December 20, 2022

The Biggest Health and Biology Breakthroughs of 2022
From reviving dead pig organs to measuring viruses in our poop, here are some of the most intriguing medical advances of the year
By Tanya Lewis

A healthcare worker administers COVID-19 booster shots at a vaccination clinic in April 2022 in San Rafael, California.
Justin Sullivan/Getty Images
It’s been a rough year, especially on the health beat. The COVID pandemic continued to bulldoze its way through the population, causing surges in cases and related deaths. Somewhat forgotten viruses such as mpox , flu and RSV reared their head unexpectedly. And the U.S. Supreme Court overturned a nearly 50-year-old right to reproductive freedom established by Roe v. Wade .
But it wasn’t all bad news in 2022. In fact, biology and medicine saw exciting advances across fields as diverse as epidemiology, human evolution and artificial intelligence. Here are some of the discoveries that gave us hope for humanity and the future of human health.
We Got Updated Versions of COVID Vaccines
On supporting science journalism.
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The development of COVID vaccines within a year of the discovery of SARS-CoV-2, the coronavirus that causes the disease, is undoubtedly one of the greatest medical achievements in recent memory. Two of the most effective vaccines, developed using mRNA technology, were proved to significantly protect against severe disease and death from SARS-CoV-2. But the virus continued to evolve, and newer variants began to find a way around human immune defenses. Fortunately, vaccine manufacturers developed new shots to target both the Omicron variant and the original strain. Early data suggest these “bivalent” vaccines effectively boost protection against the virus—all the more reason to make sure everyone in your family is up-to-date with their shots.
Discoveries in Human Evolution Won a Nobel Prize
This year’s Nobel Prize in Physiology or Medicine was awarded to Svante Pääbo for his discoveries involving the genetic relationships among our hominin ancestors. Pääbo, a Swedish geneticist and director of the Department of Evolutionary Genetics at the Max Planck Institute for Evolutionary Anthropology in Leipzig, Germany, pioneered methods for reconstructing ancient DNA. He and his colleagues sequenced the genome of Neandertals and discovered a new hominin species, Denisovans. The research led to the surprising revelation that early humans interbred with these now extinct species. These primeval trysts gave us traits that persist in some people today, including an ability to survive at high altitude and a vulnerability to infections such as COVID.
Scientists Revived Dead Pigs’ Organs
In a feat that sounds like something out of the pages of Mary Shelley’s Frankenstein , a team of scientists at Yale University developed a perfusion system that restored vitality to pigs’ organs after the animals had died. The system—known as OrganEx—pumped a mixture of blood and nutrient-rich fluid through each animal’s circulatory system. (The animals didn’t regain consciousness.) The technology holds the potential to keep more human organs alive longer for transplants.
Researchers Found Secrets in Our Poop
It sounds gross, but human waste contains a cornucopia of useful information for infectious disease scientists. Wastewater tracking systems enabled researchers to spot COVID cases and new SARS-CoV-2 variants in regions before they caused surges. By monitoring sewage, scientists also detected the virus that causes polio —a disease that has been declared eradicated in much of the world—in sewage systems in New York State and the U.K. This type of monitoring could also reveal spikes in opioid use or in levels of antibiotic-resistant microbes, scientists say.
We Learned That Indoor Air Quality Matters
Before the COVID pandemic, most of us probably didn’t give much thought to the air we breathe indoors. Over the past few years, though, it’s become clear that SARS-CoV-2 frequently spreads through airborne droplets, which can build up inside indoor spaces and make us sick. Fortunately, we can reduce that risk by ventilating buildings and filtering the air we breathe . And cleaner indoor air has other benefits: it reduces the risk of respiratory diseases in general, and it may even help us think more clearly.
AI Solved One of the Biggest Problems in Biology
One of the hardest problems for biologists is predicting the three-dimensional structure of proteins from their amino acid sequence. But earlier this year an AI program built by the Google-owned company DeepMind, called AlphaFold, solved the 3-D structures of about 200 million proteins . These structures are already enabling scientists to unlock mysteries in biology, and they could help lead to new pharmaceutical drugs and more sustainable crops.
Subscribe or renew today
Every print subscription comes with full digital access
Science News
These are the most popular science news stories of 2022.

Previously excavated bodies of two ritually sacrificed Inca children, including this girl still wearing a ceremonial headdress, have yielded chemical clues to a beverage that may have been used to calm them in the days or weeks before being killed. The discovery ranked among Science News ' most-read stories of 2022.
Johan Reinhard
Share this:
By Science News Staff
December 22, 2022 at 7:00 am
Science News drew over 13 million visitors to our website this year. Here’s a recap of the most-read news stories and long reads of 2022.
Top news stories
1. a special brew may have calmed inca children headed for sacrifice.
The mummified remains of two Inca children ritually sacrificed more than 500 years ago contain chemical clues to their final days and weeks. On the journey to the Peruvian mountain where they were sacrificed, the children may have chewed coca leaves and drunk a beverage with antidepressant-like ingredients to soothe their nerves ( SN: 6/4/22, p. 10 ).
2. A ‘mystery monkey’ in Borneo may be a rare hybrid. That has scientists worried
An unusual monkey first spotted six years ago appears to be a cross between a female silvered leaf monkey ( Trachypithecus cristatus ) and a male proboscis monkey ( Nasalis larvatus ). The possible cross-genera pairing has scientists worried because such matings are usually a sign that species are facing ecological pressures ( SN: 6/18/22, p. 11 ).
3. What experts told me to do after my positive COVID-19 at-home test
After Science News intern Anna Gibbs came down with COVID-19, she turned to health experts to figure out how to report her case to public health officials and how long she needed to isolate ( SN Online: 4/22/22 ).
4. All of the bases in DNA and RNA have now been found in meteorites
Here’s more evidence that life’s precursors could have come from space. All five of the nucleobases that store information in DNA and RNA have been discovered in meteorites. This year, scientists reported detecting cytosine and thymine in fallen space rocks , completing the list ( SN: 6/4/22, p. 7 ).
5. Humans may not be able to handle as much heat as scientists thought
For years, it was thought the human body can tolerate heat up to a “wet bulb” temperature — a measure combining humidity and air temperature — of 35° Celsius (95° Fahrenheit). But experiments hint that the threshold may be several degrees lower ( SN: 8/27/22, p. 6 ).
Science News joins TikTok
TikTok became one more way we tell stories, as we premiered our first TikTok video — a tribute to the “bambootula” tarantula. Find out what makes this spider so peculiar and discover other amazing science tidbits @sciencenewsofficial .
@sciencenewsofficial This is the only known tarantula to call bamboo home. #spiders #tarantula #science #biology #sciencetok ♬ original sound – sciencenewsofficial
Top feature stories
1. tardigrades could teach us how to handle the rigors of space travel.
Tardigrades can withstand punishing levels of radiation, the freezing cold and the vacuum of outer space. Researchers are learning the death-defying tricks of these hardy microscopic animals to better prepare astronauts for long-term voyages ( SN: 7/16/22 & 7/30/22, p. 30 ).
2. Muons spill secrets about Earth’s hidden structures
Just like doctors use X-rays to see inside the human body, scientists are using muons , a type of subatomic particle, to peer inside Egyptian pyramids, volcanoes and other hard to penetrate structures ( SN: 4/23/22, p. 22 ).
3. Multiple sclerosis has a common viral culprit, opening doors to new approaches
Evidence is mounting that Epstein-Barr virus somehow instigates multiple sclerosis. Understanding the link between the virus and MS may lead to better treatments for the neurological disorder. Vaccines against the virus may even prevent MS altogether ( SN: 8/13/22, p. 14 ).
4. The discovery of the Kuiper Belt revamped our view of the solar system
In 1992, two astronomers discovered a doughnut-shaped region far beyond Neptune, dubbed the Kuiper Belt, that’s home to a swarm of frozen objects left over from the solar system’s formation. By studying these far-off objects over the last 30 years, scientists have gained new insights into how planets form ( SN: 8/27/22, p. 22 ).
5. Clovis hunters’ reputation as mammoth killers takes a hit
Ancient Americans may have been big-game scavengers rather than big-game hunters. Some recent analyses suggest that Clovis stone points were more likely tools for butchering large carcasses than weapons for taking down mammoths and other large animals ( SN: 1/15/22, p. 22 ).
Subscribers, enter your e-mail address for full access to the Science News archives and digital editions.
Not a subscriber? Become one now .
Frontiers | Science News
- Science News
Featured news
10 frontiers articles that caught the world’s attention in 2022.
By Frontiers’ science writers

Image: Shutterstock.com
As part of Frontiers’ passion to make science available to all, we highlight just a small selection of the most fascinating research published with us each month to help inspire current and future researchers to achieve their research dreams.
2022 was no different, and saw many game-changing discoveries contribute to the world’s breadth of knowledge on topics ranging from the climate crisis to robotics, and exercise to the lives of our ancestors.
So to round of the year, here are 10 Frontiers articles from this year that got the world’s top media talking.
1. This illusion, new to science, is strong enough to trick our reflexes
Have a look at the image below. Do you perceive that the central black hole is expanding, as if you’re moving into a dark environment, or falling into a hole? If so, you’re not alone: a study published to Frontiers in Human Neuroscience showed that this ‘expanding hole’ illusion, which is new to science, is perceived by approximately 86% of people.
The researchers don’t yet know why a minority seem unsusceptible to the ‘expanding hole’ illusion. Nor do they know whether other vertebrate species, or even nonvertebrate animals with camera eyes such as octopuses, might perceive the same illusion as we do.
“Our results show that pupils’ dilation or contraction reflex is not a closed-loop mechanism, like a photocell opening a door, impervious to any other information than the actual amount of light stimulating the photoreceptor,” said Dr Bruno Laeng, a professor at the Department of Psychology of the University of Oslo and the study’s first author.
“Rather, the eye adjusts to perceived and even imagined light, not simply to physical energy. Future studies could reveal other types of physiological or bodily changes that can ‘throw light’ onto how illusions work.”
Read article: https://www.frontiersin.org/articles/10.3389/fnhum.2022.877249/full
2. A replay of life: What happens in our brain when we die?
Imagine reliving your entire life in the space of seconds. Like a flash of lightning, you are outside of your body, watching memorable moments you lived through. This process, known as ‘life recall’, can be similar to what it’s like to have a near-death experience. What happens inside your brain during these experiences and after death are questions that have puzzled neuroscientists for centuries. However, a study published to Frontiers in Aging Neuroscience suggested that your brain may remain active and coordinated during and even after the transition to death, and be programmed to orchestrate the whole ordeal.
When an 87-year-old patient developed epilepsy, Dr Raul Vicente of the University of Tartu, Estonia and colleagues used continuous electroencephalography (EEG) to detect the seizures and treat the patient. During these recordings, the patient had a heart attack and passed away. This unexpected event allowed the scientists to record the activity of a dying human brain for the first time ever.
Read article: https://www.frontiersin.org/articles/10.3389/fnagi.2022.813531/full
3. Eating vegetables does not protect against cardiovascular disease, finds large-scale study
A sufficient intake of vegetables is important for maintaining a balanced diet and avoiding a wide range of diseases. But might a diet rich in vegetables also lower the risk of cardiovascular disease (CVD)? Unfortunately, researchers from the Nuffield Department of Population Health at the University of Oxford, the Chinese University of Hong Kong, and the University of Bristol found earlier this year no evidence for this.
That the consumption of vegetables might lower the risk of CVD might at first sight seem plausible, as their ingredients such as carotenoids and alpha-tocopherol have properties that could protect against CVD. But so far, the evidence from previous studies for an overall effect of vegetable consumption on CVD has been inconsistent.
Results from a powerful, large-scale new study in Frontiers in Nutrition showed that a higher consumption of cooked or uncooked vegetables is unlikely to affect the risk of CVD. They also explain how confounding factors might explain previous spurious, positive findings.
Read article: https://www.frontiersin.org/articles/10.3389/fnut.2022.831470/full
4. Having good friendships may make for a healthier gut microbiome
Social connections are essential for good health and wellbeing in social animals, such as ourselves and other primates. There is also increasing evidence that the gut microbiome – through the so-called ‘gut-brain axis’ – plays a key role in our physical and mental health and that bacteria can be transmitted socially, for example through touch. So how does social connectedness translate into the composition and diversity of the gut microbiome? That’s the topic of a study in Frontiers in Microbiology on rhesus macaques, Macaca mulatta.
The scientists focused on a single social group (with 22 males and 16 females between the ages of six and 20 years) of rhesus macaques on the island of Cayo Santiago, off the eastern coast of Puerto Rico. Macaques originally only lived in North Africa and Asia. But in 1938, a founder population of 409 rhesus macaques was moved from India to Cayo Santiago. Today, more than 1,000 macaques live on the 15.2 hectare island, divided into several social groups. They range and forage freely, although their diet gets supplemented daily with monkey chow. Researchers do behavioral observations on the monkeys each year.
Lead author Dr Katerina Johnson, a research associate at the Department of Experimental Psychology and the Department of Psychiatry of the University of Oxford, said: “Here we show that more sociable monkeys have a higher abundance of beneficial gut bacteria, and a lower abundance of potentially disease-causing bacteria.”
Read article: https://www.frontiersin.org/articles/10.3389/fmicb.2022.1032495/full
5. Robotic arms connected directly to brain of partially paralyzed man allows him to feed himself
Two robotic arms – a fork in one hand, a knife in the other – flank a seated man, who sits in front of a table, with a piece of cake on a plate. A computerized voice announces each action: “moving fork to food” and “retracting knife.” Partially paralyzed, the man makes subtle motions with his right and left fists at certain prompts, such as “select cut location”, so that the machine slices off a bite-sized piece. Now: “moving food to mouth” and another subtle gesture to align the fork with his mouth.
In less than 90 seconds, a person with very limited upper body mobility who hasn’t been able to use his fingers in about 30 years, just fed himself dessert using his mind and some smart robotic hands.
A team led by researchers at the Johns Hopkins Applied Physics Laboratory (APL), in Laurel, Maryland, and the Department of Physical Medicine and Rehabilitation (PMR) in the Johns Hopkins School of Medicine, published a paper in Frontiers in Neurorobotics that described this latest feat using a brain-machine interface (BMI) and a pair of modular prosthetic limbs.
Read article: https://www.frontiersin.org/articles/10.3389/fnbot.2022.918001/full
6. Excessive blue light from our gadgets may accelerate the aging process
Too much screen use has been linked to obesity and psychological problems. Now a study has identified a new problem – a study in fruit flies suggests our basic cellular functions could be impacted by the blue light emitted by these devices. These results are published in Frontiers in Aging .
“Excessive exposure to blue light from everyday devices, such as TVs, laptops and phones, may have detrimental effects on a wide range of cells in our body, from skin and fat cells, to sensory neurons,“ said Dr Jadwiga Giebultowicz, a professor at the Department of Integrative Biology at Oregon State University and senior author of this study. “We are the first to show that the levels of specific metabolites – chemicals that are essential for cells to function correctly – are altered in fruit flies exposed to blue light.“
“Our study suggests that avoidance of excessive blue light exposure may be a good anti-aging strategy,“ said Giebultowicz.
The researchers at Oregon State University have previously shown that fruit flies exposed to light ‘turn on‘ stress protective genes, and that those kept in constant darkness lived longer.
“To understand why high-energy blue light is responsible for accelerating aging in flies, we compared the levels of metabolites in flies exposed to blue light for two weeks to those kept in complete darkness,“ explained Giebultowicz. Blue light exposure caused significant differences in the levels of metabolites measured by the researchers in the cells of fly heads. In particular, they found that the levels of the metabolite succinate were increased, but glutamate levels were lowered.
Read article : https://www.frontiersin.org/articles/10.3389/fragi.2022.983373/full
7. Scientific ‘detective work’ reveals South American mummies were brutally murdered
How frequent was violence in prehistoric human societies? One way to measure this is to look for trauma in prehistoric human remains. For example, a recent review of pre-Columbian remains found evidence of trauma from violence in 21% of males. So far, most studies of this kind focused on skulls and other parts of the skeleton, but a potentially richer source of information are mummies, with their preserved soft tissues.
Now in a study in Frontiers in Medicine , researchers used 3D computed tomography (3D CT) to examine three mummies from pre-Columbian South America, conserved since the late 19th century in European museums.
“Here we show lethal trauma in two out of three South American mummies that we investigated with 3D CT. The types of trauma we found would not have been detectable if these human remains had been mere skeletons,” said Dr Andreas G Nerlich, a professor at the Department of Pathology of Munich Clinic Bogenhausen in Germany, the study’s corresponding author.
Nerlich and colleagues studied a male mummy at the ‘Museum Anatomicum’ of the Philipps University Marburg, Germany, as well as a female and a male mummy at the Art and History Museum of Delémont, Switzerland. Mummies can form naturally when dry environments, for example in deserts, soak up fluids from a decomposing body faster than the decay can proceed – conditions common in the southern zones of South America.
Read article : https://www.frontiersin.org/articles/10.3389/fmed.2022.962793/full
8. WWII shipwreck has leaked many pollutants into the sea, changing the ocean floor around it
Researchers have discovered that an 80 year old historic World War II shipwreck is still influencing the microbiology and geochemistry of the ocean floor where it rests. In Frontiers in Marine Science , they showed how the wreck is leaking hazardous pollutants, such as explosives and heavy metals, into the ocean floor sediment of the North Sea, influencing the marine microbiology around it.
The seabed of the North Sea is covered in thousands of ship and aircraft wrecks, warfare agents, and millions of tons of conventional munition such as shells and bombs. Wrecks contain hazardous substances (such as petroleum and explosives) that may harm the marine environment. Yet, there is a lack of information about the location of the wrecks, and the effect they might have on the environment.
“The general public is often quite interested in shipwrecks because of their historical value, but the potential environmental impact of these wrecks is often overlooked,” said PhD candidate Josefien Van Landuyt, of Ghent University. For example, it is estimated that World War I and II shipwrecks around the world collectively contain between 2.5m and 20.4m tons of petroleum products.
As part of the North Sea Wrecks project , Van Landuyt and her colleagues investigated how the World War II shipwreck V-1302 John Mahn in the Belgian part of the North Sea is impacting the microbiome and geochemistry in its surrounding seabed.
“We wanted to see if old shipwrecks in our part of the sea (Belgium) were still shaping the local microbial communities and if they were still affecting the surrounding sediment. This microbial analysis is unique within the project,” explained Van Landuyt.
Read article : https://www.frontiersin.org/articles/10.3389/fmars.2022.928576/full
9. Verbal insults trigger a ‘mini slap to the face’, finds new research
Humans are a highly social species. We rely on ever-changing cooperation dynamics and interpersonal relations to survive and thrive. Words have a big role to play in these relations, as they are tools used to understand interpersonal behavior. As such, words can hurt, but we know little about how the impact of words comes about as someone processes an insult.
“The exact way in which words can deliver their offensive, emotionally negative payload at the moment these words are being read or heard is not yet well-understood,” said corresponding author of a Frontiers in Communication study, Dr Marijn Struiksma, of Utrecht University.
Because insults pose a threat against our reputation and against our ‘self’, they provide a unique opportunity to research the interface between language and emotion. Struiksma continued:
“Understanding what an insulting expression does to people as it unfolds, and why, is of considerable importance to psycholinguists interested in how language moves people, but also to others who wish to understand the details of social behavior.”
Read article : https://www.frontiersin.org/articles/10.3389/fcomm.2022.910023/full
10. When should I schedule my exercise? The question is more important than you think
When should I fit exercise within my daily schedule? For most, the answer depends on our family’s schedule and working hours, and perhaps on whether we’re ‘larks’ or ‘night owls’. But over the past decade, researchers have found that much more hangs on this question than these constraints. That’s because recent findings suggest that the effectiveness of exercise depends on the time of day (Exercise Time Of Day, ETOD).
Now, a randomized controlled trial not only confirms convincingly that ETOD affects the effectiveness of exercise, but also shows that these effects differ between types of exercise, and between women and men. The results are published in Frontiers in Physiology .
Principal investigator Dr Paul J Arciero, a professor at the Health and Human Physiological Sciences Department of Skidmore College in Saratoga Springs, NY, US, said: “Here we show for the first time that for women, exercise during the morning reduces belly fat and blood pressure, whereas evening exercise in women increases upper body muscular strength, power, and endurance, and improves overall mood and nutritional satiety.”
“We also show that for men, evening exercise lowers blood pressure, the risk of heart disease, and feelings of fatigue, and burns more fat, compared to morning exercise.”
Read article : https://www.frontiersin.org/articles/10.3389/fphys.2022.893783/full
REPUBLISHING GUIDELINES : Open access and sharing research is part of Frontiers’ mission . Unless otherwise noted, you can republish articles posted in the Frontiers news blog — as long as you include a link back to the original research. Selling the articles is not allowed.
Post related info
December 06, 2022
Frontiers Science Communications
Post categories, related subjects, frontiers highlights, frontiers in aging, frontiers in aging neuroscience, frontiers in communication, frontiers in human neuroscience, frontiers in marine science, frontiers in medicine, frontiers in microbiology, frontiers in neurorobotics, frontiers in nutrition, frontiers in physiology, latest posts.

Frontiers ebook releases: May 2024

Clues to mysterious disappearance of North America’s large mammals 50,000 years ago found within ancient bone collagen

‘Extraordinary’ 4,000-year-old Egyptian skull may show signs of attempts to treat cancer

AI, open science, and the extreme weather pandemic: Takeaways from SXSW 2024
Big data, AI, and personalized medicine: scientists reveal playbook aiming to revolutionize healthcare
- Data, AI, & Machine Learning
- Managing Technology
- Social Responsibility
- Workplace, Teams, & Culture
- AI & Machine Learning
- Diversity & Inclusion
- Big ideas Research Projects
- Artificial Intelligence and Business Strategy
- Responsible AI
- Future of the Workforce
- Future of Leadership
- All Research Projects
- AI in Action
- Most Popular
- The Truth Behind the Nursing Crisis
- Work/23: The Big Shift
- Coaching for the Future-Forward Leader
- Measuring Culture

The spring 2024 issue’s special report looks at how to take advantage of market opportunities in the digital space, and provides advice on building culture and friendships at work; maximizing the benefits of LLMs, corporate venture capital initiatives, and innovation contests; and scaling automation and digital health platform.
- Past Issues
- Upcoming Events
- Video Archive
- Me, Myself, and AI
- Three Big Points

The 10 Most Popular Articles in 2022 (So Far)
Managers are seeking ways to improve employee well-being and build a strong workplace culture..

- Workplace, Teams, & Culture
- Talent Management
- Organizational Behavior

Year three of a global pandemic. A war in Ukraine. Inflation in the U.S. at a 40-year high. Small talk around the watercooler (mainly the virtual one, nowadays) certainly feels heavier than it used to.
Recent Gallup data indicates that in 2022, companies and managers remain challenged by the task of raising employee engagement to pre-pandemic levels. Nearly half of global workers (44%) surveyed reported feeling “a lot” of stress in the previous day. The Great Resignation has demonstrated the power of employees to vote with their feet, and a resurgence of the labor movement in the U.S. has put pressure on even top-tier companies to improve working conditions.
Get Updates on Transformative Leadership
Evidence-based resources that can help you lead your team more effectively, delivered to your inbox monthly.
Please enter a valid email address
Thank you for signing up
Privacy Policy
Companies that have thrived amid the pandemic and worker reshuffling have focused on worker well-being from the start. Unfortunately, for many employees across the globe, this may be the exception rather than the norm. As Gallup’s Jon Clifton put it, “Improving life at work isn’t rocket science, but the world is closer to colonizing Mars than it is to fixing the world’s broken workplaces.”
To begin to fix these issues, managers must focus on two areas in particular: leadership and culture. In the first months of the year, many MIT SMR readers turned their attention to articles focused on workplace culture, talent management, and employee retention.
With many companies now adopting permanent remote and hybrid work policies, other popular articles include data-driven approaches to managing well-being on virtual teams — from scheduling meeting-free days to creating systems for supporting mental health.
The following are the 10 most popular articles of the year so far. We hope they will continue to help managers who are looking to support employee engagement and build thriving workplaces.
#1 Toxic Culture Is Driving the Great Resignation
Donald sull, charles sull, and ben zweig.
In this article, the authors discuss the top five predictors of employee turnover uncovered by their analysis of attrition data during the Great Resignation and share four actions that managers can take in the short term to improve employee satisfaction.
#2 Top Performers Have a Superpower: Happiness
Paul b. lester, ed diener, and martin seligman.
Research has found that happiness, a sense of well-being, and an optimistic outlook are powerful predictors of how well an employee will perform. Managers who consciously promote employee well-being and take steps to eliminate toxic leadership in their business units will reap the benefits.
#3 The Surprising Impact of Meeting-Free Days
Ben laker, vijay pereira, pawan budhwar, and ashish malik.
Spending too much time in meetings can detract from effective collaboration, derail workers during their most productive hours, and interrupt people’s train of thought. No-meeting policies permit team members to excel without breaking their momentum, but specific plans must be tailored to each unique organizational context to maximize the benefits. The authors suggest several ways to deploy a no-meeting policy or adjust an existing one.
#4 Orchestrating Workforce Ecosystems
Elizabeth j. altman, david kiron, robin jones, and jeff schwartz.
Research conducted by MIT SMR and Deloitte examines the challenges companies and managers face in leading and coordinating workforces that increasingly rely on external contributors.
#5 Why Every Leader Needs to Worry About Toxic Culture
Donald sull, charles sull, william cipolli, and caio brighenti.
According to research, the five most common elements of toxic workplace cultures — being disrespectful, noninclusive, unethical, cutthroat, and abusive — contribute the most to employee attrition and can damage company reputation. Being aware of these elements and understanding how they spread can help employers prevent and address them.
#6 Building the Cognitive Budget for Your Most Effective Mind
Jordan birnbaum.
There’s a limit to how much mental energy is available to us on any given day, so it’s essential that we spend it deliberately and thoughtfully. This article details the process of creating a cognitive budget, using techniques from positive psychology, cognitive behavioral therapy, and behavioral economics.
#7 Stop Telling Employees to Be Resilient
Liz fosslien and mollie west duffy.
When it comes to leadership, there’s a difference between demanding that employees be mentally tough and actually helping them take care of their mental health. The authors suggest five actions leaders can take to create a workplace that supports employees and fosters resilience.
#8 Effective Leaders Decide About Deciding
Nancy duarte.
Categorizing decisions by riskiness and urgency helps clarify when employees should move autonomously and when they should pull leaders into decision-making.
Related Articles
#9 leading change means changing how you lead, b. tom hunsaker and jonathan knowles.
Adapting your leadership approach is necessary for achieving the change your organization requires. The authors discuss three tasks — drawing the map, establishing the mindset, and communicating the message — that are essential to becoming a contextually effective leader.
#10 How Well-Designed Work Makes Us Smarter
Sharon k. parker and gwenith g. fisher.
Work that permits autonomy and demands problem-solving can bolster employees’ cognitive skills and ongoing learning. This article looks at how organizations and managers can use good work design to strengthen their workforce’s ability to adapt to new processes, tools, and roles.
About the Author
Ally MacDonald ( @allymacdonald ) is senior editor at MIT Sloan Management Review .
More Like This
Add a comment cancel reply.
You must sign in to post a comment. First time here? Sign up for a free account : Comment on articles and get access to many more articles.
Comment (1)
Peter bheda.
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
MIT’s top research stories of 2022
Press contact :, media download, *terms of use:.
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."
Previous image Next image
The dizzying pace of research and innovation at MIT can make it hard to keep up. To mark the end of the year, MIT News is looking back at 10 of the research stories that generated the most excitement in 2022.
We’ve also rounded up the year’s top MIT community-related stories .
- Designing a heat engine with no moving parts . In April, engineers at MIT and the National Renewable Energy Laboratory (NREL) designed a heat engine that might someday enable a fully decarbonized power grid. In demonstrations, the engine was able to convert heat to electricity with over 40 percent efficiency — a performance better than that of traditional steam turbines.
- Creating a lightweight material stronger than steel . In February, MIT chemical engineers used a new polymerization process to form a material that that is stronger than steel and as light as plastic, and can be easily manufactured in large quantities. The material could be used as a coating for car parts or as a building material for bridges and other structures.
- Enabling portable desalination at the push of a button . MIT researchers developed a suitcase-sized device that can remove particles and salts to generate drinking water. Unlike other desalination units that rely on filters, this device uses electrical power to purify the water. It requires less power to operate than a cell phone charger and can be driven by a small solar panel. Just push start.
- Linking human genes to function . A team of researchers created the first map tying every gene expressed in human cells to its job in the cell. The map, which is available for other scientists to use, makes it easier to study a range of biological questions. The map was created using a CRISPR-based single-cell sequencing method known as Perturb-seq.
- Improving supercomputing with a new programming language . A team of researchers based mainly at MIT invented a faster and more reliable programming language for high-performance computing. The language, which was tested on a number of small programs, could one day help computers with a number of deep learning tasks like image processing.
- Lifting people out of extreme poverty . A study co-authored by an MIT economist showed that a one-time capital boost (in this case, a cow) helped poor people in rural Bangladesh improve their lives in the long run. The study suggests the very poor are in a poverty trap, in which an initial lack of resources prevents them from improving their circumstances, and implies that large asset transfers are an effective way to reduce global poverty.
- Helping robots fly . Inspired by fireflies, MIT researchers created tiny actuators that emit light to allow insect-scale robots to communicate. Weighing barely more than a paper clip, the robots are too small to make use of traditional means of sensing and communication. Instead, the actuators that control the robots’ wings light up in different colors and patterns, which could enable them to do things like share their location and call for help.
- Detecting a radio signal in a far-off galaxy . In July, astronomers at MIT and elsewhere were surprised to find a periodic fast radio burst (FRB) originating billions of light-years from Earth. It is the longest lasting FRB pattern detected to date and is made up of intensely strong radio waves that repeat every 0.2 seconds, similar to a heartbeat. Astronomers suspect the signal is coming from a neutron star.
- Proposal for a new, low-cost battery design . Researchers at MIT developed a battery made from abundant, inexpensive materials to complement the rise of lithium-ion batteries. The new battery uses aluminum and sulfur as its two electrode materials and a molten salt electrolyte in between. It could be ideal for powering single homes or small to medium sized businesses, producing a few tens of kilowatt-hours of storage capacity.
- Immigrants as job creators . A study co-authored by an MIT economist found that compared to native-born citizens, immigrants are about 80 percent more likely to found a firm. The study, which looked at registered businesses of all types across the country, suggests that immigrants act more as "job creators" than "job takers" and play outsized roles in high-growth entrepreneurship in the U.S.
Share this news article on:
Related topics.
- MIT Sloan School of Management
- School of Architecture and Planning
- School of Humanities Arts and Social Sciences
Related Articles

MIT community in 2022: A year in review

MIT’s top research stories of 2021

MIT community in 2021: A year in review
Previous item Next item
More MIT News

MIT Corporation elects 10 term members, two life members
Read full story →

Diane Hoskins ’79: How going off-track can lead new SA+P graduates to become integrators of ideas

Chancellor Melissa Nobles’ address to MIT’s undergraduate Class of 2024

Noubar Afeyan PhD ’87 gives new MIT graduates a special assignment

Commencement address by Noubar Afeyan PhD ’87

President Sally Kornbluth’s charge to the Class of 2024
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)
Melanie j. davies.
1 Leicester Diabetes Research Centre, University of Leicester, Leicester, UK
2 Leicester National Institute for Health Research (NIHR) Biomedical Research Centre, University Hospitals of Leicester NHS Trust, Leicester, UK
Vanita R. Aroda
3 Division of Endocrinology, Diabetes and Hypertension, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA USA
Billy S. Collins
4 National Heart, Lung, and Blood Institute, Bethesda, MD USA
Robert A. Gabbay
5 ADA, Arlington, VA USA
Jennifer Green
6 Duke Clinical Research Institute, Duke University School of Medicine, Durham, NC USA
Nisa M. Maruthur
7 Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD USA
Sylvia E. Rosas
8 Kidney and Hypertension Unit, Joslin Diabetes Center, Harvard Medical School, Boston, MA USA
Stefano Del Prato
9 Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Chantal Mathieu
10 Clinical and Experimental Endocrinology, KU Leuven, Leuven, Belgium
Geltrude Mingrone
11 Università Cattolica del Sacro Cuore, Rome, Italy
12 Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy
13 Division of Diabetes and Nutritional Sciences, School of Cardiovascular and Metabolic Medicine and Sciences, King’s College London, London, UK
Peter Rossing
14 Steno Diabetes Center Copenhagen, Herlev, Denmark
15 Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Tsvetalina Tankova
16 Department of Endocrinology, Medical University – Sofia, Sofia, Bulgaria
Apostolos Tsapas
17 Diabetes Centre, Clinical Research and Evidence-based Medicine Unit, Aristotle University Thessaloniki, Thessaloniki, Greece
18 Harris Manchester College, University of Oxford, Oxford, UK
John B. Buse
19 University of North Carolina School of Medicine, Chapel Hill, NC USA
Associated Data
Details of the search strategy and list of identified articles can be found at https://data.mendeley.com/datasets/h5rcnxpk8w/2
The American Diabetes Association and the European Association for the Study of Diabetes convened a panel to update the previous consensus statements on the management of hyperglycaemia in type 2 diabetes in adults, published since 2006 and last updated in 2019. The target audience is the full spectrum of the professional healthcare team providing diabetes care in the USA and Europe. A systematic examination of publications since 2018 informed new recommendations. These include additional focus on social determinants of health, the healthcare system and physical activity behaviours including sleep. There is a greater emphasis on weight management as part of the holistic approach to diabetes management. The results of cardiovascular and kidney outcomes trials involving sodium–glucose cotransporter-2 inhibitors and glucagon-like peptide-1 receptor agonists, including assessment of subgroups, inform broader recommendations for cardiorenal protection in people with diabetes at high risk of cardiorenal disease. After a summary listing of consensus recommendations, practical tips for implementation are provided.
Graphical abstract

Supplementary Information
The online version of this article (10.1007/s00125-022-05787-2) contains peer-reviewed but unedited supplementary material.
Introduction
Type 2 diabetes is a chronic complex disease and management requires multifactorial behavioural and pharmacological treatments to prevent or delay complications and maintain quality of life (Fig. (Fig.1). 1 ). This includes management of blood glucose levels, weight, cardiovascular risk factors, comorbidities and complications. This necessitates that care be delivered in an organised and structured way, such as described in the chronic care model, and includes a person-centred approach to enhance engagement in self-care activities [ 1 ]. Careful consideration of social determinants of health and the preferences of people living with diabetes must inform individualisation of treatment goals and strategies [ 2 ].

