- Maps & Data
- Priority Populations
- Connect & Share
- COVID-19 Economy Education Environment Equity Food Health Housing Mental Health Transportation
- Suggest a Resource
- Help & Support

An Introduction to Community Health Needs Assessment (CHNA)
What is community health needs assessment.
Community health needs assessment (CHNA) is a process for determining the needs in a particular community or population through systematic, comprehensive data collection and analysis, and leveraging results to spur community change. CHNA has long been best practice within the field of public health and prompts those working to improve community health to consider local conditions—both community needs and assets--which lead to more targeted, effective community-change work.
CHNA involves exploring both quantitative and qualitative data and can be broad, examining a community at large, or it can focus on a specific issue. Many communities and community organizations regularly conduct broad CHNAs to understand their community and get a pulse of what is most needed to promote community thriving. Public health departments and nonprofit hospitals are required to complete regular CHNAs to fulfill government requirements (the Patient Protection and Affordable Care Act of 2010 (ACA) requires tax-exempt hospitals to conduct a CHNA every three years alongside stakeholders.) In addition, a community might perform a CHNA focused on a specific topic, like opioid and substance use disorders, to inform a grant application or strategic plan to decrease local rates of substance use and overdose.

Tool - Data/mapping Tool
Brought to you by ip3.

PLACES: Local Data for Better Health
Dataset - data/mapping tool, brought to you by cdc.

Community Health Needs Assessment
Topic - data & assessment.

CARES Engagement Network
Brought to you by cares.

From 500 Cities to data for all PLACES
Story - original, brought to you by community commons.

The Science of Thriving

Community Needs Assessment
Topic - possibilities, a holistic approach to chna.
CHNA is a common, widely-accepted practice within the fields of public health and health care, and the practice is applicable to any sector and/or initiative that seeks to advance equitable community well-being. Due to its widespread use by local public health agencies and organizations, as well as hospitals and hospital systems, there is potential to drastically improve the healthcare landscape and advance community well-being through improving the CHNA process. In recent years, many have advocated for the integration of more non-health data into CHNA (e.g. housing data, transportation data). Adoption of a more general, well-being frame alongside traditional health outcome data, acknowledges the interconnectedness of our physical health to the community conditions in which we live. Specifically, many have used the seven vital conditions for well-being framework to examine how the healthcare system can contribute to advancing community well-being outside of its traditionally clinical sphere.

Organizing Around Vital Conditions Moves The Social Determinants Agenda Into Wider Action
Brought to you by health affairs.

An Introduction to Data Equity

An Introduction to Data Frameworks

Seven Vital Conditions for Health and Well-Being
Advancing equity through chna.
While CHNA is a long-established process in the field of public health and other related fields, there are records of misusing CHNA results to further-marginalize communities of color, people with disabilities, LGBTQ+ groups, and other underserved populations. In order to advance equity through the CHNA process, we must approach CHNA in new, more inclusive ways. Careful conduction of CHNA that implements best practices (outlined below), including a community-driven process that engages people with lived experience in the community, can help identify root causes of inequity with regards to community conditions and health care, driving efforts to reverse these trends and improving health for all.
Vulnerable populations are at risk for disparate healthcare access and outcomes because of economic, cultural, racial, or health characteristics. For example, historically, communities of color have borne a larger burden of negative health outcomes than their white counterparts. There are myriad reasons for this, including a national legacy of systemic racism, disparities in health care access, coverage, and quality, and more. Throughout the CHNA process, examining data across different populations is important and allows you to see that people in your community have different lived experiences, resulting in different health risks and needs. If data cannot be broken out by race, for example, you’ll likely miss important differences in health needs across populations; your data won’t show health disparities. Knowing the specific health needs a population faces enables you to tailor health improvement efforts to appropriate priority populations and work to minimize disparities and promote an equitable approach to health improvement planning.

The Data Equity Framework
Brought to you by we all count.

An Introduction to the Burden of Disease Framework

An Introduction to Health Equity
Community engagement.
Ideally, CHNAs are developed through a collaborative process, involving stakeholders from various sectors, and take into consideration present-day data quantitative and qualitative data, as well as historical data, in order to examine change over time and trend lines. Community engagement can make the community a part of the CHNA process, rather than just the subject of it, and increases the likelihood that the CHNA will achieve its desired impact of building a healthier community and advancing equitable well-being.
Those who are closest to the problems we face have more knowledge about the nature of the problems and their root causes—often learning from those most affected leads to more effective, efficient, often multi-solving implementation strategies. Without community engagement, we fail to integrate the wisdom and experience of communities.

Focus Groups

Dialogue as a Process for Community Change

An Introduction to Local Data
Chna best practices .
CHNA is a complex process, often involving stakeholders from multiple sectors, organizations, and departments. There are many approaches to CHNA and an overwhelming amount of information available to guide the process. Our team has done research to discover and outline a list of best practices below.
Co-Design Processes and Solutions for Equitable Outcomes
Even before the CHNA work has begun, it's important to co-design the anticipated process with stakeholders and people in the community with lived experience. Co-designing processes ensures that people are on the same page at the onset of the work and should include designing processes for collecting, incorporating, and sharing data, as well as prioritizing areas for investment to advance equitable well-being. When more people are involved in designing a process for assessment and implementation planning, the work will take into consideration more lived experiences, and in turn, account for the needs of more people in a community.
Shift Power to Advance Shared Ownership, Action, and Wealth
Cultivating a culture of shared ownership of community well-being sets the stage for an effective community assessment—it's important that there is a shared definition of what well-being looks like in a given community. A culture of shared ownership around assessment and improvement planning includes community involvement and leadership with the design, data, processes, solutions, investments, and results.
Cultivate Shared Stewardship, Governance, and Investment for Accountability and Efficiency
Creating shared stewardship, governance, and investment is more than simply engaging the community—it means people feel invested enough in the process that they want to work together to enhance, maintain, and ensure the health of our systems. Together, shared ownership of community assessment, and co-designing of the process, pave the way for shared stewardship. Throughout the assessment, this includes data systems and implementation planning that is not top-down. In order to effectively advance equitable well-being, we must invoke reflective leadership, prioritize together, and collaborate to accomplish goals and act on priorities. Ideally, everyone who is part of a community has incentive to participate in bettering the community because they want to benefit themselves, and importantly, trust that everyone will reap the benefits (not just a subset of people).
Emphasize Assets and Strengths to Reinforce and Expand Community Resilience
Emphasizing community assets and strengths in assessment involves, first, deeply committing to the belief that communities (and their shared knowledge, cultures, and existing solutions) have immense value, and second, leading with that belief during every phase of community assessment.
Operationalize and Institutionalize Equity, Justice, and Accessibility for Mutual Liberation
Operationalizing and institutionalizing equity and justice in community assessment means that processes, activities, systems, assessment phases, and leading practices are rooted in and center equity actions , including antiracism, decolonization, accessibility, and justice. It's not always clear how to operationalize equity in community assessment—consistently reflecting on the process and questioning how we are considering and centering equity throughout each phase is helpful. Considering equity implications and operationalizing equity are not the same: at its core, equity means ensuring every person has the resources they need to produce outcomes and opportunities, and to build power. This demands proactive reinforcement of assessment and planning processes, practices, and mindsets that produce equitable power, access, opportunities, treatment, and outcomes for all.
Multi-Solve for Intergenerational Well-Being, Equity, and Sustainability
Multi-solving calls on systems stewards to work together and imagine solutions that efficiently and effectively solve complex systems challenges facing our communities. Multi-solving recognizes siloed solutions are ill equipped to solve problems at scale, and gains across multiple interrelated issues are possible. Solutions that are multi-solving in nature should be investment priorities--in that they are efficient and effective solutions for multiple, interrelated issues. Through collaboration we can identify and act on innovative, multi-solving solutions.
Foster Narrative Change to Move Hearts, Minds, and Systems
Narrative change is a tool for building public and political will to advance policy and systems transformation for health, well-being and equity. Public narrative is grounded in shared values, beliefs, norms, and assumptions that shape a collective worldview. Narrative is produced through stories that build on these commonalities, ultimately guiding behaviors and influencing how we co-create our destiny. Through narrative change strategies that use the power of story we can intentionally shift from harmful values, beliefs, norms and assumptions to those with the power to bridge divides, overcome impasses, and improve well-being and equity.
Infuse Belonging and Civic Muscle to Build Positive Community Momentum
Higher levels of social cohesion are associated with higher levels of trust, cooperation and social capital, providing the necessary foundations for creating healthy patterns for working together across groups and sectors, building the “civic infrastructure” for community members to co-create a shared future. These patterns can create a virtuous cycle—working together supports building stronger communication, develops a sense of connectedness and mutual obligation. As the sense of being valued and cared for within a community grows, people become more confident and willing to participate in the community, contributing to its vibrancy and affecting change.
CHNA to Catalyze Community Change
CHNA should catalyze community change, not just check a box—the most important consideration for CHNA is the action taken based on the results. Once you know where your community’s biggest assets lie and what the biggest needs are, you can use that information to create a plan and take action towards a healthier, more equitable community.
Data frameworks provide a powerful tool when using data to inform planning efforts to improve community conditions—they translate data into a solution through sorting indicators into categories that are easily tied to action. When examining data to inform an implementation plan, long lists of indicators aren’t helpful because they fail to shed light on levers you can actually pull to improve your community. Frameworks include categories that reflect common community programming, such as transportation, and housing, and thus make it easier to go from community insight to concerted action.
Stewardship, especially shared stewardship that engages people, organizations, local communities, etc., in collaborative work, is a promising mechanism by which we can shift investments and systems to support thriving communities. Stewardship is defined as “the careful and responsible management of something entrusted to one’s care” and is a good approach to acting on CHNA results to improve communities. Stewardship describes leaders—both people and organizations—who take responsibility for forming working relationships to drive transformative change in regions and communities. Importantly, stewards must have a vested interest in promoting an equity orientation in regard to purpose, power, and wealth.

