comprised only 18% of SOPS Nursing Home Survey respondents) and found that LPNs rated all measures of safety culture lower than the average reported in the SOPS Database. Similar to the overall SOPS Nursing Home Survey results, the lowest rated dimensions were adequate staffing (29%) and non-punitive responses to mistakes (31%). This survey also found that LPNs working in nursing homes were less satisfied with their jobs than LPNs working in other settings, and that their job satisfaction was significantly but weakly correlated with their ratings of safety culture. This low job satisfaction may lead to burnout, turnover, and increased staffing issues. According to AHRQ’s pilot study on the Workplace Safety Supplemental Item Set for Nursing Homes, 33% of nursing home staff experienced burnout, similar to the rate in hospitals. 7 Two other studies on nursing home culture in 2023 were qualitative in nature. One study asked employees how they would improve safety culture. The most prominent themes included better staff orientation, with a focus on safety; better ongoing training; improvement of infrastructure (such as reducing stairs and increasing grip handles); and procuring more security staff. Another study among nursing home leaders asked what differentiates high-performing nursing homes from lower-performing ones. The main themes that emerged were communication about resident safety, particularly the important role of physician and manager accessibility, and leadership support for and responsiveness to resident safety issues raised by frontline staff. Although the amount of research on nursing home culture was low in 2023, the increased focus on this setting in recent years provides a solid foundation for future work to illuminate the challenges to and facilitators of building a culture of safety in this setting.
Conclusion and Future Directions
Research in 2023 on PSNet has predominantly focused on understanding the psychological aspects of safety culture. Studies delved into the factors influencing HCWs’ perceptions of patient and workplace safety, including their willingness to speak up, as well as the support they received after being involved in adverse events, and the pervasive influence of burnout on safety culture. A key recommendation emerging from this research is for more proactive training aimed at empowering all staff members, irrespective of their seniority or role, to freely express their concerns and report safety events. 8 , 9 The research also emphasizes the need for leaders and organizations to respond supportively and actively, fostering a culture of psychological safety. In addition, the research underscores the importance of providing support structures, including peer and organizational support, for HCWs involved in adverse events to help rebuild their confidence. To address burnout, the research suggests strategies such as regular feedback from leaders, teamwork initiatives, and thoughtful consideration of working hours and staffing levels.
The field would benefit from more research in several areas in upcoming years. Future research areas include more studies on nonacute settings, and additional research exploring the links between safety culture, patient outcomes, and patient experience. Finally, more research on design, implementation, and evaluation of interventions to enhance safety culture would be beneficial as organizations strive to embed this foundational aspect of providing safe care.
1. Institute for Healthcare Improvement. National Steering Committee for Patient Safety. Declaration to advance patient safety. Boston: Institute for Healthcare Improvement; 2022. https://www.ihi.org/initiatives/national-steering-committee-patient-safety/declaration-advance-patient-safety
2. Agency for Healthcare Research and Quality. About SOPS. Accessed February 5, 2024. https://www.ahrq.gov/sops/about/index.html
3. Edmondson A. Psychological safety and learning behavior in work teams. Admin Sci Quart . 1999;44(2):350-383.
4. Lee SE, Dahinten VS, Lee JH. Testing the association between the enabling and enacting factors of patient safety culture and patient safety: structural equation modelling. BMC Nurs . 2023;22(1):32.
5. Fyhn B, Bang H, Sverdrup TE, et al. Safe Among the Unsafe: Psychological Safety Climate Strength Matters for Team Performance . Small Group Research, 2023; 54(4), 439-473. https://doi.org/10.1177/10464964221121273
6. Alsadaan N, Salameh B, Reshia FAAE, et al. Impact of nurse leaders behaviors on nursing staff performance: a systematic review of literature. Inquiry . 2023;60:469580231178528. doi:10.1177/00469580231178528
7. Agency for Healthcare Research and Quality. Workplace Safety Supplemental Item Set for Nursing Home SOPS. Rockville, MD: Agency for Healthcare Research and Quality; 2023. Accessed February 5, 2024. https://www.ahrq.gov/sops/surveys/nursing-home/supplemental-items/workplace-safety.html
8. Chen H-W, Wu J-C, Kang Y-N, et al. Assertive communication training for nurses to speak up in cases of medical errors: a systematic review and meta-analysis. Nurse Educ Today . 2023;126:105831. doi:10.1016/j.nedt.2023.105831.
9. Pavithra A, Mannion R, Sunderland N, et al. Speaking up as an extension of socio-cultural dynamics inhospital settings: a study of staff experiences of speaking upacross seven hospitals. J Health Organ Manag . 2022;36(9):245-271.