Decision cycle for person-centred glycaemic management in type 2 diabetes. Adapted from [5] with permission from Springer Nature, © European Association for the Study of Diabetes and American Diabetes Association, 2018
This consensus report addresses the approaches to management of blood glucose levels in non-pregnant adults with type 2 diabetes. The principles and approach for achieving this are summarised in Fig. Fig.1. 1 . These recommendations are not generally applicable to individuals with diabetes due to other causes, for example monogenic diabetes, secondary diabetes and type 1 diabetes, or to children.
Data sources, searches and study selection
The writing group members were appointed by the ADA and EASD. The group largely worked virtually with regular teleconferences from September 2021, a 3 day workshop in January 2022 and a face-to-face 2 day meeting in April 2022. The writing group accepted the 2012 [ 3 ], 2015 [ 4 ], 2018 [ 5 ] and 2019 [ 6 ] editions of this consensus report as a starting point. To identify newer evidence, a search was conducted on PubMed for RCTs, systematic reviews and meta-analyses published in English between 28 January 2018 and 13 June 2022; eligible publications examined the effectiveness or safety of pharmacological or non-pharmacological interventions in adults with type 2 diabetes. Reference lists in eligible reports were scanned to identify additional relevant articles. Details of the keywords and the search strategy are available at https://data.mendeley.com/datasets/h5rcnxpk8w/2 . Papers were grouped according to subject and the authors reviewed this new evidence. Up-to-date meta-analyses evaluating the effects of therapeutic interventions across clinically important subgroup populations were assessed in terms of their credibility using relevant guidance [ 7 , 8 ]. Evidence appraisal was informed by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines on the formulation of clinical practice recommendations [ 9 , 10 ]. The draft consensus recommendations were evaluated by invited reviewers and presented for public comment. Suggestions were incorporated as deemed appropriate by the authors (see Acknowledgements). Nevertheless, although evidence based with stakeholder input, the recommendations presented herein reflect the values and preferences of the consensus group.
The rationale, importance and context of glucose-lowering treatment
Fundamental aspects of diabetes care include promoting healthy behaviours, through medical nutrition therapy (MNT), physical activity and psychological support, as well as weight management and tobacco/substance abuse counselling as needed. This is often delivered in the context of diabetes self-management education and support (DSMES). The expanding number of glucose-lowering interventions—from behavioural interventions to pharmacological interventions, devices and surgery—and growing information about their benefits and risks provide more options for people with diabetes and providers but complicate decision making. The demonstrated benefits for high-risk individuals with atherosclerotic CVD, heart failure (HF) or chronic kidney disease (CKD) afforded by the glucagon-like peptide-1 receptor agonists (GLP-1 RA) and sodium–glucose cotransporter-2 inhibitors (SGLT2i) provide important progress in treatment aimed at reducing the progression and burden of diabetes and its complications. These benefits are largely independent of their glucose-lowering effects. These treatments were initially introduced as glucose-lowering agents but are now also prescribed for organ protection. In this consensus report, we summarise a large body of recent evidence for practitioners in the USA and Europe with the aim of simplifying clinical decision making and focusing our efforts on providing holistic person-centred care.
Attaining recommended glycaemic targets yields substantial and enduring reductions in the onset and progression of microvascular complications [ 11 , 12 ] and early intervention is essential [ 13 ]. The greatest absolute risk reduction comes from improving very elevated glycaemic levels, and a more modest reduction results from near normalisation of plasma glucose levels [ 2 , 14 ]. The impact of glucose control on macrovascular complications is less certain but is supported by multiple meta-analyses and epidemiological studies. Because the benefits of intensive glucose control emerge slowly while the harms can be immediate, people with longer life expectancy have more to gain from early intensive glycaemic management. A reasonable HbA 1c target for most non-pregnant adults with sufficient life expectancy to see microvascular benefits (generally ∼10 years) is around 53 mmol/mol (7%) or less [ 2 ]. Aiming for a lower HbA 1c level than this may have value if it can be achieved safely without significant hypoglycaemia or other adverse treatment effects. A lower target may be reasonable, particularly when using pharmacological agents that are not associated with hypoglycaemic risk. Higher targets can be appropriate in cases of limited life expectancy, advanced complications or poor tolerability or if other factors such as frailty are present. Thus, glycaemic treatment targets should be tailored based on an individual’s preferences and characteristics, including younger age (i.e. age <40 years), risk of complications, frailty and comorbid conditions [ 2 , 15 – 17 ], and the impact of these features on the risk of adverse effects of therapy (e.g. hypoglycaemia and weight gain).
Principles of care
Language matters.
Communication between people living with type 2 diabetes and healthcare team members is at the core of integrated care, and clinicians must recognise how language matters. Language in diabetes care should be neutral, free of stigma and based on facts; be strengths-based (focus on what is working), respectful and inclusive; encourage collaboration; and be person-centred [ 18 ]. People living with diabetes should not be referred to as ‘diabetics’ or described as ‘non-compliant’ or blamed for their health condition.
Diabetes self-management education and support
DSMES is a key intervention, as important to the treatment plan as the selection of pharmacotherapy [ 19 – 21 ]. DSMES is central to establishing and implementing the principles of care (Fig. (Fig.1). 1 ). DSMES programmes usually involve face-to-face contact in group or individual sessions with trained educators, and key components of DSMES are shown in Supplementary Table 1 [ 19 – 24 ]. Given the ever-changing nature of type 2 diabetes, DSMES should be offered on an ongoing basis. Critical junctures when DSMES should be provided include at diagnosis, annually, when complications arise, and during transitions in life and care (Supplementary Table 1 ) [ 22 ].
High-quality evidence has consistently shown that DSMES significantly improves knowledge, glycaemic levels and clinical and psychological outcomes, reduces hospital admissions and all-cause mortality and is cost-effective [ 22 , 25 – 30 ]. DSMES is delivered through structured educational programmes provided by trained diabetes care and education specialists (termed DCES in the USA; hereafter referred to as ‘diabetes educators’) that focus particularly on the following: lifestyle behaviours (healthy eating, physical activity and weight management), medication-taking behaviour, self-monitoring when needed, self-efficacy, coping and problem solving.
Importantly, DSMES is tailored to the individual’s context, which includes their beliefs and preferences. DSMES can be provided using multiple approaches and in a variety of settings [ 20 , 31 ] and it is important for the care team to know how to access local DSMES resources. DSMES supports the psychosocial care of people with diabetes but is not a replacement for referral for mental health services when they are warranted, for example when diabetes distress remains after DSMES. Psychiatric disorders, including disordered eating behaviours, are common, often unrecognised and contribute to poor outcomes in diabetes [ 32 ].
The best outcomes from DSMES are achieved through programmes with a theory-based and structured curriculum and with contact time of over 10 h [ 26 ]. While online programmes may reinforce learning, a comprehensive approach to education using multiple methods may be more effective [ 26 ]. Emerging evidence demonstrates the benefits of telehealth or web-based DSMES programmes [ 33 ] and these were used with success during the COVID-19 pandemic [ 34 – 36 ]. Technologies such as mobile apps, simulation tools, digital coaching and digital self-management interventions can be used to deliver DSMES and extend its reach to a broader segment of the population with diabetes and provide comparable or even better outcomes [ 37 ]. Greater HbA 1c reductions are demonstrated with increased engagement of people with diabetes [ 35 , 38 ]. However, data from trials of digital strategies to support behaviour change are still preliminary in nature and quite heterogeneous [ 22 , 37 ].
Individualised and personalised approach
Type 2 diabetes is a very heterogeneous disease with variable age at onset, related degree of obesity, insulin resistance and tendency to develop complications [ 39 , 40 ]. Providing person-centred care that addresses multimorbidity and is respectful of and responsive to individual preferences and barriers, including the differential costs of therapies, is essential for effective diabetes management [ 41 ]. Shared decision making, facilitated by decision aids that show the absolute benefit and risk of alternative treatment options, is a useful strategy to determine the best treatment course for an individual [ 42 – 45 ]. With compelling indications for therapies such as SGLT2i and GLP-1 RA for high-risk individuals with CVD, HF or CKD, shared decision making is essential to contextualise the evidence on benefits, safety and risks. Providers should evaluate the impact of any suggested intervention in the context of cognitive impairment, limited literacy, distinct cultural beliefs and individual fears or health concerns. The healthcare system is an important factor in the implementation, evaluation and development of the personalised approach. Furthermore, social determinants of health—often out of direct control of the individual and potentially representing lifelong risk—contribute to medical and psychosocial outcomes and must be addressed to improve health outcomes. Five social determinants of health areas have been identified: socioeconomic status (education, income and occupation), living and working conditions, multisector domains (e.g. housing, education and criminal justice system), sociocultural context (e.g. shared cultural values, practices and experiences) and sociopolitical context (e.g. societal and political norms that are root cause ideologies and policies underlying health disparities) [ 46 ]. More granularity on social determinants of health as they pertain to diabetes is provided in a recent ADA review [ 47 ], with a particular focus on the issues faced in the African American population provided in a subsequent report [ 48 ]. Environmental, social, behavioural and emotional factors, known as psychosocial factors, also influence living with diabetes and achieving satisfactory medical outcomes and psychological well-being. Thus, these multifaceted domains (heterogeneity across individual characteristics, social determinants of health and psychosocial factors) challenge individuals with diabetes, their families and their providers when attempting to integrate diabetes care into daily life [ 49 ].
Current principles of, and approaches to, person-centred care in diabetes (Fig. (Fig.1) 1 ) include assessing key characteristics and preferences to determine individualised treatment goals and strategies. Such characteristics include comorbidities, clinical characteristics and compelling indications for GLP-1 RA or SGLT2i for organ protection [ 6 ].
Weight reduction as a targeted intervention
Weight reduction has mostly been seen as a strategy to improve HbA 1c and reduce the risk for weight-related complications. However, it was recently suggested that weight loss of 5–15% should be a primary target of management for many people living with type 2 diabetes [ 50 ]. A higher magnitude of weight loss confers better outcomes. Weight loss of 5–10% confers metabolic improvement; weight loss of 10–15% or more can have a disease-modifying effect and lead to remission of diabetes [ 50 ], defined as normal blood glucose levels for 3 months or more in the absence of pharmacological therapy in a 2021 consensus report [ 51 ]. Weight loss may exert benefits that extend beyond glycaemic management to improve risk factors for cardiometabolic disease and quality of life [ 50 ].
Glucose management: monitoring
Glycaemic management is primarily assessed with the HbA 1c test, which was the measure used in trials demonstrating the benefits of glucose lowering [ 2 , 52 ]. As with any laboratory test, HbA 1c measurement has limitations [ 2 , 52 ]. There may be discrepancies between HbA 1c results and an individual’s true mean blood glucose levels, particularly in certain racial and ethnic groups and in conditions that alter erythrocyte turnover, such as anaemia, end-stage kidney disease (especially with erythropoietin therapy) and pregnancy, or if an HbA 1c assay insensitive to haemoglobin variants is used in someone with a haemoglobinopathy. Discrepancies between measured HbA 1c levels and measured or reported glucose levels should prompt consideration that one of these may not be reliable [ 52 , 53 ].
Regular blood glucose monitoring (BGM) may help with self-management and medication adjustment, particularly in individuals taking insulin. BGM plans should be individualised. People with type 2 diabetes and the healthcare team should use the monitoring data in an effective and timely manner. In people with type 2 diabetes not using insulin, routine glucose monitoring is of limited additional clinical benefit while adding burden and cost [ 54 , 55 ]. However, for some individuals, glucose monitoring can provide insight into the impact of lifestyle and medication management on blood glucose and symptoms, particularly when combined with education and support [ 53 ]. Technologies such as intermittently scanned or real-time continuous glucose monitoring (CGM) provide more information and may be useful for people with type 2 diabetes, particularly in those treated with insulin [ 53 , 56 ].
When using CGM, standardised, single-page glucose reports, such as the ambulatory glucose profile, can be uploaded from CGM devices. They should be considered as standard metrics for all CGM devices and provide visual cues for management opportunities. Time in range is defined as the percentage of time that CGM readings are in the range 3.9–10.0 mmol/l (70–180 mg/dl). Time in range is associated with the risk of microvascular complications and can be used for assessment of glycaemic management [ 57 ]. Additionally, time above and below range are useful variables for the evaluation of treatment regimens. Particular attention to minimising the time below range in those with hypoglycaemia unawareness may convey benefit. If using the ambulatory glucose profile to assess glycaemic management, a goal parallel to an HbA 1c level of <53 mmol/mol (<7%) for many is time in range of >70%, with additional recommendations to aim for time below range of <4% and time at <3.0 mmol/l (<54 mg/dl) of <1% [ 2 ].
Treatment behaviours, persistence and adherence
Suboptimal medication-taking behaviour and low rates of continued medication use, or what is termed ‘persistence to therapy plans’ affects almost half of people with type 2 diabetes, leading to suboptimal glycaemic and CVD risk factor control as well as increased risks of diabetes complications, mortality and hospital admissions and increased healthcare costs [ 58 – 62 ]. Although this consensus report focuses on medication-taking behaviour, the principles are pertinent to all aspects of diabetes care. Multiple factors contribute to inconsistent medication use and treatment discontinuation among people with diabetes, including perceived lack of medication efficacy, fear of hypoglycaemia, lack of access to medication and adverse effects of medication [ 63 ]. Focusing on facilitators of adherence, such as social/family/provider support, motivation, education and access to medications/foods, can provide benefits [ 64 ]. Observed rates of medication adherence and persistence vary across medication classes and between agents; careful consideration of these differences may help improve outcomes [ 61 ]. Ultimately, individual preferences are major factors driving the choice of medications. Even when clinical characteristics suggest the use of a particular medication based on the available evidence from clinical trials, preferences regarding route of administration, injection devices, side effects or cost may prevent use by some individuals [ 65 ].
Therapeutic inertia
Therapeutic (or clinical) inertia describes a lack of treatment intensification when targets or goals are not met. It also includes failure to de-intensify management when people are overtreated. The causes of therapeutic inertia are multifactorial, occurring at the levels of the practitioner, person with diabetes and/or healthcare system [ 66 ]. Interventions targeting therapeutic inertia have facilitated improvements in glycaemic management and timely insulin intensification [ 67 , 68 ]. For example, the involvement of multidisciplinary teams that include non-physician providers with authorisation to prescribe (e.g. pharmacists, specialist nurses and advanced practice providers) may reduce therapeutic inertia [ 69 , 70 ].
Therapeutic options: lifestyle and healthy behaviour, weight management and pharmacotherapy for the treatment of type 2 diabetes
This section summarises the lifestyle and behavioural therapy, weight management interventions and pharmacotherapy that support glycaemic management in people with type 2 diabetes. Specific pharmacological treatment options are summarised in Table Table1. 1 . Additional details are available in the previous ADA/EASD consensus report and update [ 5 , 6 ] and the ADA’s 2022 Standards of medical care in diabetes [ 71 ].
Medications for lowering glucose, summary of characteristics

Nutrition therapy
Nutrition therapy is integral to diabetes management, with goals of promoting and supporting healthy eating patterns, addressing individual nutrition needs, maintaining the pleasure of eating and providing the person with diabetes with the tools for developing healthy eating [ 22 ]. MNT provided by a registered dietitian/registered dietitian nutritionist complements DSMES, can significantly reduce HbA 1c and can help prevent, delay and treat comorbidities related to diabetes [ 19 ]. Two core dimensions of MNT that can improve glycaemic management include dietary quality and energy restriction.
Dietary quality and eating patterns
There is no single ratio of carbohydrate, proteins and fat intake that is optimal for every person with type 2 diabetes. Instead, individually selected eating patterns that emphasise foods with demonstrated health benefits, minimise foods shown to be harmful and accommodate individual preferences with the goal of identifying healthy dietary habits that are feasible and sustainable are recommended. A net energy deficit that can be maintained is important for weight loss [ 5 , 6 , 22 , 72 – 74 ].
A network analysis comparing trials of nine dietary approaches of >12 weeks’ duration demonstrated reductions in HbA 1c from −9 to −5.1 mmol/mol (−0.82% to −0.47%), with all approaches compared with a control diet. Greater glycaemic benefits were seen with the Mediterranean diet and low carbohydrate diet [ 75 ]. The greater glycaemic benefits of low carbohydrate diets (<26% of energy) at 3 and 6 months are not evident with longer follow-up [ 72 ]. In a systematic review of trials of >6 months’ duration, compared with a low-fat diet, the Mediterranean diet demonstrated greater reductions in body weight and HbA 1c levels, delayed the requirement for diabetes medication and provided benefits for cardiovascular health [ 76 , 77 ]. Similar benefits have been ascribed to vegan and vegetarian diets [ 78 ].
There has been increased interest in time-restricted eating and intermittent fasting to improve metabolic variables, although with mixed, and modest, results. In a meta-analysis there were no differences in the effect of intermittent fasting and continuous energy restriction on HbA 1c , with intermittent fasting having a modest effect on weight (−1.70 kg) [ 79 ]. In a 12 month RCT in adults with type 2 diabetes comparing intermittent energy restriction (2092–2510 kJ [500–600 kcal] diet for 2 non-consecutive days/week followed by the usual diet for 5 days/week) with continuous energy restriction (5021–6276 kJ [1200–1500 kcal] diet for 7 days/week), glycaemic improvements were comparable between the two groups. At 24 months’ follow-up, HbA 1c increased in both groups to above baseline [ 80 ], while weight loss (−3.9 kg) was maintained in both groups [ 81 ]. Fasting may increase the rates of hypoglycaemia in those treated with insulin and sulfonylureas, highlighting the need for individualised education and proactive medication management during significant dietary changes [ 82 ].
Non-surgical energy restriction for weight loss
An overall healthy eating plan that results in an energy deficit, in conjunction with medications and/or metabolic surgery as individually appropriate, should be considered to support glycaemic and weight management goals in adults with type 2 diabetes [ 5 , 22 ]. Structured nutrition and lifestyle programmes may be considered for glycaemic benefit and can be adapted for specific cultural indications [ 83 – 87 ].
The Diabetes Remission Clinical Trial (DiRECT) demonstrated greater remission of diabetes with a weight management programme than with usual best practice care in adults with type 2 diabetes within 6 years of diagnosis. The structured, primary care-led intensive weight management programme involved total diet replacement (3452–3569 kJ/day [825–853 kcal/day] for 3–5 months) followed by stepped food reintroduction and structured support for long-term weight loss maintenance. In the whole study population, remission directly varied with degree of weight loss [ 88 ]. At the 2 year follow-up, sustained remission correlated with extent of sustained weight loss. In the whole study population, of those maintaining at least 10 kg weight loss, 64% achieved diabetes remission. However, only 24% of the participants in the intervention group maintained at least 10 kg weight loss, highlighting both the potential and the challenges of long-term durability of weight loss [ 89 ].
The Look AHEAD: Action for Health in Diabetes (Look AHEAD) trial on the longer-term effects of an intensive lifestyle intervention in adults who were overweight/obese with type 2 diabetes showed improvements in diabetes control and complications, depression, physical function and health-related quality of life, sleep apnoea, incontinence, brain structure and healthcare use and costs, with positive impacts on composite indices of multimorbidity, geriatric syndromes and disability-free life-years. This should be balanced against potential negative effects on body composition, bone density and frailty fractures [ 90 , 91 ]. Although there was no difference in the primary cardiovascular outcome or mortality rate between the intervention and the control groups, post hoc exploratory analyses suggested potential benefits in certain groups (e.g. in those who achieved at least 10% weight loss in the first year of the study). Progressive metabolic benefits were seen with greater degrees of weight loss from >5% to ≥15%, with an overall suggestion that ≥10% weight loss may be required to see benefits for CVD events and mortality rate and other complications such as non-alcoholic steatohepatitis [ 50 , 90 , 92 – 95 ].
Physical activity behaviours including sleep
Physical activity behaviours significantly impact cardiometabolic health in type 2 diabetes (Fig. (Fig.2) 2 ) [ 96 – 117 ]. Regular aerobic exercise (i.e. involving large muscle groups and rhythmic in nature) improves glycaemic management in adults with type 2 diabetes, resulting in less daily time in hyperglycaemia and reductions of ~7 mmol/mol (~0.6%) in HbA 1c [ 118 ], and induces clinically significant benefits in cardiorespiratory fitness [ 101 , 110 , 119 ]. These glycaemic effects can be maximised by undertaking activity during the postprandial period and engaging in activities for ≥45 min [ 101 , 120 ]. Resistance exercise (i.e. using your own body weight or working against a resistance) also improves blood glucose levels, flexibility and balance [ 101 , 110 ]. This is important given the increased risk of impaired physical function at an earlier age in type 2 diabetes [ 112 ].

