Content Type
Topic Categories
- Data Visualization
- Research Briefs
- Email Signup
- Careers & Internships
- Terms & Conditions
- Privacy Policy
Home > Topics > Community Health Workers: Their Important Role in Public Health
Infographics

Community Health Workers: Their Important Role in Public Health
Coronavirus / Health Care Coverage
Published on: April 07, 2021. Updated on: April 13, 2021.
This infographic shows how Community Health Workers (CHWs) promote health equity and improve public health. The CHW workforce is diverse, growing, and drawing attention to its ability to address determinants of poor health. As trusted advocates, educators and counselors embedded in their communities, CHWs facilitate culturally competent service delivery. Tapping into this workforce can strengthen the response to COVID-19 and address longstanding inequities.
This infographic was reviewed by Denise Octavia Smith, MBA, CHW, PN, Founding Executive Director of the National Association of Community Health Workers .
Community health workers definitions : “Community Health Workers.” American Public Health Association.
CHWs’ many titles : “CDC - Community Health Worker Resources - STLT Gateway.” Centers for Disease Control and Prevention, 18 Aug. 2016.
Not defined by training : Opinion by Kangovi, Shreya, et al. “Opinion: This Group of Workers Could Help Turnaround Quality of Life -- and the Economy.” CNN, 10 Feb. 2021.
Advance health equity, improve health outcomes, and reduce health care costs : “Community Health Workers: Evidence of Their Effectiveness.” Association of State and Territorial Health Officials and the National Association of Community Health Workers.
Addressing social determinants of health : Peretz, Patricia J., et al. “Community Health Workers and Covid-19 - Addressing Social Determinants of Health in Times of Crisis and Beyond: NEJM.” New England Journal of Medicine, 10 Mar. 2021.
Root causes of poor health: Opinion by Kangovi, Shreya, et al. “Opinion: This Group of Workers Could Help Turnaround Quality of Life -- and the Economy.” CNN, 10 Feb. 2021.
Examples of services CHWs provide:
- Outreach, community education, informal counseling, social support and advocacy : “Support for Community Health Workers to Increase Health Access and to Reduce Health Inequities.” American Public Health Association. 10 Nov. 2009
- Translation/interpreting, health care navigation, and tracking progress : “Rural Health Information Hub.” Community Health Workers in Rural Settings Introduction.
86,000 CHWs : "Community Health Worker National Workforce Study." U.S. Department of Health and Human Services Health Resources and Services Administration Bureau of Health Professions. March 2007.
Expected increase : “Health Educators and Community Health Workers: Occupational Outlook Handbook.” U.S. Bureau of Labor Statistics, U.S. Bureau of Labor Statistics, 1 Sept. 2020.
Call for rapid increase: NACHW National Policy Platform: Policy Recommendations to Respect, Protect and Partner with Community Health Workers During the Pandemic and Beyond.
President Biden’s proposal : “President Biden Announces American Rescue Plan.” The White House, The United States Government, 20 Jan. 2021.
American Rescue Plan : Yarmuth, John A. “H.R.1319 - 117th Congress (2021-2022): American Rescue Plan Act of 2021.” Congress.gov, 11 Mar. 2021,
Partners in Health : “Public Health Job Corps: Responding to COVID-19, rebuilding the community health workforce.” Partners in Health United States. Updated 22 Jan. 2021.
CHWs sharing characteristics with community members : “Role of Community Health Workers.” National Heart Lung and Blood Institute, U.S. Department of Health and Human Services.
CHW race and ethnicity : National Community Health Worker Advocacy Survey: 2014 Preliminary Data Report for the United States and Territories. Tucson, Arizona: Arizona Prevention Research Center, Zuckerman College of Public Health, University of Arizona; 2014.
Bilingual : “Community Health Workers in the Midwest: Understanding and developing the workforce” Wilder Research, June 2012.
CHW Employers : “Health Educators and Community Health Workers: Occupational Outlook Handbook.” U.S. Bureau of Labor Statistics, U.S. Bureau of Labor Statistics, 1 Sept. 2020.
Shift CHW employment : Malcarney MB, Pittman P, Quigley L, Horton K, Seiler N. The Changing Roles of Community Health Workers. Health Serv Res. 2017;52 Suppl 1(Suppl 1):360-382. doi:10.1111/1475-6773.12657
Evidence of CHWs Effectiveness : “Community Health Workers: Evidence of Their Effectiveness.” Association of State and Territorial Health Officials and the National Association of Community Health Workers.
- $2.47:1 return on investment : Kangovi, Shreya, et al. “Evidence-Based Community Health Worker Program Addresses Unmet Social Needs And Generates Positive Return On Investment: Health Affairs Journal.” Health Affairs, 1 Feb. 2020.
- 34% decrease in days in hospitals: Vasan, A, Morgan, JW, Mitra, N, et al. Effects of a standardized community health worker intervention on hospitalization among disadvantaged patients with multiple chronic conditions: A pooled analysis of three clinical trials. Health Serv Res. 2020; 55: 894– 901.
- Improve Glycemic Control : Palmas W, March D, Darakjy S, Findley SE, Teresi J, Carrasquillo O, Luchsinger JA. Community Health Worker Interventions to Improve Glycemic Control in People with Diabetes: A Systematic Review and Meta-Analysis. J Gen Intern Med. 2015 Jul;30(7):1004-12.
- Mental Health : Weaver A, Lapidos A. Mental Health Interventions with Community Health Workers in the United States: A Systematic Review. J Health Care Poor Underserved.
Role of CHWs in COVID-19 response:
- Advocate for vaccinations : “Joint Statement on Ensuring Racial Equity in the Development and Distribution of a COVID-19 Vaccine.” Health Leads, 26 Jan. 2021.
- Trusted messengers : “To Strengthen The Public Health Response To COVID-19, We Need Community Health Workers, " Health Affairs Blog, May 6, 2020.
- Build Capacity : Advancing Equity & Public Health: The Community-Based Workforce Alliance.
- Address social needs and ensure care : Peretz, Patricia J., et al. “Community Health Workers and Covid-19 - Addressing Social Determinants of Health in Times of Crisis and Beyond: NEJM.” New England Journal of Medicine, 10 Mar. 2021.
Recommendations and strategies for supporting this workforce:
- Funding, training, integrate, and promote : “Advancing the Profession of Community Health Workers: CHRT.” Center for Health & Research Transformation, 19 Feb. 2021.
- Combat compassion fatigue : “Battling Burnout: Self-Care and Organizational Tools to Increase Community Health Worker Retention and Satisfaction.” Health Leads, 23 Jan. 2020.
- More research is needed : Peretz, Patricia J., et al. “Community Health Workers and Covid-19 - Addressing Social Determinants of Health in Times of Crisis and Beyond: NEJM.” New England Journal of Medicine, 10 Mar. 2021.
The National Association of Community Health Workers :
An Environmental Scan to Inform Community Health Worker Strategies within the Morehouse National COVID-19 Resiliency Network : Jane Berry, Aurora GrantWingate, and Denise Octavia Smith. The National Association of Community Health Workers, the Morehouse School of Medicine, and the National COVID-19 Resiliency Network. December 2020.
NACHW National Policy Platform : Policy Recommendations to Respect, Protect and Partner with Community Health Workers During the Pandemic and Beyond.
The Penn Center for Community Health Workers
Rural Community Health Workers Toolkit : Rural Health Information Hub
Robert Wood Johnson Foundation’s Culture of Health Blog : Proctor, Dwayne. “Community Health Workers: Walking In The Shoes of Those They Serve.” RWJF , 2 Feb. 2021.
Marill, Michele Cohen. “Community Health Workers, Often Overlooked, Bring Trust to the Pandemic Fight.” Kaiser Health News , 10 Feb. 2021 .
Waters, Rob, et al. “Community Workers Lend Human Connection To COVID-19 Response: Health Affairs Journal.” Health Affairs , 1 July 2020,
Shreya Kangovi, Uché Blackstock. “Opinion | Community Health Workers Are Essential in This Crisis. We Need More of Them.” The Washington Post , WP Company, 3 July 2020.
We think you'll also like
March 25, 2021
Community Health Workers & Pharmacists: Their Frontline Role in the Response to COVID-19
Get nihcm updates
Updates on timely topics and webinars delivered to your inbox
More Related Content
May 01, 2024
Telehealth: A Vital Piece of the Care Access Puzzle
Cost & Quality / Affordability / Health Care Coverage / Health Care Reform
Mini-Infographics
Published on: January 11, 2024.
Respiratory Illnesses are Elevated Across the Country
Coronavirus
Research Insights
Published on: November 08, 2023. Updated on: November 08, 2023.
The Health & Economic Consequences of Firearm Injuries in Children on Survivors & Families
Cost & Quality / Behavioral Health / Health Care Coverage / Social Determinants of Health
See More on: Coronavirus | Health Care Coverage
SYSTEMATIC REVIEW article
Positionality of community health workers on health intervention research teams: a scoping review.

- 1 Mel and Enid Zuckerman College of Public Health, University of Arizona, Tucson, AZ, United States
- 2 University of Arizona Health Sciences Library, University of Arizona, Tucson, AZ, United States
Community health workers (CHWs) are increasingly involved as members of health intervention research teams. Given that CHWs are engaged in a variety of research roles, there is a need for better understanding of the ways in which CHWs are incorporated in research and the potential benefits. This scoping review synthesizes evidence regarding the kinds of health research studies involving CHWs, CHWs' roles in implementing health intervention research, their positionality on research teams, and how their involvement benefits health intervention research. The scoping review includes peer-reviewed health intervention articles published between 2008–2018 in the U.S. A search of PubMed, Embase and CINAHL identified a total of 3,129 titles and abstracts, 266 of which met the inclusion criteria and underwent full text review. A total of 130 articles were identified for a primary analysis of the research and the level of CHWs involvement, and of these 23 articles were included in a secondary analysis in which CHWs participated in 5 or more intervention research phases. The scoping review found that CHWs are involved across the spectrum of research, including developing research questions, intervention design, participant recruitment, intervention implementation, data collection, data analysis, and results dissemination. CHW positionality as research partners varied greatly across studies, and they are not uniformly integrated within all stages of research. The majority of these studies employed a community based participatory research (CBPR) approach, and CBPR studies included CHWs as research partners in more phases of research relative to non-CBPR studies. This scoping review documents specific benefits from the inclusion of CHWs as partners in health intervention research and identifies strategies to engage CHWs as research partners and to ensure that CHW contributions to research are well-documented.
Introduction
Using the community health worker (CHW) workforce in health promotion programs to reach vulnerable and marginalized populations has become a best practice in addressing health disparities. A CHW is “a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served” ( 1 ). CHWs work under a variety of job titles, including promotores de salud , community health advisors, community health representatives, lay health advisors, and outreach workers. CHWs leverage their deep connections within the community to be a liaison between health services and community residents. In this effort, CHWs assume diverse and wide-ranging responsibilities, including patient outreach, health education and assessments, care coordination, cultural mediation between individuals and social service systems, and individual and community advocacy ( 2 ). Studies have shown that CHWs are highly effective in increasing healthcare utilization ( 3 – 6 ), preventive screening ( 7 ) and health behavior change ( 8 ).
While research on CHW interventions has demonstrated effectiveness in improving health outcomes, CHWs themselves are increasingly incorporated as members of intervention research teams ( 9 , 10 ). This activity is reflected in the Progress Report of the Community Health Worker (CHW) Core Consensus (C3) Project, a recent national study and consensus-building process to revisit CHW core competencies which added participation in evaluation and research as a new CHW core role and competency ( 2 ). The CHW profession encompasses competencies that have potential benefit to health intervention research ( 2 , 10 – 12 ). They have a deep understanding of the challenges faced by their communities and can ensure that health interventions address communities' needs. As trusted individuals, CHWs may be well-positioned to involve community members in research studies, particularly among underserved populations ( 12 – 14 ). CHWs can utilize their cultural insights to ensure that intervention implementation and data collection methodologies are responsive to community norms, language(s), and beliefs ( 12 ). Scholars have also noted that CHWs' input can be essential to interpreting participants' experiences and perspectives, thus elevating community members' voices within research and improving the quality of the data analysis ( 10 , 15 , 16 ).
Community-based participatory research (CBPR) that seeks to engage community members as partners may be more likely to incorporate CHWs to increase representation of community priorities ( 2 , 17 , 18 ). The CBPR approach intentionally delineates each phase of the research as an opportunity for community engagement, and CHWs' immersion within their communities positions them to represent and/or facilitate the engagement of community members in CBPR studies. While CHWs possess critical assets and skills to participate meaningfully across all phases of research, it is unknown the extent to which researchers engage with CHWs as partners, thus accessing their full scope of practice.
This article describes the results of a scoping review designed to synthesize the nature of CHW involvement across the phases of research, with the overall aim of identifying specific ways in which this workforce can enhance the quality of health intervention studies. The general purpose of a scoping review is to map key concepts underpinning a research area, especially one that is complex and/or understudied ( 19 ). In conducting the scoping review, we examined the following questions: (1) What types of research studies involve CHWs? (2) How are CHWs involved across the phases of research? (3) What is the nature of CHW positionality on research teams? (4) In what ways does CHW involvement benefit the quality of health intervention research?
Materials and Methods
Search strategy.
An initial review of the Joanna Briggs Institute Database of Scoping Reviews and Implementation Reports, the Cochrane Database of Scoping Reviews, and the Campbell Collection confirmed no existing scoping review on the subject area of CHW roles in intervention research. We collaborated with a medical librarian to design a comprehensive search strategy by developing terms for the concept areas “community health workers,” to identify CHWs working under an array of job titles, and “community-based participatory research,” to ensure that we were identifying studies that were most likely to engage the CHW workforce. Because our search term domains have numerous synonyms, we developed a full list of search terms for each. We then conducted a search for English-language articles in the electronic databases PubMed, Embase, and CINAHL on September 28, 2018.
Inclusion and Exclusion Criteria
We referred to pre-specified inclusion and exclusion criteria for both title and abstract screening and subsequent full-text review. During title and abstract screening, we applied the following criteria:
1. Articles were peer-reviewed health intervention studies published from 2008–2018
2. Articles included study results
3. Articles included “CHW” (or an alternative name included within our search) within the title and/or abstract
4. Article's description of CHWs aligns with the APHA's definition
5. Articles described interventions within the U.S.
We excluded gray literature, study protocol papers, conference abstracts, formative research (i.e., focus groups, needs assessments), literature reviews, trainings, process evaluations (no outcome data), secondary data analyses, and articles presenting only baseline results of health interventions. We focused on interventions from the U.S. only given that the aforementioned C3 report had newly identified participation in research and evaluation as a new competency for CHWs within the U.S. only. We excluded interventions that involved patient navigators and health educators based upon the CHW Standard Occupational Classification, which differentiates these positions from CHWs ( 20 ). We also ensured that the article's description of CHWs aligned with the APHA definition of CHWs ( 1 ). If it was also not explicit that the CHWs were from the community served, the article was excluded.
Study Screening
Two authors independently screened all titles and abstracts and reviewed the selected full-text articles using Covidence, a web-based program to manage literature reviews. Disagreement between reviewers was resolved through direct discussion at all stages.
Data Extraction
Two reviewers, the first and second author, independently extracted relevant data from the included studies into separate but identical Excel spreadsheets. Within the primary analysis, we noted characteristics of the health intervention, including intervention focus, study design (if the study was a randomized-control trial or not), if the study methodology included a CBPR approach, the target population and the CHW job title CHW (i.e., CHW, lay health worker, promotora , etc.). Reviewers then assessed CHW involvement (CHWs involved = 1, CHWs not involved = 0) across the following research phases: identifying the research question; intervention design; instrumentation/measurement design; recruitment/participant eligibility; intervention implementation; data collection; data analysis; and dissemination/action. Lastly, the reviewers sought to ascertain the level of expertise of CHWs by evaluating the described training and experience, with a specific focus on CHW core competencies ( 2 ). CHW core competencies refer to core roles and skills that constitute CHWs' full scope of practice such as cultural mediation, providing culturally appropriate health education and relationship building ( 2 ). Those studies that hired explicitly experienced CHWs, we interpreted as CHWs proficient in the core competencies. The reviewers then compared the information extracted and resolved any discrepancies in intervention characteristics through reexamination of the article. We calculated the total number of research phases in which CHWs were involved for each article, as well as the percentage of studies that included CHWs in each phase. To explore the benefits of CHW involvement, we conducted a secondary analysis of those articles in which CHWs were involved in 5 or more research phases.
The initial search resulted in a total of 3,129 articles for review ( Figure 1 ). After removing duplicates in Endnote, we reviewed 2,754 titles and/or abstracts articles against the inclusion criteria to determine eligibility for full-text review. A total of 266 articles underwent full-text review, and 130 articles fitting the criteria were included in the primary analysis (the list of all articles and their full citations is available in Data Sheet 1 ). For the secondary analysis, we extracted additional information from 23 of the articles which described research projects in which CHWs participated in 5 or more phases.
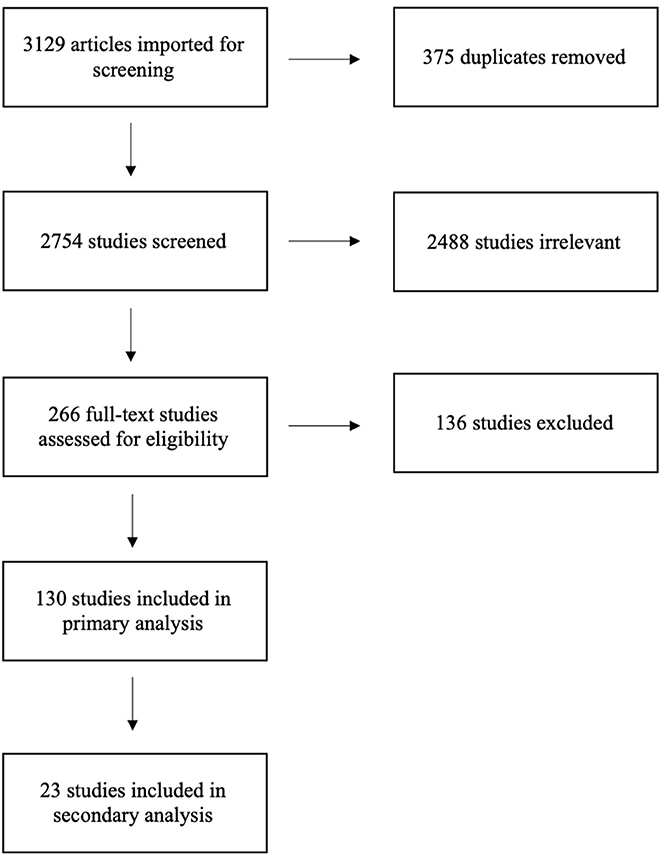
Figure 1 . PRISMA Flow Diagram of Scoping Review Process for Examining CHWs in Research.
Table 1 summarizes the characteristics of the 130 health intervention studies, the number of research phases engaging CHWs, and types of CHW training. More than half of the studies (51.5%) focused on disease prevention and promotion and 25.4% of studies targeted individuals with a chronic disease. As expected, the majority (60%) were CBPR studies, while the remaining 40% were non-CBPR studies. Additionally, 43.1% of the studies were randomized-control trials, while the remainder employed quasi-experimental or non-experimental study designs. Across the phases of research, almost all studies (98.5%) utilized CHWs to implement the health intervention. CHWs were also frequently involved in participant eligibility and/or recruitment (57.6%) and data collection (49.2%). CHWs were much less frequently involved in identifying the research question (10.8%), data analysis (2.3%), and research dissemination/action (10.8%).
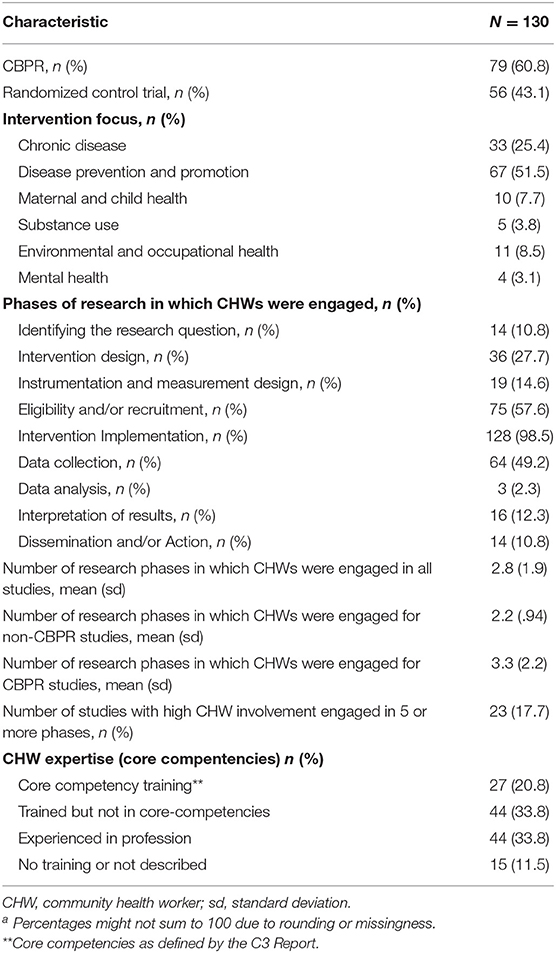
Table 1 . Summary of health intervention characteristics, CHW research engagement, and CHW training. a
In examining CHW expertise, 33.8% of the studies worked with experienced CHWs and an additional 20.8% of the studies trained newly hired CHWs in core competencies. Another 33.8% provided training with CHWs that did not explicitly include core competencies. The remaining studies (11.5%) either didn't describe the training provided or did not mention training or experience of the CHWs. Notably, 64.6% of CBPR studies included CHWs proficient in core competencies, compared to 39.2% among non-CBPR studies. This suggests that participatory researchers may have greater understanding of the relevance of the broader scope of practice in CHW effectiveness. Additionally, the range CHW involvement across phases for non-CBPR studies was one to four, while CBPR studies engaged CHWs in one to nine phases. However, the research goals of the non-CBPR studies were less focused on community engagement and may have been less likely to benefit from CHWs' strengths as a workforce.
Although not documented in Table 1 , the target populations of the interventions varied by race and ethnicity, disease focus (i.e., diabetes, hypertension), health behavior (i.e., physical activity), occupation, and/or geographic location. The titles of the CHWs within the interventions were wide-ranging, and included promotoras , lay health workers, lay health advisors, community health advisor, community health coaches, community wellness coaches, care guides, resident health advocates, and women's health advocates.
Secondary Analysis
To identify the characteristics of studies that utilized a broader scope of CHW practice and examine the extent to which the research benefited from CHW involvement, we reviewed those studies in which CHWs engaged in five or more phases ( n = 23). These studies all described utilizing a CBPR approach. For each study, we documented and synthesized the articles' descriptions of CHW roles and contributions to the quality of the study. Table 2 summarizes the results of the secondary analysis. Notably, in all but four studies, the CHWs were described as experienced or were trained in core competencies as part of the study. Across the studies, CHWs were also trained in intervention delivery, data collection methodologies, research principles, health conditions/diseases, program development, advocacy, and coalitions/networking.
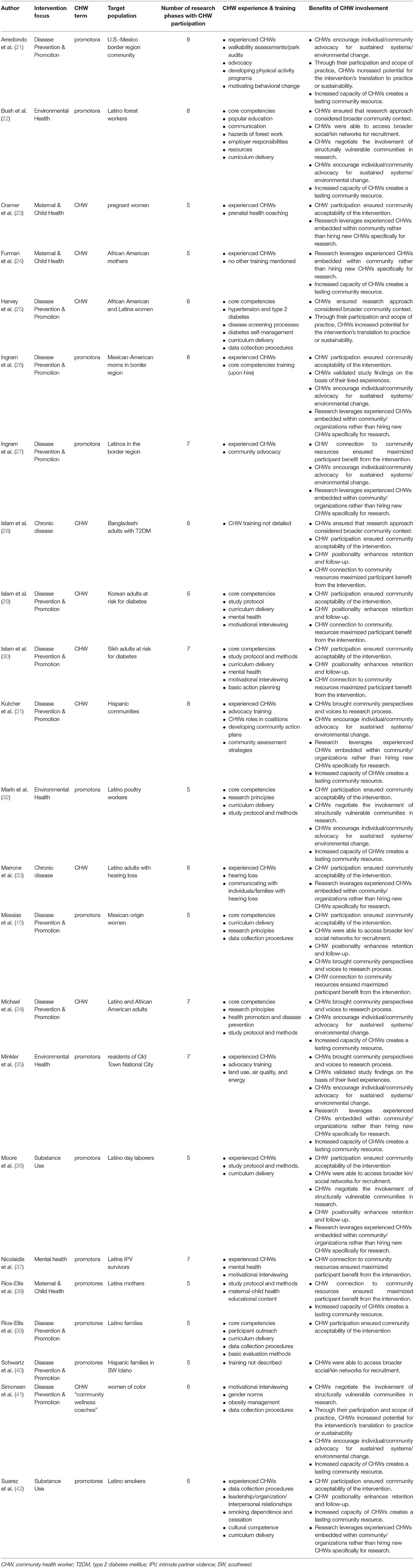
Table 2 . CHW involvement in phases of research and benefits across high CHW involvement studies.
Our examination of the 23 studies identified 12 distinct benefits of CHW involvement throughout the research process. In many of the studies, CHWs were vital to developing study approaches, methodologies, and interventions that were appropriate for the communities served. More specifically, CHWs increased the research team's awareness of the broader community context and social determinants of health impacting the daily lives of potential study participants ( 22 , 25 , 28 ). Bush et al. ( 22 ) noted the ways in which CHWs increased researchers' awareness to issues facing Latino forest workers (i.e., wage theft, immigration status, land-lord tenant retaliation, etc.) that could influence their capacity to prioritize the occupational safety concerns that were the focus of the intervention. In the study conducted by Messias et al. ( 15 ), CHWs provided researchers with crucial information regarding participants' family care-giving responsibilities, employment obligations, and transportation needs which allowed for effective planning and scheduling of intervention sessions. The articles also demonstrated that CHWs contributed to the community acceptability of interventions , particularly in ensuring the cultural congruence of the intervention and identifying culturally relevant modes of intervention delivery ( 15 , 23 , 26 , 28 – 30 , 32 , 33 , 36 , 39 , 42 ). CHWs implementing the Salud S í (Health Yes) intervention were responsible for refining intervention strategies to respond to the needs and characteristics of study participants, such as incorporating spirituality to address depression ( 26 ). In other studies, CHWs provided their insights and suggestions to adapt already developed curriculums. Moore et al. ( 36 ) explained how the CHWs made changes to the intervention manual to better incorporate Latino cultural values, such as familism, and bring awareness to important stressors confronted by day laborers (i.e., acculturative stress, discrimination, and poverty). In Suarez et al. ( 42 ), CHWs identified community settings where they could effectively engage Latino smokers and deliver health education (churches, Latino-owned businesses, home visits, Consulate of Mexico, etc.).
The studies underscored CHWs' ability to engage vulnerable or hard-to-reach populations in research, particularly ethnic-minority populations. This was often achieved by CHWs accessing their broader social and/or kin networks for participant recruitme nt ( 15 , 22 , 36 , 40 ). Recruitment efforts benefitted from the existing trust and rapport CHWs had with their community members. Messias et al. ( 15 ) documented how CHWs identified participants from their existing social networks within schools, churches, work, and the broader community. Furthermore, as noted by Bush et al. ( 22 ), CHWs tapped into their kinship networks, facilitating contact with large numbers of forest workers. The studies also demonstrated that CHWs negotiated the inclusion of structurally vulnerable communities in research ( 22 , 32 , 36 , 41 ), referring to populations whose positionality imposes physical or emotional suffering in patterned ways ( 43 ). This was particularly evident among interventions targeting low-wage laborers (i.e., forest workers and poultry workers). Sustaining the participation of these populations in the intervention required the efforts and capabilities of the CHWs. More specifically, Bush et al. ( 22 ) acknowledged that the CHWs' cultural knowledge, language fluency, and rapport were critical in engaging immigrant forest workers with deeply embedded fears related to immigration status. Similarly, Marín et al. ( 32 ) documented that their CHW program provided a safe environment for immigrant poultry workers to learn more about their rights to a safe workplace and advocate for their occupational safety, despite palpable fears of workplace retaliation.
Following recruitment, CHW positionality within the community enhanced participant retention in the study, ongoing data collection and follow-up ( 15 , 28 – 30 , 36 , 42 ). CHWs achieved this by developing trust and rapport with participants that enabled them to recognize and negotiate potential barriers to participation, as well as engendered a desire among participants to complete study processes. For example, researchers attributed high levels of participant retention and compliance with accelerometer measurements in a physical activity intervention to CHW continuous communication with participants ( 15 ). CHWs' ability to engage and retain participants throughout the study brought community perspectives and voices to research process ( 15 , 31 , 34 , 35 ). This was apparent in interventions involving CHW-led advocacy efforts. Kutcher et al. ( 31 ) described how CHWs were integral to including community residents impacted by health disparities in health coalitions, thereby providing a voice for stakeholders who traditionally lack power. CHWs were able to facilitate coalition meetings where there was equitable participation among community members, local agencies, and officials. CHWs also elevated community voices through data collection efforts. In an environmental justice initiative, CHWs served as “co-researchers” and led a survey of community residents to capture their concerns and priorities (i.e., asthma, land use, affordable housing, etc.), which later shaped local policy changes ( 35 ).
The few studies that involved CHWs in the data interpretation process demonstrated that they were able to explain or validate study findings based on their common experience with the study population ( 26 , 35 ). CHWs in Ingram et al.'s ( 26 ) study explained that women who initiated physical activity during the intervention were able to do so because the program created a culturally acceptable space for women to congregate. Without the organized classes, this activity was difficult to maintain. In an effort to enact policy changes consistent with the community's needs, Minkler et al. ( 35 ) described how CHWs presented to the City Council the results of a survey they implemented with community residents, which they supported by sharing their experiences as community members and mothers.
In several of the studies, CHW involvement increased the potential for the intervention's translation to practice or sustainability , and this finding applied to both program and systems level interventions ( 21 , 25 , 41 ). CHWs helped ensure that the intervention utilized appropriate strategies delivered in an appropriate fashion, taking into consideration the larger context of intervention delivery and the participants' lives. The CHW-driven advocacy efforts initiated as part of REACH projects were more likely to be sustained because the CHWs successfully engaged business owners in prioritizing and implementing changes ( 25 ). Similarly, the Arredondo et al. ( 21 ) study documented an increased intention to use park facilities among community members after CHWs worked with youth to identify, advocate for, and attain structural changes. On the programmatic level, the Detroit Department of Health continued to employ CHWs and outreach strategies after demonstrating the effectiveness designed by the CHWs in the HC project ( 25 ). Notably, an intervention's sustainability was maximized when the research leveraged experienced CHWs that were already embedded in community or local organizations, rather than hiring new CHWs specifically for research ( 23 , 24 , 26 , 27 , 31 , 33 , 35 , 36 , 42 ). This is largely because CHWs could incorporate intervention activities into their existing work after the conclusion of the study. In a breastfeeding intervention, the CHWs continued to use curricular models within their existing MomsFirst programming ( 24 ).
Importantly, CHWs' connections to community resources helped to maximize participants' benefit from the intervention ( 15 , 27 – 30 , 37 , 38 ). Participants were connected to a broader range of community resources more efficiently and also frequently received ongoing services from these entities. CHWs linking participants to community resources (i.e., food stamps, English language programs, etc.) were also cited as reasons for high feasibility and/or acceptability of interventions ( 28 – 30 ). CHWs connected participants to needed services even when not a stated objective of the intervention. For example, within a breastfeeding intervention for Latina mothers, participants reported an increased understanding of where to get help for post-partum depression because the CHW shared her knowledge of relevant services ( 38 ).
CHW involvement encouraged individual/community advocacy to enact sustained health-promoting individual and system level changes ( 21 , 22 , 26 , 27 , 31 , 32 , 34 , 35 , 41 ). The interventions focusing on occupational safety empowered immigrant workers to advocate for better working conditions ( 22 , 32 ). Despite notable fears and susceptibility to retaliation among the workers, the support and information from the CHWs empowered them to address workplace hazards such as notifying their supervisors ( 22 , 32 ). In other studies, CHWs mobilized community members, organizations, and policy-makers to implement policy-systems-environment (PSE) strategies. CHWs encouraged community members to think ecologically about their health and identify advocacy-oriented solutions to improve community social determinants of health. CHWs also modeled behaviors for participating in advocacy coalitions so to support the capacity of community members to work with local representatives/officials to enact PSE changes ( 31 ). The organization efforts of the CHWs led to a variety of individual and community changes, such as restorations of a local park ( 21 ), improvements to neighborhood conditions, enhanced community opportunities, better access to services ( 27 ), increased access to healthy foods, and the adoption of policies to integrate physical activity opportunities into schools ( 31 ).
Finally, the increased capacity of CHWs, through their training and increased experience, created a lasting community resource ( 21 , 22 , 24 , 31 , 32 , 34 , 35 , 38 , 41 , 42 ). As described by Bush et al. ( 22 ), after the occupational safety intervention, the CHWs' participation in the program promoted their leadership skills and established them as recognized resources within the community. The CHWs' experiences in research empowered them to take on additional roles, responsibilities, or new jobs. After their demonstrated success in advocacy, Kutcher et al. ( 31 ) mentioned that the CHWs adopted new roles facilitating coalition meetings, collaborating with local officials, and representing the project in marketing/communications efforts. At the end of the occupational safety program, Marín et al. ( 32 ) noted the promoters were provided new opportunities; one was later hired for a local literacy project, and two others were employed by a worker center supporting low-wage immigrant workers.
Thorough review of CHWs' activities within health intervention research provides important insights for community-academic research teams regarding the breadth of roles CHWs can assume within research and how they can strengthen health research initiatives. Overall, the results of the primary and secondary analysis revealed that CHW participation in health intervention research is diverse, in terms of the kinds of studies they are involved (i.e., study design and focus), their roles in the research process and their positionality on the research team. The majority of studies, and particularly those that engaged CHWs in more phases of the research applied a community based participatory research approach. This finding is consistent with the C3 report's and other scholars' assessments that CHWs facilitate community participation and representation in health research ( 2 ). However, a substantial percentage of the studies were not participatory, suggesting that both participatory and non-participatory researchers recognize the relevance of CHWs to health interventions. What did differentiate CBPR and non-CBPR studies was the range of research phases with CHW involvement. CHWs were involved in up to 9 phases within CBPR studies, relative to up to 4 within non-CBPR studies. This result indicates that CBPR studies are more likely to integrate CHWs across the entirety of research process, beginning from identification of the health issue to dissemination of the results.
In nearly all the studies, CHWs were responsible for implementing the intervention under study, and those studies that employed CHWs in this role alone are perhaps better able to distinguish the effectiveness of the CHW-facilitated intervention or the CHW workforce in addressing a particular health issue (i.e., glycemic control, hypertension, etc.). It is not surprising that intervention implementation, participant recruitment, and data collection, defined as discrete phases of research in the CBPR-framework, were the research phases with the highest CHW involvement across the studies. These phases of research involve CHWs in direct interaction with study participants to encourage their participation in the study, facilitate their engagement in the study, or talk with them about their health. Given CHWs' connections within their communities and their effectiveness in engaging with community members, it makes sense that CHWs performed these activities most frequently.
Conversely, CHWs were least involved in identifying the research question, data analysis, and research dissemination. This finding represents lost opportunities for ensuring that not only the research focus, but also research findings, are relevant to communities. Researchers would need to engage CHWs as research partners early in the process if they were to be included in defining the research question and ensuring that the interventions address relevant health issues. As underscored in the secondary analysis, CHWs can also aid in data analysis by explaining study findings, interpreting the voices and perspectives of the study participants, and further validating the data based on their lived experiences. Very few of the studies involved CHWs in a dissemination/action phase of the research, which is unfortunate. This phase is intrinsic to CBPR in ensuring that research contributes to social change ( 44 ). While it is possible that these research projects continued into an action phase not reported in the article, it is also the most difficult phase of research and the one for which researchers are least prepared. This may be the major argument for including CHWs as full members on research teams so that they are well-positioned to carry the research forward into community action.
This aspect of CHW involvement is related to their positionality on research teams and the power dynamics between community and academic partners that limit or maximize CHWs' contributions to research. The articles provide several strategies for including CHWs and building their capacity in a partnership role. In some cases, researchers invited CHWs to sit on the decision-making body of the research team, such as the community action board (CAB) or steering committee. This inclusion formalized their leadership position among academics and other stakeholders. As recognized leaders and stakeholders, CHWs are ideally positioned to share their knowledge of community during the formative phases of the study to inform the research approach at the outset. The projects also trained CHWs in research methodologies. While these trainings were frequently not described in-depth, a co-learning environment in which the mutual and shared expertise is valued among all partners would certainly facilitate recognition of CHW contributions. Additionally, CHWs that were incorporated across the phases of research had more opportunities to improve research processes and ensure community benefit. Because CHWs instinctively and are trained to prioritize community interests, they are more likely to identify and address ethical issues related to research that might otherwise go unrecognized ( 18 ).
The inclusion of CHWs did not go without challenges. Researchers noted some difficulty in CHWs adhering to research protocols due to concerns of maintaining rapport with community members. One academic-community partnership discussed CHWs encountering tension between fidelity to procedures of randomized-control trials and community norms ( 15 ). Another research team described differing goals between academic and community partners (including CHWs), where academic partners prioritized data and community partners prioritized funding and policy ( 24 ). While it is important that CHWs are trained in research ethics and procedures, the current study's results highlight how CHWs' knowledge of the community is integral to conducting successful research. For example, Furman et al. ( 24 ) explained how some of the staff were hesitant to endorse the research project due to conflicts with on-the-ground realities of the community members served. Thus, if CHWs are challenged by the research protocol, that could signal potential incongruence with community practices that the research team should address. Furthermore, it was clear that research teams valued the community rapport CHWs possessed, but some authors described how some CHWs faced difficulties in leveraging connections outside of their social networks ( 15 , 22 ). Also, a few studies documented CHWs facing personal conflict between their responsibilities as CHWs engaged in research and their obligations to spouses/family ( 32 , 35 ).
Limitations
The scoping review is also characterized by certain limitations. Our knowledge of the CHWs' involvement within the included studies is limited to what was documented in the articles. Thus, if CHWs' participation was not thoroughly described or underreported by the author(s), it was not reflected in our results. We did not seek to evaluate the quality of the research and did not compare it to similar research that did not use CHWs. Also, we did not examine individual health outcomes or community outcomes which we hope would be improved with CHW involvement. Our scoping review does not establish the desired benefits, rather it is an attempt to synthesize lessons learned from a broad variety of research studies and approaches. Lastly, these results do not capture lessons to be learned from research interventions with CHWs outside the U.S. Future research should examine the roles of CHWs within health intervention research globally.
This scoping review highlights the potential benefits of incorporating CHWs as partners in health intervention research studies. Our findings demonstrate that CHWs can improve the quality of research not only in CBPR studies that seek to engage community members in the research process, but also in non-CBPR studies, including those utilizing experimental designs. We found that CHWs inform study design to consider contextual factors, improve the content and delivery of health interventions, and validate and explain research findings and most importantly, both insure and increase the benefits of research for the individuals and communities involved.
Author Contributions
KC lead the development of the manuscript. KC and MI collaborated in developing the inclusion/exclusion criteria, conducting article screening, data analysis, and drafting of the manuscript. DM directed the development of the search strategy, implemented the search in the databases, and lead the writing of the methods section of the manuscript. AL edited continuous iterations of the manuscript draft and provided input on the direction of the data analysis.
This journal article was supported by the Grant or Cooperative Agreement No. DP005002 under the Health Promotion and Disease Prevention Research Centers Program, funded by the Centers for Disease Control and Prevention.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00208/full#supplementary-material
Data Sheet 1. Data extraction table for primary analysis articles to account for some spelling errors, more accurate listings of some of the target populations of the intervention studies, and accuracy in dates of publication.
1. American Public Health Association (APHA). Community Health Workers (2019). Available online at: https://www.apha.org/apha-communities/member-sections/community-health-workers (November 1, 2019).
Google Scholar
2. Rosenthal EL, Rush CH, Allen C. Progress Report of the Community Health Worker (CHW) Core Consensus (C3) Project: Building National Consensus on CHW Core Roles, Skills, and Qualities . (2016) Available online at: http://files.ctctcdn.com/a907c850501/1c1289f0-88cc-49c3-a238-66def942c147.pdf?ver=1462294723000
3. Pérez-Escamilla R, Damio G, Chhabra J, Fernandez ML, Segura-Pérez S, Vega-López S, et al. Impact of a community health workers–led structured program on blood glucose control among Latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. (2015) 38:197–205 doi: 10.2337/dc14-0327
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Ursua RA, Aguilar DE, Wyatt LC, Trinh-Shevrin C, Gamboa L, Valdellon P, et al. A community health worker intervention to improve blood pressure among Filipino Americans with hypertension: a randomized controlled trial. Prev Med Rep. (2018) 11:42–8. doi: 10.1016/j.pmedr.2018.05.002
5. Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. (2011) 101:2253–60. doi: 10.2105/AJPH.2010.300106
6. Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am J Public Health. (2016) 106:e3–28. doi: 10.2105/AJPH.2015.302987a
7. Han HR, Song Y, Kim M, Hedlin HK, Kim K, Ben Lee H, et al. Breast and cervical cancer screening literacy among Korean American women: a community health worker–led intervention. Am J Public Health. (2017) 107:159–65. doi: 10.2105/AJPH.2016.303522
8. Koniak-Griffin D, Brecht ML, Takayanagi S, Villegas J, Melendrez M, Balcázar H. A community health worker-led lifestyle behavior intervention for Latina (Hispanic) women: feasibility and outcomes of a randomized controlled trial. Int J Nurs Stud. (2015) 52:75–87. doi: 10.1016/j.ijnurstu.2014.09.005
9. Rosenthal EL, Wiggins N, Ingram M, Mayfield-Johnson S, De Zapien JG. Community health workers then and now: an overview of national studies aimed at defining the field. J Ambul Care Manage. (2011) 34:247–59. doi: 10.1097/JAC.0b013e31821c64d7
10. Hohl SD, Thompson B, Krok-Schoen JL, Weier RC, Martin M, Bone L, et al. Characterizing community health workers on research teams: results from the centers for population health and health disparities. Am J Public Health. (2016) 106:664–70. doi: 10.2105/AJPH.2015.302980
11. Brownstein JN, Hirsch GR, Rosenthal EL, Rush CH. Community health workers “101” for primary care providers and other stakeholders in health care systems. J Ambul Care Manage. (2011) 34:210–20. doi: 10.1097/JAC.0b013e31821c645d
12. Johnson CM, Sharkey JR, Dean WR, St John JA, Castillo M. Promotoras as research partners to engage health disparity communities. J Acad Nutr Diet. (2013) 113:638–42. doi: 10.1016/j.jand.2012.11.014
13. Choi E, Heo GJ, Song Y, Han HR. Community health worker perspectives on recruitment and retention of recent immigrant women in a randomized clinical trial. Fam Community Health. (2016) 39:53–61. doi: 10.1097/FCH.0000000000000089
14. Larkey LK, Gonzalez JA, Mar LE, Glantz N. Latina recruitment for cancer prevention education via community based participatory research strategies. Contemp Clin Trials. (2009) 30:47–54. doi: 10.1016/j.cct.2008.08.003
15. Messias DK, Parra-Medina D, Sharpe PA, Treviño L, Koskan AM, Morales-Campos D. Promotoras de Salud: roles, responsibilities, and contributions in a multi-site community-based randomized controlled trial. Hisp Health Care Int. (2013) 11:62–71. doi: 10.1891/1540-4153.11.2.62
16. Vaughn LM, Whetstone C, Boards A, Busch MD, Magnusson M, Määttä S. Partnering with insiders: a review of peer models across community-engaged research, education and social care. Health Soc Care Community. (2018) 26:769–86. doi: 10.1111/hsc.12562
17. Cupertino AP, Suarez N, Cox LS, Fernández C, Jaramillo ML, Morgan A, et al. Empowering promotores de salud to engage in community-based participatory research. J Immigr Refug Stud. (2013) 11:24–43. doi: 10.1080/15562948.2013.759034
18. Smith SA, Blumenthal DS. Community health workers support community-based participatory research ethics: lessons learned along the research-to-practice-to-community continuum. J Health Care Poor Underserved. (2012) 23(Suppl. 4):77–87. doi: 10.1353/hpu.2012.0156
19. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
CrossRef Full Text | Google Scholar
20. Malcarney MB, Pittman P, Quigley L, Seiler N, Horton KB. Community Health Workers: Health System Integration, Financing Opportunities, and the Evolving Role of the Community Health Worker in a Post-Health Reform Landsacape (2015) . Available online at: https://hsrc.himmelfarb.gwu.edu/sphhs_policy_workforce_facpubs/11/ (April 15, 2019).
21. Arredondo E, Mueller K, Mejia E, Rovira-Oswalder T, Richardson D, Hoos T. Advocating for environmental changes to increase access to parks: engaging promotoras and youth leaders. Health Promot Pract. (2013) 14:759–66. doi: 10.1177/1524839912473303
22. Bush DE, Wilmsen C, Sasaki T, Barton-Antonio D, Steege AL, Chang C. Evaluation of a pilot promotora program for Latino forest workers in southern Oregon. Am J Ind Med. (2014) 57:788–99. doi: 10.1002/ajim.22347
23. Cramer ME, Mollard EK, Ford AL, Kupzyk KA, Wilson FA. The feasibility and promise of mobile technology with community health worker reinforcement to reduce rural preterm birth. Public Health Nurs. (2018) 35:508–16. doi: 10.1111/phn.12543
24. Furman L, Matthews L, Davis V, Killpack S, O'Riordan MA. Breast for success: a Community–Academic collaboration to increase breastfeeding among high-risk mothers in Cleveland. Prog Community Health Partnersh. (2016) 10:341–53. doi: 10.1353/cpr.2016.0041
25. Harvey I, Schulz A, Israel B, Sand S, Myrie D, Lockett M, et al. The Healthy Connections project: a community-based participatory research project involving women at risk for diabetes and hypertension. Prog Community Health Partnersh. (2009) 3:287–300. doi: 10.1353/cpr.0.0088
26. Ingram M, Piper R, Kunz S, Navarro C, Sander A, Gastelum S. Salud Sí: A case study for the use of participatory evaluation in creating effective and sustainable community-based health promotion. Fam Community Health. (2012) 35:130–8. doi: 10.1097/FCH.0b013e31824650ed
27. Ingram M, Schachter KA, Sabo SJ, Reinschmidt KM, Gomez S, De Zapien JG, et al. A community health worker intervention to address the social determinants of health through policy change. J Prim Prev. (2014) 35:119–23. doi: 10.1007/s10935-013-0335-y
28. Islam NS, Wyatt LC, Patel SD, Shapiro E, Tandon SD, Mukherji BR, et al. Evaluation of a community health worker pilot intervention to improve diabetes management in Bangladeshi immigrants with type 2 diabetes in New York City. Diabetes Educ. (2013) 39:478–93. doi: 10.1177/0145721713491438
29. Islam NS, Zanowiak JM, Wyatt LC, Chun K, Lee L, Kwon SC, et al. A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J Community Health. (2013) 38:1030–41. doi: 10.1007/s10900-013-9711-z
30. Islam NS, Zanowiak JM, Wyatt LC, Kavathe R, Singh H, Kwon SC, et al. Diabetes prevention in the New York City Sikh Asian Indian community: a pilot study. Int J Environ Res Public Health. (2014) 11:5462–86. doi: 10.3390/ijerph110505462
31. Kutcher R, Moore-Monroy M, Bello E, Doyle S, Ibarra J, Kunz S, et al. Promotores as advocates for community improvement: experiences of the western states REACH Su Comunidad consortium. J Ambul Care Manage. (2015) 38:321–32. doi: 10.1097/JAC.0000000000000073
32. Marín A, Carrillo L, Arcury TA, Grzywacz JG, Coates ML, Quandt SA. Ethnographic evaluation of a lay health promoter program to reduce occupational injuries among Latino poultry processing workers. Public Health Reports . (2009) 124(Suppl. 1):36–43. doi: 10.1177/00333549091244S105
33. Marrone N, Ingram M, Somoza M, Jacob DS, Sanchez A, Adamovich S, et al. Interventional audiology to address hearing health care disparities: Oyendo Bien pilot study. Semin Hear. (2017) 38:198–211. doi: 10.1055/s-0037-1601575
34. Michael YL, Farquhar SA, Wiggins N, Green MK. Findings from a community-based participatory prevention research intervention designed to increase social capital in Latino and African American communities. J Immigr Minor Health. (2008) 10:281–9. doi: 10.1007/s10903-007-9078-2
35. Minkler M, Garcia AP, Williams J, LoPresti T, Lilly J. Sí se puede: using participatory research to promote environmental justice in a Latino community in San Diego, California. J Urban Health. (2010) 87:796–812. doi: 10.1007/s11524-010-9490-0
36. Moore AA, Karno MP, Ray L, Ramirez K, Barenstein V, Portillo MJ, et al. Development and preliminary testing of a promotora-delivered, Spanish language, counseling intervention for heavy drinking among male, Latino day laborers. J Subst Abuse Treat. (2016) 62:96–101. doi: 10.1016/j.jsat.2015.11.003
37. Nicolaidis C, Mejia A, Perez M, Alvarado A, Celaya-Alston R, Quintero Y, et al. Proyecto Interconexiones: pilot-test of a community-based depression care program for Latina violence survivors. Prog Community Health Partnersh. (2013) 7:395–401. doi: 10.1353/cpr.2013.0051
38. Rios-Ellis B, Nguyen-Rodriguez ST, Espinoza L, Galvez G, Garcia-Vega M. Engaging community with promotores de salud to support infant nutrition and breastfeeding among Latinas residing in Los Angeles County: Salud con Hyland's. Health Care Women Int . (2015) 36:711–29. doi: 10.1080/07399332.2014.900060
39. Rios-Ellis B, Espinoza L, Bird M, Garcia M, D'Anna LH, Bellamy L, et al. Increasing HIV-related knowledge, communication, and testing intentions among Latinos: Protege tu Familia: Hazte la Prueba. J Health Care Poor Underserved. (2010) 21:148–68. doi: 10.1353/hpu.0.0360
40. Schwartz R, Powell L, Keifer M. Family-based risk reduction of obesity and metabolic syndrome: an overview and outcomes of the Idaho partnership for Hispanic health. J Health Care Poor Underserved. (2013) 24:129–44. doi: 10.1353/hpu.2013.0106
41. Simonsen SE, Ralls B, Guymon A, Garrett T, Eisenman P, Villalta J, et al. Addressing health disparities from within the community: community-based participatory research and community health worker policy initiatives using a gender-based approach. Women's Health Issues. (2017) 27(Suppl. 1):S46–53. doi: 10.1016/j.whi.2017.09.006
42. Suarez N, Mendoza I, Garrett S, Ellerbeck EF. Success of “Promotores de Salud” in identifying immigrant Latino smokers and developing quit plans. Int Public Health J. (2012) 4:343–53.
43. Quesada J, Hart LK, Bourgois P. Structural vulnerability and health: Latino migrant laborers in the United States. Med Anthropol. (2011) 30:339–62. doi: 10.1080/01459740.2011.576725
44. Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. (2010) 100(Suppl. 1):S40–6. doi: 10.2105/AJPH.2009.184036
Keywords: community health workers, intervention research, participatory research, health intervention, academic-community partnerships
Citation: Coulter K, Ingram M, McClelland DJ and Lohr A (2020) Positionality of Community Health Workers on Health Intervention Research Teams: A Scoping Review. Front. Public Health 8:208. doi: 10.3389/fpubh.2020.00208
Received: 18 February 2020; Accepted: 06 May 2020; Published: 16 June 2020.
Reviewed by:
Copyright © 2020 Coulter, Ingram, McClelland and Lohr. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kiera Coulter, kcoulter@arizona.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Loading metrics
Open Access
Peer-reviewed
Research Article
Community health workers and Covid-19: Cross-country evidence on their roles, experiences, challenges and adaptive strategies
Roles Formal analysis, Methodology, Writing – original draft, Writing – review & editing
Affiliation Oxford Policy Management, Delhi, India
Roles Conceptualization, Formal analysis, Funding acquisition, Supervision, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of International Public Health, Liverpool School of Tropical Medicine, Liverpool, United Kingdom
Roles Investigation, Validation, Writing – review & editing
Affiliation Oxford Policy Management, Dhaka, Bangladesh
Roles Validation, Writing – review & editing
Affiliation Oxford Policy Management, Islamabad, Pakistan
Affiliation Oxford Policy Management, Abuja, Nigeria
Roles Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing
Affiliation Oxford Policy Management, Oxford, United Kingdom
- Solomon Salve,
- Joanna Raven,
- Priya Das,
- Shuchi Srinivasan,
- Adiba Khaled,
- Mahwish Hayee,
- Gloria Olisenekwu,
- Kate Gooding

