
How to Beat Asthma
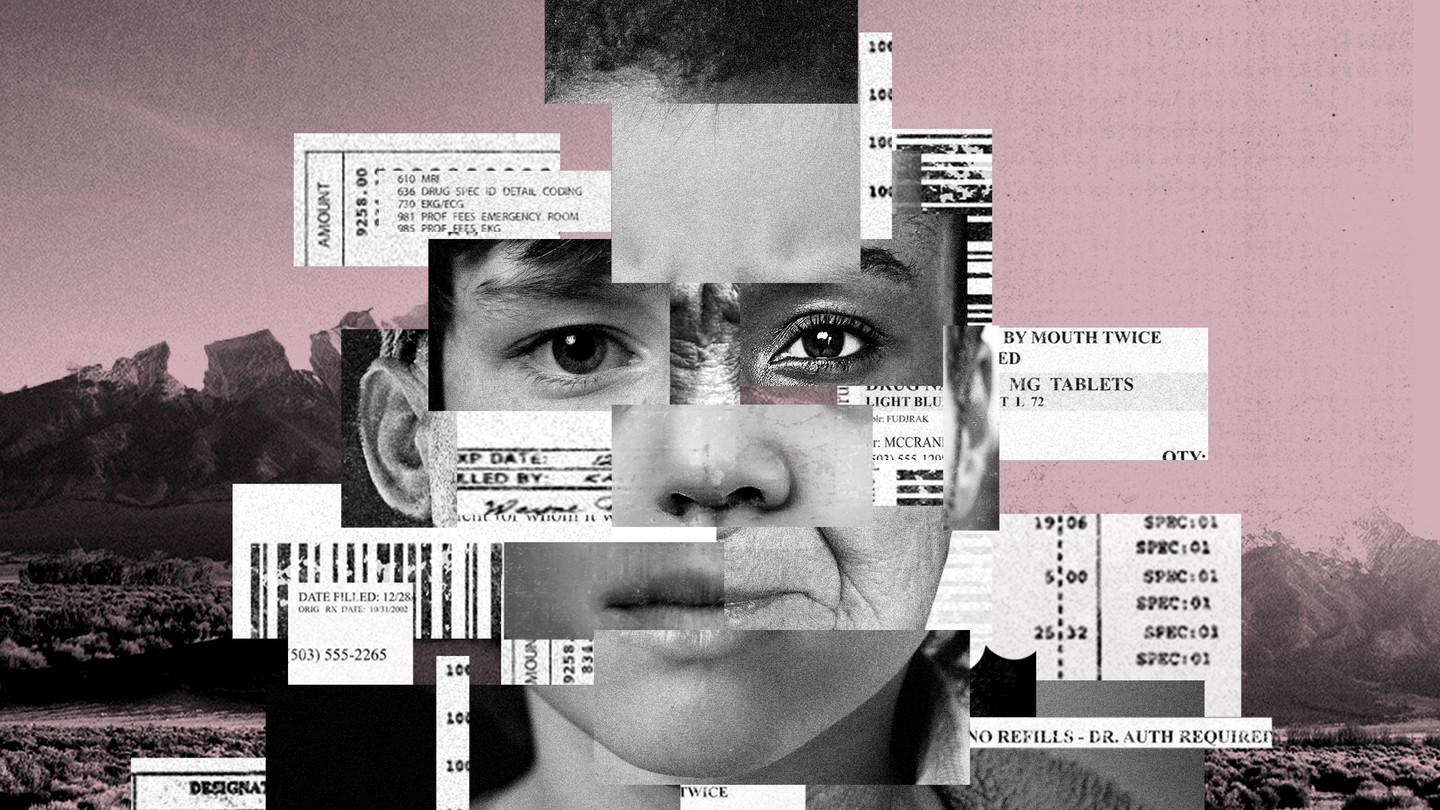
The common lung disease debilitates millions of Americans and costs the country billions of dollars, but some very new—and very old—methods are emerging in fighting it.
DENVER, Colorado—I had my first asthma attack in 10 years while working on this story about asthma.
The day had been a grind. I flew to Denver early on a March morning, hoping to give myself a full day to acclimate to the air before I did some jogging and hiking the next day. From the moment I touched down and took a Lyft away from the Denver airport, that unlucky hellhorse , the afternoon was a blur of reporting. At the end of the day, I found some comfort in a bar with some pretty good draught beers and ahi tuna guacamole. Only, the guacamole I ate turned out to be the version with crabmeat. I’m very allergic to crabmeat.
The reaction started mildly enough: a tingling about the lips, itchy arms, and some slightly constricted nasal airways. Nothing a good dose of Benadryl couldn’t fix (Note: I am a bad patient. Epinephrine auto-injectors are the recommended first-line treatments for food allergies). But on the way to the drug store, something deeper kicked in. The coughs to clear my throat became involuntary and more violent, with the whistling rattle of a wheeze. Each breath felt a little less sufficient than the last, and the effort to inhale began to consume me. The recognition of my old nemesis set in, along with that familiar animal panic. I’m having an attack .
I’d come to the Mile High City in search not of situational irony, but of new ways to fight the lung disease that affects me and almost 25 million other Americans , a cohort that has only grown over the past few years. Asthma is one of the most common chronic diseases in the country, and although it rarely kills on its own, it regularly debilitates people, impairs quality of life , and can lead to a lifetime of emergency-room visits and dangerous comorbidities that themselves shorten lives.
Most people with asthma have at least one attack per year, and the costs compound so much they often destroy households. Asthma costs more than $3,000 per year per person , around $60 billion for the country, and together with COPD it’s one of the five most costly diseases in total. Severe asthma sufferers belong to what we are calling the “ platinum patients ,” or the five percent of Americans responsible for half of all the country’s health-care costs.
There’s no cure for asthma, but the good news about it is that it can be managed, and the problems associated with it are usually directly linked to that management. Asthma also responds to environmental factors that can be identified and mitigated. There are so many ways that life for asthma patients can be improved without ever needing to visit a doctor’s office that it seems impossible to believe that its devastating effects on human life and its swelling costs can’t be beaten. And some of the most effective therapies don’t necessarily involve medicine at all, but changing the environments in which asthmatics live. For public-health officials, changing the very air people breathe might be the way forward.
Thus, Denver. The city is a good-enough case study on how to stem the tide of asthma. Metropolises are notoriously bad places for the condition, and existing evidence suggests that factors like air pollution can spur the development of asthma in children, as well as increase the likelihood of attacks among those kids and adults who already suffer from it. Denver’s a bit of a mixed bag. It is among the most polluted cities in America; in the natural bowl created in the shadow of the mountains, air pollution sometimes pools around the city to make an infamous “brown cloud.” And yet Denver’s been in the top 25 of the hundred largest cities in the country for ease of living with asthma for at least the last two years, according to the Asthma and Allergy Foundation of America .
The city performs especially well in several asthma risk factors. One of those factors is the surrounding environment. Although Denver itself faces pollution challenges, people have come to the greater Denver area for at least a century now to escape the symptoms of asthma. Just north of Denver, in Livermore, dozens of kids with asthma go to the American Lung Association-sponsored Champ Camp to hike and canoe through the forests and rivers spilling down from the Rockies, and in the process grow more resilient to attacks. Leaving the city in other directions or heading into the mountains can provide access to some of the cleanest air around.
But even inside the city, there are some unique factors that make coping with asthma easier than a comparable lowland city. In terms of altitude, at least, Denver is the highest major American city, and thus has some of the thinnest air. That might sound like a bad deal for asthma sufferers—and my lungs certainly weren’t too happy my first time jogging the trails in the foothills of the Rockies in nearby Boulder—but an emerging field of research suggests that the altitude and thin air actually can help people with asthma. In fact, a 2016 meta-analysis of that research in the European Respiratory Journal ’s Open Research imprint finds that 12 weeks of prolonged exposure to altitudes 1,500 meters or more above sea level can be just as effective in controlling asthma as budesonide, a common long-term asthma-control inhaler. Denver is just north of 1,600 meters above sea level.
Some of the perfect people to ask about altitude and asthma actually work in Colorado. The Institute for Altitude Medicine in Telluride, an old mining town in the San Juan Mountains in the southwest corner of the state, is one of the foremost research centers at the intersection of altitude, human performance, and pulmonology. I called its leading altitude expert Peter Hackett just after touching down in Denver to ask about how the air might benefit me.
“There are dozens of papers about asthma and altitude, and in general asthmatics do better when they go to high altitudes,” Hackett told me. “In fact, if you take urban children and take them to high altitudes for a while, their asthma improves. And if you take mountain kids and send them to an urban environment, their asthma gets worse.” As urban, mountain kids, the effects of altitude in Denver are perhaps limited, but they’d do better in New York than kids from New York.
Nobody knows how long those effects hold for people with asthma who head to high altitudes to gain relief from attacks and then go back to lowland areas. Hackett suggests it might be anywhere from a “few days” to months. But at least some evidence suggests that High-Altitude Climate Therapy, as the concept is known in medical circles, actually changes the immunological profile of asthma sufferers, meaning they not only benefit from reduced allergens at high altitudes, but they become less sensitive to existing allergens. If that evidence holds up, it means the therapy could become part of management routines for people with asthma who live in polluted lowland areas.
In essence, the efficacy of High-Altitude Climate Therapy validates some of the oldest therapies humans have on the books. Fresh air works. As my colleague Julie Beck wrote in reflection on her own hike through the Maroon Bells mountains near Aspen, Colorado, nature therapy is proven for a number of diseases and disorders, including several of the comorbidities like high-blood pressure and heart disease that exacerbate—and are exacerbated by—asthma.
For asthmatics, some of the best respites from the constant fear of attacks might come from finding higher ground, clean air, and perhaps the shade of a grove of non-allergenic alpine trees. There’s a beauty in the thin, crisp, clean air at the top of the world, especially when that air’s always a potential menace, waiting to trigger an attack. For people living in Denver, some of the best natural therapy is just a few miles from the city. But their lives are caught between the natural advantages of living at high altitude and the proliferation of polluting industries in the city .
Along with the altitude , there’s also some cutting-edge respiratory and allergy science that helps Denver fight asthma. National Jewish Health, located just south of the impressive green spaces and miniature lake at City Park, is consistently one of the best three research-hospital systems in the country for pulmonology. ( Interesting footnote : The research center was actually founded by the Jewish service organization B'nai B'rith in 1899 at that Denver location at least in part because of the “good air.”)
A few hours before my ill-fated guacamole encounter, I walked a few miles to National Jewish. Pediatric pulmonologist Tod Olin greeted me with enthusiasm. “I just found out I might get to meet Michael Phelps,” he told me. Turns out, Olympic-level swimmers are abnormally likely to have asthma , and Olin’s research helps train them to cope with attacks, and to even use their familiarity with controlled breathing as an advantage. More applicable to my interests, Olin teaches kids the same lessons and helps them be active.
Olin and a roundtable of his colleagues at National Jewish walked me through how their blend of new science and public-health paradigms can help cut costs and improve asthma care. The first such paradigm is a blurring of the traditional distinction between what’s known as severe refractory asthma—a condition where asthmatics regularly have attacks bad enough to land them in hospitals—and the more mundane variety.
If many or most severe asthma cases can be controlled at home, it would mean a world of difference from a spending standpoint. According to Olin’s colleague Rohit Katial, an allergist and immunologist at National Jewish, “[severe cases] use over 50 percent of all resources,” including dollars spent on care and inpatient days, even though people with severe asthma are in the minority. “That's just because they're going in and out of acute-care settings and emergency rooms, and some of that is just because their disease is bad, and some of it is because they're not in a specialist's hands or can't afford medication, or haven't been educated on the use of their medication.”
But that medication has gotten better, too. Since the advent of steroid-based inhalers, asthmatics have tended towards a generalized treatment of cycling on and off whatever medicine seems to work, and a general avoidance strategy of allergens and triggers. It’s what Michael Wechsler, an adult pulmonologist at the center, calls “a specialist’s art.” But now, they have the technology to make it a science.
“We can start to do personalized analysis now to optimize therapy,” Wechsler told me. Physicians can now blend standard data like age, race, and medical history, along with molecular data like the composition and amount of a person’s eosinophils, a type of white blood cell that mediates asthma attacks. They can also gather extensive epidemiological data on triggers, from dust mites to cockroaches to the exposure to cold air on morning runs. Then physicians can prescribe an exact medical routine, dosage, and trigger-allergen analysis. With that appropriate treatment, wasteful prescriptions, inefficient and ever-changing regimens, and hospital visits can all be reduced, which should dramatically lower how much individuals and the system as a whole spend on health care at a national level.
The science goes even further with some of the secret weapons against asthma that National Jewish researchers helped pioneer. Almost the entire field of asthma pharmaceuticals has relied on steroid-based medicines, for long-term care, and emergency asthma medicine. But for select patients—including several whose asthma doesn’t respond well to traditional management—a new set of therapies called monoclonal antibodies are now hitting the market. These wonder “biologic” drugs, the most popular of which is named Omalizumab, help limit the immune response to allergens and triggers and thus the tendency for asthma attacks , and can actually also help limit asthma attacks even among some sufferers who don’t have a clear allergy trigger.
Wechsler and Katial expressed hope that these medicines would fall in cost as they are subject to more research, and would become more widely available as their need became apparent. If so, along with the rise of personalized medicine and more granular specialist-based care for potentially manageable, the field would be on the brink of revolution. If these new medicines and techniques could cut even half of the spending among the group with severe asthma, that would decrease national spending on asthma by something on the order of $15 billion.
Katial is even more optimistic. He thinks that the existence of biologics and the kind of physiological engineering that can reshape asthma in sufferers might even be able to cure it one day. “Maybe 20 years later, if you’re taking some of these new treatments today, you won’t have attacks,” he told me.
Of course, it’s never quite that easy. In addition to the often-inescapable pressures of environment and environmental triggers, one of the underlying reasons for the runaway train of dollars spent and years of life lost to asthma is simply access to good care. Scientists and physicians at National Jewish Health aren’t typical of most areas’ asthma medical experts, and according to Olin there are some whole states and several large rural areas that don’t have pediatric pulmonologists at all.
Lisa Cicutto, the director of community outreach and at National Jewish Health, says that so few people with asthma have access to quality medicine and management early on that they often develop lifelong habits that lend themselves to attacks, like inconsistent inhaler use or failing to identify and remove home allergens. “Because asthma is episodic for a lot of people, when they don't have a lot of symptoms and they aren't really bothered by it, they don't want to do anything,” she said. “They're more on the crisis-reactive, as opposed to a crisis-proactive approach.”
Additionally, the ability to manage and effectively maintain asthma regimens are, like just about everything else, connected to income, free time, and the robustness of services in a person’s community. Those measures are in turn directly connected to where people live, the stress they deal with, the amount of environmental degradation they face, and the factors like cockroaches and smog that in turn trigger attacks.
Combined with the stark lack of specialists and services in the poorest places—both urban and rural—there is simply a monumental amount of problems to fix in the communities where asthma hits hardest before any amount of personalized medicine can help. And that’s not counting any potential change in programs like Medicaid that cover most pediatric asthma hospitalizations — changes that might be on the horizon as Congress considers repealing and replacing Obamacare.
The researchers at National Jewish Health have some solutions for those problems, too. For Cicutto, one possible solution to the shortage of health-care providers in poor areas is mobilizing the people who actually serve as first points of contact for kids with asthma: school nurses. “The school nurse is actually seeing the student all the time, and know when they have problems,” Cicutto said. “I consider them the real primary-care providers here.” For Cicutto, arming school nurses or teachers with students’ asthma profiles and training them on how to teach kids about asthma management could be a simple, yet effective strategy.
Currently, the fragmentation of the health-insurance system and medical-privacy laws make such a seamless integration of school nurses and educational professionals into medicine a tricky prospect. But the idea makes sense. If something approaching a tenth of all children will be diagnosed with asthma, and two of the key deficiencies in asthma treatment are management and education, why not emphasize that education in the places they learn everyday?
Wechsler also pointed me to another line of promising policy research. In some cities, policymakers have had success with creatively limiting the exposure of asthmatics to pollution. For example, in Stockholm, Sweden, a “ congestion tax ” levied by cameras on vehicles in heavy-traffic parts of the city reduced smog and emissions and in turn reduced asthma attacks among kids by as much as 50 percent. One key finding of that experiment is that the main reductions in asthma attacks happened only after a year or longer, which indicates that asthma interventions require patience, and planners and public-health officials have to be in it for the long haul.
These studies and strategies provide some reason for optimism for a way forward. Together, they brought images to my mind of entire communities involved in an integrated asthma-fighting model that treats the home, school, health-care providers, and the environment all as one continuous whole.
One of the worst things about asthma often comes months after an attack. Even for those with insurance, the urgent-care and emergency-room bills, the copays, the costs of tests and overnight stays, the regular cost of upgrading and maintaining asthma devices, and the cost of prescriptions that can often follow severe attacks wreak financial havoc. For people with asthma, these bills are major sources of dread. At worst, they can lead to bankruptcy or other credit disasters.
Add to that the sense of helplessness for people who endure regular attacks, and it’s possible to see how having severe or poorly controlled frequent asthma is a ceaseless cycle of fear. Quite simply, asthma can be a nightmare, even between attacks.
I experienced that nightmare for the first time in years in Denver. Even with insurance, and even in one of the best cities in the world for asthma, with leading asthma researchers at National Jewish ready to for my follow-up call, I was still at the condition’s mercy. But my time hiking around Denver and talking to the foremost experts in the field gave me fresh perspective: With the aid of a blend of personalized medicine, new public-health tools, and new paradigms for deploying these tools, people like me will be more and more likely to be able “to do what they want, when they want, and where they want to do it, and live a normal life,” according to Wechsler.
My last stop in Denver was a salt spa. I’d heard that halotherapy—an alternative-medicine technique where patients sit in a closed cave-like room and inhale aerosolized salt crystals—might be useful for asthmatics. In a touch of irony, the process feels rather like an intensified sensation of inhaling salt spray on coastal beaches, and at least some evidence suggests it might be of some use for asthma, although the overall evidence is mixed for effects on pulmonary diseases.
The spa didn’t do much for me. The air was uncomfortable for me to breathe, and left a tingle in my throat and made my lips dry. I still felt shaky from the previous day’s asthma attack, and unsure whether I should have just scrapped the whole experiment and gone home to order a rescue inhaler for the first time in years.
But, as I sat and inhaled the salt crystals and jotted down my thoughts on the experiment, Tod Olin’s words came to me. “If you look at where asthma was in 1965 versus now,” he’d told me, “lots of people before were basically disabled or worse. Therapies are much better now, and there are so many options to choose from.” The good thing about today is that those options can be as old-school as taking a stroll on a mountain or as advanced as microbiological assays and drugs tailored down to the level of our individual molecules.
And on the horizon, if you squint, perhaps a cure.
This article is part of our project “The Platinum Patients,” which is a collaboration with the Solutions Journalism Network, and is supported by a grant from the Commonwealth Fund.
Logo Left Content

Logo Right Content
Stanford University School of Medicine blog

Breathing: A reflection on living with asthma
We played cards sometimes, my mother and I, during my childhood asthma attacks in the middle of the night. I would creep past the bathroom door and to my parents' bedroom door. Mom , I would whisper. Mom .
That's all I needed to say. She came to the living room, where I waited for her, and stayed up the rest of the night to watch me breathe.
Watching me breathe meant making decisions about whether to call the doctor in the middle of the night or take me into his office in the morning.
Sometimes I put my hands on my head, fingers clasped together because latching them and pressing down on my head created more energy to suck in the next breath. As I grew older, I avoided placing my hands on my head, afraid to tip my mother off about how bad the attack was.
For a long and harrowing attack, she woke my father to drive me out into the night air, which we thought helped with the breathing. We meandered through the neighborhoods bordering the hospitals, looping repeatedly down certain streets, our leisurely pace a sham, because really, he remained close to those hospital entrances in case my breathing worsened, propelling us both into the light and warmth of the busy Emergency Departments.
Sometimes watching me meant making honey, lemon and whiskey toddies, or, if we had no whiskey, just honey and lemon, so the hot liquid could break up the phlegm in my chest. But often, as I sipped on my honey and lemon, my mother rubbed my back and shoulders, which were always hunched down with the effort of breathing. Or pounded between my shoulder blades, another strategy to break up the phlegm.
If the breathing became easier, either on its own or because I'd had some of the medicine stockpiled in our cupboard, and the rattling and wheezing diminished, my mother would pull out the cards. She still needed to watch my progress; neither one of us could rest yet. We would play two-handed Euchre. Or double solitaire.
I don't know how my mother's level of anxiety fluctuated when she watched me breathe through the night, but she never smoked in the house during my asthma attacks. For intense attacks, after waking my father, she might take a break from watching me and go into the backyard with a cigarette to look at the sky. She never fretted in front of me. She remained calm and positive.
During my senior year of high school, after a stressful week of classes, a swine flu shot, and a complicated AP chemistry experiment, I suffered an asthma attack, the worst I'd had in years. My pediatrician instructed the hospital to admit me straight to a floor. Some bureaucratic glitch delayed the delivery of one of those injections I needed to open my airways and help me breathe. My mother, summoned from work, told me to keep going, just a bit longer. Later, I told her, "I think you kept me alive." She told me that she'd never been so worried. She'd thought for sure I was dying.
Years later, when she died, her own breathing remained silent until near the end. Small puffs of sound emerged from her lips, like the snore puffs she'd made on those nights I'd returned from college for a visit and lay awake with the hums and creaks of my childhood home. In the hospital, as she lay dying, her brain stem already dead, I couldn't encourage her as she exhaled her last puffs. I just listened.
"Living is about the breathing," I might have said to my mother on one of those nights I clambered through an attack. We both knew that. But sometimes it helped to hear things aloud.
This piece, originally in longer form , is part of an ongoing collaboration with Months to Years, a nonprofit quarterly publication that showcases nonfiction, poetry and art exploring mortality and terminal illness.
Dawn Newton, a writer in East Lansing, Michigan, was diagnosed with stage IV lung cancer in November 2012 and has lived with asthma all her life. Her memoir, Winded: A Memoir in Four Stages, will be published in October by Apprentice House Press at Loyola University Maryland. Her blog is at www.dawnmarienewton.com .
Photo by Alfonso Cerezo
Related posts

Stanford team tests sleep monitoring for asthma patients

If I knew then what was to come: The importance of getting a colonoscopy
Popular posts.

Is an increase in penile length cause for concern?