Importance of 24-hour physical behaviours for type 2 diabetes
A wide range of physical activities, including leisure time activities, can significantly reduce HbA 1c levels [ 5 , 22 , 121 , 122 ]. Even small, regular changes can make a difference to long-term health, with an increase of only 500 steps/day associated with 2–9% decreased risk of cardiovascular morbidity and all-cause mortality rates [ 105 – 107 ]. Beneficial effects are evident across the continuum of human movement, from breaking prolonged sitting with light activity [ 103 ] to high-intensity interval training [ 123 ].
Healthy sleep is considered a key lifestyle component in the management of type 2 diabetes [ 124 ], with clinical practice guidelines promoting the importance of sleep hygiene [ 113 ]. Sleep disorders are common in type 2 diabetes and cause disturbances in the quantity, quality and timing of sleep and are associated with an increased risk of obesity and impairments in daytime functioning and glucose metabolism [ 114 , 115 ]. Additionally, obstructive sleep apnoea affects over half of people with type 2 diabetes and its severity is associated with blood glucose levels [ 115 , 116 ].
The quantity of sleep is known to be associated (in a ‘U’ shaped manner) with health outcomes (e.g. obesity and HbA 1c ), with both long (>8 h) and short (<6 h) sleep durations having negative impacts [ 97 ]. By extending the sleep duration of short sleepers, it is possible to improve insulin sensitivity and reduce energy intake [ 117 , 125 ]. However, ’catch-up’ weekend sleep alone is not enough to reverse the impact of insufficient sleep [ 126 ].
Weight management beyond lifestyle interventions
Medications for weight loss in type 2 diabetes.
Weight loss medications are effective adjuncts to lifestyle interventions and healthy behaviours for management of weight and have also been found to improve glucose control in people with diabetes [ 127 ].
Newer therapies have demonstrated very high efficacy for weight management in people with type 2 diabetes. In the Semaglutide Treatment Effect in People with Obesity (STEP) 2 trial, subcutaneous semaglutide 2.4 mg once a week as an adjunct to a lifestyle intervention performed better than either semaglutide 1.0 mg or placebo, with weight loss of 9.6% (6.2% more than with placebo and 2.7% more than with semaglutide 1.0 mg). More than two thirds of participants in the semaglutide 2.4 mg arm achieved an HbA 1c level of ≤48 mmol/mol (≤6.5%) [ 128 ]. However, the weight loss was less pronounced than the 14.9% weight loss (vs 2.4% with placebo) seen in the STEP 1 trial in adults with overweight or obesity without diabetes [ 129 ]. Tirzepatide, a novel glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 RA, at weekly doses of 5 mg, 10 mg and 15 mg reduced body weight by 15%, 19.5% and 20.9%, respectively, compared with 3.1% with placebo at 72 weeks in people with obesity but without diabetes; however, tirzepatide has not yet been approved for weight management by regulatory authorities [ 130 ]. Studies in adults with overweight or obesity suggest that withdrawing treatment with semaglutide leads to increases in body weight [ 131 ], highlighting the chronic nature of, and need for, obesity/weight management.
Metabolic surgery
Metabolic surgery should be considered as a treatment option in adults with type 2 diabetes who are appropriate surgical candidates [ 127 , 132 ]. Metabolic surgery also appears to be effective for diabetes remission in people with type 2 diabetes and a BMI ≥25 kg/m 2 , although efficacy for both weight loss and diabetes remission appears to vary by surgical type [ 133 – 135 ]. One mixed-effects meta-analysis model has estimated a 43% diabetes remission rate (95% CI 34%, 53%) following metabolic surgery in people with type 2 diabetes and a BMI <30 kg/m 2 [ 136 ], significantly higher than that achieved with traditional medical management [ 137 ]. However, there is a strong association between duration of diabetes and the likelihood of postoperative diabetes remission. People with more recently diagnosed diabetes are more likely to experience remission after metabolic surgery, and the likelihood of remission decreases significantly with duration of diabetes longer than about 5–8 years [ 138 ]. Even in people with diabetes who do not achieve postoperative diabetes remission, or relapse after initial remission, metabolic surgery is associated with better metabolic control than medical management [ 137 , 139 ]. In the Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently (STAMPEDE) trial, metabolic surgery was also associated with improvements in patient-reported outcomes related to physical health; however, measures of social and psychological quality of life did not improve [ 140 ]. It is important to note that many of these estimates of benefit included data from non-randomised studies and compared outcomes with medical treatments for obesity that were less effective than those available today.
Medications for lowering glucose
Cardiorenal-protective glucose-lowering medications, sodium–glucose cotransporter-2 inhibitors.
The SGLT2i are oral medications that reduce plasma glucose by enhancing urinary excretion of glucose. They have intermediate-to-high glycaemic efficacy, with lower glycaemic efficacy at lower eGFR. However, their scope of use has significantly expanded based on cardiovascular and renal outcomes studies [ 5 , 141 ]. Cardiorenal outcomes trials have demonstrated their efficacy in reducing the risk of composite major adverse cardiovascular events (MACE), cardiovascular death, myocardial infarction, hospitalisation for heart failure (HHF) and all-cause mortality and improving renal outcomes in individuals with type 2 diabetes with an established/high risk of CVD. This is discussed in the section on ‘Personalised approach to treatment based on individual characteristics and comorbidities: recommended process for glucose-lowering medication selection’. Evidence supporting their use is summarised in Table Table1 1 [ 141 , 142 ].
Recent data have increased confidence in the safety of the SGLT2i drug class [ 141 , 142 ]. Their use is associated with increased risk for mycotic genital infections, which are reported to be typically mild and treatable. While SGLT2i use can increase the risk of diabetic ketoacidosis (DKA), the incidence is low, with a modest incremental absolute risk [ 142 ]. The SGLT2i cardiovascular outcomes trials (CVOTs) have reported DKA rates of 0.1–0.6% compared with rates of <0.1–0.3% with placebo [ 143 – 147 ], with very low rates in the HF [ 148 – 151 ] and CKD [ 152 , 153 ] outcomes studies. Risk can be mitigated with education and guidance, including education on signs and symptoms of DKA that should prompt medical attention, and temporary discontinuation of the medication in clinical situations that predispose to ketoacidosis (e.g. during prolonged fasting and acute illness, and perioperatively, i.e. 3 days prior to surgery) [ 154 – 158 ]. The Dapagliflozin in Respiratory Failure in Patients With COVID-19 (DARE-19) RCT demonstrated a low risk of DKA (0.3% vs 0% in dapagliflozin-treated vs placebo-treated participants) with structured monitoring of acid–base balance and kidney function during inpatient use in adults admitted with COVID-19 and at least one cardiometabolic risk factor without evidence of critical illness [ 159 ].
While early studies brought attention to several safety areas of interest (acute kidney injury, dehydration, orthostatic hypotension, amputation and fractures) [ 5 , 6 ], longer-term studies that have prospectively assessed and monitored these events [ 160 , 161 ] have not seen a significant imbalance in risks. Analyses of SGLT2i outcomes trial data also suggest that people with type 2 diabetes and peripheral arterial disease derive greater absolute outcomes benefits from SGLT2i therapy than those without peripheral arterial disease, and without an increase in risk of major adverse limb events [ 162 ]. In post hoc analyses, SGLT2i use has been associated with reduced incidence of serious and non-serious kidney-related adverse events in people with type 2 diabetes and CKD, and greater full recovery from acute kidney injury [ 163 ].
Glucagon-like peptide-1 receptor agonists
GLP-1 RA augment glucose-dependent insulin secretion and glucagon suppression, decelerate gastric emptying, curb post-meal glycaemic increments and reduce appetite, energy intake and body weight [ 5 , 6 , 164 ]. Beyond improving HbA 1c in adults with type 2 diabetes, specific GLP-1 RA have also been approved for reducing risk of MACE in adults with type 2 diabetes with established CVD (dulaglutide, liraglutide and subcutaneous semaglutide) or multiple cardiovascular risk factors (dulaglutide) (Table (Table1) 1 ) and for chronic weight management (subcutaneous liraglutide titrated to 3.0 mg once daily; subcutaneous semaglutide titrated to 2.4 mg once weekly). This is discussed in the sections on ‘Medications for weight loss in type 2 diabetes’ and ‘Personalised approach to treatment based on individual characteristics and comorbidities: recommended process for glucose-lowering medication selection’. GLP-1 RA are primarily available as injectable therapies (subcutaneous administration), with one oral GLP-1 RA now available (oral semaglutide) [ 165 ].
The recent higher dose GLP-1 RA studies have indicated incremental benefits for glucose and weight at higher doses of GLP-1 RA, with greater proportions of people achieving glycaemic targets and the ability of stepwise dose escalation to improve gastrointestinal tolerability. The Assessment of Weekly AdministRation of LY2189265 (dulaglutide) in Diabetes (AWARD)-11 trial evaluated higher doses of dulaglutide (3.0 mg and 4.5 mg weekly) compared with 1.5 mg weekly, demonstrating superior HbA 1c reductions (−19.4 vs −16.8 mmol/mol [−1.77 vs −1.54%], estimated treatment difference [ETD] −2.6 mmol/mol [−0.24%]) and weight loss (−4.6 vs −3.0 kg, ETD −1.6 kg) with dulaglutide 4.5 mg compared with 1.5 mg at 36 weeks in people with type 2 diabetes inadequately controlled with metformin [ 166 ]. Likewise, the SUSTAIN FORTE trial studied higher doses of once-weekly subcutaneous semaglutide (2.0 mg) compared with the previously approved 1.0 mg dose, reporting a mean change in HbA 1c from baseline to week 40 of −23 vs −21 mmol/mol (−2.1 vs −1.9%; ETD −2 mmol/mol [−0.18%]) and weight change of −6.4 kg with semaglutide 2.0 mg and −5.6 kg with semaglutide 1.0 mg (ETD −0.77 kg [95% CI −1.55, 0.01]) [ 167 ].
The most common side effects of GLP-1 RA are gastrointestinal in nature (nausea, vomiting and diarrhoea) and tend to occur during initiation and dose escalation and diminish over time. Gradual up-titration is recommended to mitigate gastrointestinal effects [ 164 , 168 , 169 ]. Education should be provided when initiating GLP-1 RA therapy. GLP-1 RA promote a sense of satiety, facilitating reduction in food intake. It is important to help people distinguish between nausea, a negative sensation, and satiety, a positive sensation that supports weight loss. Mindful eating should be encouraged: eating slowly, stopping eating when full and not eating when not hungry. Smaller meals or snacks, decreasing intake of high-fat and spicy foods, moderating alcohol intake and increasing water intake are also recommended. Slower or flexible dose escalations can be considered in the setting of gastrointestinal intolerance [ 168 , 169 ].
Data from CVOTs on other safety areas of interest (pancreatitis, pancreatic cancer and medullary thyroid cancer) indicate that there is no increase in these risks with GLP-1 RA. GLP-1 RA are contraindicated in people at risk of the rare medullary thyroid cancer [ 164 ], that is, those with a history or family history of medullary thyroid cancer or multiple endocrine neoplasia type 2, due to thyroid C-cell tumours seen in rodents treated with GLP-1 RA in preclinical studies. Increased retinopathy complications seen in the SUSTAIN 6 CVOT appear attributable to the magnitude and rapidity of HbA 1c reductions in individuals with pre-existing diabetic retinopathy and high glycaemic levels, as has been seen in previous studies with insulin [ 170 , 171 ]. GLP-1 RA are also associated with higher risks of gallbladder and biliary diseases [ 172 ].
Other glucose-lowering medications
Because of its high efficacy in lowering HbA 1c , minimal hypoglycaemia risk when used as monotherapy, weight neutrality with the potential for modest weight loss, good safety profile and low cost, metformin has traditionally been recommended as first-line glucose-lowering therapy for the management of type 2 diabetes. However, there is ongoing acceptance that other approaches may be appropriate. Notably, the benefits of GLP-1 RA and SGLT2i for cardiovascular and renal outcomes have been found to be independent of metformin use and thus these agents should be considered in people with established or high risk of CVD, HF or CKD, independent of metformin use [ 173 – 175 ]. Early combination therapy based on the perceived need for additional glycaemic efficacy or cardiorenal protection can be considered at treatment initiation to extend the time to treatment failure [ 176 ]. Metformin should not be used in people with an eGFR <30 ml/min per 1.73 m 2 and dose reduction should be considered when the eGFR is <45 ml/min per 1.73 m 2 [ 177 ]. Metformin use may result in lower serum vitamin B 12 concentrations and worsening of symptoms of neuropathy; therefore, periodic monitoring and supplementation are generally recommended if levels are deficient, particularly in those with anaemia or neuropathy [ 178 , 179 ].
Dipeptidyl peptidase-4 inhibitors
Dipeptidyl peptidase-4 inhibitors (DPP-4i) are oral medications that inhibit the enzymatic inactivation of endogenous incretin hormones, resulting in glucose-dependent insulin release and a decrease in glucagon secretion. They have a more modest glucose-lowering efficacy and a neutral effect on weight and are well tolerated with minimal risk of hypoglycaemia. CVOTs have demonstrated the cardiovascular safety without cardiovascular risk reduction of four DPP-4i (saxagliptin, alogliptin, sitagliptin and linagliptin) [ 141 ]. Reductions in risk of albuminuria progression were noted with linagliptin in the Cardiovascular and Renal Microvascular Outcome Study With Linagliptin (CARMELINA) trial [ 180 ]. While generally well tolerated, an increased risk of HHF was found with saxagliptin, which is reflected in its label, and there have been rare reports of arthralgia and hypersensitivity reactions with the DPP-4i class [ 16 ].
The high tolerability and modest efficacy of DPP-4i may mean that they are suitable for specific populations and considerations. For example, in a 6 month open-label RCT comparing a DPP-4i (linagliptin) with basal insulin (glargine) in long-term care and skilled nursing facilities, mean daily blood glucose was similar, with fewer hypoglycaemic events with linagliptin compared with insulin [ 181 ]. Treatment of inpatient hyperglycaemia with basal insulin plus DPP-4i has been demonstrated to be effective and safe in older adults with type 2 diabetes, with similar mean daily blood glucose but lower glycaemic variability and fewer hypoglycaemic episodes compared with the basal–bolus insulin regimen [ 182 ].
Glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist
In May 2022, the FDA approved tirzepatide, a GIP and GLP-1 RA, for once-weekly subcutaneous administration to improve glucose control in adults with type 2 diabetes as an addition to healthy eating and exercise. In the Phase III clinical trial programme, tirzepatide demonstrated superior glycaemic efficacy to placebo [ 183 , 184 ], subcutaneous semaglutide 1.0 mg weekly [ 185 ], insulin degludec [ 186 ] and insulin glargine [ 187 ]. For HbA 1c , placebo-adjusted reductions of 21 mmol/mol (1.91%), 21 mmol/mol (1.93%) and 23 mmol/mol (2.11%) were demonstrated with tirzepatide 5, 10 and 15 mg weekly, respectively, and mean weight reductions of 7–9.5 kg were seen [ 183 ]. Additional metabolic benefits included improvements in liver fat content and reduced visceral and subcutaneous abdominal adipose tissue volume [ 188 ]. Based on meta-analysis findings, tirzepatide was superior to its comparators, including other long-acting GLP-1 RA, in reducing glucose and body weight, but was associated with increased odds for gastrointestinal adverse events, in particular nausea [ 189 ]. Similar warnings and precautions are included in the prescribing information for tirzepatide as for agents in the GLP-1 RA class. Additionally, current short-term data from RCTs suggest that tirzepatide does not increase the risk of MACE vs comparators; however, robust data on its long-term cardiovascular profile will be available after completion of the SURPASS-CVOT trial [ 190 ]. Tirzepatide has received a positive opinion in the EU.
Sulfonylureas
As per the previous consensus report and update, sulfonylureas are assessed as having high glucose-lowering efficacy, but with a lack of durable effect, and the advantages of being inexpensive and accessible [ 5 , 6 ]. However, due to their glucose-independent stimulation of insulin secretion, they are associated with an increased risk for hypoglycaemia. Sulfonylureas are also associated with weight gain, which is relatively modest in large cohort studies [ 191 ]. Use of sulfonylureas or insulin for early intensive blood glucose control in the UK Prospective Diabetes Study (UKPDS) significantly decreased the risk of microvascular complications, underscoring the importance of early and continued glycaemic management [ 192 ]. Adverse cardiovascular outcomes with sulfonylureas in some observational studies have raised concerns, although findings from systematic reviews have found no increase in all-cause mortality rates compared with other active treatments [ 191 ]. The incidence of cardiovascular events was comparable in those treated with a sulfonylurea or pioglitazone in the Thiazolidinediones Or Sulfonylureas and Cardiovascular Accidents Intervention Trial (TOSCA.IT) [ 193 ], and no difference in the incidence of MACE was found in people at high cardiovascular risk treated with glimepiride or linagliptin [ 194 ], a medication whose cardiovascular safety was demonstrated in a population at high cardiovascular and renal risk [ 195 ].
Thiazolidinediones
Thiazolidinediones (TZDs) are oral medications that increase insulin sensitivity and are of high glucose-lowering efficacy [ 5 , 6 ]. TZDs have a high durability of glycaemic response, most likely through a potent effect on preserving beta cell function [ 196 ]. In the PROspective pioglitAzone Clinical Trial In macroVascular Events (PROactive) in adults with type 2 diabetes and macrovascular disease, a reduction in secondary cardiovascular endpoints was seen, although significance was not achieved for the primary outcome [ 197 ]. In the Insulin Resistance Intervention After Stroke (IRIS) study in adults without diabetes but with insulin resistance (HOMA-IR >3.0) and recent history of stroke or transient ischaemic attack, there was a lower risk of stroke or myocardial infarction with pioglitazone vs placebo [ 198 , 199 ]. Beneficial effects on non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH) have been seen with pioglitazone [ 200 , 201 ]. However, these benefits must be balanced against possible side effects of fluid retention and congestive HF [ 196 , 197 , 202 ], weight gain [ 196 – 198 , 202 , 203 ] and bone fracture [ 204 , 205 ]. Side effects can be mitigated by using lower doses and combining TZD therapy with other medications (SGLT2i and GLP-1 RA) that promote weight loss and sodium excretion [ 199 , 206 ].
The previous consensus report and update provide detailed descriptions of the different insulins [ 5 , 6 ]. The primary advantage of insulin therapy is that it lowers glucose in a dose-dependent manner and thus can address almost any level of blood glucose. However, its efficacy and safety are largely dependent on the education and support provided to facilitate self-management [ 5 , 6 ]. Careful consideration should be given to the pharmacokinetic and pharmacodynamic profiles of the available insulins, and the matching of the dose and timing to an individual’s physiological requirements. Numerous formulations of insulin are available, with advances in therapy geared toward better mimicking physiological insulin release patterns. Challenges of insulin therapy include weight gain, the need for education and titration for optimal efficacy, risk of hypoglycaemia, the need for regular glucose monitoring, and cost. The approval of biosimilar insulins may improve accessibility at lower treatment costs. Both insulin glargine U100 and insulin degludec have demonstrated cardiovascular safety in dedicated CVOTs [ 207 , 208 ]. Comprehensive education on self-monitoring of blood glucose, diet, injection technique, self-titration of insulin and prevention and adequate treatment of hypoglycaemia are of utmost importance when initiating and intensifying insulin therapy [ 5 , 6 ]. Novel formulations and devices including prefilled syringes, auto-injectors and intranasal insufflators are now available to administer glucagon in the setting of severe hypoglycaemia and should be considered for those at risk [ 209 ].
Starting doses of basal insulin (NPH or analogue) are estimated based on body weight (0.1–0.2 U/kg per day) and the degree of hyperglycaemia, with individualised titration as needed. A modest but significant reduction in HbA 1c and the risk of total and nocturnal hypoglycaemia has been observed for basal insulin analogues vs NPH insulin [ 210 ]. Longer-acting basal insulin analogues have a lower risk of hypoglycaemia than earlier generations of basal insulin, although may cost more. Concentrated insulins allow injection of a reduced volume [ 5 ]. Cost and access are important considerations and can contribute to treatment discontinuation. Short- and rapid-acting insulin can be added to basal insulin to intensify therapy to address prandial blood glucose levels. Premixed insulins combine basal insulin with mealtime insulin (short- or rapid-acting) in the same vial or pen, retaining the pharmacokinetic properties of the individual components. Premixed insulin may offer convenience for some but reduces treatment flexibility. Rapid-acting insulin analogues are also formulated as premixes, combining mixtures of the insulin with protamine suspension and the rapid-acting insulin. Analogue-based mixtures may be timed in closer proximity to meals. Education on the impact of dietary nutrients on glucose levels to reduce the risk of hypoglycaemia while using mixed insulin is important. Insulins with different routes of administration (inhaled, bolus-only insulin delivery patch pump) are also available [ 211 – 213 ].
Combination glucagon-like peptide-1/insulin therapy
Two fixed-ratio combinations of GLP-1 RA with basal insulin analogues are available: insulin degludec plus liraglutide (IDegLira) and insulin glargine plus lixisenatide (iGlarLixi). The combination of basal insulin with GLP-1 RA results in greater glycaemic lowering efficacy than the mono-components, with less weight gain and lower rates of hypoglycaemia than with intensified insulin regimens, and better gastrointestinal tolerability than with GLP-1 RA alone [ 214 , 215 ]. In studies of people with type 2 diabetes inadequately controlled on basal insulin or GLP-1 RA, switching to a fixed-ratio combination of basal insulin and GLP-1 RA demonstrated significant improvements in blood glucose levels and achievement of glycaemic goals with fewer hypoglycaemic events than with basal insulin alone [ 216 – 220 ].
Less commonly used glucose-lowering medications
Alpha-glucosidase inhibitors improve glycaemic control by reducing postprandial glycaemic excursions and glycaemic variability and may provide specific benefits in cultures and settings with high carbohydrate consumption or reactive hypoglycaemia [ 221 , 222 ]. Other glucose-lowering medications (i.e. meglitinides, colesevelam, quick-release bromocriptine and pramlintide) are not commonly used in the USA and most are not licensed in Europe. There was no new evidence that impacts clinical practice.
Comparative efficacy of glucose-lowering agents
In a network meta-analysis of 453 trials assessing glucose-lowering medications from nine drug classes, the greatest reductions in HbA 1c were seen with insulin regimens and GLP-1 RA [ 223 ]. A network meta-analysis comparing the effects of glucose-lowering therapy on body weight and blood pressure indicates that the greatest efficacy for reducing body weight is seen with subcutaneous semaglutide followed by the other GLP-1 RA and SGLT2i, and the greatest reduction in blood pressure is seen with the SGLT2i and GLP-1 RA classes [ 224 ]. As discussed above, the novel GIP and GLP-1 RA tirzepatide was associated with greater glycaemic and weight loss efficacy than semaglutide 1 mg weekly [ 185 ].
Combination therapy
The underlying pathophysiology of type 2 diabetes is complex, with multiple contributing abnormalities resulting in a naturally progressive disease and increasing HbA 1c over time in many. While traditional recommendations have focused on the stepwise addition of therapy, allowing for clear delineation of positive and negative effects of new drugs, there are data to suggest benefits of combination approaches in diabetes care. Combination therapy has several potential advantages, including (1) increased durability of the glycaemic effect [ 225 – 227 ], addressing therapeutic inertia, (2) simultaneous targeting of the multiple pathophysiological processes characterised by type 2 diabetes, (3) impacts on medication burden, medication-taking behaviour and treatment persistence and (4) complementary clinical benefits (e.g. on glycaemic control, weight and cardiovascular risk profiles) [ 215 , 228 – 244 ].
The Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE) was a multicentre open-label RCT designed to test four different diabetes medication classes in people with type 2 diabetes and compare their ability to achieve and maintain HbA 1c levels <53 mmol/mol (<7%). Eligible participants had their metformin therapy optimised and were randomly assigned to receive a sulfonylurea (glimepiride), a DPP-4 inhibitor (sitagliptin), a GLP-1 RA (liraglutide) or basal insulin (insulin glargine), with the primary outcome being the time to metabolic failure, defined as the time to an initial HbA 1c level ≥53 mmol/mol (≥7%), if it was confirmed at the next visit to remain above that threshold. Starting with a mean baseline HbA 1c level of 58 mmol/mol (7.5%) before the addition of one of the four medications, over 5 years of follow-up, 71% of the cohort reached the primary metabolic outcome. Insulin glargine and liraglutide were significantly, albeit modestly, more effective at achieving and maintaining HbA 1c targets. Liraglutide exhibited a lower risk than the pooled effect of the other three medications on a composite cardiovascular outcome comprising MACE, revascularisation, or HF or unstable angina requiring hospitalisation [ 245 , 246 ].
Personalised approach to treatment based on individual characteristics and comorbidities: recommended process for glucose-lowering medication selection
People with cardiorenal comorbidities.
The 2018 ADA/EASD consensus report and 2019 update focused on the consideration of clinically important factors when choosing glucose-lowering therapy. In people with established CVD or with a high risk for CVD, GLP-1 RA were prioritised over SGLT2i. Given their favourable drug class effect in reducing HHF and progression of CKD, SGLT2i were prioritised in people with HF, particularly those with a reduced ejection fraction, or CKD. Since 2019, additional cardiovascular, kidney and HF outcomes trials have been completed, particularly with SGLT2i. In addition, updated meta-analyses have been published that compare subgroup populations based on clinically relevant characteristics, such as presence of CVD, use of background therapy with metformin, stage of CKD, history of HF and age. Collectively, this new evidence was systematically retrieved and appraised to be incorporated into these clinical practice recommendations (Fig. (Fig.3 3 ).

Use of glucose-lowering medications in the management of type 2 diabetes
New evidence from cardiorenal outcomes studies since the last consensus report
In the Evaluation of Ertugliflozin Efficacy and Safety CVOT (VERTIS CV), which recruited exclusively people with established CVD and type 2 diabetes, ertugliflozin was similar to placebo with respect to the primary MACE outcome and all key secondary outcomes (including a composite kidney outcome) except for HHF [ 146 ]. The Canagliflozin and Renal Endpoints in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) study included adults with type 2 diabetes with an eGFR from 30 to <90 ml/min per 1.73 m 2 and albuminuria (30–500 mg/mmol [300–5000 mg/g] creatinine) [ 152 ]. In CREDENCE, canagliflozin treatment significantly reduced the risk of a composite primary outcome of progression to renal replacement therapy, eGFR of <15 ml/min per 1.73 m 2 , a doubling of serum creatinine level or death from cardiovascular or kidney causes. The Dapagliflozin And Prevention of Adverse outcomes in Chronic Kidney Disease (DAPA-CKD) trial recruited participants with and without type 2 diabetes with an eGFR of 25–75 ml/min per 1.73 m 2 and a urinary albumin/creatinine ratio (UACR) of 20–500 mg/mmol [200–5000 mg/g] [ 153 ]. Results of the trial demonstrated a clear benefit of dapagliflozin on a composite kidney outcome, on individual kidney-specific outcomes and on cardiovascular death or HHF, both in the overall population and in the subgroup of people with diabetes (68% of participants). In CREDENCE, the SGTL2i was continued until initiation of dialysis or transplantation.
The Effect of Sotagliflozin on Cardiovascular and Renal Events in Patients with Type 2 Diabetes and Moderate Renal Impairment Who Are at Cardiovascular Risk (SCORED) trial assessed sotagliflozin (a dual SGLT1i/SGLT2i, currently not approved for type 2 diabetes in the USA or the EU) in people with type 2 diabetes who had CKD and additional cardiovascular risk factors [ 147 ]. Sotagliflozin reduced the composite endpoint of cardiovascular mortality, HHF or urgent visits for HF compared with placebo, but had no effect on the composite kidney endpoint.
SGLT2i have been recently assessed in people with HF in dedicated HF outcome trials. In the Empagliflozin Outcome Trial in Patients With Chronic Heart Failure and a Reduced Ejection Fraction (EMPEROR-Reduced), empagliflozin reduced the primary composite endpoint of cardiovascular mortality or HHF in people with HF and a reduced ejection fraction, irrespective of the presence of type 2 diabetes (50% of participants) [ 149 ]. Notably, this beneficial effect of empagliflozin regardless of diabetes status was consistently evident in those with a preserved ejection fraction (>40%), as demonstrated in the Empagliflozin Outcome Trial in Patients With Chronic Heart Failure and a Preserved Ejection Fraction (EMPEROR-Preserved) [ 151 ]. Additionally, the Effect of Sotagliflozin on Cardiovascular Events in Patients With Type 2 Diabetes Post Worsening Heart Failure (SOLOIST-WHF) trial showed that, in people with type 2 diabetes and worsening HF, sotagliflozin reduced the total number of cardiovascular deaths or hospitalisations or urgent visits for HF compared with placebo regardless of ejection fraction [ 150 ]. All these data corroborate the salutary drug class effects of SGLT2i on HF-related outcomes in the setting of HF, irrespective of ejection fraction or diabetes status.
Finally, among GLP-1 RA, the Effect of Efpeglenatide on Cardiovascular Outcomes (AMPLITUDE-O) trial demonstrated a beneficial effect of weekly efpeglenatide on MACE and on a composite kidney outcome (decrease in kidney function or severe albuminuria) [ 247 ]. Of note, an exploratory analysis suggested a possible dose–response effect of efpeglenatide on MACE. In a CVOT of an osmotic mini-pump delivering exenatide subcutaneously (ITCA 650) over 3–6 months, ITCA 650 had a neutral effect on MACE compared with placebo over 16 months [ 248 ]. Both trials recruited individuals with type 2 diabetes with an established, or high, risk for CVD. Neither efpeglenatide nor ITCA 650 have received marketing authorisation by the FDA or EMA. As mentioned previously, the cardiovascular effects of tirzepatide are being assessed in the ongoing SURPASS-CVOT trial, with dulaglutide as an active comparator.
Evidence is emerging regarding the potential benefits of combined treatment with both an SGLT2i and a GLP-1 RA on outcomes. A post hoc analysis of data from the EXenatide Study of Cardiovascular Event Lowering (EXSCEL) has suggested that the combination of exenatide once-weekly (EQW) plus open-label SGLT2i reduces all-cause mortality rates and attenuates the decline in eGFR compared with treatment with EQW alone [ 244 ]. Importantly, a prespecified exploratory analysis of the AMPLITUDE-O trial found comparable benefits of GLP-1 RA treatment in participants who were receiving an SGLT2i as background therapy (15% of the total trial population) and those who were not [ 241 ].
Results from evidence syntheses
Recent cardiovascular, kidney and HF outcomes trials have been incorporated in updated meta-analyses assessing SGLT2i or GLP-1 RA, both in the overall trial populations and in clinically relevant subgroups. Pairwise meta-analyses of SGLT2i CVOTs verified that SGLT2i reduced MACE, HHF and a composite kidney outcome in the overall population vs placebo [ 142 , 249 ]. Regarding GLP-1 RA, a meta-analysis of relevant CVOTs demonstrated the favourable effect of GLP-1 RA vs placebo on MACE and its individual components including stroke, HHF and a composite kidney outcome including severe albuminuria [ 250 , 251 ]. It should be noted, however, that the overall effect estimate for HHF seems to have been driven by CVOTs of albiglutide and efpeglenatide, which are not available for clinical use. Similarly, the overall effect estimate for the composite kidney outcome was most likely driven by the effect of GLP-1 RA on severe albuminuria only and not on hard kidney endpoints. Of note, the beneficial kidney effects of canagliflozin, dapagliflozin and empagliflozin were also evident for hard kidney outcomes including chronic dialysis and kidney transplantation [ 252 ]. When individual components of MACE were analysed separately, GLP-1 RA reduced all three outcomes, with a more pronounced effect on stroke followed by cardiovascular death and myocardial infarction [ 253 , 254 ]. Conversely, SGLT2i, albeit reducing cardiovascular death, had a neutral effect on stroke [ 142 , 255 ].
The applicability of data to support selection of subgroups has been questioned because of a lack of RCTs focusing on specific populations, such as those using vs those not using metformin. This has been examined in subgroup analyses of recent meta-analyses [ 6 ]. It should be noted that findings of subgroup analyses should not be regarded as conclusive, their credibility should always be formally assessed and, ideally, they should be complemented by findings from relevant RCTs [ 7 , 8 ]. Recently published subgroup analyses have explored the role of background use of metformin as a potential effect modifier of cardiovascular benefit. For SGLT2i, no differences were observed in MACE, cardiovascular death or HHF, major kidney outcomes and mortality rates in those using vs those not using metformin [ 174 ]. Further, for GLP-1 RA, no differences were shown in MACE and mortality outcomes [ 256 – 258 ] in metformin users compared with non-users. The similarity of the direction and magnitude of the effect estimates between individual trials, the number of trials that contributed data, mostly to within-trial comparisons, and the statistical analyses implemented support the credibility of the conclusions favouring use of SGLT2i or GLP-1 RA in individuals with compelling indications independent of the use of metformin.
Similarly, other subgroup analyses have explored the role of baseline cardiovascular risk as a potential effect modifier regarding the effect of treatment on MACE, HHF or kidney outcomes. Consistency of findings from between-trial and within-trial comparisons, formal statistical testing verifying the absence of a subgroup effect and the similarity of baseline cardiovascular risk across different cardiovascular risk categories between individual CVOTs despite the use of seemingly different enrolment criteria suggest the benefits of the use of SGLT2i or GLP-1 RA in people with type 2 diabetes and established CVD and in those at high cardiovascular and/or kidney risk [ 142 , 253 ]. Of note, the level of certainty in this recommendation is higher for the former subgroup, because some CVOTs recruited exclusively people with established CVD, while fewer events were recorded for participants with cardiovascular risk factors only in CVOTs that recruited both subgroup populations. In addition, the definition used for risk factors was not identical among CVOTs. However, in general it comprised age ≥55 years plus two or more additional risk factors (including obesity, hypertension, smoking, dyslipidaemia or albuminuria). Furthermore, in terms of absolute effects, the cardiovascular benefits of GLP-1 RA and SGLT2i were less pronounced in people with three or more cardiovascular risk factors than in those with established CVD. This was shown in a network meta-analysis that estimated the absolute effects of treatment with GLP-1 RA or SGLT2i on cardiovascular and kidney outcomes for different categories of baseline cardiovascular risk by combining relative effect estimates with baseline risk estimates [ 259 ].
Subgroup meta-analyses based on participants’ kidney function indicated that the salutary effects of SGLT2i on MACE, cardiovascular death or HHF, and a composite kidney outcome (substantial loss of kidney function, end-stage kidney disease or death due to kidney disease) do not significantly differ among subgroups based on eGFR [ 142 , 252 ]. Moreover, the overall effect on MACE and the kidney outcome seemed to be consistent across the three subgroups (normal urine albumin excretion rate [UACR <3.0 mg/mmol (<30 mg/g)], moderate albuminuria [UACR 3.0–30 mg/mmol (30–300 mg/g)] and severe albuminuria [UACR ≥30 mg/mmol (≥300 mg/g)]) [ 252 ]. In addition, no modification of the effect estimates for MACE, cardiovascular death or HHF, and the composite kidney outcome was observed for SGLT2i in subgroup meta-analyses based on history of HF [ 142 ]. Regarding GLP-1 RA, a subgroup meta-analysis found that their effect on MACE did not significantly differ between people with an eGFR <60 ml/min per 1.73m 2 and those with an eGFR ≥60 ml/min per 1.73 m 2 [ 253 ]. Moreover, the effect on MACE did not appear to differ between people with lower and higher HbA 1c at baseline, both for SGLT2i and for GLP-1 RA [ 142 , 253 ]. Nevertheless, the conclusions of all subgroup analyses should be regarded with increased caution because of the small number of trials contributing data to within-trial comparisons, heterogeneity between individual trials or lack of formal statistical testing.
Comparative effectiveness data
While CVOTs and pairwise meta-analyses allow inferences about the overall efficacy and safety of novel glucose-lowering therapies, none of them directly compared SGLT2i with GLP-1 RA. However, the comparative effectiveness of the two drug classes has been assessed in three recent network meta-analyses, which found that, in people with type 2 diabetes, SGLT2i were superior to GLP-1 RA in reducing HHF and a composite kidney outcome, while GLP-1 RA seemed more efficacious in reducing the risk of stroke [ 223 , 259 , 260 ]. No important differences between the two drug classes were evident in terms of mortality rates and other cardiovascular outcomes. These conclusions are further supported by observational data from a large population-based cohort study in the USA, which showed that SGLT2i reduced HHF compared with GLP-1 RA in people both with CVD (HR 0.71; 95% CI 0.64, 0.79) and without CVD (HR 0.69; 95% CI 0.56, 0.81). Differences between the two drug classes with regard to mortality rates and other cardiovascular outcomes were not clinically important [ 261 ].
In terms of differences among individual SGLT2i and GLP-1 RA, choice should be based on country-specific label indications and data on efficacy, safety and outcome benefits considering within-class heterogeneity. No CVOT is available focusing on people with type 2 diabetes who are at low cardiovascular risk. Some inferences about the effect of glucose-lowering medications as primary cardiovascular prevention in populations with low cardiovascular risk can be made from network meta-analyses, suggesting that no agent or drug class has a notable beneficial effect on cardiovascular events in low-risk individuals with diabetes [ 223 , 259 ].
Additional clinical considerations
Age: older people with diabetes.
Type 2 diabetes represents a model of accelerated biological ageing. As such, type 2 diabetes is associated with declines in physical capacity, underpinned by dysfunction within skeletal muscle. The ability of people with type 2 diabetes to undertake simple functional exercises in middle-age has been shown to be like those at least a decade older within the general population. Importantly, this places people living with type 2 diabetes at a high risk of impaired physical function and frailty, which in turn reduces quality of life and increases healthcare use. As such, frailty is increasingly recognised as a major complication of type 2 diabetes and an important target for treatment [ 112 , 262 ].
Informed decisions regarding treatment of older (>65 years) adults with diabetes are limited by the under-representation of such participants in clinical trials. When older individuals have been studied, analyses from trials such as Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) suggested that more frail individuals have worse outcomes and benefit less from intensive control of blood glucose levels and blood pressure [ 263 ]. However, our confidence in selecting medications to improve outcomes has improved, in part because of regulatory requirements to include older people in trials to determine the efficacy and safety of new drugs for diabetes [ 264 , 265 ]. For example, a recent meta-analysis of 11 large outcomes trials found that, in those aged 65 years or older, the cardiovascular and/or kidney outcomes benefits of GLP-1 RA or SGLT2i therapy were consistent with the effects seen in the overall trial population [ 266 ]. Therefore, recommendations for the selection of medications to improve cardiovascular and kidney outcomes do not differ for older people. Older age should not be an obstacle to treatment of individuals with established or high risk for CVD. However, medication choices for people who are frail or who have multiple comorbidities may require modification for safety and tolerability. People with diabetes should also understand and be able to appropriately modify use of their prescribed medications during times of illness. Frailty is associated with poorer prognosis, and some attenuation of benefit from intensive glucose-lowering and blood pressure-lowering treatments has been demonstrated in frail individuals [ 263 ]. Consideration of de-prescribing medication to avoid unnecessary medication or medication associated with harm, such as hypoglycaemia and hypotension, is important in such populations.

