- Faculty of Arts and Sciences
- FAS Theses and Dissertations
- Communities & Collections
- By Issue Date
- FAS Department
- Quick submit
- Waiver Generator
- DASH Stories
- Accessibility
- COVID-related Research

Terms of Use
- Privacy Policy
- By Collections
- By Departments
Improving Reproductive Health: Assessing Determinants and Measuring Policy Impacts
Citable link to this page
Collections.
- FAS Theses and Dissertations [6136]
Contact administrator regarding this item (to report mistakes or request changes)
Health Dimensions of COVID-19 in India and Beyond pp 203–217 Cite as
Sexual and Reproductive Health of Adolescents and Young People in India: The Missing Links During and Beyond a Pandemic
- Sapna Kedia 3 ,
- Ravi Verma 3 &
- Purnima Mane 4
- Open Access
- First Online: 09 April 2022
4233 Accesses
1 Citations
7 Altmetric
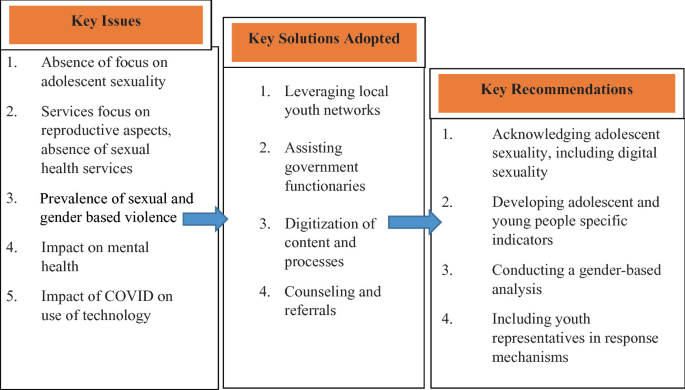
The authors discuss the impact of the pandemic on the sexual and reproductive health of adolescents and young people. Adolescents and young adults (AYA) are at low risk from COVID- 19, and hence, it may be assumed that their needs do not warrant immediate attention. However, it is important to understand how the pandemic may have affected their lives. Evidence from previous humanitarian disasters in India and elsewhere suggests that consequences for adolescents and young adults may be significant and multi-dimensional. The authors examine the impact (short- and long-term) of COVID on the sexual and reproductive needs and behaviors of AYA in India, particularly their intimate relationships, sexual violence, access to services, and impact on their mental health.
Programs for AYA should be responsive to their needs, feelings, and experiences and should treat them with the respect they deserve, acknowledging their potential to be part of the solution, so that their life conditions improve and the adverse impact of the pandemic is minimized. Programs must also address the needs of vulnerable AYA like migrants, those from the lesbian, gay, bisexual, transgender, and queer (LGBTQ) community, persons with special needs, HIV positive youth, and those who live in poverty. It is important to understand how gender impacts the sexual and reproductive health of AYA, particularly young girls and women, in terms of restriction of mobility, increase dependence on male partners/friends/relatives, gender-based violence, control of sexuality, and the lack of privacy and confidentiality. The responses to these needs by youth-based and youth-serving organizations and the government are summarized. Recommendations are made to address prevailing gaps from a sexual and reproductive health rights and justice perspective.
You have full access to this open access chapter, Download chapter PDF
Introduction
The COVID-19 pandemic has by now affected the entire world. It has highlighted the existing gaps in equitable development and re-emphasized, in a manner that we could not imagine, the need to assess our privileges—in terms of access to education, health, housing, food security, transportation, and how we treat the environment. The stay at home and isolation requirements have impacted our basic human needs of connection, relationships, physical proximity, and intimacy. Over the last eight months, a lot has been said and written about the impact of the pandemic on our lives. COVID’s impact, however, varies depending upon one’s socioeconomic position. This is crucial to note because the effect of COVID on the most vulnerable sections of society and those whose human rights are least protected is likely to be more adverse and unique.
This chapter focuses on the impact of the pandemic on adolescents and young adults (AYA) aged 10–24, in India, with reference to their sexual and reproductive health (SRH). AYA are at low risk from COVID, and hence, their needs may not seem to warrant immediate attention. However, it is important to understand how the pandemic may have affected their lives. Evidence from previous humanitarian disasters in India and elsewhere suggests that consequences for adolescents and young adults may be significant and multi-dimensional [ 1 ].
A scan of the literature available on the impact of COVID on AYA in India presents a glaring gap of evidence on how the pandemic has affected their sexual and reproductive health (SRH). Most available evidence focuses on COVID’s impact on AYA’s education, overall health and well-being, access to livelihoods, loss of agency, and decision-making. Literature also shows COVID’s impact on AYA’s reproductive health. However, this is largely limited to disruption in services due to the lockdown imposed in India on March 24, 2020, which continued for months in different forms [ 2 ].
There is a noticeable silence around sexual health of AYA during the pandemic. This is an extension of course, of the silence prevalent pre-COVID. During pre-COVID times too, access to SRH information and services for adolescents, especially unmarried adolescents in India, has always been socially stigmatized and scrutinized, resulting in limited availability and accessibility of services for sexual and reproductive health and rights (SRHR) [ 3 ]. The reasons for this silence are known—the lack of acknowledgment of AYA as sexual beings, the stigma around adolescent sexuality and pre-marital sex, particularly in relation to unmarried adolescent girls, and the association of reproductive health with marriage and child birth [ 4 ]. Not surprisingly then, there is a lack of global estimates of the pandemic’s effect on AYA’s SRH outcomes due to the non-availability of meta-data on the SRH needs of the young, unmarried population, an invisibility largely due to stigma around pre-marital sexual activity. In India, the absence of SRH services from ‘essential’ health services during COVID amplifies this undocumented need [ 3 ].
While the immediate effects of the pandemic on AYA’s lives are visible in terms of impact on education, mobility, employment, and leisure, the pandemic’s other possible impacts on AYA’s SRH will gradually be understood. The pandemic may have medium- and long- term impacts on AYA’s basic rights and agency in terms of their health and safety [ 5 ]. It is important to note that the pandemic has put a break on many of the normative aspects of AYA’s development, a period ideally marked by increased independence and peer bonding [ 6 ]. This may affect the development trajectory of AYA.
Some AYA may have been forced to enter early marriages due to the pandemic; some may have had unintended pregnancies and difficulties in accessing abortions, and some may have experienced sexual violence during this period. In addition, adolescence is also a period marked by sexual awakening within the context of lack of knowledge and guidance on sexual matters from reliable sources, which is likely to be even more limited during the pandemic. It is thus important to understand the pandemic’s impact on the SRH of AYA so that timely and adequate responses may be developed and to ensure that a crucial aspect of their lives is not overlooked (Fig. 10.1 ).
Framework to understand the impact of COVID on adolescent and young adult’s sexual and reproductive health and rights
According to the current working definition, sexual health is
…a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination, and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected, and fulfilled [ 7 ].
Reproductive health (RH) implies that people are able to have a responsible, satisfying, and safe sex life and that they have the capability to have children and the freedom to decide if, when and how often to do so [ 8 ].
From the above perspective, sexual and reproductive health are key factors in shaping AYA’s physical and mental well-being, factors that are often overlooked in the context of a country like India. This chapter seeks to examine the impact (short- and long- term) of COVID on the SRH needs and behaviors of AYA, based on available evidence. The chapter also highlights crucial gaps in the existing evidence and builds a case for addressing them. The authors adopt the following framework in their analysis of COVID and its impact on adolescent and young adults SRHR.
Adolescents and Young People in India
As per the Census of India 2011, every fifth person in India is an adolescent (10–19 years) and every third, a young person (10–24 years). Adolescents constituted 21.7% of the total rural population and 19.2% of the total urban population in the Census in 2011. The youth population constituted about 18.9% of the total rural population and 19.7% of the population in urban areas. For the country as a whole, the percentage of male adolescents and youth is slightly higher than their female counterparts in both rural and urban areas. In 2011, the sex ratio among the adolescent population in rural areas was 901 and in urban areas was 892. In the case of the youth, the sex ratio in rural areas was 901 and in the urban areas was 910. Recently released data from the National Family Health Survey (NFHS)-5 (2019–2020) highlights that low sex ratio continues to be a major challenge in most Indian states. NFHS-5 also highlights the gender differentials across several indicators [ 9 ]. For example, the proportion of adolescent girls (15–19) who became pregnant before age 18 ranges between 10 and 15% with wide rural/urban and interstate variation. Similarly, the experience of gender-based violence (GBV) by youth (18–29) is about 4% with minor rural/urban variation. Anemia continues to be alarming among adolescents and young adult girls in comparison with their male counterparts. Child marriage rates are still high to the tune of almost 30% in some states with large interstate and rural/urban differentials.
AYA is not an homogenous group. AYA’s needs vary with their age, sex, stage of development, and life circumstances—in terms of access to quality education, life skills development, place of residence (rural/urban), opportunities for collective learning and sharing, and the socioeconomic conditions of their environment .
As per the United Nations Population Fund (UNFPA), AYA in India face several development challenges, including access to quality education, gainful employment, gender inequality, child marriage, absence of youth-friendly health services, and adolescent pregnancy. These challenges have been exacerbated due to COVID [ 10 ].
A few studies, conducted during the lockdown in India, have assessed the impact of COVID on adolescents and young people in India. The Population Foundation of India (PFI) conducted a rapid assessment of the impact of COVID-19 on youth in Bihar, Rajasthan, and Uttar Pradesh [ 11 ]. Quilt Al conducted a study on the impact of COVID on adolescent reproductive health, the DASRA Adolescent Collaborative collected experiences of civil society organizations working with adolescents, and the YP Foundation reached out to its adolescent and youth network spread across 25 states and six union territories of the country, to understand the impact of the pandemic on young lives [ 1 , 12 , 13 ]. Findings from these studies are representative of diverse communities of adolescents and young adults including informal laborers, gender and sexual minorities, young people belonging to different castes and tribal affiliations, sex workers, people living with HIV (PLHIV), substance users, and young people living in shelters and correctional homes.
These studies have highlighted the impact of COVID on AYA’s education, access to health services including sanitary pads, iron and folic acid (IFA) tablets, contraception, abortion services, nutrition, skilling and employment assistance, and mental health services. They also provide information on how the pandemic has impacted AYA of different genders. This chapter will present the sexual and reproductive health-related findings and recommendations from these studies and will highlight data gaps that need to be addressed.
Impact of COVID on AYA’s Sexual Relationships
COVID has resulted in restrictions on freedom, mobility, and socialization worldwide. This has created increased isolation. AYA have experienced increased restrictions on mobility, recreational activities, and access to support networks due to closure of schools, colleges, non-formal learning opportunities, and workplaces [ 1 ]. This has resulted in limited social engagement with their peers, guides, and mentors and in increased anxiety and loneliness [ 13 ].
Increased family time, especially in cases where AYA have been living away from home for some years, has led to greater surveillance from adults, lack of privacy, and increased likelihood of sexual abuse by family members. Personal and financial agency of adolescents and young people, especially the most vulnerable—unmarried young women, queer and trans youth, young migrants, young refugees, homeless young people, those in detention, and young people living in crowded areas such as townships or informal settlements—has been severely impeded. In a country like India where extensive parental authority is exercised over adolescents and young adults especially in the case of the unmarried, way into adulthood, one can only imagine the increase in the extent of control parents would exercise during COVID.
As said earlier, since AYA are a low-risk group for COVID, their needs are the least prioritized. It has been almost taken for granted that they would have unlimited ability to adapt to online classes, to engage in hobbies and activities to keep themselves busy, to engage with friends online and in general to stay out of adults’ way, and behave as the adults would want them to.
In all the literature around AYA in the pandemic, there is hardly any reference to or discussion of how the pandemic may have affected the romantic and sexual lives of AYA. As we already know, in India, in general there is very limited to no conversation around AYA’s romantic and sexual relationships and their sexual health. Therefore, one cannot expect anything different during the pandemic, especially when COVID-related health concerns are the only ones getting priority attention. As per DASRA [ 1 ], organizations working with AYA have often struggled with obtaining information about this aspect of AYA’s lives, and the constraints on meeting privately and in groups have further increased the challenge during the pandemic.
How are AYA engaging in intimate relationships during this time? How has the pandemic affected pre-marital sex, an open secret in India? Are AYA engaging in safe sex practices, keeping COVID precautions in mind? Who is providing them with this information and from where are they accessing it? Is sexual abuse a problem AYA are facing? These questions, particularly among unmarried AYA, are important but remain unanswered.
In the case of married AYA, there is evidence to show that some young married men are coercing their partners for sex, simply because the men are bored at home. The International Center for Research on Women (ICRW) and Vihara Innovation Fund’s rapid qualitative study to understand the impact of COVID on the family planning needs of women and men in Uttar Pradesh (UP) and Bihar showed that for some male respondents, sex was a way of releasing their stress and a distraction from their ongoing economic crisis. Female respondents of the study reported being frustrated because of the constant demands of sex by their husbands [ 14 ]. Cases of coercive sex and domestic violence might also be increasing as a result of this situation, but systematic attention has not been paid to explore this issue.
Added to these issues is the rise of digital connections in the context of sex. As per Quilt AI, in India, COVID will catalyze the digital revolution as the base of Internet users is expected to increase from 574 to 639 million by the end of 2020. Quilt AI’s study shows that more and more AYA have been spending time online, especially during the pandemic [ 12 ]. How are AYA accessing online spaces for personal connections? What about practices like online dating, sexting, virtual sex, and the associated safety-related issues? Quilt AI undertook a study to examine the impact of COVID on digital engagement on issues related to sexual and reproductive health (SRH), imparting skills to girls, and their employment. The study showed that there was an increase in searches for violent porn in towns/districts from February 2020. However, there was a gradual decline in cities. This is an important pointer toward AYA sexual behavior during the pandemic, particularly the use of online platforms for accessing porn that is violent in nature. This distinction between an increase in towns/districts and a decline in cities needs to be examined further in terms of the reasons and impact on AYA and their relationships.
It is important to recognize that the pandemic is likely to have impacted the relationships and sex lives of AYA about which little is known nor is it considered in policies and programs. Keeping in mind the social situations that might arise due to this pandemic, Banerjee and Rao explain that the probable impacts may be sexual abstinence, coercive sexual practices, non-compliance to precautions, disinterest in sex, unhealthy use of technology, interpersonal problems, rise in sexual disorders, and high-risk sexual behaviors [ 15 ]. This in turn may have impacted the already vulnerable gender dynamics, attitudes, and behaviors of AYA and their partners who may or may not be adolescents or young adults.
COVID and the Rise in Partner Violence
During COVID, adolescents and young adults, especially girls and women, may experience higher levels of violence, given the isolation and requirement to stay at home. In pre-COVID times, this population group tended to face high levels of domestic and intimate partner violence [ 1 ].
Globally, there has been increasing evidence of rising domestic violence since the lockdown, especially among women and young girls [ 16 ]. In India, it has been reported that calls seeking support against violence have been increasing since the lockdown [ 17 ]. The DASRA Adolescent Collaborative report on experiences of civil society organizations working with AYA highlights that many young people witnessed and experienced violence during the lockdown. This includes physical and sexual violence perpetrated by parents, siblings, boyfriends, and/or husbands [ 1 ]. Organizations reported to DASRA that they had been approached more often by girls in comparison with boys to report instances of physical and sexual violence [ 1 ].
Several organizations reported that many girls and young women they work with shared that their husband or boyfriend had forced them to have sex. International Council for Research on Women (ICRW) and Vihara’s study on family planning during COVID also highlighted instances of forced sex between young married couples. In studies by DASRA and YP Foundation, AYA reported that they feel unsafe at home, indicating that they may be living with their abusers. Organizations also reported continued trafficking of girls and boys during the pandemic, and in some areas, organizations reported an increase in the number of trafficking cases.
Further, limited information is available on the violence that AYA with lesbian, gay, bisexual, transgender, queer, intersex, and asexual (LGBTQIA) identities may be facing. The YP Foundation highlights that LGBTQA are at increased risk of gender dysphoria, and physical and psychological violence, which is likely to be further heightened during the pandemic. A few media reports have highlighted that there has been increased discrimination against sexual minorities during the pandemic, but it is likely to be hidden in the context of India where sexual minorities are discriminated against.
As mentioned previously, AYA have been spending more time online during the lockdown. Organizations reported that more incidents of cyber bullying and use of social media to spread morphed pictures and rumors especially about girls had come to their notice. The now infamous Boys Locker Room incident from a private school in Gurgaon, Haryana, India, where male classmates created an Instagram group and were casually discussing sexual violence and rape threats against their female classmates, is one such example.
The increase in sexual and gender-based violence emphasizes the need for information and support services, response mechanisms, and access to emergency contraception and other reproductive health services. It also emphasizes the need to study the causes and impact of these increasing instances because these affect AYAs’ interpersonal relationships, gender norms among them, sexual practices, and overall mental well-being in the short as well as in the long term. Going further, this highlights the importance of finding ways to address these problems during the pandemic and ensuring that the policy and program actions have an impact post-COVID as well.
Access to Sexual and Reproductive Health Services: Growing Gap for AYA During COVID
Global media reports and research studies have highlighted that routine reproductive health services and access to supplies have been interrupted due to COVID. The majority of public health facilities in India have been converted into COVID treatment centers or have shifted their focus to managing COVID care [ 11 ]. Further, smaller clinics including private ones have been shut or have found it challenging to ensure that related precautions are in place. Diversion of infrastructure, personnel, and financial resources to COVID-related care has resulted in a shortage of supplies and other challenges in delivering health services, including reproductive health care, which was already facing challenges [ 11 ]. This has resulted in extreme difficulties, particularly for women and girls, in accessing reproductive health services, especially in the rural areas of India where they are mostly dependent on the public health system [ 18 ]. Furthermore, it has rendered any form of sexual health services, already more inaccessible than reproductive health services, more remote for young people.
Given the current situation, health services for adolescents and young adults have been generally compromised. While government guidelines specify the need to provide adolescents counseling and services through the adolescent-friendly clinics established under the Rashtriya Kishore Swasthya Karyakram (RKSK) scheme, these clinics have largely been non-operational during COVID. It is particularly troubling that even in pre-COVID times, adolescents reported that they found it difficult to access these clinics [ 13 , 19 ].
In its study, DASRA explored the extent to which youth organizations faced challenges in accessing reproductive health and other healthcare services for the young. Findings from its report suggest that many youth-based organizations received feedback from young people about difficulties in accessing a range of services. Organizations reported that girls and boys had not received regular supplies of weekly iron and folic acid (IFA) tablets since the lockdown was imposed because these were dependent on schools and community health workers. Community health workers like accredited social health activists (ASHAs), anganwadi workers (AWWs), and auxiliary nurse midwives (ANMs) also confirmed this in the dialogue series organized by Women in Global Health India to amplify the voices of health workers during COVID between June–November 2020 [ 20 ].
A critical impact of COVID has been on access to sexual and reproductive health commodities and services for young people. Services like access to sanitary napkins, routine SRHR checkups, access to contraceptives, abortion services, and pregnancy-related care for adolescents and young adults were challenging even in pre-COVID times, given India’s cultural context and denial of AYA’s sexuality. During the COVID pandemic, several youth-based organizations reported that these challenges have increased [ 1 , 13 ].
Though young girls reported chronic shortages of sanitary napkins, their difficulties in accessing the napkins increased significantly during the lockdown. As per DASRA and YP Foundation, sexually experienced young people expressed difficulty in accessing contraceptive supplies. This may result in unintended pregnancies. Here it is important to note that there is underreporting among sexually experienced young people of unintended pregnancies. Most unmarried sexual relationships are clandestine given the social taboos and stigma associated with pre-marital sex [ 4 ]. Organizations also reported to DASRA and YP Foundation that pregnant girls had trouble in accessing ante-natal, delivery, and post-natal care when the lockdown was imposed. Some women and girls were compelled to deliver at home.
Furthermore, access to abortion services was severely impacted in general. ICRW’s study in 2018 on Male Engagement in Pre-marital Abortions in New Delhi highlighted that most pre-marital abortions are clandestine and AYA rely on their informal networks to gather information on abortion services [ 4 ]. These networks may have become difficult to access during COVID.
COVID and the lockdown have had an unprecedented impact on women and girls’ access to abortion. Several questions remain to be answered. What services are women and girls accessing to get abortions? Who is assisting them? How is this impacting their health and well-being? International Pregnancy Advisory Services (IPAS) estimates that in India, access to medical abortions, which is what most women and girls rely on, must have become very challenging during the lockdown and the COVID pandemic, due to lack of availability, lack of information, and lack of privacy and confidentiality. As per IPAS, 1.5 million medical abortions may have been compromised in the first three months of the lockdown period. This could be due to closure of outlets, disruption of the supply chain, and restriction in transport services, since AYA women or their partners generally avoid their neighborhood chemist shops and prefer a more distant outlet for buying medical abortion drugs due to the attached stigma [ 18 ]. Furthermore, accessing an abortion at an approved facility is challenging to begin with, particularly for abortion beyond 12 weeks. However, given the impact of COVID, as per IPAS, facility-based first or second trimester abortion may be the only option for a majority of the 1.85 million women, including adolescent girls and young adult women needing abortion services [ 18 ].
Restrictions on mobility and lack of transportation facilities during COVID-19 increased these challenges. It is important to note the unique vulnerabilities of AYA during the lockdown: limited autonomy and age-related vulnerability, wherein they are often not taken seriously, particularly in India, and the lack of adolescent-centric services to begin with may have pushed their sexual health practices and contraceptive needs further underground [ 3 ]. Also, it is crucial to recognize that data on AYA’s SRHR experiences remains limited, since these are not seen as priority issues to be monitored.
While researching for this chapter, the authors noted that the limited evidence that has been collected on AYA SRHR during COVID primarily focuses on their reproductive health. Information on AYAs’ sexual health and relationships remains very limited and, therefore, invisible and non-quantifiable. It is important to address this gap because we remain unaware of the impact on AYA, most of whom, anyway, lack the legitimacy or ability to openly seek SRH services.
Mental Health of AYA During COVID and Its Links to Sexual and Reproductive Health and Rights
COVID and the resulting isolation have impacted the mental health of human beings globally [ 21 , 22 ]. This includes AYA more so since they are not even recognized as a group having special needs, requiring attention. DASRA’s report highlights how AYA’s mental health was impacted during COVID in India. AYA are facing high levels of anxiety and stress related to COVID, school closures, lack of socialization, and violence at home. Further, due to lack of opportunities to meet their peers and other adults whom they trust, AYA are unable to share their anxieties. They do not know who to approach with their questions and thoughts. Sexual and reproductive health issues are likely to rank quite high among these concerns.
Youth organizations reported that some young people had approached them with fears about their intimate relationships, sexual violence, about their future, and had shown symptoms of anxiety and depression and a few had also expressed suicidal thoughts. They talked about the impact of the lack of space at home, isolation from their friends and partners, and the lack of intimacy with their partners. While organizations refer to mental health and well-being of AYA, they do not have information on how the lack of access to SRHR services and information is impacting their mental health. The limited data suggests the need to explore further into this aspect.
The need for mental health services and counseling in general is paramount, including for adolescents and young people, who are further isolated since they do not have any avenues to share and learn from each other, leave alone accessing services and counseling. The effect of a worldwide pandemic on AYA’s mental health can be devastating and cannot be overlooked [ 23 ]. The potential and lives of a whole generation of young people could be impacted.
Taking Stock of Responses to Adolescents’ and Young Adults’ Sexual and Reproductive Health and Rights During the Pandemic
The challenges presented above have been highlighted by youth collectives, youth-based and youth-serving organizations as seen in our review of the literature and conversations with some of these organizations. While recognizing the impact of the pandemic on AYA’s lives, these organizations also adapted their regular programs to respond to the unique needs of AYA during this time. They leveraged technology to reach AYA, trained and worked with their field staff and peer mentors to counsel adolescents remotely during the pandemic, and worked with community health workers and the public health system to address healthcare needs of adolescents.
As per DASRA, organizations leveraged digital tools like WhatsApp and Zoom, developed apps, quizzes, newsletters, and advertisements on television and radio, interactive voice response (IVR), and telephone systems to spread awareness about government-mandated information to dispel misconceptions and stigma, to learn about the feelings and experiences of AYA, and to run their SRHR programs. Some organizations adapted their sexuality education curricula to a digital mode (videos, audios, and animations) and are continuing their programs online. Organizations held creative sessions (poetry, painting, and movie screenings) to engage AYA on COVID and related issues, as well as other educational issues. Further, tele-services during the pandemic were used to provide counseling to AYA on SRHR, for example, where to access sanitary napkins and contraceptives, where young people can go for abortions, and on safe sex practices.
Organizations trained their staff to address the unique needs of AYA during this time, to connect with AYA, and understand their needs so that appropriate responses can be developed. They have also worked to provide women and girls access to sanitary napkins. Some delivered sanitary napkins to the homes of adolescent girls in rural areas and urban slums; others conducted online classes on how to make pads at home. They also helped pregnant women access ante-natal care, institutional delivery by arranging transportation, and post-natal care. They worked with community health workers to ensure that they could provide these services—IFA tablets, sanitary napkins, contraceptives, transportation for deliveries, and counseling—wherever possible. Organizations reported working with their youth leaders, peer mentors, and girl champions to reach out to AYA. For example, in the case of an unintended pregnancy, the peer mentors helped women and girls access timely abortion services.
Organizations responded to complaints of sexual violence by providing counseling through their field staff (mostly telephonic) and provided referrals to other facilities. In some cases, organizations went to the child protection committee and reported the case to the police and district or block authorities. Organizations also counseled parents about stopping early marriages, particularly of young girls, advised them to continue their education, and encouraged parents to create a space at home where adolescents could feel safe. All of these were vital before the pandemic but took on special impetus during the pandemic.
Some organizations created safe spaces to enable AYA to share their fears, anxieties, and uncertainties, both online and offline, through WhatsApp, TikTok, Instagram, and Facebook groups, and through telephonic platforms. Organizations are experimenting with online fellowship programs to build leadership and life skills. They are leveraging virtual training kits and tools developed by UNICEF and ChildLine India to check in with adolescents about their mental health. However, the issue of equitable access remains a big challenge. Many AYA do not have access or regular access to smart phones and the Internet. This is more challenging for girls and women, especially in rural areas, because the men and boys from the household control the smart phones available at home.
While all these efforts are commendable and responsive to local needs and contexts, a key gap remains—that of addressing the sexual health of AYA. Organizations have limited understanding of the sexual relationships of AYA. The challenges that they face in gathering this information increased significantly during COVID. Another gap is the issue of appropriate and gender-disaggregated data on SRHR of AYA. Organizations have not systematically collected data on how COVID has impacted AYA’s SRH. Data gathering has been sporadic and need based, which makes it difficult to capture realities accurately and to design programs to address SRH needs.
The Way Forward
The trend of not prioritizing adolescent and young adults’ sexual and reproductive health has continued during COVID. The recommendations for adolescents and young adults that SRHR experts have been making over the years remain valid and even more urgent—such as acknowledging adolescent sexuality, talking about sex from the perspective of pleasure as well as safety, ensuring sex education in schools and colleges, creating safe spaces where adolescents can share their fears, anxieties, feelings, experiences, gathering information from AYA to ensure that programs for them are responsive to their unique needs, creating peer groups of AYA, and building capacities of community health workers to respond to AYAs’ needs. In addition to continuing to persevere on earlier recommendations, the authors of this chapter would like to emphasize the following key recommendations.