This project was funded under contract number 75Q80119C00004 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. The authors are solely responsible for this report’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report. View AHRQ Disclaimers
Perspective
Perspectives on Safety
Annual Perspective
Patient Safety Innovations
Suicide Prevention in an Emergency Department Population: ED-SAFE
Surveys on Patient Safety Culture (SOPS) Ambulatory Surgery Center Survey: User Database Report. January 14, 2024
Surveys on Patient Safety Culture (SOPS) Medical Office Survey: 2024 User Database Report. February 28, 2024
Reducing Preventable Patient Harm Due to Retained Surgical Items: The RSI Bundle
Patient safety and adverse maternal health outcomes: the missing social inequalities 'lens.' October 5, 2005
Agent of change. August 1, 2018
WebM&M Cases
Amid lack of accountability for bias in maternity care, a California family seeks justice. August 16, 2023
Simulation and the diagnostic process: a pilot study of trauma and rapid response teams. December 20, 2017
Management of drug shortages in the perioperative setting. February 6, 2013
On Patient Safety. January 13, 2024
Nursing Home Survey on Patient Safety Culture. August 31, 2022
Patient Safety Primers
Discharge Planning and Transitions of Care
Hospital Survey on Patient Safety Culture: 2010 User Comparative Database Report. May 19, 2010
Hospital Survey on Patient Safety Culture: 2011 User Comparative Database Report. April 6, 2011
Nursing Home Survey on Patient Safety Culture: 2011 User Comparative Database Report. September 14, 2011
Medical Office Survey on Patient Safety Culture: 2016 User Comparative Database Report. June 8, 2016
Hospital Survey on Patient Safety Culture: 2009 Comparative Database Report. June 10, 2009
Hospital Survey on Patient Safety Culture: 2008 Comparative Database Report. April 16, 2008
Medicines-related harm in the elderly post-hospital discharge. March 27, 2019
AHRQ Nursing Home Survey on Patient Safety Culture: 2014 User Comparative Database Report. November 19, 2014
Hospital Survey on Patient Safety Culture: 2016 User Comparative Database Report. May 11, 2016
Hospital Survey on Patient Safety Culture: 2014 User Comparative Database Report. April 23, 2014
Second victim experiences of health care learners and the influence of the training environment on postevent adaptation. June 5, 2024
Adverse Health Events in Minnesota: Annual Reports. June 4, 2024
Speaking up and taking action: psychological safety and joint problem-solving orientation in safety improvement. May 15, 2024
Perceptions of U.S. and U.K. incident reporting systems: a scoping review. May 15, 2024
Right Kind of Wrong: Why Learning to Fail can Teach us to Thrive. October 18, 2023
In search of an international multidimensional action plan for second victim support: a narrative review. September 13, 2023
Patient, carer and family experiences of seeking redress and reconciliation following a life-changing event: systematic review of qualitative evidence. August 2, 2023
Ambulatory Safety Nets to Reduce Missed and Delayed Diagnoses of Cancer
Emotional responses and support needs of healthcare professionals after adverse or traumatic experiences in healthcare-evidence from seminars on peer support. June 28, 2023
Remote Response Team and Customized Alert Settings Help Improve Management of Sepsis

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
Postpartum Depression: A Clinical Review of Impact and Current Treatment Solutions
- Review Article
- Published: 30 May 2024
Cite this article

- Cindy-Lee Dennis ORCID: orcid.org/0000-0002-0135-7242 1 , 2 , 3 ,
- Daisy R. Singla ORCID: orcid.org/0000-0001-9865-7112 1 , 3 , 4 ,
- Hilary K. Brown ORCID: orcid.org/0000-0002-8690-5841 5 , 6 , 7 ,
- Katarina Savel 1 ,
- Crystal T. Clark ORCID: orcid.org/0000-0002-5051-3766 3 , 6 , 7 ,
- Sophie Grigoriadis ORCID: orcid.org/0000-0003-3461-6850 3 , 8 &
- Simone N. Vigod ORCID: orcid.org/0000-0002-2736-9639 3 , 6 , 7
59 Accesses
Explore all metrics
Depression during the first year postpartum (postpartum depression) impacts millions of women and their families worldwide. In this narrative review, we provide a summary of postpartum depression, examining the etiology and consequences, pharmacological and psychological treatments, and potential mechanisms of change and current barriers to care. Psychological treatments are effective and preferred by many perinatal patients over medications, but they often remain inaccessible. Key potential mechanisms underlying their effectiveness include treatment variables (e.g., dosage and therapeutic alliance) and patient behaviors (e.g., activation and avoidance and emotional regulation). Among pharmacological treatments, the selective serotonin reuptake inhibitor (SSRI) sertraline is generally the first-line antidepressant medication recommended to women in the postpartum period due to its minimal passage into breastmilk and the corresponding decades of safety data. Importantly, most antidepressant drugs are considered compatible with breastfeeding. Neurosteroids are emerging as an effective treatment for postpartum depression, although currently this treatment is not widely available. Barriers to widespread access to treatment include those that are systematic (e.g., lack of specialist providers), provider-driven (e.g., lack of flexibility in treatment delivery), and patient-driven (e.g., stigma and lack of time for treatment engagement). We propose virtual care, task-sharing to non-specialist treatment providers, and collaborative care models as potential solutions to enhance the reach and scalability of effective treatments to address the growing burden of postpartum depression worldwide and its negative impact on families and society.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Preventing postpartum depression: review and recommendations.

Antidepressants and recurrence of depression in the postpartum period
The efficacy of zuranolone versus placebo in postpartum depression and major depressive disorder: a systematic review and meta-analysis
Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. J Psychiatr Res. 2018;104:235–48.
Article PubMed Google Scholar
Falah-Hassani K, Shiri R, Dennis CL. The prevalence of antenatal and postnatal co-morbid anxiety and depression: a meta-analysis. Psychol Med. 2017;47(12):2041–53.
Article CAS PubMed Google Scholar
Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3(10):973–82.
Article PubMed PubMed Central Google Scholar
Evins GG, Theofrastous JP, Galvin SL. Postpartum depression: a comparison of screening and routine clinical evaluation. Am J Obstet Gynecol. 2000;182(5):1080–2.
Whitton A, Appleby L, Warner R. Maternal thinking and the treatment of postnatal depression. Int Rev Psychiatry. 1996;8(1):73–8.
