- Search Menu
- Volume 2024, Issue 3, March 2024 (In Progress)
- Volume 2024, Issue 2, February 2024
- Case of the Year
- MSF Case Reports
- Audiovestibular medicine
- Cardiology and cardiovascular systems
- Critical care medicine
- Dermatology
- Emergency medicine
- Endocrinology and metabolism
- Gastroenterology and hepatology
- Geriatrics and gerontology
- Haematology
- Infectious diseases and tropical medicine
- Medical ophthalmology
- Medical disorders in pregnancy
- Paediatrics
- Palliative medicine
- Pharmacology and pharmacy
- Radiology, nuclear medicine, and medical imaging
- Respiratory disorders
- Rheumatology
- Sexual and reproductive health
- Sports medicine
- Substance abuse
- Author Guidelines
- Submission Site
- Open Access
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Answer to part 1, answer to part 2, answer to part 3, answer to part 4, answer to part 5.
- < Previous
Educational Case: A 57-year-old man with chest pain
Contributed equally.
- Article contents
- Figures & tables
- Supplementary Data
Nikhil Aggarwal, Subothini Selvendran, Vassilios Vassiliou, Educational Case: A 57-year-old man with chest pain, Oxford Medical Case Reports , Volume 2016, Issue 4, April 2016, Pages 62–65, https://doi.org/10.1093/omcr/omw008
- Permissions Icon Permissions
This is an educational case report including multiple choice questions and their answers. For the best educational experience we recommend the interactive web version of the exercise which is available via the following link: http://www.oxfordjournals.org/our_journals/omcr/ec01p1.html
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by paramedics in the community. He smoked 20 cigarettes daily (38 pack years) but was not aware of any other cardiovascular risk factors. On examination he appeared comfortable and was able to complete sentences fully. There were no heart murmurs present on cardiac auscultation. Blood pressure was 180/105 mmHg, heart rate was 83 bpm and regular, oxygen saturation was 97%.
What is the most likely diagnosis?
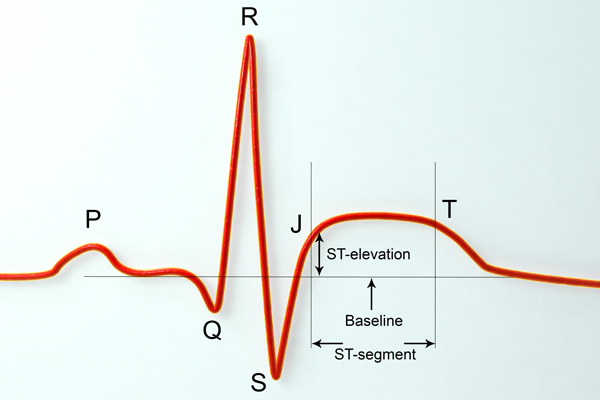
An ECG was requested and is shown in figure 1.
How would you manage the patient? (The patient has already received 300 mg aspirin).
30 minutes later the patient's chest pain returned with greater intensity whilst waiting in the emergency department. Now, he described the pain as though “an elephant is sitting on his chest”. The nurse has already done an ECG by the time you were called to see him. This is shown in figure 2.

ECG on admission.