- Published: January 4, 2023
- https://doi.org/10.1371/journal.pgph.0001447
- Reader Comments
Community health workers (CHWs) are a key part of the health workforce, with particular importance for reaching the most marginalised. CHWs’ contributions during pandemics have received growing attention, including for COVID-19. This paper contributes to learning about CHWs’ experiences during COVID-19, based on evidence from India, Bangladesh, Pakistan, Sierra Leone, Kenya and Ethiopia. The paper synthesises evidence from a set of research projects undertaken over 2020–2021. A thematic framework based on the research focus and related literature was used to code material from the reports. Following further analysis, interpretations were verified with the original research teams. CHWs made important contributions to the COVID-19 response, including in surveillance, community education, and support for people with COVID-19. There was some support for CHWs’ work, including training, personal protective equipment and financial incentives. However, support varied between countries, cadres and individual CHWs, and there were significant gaps, leaving CHWs vulnerable to infection and stress. CHWs also faced a range of other challenges, including health system issues such as disrupted medical supply chains, insufficient staff and high workloads, a particular difficulty for female CHWs who were balancing domestic responsibilities. Their work was also affected by COVID-19 public health measures, such as restrictions on gatherings and travel; and by supply-side constraints related to community access and attitudes, including distrust and stigmatization of CHWs as infectious or informers. CHWs demonstrated commitment in adapting their work, for example ensuring patients had adequate drugs in advance of lockdowns, and using their own money and time to address increased transport costs and higher workloads. Effectiveness of these adaptations varied, and some involved coping in a context of inadequate support. CHW are critical for effective response to disease outbreaks, including pandemics like COVID-19. To support CHWs’ contribution and protect their wellbeing, CHWs need adequate resources, managerial support, and motivation.
Citation: Salve S, Raven J, Das P, Srinivasan S, Khaled A, Hayee M, et al. (2023) Community health workers and Covid-19: Cross-country evidence on their roles, experiences, challenges and adaptive strategies. PLOS Glob Public Health 3(1): e0001447. https://doi.org/10.1371/journal.pgph.0001447
Editor: Amrita Daftary, York University, CANADA
Received: June 7, 2022; Accepted: December 7, 2022; Published: January 4, 2023
Copyright: © 2023 Salve et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: Synthesis and development of the paper were funded by the Foreign, Commonwealth and Development Office (FCDO), UK Aid, under the ReBUILD for Resilience Research Programme Consortium (PO 8610 to JR). Financial support for the underlying projects was provided by the Bill and Melinda Gates Foundation (BMGF), the Foreign, Commonwealth & Development Office (FCDO), the Global Financing Facility, the United Nations Children's Fund (UNICEF), the U.S. Agency for International Development (USAID) and the World Bank. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The views expressed do not necessarily reflect the UK government’s official policies.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Community health workers (CHWs) are a key part of the health workforce in many low- and middle-income countries (LMICs), increasingly recognised as integral for effective and equitable health service delivery [ 1 – 4 ]. The umbrella term “CHW” encompasses diverse categories of health worker [ 4 ], such as community distributors, community-directed health workers, health auxiliaries, health promoters, family welfare educators, health volunteers, village health workers, community health aides, and barefoot doctors [ 5 ]. For this paper, we consider CHWs as health workers who are the first point of contact at community level, based in communities or at peripheral health posts, and who have some but fewer than two to three years of training [ 1 , 6 ]. Within this group, there is substantial diversity between countries and cadres in CHW responsibilities, skills and employment conditions [ 1 , 7 ].
CHWs undertake a wide range of tasks related to core health service provision, such as community mobilization, health promotion, and provision of preventive and clinical services [ 8 , 9 ]. Over the past decade, there has been a growing recognition of potential CHW roles in responding to pandemics [ 10 ]. Based in communities, and often from these same communities, CHWs are often the frontline and first point of contact when an outbreak hits [ 3 ]. For example, CHWs played multiple roles in the 2014 Ebola outbreak in West Africa [ 11 – 15 ]. Most recently, CHWs have been active in the COVID-19 response[ 16 – 23 ]. Research has documented the roles played by CHWs in controlling COVID-19, and the challenges they have experienced [ 16 – 24 ]. As well as introducing new roles for CHWs, COVID-19 has affected their routine service delivery. International surveys in 2020 and 2021 showed significant disruption to primary and community health services, with disruptions to community care reported by more than half the countries in the world in late 2021 [ 25 – 27 ]. In many countries, community services were deliberately suspended or scaled back, but services were also affected by issues such as disruption to supply chains, shortage of health workers and demand-side constraints [ 27 ].
This article contributes to the growing understanding of CHW roles and experiences in the COVID-19 response, synthesising evidence from a set of research projects in six countries in South Asia and Africa: Ethiopia, Kenya, Sierra Leone, Bangladesh, India and Pakistan. The article examines CHWs’ contributions to the response, the support provided to CHWs, and gaps in this support, challenges experienced by CHWs in delivering services, and adaptations or coping strategies that enabled service delivery. While guidelines were developed to support CHWs at an early stage in the COVID-19 pandemic [ 24 ], indications of widespread challenges for CHWs suggest a need for further evidence that can strengthen awareness and understanding of CHWs’ experiences and inform further measures to ensure they have adequate support.
The six countries included in this synthesis have all been significantly affected by COVID-19. All reported the first case during January–March 2020, and there was significant spread and community transmission by May [ 28 , 29 ]. COVID-19 added to other shocks experienced by these countries, including climatic shocks such as drought and floods in all 6 countries, and political instability or conflict in some, notably Ethiopia and Kenya. These countries are at different levels of development, but all face significant health system challenges–including financial constraints and health worker shortages, with all significantly below the WHO recommendation minimum of 44.5 skilled health workers (doctors, nurses and midwives) per 10,000 needed to achieve UHC and SDG3 [ 30 ] (see Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0001447.t001
CHWs play a critical role in each country. Their specific titles vary between the countries (see Table 2 for information on cadres referred to in this paper). Some are voluntary positions, while others have more formal status and salaries, and their roles, levels of training and other employment conditions vary. In most countries, the majority of these CHWs are female.
https://doi.org/10.1371/journal.pgph.0001447.t002
The paper synthesises evidence from a set of research projects conducted or supported by Oxford Policy Management (OPM) over 2020–21 (see Table 3 and further details in S1 Table ). OPM is an international development consultancy organisation that works to support country governments and development partners through analysis and technical assistance across the policy cycle [ 53 ]. The projects that provided evidence for this synthesis were undertaken with a range of donor, research and country government partners, in India, Bangladesh, Pakistan, Sierra Leone, Kenya and Ethiopia. Projects and related reports were identified for inclusion based on author knowledge of OPM work and discussion with OPM country teams, with reports then reviewed to assess whether they provided relevant information.
https://doi.org/10.1371/journal.pgph.0001447.t003
CHWs’ experiences during COVID-19 were the central focus for some projects, whereas others examined community health services, health system resilience, or the COVID-19 response broadly but included information on CHWs’ roles and experiences during COVID-19. Methods varied between the research projects, but were primarily qualitative, and included interviews, focus groups and document reviews (see Table 3 ). Some studies produced multiple reports, for example through monthly updates as the pandemic progressed. In total, 25 reports based on 18 studies were used for the synthesis. One report was publicly available (a real time assessment of UNICEF’s support to COVID-19 vaccine rollout [ 54 ], but the majority were internal for specific funders or other stakeholders.
To synthesise the material, a team of two researchers (SS and KG) conducted an initial rapid reading to map the range of information available. A thematic framework (see S2 Table ) was then developed based on the research focus, knowledge of issues in the reports and other literature on CHWs’ roles and experiences with COVID-19. This framework was then adapted to clarify and add codes as reports were synthesised. Codes included roles that CHWs played during COVID-19, support provided, issues that helped or hindered CHW experience, effectiveness of service delivery, wellbeing of CHWs, and adaptation to enable continuation of service delivery. Taguette (an open-source tool for qualitative research available at https://www.taguette.org/ ) was used to import and code reports using the framework. Material under each theme was then exported for further analysis. Coding was led by one researcher (SS) and discussed among the research team (KG, JR) to support shared understanding of different themes as well as identification of new thematic areas.
Reports were not excluded on the basis of overall quality of research methods or analysis, as useful information can be obtained from reports that may otherwise have weaknesses [ 55 ]. However, reliability of report findings was considered for inclusion of specific information, for example, only drawing on reported findings with clearer underlying evidence, such as from empirical research where quotes or other evidence were sufficiently specific and detailed to be confident about interpretation. Most reports had been peer reviewed, both by senior OPM staff and external researchers, and all had some level of review from the organisations that commissioned the research.
Following initial drafting, synthesis findings were shared with a selection of researchers involved in conducting the original studies, to verify information and interpretation of their findings and so strengthen reliability of analysis. Discussion with these researchers also provided additional information from their research data or wider contextual understanding that was not included in the original project reports. This additional information was then incorporated in the analysis (where this additional information has been used in this paper, it is referenced as ‘project data’). Core OPM contacts for most projects are also authors for this article (SS, PD, GO, AK, KG). Including authors with different country contexts, professional affiliations and personal backgrounds helped to ensure that different interpretations and perspectives were considered in the analysis.
Ethics statement
All the research studies included in the synthesis ensured that participants provided informed consent and that data was confidential. Consent was verbal or written, depending on the study approach (for example, remote interviews required verbal consent) and on context-specific understanding and guidance on appropriate procedures. Formal ethical review was provided for all reports (see S1 Table ), except for two sets of rapid assessments conducted to inform government or other programming: the Intra-Action Reviews of the COVID-19 response in Ethiopia, and the rapid COVID-19 initial assessments conducted under the Maintains programme. These reports were focused on immediate feedback for programme decisions and restricted to document review and discussion with senior officials regarding health system issues; stakeholders and guidance indicated that approval was not required due to the low-risk approach and methods, restriction of interviews to areas of professional responsibility, and the focus on programme decisions.
In this section, we present findings from the different countries in line with the thematic framework developed for this synthesis, examining the roles played by CHWs in the COVID-19 response, the support they received–and gaps in this support, challenges that they experienced, and strategies used by CHWs to continue their work.
What roles have CHWs played in the COVID-19 response?
In all countries, CHWs took on new roles in the COVID-19 response. Across countries, they contributed to aspects of case identification and surveillance, such as house screening, screening of people with COVID-19 symptoms, contact tracing, or reporting potential infections to district health teams [ 11 , 29 , 56 – 58 ]. Community engagement was another key role, including education and awareness on COVID-19 [ 57 , 59 , 60 ] and in India, counselling for returnee migrants [ 58 ]. In some countries, such as India and Bangladesh, CHWs were also involved in follow-up of COVID-19 patients including providing rations to those who were isolating and in need [ 59 , 61 ] and in Bangladesh, enforcing household lockdown for people with COVID-19 as well as returnee migrants [ 59 ]. Most of the research was conducted before COVID-19 vaccine rollout, so there was limited information on CHWs involvement in vaccine delivery. However, later reports indicated that CHWs in India and Ethiopia were involved in raising awareness about COVID-19 vaccination and encouraging uptake [ 54 , 62 ], and CHWs in Ethiopia were also involved in listing target populations and delivering vaccines [ 54 ]. CHWs’ responsibilities in delivery of routine essential services also changed during COVID-19. For example, in some areas of India, Accredited Social Health Activists (ASHAs) played new roles in both antenatal services (such as blood pressure checks), because the Auxiliary Nurse Midwife (ANMs) who would usually provide this antenatal care were unavailable, and in neonatal care (particularly first vaccinations), because of a rise in home deliveries [ 63 , 64 ].
As previously noted, the majority of CHWs in these countries are female. Reflecting existing gender-based occupational segregation in the health system, there were gender differences in assignment of COVID-19-related roles across the health workforce. In India, lower status positions are largely occupied by women, with very few women in management and leadership roles. Reflecting this, managerial, coordination and supervisory roles in COVID-19 were largely assigned to men, whereas female CHWs were primarily engaged in the more frontline activities such as screening and awareness raising [ 60 ].
Support provided to enable CHWs’ work during COVID-19
CHWs received various forms of support for their roles in the COVID-19 response, as well as for conducting their routine service delivery during COVID-19. This included support through the formal health system, from the community, and through their personal relationships.
Support from the formal health system.
Support through the formal health system included training and other guidance, personal protective equipment (PPE), financial support, and some support from managers. There were gaps in support in all these areas with consequences for CHWs’ ability to deliver services and for their well-being.
Training . Reports from most countries indicated provision of training for CHWs on services related to COVID-19, such as contact tracing and case management, and in some cases also on safe provision of routine services, including topics such as infection prevention and control and routine immunization during COVID-19 [ 29 , 65 – 67 ]. Development partners supported CHW training, including the United Nations Children’s Fund (UNICEF) in Sierra Leone and African Medical and Research Foundation (AMREF) Enterprises in Kenya [ 29 , 68 ].
To comply with physical distancing requirements and enable more rapid scale up of training, several countries conducted some training online or via mobile phones: in India, some training used zoom calls on mobile phones and the new ‘Disha’ App [ 67 ], Kenya used an application called ‘Leap’ to deliver learning content to CHWs by mobile phone [ 29 ], and Ethiopia relied on mobile-based and online training [ 69 ]. These approaches were reported to reach large numbers; for example, with 53,000 CHWs in Kenya reportedly trained via LEAP during early 2020 [ 29 ]. However, gaps in smartphone access meant these approaches could not reach all CHWs. In India, alongside use of online training, information and instructions on COVID-19 tasks were often sent by WhatsApp, but some ASHAs do not have any access to smartphones, and for many others, phones are kept by husbands [ 63 , 64 ]. There were also indications of wider gaps in training. For example, in India, some ANMs reported that they and Asha has not received training to support their work in raising awareness on COVID-19, and training had instead focused on management cadre. CHW often relied on public sources for information, such as television and WhatsApp messages [ 60 ].
PPE . CHWs across countries had insufficient PPE, with issues of quantity and quality. For example, some health assistants in Bangladesh received only three PPE sets over the first year of the pandemic, and shortages of masks and sanitiser were widely reported by ASHAs in India [ 59 , 70 ]. However, supply varied between CHWs and over time. For example, in Pakistan, some LHWs reported an absence of PPE while others reported both supplies and training on PPE use [ 56 ]. In India, initial shortages eased somewhat during later months (though with ongoing gaps for some ASHAs), and there were significant differences between cadres: ANMs in some cases received more PPE than ASHAs or AWWs [ 67 ], even though ASHAs had more contact with potential infection through their screening roles. ANMs also generally had stronger personal finances than ASHAs, and so could purchase PPE when it was not provided [ 63 , 64 ].
PPE shortages partly reflected systems constraints such as limited availability on international and national markets, and inadequate government budgets. However, shortages for CHWs also reflected issues of distribution. For example, in India and Kenya, available PPE was sometimes prioritised for those working on COVID-19 or in areas with a higher case load, leaving limited supplies for health workers providing routine services or in other locations [ 58 , 71 ]. In India, PPE distribution also reflected gendered health service hierarchies: guidelines on rational PPE use from the Ministry of Health and Family Welfare (MoHFW) categorised the (largely female) ASHAs as low-risk [ 58 ],and so lower priority for PPE, even though–as above—ASHAs were undertaking most screening and outreach. Some ANMs also reported that higher quality PPE (such as N.95 masks) was allocated to (often male) doctors and managers [ 67 ]. They voiced a sense of disempowerment and neglect, and described themselves during research discussions as “small people” (or lowest in the rung) for PPE distribution [ 67 ].
In the absence of PPE, some CHWs used inadequate substitutes. For example, in one state, some AWWs used hand towels, scarfs ( dupatta) and handkerchiefs to cover their mouths when delivering home rations [ 58 ]. Some CHWs in Bangladesh and India purchased their own masks and hand sanitizer, sewed masks for themselves, or washed PPE for reuse [ 58 , 59 ].There was also some community support for availability of PPE: in India, some CHWs received masks distributed by local politicians, or made by local women’s self-help mahila groups [ 72 ].
Despite these efforts, limited and irregular supply of PPE left CHWs vulnerable to infection. This risk contributed to anxiety among CHWs, with fear both for their own safety, and of transmitting infection to their families [ 58 , 59 ]. For example, ASHAs and AWWs in India described fear of infection during household visits and community engagement due to insufficient PPE [ 58 ]. Broader fear of infection also led to reduced services elsewhere; for example, LHWs in Pakistan restricted their community outreach [ 56 ], and in Sierra Leone, some CHWs refused to come to work [ 73 ]. In addition, CHWs were also at risk due to patients either not having or not wearing PPE. For example, in Bangladesh, a healthcare assistant saw treating patients who did not wear masks as the biggest challenge faced in service delivery during COVID-19, prompting her to fear for her own safety and that of her family. Due to these concerns, some CHWs in Bangladesh chose not to serve patients who did not wear PPE [ 59 ].
When PPE was received, this enabled service delivery; for example, in Bangladesh, Shasthya Shebikas reported being able to resume TB sputum tests when they received personal safety equipment [ 59 ].
Financial support . In some countries, financial incentive schemes were introduced to recognise additional work or risks during COVID-19. In India, several incentives were announced by state or national government. For example, the central government announced in March 2020 that ASHAs would be paid INR (Indian rupees)1000 (13.10 USD) per month for three months for COVID-19-related activities, and provided insurance cover of INR 50 Lakhs (65,826 USD); and the government of one state announced remuneration of INR 400 (5.24 USD) for ASHA facilitators and 200 INR (2.62 USD) for ASHAs who undertook COVID-19 case finding surveys [ 58 ] Other announced support included 17,000 PKR (94.88 USD) per month for LHWs in Pakistan [ 56 ], and life insurance for health workers in Bangladesh [ 29 ].
Despite announcements, there were clear gaps in provision of incentives and information on this financial support. In India, in mid-2020, CHWs were often unaware of these entitlements, and additional incentives had often not been received [ 58 ]. They also saw compensation as limited in relation to the additional work required during COVID-19. Provision of incentives also varied between CHW cadres; for example, AWWs were not remunerated for their roles in COVID-19 in three states, while some ANMs and ASHAs in these states did receive additional allowances [ 58 ]. In some areas, AWWs went on strike due to lack of incentives for COVID-19, disrupting routine service delivery [ 74 ]. Elsewhere, there were examples of CHWs spending additional money out of their own pocket to provide services during COVID-19, without compensation; for example, HEWs in Ethiopia used their personal phone and air time to share information regarding COVID-19 with other health system levels [ 75 ].
Lack of financial compensation related to COVID-19 exacerbated the pre-existing situation of low and inconsistent pay. For example, in Ethiopia, HEWs reported demotivation due to low salaries, and in India, ASHAs are compensated through task-based incentives rather than a fixed salary in some states, and incentive and salary payments are often delayed, with additional disruption during COVID-19 [ 62 ].
Managerial support for CHWs during COVID-19.
Given the challenges of work during COVID-19, support from supervisors had an important potential role in addressing new knowledge, safety and CHW well-being. There were examples of support from supervisors and managers; for example, in India, ASHA supervisors provided support during COVID-19 vaccination days [ 62 ]. However, COVID-19 often further reduced the quality of already inadequate supervision for ASHAs and AWWs: supervision became less frequent, was often conducted by phone (and so more difficult for ASHAs without easy phone access), and focused on disseminating instructions and discussing tasks related to COVID-19,rather than addressing CHWs’ concerns [ 76 ]. Inadequate advance planning and communication by higher level managers also created difficulties: some ASHA facilitators and ANMs reported only being told at 9PM about tasks for the following day, particularly related to COVID-19 vaccination. This hindered their ability to plan their work and arrange service delivery [ 62 ].
Support from peers, families and the community.
Beyond support from the formal health system, some CHWs received support from peers, family and communities for their work during COVID-19. One area involves working additional hours to cover for colleagues who could not work; for example, in Bangladesh, some health assistants (HAs) worked additional days to cover for community health care provider (CHCP) who could not reach the clinic during lockdown transport restrictions [ 59 ]. However, as with formal health system support, there were mixed experiences. For example, in India, some CHWs in one state reported regular discussions among ASHAs, AWWs and ANMs as well as other stakeholders on COVID-19-related work such as management of returnee migrants and food distribution [ 58 ].However, many CHWs reported a lack of collaboration and support from their peers or other CHW cadres, with COVID-19 or routine activities [ 76 ].
Families were a source of support for some CHWs. For example, in India, when lockdown limited transport, some ANMs and ASHAs relied on their husbands and relatives to facilitate transport to facilities and communities [ 70 ].
There were also examples of support from community members. As well as the support with PPE discussed above, some CHWs reported support from communities with COVID-19-related work, for example with community members providing information, and self-help groups, community-based organisations and community volunteers providing support with activities related to quarantine, surveillance and awareness raising [ 70 , 77 , 78 ]. Elected Women’s Representative (EWRs), who work at ward level in one state of India, also provided support, for example by stepping in to conduct Anganwadi Worker (AWW service delivery activities when AWWs were on strike due to lack of incentives, or unable to travel due to lockdown measures [ 74 ].
Challenges experienced by CHWs in providing services during COVID-19
CHWs experienced a range of challenges, both for activities related to the COVID-19 response as well as their routine service delivery. These challenges included issues related to the health system, such as limited human resources and gaps in supply chains; the effects of COVID-19 public health measures such as restrictions on gatherings and transport; and demand side issues related to community access and attitudes.
Health system factors.
Staff time and availability and increased workload . Prevention and management activities related to COVID-19 added to CHWs’ existing workload, exacerbating already heavy workloads related to systemic health worker shortages [ 58 , 59 , 79 ]. In some cases, CHWs’ routine services were largely suspended, for example during the 2020 lockdown in India, but where routine services were expected to continue, this was difficult for CHWs to manage alongside new COVID-19 responsibilities. For example, in Ethiopia, new tasks such as community awareness on COVID-19, led HEW to deprioritise their nutrition services [ 79 ]. In Bangladesh, additional activities were transferred from colleagues who could not work, for example due to being classified as vulnerable, or because they were in isolation as COVID-19 patients. Lack of staff in community clinics meant health assistants (HAs) worked overtime each day and at weekends to manage the patient load and to conduct home visits to COVID-19 patients [ 59 ].
In India, in some states, some ANMs worked in facilities (to ease the shortage of general nurses), while some focused on outreach, and others played a dual outreach and facility role. During the initial COVID-19 stages, outreach ANMs were reoriented to work in facilities and quarantine centres. When their outreach activities resumed, they were stretched between COVID-19-related work such as surveys, screening and quarantine management, and conducting their routine immunisation and ANC services. In addition, without support from outreach ANMs and with resumption of routine activities, facility ANMs struggled to provide services across cold chain management, the labour room, emergency care and outpatient department, particularly as COVID-19 screening and registration of returnee migrants increased facility workloads [ 58 , 67 ]. COVID-19 also brought long hours, with all CHW leave cancelled, and notable gender variations: due to their role in screening and quarantine, ANMs were instructed to be available 24/7, and go to the field at night if needed, something not requested for male facility staff [ 60 ].
Where workload and hours increased, this created stress for CHWs, particularly with trying to balance additional work with domestic responsibilities. For example, ASHAs in one state described stress related to balancing household chores with additional COVID-19 work, such as contact tracing, and uncertain hours [ 76 ]. Afs in one state also faced difficulty in managing additional workloads alongside domestic responsibilities, particularly as the household work burden increased with return of some family members during COVID-19 [ 60 ]. However, there were also examples of ANMs who lived on their own and so had fewer household responsibilities, who were able, or required, to work additional hours, including night shifts, to cover for ANMs with more family duties.
Medical supplies . Across countries, disruption to medical supply chains led to shortages, often exacerbating existing difficulties [ 11 , 29 , 58 , 65 , 79 ]. This affected the supplies needed by CHWs for their work. For example, in Ethiopia, COVID-19 affected supply of iron and folic acid and vitamin A distributed by HEWs [ 79 ]. In Bangladesh, COVID-19 lockdown restrictions hindered transport of medical supplies needed by CHWs. Transport difficulties also increased use of community clinics as people could not access higher level facilities, which led to a shortage of medicine at community level [ 59 ]. In India, lockdown disrupted supply of the rations distributed by AWWs [ 72 ], and some ASHAs reported shortage of supplies such as paracetamol, oral rehydration sachets and contraceptives; supplies were inconsistent pre-COVID-19, but shortages were exacerbated by increased supply chain disruption [ 72 ]. The situation improved in later months, with resumed availability of supplies and rations [ 72 ].
Restrictions related to COVID-19 public health measures.
Measures taken to prevent and control COVID-19 also affected CHWs’ service delivery. In particular, national guidelines and regulations on gathering and physical distancing affected whether services were allowed to operate or seen as possible, and wider movement restrictions and associated impacts on travel affected CHWs’ ability to access their place of work and communities.
CHWs’ home visits and community outreach activities were suspended during initial periods in several countries, with some routine Reproductive, Maternal, Neonatal and Child Health services not functioning during lockdowns [ 56 , 58 , 59 , 79 ]. For example, in India, community outreach services days for ANC and immunisation and the Village Health Sanitation and Nutrition Days were paused partly due to guidelines against group gatherings [ 60 ]. In Ethiopia, COVID-19 precautions around physical distancing made it more difficult for HEWs to provide services such as nutrition screening, which are usually conducted via community gatherings [ 79 ]. In Bangladesh, several CHW services were suspended, such as immunisation, satellite clinics and household visits by Family Welfare Assistants (FWAs) for activities such as distributing contraceptives. Follow up visits to people with tuberculosis were also suspended [ 59 ]. Physical distancing requirements also limited CHWs’ work when services were provided. For example, in Bangladesh, CHWs discussed the limiting effect of safety distance on ability to conduct examinations for ANC or to check blood pressure for patients with diabetes [ 59 ].
Movement restrictions and disruption to transport related to lockdowns also hindered CHWs’ service delivery, limiting their ability to visit health facilities and communities [ 11 , 58 , 59 , 72 , 76 ]. In Bangladesh, limitations on transport and movement made CCHPs’ daily commute to the community clinic more difficult, and meant some HAs had to walk to collect COVID-19 samples from patients rather than using transport. They also hindered ability of BRAC Shasthya Shebikas to meet TB patients, affecting continuity of care, and FWAs were unable to provide household services or set up Satellite Clinics. Increased transport fares also brought additional expenses for CHWs, in some cases leading them to reduce spending on other family essentials to cover transport costs [ 59 ]. In India, transport shortages made it hard for AWWs to collect and distribute home rations [ 58 ], and combined with reallocation of ambulances to the COVID-19 response, transport shortages made it difficult for ASHAs to conduct their role of escorting women for institutional deliveries [ 70 ], and in some cases meant ASHAs used their own money to pay for taxi services. Travel restrictions also made it difficult for HEWs to visit communities in Ethiopia [ 79 ].
Community access, demand and beliefs.
Travel restrictions also affected the demand side of health services by reducing community ability to access care [ 79 , 80 ]. For example, in India, ANC services provided at community health centres were often paused when these facilities were converted to quarantine centres, but even when these centres or private facilities were providing services, lack of transport hindered women’s ability to access them for ANC [ 80 ].
Community fears of infection or quarantine also affected CHWs’ services. For example, in Ethiopia and India, fear of infection reduced community visits to facilities [ 79 , 80 ]. In Bangladesh and India, some community members did not allow CHWs to enter their homes for visits due to concern about infection [ 59 , 81 ]. Community concerns about stigma and fear of quarantine due to being identified as having COVID-19 also reduced community demand, and affected community trust in CHWs and CHWs’ ability to perform their tasks. For example, in India, CHWs were expected to identify people with potential COVID-19, but community members were often reluctant to report symptoms due to fear of stigma or quarantine [ 72 ]. CHWs were also tasked with monitoring returnees, but migrant families did not want to provide phone numbers nor allow CHWs to paste quarantine slips used to indicate families potentially affected by COVID-19 on their doors [ 76 , 78 , 81 ].Broader political contexts also contributed to concern and reluctance, for example with wider tensions between religious groups and misperception of particular groups as increasing the COVID-19 spread contributing to fear of COVID-19 screening among some sections of the community [ 67 ].
Community concerns about infection, quarantine and stigma also led to stigmatization of CHWs and in some cases, aggression from community members. For example, in Sierra Leone, some CHWs experienced stigmatisation as carriers of COVID-19 [ 11 ]. In Bangladesh, CHWs were refused access to public transport when wearing PPE, presumably because this indicated that they had been in contact with people potentially affected by COVID-19 [ 59 ]. In India, there were examples of aggressive behaviour towards ASHAs from the families of people identified as having COVID-19, and suspicion that CHWs were working as informers to facilities or the police [ 58 ].
Adaptations to enable service delivery.
Several approaches were adopted by CHWs to adapt and continue work during COVID-19, partly through their own initiative but also directed by more senior health system managers and guidelines. The use of telemedicine was widespread, helping to reach clients when face to face contact was not possible due to movement restrictions or client concerns [ 56 , 59 , 67 , 79 ]. In several countries, CHWs used phone calls to provide maternal health services. For example, in India, ANMs used phone calls to pregnant women to check their health and screen for COVID-19 symptoms [ 70 ], and ASHAs phoned pregnant women to provide guidance and counselling on nutrition and precautionary measures during COVID-19 when facilities were closed [ 77 ]. Similarly in Pakistan, LHWs in parts of Karachi used phone calls to remain in contact with pregnant women and postnatal women when households were reluctant to have LHWs visit [ 56 ]. In Bangladesh, FWVs and CHCPs provided counselling via phone when lockdowns prevented community visits. BRAC Shasthya Shebikas also used phone calls to follow up TB patients for compliance with treatment [ 59 ]. While this enabled some service continuity, some CHWs in Bangladesh felt it reduced quality of service provision and hindered interpersonal communication [ 59 ]. In addition, low access to phones by community members meant these approaches could not reach all those in need, as seen in India with use of phones by AWWs, ASHAs and ANMs to communicate with community members [ 63 , 64 ].
Another set of adaptations is related to provision of medical supplies. In Bangladesh, knowing that the coming March 2020 lockdown would prevent household visits, FWAs provided clients with additional quantities of oral pills and male condoms in advance. CHWs also advised on alternative contraceptives when lockdowns prevented injections [ 59 ]. TB patients were also provided with additional medicines in Bangladesh [ 59 ] and India [ 82 ]. However, there were also examples of CHWs reducing provision of drugs to avoid stockouts: in Bangladesh, some CHCPs rationed the supply of medicines for patients to delay stockouts [ 59 ]. There were also adaptations to ensure CHWs had access to drugs when movement restrictions disrupted supply chains. In Bangladesh, when road barricades were imposed to restrict travel, BRAC sent TB medicines up to barricades, from where Shasthya Shebikas then collected them. For remote villages, the medicines would then be relayed through multiple Shasthya Shebikas [ 59 ].
There were also changes in service delivery locations. For example, in Bangladesh, when immunisation sessions could not be held in people’s homes, CHWs instead used schools, as they were closed and so available, and provided more space [ 59 ]. In Pakistan, LHWs provided maternity services for pregnant women from their own homes [ 56 ], and in Bangladesh, some CHWs supplied TB medications or contraceptives from their own homes when facilities were closed or CHWs could not make household visits [ 59 ]. In India, when community health days were stopped, ASHAs instead provided routine services such as nutrition via household visits, and AWWs provided rations via household visits (or collection from the AWW’s house) because anganwadi centres were closed [ 58 ]. Other adaptations included changes to the structure of service delivery. For example, in Ethiopia, some services delivered by HEWs were provided as campaigns to catch up on missed appointments, some HEWs divided villages into smaller groups to enable services despite restrictions on large gatherings [ 79 ]. Other examples include making use of COVID-19-related activities to provide other services: in India, there were examples of some district officials advising ASHAs to use household visits for COVID-19 surveys to also provide routine services such as those related to ANC, child health and TB [ 82 ].
Beyond the strategies above, some CHWs found additional ways to maintain services and support communities. These strategies often demonstrated personal commitment, including long working hours (as shown in 4.3.1). For example, ASHAs in India were busy with COVID-19 response activities during the day and so worked at night to escort pregnant women to facilities for delivery [ 70 ]. CHWs also used their own financial resources to overcome constraints, including purchasing their own PPE and covering extra transport costs as indicated in section 4.3. There were also examples of CHWs providing support to community members in need; for example, some LHWs in Pakistan distributed rations on their own when rising food prices and falls in income due to lockdowns left household vulnerable to malnutrition [ 56 ]. However, while demonstrating commitment, adaptations were also associated with a lack of choice and power, with many CHWs in India describing their situation during COVID-19 as involving ’majboori’, or helplessness and lack of options [ 64 , 67 ].
This paper contributes to growing learning about CHW roles. We know that CHWs are a critical component of the workforce providing health care services to communities and often reach the most marginalised groups, and that they need support to be able to fulfil this vital role [ 1 ]. Our findings highlight these issues in the context of COVID-19: they show CHW contributions to pandemic response; the influence of health system factors, wider government decisions, gendered hierarchies and community relationships on their work; the effects of inadequate support and other challenges on CHWs’ wellbeing; and CHWs’ agency and commitment in continuing service delivery; and variation in experience between CHW. The findings can inform strategies to support CHW roles and wellbeing during shocks such as pandemics, so contributing to strengthening health system resilience in shock-prone settings.
The ever-expanding role of the CHW
CHWs continued to play crucial roles in providing routine services in all countries in our study. Our synthesis showed that apart from routine service delivery CHWs were actively involved in COVID-19 activities such as contact tracing, community education and awareness on COVID-19, screening people with potential COVID-19 symptoms, counselling migrants. Similar roles in both the COVID-19 response and continued delivery of routine services during COVID-19 have been identified by other research, both in some countries included in our research, such as India, Sierra Leone and Kenya and in other contexts, as well as in global syntheses [ 8 , 16 , 18 , 22 , 83 – 85 ].
The potential for CHWs to support delivery of COVID-19 vaccines has also been recognised [ 86 , 87 ]. CHWs on the whole enjoy trust and are often embedded within their communities which enables them to take on a role in vaccine delivery [ 51 ]. Due to the relatively recent timing of COVID-19 vaccine rollout, there was limited information on CHWs’ roles in vaccination, both in the research used for this article and in the wider literature, but our paper indicates examples of CHWs contributions to vaccine uptake, and to some extent delivery.
However, there are challenges with this ever-expanding role of the CHW. They are often the funnel through which all programmes are delivered at the community level, requiring them to acquire new skills and knowledge, and cope with an increasing workload. Understanding the challenges CHWs face is critical to providing support that enables them to take on and sustain these roles.
CHWs need a package of support
Our synthesis shows that some support from the health system, peers, community and family was provided to CHWs as they took on new responsibilities and continued with their existing tasks. However, there were significant gaps in this support.
Health systems in all countries were ill-prepared to face the challenges of the COVID-19 pandemic [ 88 – 91 ]. This is reflected in the global level shortages of PPE [ 92 ], which resulted in inadequate supply to CHWs. This has implications on CHW’s ability and willingness to deliver services, and increased fear of infection for themselves as well as their families. Allocating PPE to the health workforce must consider the critical role of CHWs in pandemic response [ 23 ].
For CHWs to effectively take on new roles, training and supervision is essential. Our synthesis shows that although some training was provided, there were gaps. Supervision was also largely absent. Timely, quality training, and refresher training, are needed, and supervision is equally important, especially when responsibilities are new, complex, often stressful, and require sensitivity. Telephone, peer and group supervision that includes space to reflect and problem solve on CHWs’ experiences could help to reduce over stretched facility level supervisors [ 51 ].
From our synthesis, plans to provide additional financial incentives to CHWs working in COVID-19 did not always materialise. In some settings, CHWs were unaware that they should receive these. This finding is consistent with other studies on financial incentives for CHWs, and particularly in fragile settings, where livelihoods are often precarious, CHWs rely on the financial incentives provided for their role [ 93 , 94 ]. Studies show financial performance-based incentives can improve CHWs service delivery outcomes [ 95 ], and needs consideration in pandemic situations as well.