Article Google Scholar
Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Interventions to prevent perinatal depression: US Preventive Services Task Force recommendation statement. JAMA. 2019;321(6):580–7.
Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA. 2010;303(19):1961–9.
Borges G, Bagge CL, Orozco R. A literature review and meta-analyses of cannabis use and suicidality. J Affect Disord. 2016;195:63–74.
Dennis CL, Marini F, Dol J, Vigod SN, Grigoriadis S, Brown HK. Paternal prevalence and risk factors for comorbid depression and anxiety across the first 2 years postpartum: a nationwide Canadian cohort study. Depress Anxiety. 2022;39(3):233–45.
Goodman JH. Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. J Adv Nurs. 2004;45(1):26–35.
Soliday E, McCluskey-Fawcett K, O’Brien M. Postpartum affect and depressive symptoms in mothers and fathers. Am J Orthopsychiatry. 1999;69(1):30–8.
Goodman J. Influences of maternal postpartum depression on fathers and on father-infant interactions. Infant Ment Health J. 2008;29:624–43.
Slomian J, Honvo G, Emonts P, Reginster JY, Bruyère O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health (Lond). 2019;15:1745506519844044.
CAS PubMed PubMed Central Google Scholar
Couto TC, Brancaglion MY, Alvim-Soares A, Moreira L, Garcia FD, Nicolato R, et al. Postpartum depression: a systematic review of the genetics involved. World J Psychiatry. 2015;5(1):103–11.
O’Hara MW, Mccabe JE. Postpartum depression: current status and future directions. Ann Rev Clin Psychol. 2013;9(1):379–407.
Henshaw C. Mood disturbance in the early puerperium: a review. Arch Womens Ment Health. 2003;6(Suppl 2):S33-42.
Forty L, Jones L, Macgregor S, Caesar S, Cooper C, Hough A, et al. Familiality of postpartum depression in unipolar disorder: results of a family study. Am J Psychiatry. 2006;163(9):1549–53.
Treloar SA, Martin NG, Bucholz KK, Madden PAF, Heath AC. Genetic influences on post-natal depressive symptoms: findings from an Australian twin sample. Psychol Med. 1999;29(3):645–54.
Silberstein M, Nesbit N, Cai J, Lee PH. Pathway analysis for genome-wide genetic variation data: analytic principles, latest developments, and new opportunities. J Genet Genom. 2021;48(3):173–83.
Comasco E, Sylvén SM, Papadopoulos FC, Sundström-Poromaa I, Oreland L, Skalkidou A. Postpartum depression symptoms: a case-control study on monoaminergic functional polymorphisms and environmental stressors. Psychiatr Genet. 2011;21(1):19–28.
Mitchell C, Notterman D, Brooks-Gunn J, Hobcraft J, Garfinkel I, Jaeger K, et al. Role of mother’s genes and environment in postpartum depression. Proc Natl Acad Sci USA. 2011;108(20):8189–93.
Article CAS PubMed PubMed Central Google Scholar
Payne JL, Maguire J. Pathophysiological mechanisms implicated in postpartum depression. Front Neuroendocrinol. 2019;52:165–80.
Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77–87.
Tabb KM, Dalton VK, Tilea A, Kolenic GE, Admon LK, Hall SV, et al. Trends in antenatal depression and suicidal ideation diagnoses among commercially insured childbearing individuals in the United States, 2008–2018. J Affect Disord. 2023;01(320):263–7.
Meyer CL, Oberman M. Mothers who kill their children: understanding the acts of moms from Susan Smith to the “Prom mom.” New York: New York University Press; 2001.
Google Scholar
Jennings KD, Ross S, Popper S, Elmore M. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54(1–2):21–8.
Da Costa D, Dritsa M, Rippen N, Lowensteyn I, Khalifé S. Health-related quality of life in postpartum depressed women. Arch Womens Ment Health. 2006;9(2):95–102.
Darcy JM, Grzywacz JG, Stephens RL, Leng I, Clinch CR, Arcury TA. Maternal depressive symptomatology: 16-month follow-up of infant and maternal health-related quality of life. J Am Board Fam Med. 2011;24(3):249–57.
Dennis CL, McQueen K. The relationship between infant-feeding outcomes and postpartum depression: a qualitative systematic review. Pediatrics. 2009;123(4):e736–51.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–19.
Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106(3):458–90.
Sameroff A, Seifer R, Zax M, Barocas R. Early indicators of developmental risk: Rochester longitudinal study. Schizophr Bull. 1987;13(3):383–94.
Cox AD, Puckering C, Pound A, Mills M. The impact of maternal depression in young children. J Child Psychol Psychiatry. 1987;28(6):917–28.
Lyons-Ruth K, Alpern L, Repacholi B. Disorganized infant attachment classification and maternal psychosocial problems as predictors of hostile-aggressive behavior in the preschool classroom. Child Dev. 1993;64(2):572–85.
Stein A, Gath DH, Bucher J, Bond A, Day A, Cooper PJ. The relationship between post-natal depression and mother-child interaction. Br J Psychiatry. 1991;158:46–52.
Bauer A, Parsonage M, Knapp M, Iemmi V, Adelaja B. The costs of perinatal mental health problems. Personal Social Services Research Unit Centre for Mental Health Maternal Mental Health Alliance; 2014. https://eprints.lse.ac.uk/59885/ .
Sarris J, O’Neil A, Coulson CE, Schweitzer I, Berk M. Lifestyle medicine for depression. BMC Psychiatry. 2014;14(1):107.