From farmworker to doctor: A bold dream is reuniting her with her Indigenous community
- Patient Care & Health Information
- Diseases & Conditions
Physical exam
Your doctor will perform a physical exam to rule out other possible conditions, such as a respiratory infection or chronic obstructive pulmonary disease (COPD). Your doctor will also ask you questions about your signs and symptoms and about any other health problems.
Tests to measure lung function
You may be given lung function tests to determine how much air moves in and out as you breathe. These tests may include:
- Spirometry. This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out.
- Peak flow. A peak flow meter is a simple device that measures how hard you can breathe out. Lower than usual peak flow readings are a sign that your lungs may not be working as well and that your asthma may be getting worse. Your doctor will give you instructions on how to track and deal with low peak flow readings.
Lung function tests often are done before and after taking a medication to open your airways called a bronchodilator (brong-koh-DIE-lay-tur), such as albuterol. If your lung function improves with use of a bronchodilator, it's likely you have asthma.
Additional tests
Other tests to diagnose asthma include:
- Methacholine challenge. Methacholine is a known asthma trigger. When inhaled, it will cause your airways to narrow slightly. If you react to the methacholine, you likely have asthma. This test may be used even if your initial lung function test is normal.
- Imaging tests. A chest X-ray can help identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems.
- Allergy testing. Allergy tests can be performed by a skin test or blood test. They tell you if you're allergic to pets, dust, mold or pollen. If allergy triggers are identified, your doctor may recommend allergy shots.
- Nitric oxide test. This test measures the amount of the gas nitric oxide in your breath. When your airways are inflamed — a sign of asthma — you may have higher than normal nitric oxide levels. This test isn't widely available.
- Sputum eosinophils. This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing. Eosinophils are present when symptoms develop and become visible when stained with a rose-colored dye.
- Provocative testing for exercise and cold-induced asthma. In these tests, your doctor measures your airway obstruction before and after you perform vigorous physical activity or take several breaths of cold air.
How asthma is classified
To classify your asthma severity, your doctor will consider how often you have signs and symptoms and how severe they are. Your doctor will also consider the results of your physical exam and diagnostic tests.
Determining your asthma severity helps your doctor choose the best treatment. Asthma severity often changes over time, requiring treatment adjustments.
Asthma is classified into four general categories:
| Asthma classification | Signs and symptoms |
|---|---|
| Mild intermittent | Mild symptoms up to two days a week and up to two nights a month |
| Mild persistent | Symptoms more than twice a week, but no more than once in a single day |
| Moderate persistent | Symptoms once a day and more than one night a week |
| Severe persistent | Symptoms throughout the day on most days and frequently at night |
- Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your asthma-related health concerns Start Here
More Information
Asthma care at Mayo Clinic
- Asthma: Testing and diagnosis
Prevention and long-term control are key to stopping asthma attacks before they start. Treatment usually involves learning to recognize your triggers, taking steps to avoid triggers and tracking your breathing to make sure your medications are keeping symptoms under control. In case of an asthma flare-up, you may need to use a quick-relief inhaler.
Medications
The right medications for you depend on a number of things — your age, symptoms, asthma triggers and what works best to keep your asthma under control.
Preventive, long-term control medications reduce the swelling (inflammation) in your airways that leads to symptoms. Quick-relief inhalers (bronchodilators) quickly open swollen airways that are limiting breathing. In some cases, allergy medications are necessary.
Long-term asthma control medications, generally taken daily, are the cornerstone of asthma treatment. These medications keep asthma under control on a day-to-day basis and make it less likely you'll have an asthma attack. Types of long-term control medications include:
Inhaled corticosteroids. These medications include fluticasone propionate (Flovent HFA, Flovent Diskus, Xhance), budesonide (Pulmicort Flexhaler, Pulmicort Respules, Rhinocort), ciclesonide (Alvesco), beclomethasone (Qvar Redihaler), mometasone (Asmanex HFA, Asmanex Twisthaler) and fluticasone furoate (Arnuity Ellipta).
You may need to use these medications for several days to weeks before they reach their maximum benefit. Unlike oral corticosteroids, inhaled corticosteroids have a relatively low risk of serious side effects.
Leukotriene modifiers. These oral medications — including montelukast (Singulair), zafirlukast (Accolate) and zileuton (Zyflo) — help relieve asthma symptoms.
Montelukast has been linked to psychological reactions, such as agitation, aggression, hallucinations, depression and suicidal thinking. Seek medical advice right away if you experience any of these reactions.
- Combination inhalers. These medications — such as fluticasone-salmeterol (Advair HFA, Airduo Digihaler, others), budesonide-formoterol (Symbicort), formoterol-mometasone (Dulera) and fluticasone furoate-vilanterol (Breo Ellipta) — contain a long-acting beta agonist along with a corticosteroid.
- Theophylline. Theophylline (Theo-24, Elixophyllin, Theochron) is a daily pill that helps keep the airways open by relaxing the muscles around the airways. It's not used as often as other asthma medications and requires regular blood tests.
Quick-relief (rescue) medications are used as needed for rapid, short-term symptom relief during an asthma attack. They may also be used before exercise if your doctor recommends it. Types of quick-relief medications include:
Short-acting beta agonists. These inhaled, quick-relief bronchodilators act within minutes to rapidly ease symptoms during an asthma attack. They include albuterol (ProAir HFA, Ventolin HFA, others) and levalbuterol (Xopenex, Xopenex HFA).
Short-acting beta agonists can be taken using a portable, hand-held inhaler or a nebulizer, a machine that converts asthma medications to a fine mist. They're inhaled through a face mask or mouthpiece.
- Anticholinergic agents. Like other bronchodilators, ipratropium (Atrovent HFA) and tiotropium (Spiriva, Spiriva Respimat) act quickly to immediately relax your airways, making it easier to breathe. They're mostly used for emphysema and chronic bronchitis, but can be used to treat asthma.
- Oral and intravenous corticosteroids. These medications — which include prednisone (Prednisone Intensol, Rayos) and methylprednisolone (Medrol, Depo-Medrol, Solu-Medrol) — relieve airway inflammation caused by severe asthma. They can cause serious side effects when used long term, so these drugs are used only on a short-term basis to treat severe asthma symptoms.
If you have an asthma flare-up, a quick-relief inhaler can ease your symptoms right away. But you shouldn't need to use your quick-relief inhaler very often if your long-term control medications are working properly.
Keep a record of how many puffs you use each week. If you need to use your quick-relief inhaler more often than your doctor recommends, see your doctor. You probably need to adjust your long-term control medication.
Allergy medications may help if your asthma is triggered or worsened by allergies. These include:
- Allergy shots (immunotherapy). Over time, allergy shots gradually reduce your immune system reaction to specific allergens. You generally receive shots once a week for a few months, then once a month for a period of three to five years.
- Biologics. These medications — which include omalizumab (Xolair), mepolizumab (Nucala), dupilumab (Dupixent), reslizumab (Cinqair) and benralizumab (Fasenra) — are specifically for people who have severe asthma.
Bronchial thermoplasty
This treatment is used for severe asthma that doesn't improve with inhaled corticosteroids or other long-term asthma medications. It isn't widely available nor right for everyone.
During bronchial thermoplasty, your doctor heats the insides of the airways in the lungs with an electrode. The heat reduces the smooth muscle inside the airways. This limits the ability of the airways to tighten, making breathing easier and possibly reducing asthma attacks. The therapy is generally done over three outpatient visits.
Treat by severity for better control: A stepwise approach
Your treatment should be flexible and based on changes in your symptoms. Your doctor should ask about your symptoms at each visit. Based on your signs and symptoms, your doctor can adjust your treatment accordingly.
For example, if your asthma is well controlled, your doctor may prescribe less medication. If your asthma isn't well controlled or is getting worse, your doctor may increase your medication and recommend more-frequent visits.
Asthma action plan
Work with your doctor to create an asthma action plan that outlines in writing when to take certain medications or when to increase or decrease the dose of your medications based on your symptoms. Also include a list of your triggers and the steps you need to take to avoid them.
Your doctor may also recommend tracking your asthma symptoms or using a peak flow meter on a regular basis to monitor how well your treatment is controlling your asthma.
- Asthma inhalers: Which one's right for you?
- Asthma medications
- Asthma treatment: 3 steps
- Allergy shots
- Dry powder disk inhaler
- Dry powder tube inhaler
- Single-dose dry powder inhaler
- Using a metered dose asthma inhaler and spacer
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Although many people with asthma rely on medications to prevent and relieve symptoms, you can do several things on your own to maintain your health and lessen the possibility of asthma attacks.
Avoid your triggers
Taking steps to reduce your exposure to asthma triggers is a key part of asthma control. To reduce your exposure, you should:
- Use your air conditioner. Air conditioning reduces the amount of airborne pollen from trees, grasses and weeds that finds its way indoors. Air conditioning also lowers indoor humidity and can reduce your exposure to dust mites. If you don't have air conditioning, try to keep your windows closed during pollen season.
- Decontaminate your decor. Minimize dust that may worsen nighttime symptoms by replacing certain items in your bedroom. For example, encase pillows, mattresses and box springs in dustproof covers. Avoid using down-filled pillows and blankets. Throughout the house, remove carpeting and install hardwood or linoleum flooring. Use washable curtains and blinds.
- Maintain optimal humidity. If you live in a damp climate, talk to your doctor about using a dehumidifier.
- Prevent mold spores. Clean damp areas in the bathroom, kitchen and around the house to keep mold spores from developing. Get rid of moldy leaves or damp firewood in the yard.
- Reduce pet dander. If you're allergic to dander, avoid pets with fur or feathers. Having pets regularly bathed or groomed may also reduce the amount of dander in your surroundings.
- Clean regularly. Clean your home at least once a week. If you're likely to stir up dust, wear a mask or have someone else do the cleaning. Wash your bedding regularly.
- Cover your nose and mouth if it's cold out. If your asthma is worsened by cold or dry air, wearing a face mask can help.
Stay healthy
Taking care of yourself can help keep your symptoms under control, including:
Get regular exercise. Having asthma doesn't mean you have to be less active. Treatment can prevent asthma attacks and control symptoms during activity.
Regular exercise can strengthen your heart and lungs, which helps relieve asthma symptoms. If you exercise in cold temperatures, wear a face mask to warm the air you breathe.
- Maintain a healthy weight. Being overweight can worsen asthma symptoms, and it puts you at higher risk of other health problems.
- Control heartburn and gastroesophageal reflux disease (GERD). It's possible that the acid reflux that causes heartburn may damage lung airways and worsen asthma symptoms. If you have frequent or constant heartburn, talk to your doctor about treatment options. You may need treatment for GERD before your asthma symptoms improve.
- Asthma diet
- Ozone air purifiers
- Video: How to use a peak flow meter
Alternative medicine
Certain alternative treatments may help with asthma symptoms. However, keep in mind that these treatments are not a replacement for medical treatment, especially if you have severe asthma. Talk to your doctor before taking any herbs or supplements, as some may interact with the medications you take.
In most cases, more research is needed to see how well alternative remedies work and to measure the extent of possible side effects. Alternative asthma treatments include:
- Breathing exercises. These exercises may reduce the amount of medication you need to keep your asthma symptoms under control.
- Herbal and natural remedies. A few herbal and natural remedies that may help improve asthma symptoms include black seed, caffeine, choline and pycnogenol.
Coping and support
Asthma can be challenging and stressful. You may sometimes become frustrated, angry or depressed because you need to cut back on your usual activities to avoid environmental triggers. You may also feel limited or embarrassed by the symptoms of the disease and by complicated management routines.
But asthma doesn't have to be a limiting condition. The best way to overcome anxiety and a feeling of helplessness is to understand your condition and take control of your treatment. Here are some suggestions that may help:
- Pace yourself. Take breaks between tasks and avoid activities that make your symptoms worse.
- Make a daily to-do list. This may help you avoid feeling overwhelmed. Reward yourself for accomplishing simple goals.
- Talk to others with your condition. Chat rooms and message boards on the internet or support groups in your area can connect you with people facing similar challenges and let you know that you're not alone.
- If your child has asthma, be encouraging. Focus attention on the things your child can do, not on the things he or she can't. Involve teachers, school nurses, coaches, friends and relatives in helping your child manage asthma.
Preparing for your appointment
You're likely to start by seeing your family doctor or a general practitioner. However, when you call to set up an appointment, you may be referred to an allergist or a pulmonologist.
Because appointments can be brief, and because there's often a lot of ground to cover, it's a good idea to be well prepared. Here's some information to help you get ready for your appointment, as well as what to expect from your doctor.
What you can do
These steps can help you make the most of your appointment:
- Write down any symptoms you're having, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Note when your symptoms bother you most. For example, write down if your symptoms tend to get worse at certain times of the day, during certain seasons, or when you're exposed to cold air, pollen or other triggers.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins and supplements that you're taking.
- Take a family member or friend along, if possible. Sometimes it can be difficult to recall all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Your time with your doctor is limited, so preparing a list of questions will help you make the most of your time together. List your questions from most important to least important in case time runs out. For asthma, some basic questions to ask your doctor include:
- Is asthma the most likely cause of my breathing problems?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What kinds of tests do I need?
- Is my condition likely temporary or chronic?
- What's the best treatment?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a specialist?
- Is there a generic alternative to the medicine you're prescribing me?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend visiting?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may reserve time to go over any points you want to spend more time on. Your doctor may ask:
- What exactly are your symptoms?
- When did you first notice your symptoms?
- How severe are your symptoms?
- Do you have breathing problems most of the time or only at certain times or in certain situations?
- Do you have allergies, such as atopic dermatitis or hay fever?
- What, if anything, appears to worsen your symptoms?
- What, if anything, seems to improve your symptoms?
- Do allergies or asthma run in your family?
- Do you have any chronic health problems?
- Weinberger SE, et al. Asthma. In: Principles of Pulmonary Medicine. 7th ed. Elsevier; 2019. https://www.clinicalkey.com. Accessed March 30, 2020.
- Asthma. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/asthma. Accessed March 25, 2020.
- AskMayoExpert. Asthma (adult). Mayo Clinic; 2020.
- Global strategy for asthma management and prevention (2019 update). Global Initiative for Asthma. https://ginasthma.org/gina-reports/. Accessed March 27, 2020.
- Khurana S, et al. Systematic approach to asthma of varying severity. Clinics in Chest Medicine. 2019; doi:10.1016/j.ccm.2018.10.004.
- Ferri FF. Asthma. In: Ferri's Clinical Advisor 2020. Elsevier; 2020. https://www.clinicalkey.com. Accessed March 30, 2020.
- Wu TD, et al. Asthma in the primary care setting. Medical Clinics of North America. 2019; doi:10.1016/j.mcna.2018.12.004.
- Fanta CH. An overview of asthma management. https://www.uptodate.com/contents/search. Accessed March 30, 2020.
- Santino TA, et al. Breathing exercises for adults with asthma. Cochrane Database of Systematic Reviews. 2020; doi:10.1002/14651858.CD001277.pub4.
- Amaral-Machado L, et al. Use of natural products in asthma treatment. Evidence-based Complementary and Alternative Medicine. 2020; doi:10.1155/2020/1021258.
- Montelukast. IBM Micromedex. https://www.micromedexsoluitions.com. Accessed April 6, 2020.
- Whyand T, et al. Pollution and respiratory disease: Can diet or supplements help? A review. Respiratory Research. 2018; doi:10.1186/s12931-018-0785-0.
- O'Keefe JH, et al. Coffee for cardioprotection and longevity. Progress in Cardiovascular Diseases. 2018; doi:10.1016/j.pcad.2018.02.002.
- Allergies and asthma
- Asthma and acid reflux
- Vocal cord dysfunction
- What is aspirin-exacerbated respiratory disease (AERD)?
Associated Procedures
News from mayo clinic.
- Mayo Clinic Minute: Can aspirin make your breathing worse? March 26, 2024, 04:00 p.m. CDT
- Mayo Clinic Minute: How to use an asthma inhaler Sept. 22, 2023, 04:00 p.m. CDT
- Mayo Clinic Minute: Signs and symptoms of asthma April 24, 2023, 04:30 p.m. CDT
Products & Services
- A Book: Mayo Clinic Guide to Home Remedies
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.

Presentations made painless
- Get Premium
110 Asthma Essay Topic Ideas & Examples
Inside This Article
Asthma is a chronic respiratory condition that affects millions of people worldwide. It is a complex disease that can have a significant impact on a person's quality of life. If you are tasked with writing an essay on asthma, you might be wondering where to start. To help you out, here are 110 asthma essay topic ideas and examples that will inspire you to write an engaging and informative essay.
Understanding Asthma:
- What is asthma? Exploring the basics of this respiratory condition.
- Historical overview of asthma: From ancient times to modern understanding.
- The prevalence of asthma worldwide: A global perspective.
- The impact of asthma on public health.
- Differentiating between asthma and other respiratory diseases.
- The role of genetics in asthma: Exploring the hereditary factors.
- Asthma in children: Understanding the unique challenges.
- Adult-onset asthma: Causes, symptoms, and management.
- The economic burden of asthma on individuals and society.
- The psychological impact of living with asthma.
Causes and Risk Factors:
- Environmental triggers of asthma: Pollutants, allergens, and irritants.
- Genetic predisposition to asthma: Unraveling the role of genes.
- The hygiene hypothesis and its relationship to asthma.
- Occupational asthma: Risks and preventive measures.
- Asthma and obesity: Understanding the connection.
- The role of stress in asthma exacerbations.
- Asthma and smoking: The detrimental effects of tobacco.
- The impact of air pollution on asthma prevalence.
- The influence of diet on asthma symptoms.
- Asthma and allergies: The intricate relationship.
Symptoms and Diagnosis:
- Identifying asthma symptoms: From wheezing to shortness of breath.
- The significance of peak flow measurements in asthma diagnosis.
- The use of spirometry in diagnosing and monitoring asthma.
- Differentiating between asthma exacerbations and other respiratory conditions.
- The role of allergy testing in diagnosing allergic asthma.
- Asthma management based on symptom severity.
- The importance of early asthma diagnosis in children.
- Asthma in the elderly: Challenges in diagnosis and management.
- The impact of gender on asthma symptoms and diagnosis.
- Asthma and vocal cord dysfunction: Overlapping symptoms.
Treatment and Management:
- Asthma medication: An overview of the different types.
- Inhalers and nebulizers: Advantages and disadvantages.
- The role of corticosteroids in managing asthma.
- Long-term control medications vs. quick-relief medications.
- The effectiveness of alternative and complementary therapies in asthma management.
- Asthma action plans: Educating patients on self-management.
- The importance of regular follow-ups in asthma management.
- Asthma self-monitoring: The use of peak flow meters and symptom diaries.
- The role of patient education in improving asthma outcomes.
- The benefits of pulmonary rehabilitation in asthma management.
Asthma and Coexisting Conditions:
- Asthma and allergic rhinitis: Understanding the link.
- The relationship between asthma and gastroesophageal reflux disease (GERD).
- Asthma and sleep apnea: A potentially dangerous combination.
- The connection between asthma and chronic sinusitis.
- Psychological comorbidities in asthma patients: Anxiety and depression.
- Asthma and obesity: The impact on disease severity and treatment response.
- Asthma and cardiovascular disease: Shared risk factors and implications.
- Asthma and pregnancy: Balancing treatment and fetal health.
- The impact of asthma on the elderly population with multiple chronic conditions.
- Asthma and autoimmune diseases: Examining the potential associations.
Asthma in Special Populations:
- Asthma in children: Effective management strategies for pediatric patients.
- Challenges in diagnosing and managing asthma in infants.
- Asthma in school-aged children: The importance of asthma-friendly schools.
- Asthma in teenagers: Addressing adherence and lifestyle factors.
- Asthma in athletes: Managing symptoms while maintaining performance.
- Asthma in the elderly: Strategies for improving disease control.
- Asthma in pregnant women: Balancing treatment and fetal health.
- Asthma in minority populations: Disparities in diagnosis and management.
- Asthma in low-income communities: Barriers to care and potential solutions.
- Asthma in developing countries: Addressing challenges in resource-limited settings.
Asthma Research and Future Directions:
- The latest breakthroughs in asthma research: Promising discoveries and advancements.
- Precision medicine in asthma: Tailoring treatment based on individual characteristics.
- The potential role of microbiota in asthma development and management.
- Stem cell therapy for asthma: Current status and future prospects.
- The impact of artificial intelligence in asthma management.
- Asthma and personalized digital health: Exploring new technologies.
- The potential of targeted biologic therapies in severe asthma.
- Asthma prevention strategies: Can we stop it before it starts?
- The future of asthma treatment: Novel therapeutic approaches.
- Asthma research in developing countries: Addressing global disparities.
Asthma Education and Awareness:
- The role of schools in asthma education and management.
- Asthma education campaigns: Evaluating their effectiveness.
- The importance of community-based interventions in asthma prevention.
- Addressing asthma stigma: Promoting understanding and empathy.
- The role of social media in asthma education and support.
- Asthma support groups: Providing a sense of community and resources.
- Asthma education for healthcare professionals: Bridging the knowledge gap.
- The impact of health literacy on asthma outcomes.
- Asthma education in low-income communities: Overcoming barriers.
- The potential role of telemedicine in asthma education and management.
Asthma and Environmental Factors:
- Indoor air quality and asthma: Strategies for reducing triggers at home.
- Outdoor air pollution and asthma: Advocating for cleaner environments.
- The impact of climate change on asthma prevalence and severity.
- Asthma and urbanization: Understanding the urban-rural divide.
- Asthma and housing: The role of substandard living conditions.
- The influence of pets on asthma symptoms and allergen exposure.
- Secondhand smoke and asthma: Protecting vulnerable populations.
- The impact of occupational exposures on asthma development and exacerbations.
- Asthma and mold: Identifying and preventing exposure.
- Asthma and air travel: Navigating the challenges.
Asthma and Policy:
- Asthma management guidelines: A critical analysis of current recommendations.
- Asthma and healthcare disparities: Addressing the unequal burden.
- The impact of health insurance coverage on asthma care.
- School asthma policies: Ensuring a safe and supportive environment.
- Workplace accommodations for employees with asthma.
- Asthma and disability rights: Advocating for equal opportunities.
- The influence of pharmaceutical policies on asthma medication access.
- The role of public health initiatives in reducing asthma prevalence.
- Asthma and emergency preparedness: Ensuring access to care during crises.
- The importance of funding asthma research: Advancing our knowledge.
Living with Asthma:
- Personal experiences with asthma: Sharing stories of resilience and triumph.
- Asthma and physical activity: Overcoming barriers to exercise.
- Asthma and mental health: Nurturing emotional well-being.
- Asthma and sleep disturbances: Strategies for improving sleep quality.
- Asthma and travel: Tips for managing symptoms while exploring the world.
- Coping with asthma as a caregiver: Balancing support and independence.
- Asthma and social life: Navigating social situations and peer pressure.
- Asthma and relationships: Communicating about the condition with loved ones.
- Asthma and self-advocacy: Empowering individuals to take control of their health.
- Asthma and hope: Inspiring stories of individuals thriving despite the condition.
These 110 asthma essay topic ideas and examples cover a wide range of aspects related to asthma, providing you with ample options to choose from. Remember to tailor your essay to your audience, whether it is a scientific paper, a personal narrative, or an advocacy piece. By exploring these topics, you can raise awareness about asthma, educate others, and contribute to the understanding and management of this chronic respiratory condition.
Want to create a presentation now?
Instantly Create A Deck
Let PitchGrade do this for me
Hassle Free
We will create your text and designs for you. Sit back and relax while we do the work.
Explore More Content
- Privacy Policy
- Terms of Service
© 2023 Pitchgrade
Home — Essay Samples — Nursing & Health — Pathophysiology — A Comprehensive Exploration of Asthma
A Comprehensive Exploration of Asthma
- Categories: Pathophysiology
About this sample