Our synthesis has shown that some CHWs experience mental distress and anxiety, as well as discrimination and stigma from family and community members. Similar issues have been identified in other studies during COVID-19 or other epidemics [ 17 , 96 – 98 ]. CHWs’ mental health and well-being needs to be protected. Recognition of the effects of the pandemic on mental health of CHWs is the first step, but this needs to be followed with provision of ongoing support for mental health and coping mechanisms, from health system actors and peers, families, and communities [ 96 ], during and after the COVID-19 pandemic [ 17 , 97 ]. We found that peer support can help with coping with the additional stress of the COVID-19 pandemic, as also highlighted in another recent review [ 98 ]. Photovoice method, albeit used more often in research, can also create space for CHWs to not only support each other but also jointly problem solve [ 51 ].
We also identified that families and community members can be a source of support, and can help CHWs carry out their responsibilities as seen in other studies [ 99 ]. However, there were also instances showing that family and community members can ostracise CHW because of fear of infection or misconceptions about COVID-19 or CHWs’ roles. This shows the need for clear messaging on CHWs’ roles and strategies to address stigma.
Many CHWs experience difficult working conditions and weak employment status during routine times [ 100 ], as noted in our synthesis in relation to the normality of fragile financial payments. Action taken to support CHWs during COVID-19 should address the systemic issues affecting CHWs, going beyond short-term measures to support stronger ongoing health system resilience and CHWs well-being [ 83 , 100 ].
CHWs show resilience and adapt their way of working
Despite numerous challenges, CHWs showed individual resilience, adapting the way that they work to continue delivery of services and take on new roles and responsibilities. Examples included using telemedicine as an alternative healthcare option, changing the way drugs were provided, and changing service delivery locations. These adaptations demonstrated high levels of personal commitment, including long working hours, as seen in other studies [ 17 , 21 , 22 ].
However, some adaptations came at personal cost for CHWs, including for their time and finances as well as mental health, suggesting that these adaptations are better viewed as ways of coping within a context of inadequate support, rather than positive resilience strategies. This signals the importance of ensuring health systems are robust, and so able to adapt without increasing population or health worker vulnerabilities [ 101 ]. Resilience should not be built on the back of a cadre that lacks system-driven support, rights and entitlements.
The article brings new evidence to the discussion on CHWs and COVID-19 and covers varied country contexts. The paper does not aim to represent the experiences of all CHW or of CHW in all countries. However, similarity of some finding with those in other articles on CHW and COVID-19 suggests some CHW experiences reported in this article are likely to be present in other contexts. However, our analysis has limitations. The nature of the pandemic and country response have changed over time, affecting CHWs’ roles, challenges and adaptations; the last report used in this synthesis was completed in November 2021, and CHWs experience may have since changed. In addition, each study had a specific purpose, and CHWs’ roles during COVID-19 were more central to some studies than others. As such, the reports do not provide directly comparable information across countries, and varied focus and purpose of the original reports means the depth and level of detail on CHWs experiences varied. Lack of evidence on a particular aspect in one country may therefore mean a gap in information in the reports, rather than indicating that this experience was not shared by CHWs in that context.
One strength of the paper is that it makes available evidence from consultancy reports that are often not accessible; few of the reports used for this synthesis were in the public domain, and none were published in the academic literature. However, the synthesis is restricted to information from research where OPM was involved, and additional evidence could be provided through a wider set of material and full evidence review. We hope this paper can contribute material for future, wider evidence synthesis by the global health community.
Finally, the heterogeneity in CHWs across cadres and countries (for example, in employment status, training and responsibilities as well as personal or household characteristics means significant diversity in CHWs experiences during COVID-19. The effects of this diversity could not be fully examined in this synthesis, but are an important avenue for further intersectional analysis.
CHW are critical for effective response to disease outbreaks, including pandemics like COVID-19. Their interface position between the community and the health system enables them to provide services to the most marginalised groups. However, this is not without challenges. To support CHWs’ contribution in providing essential services during an emergency and to protect their wellbeing, CHWs need adequate resources, managerial and financial support, and recognition of their role and challenges at all stages of the policy cycle.
Supporting information
S1 table. reports included in the synthesis..
https://doi.org/10.1371/journal.pgph.0001447.s001
S2 Table. Thematic framework for synthesis.
https://doi.org/10.1371/journal.pgph.0001447.s002
Acknowledgments
Our appreciation goes to all research participants for their contribution to the original studies used in this synthesis. We acknowledge the work of the original project team members in India, Bangladesh, Pakistan, Sierra Leone, Kenya and Ethiopia and their support for this synthesis, and the support from national and local governments in these countries. We also thank the Bill and Melinda Gates Foundation (BMGF), the Foreign, Commonwealth & Development Office (FCDO), the Global Financing Facility, the United Nations Children’s Fund (UNICEF), the U.S. Agency for International Development (USAID) and the World Bank for support and substantial technical input to the underlying projects, and for permission to use the material for this synthesis.
- 1. WHO. WHO Guideline on Health Policy and System Support to Optimize Community Health Worker Programmes. Geneva: World Health Organization. [Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK533330/ ]; 2018.
- View Article
- PubMed/NCBI
- Google Scholar
- 6. REACHOUT. Who are close-to-community health workers? [Retrieved from http://www.reachoutconsortium.org/about/ ].
- 13. Johnson G, Bedford J, Miller N, Islam K, Kapeu A, Wesseh C. Community Health Workers During the Ebola Outbreak in Liberia. New York: NY: UNICEF (2017). 2017.
- 15. MOHS. National community health workers’ policy 2016–2020. Ministry of Health and Sanitation, Sierra Leone. [Retrieved from https://www.advancingpartners.org/sites/default/files/sites/default/files/resources/sl_national_chw_policy_2016-2020_508.pdf ]; 2016.
- 24. WHO, UNICEF. Community-Based Health Care, Including Outreach and Campaigns, in the Context of the COVID-19 Pandemic. Interim guidance. Geneva: World Health Organization (WHO), United Nations Children’s Fund (UNICEF), International Federation of Red Cross (IFRC). [Retrieved from https://www.who.int/publications/i/item/WHO-2019-nCoV-Comm_health_care-2020.1 ] 2020. Contract No.: WHO/2019-nCoV/Comm_health_care/2020.1.
- 25. WHO. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. Geneva: World Health Organization; 2020 2020. Contract No.: WHO/2019-nCoV/EHS_continuity/survey/2020.1.
- 26. WHO. Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic: January-March 2021: interim report, 22 April 2021. Geneva: World Health Organization; 2021 2021. Contract No.: WHO/2019-nCoV/EHS_continuity/survey/2021.1.
- 27. WHO. Third round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic: November–December 2021: interim report, 7 February 2022. Geneva: World Health Organization; 2022 2022. Contract No.: WHO/2019-nCoV/EHS_continuity/survey/2022.1.
- 28. UNICEF. Ethiopia: COVID-19 Situation Report No. 11, 23–29 May 2020. UNICEF. [Retrieved from https://reliefweb.int/sites/reliefweb.int/files/resources/UNICEF%20Ethiopia%20Covid-19%20Situation%20Report%20No.%2011%20-%2029%20May%202020%20%281%29.pdf ]; 2020.
- 29. Hillier D, Newton-Lewis T, Nair R, Larsen C. Initial COVID-19 responses in Bangladesh, Kenya, Pakistan, Sierra Leone, and Uganda. Maintains. Oxford Policy Management; July 2020.
- 30. WHO. Health workforce requirements for universal health coverage and the Sustainable Development Goals. (Human Resources for Health Observer, 17). Geneva: World Health Organization; 2016 2016.
- 31. UNDP. Human Development Index (HDI) 2022 [Retrieved from https://www.hdr.undp.org/en/indicators/137506# ].
- 32. World B. World Bank Country and Lending Groups 2022 [Retrieved from https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups ].
- 33. Skilled health professionals density (per 10 000 population). [Internet]. World Health Organisation 2022.
- 34. Exemplars. WHAT DID BANGLADESH DO?: Exemplars in Global Health; 2022 [Retrieved from https://www.exemplars.health/topics/community-health-workers/bangladesh/what-did-bangladesh-do?login=true ].
- 36. RHIS. Duties and Responsibilities of FWA Bangladesh: Routine Health Informaiton System; 2018 [Retrieved from http://www.rhis.net.bd/fwa-eregister ].
- 37. Perry HB. Health for the People: National Community Health Worker Programs from Afghanistan to Zimbabwe: [Retrieved from https://chwcentral.org/wp-content/uploads/2021/11/Health_for_the_People_Natl_Case%20Studies_Oct2021.pdf .] Accessed on 23 April 2022; 2021 October 2021.
- 38. USAID, SPRING. Bangladesh’s Family Welfare Visitors: Getting Nutrition Messages to the Right Clients at the Right Time USA: the U.S. Agency for International Development (USAID), the Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING); 2016 [Retrieved from https://www.spring-nutrition.org/publications/success-stories/bangladeshs-family-welfare-visitors ].
- 46. MOHFW. Handbook for ASHA Facilitator. National Rural Health Mission (NRHM), Ministry of Health and Family Welfare (MOHFW), Govt. of India. [Retrieved from http://nhm.gov.in/images/pdf/communitisation/asha/Handbook_for_ASHA_Facilitators.pdf ]; 2012.
- 47. GoK. Taking the Kenya Essential Package for Health to the community: a strategy for the delivery of level one services. Division of Community Services Ministry of Health-Government of Kenya. 2006.
- 63. OPM. Frontline workers grant: project data. Oxford Policy Management; 2020.
- 64. OPM. The Bihar Technical Support Programme—learning grant: project data Oxford Policy Management; 2020.
- 66. GRHB. Intra-Action Review (IAR) on Public Health Preparedness and Response to Covid-19 in Ethiopia. Gambella Region. Gambella Region Health Bureau (GRHB), COVID-19 Public Health Emergency Operation Center in Collaboration with WHO and Partners; March 2021.
- 69. OPM., MOH., EPHI. Intra-Action Review (IAR) on Public Health Preparedness and Response to Covid-19 in Ethiopia. Final Report. Oxford Policy Managment (OPM), Federal Ministry of Health (MOH)-Ethiopia, Ethiopian Public Health Institute (EPHI); October 2020.
- 75. S-RBH., MOH., EPHI. Intra-Action Review (IAR) on Public Health Preparedness and Response to Covid-19 in Ethiopia. Sidama Region. Sidama Regional Health Bureau (S-RHB), Federal Ministry of Health (MOH)-Ethiopia, Ethiopian Public Health Institute (EPHI). March 2021.
- 79. OPM. Formative research on key nutrition specific interventions in Ethiopia. UNICEF Operational research on key nutrition specific interventions. Oxford Policy Management; August 2021.
- 82. OPM., MOHFW., NHSRC., KIIT., NTEP. Assessment of Institutional Arrangements and Human Resources of the National Tuberculosis Elimination Program (NTEP). Oxford Policy Management, Ministry of Health and Family Welfare (MOHFW)-GoI, and National Health Systems Resource Centre (NHSRC), Royal Tropical Institute (KIT), National Tuberculosis Elimination Program (NTEP).; February 2021.
- 84. ReBUILD. The gendered experience of close-to-community providers in fragile and shock-prone settings Implications for policy and practice during and post COVID-19 –A qualitative study report, Sierra Leone. ReBUILD for Resilience. [Retrieved from https://www.rebuildconsortium.com/wp-content/uploads/2022/01/CTC-Study-Final-Report_Sierra-Leone.pdf ]; 2021.
- 86. GAVI. Community health workers are critical in delivering COVID-19 vaccines: GAVI; 2021 [Retrieved from https://www.gavi.org/vaccineswork/community-health-workers-can-play-critical-role-efficient-covid-19-vaccine-delivery ].
- 87. WHO, UNICEF. The role of community health workers in COVID-19 vaccination: implementation support guide, 26 April 2021. Geneva: World Health Organization, United Nations Children’s Fund; 2021 2021. Contract No.: WHO/2019-nCoV/NDVP/CHWs_role/2021.1.
Volume 19 Supplement 3
Community Health Workers at the Dawn of a New Era
- Open access
- Published: 12 October 2021
Community health workers at the dawn of a new era: 1. Introduction: tensions confronting large-scale CHW programmes
- Stephen Hodgins ORCID: orcid.org/0000-0001-8365-3311 1 ,
- Maryse Kok ORCID: orcid.org/0000-0003-0889-8663 2 ,
- David Musoke 3 ,
- Simon Lewin ORCID: orcid.org/0000-0001-7521-9515 4 , 5 ,
- Lauren Crigler 6 ,
- Karen LeBan 7 &
- Henry B. Perry ORCID: orcid.org/0000-0003-0561-0492 8
Health Research Policy and Systems volume 19 , Article number: 109 ( 2021 ) Cite this article
8270 Accesses
32 Citations
11 Altmetric
Metrics details
Community health worker (CHW) programmes are again receiving more attention in global health, as reflected in important recent WHO guidance. However, there is a risk that current CHW programme efforts may result in disappointing performance if those promoting and delivering them fail to learn from past efforts. This is the first of a series of 11 articles for a supplement entitled “Community Health Workers at the Dawn of a New Era”.
Drawing on lessons from case studies of large well-established CHW programmes, published literature, and the authors’ experience, the paper highlights major issues that need to be acknowledged to design and deliver effective CHW programmes at large scale. The paper also serves as an introduction to a set of articles addressing these issues in detail.
The article highlights the diversity and complexity of CHW programmes, and offers insights to programme planners, policymakers, donors, and others to inform development of more effective programmes. The article proposes that be understood as actors within community health system(s) and examines five tensions confronting large-scale CHW programmes; the first two tensions concern the role of the CHW, and the remaining three, broader strategic issues:
What kind of an actor is the CHW? A lackey or a liberator? Provider of clinical services or health promoter?
Lay versus professional?
Government programme at scale or nongovernmental organization-led demonstration project?
Standardized versus tailored to context?
Vertical versus horizontal?
CHWs can play a vital role in primary healthcare, but multiple conditions need to be met for them to reach their full potential.
Key message box 1: summary
Key findings.
Across different settings, community health workers (CHWs) play diverse roles. Generally in large-scale programmes, CHWs have functions related to both health education and helping extend or bridge to primary healthcare services.
CHWs fall along a spectrum from lay/volunteer to more professionalized.
Nongovernmental organizations have played an important role in the development of CHW programmes and continue to engage with government in many public-sector CHW programmes.
While evidence-informed models, interventions, and tools are important, for programmes to be effective the approaches used also need to be responsive to the local context.
Over the past several decades, CHWs have played important roles in vertically delivered disease control programmes. Increasingly, CHWs are taking on broader roles in more integrated primary healthcare services.
Key implications
The CHW is one actor in a complex, dynamic, primary healthcare system comprised of diverse interacting actors, each having agency, interests, perspectives, and values. Robust delivery of services at the most peripheral level of the primary healthcare system—reaching all who could benefit—requires functional systems enabling CHWs to play a constructive part and that, in turn, depends on their role being well understood and appropriately supported.
The global health community is guided by the goals of achieving Universal Health Coverage (UHC) and ending preventable child and maternal deaths by 2030 [ 1 ]. Achieving these goals will require strengthened primary healthcare (PHC), which—in turn—will require well-supported CHWs . WHO and the World Health Assembly in 2016 called for renewed efforts to realize the potential contribution of CHWs as members of multi-professional PHC teams [ 2 ]. In 2018, WHO released a new guideline—based on systematic reviews of existing literature and programme experience—for health policy and systems support to optimize CHW programmes [ 3 , 4 ]. This guideline offers specific guidance on: selection, pre-service education, certification, supervision, remuneration and career advancement, planning, community embeddedness, and health systems support. In 2019, the World Health Assembly urged Member States to integrate CHWs within their health systems and provide them the necessary support to deliver safe and high-quality care, drawing on insights from the new WHO guideline [ 5 ].
The COVID-19 pandemic has drawn attention to how important it is to have a robust health workforce at the community level, available both to ensure continued delivery of key PHC services and to play a role specific to the pandemic response, including—depending on the setting—education, prevention, screening, case detection, contact tracing, promoting immunizations, and faciltating linkages with higher levels in the system [ 6 ]. For decades now, the relevance, effectiveness, and acceptability of CHW programmes have been debated, and ensuring the funding needed for these programmes to achieve good performance has generally not been a priority for governments or for donors. Over the past decade, only 2.5% of total official development assistance for health has been directed to CHW programmes and, of that, two-thirds has been earmarked for specific disease control programmes [ 7 ].
In low- and middle-income countries (LMICs), CHW programmes have often been no more than a half-hearted response from governments to what they viewed as a time-limited problem—the unmet health needs of hard-to-reach communities, including in rural and peri-urban areas. In the minds of many policy-makers and experts, CHWs will no longer be needed once more sophisticated health services are available.
In 1988, Gill Walt concluded that “unless adjustments are made, CHW programmes will drift towards demise, not because CHWs themselves cannot deliver, but because the support that makes them effective is, in general, absent” [ 8 ]. Much the same could have been said in 1998, in 2008, or in 2018. However, the notion of CHW programmes as a cheap solution to a temporary problem in low-resource settings is increasingly recognized as a fallacy, for several reasons:
Functional CHW programmes are not necessarily cheap. To operate effectively, at scale, substantial numbers of CHWs are required; and high-performing programmes require continuous, robust supervisory and logistical support.
CHWs can do far more than close temporary gaps. In addition to roles they have traditionally played in maternal/child health services, CHWs have made important contributions in epidemic response, for Ebola in West Africa [ 9 ] and, now, for COVID-19 [ 10 ]. Increasingly, CHWs are engaged in the detection and management of HIV [ 11 ], tuberculosis (TB) [ 12 ], chronic diseases (especially hypertension, diabetes and mental illness) [ 13 ], palliative care, and medical and social support for the elderly. There is every reason to believe that in the coming decades the CHW’s role will evolve, and they will also be essential in helping health systems reach their full potential in improving population health.
CHW programmes are also relevant to higher-resource settings. CHWs in high-income countries are making important contributions to address health needs [ 14 , 15 ]. It could be argued that CHW programmes will need to be an essential element—if not the foundation—for health systems in all countries regardless of their socioeconomic status and level of health system sophistication, if these systems are to fully meet the health needs of the populations they serve.
In 2014, several of the authors of this article contributed to the development of an online book, developed in response to a resurgence of interest in CHWs at that time, entitled Developing and Strengthening Community Health Worker Programs at Scale: A Reference Guide and Case Studies for Program Managers and Policymakers [ 16 ]. They were concerned that the cycle seen over the period from the 1970s to the 1990s might recur. Over that period there was at first renewed interest in CHWs, which was followed by inadequately financed and poorly planned programmes, causing weak programme performance and the eventual abandonment of the programmes altogether, as happened with the Village Health Guides programme in India [ 17 ] and other programmes.
Table 1 (below) lists the major national CHW programmes in LMICs included in a newly published compendium of case studies [ 18 ]. These programmes have over 8 million CHWs, although this is certainly not an exhaustive listing of CHW programmes; even in these countries, there are categories of health workers that could be considered CHWs that are not included. With the exception of most CHWs in South Africa and those working for Building Resources Across Communities (BRAC) in Bangladesh, who are employed by nongovernmental organizations (NGOs), all of the CHW cadres described in the compendium work within ministry of health (MOH) programmes. In this series, we will draw lessons particularly from the programme experience documented in these case studies.
Now, in 2021, we have written this series, titled “Community Health Workers at the Dawn of a New Era”, to inform the development and strengthening of large-scale CHW programmes, and to encourage the growth of new programmes in the future. This set of papers is similar to the systematic reviews commissioned in support of development of the 2018 WHO guidelines in that it is intended to provide guidance for the development of national CHW programmes, but it differs in three important respects:
It draws not only on peer-reviewed journal articles but also on grey literature sources, including the recently released 29 CHW case studies [ 18 ], as well as other recent publications (from both the peer-reviewed and the grey literature) released since the 2018 WHO guideline was written. This series draws on insights from the field from public health professionals with long experience with large-scale CHW programmes.
Its scope extends considerably beyond policy and systems supports and includes detailed exploration of broad substantive issues not covered in the 2018 WHO guideline, as shown below.
It explicitly addresses the need to accelerate progress in achieving the 2030 global health goals, especially for those goals for which the contribution of CHWs is critical.
The authors believe the tide has turned; we are seeing countries engaging in these programmes with increased political support, greater commitments of financial resources, and a more robust integration of CHWs within the PHC system. This turnabout holds the promise of more effective programmes and services, and ultimately greater impact on population health outcomes.
The papers in the series include the following:
Introduction: tensions confronting large-scale CHW programmes (this paper)
Planning, coordination, and partnerships [ 19 ]
Governance [ 20 ]
Financing [ 21 ]
Roles and tasks [ 22 ]
Training [ 23 ]
Supervision [ 24 ]
Incentives and remuneration [ 25 ]
Relationships with health systems and communities [ 26 ]
Performance and performance assessment [ 27 ]
Conclusions and leading the way to Health for All [ 28 ]
The set of papers is organized conceptually in Fig. 1 .
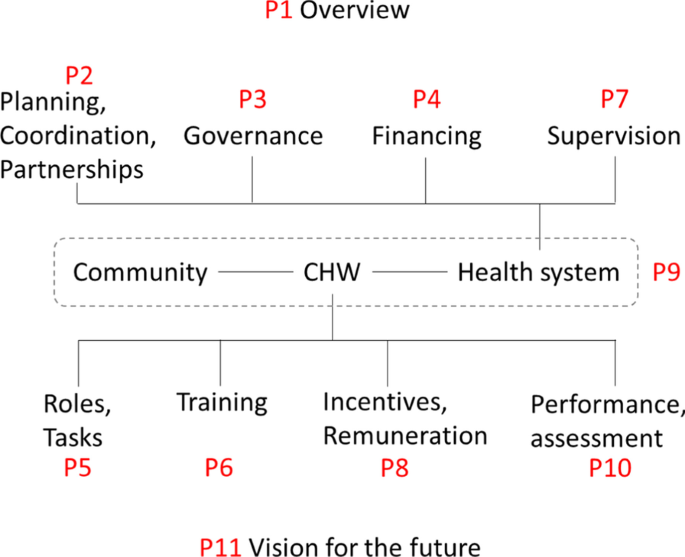
Conceptual framework for the articles included in the supplement on “Community Health Workers at the Dawn of a New Era”, grouped in relation to health systems considerations and factors relating more directly to the CHW. “P” refers to the paper in the supplement, and the number following it is the number of the paper in the supplement. The references for all the papers are in the body of the paper
These papers build on two previously published papers in Human Resources for Health focused on issues facing large-scale, generally national, CHW programmes [ 17 , 29 ]. This paper, the first in the set, is a commentary, drawing not only on the peer-reviewed literature but on the case studies referenced above, other grey literature, and the authors’ experience with large-scale CHW programmes.
The community health system and its actors
In publications about CHWs, often the context and the systems of which CHWs are a part—notably, the peripheral PHC services—are relatively neglected, giving a decontextualized picture of the role and function of CHWs. A blinkered perspective on the part of those working with these programmes will result in less appropriate policy, plans, and programme designs and, therefore, in services that less adequately meet the needs of the populations they are intended to serve.
Schneider et al. [ 30 ] explain that “CHW programs interface with both the formal health system (requiring integration) and community systems (requiring embedding) in context-specific and complex ways… [D]ebates on community-based delivery of services to achieve Universal Health Coverage could more properly reflect the emerging systems perspective, by widening the focus from a cadre to the community health system as a whole.” They describe “community health systems” as including formal and informal, community-based and government actors and service providers, who work in specific contexts shaped by local histories, economic and political systems, and sociocultural norms. Kok et al. [ 31 ] also point to the intermediary position occupied by CHWs, belonging to both the community and the formal healthcare system. This and earlier published work [ 32 ] stress the often neglected, so-called soft characteristics of community health systems: ideas, interests, relationships, power, values, and norms, and how these soft characteristics influence perceptions of support, respect, competence, honesty, fairness, and recognition. We explore these issues further in Paper 9 of this series, which focuses on the relationships of CHWs with the health system and the community [ 26 ].
To better understand CHWs, it is helpful to begin by considering the CHW within the context of the community (s)he serves as well as within the programmatic and service delivery context in which (s)he functions . CHWs work with a wide range of other cadres in their setting. The needs and requirements of each cadre, each manager, each actor in the peripheral PHC system, must be adequately addressed in order for this “ecosystem” to function optimally. Interaction among these system elements influences the performance of particular actors, including CHWs, and the evolution of these dynamics over time. Figure 2 is offered as a simplified schema, illustrating key actors at the most peripheral level of the PHC system along with the relationships and interactions among them.
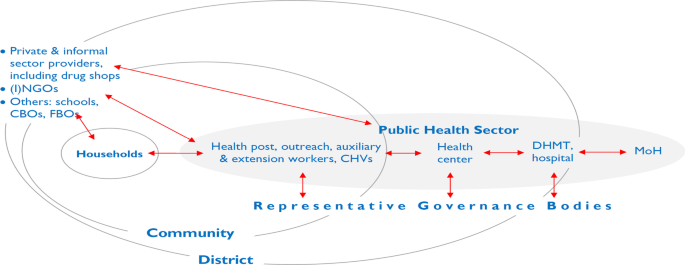
Elements and relationships in the work of the peripheral health system (public, private, and household). (I)NGOs international and national NGOs, CBOs community-based organizations, FBOs faith-based organizations, CHVs community health volunteers, DHMT district health management team, MOH Ministry of Health. Relationships indicated in red
As shown in Fig. 2 , the household has a primary role in the production of health [ 33 ], in part through its interaction with the peripheral health system. The community (consisting of complex systems of its own) overlaps here with the peripheral level of the government healthcare system. The community has a fundamentally important role to play in establishing conditions within the community that may be more or less favourable to attaining better health; furthermore, community members can also play an important role in supporting and holding accountable those providing health services, including CHWs.
The most peripheral tier of the PHC system often includes fixed structures below the level of health centre. They go by various names, including dispensary, subcentre, community clinic, and health post. In many countries, some services are offered through periodic outreach. Staffing can include CHWs and volunteers with varying profiles. In this paper, we will consistently use a typology consisting of three broad categories, which we will explain later in the paper. They include what we will refer to as:
auxiliary health workers,
health extension workers (HEWs), and
community health volunteers (CHVs).
In many CHW programmes, auxiliaries or HEWs are responsible for supervising CHVs [ 24 , 34 ]. If the CHV has tasks involving community-based distribution or case management of childhood illness, supervisory contacts can be the principal means of resupplying CHVs with programme commodities. Issues of supervision are explored further in Paper 7 of this series [ 24 ]. These contacts also provide an opportunity to systematically gather data on service delivery by CHVs. HEWs themselves may be supervised by a health worker based at the health post or a higher-level facility. In some programmes, there are dedicated supervisors who spend all or most of their time supervising HEWs (or CHVs). In other settings, the supervisory role is assumed by staff who have other management and clinical functions [ 24 , 34 ]. In many countries, there are entities at the district level (or equivalent), such as district health management teams, with technical and managerial oversight responsibility for peripheral-level PHC services, including the work of CHWs (including supervision, monitoring/reporting, logistics, and finance).
Settings with multiple tiers of CHWs (including volunteers) can be understood as dual- or multi-tier systems [ 35 ], as explored further in Paper 5 in this series [ 22 ]. Examples include: Ethiopia’s HEWs and Women’s Development Army volunteers, Niger’s agents communautaires and relais volunteers, and Nepal’s auxiliary health workers and female community health volunteers (FCHVs).
Staff in the peripheral tier of the PHC system may have oversight from health facility committees or boards [ 9 ]. In some instances, local bodies have authority over financial and hiring/firing decision-making. In Fig. 1 , representative governance bodies include entities such as village health committees, development committees, health facility community boards, and local and district government to which local health service providers are accountable. As Schaff et al. point out [ 36 ], accountability can be understood in vertical terms—up through a hierarchical management structure and down to the population to be served (accountable to locally representative governance bodies of the types noted).
In many settings, private providers play an important role, particularly in sickness care. This may include both formally recognized health professionals and uncredentialed informal providers, such as traditional healers, traditional birth attendants, and drug sellers [ 35 – 37 ]. In some country settings, government and development partners have engaged the medicine shop sector using social marketing and social franchising models that press medicine shop proprietors and staff into service to pursue public health goals, such as improving the availability (and sometimes quality) of family planning and sick-child care services by dispensing contraceptive products, and oral rehydration salts and zinc for diarrhoea. In some instances, although not officially recognized, government PHC workers supplement their incomes in private practice. This includes extension and auxiliary health workers operating medicine shops or working privately as “village doctors” [ 38 ].
Perhaps the most paradigmatic role of the CHW is interacting with members of the community in either the CHW’s or the beneficiary’s home, as we explore further in Paper 9 in this series on relationships of CHWs with communities [ 26 ]. Two prominent types of service offered during such “doorstep” or “domiciliary” contacts are counselling/health education and dispensing health-related commodities. Their role may also entail assessing aspects of their beneficiary’s health, well-being, or household health-related practices (for example, breastfeeding or correct use of an insecticide-treated bed net). CHWs may have direct contacts with all households in their catchment area, or only with households targeted because of certain demographic characteristics, for example, those households with a pregnant woman, a child younger than 2 years of age, or someone with a specific disease (TB or HIV). CHWs are commonly an important feature of TB and HIV programmes, providing adherence support, often through home visits.
CHW outreach services may be provided in various locations in the community, such as schools or other public places such as markets. This is a commonly used strategy for routine immunization, family planning, and antenatal care. In many programmes, such outreach services are offered on a monthly basis in different locations in a health facility’s catchment area. In many countries, CHWs are also involved in periodic, campaign-style outreach activities, offered on an annual or semiannual basis, during which immunizations or key health commodities are administered or dispensed. We discuss these modalities of service delivery further in the section below on vertical versus horizontal organization of services.
In some programmes, CHWs have responsibility for a specified number of households (and the associated geographic area covered). The number of households they are expected to cover can be an important determinant of programme performance [ 39 ]; programmes in which local CHWs are spread too thinly will be unable to achieve good population coverage for prioritized interventions for which they are responsible.
To the degree that CHWs are involved in delivery of services that depend on commodities, robust logistics systems (another element of the community health system) are an absolute requirement for both programme effectiveness and credibility with the intended users of community health services. In all but 9 of the 29 case studies of national CHW programmes included in the recently published compendium mentioned earlier [ 18 ], inconsistent supply of programme commodities was noted as a significant threat to performance. When commodities are not available on a regular basis, communities lose confidence in CHWs and, in turn, CHWs are less satisfied with their work.
In summary, a CHW is one actor in a complex dynamic PHC system comprised of diverse actors with agency, interests, perceptions, and values, in interaction with each other. Robust delivery of services at the most peripheral level of the PHC system—reaching all who could benefit—requires functional systems enabling CHWs to play a constructive part, and that, in turn, depends on their role being well understood and appropriately supported.
Tensions confronting CHW programmes
Rich or poor, essentially all societies fall short with regard to eliminating health and social disparities and ensuring robust, well-coordinated, comprehensive healthcare for all. It is widely recognized that having an actor at the interface between the community and the healthcare system can be part of the solution to this problem, and hence, the perennial interest in CHW programmes.
Recently, important new recommendations on policy and systems support for CHWs have been released [ 3 , 4 ], drawing on published evidence [ 2 , 3 , 34 ]. Indeed, organizations such as WHO seek to provide guidance based on the best available evidence on effectiveness and, increasingly, on considerations such as acceptability and feasibility. Relative to their importance for health systems, the body of research on large-scale CHW programmes has been modest (although there have certainly been many published small proof-of-concept trials). A range of research and evaluation methods is required to generate the evidence needed to develop large-scale effective community health services, including robust, pragmatic implementation research on large-scale programmes. As stated in the 2018 WHO guideline:
In calling for additional research on the topic, it is important to recognize that, while more methodologically robust evidence is needed, it is probably unrealistic to envisage that there would be large-scale RCTs [randomized controlled trials] to address, from a pure effectiveness perspective, all the persisting evidence gaps [particularly with regard to systems supports required for effective programmes]. Furthermore, RCT design is relatively unhelpful in providing insights into the dynamics of complex programmes. More useful would be comprehensive, critical programme case studies. [ 3 ], p. 66
Drawing lessons from such programme case studies, this article and the series of which it is a part seek to direct attention to key considerations for building strong community-based PHC services. These papers focus on programmes in LMICs, primarily serving rural areas, Footnote 1 using cadres ranging from part-time volunteers to paid, full-time, para-professional health workers.
This paper considers several important questions or issues facing those interested in delivery of services at the most peripheral level of the PHC system, which we are characterizing as “tensions”. The authors have framed these issues as tensions in the hope that this will aid policy-makers and programme developers in avoiding overly simplistic solutions and will, instead, give due attention to sometimes under-recognized tradeoffs that need to be made in optimizing for strong, effective programmes. The first two sections of the paper focus more specifically on the CHW, and the following three, on broader issues with PHC and CHW programmes.
1) What kind of a role should the CHW play?
A lackey or a liberator provider of clinical services or health promoter.
Some 40 years ago, David Werner posed the provocative question: is the CHW a “lackey” or a “liberator”? He was highlighting the distinction between extending health services and being a catalyst for social change [ 40 , 41 ]. It is clear from his choice of words that Werner had ideological reasons for preferring one over the other. Colvin has drawn attention to this same tension using the less politically charged language of “extension agent” versus “agent of change” [ 42 ]. Even now, this tension has not been altogether resolved. Dating back into the nineteenth century, there has been divergence between those who see public health as a technical and biomedical enterprise focused on disease control and those who see it as a sociopolitical effort with a broader focus on well-being and on its social and economic determinants (for example, see the work of Rudolf Virchow [ 38 ]). So it is not surprising that this tension is also evident in relation to the roles CHWs should be playing. Should CHWs be public-sector employees or activists within a people’s movement? Should they be focused on provision of biomedical interventions or on advocating for the vulnerable within their communities?
In practice, most national public-sector programmes have focused on the narrower service delivery role of CHWs. Nevertheless, in many programmes, there remains an expectation that CHWs act as intermediaries between communities and health services, and that at least part of their work consists of health education or health promotion, encouraging behavioural (if not sociopolitical) change. This role as change agent (as health promoter) is often undervalued by both governments and communities, compared to biomedical services (e.g., sick-child care, family planning, immunization, dispensing mosquito nets). Paper 5 in this series, on CHW roles and tasks, explores these issues further [ 22 ].
Policy-makers and planners have responded to the shortage of trained health professionals in underserved areas by shifting clinical tasks that would normally be done by physicians or nurses [ 41 ] to health auxiliaries, extension workers, and other types of CHWs [ 34 ]. This may include assessment and treatment decisions for illness care as well as certain procedures, such as administering injections (typically vaccines and injectable contraception). Task-shifting may be a sound choice in settings where there is a shortage of health professionals with more advanced training. Indeed, being assigned such functions is often motivating to CHWs. However, in many instances, physician and nursing associations have opposed shifting tasks to CHWs, citing concerns about safety and lack of necessary skills, but, arguably, being more concerned about protecting a monopoly provider role, even when very few of their members are interested in serving in rural areas [ 9 , 32 ]. In settings where there has been increasing professionalization and increasing numbers of health worker cadres providing services at the PHC level, there has been some upward task-shifting, with functions previously performed by lay health workers now falling within the responsibilities of paramedical professionals. For example, in Nepal immunization used to be the responsibility of village health workers, but is now primarily done by more professionalized auxiliary health workers.
Table 2 provides examples of common roles of CHWs in national programmes. Paper 5 in this series [ 22 ] explores the roles and tasks of CHWs in greater detail. In the first three roles shown in Table 2 , the CHW potentially plays more than only a service delivery role; s(he) may also be an intermediary between the community and the health system. For these functions, effectiveness can be enhanced if the CHW is not only a service provider integrated within the healthcare system but also an embedded member of the community. This may be less important for the remaining functions. Note that the roles outlined here reflect current CHW programmes; as the roles of CHWs and indeed the healthcare system as a whole continue to evolve, we can expect further evolution in the content of CHW work.
Once CHW services become reasonably well established, there is a tendency to add new functions, responsibilities, and tasks. For example, Ethiopia’s HEWs began with responsibilities related to 16 different programmes (mainly prevention- and promotion-related). However, over time, numerous other responsibilities have been added, resulting in the “overloading” of a CHW, with the inevitable result that certain tasks end up deprioritized. Even if policy-makers and programme planners intend that CHWs focus primarily on health education or health promotion, communities tend to perceive greater value in clinical services, so, in turn, CHWs tend to prioritize what is most valued by their beneficiaries. There is generally higher status accorded to a role more closely approximating that of a physician, and in addition, members of the general population may perceive CHWs as offering second-class quality of care and opt to bypass them to seek care from providers they believe to be more qualified. In brief, although in most programmes it is not expected that CHWs play a role of social or political change agent, commonly they do have a role in health education/health promotion and act as intermediaries between health services and the community. Across programmes, there is a diverse range of specific functions, roles, and responsibilities that have been assigned to CHWs.
2) CHWs, lay or professional?
Lay to professional.
In general, where a particular cadre falls along the lay-to-professional axis correlates with duration of pre-service training and licensing. CHWs who receive no more than a few days or weeks of training fall at the “lay” end of the spectrum, whereas CHWs with 1–2 years of training, or more, can be seen as falling towards the professional end. When these health workers are licensed by a formal accreditation body, they may be considered to be mid-level health workers rather than CHWs. Issues of training are explored further in Paper 6 in this series [ 23 ].
Unpaid to salaried
The second axis concerns remuneration, which ranges from volunteers who do not receive any to service providers who are in formal employment and receive a salary and other financial benefits (e.g., a pension). We explore issues of remuneration in Paper 8 in this series [ 25 ]. Between these extremes, there is a wide variety and range of remuneration packages including monthly honoraria, travel or meal allowances (per diems), and performance-based incentives based on volume of certain services performed (e.g., accompanying a woman to a hospital to give birth). In some programmes, the total value of such allowances and incentives may approximate salaries at the low end of the civil service pay scale [ 36 , 43 ]. These various arrangements reflect differences in CHW roles and responsibilities, in the settings and responsibilities, and the settings in which they work, as well as in factors such as the value placed on volunteer work, the extent to which being a paid government worker is viewed positively, and whether CHWs are able to control when they work.