Age: younger people with diabetes
Rates of impaired glucose tolerance and/or impaired fasting glucose and type 2 diabetes have increased significantly in the adolescent and young adult population, in concert with increases in obesity [ 267 ]. It is estimated that one in five adolescents and one in four young adults now have impaired glucose tolerance and/or impaired fasting glucose in the USA, which in turn increases the risks of progression to type 2 diabetes, CKD and cardiovascular complications [ 267 ]. Minority populations are particularly affected, with half or more of newly diagnosed cases of type 2 diabetes in childhood and adolescence occurring in Hispanic, non-Hispanic Black, Asian/Pacific Islander and American Indian populations [ 268 ]. Affected young people have a more rapid deterioration in blood glucose levels, an attenuated response to diabetes medication and more rapid development of diabetes complications [ 269 – 273 ]. Early disease onset, higher levels of hyperglycaemia, and the multiple cardiometabolic risk factors found in adolescents and young adults with impaired glucose tolerance and/or impaired fasting glucose and diabetes all contribute to an increase in risk of adverse outcomes [ 267 ]. Most children and adolescents who develop type 2 diabetes will have microvascular complications by young adulthood [ 274 ]; in addition, a recently identified 25% increase in the risks of hyperglycaemic crises, acute myocardial infarction, stroke and lower extremity amputation over a 5 year period was most notable in people with diabetes aged 18–44 years [ 275 ]. Younger people with type 2 diabetes should be considered at very high risk for complications and treated correspondingly. Early use of combination therapy may be considered, as the Vildagliptin Efficacy in combination with metfoRmIn for earlY treatment of type 2 diabetes (VERIFY) trial findings suggest that this approach provides superior and more durable effects on blood glucose levels than metformin monotherapy in people with both early-onset (age <40 years) and later-onset diabetes [ 276 ]. Most of the evidence for health behaviour interventions, glucose-lowering approaches and the effectiveness of medications to improve cardiovascular and kidney outcomes in younger people with diabetes is poorly understood because of the very limited enrolment of this group in completed trials [ 15 ]. Beyond the scope of this statement, there are data emerging on the use of GLP-1 RA and SGLT2i in children that suggest glycaemic benefit; however, the durability of this effect and any impact on cardiorenal outcomes in children and young adults remain unknown.
Race and ethnicity
Although specific populations are disproportionately affected by diabetes, they are consistently under-represented in outcomes and other trials. A meta-analysis of six large cardiovascular and kidney outcomes trials found that non-White participants had higher rates of cardiovascular and other comorbidities than the White cohort but comprised only about 21% of the overall enrolled trial populations. Importantly, both non-White and White subgroups had significant reductions in the risk of cardiovascular death or HHF with SGLT2i therapy compared with placebo (OR 0.66 and 0.82, respectively) [ 277 ]. The increased burden of complications in under-represented populations with diabetes should be factored into personalised treatment plans, and beneficial medications should be used irrespective of race or ethnicity. Ongoing and future trials should recruit to be representative of the overall population of people with diabetes, so that the effects of interventions in understudied subgroups may be better ascertained [ 278 , 279 ].
Sex differences
In women with reproductive potential, the use of highly effective contraception should be ensured, such as long-acting reversible contraception (intrauterine device or progesterone implant), prior to prescribing medications that may adversely affect a fetus. Diabetes significantly increases the risk of cardiovascular complications in both sexes, and CVD causes most hospitalisations and deaths in women and men with diabetes [ 280 , 281 ]. In the general population, women are at lower risk for cardiovascular events than men of the same age; however, this vascular protection or advantage is reduced in women who develop type 2 diabetes [ 282 , 283 ]. In fact, the increase in relative risk of CVD due to type 2 diabetes is greater in women than in men [ 284 – 286 ]. Despite this, women have been under-represented in recent CVOTs in diabetes, comprising between 28.5% and 35.8% of participants [ 287 ]. This analysis also described differing patterns of cardiovascular complications in women compared with men, and poorer management of cardiovascular risk factors in women [ 287 ]. Within-trial analyses and meta-analyses suggest that there are likely no between-sex differences in outcomes achieved with SGLT2i and GLP-1 RA therapy [ 288 , 289 ]. Continued efforts should be made to enrol women in outcomes trials and to identify and address modifiable cardiovascular risk factors in women with diabetes.
Obesity and weight-related comorbidities, particularly NAFLD and NASH
The care of people with diabetes who have weight-related comorbidities such as NAFLD, HF with preserved ejection fraction or obstructive sleep apnoea should include strategies intended to result in weight loss. People with type 2 diabetes frequently have NAFLD and are at increased risk for progression to more severe stages of liver disease, including NASH, hepatic fibrosis and cirrhosis [ 290 ]. The management of type 2 diabetes in people with NASH should include lifestyle modification with a goal of weight loss, including strong consideration of medical and/or surgical approaches to weight loss in those at higher risk of hepatic fibrosis [ 291 ]. Pioglitazone, GLP-1 RA therapy and metabolic surgery have all been shown to reduce NASH activity; pioglitazone therapy and metabolic surgery may also improve hepatic fibrosis [ 188 , 292 – 298 ].
Although not licensed for this purpose, it has therefore been suggested that people with type 2 diabetes at intermediate to high risk of fibrosis should be considered for treatment with pioglitazone and/or a GLP-1 RA with evidence of benefit [ 291 , 299 ]. Although SGLT2i therapy has also been shown to reduce elevated levels of liver enzymes and hepatic fat content in people with NAFLD, at this time there is less evidence to support use of this class of drug as treatment for NASH [ 300 – 302 ]. NAFLD, and in particular NASH, is also associated with an increased risk of cardiovascular complications; therefore, people with NAFLD should have their cardiovascular risk factors assessed and managed to minimise this risk [ 303 ].
SGLT2i have been shown to reduce incident obstructive sleep apnoea in two SGLT2i CVOTs based on adverse event reporting [ 304 , 305 ]. However, it is not clear that the data collected on incident obstructive sleep apnoea in these trials were complete, or that the benefit is mediated through changes in weight.
Consensus recommendations
- All people with type 2 diabetes should be offered access to ongoing DSMES programmes.
- Providers and healthcare systems should prioritise the delivery of person-centred care.
- Optimising medication adherence should be specifically considered when selecting glucose-lowering medications.
- MNT focused on identifying healthy dietary habits that are feasible and sustainable is recommended in support of reaching metabolic and weight goals.
- Adults with type 2 diabetes should engage in physical activity regularly (>150 min/week of moderate- to vigorous-intensity aerobic activity) and be encouraged to reduce sedentary time and break up sitting time with frequent activity breaks.
- Aerobic activity should be supplemented with two to three resistance, flexibility and/or balance training sessions/week. Balance training sessions are particularly encouraged for older individuals or those with limited mobility/poor physical function.
- Metabolic surgery should be considered as a treatment option in adults with type 2 diabetes who are appropriate surgical candidates with a BMI ≥40.0 kg/m 2 (BMI ≥37.5 kg/m 2 in people of Asian ancestry) or a BMI of 35.0–39.9 kg/m 2 (32.5–37.4 kg/m 2 in people of Asian ancestry) who do not achieve durable weight loss and improvement in comorbidities (including hyperglycaemia) with non-surgical methods.
- In people with established CVD, a GLP-1 RA with proven benefit should be used to reduce MACE, or an SGLT2i with proven benefit should be used to reduce MACE and HF and improve kidney outcomes.
- In people with CKD and an eGFR ≥20 ml/min per 1.73 m 2 and a UACR >3.0 mg/mmol (>30 mg/g), an SGLT2i with proven benefit should be initiated to reduce MACE and HF and improve kidney outcomes. Indications and eGFR thresholds may vary by region. If such treatment is not tolerated or is contraindicated, a GLP-1 RA with proven cardiovascular outcomes benefit could be considered to reduce MACE and should be continued until kidney replacement therapy is indicated.
- In people with HF, SGLT2i should be used because they improve HF and kidney outcomes.
- In individuals without established CVD but with multiple cardiovascular risk factors (such as age ≥55 years, obesity, hypertension, smoking, dyslipidaemia or albuminuria), a GLP-1 RA with proven benefit could be used to reduce MACE, or an SGLT2i with proven benefit could be used to reduce MACE and HF and improve kidney outcomes.
- In people with HF, CKD, established CVD or multiple risk factors for CVD, the decision to use a GLP-1 RA or SGLT2i with proven benefit should be independent of background use of metformin.
- SGLT2i and GLP-1 RA reduce MACE, which is likely to be independent of baseline HbA 1c . In people with HF, CKD, established CVD or multiple risk factors for CVD, the decision to use a GLP-1 RA or an SGLT2i with proven benefit should be independent of baseline HbA 1c .
- In general, selection of medications to improve cardiovascular and kidney outcomes should not differ for older people.
- In younger people with diabetes (<40 years), consider early combination therapy.
- In women with reproductive potential, counselling regarding contraception and taking care to avoid exposure to medications that may adversely affect a fetus are important.
Putting it all together: strategies for implementation
Importance of integrated care.
The overall goal of the management of type 2 diabetes is to maintain quality of life and avoid complications. The management approach must be holistic and multifactorial and account for the lifelong nature of type 2 diabetes (Figs (Figs1, 1 , ,3, 3 , ,4). 4 ). The person living with type 2 diabetes should be at the centre of care. The structure and organisation of the healthcare team will vary across systems but generally involves multiple disciplines, including the primary care provider, diabetologist, diabetes care and education specialist, registered dietitian/nutritionist, pharmacists, nurses and other specialists as needed (e.g. dentist, eye care professional, podiatrist, mental health provider, cardiologist, nephrologist, neurologist, hepatologist, sleep medicine specialist and pain management specialist) [ 306 ]. Technology is now an important tool to enhance communication, support and monitoring. Communication between people living with type 2 diabetes and healthcare team members is at the core of integrated care, and clinicians must recognise the importance of language in this communication.

Holistic person-centred approach to T2DM management
Practical tips for clinicians (Supplementary Fig. 1 )
- Acknowledge the lifelong and evolving nature of type 2 diabetes.
- Identify and coordinate with the team.
- Know your local resources.
- Language matters in diabetes care.
Individualisation of care
The integrated care of type 2 diabetes must consider the person with diabetes as an individual (Figs (Figs1, 1 , ,3, 3 , ,4) 4 ) with respect to specific preferences and values, social determinants of health, barriers to care, comorbid conditions, degree of hyperglycaemia, risks of complications and susceptibility to medication side effects. Attention should be given to how the balance of risks and benefits of each intervention is communicated to each person living with diabetes. ‘Risk estimator’ tools, especially for CVD risk, may also be helpful, but when using these tools one must be aware that they work best when they are derived from and/or are validated in a population similar to the population in which they are applied [ 307 ]. These risk estimator tools are often developed in populations that exclude younger and older people and under-represent women and various minority populations. Finally, shared decision making is essential to incorporating an individual’s preferences and values when formulating a management plan.
Social determinants of health must be assessed and addressed [ 47 ] to achieve health equity in diabetes. Health systems must ensure equity in the delivery of all diabetes care, including access to the more expensive, organ-protecting pharmacotherapies (SGLT2i and GLP-1 RAs) and technologies (e.g. CGM).
Many people living with type 2 diabetes have multiple comorbidities, some related to diabetes, such as obesity, hypertension, dyslipidaemia, cardiorenal disease, NASH/NAFLD and mental health problems. Other important conditions whose relationship to diabetes is not as well established, such as chronic obstructive pulmonary disease and cancer, are prevalent. Attention to these comorbidities should be paid throughout the lifespan of the person living with diabetes, as such comorbidities may impact the tailoring and implementation of the holistic plan for diabetes management, including choice of glucose-lowering medication.
Importantly, diabetes is associated with cognitive decrements, which can substantially impact management [ 308 , 309 ]. Further, long-term hyperglycaemia is associated with worsening cognitive decline. Screening for cognitive impairment should be performed when risk factors are identified such as frequent hypoglycaemia, difficulty with diabetes self-management or unexplained falls. People with cognitive impairment should be referred for additional support. Other conditions such as serious mental illness and substance use disorders must also be identified and managed appropriately in the holistic approach to diabetes. Mental illness, including depression, is associated with an increased risk of diabetes and with poorer prognosis but may also complicate diabetes management and be a barrier to self-management.
- Consider each person living with diabetes as an individual with specific context, risks and preferences.
- Healthcare systems should monitor and address inequity in the delivery of evidence-based interventions for type 2 diabetes.
- Assess and address social determinants of health for each individual living with diabetes, particularly in those not achieving goals.
- Incorporate comorbidities when developing and implementing the management plan.
DSMES is critical to integrated, holistic, person-centred care in type 2 diabetes [ 19 – 21 , 23 ] and is as important to the management plan as the selection of medication. DSMES should be offered on an ongoing basis, should be provided by trained diabetes care and education specialists and can be delivered using multiple approaches and in a variety of settings (Supplementary Table 1 ) [ 20 , 31 ]. The care team must be aware of the available local DSMES resources and how to access them. Importantly, DSMES is complementary to but does not replace MNT (see below) [ 310 ] or referral for mental health services when they are warranted [ 49 ].
- Embrace DSMES as being as important as other aspects of diabetes care such as pharmacotherapy.
- Identify and know how to access your local DSMES resources.
- Impress on the person and the healthcare team the importance of DSMES in the ongoing holistic approach to the management of type 2 diabetes.
- Initiate or refer for DSMES at diagnosis, annually, with changes in social or health status and with transitions of care or life situation.
Facilitating healthy behaviours and weight management
Promotion of healthy behaviours is central to the holistic management of type 2 diabetes and should be addressed at the time of diagnosis and throughout the course of diabetes. Healthy behaviours include healthy nutrition, regular physical activity, adequate sleep and smoking cessation. Health behaviours should always be assessed and addressed when glycaemic targets are not met and when new pharmacotherapy or interventions (e.g. metabolic surgery) are initiated.
All individuals with type 2 diabetes should be offered MNT to develop a personal food plan in the context of diabetes. The need for additional dietary advice should be re-evaluated over time [ 310 ]. There is no single dietary pattern recommended for all individuals with type 2 diabetes; many dietary patterns can be effective for achieving treatment goals and a structured food plan should be based on an individual person’s preferences and context.
Explicit physical activity and minimisation of sedentary time should be the focus of the physical activity regimen for people living with type 2 diabetes (Fig. (Fig.2). 2 ). Individual preferences and circumstances should inform the specific activity regimen. A reasonable target for physical activity is at least 150 min/week. In addition to these activity minutes, breaking up sedentary time with activity breaks (e.g. 5 min activity break every hour) can be beneficial [ 101 ]. A gradual increase in overall volume and intensity of activity does not require medical clearance [ 101 ]. Additional clinical assessment may be warranted in those with moderate-to-severe diabetic retinopathy, diabetic kidney disease, peripheral neuropathy and unstable HF and for those prescribed insulin or with a history of hypoglycaemia [ 101 ]. Individual preferences, motivations and circumstances should inform choice.
Weight management should be a central focus for individuals with type 2 diabetes with overweight or obesity, with individualised weight loss goals. For most people, a target of at least 5% weight loss is reasonable and can be expected to have clinical benefits. Substantial (>10%) weight loss and weight loss early in the course of type 2 diabetes increase the chance of remission of disease [ 50 ]. The use of glucose-lowering agents that provide significant weight loss, particularly GLP-1 RA with high weight loss efficacy, should be considered as they can often provide 10–15% weight loss or more. Metabolic surgery, which is most effective when performed early during diabetes, can be considered in those without a sufficient response to non-surgical weight loss interventions based on the specific context and preferences and should be accompanied by health behaviour interventions. The benefits of metabolic surgery need to be balanced against its potential adverse effects, which vary by procedure and include surgical complications, late metabolic or nutritional complications and impact on psychological health [ 5 , 6 , 127 ]. People being considered for metabolic surgery should be evaluated for comorbid psychological conditions and social and situational circumstances that may interfere with surgery outcomes. People who undergo metabolic surgery should receive long-term medical and behavioural support. Metabolic surgery should be performed in high-volume centres with experienced multidisciplinary teams [ 127 ].
SMART (specific, measurable, attainable, relevant, time-based) goals are more effective for achieving behaviour change than non-specific recommendations [ 311 ]. An ‘all or none’ approach related to behavioural goals should be avoided as any improvement in healthy behaviours can have a positive impact in diabetes [ 93 , 312 ]. Self-monitoring of achievements (e.g. physical activity monitoring and weight measurement) is crucial to the achievement of health behaviour goals (Fig. (Fig.1). 1 ). Behavioural health specialists or psychologists with specific training in behaviour change interventions can be of particular value as members of the team to help the person with type 2 diabetes achieve goals.
Practical tips for clinicians (Supplementary Fig. 2 )
- Specific health behaviour and weight management goals should be agreed on between the person with type 2 diabetes and the care team; shared decision making is an important component of this discussion.
- Emphasise self-monitoring behaviours and review data collected (e.g. glucose monitoring, weight, tracking physical activity) in clinical visits to convey their importance in achieving the desired health behaviour goals.
- People taking insulin or a sulfonylurea should be educated about the risk, symptoms and treatment of hypoglycaemia when undertaking physical activity or adopting a specific nutritional plan; prescribe glucagon in people at risk for severe hypoglycaemia.
- DSMES and MNT can help the person living with diabetes to identify and address barriers to implementing healthier behaviours.
Choice of glucose-lowering medication
The choice of glucose-lowering agents should be directed by the individual profile of the person with type 2 diabetes, in particular the presence of comorbidities, risk of side effects, preferences and context (Figs (Figs3, 3 , ,4). 4 ). Pharmacological treatment of hyperglycaemia must be integrated in DSMES and accompanied by a focus on healthy behaviours from diagnosis onwards. This should be integrated as part of a holistic, multifactorial approach to type 2 diabetes that includes weight, blood pressure and lipid management (Fig. (Fig.4 4 ).
Whereas the pursuit of glycaemic control and the pursuit of organ-specific (e.g. heart and kidney) protection are complementary and not mutually exclusive, clinicians should not confuse the discussion of choice of agents for their glucose-lowering effect with the discussion of choice of specific agents for their direct organ-protecting effect. Some agents, in particular SGLT2i, have been shown to protect organs (heart, kidney) partly independently of their glucose-lowering effect, as this organ protection also occurs in those not affected by type 2 diabetes.
Based on these principles, regardless of HbA 1c level or the presence of other glucose-lowering agents, all individuals with diabetes and established or subclinical CVD should be prescribed an agent with proven cardiovascular benefit from the GLP-1 RA class or SGLT2i class [ 5 , 6 ]. The evidence for cardiovascular benefits of GLP-1 RA and SGLT2i in those with only risk factors for CVD, based on MACE (myocardial infarction, stroke or cardiovascular death), is less robust, as fewer people with lower event rates are included in studies [ 313 – 315 ]. Furthermore, it is important to recognise that the predicted absolute benefit of an intervention is dependent on the absolute risk and thus those with prior CVD events are more likely to experience a benefit over intermediate time frames than those with cardiovascular risk factors only. Through shared decision making, considering an individual’s lifelong CVD risk, introduction of a GLP-1 RA or SGLT2i with proven cardiovascular benefit into the regimen for a person with CVD risk factors can be considered in the context of increased treatment burden and potential side effects with lower absolute risk reduction.
All individuals with diabetes and CKD (eGFR <60 ml/min per 1.73 m 2 or UACR >3.0 mg/mmol [>30 mg/g]) should receive an agent with proven kidney benefit from the SGLT2i class (or GLP-1 RA class if SGLT2i are contraindicated or not preferred or their use is not permitted under license). Likewise, those with HF (HF with reduced ejection fraction or HF with preserved ejection fraction) should receive an agent from the SGLT2i class with proven benefit for HF. In both instances, the goal of organ protection with SGLT2i or GLP-1 RA should be independent of background glucose-lowering therapies, current HbA 1c level or target HbA 1c level (Figs (Figs3, 3 , ,4 4 ).
While there is compelling evidence to support a place for SGLT2i and the GLP-1 RA class in the treatment of many people with type 2 diabetes based on their direct organ-protecting effects, it is acknowledged that to date these agents are expensive. In the setting of resource constraints, prioritisation of the highest risk groups for access to these agents may be needed, with consideration of absolute risk reduction in addition to relative risk reductions.
Evidence on specific agents and their effects on other comorbidities, such as NAFLD, is emerging. For those with NAFLD/NASH at high risk of fibrosis, pioglitazone could be considered. There is emerging evidence for benefits of metabolic surgery and three classes of glucose-lowering therapy (GLP-1 RA, SGLT2i, and GIP and GLP-1 RA) [ 188 , 292 – 298 , 316 ].
Overall, for treatment of hyperglycaemia, metformin remains the agent of choice in most people with diabetes, based on its glucose-lowering efficacy, minimal risk of hypoglycaemia, lack of weight increase and affordability. Often, monotherapy with metformin will not suffice to maintain glucose levels at target. As proposed in the previous consensus report and update [ 5 , 6 ], other classes of agents are useful in combination with metformin or when metformin is contraindicated or not tolerated. Selection of other glucose-lowering agents will be determined by the balance between the glucose-lowering efficacy and the side effect profile of the individual agents (see Table Table1 1 ).
Special attention needs to be given to populations in which hypoglycaemia is most dangerous, for example people with frailty, in whom agents without risk of hypoglycaemia need to be prioritised. If sulfonylureas or insulin are used, consideration of less stringent targets in such settings is prudent and de-prescribing if asymptomatic or severe hypoglycaemia ensues.
Finally, it needs to be stated that the evidence on organ-protecting or glucose-lowering effects of specific pharmacotherapies in specific subpopulations (e.g. younger and older people, women and various racial/ethnic groups) continues to be limited. This lack of evidence is, however, not a reason to withhold these medications in these subpopulations, given their proven benefits in large general populations.
- Providers should continually update their knowledge on the efficacy and side effects of diabetes pharmacotherapy (see Table Table1 1 ).
- Identify relevant comorbidities (e.g. obesity, CVD, HF, CKD, NAFLD).
- Assess the profile of the person with diabetes (e.g. younger age, frailty, limited life expectancy, cognitive impairment, social determinants of health).
- Consider risk factors for medication adverse events (e.g. hypoglycaemia, volume depletion, genital infections, history of pancreatitis).
- Prioritise the use of organ-protective medications (GLP-1 RA, SGLT2i, TZD) in those with cardiorenal disease or NASH or at high risk.
Proactive care: avoiding inertia
Reassessment of individual glycaemic targets and their achievement at regular intervals is key (Figs (Figs1, 1 , ,3, 3 , ,4). 4 ). When targets are not met, in addition to addressing health behaviours and referral to DSMES, the intensification of glucose-lowering medication by combining agents with complementary mechanisms of action should be pursued. Traditionally, a stepwise approach was advocated, in which a new agent is added to the existing regimen, but evidence is growing to support a more proactive approach in many, by combining glucose-lowering agents from initial diagnosis [ 6 ].
Early use of combinations of agents allows tighter glucose control than monotherapy with the individual agents, and thus combinations of agents are indicated in those who have HbA 1c levels >16.3 mmol/mol (>1.5%) above their target at diagnosis (e.g. ≥70 mmol/mol [8.5%] in most) [ 6 ]. In particular, among young adults with type 2 diabetes, immediate and sustained glycaemic management should be pursued, aiming for HbA 1c <53 mmol/mol (7%) (or even lower). This presents the best opportunity to avoid complications of diabetes across the lifespan. Moreover, the pathophysiology of micro- and macrovascular damage shares more commonality than usually thought, suggesting that the prevention of microvascular disease may, in the long term, contribute to a reduction in macrovascular complications as well [ 317 ].
The knowledge base guiding clinicians beyond dual therapy in type 2 diabetes is still limited. In general, intensification of treatment beyond two medications follows the same general principles as the addition of a second medication, with the assumption that the effectiveness of third and fourth medications will be generally less than when they are used alone. Whereas solid evidence exists for combining SGLT2i and GLP-1 RA for weight and glucose lowering, emerging data suggest promise for combined effects on cardiorenal outcomes [ 228 ].
As more medications are added, there is an increased treatment burden and risk of adverse effects. It is important to consider medication interactions and whether regimen complexity may become an obstacle to adherence. Fixed-dose combination preparations can improve medication-taking behaviours. Finally, with each additional medication comes increased costs, which can affect medication-taking behaviour and medication effectiveness [ 318 – 326 ].
Response to all therapies should be reviewed at regular intervals, including the impact on efficacy (HbA 1c , weight), safety and organ protection. While most people with diabetes require intensification of glucose-lowering medications, some require medication reduction or discontinuation, particularly if the therapy is ineffective or associated with side effects such as hypoglycaemia or when glycaemic goals have changed because of a change in clinical circumstances (e.g. development of comorbidities or even healthy ageing). Medication should be stopped, or the dose reduced, if there are minimal benefits or if harm outweighs any benefit. Ceasing or reducing the dose of medications that have an increased risk of hypoglycaemia is suggested when any new glucose-lowering treatment (behavioural or medication) is started and the individual’s glycaemic levels are close to target [ 66 ]. HbA 1c levels below 48 mmol/mol (6.5%) or substantially below the individualised glycaemic target as well as any increased risk of hypoglycaemia should prompt stopping or reducing the dose of medications associated with an increased risk of hypoglycaemia.
- Consider initial combination therapy with glucose-lowering agents, especially in those with high HbA 1c at diagnosis (i.e. >70 mmol/mol [>8.5%]), in younger people with type 2 diabetes (regardless of HbA 1c ) and in those in whom a stepwise approach would delay access to agents that provide cardiorenal protection beyond their glucose-lowering effects.
- Avoid therapeutic inertia and re-evaluate health behaviours, individuals’ medication-taking behaviours and side effects of agents at every clinic visit.
- When additional glycaemic control is needed, incorporate, rather than substitute, glucose-lowering therapies with complementary mechanisms of action.
- Consider fixed-dose combinations to reduce prescription burden.
- Consider de-intensification of therapy, e.g. in frail older adults and in the setting of hypoglycaemia-causing medications, in those with glycaemic metrics substantially better than target.
Place of insulin in type 2 diabetes
Insulin is a useful and effective glucose-lowering agent (Fig. (Fig.5). 5 ). When glycaemic measurements do not reach targets, and insulin is the best choice for the individual, its introduction should not be delayed. When clinicians are not familiar with insulin use, referral to specialist care is indicated. However, with the growing evidence supporting use of particular agents in people with type 2 diabetes with specific profiles (comorbidities, overweight/obesity) and with the availability of multiple glucose-lowering agents with good efficacy and acceptable side effect profiles, the initiation of insulin can be postponed in many to later stages of the disease. GLP-1 RA should be considered in all when no contraindications are present before initiation of insulin therapy, as they allow lower glycaemic targets to be reached with a lower injection burden and lower risk of hypoglycaemia and weight gain than with insulin alone.