ECG 30 minutes after admission.
What would be the optimal management for this patient?
He was taken to the catheterization lab where the left anterior descending coronary artery (LAD) was shown to be completely occluded. Following successful percutaneous intervention and one drug eluding stent implantation in the LAD normal flow is restored (Thrombosis in myocardial infarction, TIMI = 3). 72 hours later, he is ready to be discharged home. The patient is keen to return to work and asks when he could do so.
When would you advise him that he could return to work?
One week later, he receives a letter informing him that he is required to attend cardiac rehabilitation. The patient is confused as to what cardiac rehabilitation entails, although he does remember a nurse discussing this with him briefly before he was discharged. He phones the hospital in order to get some more information.
Which of the following can be addressed during cardiac rehabilitation?
A - Acute coronary syndrome
Although the presentation could be attributable to any of the above differential diagnoses, the most likely etiology given the clinical picture and risk factors is one of cardiac ischemia. Risk factors include gender, smoking status and age making the diagnosis of acute coronary syndrome the most likely one. The broad differential diagnosis in patients presenting with chest pain has been discussed extensively in the medical literature. An old but relevant review can be found freely available 1 as well as more recent reviews. 2 , 3
C - Atorvastatin 80 mg, Clopidogrel 300 mcg, GTN 500 mcg, Ramipril 2.5 mg,
In patients with ACS, medications can be tailored to the individual patient. Some medications have symptomatic benefit but some also have prognostic benefit. Aspirin 4 , Clopidogrel 5 , Atenolol 6 and Atorvastatin 7 have been found to improve prognosis significantly. ACE inhibitors have also been found to improve left ventricular modeling and function after an MI. 8 , 9 Furthermore, GTN 10 and morphine 11 have been found to be of only significant symptomatic benefit.
Oxygen should only to be used when saturations <95% and at the lowest concentration required to keep saturations >95%. 12
There is no evidence that diltiazem, a calcium channel blocker, is of benefit. 13
His ECG in figure 1 does not fulfil ST elevation myocardial infarction (STEMI) criteria and he should therefore be managed as a Non-STEMI. He would benefit prognostically from beta-blockade however his heart rate is only 42 bpm and therefore this is contraindicated. He should receive a loading dose of clopidogrel (300 mg) followed by daily maintenance dose (75 mg). 14 , 15 He might not require GTN if he is pain-free but out of the available answers 3 is the most correct.
D - Proceed to coronary angiography
The ECG shows ST elevation in leads V2-V6 and confirms an anterolateral STEMI, which suggests a completely occluded LAD. This ECG fulfils the criteria to initiate reperfusion therapy which traditionally require one of the three to be present: According to guidance, if the patient can undergo coronary angiography within 120 minutes from the onset of chest pain, then this represents the optimal management. If it is not possible to undergo coronary angiography and potentially percutaneous intervention within 2 hours, then thrombolysis is considered an acceptable alternative. 12 , 16
≥ 1 mm of ST change in at least two contiguous limb leads (II, III, AVF, I, AVL).
≥ 2 mm of ST change in at least two contiguous chest leads (V1-V6).
New left bundle branch block.
GTN and morphine administration can be considered in parallel but they do not have a prognostic benefit.
E - Not before an exercise test
This patient is a lorry driver and therefore has a professional heavy vehicle driving license. The regulation for driving initiation in a lorry driver following a NSTEMI/ STEMI may be different in various countries and therefore the local regulations should be followed.
In the UK, a lorry driver holds a category 2 driving license. He should therefore refrain from driving a lorry for at least 6 weeks and can only return to driving if he completes successfully an exercise evaluation. An exercise evaluation is performed on a bicycle or treadmill. Drivers should be able to complete 3 stages of the standard Bruce protocol 17 or equivalent (e.g. Myocardial perfusion scan) safely, having refrained from taking anti-anginal medication for 48 hours and should remain free from signs of cardiovascular dysfunction during the test, notably: angina pectoris, syncope, hypotension, sustained ventricular tachycardia, and/or electrocardiographic ST segment shift which is considered as being indicative of myocardial ischemia (usually >2 mm horizontal or down-sloping) during exercise or the recovery period. 18
For a standard car driving license (category 1), driving can resume one week after successful intervention providing that no other revascularization is planned within 4 weeks; left ventricular ejection fraction (LVEF) is at least 40% prior to hospital discharge and there is no other disqualifying condition.
Therefore if this patent was in the UK, he could restart driving a normal car one week later assuming an echocardiogram confirmed an EF > 40%. However, he could only continue lorry driving once he has passed the required tests. 18
E - All of the above
Cardiac rehabilitation bridges the gap between hospitals and patients' homes. The cardiac rehabilitation team consists of various healthcare professions and the programme is started during hospital admission or after diagnosis. Its aim is to educate patients about their cardiac condition in order to help them adopt a healthier lifestyle. This includes educating patients' about their diet, exercise, risk factors associated with their condition such as smoking and alcohol intake and finally, about the medication recommended. There is good evidence that adherence to cardiac rehabilitation programmes improves survival and leads to a reduction in future cardiovascular events. 19 , 20
Oille JA . Differential diagnosis of pain in the chest . Can Med Assoc J . 1937 ; 37 (3) : 209 – 216 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC536075/ .
Google Scholar
Lee TH , Goldman L . Evaluation of the patient with acute chest pain . N Engl J Med . 2000 ; 342 (16) : 1187 – 1195 . http://www.nejm.org/doi/full/10.1056/NEJM200004203421607 .
Douglas PS , Ginsburg GS . The evaluation of chest pain in women . N Engl J Med . 1996 ; 334 (20) : 1311 – 1315 . http://www.nejm.org/doi/full/10.1056/NEJM199605163342007 .
Baigent C , Collins R , Appleby P , Parish S , Sleight P , Peto R . ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. the ISIS-2 (second international study of infarct survival) collaborative group . BMJ . 1998 ; 316 (7141) : 1337 – 1343 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC28530/ .
Yusuf S , Zhao F , Mehta S , Chrolavicius S , Tognoni G , Fox K . Clopidogrel in unstable angina to prevent recurrent events trail investigators . effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation . N Engl J Med . 2001 ; 345 (7) : 494 – 502 . http://www.nejm.org/doi/full/10.1056/NEJMoa010746#t=articleTop .
Yusuf S , Peto R , Lewis J , Collins R , Sleight P . Beta blockade during and after myocardial infarction: An overview of the randomized trials . Prog Cardiovasc Dis . 1985 ; 27 (5) : 335 – 371 . http://www.sciencedirect.com/science/article/pii/S0033062085800037 .
Schwartz GG , Olsson AG , Ezekowitz MD et al. . Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: The MIRACL study: A randomized controlled trial . JAMA . 2001 ; 285 (13) : 1711 – 1718 . http://jama.jamanetwork.com/article.aspx?articleid=193709 .
Pfeffer MA , Lamas GA , Vaughan DE , Parisi AF , Braunwald E . Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction . N Engl J Med . 1988 ; 319 (2) : 80 – 86 . http://content.onlinejacc.org/article.aspx?articleid=1118054 .
Sharpe N , Smith H , Murphy J , Hannan S . Treatment of patients with symptomless left ventricular dysfunction after myocardial infarction . The Lancet . 1988 ; 331 (8580) : 255 – 259 . http://www.sciencedirect.com/science/article/pii/S0140673688903479 .
Ferreira JC , Mochly-Rosen D . Nitroglycerin use in myocardial infarction patients . Circ J . 2012 ; 76 (1) : 15 – 21 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527093/ .
Herlitz J , Hjalmarson A , Waagstein F . Treatment of pain in acute myocardial infarction . Br Heart J . 1989 ; 61 (1) : 9 – 13 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1216614/ .
Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, et al . ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation . Eur Heart J . 2012 ; 33 (20) : 2569 – 2619 . http://eurheartj.oxfordjournals.org/content/33/20/2569 .
The effect of diltiazem on mortality and reinfarction after myocardial infarction . the multicenter diltiazem postinfarction trial research group . N Engl J Med . 1988 ; 319 (7) : 385 – 392 . http://www.nejm.org/doi/full/10.1056/NEJM198808183190701 .
Jneid H , Anderson JL , Wright RS et al. . 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non–ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update) A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2012 ; 60 (7) : 645 – 681 . http://circ.ahajournals.org/content/123/18/2022.full .
Hamm CW , Bassand JP , Agewall S et al. . ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the european society of cardiology (ESC) . Eur Heart J . 2011 ; 32 (23) : 2999 – 3054 . http://eurheartj.oxfordjournals.org/content/32/23/2999.long .
O'Gara PT , Kushner FG , Ascheim DD et al. . 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: Executive summary: A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2013 ; 61 (4) : 485 – 510 . http://content.onlinejacc.org/article.aspx?articleid=1486115 .
BRUCE RA , LOVEJOY FW Jr . Normal respiratory and circulatory pathways of adaptation in exercise . J Clin Invest . 1949 ; 28 (6 Pt 2) : 1423 – 1430 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC439698/ .
DVLA . Https://Www.gov.uk/current-medical-guidelines-dvla-guidance-for-professionals-cardiovascular-chapter-appendix .
British Heart Foundation . Http://Www.bhf.org.uk/heart-health/living-with-heart-disease/cardiac-rehabilitation.aspx .
Kwan G , Balady GJ . Cardiac rehabilitation 2012: Advancing the field through emerging science . Circulation . 2012 ; 125 (7) : e369–73. http://circ.ahajournals.org/content/125/7/e369.full .
Author notes
- knowledge acquisition
Email alerts
Citing articles via, affiliations.
- Online ISSN 2053-8855
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Introduction
- Conclusions
- Article Information
The start of the early coronavirus disease 2019 (COVID-19) period (February 23, 2020) and later COVID-19 period (March 29, 2020), as defined by segmented regression analysis, are indicated by vertical lines. Dotted lines indicate the best-fit regression lines for the 3 periods (including the before COVID-19 period). Projected volumes with 95% CIs are displayed in gray. STEMI indicates ST-segment elevation myocardial infarction.
eTable 1. ICD-10 Codes
eTable 2. MS-DRG Codes Used in Treatment Approaches Analysis
eTable 3. Weekly Case Volumes in 2020
eFigure 1. Weekly Volumes by State
eFigure 2. Treatment Approaches
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Gluckman TJ , Wilson MA , Chiu S, et al. Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic. JAMA Cardiol. 2020;5(12):1419–1424. doi:10.1001/jamacardio.2020.3629
Manage citations:
© 2024
- Permissions
Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic
- 1 Center for Cardiovascular Analytics, Research and Data Science (CARDS), Providence Heart Institute, Providence St Joseph Health, Portland, Oregon
- 2 Clinical Analytics, Providence St Joseph Health, Renton, Washington
- 3 Heart and Vascular Institute, Providence Regional Medical Center Everett, Everett, Washington
- 4 Providence Heart Institute, Providence St Peter Hospital, Olympia, Washington
Question How have case rates, treatment approaches, and in-hospital outcomes changed for patients with acute myocardial infarction (AMI) during the coronavirus disease 2019 (COVID-19) pandemic?
Findings In this cross-sectional study of 15 244 hospitalizations involving 14 724 patients with AMI, case rates began to decrease on February 23, 2020, followed by a modest recovery after 5 weeks. Although no statistically significant difference in treatment approaches was found, the risk-adjusted mortality rate among patients with ST-segment elevation myocardial infarction increased substantially.
Meaning The findings of this study show that changes in AMI hospitalizations and in-hospital outcomes occurred during the COVID-19 pandemic periods analyzed; additional research is warranted to explain the higher mortality rate among patients with ST-segment elevation myocardial infarction.
Importance The coronavirus disease 2019 (COVID-19) pandemic has changed health care delivery worldwide. Although decreases in hospitalization for acute myocardial infarction (AMI) have been reported during the pandemic, the implication for in-hospital outcomes is not well understood.
Objective To define changes in AMI case rates, patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes during the pandemic.
Design, Setting, and Participants This cross-sectional study retrospectively analyzed AMI hospitalizations that occurred between December 30, 2018, and May 16, 2020, in 1 of the 49 hospitals in the Providence St Joseph Health system located in 6 states (Alaska, Washington, Montana, Oregon, California, and Texas). The cohort included patients aged 18 years or older who had a principal discharge diagnosis of AMI (ST-segment elevation myocardial infarction [STEMI] or non–ST-segment elevation myocardial infarction [NSTEMI]). Segmented regression analysis was performed to assess changes in weekly case volumes. Cases were grouped into 1 of 3 periods: before COVID-19 (December 30, 2018, to February 22, 2020), early COVID-19 (February 23, 2020, to March 28, 2020), and later COVID-19 (March 29, 2020, to May 16, 2020). In-hospital mortality was risk-adjusted using an observed to expected (O/E) ratio and covariate-adjusted multivariable model.