5. Co-Design - Engaging People with Lived Experience
Tool - toolkit/toolbox, brought to you by 100mhl, published on 09/10/2020.

Belonging and Civic Muscle

Civic Infrastructure for Recovery
Story - written, brought to you by medium, published on 07/15/2021.

Changing Narratives and Moving Mindsets
Resource - website/webpage.

Bridge-Building and Power-Building: An Ecosystem Approach to Social Change
Brought to you by horizons project.

Listening to the Community's Input: A Guide to Primary Data Collection
Resource - guide/handbook, brought to you by walhdab.

Co-Design/Distributed Leadership Debrief Discussion Tool

An Introduction to Stewardship

Thriving Together: A Springboard for Equitable Recovery and Resilience in Communities Across America
related topics.

Item has been added to your favorites!
Community Health Assessments & Health Improvement Plans
What is a community health assessment, what is a community health improvement plan, why complete an assessment and improvement plan.
A community health assessment (sometimes called a CHA), also known as community health needs assessment (sometimes called a CHNA), refers to a state, tribal, local, or territorial health assessment that identifies key health needs and issues through systematic, comprehensive data collection and analysis. Community health assessments use such principles as
- Multisector collaborations that support shared ownership of all phases of community health improvement, including assessment, planning, investment, implementation, and evaluation
- Proactive, broad, and diverse community engagement to improve results
- A definition of community that encompasses both a significant enough area to allow for population-wide interventions and measurable results, and includes a targeted focus to address disparities among subpopulations
- Maximum transparency to improve community engagement and accountability
- Use of evidence-based interventions and encouragement of innovative practices with thorough evaluation
- Evaluation to inform a continuous improvement process
- Use of the highest quality data pooled from, and shared among, diverse public and private sources
From Principles to Consider for the Implementation of a Community Health Needs Assessment Process [PDF – 457KB] (June 2013), Sara Rosenbaum, JD, The George Washington University School of Public Health and Health Services, Department of Health Policy.
The Public Health Accreditation board defines community health assessment as a systematic examination of the health status indicators for a given population that is used to identify key problems and assets in a community. The ultimate goal of a community health assessment is to develop strategies to address the community’s health needs and identified issues. A variety of tools and processes may be used to conduct a community health assessment; the essential ingredients are community engagement and collaborative participation. — Turnock B. Public Health: What It Is and How It Works. Jones and Bartlett, 2009, as adapted in Public Health Accreditation Board Acronyms and Glossary of Terms Version 1.0 [PDF – 536KB] , July 2011.
The Catholic Health Association defines a community health needs assessment as a systematic process involving the community to identify and analyze community health needs and assets in order to prioritize these needs, and to plan and act upon unmet community health needs.” —Catholic Health Association, Guide to Assessing and Addressing Community Health Needs [PDF-1.5MB] , June 2013.
A community health improvement plan (or CHIP) is a long-term, systematic effort to address public health problems based on the results of community health assessment activities and the community health improvement process. A plan is typically updated every three to five years.
The Public Health Accreditation Board defines a community health improvement plan as a long-term, systematic effort to address public health problems on the basis of the results of community health assessment activities and the community health improvement process. This plan is used by health and other governmental education and human service agencies, in collaboration with community partners, to set priorities and coordinate and target resources. A community health improvement plan is critical for developing policies and defining actions to target efforts that promote health. It should define the vision for the health of the community through a collaborative process and should address the gamut of strengths, weaknesses, challenges, and opportunities that exist in the community to improve the health status of that community. — Public Health Accreditation Board Acronyms and Glossary of Terms Version 1.0 [PDF – 536KB] , July 2011, as adapted from Healthy People 2010 and CDC’s National Public Health Performance Standards Program .
A community health assessment gives organizations comprehensive information about the community’s current health status, needs, and issues. This information can help develop a community health improvement plan by justifying how and where resources should be allocated to best meet community needs.
Benefits include
- Improved organizational and community coordination and collaboration
- Increased knowledge about public health and the interconnectedness of activities
- Strengthened partnerships within state and local public health systems
- Identified strengths and weaknesses to address in quality improvement efforts
- Baselines on performance to use in preparing for accreditation
- Benchmarks for public health practice improvements
Links to nonfederal materials are provided as a public service and do not constitute an endorsement of the materials by CDC or the federal government, and none should be inferred. CDC is not responsible for the content of materials not generated by CDC.
To receive email updates about this page, enter your email address:
Related Links
Exit notification / disclaimer policy.
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
11.1 Health needs assessment
- Published: November 2021
- Cite Icon Cite
- Permissions Icon Permissions
This chapter begins with a consideration of the technical processes used for conducting health needs assessment. The relationship between health needs assessment and health economics is then examined and the philosophy of utilitarianism and its influence on health economics is explored. Cost utility analysis and its links to studies of quality of life are described and the important relationships between equity and efficiency are considered. The chapter then proceeds to explore the political and philosophical issues attaching to health needs assessment. This leads to an elaboration of the concept of justice derived from the work of Sen. Using ideas about the importance of human capabilities an argument is developed about the relational approach to understanding justice. The relational as against the individualistic position is found to provide a novel and useful way of describing health need and of attempting to meet that need. It also provides a set of precepts about the ways that services might be configured.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Health Needs Assessment
- First Online: 27 April 2016
Cite this chapter

- Patrick Tobi 3
4178 Accesses
Health needs assessment (HNA) is one of the approaches used to provide intelligence and inform decision-making on the planning and deploying of resources to address the health priorities of local populations. Need is an important concept in public health but is also a multifaceted one that represents different things to different people. From a public health perspective, need is seen as the ‘ability to benefit’, which means that there must be effective interventions available to meet the need. In present-day public health practice, assessing the health needs of local populations typically involves considering not just their physical and mental health and well-being, but the wider determinants or social factors, such as housing, employment and education that influence their health. This chapter describes the historic development of health needs assessment and its use in contemporary public health practice. The different ways in which need is perceived and their implications for the health service are discussed. A step-by-step guide through the HNA process is outlined and comparisons are made with other overlapping approaches to assessment. The practical challenges of carrying out HNAs are highlighted and case studies are used to illustrate real life experiences.
By the end of this chapter, you should be able to :
Discuss the concepts of need, want and demand.
Describe what is meant by a health needs assessment (HNA) and the different approaches that currently influence thinking and practice underpinning HNA.
Identify the key steps and practical challenges involved in conducting a HNA.
Compare HNA with other overlapping assessment approaches.
Understand, through case studies, how HNA is applied in practice.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bradshaw, J. R. (1972). The taxonomy of social need. In G. McLachlan (Ed.), Problems and progress in medical care . Oxford: Oxford University Press.
Google Scholar
Bradshaw, J. (1994). The conceptualisation and measurement of need: A social policy perspective. In J. Popay & G. Williams (Eds.), Researching the people’s health (pp. 45–57). London: Routledge.
Cavanagh, S., & Chadwick, K. (2005). Health needs assessment: A practical guide . London: National Institute for Health and Clinical Excellence.
Dahlgren, G., & Whitehead, M. (1991). Policies and strategies to promote social equity in health . Stockholm: Institute for Future Studies.
Department of Health. (2007). Guidance on joint strategic needs assessment . London: DoH.
Elkheir, R. (2007). Health needs assessment: A practical approach . Retrieved September 29, 2015, from http://www.sjph.net.sd/files/vol2i2p81-88.pdf.
Hooper, J., & Longworth, P. (2002). Health needs assessment workbook . London: Health Development Agency.
Powell, J. (2006). Health needs assessment: A systematic approach . London: National Library for Health.
Quigley, R., Cavanagh, S., Harrison, D., Taylor, L., & Pottle, M. (2005). Clarifying approaches to assessment: Health needs assessment, health impact assessment, integrated impact assessment, health equity audit, and race equality impact assessment . London: Health Development Agency.
Rogers, C., & Fox, R. (2005). Health needs assessment . Wales: National Public Health Service for Wales.
Stevens, A., & Gillam, S. (1998). Needs assessment: From theory to practice. British Medical Journal, 316 , 1448–1452.
Article CAS PubMed PubMed Central Google Scholar
Stevens, A., & Rafferty, J. (1994, 1997). Health care needs assessment: The epidemiologically based needs assessment reviews . Vol. 1 and 2. Oxford: Radcliffe Medical Press.
Stevens, A. J., & Rafferty, J. (1997). Health care needs assessment . Oxford: Radcliffe.
Stevens, A., Raftery, J., Mant, J., & Simpson, S. (2004). Health care needs assessment: The epidemiologically based needs assessment reviews (Vol. 1 and 2). Oxford: Radcliffe Medical Press.
Williams, R., & Wright, J. (1998). Epidemiological issues in health needs assessment. British Medical Journal, 316 , 1379–1382.
Wright, J. (2001). Assessing health needs. In D. Pencheon (Ed.), Oxford handbook of public health practice . Oxford: Oxford University Press.
Recommended Reading
Download references
Author information
Authors and affiliations.
Institute for Health and Human Development, University of East London, Water Lane, Stratford, UK
Patrick Tobi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Patrick Tobi .
Editor information
Editors and affiliations.
University of Bedfordshire, Luton, United Kingdom
Krishna Regmi
Liverpool John Moores University, Liverpool, United Kingdom
Rights and permissions
Reprints and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Tobi, P. (2016). Health Needs Assessment. In: Regmi, K., Gee, I. (eds) Public Health Intelligence. Springer, Cham. https://doi.org/10.1007/978-3-319-28326-5_9
Download citation
DOI : https://doi.org/10.1007/978-3-319-28326-5_9
Published : 27 April 2016
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-28324-1
Online ISBN : 978-3-319-28326-5
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Parenting, childcare and children's services
- Children's health and welfare
- Children's health
- Supporting public health: children, young people and families
- Public Health England
Population health needs assessment: a guide for 0 to 19 health visiting and school nursing services
Updated 19 May 2021
Applies to England