Place of insulin 1
The preferred way of initiating insulin in people with type 2 diabetes is to add basal insulin to the existing pharmacological therapy, in conjunction with revisiting health behaviours and re-referral to DSMES. However, agents that cause hypoglycaemia in themselves, such as sulfonylureas, should be discontinued once insulin is started. Technologies allowing continuous monitoring of glucose levels without finger sticking have clear advantages in those on insulin. Other support tools and systems such as apps guiding insulin dose adaptation or phone-based guidance can also be helpful.
In specific circumstances, insulin may be the preferred agent for glucose lowering, specifically in the setting of severe hyperglycaemia (HbA 1c >86 mmol/mol [>10%]), particularly when associated with weight loss or ketonuria/ketosis and with acute glycaemic dysregulation (e.g. during hospitalisation, surgery or acute illness), in underweight people or when the diagnosis of type 1 diabetes is suspected.
If affordable, basal insulin analogue formulations are preferred to NPH insulin because of their reduced risk of hypoglycaemia, particularly nocturnal hypoglycaemia, when titrated to the same fasting glucose target [ 327 ]. Basal insulins are typically administered before bedtime but, with newer analogues, more flexibility in the timing of insulin injection is possible (i.e. any time of the day).
In some, as the disease progresses, despite titration of the basal insulin to correct fasting hyperglycaemia (typically more than 0.5 U/kg), mealtime insulin may have to be added to meet glycaemic targets, particularly postprandial glucose [ 328 ]. Mealtime insulin may be required to enhance postprandial blood glucose levels and achieve HbA 1c targets. Therapeutic inertia in intensification of insulin therapy should be avoided and, when clinicians are not familiar with multiple daily injection therapy, referral to specialist care and/or DSMES is warranted. A straightforward way to introduce mealtime insulin is to start with a short- or rapid-acting insulin injection before the meal associated with the largest glucose excursion. Adding mealtime rapid-acting insulin requires increased DSMES and self-monitoring of glucose levels and adds complexity and cost to the therapy. In contrast to basal insulin analogues, the evidence supporting the choice of mealtime rapid-acting insulin analogues is less clear [ 329 ]. Another simpler and still popular way of combining mealtime and basal insulin components is using premixed insulins. Insulin analogue-based combinations have the advantage of resulting in fewer hypoglycaemic events and weight gain than are typically observed with human premixed insulin [ 330 ].
Finally, it needs to be re-emphasised that, in all insulin-treated people with type 2 diabetes, agents associated with cardiorenal protection or weight reduction should be kept in the treatment regimen whenever possible [ 331 ]. The combination of a basal insulin analogue and GLP-1 RA in one injection may be a simple way to reduce the burden and complexity of treatment [ 332 ].
Practical tips for clinicians (Supplementary Fig. 3 )
- The use of a GLP-1 RA should be considered prior to initiation of insulin.
- When initiating insulin, start with a basal insulin and intensify the dose in a timely fashion, titrating to achieve an individualised fasting glycaemic target set for every person.
- When insulin is initiated, continue organ-protective glucose-lowering medications and metformin.
- Refer for DSMES when initiating insulin or advancing to basal–bolus therapy.
Place of technology
The use of technology in the therapy of people with type 2 diabetes is increasing through a broad range of approaches, for example telehealth, remote monitoring systems, CGM and behavioural aids to support physical activity, meal planning and monitoring, medication-taking behaviour, mindfulness and stress management. Evidence on the impact of these systems is variable and highly dependent on the embedding of the technology in a more comprehensive approach. Evidence for a beneficial impact of telehealth on achieving treatment goals in those living with type 2 diabetes is growing [ 333 , 334 ]. During the COVID-19 pandemic, telehealth has proven to be an efficient way of overseeing the treatment of people with type 2 diabetes. In particular, interventions using apps as tools to support DSMES have been shown to have an impact on outcomes [ 34 ].
For those needing insulin as part of their treatment, smart insulin pens and insulin pumps (continuous subcutaneous insulin infusion [CSII]) are available. Specific evidence on the benefit of smart pens in people with type 2 diabetes is still scarce. CSII use is associated with small improvements in HbA 1c and fewer hypoglycaemic events, suggesting that CSII can be considered in people living with type 2 diabetes treated with multiple daily insulin injections and able to manage the device [ 71 ]. Again, for optimal effect, this technology should be embedded in an integrated approach to type 2 diabetes therapy, specifically to avoid weight gain [ 335 ].
In individuals with type 2 diabetes treated with insulin, CGM, both intermittently scanned CGM and real-time CGM, has gained traction, with evidence that CGM results in better overall glucose control as defined by HbA 1c and time in range (3.9–10.0 mmol/l [70–180 mg/dl]), fewer hyperglycaemic and hypoglycaemic episodes and improvements in diabetes distress [ 336 , 337 ].
As with other wearables, for example those collecting steps walked or monitoring dietary intake, medication dose administered or sleep quality, use of CGM has also been proposed as a motivational tool for those with type 2 diabetes not on insulin therapy, but the evidence on this is modest [ 337 ].
Finally, to date, no convincing evidence is available on the use of hybrid closed loop systems specifically in people with type 2 diabetes.
- Technology can be useful in people with type 2 diabetes but needs to be part of an holistic plan of care and supported by DSMES.
- Consider CGM in people with type 2 diabetes on insulin.
- Adapt the clinic/system to optimise effective use of technology among people with type 2 diabetes, particularly to support behaviour change through self-monitoring.
Working within the system to deliver improved care
We are fortunate to have evidence on numerous effective interventions in type 2 diabetes, but translating this evidence into practice cannot rest only with front-line clinicians during individual clinic visits. The systems of care that support front-line clinicians have a significant role in improving diabetes clinical management, outcomes and experience for people living with diabetes. Front-line clinicians must inform and drive the design of care, but the systems of care should be held accountable for implementation. Supplementary Table 2 , informed by the Effective Practice and Organisation of Care (EPOC) taxonomy [ 338 ], outlines key domains and questions that must be answered to achieve the goal of better care and outcomes for people living with type 2 diabetes. All levels of the care delivery system have a role and responsibility in improving diabetes management. Clinic leaders have a responsibility to improve workflows to make it easy to provide evidence-based care and provide data to inform quality improvement efforts. Continuing education is necessary to ensure evolving evidence reaches people living with type 2 diabetes. Policy makers have a responsibility to ensure that evidence-based interventions are available and affordable to all. Interventions to improve diabetes must also include the health system (including the microsystems within a system) and governmental agencies. Policy makers, together with all stakeholders, should reflect on care delivery: How, where and by whom is care delivered? Who coordinates care and the management of care processes? Practices and systems must establish enhanced communication technology to improve engagement. Governance arrangements must be implemented specifically around accountability for health professionals, with a focus on training and evaluation of quality of practice. Finally, reflection is needed around implementation strategies at the level of the system, facility and individual healthcare workers. These principles are aligned with recommendations outlined in the recent Lancet Commission on diabetes [ 339 ].
- Identify and incorporate continuing education activities on the management of type 2 diabetes for all members of the healthcare team.
- Team-based care is required for integrated care of diabetes; this includes coordination between multiple disciplines (diabetes care and education specialist, dietitians, psychologists, etc.) and often other medical specialties (primary care, endocrinology, ophthalmology, nephrology, etc.).
- Management of type 2 diabetes requires continuous quality improvement interventions tailored to the local setting.
Key knowledge gaps and a call to action
In this 100th year since the discovery and partial purification of insulin, we should remember the remarkable speed at which this first glucose-lowering medication was developed and distributed as life-saving therapy for people with diabetes. Through our experience in the last few years with the COVID-19 pandemic, we have demonstrated how quickly many governments, industry, healthcare systems and academic institutions can respond to global healthcare crises. Within a year of identification of the SARS-CoV-2 virus, preventive and therapeutic products were not only developed and tested but also administered on a massive scale. The annual global mortality rate directly attributable to diabetes is approximately 1.5 million people, with 540 million people affected [ 340 , 341 ]. Although not as spectacular as the impact of COVID-19 on the health of society, diabetes is sure and steady in its burden, increasing in prevalence and with an increase in mortality and morbidity over time.
Two centuries of investigation into the pathophysiology of diabetes have led to the extraordinary advances in treatment of the last two decades. As reviewed in this consensus report, encouraging healthy behaviours, DSMES, medications, devices, technologies and organisation of care all represent effective tools for the management of diabetes to reduce its morbidity and mortality. However, despite the generous approach of Banting and Best in licensing the patent for insulin for one Canadian dollar, it is not yet readily available to all people with diabetes [ 342 , 343 ]. Recent events have focused attention on the contribution of social determinants of health and a lack of equity in the delivery of care to disparate and unfavourable outcomes. Today, the major opportunities to improve diabetes outcomes in the near term come from more effective implementation of best evidence through organisation of care at all levels (national to individual practices) and from addressing social determinants of health. Every reader of this consensus report has a role to play in better implementation with a focus on equity. For providers, that could involve a focus on shared decision making to improve adherence to behavioural and medication interventions as well as organising practice to minimise therapeutic inertia and enhance engagement and support for all people with diabetes. For policy makers, healthcare systems, payors and companies with marketed products or services, ensuring equitable access to minimise health disparities should be a priority.
Broad support for basic science is necessary to bring about the next generation of interventions. Implementation science is an essential area for future work, particularly in the context of ‘learning healthcare systems’, in which internal data are systematically integrated with published evidence to drive quality improvement [ 344 – 346 ]. Precision medicine initiatives, whether ‘omics’-based or focused on social determinants of health, aim to optimally target interventions based on the wide heterogeneity of the population affected by diabetes. Precision medicine has tremendous but largely unrealised promise. When these efforts are driven by real-world data, causal inference study design and analysis create greater confidence in the implementation and evaluation of insights. Studies should be conducted to support the better understanding of precision medicine approaches to the full spectrum of diabetes interventions, from medications to behavioural treatments and diabetes support.
Several key areas where further research could better inform future consensus reports were of particular interest to the writing group. For each area, one could add the need for more precision medicine insights and a better understanding of the full spectrum of investigations that are supporting efforts to advance the field from basic to implementation science. With upwards of 10% of the population affected by diabetes and the enormous attendant costs, a focus on individualising care to make sure that the right person is getting the right therapy at the right time while working to overcome barriers dependent on social determinants of health is essential. Regulatory reform, more efficient study conduct and analysis, coordinated global efforts in defining outcomes and data collection instruments, data sharing, exploration of new forms of healthcare delivery (e.g. telehealth) and increased efforts to reach underserved populations, as were made to address COVID-19, would accelerate progress in defining and implementing optimal approaches for diabetes care.
- Study conduct. Across the spectrum from highly controlled trials to observational studies, paying greater attention to subgroups, in particular vulnerable populations, is essential. Dedicated studies in young adults with type 2 diabetes, or including much larger numbers of younger adults in broader studies, are essential to better understand how to mitigate their high risk of early disability. As more younger adults are being treated with therapies that have been inadequately studied in pregnancy, it is essential to describe the reproductive safety of recommended approaches. Similarly, there have been inadequate studies of frail older people and those aged >75 years with regard to understanding both appropriate targets and interventions, to minimise harms and maximise quality of life. Sex balance is another dimension where our present studies fail to be representative. Better recruitment, retention and analysis to ensure safety and effectiveness in populations historically under-represented in studies and generally suffering from health inequities is a minimal first step to enhance health justice by sex, race/ethnicity and nationality, etc.
- Weight management. With the emergence of more effective behavioural and medical therapies and novel surgical approaches for the treatment of people who are overweight with diabetes, more direct comparisons are required to better target interventions based on impact and cost-effectiveness.
- Targets. Studies designed to explicitly examine glucose-centric vs weight-centric approaches to diabetes management are needed. The impact of prioritising early aggressive therapy to induce remission is unclear.
- Cardiorenal protection. Data are required to better inform when to select a GLP-1 RA and/or an SGLT2i in the setting of CVD but without HF or CKD, and to fully validate the recommendation for combination therapy in those at high risk who do not meet glycaemic targets. As discussed, there is considerable uncertainty about the absolute benefits of GLP-1 RA and SGLT2i for CVD outcomes in those with risk factors only. As a result, there is variability in the recommendations on how to define high-risk people with diabetes, to whom these disease-modifying agents should be prescribed to have the greatest benefit/impact. As all people with diabetes are at high risk of CVD, HF and CKD over time, real-world evidence and cost-effectiveness studies of GLP-1 RA and SGLT2i in broad populations would help to better target interventions to have the greatest impact on outcomes.
- Glucose monitoring. Further studies to understand the role and optimal implementation of CGM and/or episodic CGM in type 2 diabetes are needed.
- Comorbidities. There are numerous studies under way to understand the role of interventions in the setting of NAFLD and cognitive impairment. NAFLD is highly prevalent and thus understanding the impact of interventions on person-centred outcomes and costs is essential. Cognitive impairment is a major burden to people with diabetes, their families and society; better understanding of the pathophysiology and the impact of interventions is a challenging but high reward area for investigation. There are virtually no data to inform best practice in the care of people with diabetes and advanced CKD, particularly in dialysis-dependent kidney disease. Additional studies, particularly of GLP-1 RA, GIP and GLP-1 RA, and SGLT2i, will hopefully provide new avenues to reduce mortality in this population, in which there are enormous health disparities.
- Screening and prevention. Screening for diabetes and its complications and comorbidities remains inadequate. Early intervention to prevent progression is also generally suboptimal. National healthcare systems should comprehensively assess the implementation of recommendations and create incentives for effective programmes. To optimally target resources, additional studies may be required on natural history and subpopulations, as much of the rationale for screening is based on studies conducted decades ago.
- Technology. Remote care, wearables, apps and decision support aids have exploded in availability and clear rationale exists as to why they may be of benefit. However, their optimal application is poorly understood.
- Sleep and chronotype. Poor sleep is common and clearly associated with poor outcomes. Further studies are needed to understand behavioural sleep therapy and its benefits more fully, as well as the benefits of medication and device aids. As chronotype is potentially modifiable, future research should focus on social and lifestyle factors to optimise interventional responses.
Until science and medicine bring us further insights, we recommend empathic, person-centred decision making and support informed by an understanding of local resources and individual social determinants of health. Combined with consistent efforts to improve health behaviours (nutrition, activity, sleep and self-monitoring) and to provide DSMES, these form the foundation of diabetes management. In this context, acceptance of, adherence to and persistence with medical and behavioural interventions to support cardiorenal health, cardiovascular risk reduction and attainment of glycaemic and weight goals will prevent complications and optimise quality of life. We must establish and refine quality improvement efforts in diabetes care at the local level to equitably implement evidence-based interventions for the benefit of all people with type 2 diabetes.
(PDF 246 kb)
Acknowledgements
F. Zaccardi performed the literature searches and M. Bonar, C. Franklin and S. Jamal assisted with the conception and execution of figures and tables. T. Yates and J. Henson supported the production and content of Fig. Fig.2 2 (all from Leicester Diabetes Centre, University of Leicester and the University Hospitals of Leicester NHS Trust). T. Karagiannis (Clinical Research and Evidence-Based Medicine Unit, Aristotle University of Thessaloniki, Greece) assisted in the credibility assessment and interpretation of meta-analyses evaluating the effects of glucose-lowering medications across subgroup populations and contributed in applying GRADE guidance in the formulation of respective practice recommendations. D. Bradley (Ohio State University College of Medicine, Columbus, OH), P. Home (Newcastle University, Newcastle, UK), M. S. Kirkman (University of North Carolina, Chapel Hill, NC), S. Dinneen (Galway University Hospitals, Galway, Ireland), H. W. Rodbard (Adventis HealthCare Shady Grove Medical Center, Rockville, MD), G. Sesti (Sapienza University of Rome, Rome, Italy), P. Newland-Jones (University of Southampton, Southampton, UK), E. Montanya (University of Barcelona, Barcelona, Spain) and M. Nauck (Medical Department I, St. Josef-Hospital [Ruhr-University Bochum], Bochum, Germany) all served as invited reviewers. We acknowledge the support of N.A. El Sayed, R. R. Bannuru, M. Saraco and M. I. Hill (all ADA, Arlington, VA, USA), P. Niemann and N. Buckley-Mühge (all EASD, Dusseldorf, Germany), the Committee for Clinical Affairs of the EASD and the Professional Practice Committee of the ADA.
Authors’ relationships and activities
MJD has acted as a consultant, advisory board member and speaker for Boehringer Ingelheim, Eli Lilly, Novo Nordisk and Sanofi; an advisory board member and speaker for AstraZeneca; an advisory board member for Janssen, Lexicon, Pfizer and ShouTi Pharma; and as a speaker for Napp Pharmaceuticals, Novartis and Takeda Pharmaceuticals International. Her institution has received grants from Novo Nordisk, Sanofi-Aventis, Eli Lilly, Boehringer Ingelheim, AstraZeneca and Janssen. VRA has served as a consultant for Applied Therapeutics, Duke, Fractyl, Novo Nordisk, Pfizer and Sanofi. VRA’s spouse is an employee of Janssen and a former employee of Merck. VRA’s employer institution has received research funding for her role as investigator on clinical trials from Applied Therapeutics, Medpace, Eli Lilly, Fractyl, Premier, Novo Nordisk and Sanofi. BSC is a nominating work group member of the American Academy of Physician Assistants. RAG is an advisor to Vida and Lark. JG is a consultant for AstraZeneca, Pfizer, Boehringer Ingelheim/Lilly, Bayer, Sanofi, Anji, Vertex/ICON and Valo. She conducts research at her institution for Boehringer Ingelheim/Lilly, Merck and Roche. NMM is under a licence agreement between Johns Hopkins HealthCare Solutions and Johns Hopkins University. She and the university are entitled to royalty distributions related to an online diabetes prevention programme. SER participated in at least one advisory board for Bayer, Traverse and AstraZeneca. Her employer receives industry research support from Bayer and Astra Zeneca. SDP is a member of the advisory board for Abbott, Applied Therapeutics, AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, Hengrui Pharmaceuticals, Menarini International, Novo Nordisk, Sanofi and Vertex. He is a participant in a speaker’s bureau for AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, Novo Nordisk, Sanofi and Takeda. His employer receives research funding from AstraZeneca and Boheringer Ingelheim. CM serves or has served on the advisory panel for Novo Nordisk, Sanofi, MSD, Eli Lilly, Novartis, AstraZeneca, Boehringer Ingelheim, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Insulet and Zealand Pharma. Financial compensation for these activities has been received by KU Leuven. KU Leuven has received research support for CM from Medtronic, Novo Nordisk, Sanofi and ActoBio Therapeutics. CM serves or has served on the speaker’s bureau for Novo Nordisk, Sanofi, Eli Lilly, Boehringer Ingelheim, AstraZeneca and Novartis. Financial compensation for these activities has been received by KU Leuven. GM is a consultant to Novo Nordisk, Fractyl, Recor, Keyron and Metadeq and is on the scientific board of Fractyl. PR’s institution has received industry research funding from AstraZeneca and Novo Nordisk. Her institution has also received consultancy fees from AstraZeneca, Bayer, Boehringer Ingelheim, Novo Nordisk, Gilead and MSD, and lecture fees from Sanofi, Astellas, Novo Nordisk, Bayer and AstraZeneca. TT is on the advisory board for Boehringer Ingelheim, AstraZeneca, Sanofi, Novo Nordisk and Eli Lilly, and in the speaker’s bureau for Boehringer Ingelheim, AstraZeneca, Sanofi, Novo Nordisk, Eli Lilly, MSD, Servier and Merck. AT has served on the advisory board for Novo Nordisk and Boehringer Ingelheim and his university has received research funding. His university also receives funding for educational and research support from Eli Lilly. JBB is a paid consultant to Anji Pharmaceuticals, Boehringer Ingelheim, Eli Lilly, Fortress Biotech, Janssen, Mellitus Health, Moderna, Pendulum Therapeutics, Praetego, ReachMD, Stability Health and Zealand Pharma. He is a member of the advisory board for Boehringer Ingelheim, Eli Lilly, Mellitus Health, Moderna, Novo Nordisk, Pendulum Therapeutics, Praetego, Stability Health, vTv Therapeutics and Zealand Pharma. His employer receives research funding from Dexcom, Eli Lilly, NovaTarg, Novo Nordisk, Sanofi, Tolerion and vTv Therapeutics. He is an investor in Mellitus Health, Pendulum Therapeutics and PhaseBio.
Contribution statement
All authors were responsible for drafting the article and revising it critically for important intellectual content. All authors approved the version to be published.
Abbreviations
This activity was funded by the American Diabetes Association and the European Association for the Study of Diabetes.
Data availability
This article is being simultaneously published in Diabetologia (10.1007/s00125-022-05787-2) and Diabetes Care (10.2337/dci22-0034) by the European Association for the Study of Diabetes and American Diabetes Association.
A consensus report of a particular topic contains a comprehensive examination and is authored by an expert panel and represents the panel’s collective analysis, evaluation and opinion. MJD and JBB were co-chairs for the Consensus Report Writing Group. VRA, BSC, RAG, JG, NMM and SER were the writing group members for ADA. SDP, CM, GM, PR, TT and AT were the writing group members for EASD. The article was reviewed for EASD by its Committee on Clinical Affairs and approved by its Executive Board. The article was reviewed for ADA by its Professional Practice Committee.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Melanie J. Davies, Email: [email protected] .
John B. Buse, Email: ude.cnu.dem@esubj .
Articles on 2022
Displaying all articles.

NASA’s busiest year in decades – an astronomer sums up the dizzying array of missions in 2022
Chris Impey , University of Arizona

2022’s billion-dollar disasters: Climate change helped make it US’s 3rd most expensive year on record
Stacy Morford , The Conversation

Crime is on the ballot – and voters are choosing whether prosecutors with reform agendas are the ones who can best bring law, order and justice
Jessica S. Henry , Montclair State University

Fear of COVID-19 and fear of change are dangerously intertwined for 2022
Eli Sopow , University Canada West

The cost-of -living crisis will put more pressure on shoppers than COVID
Kokho Jason Sit , University of Portsmouth

Learn time management to make those New Year’s resolutions stick
Brad Aeon , Université du Québec à Montréal (UQAM)

Got health goals? Research-based tips for adopting and sticking to new healthy lifestyle behaviours
Ryan Rhodes , University of Victoria

Plant-based doesn’t always mean healthy
Meghan McGee , University of Toronto

Here are some of the political events that will dominate headlines in 2022
Thomas Klassen , York University, Canada

After a big year for cryptocurrencies, what’s on the horizon in 2022?
Erica Pimentel , Queen's University, Ontario ; Bertrand Malsch , Queen's University, Ontario , and Nathaniel Loh , Queen's University, Ontario
Related Topics
- Climate change
- Coronavirus
- Holidays 2021
- New Year's resolutions
- Resolutions
Top contributors
University Distinguished Professor of Astronomy, University of Arizona
Professor, Department of Justice Studies, Montclair State University
Senior Lecturer in Marketing; Associate Head (Global), University of Portsmouth
Professor of Geology and Environmental Geosciences, University of Dayton
Assistant Professor, Smith School of Business, Queen's University, Ontario
Professor, School of Public Policy and Administration, York University, Canada
Professor of Climate Science, UMass Lowell
Assistant Professor, Time Management Researcher, Université du Québec à Montréal (UQAM)
Associate Professor of Accounting, Smith School of Business, Queen's University, Ontario
Junior Fellow of the CPA Ontario Centre for Corporate Reporting and Professionalism, Queen's University, Ontario
Nutrition Scientist, Dalla Lana Fellow, University of Toronto
Professor, Health Psychology, University of Victoria
Associate Professor, MBA Faculty of Leadership & People Management, University Canada West
Lamont Research Professor of Ocean and Climate Physics, Columbia University
Assistant Professor of Earth Sciences, University of Memphis
- X (Twitter)
- Unfollow topic Follow topic
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
11 Trends that Will Shape Work in 2022 and Beyond
- Brian Kropp
- Emily Rose McRae

After two years of disruption, volatility will only continue to increase.
We’ve been living through the greatest workplace disruption in generations and the level of volatility will not slow down in 2022. New Covid variants will continue to emerge and may cause workplaces to temporarily go remote again. Hybrid work will create more unevenness around where, when, and how much different employees are working. Many employees will be greeted with real wage cuts as annual compensation increases fall behind inflation. These realities will be layered on top of longer-term technological transformation, continued DE&I journeys, and ongoing political disruption and uncertainty.
At the start of 2021, many of us expected the world to return to normalcy. Vaccines were starting to roll out, and many executives felt like it would be a matter of a few short months before we would all return to the workplace .
- Brian Kropp is chief of research for the Gartner HR practice, which delivers insights and solutions that address new and emerging executive challenges and enable HR leaders to take decisive actions. Brian’s expertise spans all aspects of HR, including talent acquisition and management, employee experience, change management, and leadership.
- Emily Rose McRae is a senior director analyst covering the future of work and workforce transformation, and she leads the talent research initiative for executive leaders. Emily Rose works across all issues related to the future of work, including emerging technologies and their impact on work and the workforce, new employment models, and creating an enterprise-wide future of work strategy.
Partner Center