First and foremost, the absence of young peoples’ voices from COVID response mechanisms set up by the government is unfortunate. It represents a dismissal of young people’s experiences and unique needs. In the task force set up by the government for COVID management, representatives from youth-based and youth-serving organizations need to be included. While the government, especially local functionaries, has benefitted from the assistance provided by youth-based organizations, their involvement in planning and developing strategies is limited and needs to be addressed.
Furthermore, while the needs of young people are deprioritized, young people from vulnerable groups—those that live in poverty, those with special needs, those from the lesbian, gay, bisexual, transgender, queer, intersex, and asexual (LGBTQIA) communities, and those that are disadvantaged because of their gender, caste, religion, and place of habitation—face greater challenges. Special focus should be given to the needs of young people from these groups, and their representatives should be a part of developing response mechanisms.
Gender is an obvious key factor in shaping young people’s experiences, and yet, this often goes unacknowledged. The gendered impact of the pandemic on young people’s lives, especially girls and women, needs to be central to the response. How has the pandemic fueled regressive gender norms, increased gender-based discrimination and violence against girls and women, and strengthened unequal power structures? This is a question that demands an answer because the pandemic will have long-term impacts on the lives of girls and women, especially those who have been married early, dropped out of school, experienced physical, economic, mental, and sexual violence, and been refused abortions. We cannot ignore or afford to sweep under the carpet, the long-term impact of the pandemic, in our current focus on immediate, short-term responses. For this purpose, timely and accurate data is required—data that captures the needs of various groups of AYA—unmarried and married, boys and girls, and so on—so that suitable and relevant responses can be developed.
We must adopt a human rights and social justice approach, something that is most overlooked with AYA, especially girls and women. This includes designating and planning sexual and reproductive health services for AYA, and re-allocating resources accordingly. For this, one must acknowledge adolescents’ and young adults’ sexuality as a reality. It is vital to integrate sexual well-being into the public health response for adolescents and young people.
Finally, COVID has shown the potential of technology in creating new opportunities for developing health content and disseminating it and delivering services. This must be extended to AYA’s sexual and reproductive health, which is currently limited. Also, the rise in digital sexual practices needs to be acknowledged; we cannot continue to ignore or look down on them. On the contrary, recognizing their value and reach, we must encourage safe digital sexual practices. As mentioned above, the digital divide in access to technology needs to be accounted for while developing tech-based solutions. However, despite digital inequalities, young people are more connected today than ever before, and therefore, these channels must be leveraged to their fullest potential, maintaining necessary caution. In all our efforts, we need to be sure that we are addressing the entire gamut of SRH without overlooking sexual health, as we have unfortunately tended to do.
Young people are a key resource and network, more so during a health emergency. This resource remains largely untapped. Peer group programs are particularly vital in this area. With the right training, young people can work with the health authorities to help respond to the pandemic. A healthy and empowered young population is an investment as we look beyond the pandemic.
Dasra. Lost in lockdown: chronicling the impact of COVID-19 on India’s adolescents; 2020.
Google Scholar
Ministry of Health and Family Welfare. Guidance note on provision of reproductive, maternal, newborn, child, adolescent health plus nutrition (RMNCAH+N) services during and post COVID-19 pandemic. Ministry of Health and Family Welfare; 2020.
Nanda P, Tandon S, Khanna A. Virtual and essential—adolescent SRHR in the time of COVID-19. Sexual and Reproductive Health Matters. 2020;28(1):1831136.
Article Google Scholar
Kedia S, Banerjee P, Nandy A, Vincent A, Sabarwal, Kato-Wallace J. Exploring men’s engagement in abortion in Delhi. International Center for Research on Women; 2018.
UNFPA. My body, my life, my world through a COVID-19 lens. The United Nations Population Fund; 2020.
Orben A, Tomova L, Blakemore S-J. The effects of social deprivation on adolescent development and mental health. The Lancet Child and Adolescent Health. 2020;4(8):634–40.
World Health organization. Sexual and reproductive health and research including the special programme HRP. World Health Organization; 2020.
World Health Organization. Reproductive health in the Western Pacific. World Health Organization; 2020.
Ministry of Health and Family Welfare. National family health survey (NFHS-5) fact sheets: Key indicators 22 states/UTs from phase-I. Ministry of Health and Family Welfare; 2020.
UNFPA. Sexual and reproductive health and rights, maternal and newborn health and COVID-19. The United Nations Population Fund; 2020.
Population Foundation of India. Impact of Covid-19 on young people. Population Foundation of India; 2020.
Quilt.AI. The pandemic’s impact on young people in India. Quilt.AI; 2020.
The YP Foundation. Youth insight: informing COVID-19 relief and response with young people’s experiences. The YP Foundation; 2020.
Sharma S, Nanda S, Seth K, Sahay A, Achyut P. Couples’ contraceptive behavior and COVID-19: understanding the impact of the pandemic on demand and access. Sexual and Reproductive Health Matters; 2020.
Banerjee D, Rao TSS. Sexuality, sexual well being, and intimacy during COVID-19 pandemic: an advocacy perspective. Indian J Psychiatry. 2020;62(4):418.
Plan International. How will COVID-19 affect girls and young women? Plan International; 2020.
Shukla AK. Govt helpline platform explodes with SOS calls, 92,000 seek help on CHILDLINE in 11 days. ETGovernment.com; 2020.
IPAS Development Foundation. Compromised abortion access due to COVID-19 : A model to determine impact of COVID-19 on women’s access to abortion. IPAS Development Foundation; 2020.
National Health Mission. Adolescent health (RKSK). National Health Mission; 2020.
WGH India. WGH India dialogue series: Amplifying the engagement of female frontline health workers in India’s COVID-19 response. International Health Policies; 2020.
Javed B, Sarwer A, Soto EB, Mashwani Z. The coronavirus (COVID‐19) pandemic’s impact on mental health. Int J Health Planning Manage. 2020.
Patra S, Patro KB. COVID-19 and adolescent mental health in India. The Lancet Psychiatry. 2020; 7(12):1015.
Gundi M, Santhya KG, Haberland AJ, Zavier F, Rampal S. The increasing toll of mental health issues on adolescents and youth in Uttar Pradesh. New Delhi: Population Council; 2020.
Download references
Author information
Authors and affiliations.
International Center for Research On Women, New Delhi, India
Sapna Kedia & Ravi Verma
Independent Consultant, International Center for Research On Women, New Delhi, India
Purnima Mane
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sapna Kedia .
Editor information
Editors and affiliations.
POP Movement, New York, USA
Saroj Pachauri
Ash Pachauri
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter.
Kedia, S., Verma, R., Mane, P. (2022). Sexual and Reproductive Health of Adolescents and Young People in India: The Missing Links During and Beyond a Pandemic. In: Pachauri, S., Pachauri, A. (eds) Health Dimensions of COVID-19 in India and Beyond. Springer, Singapore. https://doi.org/10.1007/978-981-16-7385-6_10
Download citation
DOI : https://doi.org/10.1007/978-981-16-7385-6_10
Published : 09 April 2022
Publisher Name : Springer, Singapore
Print ISBN : 978-981-16-7384-9
Online ISBN : 978-981-16-7385-6
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 29 November 2022
Barriers to vulnerable adolescent girls’ access to sexual and reproductive health
- Mojgan Janighorban 1 ,
- Zahra Boroumandfar 2 ,
- Razieh Pourkazemi 3 &
- Firoozeh Mostafavi 4
BMC Public Health volume 22 , Article number: 2212 ( 2022 ) Cite this article
9919 Accesses
7 Citations
7 Altmetric
Metrics details
Vulnerable adolescents are exposed to sexual and reproductive health harms. Ignoring the sexual and reproductive health of this group can have irreparable consequences. The present qualitative study aimed to explore the barriers to the access of vulnerable adolescent girls to sexual and reproductive health.
In this study, sixteen 14-19-year-old adolescent girls and twenty-two key informants were selected using purposive sampling method. Through in-depth semi-structured interviews, they expressed their experiences of barriers to sexual and reproductive health in vulnerable adolescent girls. The data were encoded using the conventional qualitative content analysis.
Based on the results of the study, neglecting the reproductive and sexual health of vulnerable adolescent girls at different levels leads to serious challenges and obstacles in providing and maintaining it. Lack of a responsible family, the repulsive behaviors of the family and following risky behaviors of peers led to ignoring the sexual and reproductive health of adolescent girls. Unanswered sexual questions, defective life skills, unwanted pregnancy during adolescence, lack of awareness of unsafe sex, violating cultural norms and wounded psyche in vulnerable adolescent girls threaten their sexual and reproductive health. Ineffectiveness of key organizations in providing sexual and reproductive health services alongside lack of legal, political and social support in this area indicate that the sexual and reproductive health of these girls is not a priority for the society.
Numerous personal, family, social, legal and political barriers challenge the sexual and reproductive health of vulnerable adolescent girls. Developing a comprehensive and practical program beside legal and political support for this issue can provide the basis for the sexual and reproductive health of this group of adolescents in societies.
Peer Review reports
Adolescence is a time of personal experience and choice, when personal and sexual identities are formed. Becoming a sexually healthy adult is one of the key developmental activities in adolescents. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as a pleasurable and safe sexual experience, free of coercion, discrimination and violence [ 1 ].
Risk-taking and emotion-seeking together with the misconception of invulnerability in adolescence period can lead to increased assertiveness in engaging with risky behaviors [ 2 ]. High-risk behaviors are defined as behaviors with an adverse effect on the overall growth and health of adolescents that may prevent them from future progress and success. High-risk behaviors may include violent behaviors such as physical harm or behaviors such as alcoholism, smoking, high-risk sexual behavior, and use of narcotics [ 3 ].
In a study conducted on 385 14–19-years-old adolescents, 120 subjects (23.3% of them were female and 40.4% were male), were involved at least once in their lives, in sexual relations either voluntarily or by force. 19.5% of these adolescents were exposed to high-risk sexual behaviors and sexually transmitted diseases such as HIV [ 4 ].
Vulnerable adolescents are a special group who given to their personal, family, economic, social and cultural conditions are exposed to physical and mental activities which may threaten their sexual and reproductive health. Vulnerable adolescents in this study refer to the adolescent girls who use drugs (stimulants, alcohol and hallucinogens), have high-risk sexual behaviors, a history of sexual harassment, a history of running away from home, and those living in welfare centers, social emergency centers and drug hangouts. The adolescent girls involved in any of these behaviors or a combination of them are considered to be vulnerable. In the study of Garmaroudi et al. (2010), conducted in the Welfare Organization of Iran, 50% of street women referred to rehabilitation centers were 15–19 years old and 24% of them were in the age range of 19–24 years [ 5 ].
Adolescents are among the most important target groups in sexual and reproductive health programs. Sexual relations, especially unprotected ones, are associated with irreparable consequences, such as infection with HIV and other sexually transmitted diseases, unwanted pregnancies, unsafe abortions, infertility, gender-based violence and sexual dysfunction [ 6 ].
In the United States, 20 million new sexually transmitted infections (STIs) occur each year, half of which are among 15–24-years-old adolescents. Sexually transmitted infections and the resulting complications can cause serious health consequences [ 7 , 8 ]. Adolescent pregnancy is a global problem occurring in all countries. In Iran, the highest fertility rate has been occurred between the two age groups of 15–19 and 30–39 years old [ 9 ]. Globally, at least 10 million unintended pregnancies occur each year among 15–19-years-old adolescents in developing countries. Adolescent mothers face higher risks of complications such as eclampsia, puerperal endometritis, and systemic infections than 20–24-years-old. To get rid of the problems caused by their unwanted pregnancies, most adolescents seek abortion which is often performed unsafely. Out of the estimated 5.6 million abortions that occur each year among 15–19-years-old adolescent girls, 3.9 million are unsafe. As a result, pregnancy and childbirth complications are the leading cause of death among these girls [ 10 ].
However, there are still obstacles to the implementation of reproductive health strategies for adolescent girls in many countries, especially developing ones [ 11 ]. Under the influence of the challenges of gender inequality such as child marriage, female circumcision, incomplete high school education, lack of job security, overwork at home, less decision-making power and limited travel in the community, girls are more vulnerable to social harms than boys [ 12 ]. Moreover, inadequate information and education about gender and reproduction, insufficient access to health services, unsafe sex, less control over reproductive and sexual decisions, familiar partner violence and sexual violence make girls more vulnerable than boys to the sexually transmitted diseases [ 13 ].
In some countries such as Iran, reproductive and sexual health information and services provided by the health system are usually inappropriate for the adolescent girls, as these services are actually designed for married women. In Iran, political barriers are also among other major barriers to the provision of reproductive health for adolescent girls. Cultural and social challenges, structural and administrative barriers, and unpreparedness of the health system to provide sexual and reproductive health services to vulnerable adolescents are considered as barriers to the successful implementation of sexual and reproductive health programs for adolescents in Iran [ 14 ]. Iranian mothers’ negative attitude towards sexual health education for adolescents is another important obstacle. Lack of knowledge and communication skills are the main reasons for not talking about such issues [ 15 ]. Insufficient education and information in sexual risks, restricted and difficult access to the services, high costs of the services, lack of health insurance coverage and lack of financial independence, fear, embarrassment, inadequate knowledge, misconceptions, stigma and concern about complications and contraceptive measures, absence of a reporting system on issues such as premarital sex, induced abortion, sexual abuse or sexual coercion are among the challenges associated with the sexual and reproductive health of adolescents [ 16 , 17 ]. Non-confidentiality of information during the service provision and lack of diversity in contraceptive methods are among other obstacles [ 18 ].
Iran is an Islamic and traditional country filled with strict religious rules and Iranian customs and culture. Based on the Islamic laws of Iran and other Islamic countries, premarital sex is not approved by religion, family, law and society, and out of wedlock relationship of an under 18-years-old vulnerable can often be challenging and she will be cruelly abused. Additionally, the existence of a center that provides adolescents, especially girls, with reproductive and sexual health services, is illegal and contrary to the religious rites of our country. As such, many factors affect the sexual and reproductive health of these vulnerable adolescents. Accordingly, this study aimed to explain the barriers of vulnerable adolescent girls in having access to sexual and reproductive health. To describe the sexual and reproductive health needs of vulnerable adolescent girls was other specific objective.
Study design
The present study was a part of an exploratory sequential mixed methods study (Qual-Quan) [ 19 ] which conducted from April 2019 to June 2020 through using content analysis approach.
Settings, samples and recruitment
In the present study, sixteen 14–19-years-old vulnerable adolescent girls and twenty-two key informants (health providers, nurses, midwives, reproductive health professionals, obstetricians, psychologists, psychiatrists and addiction therapist), from cities of Isfahan, Tehran and Mashhad in Iran participated in the study. These girls were selected using purposive sampling method and considering the maximum variation strategy in terms of age, education, and the economic situation. A number of girls were found based on the previous experiences of the research team in identifying and referring to drug hangouts where such girls used to go; other girls were selected from the girls who were arrested by police at boy and girl joint parties or after fleeing their homes and being handed over to the 123rd Emergency Department. All of these girls were interviewed at welfare centers. In these centers, other eligible girls who had been sexually abused were also selected for interviews. After being met by us, some of these girls introduced their other friends to us and, thus, the sampling continued based on snowball sampling method. In addition, a number of midwives and nurses, health care providers, psychiatrists, gynecologists, addiction therapists and psychologists are informally interacting with the Welfare Organization regarding sexual and fertility issues as well as the psychological problems of vulnerable adolescent girls. We had access to them through the Welfare Organization. We also included reproductive health experts from university-affiliated research centers who conduct research on sexual and reproductive health and social factors affecting health. Moreover, head of the School of Health in the health center of the province was interviewed as well.
The key informants were also selected using purposive sampling method and considering the maximum variation strategy in terms of work experience and occupation. Inclusion criteria for the adolescent girls consisted of 12–19-years-old girls, Iranian citizenship, never married, onset and stabilization of menstruation and no psychological disorders; inclusion criterion for the key informants was having at least two years of work experience. After finding eligible participants, none of them refused to participate in the study. They were recruited in person or by phone calls. Tables 1 and 2 present the demographic information of the participants.
Data collection
Data collection methods included semi-structured in-depth interviews for both adolescent girls and key informants. The third author (RP) conducted the interviews. She had 7 years of working experience in midwifery and was Ph.D. candidate in reproductive health. She had no previous contact or relationship with the participants and centers. The first and second authors had experience in qualitative studies and in the field of sexual and reproductive health. They participated in the first 10 interviews and analyzed the data. They made sure that the third author was thoroughly trained in in-depth interviews, and after making sure, the other interviews were conducted by her. All interviews were read by the first and second authors separately and it was decided to refer to the participant again in case of ambiguity, as such conditions did not occur for any of the interviews. It was also decided that the first and second authors would have 70% agreement with each other on the formation of the categories. The scheduling and location of the interviews were determined by the participants. Prior to beginning the interviews, the researcher explained the objectives of the study to the participants and obtained their written and oral consent to conduct the interview. The interviews lasted for 40 to 60 minutes, which were recorded with the permission of the participants and were immediately transcribed. The specific objectives of interviews with adolescent and key informants were: 1. To explore how unmarried adolescent girls get involved in sexual relationships, 2. To explore adolescent girls’ experiences and issues they face following such relationships, 3. To explore the experiences of key informants in dealing with and caring for vulnerable adolescent girls, 4. To explore how vulnerable adolescent girls’ sexual and reproductive health can be improved or safeguard. The interviews, then, continued with meticulous questions with regard to the provided answers. Sampling was halted when no new interview data came out.
Data analysis
Data analysis was performed manually. After completing the first interview, the data analysis was performed using the conventional (inductive) content analysis method as explained by Graneheim et al. so the codes, subcategories and categories were generated from the data [ 20 ]. The interviews were transcribed verbatim and saved in a word document by the third author (RP). The interviews were then reviewed repeatedly by the first and second authors so that a complete understanding of them related to the research aim, can be achieved. The sentences and phrases were then inductively coded, clarifying the codes that were not clear was done by reading and going back to the original data. Similar codes were merged and merged codes with a similar meaning were grouped together to create subcategories. When no new information was obtained and the concepts extracted from the codes were repeated, we found that we had reached saturation. Thereafter, comparing the subcategories with each other, the conceptually related ones were placed in a main category. The codes, subcategories and categories were discussed in many sessions among the authors [ 21 , 22 ].
Rigor and trustworthiness
In order to evaluate the quality of the data and findings, four criteria of credibility, dependability, confirmability and transferability were used. The credibility of the data in this study increased using prolonged engagement with the data, member checking and repeated reading of the interview texts and transcriptions, peer debriefing, using complementary opinions of colleagues, writing reminders and various bracketing methods for data collection. In order to achieve data dependability, a complete and continuous method of recording decisions and activities of data collection and analysis was used, with the initial codes interpreted based on the participants’ experiences and examples of extracting categories and choosing excerpts from the transcripts of the interviews for each category. The data were also examined by an expert researcher who had no connection with the research and was an external observer. For the confirmability of the data, the entire research process and decisions were recorded by the researcher, so that others would follow the research findings if necessary. Also, the texts of some interviews, extracted codes and categories were provided to the research colleagues and a number of faculty members who were familiar with the qualitative research analysis but did not participate in the research. They were asked to examine the authenticity of the coding process and their views on categories were reviewed. Finally, for the transferability of the data, the findings were studied by several individuals who had characteristics similar to those of the participants of the study but did not take part in the present research process. These subjects were introduced by the same offices of midwives, psychologists and emergency services of welfare center (123), and were selected by the research team. With regard to the hangouts, we were helpfully introduced by the hangout manager (Mamasan) and the girls were introduced by her. During the interviews, measures including the use of face masks, physical distancing, and conducting interviews in large physical spaces were considered to prevent the spread of Covid-19. This research was approved by the Ethics Committee of Isfahan University of Medical Sciences with the ethics code of IR.MUI.RESEARCH.REC.1398.396. The participation of the participants in this study was completely voluntary and informed written consent was obtained from them. The informed consent was obtained from the parents or their legal guardian or legally appointed representatives of under 16-years-old girls.
The mean age of the adolescent girls was 17.68 years . The mean age of the first sexual intercourse was 14.31 years, 75% of the participating girls were addicted to drugs or alcohol, or both, and over 40% of whom had a history of parental addiction. The mean age of key informants was 43.36 years, the average work experiences was 14.90 years and most of them were woman ( n = 19). The Demographic information of the participants are shown in Tables 1 and 2 :
Findings of the present study with regard to the barriers of vulnerable adolescent girls’ access to sexual and reproductive health were explored through six main themes as follows: “family challenges”, “peer pressure”, “adolescents’ inability to make informed decisions about sex and fertility”, “lack of awareness of sexual and reproductive health threats”, “psychosocial threats to reproductive health”, and “neglecting the girls’ sexual and reproductive health” (Table 3 ). Identifying needs was another part of our study that the main category in our study was the need for comprehensive care of vulnerable adolescents. This comprehensive care included psychological and physical support and care and the barriers extracted to meet these needs.
Family challenges
The adolescent girls of our study stated that unstable families and family rejection exposed them to family challenges. These challenges deprived them of a responsible family to take care of them.
Unstable family
Parental extremism in parenting practices, violence against adolescents, discrimination and inflexible behavior, the absence of one or both parents caused by divorce, death, or imprisonment have led to the neglect of these girls. All of these could lead to the involvement of adolescents in insecure relationships. In this regard, participant No. 5 said:
“I wasn’t allowed at all to go to my classmates’ homes. I couldn’t go out with them. I used to go to school from home and vice versa. Neither was I allowed to go to the nearby shops for shopping. I was under difficult conditions. I’d like to find a companion; either a girl or a boy”.
Participant No. 7 also said:
“My parents are so strict. My dad bickers over everything all the time. He beats me up with everything he finds. My upper part of the lip was torn when he hit it with a curtain rod. For this, I decided to get out of home, as I was so tired”.
In some other families, delinquent parents, economic poverty, prevalent sexual behavior, and disintegrated parental privacy against children, or rather, high-risk sexual behaviors in the family, provide the grounds for early sexual intercourse and the onset of vulnerability in the adolescents. As participant No. 22 said:
“Most of the time, parents themselves cause injuries, that is, they’re engaged in rampant sexual relations and extra-marital affairs. Observing such scenes, especially in a small family context, which is supposed to provide a safe haven for the kids, will cause injuries”.
Regarding the loss or absence of one of the parents in the family, participant No. 26 said:
“Another group of girls had families whose parents had separated. The father had started a new life, and the mother also had a boyfriend or was remarried. Some of these girls also lost their fathers. The girls were confused, looking for a foothold, and engaged in sexual relationship with their boyfriends that even led to pregnancy and abortion.”
Family rejection
The participants emphasized the role of confronting family values with them and the lack of an efficient parent, which led to ignoring the health status of adolescent girls, especially their reproductive and sexual health. These reprehensible behaviors of the family and their indifference had prevented the adolescent girls from expressing their injuries and remain silent about their endangered health. This issue, in turn, had accelerated the process of injury even more. Participant No. 21 said:
“These children are so repressed in the family that even if they’ve a problem, they don’t dare to tell anyone; and when the issue is over, a 14-years-old girl with genital warts and incontinence stools goes to the midwife’s office for advice and medical services”.
Participant No. 13 also said:
“I was always careful not to do vaginal sex with the boys when I was with them, because I’d to tell someone. I was both scaring and didn’t dare to talk to anyone, not even my mother. Oh, to a mother who was illiterate herself and if she knew I was having an affair with a boy, she was insulting me, what should I say, I didn’t know what to do next.”
Peer pressure
The adolescent girls participating in the present study stated that in their youthful longing, they needed to interact with their peers. Given the fact that their family was not adequately efficient, they needed the approval of their peers and in some cases even obeyed them.
Not to be left behind by the group of friends : Findings showed that being accepted in the company of friends forces the adolescent to follow the behavior of her friends. They did not want to be left unattended by their friends.
Participant No. 16 talked about the need to be accepted by her friends:
I remember I was in charge of the school student council and we only talked about sex and boys with my friends when we got together. I couldn’t leave them as they might reject me and I might lose my place among them. Thus, I even sometimes took part in their discussions “.
Defenseless against bad peers
Being in the company of bad friends and the desire to be accepted by them has been a reason for following risky behaviors such as use of alcohol, smoking, substance abuse and unprotected sex. These deceptive and misleading friends are the agent of entering the cycle of harms. In this regard, participant No. 8 said:
“I just wanted to make friendship with him, but he insisted to see some films together. Finally, after insisting and expressing some romantic words, we sat down and watched the film together; then I felt excited, something that I hadn’t experienced before. I don’t know if it was a good or bad feeling. But then we had sex”.
Other participants referred to their being seduced by a boyfriend and having sex too. As such, participant No. 3 said:
“He lied to me and said it is just a simple touch. Then, during the relationship, he filmed me and threatened that he would show the film to everyone if I didn’t move the relationship forward. For 2 years now, with this movie, I’ve been caught in a relationship that I hate and every time it’s done, I hate myself.”
Another participant referred to the surprise and defenselessness of adolescent girls in front of some of their friends:
“They’re inexperienced and immature. They can’t protect themselves. On the other hand, being deceived by bad boys, with things like a car or romantic words or a gift, they’re trapped and because of immaturity, they’re easily and cruelly abused. Some of these adolescent girls have been sexually abused; so violently that they heal their wounds and injuries with several treatments” (participant No.36).
A reproductive health expert maintained that these girls follow the risky behaviors of bad friends and, then, should tolerate the subsequent consequences:
“Another point is that most girls in the company of friends tend to use drugs and use all kinds of drugs, especially stimulants. In fact, drug use can’t be separated from having sex with the opposite sex. It means that they seem to complement each other. In this situation, in order to stay in the group, one consumes drug and has unsafe sex, which may even lead to unwanted pregnancy and abortion” (Participant No. 18).
Adolescents’ inability to make informed decisions about sex and fertility
Unanswered sexual questions and imperfect life skills prevented the female adolescents participating in the study from making quick and accurate decisions about their sexual health and fertility.
Unanswered sexual questions
The participants acknowledged that they had incomplete information about sex and pregnancy, and that there was currently no suitable platform in our country to inform adolescents about reproductive health issues. Thus, their questions about sexuality had remained unanswered. In Iranian families, parents refuse to talk with their children about sexual issues or even answer their reasonable questions about sexuality and fertility in order to protect their adolescents. In this regard, participant No. 14 said:
“I couldn’t talk to my mother about these things. Once I talked with her about my problem but I said it was my friend’s and my mom blamed her. From then on, I talked about my boyfriends with my girlfriends whom I knew they’d also boyfriends”.
“Our parents think their children are going astray. They’re not taught or guided about sexuality. This causes them to be unaware of the dangers” (participant No.37).