Words: 1260 |
Published: Feb 13, 2024
Words: 1260 | Pages: 3 | 7 min read
Table of contents
Acute asthma, chronic asthma, impact of gender on pathophysiology, diagnosis and treatment.
- Centers for Disease Control and Prevention (2018). Asthma. Retrieved from https://www.cdc.gov/nchs/fastats/asthma.htm
- Dodge, R., R., & Burrows, B. (2018). The prevalence and incidence of asthma-like symptoms in a general population sample. Am Rev Respir Dis 2018; 122:567–75.
- Holgate, S., T. (2017). Genetic and environmental interaction in allergy and asthma. J Allergy Clin Immunol 2017; 104: 1139–46
- Lemanske, R., F., & Busse., W., W. (2017). Asthma: Clinical expression and molecular mechanisms. J Allergy Clin Immunol. 2017, 125: S95-102. 10.1016/j.jaci.2009.10.047.
- Mandhane, P., J., Greene, J., M., Cowan, J., O., et al. (2015). Sex differences in factors associated with childhood and adolescent-onset wheeze. Am J Respir Crit Care Med 2015; 172:45–54
- Thomas, A., O., Lemanske, R.., F., & Jackson, D., J. (2014). Infections and their role in childhood asthma inception. Pediatr Allergy Immunol. 2014; 25: 122–128
- Wright, A., L., Stern, D., A., Kauffmann, F., et al. (2016). Factors influencing gender differences in the diagnosis and treatment of asthma in childhood: the Tucson Children' s Respiratory Study. Pediatr Pulmonol 2016; 41:318–25.
- Wright, A., L., Stern, D., A., Kauffmann, F., et al. (2016). Factors influencing gender differences in the diagnosis and treatment of asthma in childhood: the Tucson Children's Respiratory Study. Pediatr Pulmonol 2016; 41:318–25.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof. Kifaru
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
5 pages / 2415 words
3 pages / 1416 words
1 pages / 620 words
10 pages / 4461 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Pathophysiology
The article called “Frontiers in the Bioarchaeology of Stress and Disease: Cross-Disciplinary Perspectives From Pathophysiology, Human Biology, and Epidemiology” by Haagen D. Klaus (2014) reviews a few different aspects of a [...]
The human body in many ways acts like the Newton’s 3rd law which is for every action, there is an equal and opposite reaction. When the body is going through changes, the body activates the compensatory mechanism. This is what [...]
The patient is a 63-year-old, African-American retired firefighter and whose brother was recently diagnosed with prostate cancer. As a former firefighter, he has been able to maintain a healthy lifestyle with regular vitamin [...]
Anaerobic bacteria do not replicate in the presence of oxygen. Three categories of anaerobic bacteria include obligate anaerobes, aerotolerant anaerobes, and facultative anaerobes. While most species are obligate anaerobes, some [...]
Xenotransplantation could be used to treat severe burns, dealing with the issue of closure and coverage, with the best source currently being fresh cadaver allografts, of which there is a great shortage (Ge, et al., 2010). One [...]
Vesiculobullous disorders represent a heterogenous group of dermatoses with protean manifestations Vesicles and Bullae are fluid filled cavities formed within or beneath the epidermis. In this study, skin punch biopsy is used [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
173 Asthma Essay Topic Ideas & Examples
🏆 best asthma topic ideas & essay examples, 💡 interesting topics to write about asthma, 📑 good research topics about asthma, 📌 simple & easy asthma essay titles, 👍 good essay topics on asthma, ❓ research questions about asthma.
- SOAP Note for an Asthmatic Patient Today, asthma is known as one of the most common respiratory diseases in the United States, as well as in the whole world.
- Asthma Treatment Algorithm for Patients Complete the blanks in the following table to create an algorithm for asthma care using your textbook as well as GINA guidelines.
- Application: Asthma The features of the air passage include the bronchi, alveoli and the bronchioles. The pathophysiology of chronic and acute asthma exacerbation describes the process and stages that lead to airway obstruction.
- Asthma Exacerbation in Pregnancy The patient has a history of childhood asthma diagnosis, and she is presently exhibiting typical asthma symptoms like wheezing and a nonproductive cough.
- Asthma: Epidemiological Analysis and Care Plan Asthma has a variety of symptoms and pathogenesis, including acute, subacute, or chronic inflammation of the airways, intermittent blockage of airflow, and hyperresponsiveness of the bronchi.
- Asthma Diagnosis in Pregnant Women It may be essential to modify the type and dose of medication to compensate for the alterations in the female’s metabolism and the severity of her health condition.
- Healthy Lifestyle Interventions in Comorbid Asthma and Diabetes In most research, the weight loss in cases of comorbid asthma and obesity is reached through a combination of dietary interventions and physical exercise programs.
- Clinical Case of Asthma in African American Boy By combining the use of corticosteroids and exercises into the treatment plan, as well as educating the patient and his parents about the prevention and management of asthma attacks, a healthcare practitioner will be able […]
- Asthma From a Clinic Perspective And the prevalence of asthma in the European Union is 9. In UK and Ireland experience some of the greatest rates of asthma in the globe.
- Corticosteroids and Inhalants in Asthma As well as the causes of fatigue and physiological events during an asthma attack, and how the body compensates for an increase in CO2, with a focus on the effects of hypercapnia on the central […]
- The Treatment Modalities of Asthma However, in order to limit susceptibility to the triggers, the patient is advised to take long-term asthma medications on a daily basis.
- Asthma Diagnostics and Treatment According to the Asthma and Allergy Foundation of America, some of the most common symptoms of asthma include cough, wheezing, shortness of breath, chest tightness, and fainting.
- Asthma: Pathophysiology, Symptoms, and Manifestations The primary organ affected by asthma is the lungs, as the disease is caused by airway narrowing and the inability to breathe.
- Asthma: Description, Diagnosis and Treatment First of all, before discussing measures to prevent an increase in the case of the disease, it is necessary to understand the nature of the disease.
- Inflammation’s Role in Asthma Development This work is written in order to study the role of inflammation plays in the development of asthma on the basis of research papers.
- The Use of Tezspire: The Management of Asthma The brochure describes the use of Tezspire, which is a drug used for the management of asthma. The brochure’s target audience is patients with a long history of asthma and their family and caregivers.
- Asthma Treatment in Pediatric Patients: Spacer vs. Conventional Inhaler Computers and the Internet connection have become available to a considerable portion of the population, which equally serves as a facilitator of the new solution implementation.
- Physical Assessment Report for an 18-Years-Old Asthma Patient The boy and his family suspect that he is suffering frequent asthma attacks due to allergies to cold and dust, however none of his members of the family suffer from asthma.
- Asthma: Pathophysiology, Etiology, Diagnosis, and Complications The pathobiology of asthma remains greatly indeterminate, and its pathophysiology involves abnormalities of the respiratory system organs, including the lungs and the bronchial tree.
- Use of Scientific Method in Asthma and Allergic Reactions Study As in the case of asthma and allergic reactions investigations, descriptive studies can be used to describe the nature of the relationship between asthma and asthma attack, therefore explaining the cause and effect.
- COVID-19 Susceptibility in Bronchial Asthma by Green et al. The research reflected in the article aims to trace the susceptibility of patients with bronchial asthma to coronavirus disease. It is noted that the receptors that respond to those occurring in the environment are the […]
- Exercise-Induced Asthma in Children The onset of an EIA attack follows a constriction of the airways of the patient after physical exercise. When water shifts from the cells of the epithelium to the airway surface, it causes a release […]
- Child Asthma Emergency Department Visits: Plan for the Reduction The population of Central Harlem will be the target of this intervention that aims to decrease the rate of children’s asthma-related ED visits.
- The Child Asthma Emergency Department Visits The program makes it easy for medical caregivers to carry accurate assessments to pediatric patients. The program is easily scalable, and it is also sustainable, making 5A’s the best solution to Child Asthma Emergency Department […]
- Asthma Among Children of Color in New York City On the other hand, the conditioning of the matter to a particular scope hinders the determination of a rational scientific solution to the core issue.
- Asthma in Relation to Inability to Breathe: A Case Study The shortness of breath is known to be a primary cause of Asthma, whereas the asthmatic state of an individual also has the capabilities of influencing shortness of breath as a result of the lung […]
- Asthma Treatment Options, Long-Term Control, and Complications Speaking of the patient profile, the first aspects that should be mentioned are the peculiarities of asthma disease history and other health conditions that might affect the treatment pattern.
- Occupational Asthma: Case Discussion The primary diagnosis is occupational asthma; the causative agents of the indicated type of the disease are located directly at the person’s workplace.
- The Relationship Between Vitamin D Deficiency and Asthma Disease in Children The reaction of the host on the respiratory infections is closely correlated with the deficiency of the vitamin D [1]. This is because of the suggestion that providing vitamin D supplements to patients with low […]
- Asthma: Culture and Disease Analysis The cause of this condition is thought to be the narrowing of the person’s airways. This, as the experts explain, is a result of the inflammation of the airways in the lungs.
- Relationship Between Asthma and the Body Mass Index The optimal design of the study is the use of questionnaires, since the nature of the research requires the consent of individual respondents in form of writing.
- The Connection Between Asthma and Dust Emissions This is attributed to an increased rise of annual sandstorms and continued constructions that create a huge amount of dust in the air.
- Prevalence of Asthma Due to Climatic Conditions Newhouse and Levetin also conducted a study to find the correlation between the airborne fungal spores, the concentration of pollen, meteorological factors and other pollutants, and the occurrence of rhinitis and asthma.
- Helping African American Children Self-Manage Asthma The purpose of this critique is to analyze the weaknesses of the study. The title of the report Helping African American Children Self-Manage Asthma: The Importance of Self-Efficacy adequately identified the population of interest, namely […]
- Asthma Among the Japanese Population In a report by Nakazawa in which the author sought to determine the trend of asthma mortality among the Japanese population, emotional stress and fatigue emerged as the leading factors for the causation of asthma.
- Informed Consent – Ellen Roche, Asthma Study People interested in taking part in research trials have the right to know risks, benefits, procedures, the aim of the study, and protection of identity. This violation of subjects’ right led to the formation of […]
- Asthma Prevalence: Sampling and Confidence Intervals In the study which was carried out in United States in 2009 amongst the children and adults to show the prevalence of Asthma, a sample of 38,815 and confidence interval of 95% was used.
- Osteopathic Manipulation in Patients With Chronic Asthma This article seeks to criticise the application of osteopathic manipulation in the treatment of asthma patients. The focus is on the intervention of osteopathic manipulation therapy in restoring normal functioning and compliance to the thoracic […]
- 5-Year-Old With Asthma: Developmental Milestones & Care According to his mother, he also regularly grinds his teeth at night.G.J.was delivered normally and the mother had no complications. He could listen to instructions and get whatever he is being asked by his mother.
- Asthma Respiratory Disorder Treatment Asthma etiology is the classification of various risk factors responsible for causing asthma in children and adults. Asthma etiology is the scientific classification of risk factors that cause Asthma in children and adult.
- Childhood Bronchial Asthma: Process & Outcome Measures The evidence that is used to support the adoption of this measure is the guideline on clinical practice, as well as the procedure of formal consensus.
- Biological Basis of Asthma and Allergic Disease The immunological response in asthmatic people fails in the regulation of the production of the Th2 cells and the anti-inflammatory cells.
- Asthma and Medications: The Ethical Dilemma in Treating Children One of the major causes of dilemma, however, is the inability to manage and treat the condition in children under the age of 7 years due to ethical dilemma.
- Understanding Asthma in the Elderly: Triggers, Treatment, and Challenges The main objective of the given paper is to analyze the reasons of emergence of asthma among the elderly population, as well as research peculiarities of this group’s reaction to this condition as compared to […]
- Exercise-Related Asthma in the 21st Century The study has also reported that almost 48 % of parents recognize the fact that children suffering from asthma have higher probability of the emergence of the typical symptoms of IEB.
- The Nature and Control of Non-Communicable Disease – Asthma Asthma is caused due to the inflammation of the airways which in turn induces cough, wheezing, breathlessness and a feeling of tightness in the chest.
- Asthma in School Going Youth: Effects and Management The control and prevention of adverse effects of asthma are goals of managing asthma as stated in the National Asthma Education and Preventive Program asthma treatment guidelines.
- Asthma in the African American Community The paper will also highlight the effects that the treatment options used by African Americans have on the prevalence of the disease.
- Asthma Definition and Its Diagnostics The geographical area plays a major role in the distribution of the prevalence of asthma and its predisposing factors. There is scientific evidence that the presence of a history of asthma in parents is a […]
- Foot Orthosis, Asthma & Benign Tumor It is a chronic inflammatory disorder of the airways, associated with the following symptoms: variable airflow obstruction and enhanced bronchial responsiveness to a variety of irritants.
- Asthma in School Children in Saudi Arabia The purpose of this paper is to review the current literature on asthmatic disease in Saudi Arabia to accurately determine the epidemiology nature of the condition through community assessment for purposes of compiling a health […]
- Usefulness of Acupuncture in Asthma Treatment The case for the effectiveness of acupuncture in the treatment of asthma is to be further supported by more research studies, since current and past research has been affected by a number of limitations or […]
- Hypertension, Asthma and Glaucoma The assignment of duties is also a difficult task since the victim is forgetful and disoriented, which in this case may lead to delays or failures within the working system.
- The Management of Asthma According to the Australian Bureau of Statistics, the country has the highest prevalence of Asthma in the world. Quick-relief medications are used to manage symptoms that come with acute attacks of asthma-like coughing, tightening of […]
- Treatment of Asthma in Australia The rapid-acting treatments are taken to quicken the process of reversing acute asthmatic attacks by causing the relaxation of the smooth muscles of the bronchial system. These preventers reduce the sensitivity of airways hence swelling […]
- The Asthma and Emphysema Analysis According to Kinsella and others, etiology of emphysema is often associated with smocking, and this led to the hypothesis that emphysema develops with age whereas asthma is mostly prevalent in children.
- Asthma: Causes and Treatment Effects of asthma are more pronounced mostly at night and early in the morning and this results in lack of sleep.
- Acute Asthma: Home and Community-Based Care For Patients It refers to the continuum of care extended to patients from the health facility to the community and homes. An asthma attack is fatal and patients should be encouraged to perform self-administration of medication.
- How Emotions Spark Asthma Attack Although stress and emotions are known to start in a patient’s mind, asthma in itself is a physical disease that affects the patient’s lungs, and stress can create strong physiological reactions which may lead to […]
- Asthma Is a Chronic Inflammatory Disorder Hence the main purpose of the study is to investigate the association of smoking and secondhand smoke with level of asthma control, severity, and quality of life among adult asthmatics.
- Asthma: Leading Chronic Illness Among Children in the US Ample communication was to be provided to the family, Head Start personnel and the Child’s physician in relation to the asthma. A great reduction was seen in the asthma symptoms and emergency.
- Dealing With Asthma: Controversial Methods Because of the enormous speed of the illness spread, dealing with asthma is becoming a burning issue of the modern medicine. This is due to the fact that the muscles of the broche lack the […]
- Social Determinants of Health: Asthma Among Old People in Ballarat On the other hand, Melbourne is the capital city of the State of Victoria with a population of 4 million people, making it the second most populated city in Australia. This is a great challenge […]
- Asthma Investigation: Symptoms and Treatment In patients with asthma, the condition causes the inflammation of air passages that is followed by the significant narrowing of airways.
- Severe Asthma: The Alair Bronchial Thermoplasty System The article focuses on asthma and the treatment that could alleviate the condition. Most of asthma patients are used to having an inhaler with them and this way, there is not much new technology, except […]
- Asthma in Pediatric and Occupational Therapy Treatment The flow peak is more than 80% of the child’s personal best, and less than 30% variability in the day-to-day flow of the peak measurements.
- Public & Community Health: Asthma in Staten Island There is borough of Bronx, which is considered to be the poorest, and the case with it has been stated here that asthma is the fate of the residents.
- Clinical Guidelines: Report on Asthma Guideline The guideline illustrates diagnostic procedures for assessment of severity and control of asthma based on presence of airway hypersensitiveness, reversibility of airflow, detailed medical history, respiratory tract, skin and chest examinations, spirometry to assess obstruction, […]
- Clinical Management of Complex Cases in Dentistry: Case of Hypertension With Asthma Understanding the role of various drug interactions and the effect of various drugs on the medical conditions of the patients is of valuable assistance.
- Health, Culture, and Identity as Asthma Treatment Factors She is the guardian of Lanesha and, despite raising another grandson and caring for her elderly mother, she is responsible for the health of the girl.
- The Anti-Inflammatory Role of IL-26 in Uncontrolled Asthma Research findings suggest that the suppression of IL-26 secretion in the lungs would alleviate the anti-inflammatory response associated with uncontrolled asthma.
- Asthma Pathophysiology and Genetic Predisposition The pathophysiology of this disorder involves one’s response to an antigen and a subsequent reaction of the body in the form of inflammation, bronchospasm, and airway obstruction.
- Asthma: Pathopharmacological Foundations for Advanced Nursing Practice Because of the high prevalence of asthma in the USA, mortality and morbidity rates in the country are also excessive. Asthma is one of the most common diseases in the USA, with high prevalence and […]
- Asthma as Community Health Issue in the Bronx The rate of people, especially children, with asthma in this area is among the highest ones in the city. The issue of asthma in New York and the Bronx, in particular, is connected to multiple […]
- Environmental Factors of Asthma in Abu Dhabi City A countrywide evaluation of the demises related to environmental pollution that takes a significant role in the rising cases of asthma shows UAE as the most affected nations since the discovery of oil in 1958 […]
- Occupational Asthma: Michelle’s Case The first test is not prohibitively expensive, and the patient should be able to afford it if she can pay for the medications.
- Asthma Patient’s Examination and Care Plan HPI: Being discharged from the facility ten weeks ago, the patient reports having shortness of breath, severe wheezing, and coughing. To control symptoms, the patient takes HTCZ and Enalapril.
- Obstructive Pulmonary Disease-Asthma Overlap The purpose of the research was to expand the current knowledge of the overlap syndrome in order to determine its prevalence and risk factors.
- Chronic Asthma and Acute Asthma Exacerbation The consequences of the smooth muscles’ tightening can be aggravated by the thickening of the bronchial wall due to acute edema, cellular infiltration, and remodeling of the airways chronic hyperplasia of smooth muscles, vessels, and […]
- Asthma and Stepwise Management The stepwise approach to asthma treatment and management is a six-step approach, according to which the number and the dose of medications and frequency of management are increased as necessary when symptoms persist and then […]
- Asthma, Its Diagnostics, Treatment and Prevention Hippocrates was the one who labeled the disease as asthma, a Greek word that was used to denote the idea of “wind or to blow”, perhaps an attempt to describe the wheezing sound produced by […]
- Asthma: Evidence-Based Pharmacological Treatment For instance, in children under 6, the development of the disease is typically preceded by the asthma-like symptoms that manifest themselves roughly at the age of three.
- The Evaluation of Evidence Linking Asthma With Occupation Overall, the results of this study supported the initial argument of the authors in regard to the need for frequent updates and modifications of JEMs in order for them to reflect the most relevant and […]
- Pregnant Woman’s Asthma Case The case mentions the decreased effectiveness of the fluticasone MDI that she uses which can also be a clue to her condition. Her patterns of MDI use in the last two months and the bronchospasm […]
- Asthma: Causes and Mechanisms The enlargement of the dense oesinophilic line near the bronchus/airways causes the individual to wheeze and gasp for air. The drugs are mainly used in the rapid opening of the bronchus to enable airflow into […]
- Healthcare: Childhood Asthma and the Risk Factors in Australia From the findings presented above, it is evident that childhood asthma remains a considerable burden in Australia due to socioeconomic, geographic, and health-related issues such as deprived neighbourhoods, decreasing sun exposure and increasing latitude, and […]
- Intubation and Mechanical Ventilation of the Asthmatic Patient in Respiratory The title of the article gives a clear idea of the research question to be investigated. The authors have detailed the processes of intubation and mechanical ventilation in patients with acute asthma.
- Asthma Environmental Causes This essay discusses the measures that can be taken to mitigate environmental causes of asthma. In the US, the government has developed a comprehensive strategy to mitigate environmental causes of asthmatic conditions in children.
- Asthma’s Diagnosis and Treatment The complete occlusion of the airway can lead to growth of a distal at the atelectasis in the lung parenchyma. The level of AHR is connected to the signs of asthma and the urgency of […]
- The Effects Of Asthma On Pregnant African Americans
- Urban Children and Asthma Care Barriers
- Asthma: Asthma and Nocturnal Asthma
- The Health Problem of Asthma in the United States of America
- Asthma: Chronic Inflamatory Obstructive Lung Disease
- Asthma and Food-Allergy Reactions
- Asthma And Exercise Asthmatic Asthmatics Breathing
- Automobile Emissions, Co And Asthma
- Asthma Control and Treatment in Racial and Ethnic Minorities
- Asthma Is The Most Common Chronic Disease Of The Airways
- Inflammatory Mediators Of Asthma And Histamines Biology
- The Impact of Asthma on the Respiratory System, Its Causes, and Treatment
- How Asthma Affects The Airway And Lungs
- Diet and Nutrition for Asthma in a Child
- Urban Asthma And The Neighborhood Environment
- Asthma And Its Pathophysiological Structure
- The Effects of Medication on the Increased Performance of Asthma Patients
- What Parents Need To Know About Asthma
- Employment Behaviors of Mothers Who have a Child with Asthma
- The Genetic and Environmental Components of Asthma
- The Influence of Asthma on the Lives of Students
- Children’s Elevated Risk of Asthma in Unmarried Families: Underlying Structural and Behavioral Mechanisms
- The Effects Of Environmental Tobacco Smoke Among Children With Asthma
- The Effects Of Air Pollution On Children ‘s Asthma Emergency
- Is Improper Use Of The Inhaler Related To Poor Asthma Control
- Asthma Symptoms, Diagnosis, Management & Treatment
- Limitations From Suffering Chronic Asthma
- Causes And Effect Of Allergies And Asthma
- Describe The Main Limitations Suffered By Those With Chronic Asthma
- The Symptoms, Causes and Diagnosis of Asthma
- Negligent: Asthma and Nursing Interventions
- The Signs, Causes and What Triggers Asthma
- The Routine Care for Patients with Coronary Heart Disease, Asthma, Stroke, Irritable Bowel Syndrome, Urinary Tract Infections, Diabetes, and Cervical Cancer
- The Role Of Nurse Management Asthma And School Health Program
- The Scope of Asthma in the General Population and on the Health Care System
- The Most Effective Treatment for an Asthma Exacerbation
- Pathophysiology Of Chronic Asthma And Acute Asthma
- The Use Of Vitamin D Asthmatic Children Effectiveness Of Vitamin Supplements In Childhood Asthma
- The Ways in Which the Symptoms of Asthma Can Be Reduced
- Measures to Minimize Environmental Causes of Asthma
- Inner City Adult Asthma Patients and Risk Factors
- Raising Awareness to Prevent the Rise of Asthma
- Planning and Intervention in the Disease Process of Childhood Asthma
- The Anatomy And Physiology Of Respiratory System And The Diagnosis Of Asthma
- The Causes and Effects of Asthma Sufferers
- The Application of Corticosteroids in the Management of Bronchial Asthma
- Salbutamol: History of Development in Asthma Drug Compounds
- Sensitization To Plant Food Allergens In Patients With Asthma
- The Diagnosis and Treatment of Otitis Media and Asthma
- The Discrepancy between Asthma Cases in Minority and White Communities
- The Chronic Illness in Children Known as Asthma
- Does Childhood Asthma Improve With Age?
- What Are the First Warning Signs of Asthma?
- Which Child Is at Greatest Risk for Asthma?
- What Is the Genetic Predisposition of Asthma?
- Can Occupational Therapy Help With Asthma?
- How to Ventilate Obstructive and Asthmatic Patients?
- What Is a Risk Factor Associated With Childhood Asthma?
- What Type of Approach Is Used in Asthma Management?
- What Is the Difference Between Asthma and Acute Asthma?
- What Are the Pharmacological Treatment of Asthma?
- How Is Asthma Diagnosed?
- Can Asthma During Pregnancy Affect Baby?
- What Are the Three Mechanisms Involved in Asthma?
- How Does Genetics and Environment Affect Asthma?
- How Long Does It Take To Recover From Asthma Exacerbation?
- What Factors Influence the Development of Asthma?
- What Is the Physiological Cause of Asthma?
- What Are the Statistics on Asthma in Australia?
- What Is the Most Serious Type of Asthma?
- What Ethnic Group Is Especially Likely to Have Childhood Asthma?
- What Is a Nursing Care Plan of an Asthmatic Patient?
- Does Asthma Cause Smooth Muscle Hypertrophy?
- Should People With Asthma Use a Humidifier?
- What Is Mechanical Ventilation Asthma?
- What Is the Most Common Allergen to Trigger Asthma?
- What Is the Main Physiological Cause of Asthma?
- What Percent of Asthma Is Caused by Smoking?
- How Long Does the Average Person With Asthma Live?
- Which Drug Is Safe for Asthma in Pregnancy?
- How Many People With Asthma Still Smoke?
- Allergy Research Ideas
- Pneumonia Questions
- SARS Topics
- Infection Essay Ideas
- Metabolic Disorders Questions
- Immunization Paper Topics
- Viruses Research Topics
- Communicable Disease Research Topics
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 2). 173 Asthma Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/asthma-essay-topics/
"173 Asthma Essay Topic Ideas & Examples." IvyPanda , 2 Mar. 2024, ivypanda.com/essays/topic/asthma-essay-topics/.
IvyPanda . (2024) '173 Asthma Essay Topic Ideas & Examples'. 2 March.
IvyPanda . 2024. "173 Asthma Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/asthma-essay-topics/.
1. IvyPanda . "173 Asthma Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/asthma-essay-topics/.
Bibliography
IvyPanda . "173 Asthma Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/asthma-essay-topics/.
Academic Support for Nursing Students
No notifications.
Disclaimer: This essay has been written by a student and not our expert nursing writers. View professional sample essays here.
View full disclaimer
Any opinions, findings, conclusions, or recommendations expressed in this essay are those of the author and do not necessarily reflect the views of NursingAnswers.net. This essay should not be treated as an authoritative source of information when forming medical opinions as information may be inaccurate or out-of-date.
Asthma Essay With Conclusions
Info: 2061 words (8 pages) Nursing Essay Published: 11th Feb 2020
Reference this
Tagged: asthma chronic illness
If you need assistance with writing your nursing essay, our professional nursing essay writing service is here to help!
Our nursing and healthcare experts are ready and waiting to assist with any writing project you may have, from simple essay plans, through to full nursing dissertations.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services