ROLAND GRAD, MD, MSc, AND MARK H. EBELL, MD, MS
Am Fam Physician. 2023;107(4):406-414
Author disclosure: Dr. Ebell is cofounder and editor-in-chief of Essential Evidence Plus; see Editor's Note . Dr. Grad has no relevant financial relationships.
This article summarizes the top 20 research studies of 2022 identified as POEMs (patient-oriented evidence that matters), excluding COVID-19. Statins for primary prevention of cardiovascular disease produce only a small absolute reduction in a person's likelihood of dying (0.6%), having a myocardial infarction (0.7%), or having a stroke (0.3%) over three to six years. Supplemental vitamin D does not reduce the risk of a fragility fracture, even in people with low baseline vitamin D levels or a previous fracture. Selective serotonin reuptake inhibitors are preferred medical therapy for panic disorder, and patients who discontinue antidepressants are more likely to relapse (number needed to harm = 6) compared with those who continue. Combination therapy using a selective serotonin reuptake inhibitor, serotonin-norepinephrine reuptake inhibitor, or tricyclic antidepressant with mirtazapine or trazodone is more effective than monotherapy for first-line treatment of acute severe depression and when monotherapy fails. Using hypnotic agents for insomnia in adults comes with a significant trade-off between effectiveness and tolerability. In patients with moderate to severe asthma, using a combination of albuterol and glucocorticoid inhalers as rescue therapy reduces exacerbations and need for systemic steroids. Observational research shows an increased risk of gastric cancer in patients taking proton pump inhibitors (number needed to harm = 1,191 over 10 years). The American College of Gastroenterology updated its guideline for gastroesophageal reflux disease, and a new guideline provides sound advice for the evaluation and management of irritable bowel syndrome. Adults older than 60 years with prediabetes are more likely to become normoglycemic than to develop diabetes mellitus or die. Treatment of prediabetes via intensive lifestyle intervention or metformin has no impact on long-term cardiovascular outcomes. Persons with painful diabetic peripheral neuropathy have similar degrees of improvement with monotherapy using amitriptyline, duloxetine, or pregabalin and greater improvement with combination therapy. When communicating with patients about disease risk, most patients prefer numbers over words because people overestimate word-based probabilities. In terms of drug therapy, the duration of an initial varenicline prescription should be 12 weeks. Many drugs can interact with cannabidiol. No important difference was found among ibuprofen, ketorolac, and diclofenac for treatment of acute nonradicular low back pain in adults.
For the past 24 years, a team of six clinicians has systematically reviewed more than 100 medical journals to find the research most likely to change and improve primary care practice. The team includes experts in family medicine, pharmacology, hospital medicine, and women's health. 1 , 2
The goal of this process is to identify POEMs (patient-oriented evidence that matters). A POEM must report at least one patient-oriented outcome, such as improvement in symptoms, morbidity, or mortality. It should also be free of important methodologic bias, making the results valid and trustworthy. Finally, if applied in practice, the results would change what some physicians do by adopting a new practice or discontinuing an old one shown to be ineffective or harmful. Of more than 20,000 research studies published in 2022 in the journals reviewed by the POEMs team, 253 met criteria for validity, relevance, and practice change. These POEMs are emailed daily to subscribers of Essential Evidence Plus (Wiley-Blackwell, Inc.).
The Canadian Medical Association purchases a POEMs subscription, and thousands of its members receive the daily POEM. These physicians can rate each one using a validated questionnaire. 3 This process is called the Information Assessment Method ( https://www.mcgill.ca/iam ). POEM ratings address the domains of clinical relevance, cognitive impact, use in practice, and expected health benefits. In 2022, each of the 253 daily POEMs were rated by an average of 1,087 physicians. New for 2022, readers of the daily POEM saw an “overuse alert” for POEMs that align with a Choosing Wisely recommendation. 4
In this article, the 12th installment of our annual series ( https://www.aafp.org/pubs/afp/content/top-poems.html ), we summarize the 20 most clinically relevant POEMs of 2022 as determined by Canadian Medical Association members. Although some of the most highly rated POEMs addressed COVID-19, rapid changes in management as the pandemic has evolved make many of them less relevant in 2023. Therefore, we briefly summarize these COVID-19 POEMs, as well as highly rated practice guidelines, separately. The full POEMs discussed in this review are available at https://www.aafp.org/pubs/afp/content/top-poems/2022.html .
Preventive Health Care
The first two POEMs relate to preventive medicine ( Table 1 ) . 5 , 6 Many patients take statins to reduce cardiovascular events. But how large is the benefit? A meta-analysis identified 19 studies that randomized 132,763 patients to statin therapy or placebo. 5 Studies were typically three to six years in duration, and statins reduced the risk of overall death by 0.8%, myocardial infarction by 1.3%, and stroke by 0.4%. When statins were used as primary prevention, the reductions were smaller: 0.6% fewer deaths, 0.7% fewer myocardial infarctions, and 0.3% fewer strokes, for an overall number needed to treat of 63 to prevent one event over three to six years. The 95% CI around all-cause mortality alone was 88 to 250 over several years of treatment as primary prevention. Not bad, but this is probably a higher number needed to treat than most of our patients believe.
Screening for low vitamin D levels and recommending replacement in those who are deficient have become popular, although the U.S. Preventive Services Task Force (USPSTF) found insufficient evidence to recommend screening in asymptomatic individuals. 7 A trial randomized 25,871 men 50 years or older and women 55 years or older to receive 2,000 IU of vitamin D or placebo daily for a median of five years. 6 There was no difference between groups in any type of fracture, even in patients with low baseline vitamin D levels (hazard ratio = 1.04; 95% CI, 0.80 to 1.36) or a previous fracture.
Behavioral Health
The first POEM in this group provides insight into what happens when a patient discontinues an antidepressant 8 ( Table 2 8 – 13 ) . The study included primary care patients with at least two episodes of depression who had been taking an antidepressant for at least two years. 8 Patients were randomized to continue the medication or taper it over two months to placebo. After one year, the likelihood of relapse was significantly higher in the discontinuation group (56% vs. 39%; hazard ratio = 2.1; 95% CI, 1.6 to 2.7). Symptoms in the discontinuation group were also more severe.
The next study looked at the best way to treat these patients with acute severe depression. It showed that combination therapy is better than monotherapy for first-line treatment and in patients who do not respond to initial monotherapy (standardized mean difference [SMD] = 0.31; 95% CI, 0.19 to 0.44). 9 An SMD of 0.31 is consistent with a small effect size. The combination of a monoamine reuptake inhibitor (selective serotonin reuptake inhibitor [SSRI], serotonin-norepinephrine reuptake inhibitor, or tricyclic antidepressant) with mirtazapine or trazodone is more effective than monotherapy for first-line treatment and for patients who do not respond to monotherapy.
Turning to anxiety disorders, a network meta-analysis of 87 randomized controlled trials with 12,800 participants evaluated 12 drug classes to treat panic disorder. 10 Only one trial was at low risk of bias, and most trials were no more than three months in duration. The meta-analysis found that the most effective drugs were benzodiazepines, tricyclic antidepressants, and SSRIs, with SSRIs having the least risk of adverse effects. Sertraline and escitalopram have the best balance of high remission rates and low risk of adverse events. But remember, other studies have found that cognitive behavior therapy and mindfulness-based therapies are likely to be as effective as medications. 14 , 15
Finally, a network meta-analysis identified 154 double-blind randomized controlled trials that compared a broad range of hypnotic agents with each other and placebo for the treatment of insomnia. 11 There were 20 individual drugs and drug classes, including benzodiazepines, melatonin, trazodone, and newer short-acting hypnotics such as eszopiclone (Lunesta) and lemborexant (Dayvigo). The drugs most likely to be effective were eszopiclone and lemborexant in the long-term and eszopiclone, lemborexant, benzodiazepines, seltorexant (undergoing clinical trials in the United States), trazodone, trimipramine, zopiclone (not available in the United States), and zolpidem in the short-term. However, all drugs had relatively high rates of adverse effects (although so did placebo). The authors concluded that eszopiclone and lemborexant provide the best balance of effectiveness and tolerability in the short- and long-term.
One POEM reported on a study of 3,132 children and adults with moderate to severe asthma who were taking long-term inhaled corticosteroids and had experienced a severe asthma exacerbation in the previous year 16 ( Table 3 16 , 17 ) . They were randomized to two puffs each of albuterol, 90 mcg, plus budesonide, 80 mcg; albuterol, 90 mcg, plus budesonide, or albuterol alone as a rescue inhaler. In the higher-dose budesonide group, there was about 1 fewer exacerbation per 7 patients treated for one year compared with the albuterol only group, and patients also took significantly fewer systemic steroids (84 mg vs. 130 mg per year).
The second POEM in this group adds to the same evidence base as the first but in a more diverse population. Asthma disproportionately affects Black and Latinx patients, yet these groups have been underrepresented in research. This study randomized 1,201 self-identified Black and Latinx adults with moderate to severe asthma to a short-acting beta agonist (SABA) inhaler alone as reliever therapy or to a SABA plus a puff of a beclomethasone, 80 mcg, inhaler for every puff of the SABA. 17 There was approximately 1 fewer asthma exacerbation for every 8 patients in the combined therapy group compared with SABA alone over one year. Asthma control scores also improved, but the change was not clinically significant. Minority representation in studies is critical to addressing health disparities. 18
Gastroenterology
The first of three POEMs on gastroenterology topics ( Table 4 19 – 22 ) summarized an observational study of the following question: Is there an association between gastric cancer and the use of proton pump inhibitors (PPIs)? Answer: Patients taking PPIs have a small increased risk of gastric cancer (number needed to harm = 1,191 over 10 years). 19 But, remember, association is not causation. That said, physicians initiating antacid therapy should begin with a histamine H 2 blocker. If physicians are prescribing a PPI, the lowest dose and duration possible should be used. Choosing Wisely Canada provides a toolkit for helping to deprescribe PPIs (available at https://choosingwiselycanada.org/toolkit/bye-bye-ppi ).
How should clinicians evaluate and manage patients with suspected gastroesophageal reflux disease? The American College of Gastroenterology guideline panel recognizes that some patients require long-term PPI therapy, and the benefits outweigh the theoretical risks in these patients. In patients who are treatment naive and have classic symptoms and no alarm symptoms, clinicians should attempt to discontinue PPIs after a successful eight-week trial. Therefore, initial prescriptions should generally be limited to a duration of eight weeks. 21
Informed by systematic reviews, the British Society of Gastroenterology published updated recommendations for the diagnosis of irritable bowel syndrome (defined as at least six months of abdominal pain or discomfort and altered bowel habits). 22 Colonoscopy is recommended only for patients with alarm signs and symptoms or those at risk of microscopic colitis. First-line therapy includes exercise and gradually increasing doses of soluble fiber (e.g., psyllium). Recommendations for other first- and second-line treatments are summarized in the POEM.
Prediabetes/Diabetes Mellitus
The natural history of prediabetes in adults older than 60 years is the topic of the first POEM in this category ( Table 5 23 – 26 ) . This English study included more than 2,000 adults without diabetes mellitus at baseline. 23 The average age of participants was 70.6 years, and 55% were women. Over eight years of follow-up, older people with prediabetes were more likely to become normoglycemic than to develop diabetes or die. Perhaps it is time to retire the term “prediabetes” when talking with older people.
The next POEM reports on the long-term cardiovascular outcomes for participants in the original Diabetes Prevention Program trial. 24 In this trial, participants were randomized to receive metformin, 850 mg twice daily; an intensive exercise program; or placebo, and were then followed for three years. At the conclusion of the study, all patients were invited to participate in a long-term open-label follow-up study, and 86% agreed. The bottom line: In patients with prediabetes, neither an intensive lifestyle intervention nor metformin had an impact on the long-term risk of cardiovascular outcomes.
In the nursing home setting, a cohort of 42 older adults with type 2 diabetes were evaluated for the frequency and persistence of hypoglycemia. All participants were taking medications capable of inducing hypoglycemia (e.g., sulfonylureas, repaglinide, insulin). The study showed that seven people (17%) spent more than 20% of an entire day in a hypoglycemic state. Severe hypoglycemia occurred in 19 people (45%). A lower A1C level was associated with more frequent events and a longer time spent in a hypoglycemic state. 25 We should allow A1C results to be higher in frail older patients.
The last POEM in this group summarized the findings of a crossover trial that compared three drugs for decreasing pain in adults with diabetic peripheral neuropathy. 26 Similar degrees of improvement were reported with monotherapy using amitriptyline, duloxetine (Cymbalta), or pregabalin (Lyrica). Greater improvement was reported with subsequent combination therapy, regardless of initial choice of medication. This POEM included a table summarizing the adverse effects associated with three combinations of these drugs. Dizziness was more common with duloxetine plus pregabalin, nausea with pregabalin plus amitriptyline, and dry mouth with amitriptyline plus pregabalin.
Miscellaneous
Five top POEMs do not fall easily into a single category ( Table 6 27 – 31 ) . With regard to health information, understanding should clearly precede decision-making. However, when we say “rare” or “high risk,” what are we implying, and what do these terms mean to patients? A systematic review of 33 studies found significant variability in the presentation of probabilities and their subsequent interpretation by patients. This POEM also showed that most patients prefer numbers rather than word-based estimates of risk. 27
The next POEM was a randomized trial evaluating whether extending varenicline (Chantix) treatment beyond 12 weeks is beneficial for increasing the likelihood of smoking cessation. At 52 weeks of follow-up, there was no difference in quit rates between those taking varenicline for 12 weeks vs. 24 weeks. 28 Also, combining varenicline with nicotine replacement therapy produced no additional benefit. Therefore, initial varenicline prescriptions should specify a duration of 12 weeks. Using varenicline for longer than 12 weeks may be appropriate for a select group of patients who want a longer treatment course. 32
Drug interactions between cannabidiol (CBD) and commonly used medications is the topic of the next POEM. This study showed that CBD may increase serum levels of SSRIs, tricyclic antidepressants, antipsychotics, beta blockers, and opioids. 29 CBD increases levels of lamotrigine, but other anti-convulsants decrease levels of CBD. Although this reminds us of the potential for drug-drug interactions with CBD, we also need to know more about the severity of these interactions for better clinical decision-making.
The next POEM addresses the treatment of acute nonradicular low back pain. A randomized controlled trial of 198 adults 18 to 65 years of age presenting to the emergency department found no difference among ibuprofen, ketorolac, and diclofenac for the outcome of clinical improvement at five days. 30 Thus, although some nonsteroidal anti-inflammatory drugs may have a reputation of being a better analgesic, there seems to be a class effect with these drugs.
Our final top POEM identified the best topical therapy for mild to moderate acne vulgaris. The authors of this network meta-analysis of randomized controlled trials began by asking patients what was most important to them in terms of the outcome of acne treatment. Thus, the primary outcomes of this study were effectiveness, the proportion of patients who reported at least moderate improvement, tolerability, and the proportion who withdrew from the study or stopped using the medication due to adverse events. The bottom line: For a condition such as acne that has many treatment choices, good options include adapalene/benzoyl peroxide (Epiduo), followed by clindamycin/benzoyl peroxide and then adapalene alone. 31
COVID-19 and Practice Guidelines
As noted earlier, studies of COVID-19 vaccines were among the most highly rated for relevance. The uniform message across these studies was that vaccines and boosters are highly effective, especially at preventing hospitalizations and in older patients. 33 – 37 They are also very safe. Although there is a small increase in the risk of myocarditis, especially in younger men (about 2 to 6 cases per 100,000 vaccinated men 18 to 39 years of age), the risk of myocarditis and other complications associated with COVID-19 infection and the lower risk of cardiac arrest or death in vaccinated people support the importance of vaccination. 38
Several guidelines were also highly rated. The USPSTF no longer recommends initiating aspirin therapy for primary prevention in patients 60 years or older based on newer studies showing no net benefit. The USPSTF continues to recommend statins for adults 40 to 75 years of age who have one or more cardiovascular risk factors and an estimated 10-year cardiovascular event risk of at least 10%, with shared decision-making for those with a 10-year event risk of 7.5% to 9.9%. 39
The National Institute for Health and Care Excellence updated guidelines for two important conditions. Although metformin remains the cornerstone of oral drug therapy for type 2 diabetes, increased use of sodium-glucose cotrans-porter-2 inhibitors is encouraged, especially for patients with chronic heart or renal disease. 40 The updated guideline includes a helpful decision tree (see https://www.bmj.com/content/377/bmj.o775/infographic ). The National Institute for Health and Care Excellence updated guidelines for depression highlight the importance of an ongoing patient-physician relationship and for management of less severe depression to begin with various nondrug treatment options, such as guided self-help. For more severe depression, treatment should begin with cognitive behavior therapy, medication, or both. 41
Editor's Note: This article was cowritten by Dr. Mark Ebell, deputy editor for evidence-based medicine for AFP and cofounder and editor-in-chief of Essential Evidence Plus, published by Wiley-Blackwell, Inc. Because of Dr. Ebell’s dual roles and ties to Essential Evidence Plus, the concept for this article was independently reviewed and approved by a group of AFP ’s medical editors. In addition, the article underwent peer review and editing by four of AFP ’s medical editors. Dr. Ebell was not involved in the editorial decision-making process.—Sumi Sexton, MD, Editor-in-Chief
The authors thank Wiley-Blackwell, Inc., for giving permission to excerpt the POEMs; Drs. Allen Shaughnessy, Henry Barry, David Slawson, Nita Kulkarni, and Linda Speer for selecting and writing the original POEMs; the academic family medicine fellows and faculty of the University of Missouri–Columbia for their work as peer reviewers; CMA Joule for supporting the POEMs CME program in Canada; Pierre Pluye, PhD, for codeveloping the Information Assessment Method; and Maria Vlasak for her assistance with copyediting the POEMs.
Shaughnessy AF, Slawson DC, Bennett JH. Becoming an information master: a guidebook to the medical information jungle. J Fam Pract. 1994;39(5):489-499.
Ebell MH, Barry HC, Slawson DC, et al. Finding POEMs in the medical literature. J Fam Pract. 1999;48(5):350-355.
Badran H, Pluye P, Grad R. When educational material is delivered: a mixed methods content validation study of the Information Assessment Method. JMIR Med Educ. 2017;3(1):e4.
CMA Joule medical librarians. Linking POEMs with overuse alerts from Choosing Wisely Canada. Canadian Medical Association. January 11, 2023. Accessed January 26, 2023. https://www.cma.ca/clinical-blog/linking-poems-overuse-alerts-choosing-wisely-canada
Byrne P, Demasi M, Jones M, et al. Evaluating the association between low-density lipoprotein cholesterol reduction and relative and absolute effects of statin treatment: a systematic review and meta-analysis [published correction appears in JAMA Intern Med . 2022; 182(5): 579]. JAMA Intern Med. 2022;182(5):474-481.
LeBoff MS, Chou SH, Ratliff KA, et al. Supplemental vitamin D and incident fractures in midlife and older adults. N Engl J Med. 2022;387(4):299-309.
U.S. Preventive Services Task Force. Final recommendation statement. Vitamin D deficiency in adults: screening. April 13, 2021. Accessed January 28, 2023. https://uspreventiveservicestaskforce.org/uspstf/recommendation/vitamin-d-deficiency-screening
Lewis G, Marston L, Duffy L, et al. Maintenance or discontinuation of antidepressants in primary care. N Engl J Med. 2021;385(14):1257-1267.
Henssler J, Alexander D, Schwarzer G, et al. Combining antidepressants vs antidepressant monotherapy for treatment of patients with acute depression: a systematic review and meta-analysis. JAMA Psychiatry. 2022;79(4):300-312.
Chawla N, Anothaisintawee T, Charoenrungrueangchai K, et al. Drug treatment for panic disorder with or without agoraphobia: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2022;376:e066084.
De Crescenzo F, D'Alò GL, Ostinelli EG, et al. Comparative effects of pharmacological interventions for the acute and long-term management of insomnia disorder in adults: a systematic review and network meta-analysis. Lancet. 2022;400(10347):170-184.
Mysliwiec V, Martin JL, Ulmer CS, et al. The management of chronic insomnia disorder and obstructive sleep apnea: synopsis of the 2019 U.S. Department of Veterans Affairs and U.S. Department of Defense clinical practice guidelines [published correction appears in Ann Intern Med . 2021; 174(4): 584]. Ann Intern Med. 2020;172(5):325-336.
Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125-133.
Hoge EA, Bui E, Mete M, et al. Mindfulness-based stress reduction vs escitalopram for the treatment of adults with anxiety disorders: a randomized clinical trial. JAMA Psychiatry. 2023;80(1):13-21.
Imai H, Tajika A, Chen P, et al. Psychological therapies versus pharmacological interventions for panic disorder with or without agoraphobia in adults. Cochrane Database Syst Rev. 2016(10):CD011170.
Papi A, Chipps BE, Beasley R, et al. Albuterol-budesonide fixed-dose combination rescue inhaler for asthma. N Engl J Med. 2022;386(22):2071-2083.
Israel E, Cardet JC, Carroll JK, et al. Reliever-triggered inhaled glucocorticoid in Black and Latinx adults with asthma. N Engl J Med. 2022;386(16):1505-1518.
Bryant-Stephens T. Breaking the skin color barriers for asthma medications. It's not black, brown, or white. N Engl J Med. 2022;386(16):1574-1575.
Abrahami D, McDonald EG, Schnitzer ME, et al. Proton pump inhibitors and risk of gastric cancer: population-based cohort study. Gut. 2022;71(1):16-24.
Seo SI, Park CH, You SC, et al. Association between proton pump inhibitor use and gastric cancer: a population-based cohort study using two different types of nationwide databases in Korea. Gut. 2021;70(11):2066-2075.
Katz PO, Dunbar KB, Schnoll-Sussman FH, et al. ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022;117(1):27-56.
Vasant DH, Paine PA, Black CJ, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. 2021;70(7):1214-1240.
Veronese N, Noale M, Sinclair A, et al. Risk of progression to diabetes and mortality in older people with prediabetes: The English longitudinal study on ageing. Age Ageing. 2022;51(2):afab222.
Goldberg RB, Orchard TJ, Crandall JP, et al. Effects of long-term metformin and lifestyle interventions on cardiovascular events in the Diabetes Prevention Program and its outcome study. Circulation. 2022;145(22):1632-1641.
Bouillet B, Tscherter P, Vaillard L, et al. Frequent and severe hypoglycaemia detected with continuous glucose monitoring in older institutionalised patients with diabetes. Age Ageing. 2021;50(6):2088-2093.
Tesfaye S, Sloan G, Petrie J, et al. Comparison of amitriptyline supplemented with pregabalin, pregabalin supplemented with amitriptyline, and duloxetine supplemented with pregabalin for the treatment of diabetic peripheral neuropathic pain (OPTION-DM): a multicentre, double-blind, randomised crossover trial [published correction appears in Lancet . 2022; 400(10355): 810]. Lancet. 2022;400(10353):680-690.
Andreadis K, Chan E, Park M, et al. Imprecision and preferences in interpretation of verbal probabilities in health: a systematic review. J Gen Intern Med. 2021;36(12):3820-3829.
Baker TB, Piper ME, Smith SS, et al. Effects of combined varenicline with nicotine patch and of extended treatment duration on smoking cessation: a randomized clinical trial. JAMA. 2021;326(15):1485-1493.
Balachandran P, Elsohly M, Hill KP. Cannabidiol interactions with medications, illicit substances, and alcohol: a comprehensive review. J Gen Intern Med. 2021;36(7):2074-2084.
Irizarry E, Restivo A, Salama M, et al. A randomized controlled trial of ibuprofen versus ketorolac versus diclofenac for acute, nonradicular low back pain. Acad Emerg Med. 2021;28(11):1228-1235.
Stuart B, Maund E, Wilcox C, et al. Topical preparations for the treatment of mild-to-moderate acne vulgaris: systematic review and network meta-analysis. Br J Dermatol. 2021;185(3):512-525.
Leone FT, Zhang Y, Evers-Casey S, et al. Initiating pharmacologic treatment in tobacco-dependent adults. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2020;202(2):e5-e31.
Arbel R, Hammerman A, Sergienko R, et al. BNT162b2 vaccine booster and mortality due to Covid-19. N Engl J Med. 2021;385(26):2413-2420.
Magen O, Waxman JG, Makov-Assif M, et al. Fourth dose of BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2022;386(17):1603-1614.
Talic S, Shah S, Wild H, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis [published correction appears in BMJ . 2021; 375: n2997]. BMJ. 2021;375:e068302.
Altarawneh HN, Chemaitelly H, Ayoub HH, et al. Effects of previous infection and vaccination on symptomatic omicron infections. N Engl J Med. 2022;387(1):21-34.
Goldberg Y, Mandel M, Bar-On YM, et al. Protection and waning of natural and hybrid immunity to SARS-CoV-2. N Engl J Med. 2022;386(23):2201-2212.
Husby A, Hansen JV, Fosbøl E, et al. SARS-CoV-2 vaccination and myocarditis or myopericarditis: population based cohort study. BMJ. 2021;375:e068665.
Davidson KW, Barry MJ, Mangione CM, et al. Aspirin use to prevent cardiovascular disease: US Preventive Services Task Force Recommendation statement. JAMA. 2022;327(16):1577-1584.
Moran GM, Bakhai C, Song SH, et al. Type 2 diabetes: summary of updated NICE guidance. BMJ. 2022;377:o775.
National Institute for Health and Care Excellence. Depression in adults. June 29, 2022. Accessed January 28, 2023. https://www.nice.org.uk/guidance/ng222
Continue Reading