In the educational system, adolescents’ needs with regard to sexual issues have been ignored and the national media also overlook the sexual and reproductive health of adolescents. As such, there is no specific plan or training in this regard. Participant No. 27 said:
“ Schools have, to some extent, entered the area of educating such issues, but it is quite limited. When talking about AIDS, they censor the issue of the disease transmission through sex and fail to warn about perils related to this disease. I think they believe this could arouse children’s desires”.
“These words are forbidden in school. Even our biology teacher didn’t explain much about humans until we reached the reproduction chapter. So, we’d a lot of questions, but we were embarrassed to ask. No one talked about these things either in class or in the meetings that psychologists came to us. No one had the right to speak as she might be fired” (Participant No. 15).
Adolescents’ curiosity in this regard leads them to take refuge in the insecure context of cyberspace and social networks. Unlimited access to the virtual spaces and receiving inaccurate sexual information lays the ground for adolescents to enter the cycle of harm. Moreover, friends and peers are considered by adolescents as important sources of information that provide the ground for receiving deceptive information on sexual issues. In this regard, participant No. 9 stated that:
“Only on satellite networks could you understand things very well or you’d to go to the internet to find out the answer to your questions. In TV and movies, even educators don’t talk about these issues as they believe these are taboos which may make us shameless and ruin us”.
I was in the six-grade when I heard my classmates talking about sexual issues. Well, that was fun. They told me how sexual relations look like, and taught me how to do it. I really wanted to experience it” (participant No.11).
Defective life skills
Most vulnerable adolescent girls are unable to use communication skills properly when entering a relationship with the opposite sex and fail to manage their relationships correctly. Therefore, when faced with health-threatening situations, including request for substance and alcohol use or unprotected sex by the friends or opposite sex, they fail to manage the situation and cannot use problem-solving skills, especially the skill of saying no. This issue was explained by participant No. 17:
“One of them said it was in a party where girls and boys were dancing together. I hadn’t gone to such places before, but I failed to say no to my friends. Well, it was cool. I couldn’t say no. So, this can be a defective social skill”.
“It was as if we’d never learned to say no. For example, the first time my friend invited me to drink alcohol in presence of other boyfriends and girlfriends, I don’t know why I couldn’t resist. Because of that inability of saying on, I got involve in a lot of relationships with boys who sometimes I think were worthless and I wish I’d said no from the beginning” (Participant No. 13).
“I very quickly accepted any relationship and I didn’t know how to talk to the boys and which words of them I should accept and which words I shouldn’t. Thus, I entered a relationship with any boy who said he loved me and bought me something or gave me a ride” (Participant No. 10).
These factors lead to uninformed decisions in adolescents about sex and fertility.
Lack of awareness of sexual and reproductive health threats
Adolescents do not have awareness and a proper understanding of issues such as sexual affairs, pregnancy, contraceptive methods and the short- and long-term consequences of risky sexual behaviors such as unwanted pregnancies, recurrent miscarriages, and risk of infertility, as well as sexually transmitted infections and their complications. Owing to this lack of awareness they may act incautiously and heedlessly when they are engaged in a relationship with the opposite sex.
Unwanted pregnancy during adolescence
The participants stated that they did not have the necessary information about the pregnancy process and the use of contraceptive methods. Moreover, as these relationships are stigmatic, they did not have access to a center where they could receive these services. In this regard, participant No.2 stated that:
“I didn’t know what a sexual relation looks like. I didn’t know how I could be made pregnant when entering a relationship with the opposite sex. I’d refrain from all of this if I knew what they meant”.
Similarly, participant No. 1 said:
“I didn’t know anything about contraceptive methods and I couldn’t understand how to use them. When entering a relationship, I didn’t care whether or not the other side had used condom. I also took the emergency contraceptive 10 days after sex, which was useless and I got pregnant. My mother took me to a house where they aborted my baby. I was bleeding so much that I thought I was about to die”.
The psychologist of the Welfare Social Emergency Center said:
“Parents should give their children a series of trainings on sexual issues, which they don’t teach because of a series of misconceptions. For example, they believe that such teachings will make their children shameless. Accordingly, their children experience sex as they’re unaware that they may be pregnant. When they become pregnant, they begin to think about a solution” (Participant No. 29).
Lack of awareness of unsafe sex
Most of the adolescents participating in this study had incomplete, limited, or inaccurate information about safe sex and sexually transmitted infections. Thus, participant No. 12 said:
“I felt like having a sore throat, but it was gynecological infection. Because what I saw while bathing was like a sore throat when I’d a cold. I thought I must have an infection and I’d get better. Away from my mother’s eyes, I took her medicine and used it.”
About having unsafe sex, participant No. 7 said:
“ I was afraid of losing my virginity before marriage. That’s why I’d anal sex with 5 of my boyfriends. I was very annoyed and I always have sores on my anus. I have also discharge. After examination, midwife told me that I’d a severe infection in my anus and that I even had some warts that I’d not noticed myself.”
One of the participants also emphasized the need to follow up and take care of sexually transmitted infections in these adolescents and said:
“The problem for adolescent girls with unsafe sex is that they develop sexually transmitted infections such as warts, herpes and acute proctitis. This’s followed by pain, bleeding and constipation, and eventually anal sphincter involvement. They’ll go to a gynecologist if anyone guides them” (Participant No.33).
Psychosocial threats to reproductive health
Psychosocial consequences following sexual orientations and unsafe sexual behaviors are other barriers that can affect the reproductive and sexual health of vulnerable adolescent girls. Furthermore, the norms of society do not accept some of these sexual orientations, and the stigma towards these adolescent girls is increasing every day. Also, unsafe sex and sexual abuse expose these girls to mental disorders.
Being different from cultural norms
Most adolescent girls reported they had been engaged in sexual behaviors such as multiple sex or relationship with same sex. About having multiple sex partners, participant No. 15 said:
“Four guys raped me. After all, I thought I’d nothing to lose and from then on, I began to have sex relations and it didn’t matter to me whether I’d fall sick or not, and then, I felt I was free to have any affair. It was as if I was punishing and hurting myself because of that stupidity”.
With regard to same sex relationship, participant No.12 said:
“After having some relationships with boys, I’d a feeling that I was even willing to have a relationship with my sister to get rid of it. Ever since I came to this center (the center for caring for injured girls in the Welfare office), I’m always drawn to my roommates. I want to touch them. It’s as if when I do this, I’m a little calmer and I get rid of annoying thoughts.
Participant No. 22, who was a psychologist and has repeatedly dealt with these adolescent girls, said:
Sometimes, after having many relationships, these girls have a lot of mental problems and lose calmness of their mind. They’re constantly looking for a relationship and that’s why they’re even willing to enter a relationship with same sex. These relationships aren’t accepted in our society; this issue and taboos make them unable to use reproductive health services and counseling.
Wounded psyche
Numerous psychological traumas following intercourse with the opposite sex or sexual harassment were among the barriers to the maintenance of sexual health and fertility in adolescents. Intentional or unintentional engagement in sexual intercourse has led to loss of mental and behavioral balance, rumination, and psychological problems such as depression and withdrawal in adolescent girls. Participant No. 11 said in this regard:
“After the second rape, I was very sad; because I’d lost my original boyfriend and I was notorious. My screams and shouts during the rape were constantly in my head. I was no longer bored with anyone. I was always with my mother and sister. I’d nightmares at night. I turned off my cell phone and wasn’t not ready to talk to anyone, I’d an anal fissure after the rape, but it didn’t matter to me to go to the doctor”.
The psychologist spoke about the frustration of these adolescent girls:
“First come love and the passion of youth. But because of immaturity, they can’t control their emotions. They every day enter a new relationship and constantly fail to establish these relationships. On the one hand, they feel stupid and deceived and, on the other hand, they become the subject of finger-pointing by boys and their peers. Their self-esteem is damaged by sexual conflicts, and they become indifferent to their fate and future” (participant No.26).
Neglecting the adolescent girls’ sexual and reproductive health
The findings showed that vulnerable adolescents have been abandoned in the high-risk context of society. The key decision-making organizations, as well as law and policymaking institutes have not provided a suitable support platform for promoting the sexual and reproductive health of vulnerable adolescents.
Ineffectiveness of key organizations in providing sexual and reproductive health services
Currently, key organizations, that are supposed to provide sexual and reproductive health services to vulnerable adolescents, have turned to be ineffective. The participants believed that within the national health system, there is no organizational structure to identify vulnerable adolescents and provide them with the necessary services. Participant No 16 said:
“We aren’t supported anywhere. If at the health center they find out that we aren’t married and we want to be examined or even we have something in our mind and want to tell the center psychologist about our problems with our boyfriends, they don’t support us at all; they just add to our problems because they tell our parents”.
“We’ve no written and formulated guidelines on vulnerable adolescents. Hence, we’ve no specific plans in this regard for them”
( Participant No 28 ).
Similarly, participant No 32 believed that there are no necessary policies and programs in this area:
“We left these things to psychological health unit. The Ministry has limited us not to talk about these issues. We don’t have a specific program for these children at the ministry level”
There are also no necessary interaction and cooperation among organizations involved in fighting social harms. Within the health system, misbehavior coupled with blame and the judgment of health service providers, on the one hand, and concerns about non-compliance and confidentiality of information, on the other, constitute the obstacles which prevent vulnerable adolescent girls from referring to the health system and talking about their problems. In this regard, participants 5 and 2 stated that:
“I felt afraid to go to the health center for I didn’t dare to speak about my infection as they were supposed to tell my mom” (participant No.5).
“They thought I was addicted, and said that I smelled horribly of cigarette smoke, while I didn’t smoke at all and only took methadone. After I’d a cesarean section, anyone said in the room: ‘Are you dead? Are you alive? Do you want something? Don’t you want anything?’ I’d to do my works myself, they treated me differently. I was harassed; after 4 days, I ran away and I didn’t pursue any of the problems that happened to me after the cesarean section” (Participant No. 2).
There is no specialized team in the field of sexual and reproductive health in welfare centers.
“There’s only one nurse and one doctor in the welfare center where I’m. I’m a girl and ashamed to say many things to a male doctor” (Participant No. 6).
Lack of legal, political and social support
Legislators and policymakers’ failure in considering the issue of sexual and reproductive health in adolescents and their improper functioning, absence of codified laws and support policies, prejudice in some existing laws, stigmatizing behavior by legal authorities in dealing with the issue, wrong judgmental attitudes on vulnerable adolescents and shortcomings in the legal monitoring of the issue by health sector in the field of sexual and reproductive health are serious barriers to the maintenance of the sexual health and fertility of vulnerable adolescents. Participant No 35 also admitted that:
“I know a 15-years-old girl who’d been raped several times by her father and cousins. After a while, the magistrate had voted in favor of the family as the girl, the claimant, had no witnesses. We don’t have a proper-functioning court system to pay attention to the perils facing the kids”.
“I’d not have had an abortion if the law had protected me from marrying a man who’d raped me and kept the fetus. I’d go to a safe place to have an abortion so that I’d not become so infected now; because if they find out that I’m pregnant, I can’t have an abortion, even if I’m pregnant by being rape. It’s not legal” (Participant No. 1).
Influential organizations, NGOs and philanthropists’ failure to provide social support for vulnerable adolescents has led to the loss of golden opportunities to educate and empower the adolescents. This exacerbates the vulnerability of girls. In this regard, participants No. 18 and 9 stated that:
“Unfortunately, the reality is that these kids aren’t supported by any charities or benefactors because of the misconceptions that exist with regard to them. They need to be educated and supported to become a member of the society rather than become a high-profile criminal”.
“I couldn’t go to school anymore as I was fired because of having boyfriends. Now I also carry out the stigma of coming to welfare and no school will accept me anymore. I want to study and become a useful person, but no place accepts me” (Participant No. 9).
Absence of legal support for these adolescents has made it impossible for them to live in a safe place until suitable living conditions are provided for them. This can expose them to traumatic context of the family and society, and their sexual and reproductive health is further compromised. Participant No.29 also believed that:
“But the problem is that after this short stay they’ve to go back to the family context where they don’t have a good condition. This’s because our policymaking proceedings and those who codify plans for our kids don’t support the welfare Organization at all and fail to provide safe havens for these girls so that they can stay there for a longer period of time until the family situation improves and, then, they can return to their families”.
“After here (welfare) I don’t know where to go as my family is in a bad situation. My father is addicted and my mother isn’t paying attention to me. Sometimes I’m even afraid to be at home with my dad, as he may sell me for drugs. I wish there was a place where I could stay as long as I could work and earn money” (Participant No. 9).
Stigmatization of the vulnerable adolescents by the society and treating them reproachfully, social taboos, and the fear of the consequences of expressing one’s problems, lead to the adolescents’ concealment of injuries which results in their silence and indifference to their health status and exacerbates the injury.
“The kids are afraid to express their experiences and think that nobody will accept them and they’ll not be embraced by the society. They fear of being rejected by others or their mistreatments. This’s become a big taboo for the kids.” (Participant No.20).
“I didn’t go to the doctor or the health center for examination, because they might find out that there’s something wrong with me and then start blaming and insulting me. I knew that if they came to know my problem, they would look at me as a bad girl, and I didn’t like this” (participant No. 4).
The stable family contributes significantly to providing a safe environment for the growth, development and protection of the adolescents’ health in all areas. For a variety of reasons, however, family context can be a threat to an adolescent’s health. The strict and permissive parenting styles pave the way for the tendency towards high-risk behaviors in adolescents [ 23 ]. The authoritarian and permissive educational method had also a significant relationship with exclusion of children from the home and family space [ 24 ]. The home environment turning to an unsafe environment following the parents’ harmful behaviors can pave the way for adolescent behavioral problems such as drug abuse, moral and social deviations, educational decline or school drop-out, high-risk sex and early pregnancy. Deviant family behaviors such as addiction, prison history, high-risk sexual behaviors and so on lead to inability of overseeing children’s performance adequately, and prevent their emotional needs from being met [ 25 ]. In single-parent male adolescents, parental monitoring has been reported lower than two-parent male adolescents; affiliation with delinquent peers together with high risk behaviors has been also higher than two-parent male adolescents [ 26 ]. Moral and religious beliefs in the family can also play a key role in preventing risky behaviors and social harms in adolescents [ 27 , 28 ]. Furthermore, the family rejection of vulnerable girls, parents’ inappropriate behaviors along with rebuke and humiliation, can cause adolescents to get hurt and face injuries. In Ghana, the results of a study revealed that the parents’ first reaction to the problem of pregnancy in adolescent girls is an expression of anger, exclusion of them from home or sending them to another place to prevent rumors [ 29 ].
The loss of a safe and friendly home environment helps the peer group prevail over adolescent behaviors and actions. This paves the ground for them to engage in high-risk and health-threatening behaviors. Many adolescents have stated that they obey their friends unquestionably in order to protect their friendships, be accepted by them, and escape from loneliness. They argued that they engage under the pressure and support of a peer group in high-risk behaviors such as smoking and alcohol, running away from home, or unprotected sex [ 30 ].
Another barrier to reproductive health in vulnerable adolescent girls was their inability to make informed decisions about sex and fertility. The findings showed that most families, national media, and organizations involved in adolescent health issues have not addressed adolescent’ sex education. In Islamic contexts, people’s interpretation of religious principles and the belief that sex education may stimulate premarital sex, can prevent the education of issues such as sexual and reproductive health [ 31 ]. Additionally, many mothers are opposed to extensive sex education with details to their children and the extent of maternal education to girls was found to be confined to issues related to puberty and menstruation. Of the reasons mentioned by parents in choosing this educational area, one can refer to such things as feeling ashamed, shyness and embarrassment when teaching sexual issues to their children and the fear that they may become rude and tempted to experience sexual relations [ 32 ].
After the family, using the school’s capacity can provide a good opportunity for sex education. But it seems that sex education in the public-school system across the world is a controversial topic. In Iran, the current education system faces main challenges in this regard and sex education is ignored, because premarital sexuality is not acceptable [ 33 ]. In Pakistan most of the parents and teachers believed that education of sexual affairs is in conflict with Islamic identity and ideology [ 34 ]. In contrast, in other countries, there is a strong parental support and emphasis on sex education in schools [ 35 , 36 ]. From the perspective of adolescent girls, failure to receive education on sex affairs through schools leads to unprotected sex and incidence of unwanted pregnancies [ 37 ]. Under such a situation, it is natural for adolescents to resort to various media such as the Internet, satellite channels and virtual social networks to find answers to their sexual problems. Technology can facilitate easy access to sexual information sources and provide the possibility of easy search through cyberspace, easy exchange of sex content, ease of interaction and communication with the opposite sex via mobile phones and virtual networks which may arouse sex desires through online sex networks [ 38 ].
The results of the study confirm that most vulnerable adolescent girls were not able to use communication and problem-solving skills properly in their primary encounter with high-risk behaviors. The lower the life skills, the more will be the likelihood of verbal and physical aggression, criminal behavior, and alcohol and drug abuse [ 39 ].
Vulnerable adolescent girls’ unawareness of issues related to sexual and reproductive health was another obstacle in the present study. Findings of the studies in less developed countries, including Iran, on adolescents’ reproductive health suggested that a significant proportion of adolescent girls lacked sufficient knowledge on sexual and reproductive health issues, or their understanding was limited to menstruation [ 40 ]. The research among Iranian 11–14-years-old girls indicated that their level of knowledge about sexually transmitted diseases was low and AIDS was found to be the widely seen sexually transmitted disease among them [ 41 ]. Lack of knowledge of sexual and reproductive health as well as mistrust regarding contraceptive methods are the factors that influence adolescents’ decisions about not using contraceptive methods [ 42 ]. Globally, in developing countries, adolescents’ knowledge, information and education about various sexual and reproductive health issues are not enough to make well-informed decisions in this regard. This has serious consequences for the sexual and reproductive health of adolescents [ 16 , 43 ].
Another important issue that is causally associated with the incidence of high-risk behaviors in vulnerable adolescence is the development of psychological disorders. Many vulnerable adolescent girls experience one or more intimate or non-intimate sexual harassment. A history of sexual harassment in adolescent girls has serious negative consequences for them. Different findings have revealed that going through an ordeal of sexual assault in adolescence is associated with mental health disorders (depression, anxiety), drug use, alcohol use and multiple sexual relations [ 44 , 45 , 46 ]. Sexual orientations, identities, expressions and behaviors that differ from cultural norms (sexual minoritized) may expose adolescents to adverse psychosocial and health outcomes such as victimization, depression, suicide, substance use, homelessness, sexually transmitted infections, and unplanned pregnancy. In some communities, lack of acceptance and stigmatization of specific sexual behaviors, identities, and orientations may lead to these adverse outcomes [ 47 ]. Therefore, the need for psychological support following sexual harassments, unwanted pregnancies, and abortions as well as diagnosis, treatment and follow-up of psychological disorders in vulnerable adolescents seem to be essential [ 48 ].
As all sexual and reproductive health professionals agree on the need for a comprehensive attention to adolescents’ sexual and reproductive health issues as a health priority, in the current Iranian health system, vulnerable adolescent girls are not included in health sector policies. The healthcare system lacks the necessary facilities and skilled service providers to serve and cover vulnerable adolescents. Lack of professional provider in the field of sexual and reproductive health of adolescents in the Rehabilitation Organization was also observed. The results of a systematic review show that from the perspective of service providers, clinical environment, unawareness of available services and unavailability of services are major barriers to improving the adolescents’ sexual and reproductive health. By contrast, from the perspective of adolescents, judgmental and unfriendly attitude of service providers is the key barrier to adolescents’ access and use of services [ 49 ].
Our results indicated that legal authorities have disregarded legal aspects of vulnerable adolescent girls’ sexual and reproductive health, and the existing laws have significant shortcomings in this area. In addition to the legal areas, vulnerable adolescents are also neglected in the political dimension for reasons such as severe religious, social and political pressures. In Iran government leaders and Policymakers have not accepted adolescent health as a priority due to social, cultural and religious taboos. As a result, the health sector lacks a clear policy in this regard Shariati, Babazadeh et al., [ 14 ]. Provision of good-quality and adolescent-friendly services need sound national laws and polices [ 50 ]. It seems that lack of legal and political support for adolescent sexual and reproductive health in Iran is the root cause of many problems. Therefore, our society needs to codify some policies and laws to deal with such problems.
At social level, vulnerable adolescents are not socially protected. Stigmatizing behaviors of the society, education system and healthcare providers towards vulnerable adolescents provide the conditions for more and more serious injuries. Being single as a social barrier is an obstacle for Iranian girls to access sexual and reproductive health services [ 51 ]. Iranian society’s emphasis on abstinence until marriage shapes the stigma for sexual and reproductive health issues of unmarried women and restricts their use of sexual and reproductive health services [ 52 ]. As a result, existence of weak protective laws for vulnerable adolescents, on the one hand, and the stigmatization by some NGOs, on the other, have prevented this group from taking benefits of the financial and supportive assistance provided by these organizations. Looking at the activities of non-governmental organizations supporting adolescents in other countries shows that the positive attitude of these organizations in solving problems related to social harms of adolescents helps them participate in meeting the financial and educational needs of vulnerable adolescents. Findings of a study in Tanzania demonstrated that many NGOs have informally begun to teach issues related to sexual and reproductive health as the incidence of high-risk behaviors have been increasing among 12–16-years-old adolescents. However, the negative views of some non-governmental organizations also hinder the assistance and support of vulnerable adolescents [ 53 ].
Disregard for the sexual and reproductive health of vulnerable adolescents can generate irreparable consequences for society; but numerous individual, family, social, legal and political barriers in Iran have challenged the necessary platform to ensure a context to deal with this problem. Accordingly, it seems that the obstacles can possibly be overcome by developing a comprehensive and practical program and providing legal and political support for this issue.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
World Health Organization. Defining sexual health: report of a technical consultation on sexual health, 28–31 January 2002. Geneva: World Health Organization; 2006.
Google Scholar
Hashemiparast MS, Sedighian M, Asghari Jafarabadi M, Allahverdipour H. Explaining risky and unprotected sexual behaviors among young people and related reasons: a qualitative study. Scientific Journal of Kurdistan University of Medical Sciences. 2017;22(4):111–24.
Osborne V, Striley CW, Nixon SJ, Winterstein AG, Cottler LB. Sex differences in patterns of prescription opioid non-medical use among 10-18 year olds in the US. Addict Behav. 2019;89:163–71.
Article PubMed Google Scholar
Soleimaninia. Gender differences in adolescents committing all kinds of risky behavior. Youth Stud. 2010;8–9:73–86.
Garmaroudi GR, Makarem J, Alavi SS, Abbasi Z. Health related risk behaviors among high school students in Tehran, Iran. Payesh J. 2010;9(1):13–9.
World Health Organization. Sexual health and its linkages to reproductive health: an operational approach. 2017. Available from: https:// www.who.int/reproductivehealth/publications/sexual_health/sh-linkages-rh/en/ .
World Health Organization. Sexually transmitted infections. 2019. Available from: https:// www.who.int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis ).
Shannon CL, Klausner JD. The growing epidemic of sexually transmitted infections in adolescents: a neglected population. Curr Opin Pediatr. 2018;30(1):137.
Article PubMed PubMed Central Google Scholar
Statistics Center of Iran. Results of the population and housing census [Internet]. 2016. Available from: www.amar.org.ir .
World Health Organization. adolescent pregnancy 2020. Available from: https:// www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy .
World Health Organization. Overcoming barriers to adolescent health education and services.2021 [cited 2021 5/6/2021]. Available from: https:// www.who.int/reproductivehealth/topics/adolescence/education/en/ .
International Labour Organisation (ILO) United Nations Children's Fund (UNICEF). GirlForce: skills, education and training for girls now. 2018. Available from: https://www.unicef.org/sites/default/files/2018-10/Unicef_DayoftheGirl_Brochure_R7.pdf .
World Health Organization. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: World Health Organization; 2013.
Shariati M, Babazadeh R, Mousavi SA, Najmabadi KM. Iranian adolescent girls’ barriers in accessing sexual and reproductive health information and services: a qualitative study. Journal of Family Planning and Reproductive Health Care. 2014;40(4):270–5.
Shams M, Mousavizadeh A, Majdpour M. Mothers’ views about sexual health education for their adolescent daughters: a qualitative study. Reprod Health. 2017;14(1):1–6.
Article Google Scholar
Woog V, Susheela S, Alyssa B, Jesse P. Adolescent Womens need for and use of sexual and reproductive health Services in Developing Countries: Guttmacher institute. New York: Guttmacher Institute; 2015.
Vogel JP, Pileggi-Castro C, Chandra-Mouli V, Pileggi VN, Souza JP, Chou D, et al. Millennium development goal 5 and adolescents: looking back, moving forward. Arch Dis Child. 2015;100(Suppl 1):S43–S7.
Kennedy E, Gray N, Azzopardi P, Creati M. Adolescent fertility and family planning in East Asia and the Pacific: a review of DHS reports. Reprod Health. 2011;8(1):1–12.
Pourkazemi R, Janighorban M, Boroumandfar Z, Mostafavi F. A comprehensive reproductive health program for vulnerable adolescent girls. Reprod Health. 2020;17(1):13.
Graneheim UH, Lindgren B-M, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017;56(29–34):23.
Holloway I, Galvin K. Qualitative research in nursing and healthcare. New Jersey: John Wiley & Sons; 2016.
Graneheim UHLB. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Article PubMed CAS Google Scholar
Shokri N, Yusefi M, Safaye Rad I, Akbari T, Musavi S, Nazari H. Correlation between risky behaviors in the pre-university adolescent students in Hamadan with Parents' child raising method. JHPM. 2015;5(1):73–82.
Safdar S, Zahrah SM. Impact of parenting styles on the intensity of parental and peer attachment: exploring the gender differences in adolescents. Am J Appl Psychol. 2016;4(2):23–30.
Farzaneh S, Molania S, Zamani RE. A survey of family factors affecting 1218 years old Adolescentr's attitude towards delinquency in Department of Correction and Rehabilitation of Gorgan City. Sociological Studies of Youth. 2017;6(18):73–89.
Dargahi S, Rezaei Sharif A, Khodadadi Sangdeh J, Nazari M, Bakhtiari Z. Comparing parental monitoring, affiliation with delinquent peers, and high-risk behaviors in single-parent and two-parent male adolescents. Journal of Research and Health. 2018;8(5):411–7.
Ameri Z, Mirzakhani F, Nabipour AR, Khanjani N, Sullman MJM. The relationship between religion and risky behaviors among Iranian University students. J Relig Health. 2017;56(6):2010–22.
Shek DTL, Zhu X. Self-reported risk and delinquent behavior and problem behavioral intention in Hong Kong adolescents: the role of moral competence and spirituality. Front Psychol. 2018;9:430.
Aziato L, Hindin MJ, Maya ET, Manu A, Amuasi SA, Lawerh RM, et al. Adolescents' responses to an unintended pregnancy in Ghana: a qualitative study. J Pediatr Adolesc Gynecol. 2016;29(6):653–8.
Ghorbani A, Jomenia SJ. The role of social factors (family, school, peer group) in socialization of students in Golestan province. J Appl Sociol. 2018;29(2):113–28.
Tabatabaie A. Childhood and adolescent sexuality, Islam, and problematics of sex education: a call for re-examination. Sex Education. 2015;15(3):276–88.