- Nursing Essay Writing Service

- Nursing Dissertation Service

- Reflective Writing Service
Related Content
Content relating to: "chronic illness"
Chronic illnesses are non-communicable diseases which develop gradually over time. They generally cannot be solved instinctively and are barely to be cured ultimately. In most cases, chronic illnesses are more likely to be insidious where the patients have mild or no symptoms.
Related Articles

Case Study of Diabetes Mellitus and Community Health Nurse
This paper is going to illustrate a case study, which has been chosen during the two weeks of clinical practicum. It will present the medical history of the patient, focus on current health status and...
Dangers Of Diabetes And Possible Treatment Nursing Essay
Early 1500 B.C (Egyptian Papyrus) 2000 years later, Arataeus (siphon). Late 17th century, Willis and Dobson (mellitus) 1889, Mering and Minkowski, Paul Langerham 1921 to 1922, Federick Banting and Ch...
Review Of Literature Related To Diabetes Mellitus Nursing Essay
The review of literature for the present Study has been done on knowledge regarding lifestyle modification among diabetes mellitus patients from published articles, textbooks, reports, newsletters, medline and internet search....
DMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on the NursingAnswers.net website then please:
Our academic writing and marking services can help you!
- Marking Service
- Samples of our Work
- Full Service Portfolio
Related Lectures
Study for free with our range of nursing lectures!
- Drug Classification
- Emergency Care
- Health Observation
- Palliative Care
- Professional Values

Write for Us
Do you have a 2:1 degree or higher in nursing or healthcare?
Study Resources
Free resources to assist you with your nursing studies!
- APA Citation Tool
- Example Nursing Essays
- Example Nursing Assignments
- Example Nursing Case Studies
- Reflective Nursing Essays
- Nursing Literature Reviews
- Free Resources
- Reflective Model Guides
- Nursing and Healthcare Pay 2021
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- NPJ Prim Care Respir Med

Improving primary care management of asthma: do we know what really works?
Monica j. fletcher.
1 Asthma UK Centre for Applied Research, Usher Institute, University of Edinburgh, Old Medical School, Teviot Place, Edinburgh, EH8 9AG UK
Ioanna Tsiligianni
2 Department of Social Medicine, Faculty of Medicine, University of Crete, Heraklion, Greece
Janwillem W. H. Kocks
3 General Practitioners Research Institute, 59713 GH Groningen, The Netherlands
4 University of Groningen, University Medical Center Groningen, GRIAC Research Institute, Groningen, The Netherlands
5 Observational and Pragmatic Research Institute, Singapore, Singapore
Andrew Cave
6 Department of Family Medicine, 6-10 University Terrace, University of Alberta, Edmonton, AB T6G 2T4 Canada
Chi Chunhua
7 Peking University First Hospital, Beijing, China
Jaime Correia de Sousa
8 Life and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal
9 33ICVS/3B’s, PT Government Associate Laboratory, Braga/Guimarães, Portugal
Miguel Román-Rodríguez
10 Primary Care Respiratory Research Unit, Instituto de Investigación Sanitaria de las Islas Baleares (IdISBa), Palma, Spain
Mike Thomas
11 Department of Primary Care, Population Sciences and Medical Education, University of Southampton, Southampton, SO16 5ST UK
Peter Kardos
12 Respiratory, Allergy and Sleep Unit at Red Cross Maingau Hospital, Friedberger Anlage 31-32, 60316 Frankfurt, Germany
Carol Stonham
13 NHS Gloucestershire Clinical Commissioning Group, Brockworth, UK
Ee Ming Khoo
14 Department of Primary Care Medicine, Faculty of Medicine, University of Malaya, 50603 Kuala Lumpur, Malaysia
David Leather
15 Global Respiratory Franchise, GlaxoSmithKline plc., GSK House, 980 Great West Rd, Brentford, Middlesex TW8 9GS UK

Thys van der Molen
16 Department of General Practice, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands
Associated Data
Anonymised individual participant data from this study and its associated documents can be requested for further research from www.clinicalstudydatarequest.com .
Asthma imposes a substantial burden on individuals and societies. Patients with asthma need high-quality primary care management; however, evidence suggests the quality of this care can be highly variable. Here we identify and report factors contributing to high-quality management. Twelve primary care global asthma experts, representing nine countries, identified key factors. A literature review (past 10 years) was performed to validate or refute the expert viewpoint. Key driving factors identified were: policy, clinical guidelines, rewards for performance, practice organisation and workforce. Further analysis established the relevant factor components. Review evidence supported the validity of each driver; however, impact on patient outcomes was uncertain. Single interventions (e.g. healthcare practitioner education) showed little effect; interventions driven by national policy (e.g. incentive schemes and teamworking) were more effective. The panel’s opinion, supported by literature review, concluded that multiple primary care interventions offer greater benefit than any single intervention in asthma management.
Introduction
Asthma is a common chronic condition that is estimated to affect 339 million people worldwide 1 , 2 . Despite major advances in asthma treatment and the availability of both global 2 and national guidance, asthma continues to cause a substantial burden in terms of both direct and indirect costs 1 . In 2016, estimated worldwide asthma deaths were 420,000 1 and although there have been falls in some countries over the last decade, significant numbers of avoidable deaths still occur 3 . Mortality rates vary widely, with low- and middle-income countries faring worse 4 . For example, Uganda’s reported mortality rate is almost 50% higher 5 than that reported globally (0.19/100,000) 6 , although inter-country comparisons using different data sources and epidemiological methodologies have limitations. The World Health Organisation (WHO) has a global ambition for universal healthcare coverage by 2030 as millions of people worldwide do not have accessible affordable medical care 7 . The WHO moreover recognises that health systems with strong primary care have the utmost potential to deliver improved health outcomes, greater efficiency and high-quality care 7 . Perversely the availability of good quality primary and social care tends to vary inversely, those having the greatest needs being least likely to receive it 8 .
In addition to the issues of access and the quality of care, both under- and over-diagnosis of asthma is common in all healthcare settings, but the issue is of particular concern in primary care, where most initial diagnoses are made 9 , 10 .
For people with asthma, high-quality, local and accessible primary care could be a solution to poor control 11 . Our aim was to identify the factors that experts believe enable the delivery of high-quality asthma care and to review the evidence that confirms that these factors do indeed have positive outcomes in primary care.
Key drivers and their underpinning components
The expert panel identified five key drivers for the delivery of quality respiratory care in primary care and a number of components underpinning each of these drivers. These are summarised in Table Table1 1 .
Key drivers and their underpinning components identified by the expert panel.
| 1. National healthcare policy |
| − Appropriately resourced primary care services |
| − Actions to support universal health coverage |
| − Recognition of importance of non-communicable chronic disease management |
| − Balance between public and private insurance: healthcare systems |
| − Redistribution of funding from hospitals to primary care |
| 2. Clinical guidelines |
| − Recognition that primary care uses multiple disease guidelines |
| − Primary care ownership and succinct evidence-based guidelines |
| − Accessible guidelines produced in a standard recognised format |
| − Consider shifting to symptom-based guidelines |
| 3. Reward for performance |
| − Recognition and rewards for high-quality respiratory practice |
| − Clearly defined financial incentive schemes |
| − Reward for the practice not individual practitioners |
| − Reimbursement policies aligned to guidelines, including prescribing |
| 4. Practice resources and organisation |
| − Registered patient lists and fully integrated computer systems |
| − Clinical care pathways |
| − Access to high-quality lung function and other diagnostic tests |
| − Access literacy and culturally sensitive patient education |
| 5. Workforce |
| − Specialist asthma training programmes in primary care |
| − Dedicated and appropriately asthma-trained personnel |
| − Collaborative working across the wider primary healthcare team, with defined roles |
| − Excellent interdisciplinary communication processes |
Of the 50 articles selected from the review, there were comparatively smaller numbers of publications relating to the impact of National Health Policy and Guidelines. However, there was more substantial evidence relating to the other three key drivers, which is summarised in tabular format (Tables (Tables2 2 – 4 ).
Evidence summary to support reward for performance.
| Reward for performance | Reference | Country | Study type | Description | Study outcomes |
|---|---|---|---|---|---|
| Clearly defined financial incentive schemes | Langdown and Peckham | UK | Review of 11 studies | The UK quality and outcomes framework (QOF) one of the world’s largest pay-for-performance schemes. | The QOF has limited impact on improving health outcomes due to its focus on process-based indicators and the indicators’ ceiling thresholds. |
| Clearly defined financial incentive schemes | Gillam et al. | UK | Systematic review of 94 studies | Quality of care for incentivised conditions during the first year of the QOF improved at a faster rate than the preintervention trend. | Modest improvements in the quality of care for chronic diseases. |
| Recognition and rewards for high-quality respiratory practice | Gillam et al. | UK | Systematic review of 94 studies | Increased practice activity but limited evidence of improving the quality of primary healthcare or cost-effectiveness. | |
| Reward for performance | Scott et al. | Studies from the US and UK | Review of 7 studies | Pay-for-performance (P4p) schemes reviewed. | There is insufficient evidence to support or not support the use of financial incentives to improve the quality of primary healthcare |
| Reward for performance | To et al. | Canada (Ontario Asthma Surveillance System | Three primary care incentive models evaluated | Quality measured using six validated, evidence-based asthma performance indicators (traditional fee-for-service model, the blended fee-for-service and blended capitation models). | Quality of asthma care improved over time within each of the primary care models. Blended fee-for-service and blended capitation models appear to provide better quality care compared to the traditional fee-for-service model. |
| Reward for the practice not individual practitioners | Kirschener et al. | Netherlands | Observational study of 60 practices with a pre- and post-measurement | A P4p programme designed by target users containing indicators for chronic care, prevention, practice management and patient experience | After 1 year, significant improvement by +11.5% was shown for the process indicators for asthma. |
| Reimbursement policies aligned to guidelines, including prescribing | No studies found via search |
P4p pay for performance, QOF Quality and Outcomes Framework, UK United Kingdom, US United States.
Evidence summary to support workforce issues.
| Workforce | Country | Study type | Description and study outcomes |
|---|---|---|---|
| 1, 2, 3 | CA | Retrospective database study, adults. 2008–2009. PC physician/network visited ( = 1,502,916); usual care ( = 1,109,941) | PC networks designed to facilitate access to interprofessional, team-based care, using AHPs skills in providing coordinated healthcare. Health outcomes associated with PC networks compared with conventional PC. Outcomes: Pts in network practices less likely to visit ED for conditions such as asthma; fewer ED visits and shorter hospital stays. |
| 1, 2, 3 | US | Implementation study. 42 pharmacies, 2419 pts and 1284 provider interventions | Community pharmacist reviews of pts with poorly controlled asthma/no recent physician asthma review; physician referral was a service component. Outcomes: Benefits in asthma control, knowledge, inhaler technique, AAP ownership, ARQOL, and adherence. |
| 1, 2, 3 | AU | A pragmatic cluster-randomised trial 96 pharmacists, 570 pts | Community-based asthma service by specially trained pharmacists: 3 vs. 4 visits in 6 months (12-month follow-up). Outcomes: Clinically important outcomes in both groups with minimal intervention, 3-visit service feasible/effective to implement, with 12-month review. |
| 1, 2, 3 | US | Prospective pre-post study of pts receiving intervention for 9 months; 126 pts | Pts received physician−pharmacist collaborative management in PC. Pharmacists provided AAP/education/physician referral as necessary. Outcomes: Asthma-related ED visits decreased by 30% in the 9 months. |
| 1, 2, 3 | US | 5 community-based clinics Retrospective pre- and post-intervention analysis | A team-based education approach involving an electronic clinical quality management system; reminders/provision of AAPs by nurses. Outcomes: Increased AAPs prescribed, pt outcomes were not measured. |
| 2, 3 | UK | Community-based, randomised, open-label pragmatic study | SLS; a collaboration between physicians, nurses, hospital staff and pharmacists linked using electronic pt health record, improving HCP communication. Outcomes: Improved asthma control (ACT increase). |
| 2, 3 | BR | Implementation study 132 PC physicians & nurses Aim to decrease number of respiratory-related (Asthma/COPD) referrals | Educational intervention (matrix support, evaluated in PC): physicians/nurse training/support from specialists (e.g. tailored education/joint consultations/case discussions). Outcomes: referrals decreased by >50% from 13.4 to 5.4 cases/month ( = 0.09). An effective tool to improve asthma knowledge and promote changed PC/SC relations. Pt outcomes not measured. |
| 4 | US | Implementation study. 57 practices, 15,508 pts Pre-post | CATP; a provider-level intervention to improve guideline use and asthma care (education and pt resources). Outcomes: CATP improved guideline care processes but not pt outcomes, of practices: 40.4% increased ICS use, 53.2% increased AAP use; 78.7% initiated/increased spirometry use. |
| 4 | US | Implementation study (asthma pts 5–64 years) 12 months pre- and post-CATP implementation 9 practices; 2678 pts | Compared 12 months pre- and post-use of the CATP in PC practice. Outcomes: An improvement in asthma quality processes—increase in rate of asthma severity measurement and medication management, no change in outcomes across multiple domains: exacerbations, utilisation, symptom scores, and pulmonary physiology measures. |
| 4 | CA | Pragmatic improvement study. 23 physicians, 25 AHPs; 12-month pre/post-intervention knowledge | Mentorship-based intervention with interactive education/hands-on training/ unstructured peer mentoring. Aimed to address PC underuse/quality of spirometry. Outcomes: Improved spirometry test acceptability, poor overall spirometry usage (remained < 40%), health outcome effects not measured. |
| 5 | DK | Consultation guide based on GINA guidelines | Consultation included symptom evaluation, treatment, compliance, lung function, scheduled follow-up appointment based on asthma control level. Outcomes: Asthma control improved when a systematic asthma management approach was introduced/applied by dedicated nurses. |
| 5 | ES | Cluster controlled implementation study 57 practices 400 PC physicians and nurses, 6/12 pre−post-intervention 7 control | GP practices received an education programme for use of respiratory health status tools. Outcomes: In intervention practices slight improvement in pts with a record of a health status score (ACT, CAT and/or mMRC), but absolute % score recorded was still relatively low (1.70%), even after intervention. No differences in clinical outcomes. |
| 5 | AU | RCT aged ≥55 with asthma = 58 intervention group = 56 control group | Groups: brochure only (controls); person-centred education (intervention). Outcomes: Intervention pts had improved asthma control, adherence, AAP ownership, ARQOL and exacerbations over 12 months vs. control pts. |
| 5 | Global | Literature review of 24 studies | Reviewing conceptualisation/practice in PC. Enablement influenced by: open communication style/longer consultations/pt centredness of HCP. Outcomes: 2 RCTs suggest enablement linked to better pt outcomes. |
| 5 | DE | 5-year programme 2006–2010. = 109,042 in year 5 | German asthma management programme. Outcomes: Enhanced care quality; improved symptoms/adherence/pharmacotherapy/hospitalisation. |
1 = Dedicated and appropriately asthma-trained personnel; 2 = Collaborative working across the wider Primary HealthCare Team, with defined roles; 3 = Excellent interdisciplinary communication processes; 4 = Specialist asthma training programmes in PC; 5 = Dedicated and appropriately asthma-trained personnel.
AAP asthma action plan, ACT Asthma Control Test, A&E Accident and Emergency department, AHP Allied Health Practitioner, ARQOL asthma-related quality of life, AU Australia, BR Brazil, CA Canada, CAT COPD Assessment Test, CATP Colorado Asthma Toolkit Programme, COPD chronic obstructive pulmonary disease, DE Germany, DK Denmark, ED Emergency department, ES Spain, GINA Global Initiative for Asthma, GP General Practitioner, HCP healthcare practitioner, mMRC Modified Medical Research Council, PC primary care, PTS patients, RCT randomised clinical trial, SC secondary care, SLS Salford Lung Study, UK United Kingdom, US United States.
National Health Policy
The expert panel reached an agreement that the political will to prioritise asthma and to support both primary care and respiratory disease were fundamental elements for the achievement of a sustainable change. In their opinion this required national and local programmes supporting the improvements. There was however little evidence published to support this opinion with respect to patient outcome as it is not the area of research that is commonly undertaken. A review of seven national European asthma programmes to support strategies to reduce asthma mortality and morbidity concluded that national/regional asthma programmes are more effective than conventional treatment guidelines 12 . One of the most well-known and successful national programmes in Europe, which has resulted in reduced morbidity and mortality and decreased costs, is the Finnish National Asthma Programme 13 . Programmes outside of Europe have also demonstrated the impact that prioritisation of primary care can have on respiratory outcomes. Changing structures and policies in South Africa and in Brazil may start to impact on primary care 13 , 14 .
Few studies have explored the extent of adherence to guidelines for asthma management based on data provided directly by GPs. One study aimed to evaluate adherence to GINA guidelines and its relationship with disease control in real life. According to GINA guideline asthma classification, the results indicated overtreatment of intermittent and mild persistent asthma, as well as a general poor adherence to GINA treatment recommendations, despite its confirmed role in achieving a good asthma control 15 . In the US, nationally representative data showed that agreement with and adherence to asthma guidelines was higher for specialists than for primary care clinicians, but was low in both groups for several key recommendations 16 .
Reward for performance
Pay-for-performance (P4p) schemes are those that remunerate physicians for achieving pre-defined clinical targets and quality measures—so based on value—that contrasts to schemes that are simply a fee-for-service payment, which pay for volume of activity (Data from Review Table Table2). 2 ). In the UK, primary care has moved towards group practices with P4p compensation in which performance is measured using several defined quality indicators 17 , 18 . A systematic review of 94 studies showed increased practice activity but only limited evidence of improvements in the quality of primary care or cost-effectiveness, despite modest reductions in mortality and hospital admissions in some domains 18 . In another review of seven studies from the US and UK, the effects of financial incentive schemes were found to improve patient’s well-being, whilst the effects on the quality of primary healthcare were found to be modest and variable 19 .
An evaluation of three primary care incentive models, namely a traditional fee-for-service model, a blended fee-for-service model and a blended capitation model, demonstrated that the quality of asthma care improved over time within each of the primary care models 20 . The model that combined blended fee-for-service with capitation appears to provide better quality care compared to the traditional fee-for-service model in terms of outcome indicators such as a lower rate of emergency department visits.
A P4p programme in the Netherlands containing indicators for chronic care, prevention, practice management and patient experience was designed by target users 21 . A study of 65 practices that implemented the programme showed a significant improvement in the mean asthma score after 1 year. It showed that a bottom-up developed P4p programme might lead to improvements in both clinical care and patient experience.
Practice resources and organisation
Optimal patient care requires targeted and tailored management (Data from Review Table Table3). 3 ). The experts felt that the organisation of both the GP practice and the local healthcare system had an influence on the provision of high-quality care. Registered patient lists and fully integrated computer systems were its foundation. An approach called SIMPLES—developed in the UK, incorporated into a desktop reference tool by the International Primary Care Respiratory Group and adapted for use in the Netherlands 22 , 23 —identifies patients who have uncontrolled symptoms or difficult-to-manage disease and addresses preventable or treatable factors to guide their management. Electronic alerts in patient records have also been used to identify those at increased risk of an exacerbation, in order to modify care and treatment 24 – 26 .
Evidence summary to support practice resources and organisation.
| Practice resources and organisation | Country | Study type | Description and study outcomes |
|---|---|---|---|
| Registered pt lists and fully integrated computer systems AND Clinical care pathways | UK | Questionnaire; no data | SIMPLES, a structured PC approach to reviewing pts with uncontrolled asthma—encompassing pt education monitoring, lifestyle/pharmacological management and addressing support needs. Involves close cooperation between PC and SC. Outcomes: No data available. |
| Registered pt lists and fully integrated computer systems AND Clinical care pathways | NL | Questionnaire; no data | SIMPLES adapted using a modified e-Delphi approach to assess the stakeholder opinion. Outcomes: Nine-component questionnaire—a robust and holistic approach for difficult-to-manage asthma. No data available. |
| Registered pt lists and fully integrated computer systems | UK | Cluster-randomised trial in 29 PC practices with 911 at-risk asthma pts | Pilot study showed that PC intervention for targeted at-risk asthma patients had the potential for improving practice level management and reducing asthma emergency admissions. |
| Registered pt lists and fully integrated computer systems | UK | Pragmatic, 2-arm, RCT; 270 PC practices covering >10,000 registered ‘at-risk asthma’ pts | Aimed to determine whether the creation and integration of at-risk asthma registers into PC reduces asthma-related crisis events for at-risk pts over a 12-month period compared to control practices. Outcomes: No data available. |
| Registered pt lists and fully integrated computer systems | UK | Retrospective study; 26 at-risk asthma pts and 26 matched controls for 1 year pre- and post-intervention | Implementation/service use costs estimated before and 1 year after introduction of an at-risk register. More ‘at-risk’ than control pts were hospitalised/attended A&E/nebulised for asthma; also used out-of-hours services/attended GP/received OCS (all < 0.025). Outcomes: After register introduction, no at-risk pts were admitted or attended A&E. |
| Registered pt lists and fully integrated computer systems | Multi-national (US, NL, AU, UK, DK) | Systematic review of 19 studies representing 16 RCTs (2003–2013) evaluating CCDS for pts with asthma and COPD | Use of CCDS improved asthma and COPD care in 14 of the reviewed studies (74%). There was considerable improvement in healthcare process measures and clinical outcomes. The effect on workload, efficiency, safety, costs, provider and pt satisfaction remain understudied. |
| Registered pt lists and fully integrated computer systems | Multi-national (US, NL, UK, ES) | Systematic review of 8 RCT CCDS (1990–2012) for professional asthma management | Use of CCDS by HCPs was found to be low, and adherence to the advice was limited. Concluded, if used, CDSS could result in closer adherence to guidelines and improve some clinical outcomes. Better alignment to clinical workflow would enhance their use. |
| Registered pt lists and fully integrated computer systems | NL | 1-year RCT; 200 adults (18–50 years) with mild–moderate persistent asthma | Pt groups: (i) weekly asthma control monitoring via online ACQ, treatment adjusted via self-management algorithm supervised by an asthma nurse specialist; (ii) usual care. Outcomes: Weekly self-monitoring/treatment adjustment led to improved asthma control in pts with partly/uncontrolled asthma at baseline. |
| Access to high-quality lung function testing and other diagnostic tests | Unknown at present | Protocol: This will be a systematic review | Clinical prediction models can be used to aid PC asthma diagnosis by estimating outcome; models combine ≥2 predictors, e.g. clinical history/physical examination/test results/treatment response. Outcomes: No data available. |
| Access to high-quality lung function testing and other diagnostic tests | NL | Observational study | An online support system to advise GPs on pt diagnosis and treatment. Spirometry performed by local GP laboratory; spirometry results, pt history questionnaire, ACQ and CCQ reviewed online by pulmonologist; who advises GP online, supported by a guideline-based algorithm. Outcomes: Number of pts with unstable asthma (ACQ ≥ 1.5) dropped from 245 to 137. |
| Access to high-quality lung function testing and other diagnostic tests | NL | PC Diagnostic Centre study. 156 pts randomly selected from asthma/COPD-service referrals | Five respiratory specialists assessed spirometry data and pt histories. Facilities developed to provide spirometry testing by specially trained clinicians. GPs reluctant to perform or interpret spirometry themselves may be supported diagnostically by respiratory specialists in an asthma service although the reliability of this advice varies. |
| Access to high-quality lung function testing and other diagnostic tests | UK | PC study; 678 pts aged 4–80 years with first FeNO assessment at index date | FeNO use to guide ICS initiation/dosing decisions and identify poor adherence. In the year following index date, FeNO use was evaluated in 2 pt cohorts to: (i) identify steroid-responsive disease; (ii) guide asthma management. Outcomes: Algorithms to guide practical FeNO use could improve diagnostic accuracy/asthma regimen tailoring. |
| Access literacy/culturally sensitive pt education | No studies found via search |
ACQ Asthma Control Questionnaire, A&E Accident and Emergency department, AU Australia, CCQ Common Cold Questionnaire, CDDSS Computerised Clinical Decision Systems, COPD c hronic pbstructive pulmonary disease, DK Denmark, ES Spain, FeNO Exhaled Nitric Oxide Test, GP General Practitioner, HCP healthcare practitioner, ICS inhaled corticosteroid, NL Netherlands, PC primary care, PTS patients, RCT randomised clinical trial, SC secondary care, UK United Kingdom, US United States.
A systematic review of the effectiveness of computerised clinical decision systems (CCDS) in the care of patients with asthma demonstrated improvements in healthcare process measures and patient outcomes 27 . Conversely another systematic review focussing on their implementation in practice concluded that the limiting factors were the lack of their regular use by healthcare practitioners (HCPs) and adherence to the advice offered 28 . These reviews both concluded that CCDS have the potential to improve patient outcomes, practice efficiency and produce cost-saving benefits if implemented 27 , 28 .
Computerised systems linked with internet programmes to monitor asthma control can also afford benefits for patients. One study identified that the use of both weekly internet-based self-monitoring using the Asthma Control Questionnaire (ACQ) and treatment adjustment using an online management tool resulted in significant improvements in ACQ 29 .
Clinical prediction models could theoretically aid the diagnosis of asthma in primary care but supportive evidence is currently lacking 30 . However, there is strong evidence that service models aimed at supporting primary care practitioners with the diagnosis or ongoing monitoring of patients result in improved accuracy and patient outcomes 31 – 33 .
The expert panel felt that having access to dedicated and appropriately trained personnel preferably as part of multidisciplinary teams was essential (Data from Review Table Table4). 4 ). This need was accentuated because of increasing GP workloads and a shortage of primary care physicians in many countries.
There was extensive evidence 34 – 40 that a variety of models involving a range of healthcare practitioners within both the core primary healthcare team and extended community teams improve patient outcomes and healthcare process measures—such as an increased use of asthma action plans, improved medication adherence 36 , 39 —and reduces the use of emergency care 34 , 38 .
One approach in Canada is based on using primary care networks, in which additional non-physician healthcare providers are funded to help provide coordinated healthcare 34 . In these networks patients were shown to be less likely to visit the ED than patients in practices that were not part of the network.
Evidence from a range of countries supports the beneficial role of pharmacists, working alone or in teams 36 – 38 . In a study utilising community pharmacists to review patients with either poorly controlled asthma or no recent asthma review, there were benefits in terms of asthma control, inhaler technique, action plan ownership, asthma-related QOL and medication adherence 36 . The pharmacists were able to recruit patients and incorporate this as part of daily practice. Availability of referral to a physician was an important component of the service.
Evidence also indicates that education delivered by a variety of methods enhances the quality of care delivered and improves patient outcomes 41 – 45 . Approaches integrating education with other interventions, such as the Colorado Asthma Toolkit Programme (CATP) that combines education with decision support tools, electronic patient records and other online support materials, have been shown to have positive outcomes 41 , 42 . Another team-based approach that combined an educational intervention with the integration of an electronic clinical quality management system with a reminder system found that the number of action plans increased significantly 39 .
Patient education is an important factor for the improvement of self-management and asthma control. An educational programme from Australia demonstrated that patients who received person-centred education had improved asthma outcomes compared to those receiving a brochure only 46 . One review paper 47 about patient enablement concluded that HCPs need to develop their understanding of this concept to integrate this into practice as the level of this is linked to better patient outcomes.
Primary care is pivotal to any health system; however, there is no universal definition of what we mean by primary care and certainly not one standardised model of care. Without focussing on a single model, we have attempted to bring together expert opinion and the most recent evidence on strategies that improve outcomes in asthma patients in primary care. To our knowledge the methodology used in this project has not been used before. The panel of experts who identified the key drivers were knowledgeable of asthma in primary care at a national level in their respective countries and globally. A literature search to investigate the individual key drivers and their underpinning components was undertaken using a keyword search. This identified many publications but very few measured the effect on patient outcome and those that did reported conflicting results. Furthermore, we found a paucity of research relating to the components relating to national healthcare policy and guidelines.
The evidence suggests that health systems that have primary care as a cornerstone and place asthma as a healthcare priority improve asthma care and improve outcome on patient level. The highly regarded Finnish asthma initiative carried out more than 25 years ago not only identified asthma as a national priority, but also placed primary care at the centre of the programme, recognising the key role of General Practitioners and nurses and greatly reduced asthma mortality and morbidity 48 . After the successful implementation of the Finnish asthma plan, many other countries and regions have attempted to implement similar initiatives 13 , 14 . For example, in Poland and Brazil, asthma burden was reduced utilising such a strategy 49 .
Poor health outcomes in asthma patients have been attributed in primary care to gaps between evidence-based recommendations and practice 50 , 51 . Studies show that adherence to clinical guidelines is poor, whatever the clinical setting, with the main barriers being time pressures and limited resources 52 , reflecting that it is not the guidelines per se that improve care, but it is the implementation of the recommendations.
Most guidelines are complex, lengthy and generally biased towards a secondary care perspective. The Global Initiative for Asthma (GINA) committee acknowledges the difficulty of implementing their recommendations in primary care, but they are almost exclusively developed by tertiary care physicians 2 . In the Netherlands, the Dutch Royal Society of General Practitioners writes its own guidelines, which are all presented in the same recognisable brief format. Their asthma guidelines were first published in 1986 with revisions every 4 years and are relatively well followed 53 . However, there are now 194 different clinical guidelines in the Netherlands, illustrating just how difficult it is for General Practitioners to adopt all the recommendations of each clinical guideline and its update.
A survival analysis of guidelines has concluded that 86% are still up to date 3 years after their publication and yet the median lifespan of a clinical guideline is about 60 months 54 . New evidence is continually emerging and this implies that regular updates of clinical guidelines are necessary 55 , 56 . It is therefore important that all guidelines have a process for regular scrutiny 57 and are updated for contemporary applicability. Indeed, asthma and COPD guidelines published by the Association of Scientific Medical Societies in Germany and the Asthma Guidelines of the German Respiratory Society are regularly updated, at least every 5 years (more frequently as necessary); if not they are deleted from the website.
The proliferation of guidelines and their asynchronicity can result in conflicting recommendations. For example, in the UK, four asthma guidelines could be followed (the GINA Report, British Thoracic Society and Scottish Intercollegiate Guidelines (BTS) and the NICE recommendations next to local guidelines) 2 , 58 , 59 , none of which are fully aligned. A review of three contemporaneous international guidelines updated in 2012 (The Canadian Thoracic Society (CTS), BTS and GINA) also revealed significant inconsistency arising from varying approaches to evidence interpretation and recommendation formulation 60 .
Globally, there is a move away from pure fee-for-service payments towards primary care payment schemes linked to performance, which recognise and reward good practice to improve quality and reduce costs 61 . These schemes combine quality standards and targets but still tend to be process driven, not outcome based. The evidence for the effectiveness of such schemes in general on improving quality of care is both inconclusive and inconsistent 62 .
The UK quality and outcomes framework (QOF), which includes asthma, is the world’s largest primary care payment for performance (P4p) scheme 63 . Evidence however shows that improved patient outcomes may not be sustained, cost reduction is unproven 18 and leads to increased GP activity, but this does not necessarily correlate with improved individual patient benefit 64 , 65 . Furthermore, in Portugal, the recording of asthma and COPD prevalence as performance indicators in pay-for-performance contracts showed a modest but steady increase over time in physician’s diagnosis and ICPC-2 coding of these two conditions, but no direct patient benefits 66 .
Disease-specific schemes are usually aligned to clinical guidelines and some focus on prescribing. In Norway, under such a scheme, combination asthma medications were only reimbursed for patients diagnosed with asthma. As a result, asthma diagnosis significantly increased 67 .
The effect on health inequalities has also been studied. The results from UK QOF have shown that the gap between achievements from practices in the most deprived and least deprived areas narrowed 68 . Nevertheless, inequalities in morbidity and premature mortality persisted 69 , 70 . Additionally incentives can increase inequalities because those conditions that are ‘incentivised’ are afforded greater priority and resource allocation, to the detriment of those that are not 71 .
It would appear that simplistic fee-for-service schemes based purely on an activity—such as performing spirometry tests—which are not part of reimbursement of a more comprehensive assessment, have the potential to inadvertently lead to an increase in unnecessary tests. Pay-for-performance schemes have the potential to improve asthma care, but will be reliant on the specifics of the scheme and the quality indicators applied. They can be useful as part of a wider programme to raise quality and afford benefits over rewarding fee-for-service activity.
Appropriate practice organisation and systems focussing on the identification, diagnosis and treatment are pivotal for quality asthma care. There was compelling evidence to indicate that integrated, multi-faceted practice-based approaches for the management of patients improves outcomes and reduces the need for referral to secondary care 22 , 25 , 72 . Coordinated practice systems that combine several interventions such as decision support tools, flagging of electronic records, use of care pathways, staff training and structured approaches to patient education, if consistently implemented, afford the greatest benefits. Implementation of practice schemes is likely to be enhanced where there is dedicated clinical and administrative leadership.
Intuitively an accurate diagnosis should lead to better patient outcomes, although we found conflicting evidence that access to proper diagnosis has an impact on patient outcomes 33 , 73 . Nevertheless, an accurate diagnosis remains the fulcrum on which optimal asthma management depends. Indeed programmes in which an expanded medical team improved the quality of asthma care within the primary care setting (such as a diagnostic and management support organisation) show clear benefit on patient outcome 32 .
Spirometry combined with an assessment of reversibility has been set as gold standard for asthma diagnosis 2 . However, standards on quality of spirometry such as those set by the ERS and ATS are often not achieved 74 – 76 and impose an unnecessarily high and potentially unachievable threshold in primary care 73 . Nevertheless, some studies have demonstrated that primary care office spirometry can meet the acceptability criteria 77 – 79 . Although such standards are laudable particularly in a specialist setting, their practicability in primary care, where patients commonly have mild–moderate, intermittent disease, is debatable. The latest ATS-ERS spirometry guidelines (published in October 2019) may address some of these issues. 80 However, the use of spirometry in the diagnosis of asthma remains beyond reach in primary care around the world.
In many countries primary care physicians have limited or no access to tests of lung function or airway inflammation. The creation of diagnostic hubs in the community may open access to these tests 32 . A structured approach to diagnosis including applicability and feasibility for primary care is currently under development by an ERS taskforce; its outcome not available at the time of writing.
With rising clinical workloads, increasing clinical complexity and in many countries a shortage of trained primary care physicians, multi-professional teamworking is increasingly important. 81 , 82 This is accentuated by the expectation for primary care to manage patients with chronic illness.
In many parts of the world, appropriately asthma-trained personnel, such as primary care nurses, are key to the delivery of high-quality asthma care. Dedicated nursing staff can offer continuity to patients, providing education and routine follow-up 35 . Evidence supports the concept that pharmacists working alone or in teams in collaboration with GPs are an accessible asset for the effective management of asthma and can positively influence asthma outcomes 36 .
Healthcare practitioner education is pivotal and the need for guideline-focused training in primary care is well established 82 . The literature seems to support this viewpoint but in many studies the effect on outcome has not been adequately considered, highlighting a need for more outcome-focussed research. Healthcare systems faced with the challenge of moving the care of people with long-term conditions such as asthma from established specialist services to primary care should consider implementing collaborative educational strategies 44 . Matrix-support collaborative care that includes training and support for primary care physicians/nurses from specialists, including joint consultations, case discussions and tailored education, has been shown to be well-accepted by primary care professionals and was associated with improved knowledge and reduced respiratory secondary care referrals 44 . A scoping exercise and literature review of the effectiveness of educational interventions in either changing health professional practice or in improving health outcomes was commissioned by The International Primary Care Respiratory Group (IPCRG) 83 . The impact of education interventions on their own was inconclusive, although there was some evidence of effectiveness when they are combined with other quality improvement strategies or incentives 83 .
Asthma continues to be a substantial cause of morbidity and mortality worldwide and there is need for a coordinated effort to improve care. A well-resourced primary care service is central to the provision of accessible and effective asthma care. An expert team identified the drivers that could enable improvements in both clinical management and patient outcomes, and a literature search showed that each of these individual drivers is supported by varying degrees of evidence. Objectively assessing the outcomes of such interventions is challenging because studies in this area are inherently complex, difficult to undertake and resource intensive, and so definitive research is seldom undertaken. In contrast single interventions studies are easier to conduct but frequently methodologically less robust and therefore tend to be inconclusive. Nevertheless, if substantial improvements in the management of asthma in primary care at a global level are to be achieved, combinations of interventions appear to be most effective. Well-supported holistic interventions involving the entire healthcare system and including the patient voice appear to provide the best outcomes.
Expert panel
An expert panel of 12 primary care global asthma experts—ten General Practitioners and two specialist nurses—was convened in Amsterdam. An initial teleconference between the panel preceded the meeting to gather ideas. The expert panel undertook a brainstorming exercise as part of a force-field analysis in order to reveal their ideas and experience regarding drivers of successful management of asthma in primary care 84 . A force-field analysis can be used to determine the forces (factors) that may prevent change from occurring and to identify those that cultivate change. During the brainstorming session, the experts were divided into facilitated groups to discuss the relative importance of the drivers and identify the factors which underpin each of them. Results were analysed thematically and circulated after the meeting for comment and agreement.
Literature review
To identify whether evidence existed for the drivers and factors identified by the expert panel, literature was searched from PUBMED using the terms asthma and primary care in combination with other terms listed in Table Table5. 5 . Proposed search terms were combined using Boolean operators. The initial search was limited to papers published in English over the last 10 years and studies in adults aged over 18 years old. The experts were also asked for additional papers and in addition, more articles were identified from the references from the selected papers. Papers identified were subsequently screened for eligibility by MF and TM (Fig. (Fig.1). 1 ). A total of 171 were included in the summary table of which 50 papers were identified as having evidence for the factors identified by the panel.
Combinations of keywords used in PubMed search.
| Asthma AND primary care; = 6535 |
| Asthma and primary care AND outcomes; = 1502 |
| Management of asthma in primary care AND outcomes, = 821 |
| Asthma AND primary care AND outcome AND improvement; = 1728 |
| Asthma AND primary care AND team building; = 14 |
| Asthma AND primary care AND team; = 274 |
| Asthma AND primary care AND incentives; = 105 |
| Asthma AND family practice AND outcome AND improvement in adults; = 28 |
| Asthma AND general practice AND outcome AND improvement in adults; = 62 |
| Asthma AND family practice AND adults; = 950 |
| Asthma AND general practice; = 622 |
| Asthma AND quality improvement; = 455 |