Exposure Date of hospitalization.
Main Outcomes and Measures The primary outcome was the weekly rate of AMI (STEMI or NSTEMI) hospitalizations. The secondary outcomes were patient characteristics, treatment approaches, and in-hospital outcomes of this patient population.
Results The cohort included 15 244 AMI hospitalizations (of which 4955 were for STEMI [33%] and 10 289 for NSTEMI [67%]) involving 14 724 patients (mean [SD] age of 68 [13] years and 10 019 men [66%]). Beginning February 23, 2020, AMI-associated hospitalizations decreased at a rate of –19.0 (95% CI, –29.0 to –9.0) cases per week for 5 weeks (early COVID-19 period). Thereafter, AMI-associated hospitalizations increased at a rate of +10.5 (95% CI, +4.6 to +16.5) cases per week (later COVID-19 period). No appreciable differences in patient demographics, cardiovascular comorbidities, and treatment approaches were observed across periods. The O/E mortality ratio for AMI increased during the early period (1.27; 95% CI, 1.07-1.48), which was disproportionately associated with patients with STEMI (1.96; 95% CI, 1.22-2.70). Although the O/E mortality ratio for AMI was not statistically different during the later period (1.23; 95% CI, 0.98-1.47), increases in the O/E mortality ratio were noted for patients with STEMI (2.40; 95% CI, 1.65-3.16) and after risk adjustment (odds ratio, 1.52; 95% CI, 1.02-2.26).
Conclusions and Relevance This cross-sectional study found important changes in AMI hospitalization rates and worse outcomes during the early and later COVID-19 periods. Future studies are needed to identify contributors to the increased mortality rate among patients with STEMI.
The coronavirus disease 2019 (COVID-19) pandemic has profoundly changed health care delivery worldwide. Although early attention to COVID-19 was disproportionately focused on efforts to flatten the (pandemic) curve, recent studies have revealed a substantial decrease in hospitalization rates for acute myocardial infarction (AMI). Reports from Austria, 1 Italy, 2 and the US (California) 3 have noted lower admission rates for both ST-segment elevation myocardial infarction (STEMI) and non–ST-segment elevation myocardial infarction (NSTEMI). This decreased hospitalization rate likely reflects multiple factors. Most worrisome among these factors has been the reluctance of patients with AMI to seek medical attention out of fear that they may become infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). 4
We performed a retrospective, cross-sectional study of all AMI hospitalizations in a large multistate health care system. We sought to define changes in AMI case rates, patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes during the pandemic.
This study included patients aged 18 years or older with a principal discharge diagnosis of AMI who were admitted between December 30, 2018, and May 16, 2020, into 1 of 49 hospitals in the Providence St Joseph Health (PSJH) system located in 6 states (Alaska, Washington, Montana, Oregon, California, and Texas). We used International Statistical Classification of Diseases and Related Health Problems, Tenth Revision , codes to define the population (eTable 1 in the Supplement ). Individuals who were admitted as an outpatient were excluded. This study was approved by the PSJH Institutional Review Board, which waived the informed consent requirement because of the retrospective nature of the study.
The primary outcome was the weekly rate of AMI (STEMI or NSTEMI) hospitalizations before and after the pandemic onset. The secondary outcomes were patient characteristics, treatment approaches, and in-hospital outcomes (mortality, length of stay, and discharge disposition) of patients with STEMI or NSTEMI. Treatment approaches were defined by Medicare Severity-Diagnosis Related Groups (MS-DRGs) for percutaneous coronary intervention, coronary artery bypass graft surgery, and medical management of AMI (eTable 2 in the Supplement ).
Weekly volumes of AMI hospitalizations (categorized as STEMI or NSTEMI) are presented in the Figure as line graphs. Segmented regression analysis was used to ascertain volume changes over time. Using 2 identified break points (February 23, 2020 and March 29, 2020), we grouped cases into 1 of 3 periods for analysis: before COVID-19 (December 30, 2018, to February 22, 2020), early COVID-19 (February 23, 2020, to March 28, 2020), and later COVID-19 (March 29, 2020, to May 16, 2020). Segmented regression analysis was also used to identify the slope change in weekly hospitalizations during the 3 periods, with consideration of time dependence in the model.
Risk-adjusted in-hospital mortality was examined with 2 models. The first was the PSJH mortality risk model, which was a lookup table consisting of more than 5430 expected mortality rates. Such data were derived from the 3M All Patient Refined DRG, risk of mortality, and severity-of-illness grouper algorithm applied to a large inpatient database in the western US (eMethods in the Supplement ). The second was a multivariable logistic model, which considered all demographic variables listed in Table 1 . Results of the multivariable model were presented as adjusted odds ratio (OR) with 95% CI.
Patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes were summarized as descriptive statistics. Categorical data were presented as frequency (percentage). Numeric data were tested for normality and presented as mean (SD) or median (interquartile range [IQR]), as appropriate. Trends among the 3 COVID-19 periods were compared using univariate χ 2 , Fisher exact, or Kruskal-Wallis tests, as appropriate, for each variable. The level of statistical significance varied from P < .05 to P < .008, depending on Bonferroni adjustment for multiple comparisons (eMethods in the Supplement ).
The study cohort comprised 15 244 hospitalizations for AMI (4955 for STEMI [33%] and 10 289 for NSTEMI [67%]) involving 14 724 patients. Of those hospitalized, 5225 were women (34%) and 10 019 were men (66%), with a mean (SD) age of 68 (13) years ( Table 1 ). Before the COVID-19 period, the mean (SD) weekly case rate was 222 (17) patients for AMI, 72 (9) patients for STEMI, and 150 (13) patients for NSTEMI ( Figure and eTable 3 in the Supplement ). Beginning February 23, 2020, AMI hospitalizations decreased at a rate of –19.0 (95% CI, –29.0 to –9.0) cases per week for 5 weeks, marking the early COVID-19 period ( Figure ). Thereafter, AMI hospitalizations increased at a rate of +10.5 (95% CI, +4.6 to +16.5) cases per week, marking the later COVID-19 period. Weekly AMI hospitalization rates had not returned to baseline, however, by the last week evaluated (May 10, 2020; eTable 3 in the Supplement ). Similar trends in hospitalization for AMI, STEMI, and NSTEMI were observed in the PSJH system in all 6 states (eFigure 1 in the Supplement ).
Patients hospitalized for AMI in the early and later COVID-19 periods vs the before period were slightly younger (mean [SD] age, 67 [13] years vs 68 [13] years; P < .001) and more likely to be Asian (50 [6%] and 62 [6%] vs 667 [5%]; P = .01) or Native American individuals (20 [2%] and 21 [2%] vs 151 [1%]; P = .01) ( Table 1 ). Treatment approaches for patients with STEMI or NSTEMI were not statistically different across periods (eFigure 2 in the Supplement ). Median (IQR) length of stay for patients with AMI was shorter in the early COVID-19 period by 7 hours and in the later COVID-19 period by 6 hours compared with the before period (56 [41-115] hours and 57 [41-116] hours vs 63 [43-122] hours, respectively; P < .001) ( Table 2 ). Similar trends were observed for both types of AMI. A greater number of patients with AMI were discharged to home in the early and later COVID-19 periods vs the before COVID-19 period, with consistent findings among those with STEMI (235 [83%] and 284 [81%] vs 3402 [79%]; P = .02) and NSTEMI (465 [81%] and 587 [83%] vs 6976 [77%]; P = .006).
The observed (crude) in-hospital mortality rate was similar between periods for all groups ( Table 2 ). Compared with the before COVID-19 period, however, patients with STEMI had a statistically greater risk of mortality during the later COVID-19 period after adjusting for patient demographic characteristics and comorbidities (OR, 1.52; 95% CI, 1.02-2.26). Using the PSJH model, the observed to expected (O/E) hospital mortality ratio for patients with AMI was statistically increased in the early COVID-19 period (O/E ratio, 1.27; 95% CI, 1.07-1.48), with consistent findings in the later period as well (O/E ratio, 1.23; 95% CI, 0.98-1.47). These findings, however, were different for patients with STEMI vs those with NSTEMI. For patients with STEMI, the O/E mortality ratio was substantially higher in all 3 COVID-19 periods. These patients had a stepwise increase in the O/E mortality ratio from the before period (O/E ratio, 1.48; 95% CI, 1.34-1.62) to the early (O/E ratio, 1.96; 95% CI, 1.22-2.70) and later (O/E ratio, 2.40; 95% CI, 1.65-3.16) periods. The O/E mortality ratio for STEMI in the later period was statistically greater than the before period. In contrast, patients with NSTEMI had a consistently lower O/E mortality ratio for all 3 periods (before: O/E ratio, 0.80 [95% CI, 0.71-0.88]; early: O/E ratio, 0.91 [95% CI, 0.46-1.36]; later: O/E ratio, 0.71 [95% CI, 0.49-0.93]).
Consistent with previous reports, this study found a substantial decrease in AMI hospitalization rates in the early COVID-19 period. Beginning March 29, 2020, however, hospitalizations for AMI began to increase, albeit at a slower rate. Among the many factors likely associated with this rebound in cases was encouragement of patients with symptoms or signs of AMI to seek immediate medical attention, even amid the pandemic. 5 , 6
Although patient demographics and treatment approaches were fairly consistent across periods, patients with AMI hospitalized during the COVID-19 period were 1 to 3 years younger, had a shorter length of stay, and were more likely to be discharged to home. Possible explanations for these findings were greater reluctance by older patients to seek medical attention, hospital efforts to maintain bed availability, patient preference for early discharge, and concern about risk of contracting SARS-CoV-2 in post–acute care facilities.
Notable differences in risk-adjusted mortality were observed over the periods analyzed. Patients hospitalized for AMI during the early COVID-19 period had an increased O/E mortality ratio, associated disproportionately with patients with STEMI. In this population, the O/E ratio and risk-adjusted mortality rates were even greater during the later COVID-19 period. Given the time-sensitive nature of STEMI, any delay by patients, emergency medical services, the emergency department, or cardiac catheterization laboratory may have played a role. 7 , 8 Additional complications from delayed reperfusion (eg, conduction disturbances, heart failure, cardiogenic shock, and mechanical complications) 9 may have occurred in some patients. Further research is needed to identify factors associated with the higher mortality rate in patients with STEMI.
In the weeks and months to come, clinicians may see greater numbers of patients with more severe manifestations of AMI. With the uncertainty on timing of a COVID-19 vaccine, this study reinforces the need to address important care processes for patients with AMI to help mitigate further risk.
This study has several limitations. First, because the cohort was defined by coding data, it is possible that the primary reason for hospitalization was misclassified as an AMI. Second, the treatment analysis excluded outpatients and those with other MS-DRG codes. Although this group represented a small percentage of the total patient cohort (8% [1165]), treatment shifts may have been underappreciated. Third, the data set did not allow us to evaluate potential timing-related factors that may have contributed to higher in-hospital mortality (eg, time of symptom onset, first medical contact, and hospital arrival). Fourth, although the PSJH mortality risk model is not AMI-specific, we found consistent results with a multivariable model adjusted for patient demographic characteristics and comorbidities. Fifth, the COVID-19 status of patients included in the analysis was not available. As such, the higher observed rate of AMI mortality during the COVID-19 period could have been associated with concurrent SARS-CoV-2 infection.
Results of this cross-sectional study appear to validate previous concerns that large numbers of patients with AMI initially avoided hospitalization during the COVID-19 pandemic, likely out of fear of contracting SARS-CoV-2. Hospitalization rates for AMI have begun to increase but so has the risk of in-hospital mortality. Further research into factors associated with an increase in the STEMI mortality rate is warranted.
Accepted for Publication: July 10, 2020.
Corresponding Author: Ty J. Gluckman, MD, Center for Cardiovascular Analytics, Research and Data Science (CARDS), Providence Heart Institute, Providence St Joseph Health, 9427 SW Barnes Rd, Ste 594, Portland, OR 97225 ( [email protected] ).
Published Online: August 7, 2020. doi:10.1001/jamacardio.2020.3629
Author Contributions: Drs Gluckman and Chiu had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Gluckman, Chiu, Penny, Spinelli.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Gluckman, Chiu, Spinelli.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Chiu.
Administrative, technical, or material support: Gluckman, Wilson, Penny, Chepuri, Waggoner, Spinelli.
Supervision: Gluckman, Spinelli.
Conflict of Interest Disclosures: None reported.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Myocardial Infarction
Learn about the nursing care management of patients with myocardial infarction in this nursing study guide .
Table of Contents
- What is Myocardial Infarction?
Pathophysiology
Statistics and epidemiology, clinical manifestations, assessment and diagnostic findings, pharmacologic therapy, emergent percutaneous coronary intervention, nursing assessment, planning & goals, nursing priorities, nursing interventions, discharge and home care guidelines, documentation guidelines, practice quiz: myocardial infarction, what is myocardial infarction.