One shared characteristic across all LMICs is that the majority of the working-age population is employed in the informal sector. In such an economic context, most CHWs may not have the expectation of salaried, formal-sector employment. They certainly, nonetheless, need to support themselves and their families. There are often opportunity costs associated with CHW work: time spent on CHW duties is time unavailable for other income-generating activities. There are also many examples of CHWs spending their own money to perform their role without being compensated, such as transportation expenses to help a patient obtain healthcare at a facility or needed medication [ 44 ].
Part-time to full-time
The third axis refers to the number of hours or days a CHW works. Some CHWs have only occasional involvement, for example, participating in semiannual campaign-style outreach activities such as child health days, while other CHWs are full-time workers. Between the extremes on the continuum, there are cadres that do not work full-time but are engaged in CHW work almost every week and, in some programmes (and for some individual CHWs) on a close to full-time basis.
It must be noted, however, that where a particular cadre falls on any one of these axes is not perfectly correlated with where it falls on the other two.
CHW definitions
Most definitions used over the past decade have defined a spectrum of CHW cadres from volunteers with brief informal training to paid, professionalized CHWs, with up to 2 years of formal pre-service training (as illustrated in Box 1 , below).
Box 1. CHW definitions in the global literature
It is evident from the country programme case studies in the newly published compendium [ 18 ] that in most LMICs, there have been progressive improvements in levels of education over the past several decades, with the result that there has been an evolution of CHW programmes towards higher educational entry requirements, longer pre-service training, and an increasingly professionalized role. In principle, licensing bodies set standards for professional practice and serve a quality assurance function. Professional associations serve as a voice for their members, advocating for their interests. Although increasing professionalization may also serve the public’s interest, this is not always the case. In Zimbabwe, in the late 1990s, the professionalization of nursing—by phasing out enrolled nursing training (2 years) in favour of registered nursing training (3 years)—contributed to staff shortages in rural PHC services, as graduates of the 3-year training programme were less interested in working in such positions, preferring hospital-based employment (or emigration).
In some recent documents, greater than 2 years of pre-service training has been the threshold for workers to be considered mid-level health workers rather than CHWs. However, this needs to be understood as an arbitrary cut-off and one that is likely to change over time, as education standards continue to rise and there is increased professionalization across all occupational types. For now, it may be helpful to think of CHWs as falling into several major categories, along a lay/volunteer-to-professional spectrum, where—at the most professionalized end of the spectrum (what we are labelling “auxiliary health workers”)—they grade into what could be considered mid-level health workers rather than CHWs. Note that not all categories of CHW programmes fall neatly into one of the types shown in Table 3 .
Some programmes having what we are describing as “regular volunteers” make heavy use of allowances, per diems, and/or performance-based incentives. These volunteers are normally from, and live within, the communities they are serving. They are not considered to fall within formal sector employment. Although their role consists primarily of health education and linking people with health services, their functions may include dispensing (e.g., birth control pills, condoms, mosquito nets, and micronutrient supplements) and case management of childhood illness. In rare cases (e.g., Madagascar), they may give injectable contraceptives. In some programmes, duties and terms of service of regular volunteers start to approach those of HEWs (see Table 3 ), with significant part-time involvement (e.g., 10+ hours per week, as is common for accredited social health activists [ASHAs] in India) and financial incentives representing an important source of income. These may be performance- or commission-based; in some programmes, community health “volunteers” receive honoraria or allowances that could be considered de facto small salaries. In other programmes, although these CHVs perform regular functions, they normally put in less time (e.g., 5 h/week or less), and financial incentives may be minimal or not used at all.
In some countries, there are programmes with “occasional” volunteers who may be very numerous (e.g., the 3 million Women’s Development Army volunteers in Ethiopia). Typically, these episodic volunteers have functions limited to health promotion, though they may also be involved in periodic campaign-style events, distributing health commodities such as insecticide-treated nets, ivermectin (for prevention of river blindness/onchocerciasis), vitamin A, or vaccines (e.g., oral polio). Some countries in sub-Saharan Africa make use of such volunteers under a community-directed interventions model, in which the responsibility for leading and managing distribution—including selection and oversight of volunteers—rests with community leaders [ 52 ].
There are certainly categories of workers or volunteers that straddle the three categories we have identified here; as we have noted, Ethiopia’s HEWs fall at the boundary of our distinction between auxiliary health workers and HEWs, particularly with regard to duration of pre-service training. India’s ASHAs fall within the volunteer category, however in some parts of India, ASHA remuneration from allowances and performance-based incentives can approximate a salary [ 53 ].
In some local health systems, there are workers or volunteers corresponding to all the levels identified above; in many, one or more are missing. For any but the lowest of these cadre types, responsibilities may include support and supervision of lower-level cadres.
It may be most constructive to use terms and typologies descriptively (not prescriptively). Effective CHW programmes come in many shapes and sizes. The bottom line is: does it work and are arrangements fair and acceptable to those involved? But circumstances are continually changing. What was an effective model in the past will not necessarily be one in the future.
From our focus, under the first two tensions, on what roles CHWs play and how they can be defined, broader programmatic issues relevant for the organization and delivery of peripheral-level PHC services, making use of CHWs.
3) Government programme at scale or NGO-led demonstration project?
There are two related issues here: ownership/identification and scale.
Primary identification with government or with an NGO? Who is running the show?
Of the programmes addressed in the case study compendium [ 18 ], several are well established and have been in existence for decades. The CHWs are paid civil servants, and financing for their support comes entirely from domestic government sources. Examples are the community health agents in Brazil [ 54 ] and the family welfare assistants/health assistants of Bangladesh [ 55 ]. Their continued viability and contribution is not dependent on external project-based donor support. However, there are other CHW programmes that are, in effect, only nominally government programmes, in which support from external partners is essential for their continued activity. Yet other programmes lie somewhere in between, where external partner support for in-service training, supervision, and other programme inputs may result in ambiguity concerning who exactly the CHWs belong to. Thus, there is a tension inherent in coordination, partnerships, and governance—as addressed in Papers 2 and 3 of this series [ 19 , 20 ]—between the strategy for a CHW programme being driven by a national or subnational government or by development partners and donors.
Under these conditions, there are a variety of potential threats. How do inputs from external partners either contribute to or undermine the capacity of government PHC services and systems as well as the leadership role of government? We discuss this further in the papers in this series on planning, coordination and partnerships [ 19 ], governance [ 20 ], and financing [ 21 ]. How can sustainability be ensured? Who determines what should be prioritized? If the donor-supported partner is especially interested in seeing a particular intervention scaled up and delivered by CHWs, what impact could that have on other tasks the government expects of the CHW? What kind of engagement by international NGOs (INGOs), local NGOs, and faith-based organizations with government PHC services and programmes is most productive (and what practices should be avoided), with regard to both short-term gains in coverage on key interventions and longer-term strengthening of PHC services and systems?
Part of this tension has to do with the relationship between the government (at national, regional, district, and local levels) and its major development partners. To what extent does the government insist on, and development partners appropriately recognize, the government’s leadership role in setting priorities and making strategic choices, including with regard to PHC services? To what extent is the health system decentralized so that more local authorities can make context-specific decisions regarding their programmes and services and the role of development partners? These issues are also discussed in Paper 2 in this series on planning, coordination, and partnerships [ 19 ].
When resources directly available to governments are very limited, the added resources partners bring to the table can tilt priorities in directions favoured by the partners. For programmes supported by partners, often there is a felt need for some field-level worker, for example for HIV- or TB-related work, for nutrition, or for maternal/child health. Partners may then invest in supporting just these specific elements within the local health system, without regard for consequences on the broader range of services to be delivered. The best-funded programmes will then tend to bias efforts of the PHC system in the direction of their particular interventions. Moving from conditions of relatively heavy dependence on donor support to ownership by the government, there is a generally a need for (1) adequate, mainstreamed system supports, and (2) strong leadership/management. A viable, sustainable CHW programme will not be feasible—generally speaking—if implemented as part of a weak, inadequately resourced, peripheral-level PHC service. CHW programmes as add-ons or afterthoughts will not contribute much, at least not on a sustained basis. Work done by CHWs needs to be understood as part of the core work of the government’s PHC system.
Although there are circumstances in which INGOs have played and will continue to play a very constructive role contributing to ensure delivery of key services at the peripheral level of PHC, their support is often focused on comparatively narrow, mainly clinical areas (including preventive services such as immunization). Furthermore, by the nature of the funding, there is an incentive for INGOs to promote and support adoption and scale-up of new interventions, tools, and programmes. This often results in overloading, in the sense of multiplying the number of activities, interventions or vertical programmes that existing CHWs are expected to support. In practice, the problem is most often that other activities get crowded out, and the actual, on-the-ground prioritization by CHWs, as “street-level bureaucrats” [ 56 ], may not necessarily correspond to what is most likely to produce a significant population health impact.
On the other hand, there are many circumstances where NGOs play an important role at the district or subdistrict level by responding to specific needs of the peripheral health system, especially in conflict areas, areas with disease outbreaks, and those with hard-to-reach populations. They may also be instrumental for programmes in which CHWs play a social activist role by seeking to reduce inequities in health or address the social determinants of health. In some settings with fragile health systems, such as in Afghanistan, governments contract with NGOs at the provincial level to support delivery of the government’s PHC strategy.
Small-scale, demonstration project or national-scale programme?
Certainly, findings from studies of comparatively small-scale, externally supported programmes can have relevance for nationally scaled programmes. However, efforts to introduce and scale up apparently successful small-scale models often result in disappointing performance. There are two related stumbling blocks: first, merely because something has worked well on a small scale, with dedicated resources, does not necessarily mean there is any realistic prospect of achieving similar effectiveness when one attempts to implement something similar at large scale, under routine programme conditions. Second, even if a model has been quite successful at scale in one setting, this is no guarantee that the same success can be replicated in a different context with different health, political and community system arrangements. The success of any given approach is rarely due only to the intervention; invariably, characteristics of the local system and context also matter.
One common scenario is an NGO-piloted CHW programme that the NGO, in turn, seeks to have the government adopt, scale up, and institutionalize. Sometimes this can be successful. Over the past 50 years, there have been a variety of highly influential, small-scale CHW programme experiences developed and led by NGOs or university-based groups. These experiences have served as the inspiration for important global initiatives in community health. For example, the 1978 Declaration of Alma-Ata was inspired in part by such experiences [ 57 ]. Similarly, today, recommendations are made to MOHs and donors, calling for large-scale, public-sector CHW programmes based on experiences with much smaller, more intensively supported programmes.
But there are also counterexamples. An example of the disconnect between successes observed in well-supported, small-scale programmes and efforts to implement similar programmes at large scale is the intensive postnatal, home-visit approach pioneered by Bang and colleagues in Maharashtra, India [ 58 ]. Based on this documented success and a few other relatively small-scale, intensively supported RCTs and demonstration projects, in 2009 UNICEF and WHO jointly issued a call to MOHs [ 59 ] to introduce such programmes at scale. Such programmes were subsequently widely adopted, but none have achieved high rates of effective coverage (and therefore population-level health impact) [ 60 ]. The translation from a successful small-scale demonstration project to an effective large-scale programme is not straightforward; it takes time and continued nurturing. And in some instances, the translation to scale will not be feasible. It is crucial to understand the conditions necessary for successful implementation of a particular approach and what it would take to meet and sustain these conditions at scale [ 61 ]. For successful large-scale CHW programmes, it is critical to develop adequately robust organizational support, including information systems, programme-commodity supply chains, management, supervision, and quality oversight. Lack of attention to these dimensions has resulted in lost opportunities for programme impact in many CHW programmes, as is evident in some of the compendium case studies [ 18 ].
4) Standardized or tailored to context?
Recently, there has been renewed interest in CHW programmes at a global level, with new or revised programme guidelines [ 3 ] and planning tools [ 62 ]. Footnote 2 But elaboration of such guidelines introduces an inevitable tension.
It is true that those responsible for developing the current major guidance documents have generally been careful to nuance their language to acknowledge the need for contextualizing application of their recommendations. Prudent decision-makers at the country level will take such recommendations into consideration but, at the end of the day, exercise their own judgment—based on an understanding of their own programmes and key contextual factors—to determine programme approaches appropriate to their setting. Papers 2 and 3 in this series [ 19 , 20 ] address these issues further. There is a great diversity of contextual factors potentially relevant for CHW programmes. In some settings, NGOs and the private sector are engaged in direct PHC service delivery. Civil society entities, such as Red Cross/Red Crescent, may play an important role. Circumstances can differ enormously between informal urban settlements, rural areas, geographically remote populations, and pastoralist groups—each calling for different approaches to PHC, and different roles and strategies in the use of CHWs.
Countries differ markedly with regard to the degree to which management of PHC services is centralized or decentralized. Some PHC services have a hierarchical management structure reporting up to a national MOH. In other countries, the responsibility for PHC financing and delivery rests primarily with local government, with a minimal role for national or subnational levels of government. Such differences in governance have important implications for how standardized PHC services are likely to be (see Paper 3 in this series [ 20 ]).
So how standardized or tailored should CHW programmes be? And how does that vary by setting? Table 4 provides a framework for considering these questions.
A hierarchical, technocratic, managerialist perspective has the virtue of apparent simplicity and visibility [ 63 , 64 ]. This makes it inherently appealing for global-level agencies, technical assistance groups, donors, and centrally based officials and technical officers in MOHs. There have been calls for standardizing definitions and roles for CHW programmes [ 2 ]. Indeed, it complicates the lives of those trying to write about CHW programmes or trying to count CHWs across multiple jurisdictions when there is such diversity on the ground. Furthermore, for both governments and donor-supported partners, efforts to scale up programmes are much simplified by using a single set of specifications.
Because different CHW programmes have different goals and operate in a wide range of settings, specific choices that work well or are essential in one particular setting are not necessarily helpful in another. Flexibility and adaptability can often result in more responsive PHC services, including those delivered by CHWs, and can enable changes and improvements in programme design when it becomes evident that initial designs are falling short of the goals established. Workers and managers need sufficient decision space to make choices that adequately respond to the situations they are actually dealing with. Furthermore, health programmes are implemented in complex, dynamic circumstances; for programmes to be effective, they need to be well tailored to those circumstances, and adaptive as circumstances change.
5) Horizontal or vertical?
As discussed earlier in this paper, even before the first identifiable CHW programme a century ago, there were competing visions on how to do public health; one segment of the global public health community advocated for more broadly based approaches to health and well-being—including an emphasis on socioeconomic determinants of health and the need for robust primary-level preventive/promotive/curative services available to all—and another segment focused on delivery of effective, high-impact interventions at high coverage, aiming for population-level control of specific (mainly communicable) diseases. This tension was evident in the controversy through the 1980s and 1990s that pitted those calling for “comprehensive PHC” against advocates of “selective PHC” [ 65 , 66 ]. Since then, some leaders in global health have sought to build a case that this tension can be resolved, addressing broader health determinants, building local systems, and ensuring high-coverage delivery of efficacious interventions [ 67 ]. Papers 2 and 3 in this series [ 19 , 20 ] address these issues further.
The same tensions seen between more comprehensive, integrated PHC services and those focused on delivery of single interventions [ 65 , 68 ] are also seen in CHW programmes. There are programmes in which a single CHW is responsible for the full range of services provided at the most peripheral tier of the PHC system (e.g., Ethiopia’s HEWs, providing curative care as part of their work in health posts). In other settings, specific CHWs may have a narrower, more specialized role. In yet other programme contexts, there may be more than one category of CHWs working in the same community, with some division of labour. For example, one cadre (primarily male) may be responsible for immunization outreach and another (primarily female) for family planning and antenatal care. Examples include: the family welfare assistants and health assistants in Bangladesh [ 55 ], the male and female pairs of binômes of Rwanda [ 69 ], and the now phased-out village health workers and maternal child health workers in Nepal. Such gender-based role differentiation is important, in some cultural contexts [ 32 ], in determining the effectiveness of CHWs whose responsibilities include maternal/child health and family planning, for example.
In many countries, CHWs are involved in periodic, intensive, outreach campaigns offered annually or semiannually. Such models include supplementary immunization activities, [ 70 , 71 ], national or subnational [polio] immunization days [ 72 , 73 ], child health days [ 74 , 75 ], and community-directed interventions [ 76 ]. These periodic outreach activities typically deliver one or a very small number of interventions (e.g., polio vaccine, vitamin A, or long-lasting insecticide-treated nets) and seek to achieve high population coverage. Some critics have pointed to the tradeoffs this may entail, distracting those in the peripheral-level PHC system from routine services they would otherwise be delivering [ 77 ]. Can campaigns and routine delivery be complementary strategies, or do campaign-style efforts necessarily undermine and weaken routine services?
One consequence of vertical efforts superimposed on more integrated peripheral-level PHC services has been the creation of different kinds of CHWs working in the same setting. A number of countries have CHW cadres originally created for family planning services or as field vaccinators. More recently, special categories of CHWs have been created as adherence counsellors for HIV and TB programmes. Sometimes these categories of CHWs come under the same management structure, but in other settings they may report through separate management structures all the way up to the central MOH. Particularly where CHWs are managed under separate programmes, funding levels and logistical support may differ between programmes, having negative effects on the less well-resourced programmes and their CHWs, with consequences for CHW motivation and retention.
In global health, there has been a major focus on achievement of high population coverage for specific, mainly clinical, preventive and curative interventions (promotion of exclusive breastfeeding is an exception, being considered a behavioural intervention), associated with categorical funding and vertical delivery systems. Associated with this there have been genuine successes, notably immunization, which can legitimately claim credit for substantially reducing child mortality. However, arguments have been made [ 34 ] that an approach focused on specific interventions has tended to result in relative neglect of routine services (i.e., the broader set of services and functions of PHC) and, at a minimum, has represented a missed opportunity for strengthening systems and delivery of services in PHC. Frenk makes the case that it does not have to be either/or; it is possible to simultaneously build strong systems and service delivery, and ensure high coverage for the most impactful interventions [ 68 ].
CHWs perform a wide variety of roles in peripheral-level PHC, varying by country setting, as discussed elsewhere in this series [ 22 ]. Many CHW responsibilities overlap with those of other health workers, some falling into the category of task-shifting (i.e., functions performed, in other contexts, by physicians, nurses, or other more credentialed health workers). In most LMICs, the general standard of education has been increasing over the past several decades. Consequently, across all occupations, there has been some movement towards higher education standards at entry and longer periods of pre-service training, as discussed elsewhere in this series [ 23 ]. This professionalizing tendency is evident in the health sector and is reflected in changes in CHW programmes. To some extent, this has already resulted in what could be seen as task up -shifting. For example, in settings where lay health workers with only elementary education were, until recently, responsible for immunization, this function is increasingly being assumed by health workers with formal post-secondary nursing or paraprofessional training. It can be expected that in the future, this trend of up-shifting tasks to more highly trained staff will continue as the number of more highly credentialed health workers increase. With such changes, how can the benefits of having someone in an intermediary role between health services and the community be maintained? In what ways may we see a progressive professionalizing of the intermediary role of care navigator or case manager? What continuing role could there or should there be for volunteers and lay workers?
In this paper, we have noted two, closely related tensions in global health work, more generally, that also apply to CHW work, notably (1) government versus donor/INGO ownership or influence on CHW programme work, and (2) the relationship between—on the one hand—relatively well-resourced pilot or demonstration activities implemented by an NGO and—on the other—delivery of services at scale, under routine programme conditions. The dynamics among governments, donors, and other development partners play out differently, depending on the setting and the specific actors involved. What constitutes good development practice has been well articulated in the past, for example in the Paris Declaration on Aid Effectiveness [ 78 ] and the Accra Agenda for Action [ 79 ]. Nevertheless, until the problems that these international statements address are fully resolved, we will continue to see dysfunction in the relationships between key actors that undermines effectiveness and sustainability of PHC services and programmes, including those in which CHWs play an important role. These issues are further examined in the paper on financing of CHW programmes in this series [ 21 ].
One of the challenges with pilot and demonstration projects is that, in many instances, they are developed and implemented by external partners with resources not likely to be available on a continuing basis, thereby undermining the likelihood of these efforts being sustained. Such cases are complicated by the dynamic we have noted between governments, donors, and other development partners. But, even when a pilot or demonstration project is entirely “home-grown”, there is frequently a failure to appreciate that the results achievable at small scale with charismatic leadership, dedicated staff, and adequate resources do not reliably predict results that can be achieved implementing at scale under routine programme conditions in the public sector. Nevertheless, if a donor or national government commits to and actively supports a particular intervention or programme model—in the hope of replicating results from a pilot—there can be considerable momentum driving scale-up forward, regardless of whether or not the initiative is delivering its intended benefit. The bigger a programme becomes, the greater the reputational costs of acknowledging performance problems. Paper 10 in this series [ 27 ] reviews CHW programme performance and its measurement. The history of CHW programmes over the past several decades is littered with examples of programmes that have gone to scale and been sustained over years, despite evidence of poor performance [ 80 ]. All actors in global health need to be on guard against uncritically endorsing continuing, large-scale programmes in the absence of evidence of impact [ 80 ].
As reflected in the Disease Control Priorities initiative, now in its third major iteration [ 81 ], there has long been a strong technocratic element in global health development work, emphasizing delivery of specific interventions for which there is robust evidence of effectiveness in reducing the burden of the principal causes of mortality and morbidity in LMICs. Major donors, including World Bank, the US Agency for International Development, the Bill & Melinda Gates Foundation, and others continue—to a large extent—to align their efforts with such a perspective. Unquestionably, this approach has a history of major successes, including the eradication of smallpox, more recent major reductions in the burden of immunization-preventable diseases, and the large-scale delivery of antiretroviral medications for the treatment of HIV infections in sub-Saharan Africa. But, arguably, there has also been a cost to the prominent place this global health philosophy has occupied. As Packard has argued [ 38 ], this has to varying degrees crowded out efforts to strengthen basic PHC services, to address the socio-behavioural drivers of health outcomes, and involve communities in the strengthening of their own health systems.
Frenk [ 68 ] makes the case that the two areas of concern can be reconciled, putting serious efforts into building a strong peripheral-level PHC platform, which can in turn serve as the vehicle for delivery of a broad range of health interventions that address priority health problems, including those that may not be prioritized by donors. For example, with a more robust peripheral-level PHC system, CHWs could play an important role such as identifying and initiating treatment of hypertension and other important and increasingly common noncommunicable diseases. Perry [ 82 ] has laid out a vision for PHC in the twenty-first century that incorporates selective, vertical interventions along with community engagement on a common platform of peripheral health services, in which CHWs are key actors.
That brings us to the question: what place is there for CHWs in the future of PHC? First, it must be acknowledged that much will change. Almost everywhere, we are seeing rising levels of education and living standards and—with them—rising demands for better and more accessible healthcare services (as reflected in the call for UHC). Almost all societies are seeing increasing urbanization, which will certainly have consequences for the future of PHC, including CHW programmes.
Although PHC efforts in LMICs will certainly need to be directing more attention to noncommunicable diseases, the current COVID-19 pandemic is a reminder that we have not altogether left communicable diseases behind. Indeed, as health-sector leaders in Liberia and Sierra Leone learned as they responded to Ebola, reliable early detection and timely response to outbreaks is a key function that needs to be functional at the most peripheral level. Recent experience with COVID-19 has carried this lesson to a much wider audience, bringing with it a recognition of the critical role CHWs can play in disease surveillance/outbreak detection, and in a variety of other important, community-level roles [ 10 ]. The future will bring important epidemiologic and demographic transitions. Increasingly, PHC services in LMICs will need to address noncommunicable diseases and the health problems of older adults.
Historically, government PHC services have primarily targeted rural populations. In most LMICs, there has been a trend over the past several decades of rapidly increasing urbanization, which is likely to continue. Municipal governments have generally been responsible for a range of public health functions including water, sanitation, solid-waste disposal, and other environmental health issues. However, to date, government PHC services have been limited in urban areas and have largely focused on a comparatively small number of clinical preventive services (e.g., immunization, TB control). Unlike rural areas, where government PHC service may play an important role in curative services, in urban settings such a role commonly falls more to private-sector providers. In this more complex, pluralistic service delivery environment, what role is there for government PHC services in general, and for CHWs more specifically? Brazil offers a model of multidisciplinary, generally physician-led, urban community health centres, in which CHWs have an important role to play as intermediaries between health services and the community [ 54 ].
In this paper, we have discussed the variety and complexity of CHW programmes and the PHC systems of which they are a part. It is likely that the tensions we have described will continue to evolve in the coming decades, shaped by changing implementation contexts and the increasingly wide implementation of digital health interventions [ 83 ]. However, an enduring message is that those planning and managing these programmes need to avoid overly formulaic, standardized approaches that fail to adequately take local into account [ 83 ]. Local-level health systems are complex, human systems comprised of a range of actors, in interaction with one another, each with perspectives, needs, values, and interests. Efforts to strengthen local health services and systems need to engage respectfully with these various actors and—at the same time—to attend seriously to population-level effectiveness (including ongoing performance tracking and adaptation in response to observed performance and evolving circumstances).
For improvements in population health outcomes, we need robust, resilient, adequately funded, high-performing PHC systems. CHW programmes are now, in many countries, an increasingly important element in such systems, and it is likely that their importance—and our knowledge on how best to design, implement, and sustain them—will continue to grow. Paper 11 [ 84 ] summarizes the findings from this series and points the way toward the many changes that will need to be taken to achieve robust, resilient, adequately funded, high-performing CHW programmes.
Availability of data and materials
Any articles and other materials cited by the authors are available from the corresponding author.
Most LMICs are seeing significant urbanization; it can be expected that in the future, we will see an increasing number of large-scale public-sector CHWs functioning in urban settings.
Note that this discussion concerns programme approaches and strategies . The authors acknowledge that use of standardized technical guidelines and tools such as clinical protocols is less affected by context.
Abbreviations
Accredited social health activist
Community health volunteer
Community health worker
Coronavirus disease
Female community health volunteer
Health extension worker
Human immunodeficiency syndrome
International Labour Organization
International nongovernmental organization
Low- and middle-income countries
Ministry of Health
Nongovernmental organization
- Primary healthcare
Tuberculosis
USAID. Acting on the Call: Ending Preventable Child and Maternal Deaths: A Focus on Equity. 2016. https://www.usaid.gov/sites/default/files/Final-AOTC-file-v2.pdf . Accessed 4 Mar 2021.
WHO. Global Strategy on Human Resources for Health: Workforce 2030. 2016. . https://www.who.int/hrh/resources/pub_globstrathrh-2030/en/ . Accessed 4 Mar 2021.
WHO. WHO guideline on health policy and system support to optimize community health worker programmes. 2018. https://apps.who.int/iris/bitstream/handle/10665/275474/9789241550369-eng.pdf?ua=1 . Accessed 4 Mar 2021.
Cometto G, Ford N, Pfaffman-Zambruni J, Akl EA, Lehmann U, McPake B, Ballard M, Kok M, Najafizada M, Olaniran A, et al. Health policy and system support to optimise community health worker programmes: an abridged WHO guideline. Lancet Glob Health. 2018;6:e1397–404.
Article PubMed Google Scholar
World Health Assembly. Community health workers delivering primary health care: opportunities and challenges. 2019. http://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R3-en.pdf . Accessed 4 Mar 2021.
WHO and UNICEF. Community-based health care, including outreach and campaigns, in the context of the COVID-19 pandemic: interim guidance. 2019. https://www.who.int/publications/i/item/community-based-health-care-including-outreach-and-campaigns-in-the-context-of-the-covid-19-pandemic . Accessed 4 Mar 2021.
Lu C, Palazuelos D, Luan Y, Sachs SE, Mitnick CD, Rhatigan J, Perry HB. Development assistance for community health workers in 114 low- and middle-income countries, 2007–2017. Bull World Health Organ. 2020;98:30–9.
Walt G. CHWs: are national programmes in crisis? Health Policy Plan. 1988;31:1–21.
Article Google Scholar
Perry HB, Dhillon RS, Liu A, Chitnis K, Panjabi R, Palazuelos D, Koffi AK, Kandeh JN, Camara M, Camara R, Nyenswah T. Community health worker programmes after the 2013–2016 Ebola outbreak. Bull World Health Organ. 2016;94:551–3.
Article PubMed PubMed Central Google Scholar
Ballard M, Bancroft E, Nesbit J, Johnson A, Holeman I, Foth J, Rogers D, Yang J, Nardella J, Olsen H, et al. Prioritising the role of community health workers in the COVID-19 response. BMJ Glob Health. 2020. https://doi.org/10.1136/bmjgh-2020-002550 .
Schmitz K, Basera TJ, Egbujie B, Mistri P, Naidoo N, Mapanga W, Goudge J, Mbule M, Burtt F, Scheepers E, Igumbor J. Impact of lay health worker programmes on the health outcomes of mother-child pairs of HIV exposed children in Africa: a scoping review. PLoS ONE. 2019;14:e0211439.
Article CAS PubMed PubMed Central Google Scholar
Atkins S, Lewin S, Ringsberg KC, Thorson A. Towards an empowerment approach in tuberculosis treatment in Cape Town, South Africa: a qualitative analysis of programmatic change. Glob Health Action. 2012;5:1–11.
Mishra SR, Neupane D, Preen D, Kallestrup P, Perry HB. Mitigation of non-communicable diseases in developing countries with community health workers. Global Health. 2015;11:43.
Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health. 2014;35:399–421.
Haines A, de Barros EF, Berlin A, Heymann DL, Harris MJ. National UK programme of community health workers for COVID-19 response. Lancet. 2020;395:1173–5.
Perry HB, Criugler L, Hodgins S. Developing and Strengthening Community Health Worker Programs at Scale: A Reference Guide and Case Studies for Program Managers and Policy Makers. 2014. http://www.mchip.net/sites/default/files/mchipfiles/CHW_ReferenceGuide_sm.pdf , Accessed 4 Mar 2021.
Strodel RJ, Perry HB. The National Village Health Guide Scheme in India: lessons four decades later for community health worker programs today and tomorrow. Hum Resour Health. 2019;17:76.
Perry HB (ed.). Health for the People: National Community Health Programs from Afghanistan to Zimbabw. 2020. https://pdf.usaid.gov/pdf_docs/PA00WKKN.pdf . Accessed 4 Mar 2021.
Afzal M, Pariyo G, Perry H: Community Health Worker Programs at the Dawn of a New Era: 2. Planning, Coordination, and Partnerships. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00753-7 .
Lewin S, Lehmann U, Perry H. Community Health Worker Programs at the Dawn of a New Era: 3. Governance. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00749-3 .
Masis L, Gichaga A, Lu C, Perry H. Community Health Worker Programs at the Dawn of a New Era: 4. Financing. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00751-9 .
Glenton C, Javadi D, Perry H. Community Health Worker Programs at the Dawn of a New Era: 5. Roles and Tasks. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00748-4 .
Schleiff M, Aitken I, Alam M, Damtew Z, Perry H. Community Health Worker Programs at the Dawn of a New Era: 6. Recruitment, Training and Continuing Education. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00757-3 .
Carpenter C, Musoke D, Crigler L, Perry H. Community Health Worker Programs at the Dawn of a New Era: 7. Recent Advances in Supervision. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00754-6 .
Colvin C, Hodgins S, Perry H. Community Health Worker Programs at the Dawn of a New Era: 8. Motivation and Remuneration. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00750-w .
LeBan K, Kok M, Perry H. Community Health Worker Programs at the Dawn of a New Era: 9. Relationships with Communities and Health Systems. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00756-4 .
Kok M, Crigler L, Kok M, Ballard M, Musoke D, Hodgins S, Perry H. Community Health Worker Programs at the Dawn of a New Era: 10. Performance and Performance Assessment. BMC Health Res Policy Syst. 2021. https://doi.org/10.1186/s12961-021-00758-2 .
Perry H, LeBan K, Crigler L, Lewin S, Musoke D, Kok M, Scott K, Ballard M, Were M, Chowdhury M, Hodgins S. CHWs at the Dawn of a New Era: 11. Leading the Way to Health for All. Human Resour Health 2020. https://doi.org/10.1186/s12961-021-00755-5 .
Perry H, Crigler L, Lewin S, Glenton C, LeBan K, Hodgins S. A new resource for developing and strengthening large-scale community health worker programs. Hum Resour Health. 2017;15:13.
Schneider H, Lehmann U. From community health workers to community health systems: time to widen the horizon? Health Syst Reform. 2016;2:112–8.
Kok MC, Broerse JEW, Theobald S, Ormel H, Dieleman M, Taegtmeyer M. Performance of community health workers: situating their intermediary position within complex adaptive health systems. Hum Resour Health. 2017;15:59.
Glenton C, Colvin C, Carlsen B, Swartz A, Lewin S, Noyes J, Rashidian A. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD010414 .
Schumann DA, Mosley WH. The household production of health Introduction. Soc Sci Med. 1994;38:201–4.
Article CAS PubMed Google Scholar
WHO. WHO Recommendations: Optimizing Health Worker Roles to Improve Access to Key Maternal and Newborn Health Interventions through Task Shifting. 2012 http://apps.who.int/iris/bitstream/10665/77764/1/9789241504843_eng.pdf . Accessed 4 Mar 2021.
Leon N, Sanders D, Van Damme W, Besada D, Daviaud E, Oliphant NP, Berzal R, Mason J, Doherty T. The role of “hidden” community volunteers in community-based health service delivery platforms: examples from sub-Saharan Africa. Glob Health Action. 2015;8:27214.
Schaaf M, Warthin C, Freedman L, Topp S. The community health worker as service extender, cultural broker and social change agent: a critical interpretive synthesis of roles, intent and accountability. BMJ Glob Health. 2020;5:e002296.
Ban B, Hodgins S, Thapa P, Thapa S, Joshi D, Dhungana A, Kc A, Guenther T, Adhikari S, Scudder E, Ram PK. A national survey of private-sector outpatient care of sick infants and young children in Nepal. BMC Health Serv Res. 2020;20:545.
Packard R. A history of global health: interventions into the lives of other people. Baltimore: Johns Hopkins University Press; 2016.
Book Google Scholar
Morrow M, Nelson A. Community Health Worker Coverage and Capacity Tool (C3). 2019. https://www.mcsprogram.org/resource/community-health-worker-coverage-and-capacity-tool/ . Accessed 4 Mar 2021.
Werner D. The village health worker: lackey or liberator? World Health Forum. 1981;2:46–68.
Google Scholar
Walt G, editor. Community health workers in national programmes: just another pair of hands? . UK: The Open University Press; 1990.
Colvin C, Swartz A. Extension agents or agents of change? Community health workers and the politics of care work in postapartheid South Africa. Ann Anthropol Pract. 2015;39:29–41.
Glenton C, Scheel IB, Pradhan S, Lewin S, Hodgins S, Shrestha V. The female community health volunteer programme in Nepal: decision makers’ perceptions of volunteerism, payment and other incentives. Soc Sci Med. 2010;70:1920–7.
Schurer JM, Fowler K, Rafferty E, Masimbi O, Muhire J, Rozanski O, Amuguni HJ. Equity for health delivery: Opportunity costs and benefits among Community Health Workers in Rwanda. PLoS ONE. 2020;15:e0236255.
Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, van Wyk BE, Odgaard-Jensen J, Johansen M, Aja GN, Zwarenstein M, Scheel IB. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev. 2010. https://doi.org/10.1002/14651858.CD004015 .
Lehmann u, Sanders D. Community health workers: What do we know about them? The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers. 2007. http://www.who.int/hrh/documents/community_health_workers.pdf . Accessed 4 Mar 2021.
ILO. International Standard Classification of Occupations (ISCO-08): structure, group definitions and correspondence tables. 2012. http://www.ilo.org/public/english/bureau/stat/isco/isco08/ . Accessed 4 Mar 2021.