© Crown copyright 2021
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected] .
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at https://www.gov.uk/government/publications/commissioning-of-public-health-services-for-children/population-health-needs-assessment-a-guide-for-0-to-19-health-visiting-and-school-nursing-services
This guidance has been developed for health visitors, school nurses and their teams, though it may also be of use to other public health nurses. It aims to support them in their role assessing and prioritising local population health needs. Population health needs assessment is an element of the wider cycle to plan and deliver services at community and population level. It is the basis from which to continue planning, implementation, evaluation and dissemination phases to prioritise and deliver services to improve health and wellbeing outcomes.
Health visitors and school nurses have a substantial role in leading and coordinating delivery of public health interventions to address individual, community and population needs to improve health and wellbeing outcomes and reduce inequalities.
The focus is the population of children and young people that the health visitor and school nurse have responsibility for in a local community rather than assessment tools for individual children. A population may be a geographical area, school community, a specific group of children or young people, for example looked after children, young carers, or children who are asylum seekers or refugees.
It provides a framework for assessment, suggesting a range of practical steps to develop a profile of the health needs of the caseload or community that the health visitor and school nurse may be working with.
There are tools available to support health visitors and school nurses to deliver and evaluate, including the school nurse evaluation toolkit . The intention is to provide a simple approach to identifying and prioritising population health needs suggested through the commissioning for outcomes framework.
Improving health and wellbeing
A community-centred or place-based approach offers new opportunities to improve health and wellbeing outcomes, reduce health inequalities and develop local solutions that use all the assets and resources of an area. By integrating services, and building resilience in communities, individuals can take control of their health and wellbeing and have more influence on the factors that underpin good health.
This is illustrated through All Our Health , which demonstrates how improving outcomes is everyone’s business, working across settings such as community centres, green spaces and the workplace. Health visitors and school nurses are well placed to support families and communities to engage in this approach.
They have responsibility to lead, coordinate and provide services to the 0 to 19 years population. The High Impact Areas are those where the biggest difference can be made to children and young people’s health. This agenda is wide-ranging and public health challenges are increasing, health visitors and school nurses, with commissioners , make decisions about priorities and meeting local needs.
Health needs assessment is a way for health visitors and school nurses to gain a more in depth understanding of their communities and the needs that exist, enabling effective planning, prioritisation, development and delivery of services to improve outcomes for the population.
What is health needs assessment?
Health needs assessment is a systematic approach to understanding the needs of a population. The health needs assessment can be used as part of the commissioning process so that the most effective support for those in the greatest need can be planned and delivered. Responding to a health needs assessment provides an opportunity to improve outcomes where a population may be a group with a specific health need, school, cluster of schools, or a geographical community.
It is a holistic assessment considering social, economic, cultural and behavioural factors that influence health. In addition to readily available public health data, for example Child Health Profiles , a participatory approach should be adopted. It is important that the health visitor and school nurse recognise that there are different types of need, that some needs may be hidden and to make use of different perspectives.
Understanding the community, and the needs that exist, enables health visitors and school nurses to plan work to meet those needs, prioritise areas for service development, and determine any associated professional development required. Additionally, health needs assessment will enable teams and commissioners to work more closely together to ensure appropriate delivery. Health needs assessment should not be a one-off process but a continuous cycle to review the issues facing a population, leading to agreed priorities to improve health and reduce inequalities.
Planning for health needs assessment
Prior to starting the health needs assessment, it is important to have a clear understanding of the scope of the assessment. It is important to define the following:
- aims and objectives for the assessment – defining purpose and intended outcomes
- a target population to be assessed
- the data and information required
- a timeline for the health needs assessment – when, what, how and who. For example, for a health needs assessment of a school population, consider the school calendar for exam and revision periods
- potential challenges and how to manage them
- stakeholders who need to be involved, which may involve members of the health visiting team, school nurse team, key partners for example early years, schools, local authorities, voluntary, community and social enterprise ( VCSE ) sector
- resources required for example including IT equipment, room or space
- the strengths, limitations and opportunities of the health needs assessment
Other points to consider include:
- being clear on the intended outcome
- local or national priorities and issues of concern
- expectations of completing a population health needs assessment
- what is achievable within the resources available
- the boundaries and limitations of the health needs assessment
Stages of health needs assessment
There are 3 stages in health needs assessment:
- identifying need
- identifying assets
- determining priorities
Identifying health needs
The first stage of the health needs assessment involves gathering information and data. These sources will provide a breadth of perspectives on health and needs necessary for holistic assessment. The different sources of information help to define what influences the health needs as well as how many people are affected. When involving the children, young people and other key stakeholders, they will need to know why you are asking them to be involved, and to receive feedback on the results and outcome of the health needs assessment.
There is a wealth of quantitative data available to health visitors and school nurses about the health of the local population, which can be found in Child Health Profiles , that can be narrowed to the local area and compared to regional and national values.
Some example indicators are:
- children in poverty (under 16s)
- breast feeding
- immunisation uptake
- maternal mental health
- dental extractions
- family homelessness
- childhood obesity
- admission episodes for alcohol-specific conditions (under 18s)
- hospital admissions for asthma (under 19 years)
When the existing public health data is summarised in the health needs assessment report, consider the size and the severity of the issue, and how they relate to the High Impact Areas .
Every local authority publishes the latest statistics about the key issues affecting the health and wellbeing of their residents, including children and young people. The information, accessed through the local authority website, will include the Joint Strategic Needs Assessment (JSNA), ward profiles, the annual public health report or local authority school health profile.
Presentation in a spine chart format allows for easy comparison to England or regional benchmarks. This information can be accessed via the Public Health Outcomes Framework , the Overview of Child Health and Mortality Rankings web pages. Much of this information, which can be viewed by life course stage (for example school age children) or by theme (for example children and young people’s mental health and wellbeing). The findings should be summarised in a health needs assessment report.
Health visitor and school nurse knowledge and experience
Knowledge and experience of a locality are also an important data source. Health vistor and school nursing teams have rich knowledge and understanding about the communities that they work in and their experiences working with children and young people. This includes what is important to communities and issues affecting service provision and access.
Issues to consider include:
- any underlying local health and wellbeing issues
- current child health and school profiles
- any continually highlighted issues and the support evidence for them
- the top 5 health and wellbeing concerns and impact on local population
- whether these issues can be influenced
- the factors affecting health locally (positively or negatively)
- services that are currently being provided and how accessible they are
- how can children, young people and families be reached
Children, young people, carer and family views
It’s important to understand the experiences of the population themselves. Views and ideas about their health and influencing factors such as lifestyles and experiences of services may differ to those of professionals and other stakeholders and are a vital component of health needs assessment.
Consideration should be given to how to include the views of people who may be underserved and whose voices are often not heard. These groups may include looked after children, young carers, families from black and minority ethnic communities, families of asylum seekers, and lone parents. In addition, there are individuals or groups (for example early years, maternity voices, school council, year group, class of pupils, existing service users, and youth clubs and local authority youth councils) who may contribute to the heath needs assessment and should be identified.
There are a variety of methods for involvement. Plans should consider the time available and the skills needed by staff for some methods. The activity chosen will depend on the group, for example, the age of the children. Through these activities, it’s possible to work with stakeholders to explore local understanding of health issues, the issues that are important to the population, the impact and changeability of these issues, and the quality of services currently delivered. The results should also be summarised in the health needs assessment report.
Methods for population involvement
Informal discussion group (focus group).
- Optimum focus group size is 8 to 12 participants
- Outline questions should be devised in advance
- Facilitator introduces topics for discussion
- Findings should be audio recorded and transcribed, or notes taken (preferably by another facilitator)
- A variety of groups may be needed for a wide range of views
Individual interview (semi-structured)
- Findings may be audio recorded and transcribed, or notes taken
Questionnaire
- Questionnaire can be paper-based or online
- An existing questionnaire should be used or adapted where available, for example WHO Global School-based Student Health Survey and Health Behaviour of School aged Children
- If a new questionnaire or survey is developed, this should be piloted first
Talking wall
- Interactive group discussion with individuals recording their comments
- Flip chart displayed on wall with topic headings; individuals add post-it note with their comments
- Online recording methods are available (for example Mentimeter )
- Suggestion boxes, You’re Welcome criteria , NHS Friends and Family test , complaints or compliments and local service audits
- Mentimeter : a free interactive voting tool, which can display real-time responses including text comments
Other stakeholders
It’s important to gather further intelligence on population needs from other professionals working locally who have knowledge of the area. Pooling this knowledge can support the identification of health and social problems that affect the population group and provide information about uptake of services.
This may include teachers, school governors, education welfare officers, commissioners, early year’s practitioners, community leaders, youth groups, the police, community groups, social workers or elected members. Commissioners are a strategic stakeholder and will be a key partner once the health needs are prioritised and the action plan is being prepared for the target population, such as the school or community. Following the school nurse health needs assessment, the commissioners may consider making changes to the services commissioned locally. The same methods for involvement used with the population can be used to engage stakeholders. The findings should be summarised in the health needs assessment report.
Apart from ensuring that the health needs assessment captures information from different perspectives, engaging others in the process helps to strengthen networks and, during the process, solutions to some of the issues may be suggested by others. It is important to make a note of these.
Identifying assets
Identifying assets is an important part of the health needs assessment to ensure the views, perceptions and experiences of children, young people and local communities are captured. Other stakeholders will also have perspectives, for example residents’ or voluntary sector partners’ views on the strengths and assets in a locality. This will support the development of solutions to meet the needs of the population.
To identify what enablers of health exist, consider:
- the strengths and resources locally
- services available, for example, mental health services and sexual health services
- any early years opportunities
- any school-based opportunities
- the skills and expertise in the health visiting and school nursing service
- who else is available to support health needs, for example, community leaders
- local community groups, for example, youth groups, voluntary, community and social enterprises
- community facilities, for example, sports, leisure facilities and community pharmacies
Determining priorities
The different needs and findings should be determined and defined. This could include linking them to poor health indicators locally and to local policies . The identified needs can then be compared using an agreed process, where possible involving stakeholders, parents, children and young people, to determine 2 to 3 priorities.
The health visitor and school nurse should consider the following factors, whichever method is used to prioritise need:
- impact – the severity and size of the issue
- changeability – the realistic chance of achieving change
- acceptability – acceptable solutions available
- feasibility – resource implications of solutions are feasible
See Taxonomy of social need (Bradshaw 1972) .
Several simple methods can enable health visitors and school nurses to prioritise the most important health needs and are presented below.
If each method used produces a different order of priorities, it is important to give a rationale in the final health needs assessment report for the final priority list of needs. For example, this could include a list that supports a key local public health priority or national policy may be more successful in attracting funding from the local commissioner. Engaging commissioners in considerations will support the prioritisation of joint needs.
Forced ranking
In this simple method, each person or group of people rank every health need on a scale of importance. Overall ranking scores for each need are combined to identify the order of priority. This approach produces a priority list based on the experience of the individuals taking part.
Instructions for the process are as follows:
- if 5 health needs are identified, the most important need is allocated a ‘1’, the second most important is ranked ‘2’ and subsequently follows on to the least important need, which will be ‘5’
- when the ranking process has been repeated by each person or group, the ranking scores are added together to provide a total score for each health need. The lowest score has the highest priority and follows on until all needs have been ranked
An example:
This example indicates that mental health is the highest priority need as it has received the lowest score overall, followed by obesity and then alcohol.
Strategy grid
Prioritising needs using the strategy grid method places the focus on addressing needs within the resources available. Strategy grids provide a way of thinking about problems so that the greatest results can be achieved with limited resources.
Instructions for the process are as follows.
- Identify 2 criteria to prioritise need, which should be relevant to health visiting or school nursing. The example below uses impact and feasibility, but other examples may be ‘need and impact’, ‘importance and changeability’ or ‘impact and cost’
- Set up a grid with 4 boxes and allocate one criteria to each axis. Create arrows on the axes to indicate ‘high’ or ‘low’, as shown in the example below.
- Place needs in the appropriate box based on the criteria. The needs have been prioritised as:
- High impact and High feasibility – these are the highest priority needs and require resources and input to address and improve health outcomes
- Low impact and High feasibility – politically important, interventions for these needs can be redesigned to reduce investment and maintain outcomes
- High impact and Low feasibility – these needs often require long-term investment and creative solutions. Too many can be overwhelming. These needs may require breaking down into smaller component parts.
- Low impact and Low feasibility – these are low priority needs. Interventions provide minimal return on investment, so resources should be reallocated to high priority needs.
Priority grid
This is another grid method that scores health needs against a series of locally identified questions.
Enter the issues into the grid and allocate a mark based on the scoring mechanism identified. Scores are totalled to identify 2 to 3 priority needs to be addressed. The remaining needs can be tackled by others or managed later.
Download an example of a priority grid.
Nominal group technique
The nominal group technique supports the involvement of stakeholders by prioritising a wide number of needs in a short time. It encourages debate and quick decisions. It is a democratic process where stakeholders have an equal say regardless of seniority or background. This can be done with everyone together in a room at the same time, or the first 2 stages can be completed remotely.
The first task is to establish a group structure. This part of the process involves gathering a group of 8 to 10 people to participate including health visitors or school nurses, children or young people, or others. The group objective is to prioritise health needs.
Once the group is established, the health visitor or school nurse provides identified health needs and allows the participants to silently record their top 5 potential priorities and rationale for selection. A group meeting follows to share and record all potential priority needs.
The recorded list is then simplified by grouping similar needs or priorities together. The moderator reads out the priorities and participants feedback on how to group them together. Any suggestions that are unclear can be clarified. The moderator then facilitates a group discussion about the potential priorities, the importance of each and interventions.
Participants can then silently and anonymously rank each listed health need on a scale from 1 to 5, where 1 is the highest priority and 5 is the lowest. The moderator collects the results and calculates the total score for each health need. Those with no score are rejected. Of the remainder, the need with the lowest score is the highest priority need, and that with the highest score is the lowest priority need, with the rest on a sliding scale in between. If the list results in tied scores or the results need to be narrowed, the process can be repeated.
Presenting the results of the health needs assessment is an important stage in moving to action planning for change. The findings should be shared with all who participated in the process along with other stakeholders such as the wider health visiting, school nurse team, managers and commissioners. The report should be concise, accessible, informative and tailored to the intended audience.
Reporting will vary depending on the audience but consideration should be given to:
- an executive summary giving the population health needs assessment background, summary of needs assessment methodology and summary of prioritised needs
- an introduction setting out the purpose of the health needs assessment, description of practice area or school nurse service and description of the community or population
- the method for data collection, prioritisation strategy and who was involved
- findings of needs review including data, views from health visiting and school nursing service, population and other stakeholders
- findings of the assets review and details of health resources available
- results of the prioritisation stage and the priority needs determined
- analysis to include making the case for addressing priorities, why these are important and the impact if they were addressed
- actions and next steps, including who will be involved in planning the interventions to address the priorities
- conclusion to restate your key points and link to evidence with a case for change
- acknowledgements: include stakeholders who had an input
The final stage of the health needs assessment process involves reflection. This is a vital part of the process if health needs assessment is to continue to be a relevant and effective tool in improving health and tackling health inequalities. Evaluation of the assessment process should consider:
- whether the objectives set at the start of the health needs assessment process were met
- was the range of stakeholders diverse and involved
- have the findings of the health needs assessment been shared
- what impact will the health needs assessment report have
- who is going to be involved in responding to the health needs assessment – for example in planning changes or a new intervention
- how will the local assets be incorporated into future work
- what opportunities were identified in this process
- were the barriers and limitations, identified at the start of the process, successfully overcome
The next stage is planning the interventions and changes that will be implemented as a result of the health needs assessment. This next stage is beyond the scope of this guidance, however, a useful guide for changing and improving services is the Plan, Do, Study, Act cycle.
Health visitors and school nurses are leaders of the Healthy Child Programme (0 to 19) and in improving health outcomes and reducing inequalities for children and young people. It is important to allocate resources according to need and where maximum impact can be achieved. This guidance provides health visitors and school nurses with the means to assess the priority health needs for their defined population. From this position, effective planning, development and delivery of services to improve outcomes for the population can be undertaken.
Acknowledgements
This guidance has been developed with our key partner, Liverpool John Moores University.
Gill Turner is Senior Lecturer and Programme Leader for Specialist Community Public Health Nursing at Liverpool John Moores University. Gill is a school nurse with an interest in healthy weight. She has written on contemporary school nursing issues.
Dr Sean Mackay is the Programme Lead for Primary Care and Advanced Practice at the School of Nursing and Allied Health at Liverpool John Moores University. He is a health visitor with a research interest in fatherhood and has written on evidence-based health promotion.
Tasneem Patel is Research Assistant at Liverpool John Moores University.
Is this page useful?
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
- School of Public Health
- Research Methods
Needs Assessment and Evaluation