Myocardial infarction (MI) , is used synonymously with coronary occlusion and heart attack, yet MI is the most preferred term as myocardial ischemia causes acute coronary syndrome (ACS) that can result in myocardial death .
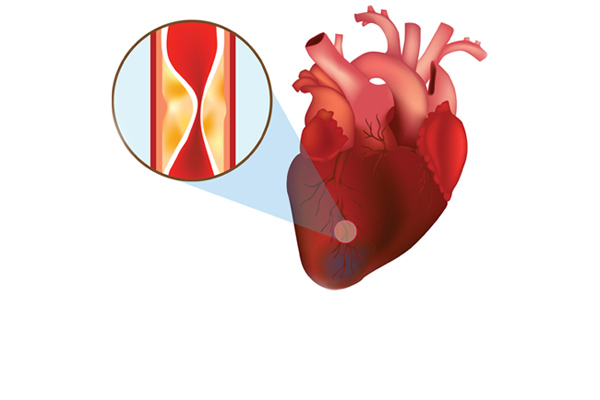
- In an MI, an area of the myocardium is permanently destroyed because plaque rupture and subsequent thrombus formation result in complete occlusion of the artery.
- The spectrum of ACS includes unstable angina , non-ST-segment elevation MI , and ST-segment elevation MI .
In each case of MI, a profound imbalance exists between myocardial oxygen supply and demand.
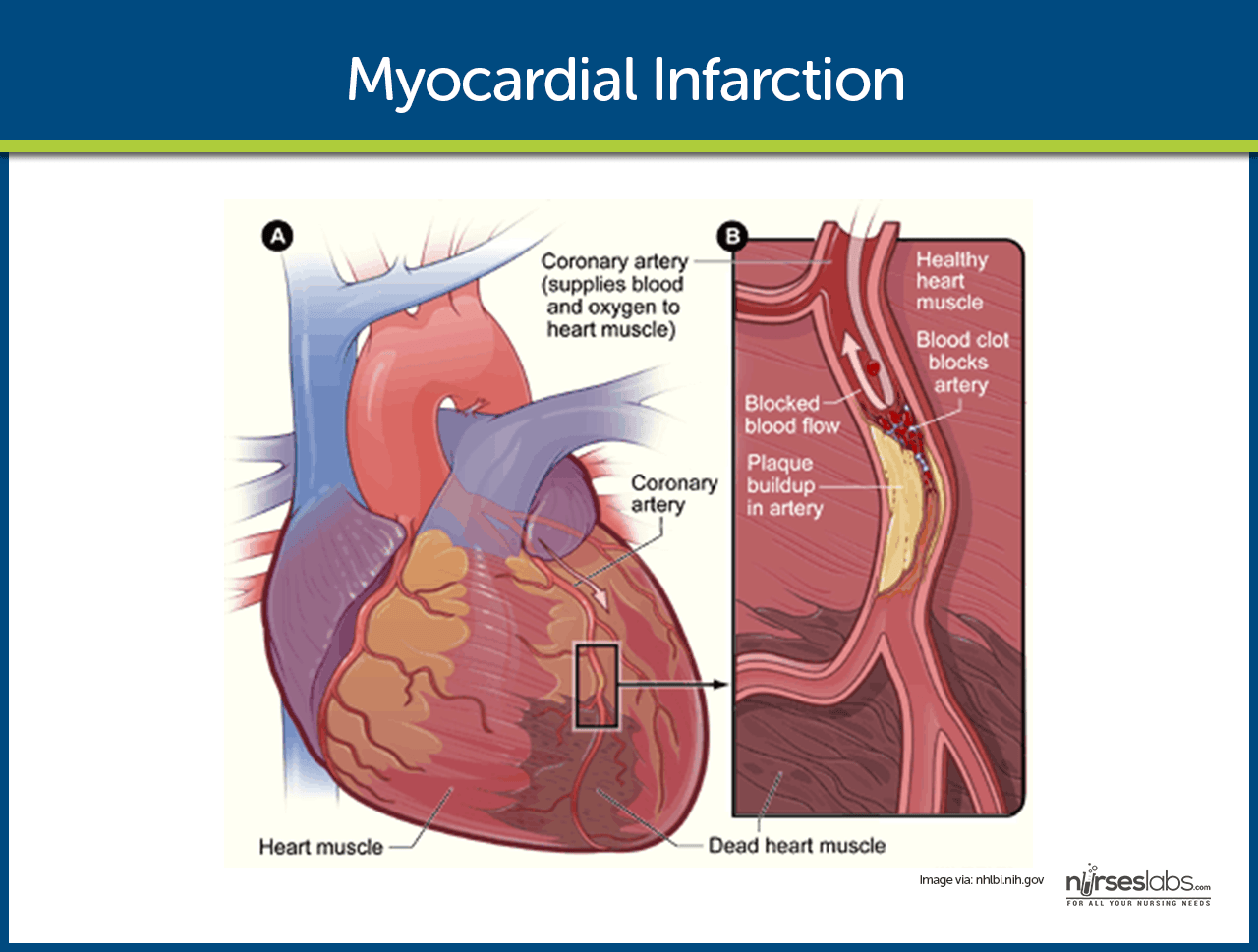
- Unstable angina . There is reduced blood flow in a coronary artery, often due to rupture of an atherosclerotic plaque, but the artery is not completely occluded.
- Development of infarction. As the cells are deprived of oxygen, ischemia develops, cellular injury occurs, and lack of oxygen leads to infarction or death of the cells.
- Schematic Diagram of Myocardial Infarction via Scribd
“Time is muscle ”; this is the reflection of the urgency of appropriate treatments to improve patient outcome.
- Each year in the United States, nearly 1 million people have acute MIs.
- One fourth of the people with the disease die of MI.
- Half of the people who die with acute MI never reach the hospital.
The causes of MI primarily stems from the vascular system.
- Vasospasm. This is the sudden constriction or narrowing of the coronary artery.
- Decreased oxygen supply. The decrease in oxygen supply occurs from acute blood loss , anemia , or low blood pressure .
- Increased demand for oxygen. A rapid heart rate, thyrotoxicosis, or ingestion of cocaine causes an increase in the demand for oxygen.
Some of the patients have prodromal symptoms or a previous diagnosis of CAD, but about half report no previous symptoms.
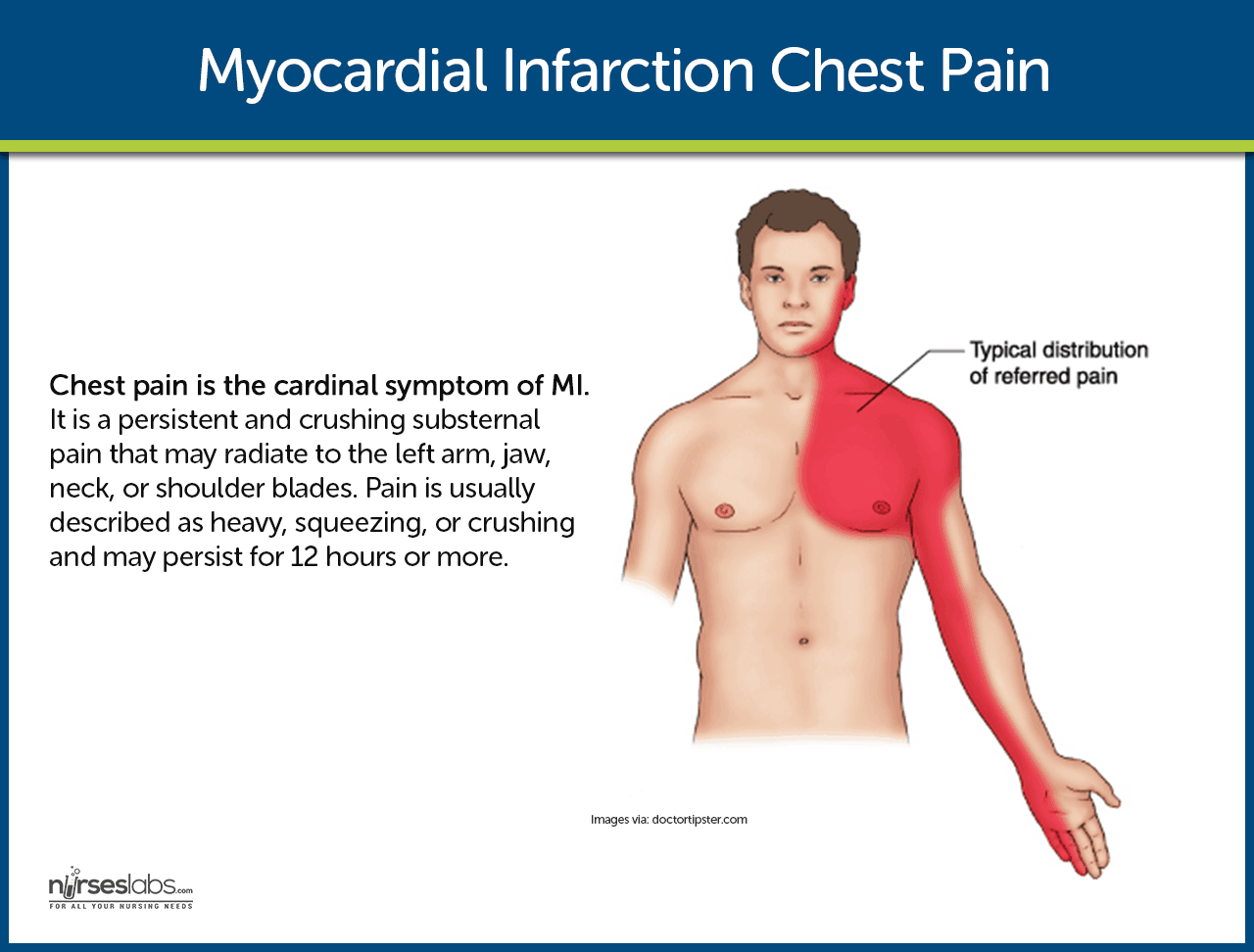
- Chest pain . This is the cardinal symptom of MI. Persistent and crushing substernal pain that may radiate to the left arm, jaw, neck, or shoulder blades. Pain is usually described as heavy, squeezing, or crushing and may persist for 12 hours or more.
- Shortness of breath. Because of increased oxygen demand and a decrease in the supply of oxygen, shortness of breath occurs.
- Indigestion. Indigestion is present as a result of the stimulation of the sympathetic nervous system .
- Tachycardia and tachypnea. To compensate for the decreased oxygen supply, the heart rate and respiratory rate speed up.
- Catecholamine responses. The patient may experience such as coolness in extremities, perspiration, anxiety , and restlessness.
- Fever. Unusually occurs at the onset of MI, but a low-grade temperature elevation may develop during the next few days.
A healthy lifestyle could help prevent the development of MI.
- Exercise. Exercising at least thrice a week could help lower cholesterol levels that cause vasoconstriction of the blood vessels.
- Balanced diet. Fruits, vegetables, meat and fish should be incorporated in the patient’s daily diet to ensure that he or she gets the right amount of nutrients he or she needs.
- Smoking cessation. Nicotine causes vasoconstriction which can increase the pressure of the blood and result in MI.
The diagnosis of MI is generally based on the presenting symptoms.
- Patient history. The patient history includes the description of the presenting symptoms, the history of previous cardiac and other illnesses, and the family history of heart diseases.
- ECG . ST elevation signifying ischemia; peaked upright or inverted T wave indicating injury; development of Q waves signifying prolonged ischemia or necrosis.
- Cardiac enzymes and isoenzymes. CPK-MB (isoenzyme in cardiac muscle): Elevates within 4–8 hr, peaks in 12–20 hr, returns to normal in 48–72 hr.
- LDH. Elevates within 8–24 hr, peaks within 72–144 hr, and may take as long as 14 days to return to normal. An LDH 1 greater than LDH 2 (flipped ratio) helps confirm/diagnose MI if not detected in acute phase.
- Troponins. Troponin I (cTnI) and troponin T (cTnT): Levels are elevated at 4–6 hr, peak at 14–18 hr, and return to baseline over 6–7 days. These enzymes have increased specificity for necrosis and are therefore useful in diagnosing postoperative MI when MB-CPK may be elevated related to skeletal trauma .
- Myoglobin. A heme protein of small molecular weight that is more rapidly released from damaged muscle tissue with elevation within 2 hr after an acute MI, and peak levels occurring in 3–15 hr.
- Electrolytes . Imbalances of sodium and potassium can alter conduction and compromise contractility.
- WBC. Leukocytosis (10,000–20,000) usually appears on the second day after MI because of the inflammatory process.
- ESR. Rises on second or third day after MI, indicating inflammatory response.
- Chemistry profiles. May be abnormal, depending on acute/chronic abnormal organ function/perfusion.
- ABGs / pulse oximetry . May indicate hypoxia or acute/chronic lung disease processes.
- Lipids (total lipids, HDL, LDL, VLDL, total cholesterol, triglycerides, phospholipids). Elevations may reflect arteriosclerosis as a cause for coronary narrowing or spasm.
- Chest x-ray . May be normal or show an enlarged cardiac shadow suggestive of HF or ventricular aneurysm .
- Two-dimensional echocardiogram . May be done to determine dimensions of chambers, septal/ventricular wall motion, ejection fraction (blood flow), and valve configuration/function.
- Nuclear imaging studies: Persantine or Thallium. Evaluates myocardial blood flow and status of myocardial cells, e.g., location/extent of acute/previous MI.
- Cardiac blood imaging/MUGA. Evaluates specific and general ventricular performance, regional wall motion, and ejection fraction.
- Technetium. Accumulates in ischemic cells, outlining necrotic area(s).
- Coronary angiography. Visualizes narrowing/occlusion of coronary arteries and is usually done in conjunction with measurements of chamber pressures and assessment of left ventricular function (ejection fraction). Procedure is not usually done in acute phase of MI unless angioplasty or emergency heart surgery is imminent.
- Digital subtraction angiography (DSA). Technique used to visualize status of arterial bypass grafts and to detect peripheral artery disease.
- Magnetic resonance imaging (MRI). Allows visualization of blood flow, cardiac chambers or intraventricular septum, valves, vascular lesions, plaque formations, areas of necrosis/infarction, and blood clots.
- Exercise stress test. Determines cardiovascular response to activity (often done in conjunction with thallium imaging in the recovery phase).
Medical Management
The goals of medical management are to minimize myocardial damage, preserve myocardial function, and prevent complications.
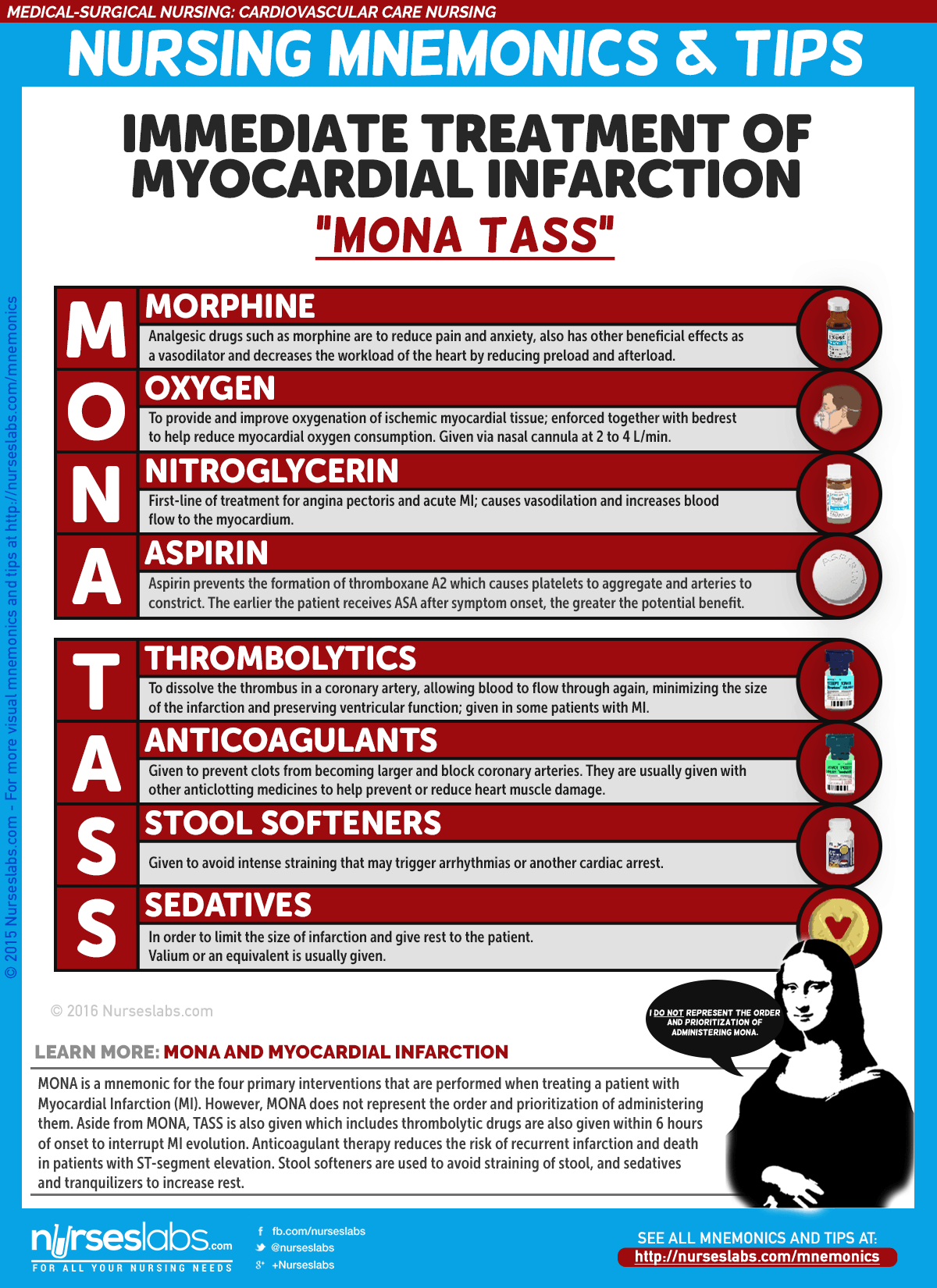
- Morphine administered in IV boluses is used for MI to reduce pain and anxiety.
- ACE Inhibitors . ACE inhibitors prevent the conversion of angiotensin I to angiotensin II to decrease blood pressure and for the kidneys to secrete sodium and fluid, decreasing the oxygen demand of the heart.
- Thrombolytics. Thrombolytics dissolve the thrombus in the coronary artery,allowing blood to flow through the coronary artery again, minimizing the size of the infarction and preserving ventricular function.
- The procedure is used to open the occluded coronary artery and promote reperfusion to the area that has been deprived of oxygen.
- PCI may also be indicated in patients with unstable angina and NSTEMI for patients who are at high risk due to persistent ischemia.
Nursing Management
The nursing management involved in MI is critical and systematic, and efficiency is needed to implement the care for a patient with MI.
One of the most important aspects of care of the patient with MI is the assessment.
- Assess for chest pain not relieved by rest or medications.
- Monitor vital signs, especially the blood pressure and pulse rate.
- Assess for presence of shortness of breath, dyspnea , tachypnea, and crackles.
- Assess for nausea and vomiting .
- Assess for decreased urinary output.
- Assess for the history of illnesses.
- Perform a precise and complete physical assessment to detect complications and changes in the patient’s status.
- Assess IV sites frequently.
Based on the clinical manifestations, history, and diagnostic assessment data, major nursing diagnoses may include.
- Ineffective cardiac tissue perfusion related to reduced coronary blood flow.
- Risk for ineffective peripheral tissue perfusion related to decreased cardiac output from left ventricular dysfunction.
- Deficient knowledge related to post-MI self-care .
Main Article: 7 Myocardial Infarction (Heart Attack) Nursing Care Plans
To establish a plan of care, the focus should be on the following:
- Relief of pain or ischemic signs and symptoms.
- Prevention of myocardial damage.
- Absence of respiratory dysfunction.
- Maintenance or attainment of adequate tissue perfusion.
- Reduced anxiety.
- Absence or early detection of complications.
- Chest pain absent/controlled.
- Heart rate/rhythm sufficient to sustain adequate cardiac output/tissue perfusion.
- Achievement of activity level sufficient for basic self-care.
- Anxiety reduced/managed.
- Disease process, treatment plan, and prognosis understood.
- Plan in place to meet needs after discharge.
- Relieve pain, anxiety.
- Reduce myocardial workload.
- Prevent/detect and assist in treatment of life-threatening dysrhythmias or complications.
- Promote cardiac health, self-care.
Nursing interventions should be anchored on the goals in the nursing care plan .
- Administer oxygen along with medication therapy to assist with relief of symptoms.
- Encourage bed rest with the back rest elevated to help decrease chest discomfort and dyspnea.
- Encourage changing of positions frequently to help keep fluid from pooling in the bases of the lungs .
- Check skin temperature and peripheral pulses frequently to monitor tissue perfusion.
- Provide information in an honest and supportive manner.
- Monitor the patient closely for changes in cardiac rate and rhythm, heart sounds, blood pressure, chest pain, respiratory status, urinary output, changes in skin color, and laboratory values.
After the implementation of the interventions within the time specified, the nurse should check if:
- There is an absence of pain or ischemic signs and symptoms.
- Myocardial damage is prevented.
- Adequate tissue perfusion maintained.
- Anxiety is reduced.
The most effective way to increase the probability that the patient will implement a self-care regimen after discharge is to identify the patient’s priorities.
- Education. This is one of the priorities that the nurse must teach the patient about heart-healthy living.
- Home care. The home care nurse assists the patient with scheduling and keeping up with the follow-up appointments and with adhering to the prescribed cardiac rehabilitation management.
- Follow-up monitoring. The patient may need reminders about follow-up monitoring including periodic laboratory testing and ECGs, as well as general health screening.
- Adherence. The nurse should also monitor the patient’s adherence to dietary restrictions and prescribed medications.
To ensure that every action documented is an action done, documentation must be secured. The following should be documented:
- Individual findings.
- Vital signs, cardiac rhythm , presence of dysrhythmias.
- Plan of care and those involved in planning.
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress towards desired outcomes.
- Modifications to plan of care.
Let’s reinforce what you’ve learned with this 5-item NCLEX practice quiz about Myocardial Infarction. Please visit our nursing test bank for more NCLEX practice questions .
1. Which of the following is the most common symptom of myocardial infarction (MI)?
A. Chest pain B. Dyspnea C. Edema D. Palpitations
2. An intravenous analgesic frequently administered to relieve chest pain associated with MI is:
A. Meperidine hydrochloride B. Hydromorphone hydrochloride C. Morphine sulfate D. Codeine sulfate
3. The classic ECG changes that occur with an MI include all of the following except:
A. An absent P wave B. An abnormal Q wave C. T-wave inversion D. ST segment elevation
4. Which of the following statements about myocardial infarction pain is incorrect?
A. It is relieved by rest and inactivity. B. It is substernal in location. C. It is sudden in onset and prolonged in duration. D. It is viselike and radiates to the shoulders and arms.
5. Myocardial cell damage can be reflected by high levels of cardiac enzymes. The cardiac-specific isoenzyme is:
A. Alkaline phosphatase B. Creatine kinase (CK-MB) C. Myoglobin D. Troponin
1. Answer: A. Chest pain
- A: The most common symptom of an MI is chest pain, resulting from deprivation of oxygen to the heart.
- B: Dyspnea is the second most common symptom, related to an increase in the metabolic needs of the body during an MI.
- C: Edema is a later sign of heart failure , often seen after an MI.
- D: Palpitations may result from reduced cardiac output, producing arrhythmias.
2. Answer: C. Morphine sulfate
- C: Morphine administered in IV boluses is used for MI to reduce pain and anxiety.
- A: Meperidine hydrochloride is not the analgesic of choice for MI.
- B: Hydromorphone hydrochloride is not the analgesic of choice for MI.
- D: Codeine sulfate is not the analgesic of choice for MI.
3. Answer: A. An absent P wave
- A: An absent P wave is not part of the classic changes seen in an ECG result.
- B: An abnormal Q wave is an indication of MI.
- C: T-wave inversion is a classic ECG change in a patient with MI.
- D: ST segment elevation is an indication of MI.
4. Answer: A. It is relieved by rest and inactivity.
- A: MI pain continues despite rest and medications.
- B: The pain occurs substernally or at the chest area.
- C: MI pain occurs suddenly and is prolonged in duration.
- D: The pain grips the patient like a vise and radiates towards the arms or the shoulders.
5. Answer: B. Creatine kinase (CK-MB)
- B: CK-MB is the isoenzyme for the heart muscle and the cardiac-specific enzyme.