More in AFP
More in pubmed.
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
The 10 Most Popular Articles of 2022
Two intense years of pandemic distancing and disruption gave way to another sort of distress in 2022—a year of soul searching, burnout, and quiet quitting.
The 10 most-read articles on Harvard Business School Working Knowledge showed a year that had many asking: “Is this what I really want?” Of course, new COVID-19 variants, rampant inflation, a labor shortage, and the sometimes awkward adjustment to new work arrangements didn’t help the mood. And yet, despite all these challenges, many leaders were determined to move forward, prioritizing digital transformation, racial equity, and collaboration.
1. Scrap the Big New Year's Resolutions. Make 6 Simple Changes Instead.
Self-improvement doesn't need to be painful. Rather than set yet another gym goal, look inward, retrain your brain, and get outside, says Hirotaka Takeuchi .
2. More Proof That Money Can Buy Happiness (or a Life with Less Stress)
It's not about the bigger home or the better vacation. Financial stability helps people escape the everyday hassles of life, says research by Jon Jachimowicz .
3. Curiosity, Not Coding: 6 Skills Leaders Need in the Digital Age
Transforming an organization starts with transforming its leaders. Data from 1,700 executives by Linda Hill and colleagues reveals the most important skills and traits leaders need now.
4. When Working Harder Doesn’t Work, Time to Reinvent Your Career
The second half of your life could be better than the first. Really. In the book From Strength to Strength , Arthur Brooks shows how letting go of past glory can open the possibilities of life's "second curve."
5. Where Can Digital Transformation Take You? Insights from 1,700 Leaders
Digital transformation seems like a journey without end, but many companies are forging ahead. Linda Hill and colleagues reveal six qualities that set digitally mature organizations apart.
6. Digital Transformation: A New Roadmap for Success
Is your company reaping the rewards of digital transformation yet? Linda Hill and colleagues offer seven guiding principles for transformations at any stage—nascent, progressing, or stalled.
7. Dick’s Sporting Goods Followed Its Conscience on Guns—and It Paid Off
After the 2018 school shooting in Parkland, Florida, Dick's Sporting Goods' CEO declared: "I don't want to be part of the story anymore." Two new case studies by George Riedel go inside the retailer's decision to remove certain firearms from stores and restrict gun sales.
8. You Don’t Have to Quit Your Job to Find More Meaning in Life
Before you give notice and go on a vision quest, consider this: Fulfillment doesn't require big change, says research by Julian De Freitas and colleagues. In fact, you can find more meaning even in a job you don't love.
9. Rituals at Work: Teams That Play Together Stay Together
Rituals—even seemingly silly ones—help employees bond and add meaning to their work, says research by Michael Norton , Francesca Gino , and colleagues. Who wouldn't welcome a workday pick-me-up?
10. When Parents Tell Kids to ‘Work Hard,’ Do They Send the Wrong Message?
It takes more than grit to succeed in a world rife with systemic inequity. So why don't we tell children that? Research by Ashley Whillans and colleagues shows how honest talk about social barriers could empower kids to break them down.
And don’t forget these:
Does Hybrid Work Actually Work? Insights from 30,000 Emails
How often should employees come to the office? In the first large-scale study of its kind, Prithwiraj Choudhury finds that hybrid schedules might offer the best answer for everyone.
Why Are Prices So High Right Now—and Will They Ever Return to Normal?
Research by Alberto Cavallo probes the complex interplay of product shortages, prices, and inflation.
Feeling Seen: What to Say When Your Employees Are Not OK
Managers who let down their guard and acknowledge their employees' emotions can ease distress and build trust, says research by Julian Zlatev and colleagues.
Your Best Employees Are Burning Out: A Framework for Retaining Talent
Companies have long ignored the factors that are burning out employees. Hise Gibson and MaShon Wilson offer a five-step approach for leaders who are ready to support their talent.
Feedback or ideas to share? Email the Working Knowledge team at [email protected] .
Image: iStockphoto/designer491
- 28 May 2024
- In Practice
Job Search Advice for a Tough Market: Think Broadly and Stay Flexible
- 22 May 2024
Banned or Not, TikTok Is a Force Companies Can’t Afford to Ignore
- 22 Nov 2023
- Research & Ideas
Humans vs. Machines: Untangling the Tasks AI Can (and Can't) Handle
- 24 Jan 2024
Why Boeing’s Problems with the 737 MAX Began More Than 25 Years Ago
- 31 Mar 2020
- Cold Call Podcast
Controlling the Emotion of Negotiation
Sign up for our weekly newsletter.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Publish with us
- About the journal
- Meet the editors
- Specialist reviews
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 3, Issue 1
- Regular use of fish oil supplements and course of cardiovascular diseases: prospective cohort study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Ge Chen 1 ,
- Zhengmin (Min) Qian 2 ,
- Junguo Zhang 1 ,
- Shiyu Zhang 1 ,
- http://orcid.org/0000-0002-7003-6565 Zilong Zhang 1 ,
- Michael G Vaughn 3 ,
- Hannah E Aaron 2 ,
- Chuangshi Wang 4 ,
- Gregory YH Lip 5 , 6 and
- http://orcid.org/0000-0002-3643-9408 Hualiang Lin 1
- 1 Department of Epidemiology , Sun Yat-Sen University , Guangzhou , China
- 2 Department of Epidemiology and Biostatistics, College for Public Health and Social Justice , Saint Louis University , Saint Louis , Missouri , USA
- 3 School of Social Work, College for Public Health and Social Justice , Saint Louis University , Saint Louis , Missouri , USA
- 4 Medical Research and Biometrics Centre , Fuwai Hospital, National Centre for Cardiovascular Diseases, Peking Union Medical College , Beijing , China
- 5 Liverpool Centre for Cardiovascular Science , University of Liverpool and Liverpool Heart and Chest Hospital , Liverpool , UK
- 6 Department of Clinical Medicine , Aalborg University , Aalborg , Denmark
- Correspondence to Dr Hualiang Lin, Department of Epidemiology, Sun Yat-Sen University, Guangzhou, Guangdong 510080, China; linhualiang{at}mail.sysu.edu.cn
Objective To examine the effects of fish oil supplements on the clinical course of cardiovascular disease, from a healthy state to atrial fibrillation, major adverse cardiovascular events, and subsequently death.
Design Prospective cohort study.
Setting UK Biobank study, 1 January 2006 to 31 December 2010, with follow-up to 31 March 2021 (median follow-up 11.9 years).
Participants 415 737 participants, aged 40-69 years, enrolled in the UK Biobank study.
Main outcome measures Incident cases of atrial fibrillation, major adverse cardiovascular events, and death, identified by linkage to hospital inpatient records and death registries. Role of fish oil supplements in different progressive stages of cardiovascular diseases, from healthy status (primary stage), to atrial fibrillation (secondary stage), major adverse cardiovascular events (tertiary stage), and death (end stage).
Results Among 415 737 participants free of cardiovascular diseases, 18 367 patients with incident atrial fibrillation, 22 636 with major adverse cardiovascular events, and 22 140 deaths during follow-up were identified. Regular use of fish oil supplements had different roles in the transitions from healthy status to atrial fibrillation, to major adverse cardiovascular events, and then to death. For people without cardiovascular disease, hazard ratios were 1.13 (95% confidence interval 1.10 to 1.17) for the transition from healthy status to atrial fibrillation and 1.05 (1.00 to 1.11) from healthy status to stroke. For participants with a diagnosis of a known cardiovascular disease, regular use of fish oil supplements was beneficial for transitions from atrial fibrillation to major adverse cardiovascular events (hazard ratio 0.92, 0.87 to 0.98), atrial fibrillation to myocardial infarction (0.85, 0.76 to 0.96), and heart failure to death (0.91, 0.84 to 0.99).
Conclusions Regular use of fish oil supplements might be a risk factor for atrial fibrillation and stroke among the general population but could be beneficial for progression of cardiovascular disease from atrial fibrillation to major adverse cardiovascular events, and from atrial fibrillation to death. Further studies are needed to determine the precise mechanisms for the development and prognosis of cardiovascular disease events with regular use of fish oil supplements.
- Health policy
- Nutritional sciences
- Public health
Data availability statement
Data are available upon reasonable request. UK Biobank is an open access resource. Bona fide researchers can apply to use the UK Biobank dataset by registering and applying at http://ukbiobank.ac.uk/register-apply/ .
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/bmjmed-2022-000451
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Findings of the effects of omega 3 fatty acids or fish oil on the risk of cardiovascular disease are controversial
Most previous studies focused on one health outcome and did not characterise specific cardiovascular disease outcomes (eg, atrial fibrillation, myocardial infarction, stroke, heart failure, and major adverse cardiovascular events)
Whether fish oil could differentially affect the dynamic course of cardiovascular diseases, from atrial fibrillation to major adverse cardiovascular events, to other specific cardiovascular disease outcomes, or even to death, is unclear
WHAT THIS STUDY ADDS
In people with no known cardiovascular disease, regular use of fish oil supplements was associated with an increased relative risk of atrial fibrillation and stroke
In people with known cardiovascular disease, the beneficial effects of fish oil supplements were seen on transitions from atrial fibrillation to major adverse cardiovascular events, atrial fibrillation to myocardial infarction, and heart failure to death
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE, OR POLICY
Regular use of fish oil supplements might have different roles in the progression of cardiovascular disease
Further studies are needed to determine the precise mechanisms for the development and prognosis of cardiovascular disease events with regular use of fish oil supplements
Introduction
Cardiovascular disease is the leading cause of death worldwide, accounting for about one sixth of overall mortality in the UK. 1 2 Fish oil, a rich source of omega 3 fatty acids, containing eicosapentaenoic acid and docosahexaenoic acid, has been recommended as a dietary measure to prevent cardiovascular disease. 3 The UK National Institute for Health and Care Excellence recommends that people with or at high risk of cardiovascular disease consume at least one portion of oily fish a week, and the use of fish oil supplements has become popular in the UK and other western countries in recent years. 4 5
Although some epidemiological and clinical studies have assessed the effect of omega 3 fatty acids or fish oil on cardiovascular disease and its risk factors, the findings are controversial. The Agency for Healthcare Research and Quality systematically reviewed 37 observational studies and 61 randomised controlled trials, and found evidence indicating the beneficial effects of higher consumption of fish oil supplements on ischaemic stroke, whereas no beneficial effect was found for atrial fibrillation, major adverse cardiovascular events, myocardial infarction, total stroke, or all cause death. 6 In contrast, the Reduction of Cardiovascular Events with Icosapent Ethyl-Intervention Trial (REDUCE-IT) reported a decreased risk of major adverse cardiovascular events with icosapent ethyl in patients with raised levels of triglycerides, regardless of the use of statins. 7 Most of these findings, however, tended to assess the role of fish oil at a certain stage of cardiovascular disease. For example, some studies restricted the study population to people with a specific cardiovascular disease or at a high risk of cardiovascular disease, 8 9 whereas others evaluated databases of generally healthy populations. 10 All of these factors might preclude direct comparison of the effects of omega 3 fatty acids on atrial fibrillation events or on further deterioration of cardiovascular disease. Few studies have fully characterised specific cardiovascular disease outcomes or accounted for differential effects based on the complex disease characteristics of participants. Hence, in this study, we hypothesised that fish oil supplements might have harmful, beneficial, or no effect on different cardiovascular disease events in patients with varying health conditions.
Most previous studies on the association between fish oil and cardiovascular diseases generally focused on one health outcome. Also, no study highlighted the dynamic progressive course of cardiovascular diseases, from healthy status (primary stage), to atrial fibrillation (secondary stage), major adverse cardiovascular events (tertiary stage), and death (end stage). Clarifying this complex pathway in relation to the detailed progression of cardiovascular diseases would provide substantial insights into the prevention or treatment of future disease at critical stages. Whether fish oil could differentially affect the dynamic course of cardiovascular disease (ie, from atrial fibrillation to major adverse cardiovascular events, to other specific cardiovascular disease outcomes, or even to death) is unclear.
To deal with this evidence gap, we conducted a longitudinal cohort study to estimate the associations between fish oil supplements and specific clinical cardiovascular disease outcomes, including atrial fibrillation, major adverse cardiovascular events, and all cause death in people with no known cardiovascular disease or at high risk of cardiovascular disease for the purpose of primary prevention. We also assessed the modifying effects of fish oil supplements on the disease process, from atrial fibrillation to other outcomes, in people with known cardiovascular disease for the purpose of secondary prevention.
The UK Biobank is a community based cohort study with more than half a million UK inhabitants aged 40-69 years at recruitment. 11–13 Participants were invited to participate in this study if they were registered with the NHS and lived within 35 km of one of 22 Biobank assessment centres. Between 1 March 2006 and 31 July 2010, a baseline survey was conducted, based on a touch screen questionnaire and face-to-face interviews, to collect detailed personal, socioeconomic, and lifestyle characteristics, and information on diseases. 11–13
We excluded patients who had a diagnosis of atrial fibrillation (n=8326), heart failure (n=2748), myocardial infarction (n=11 949), stroke (n=7943), or cancer (n=48 624) at baseline; who withdrew from the study during follow-up (n=1299); or who had incomplete or outlier data for the main information (n=11 748). Because we focused only on a specific sequence of progression of cardiovascular disease (ie, from healthy status to atrial fibrillation, to major adverse cardiovascular events, and then to death), we excluded 1983 participants with other transition patterns. The remaining 415 737 participants were included in this analysis ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Flowchart of selection of participants in study. The count of diagnosed diseases does not equate to the total number of individuals, because each person could have multiple diagnoses
Determining use of fish oil supplements
Information on regular use of fish oil supplements was collected from a self-reported touchscreen questionnaire during the baseline survey. 14 15 Each participant was asked whether they regularly used any fish oil supplement. Trained staff conducted a verbal interview with participants, asking if they were currently receiving treatments or taking any medicines, including omega 3 or fish oil supplements. Based on this information, we classified participants as regular users of fish oil supplements and non-users.
Follow-up and outcomes
Participants were followed up from the time of recruitment to death, loss to follow-up, or the end date of follow-up (31 March 2021), whichever came first. Incident cases of interest, including atrial fibrillation, heart failure, stroke, and myocardial infarction, were identified by linkage to death registries, primary care records, and hospital inpatient records. 11 Information on deaths was obtained from death registries of the NHS Information Centre, for participants in England and Wales, and from the NHS Central Register Scotland, for participants in Scotland. 11 Outcomes were defined by a three character ICD-10 (international classification of diseases, 10th revision) code. In this study, atrial fibrillation was defined by ICD-10 code I48, and major adverse cardiovascular events was determined by a combination of heart failure (I50, I11.0, I13.0, and I13.2), stroke (I60-I64), and myocardial infarction (I21, I22, I23, I24.1, and I25.2) codes.
We collected baseline data on age (<65 years and ≥65 years), sex (men and women), ethnic group (white and non-white), Townsend deprivation index (with a higher score indicating higher levels of deprivation), smoking status (never, previous, and current smokers), and alcohol consumption (never, previous, and current drinkers). Data for sex were taken from information in UK Biobank rather than from patient reported gender. Baseline dietary data were obtained from a dietary questionnaire completed by the patient or by an interviewer. The questionnaire was established for each nation (ie, England, Scotland, and Wales) to assess an individual's usual food intake (oily fish, non-oily fish, vegetables, fruit, and red meat). Diabetes mellitus was defined by ICD-10 codes E10-E14, self-reported physician's diagnosis, self-reported use of antidiabetic drugs, or haemoglobin A1c level ≥6.5% at baseline. Hypertension was defined by ICD-10 code I10 or I15, self-reported physician's diagnosis, self-reported use of antihypertensive drugs, or measured systolic and diastolic blood pressure ≥130/85 mm Hg at baseline. Information on other comorbidities (obesity (ICD-10 code E66), chronic obstructive pulmonary disease (J44), and chronic renal failure (N18)) was extracted from the first occurrence (UKB category ID 1712). Information on the use of drugs, including antihypertensive drugs, antidiabetic drug, and statins, was extracted from treatment and drug use records. Biochemistry markers were measured immediately at the central laboratory from serum samples collected at baseline. Binge drinking was defined as consumption of ≥6 standard drinks/day for women or ≥8 standard drinks/day for men. Detailed information on alcohol consumption and binge drinking in the UK Biobank was reported previously. 16
Statistical analysis
Characteristics of participants are summarised as number (percentages) for categorical variables and mean (standard deviation (SD)) for continuous variables. Comparisons between regular users of fish oil supplements and non-users were made with the χ 2 test or Student's t test.
We used a multi-state regression model to assess the role of regular use of fish oil supplements in the temporal disease progression from healthy status to atrial fibrillation, to major adverse cardiovascular events, and subsequently to death. The multi-state model is an extension of competing risks survival analysis. 17–19 The model allows simultaneous estimation of the role of risk factors in transitions from a healthy state to atrial fibrillation (transition A), healthy state to major adverse cardiovascular events (transition B), healthy state to death (transition C), atrial fibrillation to major adverse cardiovascular events (transition D), atrial fibrillation to death (transition E), and major adverse cardiovascular events to death (transition F) (transition pattern I, figure 2 ). The focus on these six transitions rather than on all possible health state transitions was preplanned and evidence based. If participants entered different states on the same date, we used the date of the theoretically previous state as the entry date of the latter state minus 0.5 days.
Numbers of participants in transition pattern I, from baseline to atrial fibrillation, major adverse cardiovascular events, and death
We further examined the effects of regular use of fish oil supplements on other pathways. For example, we divided major adverse cardiovascular events into three individual diseases (heart failure, stroke, and myocardial infarction), resulting in three independent pathways (transition patterns II, III, and IV, online supplemental figures S1–S3 ). All models were adjusted for age, sex, ethnic group, Townsend deprivation index, consumption of oily fish, consumption of non-oily fish, smoking status, alcohol consumption, obesity, hypertension, diabetes mellitus, chronic obstructive pulmonary disease, chronic renal failure, and use of statins, antidiabetic drugs, and antihypertensive drugs.
Supplemental material
We conducted several sensitivity analyses for the multi-state analyses of transition pattern A: additionally adjusting for setting (urban and rural), body mass index (underweight, normal, overweight, and obese), and physical activity (low, moderate, and high) in the model; adjusting for binge drinking rather than alcohol consumption; additionally adjusting for other variables of dietary intake (consumption of vegetables, fruit, and red meat); calculating participants' entry date into the previous state with different time intervals (0.5 years, one year, and two years); excluding participants who entered different states on the same date; excluding events occurring in the first two years of follow-up; restricting the follow-up date to 31 March 2020 to evaluate the influence of the covid-19 pandemic; and the use of the inverse probability weighted method to deal with biases between the regular users and non-users of fish oil supplements. Also, we conducted grouped analyses for sex, age group, ethnic group, smoking status, consumption of oily fish, consumption of non-oily fish, hypertension, and drug use, to examine effect modification. The interactions were tested with the likelihood ratio test. All analyses were carried out with R software (version 4.0.3), and the multi-model analysis was performed with the mstate package. A two tailed P value <0.05 was considered significant.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research. Participants were involved in developing the ethics and governance framework for UK Biobank and have been engaged in the progress of UK Biobank through follow-up questionnaires and additional assessment visits. UK Biobank keeps participants informed of all research output through the study website ( https://www.ukbiobank.ac.uk/explore-your-participation ), participant events, and newsletters.
A total of 415 737 participants (mean age 55.9 (SD 8.1) years; 55% women), aged 40-69 years, were analysed, and 31.4% (n=1 30 365) of participants reported regular use of fish oil supplements at baseline ( figure 1 ). Table 1 shows the characteristics of regular users (n=130 365) and non-users (n=285 372) of fish oil supplements. In the group of regular users of fish oil supplements, we found higher proportions of elderly people (22.6% v 13.9%), white people (95.1% v 94.2%), and women (57.6% v 53.9%), and higher consumption of alcohol (93.1% v 92.0%), oily fish (22.1% v 15.4%), and non-oily fish (18.0% v 15.4%) than non-users. The Townsend deprivation index (mean −1.5 (SD 3.0) v −1.3 (3.0)) and the proportion of current smokers (8.1% v 11.4%) were lower in regular users of fish oil supplements. Online supplemental table S1 provides more details on patient characteristics and online supplemental table S2 compares the basic characteristics of included and excluded people.
- View inline
Baseline characteristics of study participants grouped by use of fish oil supplements
Over a median follow-up time of of 11.9 years, 18 367 participants had atrial fibrillation (transition A) and 17 826 participants had major adverse cardiovascular events (transition B); 14 902 participants died without having atrial fibrillation or major adverse cardiovascular events (transition C). Among patients with incident atrial fibrillation, 4810 developed major adverse cardiovascular events (transition D) and 1653 died (transition E). Among patients with incident major adverse cardiovascular events, 5585 died during follow-up (transition F, figure 2 ). In separate analyses for individual diseases (transition patterns II, III, and IV, online supplemental figures S1–S3 ), in patients with atrial fibrillation, 3085 developed heart failure, 1180 had a stroke, and 1415 had a myocardial infarction. During follow-up, 2436, 2088, and 2098 deaths occurred in patients with heart failure, stroke, and myocardial infarction, respectively.
Multi-state regression results
Table 2 shows the different roles of regular use of fish oil supplements in transitions from healthy status to atrial fibrillation, to major adverse cardiovascular events, and then to death. For individuals in the primary stage (healthy status), we found that the use of fish oil supplements had a harmful effect on the transition from health to atrial fibrillation, with an adjusted hazard ratio of 1.13 (95% CI 1.10 to 1.17, transition A). The hazard ratio for transition B (from health to major adverse cardiovascular events) was 1.00 (95% CI 0.97 to 1.04) and for transition C (from health to death) was 0.98 (0.95 to 1.02).
Hazard ratios (95% confidence intervals) for each transition, for different transition patterns for progressive cardiovascular disease by regular use of fish oil supplements
For individuals in the secondary stage (atrial fibrillation) at the beginning of the study, regular use of fish oil supplements decreased the risk of major adverse cardiovascular events (transition D, hazard ratio 0.92, 95% CI 0.87 to 0.98), and had a borderline protective effect on the transition from atrial fibrillation to death (transition E, 0.91, 0.82 to 1.01). For transition F, from major adverse cardiovascular events to death, after adjusting for covariates, the hazard ratio was 0.99 (0.94 to 1.06, transition pattern I, table 2 ).
We divided major adverse cardiovascular events into three individual diseases (ie, heart failure, stroke, and myocardial infarction) and found that regular use of fish oil supplements was marginally associated with an increased risk of stroke in people with a healthy cardiovascular state (hazard ratio 1.05, 95% CI 1.00 to 1.11), whereas a protective effect was found in transitions from healthy cardiovascular states to heart failure (0.92, 0.86 to 0.98). For patients with atrial fibrillation, we found that the beneficial effects of regular use of fish oil supplements were for transitions from atrial fibrillation to myocardial infarction (0.85, 0.76 to 0.96), and from atrial fibrillation to death (0.88, 0.81 to 0.95) for transition pattern IV. For patients with heart failure, we found a protective effect of regular use of fish oil supplements on the risk of mortality (0.91, 0.84 to 0.99) (transition patterns II, III, and IV, table 2 ).
Stratified and sensitivity analyses
We found that age, sex, smoking, consumption of non-oily fish, prevalent hypertension, and use of statins and antihypertensive drugs modified the associations between regular use of fish oil supplements and the transition from healthy states to atrial fibrillation ( online supplemental figure S4 ). We found that the association between regular use of fish oil supplements and risk of transition from healthy states to major adverse cardiovascular events was greater in women (hazard ratio 1.06, 95% CI 1.00 to 1.11, P value for interaction=0.005) and non-smoking participants (1.06, 1.06 to 1.11, P value for interaction=0.001) ( online supplemental figure S4 ). The protective effect of regular use of fish oil supplements on the transition from healthy states to death was greater in men (hazard ratio 0.93, 95% CI 0.89 to 0.98, P value for interaction=0.003) and older participants (0.91, 0.86 to o 0.96, P value for interaction=0.002) ( online supplemental figures S5 and S6 ). The results were not substantially changed in the sensitivity analyses ( online supplemental table S3 ).
Principal findings
Our study characterised the regular use of fish oil supplements on the progressive course of cardiovascular disease, from a healthy state (primary stage), to atrial fibrillation (secondary stage), major adverse cardiovascular events (tertiary stage), and death (end stage). In this prospective analysis of more than 400 000 UK adults, we found that regular use of fish oil supplements could have a differential role in the progression of cardiovascular disease. For people with a healthy cardiovascular profile, regular use of fish oil supplements, a choice of primary prevention, was associated with an increased risk of atrial fibrillation. For participants with a diagnosis of atrial fibrillation, however, regular use of fish oil supplements, as secondary prevention, had a protective effect or no effect on transitions from atrial fibrillation to major adverse cardiovascular events, atrial fibrillation to death, and major adverse cardiovascular events to death. When we divided major adverse cardiovascular events into three individual diseases (ie, heart failure, stroke, and myocardial infarction), we found associations that could suggest a mildly harmful effect between regular use of fish oil supplements and transitions from a healthy cardiovascular state to stroke, whereas potential beneficial associations were found between regular use of fish oil supplements and transitions from atrial fibrillation to myocardial infarction, atrial fibrillation to death, and heart failure to death.
Comparison with other studies
Primary prevention.
The cardiovascular benefits of regular use of fish oil supplements have been examined in numerous studies but the results are controversial. Extending previous reports, our study estimated the associations between regular use of fish oil supplements and specific clinical cardiovascular disease outcomes in people with no known cardiovascular disease. Our findings are in agreement with the results of several previous randomised controlled trials and meta-analyses. The Long-Term Outcomes Study to Assess Statin Residual Risk with Epanova in High Cardiovascular Risk Patients with Hypertriglyceridaemia (STRENGTH) reported that consumption of 4 g/day of marine omega 3 fatty acids was associated with a 69% higher risk of new onset atrial fibrillation in people at high risk of cardiovascular disease. 20 A meta-analysis of seven randomised controlled trials showed that users of marine omega 3 fatty acids supplements had a higher risk of atrial fibrillation events, with a hazard ratio of 1.25 (95% CI 1.07 to 1.46, P=0.013). 21 The Vitamin D and Omega-3 Trial (VITAL Rhythm study), a large trial of omega 3 fatty acids for the primary prevention of cardiovascular disease in adults aged ≥50 years, however, found no effects on incident atrial fibrillation, major adverse cardiovascular events, or cardiovascular disease mortality among those treated with 840 mg/day of marine omega 3 fatty acids compared with placebo. 10 22
One possible explanation for the inconsistent results in these studies is that adverse effects might be related to dose and composition. Higher doses of omega 3 fatty acids used in previous studies might have had an important role in causing an adverse effect on atrial fibrillation. 21 One study found that high concentrations of fish oil altered cell membrane properties and inhibited Na-K-ATPase pump activity, whereas a low concentration of fish oil minimised peroxidation potential and optimised activity. 23 In another study, individuals with atrial fibrillation or flutter had higher percentages of total polyunsaturated fatty acids, and n-3 and n-6 polyunsaturated fatty acids, on red blood cell membranes than healthy controls. 24
In terms of composition of omega 3 fatty acids, a recent meta-analysis showed that eicosapentaenoic acid alone can be more effective at reducing the risk of cardiovascular disease than the combined effect of eicosapentaenoic acid and docosahexaenoic acid. 25 Similar outcomes were reported in the INSPIRE study, which showed that higher levels of docosahexaenoic acid reduced the cardiovascular benefits of eicosapentaenoic acid when given as a combination. 26 Another possible explanation is that age, sex, ethnic group, smoking status, dietary patterns, and use of statins and antidiabetic drugs by participants might modify the effects of regular use of fish oil supplements on cardiovascular disease events. Despite these differences in risk estimates, our findings do not support the use of fish oil or omega 3 fatty acid supplements for the primary prevention of incident atrial fibrillation or other specific clinical cardiovascular disease events in generally healthy individuals. Caution might be warranted when fish oil supplements are used for primary prevention because of the uncertain cardiovascular benefits.
Secondary prevention
Our large scale cohort study assessed the role of regular use of fish oil supplements on the disease process, from atrial fibrillation to more serious cardiovascular disease stages, to death, in people with known cardiovascular disease. Contrary to the observations for primary prevention, we found associations that could suggest beneficial effects between regular use of fish oil supplements and most cardiovascular disease transitions. No associations were found between regular use of fish oil supplements and transitions from atrial fibrillation to death, or from major adverse cardiovascular events to death.
Consistent with our hypothesis, the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI) Prevenzione study reported an association between administration of low dose prescriptions of n-3 polyunsaturated fatty acids and reduced cardiovascular events in patients with recent myocardial infarction. 27 A meta-analysis of 16 randomised controlled trials also reported a tendency towards a greater beneficial effect for secondary prevention in patients with cardiovascular disease. 28 Why patients with previous atrial fibrillation benefit is unclear. These findings indicate that triglyceride independent effects of omega 3 fatty acids might in part be responsible for the benefits in cardiovascular disease seen in previous trials. 29–31 No proven biological mechanism for this explanation exists, however, and the dose and formulation of omega 3 fatty acids used in clinical practice are not known.
For the disease process, from cardiovascular disease to death, our findings are consistent with the results of secondary prevention trials of omega 3 fatty acids, which have mostly shown a weak or neutral preventive effect in all cause mortality with oil fish supplements. The GISSI heart failure trial (GISSI-HF), conducted in 6975 patients with chronic heart failure, reported that supplemental omega 3 fatty acids reduced the risk of all cause mortality by 9% (hazard ratio 0.91, 95% CI 0.833 to 0.998, P=0.041). 32 Zelniker et al showed that omega 3 fatty acids were inversely associated with a lower incidence of sudden cardiac death in patients with non-ST segment elevation acute coronary syndrome. 33 A meta-analysis found that use of omega 3 supplements of ≤1 capsule/day was not associated with all cause mortality, but among participants with a risk of cardiovascular disease, taking a higher dose was associated with a reduction in cardiac death and sudden death. 28 Individuals who might benefit the most from fish oil or omega 3 fatty acid supplements are possibly more vulnerable individuals, such as those with previous cardiovascular diseases and those who can no longer live in the community. How fish oil supplements stop further deterioration of cardiovascular disease is unclear, but the theory that supplemental omega 3 fatty acids might protect the coronary artery is biologically plausible, suggesting that omega 3 fatty acids have anti-inflammatory and anti-hypertriglyceridaemia effects, contributing to a reduction in thrombosis and improvement in endothelial function. 34–41 Nevertheless, the effects of omega 3 fatty acids vary according to an individual's previous use of statins, which might partly explain the different effects of fish oil supplements in people with and without cardiovascular disease.
Many studies of omega 3 fatty acids, including large scale clinical trials and meta-analyses, have not produced entirely consistent results. 21 25 42 Our study mainly explored the varied potential effects of regular use of fish oil supplements on progression of cardiovascular disease, offering an initial overview of this ongoing discussion. Our findings suggest caution in the use of fish oil supplements for primary prevention because of the uncertain cardiovascular benefits and adverse effects. Further studies are needed to determine whether potential confounders modify the effects of oil fish supplements and the precise mechanisms related to the development and prognosis of cardiovascular disease events.
Strengths and limitations of this study
The strengths of our study were the large sample size, long follow-up period, which allowed us to analyse clinically diagnosed incident diseases, and complete data on health outcomes. Another strength was our analytical strategy. The multi-state model gives less biased estimates than the conventional Cox model, and distinguished the effect of regular use of fish oil supplements on each transition in the course of cardiovascular disease.
Our study had some limitations. Firstly, as an observational study, no causal relations can be drawn from our findings. Secondly, although we adjusted for multiple covariates, residual confounding could still exist. Thirdly, information on dose and formulation of the fish oil supplements was not available in this study, so we could not evaluate potential dose dependent effects or differentiate between the effects of different fish oil formulations. Fourthly, the use of hospital inpatient data for determining atrial fibrillation events could have excluded some events triggered by acute episodes, such as surgery, trauma, and similar conditions, resulting in underestimation of the true risk because undiagnosed atrial fibrillation is a common occurrence. 43 Fifthly, most of the participants in this study were from the white ethnic group and whether the findings can be generalised to other ethnic groups is not known. Finally, our study did not consider behavioural changes in populations with different cardiovascular profiles because of limited information, and variations in outcomes for different cardiovascular states merits further exploration.
Conclusions
This large scale prospective study of a UK cohort suggested that regular use of fish oil supplements might have differential roles in the course of cardiovascular diseases. Regular use of fish oil supplements might be a risk factor for atrial fibrillation and stroke among the general population but could be beneficial for disease progression, from atrial fibrillation to major adverse cardiovascular events, and from atrial fibrillation to death. Further studies are needed to determine whether potential confounders modify the effects of oil fish supplements and the precise mechanisms for the development and prognosis of cardiovascular disease events.
Ethics statements
Patient consent for publication.
Consent obtained directly from patients.
Ethics approval
The UK Biobank study obtained ethical approval from the North West Multicentre Research ethics committee, Information Advisory Group, and the Community Health Index Advisory Group (REC reference for UK Biobank 11/NW/0382). Participants gave informed consent to participate in the study before taking part.
Acknowledgments
This study was conducted with UK Biobank Resource (application No: 69550). We appreciate all participants and professionals contributing to UK Biobank.
- Mensah GA ,
- Johnson CO , et al
- Gao MM , et al
- Saravanan P ,
- Davidson NC ,
- Schmidt EB , et al
- National Institute for Health and Care Excellence
- Lichtenstein AH ,
- Vadiveloo M , et al
- Djuricic I ,
- Miller M , et al
- Kesse-Guyot E ,
- Czernichow S , et al
- Klemsdal TO ,
- Sandvik L , et al
- Manson JE ,
- Lee I-M , et al
- Gallacher J ,
- Allen N , et al
- Littlejohns TJ ,
- Sudlow C , et al
- Allen NE , et al
- Zhong W-F ,
- Liu S , et al
- Wu Z , et al
- Gallagher C ,
- Elliott AD , et al
- Qian SE , et al
- Nicholls SJ ,
- Lincoff AM ,
- Garcia M , et al
- Djousse L ,
- Al-Ramady OT , et al
- Bassuk SS ,
- Cook NR , et al
- Cazzola R ,
- Della Porta M ,
- Castiglioni S , et al
- Viviani Anselmi C ,
- Ferreri C ,
- Novelli V , et al
- Khan MS , et al
- Knowlton K , et al
- Marchioli R ,
- Bomba E , et al
- Olmastroni E ,
- Gazzotti M , et al
- Al Rifai M , et al
- Tavazzi L ,
- Maggioni AP ,
- Marchioli R , et al
- Zelniker TA ,
- Morrow DA ,
- Scirica BM , et al
- Limonte CP ,
- Zelnick LR ,
- Ruzinski J , et al
- Nelson JR ,
- Miller PE ,
- Van Elswyk M ,
- Alexander DD
- Mozaffarian D ,
- Bornfeldt KE
- Harris WS ,
- Ginsberg HN ,
- Arunakul N , et al
- Markozannes G ,
- Tsapas A , et al
- Svennberg E ,
- Engdahl J ,
- Al-Khalili F , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
GYL and HL are joint senior authors.
Contributors HL supervised the whole project and designed the work. GC and HL directly accessed and verified the underlying data reported in the manuscript. GC contributed to data interpretation and writing of the report. ZQ, SZ, JZ, ZZ, MGV, HEA, CW, and GYHL contributed to the discussion and data interpretation, and revised the manuscript. All authors had full access to all of the data in the study and had final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. HL is the guarantor. Transparency: The lead author (guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Funding This work was supported by the Bill and Melinda Gates Foundation (grant No INV-016826). Under the grant conditions of the foundation, a creative commons attribution 4.0 generic license has already been assigned to the author accepted manuscript version that might arise from this submission. The funder had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from Bill and Melinda Gates Foundation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Next Generation Research Uses Real-World Data to Identify Most Effective Hypertension Drugs for Patients
Listen to "next generation research uses real-world data to identify most effective hypertension drugs for patients".
More than 100 million U.S. adults have been diagnosed with hypertension , one of the leading risk factors for cardiovascular disease. While more than 70% of people with hypertension cannot achieve adequate blood pressure control with just one drug, current guidelines only make recommendations for first-line therapy.
“The question is: when the first drug is not enough, what is the optimal second drug to add?” said Yuan Lu, ScD , assistant professor of medicine (cardiology) and assistant professor of biomedical informatics and data science and of epidemiology (chronic disease). “There are more than 50 drugs across five major classes available for treating hypertension. Conducting clinical trials to compare every possible drug and combination thereof is impractical; it would be incredibly time-consuming and costly. Consequently, this creates a significant gap in evidence.”
Lu recently received a Research Project Grant (R01) from the National Institutes of Health (NIH) for the project, “Real-World Evidence to Inform Decisions for Hypertension Treatment Escalation,” to help address this question.
Lu and her team will analyze real-world data that is routinely collected by clinicians in health care settings to compare the effectiveness of second antihypertensive agents on major cardiovascular events as well as their comparative risk on potential drug-related adverse events. This study will also look at the effectiveness and safety of each second hypertensive agent when used in different patient subgroups defined by age, sex, race, ethnicity, and comorbidities, which Lu hopes will help address disparities for patients with hypertension. This is the first research study of its kind that uses real-world data assets and reproducible methods to comprehensively evaluate the safety and effectiveness of second anti-hypertensive drugs added after monotherapy.
“Clinicians often face this important patient scenario and lack comprehensive, high-quality evidence on how best to guide the implementation of the available drug options for patients into real-world practice,” said Eric Velazquez, MD , Robert W. Berliner Professor of Medicine and chief of Yale Cardiovascular Medicine. “Hypertension impacts nearly every family in the world. It has been a substantial frustration for me that randomized clinical trials such as ACCOMPLISH , which we completed over 15 years ago, have not been adequately integrated into everyday care. Yuan’s work is pivotal to ensure our research meets its potential to improve the lives of millions of people living with hypertension.”
The study will analyze data from more than 100 million patients in the United States in five electronic health record (EHR) databases. Lu and her team are collaborating with the Observational Health Data Science and Informatics (OHDSI) , a multi-stakeholder, international organization that aims to use systematic approaches to improve observational study. OHDSI created the OMOP Common Data Model , which is an open community data standard that allows institutions to efficiently share data for analysis.
“By mapping EHR data into a common data model, we can now combine the power of computing, data science, and clinical knowledge to generate new evidence to address these important clinical questions,” said Lu. “We hope our research will inform the prioritization of future clinical trials, assisting investigators in selecting the most promising drug combinations for testing.”
Lu joined Yale in 2015 after receiving her ScD in Global Health and Population at the Harvard School of Public Health. “I was intrigued by this area of study because instead of a doctor, who can only treat 20 or 30 patients a day, I would have the opportunity to impact health at the population level,” she said.
She hopes that this research will inform the development of clinical guidelines. Even though clinical trials provide the highest quality of evidence, real-world data from observational studies can provide important evidence to complement clinical trials and support guideline development, especially when clinical trials are too expensive or unethical to conduct.
“Physicians can’t just wait for clinical trials to end before they help their patients. They need to keep treating people using the best available information and practices,” said Lu.
Eventually, Lu and her team plan to develop a clinical decision support tool that would incorporate the knowledge gained from this project. The tool would help doctors quickly and easily see recommendations about the types of combination therapies that may work best for their individual patients. “It’s often said that it takes about 17 years to translate about 14% of research findings to be implemented into routine clinical practice. It’s a long time. I want to try to reduce the time it takes to get research into clinical practice and increase the percentage of knowledge translation," she said.
The research team is beginning to refine their protocol for the study, which they aim to publish online via GitHub so that anyone interested in this work can read the proposal and provide feedback to help make improvements. Lu sees tremendous potential for this type of study in other areas of medicine, including diabetes, obesity, and other common health conditions. She and other team members are already beginning work on other projects using real-world data.
For example, Lu, along with other researchers from Yale and colleagues at Sentara Health, recently published a paper in the Journal of the American Heart Association (JAHA) , which used real-world EHR data to identify the prevalence, control rates, and diagnostic codes used in a large patient population. The study found that prevalence is increasing, a quarter of patients’ hypertension was not controlled, and there were marked disparities between non-Hispanic Black patients and other racial and ethnic groups. Lu and the study authors say other regional health systems could emulate this study to better understand their hypertension prevalence and control rates and to inform strategies to improve hypertension care. Other study authors include: Yuntian Liu, MPH , Shu-Xia Li, PhD , Mitsuaki Sawano, MD , Patrick Young, PhD , Wade Schulz, MD , and Harlan Krumholz, MD, SM , from Yale, and John E. Brush, Jr., MD, Jordan R. Asher, MD, MS, Mark Anderson, AS, and John S. Burrows, MBA.
“I feel so fortunate that I decided to come to Yale. As an investigator, it can sometimes seem like the only deliverable is a paper. But at Yale, I’m able to work closely with clinicians and see how this knowledge can inform their clinical practice or help them do their job better,” Lu said. “I’m excited to come to work every day.”
- National Institutes of Health (NIH)
- Internal Medicine
- Cardiovascular Medicine
Featured in this article
- Yuan Lu, ScD Assistant Professor of Medicine (Cardiology) and of Biomedical Informatics and Data Science and of Epidemiology (Chronic Diseases)
- Yuntian Liu Statistician I
- Shu-Xia Li, PhD Staff Affiliate - YNHH; Associate Director, Data Management & Analytics, Center for Outcomes Research & Evaluation (CORE)
- Mitsuaki Sawano, MD, PhD Associate Research Scientist
- Wade Schulz, MD, PhD Assistant Professor; Director of Informatics, Laboratory Medicine; Director, CORE Center for Computational Health, Center for Outcomes Research & Evaluation (CORE)
- Patrick Young, PhD Associate Research Scientist
- Harlan Krumholz, MD, SM Harold H. Hines, Jr. Professor of Medicine (Cardiology) and Professor in the Institute for Social and Policy Studies, of Investigative Medicine and of Public Health (Health Policy); Founder, Center for Outcomes Research and Evaluation (CORE)
- Eric Velazquez, MD Robert W. Berliner Professor of Medicine (Cardiology); Chief, Cardiovascular Medicine; Chief, Cardiovascular Medicine, Yale New Haven Hospital; Physician-in-Chief, Heart and Vascular Center, Yale New Haven Health System; Deputy Director, Clinical Trials Innovation, Yale Center for Clinical Investigation (YCCI); Co-Chair, Clinical and Translational Research Oversight Committee; President’s contingency planning committee, Clinical Practice/Clinical Research Subcommittee
Related Links
- Digital Health Tools Help Manage Hypertension for Populations Experiencing Health Disparities
- Enhancing Treatment for Persistent Hypertension: Unleashing the Power of Actionable Taxonomy from EHR Data for Precision Medicine
- The Unmet Potential of Clinical Decision Support Tools in Cardiology
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Financial Toxicity of Cancer Treatment
- 1 Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins Medicine, Baltimore, Maryland
- 2 Masonic Cancer Center, University of Minnesota, Minneapolis
- 3 Department of Health Policy, Vanderbilt University School of Medicine, Nashville, Tennessee
What Is Financial Toxicity?
Cancer is one of the most expensive medical conditions to treat in the US. Financial toxicity is a term used to describe the harmful effect of high cost of treatment on a person’s quality of life. It may also be described as financial burden or financial distress.
Am I at Risk of Financial Toxicity During Treatment?
Many factors may cause financial stress during treatment:
Type of cancer, its severity, and treatment: Treatment may range from a single daily pill to daily or weekly visits or long hospital stays.
Financial status: Factors include whether you are the primary earner in your family, how much money you have saved, and whether you or a family member can continue working during treatment.
Health insurance coverage: This dictates your out-of-pocket costs during treatment.
What Are the Consequences of Financial Distress During Treatment?
Every household adjusts differently. Some people may use a large portion of their savings, open a new credit card, or refinance their home to help pay for treatment. Others may skip medical visits or take less medication than they are prescribed. Some families may cut back on food, clothing, or leisure activities, such as going to movies or vacations. Making ends meet in this manner can be stressful, which in turn can trigger symptoms of anxiety and depression. It is important to recognize these changes early and talk to your treatment team if you are having problems affording your care.
How Is Financial Toxicity “Treated”?
Having health insurance is the most effective way to reduce financial toxicity. Understanding your coverage and what you can expect to pay for treatment is important. Terms such as premium , deductible , copayment , and coinsurance are often difficult to fully understand, even for medical professionals.
Before you begin treatment, you should ask to speak with the financial team that will obtain authorization for your treatment so that you can understand the billing process and possibility of any “surprise” bills. Your social worker can help find grants from community programs, connect you with family or group support, and discuss medical leave options with your employer.
Even if you are uninsured or underinsured, they can help find financial assistance options. Open enrollment periods throughout the year allow you to enroll in a new federal, state, or private insurance plan or adjust current coverage to better fit future needs.
You can be your best advocate by raising concerns about costs at the beginning of or during treatment. Your quality of care will not change. In fact, this may give the team an opportunity to improve parts of treatment, such as switching to a generic drug, consolidating clinic visits, or giving vouchers for transportation or parking.
For Further Information
National Cancer Institute www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-pdq
Published Online: March 10, 2022. doi:10.1001/jamaoncol.2021.7987
Conflict of Interest Disclosures: Dr Dusetzina reported grants from Arnold Ventures, Commonwealth Fund, Leukemia & Lymphoma Society, and Robert Wood Johnson Foundation during the submitted work, and personal fees from West Health, National Academy for State Health Policy, and Institute for Clinical and Economic Review outside the submitted work, as well as serving on the Medicare Payment Advisory Commission. The views presented are those of the authors and do not reflect those of the Commission. No other disclosures were reported.
See More About
Hussaini SMQ , Gupta A , Dusetzina SB. Financial Toxicity of Cancer Treatment. JAMA Oncol. 2022;8(5):788. doi:10.1001/jamaoncol.2021.7987
Manage citations:
© 2024
Artificial Intelligence Resource Center
Oncology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
European talent is ready to walk out the door. How should companies respond?
How do companies keep their current workforces happy while drawing the best people to join them? Talent leaders have been asking that question forever, of course, but the answers have grown much more complex since the COVID-19 pandemic set off an employee exodus that has shaken organizations across the globe.
McKinsey has analyzed this Great Attrition talent trend in depth, showing why people began quitting in droves and how companies, caught unaware, could respond. 1 Aaron De Smet, Bonnie Dowling, Marino Mugayar-Baldocchi, and Bill Schaninger, “ ‘Great Attrition’ or ‘Great Attraction’? The choice is yours ,” McKinsey Quarterly , September 8, 2021. We updated our research earlier this year, finding that workers were not only still quitting but also switching roles and industries, in what we dubbed the Great Renegotiation . 2 Aaron De Smet, Bonnie Dowling, Bryan Hancock, and Bill Schaninger, “ The Great Attrition is making hiring harder. Are you searching the right talent pools? ,” McKinsey Quarterly , July 13, 2022. We offered ideas for how organizations could look to different employee groups to help fill jobs.
Now, we turn to Europe, where the destabilizing war in Ukraine , rising inflation , and growing fears of hiring freezes and job losses have created a difficult set of conditions for companies. We wanted to know if the talent trends we’ve followed for the past two years in the United States and other countries are having a similar effect in Europe. The answer is a resounding yes. Companies can’t get the people they need, and they are losing the workers they already have, while falling behind in areas such as technology and innovation that affect the region’s long-term competitiveness . 3 Between 2014 and 2019, large European companies were 20 percent less profitable, grew revenues 40 percent more slowly, invested 8 percent less, and spent 40 percent less on R&D than other companies, according to a sample of more than 2,000 European and US companies with revenue of more than $1 billion. For more, see “Securing Europe’s competitiveness: Addressing its technology gap,” McKinsey Global Institute, September 22, 2022.
About the research
To better understand the current state of the European labor market, we surveyed 16,246 respondents in Austria (n = 1,444), Belgium (n = 1,901), France (n = 1,924), Germany (n = 1,968), Italy (n = 1,944), Poland (n = 2,012), Portugal (n = 1,958), Spain (n = 1,944), and Switzerland (n = 1,151). The survey data, collected in September 2022, included people of working age across 16 industries.
Our new analysis, which includes a survey of more than 16,000 respondents in nine European countries, shows that fully one-third of respondents say that they expect to quit their jobs in the next three to six months (see sidebar, “About the research”). While that slice of the workforce is lower than the 40 percent in our global survey from April, 4 The six countries surveyed were Australia, Canada, India, Singapore, the United Kingdom, and the United States. it is a remarkably high churn rate for Europe, where labor protections and cultural factors—not to mention a likely economic slowdown —tend to favor remaining in a job. Companies that believe attrition is a problem limited to the United States should understand that one in three of their workers may quit over the near term.
Yet high attrition is just one of the challenges facing European employers. The job vacancy rate has almost doubled, to 3 percent in June 2022, from 1.6 percent in June 2020, 5 Although the percentage of people who started a new job in the past three to six months is increasing, the job vacancy rate is still well above normal. For more, see “Job vacancy statistics,” Eurostat, September 2022. making it harder for companies to fill open positions. Organizations also face a skills gap across industries, as well as a high number of retirees who are unlikely to return to the workforce.
At the same time, European employers have an opportunity to sharpen their value proposition. They can use this moment to address chronic, systemic talent issues by offering adequate compensation, career advancement, and caring leaders, while also focusing on more recent employee needs born of the pandemic. In this article, we analyze our new data to show how companies can retain those who are considering leaving, provide support to turn “quiet quitters” into more engaged employees, and recruit top talent more effectively to build a productive workforce that can deliver in times of radical uncertainty.
The European talent landscape: Top reasons for leaving reflect shifting employee values
Our survey revealed a consistent rate of attrition, at about a third of respondents. The outlier was Poland, where half the people say that they are at least somewhat likely to leave their jobs in the next three to six months (Exhibit 1). 6 That higher number for Poland can be attributed in part to the impact of higher inflation and a refugee crisis from the war in Ukraine, along Poland’s eastern border.
That this many workers are considering leaving revealed a dramatic level of attrition for Europe, where labor protections are more extensive than in other countries. Retirement, too, is often a milestone to look forward to because of pensions and a robust social safety net. Our survey showed that 24 percent of Europeans have retired (early or of natural age) in the past seven years. In contrast with the United States, retirees in Europe aren’t as interested in returning to work for the right offer. When they do retire, they’re more likely to be gone for good 7 Only 5 percent of those who retired, early or of natural age, are planning to return to the workplace sometime in the future, our research showed. For more, see Aaron De Smet, Bonnie Dowling, Marino Mugayar-Baldocchi, and Bill Schaninger, “ Gone for now, or gone for good? How to play the new talent game and win back workers ,” McKinsey Quarterly , March 9, 2022. —reducing the pool of potential workers for European employers.
This large number of people eyeing the exits is not much lower than the 40 percent in our earlier sample of six countries. In fact, when comparing vastly different labor markets and staggered time frames—April for the global data and September for Europe—and factoring in worsening economic conditions, we see similar attrition rates. That’s not a favorable environment for European companies looking to keep and attract workers.
Despite the structural and perceived differences in the European labor market, we unexpectedly found that the top three reasons Europeans give for leaving their jobs are similar to those of our global sample: inadequate compensation, lack of career development and advancement, and uncaring and uninspiring leaders (Exhibit 2).
Fair compensation and having a clear career path are perennial top motivators for workers in any job. We consider compensation table stakes because it’s enough to buy you a seat at the table but not enough to give you a winning hand. A lack of caring leaders, also a consistent reason for why people across countries quit their jobs, has grown in importance since the pandemic began. The similarities in top quitting factors across regions and time periods show that the pandemic has normalized these employee attitudes across segments of workers.
People across age groups and experience levels are putting more emphasis on whether these factors in combination are enough to make them want to stay at an organization for the long term. They need tangible and consistent proof that they have a positive future—in other words, the whole package: compensation, caring leaders, advancement. The fact that a large number of Europeans are saying, “I need a job, but I don’t need your job,” is a clear sign of this new emphasis.
Meanwhile, other factors have grown in importance for European respondents since the pandemic began, particularly those related to unreliable and unsupportive people at work, as well as a noninclusive and unwelcoming community.
The emphasis on these relational “people factors” marks a notable mindset shift among European workers. More than ever, employees say that they need to feel engaged and supported in an inclusive and welcoming environment. Unsustainable work expectations and a lack of support for employee well-being in particular align with rates of employee burnout that McKinsey research shows are at all-time highs . 8 “ Addressing employee burnout: Are you solving the right problem? ,” McKinsey, May 27, 2022.
We also found that the reasons employees are considering changing jobs are remarkably consistent across European countries. The top two factors in every country are inadequate compensation and insufficient career advancement. But relational factors also rank highly, including having uncaring and uninspiring leaders and unsupportive coworkers.
Focus on the whole workforce (the happy, the unhappy, and the in-between)
Most Europeans in our sample say that they intend to stay on the job, and their motivations shade differently than those of their exiting counterparts. Compensation is a top reason here as well, but it is more of a hygiene factor than anything else. Motivators include flexibility, meaningful work, and supportive coworkers—once again, an endorsement of factors that have grown in importance for Europeans during the pandemic.
People stay in a job for the opposite reasons than they leave it: because they are rewarded adequately, their needs for advancement and skill building are met, and they see a future for themselves. What sets Europeans apart, though, is the degree to which they prize a safe workplace environment; that factor is in the top three for Europeans, while it is eighth overall for the global group (Exhibit 3). Reasons for that include the fact that many COVID-19 restrictions ended over the summer, leading employees to worry about how safe they would be back in the office and whether they wanted to be back at all.
Companies must continue to deliver on flexibility if they want to retain people who have not yet indicated a willingness to leave. Throughout the pandemic, employees—ranging from working parents to younger folks just starting out to workers nearing retirement age—all say that they want more control over their working hours so that they can better balance life and career . 9 “ To slow down attrition, pay closer attention to what workers really need ,” McKinsey, September 22, 2022.
This raises a crucial point: in crafting an alluring employee experience, European organizations have to avoid falling into the trap of focusing solely on the workers who are unhappy enough to quit over the short term. Of course, it’s essential to retain them, but companies also need to be sure that the majority who aren’t indicating that they are leaving don’t move into that category.
In other words, leaders have to care about retaining talent before they can start to think about those who are walking out the door. Making the organization sticky, which we discuss below, is part of that active investment in the entire workforce.
The sound of ‘quiet quitting’
To help assess all their workers, companies can group their employees in four broad categories—those who are happy with their job but are considering better options, those leaving because they dislike their job, those staying because they’re happy, and those who are passively staying but who don’t really want to be there. This last group consists of “quiet quitters,” or members of the employed-yet-disengaged workforce. 10 This group does not include individuals who continue to be engaged in their roles but who have sought to reduce their workloads to a more manageable level to prevent burnout.
European employers, like organizations everywhere now, face the problem of workers who leave—and workers who stay but who might act like they have already left. Our research shows that in Europe, the majority (79 percent) of those reporting low levels of engagement or support factors are likely to leave. However, a small but significant portion (21 percent) of those reporting low levels of engagement or support factors are planning to stay at their jobs. Although these employees aren’t quitting, they are likely to become disengaged from their work, which could manifest as withdrawal from or neglect of their duties.
If we do the math, with one-third leaving and one-fifth of those who remain falling into the ranks of those not necessarily working to pace, that adds up to about 44 percent of the workforce. Clearly, that number of dissatisfied employees is not sustainable in a healthy organization.
Some employers believe that quiet quitting is just a phase, but there are two reasons to discount that. One is that despite the trendy name, quiet quitters have been around forever—as people whose level of engagement is below what managers might want. The other is that in a predicted economic downturn, when companies are often forced to turn to hiring freezes or job cuts, they will need the workforce that remains to be that much more productive.
Quiet quitting is not just an individual problem, it’s a mutual responsibility between the employee who is disengaged and the organization that isn’t offering enough support. Both higher engagement and higher support are needed to solve this problem.
An overwhelming majority of employees who report high levels of engagement factors (such as finding meaning in their work) and support factors (such as reliable and supportive people at work) are likely to stay at their jobs and be productive in them (Exhibit 4).
The (new) value system: Emphasize personal development and recognition to reward workers
Europe’s labor market is unique, with stronger worker protections, more extensive pension offerings, and longer parental leaves, to name but a few examples that benefit employees—and society writ large. Culturally, workers in this region don’t leave their jobs as often as those in the United States and other countries do.
However, with an aging population and a darkening economic picture, European employers face a complex environment in which to operate. This calls for more creative solutions. Companies can draw inspiration from the way other organizations, even those in other regions, are attempting to solve the problem that attrition brings. They can find novel ways to attract younger people to jobs and keep the workers they have feeling more engaged and productive.
Here are five ways that European companies can be proactive about retention, reinforce a healthy working environment, and look beyond traditional recruitment pools.
Address the attrition
The first step is to turn inward. Companies should take stock of the attrition they have already experienced and move to reduce further quitting by addressing what is motivating their employees. Our European data shows that the reasons people have left a job and why they plan to leave are the same, so companies can get ahead of the next wave of attrition by understanding why others have already left. Employers should consider doubling down on providing adequate total compensation packages, investing in employees’ development, and providing meaningful advancement opportunities, while showing more caring and inspiring day-to-day and strategic leadership .
Don’t overlook ‘the others’
When companies focus mostly on attrition and attraction, they tend to overlook the need to actively support workers who are staying. Sticky companies anticipate and address employees’ concerns . They ask people what they need to be successful in their roles—and they listen to the answers. They push people to grow in their jobs and encourage a growth mindset throughout the organization. Based on feedback, these companies might innovate jobs, teams, or hiring practices. They are not afraid to provide the flexibility that employees need to create a work–life balance that helps keep workers engaged and productive. These cultural factors help make a company more attractive to join and, ideally, provide more incentives for employees to stay and remain engaged. They can also reengage those who are quietly quitting.
Reward loyalty by building capabilities
Career advancement is a top priority for European workers. A company that rewards its employees by investing in their development reduces their incentive to look elsewhere while also increasing overall engagement. With that in mind, leaders can start by rewarding those who are already inside the company with career development and advancement opportunities. This investment in the workforce is based on gratitude and trust, highlighting that past work is valued and that the company believes in their employees’ ability to deliver the future work that builds value. Then, leaders can look outside the company to deliberately find the talent that they still need. In the broader context, Europe is experiencing a widening gap in technology, innovation, and corporate performance compared with other regions. With recent headlines of job losses in the technology sector, companies that need to expand their tech expertise could look to those who are newly available. However, companies should also focus on using the right levers to prevent those potential hires from going to a nontraditional job, or worse, to the competition.
Rethink the corporate culture
Since the start of the pandemic, organizations have been striving to help employees who are burned out. However, it’s crucial to focus on affirmative behaviors so that burnout doesn’t become a problem to begin with. Once it takes hold, even the most well-intentioned remediation efforts (or yoga classes) won’t fix the problem. As our survey data shows, European workers now emphasize other factors when it comes to a satisfying employee experience. They want more workplace flexibility and a physically and psychologically safe workplace . 11 “ Psychological safety, emotional intelligence, and leadership in a time of flux ,” McKinsey Quarterly , July 2, 2020. McKinsey research shows that caring managers can also make a huge difference in engagement by reaching out more frequently and honing in on what excites employees and gives them a sense of purpose.
Think outside the (recruitment) box
The existing talent pools of traditional workers in an aging market are not sufficient to replenish those who have retired. European organizations will need to go after those who have left the traditional workforce, including people who are self-employed, those in the gig economy or not currently in full-time corporate jobs, younger people just entering the workforce, and those who are considering retirement. Because these groups emphasize different factors (with older workers wanting more caring leaders and younger people valuing strong support networks), companies must target these groups differently. And while these pools of workers may be smaller in Europe than they are in the United States, for example, they’re out there, and companies can go get them.
The European workforce is not immune to the attrition trend we’ve seen sweep across countries over the past several years. The mindsets of European employees have changed since the pandemic began, and many are no longer willing to stay at organizations that don’t value their contributions or offer a future that excites them. Now more than ever, companies should demonstrate a commitment that is both widespread and targeted to individuals—a commitment that is core to their health and future growth.
Vincent Bérubé is a senior partner in McKinsey’s Montréal office, Dana Maor is a senior partner in the Tel Aviv office, Marino Mugayar-Baldocchi is a research science expert in the New York office, and Angelika Reich is a partner in the Vienna office.
The authors wish to thank Nancy Busellato, Pawel Poplawski, Mukhunth Raghavan, and Bill Schaninger for their contributions to this article.
This article was edited by Barbara Tierney, a senior editor in the New York office.
Explore a career with us
Related articles.