Process by which papers identified by literature review were subsequently screened for eligibility and the different stages in this process. This highlights the number of articles that were selected at each stage of the process, as well as the number of articles excluded and the reasons for exclusion. n number of articles.
Acknowledgements
The authors gratefully acknowledge the Expert Panel contributions of Tan Tze Lee (Singapore). Editorial support (in the form of writing assistance, collating author comments, assembling tables/figures, grammatical editing, fact checking, and referencing) was provided by Diana Jones, Ph.D., of Cambrian Clinical Associates Ltd. (UK) and was funded by GlaxoSmithKline plc. The expert panel meeting was funded by GlaxoSmithKline plc.
Author contributions
All authors participated in the expert panel meeting. M.F. and T.v.d.M. were responsible for screening the papers identified in the literature search for suitability for inclusion in the article. All authors developed the manuscript and approved the final version to be submitted.
Data availability
Competing interests.
D.L. is an employee of GlaxoSmithKline plc., and holds stocks in GlaxoSmithKline plc. M.F. and T.v.d.M. are former employees of GlaxoSmithKline plc., and M.F. holds stocks in GlaxoSmithKline plc. I.T. reports advisory boards from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline plc. and Novartis and a grant from GlaxoSmithKline Greece, outside the submitted work. J.K. reports grants and personal fees from AstraZeneca, grants and personal fees from Boehringer Ingelheim, grants from Chiesi, grants and personal fees from GlaxoSmithKline plc., grants and personal fees from Novartis, grants from Mundipharma, grants from TEVA, outside the submitted work. A.C. reports a grant from AstraZeneca for an asthma study. C.C. reports grants from Pfizer China, outside of the submitted work. M.T. reports the following conflicts of interest: neither M.T. nor any member of his close family has any shares in pharmaceutical companies; receipt in the last 3 years of speaker’s honoraria for speaking at sponsored meetings or satellite symposia at conferences from GlaxoSmithKline plc. and Novartis, companies marketing respiratory and allergy products; receipt of honoraria for attending advisory panels with Boehringer Inglehiem, GlaxoSmithKline plc. and Novartis; membership of the BTS SIGN Asthma guideline steering group and the NICE Asthma Diagnosis and Monitoring guideline development group. P.K. reports personal fees from AstraZeneca, GlaxoSmithKline plc., Chiesi, Menarini, Novartis, Klosterfrau, Bionorica, Willmar Schwabe and MSD, and other support (for a phase 3 investigator cough study) from MSD, all outside the submitted work. C.S. has no shares in any pharmaceutical companies, she has received consultant agreements and honoraria for presentations from several pharmaceutical companies that market inhaled medication including AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline plc., Napp Pharmaceuticals and Teva. J.C.d.S. reports personal fees and speaker’s honoraria from Boheringer Ingelheim, personal fees and speaker’s honoraria from GlaxoSmithKline plc., personal fees and speaker’s honoraria from AstraZeneca, personal fees and speaker’s honoraria from Mundipharma outside the submitted work. M.R.R. reports personal fees from AstraZeneca, personal fees from Boehringer Ingelheim, personal fees from Chiesi, grants and personal fees from GlaxoSmithKline plc., personal fees from Menarini, personal fees from Mundipharma, personal fees from Novartis, personal fees from Pfizer, personal fees from Teva, personal fees from Bial, outside the submitted work. E.M.K. received honoraria for attending advisory board meeting from GlaxoSmithKline plc., Boehringer Inglehiem and grant from Novartis outside the submitted work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- What is the evidence...
What is the evidence for different management options for difficult to treat severe asthma?
- Related content
- Peer review
- Drug and Therapeutics Bulletin
- Drug and Therapeutics Bulletin Editorial Office, London WC1H 9JR, UK
- dtb{at}bmjgroup.com
What you need to know
Asthma causes 1000 deaths a year in the UK
The goals of treatment should be identified with the patient and agreed as part of an asthma action plan.
Assessment of people with difficult asthma should be facilitated through a dedicated multidisciplinary asthma service
Some patients are misdiagnosed with asthma, when they may not have asthma at all or there may be other pathology contributing to symptoms
Oral corticosteroids are the mainstay of treatment for patients with severe asthma and are effective for most patients, but should be used at the lowest dose that maintains asthma control
The management of adults with asthma that remains uncontrolled despite treatment with high dose therapies poses a challenge to clinicians and patients. National and international guidelines recommend intensification of treatment that typically involves the use of oral corticosteroids. 1 2 The risks associated with long term systemic corticosteroid treatment are well documented and have led to the search for alternatives. Recent advances in the understanding of the pathology of asthma have prompted the development of other treatment options. Here, we consider the options available for people who require continuous or frequent use of oral corticosteroids and review the safety and efficacy of such treatments.
How common is it?
In the UK, over four million adults are being treated for asthma, and it remains responsible for more than 1000 deaths a year. 3 4 Asthma exacerbations resulted in over 60 000 hospital admissions in 2013-14, with an estimated annual cost of £1bn to the NHS. 3 4
The goals of asthma management are good symptom control with minimal exacerbations (see box 1). 1 2
Box 1: Definition of complete control of asthma 1
No daytime symptoms
No night time awakening due to asthma
No need for rescue medication
No asthma attacks
No limitations on activity, including exercise
Normal lung function
Minimal adverse effects from medication
The goals of treatment …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £33 / $40 / €36 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
- Newsletters
- Account Activating this button will toggle the display of additional content Account Sign out
The People Who Dismantled Affirmative Action Have a New Strategy to Crush Racial Justice
Last summer, in Students for Fair Admissions v. Harvard College , the Supreme Court’s conservative supermajority struck down race-conscious admission programs adopted by Harvard College and the University of North Carolina as violations of the 14 th Amendment’s equal protection clause. In doing so, the court’s conservative supermajority both ignored that the Framers of the 14 th Amendment were the originators of affirmative action and turned a blind eye to entrenched racial inequalities that make a mockery of the constitutional promise of equal citizenship. Now, Edward Blum, who was behind the attack on affirmative action in the SFFA case, and other conservative litigants intent on blocking racial justice efforts have a new strategy: remake the nation’s oldest federal civil rights law, the Civil Rights Act of 1866, into a weapon to challenge private efforts to ameliorate systemic racial discrimination and to redress the racial wealth gap.
Last week, in American Alliance for Equal Rights v. Fearless Fund Management , a divided panel of the U.S. Court of Appeals for the 11 th Circuit became the first federal court of appeals to place its imprimatur on Blum’s new tactic. In a 2–1 ruling, the court of appeals held that Fearless Fund’s grant program to provide capital funding to small businesses run by Black women violated a key federal civil rights statute that dates back to the Civil Rights Act of 1866. Known as Section 1981, this law guarantees the equal right to make and enforce contracts.
The court’s opinion, written by Judge Kevin Newsom and joined by Judge Robert Luck, both Donald Trump appointees, held that Fearless Fund’s privately financed effort to rectify the near-total exclusion of Black women from venture capital and ensure that women of color have access to the resources they need to enjoy economic freedom and succeed in business was an unlawful form of racial discrimination. Adopting a strict colorblind reading of Section 1981, Newsom insisted that permitting a grant program open only to Black women “would be anathema to the principles that underlie all antidiscrimination provisions” and preliminarily enjoined its operation.
Newsom’s majority opinion works hard to portray the result as compelled by settled legal principles, but make no mistake, Fearless Fund is a big deal: It perverts a landmark civil rights statute aimed at guaranteeing basic rights of economic citizenship to Black Americans and redressing the long shadow of enslavement, and it creates new barriers to efforts to ensure racial inclusion. Never mind that eradicating racial subordination and guaranteeing economic justice lie at the very core of Section 1981. The two Trump-appointed jurists in the majority effectively read these fundamental precepts out of the statute, holding that Black-owned companies cannot put their own private money into the work of redressing the racial wealth gap and helping to ensure the success of Black-owned companies. According to the court of appeals, Fearless Fund’s grant program must be available to white-owned businesses as well.
The colorblind reading of Section 1981 advanced by Newson’s majority opinion is profoundly antitextual. The Civil Rights Act of 1866 was intentionally written in a race-conscious manner. The act declares that citizens “of every race and color … shall have the same right … to make and enforce contracts, to sue, be parties, and give evidence, to inherit, purchase, lease, sell, hold, and convey real and personal property, and to full and equal benefit of all laws and proceedings for the security of person and property, as is enjoyed by white citizens.” Recognizing that enslaved Black Americans never had rights to contract and property—rights essential to equal citizenship—Congress used sweeping language to ensure that persons of “every race and color” would “enjoy” the same economic freedoms as “white citizens.” The statute is not aimed at the use or consideration of race at all; instead, it uses the rights of white citizens as a baseline to guarantee to Black Americans rights of economic citizenship that white citizens have long taken for granted. Newsom quotes the relevant statutory language, but pays the text lip service.
Congress chose this text for good reason: The Reconstruction-era Civil Rights Act was critical to enforcing the 13 th Amendment, eradicating badges of slavery and ensuring that Black Americans freed from bondage were entitled to basic economic rights and enjoyment of the fruits of their labor. It came in direct response to former enslavers seeking to impose new forms of servitude and reduce Black Americans to serfdom. With these new race-conscious protections, the Reconstruction-era Civil Rights Act’s Framers insisted, “all features of slavery which are oppressive in their character, which extinguish the rights of free citizens, and which unlawfully control their liberty shall be abolished and destroyed forever.” The Fearless Fund ruling perverts the statute’s roots in securing economic justice, even as it forbids Black-led businesses from using their own money to ameliorate systemic patterns of economic exclusion and inequality.
The Congress that enacted the Civil Rights Act of 1866 knew that private efforts were crucial to racial and economic uplift. One of the singular successes of Reconstruction was the creation of the nation’s first schools and colleges for Black Americans in the South , spurred by charitable giving by abolitionists and others who devoted significant resources to education in recognition that knowledge is power. In throwing up new roadblocks to the use of private money to redress racial and economic inequality, the Fearless Fund ruling is both deeply antitextual and antihistorical.
Fearless Fund will be far from the last word on the meaning of Section 1981. As other courts consider Ed Blum’s conservative effort to rewrite that critical act, they should remember that the Civil Rights Act of 1866 sought to redress continuing badges of enslavement and to make economic justice a reality. Reconstruction’s great constitutional transformations were race-conscious to the core. In passing statutes like the Civil Rights Act of 1866, Congress understood the need for far-reaching remedies to rectify centuries of racial enslavement, oppression, and violence and to ensure some measure of economic justice to Black Americans. Getting this history right is essential to exposing the glaring flaws in conservative rulings, like Fearless Fund , and to addressing the next wave of coming cases seeking to roll back racial justice efforts.
Javascript is currently disabled in your browser. Several features of this site will not function whilst javascript is disabled.
- Why Publish With Us?
- Editorial Policies
- Author Guidelines
- Peer Review Guidelines
- Open Outlook
- Submit New Manuscript
- Sustainability
- Press Center
- Testimonials
- Favored Author Program
- Permissions
- Pre-Submission