Majdpour M, Parhizkar S, Mousavizadeh A, Shams M. Mothers’ views about sexuality education to their adolescent girls. A qualitative study J Tolooebehdasht Sci. 2017;16(3):93–105.
Tabatabaie A. Constructing the ideal Muslim sexual subject: problematics of school-based sex education in Iran. Sex Education. 2015;15(2):204–16.
Nadeem A, Cheema MK, Zameer S. Perceptions of Muslim parents and teachers towards sex education in Pakistan. Sex Education. 2021;21(1):106–18.
Kantor L, Levitz N. Parents’ views on sex education in schools: how much do democrats and republicans agree? PLoS One. 2017;12(7):e0180250.
Millner V, Mulekar M, Turrens J. Parents’ beliefs regarding sex education for their children in southern Alabama public schools. Sexuality Research and Social Policy. 2015;12(2):101–9.
Krugu JK, Mevissen F, Prinsen A, Ruiter RA. Who’s that girl? A qualitative analysis of adolescent girls’ views on factors associated with adolescent pregnancies in Bolgatanga. Ghana Reproductive health. 2016;13(1):1–12.
Taleghani F, EaSM K, Noroozi M, Tavakoli M, Gholami A. The role of mass media in Iranian youth’s premarital sexual relationships: a qualitative study. International journal of community based nursing and midwifery. 2017;5(1):91.
PubMed Google Scholar
Ahmadi H, Moeini M. An investigation of the relationship between social skills and high risk behaviors among the youth: the case of shiraz city. Strategic Rssearch on Social Problems in Iran University of Isfahan. 2015;4(1):1–24.
Mirzaii Nagmabadi K, Babazadeh R, Shariati M, Mousavi SA. Iranian adolescent girls and sexual and reproductive health information and services: a qualitative study. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2014;17(92):9–18.
Afshary P, Pazhohideh SZ, Yazdi Zadeh H, Mohammadi S, Tabesh H. Survey educational needs of 11-14 years old girls about sexual health. Journal of Holistic Nursing And Midwifery. 2016;26(1):1–9.
Shahabuddin A, Nöstlinger C, Delvaux T, Sarker M, Bardají A, Brouwere VD, et al. What influences adolescent girls’ decision-making regarding contraceptive methods use and childbearing? A qualitative exploratory study in Rangpur District, Bangladesh. PLoS One. 2016;11(6):e0157664.
Article PubMed PubMed Central CAS Google Scholar
Ivanova O, Rai M, Mlahagwa W, Tumuhairwe J, Bakuli A, Nyakato VN, et al. A cross-sectional mixed-methods study of sexual and reproductive health knowledge, experiences and access to services among refugee adolescent girls in the Nakivale refugee settlement. Uganda Reproductive health. 2019;16(1):1–11.
Norcott C, Keenan K, Wroblewski K, Hipwell A, Stepp S. The impact of adolescent sexual harassment experiences in predicting sexual risk-taking in young women. Journal of interpersonal violence. 2021;36(15-16):NP8961.
Reed E, Salazar M, Agah N, Behar AI, Silverman JG, Walsh-Buhi E, et al. Experiencing sexual harassment by males and associated substance use & poor mental health outcomes among adolescent girls in the US. SSM-population health. 2019;9:100476.
McGinley M, Rospenda KM, Liu L, Richman JA. It isn't all just fun and games: collegiate participation in extracurricular activities and risk for generalized and sexual harassment, psychological distress, and alcohol use. J Adolesc. 2016;53:152–63.
UpToDate. Lesbian, gay, bisexual, and other sexual minoritized youth: Epidemiology and health concerns -. (n.d.). Retrieved October 11, 2021, Available from: https://www3.utdos.ir/contents/lesbian-gay-bisexual-and-othersexual-minoritized-youth-epidemiology-and-health-concerns?search=masturbation&source=search_result&selectedTitle=10~118&usage_type=default&display_rank=10 .
Pourkazemi R, Janighorban M, Mostafavi F, Boroumandfar Z. Reproductive and sexual health facilitators and needs of vulnerable adolescent girls. International Journal of Body, Mind and Culture. 2020;7(4):184-95.
Onukwugha FI, Hayter M, Magadi MA. Views of service providers and adolescents on use of sexual and reproductive health services by adolescents: a systematic review. Afr J Reprod Health. 2019;23(2):134–47.
Chandra-Mouli V, Parameshwar PS, Parry M, Lane C, Hainsworth G, Wong S, et al. A never-before opportunity to strengthen investment and action on adolescent contraception, and what we must do to make full use of it. Reprod Health. 2017;14(1):1–13.
Kohan S, Mohammadi F, Mostafavi F, Gholami A. Being single as a social barrier to access reproductive healthcare services by Iranian girls. Int J Health Policy Manag. 2017;6(3):147.
Mohammadi F, Kohan S, Mostafavi F, Gholami A. The stigma of reproductive health services utilization by unmarried women. Iran Red Crescent Med J. 2016;18(3):e24231.
Cardoso JC, Mwolo MP. Assessment of non-formal sexual education strategies for adolescent girls: the case of Tanzania. Ensaio: Avaliação e Políticas Públicas em Educação. 2017;25(95):527–47.
Download references
Acknowledgements
We would like to express our gratitude to the Vice-chancellor for Research of Isfahan University of Medical Sciences for their support and all the participants who shared their experiences with us.
Research deputy of Isfahan University of medical sciences.
Author information
Authors and affiliations.
Department of Midwifery and reproductive health, Nursing and Midwifery Care Research Center, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran
Mojgan Janighorban
Reproductive Sciences and Sexual Health Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Zahra Boroumandfar
Nursing and Midwifery Care Research Center, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran
Razieh Pourkazemi
Department of Health Education and Promotion, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
Firoozeh Mostafavi
You can also search for this author in PubMed Google Scholar
Contributions
MJ designed the work, analyzed and interpreted the data, was a major contributor in writing the manuscript; ZB analyzed and interpreted the data, was a major contributor in writing the manuscript, RP designed the work, analyzed and interpreted the data, FM designed the work. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Zahra Boroumandfar .
Ethics declarations
Ethics approval and consent to participate.
This research was approved by the Ethics Committee of Isfahan University of Medical Sciences with the ethics code of IR.MUI.RESEARCH.REC.1398.396. The participation of the participants in this study was completely voluntary and informed written consent was obtained from them. The informed consent was obtained from the parents or their legal guardian or legally appointed representatives of girls with age less than 16 years. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Janighorban, M., Boroumandfar, Z., Pourkazemi, R. et al. Barriers to vulnerable adolescent girls’ access to sexual and reproductive health. BMC Public Health 22 , 2212 (2022). https://doi.org/10.1186/s12889-022-14687-4
Download citation
Received : 26 February 2022
Accepted : 21 November 2022
Published : 29 November 2022
DOI : https://doi.org/10.1186/s12889-022-14687-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescent health
- Sexual and reproductive health
- Sexual and reproductive health services
- Qualitative study
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 24 January 2018
Adolescents’ reproductive health knowledge, choices and factors affecting reproductive health choices: a qualitative study in the West Gonja District in Northern region, Ghana
- Joseph Maaminu Kyilleh 1 ,
- Philip Teg-Nefaah Tabong 2 &
- Benson Boinkum Konlaan 3
BMC International Health and Human Rights volume 18 , Article number: 6 ( 2018 ) Cite this article
66k Accesses
51 Citations
18 Altmetric
Metrics details
In Ghana, adolescents constitute about a quarter of the total population. These adolescents make reproductive health decisions and choices based on their knowledge and the availability of such choices. These reproductive health decisions and choices can either negatively or positively affect their lives. This study therefore explored adolescents’ reproductive health knowledge and choices, the type of choices they make and the factors that affect these choices.
This qualitative study adopted a narrative approach to qualitative enquiry. Eight focus group discussions ( N = 80) were conducted among both in-school and out-of-school adolescents aged 10–19 years. The discussions were stratified by sex and studentship. In addition, nine in-depth interviews were conducted with various stakeholders in reproductive health services and community opinion leaders. Both the focus group discussions and in-depth interviews were recorded, transcribed and analysed using NVivo 11. Thematic analysis was employed in analysing data.
The study found that knowledge on reproductive health choices was low among respondents with majority of them relying on their peers for information on sexual and reproductive health. Having a sexual partner(s) and engaging in premarital sex was common and viewed as normal. Adolescents engaged in unprotected sexual practices as a way of testing their fertility, assurance of love, bait for marriage and for livelihood. Inserting herbs into the vagina, drinking concoctions and boiled pawpaw leaves were identified as local methods employed by adolescents to induce abortion. Reproductive health services were available in the community but received low utilization because of perceived negative attitude of health workers, confidentiality and social norms.
Conclusions
Adolescents in this study generally engaged in risky reproductive health choices that can negatively affect their reproductive health. Adolescents in this part of Ghana have challenges utilizing available reproductive health services because of socio-cultural and health system barriers.
Peer Review reports
Adolescence is a period of life during which individuals reach sexual maturity [ 1 ]. It is the period of transition from childhood to adulthood and it is often characterized by biological and psychosocial changes as well as sexual experimentation [ 2 ]. Globally, adolescents constitute about one billion of the world’s population, with 70% living in developing nations [ 3 ]. In sub-Saharan Africa, young people constitute about 33% of the 973.4 million population. The population of adolescents and young adults is expected to continue to increase over the next 35 years [ 4 , 5 ]. In sub-Saharan Africa, where a fourth of all adolescents are reported to have sexual experience, education on sexual and reproductive health are generally reported to be low [ 3 ]. In Ghana, the 2010 Population and Housing Census reported that the ratio of adolescents between 10 and 19 years to the total population is 1: 4.5; meaning this age group constitute about 22.4% of the national population [ 6 ]. In the northern region of Ghana, adolescents between 10 and 19 years are about 22.3% of the regional population and about 10.1% of the national adolescents’ population [ 7 ].
Evidence abound that adolescents experience very critical and life defining events, namely; first marriage, first sexual intercourse, and parenthood [ 8 ]. The downward trend in age at menarche from 15.5 years [ 9 ] to an average of 12–13 years in most developing countries [ 10 ] also means an increase in the interval between menarche and marriage. According to the Ghana National Population Council, the age at first marriage was 18.3 years for females and around 25 years for males in 1988, but this age has increased to around 21.4 years for females living in urban areas and 20.9 years for their counterparts in rural areas. For males, it increased to 26.1 years (urban residents) and 24.9 years for rural dwellers [ 11 ].
Adolescents’ knowledge and access to reproductive health services is important for their physical and psychosocial wellbeing. It has been found in an earlier study that the lack of knowledge about the consequences of unprotected premarital sex among adolescent females predisposed them to unwanted pregnancies, unsafe abortion and its complications, and sexually transmitted infections [ 12 ]. According to the 2014 Ghana Demographic and Health Survey (GDHS), about 14% of females aged 15–19 years had begun child bearing. Of these 14%; about 11% have had a life births and 3% were pregnant at the time of the survey [ 13 ]. Abstinence, use of condom, use of contraceptives, decision to keep a pregnancy, use of safe abortions services are some of the choices and reproductive health decisions adolescents make [ 14 ]. The International Conference on Population and Development (ICPD) which was held in Cairo in 1993 recognised the negative effects of risky sexual behaviour. Several countries including Ghana were implored to institute measures to ameliorate the situation [ 15 ]. Therefore, adolescent-friendly reproductive health services and comprehensive abortion care were instituted in Ghana to increase access to reproductive health and safe abortion services. This notwithstanding, many adolescents still encounter significant obstacles in accessing sexual and reproductive health services [ 16 ]. Knowledge on reproductive health services is essential to enable them make informed choices. The type of choices made by these young adults could either impact positively or negatively on their lives, their families and the society at large [ 15 ]. This study therefore explored adolescents’ knowledge about reproductive health and choices, what choices they make and the factors that affect those choices.
Study design
This study adopted a narrative approach to qualitative enquiry. Narrative research allows participants in a study to share their experiences in the community [ 17 ]. Since the researchers were interested in exploring the adolescents’ knowledge on reproductive health services and choices, factors affecting their reproductive health choices, and how these choices affects their lives, the narrative approach was deemed appropriate [ 18 ]. We conducted focus groups discussions with adolescents and individual interviews with stakeholders. In this study, we adopted the ecological model (Fig. 1 ). The ecological model provides a framework for understanding the multiple and interacting factors of adolescent sexual and reproductive health behaviour and their effects [ 19 , 20 ]. This framework posits that adolescent sexual and reproductive health behaviour and their choices are influenced by interpersonal, organisational, community and public policy factors. This model recognises that these factors (interpersonal, organisational, community and public policy) interact across different levels, focus on specific health behaviour and that interventions that address the multiple levels are more effective [ 21 ]. In the entire research process, steps were taken to adhere to the requirements of RATS guideline for conducting and reviewing a qualitative research [ 22 ].
Ecological model for adolescents’ reproductive health choices and factors influencing the choices [ 20 ]
The study was conducted in the West Gonja district of the Northern region of Ghana. The West Gonja district is one of the 26 districts in the region which lies within the savannah belt. The district has an estimated population of 46,803 with an annual growth rate of 2.9%. There are four major religious groups in the district, namely: Islam (about 70%), Catholics (10%), Protestants (8%) and Traditional Worshippers (12%) [ 23 ]. The 2011 and 2012 annual reports of the West Gonja District Health Directorate showed that the district recorded 13.7% and 14.4% of teenage pregnancies with 9.9% and 11.4% delivery rates respectively.
Selection of participants and data collection
The participants in this study were adolescents aged 10–19 years who lived in the West Gonja District at the time of the study. Both male and female in-school and out-of-school adolescents were recruited for the study. The communities were selected based on two criteria; high school dropout rates and teenage pregnancies. The researcher first collected the annual reports from the district and based on that communities were grouped into two; those with high teenage pregnancy and school dropout rates; and those with low teenage pregnancies and school dropout rates. From each category four communities were selected where the study was conducted. At the community level, school authorities were contacted for approval to recruit in-school adolescents. However, for the out-of-school participants, these were selected through the assistance of community leaders.
For stakeholders in adolescents’ sexual and reproductive health, a purposive sampling technique was used. In purposive sampling technique, researchers choose the sample based on who they think are appropriate for the study [ 24 ]. Hence, community opinion leaders and health workers who provide adolescent reproductive health services were selected.
Two main data collection strategies were employed in this study namely; focus group discussions (FGDs) and in-depth interviews (IDIs). Focus group discussion (FGD) refers to a qualitative data collection method where between 6 and 10 individuals with similar background or experiences are brought together to discuss a specific topic of interest with a researcher [ 25 ]. Thus, the use of focus group allows small number of participants to discuss a study topic led by a moderator using a discussion guide [ 26 ]. The focus discussion groups were homogenous for sex and studentship. The FGDs aimed at capturing the local context of sexual and reproductive health of the adolescents and, to enable the investigators get a true picture of the social reality. The FGD guide focused on individual, relationship, and community level factors that affect adolescents’ reproductive health knowledge and choices as required by the ecological framework used for this study. With the aid of an interview guide the investigators introduced the topic to the group and gave them leeway to express themselves. Their responses gave room for further probes. Participants’ responses were written in a field note book and recorded using a digital recorder as well.
Eight FGDs were conducted; four among in-school adolescents (2 males, 2 females) and four among adolescents who were out of school (2 males, 2 females). Each group comprised of 10 discussants making a total of 80 participants in all. Some of the adolescents were married whilst others were not married.
In-depth interviews using semi-structured topic guide were conducted with individuals who were engaged in reproductive health services in the district as well as opinion leaders in the community. This was done to elicit information on both community and the health service related factors that may inform the choices that adolescents make. In all nine IDIs were conducted among various stakeholders. The stakeholders were: one medical doctor, one public health nurse, two midwives, two community health nurses, two community opinion leaders (1 male, 1 female) and the programme manager of World Vision International, a non-governmental organisation engaged in child and adolescent educational programmes in the study area. The data collection was ended at the point of saturation as required in qualitative research [ 24 ]. The IDI topic guide covered areas such community and health system related factors, policies and strategies to ensure safe reproductive health practices among adolescents in line with the societal construct in the ecological model.
Data analysis
Data collected during the FGDs and IDIs were digitally recorded and transcribed verbatim. The field notes were converted into data documents. All transcripts were reviewed by an independent person who is an experienced qualitative researcher. In the review, the independent person listened to the recorded voices and compared the voices with the transcripts. Qualitative narrative data in English were then entered into a word processor (Microsoft Word) and imported into NVivo 11 for analysis.
Thematic analysis was employed in analysing the data. Thematic data analysis process involves data reduction, data display and data conclusion-drawing/verifying [ 27 ]. Line-by-line coding of the various transcripts were done as either free nodes or tree nodes. Queries (analysis in Nvivo) were performed to compare the coding against nodes and attributes to compare and contrast within-group and between-group responses and themes.
Knowledge on reproductive health services and choices
The results from the study revealed that both in-school and out-of-school adolescents had little or no understanding of adolescent reproductive health services and choices. However, some adolescents (15 in-school, and 6 out-of-school) were able to identify abstinence, use of condoms, and other contraceptives to prevent unplanned pregnancies. The following quotes illustrate the understanding of participants as to what reproductive health services are all about:
“Reproductive health services are the service that teach us how to protect ourselves from getting pregnant through the use of condom during sex…also use contraceptives though it is sometimes difficult for us to use contraceptive” (female, FGD, in-school).
“As adolescents, we have to make choices between not having sex until we are married, or if we cannot wait we have to use contraceptive methods that would prevent us from becoming pregnant” (Female, FGD, in-school).

Sources of reproductive health knowledge
FGDs respondents identified peers, parents, teachers, radio and television as the main sources of information on reproductive health. However, most of the adolescents especially those out of school relied mostly on their peers for information on reproductive health. The results showed that parents were an important source of information. For in-school adolescents, teachers emerged as another important source of information on reproductive health as it was unanimous among FGD participants. The following are quotes from some participants to illustrate these views:
“….the major sources of information are through our teachers and nurses. Most of us actually prefer getting our “filla” [information] from our friends and sometimes nurses” (female, FGD, in-school).
“…we get some information from the schools we attend. Sometimes too our parents give us some of the information we need in the form of a warning. I think most of the time when we discuss about it with friends we get to know more about the issues” (male, FGD, in-school).
“When we meet our friends who are more experienced they teach us how to protect ourselves from becoming pregnant. If you have a problem then you bring it out and people will advise you appropriately” (female, FGD, out-of-school).
The study also found that health workers generally believed that there was the need to provide adolescents with reproductive health information. Therefore health education sessions are organized in schools by trained nurses to talk to the students about sexual and reproductive health matters. This opinion is captured in the following statements:
“We have arranged with the schools so that from time to time we give them health talks on sexual and reproductive health” (Midwife-1, IDI).
“In one of the communities here, we noticed that teenage pregnancy was very common resulting in high school dropout rate among female adolescents. So we organised to go and educate them and also provide them with some contraceptives at the school, but the school authorities did not agree. When the community heard about it, they sent a delegation to warn us to desist from such acts. They said we wanted to encourage premarital sex. But you see, the teenagers were becoming pregnant and when you ask about the one responsible, you see it is usually an adult not a colleague teenager” (Public Health Nurse, IDI).
Views on having sexual partners and premarital sex
The findings of this study showed that having multiple sexual partners was considered a source of pride among both male and female participants. It emerged also that while the adolescent male had adolescent female as partners; majority of their counterparts (females) had adult males as partners. The following are quotes from the FGDs to buttress these points:
“As for boyfriends most of us have them, and some girls have sexual intercourse with their boyfriends. So teen pregnancies among the youth are uncountable around here” ( female, FGD, in-school).
“Abstinence among the youth is very difficult. Some people try to abstain from having intercourse, but they are usually described in derogatory terms such as; your penis is not good or manhood is not working” ( male, FGD, in-school).
“For us males, our sexual partners are our colleagues but for the females, their partners are mostly adults. So it is common to find a female having multiple partners because they will have one schoolmate as a boyfriend and an adult who will be providing her with material things and money” ( male, FGD, out-of-school).
Furthermore, both adolescents and stakeholders in this study perceive that sexual activities was rife among both in-school and out-of-school adolescents. The reasons adduced for adolescent engaging in sexual activities include: for sexual pleasure, to comply with his/her group norms, for gifts and also as an expression of love to their partners. Though adolescents in this study acknowledged that premarital sex is risky, it was equally generally believed to be worth the risk and therefore perceived to be indispensable. It also emerged that having sex with multiple partners by female adolescents was common especially sexual activities for gifts or favour from men. The following quotes support these points:
“Their expectations are that they will marry each other. Some expects to have fun and feel good as a girl or boy. Others expect support like money, gifts, clothing and other things from the boyfriend or the girlfriend. Some too expect trust from their girlfriends such that the girl should not have any other boy as a friend” (male, FGD, out-of-school).
“Yes the risk is there because one can get pregnant by having sex but we still do it. You can also get other sicknesses by having sex but what can we do? We have to do it to get what we want” (female, FGD, in-school).
“For us girls, it mostly for gifts from adults. Sometimes, there is nothing you can do about it because that adult is the one taking care of you so you risk losing him to another girl if you do not oblige. My first sex was with a man taking care of me. When I wanted to resist, he threatened to stop taking care of me and get another girl. So because of that I agreed” (female, FGD, in-school).
Interview with community opinion leaders revealed that this practice was really common and many female adolescents relied on it for their upkeep and also to take care of their education. Despite acknowledging this fact, opinion leaders we interviewed believed that advocating for the use of contraceptives was not the way to go. In their view, modern contraceptives can cause infertility among female users. To community opinion leaders, men who are not biological parents to adolescent females take care of their educational needs with the intention of marrying them in future. Also, a woman’s ability to beget children for the husband was perceived as a reward for the investment the man made in her education. So, with the belief that modern contraceptives could cause infertility, their use was seen as something that could lead to a loss in the man’s investment in the adolescent female. The following quotes illustrate these points:
“Premarital sex is very common in the community and for the girls, it is the adults that take them as their partner. Because of poverty, the girls have to rely on these adults for money and upkeep, so they take advantage of them” (Female, Opinion Leader, IDI).
“As for the contraceptives, the men will not agree because, it is believed that it can cause infertility in future. Men in this community take care of female adolescents to marry and have children with them in future. So, if the girl uses contraceptives and become infertile in future, it will mean the man has invested in vain. It is a serious problem, so some NGO is assisting the girls” (Male Opinion Leader, IDI).
The study also explored the use of condoms during such premarital sex since the use of female contraceptives were deemed inappropriate. Adolescents in this study believed most of them engage in unprotected sex. Condoms were believed to inhibit the pleasure in sex and since many engaged in sex for pleasure, the use of a condom was also regarded as impracticable. Another reason for the non-use of condom during sex was the inconvenience or challenges involved in getting one. Some adolescents were of the view that it was difficult going to buy condoms. This is because an adolescent who goes to buy a condom will be perceived as a “bad boy or girl” In their opinion, many of the drugstore sellers in the community know their parents. Therefore they were afraid the sellers may convey that information to their parents. The following quotes illustrate these points:
“Oh yes, condom is a waste of time and no feelings. Everything in life there is a risk and sex itself is a risk. The risk is there in having sex because most do not use condoms; some too have about two or more girlfriends and always have sex with all of them. Through that you can get any disease or even impregnate a girl that you may not even like to marry or have a child with” (male, FGD, out-of-school).
“Yes sometimes when you want to have sex you tell the boy to use condom. Some males agree and use but there are some males who will tell you that if you put a toffee with the wrapper in your mouth do you get the sweetness of the toffee?” ( female, FGD, out-of-school).
“You know, the condoms are sold at drug stores so when you want it, it is difficult to go there and buy especially us the girls. Yes, because of your age some say, you are too small to buy condoms” (female adolescent, FGD in-school).
“….Young people feel shy or afraid to buy condoms because the chemist shop owner may go and tell your parents that you have started using condoms or having sex” (male adolescent, FGD in-school).
Common strategies adopted to prevent pregnancy
This study explored what adolescents do to prevent getting pregnant. The results revealed that local remedies were available and widely used by community members. One of the strategies adopted by adolescents to prevent pregnancy is the use of a local herb called “yigewulso”. This herb is believed to have contraceptive effects. Other herbs also believed to have similar effects are used as emergency contraceptives after unprotected sex. This study also found that some adolescents believed that wearing of some local beads around the waist during sexual intercourse could prevent a pregnancy outcome. The following quotes serve to illustrate their views:
“We have this herb called “yigewulso” which is usually taken before sexual intercourse if you don’t want to get pregnant” (male, FGD, in-school).
“If you have sexual intercourse and you don’t want to be pregnant, you have to take “kaligutim” immediately. Normally, we buy it from the local chemist shop. It can be used either as an emergency contraceptive or when you miss your period” (Female, FGD, Out-school).
“In this community there is a belief that you can prevent getting yourself pregnant if you wear beads in your waist during sexual intercourse. This is why most girls wear beads around the waist before they have sex. Even women who are breastfeeding babies also wear beads to avoid pregnancy while the child is still young”. (IDI, Midwife-1).
These adolescents also reported that other techniques they employed to prevent pregnancy outcome was for the female to lie in the prone position or wash her vagina with soap and water immediately after sexual intercourse. These practices in their opinion would evacuate or kill the sperms in their vagina. They were also of the view that these practices were safe and produced no adverse effects. They had this to say:
“I was told by my friend that when you wash your vagina with soap and water and also lie on your stomach (prone position) immediately after sex, you won’t get pregnant. So, we do it to prevent pregnancy” (female, FGD, out-of-school).
“ ..Some of the traditional methods are better. If your girlfriend knows them and practice them there is no way she will get pregnant, and won’t have problems like those who use the modern contraceptive method” (male, FGD, out-of-school).
Unplanned pregnancies, abortions and sexually transmitted infections
Participants in this study were of the view that unplanned pregnancies were common among adolescents in the district. It emerged that some adolescents in this community believed that getting oneself pregnant was the guarantee or proof of one’s fertility. Male adolescents will also test their manhood by insisting on having unprotected sexual intercourse with the partner and hoping to be told she had “missed her period” (meaning she is pregnant). Sometimes the females may also prefer to have unprotected sexual intercourse in the hope of becoming pregnant as a bait for marriage as well as test for future fertility. The following quotes support these assertions:
“A lady became pregnant and she decides to abort it because she has nobody to take care of the baby. Another lady became pregnant for a guy she loved but her parents disapproved of their relationship because the boyfriend was not doing any work” (Female, FGD, out-of-school).
“Their knowledge level is little. This is because, data gathered in the district indicates high rate of teenage pregnancy and sexually transmitted infections” ( IDI, Midwife-2).
“In this community some of the girls try to get pregnant intentionally to show that they are fertile. Even a girl can tell the colleague you have been having sex with your boyfriend without ever becoming pregnant, it means either you or boyfriend is infertile” (IDI, Opinion Leader).