The Great Attrition is making hiring harder. Are you searching the right talent pools?
‘Great Attrition’ or ‘Great Attraction’? The choice is yours
Securing Europe’s competitiveness: Addressing its technology gap
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Articles in 2022

One year on
As we celebrate the first anniversary of Nature Reviews Psychology , we look back at year one.
Lived experiences of coercive intervention in psychosis
- Jenn Richler
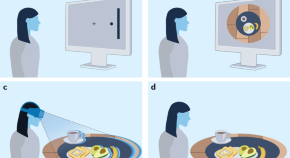
Spatial coding for action across spatial scales
Complex spatial cognition supports seemingly simple actions such as picking up a coffee mug. In this Review, Fiehler and Karimpur discuss the spatial coding underlying such actions, highlighting high-level factors and suggesting that research should integrate across spatial scales.
- Katja Fiehler
- Harun Karimpur
Computational psychiatry and the lived experience of mental illness
The next generation of translational measures must exhibit greater construct validity in their capacity to capture the dynamic nature of mental illness.
- Michael T. Treadway

Enumeration across the visual field
- Teresa Schubert
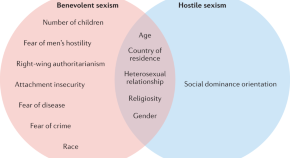
Benevolent and hostile sexism in a shifting global context
Sexism encompasses attitudes that are both overtly negative and those that seem subjectively positive but are actually harmful. In this Review, Barreto and Doyle describe the predictors of ambivalent sexism and its effects on women, and consider societal shifts that might influence how sexism is manifested, experienced and understood.
- Manuela Barreto
- David Matthew Doyle
Understanding attention with a computational model
- Jasmine Pan

The fundamental importance of method to theory
Philosophers of science have identified epistemological criteria for evaluating the promise of a scientific theory. In this Perspective, Dale et al. propose that a principle of methodological variety should be one of these criteria, and argue that psychologists should actively cultivate methodological variety to advance theory.
- Anne S. Warlaumont
- Kerri L. Johnson

Learned industriousness as a translational mechanism in anorexia nervosa
Individuals with anorexia nervosa persistently exert effortful behaviour such as restrictive eating that most individuals find aversive. In this Perspective, Haynos et al. propose a novel mechanistic account for why such behaviours persist from the social psychology theory of learned industriousness.
- Ann F. Haynos
- Emily Koithan
- Kelsey E. Hagan
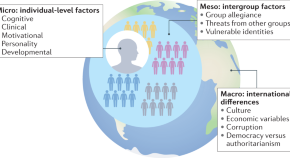
Individual, intergroup and nation-level influences on belief in conspiracy theories
Conspiracy theories have the potential to undermine governments, promote racism, ignite extremism and threaten public health efforts. In this Review, Hornsey et al. synthesize the literature on factors that shape conspiracy beliefs at the individual, intergroup and national level.
- Matthew J. Hornsey
- Kinga Bierwiaczonek
- Karen M. Douglas

Single case studies are a powerful tool for developing, testing and extending theories
The majority of methods in psychology rely on averaging group data to draw conclusions. In this Perspective, Nickels et al. argue that single case methodology is a valuable tool for developing and extending psychological theories, with applied benefits of understanding neuropsychological deficits and developing interventions.
- Lyndsey Nickels
- Simon Fischer-Baum
Revisiting person–situation interactionism
Norm messaging counters the gender pay gap.
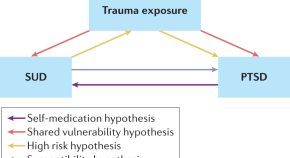
Trauma-focused treatment for comorbid post-traumatic stress and substance use disorder
Post-traumatic stress disorder and substance use disorder frequently co-occur, and this combination is more difficult to treat than either disorder alone. In this Review, Kline and colleagues discuss effective treatments for this combination, focusing on trauma-focused treatments, and provide recommendations to improve treatment response and reduce dropout.
- Alexander C. Kline
- Kaitlyn E. Panza
- Sonya B. Norman
Examining mental disorders with computational neuroscience
Perceiving the probable present.
- William Turner
Labels aid visual working memory
Post-publication dialogue.
Our Correspondence section provides a forum to discuss content published in the journal.
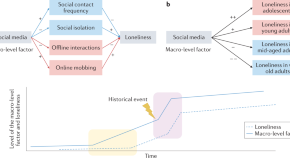
Loneliness across time and space
People feel lonely when their social needs are not met, which can lead to long-term health issues. In this Review, Luhmann et al. summarize empirical findings on differences in the prevalence of loneliness across time and space and consider macro-level factors that might account for these differences.
- Maike Luhmann
- Susanne Buecker
- Marilena Rüsberg
Ambiguous perception from bottom to top
- Caroline Myers
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
COMMENTS
Articles in 2022. Filter By: Article Type. All. All; Article (1079) Author Correction (78) ... Research Highlight 22 Dec 2022. Daily briefing: Watch spines form in an artificial human embryos.
In this end-of-year roundup, we share key insights and trends from HBR's most-read research articles of 2022, exploring topics from embracing a new identity to fostering equity in the workplace ...
Smartphones dependency risk analysis using machine-learning predictive models. Claudia Fernanda Giraldo-Jiménez. Javier Gaviria-Chavarro. André Luiz Felix Rodacki. Article Open Access 31 Dec 2022.
Journal Top 100 - 2022. This collection highlights our most downloaded* research papers published in 2022. Featuring authors from around the world, these papers highlight valuable research from an ...
A healthcare worker administers COVID-19 booster shots at a vaccination clinic in April 2022 in San Rafael, California. ... The research led to the surprising revelation that early humans ...
Show / hide sections navigation 2022 Breakthrough of the Year Runners-up Breakdowns Videos. On 11 July, in a live broadcast from the White House, U.S. President Joe Biden unveiled the first image from what he called a "miraculous" new space telescope. ... Last year, the research lab OpenAI presented a software system called DALL-E that when ...
stories of 2022. Previously excavated bodies of two ritually sacrificed Inca children, including this girl still wearing a ceremonial headdress, have yielded chemical clues to a beverage that may ...
By Frontiers' science writers Image: Shutterstock.com As part of Frontiers' passion to make science available to all, we highlight just a small selection of the
1. Like this meta-analysis: Screen media and mental health. Ferguson, C. J., et al. This meta-analysis in Professional Psychology: Research and Practice (Vol. 53, No. 2) suggests that exposure to screen time, including smartphones and social media, is not linked to mental health issues in adults or children. Researchers analyzed 37 data sets from 33 separate studies published between 2015 and ...
Inflation in the U.S. at a 40-year high. Small talk around the watercooler (mainly the virtual one, nowadays) certainly feels heavier than it used to. Recent Gallup data indicates that in 2022, companies and managers remain challenged by the task of raising employee engagement to pre-pandemic levels. Nearly half of global workers (44%) surveyed ...
January 25, 2022. Prevalence and Durability of SARS-CoV-2 Antibodies Among Unvaccinated US Adults by History of COVID-19. JAMA. Research Letter. March 15, 2022. Association Between 3 Doses of mRNA COVID-19 Vaccine and Symptomatic Infection Caused by the SARS-CoV-2 Omicron and Delta Variants. JAMA.
To mark the end of the year, MIT News is looking back at 10 of the research stories that generated the most excitement in 2022. We've also rounded up the year's top MIT community-related stories. Designing a heat engine with no moving parts. In April, engineers at MIT and the National Renewable Energy Laboratory (NREL) designed a heat ...
In May 2022, the FDA approved tirzepatide, a GIP and GLP-1 RA, for once-weekly subcutaneous administration to improve glucose control in adults with type 2 diabetes as an addition to healthy eating and exercise. ... Several key areas where further research could better inform future consensus reports were of particular interest to the writing ...
NASA's busiest year in decades - an astronomer sums up the dizzying array of missions in 2022. Chris Impey, University of Arizona. NASA has been gaining momentum in recent years as investment ...
Research Highlight 02 Dec 2022 New Year's fireworks chase wild geese high into the sky Tracking data show that the birds fly farther than usual on the last evening of the year and are more ...
Research Article May 31, 2024. Manipulating ultrafast even-order nonlinear chiral responses of L-tryptophan by polarization pulse shaping. Jérémy R. Rouxel, Yeonsig Nam, Vladimir Y. Chernyak, Shaul Mukamel, This is an addendum to Complex viscosity of helical and doubly helical polymeric liquids from general rigid bead-rod theory.
In 2022, 21 Research Exchange articles were published, which represent a 50% increase from the previous volume year (Volume 45 (2021), n = 14). With this increase in published Research Exchange, the journal published one less full-length article in 2022 (n = 57) when compared to the previous volume year (n = 58). Additionally ...
Brian Kropp is chief of research for the Gartner HR practice, which delivers insights and solutions that address new and emerging executive challenges and enable HR leaders to take decisive ...
This article summarizes the top 20 research studies of 2022 identified as POEMs (patient-oriented evidence that matters), excluding COVID-19. Statins for primary prevention of cardiovascular ...
2. More Proof That Money Can Buy Happiness (or a Life with Less Stress) It's not about the bigger home or the better vacation. Financial stability helps people escape the everyday hassles of life, says research by Jon Jachimowicz. 3. Curiosity, Not Coding: 6 Skills Leaders Need in the Digital Age.
Objective To examine the effects of fish oil supplements on the clinical course of cardiovascular disease, from a healthy state to atrial fibrillation, major adverse cardiovascular events, and subsequently death. Design Prospective cohort study. Setting UK Biobank study, 1 January 2006 to 31 December 2010, with follow-up to 31 March 2021 (median follow-up 11.9 years). Participants 415 737 ...
Large-scale genotyping and phenotyping of a worldwide winter wheat genebank for its use in pre-breeding. Albert W. Schulthess. Sandip M. Kale. Jochen C. Reif. Data Descriptor Open Access 26 Dec 2022.
More than 100 million U.S. adults have been diagnosed with hypertension, one of the leading risk factors for cardiovascular disease.While more than 70% of people with hypertension cannot achieve adequate blood pressure control with just one drug, current guidelines only make recommendations for first-line therapy.
Antiretroviral Drugs for HIV Treatment and Prevention in Adults - 2022 IAS-USA Recommendations CONSERVE 2021 Guidelines for Reporting Trials Modified for the COVID-19 Pandemic Creation and Adoption of Large Language Models in Medicine Global Burden of Cancer, 2010-2019 Global Burden of Long COVID Global Burden of Melanoma Global Burden of Skin ...
How to play the new talent game and win back workers ," McKinsey Quarterly, March 9, 2022. —reducing the pool of potential workers for European employers. This large number of people eyeing the exits is not much lower than the 40 percent in our earlier sample of six countries. In fact, when comparing vastly different labor markets and ...
Misinformation is false or inaccurate information—getting the facts wrong. Disinformation is false information which is deliberately intended to mislead—intentionally misstating the facts. The spread of misinformation and disinformation has affected our ability to improve public health, address climate change, maintain a stable democracy ...
In 2022, with increasing population level immunity, there will be substantial reductions in the number of people experiencing severe disease and death. ... Research articles Reviews & Analysis ...
Reports the retraction of "Predictors of depression among school adolescents in Northwest, Ethiopia, 2022: Institutional based cross-sectional" by Aklile Tsega Chekol, Mastewal Aschale Wale, Agmas Wassie Abate, Eyerusalem Abebe Beo, Eman Ali Said and Berhan Tsegaye Negash (BMC Psychiatry, 2023[Jun][14], Vol 23[1][429]). The Editors have retracted this article after concerns were raised.
Research Highlight 09 Dec 2022 Benevolent and hostile sexism in a shifting global context Sexism encompasses attitudes that are both overtly negative and those that seem subjectively positive but ...
Former President Trump declared himself a "very innocent man" on Thursday and said the U.S. has "has gone to hell" after becoming the first American president to be convicted of a felony.. The big picture: Trump joins a long list of leaders across at least 78 countries who, since 2000, have left office and been jailed or prosecuted — including in democracies like France, Israel and South Korea.