open access to scientific and medical research
Back to Journals » Journal of Asthma and Allergy » Volume 12
Approaches to the assessment of severe asthma: barriers and strategies
- Get Permission
- Cite this article
Authors Majellano EC , Clark VL , Winter NA , Gibson PG , McDonald VM
Received 4 June 2019
Accepted for publication 25 July 2019
Published 23 August 2019 Volume 2019:12 Pages 235—251
DOI https://doi.org/10.2147/JAA.S178927
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Amrita Dosanjh
Eleanor C Majellano, 1, 2 Vanessa L Clark, 1, 2 Natasha A Winter, 1, 3 Peter G Gibson, 1, 4 Vanessa M McDonald 1, 2, 4 1 Faculty of Health and Medicine, National Health and Medical Research Council Centre for Research Excellence in Severe Asthma and the Priority Research Centre for Healthy Lungs, The University of Newcastle, Newcastle, NSW, Australia; 2 Faculty of Health and Medicine, School of Nursing and Midwifery, The University of Newcastle, Newcastle, NSW, Australia; 3 Faculty of Health and Medicine, School of Medicine and Public Health, The University of Newcastle, Newcastle, NSW, Australia; 4 Department of Respiratory and Sleep Medicine, John Hunter Hospital, Hunter Medical Research Institute, Newcastle, NSW, Australia Correspondence: Vanessa M McDonald Level 2 West Wing, Hunter Medical Research Institute, Locked Bag 1000, New Lambton Heights, NSW 2305, Australia Tel +61 24 042 0146 Fax +61 4 042 0046 Email [email protected] Abstract: Asthma is a chronic condition with great variability. It is characterized by intermittent episodes of wheeze, cough, chest tightness, dyspnea and backed by variable airflow limitation, airway inflammation and airway hyper-responsiveness. Asthma severity varies uniquely between individuals and may change over time. Stratification of asthma severity is an integral part of asthma management linking appropriate treatment to establish asthma control. Precision assessment of severe asthma is crucial for monitoring the health of people with this disease. The literature suggests multiple factors that impede the assessment of severe asthma, these can be grouped into health care professional, patient and organizational related barriers. These barriers do not exist in isolation but interact and influence one another. Recognition of these barriers is necessary to promote precision in the assessment and management of severe asthma in the era of targeted therapy. In this review, we discuss the current knowledge of the barriers that impede assessment in severe asthma and recommend potential strategies for overcoming these barriers. We highlight the relevance of multidimensional assessment as an ideal approach to the assessment and management of severe asthma. Keywords: asthma, severe asthma, severity, assessment, barriers, strategies
Introduction
Asthma is a significant public health threat, affecting more than 300 million individuals globally. 1 Asthma is classified as a non-communicable disease and leads to reduced quality of life, 2 poor physical functioning 3 and reduced emotional well-being. 4 The impact of this disease can be widespread and extends beyond the person living with the disease, affecting the lives of their family members, carers, communities and the health care system. 5
Asthma is a variable chronic respiratory condition. It is characterized by symptoms of wheeze, cough, chest tightness, dyspnea and backed by variable airflow limitation, airway inflammation and airway hyper-responsiveness (AHR). 1 The severity of asthma varies considerably, both between individuals and within individuals over time. 1 Some people may have intermittent asthma and others may experience severe, potentially life-threatening disease. In mild-to-moderate asthma, inhaled corticosteroids (ICS), bronchodilators and self-management education are the cornerstone of effective treatment. 5 However, 3% 6 to 10% 7 of the patients experience a severe form of asthma that fails to respond to standard therapy despite receiving maximal treatment. Thus, severe asthma is defined as “asthma which requires maximum controller therapy to prevent a patient from becoming uncontrolled or which, despite high dose therapy remains uncontrolled.” 7 Patients diagnosed with severe asthma endure significant difficulties in daily living, a decrease in physical activity, 3 work capacity or productivity 8 and social exclusion. 2 Furthermore, patients with severe asthma are faced with an increased comorbidity burden. 2 , 7
There is a wide array of comorbidities present in severe asthma that may contribute to disease severity, mimic asthma symptoms, and therefore confound assessment and treatment. 9 For example, chronic rhinosinusitis is a prevalent comorbidity of asthma and contributes to disease severity. 7 Similarly, obstructive sleep apnea, obesity and psychological factors often co-exist and complicate management. 7 These comorbidities mimic asthma symptoms and affect the intensity of the disease, management or diagnosis, leading to a much greater risk of asthma morbidity and mortality. 7 Given the complexity and heterogeneity of the disease, assessment and management of severe asthma warrants advanced approaches. 5 , 10
Guidelines for asthma management have proposed that evaluation of disease severity is necessary to initialize therapy and maintain treatment through a step-wise process. 11 Misclassification of the levels of severity may contribute to the underuse or overuse of anti-inflammatory medications, resulting in either poor asthma control or adverse side-effects associated with overtreatment. 11 With the advent of biological therapies, 12 recognition of the level of asthma severity is imperative to facilitate treatment interventions to the right patients. 12
The literature on diagnosing, treating and managing severe asthma indicates that significant barriers exist across health care settings and that these barriers relate to health care providers, patients and organizational systems. 10 Overcoming these barriers is necessary in order to facilitate effective assessment and accelerate appropriate treatment for severe asthma patients. 13 Therefore, identification of the barriers related to precision assessment of severe asthma is an important step. The purpose of this review is to discuss current knowledge of the barriers that impede assessment in severe asthma and to recommend potential strategies for overcoming these barriers. We highlight the importance of multidimensional assessment as an approach to the assessment and management of severe asthma.
Search strategy
The literature search is current as of March 2019 using the electronic databases CINAHL, Pub Med, Web of Science, Google Scholar, Wiley, and Medline. The search strategy includes the keywords of asthma, severe asthma, severity, assessment, barriers and strategies. English written articles between 2014 and 2019 were retrieved and included to reflect the current literature. However, we did not exclude seminal papers which were highly cited and judged to be relevant to answer our aims. We also checked reference lists to identify relevant studies significant for our review.
Measurement of asthma severity
Severity-based stratification of patients with asthma is an integral part of management, providing a useful blueprint for treatment decision making. 11 Categorization of asthma severity reinforces the regulation, duration and calculation of the amount and type of therapy to establish asthma control. 11 Patients with well-controlled asthma have minimal symptoms or functional impairment related to their disease. 11
The general definition of severity implies “the intrinsic intensity of the disease process,” 11 however, defining severity is often challenging because asthma is associated with a wide range of heterogeneity. 14 In addition, genes and environmental exposures like allergens, cigarette smoke or air pollution play a crucial role that may change or influence disease progression over time. 14 Therefore, periodic assessment is necessary to assist asthma management and treatment. To date, there is no gold standard for classifying asthma severity or robust data showing significant changes in disease severity in a longitudinal cohort. 15 The Global Initiative for Asthma (GINA) strategy recommends that asthma severity should be determined according to the level of treatment required to control and reduce symptoms and exacerbations. 1 A step-wise approach to treatment is recommended where each of the five steps constitutes five levels of increasing treatment recommended according to severity. Step 1 to 3 represents mild–moderate disease, with steps 4 and 5 depicting moderate-severe asthma, which requires high-dose ICS/Long-Acting Beta-Agonist (LABA) treatment to achieve and maintain asthma control. 1 In some cases, severe asthma may remain uncontrolled despite high-dose therapy, suggesting the need for further multidimensional and systematic assessment and treatment ( Figure 1 ).
Severe asthma assessment
The assessment of severe asthma is complex. This is because the disease is heterogeneous in nature and associated with many comorbidities; therefore, a multidimensional evaluation is essential. 16 Figure 1 shows a practical guide designed to critically diagnose, characterize and manage severe asthma. We elaborate on these steps further in the next section.
Diagnosis confirmed
Harm from asthma medications may arise from misdiagnosis. 15 , 17 Hence, a comprehensive work-up is important to ascertain whether the patient has severe asthma. 9 A detailed history is the first step to the assessment and diagnosis. 9 The medical history should focus on characterizing the specific symptoms, their frequency and severity. 7 Clarification of the onset of symptoms, determination of the severity of exacerbations and associated comorbidities are also essentials. 9 Accordingly, clinical questionnaires can facilitate these assessments. 9 Physical examination of the cardio-respiratory system is also important. 9 When critical information of the patient’s symptoms is gathered, clinicians gain a better understanding of the patient’s problem.
| Pulmonary function tests to consider in severe asthma |
Biomarkers are observable characteristics that are objectively measured as an indicator of normal or abnormal biologic processes. 28 The clinical utility of biomarkers includes four main roles: 1) diagnosis, 2) disease staging, 3) ongoing assessment of disease progression and 4) assessment of treatment response. In addition to being a guide for clinicians, the process of biomarker investigation allows for a comprehensive understanding of the underlying molecular pathways behind disease pathogenesis as well as the discovery of new targets for novel therapies. At present, airway inflammatory biomarkers used in practice include serum immunoglobulin-E (IgE), peripheral blood eosinophils, sputum eosinophil counts and exhaled fraction of nitric oxide (FeNO). 29 However, limitations of biomarkers do exist, impeding implementation in clinical practice. Barriers and strategies to overcome these limitations will be discussed in the sections below.
Is it severe?
| Criteria for uncontrolled asthma |
| Asthma definitions and characteristics |
| Checklist for the multidimensional assessment of severe asthma. Figure reproduced with permission from the Centre of Excellence in Severe Asthma, originally developed as part of the Severe Asthma Toolkit © ( ). |
| Checklist of important contributory factors in severe asthma |
Is treatment optimized?
| Useful tools for assessing adherence |
Multidimensional assessment
| Clinical domains in the phenotyping of severe refractory asthma. Figure reproduced with permission from the Centre of Excellence in Severe Asthma, originally developed as part of the Severe Asthma Toolkit © ( ). |
To demonstrate the possible benefits of multidimensional assessment, a meta-analysis of three observational studies has reported improvements in health-related quality of life (HRQoL), asthma control and reduction in exacerbations, up to a year after the implementation of multidimensional assessment. 43 More recently, McDonald and colleagues completed the first randomized controlled trial (RCT) in severe asthma utilizing multidimensional assessment and individualized management targeting the traits identified in each individual and demonstrated improved outcomes for patients. 45
Individualized management plan
Patients with severe asthma require tailored evidence-based interventions to meet their needs. Case-management is one approach that can assess, plan, facilitate and coordinate health care delivery through partnerships with clinicians, patients and their families. 46 In a study of older patients with asthma and COPD, significant improvements in quality of life were sustained for 1 year in COPD patients who underwent multidimensional assessment and individualized management. 47 More recently, this approach has been tested in patients with severe asthma as described earlier. 45
Barriers to severe asthma assessment
| Barriers to assessment of severe asthma by stakeholders. |
Barriers related to health care practitioners (HCP)
A number of barriers that relate to HCPs have been identified ( Figure 3 ). These include a lack of knowledge about guideline-recommended therapies, inconsistent diagnosis and management, referral pathway issues and communication gaps. 10 , 13 , 32
The role of guidelines and checklists
Although evidence suggests that the use of clinical guidelines and checklists are beneficial and are prime components in asthma management, unfortunately there is also evidence showing HCPs’ low adherence to guidelines. 32 , 48 , 49 Findings from a national survey of severe asthma experts in Australia report that 60% of the clinicians managing patients with severe asthma do not use checklists, but believed they would find one useful. 10 In an observational study that assessed the barriers to improving the management of patients with severe asthma, the underuse of guidelines suggested suboptimal asthma control. 48
There are several proposed reasons as to why HCP adherence to guidelines and checklists may be suboptimal. 50 These include professional issues relating to clarity of roles, 51 lack of familiarity with guidelines, 15 , 52 lack of training and skills, 53 distrust about guidelines in general, 54 complex and lengthy guidelines, 55 poor teamwork, lack of self-efficacy, 51 poor communication, 56 limited access to spirometry 57 or lack of belief that a guideline or checklist will produce positive outcomes. 10 , 49 Other HCPs viewed guidelines as inflexible 15 or identified that asthma guidelines do not thoroughly focus on severe asthma. 10 Moreover, external barriers influencing HCPs’ adherence to guidelines include lack of time, 51 organizational constraints 10 and inability to reconcile patient preferences with guideline recommendations. 52 Several approaches have been undertaken to address these issues in severe asthma. GINA published practical recommendations about how to identify, assess and manage difficult to treat and severe asthma in adolescent and adult patients. 1 Practice guidelines are designed to provide recommendations to assist and guide HCPs in making clinical decisions. 58 When used by an HCP in practice, asthma guidelines could minimize diagnosis and assessment inconsistencies, reducing avoidable emergency department visits and hospitalizations. 58 Furthermore, to overcome the barriers related to the lack of training and resources available for severe asthma clinicians, the Australian Centre of Excellence in Severe Asthma produced an online toolkit to provide evidence-based guidance to clinicians globally ( http://toolkit.severeasthma.org.au ). The main goal of providing the toolkit is to equip HCPs with clinical resources essential in the management of severe asthma. 59 Thus, better meeting the needs of HCPs across health care settings irrespective of geographical locations. 59 The Severe Asthma Toolkit offers the latest treatment options to optimize care in severe asthma patients, covering various modules ranging from medications, diagnosis, assessment, management and comorbidities among others. 59 The toolkit was created by a world-class multidisciplinary team with clinical expertise in severe asthma. 59
Inconsistent approach for diagnosis or management
Despite the significance of spirometry in respiratory function testing for assessing severity, the test is widely underutilized for asthma in primary care. 32 Furthermore, biomarkes used in severe asthma management are also underutilized, in an online survey to clinicians involved in severe asthma management, 53% of the respondents indicated that they never used FeNO testing, 10 a surrogate marker of eosinophilic airway inflammation.
Similarly, this survey also reported that assessments for some comorbidities such as naso-endoscopy, functional exercise test or bone mineral densitometry were never initiated, by 60%, 46% and 32% of the respondents, respectively. 10 Health status, asthma control and comorbidities questionnaires were also inconsistently used. 10 Of note, determining whether or not a treatment effect is clinically meaningful is a great challenge in severe asthma. 60 Barriers to routine use of self-reported questionnaires include logistical, technical and lengthy administration inhibiting successful adoption of some patient-reported outcome measures (PROMs) in clinical practice. 2 PROMs that have been developed specifically for severe asthma provide a valid assessment of the patient’s health status, level of control and experience of severe asthma and are useful in the clinic. 2 Variability in diagnosis, assessment and management could lead to serious consequences for patients with severe asthma. 15 Diagnostic uncertainty in asthma still exists, with severe asthma being underdiagnosed or overdiagnosed, 61 indicating that diagnostic precision remains a serious issue in the era of targeted therapy.
Referral pathways
Referral systems offer patients access to expert HCPs in the field of severe asthma. 32 , 52 A timely referral to specialized care should be actioned when patients in primary health care continue to experience suboptimal control, with increased severity, despite guideline-based treatment. 62 Notwithstanding the importance of a linkage pathway, variations in referral patterns from primary health care to secondary health care have been a constant concern both at the international 48 and national scene. 10 The lack of clear referral criteria limits success in optimal management. McDonald et al 10 highlighted that for a referral system to work in severe asthma, a referral at all levels of care should be defined. One example of a referral intervention from primary health care to secondary health care is the SIMPLES model. 63 The SIMPLES model is a structured framework used in primary health care to evaluate patients with difficult to control asthma. 62 , 63 If patients have not achieved control despite structured reviews, a referral to severe asthma specialist clinic is warranted for further evaluation and management. 62 The SIMPLES approach suggests a good interface between primary and specialist care, integrating clinical assessment and management, whilst avoiding inappropriate escalation of treatments. 62 , 63
Orozco-Beltran et al 48 conducted a study using a modified Delphi method on the management and referral of severe and poorly controlled asthma where they found physicians dissatisfaction in the referral process. The majority of non-severe asthma patients are treated in secondary health care when they can be appropriately managed in primary health care. 48 The lack of clarity and consensus of the referral criteria between primary health care and secondary health care drives up costs and diversion of resources. 48 A retrospective observational study 64 has also reported findings that are consistent with the outcomes of Beltran et al. 48 HCPs have identified the need for a well-defined and extensive criteria to guide referral decision making and to ensure equitable access to available health services. 10 , 48
Barriers related to patients and clinicians
A number of factors have been identified as contributing to suboptimal severe asthma assessment: patient–provider communication, personal perceptions or beliefs 65 and managing symptoms and risk factors. 60
Poor patient–physician communication
Effective patient–provider relationships are important for patients with asthma and can lead to improved outcomes. 66 Communication is a cardinal component and foundation for a positive patient–provider relationship, increasing patient satisfaction and better adherence to treatment. 66 As a result, satisfied patients are more likely to share critical health information with their physicians. 66
However, conflicting perception between the patient and the HCP can negatively impact patients’ health. 67 The observational study of discordance in patients and HCPs’ views on asthma control by Crespo-Lessmann et al 67 concluded that patient–provider discordance is likely to contribute to an increased risk of poor asthma control. Communication is a fundamental element to developing a patient-centered treatment plan but authoritarianism or paternalism in clinical settings disempowers patients, limiting a two-way conversation. 68 The level of respect, time constraint, cultural and language diversity also impede stronger relationships and communication between patients and physicians. 69
Patient personal perceptions
The patient’s perspective is essential to both assessment and management of severe asthma, but when patients overestimate or underestimate disease severity or the level of asthma control required, then it becomes a significant barrier. 70 A qualitative study by Bidad et al 71 that sought to determine patients’ perception of asthma control identified five themes: (a) personal meaning of control, (b) intermittent prevention, (c) compromising control to avoid medication, (d) pharmacological agents overemphasized in control and (e) the role of asthma review in control. 71 In one of the themes, patients described having their own “internal barometer” of the level of symptoms in determining when their level of control was decreasing and this was determined to be much higher than the asthma control test (ACT) cut points. 71 Moreover, primary care patients did not perceive asthma review appointments as an advantage to asthma control, but rather as an additional burden. 71 This perception was compounded by clinical practice variations and conflicting advice provided by HCPs. 71
Managing symptoms and risk factors
The complexity of severe asthma explains why patients seek a comprehensive understanding about their disease. 60 When patients acquire greater understanding of their illness, a sense of control and empowerment is achieved enabling them to make positive choices and set goals. 68 Unfortunately, the patients’ journey toward acquiring the desired knowledge is not straightforward. When faced with ambiguity, patients have reported that they receive little information from their HCPs. 68 As a result, patients will seek information from elsewhere, including potentially unreliable sources. 68 Individuals with limited knowledge about asthma symptoms, common triggers and risk factors are at a heightened risk for poor asthma control. Limited health literacy in patients and an absence of patient-centered care can lead to non-adherence to medications and suboptimal self-management. 68 In an explorative study by Lingner et al 72 on patient and HCPs’ concept of good asthma treatment, patients desired to share the decision-making process with their HCPs. However, several patients discussed their reluctance to discuss their asthma with their HCP due to their perception that their HCPs had preconceived notions, for example, “they always blame your weight”, 68 implicating a barrier to the patient–clinician relationship. 60
Barriers related to system factors and equitable access to specialized service
There are numerous factors influencing delivery of care. Barriers arising from the structural level include longer waiting lists due to lack of specially trained HCPs, high service demand 32 coupled with insufficient resources. 10 In addition, there is a complex procedure required to access novel therapies 12 and there is limited access to some biomarkers in many facilities. 73
Geographic barriers disproportionately burden patients with financial incapacities or even severe asthma patients who require closer attention from the specialist and multidisciplinary team (MDT). 10 MDTs are a group of HCPs who coordinate, manage and organize care for people with severe asthma. 31 The core staff necessary to run a severe asthma clinic includes respiratory physician, specialist nurse, pulmonary function scientist and speech pathologist. 31
Often rural patients have to travel long distances to specialized services and therefore, places severe asthma patients in a difficult position, weighing up travel costs and benefits. 10
Waitlist and appointment delays
Longer waiting times suggest underlying issues or unresolved conflicts in resources, stakeholders, policies or systems in the delivery of services. 74 This means that prolonged waiting periods are significant barriers for patients. Not being able to obtain the right services and appropriate treatments at the right time impacts patient expectations and satisfactions. 75 Some studies have demonstrated that appointment delay causes stress for both patients and HCPs reducing positive outcomes. 74 Fielden et al 76 demonstrated that prolonged waiting times of >6 months result in greater economic costs and deterioration in physical function and in HRQoL.
Complexities of accessing novel biological therapies
With the use of novel biological therapies on the rise, patients deserve timely access to these targeted treatments. 62 Access to novel therapies can vary significantly across international health care settings and requires different prerequisites before these drugs can be prescribed. In Australia, the long waiting periods of usually 6–12 months deter access to biologics. 10 , 12 During those months, specialists, for their part, are trying one or more add-on therapies before initiating biological therapies. 12
Lack of accessible biomarkers
In order to improve outcomes for severe asthma patients, it is critical that we devise a more definitive approach to assessing patients with asthma. Biomarkers represent a solution to characterizing patients in order to predict prognosis and treatment response. 77 Airway inflammation is an acceptable starting point for discovering biomarkers as inflammation plays a critical role in underlying pathologies. 78 – 80 The current gold standard of assessing airway inflammation is sputum cell counts but this has limitations in the clinical setting. Techniques involved in collecting and processing specimens are time-consuming, require skill and there are issues with reproducibility and inconsistent cut-off values, restricting sputum cell counting to specialized- or research-based centers. 81 In response, surrogates of airway inflammation have been developed, including blood eosinophils, 82 FeNO 83 , 84 and periostin. 85 However, none are free from contradicting results 81 , 86 , 87 and confounding factors. 88 , 89 As a result, the use of these markers in diagnosis and assessment, prediction and prognosis has had slow uptake but is a priority for future research and current practice. In addition, although biomarkers indicative of eosinophilic inflammation have been developed and validated, there are currently no biomarker surrogates for non-eosinophilic inflammation. 90 , 91 This is of critical importance as many severe asthma patients present with non-eosinophilic inflammation and some may have persistent neutrophilic inflammation. 92
So how do we develop the “ideal biomarker”? Many factors determine the ideal biomarker and can act as hindrances to biomarker development and its clinical utility. 93 Important in the clinical setting are that biomarkers are accessible and non-invasive and the techniques to measure are rapid, straightforward and relatively inexpensive. 93 Whereas, it is completely valid to use invasive techniques, such as bronchial biopsies and bronchial lavage, to detect new molecular pathways and mechanisms, accessible biomarker sources such as blood, urine, sputum and exhaled breath are preferred. Additionally, due to the complexity of asthma, a single biomarker will not be sufficient to capture the full disease process. Therefore, we need further research generating composite panels of biomarkers from varying non-invasive sources. 73 , 94
Commendations must be made to the surrogate inflammatory biomarkers that do exist. But unfortunately, biomarkers must also be reliable and reproducible and despite the great amount of research that has been invested in biomarker discovery and testing, the ideal biomarker does not yet exist in asthma and conflicting results and limitations still remain a reality.
Overcoming barriers
To facilitate optimal evaluation and assessment of severe asthma, the following key recommendations should be taken into consideration.
Strategies related to health professional factors
Optimization of referral avenues and guidelines.
A centralized web-based database system can facilitate the transmission of valuable information. 10 When necessary, treating physicians have the capacity to access details including asthma symptom severity, exacerbation frequency, past and current therapies and spirometry outcomes. 32 The accessibility of this information can shorten the patients’ journey through the referral pathways, which can lead to improved HRQoL for severe asthma patients. 62 In addition, establishing a universal referral pathway to help select patients who will likely benefit from specialist evaluation can also streamline care. 10 , 13 To reinforce suitable referrals, regular monitoring should be implemented especially to patients with moderate or severe asthma. 95 For example, pulmonary specialists should follow-up patients admitted with severe asthma exacerbations for at least 1 year after the admission. 52
Provision for telehealth consultations from primary health care to secondary health care strengthens referral pathway as well. 48 It should be noted that primary care implements a gatekeeping system, whereby the general practitioner (GP) is in the principal position to recognize poorly controlled asthma. 32 The need to establish and develop a mechanism for involving GPs in the management of asthma should be consistent from the assessment all the way to the administration of biological therapies. 32 Systems in which patients can have their novel biological therapies administered within primary care, similar to rheumatoid arthritis, have been proposed to substantially reduce the burden of specialists in asthma services, paving the way to conveniently accommodate more patients. 10 , 32