Sigurdsson E, Olafsdottir T, Gottfredsson M. Public views on antidepressant treatment: lessons from a national survey. Laeknabladid. 2009;95(12):837–41.
PubMed Google Scholar
Physical activity and exercise during pregnancy and the postpartum period: ACOG Committee Opinion, Number 804. Obstet Gynecol. 2020;135(4):e178–e88.
Morres ID, Tzouma NA, Hatzigeorgiadis A, Krommidas C, Kotronis KV, Dafopoulos K, et al. Exercise for perinatal depressive symptoms: a systematic review and meta-analysis of randomized controlled trials in perinatal health services. J Affect Disord. 2022;298(Pt A):26–42.
Ribeiro MM, Andrade A, Nunes I. Physical exercise in pregnancy: benefits, risks and prescription. J Perinat Med. 2022;50(1):4–17.
La Forge RMS. Aligning mind and body: exploring the disciplines of mindful exercise. ACSM’s Health Fit J. 2005;9(5):7.
Quirk SE, Williams LJ, O’Neil A, Pasco JA, Jacka FN, Housden S, et al. The association between diet quality, dietary patterns and depression in adults: a systematic review. BMC Psychiatry. 2013;13(1):175.
Jacka FN, Cherbuin N, Anstey KJ, Butterworth P. Does reverse causality explain the relationship between diet and depression? J Affect Disord. 2015;01(175):248–50.
Sun Y, Ferguson M, Reeves MM, Kelly JT. Maternal dietary patterns and risk of postpartum depression: a systematic review. Matern Child Health J. 2023;27(12):2077–90.
Tsai Z, Shah N, Tahir U, Mortaji N, Owais S, Perreault M, et al. Dietary interventions for perinatal depression and anxiety: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2023;117(6):1130–42.
Dennis C-L. Peer support within a health care context: a concept analysis. Int J Nurs Stud. 2003;40(3):321–32.
Dennis C-L, Hodnett E, Kenton L, Weston J, Zupancic J, Stewart DE, et al. Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. BMJ. 2009;338: a3064.
Feinberg ME. The internal structure and ecological context of coparenting: a framework for research and intervention. Parenting. 2003;3(2):95–131.
Xiao X, Loke AY. The effects of co-parenting/intergenerational co-parenting interventions during the postpartum period: a systematic review. Int J Nurs Stud. 2021;119:103951.
Sockol LE. A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J Affect Disord. 2015;177:7–21.
Dennis C-L, Creedy D. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2004. https://doi.org/10.1002/14651858.CD001134.pub2 .
O’Connor E, Senger CA, Henninger ML, Coppola E, Gaynes BN. Interventions to prevent perinatal depression: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2019;321(6):588–601.
Singla DR, Savel K, Dennis C-L, Kim J, Silver RK, Vigod S, et al. Scaling up mental healthcare for perinatal populations: is telemedicine the answer? Curr Psychiatry Rep. 2022;24:881–7.
Singla DR, Lawson A, Kohrt BA, Jung JW, Meng Z, Ratjen C, et al. Implementation and effectiveness of nonspecialist-delivered interventions for perinatal mental health in high-income countries: a systematic review and meta-analysis. JAMA Psychiat. 2021;78(5):498–509.
Kazdin AE. Addressing the treatment gap: a key challenge for extending evidence-based psychosocial interventions. Behav Res Ther. 2017;88:7–18.
Hafeman DM, Schwartz S. Opening the black box: a motivation for the assessment of mediation. Int J Epidemiol. 2009;38(3):838–45.
Kraemer HC. Messages for clinicians: moderators and mediators of treatment outcome in randomized clinical trials. Am J Psychiatry. 2016;173(7):672–9.
Magill M, Kiluk BD, McCrady BS, Tonigan JS, Longabaugh R. Active ingredients of treatment and client mechanisms of change in behavioral treatments for alcohol use disorders: progress 10 years later. Alcohol Clin Exp Res. 2015;39(10):1852–62.
Tissera H, Auger E, Séguin L, Kramer MS, Lydon JE. Happy prenatal relationships, healthy postpartum mothers: a prospective study of relationship satisfaction, postpartum stress, and health. Psychol Health. 2021;36(4):461–77.
Hagaman A, LeMasters K, Zivich PN, Sikander S, Bates LM, Bhalotra S, et al. Longitudinal effects of perinatal social support on maternal depression: a marginal structural modelling approach. J Epidemiol Community Health. 2021;75(10):936–43.
Singla DR, MacKinnon DP, Fuhr DC, Sikander S, Rahman A, Patel V. Multiple mediation analysis of the peer-delivered Thinking Healthy Programme for perinatal depression: findings from two parallel, randomised controlled trials. Br J Psychiatry. 2021;218(3):143–50.
Singla DR, Kumbakumba E, Aboud FE. Effects of a parenting intervention to address maternal psychological wellbeing and child development and growth in rural Uganda: a community-based, cluster randomised trial. Lancet Glob Health. 2015;3(8):e458–69.
McDonald S, Kehler H, Bayrampour H, Fraser-Lee N, Tough S. Risk and protective factors in early child development: results from the All Our Babies (AOB) pregnancy cohort. Res Dev Disabil. 2016;58:20–30.
Dimidjian S, Goodman SH, Sherwood NE, Simon GE, Ludman E, Gallop R, et al. A pragmatic randomized clinical trial of behavioral activation for depressed pregnant women. J Consult Clin Psychol. 2017;85(1):26.