Global Health Workforce Alliance and Frontline Healthworker Coaltion. Joint Commitment to Harmonized Partner Action for Community Health Workers and other Frontline Health Workers https://www.who.int/workforcealliance/knowledge/resources/chw_outcomedocument01052014.pdf?ua=1 . Accessed 4 Mar 2021.
Scott K, Beckham SW, Gross M, Pariyo G, Rao KD, Cometto G, Perry HB. What do we know about community-based health worker programs? A systematic review of existing reviews on community health workers. Hum Resour Health. 2018;16:39.
Olaniran A, Smith H, Unkels R, Bar-Zeev S, van den Broek N. Who is a community health worker? A systematic review of definitions. Glob Health Action. 2017;10:1272223.
Brieger W, Orji B: Nigeria’s paths to primary health care. In: Health for the People: National Community Health Worker Programs from Afghanistan to Zimbabwe. 2020. weblink: https://chwcentral.org/wp-content/uploads/2020/05/Healthfor-the-People-National-ommunity-Health-Worker-Programs-from-Afghanistan-to-Zimbabwe.pdf .
CDI Study Group. Community-directed interventions for priority health problems in Africa: results of a multicountry study. Bull World Health Organ. 2010;88:509–18.
Natinal Health Systems Resource Centre. Which Way Forward? Evaluation of AHSA Programme. New Delhi: Natinal Health Systems Resource Centre and the National Rural Health Mission; 2011.
Giugliani C, Zulliger R. The Community health agent program of Brazil. In: Perry H, editor. Health for the People: National Community Health Programs from Afghanistan to Zimbabwe. Washingon: USAID/Maternal and Child Survival Program; 2020. p. 61–73.
Joardar T, Javadi D, Gergen J, Perry H: The Government Family Welfare Assistants, and Community Health Care Providers in Bangladesh. In: Health for the People: National Community Health Worker Programs from Afghanistan to Zimbabwe. 2020. weblink: https://chwcentral.org/wp-content/uploads/2020/05/Healthfor-the-People-National-ommunity-Health-Worker-Programs-from-Afghanistan-to-Zimbabwe.pdf .
Lipsky M. Street-level Bureacracy: Dilemmas of the Individual in Public Services. New York: Russell Sage; 1980.
Newell KW. Health by the people. Geneva: World Health Organization; 1975. p. 224.
Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmukh MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet. 1999;354:1955–61.
WHO and UNICEF. Joint Statement: Home Visits for the Newborn Child: A Strategy to Improve Survival. 2009. http://whqlibdoc.who.int/hq/2009/WHO_FCH_CAH_09.02_eng.pdf?ua=1 . Accessed 4 Mar 2021.
McPherson R, Hodgins S. Postnatal home visitation: Lessons from country programs operating at scale. J Glob Health. 2018;8:010422.
Hodgins S, McPherson R, Kerber K. Postnatal Care, with a focus on home visitation: a design decision-aid for policymakers and program managers. 2017. https://www.healthynewbornnetwork.org/hnn-content/uploads/PostnatalCarewithaFocusonHomeVisitation.pdf . Accessed 4 Mar 2021.
CHIC, Initiatives, UNICEF, USAID. Updated Program Functionality Matrix for Optimizing Conmmunity Health Programs: Community Health Worker Assessment and Improvement Matix (CHW AIM). 2019. https://www.unicef.org/media/58176/file . Accessed 4 Mar 2021.
Scott J. Seeing like a state. New Haven: Yale University Press; 1998.
Andrew M, Pritchett L, Woolcock M. Building state capabililty. Oxford: Oxford University Press; 2017.
Sepulveda J, Bustreo F, Tapia R, Rivera J, Lozano R, Olaiz G, Partida V, Garcia-Garcia L, Valdespino JL. Improvement of child survival in Mexico: the diagonal approach. Lancet. 2006;368:2017–27.
Cueto M. The origins of primary health care and selective primary health care. Am J Public Health. 2004;94:1864–74.
Knaul FM, Bhadelia A, Atun R, Frenk J. Achieving effective universal health coverage and diagonal approaches to care for chronic illnesses. Health Aff (Millwood). 2015;34:1514–22.
Frenk J. Bridging the divide: global lessons from evidence-based health policy in Mexico. Lancet. 2006;368:954–61.
Napier H, Mugeni C, Crigler L. Rwanda’s community health worker program. In: Perry H, editor. National Community Health Programs: Descriptions from Afghanistan to Zimbabwe. Washington: USAID/Jhpiego/Maternal and Child Survival Program; 2020. p. 320–44.
Santos LM, Paes-Sousa R, Silva Junior JB, Victora CG. National Immunization Day: a strategy to monitor health and nutrition indicators. Bull World Health Organ. 2008;86:474–9.
Closser S, Cox K, Parris TM, Landis RM, Justice J, Gopinath R, Maes K, Banteyerga Amaha H, Mohammed IZ, Dukku AM, et al. The impact of polio eradication on routine immunization and primary health care: a mixed-methods study. J Infect Dis. 2014;210(Suppl 1):S504-513.
Mounier-Jack S, Edengue JM, Lagarde M, Baonga SF, Ongolo-Zogo P. One year of campaigns in Cameroon: effects on routine health services. Health Policy Plan. 2016;31:1225–31.
Verguet S, Jassat W, Bertram MY, Tollman SM, Murray CJ, Jamison DT, Hofman KJ. Impact of supplemental immunisation activity (SIA) campaigns on health systems: findings from South Africa. J Epidemiol Community Health. 2013;67:947–52.
Palmer AC, Diaz T, Noordam AC, Dalmiya N. Evolution of the child health day strategy for the integrated delivery of child health and nutrition services. Food Nutr Bull. 2013;34:412–9.
Doherty T, Chopra M, Tomlinson M, Oliphant N, Nsibande D, Mason J. Moving from vertical to integrated child health programmes: experiences from a multi-country assessment of the Child Health Days approach in Africa. Trop Med Int Health. 2010;15:296–305.
Amazigo U, Okeibunor J, Matovu V, Zoure H, Bump J, Seketeli A. Performance of predictors: evaluating sustainability in community-directed treatment projects of the African programme for onchocerciasis control. Soc Sci Med. 2007;64:2070–82.
Atun RA, Bennett S, Duran A. Policy Brief: When do vertical (stand-alone) programmes have a place in health systems? 2008. https://www.who.int/management/district/services/WhenDoVerticalProgrammesPlaceHealthSystems.pdf . Accessed 4 Mar 2021.
The Paris Declaration on Aid Effectiveness. 2005 https://www.oecd.org/dac/effectiveness/45827300.pdf . Accessed 4 Mar 2021.
The Accra Agenda for Action. 2008. https://www.oecd.org/dac/effectiveness/45827311.pdf . Accessed 4 Mar 2021.
Hodgins S, Quisell K. Scale-Up as if Impact Mattered: Learning and Adaptation as the Essential (often missing) Ingredient. 2016. https://www.healthynewbornnetwork.org/hnn-content/uploads/Empty-Scale-Up-Working-Paper_Dec2016.pdf . Accessed 4 Mar 2021.
Jamison DT, Nugent R, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN. Disease control priorities, Third edition. 9 volumes. 2015–2018. http://dcp-3.org/ . Accessed 4 Mar 2021.
Perry HB. An extension of the Alma-Ata vision for primary health care in light of twenty-first century evidence and realities. Gates Open Res. 2018;2:70.
Taylor CE. What would Jim Grant say now? Lancet. 2010;375:1236–7.
Perry H, Crigler L, Kok M, Ballard M, Musoke D, LeBan K, Lewin S, Scott K, Hodgins S. Community Health Worker Programs at the Dawn of a New Era: 11. Leading the Way to Health for All. BMC Health Res Policy Syst 2021. https://doi.org/10.1186/s12961-021-00755-5 .
Download references
Acknowledgements
We are grateful for the financial support from the Bill & Melinda Gates Foundation and the United States Agency for International Development that made this work possible.
About this supplement
This article has been published as part of Health Research Policy and Systems Volume 19, Supplement 3 2021: Community Health Workers at the Dawn of a New Era. The full contents of the supplement are available at https://health-policysystems.biomedcentral.com/articles/supplements/volume-19-supplement-3 .
HP’s contribution as well as publication expenses were supported in part by the Bill & Melinda Gates Foundation (Investment ID OPP 1197181) and by the Maternal and Child Health Integrated Program (MCHIP) of Jhpiego, funded by the United States Agency for International Development. The funders had no role in the conduct of our work.
Author information
Authors and affiliations.
School of Public Health, University of Alberta, Edmonton, Alberta, Canada
Stephen Hodgins
Department of Global Health, KIT Royal Tropical Institute, Amsterdam, The Netherlands
Department of Disease Control and Environmental Health, School of Public Health, Makerere University College of Health Sciences, Kampala, Uganda
David Musoke
Norwegian Institute of Public Health, Oslo Town, Norway
Simon Lewin
Health Systems Research Unit, South African Medical Research Council, Cape Town, South Africa
Crigler Consulting, LLC, Hillsborough, NC, United States of America
Lauren Crigler
Independent Consultant, Washington, DC, United States of America
Karen LeBan
Health Systems Program, Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States of America
Henry B. Perry
You can also search for this author in PubMed Google Scholar
Contributions
SH conceived of this article and wrote the first draft. HP contributed portions of the first draft. MK, DM, SL, LC, and KL each reviewed and contributed to subsequent drafts. All authors read and approved the final version,
Corresponding author
Correspondence to Henry B. Perry .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
No consent to publish is required.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hodgins, S., Kok, M., Musoke, D. et al. Community health workers at the dawn of a new era: 1. Introduction: tensions confronting large-scale CHW programmes. Health Res Policy Sys 19 (Suppl 3), 109 (2021). https://doi.org/10.1186/s12961-021-00752-8
Download citation
Received : 16 June 2021
Accepted : 17 June 2021
Published : 12 October 2021
DOI : https://doi.org/10.1186/s12961-021-00752-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Community health workers
- Community health worker programmes
- Community health
- Health systems
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Introduction
- Conclusions
- Article Information
CHW indicates community health worker.
Adjusted for age, race/ethnicity, sex, number of hospitalizations, insurance, and living alone; discharge disposition was also applied for panel A only. ED indicates emergency department; error bars, 95% CI.
Trial Protocol
eAppendix. Summary of IRB Protocol Changes
eTable 1. Adjusted and Unadjusted Analysis for Clinical Outcomes of All Intervention and Control Participants
eTable 2. Discharge Disposition Subgroup Analysis With Clinical Outcomes for Intervention and Control Participants Discharged to Rehabilitation vs Home
eTable 3. Adjusted and Unadjusted Analysis for Clinical Outcomes of 127 Participants Discharged to Short-Stay Rehabilitation Prior to Home
eTable 4. Adjusted and Unadjusted Analysis for Clinical Outcomes of 423 Participants Discharged Home
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Carter J , Hassan S , Walton A , Yu L , Donelan K , Thorndike AN. Effect of Community Health Workers on 30-Day Hospital Readmissions in an Accountable Care Organization Population : A Randomized Clinical Trial . JAMA Netw Open. 2021;4(5):e2110936. doi:10.1001/jamanetworkopen.2021.10936
Manage citations:
© 2024
- Permissions
Effect of Community Health Workers on 30-Day Hospital Readmissions in an Accountable Care Organization Population : A Randomized Clinical Trial
- 1 Department of Medicine, Massachusetts General Hospital, Boston
- 2 Division of General Internal Medicine, Massachusetts General Hospital, Boston
- 3 Mongan Institute, Massachusetts General Hospital, Boston
- 4 Brandeis University, Waltham, Massachusetts
- 5 Division of General Internal Medicine, Massachusetts General Hospital, Harvard Medical School, Boston
Question Does community health worker care reduce 30-day hospital readmissions in inpatient adults participating in accountable care organization plans?
Findings In this randomized clinical trial including 550 adults, intervention patients were significantly less likely to experience 30-day hospital readmissions than control participants. In post hoc subgroup analysis, the effect remained significant for participants discharged to short-term rehabilitation but not for those discharged home.
Meaning In this study, community health workercare improved postdischarge outcomes in clinically complex patients insured by accountable care organizations, particularly for those discharged to short-term rehabilitation.
Importance Value-based care within accountable care organizations (ACOs) has magnified the importance of reducing preventable hospital readmissions. Community health worker (CHW) interventions may address patients’ unmet psychosocial and clinical care needs but have been underused in inpatient and postdischarge care.
Objective To determine if pairing hospitalized patients with ACO insurance with CHWs would reduce 30-day readmission rates.
Design, Setting, and Participants This randomized clinical trial was conducted in 6 general medicine hospital units within 1 academic medical center in Boston, Massachusetts. Participants included adults hospitalized from April 1, 2017, through March 31, 2019, who had ACO insurance and were at risk for 30-day readmission based on a hospital readmission algorithm. The main inclusion criterion was frequency of prior nonelective hospitalizations (≥2 in the past 3 months or ≥3 in the 12 months prior to enrollment). Data were analyzed from February 1, 2018, through March 3, 2021.
Intervention CHWs met with intervention participants prior to discharge and maintained contact for 30 days postdischarge to assist participants with clinical access and social resources via telephone calls, text messages, and field visits. CHWs additionally provided psychosocial support and health coaching, using motivational interviewing, goal-setting, and other behavioral strategies. The control group received usual care, which included routine care from primary care clinics and any outpatient referrals made by hospital case management or social work at the time of discharge.
Main Outcomes and Measures The primary outcome was 30-day hospital readmissions. Secondary outcomes included 30-day missed primary care physician or specialty appointments.
Results A total of 573 participants were enrolled, and 550 participants (mean [SD] age, 70.1 [15.7] years; 266 [48.4%] women) were included in analysis, with 277 participants randomized to the intervention group and 273 participants randomized to the control group. At baseline, participants had a mean (SD) of 3 (0.8) hospitalizations in the prior 12 months. There were 432 participants (78.5%) discharged home and 127 participants (23.1%) discharged to a short rehabilitation stay prior to returning home. Compared with participants in the control group, participants in the intervention group were less likely to be readmitted within 30 days (odds ratio [OR], 0.44; 95% CI, 0.28-0.90) and to miss clinic appointments within 30 days (OR, 0.56; 95% CI, 0.38-0.81). A post hoc subgroup analysis showed that compared with control participants, intervention participants discharged to rehabilitation had a reduction in readmissions (OR, 0.09; 95% CI, 0.03-0.31), but there was no significant reduction for those discharged home (OR, 0.68; 95% CI, 0.41-1.12).
Conclusions and Relevance This randomized clinical trial found that pairing ACO-insured inpatient adults with CHWs reduced readmissions and missed outpatient visits 30 days postdischarge. The effect was significant for those discharged to short-term rehabilitation but not for those discharged home.
Trial Registration ClinicalTrials.gov Identifier: NCT03085264
Hospitalizations account for one-third of US health care costs. 1 , 2 Readmissions in the first 30 days after hospital discharge are common, and approximately 27% of adult 30-day readmissions are estimated to be preventable. 3 Increasing movement toward value-based care within accountable care organizations (ACOs) has magnified the importance of reducing preventable readmissions. 4 Factors associated with hospital readmissions include medical complexity, 5 clinical comorbidities, 6 , 7 and social determinants of health. 8 - 10 Many health care organizations have increasing interest in developing interventions within the ACO framework that address clinical care gaps and unmet social needs. Integration of community health workers (CHWs) is one of few interventions that have generated promising outcomes in terms of reducing hospitalizations and health care costs. 11 - 13
CHWs are trained to have basic knowledge of clinical conditions and to provide health coaching using motivational interviewing and psychosocial support. 14 - 16 CHWs also have expertise in social determinants of health and can assist patients with economic, health care access–associated, social, educational, and environmental resources to help close gaps in patient health care. 17 , 18 Specifically, CHWs can augment patient engagement by strengthening patient connections to primary care and identifying relevant community-, state-, or federal-based patient resources to meet unmet patient needs (eg, food, housing, transportation). 19 , 20
While most CHW studies have focused on specific disease-based cohorts, 21 - 26 some randomized clinical trials have examined the effectiveness of using CHWs to improve postdischarge outcomes in adult inpatient and outpatient general medicine populations. In a study of 222 Medicaid inpatients randomized to a CHW intervention, Kangovi et al 27 found that having at least one 30-day readmission did not differ between the intervention and control groups; however, there was a significant reduction in the number of intervention participants with 2 or more 30-day readmissions. In a randomized clinical trial of 1009 inpatients older than 60 years, Balaban et al 28 found that CHW care reduced 30-day readmission rates in intervention participants compared with control participants. Another randomized clinical trial by Kangovi et al 29 of 592 primary care outpatients tested a 6-month CHW intervention and demonstrated a reduced likelihood of readmission. Two other randomized clinical trials examining 6-month interventions with CHWs demonstrated no significant difference in hospitalizations. 30 , 31
To determine the effect of CHW care delivery on 30-day readmissions within an ACO population, we conducted a randomized clinical trial to test a 30-day CHW intervention for patients admitted to the internal medicine service in an academic medical center in Boston, Massachusetts. The hypothesis was that CHW care delivery initiated in the hospital and extending for 30 days after discharge would reduce 30-day readmissions compared with usual care.
This randomized clinical trial was approved by the of Partners Human Research Committee (Trial Protocol in Supplement 1 ; eAppendix in Supplement 2 ). All enrolled patients provided written informed consent for study enrollment. This study is reported following the Consolidated Standards of Reporting Trials ( CONSORT ) reporting guideline for randomized clinical trials.
The Community Care Transitions study was a randomized clinical trial was designed to improve health care outcomes for patients at high risk for readmission by pairing CHWs with inpatients for 30 days after discharge. 32 CHW care delivery was implemented in partnership with clinical teams that were unaware of outcomes until trial completion. The CHWs addressed and integrated patient-identified needs (eg, food, housing, transportation) into the clinical care plans and used motivational interviewing and psychosocial support strategies to improve adherence to clinical care.
The study was conducted at Massachusetts General Hospital, a 999-bed teaching hospital in Boston, Massachusetts. Six internal medicine hospital units (or clinical wards) were used for trial recruitment. Each unit had similar percentages of 30-day readmissions with no differences in the diagnoses or ages of hospitalized patients.
Eligibility criteria were developed based on findings from 2 prior studies by Carter et al. 33 , 34 Briefly, patients aged 18 years or older who were admitted to 1 of the study units were potentially eligible if they met the high-risk hospital criteria for 30-day readmission, with threshold of 16% or greater readmission risk. This was determined by a Massachusetts General Hospital–based 12-factor risk algorithm that included prior hospitalizations, fall risk, wound care needs, and frailty. After being identified by this algorithm, patients were evaluated by research staff for additional study inclusion criteria: prior history of 2 or more nonelective hospitalizations in the 3 months prior to enrollment or 3 or more nonelective hospitalizations in the 12 months prior to enrollment; participation in a hospital-based ACO benefit (Medicare, Medicaid, or private insurance); living within a 20-mile radius of the main hospital; having access to a working telephone; being fluent in English; having 1 or more unmet care-related needs identified during inpatient multidisciplinary rounds (eg, difficulties with medication management, appointment scheduling, access to transportation, or social support); and having a primary care physician (PCP). Patients were ineligible if they were experiencing homelessness, unable to provide consent owing to cognitive impairment, or had an invoked health care proxy or prisoner status ( Figure 1 ). Patients with preexisting outpatient program support (ie, integrated care management services with telephonic nursing, social work, and clinical resource care coordination), home nursing, or other supportive programming (eg, physical therapy) were eligible for participation in the trial. Patients living in nursing homes or discharged to long-term care were excluded prior to randomization.
Patients were identified with a hospital-based database that generated a daily report of inpatients at high risk for readmission. Eligible patients were discussed at multidisciplinary rounds daily on each inpatient unit with CHW staff, case managers, unit nurses, bedside nurses, and physicians who reviewed the potential barriers to discharge. After confirming eligibility, research staff approached patients for enrollment. After providing consent and agreeing to enrollment, patients were randomized by study staff via block randomization using the team statistician’s preloaded Excel spreadsheet version 16.0 (Microsoft) block with 6 participants per block to either the intervention or the control group. To allow enough time for enrollment procedures, most participants had to be enrolled prior to finalization of their discharge plans; therefore, it was not feasible to preidentify which participants would be discharged to home or to a short-term rehabilitation facility.
CHWs met with intervention participants and inpatient multidisciplinary teams prior to discharge to establish goals identified by patients and clinical teams. After discharge, CHWs delivered care using multiple communication strategies, including telephone calls, text messages, home visits, rehabilitation facility visits, and field visits (eg, accompanying patient for medical or social service encounters). CHWs provided health coaching, as well as assistance with obtaining any needed clinical access or social resources. CHWs were trained in CHW core competencies, 19 consisting of motivational interviewing, goal-setting, behavior change, and psychosocial support.
Three CHWs delivered the study intervention, and all had experience working with or living in communities similar to those of participants. All CHWs received 1 month of protocol training led by the study CHW supervisor. CHW core competencies were emphasized during training and applied to case-based scenarios. CHWs documented all encounters in the electronic medical record (EMR) (eg, enrollment notes, progress notes for in-person visits and telephone calls); all patient and care team interactions were documented by CHWs in a REDCap database (Vanderbilt University). Each patient’s clinical team members were copied on all CHW EMR notes and contacted directly by CHWs during the intervention when needed. CHW staff also communicated directly with any practitioners of each patient’s outpatient primary care based–support, such as care management, nursing, or physical therapy, to streamline care delivery.
Usual care was defined as routine postdischarge care from the hospital discharge team. Any outpatient referrals made by hospital case management (eg, visiting nursing association, physical therapy, occupational therapy) or social work (eg, meal preparation, transportation, elder care services) at the time of discharge were also considered part of usual care.
Study participants completed an enrollment questionnaire adapted from a previous survey instrument. 26 This survey instrument was derived from some standard established measures of patient experience for benchmarking as well as validated questions generated by prestudy qualitative interviews with patients and physicians. Questionnaire domains included health-related social needs (eg, food, housing, transportation), perceptions of their physical and mental health, confidence in their ability to care for themselves after discharge, satisfaction with inpatient care, perceived likelihood of readmission, understanding of the care plan, and ability to independently perform activities of daily living. Basic demographic characteristics, insurance status, primary diagnosis associated with admission, and major medical and psychiatric comorbidities were collected by EMR review. All participants were asked to complete a 30-day postdischarge questionnaire that included questions to assess perceived likelihood of 30-day readmission and confidence in caring for oneself outside the hospital.
The primary outcome was 30-day hospital readmission during the study period. Prespecified secondary outcomes were 30-day postdischarge missed outpatient physician appointments and emergency department (ED) visits. Outcomes were determined by the number of participants with 1 or more hospital admissions, ED visits (including ED observation stays but excluding ED visits resulting in hospitalization), or missed appointments during the 30 days after discharge from the index hospitalization. Automated email notifications of Partners Healthcare admissions and ED visits were generated by a hospital readmissions database and sent to study staff within 1 hour of occurrence. Hospital admissions were captured at Partners Healthcare–affiliated hospitals in Massachusetts (3 academic hospitals; 6 community hospitals) and New Hampshire (1 community hospital). Missed appointments were captured similarly by a hospital database and tabulated quarterly. Since the EMR was unable to capture encounters outside Partners Healthcare, participants were asked about clinical encounters during a 30-day postdischarge questionnaire. Owing to the nature of the intervention, patients and CHW staff were unable to be blinded to the study treatment arms. Study staff collecting EMR and patient-reported outcomes and performing data analysis were blinded. Clinical outcomes were adjudicated independently of the trial.
For the power calculation, we assumed a readmission rate of 18% for usual care and a readmission rate of 13% with use of CHW care delivery, requiring a sample size of 1200 adults (600 intervention and 600 control) with more than 90% power to reject the null hypothesis that the readmission rate was greater than 13% using 1-sided binomial testing with 5% type I error. However, we were unable to enroll 1200 patients within the study funding timeline; therefore, recruitment was stopped prior to achieving the planned sample size.
Demographic characteristics and baseline survey item responses were summarized between intervention and control groups. Bivariate analyses, using Pearson χ 2 tests for categorical variables and t test for continuous variables, were performed to assess differences between binary clinical outcomes (30-day hospital readmission, missed appointments, ED visits) and study arms, as well as demographic characteristics and survey item responses. For every clinical outcome, a logistic regression model was applied to obtain unadjusted and adjusted odds ratios (ORs) to assess the intervention effect. Covariates adjusted for in the model included age, race/ethnicity, sex, number of hospitalizations, insurance, living alone status, and discharge disposition. Race/ethnicity was self-reported and collected as a potential confounder of readmissions, missed appointments, and ED visits. For 30-day patient experience outcomes, patient responses at admission and 30 days after discharge were compared, and a difference-in-differences analysis was performed. P values were 2-sided, and P < .05 was considered statistically significant. A separate univariate analysis was performed to identify types of CHW-patient contact along with categories of resources or care delivery administered. All analyses were performed using SAS statistical software version 9.4 (SAS Institute). Data were analyzed from February 1, 2018, through March 3, 2021.
Patients were enrolled April 1, 2017, through March 31, 2019. A total of 1843 patients at high risk for readmission were screened, 1230 patients were deemed eligible, and 573 patients were randomized to the intervention (288 patients) or control (285 patients) groups ( Figure 1 ). Six participants (1.0%), including 4 from the intervention group and 2 from the control group, withdrew from the study, and 17 participants (3.1%), including 7 from the intervention group and 10 from the control group, died prior to completing the study and were excluded. The remaining 550 participants were included in the final analyses, with 277 participants in the intervention group and 273 participants in the control group.
The mean age (SD) of participants was 70.1 (15.7) years, and 266 (48.4%) were women ( Table 1 ). The most common insurance was Medicare (388 participants [70.5%]). All trial participants had a mean (SD) of 3 (0.8) hospitalizations in the 12 months prior to index hospitalization ( Table 1 ). Overall, 67 participants (24.5%) in the control group and 60 participants (21.7%) in the intervention group were discharged to rehabilitation. The mean (SD) length of participant rehabilitation stay was 3.9 (1.1) days. Identified covariates were balanced in intervention and control groups.
Overall, compared with the control group, fewer participants in the intervention group were readmitted in the 30 days after hospital discharge (67 participants [24.5%] vs 35 participants [12.6%]; OR, 0.44; 95% CI, 0.28-0.90; P < .001) ( Figure 2 A). In a post hoc subgroup analysis of this cohort (eTable 2 in Supplement 2 ), we found that intervention participants discharged to rehabilitation demonstrated a reduction of 32.3 percentage points in readmissions compared with control participants (3 participants [5.0%] vs 25 participants [37.3%]; OR, 0.09; 95% CI, 0.03-0.31; P < .001) ( Figure 2 B), but the difference observed in intervention vs control participants discharged home was not statistically significant (32 participants [14.7%] vs 42 participants [20.4%]; OR, 0.68; 95% CI, 0.41-1.12; P = .13) ( Figure 2 C). A total of 4 readmissions occurred outside the hospital system and were identified by the patient questionnaire.
Fewer intervention than control participants had missed appointments (61 participants [22.0%] vs 92 participants [33.7%]; OR, 0.56; 95% CI, 0.38-0.81; P = .002), but the difference in ED visits was not statistically significant (31 participants [11.2%] vs 46 participants [16.8%]; OR, 0.62; 95% CI, 0.38-1.02; P = .06) ( Figure 2 A). Similar effects were observed in the subgroup analysis among intervention vs control participants discharged to rehabilitation (missed appointments: 13 participants [21.7%] vs 24 participants [35.8%]; OR, 0.5; 95% CI, 0.22-1.09; P = .08; ED visits: 5 participants [8.3%] vs 14 participants [20.9%]; OR = 0.34; 95% CI, 0.12-1.02; P = .05) ( Figure 2 B) or to home (missed appointments: 48 participants [22.1%] vs 68 participants [33.0%]; OR, = 0.58; 95% CI, 0.37-0.89; P = .01; ED visits: 26 participants [12.0%] vs 32 participants [15.5%]; OR, 0.74; 95% CI, 0.42-1.29; P = .30) ( Figure 2 C). In multivariate analyses of all participants controlling for demographic and clinical covariates (ie, age, race/ethnicity, sex, number of hospitalizations, insurance, living alone status, and discharge to home vs rehabilitation), the adjusted ORs for clinical outcomes in intervention vs control participants were similar to the unadjusted ORs (30-day hospital readmissions: adjusted OR, 0.45; 95% CI, 0.29-0.72; missed appointments: adjusted OR, 0.56; 95% CI, 0.38-0.82; ED visits: adjusted OR, 0.62; 95% CI, 0.38-1.02) (eTable 1 in the Supplement ). A similar analysis was performed for participants discharged home and to short-stay rehabilitation (eTable 3 and eTable 4 in the Supplement ).
More than 80% of all participants indicated they were very or somewhat confident in caring for themselves at the time of enrollment, including 234 participants (84.5%) in the intervention group and 240 participants (87.9%) in the control group, and this did not change in their poststudy questionnaire ( Table 2 ). Intervention participants demonstrated a decrease in their perceived likelihood of 30-day readmission in the poststudy questionnaire compared with the enrollment questionnaire (24 participants [12.5%] vs 53 participants [19.1%]; P = .04); this difference was not statistically different from the control group.
Intervention participants had a mean (SD) of 3.2 (2.4) contacts with CHWs after hospital discharge during the 30-day study period. Of 277 intervention participants, 247 (88.9%) communicated with CHW staff during at least 1 phone call. In addition, 198 participants (71.4%) in the intervention group received at least 1 home, rehabilitation, or field visit during the study interval ( Table 3 ). CHWs completed different types of interactions focused on medical, social, or basic needs and coaching or education. CHWs most commonly provided participants with counseling to reinforce adherence to their clinical care plans (239 participants [86.3%]) and with psychosocial support (229 participants [82.7%]). Other CHW-patient activities ranged widely across supportive clinical and social domains ( Table 3 ), including making and confirming clinical appointments (128 participants [46.2%]), assistance with securing basic needs like food or housing (108 participants [39.1%]), helping with access to medications (97 participants [35.0%]), creating plans for reliable transportation (91 participants [32.9%]), initiating elder care services (80 participants [28.9%]), engaging case management support (76 participants [27.4%]), and assisting with completing insurance forms or obtaining benefits (75 participants [27.0%]).
In this randomized clinical trial at 1 academic medical center, a CHW intervention reduced 30-day hospital readmissions in adult general medicine inpatients by nearly 50%. However, subgroup analyses revealed that most of the effect occurred for participants initially discharged to short-term rehabilitation. Intervention participants also were less likely to miss clinic appointments, but no significant reductions in ED visits were noted. These results indicate that CHW interventions may help reduce hospital readmissions and improve preventive care among some clinically complex patients within an ACO.
A subgroup analysis of participants who were discharged directly home compared with those discharged to short-term rehabilitation before going home demonstrated that the CHW intervention effect on 30-day readmissions was large for participants who went to rehabilitation. Prior studies have shown that deconditioned patients with complex comorbidities who are discharged to rehabilitation facilities have elevated rates of readmission, ranging from 28% to 75%. 35 , 36 The findings of our study suggest that CHWs had a significant effect on preventing readmissions during or after short rehabilitation stays. Potential reasons for this effect may be that CHWs addressed unmet medical and social needs that occurred during the transition from rehabilitation to home and that CHWs improved communication among the patient, rehabilitation staff, and primary physician prior to return to home. While inpatients discharged to rehabilitation prior to transitioning home have been identified as high-risk for 30-day readmission, little research has been done to determine effective interventions to reduce readmissions. Results from our post hoc analyses demonstrated that CHWs are a promising intervention for this population, but future studies are needed to confirm these findings.
Most CHW-focused trials have not demonstrated significant reductions in hospital readmissions. However, a 2020 pooled analysis of 3 CHW randomized clinical trials 37 found a combined significance in reduced hospital readmissions. The Community Care Transitions intervention used in this study differed from prior studies in that all participants were affiliated with a hospital ACO insurance benefit and had a PCP, a working phone number, and a residential address within a specific radius. Preexisting participant connections to primary care and the ACO network were essential for effective communication between CHWs and clinical teams and for assisting participants with access to postdischarge care. This was key to CHWs connecting participants with resources and programs when they needed them. As in most prior published trials, CHWs in our study received unique training focused on reaching patients after discharge and identifying resources for patient health-related social needs. Each of these elements likely contributed to improved clinical outcomes.
The results of this randomized clinical trial also emphasized that even in an ACO where there are more resources than in prior published CHW-intervention focused trials, readmission rates for control participants were relatively high. Although an equal proportion of intervention and control participants were enrolled in comprehensive case management or nursing programs as a part of usual care in an ACO, adding CHW care significantly reduced readmission rates. This difference highlights CHW capacity to address gaps in care related to unmet psychosocial needs (eg, securing meal delivery, transportation, access to medications, elder care services, accompaniment to clinic visits). CHWs can add value to the ACO model in a large health care organization by better connecting patients to community resources and programs as well as primary and subspecialty clinical homes.
Overall, there was a reduction of more than 30 percentage points in missed appointments among intervention participants 30 days after discharge compared with control participants. This effect was sustained in the subgroup analysis for participants discharged to rehabilitation and home. This difference has been demonstrated in prior care transitions studies 38 , 39 and underlines the efficacy of CHWs in improving postdischarge follow-up. Baseline and postintervention period surveys demonstrated a reduction in perceived likelihood of hospital readmission for intervention participants, although this reduction was not statistically significantly different from the control group. This suggests that CHWs may promote increased competence, knowledge, and engagement influencing perceptions about readmission. 40 , 41
The most frequent CHW activities were psychosocial support and reinforcement of adherence to care plans. These activities were similar to those described in studies by Kangovi et al 21 and Wells et al, 23 but most studies to date have not established a standard of care for CHW interventions, making direct comparisons between studies challenging. This represents an area of opportunity to more completely categorize and describe CHW outreach as part of an evidence base. 42 - 45
This study has limitations. Despite use of validated self-reported measures of health care utilization in our 30-day postdischarge survey, we may not have identified all encounters occurring outside our hospital system. However, the fact that all participants were within the ACO network helped ensure that enrolled participants received most, if not all, of their care within designated ACO coverage. Also, healthy user bias, with patients who were the most ill being unable to enroll, may have resulted in underrepresentation of patients with even higher rates of medical complexity. While we considered individuals discharged to rehabilitation to be a legitimate group to study, study participants were enrolled and randomized while hospitalized, and it was not possible to determine who was going to rehabilitation vs home until the time of discharge. Therefore, we were unable to stratify on this characteristic at the time of randomization. Approximately 32% of 1280 patients identified as eligible for the study were unable to be enrolled owing to being busy with clinical care or discharged prior to meeting with study staff. In the future, this could be addressed by having CHWs contact patients via phone after discharge. We were unable to enroll non–English-speaking participants because of limited funding for bilingual study materials and staff. The study was conducted at a single urban hospital and enrolled ACO-insured inpatients with a working telephone and who lived within a 20-mile hospital radius. Therefore, study findings may not be generalizable to patients who have non-ACO health insurance, are uninsured, do not speak English, do not have a working telephone, or live in rural settings.
This randomized clinical trial found that integration of CHWs into clinical care improved preventive care and reduced 30-day readmissions for patients discharged to rehabilitation. Reducing preventable readmissions is a central priority for the Centers for Medicare & Medicaid Services and principal health care stakeholders. As US health care organizations continue to adopt ACO models with the goal of achieving higher quality care at lower costs, policies supporting insurance-based reimbursement for CHW care and investment in comprehensive training and integration of CHWs as valued members of patient care teams will continue to be critical. 46 Future research is needed to identify which patients benefit most from certain CHW intervention activities.
Accepted for Publication: March 30, 2021.
Published: May 20, 2021. doi:10.1001/jamanetworkopen.2021.10936
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2021 Carter J et al. JAMA Network Open .
Corresponding Author: Jocelyn Carter, MD, MPH, Department of Medicine, Massachusetts General Hospital, 55 Fruit St, Blake 15, Boston, MA 02114 ( [email protected] ).
Author Contributions: Dr Carter had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Carter, Walton, Donelan.
Acquisition, analysis, or interpretation of data: Carter, Hassan, Yu, Donelan, Thorndike.
Drafting of the manuscript: Carter, Yu, Thorndike.
Critical revision of the manuscript for important intellectual content: Carter, Hassan, Walton, Donelan, Thorndike.
Statistical analysis: Carter, Yu, Donelan, Thorndike.
Obtained funding: Carter.
Administrative, technical, or material support: Carter, Donelan.
Supervision: Carter, Donelan, Thorndike.
Conflict of Interest Disclosures: Dr Donelan reported receiving grants from the Patient-Centered Outcomes Research Institute, Gordon and Betty Moore Foundation, American Cancer Society, National Institutes of Health, and Physicians Foundation and serving as an unpaid reviewer for the National Academies of Sciences, Engineering, and Medicine outside the submitted work. No other disclosures were reported.
Funding/Support: This study was supported by grants from the Partners Healthcare Center for Population Health (Dr Carter) and the Healthcare Transformation Lab at Mass General (Dr Carter).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 3 .
Additional Contributions: The Boston Public Health Association and the Massachusetts Association of Community Health Workers provided strategic project planning support. Both were compensated for their contributions.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Community Health Worker Integration with and Effectiveness in Health Care and Public Health in the United States
Affiliations.
- 1 Division of General Internal Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, USA; email: [email protected].
- 2 Penn Center for Community Health Workers, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
- 3 Department of General Pediatrics, Children's Hospital of Philadelphia, Philadelphia, Pennsylvania, USA.
- PMID: 37010928
- DOI: 10.1146/annurev-publhealth-071521-031648
Community health workers (CHWs) have worked in a variety of settings in the United States for more than 70 years and are increasingly recognized as an essential health workforce. CHWs share life experience with the people they serve and have firsthand knowledge of the causes and impacts of health inequity. They provide a critical link between marginalized communities and health care and public health services. Several studies have demonstrated that CHWs can improve the management of chronic conditions, increase access to preventive care, improve patients' experience of care, and reduce health care costs. CHWs can also advance health equity by addressing social needs and advocating for systems and policy change. This review provides a history of CHW integration with health care in the United States; describes evidence of the impact of CHW programs on population health, experience, costs of care, and health equity; and identifies considerations for CHW program expansion.
Keywords: clinical integration; community health workers; health equity; social determinants of health.