- Dr. Ashenafi S Cherkos
- Dr. Stacey Griner
- Dr. Erika Thompson
Aiken, J.A., & Griner, S.B. (2021). Health associations for male survivors of unwanted and non-consensual sex. Journal of Interpersonal Violence. doi.org/10.1177/08862605211042806
Griner, S.B., Vamos, C.A., Phillips, A.C., Puccio, J.A., Thompson, E.L., & Daley, E.M. (2021). Assessing college students’ interest in university-based oral health information and services. Journal of American College Health, 12, 1-5. tandfonline.com/doi/full/10.1080/07448481.2021.1876706
Thompson, E.L., Garg, A., Collier Esser, K., Caddy, D., Matthes, S., Rohr, D., & Spence, E.E. (2021). Development and validation of a child physical and sexual abuse prevention scale. American Journal of Health Behavior, 45 (5), 947-955.
Thompson, E.L., Fulda, K.G., Grace, J., Galvin, A.M., & Spence, E.E. (2021). The implementation of an interpersonal violence screening program in primary care settings: Lessons learned. Health Promotion Practice, [Epub ahead of print]. doi: 10.1177/1524839921989273
Thompson, E.L., Zhou, Z., Garg, A., Rohr, D., Ajoku, B., & Spence, E.E. (2021). Evaluation of a school-based child physical and sexual abuse prevention program. Health Education and Behavior, [Epub ahead of print]. doi: 10.1177/1090198120988252.
Vamos, C.A., Puccio, J., Griner, S.B., Logan, R., Piepenbrink, R., Richardson, M., Lovett, S., Mahony, H., & Daley, E. (2022). Health literacy needs and preferences for a technology-based intervention to improve college students’ sexual and reproductive health. Journal of American College Health . doi.org/10.1080/07448481.2022.2040517
This page was last modified on March 5, 2024