Cooper AA, Clifton EG, Feeny NC. An empirical review of potential mediators and mechanisms of prolonged exposure therapy. Clin Psychol Rev. 2017;56:106–21.
Gros DF, Price M, Strachan M, Yuen EK, Milanak ME, Acierno R. Behavioral activation and therapeutic exposure: an investigation of relative symptom changes in PTSD and depression during the course of integrated behavioral activation, situational exposure, and imaginal exposure techniques. Behav Modif. 2012;36(4):580–99.
Wilhelm FH, Pfaltz MC, Gross JJ, Mauss IB, Kim SI, Wiederhold BK. Mechanisms of virtual reality exposure therapy: the role of the behavioral activation and behavioral inhibition systems. Appl Psychophysiol Biofeedback. 2005;30(3):271–84.
Goldstein BL, Briggs-Gowan MJ, Greene CC, Chang R, Grasso DJ. An item response theory examination of the original and short forms of the Difficulties in Emotion Regulation Scale (DERS) in pregnant women. J Clin Psychol. 2021;77(7):1591–606.
Howard LM, Megnin-Viggars O, Symington I, Pilling S, Guideline DG. Antenatal and postnatal mental health: summary of updated NICE guidance. BMJ. 2014;18(349): g7394.
Vigod SN, Stewart DE. Postpartum depression. N Engl J Med. 2017;376(9):895.
Meltzer-Brody S, Colquhoun H, Riesenberg R, Epperson CN, Deligiannidis KM, Rubinow DR, et al. Brexanolone injection in post-partum depression: two multicentre, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet. 2018;392(10152):1058–70.
Kanes S, Colquhoun H, Gunduz-Bruce H, Raines S, Arnold R, Schacterle A, et al. Brexanolone (SAGE-547 injection) in post-partum depression: a randomised controlled trial. Lancet. 2017;390(10093):480–9.
Kanes SJ, Colquhoun H, Doherty J, Raines S, Hoffmann E, Rubinow DR, et al. Open-label, proof-of-concept study of brexanolone in the treatment of severe postpartum depression. Hum Psychopharmacol. 2017;32(2):e2576.
FDA approves first oral treatment for postpartum depression. 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-oral-treatment-postpartum-depression . Accessed 09 Aug 2023.
Konstantinou GN, Vigod SN, Mehta S, Daskalakis ZJ, Blumberger DM. A systematic review of non-invasive neurostimulation for the treatment of depression during pregnancy. J Affect Disord. 2020;01(272):259–68.
Gressier F, Rotenberg S, Cazas O, Hardy P. Postpartum electroconvulsive therapy: a systematic review and case report. Gen Hosp Psychiatry. 2015;37(4):310–4.
Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: section 3. Pharmacological treatments. Can J Psychiatry. 2016;61(9):540–60.
Brown JVE, Wilson CA, Ayre K, Robertson L, South E, Molyneaux E, et al. Antidepressant treatment for postnatal depression. Cochrane Database Syst Rev. 2021;2(2):CD013560.
Schoretsanitis G, Westin AA, Stingl JC, Deligiannidis KM, Paulzen M, Spigset O. Antidepressant transfer into amniotic fluid, umbilical cord blood & breast milk: a systematic review & combined analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2021;20(107): 110228.
Weissman AM, Levy BT, Hartz AJ, Bentler S, Donohue M, Ellingrod VL, et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiatry. 2004;161(6):1066–78.
Orsolini L, Bellantuono C. Serotonin reuptake inhibitors and breastfeeding: a systematic review. Hum Psychopharmacol Clin Exp. 2015;30(1):4–20.
Article CAS Google Scholar
Huybrechts KF, Palmsten K, Avorn J, Cohen LS, Holmes LB, Franklin JM, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397–407.
Sriraman NK, Melvin K, Meltzer-Brody S. ABM Clinical Protocol #18: use of antidepressants in breastfeeding mothers. Breastfeed Med. 2015;10(6):290–9.
Smit M, Dolman KM, Honig A. Mirtazapine in pregnancy and lactation—a systematic review. Eur Neuropsychopharmacol. 2016;26(1):126–35.
Drugs and Lactation Database (LactMed®). 2006.
Gentile S. Tricyclic antidepressants in pregnancy and puerperium. Expert Opin Drug Saf. 2014;13(2):207–25.
Sharma V, Sommerdyk C, Xie B. Aripiprazole augmentation of antidepressants for postpartum depression: a preliminary report. Arch Womens Ment Health. 2015;18(1):131–4.
Kittel-Schneider S, Felice E, Buhagiar R, Lambregtse-van den Berg M, Wilson CA, Banjac Baljak V, et al. Treatment of peripartum depression with antidepressants and other psychotropic medications: a synthesis of clinical practice guidelines in Europe. Int J Environ Res Public Health. 2022;19(4):1973.
Misri S, Corral M, Wardrop AA, Kendrick K. Quetiapine augmentation in lactation: a series of case reports. J Clin Psychopharmacol. 2006;26(5):508–11.
Lee A, Giesbrecht E, Dunn E, Ito S. Excretion of quetiapine in breast milk. Am J Psychiatry. 2004;161:1715–6.
Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther. 2021;28(1):e118–26.
Fortinguerra F, Clavenna A, Bonati M. Psychotropic drug use during breastfeeding: a review of the evidence. Pediatrics. 2009;124(4):e547–56.
Olanzapine. 2022. https://www.ncbi.nlm.nih.gov/sites/books/NBK501056/ . Accessed 11 July 2023.