- A: Alkaline phosphatase is not part of the creatine kinase isoenzymes.
- C: Myoglobin is a heme protein that helps transport oxygen.
- D: Troponin regulates the myocardial contractile process.
Posts related to Myocardial Infarction:
- 7 Myocardial Infarction (Heart Attack) Nursing Care Plans
- Myocardial Infarction and Heart Failure NCLEX Practice Quiz (70 Items)
- Heart Failure
- Cardiovascular Care Nursing Mnemonics and Tips
3 thoughts on “Myocardial Infarction”
Good lecture
Very refreshing lecture
Leave a Comment Cancel reply
Myocardial Infarction (MI) Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Definition of Myocardial Infarction (MI)
Myocardial infarction, commonly known as a heart attack, is a critical medical event that occurs when the blood supply to the heart muscle is severely reduced or completely blocked. It is a leading cause of death worldwide and a significant public health concern.
Introduction to Myocardial Infarction (MI)
This nursing case study aims to provide a comprehensive understanding of myocardial infarction by delving into its various aspects, including its pathophysiology, risk factors, clinical presentation, diagnostic methods, and management strategies. Through the exploration of a fictional patient’s journey, we will shed light on the intricate nature of this life-threatening condition and highlight the importance of early recognition and intervention.
Background and Significance of Myocardial Infarction
Myocardial infarction is a sudden and often catastrophic event that can have profound consequences on an individual’s health and well-being. Understanding its underlying mechanisms and risk factors is essential for healthcare professionals, as timely intervention can be life-saving. This case study not only serves as a learning tool but also emphasizes the critical role of medical practitioners in identifying and managing myocardial infarctions promptly.
Pathophysiology of Myocardial Infarction
A crucial aspect of comprehending myocardial infarction is exploring its pathophysiology. We will delve into the intricate details of how atherosclerosis, the buildup of plaque in coronary arteries, leads to the formation of blood clots and the subsequent interruption of blood flow to the heart muscle. This disruption in blood supply triggers a cascade of events, ultimately resulting in the death of cardiac cells.
Risk Factors of Myocardial Infarction
Understanding the risk factors associated with myocardial infarction is vital for prevention and early detection. This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental in developing effective strategies for prevention and risk reduction.
Clinical Presentation Myocardial Infarction
Recognizing the signs and symptoms of myocardial infarction is crucial for timely intervention. We will present a fictional patient’s experience, illustrating the typical clinical presentation, which often includes chest pain or discomfort, shortness of breath, nausea, lightheadedness, and diaphoresis. Through this patient’s journey, we will highlight the importance of accurate symptom assessment and prompt medical attention.
Diagnostic Methods for Myocardial Infarction
Modern medicine offers various diagnostic tools to confirm a myocardial infarction swiftly and accurately. This case study will explore these diagnostic methods, such as electrocardiography (ECG), cardiac biomarkers, and imaging techniques like coronary angiography. By understanding these diagnostic modalities, healthcare professionals can make informed decisions and initiate appropriate treatments promptly.
Management Strategies for Myocardial Infarction
The management of myocardial infarction involves a multidisciplinary approach, including medication, revascularization procedures, and lifestyle modifications. We will discuss the fictional patient’s treatment plan, emphasizing the importance of reestablishing blood flow to the affected heart muscle and preventing further complications.
Nursing Case Study for Myocardial Infarction (MI)
Having established a foundational understanding of myocardial infarction, we will now delve deeper into Mr. Salazar’s case, tracing his journey through diagnosis, treatment, and recovery. This in-depth examination will shed light on the real-world application of the principles discussed in the introduction, providing valuable insights into the clinical management of myocardial infarction and its impact on patient outcomes.
Mr. Salazar, a 57-year-old male, arrives at the Emergency Department (ED) with complaints of chest pain that began approximately one hour after dinner while he was working. He characterizes the discomfort as an intense “crushing pressure” located centrally in his chest, extending down his left arm and towards his back. He rates the pain’s severity as 4/10. Upon examination, Mr. Salazar exhibits diaphoresis and pallor, accompanied by shortness of breath (SOB).
What further nursing assessments need to be performed for Mr. Salazar?
- Heart Rate (HR): The number of heartbeats per minute.
- Blood Pressure (BP): The force of blood against the walls of the arteries, typically measured as systolic (during heartbeats) and diastolic (between heartbeats) pressure.
- Respiratory Rate (RR): The number of breaths a patient takes per minute.
- Body Temperature (Temp): The measurement of a patient’s internal body heat.
- Oxygen Saturation (SpO2): The percentage of oxygen in the blood.
- S1: The first heart sound, often described as “lub,” is caused by the closure of the mitral and tricuspid valves.
- S2: The second heart sound, known as “dub,” results from the closure of the aortic and pulmonic valves.
- These sounds provide important diagnostic information about the condition of the heart.
- Clear: Normal, healthy lung sounds with no added sounds.
- Crackles (Rales): Discontinuous, often high-pitched sounds are heard with conditions like pneumonia or heart failure.
- Wheezes: Whistling, musical sounds often associated with conditions like asthma or chronic obstructive pulmonary disease (COPD).
- Pulses refer to the rhythmic expansion and contraction of arteries with each heartbeat. Common pulse points for assessment include the radial artery (wrist), carotid artery (neck), and femoral artery (groin). Evaluating pulses helps assess the strength, regularity, and rate of blood flow.
- Edema is the abnormal accumulation of fluid in body tissues, leading to swelling. It can occur in various body parts and may indicate underlying conditions such as heart failure, kidney disease, or localized injury. Edema assessment involves evaluating the degree of swelling and its location.
- Skin condition (temperature, color, etc.)
What interventions do you anticipate being ordered by the provider?
- Oxygen therapy involves administering oxygen to a patient to increase the level of oxygen in their blood. It is used to treat conditions such as respiratory distress, and hypoxia (low oxygen levels), and to support patients with breathing difficulties.
- Nitroglycerin is a medication used to treat angina (chest pain) and to relieve symptoms of heart-related conditions. It works by relaxing and widening blood vessels, which improves blood flow to the heart, reducing chest pain.
- Aspirin is a common over-the-counter medication and antiplatelet drug. In the context of myocardial infarction (heart attack), it is often administered to reduce blood clot formation, potentially preventing further blockage in coronary arteries.
- A 12-lead EKG is a diagnostic test that records the electrical activity of the heart from 12 different angles. It provides information about the heart’s rhythm, rate, and any abnormalities, helping diagnose conditions like arrhythmias, heart attacks, and ischemia.
- Cardiac enzymes are proteins released into the bloodstream when heart muscle cells are damaged or die, typically during a heart attack. Measuring these enzymes, such as troponin and creatine kinase-MB (CK-MB), helps confirm a heart attack diagnosis and assess its severity.
- A chest X-ray is a diagnostic imaging procedure that creates images of the chest and its internal structures, including the heart and lungs. It is used to identify issues like lung infections, heart enlargement, fluid accumulation, or fractures in the chest area.
- Possibly an Echocardiogram
Upon conducting a comprehensive assessment, it was observed that the patient exhibited no signs of jugular vein distention (JVD) or edema. Auscultation revealed normal heart sounds with both S1 and S2 present, while the lungs remained clear, albeit with scattered wheezes. The patient’s vital signs were recorded as follows:
- BP 140/90 mmHg SpO 2 90% on Room Air
- HR 92 bpm and regular Ht 173 cm
- RR 32 bpm Wt 104 kg
- Temp 36.9°C
The 12-lead EKG repor t indicated the presence of “Normal sinus rhythm (NSR) with frequent premature ventricular contractions (PVCs) and three- to four-beat runs of ventricular tachycardia (VT).” Additionally, there was ST-segment elevation in leads I, aVL, and V2 through V6 (3-4mm), accompanied by ST-segment depression in leads III and aVF.
Cardiac enzyme levels were collected but were awaiting results at the time of assessment. A chest x-ray was also ordered to provide further diagnostic insights.
In response to the patient’s condition, the healthcare provider prescribed the following interventions:
- Aspirin: 324 mg administered orally once.
- Nitroglycerin: 0.4 mg administered sublingually (SL), with the option of repeating the dose every five minutes for a maximum of three doses.
- Morphine: 4 mg to be administered intravenously (IVP) as needed for unrelieved chest pain.
- Oxygen: To maintain oxygen saturation (SpO2) levels above 92%.
These interventions were implemented to address the patient’s myocardial infarction (heart attack) and alleviate associated symptoms, with a focus on relieving chest pain, improving oxygenation, and closely monitoring vital signs pending further diagnostic results.
What intervention should you, as the nurse, perform right away? Why?
- Apply oxygen – this can be done quickly and easily and can help to prevent further complications from low oxygenation.
- Oxygen helps to improve oxygenation as well as to decrease myocardial oxygen demands.
- Often it takes a few minutes or more for medications to be available from the pharmacy, so it makes sense to take care of this intervention first.
- ABC’s – breathing/O 2 .
What medication should be the first one administered to this patient? Why? How often?
- Nitroglycerin 0.4mg SL – it is a vasodilator and works on the coronary arteries. The goal is to increase blood flow to the myocardium. If this is effective, the patient merely has angina. However, if it is not effective, the patient may have a myocardial infarction.
- Aspirin should also be given, but it is to decrease platelet aggregation and reduce mortality. While it can somewhat help prevent the worsening of the blockage, it does little for the current pain experienced by the patient.
- Morphine should only be given if the nitroglycerin and aspirin do not relieve the patient’s chest pain.
What is the significance of the ST-segment changes on Mr. Salazar's 12-lead EKG?
- ST-segment changes on a 12-lead EKG indicate ischemia (lack of oxygen/blood flow) or infarction (death of the muscle tissue) of the myocardium (heart muscle).
- This indicates an emergent situation. The patient’s coronary arteries are blocked and need to be reopened by pharmacological (thrombolytic) or surgical (PCI) intervention.
- Time is tissue – the longer the coronary arteries stay blocked, the more of the patient’s myocardium that will die. Dead heart tissue doesn’t beat.
Mr. Salazar’s chest pain was unrelieved after three (3) doses of sublingual nitroglycerin (NTG). Morphine 5 mg intravenous push (IVP) was administered, as well as 324 mg chewable baby aspirin. His pain was still unrelieved at this point
Mr. Salazar’s cardiac enzyme results were as follows:
Troponin I 3.5 ng/mL
Based on the results of Mr. Salazar's labs and his response to medications, what is the next intervention you anticipate? Why?
- Mr. Salazar needs intervention. He will either receive thrombolytics or a heart catheterization (PCI).
- Based on the EKG changes, elevated Troponin level, and the fact that his symptoms are not subsiding, it’s possible the patient has a significant blockage in one or more of his coronary arteries.
- It seems as though it may be an Anterior-Lateral MI because ST elevation is occurring in I, aVL, and V 2 -V 6 .
Mr. Salazar was taken immediately to the cath lab for a Percutaneous Coronary Intervention (PCI). The cardiologist found a 90% blockage in his left anterior descending (LAD) artery. A stent was inserted to keep the vessel open.
What is the purpose of Percutaneous Coronary Intervention (PCI), also known as a heart catheterization?
- A PCI serves to open up any coronary arteries that are blocked. First, they use contrast dye to determine where the blockage is, then they use a special balloon catheter to open the blocked vessels.
- If that doesn’t work, they will place a cardiac stent in the vessel to keep it open.[ /faq]
[faq lesson="true" blooms="Application" question="What is the expected outcome of a PCI? What do you expect to see in your patient after they receive a heart catheterization?"]
- Blood flow will be restored to the myocardium with minimal residual damage.
- The patient should have baseline vital signs, relief of chest pain, normal oxygenation status, and absence of heart failure symptoms (above baseline).
- The patient should be able to ambulate without significant chest pain or SOB.
- The patient should be free from bleeding or hematoma at the site of catheterization (often femoral, but can also be radial or (rarely) carotid.
Mr. Salazar tolerated the PCI well and was admitted to the cardiac telemetry unit for observation overnight. Four (4) hours after the procedure, Mr. Salazar reports no chest pain. His vital signs are now as follows:
- BP 128/82 mmHg SpO 2 96% on 2L NC
- HR 76 bpm and regular RR 18 bpm
- Temp 37.1°C
Mr. Salazar will be discharged home 24 hours after his arrival to the ED and will follow up with his cardiologist next week.