The results from this study also suggest that most of these unplanned pregnancies are aborted through unsafe practices using a combination of methods such as drinking concoctions of boiled pawpaw leaves, Nescafe, grinded bottles, alcoholic beverages and inserting herbs into the vagina. Participants in this study were of the view that these methods of terminating pregnancy are widely used in the community. The information gathered by this study suggest that some of the unsafe abortions have often resulted in fatal outcomes as illustrated by the following quotes:
“In fact we have plenty illegal abortion in this district particularly in Damongo town. For example one girl just died here last week. What we found out later was that she was given grinded bottles to drink. It is a very common practice” (IDI, Midwife).
“….A friend recently got pregnant and decided to abort using “Salaamalekum” leaves [herb] to do the abortion. Some also use some type of fruits, pawpaw leaves, Nescafe and sugar, alcoholic and non-alcoholic drinks as well as broken bottles to cause the abortion” ( female, FGD, out-of-school).
“I know a girl who was pregnant and the boyfriend bought malt and mixed it with grinded bottle and gave it to her and she drank, few hours after drinking that she bled and finally died” (female, FGD, in-school).
Participants in this study also indicated that sexually transmitted infections (STIs) were common in the community. They attributed this to the youth practicing unprotected sexual intercourse with multiple partners. In their opinion, there is risk in every activity. So it was normal to enjoy sexual intercourse and treat any STI that may arise. The following quotes illustrate these points:
“Sexually transmitted infections especially white (candidiasis) is very common among the females in the area. Often when they come they will just say…madam I have white and we have to test them for STIs” (IDI, Midwife-3).
“The STIs you are talking about is very common in this community because many of the youth have multiple partners which they call it “inter” and “exter” one in your school and one outside your school” (male, FGD, in-school).
“There is risk in everything we do, so it is better to enjoy yourself during sexual intercourse and if you get a disease, you treat it. I don’t ask the man to use condom, I don’t like it myself” (female, FGD, in-school).
Access to reproductive and sexual health services in the community
The findings of our study show that reproductive health services are generally available in the community. There are outreach services for the communities. These include; health education, counselling, and provision of contraceptive services. The study also found that adolescents were generally aware of some of these services and how to access them except for comprehensive abortion care. The following quotes illustrate these points:
“We have service-points for adolescent reproductive health service in this district where we provide education, counselling, contraceptive service and comprehensive abortion care to adolescent who visit us” (IDI, Public Health Nurse).
“There are outreach services for communities where there is no clinic or hospital to provide reproductive health service” (IDI, Midwife-2).
“The nurses have been coming to tell us that we can come to them for reproductive health service, so we know those services are available at the hospitals and clinics” (female, FGD, in-school).
The above notwithstanding, the results of this study show that there were some barriers to accessing these services. Four main sub-themes emerged in this respect, namely; sociocultural, attitude of service-providers, lack of privacy and confidentiality on the part of service providers and finally perceived adverse effects. The study found that the community generally perceived issues about sexual and reproductive health as only suitable for adults. Therefore, it was the general believe that it would be inappropriate to discuss such issues with adolescents. Though health workers were trained to provide these services to adolescents, there was the general believe and fear among adolescents that they may be scolded or described as “bad boys or girls” if they should go for such services. Some adolescents were also of the view that health care providers do not treat adolescents who seek for reproductive sexual health services well. The poor attitude of health providers towards adolescents deters the later from patronizing the available services.
Another barrier reported in this study was the lack of privacy. Adolescents who participated in this study were of the view that the service points did not provide enough privacy and confidentiality. In their opinion, the present environment does make it possible for people to see adolescents who seek such services as ‘spoilt children’ or may even conclude that you have come to do abortion or contraception. Another issue of confidentiality was the general believe that service providers sometimes tell parents of adolescents who seek such services that their ward was sexually active. The following quotes support these points:
“In this community, if an adolescent ask about sexual and reproductive issues, the person will be seen as a bad girl or boy. So we are afraid to go to the clinic and hospital for such services. Imagine a girl going to the hospital to do something and the information comes out that you went there to do abortion. People will say you are bad, and if you are not lucky, the information could spread to all over town the next day” (female, FGD, out-of-school).
“… Some of the nurses are not polite especially to us the young people. You go there with a problem then they will be shouting at you or even insulting you saying you are bad girl or boy. The authorities should punish or even sack such people, but you see, some of us do complain about these things but nothing happens to them” (Male, FGD, In-school).
Interviews with services providers revealed that the design of some of the service points makes it difficult to provide optimum privacy to clients. The study also found that some staff were not trained on adolescent friendly reproductive health services as illustrated:
“…The lack of privacy is due to how our facilities were designed. Many of our facilities in this district have no space provided for that. Lack of confidentiality from health personnel, as well as inadequate qualified personnel are serious challenges that we face on the daily basis” (IDI, Midwife-1).
“Our staff are not well trained as adolescent friendly reproductive health service providers. We are all using our previous knowledge from school which may not be enough and also the working experiences… everybody is committed in helping out to make the situation better. Inadequate staff numbers is also a big problem for us. The work is, actually too much for us” (IDI, Midwife-2).
“….Our consulting rooms are not safe. When a person comes with a sexually transmitted infection, they often not able tell us because some people may hear the conversation. They rather try to hide the truth from you and begin to tell you about other things, leaving you to guess the problem” (IDI, Public Health Nurse).
Stakeholders interviewed in this study noted that access to SRH information and services could reduce school dropout rate among females. However, stakeholders indicated that some health workers were uncomfortable providing adolescents with reproductive health services. In their view, availing condoms to adolescents may lead them to experiment with sex. Also, increasing access to comprehensive abortion services will encourage sexual activity among adolescents. Some stakeholders were of the view that some health workers have a negative attitude towards comprehensive abortion service because it conflicts with their religious beliefs. The following quotes illustrate these points:
“Allowing adolescent access to condom will encourage sexual practice among them. As for access to abortion, it means we will be encourage them to experiment with sex. After all when you become pregnant you can abort it at the hospital” (IDI, Opinion Leader).
“Some health workers are uncomfortable providing comprehensive abortion care to adolescents. They perceive abortion as something that is against their religious beliefs. So, it is even worse when they are to provide such a service to adolescent” (IDI, Public Health Nurse).
Knowledge on reproductive health and sources of information
The study found that both in-school and out-of-school adolescents in this part of Ghana did not have comprehensive knowledge on reproductive health issues and choices. The lack of knowledge makes them vulnerable to unsafe reproductive health behaviour and inappropriate choices. Some of these choices may have detrimental effects on their reproductive health and future. For example, a wrong choice can lead to unplanned pregnancy or STI infection [ 28 ]. In another study, it was found that lack of knowledge on reproductive health was associated with early initiation of coital relations and of unwanted pregnancies [ 29 ]. The effects of these unplanned pregnancies are multifarious with some capable of lasting for a lifetime. These potential human resource and future leaders end up as school dropouts due to unplanned pregnancy and other attendant complications. Additionally, a good number of adolescents who indulge in early sexual debut may contract HIV and other STIs [ 30 ]. These have social and economic implications for their households and the nation as whole as funds will be required to provide lifetime medication for people with HIV [ 31 ], and may even affect their line of generations yet unborn [ 32 ].
As we have shown, most out-of-school adolescents are reliant on their peers who are in-school and the mass media for information on reproductive health. These sources make them vulnerable to misinformation. In that case, they will be making decisions based on an incorrect information which can negatively affect them. Parents who could be the most appropriate source of information are inhibited by socio-cultural barriers that prevent them from discussing reproductive health issues with their children as has been reported by Owusu, Blankson & Abane [ 33 ] in the Central Region of Ghana. Similarly, studies in Nigeria and Uganda found that adolescents preferred parents as a source of information about sexual and reproductive health, however cultural sensitivity and social norms inhibited them [parents] from playing that role effectively [ 34 , 35 , 36 ]. Talking about sex is often frowned upon by both traditional and religious adherents in the Ghanaian society. This environment makes it difficult and sometimes impossible for adolescents to discuss sex and related issues with parents or adult family members [ 37 ]. The findings of this study underscore the need for innovative ways to expand access to reproductive health education and services to both in-school and out-of-school adolescents. School-based approaches which are linked to the community have been found to be effective in other countries [ 21 , 38 , 39 ]. These approaches could be adopted for Ghanaian adolescents as a community-related strategy (intervention) in the ecological model.
Views on having sexual partners and premarital sexual practices
The study found that having a sexual partner was a common practice among adolescents in the community, and is widely viewed as an acceptable practice. Among adolescents, this is done to conform to peer norms and a way of demonstrating that one had what it takes to be a woman or man. The act of engaging in sexual practice among adolescents has been widely reported across the sub-Saharan African region, with about 25% reporting having sexual contact before attaining 15 years of age [ 40 ].
This study also found that having multiple partners was a common practice. Similar findings were reported among adolescents in Tanzania [ 41 ]. Despite the fact that many adolescents reported having multiple partners, the use of condom was reportedly low during sexual encounters. This is a challenge to public health workers involved in sensitizing the population against risk of STIs and HIV among Ghanaians. The use of condom is one of the key strategies employed by the National AIDS Control Programme (NACP) to reduce the burden of HIV and STIs. Having sex with multiple partners without the use condom is one of the risk factors in HIV transmission and many studies have documented high prevalence of HIV infection among people with multiple partners [ 42 , 43 , 44 ].
The study found that transactional sex (sex for gift) was common in the community and many adolescents were engaging in this type of sexual acts with adults in the community. Female adolescents were engaged is this practice as a way of survival as a result of endemic poverty in the community [ 45 ]. This will require interventions at the community level to empower females. Also enforcing laws that protect the human right of females in the community and use of mass media approaches to create awareness about the existing laws and policies about adolescent sexual and reproductive health related issues may be essential in addressing transactional sexual practices. The policies and laws fall under the societal construct in the ecological model. Transactional sex has been found to be associated with having multiple partners as well as engaging in HIV-related risky behaviour [ 46 ]. An earlier study has found high prevalence of HIV infection among people engaged in transactional sex [ 47 ]. This high prevalence may not necessarily be due to the high level of exposure as a result of multiple partners [ 47 , 48 ] but it also creates a situation which makes it impossible for females especially to negotiate for the use of condom as found in this study. Therefore people engaged in HIV prevention must be concern about transactional sex.
Strategies against unplanned pregnancies, and abortions
From this study, it emerged that respondents believe that some local preparations and herbs are effective abortifacients. Such believes were widespread and well-known thereby resulting in low patronage for modern contraceptives. A study in southern Ghana reported similar believes where there was the widespread notion that ingestion of panacin and cafalgen (painkillers) before sex had some contraceptive effects [ 49 ]. Washing of the vagina and vulva with soap and water which is another local practice to avoid pregnancy after unprotected sex has implications on the reproductive health of adolescents. This practice can predispose adolescents to reproductive tract infections which can negatively affect their reproductive functions. Washing the vagina with soap is capable of destroying the normal flora of the vagina and vulva predisposing the female to vaginosis [ 50 ]. Vagina cleaning using soap and water has also been reported to increase HIV infection [ 50 , 51 ]. Health education to community should highlight the negative effects of these practices on the future reproductive health of adolescents.
It is however obvious in the study that these preparations believed to be abortifacients were ineffective as participants in this study indicated that the incidence of unplanned pregnancies was high even among people who had used these items to prevent pregnancy. The findings of this study further show that adolescents who become pregnant do not seek for safe abortion services but engage in unsafe abortion practices using grinded bottles, inserting herbs into the vagina and use of drinks that contain alcohol. These unsafe abortion practices have very serious implications on the health of adolescents as it can result in complications and death. Unsafe abortion is one of the leading preventable causes of maternal mortality across the world [ 52 , 53 , 54 , 55 ]. Increasing access to safe abortion and comprehensive abortion care were introduced to ameliorate the negative effects of unsafe abortion. Comprehensive abortion care have been found to have high impact in reducing maternal mortality [ 56 , 57 , 58 ]. Though Ghana has been implementing comprehensive abortion care in health facilities across all regions [ 59 ], the finding of this study reveals a lack of knowledge and awareness about comprehensive abortion care among adolescents as many still engaged in unsafe practices with detrimental effects on their health. More community sensitization should be done to create awareness on the existence of comprehensive abortion care service in health facilities in Ghana.
The study generally found that reproductive health services were available in the community. Also, efforts are being made to bring service close to the communities through outreach programme. However, these efforts were undermined by service-related barriers. Key amongst these was the attitude of health workers towards providing services to adolescents. The study reported there was widespread feeling of negative attitude of service providers towards adolescents, hence their refusal to patronize the services. The negative attitude was reported by both adolescents and stakeholders in this study. This negative attitude was due to community norms and beliefs of health workers concerning some services such as contraceptive use and safe abortion. This will require training of health workers on adolescent-friendly approaches to reproductive health services. Sensitization of community will also be required to increase acceptance. Adolescents’ reproductive health service programmes that target health workers to provide adolescent friendly facility-based services with the approval of community have been found to be more effective [ 39 ]. Lack of training has been found to negatively affect the quality of care provided to adolescents in an earlier study [ 60 ]. When the attitude of health service providers improves, it will lead to utilization of the services. A study in Kenya found a significant association between friendliness of service provider, and proximity to service provider and uptake of contraceptives [ 61 ].
Adolescents in this study were of the view that the designs of reproductive health service outlets did not provide enough privacy. This was therefore a barrier to uptake of such services in the community. Service outlets for adolescent reproductive health services should be designed to provide good privacy. This is because there are socio-cultural norms that prevent adolescent from using reproductive health services. Therefore, adolescents found utilizing reproductive health service risk been described in derogatory terms. This therefore call for measure to ensure strict privacy as that is the only way such services can be patronized by adolescents.
Limitation of the study
The main limitation of this study is that it was conducted in one rural district in Northern Ghana and the findings cannot be assumed to be the same in other settings. However, the study provides insight into areas to target for health promotion and interventions on adolescent reproductive health choices.
This study concludes that adolescents in this study generally engaged in risky reproductive health choices with potential of negatively affecting their reproductive health in future. Social and health systems barriers inhibited the utilization of existing reproductive health services. Advocates for reproductive health service providers need to develop better innovative ways to provide this important service to adolescent especially those who are out of school. Sexual and reproductive health promotional activities should target parents as a way of breaking the social barriers. Community sensitization and training of health workers is required to remove barriers and increase the utilization of reproductive health services.
Abbreviations
Focus group discussion
Ghana Demographic and Health Survey
Human Immunodeficiency Virus
International Conference on Population and Development
in-depth interview
National AIDS/STIs Control Programme
Sexual Transmitted Infections
Mba CJ. Sexual Behaviour and The risks of HIV/AIDS and other STDs among young people in sub-Saharan Africa : a REVIEW. Res Rev. 2003;1:15–25.
Google Scholar
Esere MO. Effect of sex education programme on at-risk sexual behaviour of school-going adolescents in Ilorin. Nigeria African Heal Sci. 2008;8:120–5.
Ayalew M, Mengistie B, Semahegn A. Adolescent-parent communication on sexual and reproductive health issues among high school students in Dire Dawa, Eastern Ethiopia: a cross sectional study. Reprod. Health. BioMed Central Ltd. 2014;11:77.
Kabiru C, Izugbara C, Beguy D. The health and wellbeing of young people in sub-Saharan Africa: an under-researched area? BMC Int. Health Hum. Rights. 2013;13:11.
Article Google Scholar
World Bank. Data: Sub-Saharan Africa (developing only). Washington, DC.; 2015.
GSS. 2010 Population and housing census final results. Accra-Ghana; 2012.
GSS. 201 Population and Housing Census Regional Analytic Report for Northern Region. Accra; 2013.
Akther N, Begum N, Chowdhury S, Sultana S. Knowledge on reproductive health issues among the unmarried adolescent girls. J Fam Reprod Heal. 2012;6:169–77.
Aryeetey R, Ashinyo A, Adjuik M. Age of menarche among basic level school girls in Medina, Accra. Afr J Reprod Health. 2011;15:103–10.
PubMed Google Scholar
Dixon-Mueller R. The sexual and reproductive health of younger adolescents: research issues in developing countries. WHO doc. Prod. Serv. Geneva: World health Organization; 2011. p. 57.
Ghana Statistical Service (GSS) GHS (GHS), Macro I. Ghana Demographic and Health Survey 2008. Accra: GSS, GHS and ICF Macro; 2009.
Okereke CI. Unmet Reproductive Health needs and health-seeking behaviour of adolescents in Owerri , Nigeria. Afr J Reprod Health. 2010;14:43–54.
GSS/GHS/ICF Macro. Ghana Demographic and health Survey. Accra; 2014.
UN Millennium Project. Public choices, Private Decisions: Sexual and Reproductive Health and the Millennium Development Goals. USA; 2006.
UNFPA. International Conference on Population Development: Investing in People: National Progress in Implementing the ICPD Programmme of Action 1994-2004. A Summ. Rep. New York: UNFP; 2004.
Global Forum For Health Research. Poverty, Equity and Health Research. In: Matlin S, editor. Global Forum Update on Research for Health, vol. Volume 2. 1st ed. London: Pro-Book Publishing Limited; 2005.
Andrews M, Tamboukou M. Doing narrative research. Second. Andrews M, Tamboukou M, editors. Washington, DC: SAGE Publications, Inc; 2013.
Creswell JW, Garrett AL. The ‘ movement ’ of mixed methods research and the role of educators. South African J Educ. 2008;28:321–33.
Bronfenbrenner V. The ecology of human development: experiments by nature and design. Cambridge, MA: Harvard University Press; 1979.
Garbarino J. Adolescent development: an ecological perspective. California: C.E. Merrill Pub. Co.; 1985.
Svanemyr J, Amin A, Robles OJ, Greene ME. Creating an enabling environment for adolescent sexual and reproductive health: a framework and promising approaches. J Adolesc Health. 2015;56:S7–14.
Article PubMed Google Scholar
Clark JP. Qualitative Research Review Guidelines - RATS. How to peer Rev. a Qual. Manuscr. Peer Rev. Heal. Sci. 2003. p. 219–35.
WGDHD. 2012 Annual report. Damongo, N/R; 2013.
Green J, Thorogood N. Qualitative methods for Health Research. London: Sage Publications; 2004.
Dawson S, Manderson L, Tallo V. Methods for Social Research in Disease: A Manual for the Use of Focus Groups. Boston, MA: International Nutrition Foundation for Developing Countries; 1993. p. 1–96.
Patton M. Qualitative research and evaluation methods. Nurse Educ. Today, vol. 2. 3rd ed. London, Sage Publications Ltd; 2002. p. 107–34.
Miles MB, Huberman MA. Quliatative data analysis: An expanded sourcebook. Thousan Oaks: SAGE Publications, Inc; 1994.
Harden A, Brunton G, Fletcher A, Oakley A. Teenage pregnancy and social disadvantage: systematic review integrating controlled trials and qualitative studies. BMJ. 2009;339:b4254.
Article PubMed PubMed Central Google Scholar
Minnick DJ, Shandler L. Changing adolescent perceptions on teenage pregnancy. Child Sch. 2012;33:241–8.
Idele P, Gillespie A, Porth T, Suzuki C, Mahy M, Kasedde S, et al. Epidemiology of HIV and AIDS among adolescents: current status, inequities, and data gaps. J Acquir Immune Defic Syndr. 2014;66:S144–53.
NACP. HIV sentinel survey report. Accra; 2015.
Walker I, Navarro Paniagua M. The impact of teenage motherhood on the the impact of teenage motherhood on the education and fertility of their children: evidence for Europe. Bonn; 2012.
Owusu SA, Blankson EJ, Abane AM. Sexual and reproductive health education among dressmakers and hairdressers in the Assin South District of Ghana. Afr J Reprod Health. 2011;15:109–19.
Ybarra ML, Emenyonu N, Nansera D, Kiwanuka J, Bangsberg DR. Health Information seeking among Mbararan adolescents: results from the Uganda media and you survey. Health Educ Res. 2008;23:249–58.
Nwagwu WE. The internet as a source of reproductive health information among adolescent girls in an urban city in Nigeria. BMC Public Health. 2007;7:354.
Nwalo KIN, Anasi SNI. Access to and use of reproductive health information among in-school adolescent girls in Lagos state, Nigeria. Health Educ J. 2012;71:90–101.
Awusabo-asare K, Biddlecom A, Kumi-Kyereme A, Patterson K. Adolescent Sexual and Reproductive Health in Ghana : Results from the 2004 National Survey of Adolescents. Occas. Reeport No 22. New York; 2006.
Chandra-Mouli V, Svanemyr J, Amin A, Fogstad H, Say L, Girard F, et al. Twenty years after international conference on population and development: where are we with adolescent sexual and reproductive health and rights? J Adolesc Health. 2015;56:S1–6.
Denno DM, Hoopes AJ, Chandra-Mouli V. Effective strategies to provide adolescent sexual and reproductive health services and to increase demand and community support. J. Adolesc. Heal. 2015;56:S22–41.
Doyle AM, Mavedzenge SN, Plummer ML, Ross DA. The sexual behaviour of adolescents in sub-Saharan Africa: patterns and trends from national surveys. Trop Med Int Heal. 2012;17:796–807.
Exavery A, Lutambi AM, Mubyazi GM, Kweka K, Mbaruku G, Masanja H. Multiple sexual partners and condom use among 10 - 19 year-olds in four districts in Tanzania: what do we learn? BMC Public Health. 2011;11:490.
Townsend L, Zembe Y, Mathews C, Mason-Jones A. Estimating HIV prevalence and HIV-related risk behaviors among heterosexual women who have multiple sex partners using respondent-driven sampling in a high-risk Community in South Africa. J Acquir Immune Defic Syndr. 2013;62:457–64.
Saggurti N, Raj A, Mahapatra B, Cheng DM, Coleman S, Bridden C, et al. Prevalence and correlates of non-disclosure of HIV serostatus to sex partners among HIV-infected female sex workers and HIV-infected male clients of female sex workers in India. AIDS Behav. 2013;17:399–406.
Kalichman SC, Ntseane D, Nthomang K, Segwabe M, Phorano O, Simbayi LC. Recent multiple sexual partners and HIV transmission risks among people living with HIV/AIDS in Botswana. Sex Transm Infect. 2007;83(5):371.
GSS. Ghana Poverty Mapping Report. Accra, Ghana; 2015.
Choudhry V, Ambresin A-E, Nyakato VN, Agardh A. Transactional sex and HIV risks - evidence from a cross-sectional national survey among young people in Uganda. Glob Health Action. 2015;8:27249.
Jewkes R, Dunkle K, Nduna M, Shai NJ. Transactional sex and HIV incidence in a cohort of young women in the stepping stones trial. J AIDS Clin Res. 2012;3:7.
Jewkes R, Morrell R, Sikweyiya Y, Dunkle K, Penn-Kekana L. Transactional relationships and sex with a woman in prostitution: prevalence and patterns in a representative sample of south African men. BMC Public Health. 2012;12:325–35.
Adongo PB, Tapsoba P, Phillips JF, Tabong PT-N, Stone A, Kuffour E, et al. ‘If you do vasectomy and come back here weak, I will divorce you’: a qualitative study of community perceptions about vasectomy in southern Ghana. BMC Int. Health Hum Rights. 2014;14:16.
McClelland RS, Lavreys L, Hassan WM, Mandaliya K, Ndinya-Achola JO, Baeten JM. Vaginal washing and increased risk of HIV-1 acquisition among African women: a 10-year prospective study. AIDS. 2006;20:269–73.
Cohen CR, Lingappa JR, Baeten JM, Ngayo MO, Spiegel CA, Hong T, et al. Bacterial vaginosis associated with increased risk of female-to-male HIV-1 transmission: a prospective cohort analysis among African couples. PLoS Med. 2012;9:e1001251.
Haddad LB, Nour NM. Unsafe abortion: unnecessary maternal mortality. Rev Obstet Gynecol. 2009;2:122–6.
PubMed PubMed Central Google Scholar
Åhman E, Shah IH. New estimates and trends regarding unsafe abortion mortality. Int J Gynecol Obstet. 2011:121–6.
World Health Organization. WHO | Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. WHO. 2014;5th editio:1–67.
Regmi MC, Rija P, Subedi SS, Uprety D, Budathoki B, Agrawal A. Unsafe abortion: a tragic saga of maternal suffering. J Nepal Med Assoc. 2010;49:19–22.
CAS Google Scholar
Abdella A, Fetters T, Benson J, Pearson E, Gebrehiwot Y, Andersen K, et al. Meeting the need for safe abortion care in Ethiopia: results of a national assessment in 2008. Glob Public Health. 2013;8:417–34.
Prata N, Bell S, Gessessew A. Comprehensive abortion care: evidence of improvements in hospital-level indicators in Tigray, Ethiopia. BMJ Open. 2013;3:e002873–e002873.
Basnett I, Shrestha MK, Shah M, Pearson E, Thapa K, Andersen KL. Evaluation of nurse providers of comprehensive abortion care using MVA in Nepal. J Nepal Health Res Counc. 2012;10:5–9.
CAS PubMed Google Scholar
GHS Family Health Division. 2014 family health annual report of Ghana. Accra; 2015.
Mbeba RM, Mkuye MS, Magembe GE, Yotham WL, Mellah AO, Mkuwa SB. Barriers to sexual reproductive health services and rights among young people in Mtwara district, Tanzania: a qualitative study. Pan Afr Med J. 2012;13(Suppl 1):13.
Okech TC, Wawire NW, Mburu TK. Contraceptive Use among Women of Reproductive Age in Kenya ’ s City Slums. Int J Bus Soc Sci. 2011;2:22–43.
The Constitution of Ghana. The Constitution of the Republic of Ghana. Accra: Ghana Assembly Press; 1992.
Download references
Acknowledgements
We wish to thank the district director of health services of the West Gonja District in Northern region and all the participants for their cooperation in this study.
The study was funded by the authors.
Availability of data and materials
All relevant data and materials are within the manuscript. The transcripts are also available on request to corresponding author.
Author information
Authors and affiliations.
Nurses Training College, Box 565, Tamale, Northern region, Ghana
Joseph Maaminu Kyilleh
Department of Social and Behavioural Science, School of Public Health, Box LG 13, Legon, Ghana
Philip Teg-Nefaah Tabong
Department of Community Health and Family Medicine, University for Development Studies, Tamale, Ghana
Benson Boinkum Konlaan
You can also search for this author in PubMed Google Scholar
Contributions
Conceived and designed the experiments: JMK, BBK, PT-NT. Performed the experiments: JMK Analyzed the data: PT-NT, JMK, BBK. Contributed reagents/materials/analysis tools: JMK, PT-NT, BBK. Wrote the paper: PT-NT, JMK BBK. All authors read and approved the final manuscript
Corresponding author
Correspondence to Philip Teg-Nefaah Tabong .
Ethics declarations
Ethical approval and consent to participate.