Gilad O, Merlob P, Stahl B, Klinger G. Outcome of infants exposed to olanzapine during breastfeeding. Breastfeed Med. 2011;6(2):55–8.
Hale T. Medications and mothers’ milk. Amarillo: Hale Publishing; 2014.
Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384(9956):1775–88.
Kelly LE, Poon S, Madadi P, Koren G. Neonatal benzodiazepines exposure during breastfeeding. J Pediatr. 2012;161(3):448–51.
Kohen D. Psychotropic medication and breast-feeding. Adv Psychiatr Treat. 2005;11(5):371–9.
Zolpidem. 2023. https://www.ncbi.nlm.nih.gov/books/NBK501265/ . Accessed 11 July 2023.
Pregnancy and breastfeeding treatment of psychiatric and substance misuse disorders. CNWL NHS Foundation Trust; 2017. https://www.transformationpartners.nhs.uk/wp-content/uploads/2019/05/Pre-conception-advice-Best-Practice-Toolkit-for-Perinatal-Mental-Health-Services.pdf .
MacKenzie G, Maguire J. The role of ovarian hormone-derived neurosteroids on the regulation of GABAA receptors in affective disorders. Psychopharmacology. 2014;231(17):3333–42.
Schiller CE, Meltzer-Brody S, Rubinow DR. The role of reproductive hormones in postpartum depression. CNS Spectr. 2015;20(1):48–59.
Wald J, Henningsson A, Hanze E, Hoffmann E, Li H, Colquhoun H, et al. Allopregnanolone concentrations in breast milk and plasma from healthy volunteers receiving brexanolone injection, with population pharmacokinetic modeling of potential relative infant dose. Clin Pharmacokinet. 2022;61(9):1307–19.
Deligiannidis KM, Meltzer-Brody S, Maximos B, Peeper EQ, Freeman M, Lasser R, et al. Zuranolone for the treatment of postpartum depression. Am J Psychiatry. 2023;180:668–75.
Byatt N, Simas TAM, Lundquist RS, Johnson JV, Ziedonis DM. Strategies for improving perinatal depression treatment in North American outpatient obstetric settings. J Psychosom Obstet Gynecol. 2012;33(4):143–61.
Byatt N, Biebel K, Lundquist RS, Moore Simas TA, Debordes-Jackson G, Allison J, et al. Patient, provider, and system-level barriers and facilitators to addressing perinatal depression. J Reprod Infant Psychol. 2012;30(5):436–49.
Hicks LM, Ou C, Charlebois J, Tarasoff L, Pawluski J, Roos LE, et al. Assessment of Canadian perinatal mental health services from the provider perspective: where can we improve? Front Psychiatry. 2022;13: 929496.
Bruckner TA, Scheffler RM, Shen G, Yoon J, Chisholm D, Morris J, et al. The mental health workforce gap in low- and middle-income countries: a needs-based approach. Bull World Health Organ. 2011;89(3):184–94.
Bayrampour H, Hapsari AP, Pavlovic J. Barriers to addressing perinatal mental health issues in midwifery settings. Midwifery. 2018;59:47–58.
Byatt N, Biebel K, Friedman L, Debordes-Jackson G, Ziedonis D, Pbert L. Patient’s views on depression care in obstetric settings: how do they compare to the views of perinatal health care professionals? Gen Hosp Psychiatry. 2013;35(6):598–604.
Kim JJ, La Porte LM, Corcoran M, Magasi S, Batza J, Silver RK. Barriers to mental health treatment among obstetric patients at risk for depression. Am J Obstet Gynecol. 2010;202(3):312.e1-5.
DiBari JN, Yu SM, Chao SM, Lu MC. Use of postpartum care: predictors and barriers. J Pregnancy. 2014;2014: 530769.
Sambrook Smith M, Lawrence V, Sadler E, Easter A. Barriers to accessing mental health services for women with perinatal mental illness: systematic review and meta-synthesis of qualitative studies in the UK. BMJ Open. 2019;9(1): e024803.
Megnin-Viggars O, Symington I, Howard LM, Pilling S. Experience of care for mental health problems in the antenatal or postnatal period for women in the UK: a systematic review and meta-synthesis of qualitative research. Arch Womens Ment Health. 2015;18(6):745–59.
Evagorou O, Arvaniti A, Samakouri M. Cross-cultural approach of postpartum depression: manifestation, practices applied, risk factors and therapeutic interventions. Psychiatr Q. 2016;87(1):129–54.
Callister LC, Beckstrand RL, Corbett C. Postpartum depression and help-seeking behaviors in immigrant Hispanic women. J Obstet Gynecol Neonatal Nurs. 2011;40(4):440–9.
Singla DR, Meltzer-Brody S, Savel K, Silver RK. Scaling up patient-centered psychological treatments for perinatal depression in the wake of a global pandemic. Front Psychiatry. 2022. https://doi.org/10.3389/fpsyt.2021.826019 .
Wichman CL, Laszewski A, Doering JJ, Borchardt S. Feasibility of model adaptations and implementation of a perinatal psychiatric teleconsultation program. Gen Hosp Psychiatry. 2019;59:51–7.
Dennis C-L, Grigoriadis S, Zupancic J, Kiss A, Ravitz P. Telephone-based nurse-delivered interpersonal psychotherapy for postpartum depression: nationwide randomised controlled trial. Br J Psychiatry. 2020;216(4):189–96.
Dennis CL. The effect of peer support on postpartum depression: a pilot randomized controlled trial. Can J Psychiatry. 2003;48(2):115–24.