Use of assessment tools
The use of assessment tools, specifically subjective and objective tools in severe asthma assists in viewing patients from a multidimensional perspective. 9 Furthermore, outcomes from the assessment form the basis of the care plan. The Centre of Excellence in Severe Asthma has developed valuable resources for HCPs, packaged in an online toolkit https://toolkit.severeasthma.org.au/ . 96 The Severe Asthma Toolkit is comprehensive and provides a convenient, easy-to-use resource to support and equip clinicians on how to achieve optimal severe asthma management. 96 Furthermore, to enhance diagnostic and assessments proficiency, knowledge dissemination within the workplace either through video conferencing, seminars and webinars can aid in practice. 97 Decision support tools like computerized systems, treatment guides, and standardized prescriptions assist HCPs in treatment decision making. 97
Strategies related to patient factors
Patient–physician communication.
The patient–provider relationship is dependent on good communication skills. 66 Apart from clinical competence, HCPs are required to master and demonstrate empathy, compassion, caring, non-judgment, open and concern during patient encounters. 68 There is a wealth of evidence in the literature that supports the benefit of efficient and effective communication resulting in increased patient satisfaction, better health outcomes, and decreased health care utilization 98 even without lengthening appointment times. 99 Providing a patient-centered care (PCC) approach is essential in asthma management. Under a PCC model, partnerships in health between HCPs, patients and carers are highlighted. 100 Consideration of patients’ preferences and values is demonstrated through patients’ active participation in clinical decision making. 100 A PCC model acts as a springboard in promoting flexible provision of health care and is moving beyond the traditional paternalistic approach. 100 Additionally, the role of patient advocates help patients navigate the health care system and bridge between patient and their treating clinicians reducing communication gaps. 101 Furthermore, communication failures between HCPs can be fostered through regular meetings and joint clinical sessions. 48
Strategies related to organizational factors
Assuring appropriate resourcing.
The severe asthma health workforce depends on the size of the service. In a conservative setting, at least one pulmonary physician and nurse specialist are needed; a second physician is necessary to overcome patient load or absences. 31 When workforce shortages exist, partnerships with nearby asthma network services may mitigate short-term periods of absence. 13 Benefits of a shared-care model, wherein special arrangements between public and private providers offer opportunity for expanding services and resources. 13 , 102
Improve access to MDT
Specialist MDTs are core for confirming diagnosis of severe asthma. 13 To optimize phenotyping and targeted therapy, providing continuous education and trainings for MDT members in severe asthma management is warranted. 10 Onsite availability and participation of nursing and allied health offer efficient services. 13 Funding for MDT could be achieved through a clinical re-design approach. 31 This method seeks to balance the costs and benefits, by reducing health care utilization and justifying the utilization of expensive therapies and patient outcomes. The use of teleconferencing or video-linked MDT discussion to its full advantage allows other practitioners to collaborate in decision-making process. 13 Telehealth can break down the wall of geographical barriers for patient treatment, follow up or initial in-person consultation. 10 , 13
Accessible biomarkers
A two-step approach can be taken to develop strategies to overcome barriers obstructing biomarker development and use in primary care. The first step is to discover novel biomarkers. Followed by the investigation and validation of newly discovered biomarkers from non-invasive sources, using easy-to-measure techniques.
“Omics” technology epitomizes the advancements that have been made in medicine and science. This new generation of exploratory science refers to the study of the biological system. They include, but are not limited to, genomics, proteomics, transcriptomics and metabolomics. The use of computational networking, bioinformatics and systems biology seeks to interpret the “big data” generated from the extensive exploration of the human organism. 103 , 104 In asthma, unbiased “omics” screening studies have been used to discover novel biomarkers, such as protein measurements in proteomics studies 105 and differential gene expression in transcriptomic studies. 106 With methods used to obtain data becoming less expensive and databases becoming larger and more secure to store the deluge of data, “omics” studies are becoming more prevalent and the combination of “omics” data, known as “multiomics”, is expanding, 107 deepening our understanding of the molecular and genetic pathways underlying disease.
In tying in with the characteristics of the “ideal biomarker”, new biomarkers must also be easy to obtain from non-invasive sources, using feasible techniques. Biomarkers from easily accessible tissues and fluids such as blood, urine, sputum and exhaled breath are ideal. Serum provides one of the most ideal sources for biomarkers as blood collection, serum preparation and analysis are highly standardized techniques and collection is minimally invasive. 73 However, recent studies in asthma have found that urine 73 and exhaled breath 88 are also promising sources of novel biomarkers, especially for children. 108 Although, these will require further research to validate. An example of ongoing research into non-invasive alternatives to sputum induction and more feasible measurements of airway biomarkers are through the recently developed absorptive nasal strip technology. Technology within absorptive strips permits the sampling of mucosal fluid within the upper respiratory tract 109 and measurement of airway inflammatory biomarkers, successfully shown to reflect sputum eosinophilia in a recent small study in asthma. 110 As a result, the powerful use of new technologies that convert ongoing advances of biomedical research into user-friendly tools that supplements and enhances current clinical tools can facilitate inter-professional communication between basic scientists, medical researchers and clinicians. 111
Point-of-care testing will also allow for fast and on-site assessment of multiple biomarkers. 112 In addition to biosensors and wearable monitoring devices, technology that continuously measures analytes in body fluids are currently being developed that could give real-time data on the measurement of specific molecules or biomarkers. 113 These point-of-care tests empower clinicians and allow patients to participate in the clinical decision-making process; an enabler for patient–clinician dialogue regarding treatment and management options.
Barriers to severe asthma assessment are influenced by multiple factors and can be grouped according to HCP-, patient- and systems-related factors. We have identified the barriers to assessing severe asthma and presented strategies to overcome these barriers. The highlighted barriers relate to inconsistent approaches to diagnosis and assessment, under referral, gaps in communication, poor perception on asthma control and organizational delimitations. Facilitators to overcome barriers to severe asthma assessment are standardized approaches and referrals, use of assessment tools and guidelines, implementation of a patient-centered care approach and better resources. Important opportunities of utilizing multidimensional assessment as an approach for implementation of care needs to be pursued where possible, to help overcome barriers in the assessment of severe asthma. Multidimensional assessment requires systematic assessment across three key domains (pulmonary/airway, extra-pulmonary/comorbidity and risk factor/behavioral domains) and can help identify important and clinically relevant traits, and help guide treatment decisions. Recognizing that multidimensional assessment can be time consuming and requires specialist teams, we propose that the benefits of this approach outweigh these barriers. This review highlights the need for further research into determining HCPs’ views of a feasible and acceptable approach to implement effective severe asthma management and generating composite panels of biomarkers from various non-invasive resources. These barriers are worthy of our attention if we desire a precision assessment in severe asthma.
Abbreviations
AHR, airway hyper-responsiveness; ICS, inhaled corticosteroids; GINA, Global Initiative for Asthma; LABA, long-acting beta agonist; IgE, immunoglobulin-E; FeNO, exhaled fraction of nitric oxide; ACQ, Asthma Control Questionnaire; ACT, asthma control test; FEV1, forced expiratory volume in one second; FVA, forced vital capacity; RCT, randomized controlled trial; HCP, health care professional; MDT, multidisciplinary team; GP, general practitioner; PCC, patient-centered care; HRQoL, health-related quality of life; PROMs, patient-reported outcome measures.
Dr Vanessa L Clark reports personal fees from Astra Zeneca and grants from National Health and Medical Research Council, outside the submitted work. Professor Peter G Gibson reports grants and personal fees from AstraZeneca, GlaxoSmithKline, Sanofi and Novartis, outside the submitted work. Professor Vanessa McDonald reports grants and personal fees from AstraZeneca, GSK and personal fees from Menarini, outside the submitted work. The authors report no other conflicts of interest in this work.
1. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, [Updated 2018]. Available from: https://ginasthma.org/wp-content/uploads/2018/04/wms-GINA-2018-report-V1.3-002.pdf . Accessed December 2, 2018.
2. McDonald VM, Hiles SA, Jones KA, Clark VL, Yorke J. Health-related quality of life burden in severe asthma. Med J Aust . 2018;209(2 Suppl):S28–S33.
3. Cordova-Rivera L, Gibson PG, Gardiner PA, Powell H, McDonald VM. Physical activity and exercise capacity in severe asthma: key clinical associations. J Allergy Clin Immunol Pract . 2018;6(3):814–822. doi:10.1016/j.jaip.2017.09.022
4. Foster JM, McDonald VM, Guo M, Reddel HK. “I have lost in every facet of my life”: the hidden burden of severe asthma. Eur Respir J . 2017;50:3. doi:10.1183/13993003.00711-2017
5. Reddel HK, Bateman ED, Becker A, et al. A summary of the new GINA strategy: a roadmap to asthma control. Eur Respir J . 2015;46(3):622–639. doi:10.1183/13993003.00853-2015
6. Hekking PP, Wener RR, Amelink M, et al. The prevalence of severe refractory asthma. J Allergy Clin Immunol . 2015;135(4):896–902. doi:10.1016/j.jaci.2014.08.042
7. Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J . 2014;43(2):343–373. doi:10.1183/09031936.00202013
8. Hiles SA, Harvey ES, McDonald VM, et al. Working while unwell: workplace impairment in people with severe asthma. Clin Exp Allergy . 2018;48(6):650–662. doi:10.1111/cea.13153
9. Wark PA, Hew M, Maltby S, McDonald VM, Gibson PG. Diagnosis and investigation in the severe asthma clinic. Expert Rev Respir Med . 2016;10(5):491–503. doi:10.1586/17476348.2016.1165096
10. McDonald VM, Maltby S, Reddel HK, et al. Severe asthma: current management, targeted therapies and future directions-A roundtable report. Respirology . 2017;22(1):53–60. doi:10.1111/resp.12957
11. National AE. Prevention P. Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol . 2007;120(5 Suppl):S94. doi:10.1016/j.jaci.2007.09.029
12. Upham JW, Chung LP. Optimising treatment for severe asthma. Med J Aust . 2018;209(S2):S22–S27.
13. Chung LP, Hew M, Bardin P, McDonald VM, Upham JW. Managing patients with severe asthma in Australia: current challenges with the existing models of care. Intern Med J . 2018;48(12):1536–1541. doi:10.1111/imj.14103
14. Carr TF, Bleecker E. Asthma heterogeneity and severity. World Allergy Organ J . 2016;9(1):41. doi:10.1186/s40413-016-0118-z
15. Papaioannou AI, Kostikas K, Zervas E, et al. Control of asthma in real life: still a valuable goal? Eur Respir Rev . 2015;24(136):361. doi:10.1183/16000617.00002215
16. Gibson P, McDonald VM. Management of severe asthma: targeting the airways, comorbidities and risk factors. Intern Med J . 2017;47(6):623–631. doi:10.1111/imj.13441
17. Tay TR, Lee JW-Y, Hew M. Diagnosis of severe asthma. Med J Aust . 2018;209(2 Suppl):S3–S10.
18. Moore VC. Spirometry: step by step. Breathe . 2012;8(3):232. doi:10.1183/20734735.0021711
19. Ayuk AC, Uwaezuoke SN, Ndukwu CI, et al. Spirometry in asthma care: a review of the trends and challenges in pediatric practice. Clin Med Insights Pediatr . 2017;11:1179556517720675. doi:10.1177/1179556517720675
20. Brannan JD, Lougheed MD. Airway hyperresponsiveness in asthma: mechanisms, clinical significance, and treatment. Front Physiol . 2012;3:460. doi:10.3389/fphys.2012.00460
21. Sanguinetti CM. When to perform a bronchial challenge with mannitol? Multidiscip Respir Med . 2011;6(2):76–78. doi:10.1186/2049-6958-6-2-76
22. Taylor DR, Pijnenburg MW, Smith AD, De Jongste JC. Exhaled nitric oxide measurements: clinical application and interpretation. Thorax . 2006;61(9):817–827. doi:10.1136/thx.2005.056093
23. Pijnenburg MW. The role of FeNO in predicting asthma. Front Pediatr . 2019;7:41. doi:10.3389/fped.2019.00041
24. Ruppel GL. What is the clinical value of lung volumes? Respir Care . 2012;57(1):26–38. doi:10.4187/respcare.01374
25. Ritz T, Dahme B, Dubois AB, et al. Guidelines for mechanical lung function measurements in psychophysiology. Psychophysiology . 2002;39(5):546–567.
26. Graham BL, Brusasco V, Burgos F, et al. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J . 2017;49(1):1600016. doi:10.1183/13993003.00016-2016
27. Bailey KL. The importance of the assessment of pulmonary function in COPD. Med Clin North Am . 2012;96(4):745–752. doi:10.1016/j.mcna.2012.04.011
28. McDonald VM, Fingleton J, Agusti A. et al. Treatable traits: a new paradigm for 21st century management of chronic airway diseases: treatable traits down under international workshop report. Eur Respir J . 2019;1802058. doi:10.1183/13993003.02058-2018
29. Fricker M, Heaney LG, Upham JW. Can biomarkers help us hit targets in difficult-to-treat asthma? Respirology . 2017;22(3):430–442. doi:10.1111/resp.13014
30. Centre of Excellence in Severe Asthma. The severe asthma toolkit. Available from: https://toolkit.severeasthma.org.au/ . Accessed July 15 , 2019 .
31. McDonald VM, Vertigan AE, Gibson PG. How to set up a severe asthma service. Respirology . 2011;16(6):900–911. doi:10.1111/j.1440-1843.2011.02012.x
32. Chung LP, Johnson P, Summers Q. Models of care for severe asthma: the role of primary care. Med J Aust . 2018;209(2 Suppl):S34–S40.
33. McDonald VM, Yorke J. Adherence in severe asthma: time to get it right. Eur Respir J . 2017;50:6. doi:10.1183/13993003.00711-2017
34. Chuenjit W, Engchuan V, Yuenyongviwat A, Sangsupawanich P. Achieving good adherence to inhaled corticosteroids after weighing canisters of asthmatic children. F1000Res . 2017;6:266. doi:10.12688/f1000research.10710.1
35. McNicholl DM, Stevenson M, McGarvey LP, Heaney LG. The utility of fractional exhaled nitric oxide suppression in the identification of nonadherence in difficult asthma. Am J Respir Crit Care Med . 2012;186(11):1102–1108. doi:10.1164/rccm.201204-0587OC
36. Lindsay JT, Heaney LG. Nonadherence in difficult asthma - facts, myths, and a time to act. Patient Prefer Adherence . 2013;7:329–336. doi:10.2147/PPA.S38208
37. Taylor TE, Zigel Y, Egan C, et al. Objective assessment of patient inhaler user technique using an audio-based classification approach. Sci Rep . 2018;8(1):2164. doi:10.1038/s41598-018-20523-w
38. Lavorini F, Fontana GA, Usmani OS. New inhaler devices-the good, the bad and the ugly. Respiration . 2014;88(1):3–15. doi:10.1159/000363390
39. Faruqi S, Thompson J, Robinson T, et al. Fractional exhaled nitric oxide (FeNO) suppression with directly observed inhaled corticosteroid therapy: does it make a difference to patient outcomes? Eur Respir J . 2018;52(suppl62):PA4453. doi:10.1183/13993003.01675-2018
40. Gamble J, Stevenson M, McClean E, Heaney LG. The prevalence of nonadherence in difficult asthma. Am J Respir Crit Care Med . 2009;180(9):817–822. doi:10.1164/rccm.200902-0166OC
41. Murphy AC, Proeschal A, Brightling CE, et al. The relationship between clinical outcomes and medication adherence in difficult-to-control asthma. Thorax . 2012;67(8):751–753. doi:10.1136/thoraxjnl-2011-201096
42. Gibson PG, McDonald VM, Marks GB. Asthma in older adults. Lancet . 2010;376(9743):803–813. doi:10.1016/S0140-6736(10)61087-2
43. Clark VL, Gibson PG, Genn G, et al. Multidimensional assessment of severe asthma: a systematic review and meta-analysis. Respirology . 2017;22(7):1262–1275. doi:10.1111/resp.13134
44. Gibson P, McDonald V. Phenotyping asthma and COPD. BRN Rev . 2016;2:239–252.
45. McDonald V, Clark V, Wark P, Baines K, Gibson P. Multidimensional assessment and targeted therapy of severe asthma: a randomised controlled trial (RCT). Eur Respir J . 2017;50(suppl 61):OA1482. doi:10.1183/13993003.00711-2017
46. Hudon C, Chouinard M-C, Lambert M, Dufour I, Krieg C. Effectiveness of case management interventions for frequent users of healthcare services: a scoping review. BMJ Open . 2016;6(9):e012353. doi:10.1136/bmjopen-2016-012353
47. McDonald VM, Higgins I, Wood LG, Gibson PG. Multidimensional assessment and tailored interventions for COPD: respiratory utopia or common sense? Thorax . 2013;68(7):691–694. doi:10.1136/thoraxjnl-2012-202646
48. Orozco-Beltrán D, Carratalá-Munuera C, Arriero JM, et al. Management and referral of patients with severe and poorly controlled asthma in primary care. Fam Pract . 2016;33(6):678–683. doi:10.1093/fampra/cmw081
49. Braido F, Baiardini I, Stagi E, et al. Unsatisfactory asthma control: astonishing evidence from general practitioners and respiratory medicine specialists. J Investig Allergol Clin Immunol . 2010;20(1):9–12.
50. Cousins JL, Wark PA, McDonald VM. Acute oxygen therapy: a review of prescribing and delivery practices. Int J Chron Obstruct Pulmon Dis . 2016;11:1067–1075. doi:10.2147/COPD.S103607
51. Morrow S, Daines L, Wiener-Ogilvie S, et al. Exploring the perspectives of clinical professionals and support staff on implementing supported self-management for asthma in UK general practice: an IMP(2)ART qualitative study. NPJ Prim Care Respir Med . 2017;27(1):45. doi:10.1038/s41533-017-0041-y
52. Price D, Bjermer L, Bergin DA, Martinez R. Asthma referrals: a key component of asthma management that needs to be addressed. J Asthma Allergy . 2017;10:209–223. doi:10.2147/JAA.S134300
53. Baiardini I, Braido F, Bonini M, Compalati E, Canonica GW. Why do doctors and patients not follow guidelines? Curr Opin Allergy Clin Immunol . 2009;9(3):228–233. doi:10.1097/ACI.0b013e32832b4651
54. Lugtenberg M, Zegers-van Schaick JM, Westert GP, Burgers JS. Why don’t physicians adhere to guideline recommendations in practice? An analysis of barriers among Dutch general practitioners. Implement Sci . 2009;4:54. doi:10.1186/1748-5908-4-54
55. Lenney W, Bush A, Fitzgerald DA, et al. Improving the global diagnosis and management of asthma in children. Thorax . 2018;73(7):662. doi:10.1136/thoraxjnl-2018-211626
56. Moffat M, Cleland J, van der Molen T, Price D. Poor communication may impair optimal asthma care: a qualitative study. Fam Pract . 2007;24(1):65–70. doi:10.1093/fampra/cml062
57. Dombkowski KJ, Hassan F, Wasilevich EA, Clark SJ. Spirometry use among pediatric primary care physicians. Pediatrics . 2010;126(4):682–687. doi:10.1542/peds.2010-0362
58. Mazrou SHA. Expected benefits of clinical practice guidelines: factors affecting their adherence and methods of implementation and dissemination. JHS . 2013;1(3):141.
59. McDonald VM, Gibson PG. The severe asthma toolkit: a new online resource for clinicians. Respir Med Today . 2018;3(1):26–27.
60. McDonald V, Kennington E, Hyland M. Understanding the experience of people living with severe asthma. In: Chung KF, Israel E, Gibson P, editors. Severe Asthma (ERS Monograph) . Sheffield: European Respiratory Society; 2019:16–29.
61. Aaron SD, Boulet LP, Reddel HK, Gershon AS. Underdiagnosis and overdiagnosis of asthma. Am J Respir Crit Care Med . 2018;198(8):1012–1020. doi:10.1164/rccm.201804-0682CI
62. Menzies-Gow A, Canonica GW, Winders TA, et al. A charter to improve patient care in severe asthma. Adv Ther . 2018;35(10):1485–1496. doi:10.1007/s12325-018-0777-y
63. Ryan D, Murphy A, Stallberg B, Baxter N, Heaney LG. ‘SIMPLES’: a structured primary care approach to adults with difficult asthma. Prim Care Respir J . 2013;22(3):365–373. doi:10.4104/pcrj.2013.00075
64. Laforest L, Van Ganse E, Devouassoux G, et al. Management of asthma in patients supervised by primary care physicians or by specialists. Eur Respir J . 2006;27(1):42–50. doi:10.1183/09031936.06.00035805
65. Dennis SM, Zwar NA, Marks GB. Diagnosing asthma in adults in primary care: a qualitative study of Australian GPs’ experiences. Prim Care Respir J . 2010;19(1):52–56. doi:10.4104/pcrj.2009.00046
66. Young HN, Len-Rios ME, Brown R, Moreno MM, Cox E. How does patient-provider communication influence adherence to asthma medications? Patient Educ Couns . 2017;100(4):696–702. doi:10.1016/j.pec.2016.11.022
67. Crespo-Lessmann A, Plaza V, González-Barcala F-J, Fernández-Sánchez T, Sastre J. Concordance of opinions between patients and physicians and their relationship with symptomatic control and future risk in patients with moderate–severe asthma. BMJ Open Respir Res . 2017;4(1):e000189. doi:10.1136/bmjresp-2017-000189
68. Eassey D, Reddel HK, Foster JM, et al. “…I've said I wish I was dead, you'd be better off without me”: A systematic review of people's experiences of living with severe asthma. J Asthma . 2019;56(3):311-322.
69. Moffat M, Cleland J, van der Molen T, Price D. Sub-optimal patient and physician communication in primary care consultations: its relation to severe and difficult asthma. Prim Care Respir J . 2006;15(3):159–165. doi:10.1016/j.pcrj.2006.02.006
70. Taylor DR, Bateman ED, Boulet LP, et al. A new perspective on concepts of asthma severity and control. Eur Respir J . 2008;32(3):545–554. doi:10.1183/09031936.00155307
71. Bidad N, Barnes N, Griffiths C, Horne R. Understanding patients’ perceptions of asthma control: a qualitative study. Eur Respir J . 2018;51(6):1701346. doi:10.1183/13993003.01346-2017
72. Lingner H, Burger B, Kardos P, et al. What patients really think about asthma guidelines: barriers to guideline implementation from the patients’ perspective. BMC Pulm Med . 2017;17(1):13. doi:10.1186/s12890-016-0346-6
73. Fitzpatrick AM. Biomarkers of asthma and allergic airway diseases. Ann Allergy Asthma Immunol . 2015;115(5):335–340. doi:10.1016/j.anai.2015.09.003
74. Ward PR, Rokkas P, Cenko C, et al. ‘Waiting for’ and ‘waiting in’ public and private hospitals: a qualitative study of patient trust in South Australia. BMC Health Serv Res . 2017;17(1):333. doi:10.1186/s12913-017-2281-5
75. Normansell R, Welsh E. “Asthma can take over your life but having the right support makes that easier to deal with.” Informing research priorities by exploring the barriers and facilitators to asthma control: a qualitative analysis of survey data. Asthma Res Pract . 2015;1(1):11. doi:10.1186/s40733-015-0011-5
76. Fielden JM, Cumming JM, Horne JG, et al. Waiting for hip arthroplasty: economic costs and health outcomes. J Arthroplasty . 2005;20(8):990–997. doi:10.1016/j.arth.2004.12.060
77. Eguiluz-Gracia I, Tay TR, Hew M, et al. Recent developments and highlights in biomarkers in allergic diseases and asthma. Allergy . 2018;73(12):2290–2305. doi:10.1111/all.13628
78. Berry M, Morgan A, Shaw DE, et al. Pathological features and inhaled corticosteroid response of eosinophilic and non-eosinophilic asthma. Thorax . 2007;62(12):1043–1049. doi:10.1136/thx.2006.073429
79. Green RH, Brightling CE, McKenna S, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet . 2002;360(9347):1715–1721. doi:10.1016/S0140-6736(02)11679-5
80. Haldar P, Brightling CE, Hargadon B, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med . 2009;360(10):973–984. doi:10.1056/NEJMoa0808991
81. Pavlidis S, Takahashi K, Ng Kee Kwong F, et al. “T2-high” in severe asthma related to blood eosinophil, exhaled nitric oxide and serum periostin. Eur Respir J . 2019;53:1. doi:10.1183/13993003.01184-2018
82. Zhang XY, Simpson JL, Powell H, et al. Full blood count parameters for the detection of asthma inflammatory phenotypes. Clin Exp Allergy . 2014;44(9):1137–1145. doi:10.1111/cea.12345
83. Smith AD, Cowan JO, Brassett KP, Herbison GP, Taylor DR. Use of exhaled nitric oxide measurements to guide treatment in chronic asthma. N Engl J Med . 2005;352(21):2163–2173. doi:10.1056/NEJMoa043596
84. Schleich FN, Seidel L, Sele J, et al. Exhaled nitric oxide thresholds associated with a sputum eosinophil count ≥3% in a cohort of unselected patients with asthma. Thorax . 2010;65(12):1039–1044. doi:10.1136/thx.2009.124925
85. Jia G, Erickson RW, Choy DF, et al. Periostin is a systemic biomarker of eosinophilic airway inflammation in asthmatic patients. J Allergy Clin Immunol . 2012;130(3):647-654.e10.
86. Simpson JL, Yang IA, Upham JW, et al. Periostin levels and eosinophilic inflammation in poorly-controlled asthma. BMC Pulm Med . 2016;16(1):67. doi:10.1186/s12890-016-0276-3
87. Wagener AH, de Nijs SB, Lutter R, et al. External validation of blood eosinophils, FENO and serum periostin as surrogates for sputum eosinophils in asthma. Thorax . 2015;70(2):115–120. doi:10.1136/thoraxjnl-2014-205634
88. Medrek SK, Parulekar AD, Hanania NA. Predictive biomarkers for asthma therapy. Curr Allergy Asthma Rep . 2017;17(10):69. doi:10.1007/s11882-017-0739-5
89. Gibson PG. Variability of blood eosinophils as a biomarker in asthma and COPD. Respirology . 2018;23(1):12–13. doi:10.1111/resp.13200
90. Schleich FN, Manise M, Sele J, et al. Distribution of sputum cellular phenotype in a large asthma cohort: predicting factors for eosinophilic vs neutrophilic inflammation. BMC Pulm Med . 2013;13:11. doi:10.1186/1471-2466-13-11
91. Hastie AT, Moore WC, Li H, et al. Biomarker surrogates do not accurately predict sputum eosinophil and neutrophil percentages in asthmatic subjects. J Allergy Clin Immunol . 2013;132(1):72–80. doi:10.1016/j.jaci.2013.03.044
92. Gibson PG. Inflammatory phenotypes in adult asthma: clinical applications. Clin Respir J . 2009;3(4):198–206. doi:10.1111/j.1752-699X.2009.00162.x
93. Wadsworth S, Sin D, Dorscheid D. Clinical update on the use of biomarkers of airway inflammation in the management of asthma. J Asthma Allergy . 2011;4:77–86. doi:10.2147/JAA.S15081
94. Korevaar DA, Westerhof GA, Wang J, et al. Diagnostic accuracy of minimally invasive markers for detection of airway eosinophilia in asthma: a systematic review and meta-analysis. Lancet Respir Med . 2015;3(4):290–300. doi:10.1016/S2213-2600(15)00050-8
95. Trevor JL, Chipps BE. Severe asthma in primary care: identification and management. Am J Med . 2018;131(5):484–491. doi:10.1016/j.amjmed.2017.12.034
96. Mcdonald VM, Maltby S, Clark VL, et al. Development of the Severe Asthma Toolkit: A Clinical Website Resource for the Management of Severe Treatment-refractory Asthma. Respirology . 2018;23(S2):28-28.
97. Alexandrine JL, Sandra P, Roland G, et al. Facilitators and solutions for practicing optimal guided asthma self-management: the physician perspective. Can Respir J . 2013;20(4):285. doi:10.1155/2013/562104
98. Cabana MD, Slish KK, Evans D, et al. Impact of physician asthma care education on patient outcomes. Pediatrics . 2006;117(6):2149–2157. doi:10.1542/peds.2005-1055
99. Clark NM, Cabana MD, Nan B, et al. The clinician-patient partnership paradigm: outcomes associated with physician communication behavior. Clin Pediatr (Phila) . 2008;47(1):49–57. doi:10.1177/0009922807305650
100. Wolf A, Moore L, Lydahl D, et al. The realities of partnership in person-centred care: a qualitative interview study with patients and professionals. BMJ Open . 2017;7(7):e016491. doi:10.1136/bmjopen-2017-016491
101. Apter AJ, Morales KH, Han X, et al. A patient advocate to facilitate access and improve communication, care, and outcomes in adults with moderate or severe asthma: rationale, design, and methods of a randomized controlled trial. Contemp Clin Trials . 2017;56:34–45. doi:10.1016/j.cct.2017.03.004
102. Kane B, Cramb S, Hudson V, et al. Specialised commissioning for severe asthma: oxymoron or opportunity? Thorax . 2016;71(2):196–198. doi:10.1136/thoraxjnl-2015-207380
103. Loscalzo J, Kohane I, Barabasi AL. Human disease classification in the postgenomic era: a complex systems approach to human pathobiology. Mol Syst Biol . 2007;3:124. doi:10.1038/msb4100163
104. Ritchie MD, de Andrade M, Kuivaniemi H. The foundation of precision medicine: integration of electronic health records with genomics through basic, clinical, and translational research. Front Genet . 2015;6:104. doi:10.3389/fgene.2015.00104
105. Verrills NM, Irwin JA, He XY, et al. Identification of novel diagnostic biomarkers for asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med . 2011;183(12):1633–1643. doi:10.1164/rccm.201010-1623OC
106. Baines KJ, Simpson JL, Wood LG, et al. Sputum gene expression signature of 6 biomarkers discriminates asthma inflammatory phenotypes. J Allergy Clin Immunol . 2014;133(4):997–1007. doi:10.1016/j.jaci.2013.12.1091
107. Kim S, Oesterreich S, Kim S, Park Y, Tseng GC. Integrative clustering of multi-level omics data for disease subtype discovery using sequential double regularization. Biostatistics . 2017;18(1):165–179. doi:10.1093/biostatistics/kxw039
108. Dallinga JW, Robroeks CM, van Berkel JJ, et al. Volatile organic compounds in exhaled breath as a diagnostic tool for asthma in children. Clin Exp Allergy . 2010;40(1):68–76. doi:10.1111/j.1365-2222.2009.03343.x
109. Thwaites RS, Jarvis HC, Singh N, et al. Absorption of nasal and bronchial fluids: precision sampling of the human respiratory mucosa and laboratory processing of samples. J Vis Exp . 2018(131):e56413.
110. Melo JT Jr. , Tunstall T, Pizzichini MMM, et al. IL-5 levels in nasosorption and sputosorption correlate with sputum eosinophilia in allergic asthma. Am J Respir Crit Care Med . 2019;199(2):240–243. doi:10.1164/rccm.201807-1279LE
111. Restifo LL, Phelan GR. The cultural divide: exploring communication barriers between scientists and clinicians. Dis Model Mech . 2011;4(4):423–426. doi:10.1242/dmm.008177
112. St John A. The evidence to support point-of-care testing. Clin Biochem Rev . 2010;31(3):111–119.
113. Ferguson BS, Hoggarth DA, Maliniak D, et al. Real-time, aptamer-based tracking of circulating therapeutic agents in living animals. Sci Transl Med . 2013;5(213):213ra165–213ra165. doi:10.1126/scitranslmed.3007095