Ethical approval was obtained from the ethical committee of the School of Medicine and Allied Health Science of the University for Development Studies. In addition, permission to conduct the study was solicited and obtained from the West Gonja District Health Directorate. A written informed consent was obtained from parents and guardians for those respondents < 18 years of age. In addition, an assent was also obtained from the minors before the interview. However, for respondents who were ≥18 year, informed consent was obtained from them as required in Ghana [ 62 ]. Participation in the study was voluntary and they were informed of their right to withdrawal from participation at any time during the interview. Data collected for this study were anonymized by de-linking personal information from the main data.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Kyilleh, J.M., Tabong, P.TN. & Konlaan, B.B. Adolescents’ reproductive health knowledge, choices and factors affecting reproductive health choices: a qualitative study in the West Gonja District in Northern region, Ghana. BMC Int Health Hum Rights 18 , 6 (2018). https://doi.org/10.1186/s12914-018-0147-5
Download citation
Received : 28 April 2017
Accepted : 17 January 2018
Published : 24 January 2018
DOI : https://doi.org/10.1186/s12914-018-0147-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents
- Reproductive health
- Health choices
- Risky behaviours
BMC International Health and Human Rights
ISSN: 1472-698X
- General enquiries: [email protected]
- Architecture and Design
- Asian and Pacific Studies
- Business and Economics
- Classical and Ancient Near Eastern Studies
- Computer Sciences
- Cultural Studies
- Engineering
- General Interest
- Geosciences
- Industrial Chemistry
- Islamic and Middle Eastern Studies
- Jewish Studies
- Library and Information Science, Book Studies
- Life Sciences
- Linguistics and Semiotics
- Literary Studies
- Materials Sciences
- Mathematics
- Social Sciences
- Sports and Recreation
- Theology and Religion
- Publish your article
- The role of authors
- Promoting your article
- Abstracting & indexing
- Publishing Ethics
- Why publish with De Gruyter
- How to publish with De Gruyter
- Our book series
- Our subject areas
- Your digital product at De Gruyter
- Contribute to our reference works
- Product information
- Tools & resources
- Product Information
- Promotional Materials
- Orders and Inquiries
- FAQ for Library Suppliers and Book Sellers
- Repository Policy
- Free access policy
- Open Access agreements
- Database portals
- For Authors
- Customer service
- People + Culture
- Journal Management
- How to join us
- Working at De Gruyter
- Mission & Vision
- De Gruyter Foundation
- De Gruyter Ebound
- Our Responsibility
- Partner publishers

Your purchase has been completed. Your documents are now available to view.
Exploring the relationship between mothers’ competence and comfort in sexual and reproductive health discourse with adolescent girls and its related factors
The mothers–adolescent discussion regarding sexual and reproductive health (SHR) issues plays an important role in preventing negative outcome associated with sexual risk behaviors. The present study aimed to explore the relationship between mothers’ competence and comfort in SHR discourse with adolescent girls and its related factors.
A cross-sectional study was conducted involving 160 mothers from July to September 2020. Data were collected through questionnaires covering demographic characteristics, Mother’s Comfort in Sexual Discourse (MCSD), Mother’s Interest in Sexual Discourse (MISD), and Parenting Sense of Competence (PSOC). The collected data were analyzed using simple and multiple linear regression models.
The mean scores for MCSD, MISD, and PSOC were 45.49±16.15 (13–78), 7.9±4.2 (0–13), and 64.07±9.44 (45–94), respectively. The primary topics of mother–adolescent discourse on SRH were menstruation (5.61±0.98) and the delivery process (4.55±1.57). The mean age for “sex talks” and age-appropriate “sex talks” with daughters was 11.76±1.85 (range: 6–15) and 17.05±1.86 (range: 14–23) years, respectively. Significant associations were found between MCSD and MISD (β=0.482, p<0.0001), PSOC (β=0.223, p<0.005), self-efficacy (β=0.202, p<0.011), mother’s job (β=0.185, p<0.019), mother’s education (β=0.173, p<0.029), and father’s age (β=0.161, p<0.042). After adjusting for other variables, major influencing factors on MCSD included MISD (β=0.487, p<0.0001), self-efficacy (β=0.143, p<0.039), satisfaction (β=0.169, p<0.015), daughter number (β=−0.235, p<0.014), son number (β=−0.219, p<0.024), birth rank (β=0.263, p<0.008), and residency (β=0.172, p<0.014).
Conclusions
MISD, PSOC, and certain demographic characteristics emerge as significant factors influencing MCSD in mother–daughter sexual discourse. As such, it is imperative to consider these determinants when devising strategies to maintain and enhance the sexual health of teenage girls.
Acknowledgments
The authors would like to appreciate the authorities of the Research Deputy of Babol University of Medical Sciences, the health workers in centers, and all the participating mothers.
Research ethics: The authors confirm safeguards of ethical standards. This project was confirmed by the ethics committee of the research unit of Medical Sciences University with code IR.MUBABOL.REC.1399.207 dated 1.06.2020.
Informed consent: Written informed consent was provided to all mothers before data collection for the present research. The study was conducted under the declaration of Helsinki.
Author contributions: Author’s HA-R, HP, and FGH conducted the design of the research. HP, MF, and SHO did data collection and management. An analysis was completed by authors HP, and MCH. The authors revised this protocol. All authors read and approved the final manuscript.
Competing interests: The authors declare that have no conflict of interest.
Research funding: None declared.
Data availability: The datasets used during the present research can be available from the corresponding author upon reasonable request.
1. Vasilenko, SA, Kugler, KC, Butera, NM, Lanza, ST. Patterns of adolescent sexual behavior predicting young adult sexually transmitted infections: a latent class analysis approach. Arch Sex Behav 2015;4493:705–15. https://doi.org/10.1007/s10508-014-0258-6 . Search in Google Scholar PubMed PubMed Central
2. Adam, ND, Demissie, GD, Gelagay, AA. Parent-adolescent communication on sexual and reproductive health issues and associated factors among preparatory and secondary school students of Dabat Town, Northwest Ethiopia, Hindawi. J Environ Public Health 2020;2020:4708091. https://doi.org/10.1155/2020/4708091 . Search in Google Scholar PubMed PubMed Central
3. Johnson, BD, Berdahl, LD, Horne, M, Richter, EA, Walters, Mg. A parenting competency model. Parenting 2014;14:92–120. https://doi.org/10.1080/15295192.2014.914361 . Search in Google Scholar
4. Kurtuncu, M, Akhan, LU, Tanir, İM, Yildiz, H. The sexual development and education of preschool children: knowledge and opinions from doctors and nurses. Sex Disabil 2015;33:207–21. https://doi.org/10.1007/s11195-015-9393-9 . Search in Google Scholar PubMed PubMed Central
5. Grossman, JM, Jenkins, LJ, Richer, AM. Parents’ perspectives on family sexuality communication from middle school to high school. Int J Environ Res Publ Health 2018;2018:107. https://doi.org/10.3390/ijerph15010107 . Search in Google Scholar PubMed PubMed Central
6. Martin, K, Torres, J. Where did I come from? US parents’ and preschool children’s participation in sexual socialization. Sex Educ 2014;14:174–90. https://doi.org/10.1080/14681811.2013.856291 . Search in Google Scholar
7. Bekele, D, Deksisa, A, Abera, W, Megersa, G. Parental communication on sexual and reproductive health issues to their adolescents and affecting factors at Asella town, Ethiopia: a community-based, cross-sectional study. Reprod Health 2022;19:114. https://doi.org/10.1186/s12978-022-01408-8 . Search in Google Scholar PubMed PubMed Central
8. Noe, MT, Saw, YM, Soe, PP, Khaing, M, Saw, TN, Hamajima, N, et al.. Barriers between mothers and their adolescent daughters with regards to sexual and reproductive health communication in Taunggyi Township, Myanmar: what factors play important roles? PLoS One 2018;13:e0208849. https://doi.org/10.1371/journal.pone.0208849 . Search in Google Scholar PubMed PubMed Central
9. Fanta, M, Lemma, S, Gamo, G, Meskele, M. Factors associated with adolescent-parent communication of reproductive health issues among high school and preparatory students in Boditi town, Southern Ethiopia: a cross-sectional study. Patient Intell 2016;8:57–70. https://doi.org/10.2147/pi.s97838 . Search in Google Scholar
10. Efrati, Y, Gola, M. Adolescents’ compulsive sexual behavior: the role of parental competence, parents’ psychopathology, and quality of parent–child communication about sex. J Behav Addict 2019;8:420–31. https://doi.org/10.1556/2006.8.2019.33 . Search in Google Scholar PubMed PubMed Central
11. Holman, AJ. How adolescents perceive their parents’ communication about sex: toward reducing adolescent sexual risk [communication studies theses, dissertations, and student research]. Lincoln, NE, USA: University of Nebraska-Lincoln; 2014:29 p. Search in Google Scholar
12. Balaji, AB, Oraka, E, Fasula, AM, Jayne, PE, Carry, MG, Raiford, JL. Association between parent–adolescent communication about sex-related topics and HIV testing, United States, 2006–2013. AIDS Care 2017;29:344–9. https://doi.org/10.1080/09540121.2016.1238443 . Search in Google Scholar PubMed
13. Drioane, E. Rewriting “the talk”: effects of parental communication education on perceived comfortableness and willingness to have discussions with their children about sex . Faculty of the Graduate School of the University of Colorado, California State University at Fresno; 2014. Search in Google Scholar
14. Heisler, M. Different models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Fam Pract 2010;27:i23–2. https://doi.org/10.1093/fampra/cmp003 . Search in Google Scholar PubMed PubMed Central
15. Guilamo-Ramos, V, Jaccard, J, Dittus, P, Collins, S. Parent-adolescent communication about sexual intercourse: an analysis of maternal reluctance to communicate. Health Psychol 2008;27:760–9. https://doi.org/10.1037/a0013833 . Search in Google Scholar PubMed
16. Esmaeelpanah Amlashi, Z, Hosseinkhanzadeh, AA, Akbari, B, Moghtader, L. Psychometric properties of the parenting self-efficacy questionnaire (TOPSE). J Psychol Sci 2021;20:939–51. Search in Google Scholar
17. Zhu, Y, Zhou, X, Yin, X, Qiu, L, Sun, N, An, R, et al.. Parenting sense of competence and its predictors among Primiparous women: a longitudinal study in China. BMC Pregnancy Childbirth 2022;22:548. https://doi.org/10.1186/s12884-022-04881-y . Search in Google Scholar PubMed PubMed Central
18. Sooki, Z, Tagharrobi, Z, Sharifi, K. Investigating the level of mothers’ comfort in sexual discourse with adolescent girls and related factors. Int Arch Health Sci 2022;9:140–444. https://doi.org/10.4103/iahs.iahs_123_22 . Search in Google Scholar
19. Motamed, N, Zamani, F. Sample size in medical research, an applied approach , 1st ed. Tehran: Asr Roshanbin Publications; 2016. Search in Google Scholar
20. Koblinsky, S, Atkinson, J. Parental plans for children’s sex education. Fam Relat 1982;31:29–35. https://doi.org/10.2307/584198 . Search in Google Scholar
21. Youzbashi, B, Maarefvand, M, Hosseinzadeh, S. Evaluation of validity and reliability of “parents comfort to discuss about sex topics” and “Parents intention to discuss about sex topics” questionnaires. Soc Work 2017;6:37–43. Search in Google Scholar
22. Rashid, K, Hosseini Nazarlou, M. Investigating the effect of sex education on enhancing parents’ sexual knowledge and their sense of competence. J Instr Eval 2017;10:143–62. Search in Google Scholar
23. Shin, H, Lee, JM, Min, JY. Sexual knowledge, sexual attitudes, and perceptions and actualities of sex education among elementary school parents. Child Health Nurs Res 2019;25:312–23. https://doi.org/10.4094/chnr.2019.25.3.312 . Search in Google Scholar PubMed PubMed Central
24. Depauli, C, Plaute, W. Sexuality education in Austrian Middle Schools. Z Sex Forsch 2019;32:90–9. https://doi.org/10.1055/a-0894-9400 . Search in Google Scholar
25. Zakaria, M, Xu, J, Karim, F, Cheng, F. Reproductive health communication between mother and adolescent daughter in Bangladesh: a cross-sectional study. Reprod Health 2019;16:114. https://doi.org/10.1186/s12978-019-0778-6 . Search in Google Scholar PubMed PubMed Central
26. Fletcher, KD, Ward, LM, Thomas, K, Foust, M, Levin, D, Trinh, S. Will it help? Identifying socialization discourses that promote sexual risk and sexual health among African American youth. J Sex Res 2015;52:199–212. https://doi.org/10.1080/00224499.2013.853724 . Search in Google Scholar PubMed
27. Smith, SJ. A comparison of self-efficacy in mothers of children with autism spectrum disorder and typically developing children: contributions of depression and Co-parenting relationships . Mills College: ProQuest LLC; 2020. Search in Google Scholar
28. Albanese, AM, Russo, GR, Geller, PA. The role of parental self-efficacy in parent and child well-being: a systematic review of associated outcomes. Child Care Health Dev 2019;45:333–63. https://doi.org/10.1111/cch.12661 . Search in Google Scholar PubMed
29. Ghorbani, Y, Lotfi Kashani, F, Akbari, ME, Vaziri, S. A comparison of parent-child communication and self-efficacy in women with breast cancer and healthy women. J Psychol Sci 2018;17:259–70. Search in Google Scholar
30. Klein, V, Becker, I, Štulhofer, R. Parenting, communication about sexuality, and the development of adolescent womens’ sexual agency: a longitudinal assessment. J Youth Adolesc 2018;47:1486–98. https://doi.org/10.1007/s10964-018-0873-y . Search in Google Scholar PubMed
31. Li, M, Lan, R, Ma, P, Gong, H. The effect of positive parenting on adolescent life satisfaction: the mediating role of parent-adolescent attachment. Front Psychol 2023:1–9. https://doi.org/10.3389/fpsyg.2023.1183546 . Search in Google Scholar PubMed PubMed Central
32. Byers, ES, Sears, HA, Weaver, AD. Parents’ reports of sexual communication with children in kindergarten to Grade 8. J Marriage Fam 2008;70:86–96. https://doi.org/10.1111/j.1741-3737.2007.00463.x . Search in Google Scholar
33. Widman, L, Choukas-Bradley, S, Noar, SM, Nesi, J, Garrett, K. Parent–adolescent sexual communication and adolescent safer sex behavior: a meta-analysis. JAMA Pediatr 2016;170:52–61. https://doi.org/10.1001/jamapediatrics.2015.2731 . Search in Google Scholar PubMed PubMed Central
34. Botha, E, Helminen, M, Kaunonen, M, Lubbe, W, Joronen, K. Mothers’ parenting self-efficacy, satisfaction and perceptions of their infants during the first days postpartum. Midwifery 2020;88:102760. https://doi.org/10.1016/j.midw.2020.102760 . Search in Google Scholar PubMed
© 2024 Walter de Gruyter GmbH, Berlin/Boston
- X / Twitter
Supplementary Materials
Please login or register with De Gruyter to order this product.
- Open access
- Published: 19 July 2023
Effectiveness of school-based sexual and reproductive health education among adolescent girls in Urban areas of Odisha, India: a cluster randomized trial
- G. Alekhya 1 ,
- Swayam Pragyan Parida 1 ,
- Prajna Paramita Giri 1 ,
- Jasmina Begum 3 ,
- Suravi Patra 2 &
- Dinesh Prasad Sahu 4
Reproductive Health volume 20 , Article number: 105 ( 2023 ) Cite this article
3856 Accesses
1 Citations
6 Altmetric
Metrics details
A Correction to this article was published on 13 September 2023
This article has been updated
Various studies revealed that adolescent girls have limited knowledge pertaining to sexual and reproductive health (SRH). The current study assessed the effectiveness of SRH education among adolescent girls in urban areas of Odisha, India.
The study design was a cluster randomized trial, where the clusters composed of eight Odia (regional language) medium government girls’ high schools in Bhubaneswar, the capital city of the state of Odisha, India . For the selection of study participants, adolescent girls who were studying in the ninth and tenth standards were recruited from each school. Eight schools were randomized through restrictive randomization at a 1:1 ratio, with four schools each in the intervention and control arm. Baseline and end-line assessments were done using a pre-tested, semi-structured questionnaire. Following baseline assessment, an intervention was given with the help of handbooks developed by the study authors to the schools in the intervention arm. Outcomes included change in knowledge, attitude and practices pertaining to SRH.
In our study at baseline, there were a total of 790 students, where 469 (59.4%) students were in the intervention arm, and 321 (40.6%) students were in the control arm. At baseline, only 282 (60.1%) in the intervention arm and 171 (53.3%) in the control arm were aware that physical bodily changes due to puberty were normal. After the intervention, there was a statistically significant increase in knowledge in intervention group 367 (94.8%) (p-value < 0.001). Most students used sanitary pads as absorbent, 97.2% in the intervention group and 98.4% in the control group. However, after the intervention, the use of other absorbents reduced to zero in the intervention group with a statistically significant difference (p < 0.05). The number of students having awareness on different methods of contraception increased from 51 (10.9%) to 337 (87.1%) in the intervention arm (p < 0.001), and of those having awareness on STIs/RTIs increased from 177 (38.2%) to 371 (96.1%) in the intervention group (p < 0.001).
From our study, there is a significant proportional change in knowledge, attitude, and practices pertaining to SRH. Our study recommends policymakers and program managers for the implementation of comprehensive SRH in the regular school curriculum.
Trial registration CTRI/2021/01/030490, registered on January 15, 2021. Prospectively registered at https://ctri.nic.in/Clinicaltrials/login.php
Plain language summary
Adolescent girls lack adequate knowledge pertaining to sexual and reproductive health, for which they face various issues such as teenage pregnancy, unsafe abortions and sexually transmitted infections. Hence the authors conducted this study to assess the effectiveness of school-based sexual and reproductive health education among adolescent girls in Odisha state of India in terms of improving knowledge, attitude and practices pertaining to reproductive health. A total of eight vernacular (Odia language) medium schools were selected for the conduct of the study, and the schools were randomly assigned where four schools received SRH education, and the other four received no intervention. A baseline assessment pertaining to SRH was done among adolescent girls studying in ninth and tenth classes of all eight schools, and then education was given to the four schools in the intervention arm. Students were educated on topics such as puberty, menstrual health, pregnancy, contraception and STIs/RTIs with the help of handbooks prepared by the authors. After 3 months of providing education, an endline assessment was done for the adolescent girls in all eight schools. There was an increase in knowledge, attitude and practices pertaining to SRH among the students who received education when compared to those who didn’t. Hence our study recommends policymakers and program managers include SRH education in the regular school curriculum.
Peer Review reports
As per United Nations Children’s Fund (UNICEF), there are approximately 1.3 billion adolescents worldwide, with 90% of them living in developing countries. Among these, there are around 880 million adolescent girls [ 1 ]. Gender inequality has persisted in the communities marginalizing adolescent girls who are victims of pernicious social norms affecting their ability to make decisions regarding education, work, marriage and social relationships [ 2 ]. The United Nations Population Fund (UNFPA) defines Sexual and Reproductive health (SRH) as a state of complete physical, mental, and social well-being related to the reproductive system [ 3 ]. Literature shows that adolescent girls lack adequate knowledge on SRH, for which they face issues such as early pregnancy and childbirth, abortion, violence, unintended pregnancies, maternal mortality, reproductive tract infections (RTIs) and sexually transmitted diseases (STDs) [ 4 ]. Around twelve million girls aged 15–19 years and seven million girls under 15 years give birth each year in developing countries. Complications arising due to pregnancy and childbirth are the leading cause of death for girls aged 15–19 years globally [ 5 ]. Each year around 39,000 child marriages happen every day [ 6 ]. Available data suggest that adolescent mothers succumb to depression compared to non-pregnant peers and adult mothers [ 7 ]. The Sustainable Development Goal (SDG) 3.7 states that by the year 2030, there should be universal access to sexual and reproductive health care services, including family planning, education, and integration of reproductive health into national programs. Also, SDG 5 focuses on gender equality by empowering women and girls, but data suggests only 57% of women aged 15–49 years make informed decisions regarding sexual and reproductive health care [ 8 ]. International organizations such as the World health organization (WHO), United Nations Children’s Fund (UNICEF), and the Lancet Commission highlight the need to prioritize adolescents in achieving the SDGs [ 9 ].
India, with a population of 253 million, has the world’s largest adolescent population [ 10 ]. In 2014, the Government of India (GOI) launched the “Rashtriya Kishor Swasthya Karyakram (RKSK)” to provide services to adolescents, including SRH services [ 11 ]. However, studies have shown that service utilization remains poor, and adolescents are often unaware of these services [ 12 ]. In Odisha state, under the RKSK program, Adolescent friendly health clinics (AFHCs) are operational at Urban Primary Health Centers (PHC), with adolescent health counsellors providing clinical, counselling and outreach services to schools, colleges and youth clubs [ 13 ]. However, in a scoping review measuring adolescent-friendly health services in India, in Odisha state, community health workers had more knowledge about adolescent health programs than the teachers and the prevalence of SRH knowledge was low in the adolescent community [ 14 ]. As per the latest National family health survey-5 (NFHS-5), data shows that 6.8% of women aged 15–19 have begun childbearing, and 23.3% of women aged 20–24 married before the age of 18. In Odisha, a state in India, the prevalence of teenage pregnancy is 7.6%, and 20.5% of married women were below 18 years of age, similar to the national data [ 15 ]. These rates are far from the recommendations of the Lancet Commission on adolescent health, which states the prevalence of teenage pregnancy to be less than 1 per cent by the year 2030 [ 16 ]. SRH education in India has not been given much importance due to existing taboos. A report on sexuality education in India by Youth Coalition for Sexual and reproductive rights stated that higher secondary schools do not have SRH education in the curriculum; however, private schools had the liberty to choose for inclusion of SRH education in the curriculum, but no attempts have been made from public schools mainly vernacular government schools [ 17 ]. This report was made in accordance with the International Conference on Population and Development (ICPD), which states governments are obliged to provide comprehensive sexuality education for youth to make informed decisions [ 17 ]. But some Indian states, such as Maharashtra, Gujarat, Karnataka, Rajasthan, Kerala, Goa, Madhya Pradesh, and Chhattisgarh, have banned sex education [ 18 ]. Studies conducted across various states in India assessed the knowledge, attitude and practices (KAP) related to SRH among adolescent girls and showed poor awareness among adolescents [ 19 ]. While some interventional studies assessed SRH education among adolescent girls in India, most of them were non-randomized studies [ 20 , 21 ]. Only one randomized study compared conventional education delivered by nurses with peer education among school-going adolescent girls in Punjab state, which found that both approaches improved knowledge [ 22 ]. However, no studies assessed the effectiveness of a comprehensive SRH intervention package with a control arm.
Schools act as a platform for providing educational interventions, given the concentration of the adolescent population at schools and the ease of access to health promotion in poor communities without effective health systems [ 23 ]. The authors of the study aimed to assess the effectiveness of school-based comprehensive SRH education in improving knowledge, attitude, and practices related to puberty, menstrual health, pregnancy, contraception, and RTIs/STDs among adolescent girls studying in vernacular (Odia medium) secondary girls’ high schools in Odisha, India.
Study setting
The current study was conducted in Bhubaneswar, the capital city of Odisha state in India. Schools in India are broadly categorized into four types based on the enrollment of students: Lower primary school (classes 1 to 5), Upper primary school (classes 6th and 7th), High school (classes 8th, 9th and 10th), and Higher secondary school (class 11th and 12th). Each state in the country runs its own Department of Education. Schools in each state are of three kinds: government schools, privately owned schools, and schools that are provided grant-in-aid by the government [ 24 ]. After reviewing the syllabus, it was found that there was not much emphasis made on SRH in the state curriculum. Hence schools under the Odisha State Board of Education were selected to conduct the present study. The study was conducted among vernacular (Odia medium) girls’ high schools in Bhubaneswar city. For the conduct of the study, permission was obtained from District Education Officer (DEO), Khordha. There are a total of eight vernacular girls’ high schools in Bhubaneswar City, and all the schools were included in the study.
Study design and sampling strategy
The study design was a cluster randomized trial conducted from May 2020 to April 2022. During this period, there was an ongoing COVID-19 pandemic. The schools remained closed as per guidelines from the Government of Odisha (GOO). The schools conducted online classes using various virtual platforms such as Zoom meetings, Google Meet, and YouTube. Permission was taken to assess the students through online and offline modes when required and to give education to school students through both online and offline modes depending upon the school closure. Written informed consent was taken from parents of adolescent girls, and assent was sought from adolescent girls.
For sample size calculation, as per a study conducted in Gujarat in the year 2017, the proportion of participants having awareness about STIs varied between 23 and 29% [ 25 ]. Considering a total average of 26% as a baseline and assuming a 15% increase at end-line assessment, the sample size was calculated using nMaster software. The total sample size obtained was 345, with α at a significance level of 0.05 and the power of study being 91, and with design effect 2. Considering attrition of ten per cent, the calculated sample size was 380 per arm.
The sampling frame included all eight government girls’ high schools (GHS) in Bhubaneswar, Odisha. Schools were considered as clusters, and restrictive randomization was done to randomize eight schools at a ratio of 1:1, with four schools in each intervention and control arm. For the selection of study participants as per protocol, systematic random sampling was to be done among adolescent girls studying in ninth and tenth classes. However, due to the COVID-19 pandemic, all those who responded to the baseline questionnaire were included, and an amendment in protocol was done regarding the same and was approved by Institute Ethics Committee (IEC), AIIMS Bhubaneswar. Outcome variables included changes in KAP pertaining to domains such as puberty, menstrual health, pregnancy and contraception, STIs/RTIs, and HIV/AIDS.
Baseline assessment
A pre-tested semi-structured questionnaire was developed, which was adopted from the Illustrative questionnaire for interview surveys with young people, World Health Organization [ 26 ]. The questionnaire consists of components such as socio-demographic details of the students and KAP in domains such as puberty, menstrual health, pregnancy, contraception, STIs/RTIs, and HIV/AIDS. The questions on KAP related to various domains of SRH were prepared with reference to the International technical guidance on sexuality education by the UNESCO education sector [ 27 ]. The document includes a section on key concepts pertaining to different topics, including SRH, where learners should acquire knowledge, attitudes and skills based on these key concepts. The knowledge component focused on evaluating adolescent girls’ understanding of pubertal changes, including the concept of the menstrual cycle, the process of pregnancy, risks associated with teenage pregnancy, the concept of contraception and its various methods, as well as awareness of RTI/STIs, and HIV/AIDS. The attitude component aimed to gauge adolescent girls’ beliefs regarding pubertal changes, menstruation hygiene management, their opinions on sex education, and their perception of how an HIV-infected person should be treated. The practice component primarily examined menstrual hygiene practices. Due to the cultural context of the Indian setting, the authors made a decision not to include questions on contraceptive practices in the assessment. The questionnaire was developed in English and later translated into the local language (Odia) with the help of a professional translator. Also, a back translation of the questionnaire from Odia to English was done to test the accuracy of the translation. The questionnaire was pre-tested among 36 students who were not a part of the selected schools. The questionnaire for the baseline assessment of students was delivered to the students through online Google forms. The assessment was done in August–September 2021 during the second wave of the COVID-19 pandemic. Google forms were delivered in WhatsApp groups of seven selected schools after obtaining consent from the school principal and teachers at respective schools. Of eight schools, one was a residential school, where students who resided in rural areas lacked access to smartphones. In the month of August 2021, schools were re-opened, and assessment of the students at residential school was done through offline forms.
Intervention
A literature search was done for the preparation of an intervention package on SRH education. The intervention package consisted of handbooks covering the following topics.