Quick links
- Alumni Relations
- Media Contact
- Accessibility Statement
- Accreditation Summary
- Bondholder Information
- Careers at HSC
- HSC Trust Line
- Mental Health Services
- Minors on Campus
- Notice of Nondiscrimination
- Privacy Policy
- Report Behavioral Misconduct
- Report Fraud, Waste or Abuse
- Report Sexual Misconduct, Intimate Partner Violence and Stalking
- Texas Veterans Portal
Connect with us
- 3500 Camp Bowie Blvd.
- Fort Worth, Texas, 76107
- (817) 735-2000
Social media

- Student Life
- Patient Care
- After-Action Review
- Continuing studies
- COVID-19 information
- Student services
- MyU : For Students, Faculty, and Staff
National Resource Center for Refugees, Immigrants, and Migrants (NRC-RIM)
Health Needs Assessment (HNA) Toolkit

Providing timely and appropriate support
Over 75,000 of the Afghans who were displaced when the Taliban took control of Kabul were resettled in the United States through Operation Allies Welcome (OAW) Response. OAW was organized in 2021 as a coordinated effort across federal government offices, national non-profit organizations, state and local resettlement agencies, private businesses, and other stakeholders to resettle and support Afghan newcomers. As Afghans arrive in the United States, resettlement agencies, federal partners, healthcare systems, public health professionals, social service providers, and community-based organizations need to collaborate to provide timely and appropriate support. Conducting a health needs assessment is an important first step in designing and implementing public health interventions.
What is a Health Needs Assessment?
A health needs assessment is a systematic process of collecting, analyzing, and using information to identify the health needs and priorities of a specific population or community. The goal is to identify gaps in health services, resources and health outcomes, and use the information to plan and implement programs and services to increase health equity and improve the overall health and well-being of the community. It typically involves gathering data on knowledge, attitudes, health behaviors, demographics, health status, access to care, and other factors, and using this information to identify health priorities and develop a plan to address them.
Purpose of Conducting a Health Needs Assessment
- Identify the health problems and priorities of a community, including any disparities and inequities in health outcomes.
- Assess the existing health system, including health infrastructure, resources, and capacity, to determine if it can meet the health needs of the community.
- Guide the allocation of resources and the design of health interventions that are tailored to the specific needs and context of the community.
- Evaluate the effectiveness of health interventions and track progress over time.
+ Surveys and Questionnaires
Surveys and questionnaires are standardized tools used to collect information about the health needs and behaviors of a community. They often include closed-ended questions that can be analyzed quantitatively.
+ Focus Group Discussions
Focus group discussions involve a small group of individuals who share their opinions and experiences on a specific health issue. This method allows for in-depth exploration of a particular topic and provides rich qualitative data.
+ Key Informant Interviews
Key informant interviews involve talking with individuals who have expert knowledge or experience with a particular health issue or community. These interviews provide valuable insights into local health needs and issues.
+ Medical and Health Records Review
Reviewing medical and health records can provide insight into the health status and needs of a particular community. This method can also help identify gaps in care and areas for improvement.
+ Direct Observation and Physical Examination
Direct observation and physical examination involve observing and assessing individuals or communities for signs of illness or disease. This method can provide valuable information about the health status of a community and identify health needs.
+ Community Mapping and Participatory Approaches
Community mapping and participatory approaches involve working with community members to identify local health needs and resources. This method can promote community engagement and ownership of health initiatives. It can also help identify barriers to accessing care and opportunities for community-based interventions.
Identify the community to be assessed.
Gather data on the community's health status, behaviors, and needs.
Analyze the data to identify priority health issues.
Involve the community in the assessment process.
Develop and Implement
Develop and implement a plan to address the identified health needs.
Evaluate the effectiveness of the plan and make necessary adjustments.
Best Practices for Conducting a Health Needs Assessment Among RIM Communities
This guide offers tips and reminders on what to remember or avoid when conducting an HNA among RIM communities. It emphasizes the importance of a community-driven approach and a thorough understanding a community's health needs to effectively address health disparities and promote health equity.
Download now >>
Health Needs Assessment Question Checklist
This checklist provides questions for service providers to use as a guide when conducting health needs assessments among RIM communities. Included are examples that showcase the varied ways that organizations can use HNAs to achieve their own program goals.
Promising Practice: Sexual and Reproductive Health Needs Assessments
Discover how Health Needs Assessments (HNAs) are addressing the unique healthcare challenges faced by Afghan women in the U.S. Learn about tailored interventions and impactful findings to enhance healthcare accessibility and cultural sensitivity.
Learn More >>
Assessing Afghan Newcomer's Health Needs: A Home Visit Guide
This guidance document aims to assist Health Navigators, Community Health Workers, or other service providers in conducting an individualized health needs assessment with Afghan newcomers during a home visit to gauge Afghan clients' immediate healthcare needs and their understanding of navigating the U.S. healthcare system.
Download Now >>
Individualized Health Needs Assessment for Afghan Newcomers
The Afghan Newcomers Individual Health Needs Assessment Form is a comprehensive tool designed to identify the unique health requirements of individuals migrating from Afghanistan to their new community. This fillable form aims to gather essential information to ensure that newcomers receive appropriate healthcare support and access to available resources.
In-Home Health And Safety Checklist
This checklist, which focuses mostly on safety concerns inside of the home, is based on a survey of providers’ experiences. It can be a useful reference during meetings or home visits with clients.
Download Now >>
Example 1: IRC Atlanta
- Purpose : HNA used by IRC Atlanta for determining both gaps in knowledge around U.S. healthcare and gaps in health services needed by the client after the first 90 days in the U.S.
- Assessment Type : Questionnaire
- Implementation : This HNA guiding document is used by IRC Atlanta’s bilingual community health workers (CHWs) during home health visits with Afghan clients. In these home health visits, the CHW visits the client(s) in their home at a time that is most convenient for the client(s). After conducting the HNA, the CHW will refer the client(s) to the necessary health services that are needed (e.g., dental care, mental health, specialty care, etc.)
Below are examples of HNAs that were created by two IRC offices, IRC Atlanta and IRC Salt Lake City. These two examples showcase the varied ways that organizations can use HNAs to achieve their program goals.


Example 2: IRC Salt Lake City
- Purpose : HNA used by IRC Salt Lake City for determining community needs around Afghan women’s health.
- Assessment Type : Survey with facilitator scripts and notes
- Implementation : This sample includes a call script to introduce the HNA and recruit participants, notes to help guide facilitators in each section of the HNA, and different questions around women’s health topics, including health access, maternal health and family planning, preventative gynecological health, sexual and reproductive health rights, gender equity, etc. The HNA was created in collaboration with members of the Afghan community.
- More information: Download the Slides | Promising Practice
- Our Partners
- Community Leadership Board
- Guiding Principles
- Our Publications
- On the Ground
- Translation Process
- Technical Assistance
- RIM Communities
- Newsletter Sign Up
- Case Investigation + Contact Tracing
- Clinicians' Corner
- Communications
- Community Engagement
- Community Health Workers
- Employer Engagement
- Healthy Spaces Toolkit
- Partnerships
- View All Resources
- On-Demand Training
- About Afghan New Arrivals
- Promising Practices
- Mental Health and Stress
- Women's Wellness
- Respiratory Illnesses
- Wildfire Smoke
- Lead Poisoning
- Sexual and Reproductive Health
- Summer Safety
- Hurricane Readiness
- Health Needs Assessments
- Healthcare Navigation
- Mental Health
- Curated Health Resources
- Settle In for Afghans
- Virtual Resettlement Line
- Public Health Initiatives
- Health Benefits and Requirements
- COVID-19 Resources for Ukrainians
- Ukrainian Community Engagement
- Community Mapping
- Settle In for Ukrainians
- Fact Sheets
- Social Media
- Conversation Guides
- Vaccine Central
- For Newcomers
- Public Health Emergency
- Vaccines for Children
- Vaccines and Ramadan
- All Vaccine Translations
- Health & Wellness Health & Wellness
- Who We Are Who We Are
- Commitments & Impact Commitments & Impact
- Health & Wellness Health & Wellness Our care Health research Climate events & health Recipes Health tips
- Who We Are Who We Are Our mission Fast facts Our history Our people Leadership team Permanente Medicine Annual reports Risant Health
- Commitments & Impact Commitments & Impact Healthy communities Equity, inclusion, & diversity Public policy
- Our care Health research Climate events & health Recipes Health tips
- Our mission Fast facts Our history Our people Leadership team Permanente Medicine Annual reports Risant Health
- Healthy communities Equity, inclusion, & diversity Public policy
Community Health Needs Assessments
In this section.
- About community health
- Community Health Needs Assessments Charitable contributions
- Our focus and impact
- Increasing health access
- Building healthier communities
- Communities we serve
2022 Community Health Needs Assessments and Implementation Strategies
Every 3 years, Kaiser Permanente conducts Community Health Needs Assessments, which guide and inform Kaiser Permanente’s investments and business decisions. They are a critical tool for identifying and measuring community needs and assets, which lets us better tailor our engagement with communities and use our organizational resources to further community health at every opportunity.
The Community Health Needs Assessments and development of Implementation Strategies are driven by a commitment to improving health equity and are intended to be transparent, rigorous, and collaborative. The CHNA use local data, information from the Community Health Data Platform , and input from the community to help us understand our communities’ needs and the best way to respond to them. The CHNA also provide information and data on how social drivers of health — including financial opportunity, income and employment, housing, food, and transportation — affect communities.
Kaiser Permanente developed the accompanying Implementation Strategy reports, which demonstrate how Kaiser Permanente will respond to the health needs identified by the CHNA.
We welcome feedback on these assessments. For more information or to provide feedback on any of the CHNA reports, please email [email protected] .
Northern California
Southern california, the mid-atlantic states, the northwest.
View past Community Health Needs Assessments and Implementation Strategy reports.
News and views from one of America’s leading health care providers and not-for-profit health plans.
On this site.