Publication types
- Community Health Workers
- Delivery of Health Care
- Health Equity*
- Public Health*
- United States
CHW Advocates

THE DUAL HUMAN RIGHTS ISSUE
Millions of community health workers are not salaried, skilled, supervised, and supplied.
70% of chws are women. half in low- and middle-income countries are unsalaried. the ultimate injustice one billion people will never see a health worker..
THE SOUND SOLUTION
Community Health Impact Coalition is making professional community health workers (proCHWs) the norm worldwide. We create international guidelines. We increase global funding. And we win national policy.
Indisputable evidence confirms that CHWs improve health outcomes—with considerable equity and economic dividends. Governments can generate a 10:1 return on investment with community health workers. And proCHWs could save two million lives annually.

CHIC is a fiscally sponsored nonprofit founded in 2019. The Coalition includes thousands of CHWs and dozens of global health organizations in 60+ countries across five WHO regions. Collective strength, collective impact.
A powerful, symbiotic machine for policy change.
See our tactics
We equip international norm setters with evidence to create proCHW guidelines.
We influence global financing institutions to increase proCHW funding.
We mobilize in-country networks to win national proCHW policy.

OUR UNAPOLOGETIC VISION
Quality care for all, including those who provide it.
“The progress of professional community health workers is a beautiful story of a scalable solution. CHIC is emergent, brought into being by the doers themselves. It is wisely organized around explicit best practices for an effective proCHW model.”
—Kevin Starr, Mulago Foundation
proCHW best practices enshrined in inaugural WHO CHW guidelines
$100,000,000
largest-ever fund for national proCHW programs with Africa Frontline First
CHW Advocates on the first ever CHW Speaker Bureau
CHWs from 20 countries completed the CHW Advocates course (so far)
countries with a confirmed proCHW policy
PROCHW RESOURCES
New opportunity in an old idea.

The problem: a dual human rights issue.
Despite decades of global health investment, 1 billion people cannot access essential health services.

A blueprint for community health worker success – The Community Health Worker Assessment and Improvement Matrix.

Despite their vital work CHWs have long been subject to global debate about remuneration. But the discussion should move on to how to pay CHWs, not whether they should be paid.
RADICAL COLLABORATORS
Large-scale social change is a team sport.
Featured chws.

Nuru Muhamed Ali

Dramane Konaté

Dickson Nansima Mbewe

Margaret Odera
Funders & partners

Join the movement.
Social change is a team sport. subscribe to our mailing list and join the movement..
Privacy Policy
Web Policies & Notices
- Accessibility
- No FEAR Act Data
- Privacy Policy
- Freedom of Information Act (FOIA)
- HHS Vulnerability Disclosure external link
Related Government Websites
- Health and Human Services external link
- National Institutes of Health
- Office of the Inspector General external link
- USA.gov external link
Stay Connected
Live Chat with us, Monday through Friday, 8:30 a.m. to 5:00 p.m. EST.
Receive automatic alerts about NHLBI related news and highlights from across the Institute.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Preventing Chronic Diseases: What You Can Do Now
- Living with a Chronic Condition
- Chronic Disease Data
- Community Health Workers
- Workgroup on Translation Tools
- National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP)
Public Health Guidance for Community Health Workers
- Community health workers (CHWs) help people manage chronic diseases and get the health services they need by breaking down barriers to care related to social determinants of health.
- These resources can guide CHWs, health systems, and others in serving communities more effectively.