Contact Us • Privacy Policy • Associations & Partners • Testimonials • Terms & Conditions • Recommend this site • Cookies • Top
Contact Us • Privacy Policy
- The exponential growth of solar power will change the world
An energy-rich future is within reach

Your browser does not support the <audio> element.
I t is 70 years since AT&T ’s Bell Labs unveiled a new technology for turning sunlight into power. The phone company hoped it could replace the batteries that run equipment in out-of-the-way places. It also realised that powering devices with light alone showed how science could make the future seem wonderful; hence a press event at which sunshine kept a toy Ferris wheel spinning round and round.
Today solar power is long past the toy phase. Panels now occupy an area around half that of Wales, and this year they will provide the world with about 6% of its electricity—which is almost three times as much electrical energy as America consumed back in 1954. Yet this historic growth is only the second-most-remarkable thing about the rise of solar power. The most remarkable is that it is nowhere near over.
To call solar power’s rise exponential is not hyperbole, but a statement of fact. Installed solar capacity doubles roughly every three years, and so grows ten-fold each decade. Such sustained growth is seldom seen in anything that matters. That makes it hard for people to get their heads round what is going on. When it was a tenth of its current size ten years ago, solar power was still seen as marginal even by experts who knew how fast it had grown. The next ten-fold increase will be equivalent to multiplying the world’s entire fleet of nuclear reactors by eight in less than the time it typically takes to build just a single one of them.
Solar cells will in all likelihood be the single biggest source of electrical power on the planet by the mid 2030s. By the 2040s they may be the largest source not just of electricity but of all energy. On current trends, the all-in cost of the electricity they produce promises to be less than half as expensive as the cheapest available today. This will not stop climate change, but could slow it a lot faster. Much of the world—including Africa , where 600m people still cannot light their homes—will begin to feel energy-rich. That feeling will be a new and transformational one for humankind.
To grasp that this is not some environmentalist fever dream, consider solar economics. As the cumulative production of a manufactured good increases, costs go down. As costs go down, demand goes up. As demand goes up, production increases—and costs go down further. This cannot go on for ever; production, demand or both always become constrained. In earlier energy transitions—from wood to coal, coal to oil or oil to gas—the efficiency of extraction grew, but it was eventually offset by the cost of finding ever more fuel.
As our essay this week explains, solar power faces no such constraint. The resources needed to produce solar cells and plant them on solar farms are silicon-rich sand, sunny places and human ingenuity, all three of which are abundant. Making cells also takes energy, but solar power is fast making that abundant, too. As for demand, it is both huge and elastic—if you make electricity cheaper, people will find uses for it. The result is that, in contrast to earlier energy sources, solar power has routinely become cheaper and will continue to do so.
Other constraints do exist. Given people’s proclivity for living outside daylight hours, solar power needs to be complemented with storage and supplemented by other technologies. Heavy industry and aviation and freight have been hard to electrify. Fortunately, these problems may be solved as batteries and fuels created by electrolysis gradually become cheaper.
Another worry is that the vast majority of the world’s solar panels, and almost all the purified silicon from which they are made, come from China. Its solar industry is highly competitive, heavily subsidised and is outstripping current demand—quite an achievement given all the solar capacity China is installing within its own borders. This means that Chinese capacity is big enough to keep the expansion going for years to come, even if some of the companies involved go to the wall and some investment dries up.
In the long run, a world in which more energy is generated without the oil and gas that come from unstable or unfriendly parts of the world will be more dependable. Still, although the Chinese Communist Party cannot rig the price of sunlight as OPEC tries to rig that of oil, the fact that a vital industry resides in a single hostile country is worrying.
It is a concern that America feels keenly, which is why it has put tariffs on Chinese solar equipment. However, because almost all the demand for solar panels still lies in the future, the rest of the world will have plenty of scope to get into the market. America’s adoption of solar energy could be frustrated by a pro-fossil-fuel Trump presidency, but only temporarily and painfully. It could equally be enhanced if America released pent up demand, by making it easier to install panels on homes and to join the grid—the country has a terawatt of new solar capacity waiting to be connected. Carbon prices would help, just as they did in the switch from coal to gas in the European Union.
The aim should be for the virtuous circle of solar-power production to turn as fast as possible. That is because it offers the prize of cheaper energy. The benefits start with a boost to productivity. Anything that people use energy for today will cost less—and that includes pretty much everything. Then come the things cheap energy will make possible. People who could never afford to will start lighting their houses or driving a car. Cheap energy can purify water, and even desalinate it. It can drive the hungry machinery of artificial intelligence. It can make billions of homes and offices more bearable in summers that will, for decades to come, be getting hotter.
But it is the things that nobody has yet thought of that will be most consequential. In its radical abundance, cheaper energy will free the imagination, setting tiny Ferris wheels of the mind spinning with excitement and new possibilities.
This week marks the summer solstice in the northern hemisphere. The Sun rising to its highest point in the sky will in decades to come shine down on a world where nobody need go without the blessings of electricity and where the access to energy invigorates all those it touches. ■
For subscribers only: to see how we design each week’s cover, sign up to our weekly Cover Story newsletter .
This article appeared in the Leaders section of the print edition under the headline “The solar age”
Leaders June 22nd 2024
Ai will transform the character of warfare, emmanuel macron’s project of reform is at risk, how to tax billionaires—and how not to, javier milei’s next move could make his presidency—or break it, india should liberate its cities and create more states.

From the June 22nd 2024 edition
Discover stories from this section and more in the list of contents
More from Leaders

Nigel Farage’s claim that NATO provoked Russia is naive and dangerous
It is also a wilful misreading of history

Technology will make war faster and more opaque. It could also prove destabilising

A snap election in France reveals the flimsiness of his legacy
It doesn’t need more government. It needs more governments
Radical experiments with the currency could spell disaster
Closing loopholes would be a better bet than a levy on unrealised capital gains

COMMENTS
In fact, a 2016 meta-analysis of that research in the European Respiratory Journal 's Open Research imprint finds that 12 weeks of prolonged exposure to altitudes 1,500 meters or more above sea ...
Dawn Newton, a writer in East Lansing, Michigan, was diagnosed with stage IV lung cancer in November 2012 and has lived with asthma all her life. Her memoir, Winded: A Memoir in Four Stages, will be published in October by Apprentice House Press at Loyola University Maryland. Her blog is at www.dawnmarienewton.com.
Asthma treatment is based on a stepwise approach. The management of the patient is control-based; that is, it involves an iterative cycle of assessment (e.g. symptoms, risk factors, etc.), adjustment of treatment (i.e. pharmacological, non-pharmacological and treatment of modifiable risk factors) and review of the response (e.g. symptoms, side ...
Introduction. Asthma is a significant public health threat, affecting more than 300 million individuals globally. 1 Asthma is classified as a non-communicable disease and leads to reduced quality of life, 2 poor physical functioning 3 and reduced emotional well-being. 4 The impact of this disease can be widespread and extends beyond the person living with the disease, affecting the lives of ...
To facilitate access to healthcare and therefore self-management, patient advocates can help patients overcome access issues and asthma nurses can provide information about asthma management, particularly when GP appointments are not possible. Finally, professional issues were reported in 7 (13%) of the papers. Only barriers were raised in this ...
Follow this three-step approach to keep asthma symptoms under control and prevent asthma attacks. The goals of asthma treatment are to limit symptoms, prevent asthma attacks and avoid side effects of asthma medicines. The following three steps can help you take control of your asthma treatment. 1. Follow your asthma action plan.
Regular exercise can strengthen your heart and lungs, which helps relieve asthma symptoms. If you exercise in cold temperatures, wear a face mask to warm the air you breathe. Maintain a healthy weight. Being overweight can worsen asthma symptoms, and it puts you at higher risk of other health problems.
Asthma and physical activity: Overcoming barriers to exercise. Asthma and mental health: Nurturing emotional well-being. ... These 110 asthma essay topic ideas and examples cover a wide range of aspects related to asthma, providing you with ample options to choose from. Remember to tailor your essay to your audience, whether it is a scientific ...
Asthma, a chronic inflammatory airway disease, is one of the most common long-term conditions worldwide and can affect people of all ages. The Global Burden of Disease study estimated that 262 million people were living with asthma in 2019. Asthma accounts for about half a million deaths per year and is a major global economic burden in terms of both direct and indirect costs.1,2
This study will describe asthma as a chronic condition, including its symptoms and signs, incidences, surveillance, reporting, epidemiological analysis, screening, prevention, and prevalence by state and national statistics. Get a custom Essay on Asthma: Epidemiological Analysis and Care Plan. 809 writers online.
A Comprehensive Exploration of Asthma. Asthma is a chronic lung disease marked by chest tightness, wheezing, breathlessness, and coughing (Dodge & Burrows, 2018). In the United States alone, there are 19 million adults and 6.2 million children living with asthma (Centers for Disease Control and Prevention, 2018).
About Overcoming Asthma. This unique book from doctor and international best-selling author Sarah Brewer provides a highly authoritative yet easy-to-follow program of complementary medicine and self-care treatments, specially designed to support the conventional treatment for asthma.
Introduction. Asthma is a significant public health threat, affecting more than 300 million individuals globally. Citation 1 Asthma is classified as a non-communicable disease and leads to reduced quality of life, Citation 2 poor physical functioning Citation 3 and reduced emotional well-being. Citation 4 The impact of this disease can be widespread and extends beyond the person living with ...
Inflammation's Role in Asthma Development. This work is written in order to study the role of inflammation plays in the development of asthma on the basis of research papers. The Use of Tezspire: The Management of Asthma. The brochure describes the use of Tezspire, which is a drug used for the management of asthma.
Healthcare providers that adhere to asthma guidelines-based care can help their patients better manage their asthma. However, the American Lung Association's Asthma Guidelines-Based Care Coverage Project found many barriers in state Medicaid programs in all 50 states, D.C. and Puerto Rico in 2018-2019. Barriers are associated with reduced
It will also cover the client education needed to provide for those with asthma, asthma's risk factors and its prognosis. According to the National Asthma Council of Australia or NACA (2006) more than 2.2 million Australians are suffering from asthma. This essay will therefore also describe how asthma impacts on its victims and their life style.
Introduction. Asthma is a common chronic condition that is estimated to affect 339 million people worldwide 1,2.Despite major advances in asthma treatment and the availability of both global 2 and national guidance, asthma continues to cause a substantial burden in terms of both direct and indirect costs 1.In 2016, estimated worldwide asthma deaths were 420,000 1 and although there have been ...
papers have been selected from major international biomedical journals reporting on clinical and epidemiological studies of asthma, each of which explores one or a few possible causes of the disorder in everyday life. A different paper is assigned to each student or group of students. Background material on asthma and alternative research
asthma diagnosis. The following sections provide an overview o. t. e discussions.1. Development of a low-cost, accurate diagnostic test that improves diagnosis of asth. a in primary careThe challenge here is to try to improve the accuracy and ease of use of existing tests and bring the costs down to enable wi. es.
#### What you need to know The management of adults with asthma that remains uncontrolled despite treatment with high dose therapies poses a challenge to clinicians and patients. National and international guidelines recommend intensification of treatment that typically involves the use of oral corticosteroids.12 The risks associated with long term systemic corticosteroid treatment are well ...
Inadequate patient adherence to prescribed treatment regimens is a major cause of poor clinical outcomes in the treatment of asthma. Among children with asthma, adherence rates are often below 50%. Multiple treatment-, clinician-, and patient-related barriers prevent the achievement of satisfactory levels of adherence. Treatment-related barriers include prolonged and complex regimens, adverse ...
View english essay.docx from EDUC 1300 at Houston Community College. Bangura 1 Dianna Bangura Professor Hasell English 1301 September 10, 2022 Personal Literacy Narrative In life people will always. ... Asthma has had a large impact on my life since I was a small child.
Last week, in American Alliance for Equal Rights v.Fearless Fund Management, a divided panel of the U.S. Court of Appeals for the 11 th Circuit became the first federal court of appeals to place ...
Introduction. Asthma is a significant public health threat, affecting more than 300 million individuals globally. 1 Asthma is classified as a non-communicable disease and leads to reduced quality of life, 2 poor physical functioning 3 and reduced emotional well-being. 4 The impact of this disease can be widespread and extends beyond the person living with the disease, affecting the lives of ...
As our essay this week explains, solar power faces no such constraint. The resources needed to produce solar cells and plant them on solar farms are silicon-rich sand, sunny places and human ...