Health Needs Assessment

When you think about the word health, you may probably be thinking about healthy meals, healthy living, and any other way to make you stay healthy , especially in times like these. A lot of people would find it difficult to stay healthy or at least to remain healthy. There are those who are fortunate to find ways, while there are others who may not be as fortunate. The same goes as there are others who are able to afford the lifestyle, while others, not so much. It goes without saying, finding a good way to keep your health as a number one priority should also be for everyone especially those in communities that are not as privileged as others.
Of course, you may not immediately be able to tell which community or family or anyone in public may need all the help they would need. This is why making a health needs assessment can help you . It helps you by giving a complete list of the things that you can do to make your health needs assessment successful. For more ideas on what you can do with a health needs assessment, you should take a look at these 10+ examples of health needs assessment now.
10+ Health Needs Assessment Examples
1. community health needs assessment.
Size: 268 KB
2. Health Needs Assessment Template
Size: 90 KB
3. Health Needs Assessment Form
Size: 44 KB
4. Basic Health Needs Assessment
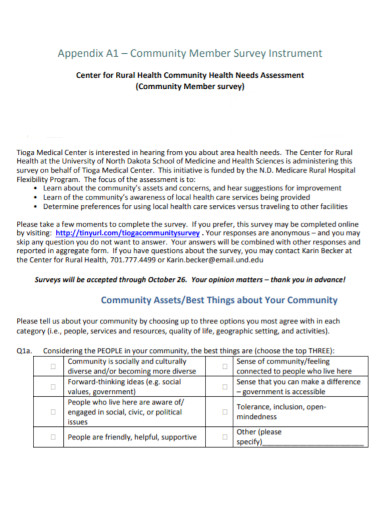
5. Public Health Needs Assessment
Size: 582 KB
6. Population Needs Assessment for Health
Size: 86 KB
7. Health Needs Assessment Report
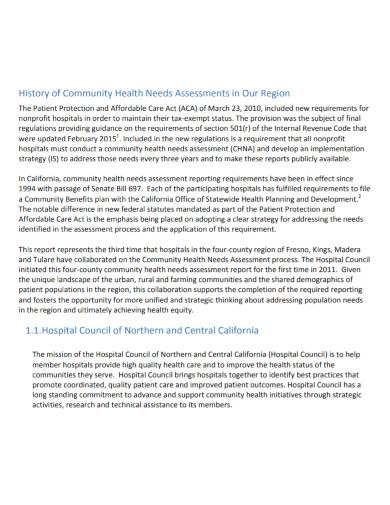
8. Rural Health Needs Assessment
9. Health Needs Assessment Questionnaire
Size: 338 KB
10. Health Care Needs Assessment
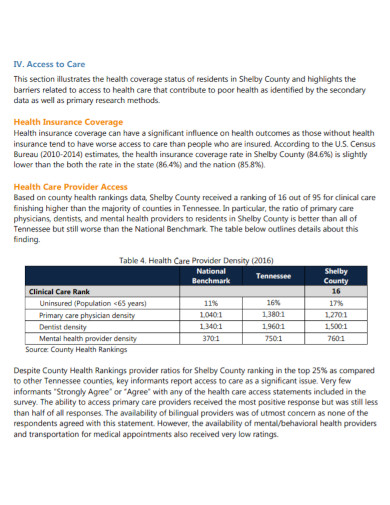
Size: 473 KB
11. Standard Health Needs Assessment
What Is a Health Needs Assessment?
A health needs assessment is a method used by nongovernment organizations in order to check, review, assess, analyze and evaluate a community’s health needs, the public’s health needs, or even a specific family’s health needs. This assessment consists of a series of questions in the form of a checklist . The assessment is given to the community or the head of the community in order to know how bad or how severe the problem is with regard to the overall health of the people living.
In order to be able to get the right type of information about a community, a family, or the general public, organizations use the health needs assessment to aid them through that. Basically, the general purpose of a health needs assessment is to give the estimated number of people whose illnesses or diseases may not be addressed due to the fact that it is not as well known or there are no correct medications for them. For that to stop, the health needs assessment comes to play.
How Do You Write a Health Needs Assessment?
There are a lot of ways to write a health needs assessment. This of course would depend on the target or the aim of your health needs assessment. If you are aiming for a community health needs assessment, a family health needs, or even a public one, they are all the same except for some other specific things.
1. Gather Your Information for the Assessment
Information for the assessment means that you must at least know what you are planning to do, what you are going to be doing, and how you are going to do that. Since you are going to be doing a health needs assessment in a community, at least find out more about the place first. This does not necessarily mean that you should not be thinking about the risks, but you should at least have some idea as to how to approach this situation.
2. Make the Assessment Something Specific
Match your assessment to something specific as possible. That way, it would be easier for you to conclude the entire assessment and the entire result of the assessment later. It is also going to be easier for you to gather the right materials to help out with the health needs of the community. However, if you think that a general assessment is a better and safer way to conduct it, you may do so as well as long as you are able to hit the target reason for using the needs assessment.
3. Aim the Assessment for Something Good
When making your assessments, always aim for the good parts. Of course, there are certain circumstances that may make you think that the needs assessment has to be aimed in a different way; however, as much as possible, aim it at the goal you have made in order for the assessment to be complete.
4. Analyze the Total Answers to the Assessment
The total percentage of their answers is what you are going to be basing on your future needs assessment. The percentage helps you find the right health needs assessment answers. It also helps you figure out which type of needs assessment they should have and what type of help they should also be getting.
What is a health needs assessment?
A health needs assessment is a kind of documented checklist that ensures the people who may be a target for this to have the correct and right health needs that they can get.
Who benefits from the results of the assessment?
The people who took the time to fill out the assessment would benefit from the results. The results help those organizations know what can be done in order to make it better for those affected.
How can the health needs assessment work for a community?
The health needs assessment helps by assessing the needs of the people in a community.
It goes without saying making a health needs assessment is necessary. It helps you find the general issue that could be used as a way to help you find the correct needs for that issue. It helps you understand the correct needs of a community, of a family, or of the general public.
AI Generator
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting
Needs assessment
On this page, how can i apply for a needs assessment, how long will i have to wait for a needs assessment, is there a time limit on the validity of my needs assessment, interrai assessment process.
Every person who wishes to receive disability support services funded by a Health District must be needs assessed by the NASC. The information from the assessment is then used to determine the level of need the person has – very low, low, medium, high or very high.
The criteria for residential care entry is that the person has been assessed as having high or very high needs which are indefinite and cannot be safely met with a package of care in the community.
Find your local NASC on the Needs Assessment and Service Co-ordination Association website.
Any person can apply for a needs assessment, either in person or by referral from any other person, such as a general practitioner. The contact details for a local needs assessment and service coordination service are available by clicking on the following link, contacting the local Health District. If a person is living in the community and requires support, they should apply as soon as possible for a needs assessment by a NASC. The person may be eligible for health and disability support services that help them to maintain their independence at home. If a person receiving a support services package is unable to live safely in the community, and is re-assessed as requiring a high or very high level of care, then long-term residential care is available. If a person is currently living in the community, and their health circumstances have changed they are able to apply for a re-assessment of their needs. If a person is currently living in a residential care facility but has not been officially needs assessed by the NASC and wishes to apply for a needs assessment, then the person should apply for a needs assessment as soon as possible. This first step is necessary before the person applies for a financial means assessment to determine if they are eligible for government funding (the residential-care subsidy).
Go to Residential care questions and answers for more information.
The NASC should contact the referred person within two days of receiving a referral. A completed needs assessment application should be processed within 20 working days, but it may take longer depending on the demands on the assessment service.
There is no time limit on the validity of your needs assessment. You might need a reassessment if there has been a significant change to your needs or circumstances that means your existing support plan doesn't work for you any more.
Part 1. Overview Information
National Institutes of Health ( NIH )
National Heart, Lung, and Blood Institute ( NHLBI )
National Institute on Aging ( NIA )
National Institute on Alcohol Abuse and Alcoholism ( NIAAA )
National Institute of Allergy and Infectious Diseases ( NIAID )
National Institute of Arthritis and Musculoskeletal and Skin Diseases ( NIAMS )
February 14, 2024 - Participation Added ( N0T-HD-24-007 ) Eunice Kennedy Shriver National Institute of Child and Human Development ( NICHD )
National Institute on Deafness and Other Communication Disorders ( NIDCD )
National Institute of Dental and Craniofacial Research ( NIDCR )
National Institute on Drug Abuse ( NIDA )
National Institute of Environmental Health Sciences ( NIEHS )
National Institute of General Medical Sciences ( NIGMS )
National Institute of Mental Health ( NIMH )
National Institute of Nursing Research ( NINR )
National Center for Advancing Translational Sciences ( NCATS )
National Center of Complementary and Integrative Health ( NCCIH )
All applications to this funding opportunity announcement should fall within the mission of the Institutes/Centers. The following NIH Offices may co-fund applications assigned to those Institutes/Centers.
Division of Program Coordination, Planning and Strategic Initiatives, Office of Disease Prevention ( ODP )
Office of Research on Women's Health ( ORWH )
UC2 High Impact Research and Research Infrastructure Cooperative Agreement Programs
- March 20, 2024 - Notice of Informational Webinar for PAR-23-144, STrengthening Research Opportunities for NIH Grants (STRONG): Structured Institutional Needs Assessment and Action Plan Development for Resource Limited Institutions (RLIs) (UC2 - Clinical Trial Not Allowed). See Notice NOT-MD-24-011
- February 14, 2024 - Notice of NICHD Participation in PAR-23-144 "Strengthening Research Opportunities for NIH Grants (STRONG): Structured Institutional Needs Assessment and Action Plan Development for Resource Limited Institutions"). See Notice NOT-HD-24-007
- August 31, 2023 - Notice of Correction to Eligibility Criteria of PAR-23-144, STrengthening Research Opportunities for NIH Grants (STRONG): Structured Institutional Needs Assessment and Action Plan Development for Resource Limited Institutions (RLIs) (UC2). See Notice NOT-MD-23-018