A community health worker (CHW) is a frontline public health worker who lives in or is trusted by the community. A CHW connects people to health and social services by breaking down barriers related to the social determinants of health.
The following audiences are most likely to find these resources useful:
- CHWs, who might be known by other names (e.g., promotores de salud, coaches, lay health advisors, community health representatives, peer mentors, peer navigators).
- Certified educators, who might be CHWs or belong to another allied clinical group.
- Community-based organizations, including faith-based organizations and other community groups that work with or host CHWs.
- Health insurers, purchasers, and payers―including Medicaid, Medicare, commercial insurers, and employers―who have questions about reimbursing for the services that CHWs provide.
- Health care providers, who want to incorporate CHWs into their practices.
- Public health professionals who work with CHWs and other groups listed here.
If you identify a CDC resource not listed here, see an error, or have additional feedback, please email the Community Health Worker Workgroup .
Resources by Topic
CDC's National Asthma Control Program Evaluation Resources
This web page hosts evaluation resources relevant to asthma and other public health programs. The document "Learning As We Grow: Evaluation Highlights from National Asthma Control Program Grantees" is part of the materials on this page.
Type of Resource: Web page
Language: English
Audiences: All
Related CDC programs: National Asthma Control Program
Asthma Control: Home-Based Multi-Trigger, Multicomponent Environmental Interventions—Children and Adolescents with Asthma
The Community Preventive Services Task Force recommends the use of home-based multi-trigger, multicomponent interventions with an environmental focus for children and adolescents with asthma to improve overall quality of life and productivity. These interventions involve home visits by trained personnel who may be CHWs. This finding is based on a systematic review of evidence.
Related CDC programs: The Community Guide , National Asthma Control Program
Improving Cancer Prevention and Control: How State Health Agencies Can Support Patient Navigators and Community Health Workers
This article focused on how state health agencies and ASTHO members can further bolster the sustainability of patient navigator and community health worker programs to support health reform and improve health outcomes for all populations.
Type of Resource: Report
Audiences: Community-based organizations, health insurers, purchasers, and payers, healthcare providers, public health professionals
Related CDC programs: Cancer Prevention and Control
AMIGAS: Ayudando a las Mujeres con Información, Guía, y Amor para su Salud (Helping Women with Information, Guidance, and Love for their Health)
AMIGAS is a bilingual educational outreach intervention designed to help promotoras ( CHWs) and other lay health educators increase cervical cancer screening among Hispanics who have rarely or never had a Pap test.
Type of Resource: Educational materials
Language: English, Spanish
Audiences: Certified educators, community health workers, community-based organizations, NGOs, general public, healthcare providers
Related CDC programs: Gynecologic Cancers , Cancer Prevention and Control
Community Cancer Screening Program: Implementing Interventions to Address Disparities
The Cancer Coalition of South Georgia hired health navigators to help implement interventions recommended by the Community Preventive Services Task Force to reduce cancer-related disparities in a rural, medically underserved region.
Type of Resource: Fact sheet
Related CDC programs: The Community Guide , Cancer Prevention and Control
Black Corals: A Gem of a Cancer Screening Program in South Carolina
In rural South Carolina, where many African American women have limited access to lifesaving medical screenings, the St. James-Santee Family Health Center launched Black Corals to increase cancer screening among women. The Community Guide served as a resource to help the Black Corals program dramatically increase breast and cervical cancer screenings in their community. Activities included promoted events and educational sessions in local churches, hair salons, and restaurants throughout the community.
Increasing Cancer Screening: Group Education for Clients—Breast Cancer
The Community Preventive Services Task Force recommends group education to increase breast cancer screening. Interventions are conducted by health professionals or by trained laypeople. This finding is based on a systematic review of evidence.
Increasing Cancer Screening: One-on-One Education for Clients—Breast Cancer
The Community Preventive Services Task Force recommends the use of one-on-one education to increase screening for breast cancer. Interventions are delivered by healthcare workers or other health professionals, lay health advisors, or volunteers. This finding is based on a systematic review of evidence.
Increasing Cancer Screening: One-on-One Education for Clients—Cervical Cancer
The Community Preventive Services Task Force recommends the use of one-on-one education to increase screening for cervical cancer. Interventions are delivered by healthcare workers or other health professionals, lay health advisors, or volunteers. This finding is based on a systematic review of evidence.
Increasing Cancer Screening: One-on-One Education for Clients—Colorectal Cancer
The Community Preventive Services Task Force recommends the use of one-on-one education to increase screening for colorectal cancer. Interventions are delivered by healthcare workers or other health professionals, lay health advisors, or volunteers. This finding is based on a systematic review of evidence.
Use of Community Health Workers and Patient Navigators to Improve Cancer Outcomes Among Patients Served by Federally Qualified Health Centers: A Systematic Literature Review
Systematic literature review that identified studies of cancer-related CHW/ Patient Navigator (PN) interventions in Federally Qualified Health Centers described the components and characteristics of those interventions. Findings may guide future CHW/PN intervention development and evaluation.
Type of Resource: Journal article
Audiences: CHWs, community-based organizations, NGOs, general public, health insurers, purchasers, and payers, healthcare providers, public health professionals
New York: Increasing Cancer Screenings, Saving Lives
The New York State Department of Health Bureau of Cancer Prevention and Control coordinates multiple programs based on Community Preventive Services Task Force recommendations to increase the screening rates for breast, cervical, and colorectal cancers. Interventions include client reminders, small media, mass media, and programs to reduce structural barriers.
Cancer Screening: Multicomponent Interventions—Breast Cancer
The Community Preventive Services Task Force recommends multicomponent interventions to increase breast cancer screening. Some components may be conducted by health professionals, CHWs, or patient navigators. This finding is based on a systematic review of evidence.
Cancer Screening: Multicomponent Interventions—Cervical Cancer
The Community Preventive Services Task Force recommends multicomponent interventions to increase cervical cancer screening. Some components may be conducted by health professionals, CHWs, or patient navigators. This finding is based on a systematic review of evidence.
Cancer Screening: Multicomponent Interventions—Colorectal Cancer
The Community Preventive Services Task Force recommends multicomponent interventions to increase colorectal cancer screening. Some components may be conducted by health professionals, CHWs, or patient navigators. This finding is based on a systematic review of evidence.
Cardiovascular Disease
Heart Disease and Stroke Prevention: Interventions Engaging Community Health Workers
This web page provides information and supporting materials for the Community Preventive Services Task Force (CPSTF) recommendation about interventions engaging CHWs to prevent cardiovascular disease. It includes the CPSTF finding and rationale statement and a summary of the evidence that serves as the basis for this recommendation.
Related CDC programs: The Community Guide , Heart Disease and Stroke Prevention
Heart Disease and Stroke Prevention: Team-based Care to Improve Blood Pressure Control
This web page provides information and supporting materials for the Community Preventive Services Task Force (CPSTF) recommendation about team-based care to improve blood pressure control. It includes the CPSTF finding and rationale statement and a summary of the evidence that serves as the basis for this recommendation.
Effectiveness of Community Health Workers in the Care of Persons with Diabetes
This CDC staff-authored paper evaluated the effectiveness of CHWs in the care of people with diabetes and concluded that interventions involving CHWs showed some improvements in participant knowledge, behavior, and physiological measures and decreased hospital admissions, particularly in minority populations.
Audiences: Health insurers, purchasers, and payers, healthcare providers, public health professionals
Related CDC programs: Division of Diabetes Translation
Road to Health Toolkit
Road to Health Toolkit resources were developed for CHWs and educators working with African-American or Hispanic/Latino populations at risk for type 2 diabetes. Resources include the toolkit and all its components, a training guide and video, and an evaluation guide. Training and technical assistance resources are also available.
Type of Resource: Training
Audiences: Certified educators, CHWs, community-based organizations, NGOs, healthcare providers, public health professionals
Community-based Organizations (CBOs)
This web page contains a collection of toolkits related to diabetes prevention and control.
Do It for them! But for You, Too. (¡Hazlo por ellos! Pero por ti también)
This diabetes fotonovela describes simple ways to prevent or delay type 2 diabetes, especially if a person has a family history of the condition.
Audiences: Certified educators, CHWs, community-based organizations, NGOs, general public, public health professionals
Stories to Reach, Teach, and Heal
Over the ages and across the cultures and continents, stories have served to reach, teach, and speak for people in times of hardship and illness. CDC's Division of Diabetes Translation developed a guide: Stories to Reach, Teach, and Heal: A Guide for Diabetes Health Educators . The stories illustrate how health educators can use storytelling to share wisdom and inspiration.
Audiences: CHWs, general public, healthcare providers, public health professionals
Related CDC programs: Native Diabetes Wellness Program , Division of Diabetes Translation
Eagle Books for Early Readers
The four-volume Eagle Book series was written by Georgia Perez, a veteran community health representative for the Nambe Pueblo. The books convey to Native children healthy ways of living that are rooted in traditional Native values. Additional resources that coordinate with the books are also available on this web page.
Eagle Books for Youth
Books and materials on this web page are follow-ups to the original Eagle Book stories, a series of books for Native American children, youth and others interested in healthy living. The youth materials continue to promote type 2 diabetes prevention and encourage a respect for traditional ways, including physical activity and healthy eating.
Traditional Foods
American Indian and Alaska Native communities across the country are reclaiming traditional foods as part of the global Indigenous food sovereignty movement, which embraces identity, history, and traditional ways and practices to address health. This web page lists resources that community health representatives can use to educate their communities about traditional foods.
Audiences: Certified educators, CHWs, community-based organizations, NGOs, general public, healthcare providers, public health professionals
Diabetes Prevention: Interventions Engaging Community Health Workers
This web page provides information and supporting materials for the Community Preventive Services Task Force recommendation about interventions engaging CHWs to prevent diabetes. It includes the Task Force finding, rationale statement, and summary of the evidence that serves as the basis for this recommendation.
Related CDC programs: The Community Guide , Division of Diabetes Translation
General Resources
Community Health Workers Can Be a Public Health Force for Change in the United States: Three Actions for a New Paradigm
This CDC staff-authored paper discusses how to strengthen the roles of CHWs, enabling them to become collaborative leaders in a healthcare environment dramatically changing from "sickness care" systems to systems that provide comprehensive care for individuals and families and supports community and tribal wellness.
Related CDC programs: Heart Disease and Stroke Prevention
Community Health Workers: Part of the Solution
This CDC staff-authored paper describes how two states, Massachusetts and Minnesota, initiated comprehensive policies to foster far more use of CHWs and, in the case of Minnesota, to make CHW services reimbursable under Medicaid.
Audiences: Community-based organizations, NGOs, health insurers, purchasers, and payers, healthcare providers, public health professionals
Making the Business Case for Prevention Video Series: Community Health Workers Bridge Health Care Gap
Improved quality of care, increased compliance, and reduced costs—these are just a few of the many benefits of including CHWs as part of a comprehensive health care team. This video shows how CHWs help patients , especially those with language or other barriers , navigate complex health care systems.
Type of Resource: Multimedia
Related CDC programs: Division of Nutrition, Physical Activity, and Obesity
Community-Clinical Linkages for the Prevention and Control of Chronic Diseases: A Practitioner's Guide
This guide is a resource for public health practitioners to define and facilitate community-clinical linkages.
Infectious Disease
Using Community Health Workers to Prevent Infectious Diseases in Women
This is a conference summary from the International Conference on Women and Infectious Disease. It discusses the use of CHWs to deliver infectious disease prevention services in the United States.
Related CDC programs: National Center for Emerging and Zoonotic Infectious Diseases
Vaccination Programs: Home Visits to Increase Vaccination Rates
The Community Preventive Services Task Force recommends home visits to increase vaccination rates in children and adults. Home visits may be conducted by vaccination providers (e.g., nurses) or others (e.g., social workers, CHWs). This finding is based on a systematic review of evidence.
Related CDC programs: The Community Guide , Vaccines & Immunizations
Injury Prevention
Use of Child Safety Seats: Distribution and Education Programs
The Community Preventive Services Task Force recommends interventions that use distribution and education programs to increase child safety seat use. Programs may be implemented in hospitals, clinics, or homes and often use community volunteers. This finding is based on a systematic review of evidence.
Related CDC programs: The Community Guide , Motor Vehicle Safety Program
Early Childhood Home Visitation to Prevent Child Maltreatment
The Community Preventive Services Task Force recommends early childhood home visitation programs to reduce child maltreatment among high-risk families. Programs may be implemented by nurses, social workers, paraprofessionals, or community peers. This finding is based on a systematic review of evidence.
Related CDC programs: The Community Guide , Child Abuse and Neglect, Division of Violence Prevention
Obesity Prevention and Control: Technology-Supported Multicomponent Coaching or Counseling Interventions to Reduce Weight
The Community Preventive Services Task Force recommends multicomponent coaching or counseling interventions that use technology to help clients lose weight. Interventions are delivered by health professionals, including coaches and counselors. This finding is based on a systematic review of evidence.
Related CDC programs: The Community Guide , Overweight and Obesity
Obesity Prevention and Control: Technology-Supported Multicomponent Coaching or Counseling Interventions to Maintain Weight Loss
The Community Preventive Services Task Force recommends multicomponent coaching or counseling interventions that use technology to help clients maintain weight loss. Interventions are delivered by health professionals, including coaches and counselors. This finding is based on a systematic review of evidence.
Physical Activity
Familias Sanas y Activas: Improving Health among Latinos in San Diego
Based on recommendations from the Community Preventive Services Task Force, the San Diego Prevention Research Center is improving the health of Latinos in the city with a free physical activity program that includes training promotores de salud to lead group exercise classes.
Related CDC programs: The Community Guide , Physical Activity
Chronic Disease
Prevalence, costs, risks, prevention, and management of chronic diseases in the United States
For Everyone
Public health.
- Open access
- Published: 14 May 2024
Health systems challenges, mitigation strategies and adaptations to maintain essential health services during the COVID-19 pandemic: learnings from the six geopolitical regions in Nigeria
- Segun Bello 1 ,
- Rachel Neill 2 ,
- Ayodele S Jegede 1 ,
- Eniola A. Bamgboye 1 ,
- Mobolaji M. Salawu 1 ,
- Rotimi Felix Afolabi 1 ,
- Charles Nzelu 3 ,
- Ngozi Azodo 3 ,
- Anthony Adoghe 3 ,
- Munirat Ogunlayi 2 ,
- Saudatu Umma Yaradua 2 ,
- William Wang 4 ,
- Anne Liu 4 &
- Olufunmilayo I. Fawole 1
BMC Health Services Research volume 24 , Article number: 625 ( 2024 ) Cite this article
146 Accesses
1 Altmetric
Metrics details
The COVID-19 pandemic control strategies disrupted the smooth delivery of essential health services (EHS) globally. Limited evidence exists on the health systems lens approach to analyzing the challenges encountered in maintaining EHS during the COVID-19 pandemic. This study aimed to identify the health system challenges encountered and document the mitigation strategies and adaptations made across geopolitical zones (GPZs) in Nigeria.
The national qualitative survey of key actors across the six GPZs in Nigeria involved ten states and the Federal Capital Territory (FCT) which were selected based on resilience, COVID-19 burden and security considerations. A pre-tested key informant guide was used to collect data on service utilization, changes in service utilization, reasons for changes in primary health centres’ (PHCs) service volumes, challenges experienced by health facilities in maintaining EHS, mitigation strategies implemented and adaptations to service delivery. Emerging sub-themes were categorized under the appropriate pillars of the health system.
A total of 22 respondents were interviewed. The challenges experienced in maintaining EHS cut across the pillars of the health systems including: Human resources shortage, shortages in the supply of personal protective equipments, fear of contracting COVID-19 among health workers misconception, ignorance, socio-cultural issues, lockdown/transportation and lack of equipment/waiting area (. The mitigation strategies included improved political will to fund health service projects, leading to improved accessibility, affordability, and supply of consumables. The health workforce was motivated by employing, redeploying, training, and incentivizing. Service delivery was reorganized by rescheduling appointments and prioritizing some EHS such as maternal and childcare. Sustainable systems adaptations included IPC and telehealth infrastructure, training and capacity building, virtual meetings and community groups set up for sensitization and engagement.
The mitigation strategies and adaptations implemented were important contributors to EHS recovery especially in the high resilience LGAs and have implications for future epidemic preparedness plans.
Peer Review reports
The COVID-19 pandemic remains the biggest global health systems shock of the 21st century leading to about 6.8 million deaths as of 26th February, 2023 [ 1 ]. The interventions implemented to control the pandemic have had far-reaching consequences, ranging from disruptions to socio-economic activities, to decline in health services provision and utilization. According to the World Health Organization (WHO), countries henceforth need to make trade-offs between the scale of direct response to health threats and the actions geared towards maintaining essential health service delivery, to mitigate the risk of system collapse [ 2 ].
Disruptions are defined as “unforeseen events that interfere with the provision of healthcare goods and services” [ 3 ]. During the COVID-19 pandemic, disruptions in health service delivery and decline in essential health services utilization was documented across all health systems including high, medium and low-income countries [ 4 ]. These disruptions were attributed to aspects of the COVID-19 pandemic response including lockdowns and reorganization of health service delivery with a shift in focus to COVID-19 control [ 2 ]. For example, in Europe, screening for cancers decreased by as much as 65 − 95% during the early phase of the pandemic [ 5 ]. In Africa, several health programmes including the malaria elimination programme, HIV/tuberculosis control, diabetes, and hypertension services were deprioritized during the pandemic [ 6 , 7 ]. Heavy declines were also reported for maternal, child health and immunization programmes [ 8 , 9 ]. effectively threatening the gains achieved in health programme outcomes over decades of investment [ 10 ]. These health programmes reported decline in service output as well as set- backs in performance indicators as similarly demonstrated during the West Africa Ebola outbreak pandemic. Analysis of the 2014–2015 Ebola outbreak suggested that the number of deaths caused by measles, malaria, HIV/AIDS and tuberculosis attributable to health systems failure during the Ebola outbreak exceeded deaths from Ebola [ 11 , 12 , 13 , 14 ].
The WHO health systems framework describes the core building blocks or pillars of the health systems which contribute to the resilience of a health system [ 15 ]. The performance of the health system in handling health crisis depends on its baseline capacity predating the crisis, as well as the magnitude of the crisis [ 2 ]. Kruk et al. defined health systems resilience as ‘the capacity of health actors, institutions, and populations to prepare for and effectively respond to crises; maintain core functions when a crisis hits; and, informed by lessons learned during the crisis, reorganize if conditions require it.’ [ 16 ] Thus, apart from maintaining the core functions of a health system, resilience includes the health system’s ability to transform, evolve and enhance its performance in improving the health of the population [ 17 ].
A well-prepared health system should have the capacity to maintain essential health services delivery to reduce morbidity and mortality from sources other than the cause of the health systems shock, throughout the duration of an emergency. Both demand and supply factors have been documented as challenges mitigating against the maintenance and utilization of essential services across health systems during the COVID-19 pandemic. The pandemic increased the workload for health systems, resulting in pressure and inadequate health workforce all over the world [ 5 ]. However, LMICs have been particularly affected from operating more vulnerable health systems with challenges that predated the COVID-19 pandemic. To compound the challenges of human resource shortages, about 50% of health facilities across Africa reported COVID-19 infection among staff, shortages in personal protective equipment (PPE), underfunding, reduced supply of medications and poor information systems [ 6 , 18 ]. Most African countries are dependent on importation of essential medicines and products. These countries were affected by the disruptions in the global supply chain because drugs were not readily available or were expensive because of the high demand relative to supply [ 19 ]. Patients expressed difficulties in accessing medicines due to the high cost [ 20 ].
Geographic variability in the level of disruptions and restorations to EHS were reported within countries [ 21 ]. The COVID-19 high burden states/areas were likely to have experienced a higher level of restrictions and enforcements of protocols which could affect the levels of disruptions and the time taken for restorations. Furthermore, recovery may be slow, temporary, or partial depending on sub-national health systems resilience. Reported innovative adaptations to halt or reverse decline in EHS delivery included home delivery, use of phones, improved triaging, shift to remote consultations, and expansion of the scope of work of community health workers and task shifting [ 21 , 22 ]. Limited evidence exists on the health systems lens approach to analyzing the challenges encountered in maintaining EHS delivery during the COVID-19 pandemic, particularly at the sub-national levels. Therefore, this study aimed to identify the health system challenges encountered during the COVID-19 pandemic and document the mitigation strategies and adaptations made across the geopolitical zones (GPZs) in Nigeria. The learnings will guide policymakers, decision makers and health administrators on how to improve health systems in Nigeria to ensure that they are resilient and prepared to respond to public health emergencies. Learnings from Nigeria especially on the mitigation and adaptation strategies may be transferrable to similar decentralized health systems.
Study setting
The study was qualitative in design involving interviews of key persons at state ministries of health (SMoH) and State Primary Health Care Development Agencies (SPHCDA) across the six geopolitical zones of Nigeria. Following the Alma Ata declaration in 1978, the primary health care (PHC) system became the fulcrum of health systems development in Nigeria. Not much progress was made in PHC however, until 1985 when the then Minister of Health adopted 52 Local Government Areas (LGAs) to build models based on the Alma Ata declaration [ 23 ]. Thereafter, the model was expanded to include all LGAs and the responsibility for overseeing the working of the PHC including immunization, antenatal care services was devolved to the LGAs [ 23 ]. PHC in Nigeria focuses on preventive services including immunization, antenatal care services, as well as the provision of basic health care services at the grass root level [ 23 ].
The Primary Health Care Under One Roof policy was introduced in 2010 and approved in 2011 [ 24 ]. It aims to strengthen the national health system by integrating all PHC services under one authority. By implications, all resources for PHC implementation are to be repositioned from all agencies, departments and ministries to the new State PHC development agencies or boards [ 24 ]. This initiative produced some improvements in health outcomes [ 25 ].
Like many other African countries, Nigeria has consistently failed to implement the 2001 Abuja declaration at which African heads of state pledged to allocate 15% of the annual national budget to health [ 26 , 27 ]. Currently, the PHC system has deteriorated with most of the 30,000 PHC facilities across the country lacking the capacity to provide essential healthcare services thereby, transferring enormous pressure to the higher levels of healthcare [ 28 ]. The challenges PHC facilities experienced before COVID-19 included poor staffing, inadequate equipment, poor distribution of health workers, poor quality of healthcare services, poor condition of infrastructure, and lack of essential drug supply.
Study design and approach
The study was part of a large national qualitative survey on resilience of the health system which aimed at identifying the key challenges to maintaining essential health services during the pandemic, from the perspective of subnational actors. This current report focused on the regional level data, but the other aspect of the study focused on comparative LGA-level data on how some LGAs overcame challenges and sustained essential health services, while comparable, neighbouring LGAs experienced ongoing disruptions [ 29 ].
Study site and participants’ selection
The study enrolled subnational actors at the state level, across the six geopolitical zones of Nigeria. These participants were engaged in the COVID-19 response and were at decision-making levels such as directors, assistant directors and heads of programmes.
Selection of study sites was guided by multiple criteria namely High Resilience (HR) LGAs; COVID 19 disease burden and regional hotspots such as LGAs with the highest cumulative cases and those with international airport or land borders; security considerations, by avoiding LGAs with considerable security challenges such as LGAs with insurgents and banditry. The procedure for identifying high resilience LGAs has been described in detail elsewhere [ 29 ]. In brief, the general outpatient (GOPD) and Ante-natal care (ANC) health services data from the National Health Management Information System (NHMIS) (January 2019 – December 2021) was analyzed using the interrupted time series. The analysis identified HR LGAs. HR LGAs were defined as LGAs which experienced a recovery in service volumes within three months of decline precipitated by the COVID-19 pandemic. LGAs were then stratified and ranked within each geopolitical zones and, in combination with COVID-19 burden and security considerations, 12 h LGAs were finally selected from 10 states and the Federal Capital Territory (FCT) across the six geopolitical zones: South-West [ 3 ], South-South [ 2 ], South-East [ 2 ], North-West [ 1 ], North-Central [ 2 ], North-East [ 1 ].
Participants for the parent study were selected purposively across state, LGA, health facilities, and community levels. However, this report is limited to the analysis of response from state-level participants across the GPZs where two participants each were selected per state.
Data collection
A key informant guide was developed following extensive review of literature on health systems resilience and essential health service maintenance (see Supplementary File). The guide was pretested among similar personnel in Nasarawa state before data collection. The interview guide was sectioned according to: profile of the study participants; services used during COVID-19; data monitoring and use; self-regulation; adaptive-short term; integrated capacities or planning; relevance to maternal neonatal and child health (MNCH); and adaptive-long term. The data presented in this report focuses on the following sections of the tool: services used during the COVID-19 pandemic and self-regulation which contained information on participants’ assessment of changes in service utilization during the COVID-19 pandemic; reasons for the changes in Primary Health Centres (PHCs) attendance, challenges experienced by facilities to maintain routine services during the pandemic, specific countermeasures that the state governments took to overcome the challenges and activities done by the state governments to encourage clients to continue to utilize the PHCs.
The Federal Ministry of Health (FMoH) led the project and played an oversight role in data collection with supervisors leading research teams to the states. The interview teams paid advocacy visits to explain the purpose of the research and obtain the support of stakeholders in the ministries of health. The interview team comprised of a supervisor, a moderator and a note taker per state. All data collectors and supervisors were trained for the purpose of this research. All participants gave informed consent before they were interviewed face-to-face and audio-recorded in their offices. A data collection pause was implemented after the first few interviews during which the interviews conducted were transcribed, reviewed and feedback were communicated to the field teams. The interview took an average of 73 min. Data was collected between June through July, 2022.
Data management
The recorded interview audios were transcribed verbatim in the original language of the interview. Transcripts were complemented with notes taken during the interviews. The transcripts, audio files and notes were labelled with unique identifiers that enabled data linkage across files. A data security protocol was implemented to safeguard against data breach. A Dropbox folder, which was only accessible to designated research team members, was created for the safe storage of the audio files, transcripts and summary notes.
Coding was done using Atlas.ti. One coder was involved in the coding the data while multiple coders coded subsets of the data for agreement. The entire research team interrogated the data and review the coding. Emerging sub-themes were categorized under the appropriate pillars of health system including (i) service delivery, (ii) health workforce, (iii) health information systems, (iv)medicines and supplies, (v) financing, (vi) leadership/governance [ 15 ].
Respondent socio-demographic characteristics
A total of 22 state-level participants were interviewed from 10 states and the Federal Capital Territory (FCT). Respondents’ age ranged from 40 to 60 years. The majority 18(82%) were male while the median total duration of employment was 23.5 years. The respondents held leadership positions in SMoH and SPHCDA, with many being Deputy/Acting Directors 6 (27%) and Directors 5 (23%) and commissioners for health 2 (9%) (Table 1 ). Most 20 (91%) had been in their current position for at least 2 years.
Health services delivery volumes at the PHC during the COVID-19 pandemic
All participants acknowledged reduction in patients’ attendance at the PHCs while some also mentioned interruption in health services delivery. The decrease in facility utilization was more pronounced during the early stage of the pandemic particularly from March 2020 through June/July, 2020. Notably, there was a drastic reduction in the antenatal clinic attendance by pregnant women and the under-5 children outpatient visits across all regions of the country.
The movement restriction during lockdowns and the fear of contracting COVID-19 were the two most prominent reasons stated for reduction in health facility patients’ attendance. Where facilities were still in operation, fear of contracting the virus among patient and health workers was common in all regions.
On the supply side, some health workers did not go to work, while some facilities were instructed to close completely. The lockdown reduced the number of health workers who were able to commute to work especially those who did not have personal means of transportation. Some state governments (such as Lagos) tried to ameliorate this by providing ambulances that took frontline workers to work. Health workers were also given stickers to identify them as essential workers so that the law enforcement agents would allow them to move through the lockdown. Like the patients, the health workers were also scared of contracting COVID-19 infection and they encouraged patients that could be managed at home to stay away from the health centers. They also referred patients very readily to the next level of health care with minimal investigations. The decline in services were attributed majorly to the COVID-19 pandemic.
On the demand side, patients were unable to travel to health facilities because of lockdown restrictions. Participants also emphasized on the economic challenges and bank closures which reduced people’s ability to purchase goods and services including healthcare. Community members exhibited fears from the belief that COVID-19 was domiciled in the health facilities. People were further afraid of being isolated in the event that they were diagnosed with COVID-19.
Differential impact of COVID-19 on LGAs
There was consensus between the participants from the different regions that urban areas had a higher burden of COVID-19 infection including disease incidence and case fatality. Consequently, there were more COVID-19 response activities in urban areas.
Participants in all regions believed that health service provision had returned to normal by June, 2022 especially for some suspended activities in the pandemic. Such activities included the integrated supportive supervision of health facilities which was believed to have returned to pre-COVID-19 levels. The isolation centers were no longer in existence and ad-hoc workers were no longer in employment. However, some COVID-19 prevention strategies such as the social mobilization, advocacy and risk communication were still on-going at the time of data collection.
Challenges faced in maintaining essential health services
Key challenges were identified by participants. Human resources shortage was the most commonly mentioned challenge from 4 GPZs, 6 states (Lagos, FCT, Imo, Kano, Abia, Ogun) of the country. Other commonly mentioned challenges included: Shortages in the supply of Personal Protective Equipments (PPEs) 4 GPZs, 5 states (Imo, Lagos, Ogun, FCT, Gombe); fear of contracting COVID-19 among health workers 4 GPZs, 4 states (Imo, Ogun, FCT, Rivers); misconception, ignorance, socio-cultural issues 2 GPZs, 2 states (Rivers, Imo); lockdown/transportation 2 GPZs, 2 states (Abia, Lagos); and lack of equipment/waiting area 2 GPZs, 2 states (FCT, Oyo). Less commonly mentioned challenges included: training gap, inadequate referral, diversion of other facility budget lines to PPEs purchase, and insecurity. The challenges considered to pre-date COVID-19 included: human resources shortage, shortages in equipment and PPEs, poor infrastructure and inadequate funding.
The challenges faced in maintaining essential health services in different health systems pillars are highlighted below with sample quotes from individual respondents (Table 2 ):
Leadership and governance
The respondent from the North Central (NC) zone explained that most of the resources allocated to various other activities in health facilities were redirected to meet the needs of COVID-19 response especially the provision of PPEs (Table 2 ):
…. the challenge of diversion… of resources [budget for other facility needs]… for PPEs.
From the Southwest (SW) zone, a respondent stated that insufficient funding had always been a challenge in carrying activities such as providing electricity in the PHCs. The challenge pre-dated COVID-19 pandemic.
“Insufficient funding has always been on ground. It is not really related to COVID-19. It has always been a case in most of the PHCs getting stipend to run the PHC like lightings, generators, pumping of water.” ( SW , )
Service delivery
The majority of the PHCs lacked infrastructure that could aid organization of services to provide physical distancing for the patients. A participant in the SW was quoted:
…majority of the health facilities do not have waiting area….
The health facilities experienced difficulty in transporting COVID-19 patients referred to isolation center for care. This was expressed by a participant in the NC zone:
“…referral, when somebody is positive having to evacuate from the hospital to the treatment center was a challenge” ( NC ) .
In the South-south (SS) and Southeast (SE) zone, the participants expressed concerns about patients’ misconceptions about COVID-19. Many patients did not believe that COVID-19 exist and as a result, were unwilling to adhere to facility COVID 19 prevention protocols. These misconceptions were reinforced by socio-cultural norms and reliance on dictates of religious leaders.
“.Misconceptions about the disease… with thoughts that there was no COVID-19 in the first place” ( SS ) .
“…the person [patient], and/or.relatives are not willing to adhere to the protocols, …what do you do?.socio-cultural issues,…where some people will say my pastor said…” ( SE ) .
Human resources
Inadequate human resource which predated the COVID-19 pandemic was expressed by both northern and southern zone respondents across six states. However, this challenge was amplified by the pandemic. There was limited number of personnel with the requisite skills to perform tasks related to the response. The task shifting strategy implemented to share task and thereby, reduce the number of health workers in facilities at any one time, also reduced the human resource capacity in the PHCs.
“The major challenge is… inadequate man power which has existed before COVID-19….” ( SW ) .
“Then during the pandemic too some health care workers absconded….health workers who had the requisite capacity were quite few” ( SE ) .
“….there was some sort of shifting done to reduce the number of health workers working at the same time…” ( NC ) .
Respondents in SW and SE also described the challenges that health workers encountered in getting to the health facility during the early period of the pandemic due to the lockdown. This was said to compound the human resource shortages.
“They [workers] find it a bit difficult to get to their work place some of them have to use their workplace as home …” ( SW ) .
“It included even the health service providers. They were locked down. They could not even access the facilities” ( SE) .
The human resources shortages in the facilities was confirmed to have been a long-standing problem that existed before the pandemic across all regions of the country which was now amplified by the pandemic.
“It [staff shortfalls] was on ground before …” ( SW ) .
“Yes, I said it that staff shortfall has been a long-term issue. The work is becoming voluminous everyday” ( SW ) .
“Of course, we have human resources gaps, before and even during the pandemic” ( NC ) .
“Well, I will say the issue of the human resource for health, it has been a long-lasting challenge even before the pandemic. So, it was now heightened by the pandemic…” ( SE ) .
Health workers’ attitude to work was stated as being a challenge to utilization of PHCs by clients. Due to the fear of contracting COVID-19, health workers were not committed to work.
“We had challenges with attitude to work you understand? Some people were more reluctant” ( SS ) .
“…health workers had a ground to be afraid because there were gaps [in] science” ( SE) .
“…even health workers were scared and they were not so committed to work because there was risk [of infection]” ( NC) .
Medicines and supplies
Respondents across most of the regions reported shortages in medical consumables such as PPEs, face masks and sanitizers especially at the beginning of the pandemic. One respondent decried challenges with the supply chain because of restricted access to PPEs even though some facilities had supplies locked up in the store.
“… it was so bad that some doctors will even use their money to buy sanitizers and face masks so as to protect themselves” (SW) .
“…dearth in supply of PPEs….but that was at the initial period. Before COVID − 19, there were no local manufacturers” (SE) .
“…when we started there was really a challenge in the facilities because even face masks were running out. Sanitizers were running out because of the increased use.” (NE) .
“…challenges about the supply chain in terms of internal access to the PPE. We put the PPE in the store and health workers in the emergency unit were not having access” (NC) .
“Rapid test for SARS-CoV-2 was not available at the beginning [of the pandemic]” as expressed by a respondent from the FCT (NC) .
The dearth in supply of consumables was confirmed to be a challenge that existed before the COVID-19 pandemic. However, the increase in the cost of some consumables such as PPE, gloves and face masks was a challenge that came with the COVID-19 pandemic.
“Dearth in supply of PPEs was actually a challenge that was in existence beforehand” ( SW) .
Mitigation strategies to health systems challenges during COVID-19 pandemic
Several interventions were implemented by state governments to address the challenges of maintaining essential health services (Table 3 ). State governments focused on the provision of consumables; recruitment, redeployment and provision of training for health workers; expansion of the infrastructural capacity; provision of vaccines, stipends, security and subsidizing health services costs. These interventions were in all regions of the country.
Political will improved during the COVID-19 pandemic, state governments were positively disposed to improving health services delivery.
“Government was ready to approve all the ongoing projects, all the ongoing services, basic medical services were being provided, they also were fighting stigma within the facilities” (NC) .
“They [government] made some services affordable, available and accessible and within the reach of the community member. They were taking services even to the community outside the facilities, services like outreach services, information dissemination and empowerment. ” (NC) .
Key interventions implemented across the regions were cascaded from state level to the LGA and facility levels down to the community. Across all regions, training and capacity building were stepped down to LGAs, facility heads and community. These activities were facilitated through LGA officers and community stakeholders.
“Health worker training was also done for health workers at the primary care centres and the secondary facilities at each of the area council. So, all the activities, all the IPC was also done.” ( NC ) .
“At the state, we have a state officer, we have the Local Government officers, we also have the health facility officers. These trainings were cascaded down from the State to the Local Government and to the health facilities to ensure that the various layers of response are well equipped in terms of capacity.” ( SE ) .
“We train and monitor. We also conduct supportive supervision from the state level down to the local government levels then to the ward and facility level; we do that routinely. We check their knowledge gap and also do on the spot training for whichever gap that we are able to identify.” ( SE ) .
“…there were trainings that we received, training upon training which usually comes from the national to the State and then we step it down to the local government and then from the local government to the wards within local governments and the facilities.” ( SW ) .
“We work with the medical officers of health in the twenty-three LGAs and the heads of facility to redistribute our staffs.” ( SS ) .
Coordination across levels of the health systems also ensured timely distribution of health facility materials:
“The moment the supply comes into the state with immediate effect they write to the MOHs (Medical office of health) in the local government stating we have some materials for you, because we do not wait until the MOHs come to collect the materials, so we send a letter to them via email communicating the delivery time. E.g. we are bringing it tomorrow morning or we are bringing it this evening be available to receive it. The moment it gets to the MOHs, the MOHs step it down to all the facilities and PHCs with immediate effect.” ( SW ) .
“The state primary health board makes funds and logistics available at the local government level” ( SW ) .
“The intervention trickles down to the facility level. The State made sure that the issue of man power, issue of adequacy of jobs you know and consumables at the health facility are addressed at the highest decision level” ( SW ) .
The COVID-19 response was supported by donor partners such as in the provision of PPEs. The government also mobilized funds from the private sector which was made available to the hospitals and PHCs.
“The state government provided PPEs, because there were also donations to them, many private sectors also donated and… they made it available for the public hospitals” ( SE) .
Regarding service delivery during the pandemic, interventions implemented included reorganizing service delivery for more facilities to render more services.
“We had to reorganize our system to ensure that more facilities in some strategic locations were rendering more services, had more people to render services, you understand, 24/7. We actually had to do that” ( SS) .
The government also built COVID-19 isolation and treatment centers to relieve the pressure on the hospitals and ensure COVID-19 patients had good care.
“They [state government] provided treatment centers for those who required admission,” ( NC) .
“Government-built isolation centers all across the 20 local government in Ogun state that is the jurisdiction.” ( SW ) .
In the Northwest (NW) zone, the government organized the Emergency Maternal and Child (EMC) services where they provided ambulances to pick up pregnant woman that required emergency surgery. Provision of ambulances was not limited to the NW region as other regions also mentioned government support by providing ambulances.
“For example, during COVID-19 pandemic people there had emergency cesarean sections especially pregnant women. There is an ambulance that picks them and there is also another one that is called EMC services, it is a special service provided by the State government for Maternal and newborn child free up to this moment” (NW) .
Intervention strategies in facilities also included prioritization of facilities in terms of services and staffing needs, rescheduling of patients’ appointment that were not emergency cases.
Clients were also redirected from facilities that were shutdown to nearby facilities that could provide treatment services. Services prioritized included patient monitoring/treatment, immunization services and provision of ambulance for transportation.
“Well, the patient monitoring evaluation and treatment were prioritized because we do not want to come down with a lot of mortality. So adequate equipment [and] consumables were provided by the State and the manpower involved were adequately remunerated and then the State paid a lot of money for them to maintain this service” ( SE ) .
“The services like maternal and child care…. those services are key. We want to make sure that mothers, pregnant mothers access care on time, the children too… Those that need to be immunized and all of that.” ( SW ) .
“The maternal, new born and child health services were prioritized and also the health workers themselves were prioritized because they are the frontliners” ( SE ) .
“…anybody that falls sick and gets to the hospital will receive care but we pay attention on pregnant women and little babies more because their own case is peculiar” ( SW ) .
“The mother too who attended antenatal clinic and even the test that will be run everything was done for free and was sponsored bby the PHC Board to the extent that they printed cards and gave it to them for free that they were not supposed to pay. The registration, everything was made free at that time. This is just to act as reliefs at that time for those who access health at the health facilities” ( SW ) .
To address the shortfall in human resources, the SW region employed health worker cadres such as doctors and nurses in batches per time, as the budget could accommodate. In some other regions such as the SE, health workers were redeployed to work at facilities which were near where they lived to improve delivery. Ad hoc staff were also engaged to work for a few months.
Workshops were organized by the state governments to train and inform the health workers on IPC and to improve their skills. This helped to alleviate their fears on contracting the virus so as to alleviate their apprehension.
Health workers including adhoc staff were motivated by increasing the hazard allowance, which led to the increment in their monthly salary.
“They [government] gave some allowances to adhoc workers for a few months. So those adhoc workers helped….The state government also provided ambulances, one ambulance to one local government. They gave ambulances and drivers…also provided security…” ( SE ) .
“Health care workers were also provided with the relief materials to also help them continue in their work” ( SE ) .
“Increasing the health workers hazard allowance is something that the government did….” ( SW ) .
“Yes, the government provided allowances to encourage those who were at the frontline to ensure that they [health workers] at least had something reasonable to hold on to while offering their services and apart from that government was coordinating the activities of the various fronts including that of security.” ( SE ) .
“Giving reliefs, packages, and giving us bonus that was all.” ( SW ) .
“Those that took part in surveillance were given certain stipends, those that did case management were given certain stipends, those that took part IPC, risk communication, point of entry was given certain stipends.” ( SS ) .
“Governor continued, was even giving transport stipends to surveillance officers, laboratory personnel, just to encourage them to do the work and so, these things were going on as a kind of stimulant, a kind of motivation to assist in getting the job done. So as at that period those things were not lacking for us, so that is what I can say about that .” ( SS ) .
“The support is the trainings that were done, stipends were paid adequately as at when due and the health workers were happy with that, as they carried out their duties” ( SE ) .
“The hazard allowance was increased, I think to about 15% or thereabout, so all those incentives were there for health workers to actually motivate them to do more, so the State government did that.” ( SW ) .
“Palliatives, all the health workers were given palliatives.” ( SW ) .
“All the health workers were given adequate and reasonable support; number one, in the FCT, they were well paid. Those that were directly involved [in COVID-19 control] were well paid by the honorable minister of the FCT, secondly, they were all provided at any given point in time with PPEs, they were also well trained to monitor patient, and even the family of those who died were given some support, I think some were promised land, I don’t know if they have given them. They were given high level of support.” ( NC ) .
Other support granted by the State to motivate health workers included training, recruitment to support existing staff, provision of security, relief packages and ambulances.
“I know I have talked about redistribution of workers, of course ad-hoc workers for those very few months, then some of the PPEs and some of the security, I think that’s the only thing I can say.” ( SE ) .
“To be sincere we have to appreciate the state government, at that time they even gave us accommodations, food and everything during the first pandemic. They support us with training of case management for us to take care of patients as well as series of other training. We all attended online training on oxygen therapy and it was even paid for” ( NW ) .
“At one point, it was difficult for health workers to move from one point to the other, so government aided the movement of health workers by providing certain things to identify them, also providing ambulances, movement support to enable them move from their homes. They also provided accommodation for health workers at the isolation center.” ( SE ) .
“And also, they bring in special teams to also support the teams on ground.” ( SE ) .
“Well, we did some form of reorganization and that did include the personnel. So, we had to increase the number of personnel in our focal facilities which increase the services” ( SS ) .
“Yes training has always been in existence so they do refresher training but during the COVID it become more intensified because of the session or season we are.” ( SW ) .
Information systems
Respondents mentioned that government engaged in communication/sensitization programmes to improve service utilization using different media including the traditional and social media. The targets of the communication programmes were the community members including religious and ethnic groups. Communities, markets, churches and mosques were some of the places where the health promotion campaigns took place (Table 3 ).
Adaptations of the health systems during COVID-19
Sustainable adaptations.
Table 4 shows the emerging themes on sustainable adaptations done by the health systems. Respondents considered the infection, prevention and control (IPC) infrastructure (taps for running water), the telehealth call center, the IPC protocols and the service reorganization, as sustainable. A respondent mentioned that each health facility had an IPC focal person and also IPC teams which the health system can continually optimize.
Respondents considered that the training programs and capacity building efforts (especially the ‘network electronic platform’), implemented during the pandemic were sustainable. They opined that IPC training should be mainstreamed because the topic was broad and had impact on prevention of other infectious disease areas apart from COVID-19.
Respondents also mentioned that the volunteer groups formed during the pandemic for community sensitization and community engagement, were retained and would be used for other intervention programmes. Health teams have also retained the virtual mode of conducting team meetings.
Unsustainable adaptations
Respondents considered some adaptations in financing, service delivery and supplies, as unsustainable (Table 5 ). The funds that the government mobilized in form of incentives to health workers, stipends for campaigns team members and payment for other ad hoc staff such as town criers, were no longer being provided. The free testing and healthcare for COVID-19 patients which governments implemented was not sustained. The health workers who were redeployed have returned to their pre-pandemic assignments. In addition, all the services rendered to patients at the COVID-19 treatment centers including treatment, accommodation, consumables, were free and therefore, considered unsustainable. This also included the free consumables supplied to the health workers.
Summary of findings
The qualitative study selected senior persons in decision-making positions. Respondents acknowledged a reduction in patients’ attendance at the PHCs and interruption in service delivery. This prominently affected antenatal care attendance by pregnant women and the care for the under-5 children across all regions in the country. There was consensus among the regions that the urban communities had a higher burden of COVID-19 infection making the activities around COVID-19 control more intense in these communities. Unfortunately, this negatively impacted the provision of care in health facilities in these communities, leading to a negative impact on provision of EHS.
The challenges experienced in maintaining essential health services cut across the pillars of the health systems. Resources were reallocated to COVID-19 control activities from other budgetary lines due to insufficient funds to implement control activities. The infrastructure of most of the PHCs could not accommodate changes in service reorganization which was needed to enable physical distancing. It was also challenging to transport referred COVID-19 patients to isolation centers. Patients had misconceptions on the cause and transmission of COVID-19 and were unwilling to adhere to facility protocols. There was severe shortage of human resources which predated and was accentuated by COVID-19 control interventions such as lockdowns, staff redeployment and task shifting. Health workers were reluctant to discharge their duties because of fear of contracting the infection. There was inadequate consumables for use albeit sometimes due to deficient supply chain management.
Several mitigation strategies were implemented to address the challenges encountered. Political will towards improvement of health service projects was increased during the COVID-19 pandemic. This was reflected in government efforts to make health services available, accessible and affordable. Efforts were also made to provide consumables, recruit both permanent and ad-hoc staff, motivate existing health workforce, and redeploy/train health workers. The health infrastructure capacity was also expanded across regions, to free up spaces for provision of EHS by building/renovating COVID-19 isolation and treatment centers. Service delivery was also reorganized by rescheduling appointment for non-emergency to a later date and prioritizing essential services such as immunization, maternal and child care. Health promotion campaigns to groups and communities, were conducted to improve service patronage. Sustainable systems adaptations included IPC and telehealth infrastructure, IPC protocols, IPC teams and focal persons, training and capacity building, virtual meetings and community groups set up for sensitization and engagement. Unsustainable adaptations included funding, free healthcare and consumables, redistribution of staff, and the maintenance of COVID-19 treatment centers.
Results in the context of the literature
The COVID-19 pandemic disrupted EHS in almost all countries of the world and the disruption continued for over two years in more than 90% of countries surveyed by the WHO [ 30 ]. Particularly affected were the maternal and childcare services as corroborated in both quantitative and mixed methods design studies [ 31 , 32 , 33 ]. Our study corroborated findings from surveys among health workers and community members in Burkina Faso, Ethiopia and Nigeria, confirmed partial-to-total interruptions in health services delivery and utilization especially maternal and child health services [ 34 ] due to lockdowns, fear of infection/stigmatization, misconceptions/misinformation about the disease, stockout of drugs, and lack of transportation due to lockdowns [ 35 , 36 ]. As noted in this study, the disruption affected most services to the extent that some PHCs with low capacity were closed down. Studies indicated that disruptions appeared to affect disproportionately maternal and child care including immunization [ 30 ]. As noted in the WHO survey and as corroborated by our study, the major barriers to health service recovery were health systems challenges which predated the COVID-19 pandemic. Very prominent pre-existing health systems deficiencies identified by our study were in the human resources, service delivery and the finance pillars.
The adaptations to service delivery implemented in healthcare facilities were similar across regions in Nigeria and notably, were designed to reduce patient inflow. Non-emergency cases were discouraged from accessing clinics and follow-up appointments were rescheduled because the facilities lacked the capacity to implement the recommended physical distancing between patients. In Ghana [ 37 ] similar adaptations were made to routine healthcare service delivery which also aimed at reducing patient flow to the health facilities. In this study, only clients with extremely important conditions were encouraged to visit the health facilities, appointments were reduced, non-essential medical and surgical procedures were less prioritized.
Although, facility closures occurred in most settings around the world during lockdowns because there was no health manpower to provide services [ 3 ], the telemedicine infrastructure which existed before the pandemic in some settings, were deployed to bridge the gap in consultation demands [ 3 , 38 ]. Nigeria developed a telehealth call center which was mainly for COVID-19 case finding but provides opportunities for general health consultations use.
Also, some health professionals were reassigned to COVID-19 control programmes which ultimately affected services such as home visits, immunization and other community health services [ 37 ]. A study conducted in Lagos, Nigeria highlighted the willingness of community health workers to function as care providers during the pandemic but were challenged by heavy workload and lack of transportation [ 39 ]. These recommendations informed some of the decisions to improve health workforce care packages including financial incentives and employment of additional staff [ 39 ].
Limited evidence exist in the literature on the challenges encountered in maintaining EHS in health systems. In Bangladesh, similar challenges were reported as we found in our study. The demand pull challenges in Bangladesh included fear of COVID-19 infection, difficulty with commuting during lockdown and reduction in health seeking behavior emanating from closure of health facilities without providing alternatives [ 40 ]. Also, as found in our study, health resources were redirected to COVID-19 leaving other important health programmes deprived. Likewise, there were staff shortages which predated COVID-19: Acting in synergy with panic among health workers, more health facilities and programmes were further abandoned as similarly documented in our study.
The literature was richer in terms of mitigation and adaptation strategies implemented to maintain EHS during the COVID-19 pandemic. Kabwama et al., used the same health systems pillar thematic framework to analyze the interventions implemented in maintaining EHS in Uganda [ 41 ]. Prominent in the Uganda analysis was the private sector engagement for public-private partnership in fund mobilization as reported in our Nigeria analysis. Unique adaptation in service provisions in Uganda involved leveraging patient networks to deliver medicine which was not found in our analysis. The Ugandan study appeared to focus more on general interventions that were not specifically directed at challenges in maintaining EHS contrary to what our study did. The mitigation strategies implemented in Bangladesh closely mirrored what our study found such as provision of consumables under the medicines and supply pillar, fund mobilization under the leadership/governance and finances pillars among others [ 40 ].
Perhaps, the most robust survey on service adaptations involved 129 countries and was conducted by the WHO [ 30 ]. It was clear that in all countries, services were shifted off the health facilities and moved to home-based or to tele-infrastructure. Low and middle income countries like Nigeria may benefit from such easily adaptable strategies because creating separate facilities for COVID-19 and EHS delayed implementation as a result of the considerable financial investment required. Policy makers involved in emergency and epidemic preparedness plans may incorporate proactive plans to achieve rapid implementation of similar strategies. Other prominent cross-cutting mitigation strategies reported across countries in the WHO survey included healthcare financing, health workforce training and capacity building, procuring of essential medicines and consumables, risk communications and community engagement.
Implication of findings and lessons learned
The WHO recommends that advanced planning and long-term investments in health systems is important for epidemic preparedness and in safeguarding the continued provision of EHS during a health crisis [ 42 ]. Findings derived from this study are imperative for a robust epidemic preparedness plan. Strategies to maintain supply and demand for EHS should be incorporated as essential elements of epidemic preparedness plans. Response to health crisis require a more holistic and proactive approach at planning. The challenges facing the Nigerian health system are long-term which will require considerable and consistent efforts to resolve. Thus, learnings on mitigation strategies and adaptations during the COVID-19 pandemic would be applicable for future public health emergencies as well as routine health services delivery. The sustainable adaptations can potentially serve as a foundation for a gradual, planned, and intentional investments in the core functions of the Nigerian health system in order to improve its resilience and preparedness. For example, maintaining a pool of potential ad hoc volunteers consisting of retired health workers and community volunteers who can be mobilized at short notice. Also, the partnership built during the COVID-19 pandemic between the government of Nigeria and the private sector could be strengthened and optimized for epidemic preparedness and EHS delivery. The government at all levels received funds and donations from the private sector which was channelled to COVID-19 control and health care service delivery.
Our study also highlights the importance of adequate and timely public health messaging. Misconceptions and misinformation were rife during the COVID-19 pandemic in Nigeria [ 23 ]. Also noted [ 23 ], most of the information provided were technical and focused on prevention of COVID-19, with only minimal messaging on the provision/utilization of EHS. Thus, on the social media, misconceptions festered and was a major cause of demand-pull decline in EHS utilization by communities. Both patients in need of treatment and those who were on follow-up appointments, largely stayed away from the health facilities due to fear of contracting COVID-19. Health facilities were stigmatized, and health providers discriminated against for fear of contracting the virus. Another driver of decline in demand was the fear of testing positive and being isolated [ 43 ]. Although, adaptations to EHS later reduced the need for physical contact with the health facilities, a large proportion of potential clients stayed away from the formal health system. The learnings derived from adaptations during the pandemic could provide opportunities for a transformative evolution of the primary health care system in Nigeria. Before the pandemic, across the country, only about 20% of the PHCs were assessed as functional [ 28 ], resulting in consultation overload of the secondary and tertiary facilities. The participants considered the telehealth call center to be a sustainable innovation. The Nigerian health system could benefit from upgrading and expanding telemedicine infrastructure to shift some of the PHC overload to this platform. This will enhance an elastic, epidemic prepared EHS delivery system.
As confirmed in this study, poor funding was a systemic challenge that predated COVID-19 pandemic. EHS delivery suffered major set-backs partly because the meagre financial resources available for healthcare delivery were diverted to COVID-19 control. The budget for the State PHC Board in a state in North Central zone of Nigeria was reduced by 11.5% in order to secure funds for COVID-19 control activities [ 44 ]. The government was able to raise some funds mainly from the private sector most of which was deployed towards public health measures for COVID-19 control with little investment to strengthen the health system [ 45 ]. Public-private partnership could be strengthened to form an extra-budgetary sovereign wealth fund which will be used for emergency health purpose only and which can be mobilized at short notice. The state governments demonstrated commitment to long-term public health investments and reforms during, and in the immediate post-pandemic period [ 46 ]. A sustained commitment will improve the overall performance of primary healthcare in Nigeria in the near future.
Strengths and limitations of the study
The strength of this study is that participants were actors at the sub-national (state) -level. They were senior personnel who were decision makers in COVID-19 control and provision of EHS. They had good knowledge of activities that transpired in the states during the COVID-19 pandemic. Also, we sampled participants from all geopolitical zones of Nigeria in the interviews, which ensured representativeness. We translated and back-translated tools across zones to ensure accuracy.
The tool was designed using the conceptual framework developed by Kruk et al. [ 16 ], which was not initially based on the health systems pillars. It is possible that data on some health systems pillars exist which were not captured during the interviews. Conceptual framework used in the Kruk’s framework are not strictly health systems pillars or building blocks. Our study recruited mainly senior personnel in the ministries which might skew observations without the views of the junior personnel. Readers should interpret the findings with the view that potential richer health systems context may exist.
This study showed that there were significant challenges in maintaining essential health services delivery and utilization during the COVID-19 pandemic in Nigeria. The maternal and child care services were particularly affected. The core health systems challenges which prevented the maintenance of EHS delivery were mainly in the human resources, service delivery and the financing pillars. The mitigation strategies and adaptations implemented were important contributors to EHS recovery especially in the high resilience LGAs and have implications for future epidemic preparedness plans.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
The authors appreciate all participants who invested their time in responding to the interviews, colleagues at the FMoH who guided the smooth execution of this work and Hanovia Limited colleagues for the implementation of the qualitative data collection and transcription. Mohammad Tawab Hashemi provided additional support from the Global Financing Facility for Women, Children, and Adolescents.
Funding for this study was provided by Gates Ventures and the Global Financing Facility for Women, Children, and Adolescents. The funders of this study were involved in the study design, data collection, interpretation, and reporting. The views, opinions, and content of this publication are those of the authors and do not necessarily reflect the views, opinions, or policies of the funders.
Author information
Authors and affiliations.
University of Ibadan, Ibadan, Nigeria
Segun Bello, Ayodele S Jegede, Eniola A. Bamgboye, Mobolaji M. Salawu, Rotimi Felix Afolabi & Olufunmilayo I. Fawole
The Global Financing Facility for Women, Children, and Adolescents, 1818 H ST NW, Washington, DC, 204333, USA
Rachel Neill, Munirat Ogunlayi & Saudatu Umma Yaradua
Nigeria Federal Ministry of Health, Federal Secretariat Complex, Phase III, Shehu Shagari Way, Central Business District, Abuja, Nigeria
Charles Nzelu, Ngozi Azodo & Anthony Adoghe
Gate Ventures, Seattle, Washington, USA
William Wang & Anne Liu
You can also search for this author in PubMed Google Scholar
Contributions
SB, RN, ASJ, EAB, MMS, RFA, CN, NA, AA, MO, SUY, WW, AL, & OIF were involved in the conceptualization and/or design of this study. RN, SB, ASJ, NA, CN, AA, MO, SUY, & OIF were involved in data collection and analysis. SB and OIF developed the first draft of the manuscript. SB, RN, ASJ, EAB, MMS, RFA, CN, NA, AA, MO, SUY, WW, AL, & OIF reviewed and revised the manuscript. All coauthors have approved the manuscript for publication.
Corresponding author
Correspondence to Segun Bello .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from the participants. Ethical clearance was obtained from National Health Research Ethics Committee NHREC/01/01/2007.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bello, S., Neill, R., Jegede, A.S. et al. Health systems challenges, mitigation strategies and adaptations to maintain essential health services during the COVID-19 pandemic: learnings from the six geopolitical regions in Nigeria. BMC Health Serv Res 24 , 625 (2024). https://doi.org/10.1186/s12913-024-11072-2
Download citation
Received : 09 September 2023
Accepted : 03 May 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12913-024-11072-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health systems resilience
- Essential health services
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Content Search
World + 10 more
On the Front Line: Investing in community health workers to improve health and nutrition [EN/AR]
Attachments.