Handbook Part 1—Adolescent health statistics, Female reproductive system, Puberty, and Menstrual Health
Handbook Part 2—Pregnancy, Contraception, STIs/RTIs, and HIV/AIDS
The principal investigator has done a literature search through various websites of WHO and UNICEF, which focused on adolescent health. The relevant documents were then downloaded. The content required as per need has been retrieved from the documents and has been included in handbooks. Also, various Indian documents and modules pertaining to adolescent health, textbooks of school, and Obstetrics and Gynaecology, were referred for handbook preparation. The handbooks were developed in the English language. Since the vernacular language is Odia, the handbooks were translated into Odia by a professional Odia translator. The translated handbooks were given to two medico-social workers (MSWs) separately to verify comprehension of the language. The intervention was given in the months of November and December 2021 for the schools in the intervention arm. Owing to the COVID-19 pandemic, schools were running only half—a day, and accordingly, intervention timing was fixed. The author (AG) visited all the four schools in the intervention arm to provide SRH education to school-going adolescent girls. In each school, the intervention included three sessions. Three sessions were done on 3 consecutive days in each school. Each session lasted for about 2 h. The intervention was given to adolescent girls studying in ninth and tenth classes separately. In the first session, education was given on topics such as the female reproductive system, puberty, and menstrual health with the help of the first part of the handbook. The second session included the topics of part 2 of the handbook, i.e., pregnancy, contraception, STIs/RTIs, and HIV/AIDS. The intervention included a PowerPoint presentation with the help of a projector, brainstorming sessions, and a discussion of case scenarios. The third session was an interactive session between the students and teachers, and various doubts were cleared.
Following the intervention, an endline assessment was conducted 3 months later among all eight schools using online Google forms. The assessment of each school was done on 8 different days between the months of February and March 2022. Once the endline assessment was completed, the same intervention was provided to students in the control arm. The flow of the study design is depicted in Fig. 1 .
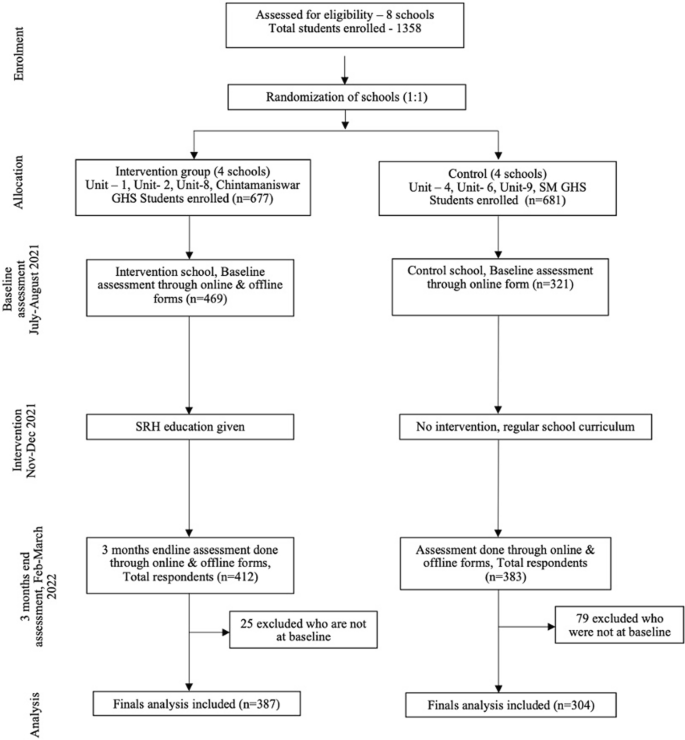
CONSORT flow diagram
Data entry and statistical analysis
The recorded responses were exported to Microsoft (MS) Excel except in one school where data was collected through offline forms and entered manually into MS Excel. The data entry was done simultaneously on the same day of the collection of data by the principal investigator. Statistical analysis was done using International Business Machines (IBM)—Statistical Package for social sciences (SPSS) version 26. Descriptive data on socio-demographic details of students are presented in percentage or proportion. Quantitative variables such as the age of the students are expressed as mean and standard deviation. To assess the effectiveness of the intervention, the proportion of students in KAP of all domains was considered. The proportional change was measured among the intervention and control groups before and after the intervention by using the Chi-square test. With the cells having a count less than five, Fischer exact test was used. A p-value of < 0.05 was considered significant.
The baseline sample included a total of 790 students from eight government vernacular (Odia medium) girls’ high schools. Among 790 students, 469 (59%) were in the intervention arm, and 321 (41%) were in the control arm. The mean age of students in the intervention arm was 14.4 ± 0.92 years, whereas in the control arm was 14.4 years ± 0. 8 years. The majority of students’ parents, both mother and father, studied till high school (37% and 34.3% respectively), and occupations included mothers being homemakers (91%) and fathers either clerk/shopkeeper/worker (39.7%). There was no statistically significant difference in baseline characteristics between intervention and control groups (Table 1 ).
Table 2 shows KAP pertaining to puberty and menstrual health among intervention and control arms at baseline and 3 months endline. At baseline, only 282 (60.1%) in the intervention arm and 171 (53.3%) in the control arm were aware that physical bodily changes due to puberty were normal. After the intervention, there was a statistically significant increase in knowledge in the intervention arm to 94.8% (n = 367) (p < 0.01). At baseline, 297 (63.3%) in the intervention arm and 215 (67%) in the control arm considered menstruation as a good thing, and after the intervention, there was a statistically significant (p < 0.01) increase in knowledge in the intervention group, where 362 (93.5%) considered menstruation a good thing in comparison to the control arm 219 (72%). Most students used sanitary pads as absorbent, 97.2% in the intervention group and 98.4% in the control group. However, after the intervention, the use of other absorbents was reduced to zero in the intervention group (p < 0.05).
Table 3 shows KAP pertaining to pregnancy, contraception, RTIs/STIs and HIV/AIDS among intervention and control arms at baseline and 3 months endline. Only 78 (16.6%) in the intervention group and 67 (20.9%) in the control group were aware that pregnancy could occur with a single sexual act; however, after the intervention, it increased to 81.3% in the intervention arm and in the control arm it was 16.8% (p < 0.01). Awareness on contraception was only 134 (28.6%) in the intervention arm and 113 (35.2%) in the control arm. After the intervention, there was a statistically significant increase, where 360 (93%) in the intervention arm and 105 (34.5%) in control became aware that pregnancy could be prevented by using contraceptives. Awareness on different methods of contraception was 51 (10.9%) in the intervention arm and 39 (12.1%) in the control. After the intervention, the awareness increased, where 337 (87.1%) in the intervention arm became aware of different methods of contraception (p < 0.01). At baseline, 177 (38.2%) in the intervention arm and 116 (36.4%) in the control arm were aware of STIs/RTIs; after the intervention, awareness increased to 96.1% in the intervention arm, and 44.1% in the control group were aware (p < 0.01). Regarding awareness on HIV/AIDS at baseline, students in the control arm (50.2%) were more aware when compared to the intervention arm (42.6%) with statistical significance (p < 0.05). However, after the intervention, awareness increased to 95.6% in the intervention arm and in the control arm, only 44.1% were aware (p < 0.01).
The current study assessed the effectiveness of SRH education among vernacular school-going adolescent girls. At baseline assessment, adolescent school-going girls lacked adequate knowledge pertaining to SRH. However, post-intervention, there was a significant increase in KAP in the intervention arm when compared to the control arm. There are studies conducted across various countries to assess the effectiveness of SRH education among adolescent girls, with outcomes having an increase in knowledge pertaining to SRH [ 28 , 29 , 30 , 31 , 32 , 33 , 34 ]. In India, only one randomized trial was conducted assessing peer education and conventional educational strategies for improving SRH. However, both were effective, and peer education was found to be more cost-effective [ 22 ]. To our knowledge, this is the first cluster randomized trial in India to assess the effectiveness of SRH education among school-going adolescent girls.
In our study, the intervention was provided by a community physician, with the intervention delivered using PowerPoint presentations and handbooks. The KAP increased in all domains, such as puberty, menstrual health, pregnancy, contraception, RTIs/STIs and HIV/AIDS following the intervention. In our study at baseline, about 50–60% of adolescent girls were aware of pubertal changes, and forty per cent of students said they were not comfortable when puberty-related topics were discussed. After the intervention, awareness on puberty increased to 94.8%. Our finding was similar to an interventional study conducted in Kerala among school-going adolescent girls, where pubertal awareness increased from 32 to 83.9%, where intervention was delivered through interactive and quiz sessions [ 20 ]. Hence, there is a need for sensitizing students regarding pubertal changes, and training of schoolteachers would be helpful. In our study, 60% of adolescents felt restriction of activities during menstruation. However, it was reduced to 22% following the intervention, indicating that there are still myths about menstruation. The majority of students attended schools during menstruation; Our study finding could be due to the provision of sanitary napkins free of cost under the “Khushi scheme” by the government of Odisha [ 35 ]. It can be inferred that the provision of sanitary napkins facilitated the attendance of adolescent girls, which can be correlated with a study conducted in Gujarat, where the provision of sanitary napkins reduced absenteeism from 24 to 14% [ 21 ]. In our study, most of the students, both in the intervention and control arm, felt that menstrual hygiene should be taught in schools as vernacular government girls’ high schools did not provide education on menstrual hygiene management (MHM) when imparted priorly at an earlier age before attaining menarche will inculcate healthy menstrual hygiene practices among adolescent girls.
In our study at baseline, only 20–30% of adolescent girls were aware of pregnancy and contraception. However, after the intervention, knowledge on pregnancy, different contraception and emergency contraception methods increased to 90%. In an interventional study conducted in Gujarat, knowledge pertaining to contraception increased from 10 to 32% among adolescent boys and girls [ 25 ]. In the study done in Kerala, adolescent girls who were unaware of the prevention of pregnancy reduced from 63 to 13% [ 20 ]. The study done in Kerala was about a decade ago, but still, no efforts have been made to provide a comprehensive SRH curriculum. Our study noted that at baseline, students were more aware of HIV/AIDS as a disease but were not aware of RTIs/STIs. This finding may be due to HIV/AIDS being a more deadly disease than RTIs/STIs and awareness being provided on various platforms such as social media and celebrating World AIDS Day. Also, at baseline, awareness of HIV/AIDS was more in the control arm when compared to intervention, and this finding was statistically significant. This could be because one of the intervention schools was a residential school with students hailing from rural areas, whereas students from control schools were residing in urban areas. However, after the intervention, awareness of RTIs/STIs increased to 90%. Our study finding was similar to a randomized trial conducted in countries such as Zimbabwe among secondary school students, where awareness of RTIs/STDs increased from 20 to 96% [ 36 ] and in the study conducted in Gujarat state, awareness regarding STIs increased from 29 to 32% [ 25 ]. Hence, by imparting education on pregnancy and contraception, adolescent girls can make informed choices regarding their sexual health. Moreover, in the study, about two-thirds of students favoured sex education to be taught in school. As mentioned earlier, in India, various states have banned sex education, but evidence from various studies conducted in India showed parents, teachers, and students favoured sex education in school and to be provided by doctors [ 37 , 38 , 39 ]. Also, evidence reviews from various countries by UNESCO have stated that CSE should be a holistic strategy where young people shape their sexual and reproductive future [ 40 ]. From our study findings, the inclusion of comprehensive education in regular schools, mainly government vernacular schools, is the key recommendation, along with the training of teachers pertaining to SRH by community physicians.
The current study design was ideal for knowing the real effectiveness of an intervention package. Even though the study was conducted during the ongoing COVID-19 pandemic, the study achieved an adequate sample size. Other randomized studies had lesser sample sizes. The intervention package was comprehensive and included all the topics pertaining to SRH; hence intervention was effective in improving KAP among all domains in the intervention arm. Efforts were made by the authors of the study to include all the participants at the follow-up who were present at baseline through phone calls to students and informing parents and teachers regarding the importance of the study, which resulted in less attrition even though the study was conducted during COVID-19 pandemic. Our study demonstrated that schools act as an excellent platform for imparting SRH education.
A few limitations of our study include, the study was conducted only among adolescent girls studying in vernacular (Odia) medium schools. From various study findings, it was observed that adolescent boys had more knowledge of SRH when compared to girls; the former could not be assessed in our study. Our follow-up period was 3 months; hence there is a need for long-term follow-up in further studies. The effectiveness of intervention can be compared between urban and rural areas and in all types of schools, such as private and English medium schools. Our study did not assess the contraceptive practices among adolescent girls; where only the knowledge component was assessed. The gap between the awareness and utilization of contraceptive methods needs to be assessed. Also, the study did not assess sexual activity following intervention which recommends further studies to assess contraceptive usage, sexual activity, and incidence of teenage pregnancies. There are no randomized trials conducted which assessed these domains in an Indian setting owing to cultural taboos. Hence, there is a need for further evidence to strengthen the interventions pertaining to adolescent SRH.
Scale-up assessment: considering the seven key categories for scaling up in the sense of global health, an assessment of the current strategy was done [ 41 ]. The National Health Policy of India (NHP), 2017 clearly envisages the provision of sexual health education to adolescents [ 42 ]. Thus, the current strategy of implementing comprehensive SRH education in schools has a national focus, scale neutral, with a well-defined scaling strategy for a targeted group of adolescents in any geographic region. The intervention package developed was in accordance with recommendations provided by WHO on comprehensive sexuality education and addresses a significant and persistent problem that is currently high on the agenda of NHP of India. The current strategy resulted in KAP in all domains of SRH with a large effect size when compared to any other study conducted in the Indian state. Each section of the module was prepared after a robust review of the literature, making it both country and state specific to meet the need of adolescent girls. The study was funded by the Indian Council of medical research and the MAMTA Institute for Mother and Child, implicating support for change.
The intervention was delivered through schools, which are already established educational institutions. Training teachers and frontline workers to deliver SRH education could potentially be integrated into existing educational programs. Thus, the model can be implemented with existing educational institutional mechanisms, infrastructure, and human resources, including field functionaries of the health department, NGOs and other private stakeholders engaged in implementing health programs at the micro level, indicating a great fit between intervention and any adopting organization. The intervention provided is a collaborative approach with permission obtained from school mass education. National health programs, namely Ayushmann Bharat [ 43 ], envisage outreach visits to schools by healthcare workers to provide counselling services to adolescents. The intervention can be integrated through and scaled out through current programs such as Ayushman Bharat, RKSK, state-owned programs, and various international organizations working on adolescent health with adequate and sustainable funding, a strong network, trained manpower and microlevel institution mechanisms.
Adolescent girls face various issues pertaining to sexual and reproductive health in day-to-day life. Our study assessed the effectiveness of school-based SRH education among school-going adolescent girls in urban areas of Odisha, India. The study showed a significant increase in knowledge, attitude, and practices pertaining to SRH among students in the intervention arm compared to the control arm. The study has generated evidence that schools can act as a platform for providing SRH education to adolescents, which is an immediate need of the hour in shaping healthy young people for the future. Based on the evidence, policymakers and the Department of School Mass Education should include comprehensive SRH education in the regular school curriculum for adolescents’ health and well-being.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Change history
13 september 2023.
A Correction to this paper has been published: https://doi.org/10.1186/s12978-023-01668-y
Abbreviations
Sexual and Reproductive Health
World Health Organization
United Nations Children’s Fund
Comprehensive sexuality education
United Nations Population Fund
National family health survey
Government of India
Rashtriya Kishore Swasthya Karyakram
Adolescent friendly health Clinics
Sexually Transmitted Infections
Reproductive Tract Infections
Human immunodeficiency virus/acquired immunodeficiency syndrome
Knowledge, Attitude, and Practices
Government of Odisha
District Education Officer
Institute Ethics Committee
Government Girls’ High School
Medico-Social Workers
Microsoft; IBM: International Business Machines
Statistical package for social sciences
Menstrual hygiene management
National Health Policy
Adolescents statistics—UNICEF data. https://data.unicef.org/topic/adolescents/overview/ . Accessed 29 June 2022.
Porroche-Escudero A. Health systems and quality of healthcare: bringing back missing discussions about gender and sexuality. Health Syst. 2022. https://doi.org/10.1080/20476965.2022.2096487 .
Article Google Scholar
Sexual & reproductive health. https://www.unfpa.org/sexual-reproductive-health . Accessed 29 June 2022.
Adolescent sexual and reproductive health. https://www.who.int/southeastasia/activities/adolescent-sexual-reproductive-health . Accessed 23 Apr 2023.
Weis JR, Greene JA. Mental health in pregnant adolescents: focus on psychopharmacology. J Pediatr. 2016;169:297–304.
Article PubMed Google Scholar
Child marriages—39,000 every day: more than 140 million girls will marry between 2011 and 2020. https://www.who.int/news/item/07-03-2013-child-marriages-39-000-every-day-more-than-140-million-girls-will-marry-between-2011-and-2020 . Accessed 4 July 2022.
Hodgkinson SC, Colantuoni E, Roberts D, Berg-Cross L, Belcher HME. Depressive symptoms and birth outcomes among pregnant teenagers. J Pediatr Adolesc Gynecol. 2010;23(1):16.
THE 17 GOALS | Sustainable development. https://sdgs.un.org/goals . Accessed 21 June 2023.
WHO. Global accelerated action for the health of adolescents (AA-HA!) guidance to support country implementation. WHO. 2017;9. https://apps.who.int/iris/bitstream/handle/10665/255415/9;jsessionid=B309C8C56E5EEFA24FA2F606422AB847?sequence=1 . Accessed 14 Aug 2022.
Adolescent development and participation | UNICEF India. https://www.unicef.org/india/what-we-do/adolescent-development-participation . Accessed 5 July 2022.
Adolescent health (RKSK): National Health Mission. https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=818&lid=221 . Accessed 29 June 2020.
Barua A, Watson K, Plesons M, Chandra-Mouli V, Sharma K. Adolescent health programming in India: a rapid review. Reprod Health. 2020;17(1):1–10.
ARSH programme overview: National Health Mission Odisha. https://nhmodisha.gov.in/writereaddata/Upload/Documents/ARSH%20for%20web.pdf . Accessed 20 June 2023.
Hoopes AJ, Agarwal P, Bull S, Chandra-Mouli V. Measuring adolescent friendly health services in India: a scoping review of evaluations. Reprod Health. 2016;13(1):1–38.
Release of NFHS-5 (2019–21)—compendium of factsheets | Ministry of Health and Family Welfare | GOI. https://main.mohfw.gov.in/basicpage-14 . Accessed 16 Aug 2022.
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–78.
Article PubMed PubMed Central Google Scholar
Sood N, Suman P. Report to the United Nations Human Rights Council for the universal periodic review of the Republic of India on the lack of comprehensive sexuality education in India. Youth Coalition.
States in India ban sex ed to preserve culture. https://www.nbcnews.com/id/wbna18723555 . Accessed 5 July 2022.
Deshmukh DD, Chaniana SS. Knowledge about sexual and reproductive health in adolescent school-going children of 8th, 9th, and 10th standards. J Psychosexual Health. 2020;2(1):56–62.
Nair MKC, Paul MK, Leena ML, Thankachi Y, George B, Russell PS, et al. Effectiveness of a reproductive sexual health education package among school going adolescents. Indian J Pediatr. 2012;79(S1):64–8. https://doi.org/10.1007/s12098-011-0433-x .
Dongre AR, Deshmukh PR, Garg BS. The effect of community-based health education intervention on management of menstrual hygiene among rural Indian adolescent girls. World Health Popul. 2007;9(3):48–54.
Article CAS PubMed Google Scholar
Parwej S, Kumar R, Walia I, Aggarwal AK. Reproductive health education intervention trial. Indian J Pediatr. 2005;72:287–91.
Bundy DAP, Schultz L, Sarr B, Banham L, Colenso P, Drake L. The school as a platform for addressing health in middle childhood and adolescence. In: Child and adolescent health and development, vol. 8. 3rd ed. Disease control priorities. Washington: World Bank Group; 2017. p. 269–86.
Google Scholar
The education system in India—GNU project—free software foundation. https://www.gnu.org/education/edu-system-india.en.html . Accessed 22 July 2022.
Patel P, Puwar T, Shah N, Saxena D, Trivedi P, Patel K, Yasobant S, Fancy M, Matela H, Savaliya S, Kalpana P. Improving adolescent health: learnings from an interventional study in Gujarat, India. Indian J Community Med Off Publ Indian Assoc Prev Soc Med. 2018;43(Suppl 1):S12.
Cleland J. Illustrative questionnaire for interview-surveys with young people. World Health Organization. References—Scientific Research Publishing. 2001. https://www.scirp.org/(S(czeh2tfqyw2orz553k1w0r45))/reference/ReferencesPapers.aspx?ReferenceID=1950110 . Accessed 24 July 2022.
International technical guidance on sexuality education: an evidence-informed approach. 2018. https://unesdoc.unesco.org/ark:/48223/pf0000260770 . Accessed 21 June 2023.
Thato R, Jenkins RA, Dusitsin N. Effects of the culturally-sensitive comprehensive sex education programme among Thai secondary school students. J Adv Nurs. 2008;62(4):457–69.
Stephenson JM, Strange V, Forrest S, Oakley PA, Copas A, Allen E, et al. Pupil-led sex education in England (RIPPLE study): cluster-randomised intervention trial. Lancet. 2004;364(9431):338–46.
Conboy Martiniuk AL, O’Connor KS, King WD. A cluster randomized trial of a sex education programme in Belize, Central America. Int J Epidemiol. 2003;32(1):131–6.
Darabi F, Yaseri M, Kaveh MH, Khalajabadi Farahani F, Majlessi F, Shojaeizadeh D. The effect of a theory of planned behavior-based educational intervention on sexual and reproductive health in Iranian adolescent girls: a randomized controlled trial. J Res Health Sci. 2017;17(4):400.
PubMed Central Google Scholar
Kirby D, Laris BA. Effective curriculum-based sex and STD/HIV education programs for adolescents. Child Dev Perspect. 2009;3(1):21–9.
Kemigisha E, Bruce K, Ivanova O, Leye E, Coene G, Ruzaaza GN, et al. Evaluation of a school based comprehensive sexuality education program among very young adolescents in rural Uganda. BMC Public Health. 2019;19(1):1393.
Li C, Cheng Z, Wu T, Liang X, Gaoshan J, Li L, et al. The relationships of school-based sexuality education, sexual knowledge and sexual behaviors—a study of 18,000 Chinese college students. Reprod Health. 2017;14(1):1–9.
Odisha government approves Rs 466 crore for ‘Khushi’ scheme to provide free sanitary pads | menstrual hygiene. NDTV. 2019. https://swachhindia.ndtv.com/odisha-government-approves-rs-466-crore-for-khushi-scheme-to-provide-free-sanitary-pads-31591 . Accessed 7 July 2020.
Rusakaniko S, Mbizvo MT, Kasule J, Gupta V, Kinoti SN, Mpanju-Shumbushu W, et al. Trends in reproductive health knowledge following a health education intervention among adolescents in Zimbabwe. Cent Afr J Med. 1997;43(1):1–6.
CAS PubMed Google Scholar
Kumar R, Goyal A, Singh P, Bhardwaj A, Mittal A, Yadav SS. Knowledge attitude and perception of sex education among school going adolescents in Ambala District, Haryana, India: a cross-sectional study. J Clin Diagn Res. 2017;11(3):LC01.
PubMed PubMed Central Google Scholar
McManus A, Dhar L. Study of knowledge, perception and attitude of adolescent girls towards STIs/HIV, safer sex and sex education: (a cross sectional survey of urban adolescent school girls in South Delhi, India). BMC Womens Health. 2008;8:1–6.
Ahuja V, Patnaik S, Gurchandandeep, Lugani Y, Sharma N, Goyal S, et al. Perceptions and preferences regarding sex and contraception, amongst adolescents. J Fam Med Prim Care. 2019;8(10):3350.
Review of the evidence on sexuality education: report to inform the update of the UNESCO International technical guidance on sexuality education. https://healtheducationresources.unesco.org/library/documents/review-evidence-sexuality-educationreport-inform-update-unesco-international . Accessed 18 July 2020.
Cooley L, Kohl R, Ved R. Scaling up—from vision to large scale change: a management framework for practitioners. Washington, DC: Management Systems International; 2016.
Ministry of Health and Family Welfare, Government of India. National health policy 2017. https://main.mohfw.gov.in/sites/default/files/9147562941489753121.pdf . Accessed 24 Apr 2023.
About Pradhan Mantri Jan Arogya Yojana (PM-JAY) | Official Website Ayushman Bharat Pradhan Mantri Jan Arogya Yojana | National Health Authority. https://pmjay.gov.in/about/pmjay . Accessed 4 Jan 2022.
Download references
Acknowledgements
Not applicable.
The study is funded by an ICMR grant [No 3/2/June-2020/PG-Thesis-HRD (15)] and MAMTA fellowship ID: 2020 21/MD/006 health institute for Mother and Child, New Delhi. Funding was used for the preparation of handbook materials, assessment forms, travel to the schools, stationaries, and refreshments for school students.
Author information
Authors and affiliations.
Department of Community Medicine and Family Medicine, AIIMS Bhubaneswar, 3rd Floor, Academic Block, Bhubaneswar, Odisha, 751019, India
G. Alekhya, Swayam Pragyan Parida & Prajna Paramita Giri
Department of Obstetrics and Gynaecology, AIIMS Bhubaneswar, Bhubaneswar, Odisha, India
Suravi Patra
Department of Psychiatry, AIIMS Bhubaneswar, Bhubaneswar, Odisha, India
Jasmina Begum
WHO NTEP, Bhubaneswar, Odisha, India
Dinesh Prasad Sahu
You can also search for this author in PubMed Google Scholar
Contributions
SPP, PPG, JB, and SP conceptualized the study. Data collection was done by AG. AG and DPS prepared the handbook materials for intervention under the guidance of SPP, PPG, JB, and SP. AG and DPS conducted and analyzed the study under the supervision of SPP, PPG, JB, and SP. AG wrote the manuscript with inputs from SPP, PPG, JB, SP, and DPS. All authors approved the final manuscript.
Corresponding author
Correspondence to Swayam Pragyan Parida .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from Institute Ethics Committee (IEC), AIIMS Bhubaneswar, with reference number IEC/AIIMS BBSR/PG Thesis/2020-21/51. Permission was obtained from the District Education Officer (DEO), Khordha, for the conduct of the study. Informed verbal consent was taken from the principal and school teachers. Assent from the students and written informed consent from their parents were taken.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: the legend for Table 3 was inadvertently omitted.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Alekhya, G., Parida, S.P., Giri, P.P. et al. Effectiveness of school-based sexual and reproductive health education among adolescent girls in Urban areas of Odisha, India: a cluster randomized trial. Reprod Health 20 , 105 (2023). https://doi.org/10.1186/s12978-023-01643-7
Download citation
Received : 31 March 2023
Accepted : 27 June 2023
Published : 19 July 2023
DOI : https://doi.org/10.1186/s12978-023-01643-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescence
- Adolescent girls
- Sexual and reproductive health
- Adolescent sexual and reproductive health
- School health
- Health education
- Randomized trials
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health
- PMC10002018

Adolescent Pregnancy Outcomes and Risk Factors
Jana diabelková.