Letourneau N, Stewart M, Dennis CL, Hegadoren K, Duffett-Leger L, Watson B. Effect of home-based peer support on maternal-infant interactions among women with postpartum depression: a randomized, controlled trial. Int J Ment Health Nurs. 2011;20(5):345–57.
Vigod SN, Slyfield Cook G, Macdonald K, Hussain-Shamsy N, Brown HK, de Oliveira C, et al. Mother matters: pilot randomized wait-list controlled trial of an online therapist-facilitated discussion board and support group for postpartum depression symptoms. Depress Anxiety. 2021;38(8):816–25.
Zhou C, Hu H, Wang C, Zhu Z, Feng G, Xue J, et al. The effectiveness of mHealth interventions on postpartum depression: a systematic review and meta-analysis. J Telemed Telecare. 2022;28(2):83–95.
Vigod SN, Dennis CL. Advances in virtual care for perinatal mental disorders. World Psychiatry. 2020;19(3):328–9.
Organization WH. Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines. 2007.
Singla DR, Lawson A, Kohrt BA, Jung JW, Meng Z, Ratjen C, et al. Implementation and effectiveness of nonspecialist-delivered interventions for perinatal mental health in high-income countries. JAMA Psychiat. 2021;78(5):498.
Fang Q, Lin L, Chen Q, Yuan Y, Wang S, Zhang Y, et al. Effect of peer support intervention on perinatal depression: a meta-analysis. Gen Hosp Psychiatry. 2022;74:78–87.
Dennis CL. Psychosocial interventions for the treatment of perinatal depression. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):97–111.
Leung SS, Lee AM, Chiang VC, Lam SK, Kuen YW, Wong DF. Culturally sensitive, preventive antenatal group cognitive-behavioural therapy for Chinese women with depression. Int J Nurs Pract. 2013;19(Suppl 1):28–37.
Singla DR, Hossain S, Andrejek N, Cohen MJ, Dennis C-L, Kim J, et al. Culturally sensitive psychotherapy for perinatal women: a mixed methods study. J Consult Clin Psychol. 2022;90(10):770–86.
Moore Simas TA, Flynn MP, Kroll-Desrosiers AR, Carvalho SM, Levin LL, Biebel K, et al. A systematic review of integrated care interventions addressing perinatal depression care in ambulatory obstetric care settings. Clin Obstet Gynecol. 2018;61(3):573–90.
Pawar D, Huang CC, Wichman C. Co-located perinatal psychiatry clinic: impact of adding a psychologist on clinical quality improvement metrics. J Psychosom Obstet Gynaecol. 2019;40(2):123–7.
Download references
Author information
Authors and affiliations.
Lunenfeld-Tanenbaum Research Institute, Sinai Health, Toronto, Canada
Cindy-Lee Dennis, Daisy R. Singla & Katarina Savel
Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, 155 College Street, Rm 280, Toronto, ON, M6J 1H4, Canada
Cindy-Lee Dennis
Department of Psychiatry, Temerty Faculty of Medicine, University of Toronto, Toronto, Canada
Cindy-Lee Dennis, Daisy R. Singla, Crystal T. Clark, Sophie Grigoriadis & Simone N. Vigod
Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, Toronto, Canada
Daisy R. Singla
Department of Health and Society, University of Toronto, Toronto, Canada
Hilary K. Brown
Women’s College Hospital, Toronto, Canada
Hilary K. Brown, Crystal T. Clark & Simone N. Vigod
Women’s College Research Institute, Toronto, Canada
Sunnybrook Research Institute, Sunnybrook Health Sciences Centre, Toronto, Canada
Sophie Grigoriadis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Cindy-Lee Dennis .
Ethics declarations
The other authors have no disclosures.
Conflict of interest
Dr. Vigod receives royalties from UpToDate Inc. for authorship of materials related to depression and pregnancy. Dr. Clark receives consulting fees for Seven Starling as a Mental Health Consultant. Sophie Grigoriadis has received royalties from UpToDate, Compendium of Pharmaceuticals, and IPT to Go outside the submitted work over the last year. The other authors have no disclosures.
Ethics approval
Not applicable.
Consent to participate
Availability of data and material, code availability, author’s contributions.
CLD, DRS and SNV drafted the initial version of this manuscript with significant contributions from KS, HKB, CTC, and SG. All authors have critically reviewed this manuscript, have provided consent for publication, and agree to be accountable for the work.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Dennis, CL., Singla, D.R., Brown, H.K. et al. Postpartum Depression: A Clinical Review of Impact and Current Treatment Solutions. Drugs (2024). https://doi.org/10.1007/s40265-024-02038-z
Download citation
Accepted : 25 April 2024
Published : 30 May 2024
DOI : https://doi.org/10.1007/s40265-024-02038-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Our review of the literature led to a number of key observations. As can be seen in Fig. 1, although psychological safety is a multilevel construct, our review suggests that it is likely to be more potent and meaningful at the team level, as opposed to the organizational level, unless the organization is small.This may be the reason why few studies have been conducted at the organizational level.
Since the concept of psychological safety was introduced, empirical research on its antecedents, outcomes, and moderators at different levels of analysis has proliferated. Given a burgeoning body of empirical evidence, a systematic review of the psychological safety literature is warranted. As well as reviewing empirical work on psychological safety, the present article highlights gaps in the ...
Since high psychological safety is a promotor of good communication within teams (allowing those with differing aims and working practices to communicate and work together successfully ), the benefit of this review lies in its potential to further understand how psychological safety has been explored within the clinical literature, looking at ...