- May 12, 2023 - Notice of Participation of the NIAAA in PAR-23-144. See Notice NOT-AA-23-012 .
- April 25, 2023 - Notice of NCCIH Participation in PAR-23-144, "STrengthening Research Opportunities for NIH Grants (STRONG): Structured Institutional Needs Assessment and Action Plan Development for Resource Limited Institutions (RLIs) (UC2 - Clinical Trial Not Allowed). See Notice NOT-AT-24-004
- August 5, 2022 - Implementation Details for the NIH Data Management and Sharing Policy - see Notice NOT-OD-22-189 .
- August 8, 2022 - New NIH "FORMS-H" Grant Application Forms and Instructions Coming for Due Dates on or after January 25, 2023 - See Notice NOT-OD-22-195 .
- August 31, 2022 - Implementation Changes for Genomic Data Sharing Plans Included with Applications Due on or after January 25, 2023 - See Notice NOT-OD-22-198 .
See Section III. 3. Additional Information on Eligibility .
The STrengthening Research Opportunities for NIH Grants (STRONG): The STRONG-RLI program will support research capacity needs assessments by eligible Resource-Limited Institutions (RLIs). The program will also support the recipient institutions to use the results of the assessments to develop action plans for how to meet the identified needs.
RLIs are defined as institutions with a mission to serve historically underrepresented populations in biomedical research that award degrees in the health professions (and in STEM fields and social and behavioral sciences) and have received an average of $0 to $25 million per year (total costs) of NIH Research Project Grant (RPG) support for the past three fiscal years.
August 18, 2023
All applications are due by 5:00 PM local time of applicant organization.
Applicants are encouraged to apply early to allow adequate time to make any corrections to errors found in the application during the submission process by the due date.
Not Applicable
It is critical that applicants follow the instructions in the Research (R) Instructions in the SF424 (R&R) Application Guide , except where instructed to do otherwise (in this NOFO or in a Notice from NIH Guide for Grants and Contracts).
Conformance to all requirements (both in the Application Guide and the NOFO) is required and strictly enforced. Applicants must read and follow all application instructions in the Application Guide as well as any program-specific instructions noted in Section IV . When the program-specific instructions deviate from those in the Application Guide, follow the program-specific instructions.
Applications that do not comply with these instructions may be delayed or not accepted for review.
There are several options available to submit your application through Grants.gov to NIH and Department of Health and Human Services partners. You must use one of these submission options to access the application forms for this opportunity.
- Use the NIH ASSIST system to prepare, submit and track your application online.
- Use an institutional system-to-system (S2S) solution to prepare and submit your application to Grants.gov and eRA Commons to track your application. Check with your institutional officials regarding availability.
- Use Grants.gov Workspace to prepare and submit your application and eRA Commons to track your application.
Part 2. Full Text of Announcement
Section i. notice of funding opportunity description.
Purpose: The purpose of the STRONG-RLI Notice of Funding Opportunity (NOFO) is to invite applications to conduct biomedical research capacity needs assessments by Resource-Limited Institutions (RLIs) and then to use the results of the assessments to create action plans for meeting identified needs. The program’s goal is to increase competitiveness in the biomedical research enterprise and foster institutional environments conducive to research career development. Awards are intended to support RLIs in analyzing their institutional research capacity needs and strengths. Resource-Limited Institutions (RLIs) are defined for this NOFO as institutions with a mission to serve historically underrepresented populations in biomedical research that award degrees in the health professions or the sciences related to health, in STEM fields including social and behavioral sciences, and have received an average of $0 to $25 million (total costs) per year of NIH research project grant (RPG) support for the past three fiscal years (as defined in Section III -Eligibility).
Background:
NIH’s ability to help ensure that the nation remains a global leader in scientific discovery and innovation is dependent upon a pool of highly talented scientists from diverse backgrounds who will help to further NIH's mission (see NOT-OD-20-031 ). NIH recognizes the importance of diversity in biomedical, clinical, behavioral, and social sciences (collectively termed "biomedical") research. This includes the diversification of NIH-funded institutions, where researchers with a wide range of skill sets and viewpoints can bring different perspectives, creativity, and individual enterprise to address complex scientific problems.
RLIs, as defined below, play an important role in supporting scientific research, particularly on diseases or conditions that disproportionately impact racial ethnic minority groups and other U.S. populations that experience health disparities. Although these institutions are uniquely positioned to engage underserved populations in research and in the translation of research advances into culturally competent, measurable and sustained improvements in health outcomes, they may benefit from enhancing their capacity to conduct and sustain cutting-edge health-related research.
NIH is committed to assisting RLIs in building institutional research capacity. Scientists at RLIs are critical to advancing knowledge in the biomedical research enterprise. NIH has many programs designed to support researchers at RLIs and broaden the participation of researchers through inclusive excellence across regions, institutions, and demographic groups. The role of RLIs in the nation’s overall competitiveness in research is integrally related to current resources, departmental and disciplinary strengths and capabilities, and campus research support systems and infrastructure. It is critical that RLIs recognize and utilize their research and organizational capabilities so they can leverage existing strengths and develop strategic approaches in areas that require additional attention. Structured needs assessments to examine research and organizational capabilities can offer metrics for short-term/long-term action plans. These assessments will enable institutions to develop benchmarks and action items to increase their competitiveness for NIH, Federal, and other funding opportunities.
RLIs face unique challenges depending on the institution type, resources, infrastructure, and policies as they seek to acquire NIH or other federal agency funding. The areas at RLIs that need to be identified and addressed to reduce the barriers to scientific advancement and increase independent research funding can best be determined by the institution itself. A fundamental principle for organizational development and change is the use of a structured assessment to understand these barriers.
This Funding Opportunity will provide resources to the institutions to 1) conduct the assessment of research infrastructure and other requirements that will enhance administrative and research resources, institutional policies, and expanded opportunities for faculty and students in the biomedical research enterprise; and 2) Use the results of these institutional assessments to develop action plans that will support the conduct of high-quality biomedical research.
Program Objectives:
The purpose of this NIH-wide initiative, STRONG-RLI, is to support research active RLIs to;1. conduct rigorous research capacity needs assessments.2. use the results of the assessments to develop action plans for how to meet the identified needs.
Because of the significant variability in the types of RLIs, two separate categories have been created for this initiative. Please refer to Section III for eligibility criteria for RLIs.
The two categories of research active RLIs are defined in Section III of the NOFO:
1) Low Research Active (LRA) : An RLI that is an undergraduate or graduate degree granting institution and has had less than six million dollars (total costs) in NIH research project grant (RPG) support per year in three of the last five years. In addition, undergraduate granting institutions must have at least 35% of undergraduate students supported by Pell grants.
2) High Research Active (HRA) : An RLI that grants doctoral degrees and has had between six million and 25 million dollars (total costs) in NIH RPG support per year in three of the last five years.
Both LRA and HRA RLIs must have a historical mission to support underrepresented groups in biomedical sciences. Each institution should describe the specific category into which they fit and provide documentation to verify those requirements.
Each RLI will provide details on how they plan to conduct their needs assessments and create/use/adapt/ instruments to study research capacity at the institution. Please note that institutional climate or culture assessment is not a priority for this funding announcement.
As part of the funding announcement , the recipient institutions are expected to use the results of needs assessments to develop action plans for short term and long term goals, to meet the identified needs . Applicants are encouraged to provide detailed approaches for conducting the needs assessment and action plan development. The action plan should include identification of possible sources of funding for increasing research capacity. The implementation of the action plan is beyond the scope of this funding opportunity.
A. Institutional Needs-Assessment for research capacity
NIH recognizes and values the heterogeneity in institutional settings and the students they serve. Applicants must describe their distinctive biomedical research and research training environment and the current services to support them.
Applicants for this needs assessment can use any available tools, or adapt existing tools, to fit their context and needs.
B. Development of Institutional Action Plans
- After completion of the needs assessment, the recipient institutions are expected to develop an action plan. The Institutional Action Plan for research capacity is intended to serve as a roadmap for enhancing the infrastructure and capacity at the applicant institution.
- The outcomes of the needs assessment should determine the capacity building interventions that the institution can undertake to strengthen the institutional framework and research capacity. The Institutional Action Plan that will be developed is expected to be supported by an institutional leader, e.g., the Provost or President (see Letters of Support).