What patient education topics would need to be covered with Mr. Salazar?
- He should be taught any dietary and lifestyle changes that should be made.
- Diet – low sodium, low cholesterol, avoid sugar/soda, avoid fried/processed foods.
- Exercise – 30-45 minutes of moderate activity 5-7 days a week, u nless instructed otherwise by a cardiologist. This will be determined by the patient’s activity tolerance – how much can they do and still be able to breathe and be pain-free?
- Stop smoking and avoid caffeine and alcohol.
- Medication Instructions
- Nitroglycerin – take one SL tab at the onset of chest pain. If the pain does not subside after 5 minutes, call 911 and take a second dose. You can take a 3rd dose 5 minutes after the second if the pain does not subside. Do NOT take if you have taken Viagra in the last 24 hours.
- Aspirin – take 81 mg of baby aspirin daily
- Anticoagulant – the patient may be prescribed an anticoagulant if they had a stent placed. They should be taught about bleeding risks.
- When to call the provider – CP unrelieved by nitroglycerin after 5 minutes. Syncope. Evidence of bleeding in stool or urine (if on anticoagulant). Palpitations, shortness of breath, or difficulty tolerating activities of daily living.
Linchpins for Myocardial Infarction Nursing Case Study
In summary, Mr. Salazar’s case highlights the urgency of recognizing and responding to myocardial infarction promptly. The application of vital signs, EKG, cardiac enzymes, and medications like aspirin, nitroglycerin, and morphine played a pivotal role in his care. Diagnostic tools like echocardiography and chest X-rays contributed to a comprehensive evaluation.
Nurses must remain vigilant and compassionate in such emergencies. This case study emphasizes the importance of adhering to best practices in the assessment, diagnosis, and management of myocardial infarction, with the ultimate goal of achieving favorable patient outcomes.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
- Campus Directory
- Current Students
- Faculty & Staff