Previous literature has shown that psychological safety has a direct influence on work performance (Baer and Frese, 2003; Schaubroeck et al., 2011). Besides, more authors insisted that organizational support, safety climate, and performance are unquestionably related, implying that psychological safety might involve benefits that extend its ...
Since its renaissance in the 1990s, psychological safety research has flourished—a boom motivated by recognition of the challenge of navigating uncertainty and change. Today, its theoretical and practical significance is amplified by the increasingly complex and interdependent nature of the work in organizations. Conceptual and empirical research on psychological safety—a state of reduced ...
Although psychological safety research has flourished in recent years, and despite the empirical support for the important role of psychological safety in the workplace, several critical questions remain. In order to address these questions, we aggregate theoretical and empirical works, and draw on 136 independent samples representing over 22,000 individuals and nearly 5,000 groups, to conduct ...
Newman et al. (2017) who systematically reviewed the psychological safety literature argue that it is often determined based on the assessment of external factors, such as social environment ...
Psychological safety describes people's perceptions of the consequences of taking interpersonal risks in a particular context such as a workplace. First explored by pioneering organizational scholars in the 1960s, psychological safety experienced a renaissance starting in the 1990s and continuing to the present. Organizational research has identified psychological safety as a critical factor ...
extant literature measures psychological safety with the original or an adapted version of the Edmondson's Psychological Safety Scale (PSS) [1]. However, it is important to consider that the conceptualization of psychological safety and the context under which the scale was developed may have evolved since its introduction in 1999.
Psychological safety has emerged as a critical feature of high-performing teams across many industries, including health care. It facilitates patient safety, quality improvement, learning, and innovation. This review presents an overview of psychological safety in medicine, describing its impact on learning, patient safety, and quality improvement.
Network of key variables related to psychological safety based on literature review. psychological safety and influence outcomes such as learning, performance, innovation, and creativity. These occur through facilitation of information sharing, employee voice, feedback seeking, and experimentation (e.g., Carmeli, 2007; Liu et al., 2014).
Psychological safety has emerged as a critical feature of high-performing teams across many industries, including health care. It facilitates patient safety, quality improvement, learning, and innovation. This review presents an overview of psychological safety in medicine, describing its impact on learning, patient safety, and quality improvement.
This evidence synthesis had 3 objectives: explore the current literature regarding psychological safety, identify methods used in its assessment and investigate for evidence of consequences of a psychologically safe environment. Methods: We searched multiple trial registries through December 2018. All studies addressing psychological safety ...
Since the concept of psychological safety was introduced, empirical research on its antecedents, outcomes, and moderators at different levels of analysis has proliferated. Given a burgeoning body of empirical evidence, a systematic review of the psychological safety literature is warranted. As well as reviewing empirical work on psychological safety, the present article highlights gaps in the ...
Psychological safety describes people's perceptions of the consequences of taking interpersonal risks in a particular context such as a workplace. First explored by pioneering organizational ...
Purpose: The current systematic review will identify enablers of psychological safety within the literature in order to produce a comprehensive list of factors that enable psychological safety specific to healthcare teams. Data sources: A keyword search strategy was developed and used to search the following electronic databases PsycINFO, ABI/INFORM, Academic search complete and PubMed and ...
examine the role of national culture in psychological safety perceptions (Edmondson & Lei, 2014). Accordingly, our study contributes to a more contextualized understanding of psychological safety. Finally, we examine and compare the effect sizes of the antecedents and outcomes of psychological safety across individual and group levels of analysis.
Conceptual and empirical research on psychological safety—a state of reduced interpersonal risk—is thus timely, relevant, and extensive. In this article, we review contemporary psychological safety research by describing its various content areas, assessing what has been learned in recent years, and suggesting directions for future research.
Background Psychological safety—speaking up about ideas and concerns, free from interpersonal risk—are essential to the high-risk environment, such as healthcare settings. Psychologically safe working is particularly important in mental health where recovery-oriented approaches rely on collaborative efforts of interprofessional teams to make complex decisions. Much research focuses on ...
We respond directly to Newman et al.'s (2017) call in their review of the psychological safety literature to "to explore possible negative consequences of 'too much' psychological safety at the individual, team, and organizational levels and potential curvilinear effects of psychological safety on outcomes at different levels of ...
However, given the dearth of interventions targeting psychological safety, this review will take a broader view by including interventions targeting speaking up and voice behaviour, which are closely related to psychological safety. ... Newman A, Donohue R, Eva N. Psychological safety: A systematic review of the literature. Hum Res Manag Rev ...
What exactly is psychological safety? It's a term that's used a lot but is often misunderstood. In this piece, the author answers the following questions with input from Harvard Business ...
Background Existing researches on nurses' work engagement and job burnout have mostly stayed at the individual level, and limited researches test the cross-level effects of psychosocial safety climate (PSC). The study aimed to explore the cross-level mediating effect of organization-based self-esteem (OBSE) and the moderating effect of psychological detachment between the relationship of PSC ...
This Year in Review Perspective for 2023 discusses concepts of psychological safety and employee voice, individual and team factors, and leadership and organizational factors related to safety culture. ... et al. Impact of nurse leaders behaviors on nursing staff performance: a systematic review of literature. Inquiry. 2023;60:469580231178528 ...
Depression during the first year postpartum (postpartum depression) impacts millions of women and their families worldwide. In this narrative review, we provide a summary of postpartum depression, examining the etiology and consequences, pharmacological and psychological treatments, and potential mechanisms of change and current barriers to care. Psychological treatments are effective and ...