Recommendations :
- Build on the work of the Community Health Delivery Partnership. Call on partners at the global, regional and country levels to commit to increasing their investment in community-based primary health care and essential nutrition services.
- Organize high-level political missions. Heads of government and ministers need to be convinced that prioritizing community-based primary health care and nutrition is the best way to strengthen their country’s health system. Programmes need long-term financing if they are to achieve their full potential.
- Coordinate and streamline partner support under the One Plan approach and align domestic and partner funding under the One Budget approach. This will support longer-term sustainable financing of community health systems, highlight funding gaps and allow the rapid mobilization of resources from different sources to fill them. Countries need to find alternative sustainable financing for community health and nutrition programmes to supplement funding from donors and domestic resources.
- Integrate community health and nutrition programmes into the primary health-care system. This is key to fulfilling the potential of the programme and strengthening the health system. The One Plan approach links communities with the primary health-care system.
- Engage and strengthen community leadership. This fosters ownership and is key to the success of community health and nutrition programmes. The One Plan approach involves community leaders and health workers in designing improved community health and nutrition programmes and encourages feedback from the community.
- Professionalize the role of community health workers. The One Plan approach recognizes the gender discrimination that front-line workers face and the importance of their role, and requires them to be adequately trained, paid, protected, supervised, equipped and supported.
- Strengthen the accountability of community health and nutrition programmes. The Community Health Delivery Partnership will collect and analyse data through a community health dashboard with the aim of monitoring and evaluating community health and nutrition programmes, developing key metrics for services provided by front-line health workers and recording investment in community health.
- Ensure that community health and nutrition workers have supplies of the life-saving commodities they need under the One Plan, One Budget approach. This includes developing training and quality assurance programmes and innovative products and material more suited for use in developing countries.
- Promote and strengthen the sharing of best practices. Insights and lessons learned from implementing community health and nutrition programmes across countries should be shared through the Community Health Delivery Partnership’s knowledge exchange platform to ensure that practices are continually evolving and improving.
Related Content
En primera línea: invertir en los agentes de salud comunitarios para mejorar la salud y la nutrición, en première ligne: investir en faveur des agents de santé communautaires pour améliorer la santé et la nutrition.
Bangladesh + 5 more
Research Report: Impact of Climate Change on the Migration and Displacement Dynamics of Rohingya Refugees (May 2024)
Inundaciones y lluvias extremas azotan brasil con un impacto sin precedentes en la historia del país.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Public Health
- v.106(4); Apr 2016
Characterizing Community Health Workers on Research Teams: Results From the Centers for Population Health and Health Disparities
All authors contributed to the study conceptualization and design, questionnaire development, and interpretation of results. S. D. Hohl administered the survey, conducted data analysis, and cowrote the first draft of the article. B. Thompson oversaw data collection and analysis and cowrote the article. All authors contributed significant revisions to multiple drafts and approved the final version of the article before submission.
Objectives. To quantify the characteristics of community health workers (CHWs) involved in community intervention research and, in particular, to characterize their job titles, roles, and responsibilities; recruitment and compensation; and training and supervision.
Methods. We developed and administered a structured questionnaire consisting of 25 closed- and open-ended questions to staff on National Institutes of Health–funded Centers for Population Health and Health Disparities projects between March and April 2014. We report frequency distributions for CHW roles, sought-after skills, education requirements, benefits and incentives offered, and supervision and training activities.
Results. A total of 54 individuals worked as CHWs across the 18 research projects and held a diverse range of job titles. The CHWs commonly collaborated on research project implementation, provided education and support to study participants, and collected data. Training was offered across projects to bolster CHW capacity to assist in intervention and research activities.
Conclusions. Our experience suggests national benefit in supporting greater efforts to recruit, retain, and support the work of CHWs in community-engagement research.
Community health workers (CHWs), variously known as lay health workers, lay health advisors, health navigators, community educators, promotores , and other titles, are increasingly involved in intervention research studies and health care teams and have garnered growing national attention in recent years. 1–3 The US Department of Health and Human Services defines CHWs as
lay members of communities who work either for pay or as volunteers in association with the local health care system in both urban and rural environments and usually share ethnicity, language, socioeconomic status, and life experiences with the community members they serve. 4 (piii)
In 2009, the US Department of Labor recognized the important role CHWs could play as members of the health care team and recommended a single labor category for these professionals. 5
As diverse as their titles, the varying roles of CHWs and efficacy of CHW-led interventions in public health promotion and disease prevention are the focus of much of the extant literature on CHWs. 6–11 Although a general responsibility of CHWs has been described in the literature as working with communities to improve health outcomes, the depth and breadth of CHW roles in health promotion and disease prevention work appears to be as diverse as the projects to which they contribute. 12,13 Findings from the National Community Health Advisor Study elucidated 7 core competencies of members of this profession: cultural mediation, informal counseling and support, providing culturally appropriate health education, advocating individual and community needs, ensuring that people receive the health services they need, building individual and community capacity, and providing direct services. 12 Other studies have added to these roles, describing the function of CHWs as monitoring health status, promoting screening, facilitating treatment adherence and community participation in the health system, and encouraging self-management. 11,14,15
Several reports document that CHWs are effective in increasing community engagement, connecting host communities to health services, and improving health outcomes, particularly among vulnerable populations. 6–8 Although many research articles describe the efficacy of individual CHW interventions, little is known about the overall characteristics of CHWs who work on research teams, where they may function as research assistants, educators, or interventionists. 11,14,16–18 The contributions of CHWs as members of research teams that address health disparities are seen as critical to reaching and engaging individuals in underserved populations. Because they are members of the community being served, CHWs are well-situated to provide insights to researchers about realities faced by their communities. 9,18 Integrating CHWs into research teams also may increase community involvement in research and reduce health disparities in underserved populations. 1,8,19 Furthermore, because CHWs often have similar demographic and social characteristics (e.g., ethnicity, socioeconomic status) to the populations they serve, including CHWs in research projects may be an effective strategy for addressing fear, mistrust, and historically low participation of the underserved in public health and clinical research. 19–22
Studies describing CHW involvement in research have qualitatively examined the role of CHWs in specific research studies 3,17 and have contributed much to the understanding of CHW participation in individual research projects. Few studies, however, have systematically collected data from a national sample of research projects that employ CHWs; thus, little information exists about CHW roles, responsibilities, recruitment, hiring, and training in diverse research projects. Such activities may include recruiting participants, obtaining informed consent, collecting data for intervention activities, and carrying out behavioral interventions. Furthermore, there is limited evidence to provide a framework for academic and research partners aiming to meet community needs by integrating CHWs into their teams. Evidence to guide the operational integration of CHWs into research teams would be useful for researchers who propose to work with CHWs. The current study contributes to the literature examining the characteristics, skills, and effective integration of CHWs into research teams.
Since 2010, 10 centers throughout the United States have been involved in the National Institutes of Health–funded Centers for Population Health and Health Disparities (CPHHD) initiative. 23,24 Each center leads multiple research projects focused on reducing health disparities in cancer and cardiovascular disease among diverse underserved populations across the United States. Among the requirements for funding was that each CPHHD conduct at least 1 community-engaged intervention project. Several of these projects used a community-based participatory research approach, in which communities are expected to be involved in every aspect of the research, from study design to results dissemination. 25 Each project consisted of a unique, often multilevel intervention (e.g., home- or community-based lifestyle intervention, clinic-based educational intervention) in which CHWs played a role in engaging members of an underserved population (e.g., urban African Americans, urban Puerto Ricans, rural Mexicans, rural Appalachians) in the intervention. Across all projects, community engagement was operationalized by including CHWs, establishing community advisory boards, and partnering with community-based organizations (CBOs) to conduct research. The components of CPHHD community-engaged research projects presented a unique opportunity to examine the involvement of CHWs in an effort to add to the understanding of how CHWs engage in and contribute to research.
Investigators and staff representatives from 9 of the 10 CPHHDs convened to form the CHW Working Group. The group’s overarching goal was to examine the roles and contributions of CHWs to CPHHD research projects. After reviewing definitions of CHWs from multiple sources, the CHW Working Group determined that no existing definition encompassed the diversity of CHWs on CPHHD projects. Therefore, during study conceptualization, the working group established a working definition of CHWs for the current study, as “lay individuals from the community who function essentially as research assistants, educators, and/or interventionists on CPHHD research projects.”
Working group members engaged CPHHD center directors, principal investigators, and project staff to self-select which of their projects included individuals who met this loose definition. Subsequently, the working group ascertained that 18 projects in the 10 centers involved CHWs. To elucidate the roles that CHWs fulfill, as well as information about recruiting, hiring, supervisory strategies, and training provided to CHWs, the CHW Working Group proposed to administer a survey to the staff person(s) at each CPHHD who was most knowledgeable about the role of CHWs on each project. Subsequently, each principal investigator was asked to provide the name of the projects and the person(s) who met this criterion. Once eligible projects and corresponding representatives were identified, a recruitment letter containing a link to a Web-based questionnaire was e-mailed to each identified project representative.
The CHW Working Group developed a structured questionnaire consisting of 25 closed- and open-ended questions that aimed to (1) characterize the job titles, roles, and responsibilities of CHWs; (2) identify approaches to recruiting, hiring, and compensating CHWs; and (3) describe training and supervision provided to CHWs involved in intervention research. We collected and managed study data by using REDCap electronic data capture tools, a secure, Web-based application designed to support data capture for research studies. 26
We exported data from the Web-based questionnaire into SPSS version 21.0 (IBM, Somers, NY) for analysis. We used descriptive statistics to obtain frequency distributions for CHW roles, sought-after skills, education requirements, benefits and incentives offered, supervision, and training activities.
Between March and April 2014, 16 representatives from all 18 projects across the 10 CPHHDs that involved CHWs in their research studies completed the Web-based questionnaire. Respondents most commonly self-identified as a CPHHD project manager or coordinator (70.6%) or CBO manager or coordinator (11.8%).
Community Health Workers and Projects
A total of 54 individuals worked as CHWs across the 18 CPHHD research projects. Of these, 11 (20%) CHWs worked on more than 1 CPHHD research project at their center. They held a variety of functional job titles, including terms that reflected the type of work they performed ( Table 1 ). One project employed 15 (27.8%) CHWs with the title youth advocate, and 2 projects employed a total of 15 (27.8%) CHWs who held the title research assistant. Five (27.8%) projects employed a total of 12 (22.2%) CHWs with the title community health worker, and 4 (22.2%) projects employed a total of 4 (7.4%) CHWs with the title community health educator . Less commonly used functional titles across the CPHHD projects were health counselor, community health advocate, community supervisor, and phone coach.
TABLE 1—
Community Health Worker Titles in Centers for Population Health and Health Disparities Research Projects: Seattle, WA, April 2014
Note. CHW = community health worker; CPHHD = Centers for Population Health and Health Disparities.
The CPHHD projects used human resource (HR) departments housed both at the research institution and at CBOs to hire and compensate CHWs. All HR departments assigned an even greater number of miscellaneous titles to the role of CHW. Across the 18 projects, 14 distinct titles were assigned, including promotor/promotora , community health worker, health care research assistant 1, patient navigator, project coordinator, research project interviewer, and social research assistant.
Community Health Worker Selection Criteria
The educational requirements for CHW positions in these projects varied. Only 4 projects (22.2%) had no minimum educational requirement for the CHWs; some projects required that CHW applicants have a high-school education (27.8%), and half required some college or a bachelor’s degree (50%).
Respondents were asked to identify the top-5 sought-after skills and attributes of CHW applicants ( Table 2 ). Among the 18 projects, 15 (83.3%) reported that knowledge of the host community and communication skills were the most highly sought-after skills and attributes, followed by personality attributes (72.2%), being bilingual or bicultural (44.4%), and having experience with administrative tasks such as report writing (44.4%; Table 2 ). The CHW applicants were less frequently required to possess health literacy, group facilitation or conflict resolution skills, or knowledge of current technology.
TABLE 2—
Education, Sought-After Skills, Roles, and Attributes of Community Health Workers on Centers for Population Health and Health Disparities Research Projects (n = 18): Seattle, WA, April 2014
The CHWs most commonly collaborated on intervention research project planning and implementation (e.g., developing intervention tools; 88.9%), provided education and support (83.3%), delivered interventions (77.8%), and recruited participants (77.8%; Table 2 ). Although they were involved in collecting both quantitative (66.7%) and qualitative data (44.4%) and contributed to manuscript writing (27.8%), no respondents reported that CHWs were involved in analyzing the collected data. The CHWs were similar to the populations they served in most respects, particularly in race/ethnicity, languages spoken, and gender ( Table 2 ).
Recruiting, Hiring, and Compensating CHWs
Multiple mechanisms—both research institution–based and community-based—were used to recruit and hire CHWs across the 18 projects ( Table 3 ). Recruitment was most often conducted in the community by community advisory boards, contacts at the CBO, or a CBO coordinator. Half of the projects relied on referrals to recruit new CHWs, and about 22.2% of project representatives reported distributing and posting flyers around the community (e.g., schools, youth agencies, parent groups). Although communities were often engaged in CHW recruitment, hiring was more often carried out by research institution–affiliated entities, such as by the research project manager (61.1%) and the research institution’s HR department (38.9%).
TABLE 3—
Responsible Entities for Recruiting, Hiring, and Supervising Community Health Workers on Centers for Population Health and Health Disparities Research Projects (n = 18): Seattle, WA, April 2014
Note. CBO = community-based organization; CHW = community health worker; CPHHD = Centers for Population Health and Health Disparities.
The CHWs were employed in a combination of hourly, full-time, and part-time positions, based on the needs of each project. Seven projects (38.9%) employed exclusively full-time CHWs; 2 (11.1%) employed exclusively part-time CHWs; 2 (11.1%) employed exclusively hourly CHWs; and 5 (27.8%) projects employed a combination of hourly, full-time, and part-time CHWs. The CHWs offered their time as volunteers on 1 project and were provided a stipend. The CHWs on all other projects were paid as employees by the research institution or CBO.
Paid CHWs were compensated with funds from the CPHHD grant at each institution. Paychecks were most commonly issued by the CBO (44.4%), followed by the research institution (38.9%). Three projects (16.7%) reported using a third party to issue paychecks (n = 2) or volunteer stipends (n = 1). The CHWs on those projects, regardless of their employment status, were offered various benefits, including health insurance (77.8%), paid time off as vacation (77.8%) or sick leave (77.8%), holidays (72.2%), life insurance (72.2%), and retirement benefits (61.1%). Half of the projects also offered tuition support to CHWs who wished to pursue further education.
Supervision, Retention, and Training
The CHWs received different levels of support and supervision as members of CPHHD research teams ( Table 3 ). Supervision was provided by CPHHD project managers or coordinators (66.7%) or CBO managers or coordinators (11.1%). The majority of supervisors held a college (33.3%) or graduate degree (50%). Supervisors implemented different strategies for increasing retention and support, including team meetings (100%), one-on-one meetings (83.3%), and annual or biannual performance reviews (77.8%). The CHWs on 8 of the 18 projects had left the CPHHD projects at the time this survey was administered. The main reasons for leaving included project termination (50.0%), job advancement at another organization (22.2%), pursuing further education (16.7%), or poor work performance (16.7%).
The CHWs involved in 15 (83.3%) CPHHD projects were offered ongoing training to build capacity for intervention activities, research activities, and basic skills necessary to fulfill their job duties ( Table 4 ). The training topics delivered most commonly to CHWs were confidentiality (i.e., Health Insurance Portability and Accountability Act of 1996 [HIPAA]; 94.4%), research ethics (83.3%), quantitative data collection (i.e., administering surveys; 61.1%), and qualitative data collection (i.e., conducting in-depth interviews, focus groups; 55.6%).
TABLE 4—
Training Activities Offered to Community Health Workers on Centers for Population Health and Health Disparities Research Projects (n = 18): Seattle, WA, March–April 2014
Note. CHW = community health worker; CPHHD = Centers for Population Health and Health Disparities; HIPAA = Health Insurance Portability and Accountability Act of 1996.
In this study, we provided an overview of the variety of CHW titles, roles, and responsibilities, and the recruitment, hiring, and training practices used with CHWs involved in CPHHD health disparities research projects. The role of CHWs in health promotion and disease prevention is well established; our data contribute important information about how CHWs may be integrated into research teams.
The CHW applicants were most sought after when they possessed knowledge of the host community and were able to communicate effectively across both study populations and researchers. Not surprisingly, in the CPHHD projects under study, researchers relied heavily on community-affiliated entities to assist in recruiting CHW applicants. Our findings suggest that establishing and using community contacts to recruit candidates who are knowledgeable about and, ideally, part of the community, may enable researchers to access a qualified CHW applicant pool. Current CHWs themselves are valuable resources for recruiting new applicants because of their familiarity with the study population, job duties, and likely personal connections to eligible applicants. In addition, the formation of community advisory boards may be a successful approach to bolstering CHW recruitment efforts. Ideal community advisory board members are local stakeholders who, like CHWs themselves, are often well-connected in the community. Furthermore, they are familiar with community health priorities as well as the multilevel factors that affect health in the community. 27 Such individuals therefore are well equipped to provide valuable insight into CHW recruiting strategies and hiring decisions.
The primary role of CHWs on CPHHD projects was to serve as a bridge between the community, health and social services, and researchers; however, they performed a multitude of job responsibilities across the 18 projects. The CHWs described in our study performed roles beyond those of the health promotion and disease prevention activities described in other studies. 10–14 For example, in addition to providing education and support and mobilizing communities, they were engaged as staff on the research team and were expected to assist in recruiting study participants, designing and implementing research interventions, and collecting data. Although survey responses indicated that no CHWs analyzed data, anecdotal evidence suggested that CHWs on one project did in fact contribute to interpreting qualitative data. The CHWs in a single study held numerous roles and multiple job titles. Many CHWs worked across 2 or more studies at a CPHHD, indicating the need for them to be quick learners, flexible, and simultaneously responsive to the evolving needs of the research project, the health system, and the community. The myriad job responsibilities held by CHWs may help explain the lack of consistency in functional and HR job titles, an issue documented in previous studies. 16,28,29
Several CPHHD projects had no minimum education requirement for CHW applicants. Furthermore, previous experience as a CHW or experience with research design or data collection activities were not viewed as priority attributes in the recruiting and hiring process. Instead, CHWs were often hired because of a combination of their knowledge of the host community, warm personality, and communication skills—qualities that enable CHWs to serve as ideal candidates to liaise effectively between researchers and communities. All CHWs on CPHHD research projects were offered monetary compensation for their work, as well as various benefits including health insurance and paid time off.
To integrate CHWs on the research team, most projects reported training the CHWs in research skills and basic computer skills important to optimizing their CPHHD project role. Our findings indicate that to prepare CHWs to meet the diverse demands of their work as members of health research teams, it may be necessary to provide ongoing training to develop and hone research-specific topics and skills, such as confidentiality (i.e., HIPAA), research methodology (i.e., data collection and analysis), and communication. Such training, combined with ongoing refresher courses in basic technology and communication, has the potential to complement the personal characteristics and skills CHWs bring to CPHHD projects, thereby enhancing their contributions to the research. Our findings suggest that regular face-to-face supervisory activities may also serve as an informal, reciprocal type of training in which CHWs and supervisors are invited to engage in dialogue about their experiences, ideas, and problem-solving strategies.
Limitations
This study had several limitations. Although they provide examples of experiences in a nationwide network, the CPHHD projects are not necessarily representative of all CHWs working on research projects in the United States; therefore, the results of this study may not be generalizable to the overall profession of CHWs in research. The CHW Working Group’s working definition of CHW may not align completely with other definitions.
A Web-based questionnaire is an efficient way to obtain information from a geographically dispersed group of respondents. However, the closed-ended nature of most of the questions may have limited our ability to fully characterize the diverse roles of CHWs on research projects.
Finally, information was obtained from project representatives who are familiar with CHWs on research projects. Information about roles and responsibilities provided by CHWs themselves would provide a complementary and potentially more detailed depiction of the work that these individuals performed in the 18 CPHHD research projects that constituted our sampling frame.
Conclusions
Our findings highlight the diversity of titles and roles that CHWs fulfill, as well as the community involvement in recruiting and hiring CHWs. Furthermore, our data emphasize the use of supervision strategies that included regular face time and continuous training to bolster adherence to the research protocol, communication, and basic computer skills. Standardizing the framework within which researchers and health teams recruit, hire, supervise, and train CHWs may facilitate the successful integration and acceptance of CHWs into health research teams. Future research is needed to examine the specific, project-tailored processes and training approaches that ensure improved health and social outcomes for communities targeted by projects that include the active participation of CHWs as staff.
The CPHHD investigators are leaders in NIH-funded community engagement research. Thus, their experiences may provide insight into the recruitment, hiring, and training of CHWs in community-engaged research projects. This information may help researchers conducting future studies involving CHWs as research staff. Characterizing CHWs and exploring the roles they fulfill in health disparities research on the basis of the experiences of a nationwide network such as the CPHHD program can provide useful information to other researchers, practitioners, and governmental agencies who seek to involve CHWs in similar capacities. Because CHWs served as critically important members of the CPHHD research projects, our experience suggests that there is national benefit in supporting greater efforts to recruit, retain, and support the work of CHWs in community engagement research.
ACKNOWLEDGMENTS
This project was supported by grants P50CA148143, P50CA105632, P50CA148596, P50HL105185, P50HL105188, P50CA106743, P50HL105184, and P50CA148110 from the National Cancer Institute (NCI), National Institutes of Health (NIH), and National Heart, Lung, and Blood Institute (NHLBI). The Web-based survey for this project was supported by the University of Washington Institute of Translational Health Sciences grant UL1TR000423 from the NIH, National Center for Research Resources (NCRR).
The authors would like to thank the project representatives at each of the Centers for Population Health and Health Disparities (CPHHDs), who provided their insight by responding to the survey; the CPHHD Community Health Workers Working Group members, who provided feedback on the survey instrument and article; Nanci Hemberger of The Scientific Consulting Group Inc, who provided invaluable organization and communication for the working group; and Joanne Brodsky, who copyedited the article. The authors would also like to thank Shioban Torres for her assistance on this article.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH, NCI, NHLBI, NCCR, the Fred Hutchinson Cancer Research Center, the University of Washington, The Ohio State University Comprehensive Cancer Center, the University of Illinois at Chicago, Johns Hopkins University, the University of California Los Angeles, University of North Carolina at Chapel Hill, Northeastern University, or the University of Massachusetts Lowell.
HUMAN PARTICIPANT PROTECTION
This study was approved by the CPHHD steering committee and the institutional review board of the Fred Hutchinson Cancer Research Center, the lead organization of this collaborative research study (institutional review board file 8228).
See also Landers and Levinson, p. 591 .

COMMENTS
Peretz PJ, Matiz LA, Findley S, Lizardo M, Evans D, McCord M. Community health workers as drivers of a successful community-based disease management initiative. Am J Public Health 2012;102:1443 ...
Community health workers (CHWs) have long been an essential component of the US public health workforce. 1,2 They effectively manage chronic disease, promote health, and facilitate access to health care, particularly with underserved populations. 2-4 In the last decade, the CHW workforce has expanded, in part because of the 2010 Affordable Care Act 5 and recognition of the CHW model as a ...
Overview. Community health workers (CHWs) are health care providers who live in the community they serve and receive lower levels of formal education and training than professional health care workers such as nurses and doctors. This human resource group has enormous potential to extend health care services to vulnerable populations, such as ...
1. Introduction. There is growing recognition of how community health workers (CHWs) make significant impacts on the health and wellbeing of individuals and communities most affected by inequities (1-8).The American Public Health Association (APHA) definition of a CHW, endorsed by the National Association of CHWs (NACHW), is "a frontline public health worker who is a trusted member of and ...
To provide guidance on their integration, we characterized roles and functions of community health workers in primary care through a literature review and synthesis. Analysis of 30 studies identified 12 functions (ie, care coordination, health coaching, social support, health assessment, resource linking, case management, medication management ...
Community health workers (CHWs) are an important cadre of the primary health care (PHC) workforce in many low- and middle-income countries (LMICs). The Philippines was an early adopter of the CHW model for the delivery of PHC, launching the Barangay (village) Health Worker (BHW) programme in the early 1980s, yet little is known about the factors that motivate and sustain BHWs' largely ...
Use of Community Health Workers in Community Health Centers, 2016-2018. 1 ). The rate of CHCs that employed any CHW rose from 20.04% in 2016 to 28.34% in 2018 (an average growth rate of 41%). Over the same time period, the average CHW FTEs employed in those CHCs were 3.32 (SD=4.33). Use of CHWs in CHCs, 2016-2018.
The use of participatory action research to design a patient-centered community health worker care transitions intervention. Healthc (Amst) . 2014 ;2(2):136-44.
There is growing interest globally in large-scale community health worker (CHW) programmes. This is based on the increasing evidence of their potential to (1) contribute towards attaining local, national, and global health goals, including universal health coverage, and to (2) tap into the one of the critical resources for improving health in low-income settings—the communities themselves [1 ...
Updated on: April 13, 2021. This infographic shows how Community Health Workers (CHWs) promote health equity and improve public health. The CHW workforce is diverse, growing, and drawing attention to its ability to address determinants of poor health. As trusted advocates, educators and counselors embedded in their communities, CHWs facilitate ...
Community health workers (CHWs) play a critical role in grassroots healthcare and are essential for achieving the health-related Sustainable Development Goals. While there is a critical shortage of essential health workers in low- and middle-income countries, WHO and international partners have reached a consensus on the need to expand and strengthen CHW programmes as a key element in ...
Keywords: community health workers, intervention research, participatory research, health intervention, academic-community partnerships. Citation: Coulter K, Ingram M, McClelland DJ and Lohr A (2020) Positionality of Community Health Workers on Health Intervention Research Teams: A Scoping Review. Front. Public Health 8:208. doi: 10.3389/fpubh ...
gap in health disparities. The number of research articles on the impact of CHW-led interventions and programs has escalated dramatically over the past fifty years, and the scientific rigor of study designs has improved notably. Figure 1. Number of studies on community health workers. 1964-1973 14 1994-2003 252 2014-2016 574
Community health workers (CHWs) are a key part of the health workforce, with particular importance for reaching the most marginalised. CHWs' contributions during pandemics have received growing attention, including for COVID-19. This paper contributes to learning about CHWs' experiences during COVID-19, based on evidence from India, Bangladesh, Pakistan, Sierra Leone, Kenya and Ethiopia.
Community health worker (CHW) programmes are again receiving more attention in global health, as reflected in important recent WHO guidance. However, there is a risk that current CHW programme efforts may result in disappointing performance if those promoting and delivering them fail to learn from past efforts. This is the first of a series of 11 articles for a supplement entitled "Community ...
This randomized clinical trial examines the effect of community health worker care on hospital readmissions within 30 days for adults enrolled in an ... Identifying the core elements of effective community health worker programs: a research agenda. Am J Public Health. 2012;102(9):1633-1637. doi: ...
Community health workers (CHWs) have worked in a variety of settings in the United States for more than 70 years and are increasingly recognized as an essential health workforce. CHWs share life experience with the people they serve and have firsthand knowledge of the causes and impacts of health inequity. They provide a critical link between ...
The Community Health Worker Research & Resource Center (CHW-RRC) is housed in the Department of Population Health and supported by NYU Langone's Community Service Plan. The CHW-RRC was launched in 2018 to create an organized approach to leveraging NYU Langone's extensive community health worker (CHW)-related knowledge and expertise to ...
THE SOUND SOLUTION. Community Health Impact Coalition is making professional community health workers (proCHWs) the norm worldwide. We create international guidelines. We increase global funding. And we win national policy. Indisputable evidence confirms that CHWs improve health outcomes—with considerable equity and economic dividends.
Among the many known outcomes of CHWs' service are the following: Improved access to health care services. Increased health and screening. Better understanding between community members and the health and social service system. Enhanced communication between community members and health providers. Increased use of health care services.
Montefiore-Einstein has worked with community health workers since the 1970s. And in various models 00;02;31;25 - 00;03;01;27 Renee Whiskey-LaLanne mostly in in part working with community-based organizations to employ community health workers and work in partnership with our system to serve our patients. But this institute is really a new ...
The primary objective of the study was to understand the unique perspectives of frontline community health workers (CHWs) to identify actionable barriers and facilitators that may impact representation of diverse groups in health research. Focus groups with CHWs were conducted followed by thematic analysis. Results revealed five main themes ...
Community Health Worker Research & Evaluation in Louisiana Ashley Wennerstrom, PhD, MPH February 20, 2024. CHW Definition • "A Community Health Worker (CHW) is a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the
Overview. A community health worker (CHW) is a frontline public health worker who lives in or is trusted by the community. A CHW connects people to health and social services by breaking down barriers related to the social determinants of health. The following audiences are most likely to find these resources useful:
The COVID-19 pandemic control strategies disrupted the smooth delivery of essential health services (EHS) globally. Limited evidence exists on the health systems lens approach to analyzing the challenges encountered in maintaining EHS during the COVID-19 pandemic. This study aimed to identify the health system challenges encountered and document the mitigation strategies and adaptations made ...
Ensure that community health and nutrition workers have supplies of the life-saving commodities they need under the One Plan, One Budget approach. ... Research Report: Impact of Climate Change on ...
Child, family, and school social workers 38,928 16.0% 84.0% Health care social workers 78,009 22.9% 77.1% Mental health social workers 23,121 19.2% 80.8% All other social workers 412,832 16.7% 83.3% . Health Care Diagnosing and Treating Practitioners . Occupation Total Count Male Female . Audiologists 19,480 16.1% 83.9%
The Coalition of Partnerships for UHC and Global Health urges Member States to support the resolution on social participation for universal health coverage and well-being at the 77th WHA and turn their commitments into tangible action. Authors: Svetlana Akselrod, Michael Adekunle Charles, Pamela Cipriano, Katie Dain, Rajat Khosla, Magda Robalo.
The new strategy, spanning from 2024 to 2028, aims to deepen engagement with country priorities, promote equity and enhance the utility of health policy and systems research globally. It was developed following extensive consultation with the health policy and systems research community. Aiming for impact: webinar recording.
Community health workers (CHWs), variously known as lay health workers, lay health advisors, health navigators, community educators, promotores, and other titles, are increasingly involved in intervention research studies and health care teams and have garnered growing national attention in recent years. 1-3 The US Department of Health and Human Services defines CHWs as