Acute Myocardial Infarction Case Study
Myocardial infarction (heart attack) is the leading cause of death in the United States. It is estimated that one in every five deaths in the US is due to a heart attack. Approximately one million patients are admitted to hospitals each year due to heart attacks. 200,000 to 300,000 individuals die from heart attacks before ever receiving medical care. In Case #2 we’ll join 48-year-old Jason Dixon as he experiences a life-threatening heart attack.
Module 7: Acute Myocardial Infarction
48 year old Jason Dixon had not been feeling well all day and around 10:00 p.m he went to bed...
AMI - Page 1
Before we progress further into this relatively complex case, please review module 6 in the...
AMI - Page 2
Case continued: Enroute to the ER, the patient's acute symptoms had been relieved...
AMI - Page 3
This is a critical decision point for the cardiologist. There are several algorithms...
AMI - Page 4
Case Summary
Summary of the Case
AMI - Summary

Answers to Case Questions
AMI - Answers

Professionals
Health Professionals Introduced in Case
AMI - Professionals
Additional Links
Optional Links to Explore Further
AMI - Links
Acute triggers of myocardial infarction: A case-crossover study
Affiliations.
- 1 Guilan Social Security Organization, Rasool-e-Akram Hospital, Rasht, Iran.
- 2 Department of Disaster Public Health, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
- 3 Department of Nursing (Medical-Surgical), Instructor, Social Determinants of Health Research Center (SDHRC), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
- 4 Department of Operating Room & Anesthesia, Paramedical School, Guilan University of Medical Sciences, Rasht, Iran.
- 5 Nursing and Midwifery Faculty, Guilan University of Medical Sciences, Rasht, Iran.
- PMID: 29622981
- PMCID: PMC5883494
- DOI: 10.1016/j.ehj.2017.03.003
Background: Acute myocardial infarction (AMI) is one of the most preventable non-communicable diseases in human. Identifying triggers of myocardial infarction (MI) and prevention ways of exposure-induced complications can reduce morbidity and mortality in people at risk.
Aim: The aim of this study was to identify the emotional, environmental, physical and chemical dimensions of acute triggers in patients with AMI.
Methods: This case-crossover study was conducted on 269 patients with AMI, hospitalized at two remedial centers in Rasht in 2015. The study samples were selected by convenient sampling method. Data were collected using researcher-made questionnaire through interviews. Hazard and control periods for each trigger and its effects on the development of MI were studied. The collected data were analyzed using descriptive and analytical statistical methods, Cochran test, and generalized estimating equation (GEE) model with logistics function default in SPSS version 21, and p < 0.05 was considered statistically significant.
Results: The results showed that quarrel ( P = 0.008, OR = 2.01) and hearing the sudden news ( P = 0.001, OR = 2.19) were the most common emotional triggers. Respiratory infections ( P = 0.0001, OR = 6.78) and exposure to hot or cold weather ( P = 0.005, OR = 2.19) were the most frequent environmental triggers. Doing heavy activities ( P = 0.005, OR = 1.66) and sexual activities ( P = 0.003, OR = 2.36) were among the most common physical triggers. High-fat foods consumption and overeating ( P = 0.0001, OR = 3.79) were the most frequent chemical triggers of AMI.
Conclusion: It seems that given the importance of the triggers in the incidence of AMI, planning is necessary to train vulnerable individuals to reduce exposure to triggers.
Keywords: Control period; Hazard period; Myocardial infarction; Triggers.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Egypt Heart J
- v.69(4); 2017 Dec
Acute triggers of myocardial infarction: A case-crossover study ☆
Maryam ghiasmand.
a Guilan Social Security Organization, Rasool-e-Akram Hospital, Rasht, Iran
Mohammad Taghi Moghadamnia
b Department of Disaster Public Health, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
c Department of Nursing (Medical-Surgical), Instructor, Social Determinants of Health Research Center (SDHRC), School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
Majid Pourshaikhian
d Department of Operating Room & Anesthesia, Paramedical School, Guilan University of Medical Sciences, Rasht, Iran
Ehsan Kazemnejad Lili
e Nursing and Midwifery Faculty, Guilan University of Medical Sciences, Rasht, Iran
Acute myocardial infarction (AMI) is one of the most preventable non-communicable diseases in human. Identifying triggers of myocardial infarction (MI) and prevention ways of exposure-induced complications can reduce morbidity and mortality in people at risk.
The aim of this study was to identify the emotional, environmental, physical and chemical dimensions of acute triggers in patients with AMI.
This case-crossover study was conducted on 269 patients with AMI, hospitalized at two remedial centers in Rasht in 2015. The study samples were selected by convenient sampling method. Data were collected using researcher-made questionnaire through interviews. Hazard and control periods for each trigger and its effects on the development of MI were studied. The collected data were analyzed using descriptive and analytical statistical methods, Cochran test, and generalized estimating equation (GEE) model with logistics function default in SPSS version 21, and p < 0.05 was considered statistically significant.
The results showed that quarrel ( P = 0.008, OR = 2.01) and hearing the sudden news ( P = 0.001, OR = 2.19) were the most common emotional triggers. Respiratory infections ( P = 0.0001, OR = 6.78) and exposure to hot or cold weather ( P = 0.005, OR = 2.19) were the most frequent environmental triggers. Doing heavy activities ( P = 0.005, OR = 1.66) and sexual activities ( P = 0.003, OR = 2.36) were among the most common physical triggers. High-fat foods consumption and overeating ( P = 0.0001, OR = 3.79) were the most frequent chemical triggers of AMI.
It seems that given the importance of the triggers in the incidence of AMI, planning is necessary to train vulnerable individuals to reduce exposure to triggers.
1. Introduction
The cardiovascular diseases impose an enormous cost on country's health and therapeutic systems. However, they are among the most preventable non-communicable diseases in human beings. 1 Two kinds of factors are involved in developing heart diseases, the chronic and acute risk factors (ARFs). 2 , 3 ARFs engage by sympathetic or parasympathetic stimulation leading to vasoconstriction, prothrombotic or biomechanical activities, thrombosis plaque rupture and myocardial infarction (MI) or acute coronary syndrome. 4
During 1980s, a relationship between sexual activity, insomnia, and MI was found, and it was estimated that 50% of acute myocardial infarction (AMI) can be triggered by external factors. A relationship between physical activities, anger, sexual activity, cocaine abuse, overeating and AMI incidence has been shown hours before its onset over recent two decades. 4 AMI may be triggered by several factors such as physical activities, stressful events, overeating and increased air pollution, and the importance and prevalence of each of these triggers are unclear. 5 A trigger is, in fact, an external stimulus that causes pathological changes, and there is a direct relationship between exposure to a stimulus and disease incidence happening during some hour period (some minutes to 24 h before acute coronary syndrome (ACS) onset). This time interval is known as “hazard period”. 6 , 7 If there is a vulnerable atherosclerotic plaque, the trigger, through vasoconstriction and prothrombotic construction, causes the thrombosis plaque rupture and reduces the heart's electrical stability threshold, and increases sympathetic activity via the release of central mediators such as catecholamine leading to ventricular fibrillation and sudden cardiac death. 2 , 8 Acute triggers fall in four categories, including emotional, physical, environmental and chemical triggers. 8 , 9 , 10 , 11 , 12 , 13 , 14 Karek et al. reported deaths increase as 58% in Persian Gulf War in 1991 following Iraqi missile attacks on Israel and resulted in stresses caused by a combination of emotional and chemical triggers. Also, emotional stresses caused by September 11, 2001, attacks in New York showed that terrorist attacks-induced psychological stresses can trigger cardiovascular events resulted from the combination of environmental and emotional triggers. 8
Evidence suggests that air pollution, time spent in a traffic jam, and temperature changes are among the environmental triggers of MI. Exposure to micro-pollutant with 2.5 μm is associated with the incidence of cardiovascular events and increases the risk of AMI. 4 Also, there is a relationship between respiratory infections 15 and seasonal temperature changes with the incidence of AMI. 16 Some studies have reported increased rates of hospitalization and mortality resulted from AMI in winter and the lowest hospitalization and death in summer. In a study conducted by Mohammadian, it was shown that the increase in AMI cases was not confirmed in cold seasons, and the results demonstrated that the incidence of AMI grew in spring season. 17 Physical triggers of AMI such as sexual activities and heavy exercises can play a role in AMI incidence. Despite the benefits of regular exercise, physical activities and exposure to acute factors such as sexual activities and psychological stress can trigger heart diseases. 13 Chemical triggers of AMI including eating high-fat foods, drinking coffee even a cup of it, 18 abusing alcohol, and smoking marijuana can cause heart diseases. According to official data provided by the Ministry of Health in IRAN 33–38% of deaths were caused by cardiovascular disease especially acute myocardial infarction. 9
Therefore, given the importance of triggers effects on accelerating the process of sclerotic plaque rupture and the development of AMI, this study aimed to identify acute triggers in people with AMI and the relationship between acute risk factors and odds of AMI in patients at risk and to determine the most common type of trigger. By achieving these objectives, we can promote awareness of people at risk to prevent and reduce morbidity and mortality.
In this case-crossover, study triggers of AMI were examined at two remedial centers of Rasht. Rasht is the biggest city located in northern Iran with more than one million people. This city has a humid subtropical climate with relatively high temperatures in summer and rainfall coming from convectional thunderstorm activity and tropical cyclones in winter. The required sample size was determined as 269 based on results of Harrison’s Principles of Internal Medicine, Lanky et al.’s study and the National Census of America. 20 , 21 , 22 In this study, each patient was his/her own control during the 24 h before the onset of symptoms and was compared with that at the time of a few days, few weeks, and few months before the onset of AMI. The first 24 h was considered as the hazard period. In addition to hazard period, another time interval, known as a control period, was considered to study the trigger effect. In this study, three control periods were used to study on triggers’ effect with regard to their nature. This period was determined as one day, two days, and five days before AMI onset for triggers such as anger, quarrel, hearing sudden news, insomnia, watching sport games, sudden exposure to hot or cold weather, exposure to traffic jam, witnessing a car accident, doing heavy and sexual activities, eating high-fat foods and overeating, alcohol and drug abuse, and coffee or tea drinking, while this period was established as one week, two weeks, and more than four weeks before AMI onset for triggers such as respiratory infections and losing a job due to the chronic nature of the trigger. The control period was determined as one month, one to six months, and six to 12 months before AMI onset for loss of loved one trigger. According to previous studies that showed loss of loved ones living with a long-term effect on the incidence of myocardial infarction, 12 for this trigger the longest period of control time was considered. Cochran method was used to consider significant differences between triggers in the four time periods including one hazard period and three control periods. GEE method with logistic function default was applied in order to determine exposure to triggers and study incidence relative odds of AMI. Triggers were measured based on patient's exposure or non-exposure to a trigger. The unit for hazard period was an hour, and that for the control period was the day, week or month.
Patients were selected through convenience sampling, and they were enrolled based on medical records contents including changes in the electrocardiogram, laboratory findings, clinical symptoms, and AMI diagnosis by a cardiologist. The patient with STEMI and NSTEMI included in this study and unstable angina pectoris (UAP) were removed. Sampling was conducted over a period of 5 months, from September to February 2015. Inclusion criteria included patients’ willing to participate in the interviews (having written informed consent), having appropriate consciousness, age over 18 years, and lack of memory disorder or psychosis. Data were collected using researcher-made questionnaire through the interview. Before data collection, a written informed consent was obtained from all patients. The questionnaire contained two parts: 1. demographic data and 2. triggers in four sections, and included 30 items, totally. The first part of the questionnaire contained 13 questions on demographic data such as gender, age, marital status, education, income, history of diabetes, hypertension, body mass index (BMI) based on the data recorded by the nurse on time of admission, cigarette smoking, alcohol and drugs abuse, drinking coffee or tea over three cups a day, and previous history of MI. The second part comprised of 17 questions to identify the acute triggers (emotional, environmental, physical, and chemical). This part was, in turn, divided into four sections. The first section contained the questions on identifying the emotional triggers including anger, insomnia, quarrel, hearing the sudden news, losing a job, the death of a loved one, excitement resulted from watching sports games and competitions and dramatic serials, and that exposure to these triggers was studied through calculating time interval. The second section composed of the questions on environmental triggers including long-term driving, exposure to traffic jam, witnessing a traffic accident or being involved in a driving accident, catching respiratory infections and exposure to hot or cold weather. The third section consisted of physical triggers including heavy and sexual activities, and the fourth section of the questionnaire included chemical triggers such as overeating, alcohol, and drugs abuse, and taking coffee or tea measures with a drunk cup of coffee or tea a day. The hazard and control period were evaluated for each trigger.
The questionnaire was given to 10 university faculty members to determine validity, and content validity index was obtained as 98.6%. Test-retest method was used for reliability. Since the answers to the questions were qualitative, kappa coefficient was used, and the consensus coefficient degree was determined as 1 indicating the patients’ agreement in measurement. In this study, five patients were reluctant to participate, and one patient was excluded due to misdiagnosis. The collected data were then encoded and were analyzed using SPSS version 21. Demographic data were reviewed using descriptive statistics methods (frequency, mean, and standard deviation). Cochran test was used to examine triggers’ significance in four time periods including one hazard period and three control periods, while GEE with logistics function default was applied to categorize triggers. Statistically, P < 0.05 was considered as significant.
This study was approved by the Ethics Committee of Guilan University of medical sciences with a code number of IR.GUMS.REC.1394.218.
In the case-crossover study, 269 patients with AMI were studied for six months. The results showed that 62.8% and 37.2% of patients were male and female, respectively. Most of the patients were in the sixth decade of life 31.6%, with the low education level (primary level) of 38.3%, and 43.1% were low-income with 200–400 US dollars income per month. According to Table 1 , 59.5% of patients had body mass index (BMI) above 25, and 43.9% had high blood pressure history and 36.4% suffered from diabetes.
Frequency of the underlying diseases history in the studied patients.
There was a statistically significant difference between hazard and control periods of triggers in anger, insomnia, hearing sudden news, loss of loved ones, watching sport games, respiratory infections, exposure to sudden hot or cold weather, physical and sexual activities, overeating and high-fat foods consumption, and drinking tea in four time periods ( Table 2 ). The most frequent emotional triggers were anger and insomnia, and the most common environmental, physical, and chemical triggers were respiratory tract infections, heavy activities, and drinking tea, respectively ( Table 2 ).
Triggers frequency and significance level of time periods.
Of emotional triggers, hearing the sudden news ( P = 0.001, CI = 1.35–3.53), and quarrel ( P = 0.008, CI = 1.19–3.38) were associated with a twofold increased odds of AMI, while the loss of loved one was related to very little odds (OR = 0.27, P = 0.02, CI = 0.08–0.84). Among the environmental triggers, sudden exposure to hot or cold weather was associated with significantly increased odds of AMI. Respiratory infections increased the odds of AMI during the hazard period with OR = 6.7 ( P = 0.0001, CI = 3.94–11.65), and sudden exposure to hot or cold weather was related to a raised odds of AMI with OR = 2.19 ( P = 0.005, CI = 1.27–3.77). Of physical triggers, both heavy and sexual activities increased the odds of AMI. Heavy activities were associated with an increased odds of AMI with OR = 1.6 ( P = 0.005, Cl = 1.16–2.37), and sexual activities increased the odds of AMI with OR = 2.3 ( P = 0.003, CI = 1.33–4.19). Among the chemical triggers, overeating and high-fat foods consumption can heighten the odds of AMI with OR = 3.7 ( P = 0.0001, CI = 2.41–5.96) ( Table 3 ).
Types of triggers and each trigger’s odds ratio for acute myocardial infarction (AMI)
4. Discussion
This study was conducted to identify acute triggers of AMI, to prevent heart attack, and to increase awareness about MI in people at risk. The results of this study showed that emotional triggers: quarrel and hearing sudden news were associated with significantly twofold increased odds of AMI. In a study conducted by Masoumi, it was shown that hearing bad news caused a 6.9-fold rise in odds of AMI; hence, the current study is consistent with Masoumi one. Also, a quarrel in the study was related to twofold increased odds of AMI. Furthermore, Colombo stated that quarrel at work or home can increase the odds of AMI. 4 Here, acute psychological stress mechanism is a common factor. Despite a higher frequency of occurrence of anger and insomnia, they were not the predictive factors for AMI. Mostofsky and Penner reported that anger trigger was associated with 2.3-fold increased odds of AMI. 23 Bulkey indicated that anger trigger was related to 8.5-fold increased relative risk rate of AMI. 24 The results of this study contradict those of Mostofsky and Bulkey in the case of anger trigger. It seems that due to the lack of categories in the study and different interpretations of anger in various cultures, the contradiction emerges. Anger in Bulkey’s study was divided into seven degrees, and anger with more than five degrees increased odds of AMI, while the only measure was the presence of anger trigger in this study. In a study performed by Clark, insomnia was associated with 1.69-fold increased odds of AMI, 25 which is incompatible with that in our study. The discrepancy could be due to differences in individual interpretation of insomnia. Also, the patient may not have enough accuracy to report insomnia period. In the case of loss of loved one, relative odds of AMI was low and had a conflict with Mostofsky 12 and Carey studies. 26 The discrepancy could be due to very limited exposure to the above-mentioned trigger and short-term hazard period in this study. In Carey and Mostofsky studies, the hazard period was considered as by one month, while this period was 24 h before the onset of AMI. In the case of losing a job and watching sports games, the results cannot be generalized due to very limited exposure.
Of environmental triggers, respiratory infections and exposure to hot and cold weather increased odds of AMI. The study found that respiratory infections were associated with 6.78-fold raised odds of AMI. Warren-Gash et al. reported that 1–3 days following respiratory infections onset caused 4.19-fold increased odd of AMI. 27 Corrales et al. showed that pneumonia was associated with fourfold raised odds of AMI. 15 , 28 Also, Colombo et al. noted that respiratory infections were related to 2.7-fold increased odds of AMI. 4 In the conducted study, exposure to hot and cold weather was among the most important environmental trigger of developing AMI that was associated with 2.19-fold heightened odds of AMI. In a study done by Masoumi, it was expressed that exposure to cold weather was not AMI predictor 14 ; it seems that difference in results is because of dissimilar weather conditions in Kerman and Guilan. Behaskaran in a study showed that temperatures above 20 °C can be associated with twofold increased odds of AMI. 29 In this study, the daily temperature was not recorded, and results of summer, autumn, and winter were studied; therefore, they cannot be generalized. Of physical triggers, both physical and sexual activities were AMI triggers and increased its odds. Sexual and heavy activities were related to 2.36- and 1.66-fold raised odds of MI, respectively. Masoumi et al. reported that sexual activities were associated with 3.4-fold heightened odds of AMI. 14 Also, Colombo showed that physical activities were related to 4.3-fold increased odds of MI. 4
The most common chemical triggers for AMI were eating high-fat foods and overeating. In this study, overeating was associated with 3.7-fold increased odds of MI. Mitelman and Colombo introduced overeating as MI trigger, and Colombo indicated that overeating was related to sevenfold raised odds of MI. 4 , 8 There was no significant difference between tea, alcohol, and opium consumption among participants. Thus, these factors could not be AMI predictors. Mitelman and Mostofsky stated that alcohol abuse was associated with 2.3-fold heightened odds of ischemic stroke, but it has no effect on the incidence of MI, and this result is consistent with that of our study. 30 Moreover, Mitelman and Mostofsky showed that cocaine and marijuana abuse was related to 23.7- and 4.8-fold increased odds of MI, respectively. 8 There is a contradiction between the results of this study and those of Mostofsky one in terms of drug abuse and AMI trigger. This inconsistency derives from a common drug that is opium in our society, while Mostofsky worked on cocaine and marijuana having a different mechanism. Despite tea high consumption, no relationship between tea drinking and the incidence of AMI was observed. Likewise, no similar study showed a relationship between tea consumption and AMI incidence. Bylin et al. found that coffee drinking is an AMI trigger. 18 The results of our study were different from Bylin ones, which may be due to the difference in the type of beverage and the dissimilarity in the caffeine level in tea and coffee. Also, Nikpazhoh noted that there is no clear relationship between taking caffeine and heart diseases, and it appears that moderate consumption of coffee is not harmful to the heart. For some people having a particular sensitivity to caffeine, a physician may recommend that they avoid drinking coffee. 31
5. Conclusion
This study showed that quarrel and hearing sudden news are among the most important triggers of AMI. It is essential that people at risk avoid exposure to stressful situations, and relaxation techniques to be taught to them. The study found that in addition to doing heavy activities, inactivity is an AMI trigger. Therefore, adjustments in daily activities and doing regular exercise are recommended to society’s people. Furthermore, to avoid overeating, to treat respiratory infections at the proper time, and to reduce exposure to sudden hot or cold weather are recommended to prevent triggers’ effects.
Conflict of interest
The authors declare they have no conflict of interest in the research domain.
Acknowledgment
The authors express gratitude to the research and technology of Guilan University of Medical Sciences, and officials and staff of Dr. Heshmat educational and remedial center and Rasool-e-Akram hospital in Rasht, who contributed cooperatively in this research, as well as all patients participating in the study for their collaboration in the research project.
☆ Funding Source : The study is supported financially by Guilan University of Medical Sciences.
Peer review under responsibility of Egyptian Society of Cardiology.
EMPACT-MI Results: Empagliflozin After Acute MI
Apr 09, 2024 | Alison Bailey, MD, FACC ; Javed Butler, MBBS, FACC ; Sun Moon Kim, MD, FACC
Patients with acute myocardial infarction are at a high risk of heart failure and death. Despite advances in care and reduction in the rate of recurrent myocardial infarctions, the risk for heart failure continues to be unacceptably high. No intervention in 2 decades has been shown to improve this risk.
In this interview, Javed Butler, MD, MPH, MBA , and Sun Moon Kim, MD, FACC , discuss the results of the EMPACT-MI trial.
Related References:
- Harrington, J., Udell, J. A., Jones, W. S., Anker, S. D., Bhatt, D. L., Petrie, M. C., Andersen, K. R., Sumin, M., Zwiener, I., Hernandez, A. F., & Butler, J. (2023). Baseline characteristics of patients enrolled in the EMPACT-MI trial. European journal of heart failure, 25(9), 1708–1715. https://doi.org/10.1002/ejhf.2990
- Harrington, J., Udell, J. A., Jones, W. S., Anker, S. D., Bhatt, D. L., Petrie, M. C., Vedin, O., Sumin, M., Zwiener, I., Hernandez, A. F., & Butler, J. (2022). Empagliflozin in patients post myocardial infarction rationale and design of the EMPACT-MI trial. American heart journal, 253, 86–98. https://doi.org/10.1016/j.ahj.2022.05.010
Your browser doesn't support HTML5 audio. Here is a link to the audio instead.
Clinical Topics: Heart Failure and Cardiomyopathies, Acute Heart Failure, Invasive Cardiovascular Angiography and Intervention
Keywords: ACCELLite, Heart Failure, Myocardial Infarction, ACC Annual Scientific Session, ACC24
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Diversity and Inclusion
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
Latest in Cardiology
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
Education and Meetings
- Online Learning Catalog
- Understanding MOC
- Products and Resources
- Image and Slide Gallery
- Certificates and Certifications
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- CardioSmart
- Accreditation Services
- Clinical Solutions
- Clinician Well-Being Portal
- Mobile and Web Apps
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms

- Advanced Search
- See Studies by Topic
- See Studies on Map
- How to Search
- How to Use Search Results
- How to Find Results of Studies
- How to Read a Study Record

- Learn About Studies
- Other Sites About Studies
- Glossary of Common Site Terms

- Submit Studies to ClinicalTrials.gov PRS
- Why Should I Register and Submit Results?
- FDAAA 801 and the Final Rule
- How to Apply for a PRS Account
- How to Register Your Study
- How to Edit Your Study Record
- How to Submit Your Results
- Frequently Asked Questions
- Support Materials
- Training Materials

- Selected Publications
- Clinical Alerts and Advisories
- Trends, Charts, and Maps
- Downloading Content for Analysis

- ClinicalTrials.gov Background
- About the Results Database
- History, Policies, and Laws
- ClinicalTrials.gov Modernization
- Media/Press Resources
- Linking to This Site
- Terms and Conditions
- Search Results
- Study Record Detail

MiSaver® Stem Cell Treatment for Acute Myocardial Infarction (MiSaver®)
- Study Details
- Tabular View
- No Results Posted

Despite advancements in treatments, cardiovascular diseases, especially acute myocardial infarction (AMI), remain significant health concerns. This study hypothesized that stem cells could improve left ventricular function post-AMI. An open-label trial was initiated to assess the safety and feasibility of intravenous infusion of ABO blood group-matched allogeneic umbilical cord blood stem cells (USC) prefabricated into MiSaver (Myocardial Infarction Saver) in AMI patients.
Primary Endpoint:
The primary endpoint focused on safety and adverse events over a 12-month observational period. Results showed the treatment was well-tolerated with no AEs attributed to the study product.
Secondary Outcomes:
Secondary outcomes evaluated changes in left ventricular ejection fraction (LVEF) from baseline to 12 months post-treatment. A retrospective study compared eligible controls with low and middle dosage groups.
Cardiovascular diseases, particularly acute myocardial infarction (AMI), persist as significant health concerns despite advancements in pharmaceutical and interventional treatments. Herein,investigators hypothesized stem cells could enhance left ventricular functional outcomes in patients recently afflicted by acute myocardial infarction (AMI). To investigate this hypothesis, investigators initiated an open-label, dose-escalating trial to evaluate the safety and feasibility of intravenous infusion of ABO matched allogeneic umbilical cord blood stem cells (USC), prefabricated into our study product MiSaver (Myocardial Infarction Functional Saver), in patients following recent AMI. Participants were enrolled in cohorts of five, each receiving low or middle dosages (0.5x10^7 and 1.6x10^7 cells/kg, respectively), with infusions administered 2-5 days post-AMI onset.
(Study details for low and middle dose please see study NCT04050163)
Retrospective participants meeting similar inclusion criteria of recent AMI and LVEF < 45% were identified from the study site. Twenty eligible participants were selected as controls and compared for analysis with the low and middle dosage groups.

Inclusion Criteria:
- Patients aged between 20 and 80 years
- Diagnosed with AMI within 7 days
- Elevated cardiac enzymes (Creatine Kinase-MB or troponin) greater than 2 times the upper limit of normal
- Presence of regional wall motion abnormality
- LVEF ≤ 45% on echocardiography
- Hemodynamically stable
- Not requiring inotropic support
- Systolic blood pressure below 80mm Hg for less than 1 hour
- Resting heart rate above 100 beats/min for less than 1 hour in the past 24 hours
- Peripheral artery oxygen saturation of ≥97%
Exclusion Criteria:
- Pregnancy or breastfeeding
- Positive adventitious infections (such as HIV, hepatitis)
- Need for coronary artery bypass surgery or anticipated further revascularization procedures during the 6-month study period
- Severe aortic or mitral valve narrowing
- Evidence of life-threatening arrhythmia on baseline electrocardiogram (ECG)
- Inability to receive PCI examination or treatment (including New York Heart Association (NYHA) Fc.IV) due to shortness of breath
- Malignant tumor
- Hematopoietic dysplasia
- Other severe organ disease
- Less than 1 year of life expectancy
- Chronic kidney disease with estimated Glomerular Filtration Rate (eGFR)<20 and/or on renal dialysis
- For Patients and Families
- For Researchers
- For Study Record Managers
- Customer Support
- Accessibility
- Viewers and Players
- Freedom of Information Act
- HHS Vulnerability Disclosure
- U.S. National Library of Medicine
- U.S. National Institutes of Health
- U.S. Department of Health and Human Services

IMAGES
VIDEO
COMMENTS
This is an educational case report including multiple choice questions and their answers. ... 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. the ISIS-2 (second international study of infarct survival) collaborative group ...
Case 4/2014 - A 66-Year-Old Man with Acute Myocardial Infarction and Death in Asystole after Primary Coronary Angioplasty ... acute myocardial infarction involving the left ventricular anterosseptal wall and the right ventricular anterior ... Sudden death risk in overt coronary heart disease: the Framingham Study. Am Heart J. 1987; 113 (3):799 ...
A Case Report: Acute Myocardial Infarction in a 29-year-old Male. 2/5/2019 Aaron Tiffee, MD, FACEP , Zariad Saran, DO , Tyler Ingersoll, MS. The HEART score is a go-to tool in assessing the risk of an acute coronary syndrome. But in this case, a score of 3 did not mean the 29-year-old patient was safe. Cardiovascular disease (CVD) is currently ...
Acute myocardial infarction complicated by cardiogenic shock is defined by a systolic blood pressure of less than 90 mm Hg, end-organ hypoperfusion, and a cardiac index of less than 2.2 liters per ...
Key Points. Question How have case rates, treatment approaches, and in-hospital outcomes changed for patients with acute myocardial infarction (AMI) during the coronavirus disease 2019 (COVID-19) pandemic?. Findings In this cross-sectional study of 15 244 hospitalizations involving 14 724 patients with AMI, case rates began to decrease on February 23, 2020, followed by a modest recovery after ...
A 67-year-old woman sought emergency medical care due to prolonged chest pain. In April 2009 the patient had prolonged chest pain and at that time she sought medical care. She was admitted at the hospital and diagnosed with myocardial infarction. The patient had hypertension, diabetes mellitus, dyslipidemia and was a smoker.
Introduction. Myocardial infarction in the absence of obstructive (>50% stenosis) coronary artery disease (MINOCA) is found in approximately 6% of all patients with acute myocardial infarction (MI) who are referred for coronary angiography. 1, 2 The term MINOCA should be reserved for patients in whom there is an ischaemic basis for their clinical presentation and should be considered a ...
Owing to recent advances in early reperfusion strategies, pharmacological therapy, standardized care, and the identification of vulnerable patient subsets, the prognosis of acute myocardial infarction has improved. However, there is still considerable room for improvement. This review article summarizes the latest evidence concerning clinical diagnosis and treatment of acute myocardial infarction.
Individuals (regardless of COVID-19 status) who had had an acute myocardial infarction previously were excluded from this analysis. The results of the matched cohort study for acute myocardial infarction excluding day 0 are shown in table 2, and including day 0 are shown in the appendix (p 7). The overall number of patients with missing ...
Cardiovascular events frequently recur after acute myocardial infarction, and low cholesterol efflux — a process mediated by apolipoprotein A1, which is the main protein in high-density ...
Acute myocardial infarction (AMI) is one of the most preventable non-communicable diseases in human. Identifying triggers of myocardial infarction (MI) and prevention ways of exposure-induced complications can reduce morbidity and mortality in people at risk. ... This case-crossover study was conducted on 269 patients with AMI, hospitalized at ...
This case study aims to explain and illustrate how to care for patients with acute myocardial. infarction based on the rationale and nursing practice evidence underlying the holistic approach ...
The incidence of acute myocardial infarction was elevated regardless of influenza vaccination status or history of admission for acute myocardial infarction before the study period . Table 3 Subgroup
Objective: Acute myocardial infarction (AMI) is the leading cause of death and disability globally. There is increasing evidence from observational studies that influenza infection is associated with AMI. In patients with known coronary disease, influenza vaccination is associated with a lower risk of cardiovascular events.
Acute myocardial infarction (AMI) is a life-threatening condition that requires prompt diagnosis and treatment. This book chapter provides a comprehensive overview of the causes, types, diagnosis, management, and complications of AMI, based on the latest evidence and guidelines. Learn from the experts how to optimize the care and outcomes of patients with AMI.
Nursing Assessment. One of the most important aspects of care of the patient with MI is the assessment. Assess for chest pain not relieved by rest or medications. Monitor vital signs, especially the blood pressure and pulse rate. Assess for presence of shortness of breath, dyspnea, tachypnea, and crackles.
Understanding the risk factors associated with myocardial infarction is vital for prevention and early detection. This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental ...
Metabolic Syndrome and Risk of Acute Myocardial Infarction: A Case-Control Study of 26,903 Subjects From 52 Countries. ... The INTERHEART study is a standardized case-control study of incident acute MI in 52 countries. Study participants consisted of 12,297 cases and 14,606 controls recruited from 262 centers in Asia, Europe, the Middle East ...
The objectives of INTER-HEART are to determine the association between risk factors and AMI within populations defined by ethnicity and/or geographic region and to assess the relative importance of risk factors across these populations. Methods: INTER-HEART is a study of 14,000 cases of AMI and 16,000 matched control patients from 46 countries ...
Acute Myocardial Infarction Case Study. Myocardial infarction (heart attack) is the leading cause of death in the United States. It is estimated that one in every five deaths in the US is due to a heart attack. Approximately one million patients are admitted to hospitals each year due to heart attacks. 200,000 to 300,000 individuals die from ...
Background: Acute myocardial infarction (AMI) is one of the most preventable non-communicable diseases in human. Identifying triggers of myocardial infarction (MI) and prevention ways of exposure-induced complications can reduce morbidity and mortality in people at risk. ... Methods: This case-crossover study was conducted on 269 patients with ...
Acute myocardial infarction (AMI) is one of the most preventable non-communicable diseases in human. Identifying triggers of myocardial infarction (MI) and prevention ways of exposure-induced complications can reduce morbidity and mortality in people at risk. ... This case-crossover study was conducted on 269 patients with AMI, hospitalized at ...
A. Patients with acute myocardial infarction are at a high risk of heart failure and death. Despite advances in care and reduction in the rate of recurrent myocardial infarctions, the risk for heart failure continues to be unacceptably high. No intervention in 2 decades has been shown to improve this risk. In this interview, Javed Butler, MD ...
Study Description. Despite advancements in treatments, cardiovascular diseases, especially acute myocardial infarction (AMI), remain significant health concerns. This study hypothesized that stem cells could improve left ventricular function post-AMI. An open-label trial was initiated to assess the safety and feasibility of intravenous infusion ...
Acute Myocardial Infarction - Page 3 Case continued: Enroute to the ER, the patient's acute symptoms had been relieved by the prompt action of the emergency care personnel. Vital signs had stabilized, his chest pain was relieved by nitroglycerin, and breathing was made easier by the increased oxygen flow.
assessment process. This case study aims to explain and illustrate how to care for patients with acute myocardial infarction based on the rationale and nursing practice evidence underlying the holistic approach. Nurses have been shown to have an essential role in the diagnosis, management, and treatment of acute coronary syndromes.
Background: Acute myocardial infarction is often accompanied by malnutrition, which is associated with an imbalance between catabolic and anabolic processes. This ultimately leads to cardiac cachexia, which worsens the patient's prognosis. We aimed to assess the correlation between nutritional status, assessed using the controlling nutritional status (CONUT) score, and the rate of major ...