1 Department of Public Health and Hygiene, Medical Faculty, University of Pavol Jozef Šafárik, Šrobárova 2, 041 80 Košice, Slovakia
Kvetoslava Rimárová
Peter urdzík.
2 Department of Gynaecology and Obstetrics, Medical Faculty, Louis Pasteur University Hospital, University of Pavol Jozef Šafárik, Trieda SNP 1, 040 11 Košice, Slovakia
Andrea Houžvičková
Ľubica argalášová.
3 Institute of Hygiene, Faculty of Medicine, Comenius University in Bratislava, Špitálska 24, 813 72 Bratislava, Slovakia
Associated Data
The data presented in this study are available on request from the corresponding author.
One of the major social and public health problems in the world is adolescent pregnancy. Adolescent pregnancy is strongly associated to less favorable results for both the mother and the newborn. We conducted this research to ascertain the impact of teenage age on neonatal outcomes and also observed the lifestyles of pregnant teenage girls. We conducted a study of 2434 mothers aged ≤19 years (n = 294) or 20–34 years (n = 2140) who gave birth in 2019–2020 at the Department of Gynaecology and Obstetrics of Louis Pasteur University Hospital in Košice. The data on mothers and newborn infants have been reported from the reports on mothers at childbirth. Women between the ages of 20 and 34 served as the reference group. The teenage mothers were more likely to become pregnant if they were unmarried (OR = 14.2; 95% CI = 9.3–21.6; p < 0.001) and had a basic education or lack of education (OR = 16.8; 95% CI = 11.5–24.6; p < 0.001). Additionally, they were more likely to smoke when pregnant (OR = 5.0; 95% CI = 3.8–6.6; p < 0.001). Low birth weight was more common in newborns born to adolescent mothers than in those born to adult mothers ( p < 0.001). Our findings showed that infants of teenage mothers often had lower birth weights (−332.6 g, p < 0.001). Adolescent mothers were associated with lower Apgar scores at the first minute ( p = 0.003). As compared with the control group, pregnant teenage girls had a greater prevalence of preterm deliveries in our research ( p = 0.004). This study finds significant age-related disparities in neonatal outcomes between mothers. These results might be used to identify vulnerable groups who need special assistance and actions to reduce the probability of negative outcomes for such groups.
1. Introduction
Adolescent pregnancies are a global public health problem. Teenage pregnancy is the pregnancy of 10- to 19-year-old girls [ 1 ]. Adolescents are further divided into early (10–14 years old), middle (15–17 years old), and late adolescents (over 17 years old) [ 2 ].
According to the World Health Organization, adolescent pregnancies are a global problem for both developed and developing countries. Although the global teenage birth rate has decreased, there are regional differences in the rates of change. Adolescent pregnancies have decreased globally, from 64.5 per 1000 women in 2000 to 42.5 per 1000 women in 2021. However, there are huge differences in levels between and within countries. While the estimated global teenage birth rate has decreased, the actual number of childbirths to teenagers continues to be high. Pregnancy in girls under the age of 19 is severe in every aspect and requires very complex and long-term solutions [ 1 ].
The transition from childhood to adulthood occurs during the phase of adolescence, during which there are numerous changes in the physiological, anatomical, structural, and psychological aspects. Because many teenagers are not physically or mentally prepared for pregnancy and childbirth, they are more likely to experience complications that can have serious health consequences. Giving birth during adolescence has serious consequences for the health of the mother and her infant [ 1 ]. The adolescent age group is associated with adverse pregnancy outcomes [ 2 , 3 ].
The rate of teenage pregnancies has recently been greatly affected by several significant factors. The decreasing age at menarche is one of the factors that can affect a woman’s fertility. Since the 19th century, the age at menarche has been decreasing at a rate of 2–3 months per decade in many European countries, resulting in an overall decrease of about 3 years. Most of the decrease in menarche age is related to better nutrition and health. The onset of first sexual activity occurs at a significantly younger age, which is another contributing element. Teenage pregnancy, therefore, remains a serious social, economic, and health problem [ 4 ].
Young maternal age is more likely a marker for one or more other maternal risk factors associated with poor birth outcomes. Poverty, low education, and inadequate family support are also problems. These factors increase the risk of sexually transmitted infections, unsafe abortions, and birth complications, all of which are exacerbated by inadequate prenatal care [ 5 ]. For girls, early pregnancies can have social consequences such as lower status in the household and community; stigmatization; abuse by family, peers, and partners; and early and forced marriage. Early pregnancy and childbirth during adolescence can hinder a girl’s otherwise healthy development into adulthood and negatively affect her educational opportunities, financial security, and health. Many teenage girls who are pregnant cannot continue their education or work because they are pregnant. This can have a big impact on their future [ 6 ]. In addition, children born to parents who cannot care for them face additional dangers. In the first few years of a child’s life, the mother–child relationship declines. This is primarily due to the mother’s immaturity. When teenage mothers are victims of sexual assault, the situation is even worse. Apart from their mothers, these children tend to be brought up by their grandparents and relatives, with frequent changes in caregivers. Children have a higher risk of being abused or neglected and a higher risk of failing in school and are more likely to engage in criminal behavior later on [ 7 ].
The economic, social, and political development and progress of any country depend on the healthy size of adolescents and children. As a result, the healthier the teenager is, the healthier the nation and future generations will be. Teenagers thus need special attention from us.
Understanding the issue is necessary to develop and carry out prevention initiatives to decrease teen pregnancy. Knowledge about the target groups, teenage pregnancy and birth outcomes, and the risk and preventive factors related to teenage pregnancy is needed. This information is important in choosing which risk and protective factors to target and, thus, better implementing the effective implementation of evidence-based adolescent pregnancy prevention practices.
Examining the newborn outcomes and risk variables associated with adolescent pregnancies was the aim of the present research.
2. Materials and Methods
The research took place in the years 2019–2020 in eastern Slovakia. This study included 2434 newborns and their mothers. Data were collected at the University of Pavel Jozef Šafárik’s Faculty of Medicine and the Louis Pasteur University Hospital’s Gynecology and Obstetrics Clinic in Košice. This hospital has a higher prevalence of mothers with high-risk pregnancies because it is the East Slovakian center for low birth weight and preterm birth.
The data were obtained from hospital records. Available information included the mother’s education, marital status, lifestyle, and when prenatal care began. Additionally, the Apgar scores at 1 and 5 min, the newborn’s gestational age, and the newborn’s weight were recorded. The total number of mothers in the results tables was different because not all the data for each mother were available in the clinical records. The study excluded women who were carriers of multiple pregnancies because they had a higher risk of preterm birth and lower birth weights of their newborns. Thus, women with multiple pregnancies were not included among the participants.
Maternal age was defined as the mother’s age in completed years at the time of delivery. The youngest women recruited to the cohort were 14 years old; therefore, the data for this study were limited to women aged 14–34 years at delivery who had a singleton pregnancy. The results for women under the age of 19 were compared with the results for women in the reference group (20–34 years). The age range of 20 to 34 years was chosen as the reference group because this age range had the lowest risk of developing age-related problems.
In our records, a woman who smoked at least one cigarette per day while pregnant was considered a smoker. All women who consumed 15 g of alcohol per day were considered alcohol consumers. This is equivalent to 0.5 L of 12-degree beer, 0.3 L of wine, or 0.5 dL of strong alcohol.
The neonatal outcome variables of interest in this study were low birth weight (less than 2500 g), very low birth weight (less than 1500 g), extremely low birth weight (less than 1000 g), macrosomia (birth weight greater than 4000 g), preterm birth (less than 37 weeks gestation), very preterm birth (less than 32 weeks gestation), extremely preterm birth (less than 28 weeks gestation), and low Apgar score at the first and fifth minutes (less than 7).
Most mothers completed eight prenatal care visits. Thus, we divided the group of mothers into two groups: those who had fewer than eight antenatal visits and those who had eight or more visits.
The IBM SPSS Statistics 23.0 program (IBM SPSS Statistics for Windows, Version 23.0. IBM Corp., Armonk, NY, USA) was used to analyze the data. The data were given as median (min–max), mean (standard deviation), and number (percent).
The data were processed using both primary characters and modified characters (categorized). Most of the findings were statistically significant, and the analysis included important discoveries that were related to the collected empirical data. The χ2 independence test, with a significance level of 0.05, was used to assess the frequency of individual variations of characteristics in the analyzed groups and subgroups. The Student’s t -test was used to compare the arithmetic means of continuous variables. The odds ratio, or, was used to compare the frequency of social and anamnestic variables in the adolescent mothers and mothers from the reference group.
Data were available for 2434 pregnancies for this analysis. A total of 294 (12.1%) of these births included teenagers between the ages of 14 and 19. The controls were 27.9 ± 3.9 years old on average, whereas the adolescents’ mean age was 17.4 ± 1.4. Table 1 displays the characteristics of the study’s participants.
Characteristics of the sample by maternal age.
Numbers in bold indicate statistically significant values.
Our study demonstrated that adolescent mothers had lower levels of education ( p < 0.001), only primary school (84.1%). About 46% of teenage girls reported smoking during pregnancy. In the reference group, the proportion of smokers was 14.6% ( p < 0.001). Alcohol consumption during pregnancy was relatively low at 0.6%, and the data on alcohol use were not statistically significant ( Table 1 ).
In the adolescent group, there were up to 45.7% of women ( p < 0.001) who went to the doctor after the first trimester. Most mothers completed eight prenatal care visits. Therefore, we divided the group of mothers into two groups: those who had fewer than eight antenatal visits and those who had eight or more visits. Up to 75.9% of teenage girls who were pregnant had fewer than eight clinic visits ( p < 0.001) ( Table 2 ).
Antennal care received by the respondents.
Adolescent girls were significantly more likely to be single (OR = 14.2; 95% CI = 9.3–21.6; p < 0.001), to have less education (OR = 16.8; 95% CI = 11.5–24.6; p < 0.001), and to smoke during pregnancy (OR = 5.0; 95% CI = 3.8–6.6; p < 0.01). They were more likely to visit a doctor for the first time during pregnancy after the first trimester (OR = 0.3; 95% CI = 0.2–0.3; p < 0.001) and were more likely to visit a doctor fewer than eight times (OR = 4.0; 95% CI = 3.0–5.3; p < 0.001) during pregnancy ( Table 3 ).
OR of various risk variables for adolescent mothers’ reproductive outcomes.
OR—odds ratio; CI—confidence interval. Numbers in bold indicate statistically significant values.
Table 4 shows the results for newborns. Infants born to teenage mothers had a significantly higher rate of low birth weight than those born to women who were adults ( p < 0.001). Our findings showed that children born to teenage mothers weighed less on average (−332.6 g, p < 0.001). In contrast to the control group, pregnant adolescents in our analysis had a higher prevalence of premature births ( p = 0.004). Children of adolescent mothers had a lower first-minute Apgar score ( p = 0.003).
Neonatal outcomes.
4. Discussion
Pregnancy in adolescence is a health problem worldwide. Teenagers themselves are a high-risk group in need of high-priority interventions. In general, most pregnancies in adolescence are extra-marital and unintended [ 2 ]. The teenage mothers in this research were more likely to be single (OR = 14.2; 95% CI = 9.3–21.6; p < 0.001), which is similar to previous studies [ 5 , 8 , 9 , 10 ].
Psychological immaturity is common among adolescent mothers. Because they do not understand the value of family planning, they often engage in risky sexual behavior and become pregnant while still in school and still living with their parents [ 9 ]. This study confirms that teenage mothers are significantly more likely to have a low level of education ( p < 0.001). These findings agreed with those of other research investigations carried out in other nations [ 2 , 9 ]. Adolescent girls often drop out of school due to pregnancy or childbirth. Sometimes problems at school and poor school performance appear even before pregnancy. Some teenage girls who are not doing well in school may find motherhood an attractive option. When these variables combine, young mothers have fewer career possibilities, often resulting in lower earnings for the rest of their lives [ 9 , 11 ]. Early pregnancies are significantly reduced by education; the more years of education, the lower the rate of early pregnancies [ 1 ].
Quitting smoking has a direct impact on the health of the fetus. Teenagers in our research were more likely to smoke during pregnancy (OR = 5.0; 95% CI = 3.8–6.6; p < 0.001). Previous research has shown that several high-risk activities are associated with a higher likelihood of pregnancy. These activities included the use of tobacco products, drinking alcohol, drug use, and risky sexual behavior [ 9 , 10 , 12 , 13 , 14 ].
Teenagers need accurate information about where to go when they need advice and help. Numerous studies have highlighted the benefits of prenatal care in minimizing pregnancy risks [ 9 , 15 , 16 , 17 ]. Unlike controls, pregnant adolescent girls in our study used prenatal care services less frequently. This was confirmed by a later gestational age at the first visit ( p < 0.001) and a lower number of visits to the doctor during pregnancy ( p < 0.001). This may be a result of a lack of information about the community services offered and the benefits of providing early and routine care. Teenagers may think they are not entitled to prenatal care, or they may choose to keep the pregnancy a secret [ 9 , 11 , 18 ]. Pregnant teenagers often interrupt school attendance, partly because of their participation in prenatal care. If clinic times are compatible with school attendance and medical staff are sensitive to adolescent needs, antenatal visits are more likely to be attended. Therefore, the needs of adolescents must be taken into account when providing prenatal care. However, direct study comparisons are difficult as there are different definitions of appropriate prenatal care. Regardless of how prenatal care is defined, the data suggest that adolescents tend to receive less adequate care than adult women [ 3 , 8 , 14 , 19 , 20 , 21 ]. Similar findings were obtained by Kassa et al. [ 22 ], who found that the number of antenatal care visits was lower in the teenage group and that doctor visits started later in pregnancy in this group. De Vienne et al. [ 23 ], on the other hand, did not find a difference between younger and older women in the analyzed age categories. Quinlivan and Evans published a study [ 24 ] comparing the outcomes of adolescents attending either a general or a specialist antenatal clinic for teenagers. In adolescent pregnancy clinics, prenatal care was provided by a multidisciplinary team and included social support and thorough infection screening. The rate of preterm births has decreased significantly as a result of the care provided at teen pregnancy clinics. According to the authors, the key strategies were the prevention of ascending infections of the genital tract and the provision of comprehensive treatment for teenagers. Healthcare professionals should be aware that teenage pregnancies are high-risk pregnancies and educate young women about the value of prenatal care and frequent antenatal visits.
In our study, preterm births were more common among pregnant teenage mothers than in controls ( p = 0.004), which is similar to previous studies [ 25 , 26 , 27 , 28 , 29 , 30 ]. Due to the fact that preterm birth is a complex pregnancy problem, it is complicated to identify the exact cause. According to Debiec et al. [ 17 ], preterm birth is more common in teenagers who receive insufficient prenatal care, which supports the hypothesis that poor prenatal care is a risk factor for preterm birth. However, Chen et al. [ 4 ] point out that the risk of preterm birth persisted even in women who received adequate prenatal care. Yadav et al. [ 10 ] found that preterm birth was significantly more common in teenagers. According to them, the rise might be attributed to biological immaturity and socioeconomic deprivation. Clinically indicated preterm births may be the result of medical conditions such as intrauterine growth restriction or spontaneous labor. Both spontaneous preterm birth and intrauterine growth restriction are associated with maternal malnutrition, and there is strong evidence linking both conditions to maternal smoking during pregnancy [ 13 , 18 , 31 , 32 , 33 , 34 , 35 ]. Adolescent mothers are more likely to deliver preterm due to gynecological immaturity (such as a short cervix [25 mm] and a small uterine volume) and susceptibility to subclinical infections. Other studies suggest that these risks are related to biological immaturity in adolescent females and are not related to social deprivation, smoking, or inadequate prenatal care [ 27 , 36 , 37 ].
In this study, the percentage of low birth weight in infants born from adolescent mothers was higher than in mothers who gave birth in adulthood ( p < 0.001), which is similar to previous studies [ 23 , 27 , 28 , 29 , 38 , 39 ]. It is thought that growing adolescents may compete with the fetus for resources, which might hinder fetal development and lead to low-birth-weight newborns or newborns that are small for their gestational age [ 40 ]. Marvin-Dowle et al. [ 40 ] conducted research in England among women aged 19 years and 20–34 years to examine the relationship between maternal and newborn outcomes in teenage women. Extremely low birth weight was found to be significantly more common in the teenager group compared with the control group.
Extremely underweight newborns have a higher risk of death within the first few months of life [ 12 ] as well as long-term problems with their physical and cognitive development [ 9 , 11 ]. Extremely low birth weight was not more common in our study cohort of adolescent mothers ( p = 0.246).
The term Apgar, or appearance, pulse, grimace, activity, and respiration, was created by Doctor Virginia Apgar. This score is a simple method for evaluating neonates one and five minutes after birth. A newborn’s Apgar score is determined by several variables, including color, heart rate, reflexes, muscle tone, and breathing. Scores for each item range from 0 (zero), 1, or 2, with a total score of 7 to 10 considered good [ 41 ]. No significant difference in the low Apgar score between adolescent and adult pregnancies was found when compared with hospital-based retrospective cohort research in Nepal by Yadav et al. [ 10 ]. Due to several sociodemographic, obstetric, and dietary factors, low Apgar scores occur more frequently in teenage pregnancies than in adult pregnancies [ 3 , 22 ]. In a study conducted over 6 years in Japan with 30,831 women under the age of 25 who were pregnant with a singleton, Ogawa et al. [ 29 ] examined the relationship between adolescent pregnancy and adverse outcomes. They found that low Apgar scores were significantly more common among adolescent mothers than among mothers aged 20 to 24 [ 29 ]. Low Apgar scores are associated with infant complications such as breathing difficulties, feeding problems, hypothermia, and seizures [ 42 ]. Low Apgar scores at five minutes correlate with mortality and may indicate a higher likelihood of cerebral palsy [ 41 ]. In our study, the difference in the prevalence of low Apgar scores between adolescent mothers and the control group was confirmed only when the Apgar score was evaluated after the first minute ( p = 0.003).
The development of social policy can be improved by having a thorough understanding of all these socioeconomic factors that influence teen pregnancy.
The first and most important step in strategies to reduce adolescent pregnancies and associated poor neonatal outcomes should be to “prevent it”. Measures to reduce the prevalence of teenage pregnancy also include increasing the importance of education. Although there are many different techniques to prevent a young girl from becoming pregnant, sexual abstinence is the only one that is 100% successful. This approach is the only one that ensures zero pregnancy risk and safeguards the adolescent from contracting any STDs. It is important to make teenagers aware of the responsibility that comes with sexual activity. The more information teenagers receive about this topic, the higher the chance that they will behave cautiously.
Teenagers should be educated about the negative consequences of teenage pregnancy, especially by their parents and at school. Building adolescents’ knowledge, skills, resilience, and aspirations through relationships and education helps them delay sexual activity until they are ready; enjoy healthy, consensual relationships; and use family planning methods. Schools may play a role by encouraging students to make mature decisions about their sex and by disseminating the knowledge needed to prevent adolescent pregnancy.
Teenagers are more likely to have their first sexual experience later in life if they and their parents have open discussions about relationships and sexual health from a young age. When parents spend time discussing sex and family planning with their children, they can have a significant impact on their decisions. Some parents have trouble talking about this topic. The barriers to parental communication include embarrassment, concern that discussion may encourage early sexual activity, and uncertainty about how to properly answer questions. Parents and all practitioners who come into contact with young people therefore need guidance on how to talk to them.
5. Conclusions
In conclusion, pregnancies in adolescents should be considered high-risk pregnancies. It is necessary to emphasize the need for comprehensive prenatal care for pregnant adolescent children because insufficient prenatal care can be harmful to both the mother and her fetus. Promoting early and thorough prenatal care is a key strategy if adolescent pregnancy outcomes are to be improved. Addressing teen pregnancy also requires a major effort by families, service providers, schools, faith-based and community organizations, recreation centers, policymakers, and youth. Teenagers should be educated about the negative consequences of teenage pregnancy, especially by their parents and at school. Our results confirm the relatively high prevalence of pregnant adolescent girls who smoked. Education should therefore also focus more on the risks associated with the use of substances during pregnancy.
The most important elements in preventing unwanted teenage pregnancies are a functional and stable family, good relations between parents, and good relations between parents and children. Parents should be the main source of information about sex. Adolescent pregnancy is not only a medical problem but also a social and societal problem, so society also plays an important role in preventing unwanted pregnancies, spreading awareness among young people, and holding them accountable for their actions.
6. Limitation
The conclusions of this study must be interpreted in light of limitations in the dataset and study design. For example, this study cannot adequately control for such factors as infectious exposure and drug use, which may differ between the groups.
Funding Statement
This work was supported by grants KEGA No. 008UPJŠ-4/2020, KEGA 010UPJŠ-4/2021 of the Ministry of Education, Science, Research and Sport of the Slovakia and 015UK-4/2022. We also thank the directory board of the Department of Gynaecology and Obstetrics at Louis Pasteur University Hospital in Košice for assistance with organization of sample collection at the hospital wards.
Author Contributions
J.D., K.R. and P.U. designed the project; J.D. and A.H. participated in data analysis; J.D. was responsible for interpretation and writing of the final version for publication; K.R. and E.D. were responsible for funding acquisition and project administration; J.D. performed the literature search and drafted sections of the manuscript; K.R., E.D. and Ľ.A. provided critical revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Louis Pasteur University Hospital, Košice, Slovakia, 2019/EK/2014.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

IMAGES
VIDEO
COMMENTS
Adolescents have special sexual and reproductive health needs that remain unmet, mainly due to lack of knowledge, social stigma, laws and policies preventing provision of contraception and abortion to unmarried (or any) adolescents, and judgmental attitudes among service providers . To maintain sexual and reproductive health, adolescents need ...
Miracle Adesina. Reproductive health is a relatively new concept which recognizes that especially a young girl has special reproductive health needs before, during and beyond the child bearing age ...
reproductive health information and services to enable them to deal in a "positive and responsible way" with their sexuality. The evidence base for what adolescents know about their sexual and reproductive health—together with evidence on the sexual and reproductive attitudes and behaviours of boys and girls living in diverse
Improving the sexual and reproductive health (SRH) of adolescent girls is one of the primary aims of the Sustainable Development Goals (SDGs). Adequate and accurate knowledge, a favorable attitude, safe behavior, and regular practice contribute to adolescent girls' SRH, maternal health, and child health.
In this thesis, I investigate policies and programs to improve reproductive health. My thesis makes a substantive contribution to reproductive health policy and a methodological contribution to quasi-experimental research. In chapter 1, I evaluate the impact of a mobile phone intervention for adolescent girls. I design
adolescents in their reproductive health matters, continuous data gathering on reproductive health indicators of adolescents, monitoring and evaluation of adolescents services. All these have implications for immediate and future reproductive health of adolescents, and for bridging the reproductive health service gap across the lifespan.
African Journal of Reproductive Health June 2019; 23 (2):134 REVIEW ARTICLE Views of Service Providers and Adolescents on Use of Sexual and Reproductive Health Services by Adolescents: A Systematic Review DOI: 10.29063/ajrh2019/v23i2.13 ... Network digital library of Thesis and Dissertation, ZETOC (Global Research Publication), and JournalTOCs. ...
This study identified and compiled a literature review published in 2000-2018 that focused on adolescents (10-24 years), reported reproductive and sexual health outcomes (pregnancy, sexually ...
Abstract. In this thesis, I investigate policies and programs to improve reproductive health. My thesis makes a substantive contribution to reproductive health policy and a methodological contribution to quasi-experimental research. In chapter 1, I evaluate the impact of a mobile phone intervention for adolescent girls.
Master's Thesis Institute of Public Health and Clinical Nutrition Faculty of Health Sciences University of Eastern Finland, Kuopio February, 2016. ... developing special programs on population control and reproductive health of adolescents which was followed by development of National reproductive health strategy in 1998. (National
Reproductive health (RH) implies that people are able to have a responsible, satisfying, and safe sex life and that they have the capability to have children and the freedom to decide if, when and how often to do so [].From the above perspective, sexual and reproductive health are key factors in shaping AYA's physical and mental well-being, factors that are often overlooked in the context of ...
reproductive health (SRH) outcomes.1-5 The SSA region accounts for the highest burden of adolescent HIV globally, and adolescent girls, in particular, are disproportionately affected, Key questions What is already known? There is a large body of studies on adolescent sex-ual and reproductive health (ASRH) outcomes in sub-Saharan Africa (SSA).
Vulnerable adolescents are exposed to sexual and reproductive health harms. Ignoring the sexual and reproductive health of this group can have irreparable consequences. The present qualitative study aimed to explore the barriers to the access of vulnerable adolescent girls to sexual and reproductive health. In this study, sixteen 14-19-year-old adolescent girls and twenty-two key informants ...
Reproductive health of vulnerable adolescent girls is a top priority in global programs. Alcohol consumption, drug abuse, high risk sexual behaviors, sexually transmitted diseases, sexual assault, escape from home, unrestrained sex in the family, history of robbery, imprisonment and living in drug hangouts expose adolescents to different sorts of damage and injury.
Background In Ghana, adolescents constitute about a quarter of the total population. These adolescents make reproductive health decisions and choices based on their knowledge and the availability of such choices. These reproductive health decisions and choices can either negatively or positively affect their lives. This study therefore explored adolescents' reproductive health knowledge and ...
school of public health college of health sciences university of ghana utilization of reproductive health services among adolescents in ghana: analysis of the 2007 and 2017 ghana maternal health surveys by james tetteh-boawolor ehiawey (10316744) this dissertation is submitted to the university of ghana, legon in partial fulfillment of the
I NTRODUCTION. Adolescents constitute about 20% of the world population.1 An estimate done in a study puts the adolescent's population globally at 1.2 billion with 85% of them living in the developing countries.2 According to the World Health Organization, adolescence is the period of transition from childhood to adulthood and this begins with the onset of puberty.
Objectives The mothers-adolescent discussion regarding sexual and reproductive health (SHR) issues plays an important role in preventing negative outcome associated with sexual risk behaviors. The present study aimed to explore the relationship between mothers' competence and comfort in SHR discourse with adolescent girls and its related factors. Methods A cross-sectional study was ...
The primary goal of this report is to summarize what is known about adolescent sexual and reproductive health in Malawi and to identify knowledge and program gaps requiring further research and program action. ... The thesis concludes that the way facility-based YFRHS is implemented has limited impact on SRH promotion among unmarried ...
Lack of accurate information about reproductive health and sexuality, lack of access to health services including contraception, and vulnerability to sexual abuse put adolescents at the highest risk . With regard to sexuality and communication about sexual matters, perhaps now more than any other time in history, the issue of sexual health is ...
Various studies revealed that adolescent girls have limited knowledge pertaining to sexual and reproductive health (SRH). The current study assessed the effectiveness of SRH education among adolescent girls in urban areas of Odisha, India. The study design was a cluster randomized trial, where the clusters composed of eight Odia (regional language) medium government girls' high schools in ...
Teenage pregnancy is the pregnancy of 10- to 19-year-old girls [ 1 ]. Adolescents are further divided into early (10-14 years old), middle (15-17 years old), and late adolescents (over 17 years old) [ 2 ]. According to the World Health Organization, adolescent pregnancies are a global problem for both developed and developing countries.