C. Needs assessment topics may include (but are not limited to):
The institution will determine the needs assessment foci but may include broad categories such as administrative/research/student/faculty.
Administrative topics may include -
- Establishing or enhancing the Office of Sponsored Programs (OSP), examining efficiencies and staffing requirements and personnel needs for administrative support
- Available resources for effective business practices, automation, information dissemination, documentation and tracking progress for research activities,
- Process management and process improvement for grant application, grant award, and grant administration.
Research topics may include-
- Research infrastructure may include physical research facilities, lab equipment, and computing resources, core facility for technology, support staff, professional development, laboratories. Appropriate physical research facilities and skilled research support to enable competitiveness.
- Research readiness in areas, such as basic, behavioral or clinical research, grantsmanship support, seminars and workshops for grant writing, for sharing research ideas to enhance knowledge in the field. Potential and current scientific research areas of interest.
- Capacity to conduct Human Subjects Research
- Capacity for Community Engagement research
- Partnerships/ collaboration with other academic institutions, the public sector, and community-based organizations that are sustainable and equitable
Student and faculty topics may include-
- Training needs, Mentoring/Sponsorship, faculty development.
- Student resources for research, support for research experiences, and for post-bac and graduate career progression in biomedical research and in STEM topics
- Research staff recruitment and benefits packages, retention bonuses,
- Faculty teaching workloads that allow time for research pursuits, and department/college-based research staff and administrative support
- Institutional policies for assessment of teaching versus research assignments and support
- Tenure evaluations of faculty services for research, committee, community engagement, etc., protected time for research program development
Technical Assistance Webinar:
NIH will conduct a Technical Assistance Webinar for prospective applicants on July 21st from 2-3.30pm EST. Please join the webinar using the link below:
Join Zoom Meeting https://nih.zoomgov.com/j/1614627302?pwd=RmVXc0RjWjV2WTZsUzd1WmFSWU1NZz09&from=addon Meeting ID: 161 462 7302 Passcode: 919936 One tap mobile +16692545252,,1614627302#,,,,*919936# US (San Jose) +16468287666,,1614627302#,,,,*919936# US (New York)
See Section VIII. Other Information for award authorities and regulations.
Section II. Award Information
Cooperative Agreement: A support mechanism used when there will be substantial Federal scientific or programmatic involvement. Substantial involvement means that, after award, NIH scientific or program staff will assist, guide, coordinate, or participate in project activities. See Section VI.2 for additional information about the substantial involvement for this FOA.
The OER Glossary and the SF424 (R&R) Application Guide provide details on these application types. Only those application types listed here are allowed for this NOFO.
Not Allowed: Only accepting applications that do not propose clinical trials.
Need help determining whether you are doing a clinical trial?
The number of awards is contingent upon NIH appropriations and the submission of a sufficient number of meritorious applications.
Application budgets for direct costs should not exceed $250,000/year.
The scope of the proposed project should determine the project period. The maximum project period is three years
NIH grants policies as described in the NIH Grants Policy Statement will apply to the applications submitted and awards made from this NOFO.
Section III. Eligibility Information
1. Eligible Applicants
Higher Education Institutions
- Public/State Controlled Institutions of Higher Education
- Private Institutions of Higher Education
The following types of Higher Education Institutions are always encouraged to apply for NIH support as Public or Private Institutions of Higher Education:
- Hispanic-serving Institutions
- Historically Black Colleges and Universities (HBCUs)
- Tribally Controlled Colleges and Universities (TCCUs)
- Alaska Native and Native Hawaiian Serving Institutions
- Asian American Native American Pacific Islander Serving Institutions (AANAPISIs)
For this funding opportunity, an applicant must be a Resource-Limited Institution (RLI), defined as an institution with a mission to serve historically underrepresented populations that awards degrees in the health professions (and related sciences) and has received an average of $0 to $25 million per year (total costs) of NIH Research Project Grants (RPG) support for the past three fiscal years.
A mission to serve historically underrepresented populations may be demonstrated by a documented historical and current mission to educate students from any of the populations that have been identified as underrepresented in biomedical research as defined by the National Science Foundation NSF, see http://www.nsf.gov/statistics/wmpd/ ) (i.e., African Americans or Blacks, Hispanic or Latino Americans, American Indians, Alaska Natives, Native Hawaiians, U.S. Pacific Islanders, and persons with disabilities) or by a documented record of recruiting, training and/or educating, and graduating underrepresented students as defined by NSF (see above), which has resulted in increasing the institution's contribution to the national pool of graduates from underrepresented backgrounds who pursue biomedical research careers.
RLIs, as defined above, are classified into the following two categories for this opportunity:
Institutional letters will attest to the category of the institution whether they are LRA or HRA and provide information to verify which can be included as an attachment.
Non-domestic (non-U.S.) Entities (Foreign Institutions) are not eligible to apply.
Non-domestic (non-U.S.) components of U.S. Organizations are not eligible to apply.
Foreign components, as defined in the NIH Grants Policy Statement , are not allowed.
Applicant Organizations
Applicant organizations must complete and maintain the following registrations as described in the SF 424 (R&R) Application Guide to be eligible to apply for or receive an award. All registrations must be completed prior to the application being submitted. Registration can take 6 weeks or more, so applicants should begin the registration process as soon as possible. The NIH Policy on Late Submission of Grant Applications states that failure to complete registrations in advance of a due date is not a valid reason for a late submission.
- NATO Commercial and Government Entity (NCAGE) Code Foreign organizations must obtain an NCAGE code (in lieu of a CAGE code) in order to register in SAM.
- Unique Entity Identifier (UEI)- A UEI is issued as part of the SAM.gov registration process. The same UEI must be used for all registrations, as well as on the grant application.
- eRA Commons - Once the unique organization identifier is established, organizations can register with eRA Commons in tandem with completing their Grants.gov registrations; all registrations must be in place by time of submission. eRA Commons requires organizations to identify at least one Signing Official (SO) and at least one Program Director/Principal Investigator (PD/PI) account in order to submit an application.
- Grants.gov Applicants must have an active SAM registration in order to complete the Grants.gov registration.
Program Directors/Principal Investigators (PD(s)/PI(s))
All PD(s)/PI(s) must have an eRA Commons account. PD(s)/PI(s) should work with their organizational officials to either create a new account or to affiliate their existing account with the applicant organization in eRA Commons. If the PD/PI is also the organizational Signing Official, they must have two distinct eRA Commons accounts, one for each role. Obtaining an eRA Commons account can take up to 2 weeks.
Any individual(s) with the skills, knowledge, and resources necessary to carry out the proposed research as the Program Director(s)/Principal Investigator(s) (PD(s)/PI(s)) is invited to work with their organization to develop an application for support. Individuals from diverse backgrounds, including underrepresented racial and ethnic groups, individuals with disabilities, and women are always encouraged to apply for NIH support. See, Reminder: Notice of NIH's Encouragement of Applications Supporting Individuals from Underrepresented Ethnic and Racial Groups as well as Individuals with Disabilities , NOT-OD-22-019 .
For institutions/organizations proposing multiple PDs/PIs, visit the Multiple Program Director/Principal Investigator Policy and submission details in the Senior/Key Person Profile (Expanded) Component of the SF424 (R&R) Application Guide.
2. Cost Sharing
This NOFO does not require cost sharing as defined in the NIH Grants Policy Statement.
3. Additional Information on Eligibility
Number of Applications
Only one application per institution (normally identified by having a unique UEI or NIH IPF number) is allowed
The NIH will not accept duplicate or highly overlapping applications under review at the same time, per 2.3.7.4 Submission of Resubmission Application . This means that the NIH will not accept:
- A new (A0) application that is submitted before issuance of the summary statement from the review of an overlapping new (A0) or resubmission (A1) application.
- A resubmission (A1) application that is submitted before issuance of the summary statement from the review of the previous new (A0) application.
- An application that has substantial overlap with another application pending appeal of initial peer review (see 2.3.9.4 Similar, Essentially Identical, or Identical Applications ).
Only one application per institution (normally identified by having a unique UEI number or NIH IPF number) is allowed.
Section IV. Application and Submission Information
1. Requesting an Application Package
The application forms package specific to this opportunity must be accessed through ASSIST, Grants.gov Workspace or an institutional system-to-system solution. Links to apply using ASSIST or Grants.gov Workspace are available in Part 1 of this NOFO. See your administrative office for instructions if you plan to use an institutional system-to-system solution.
2. Content and Form of Application Submission
It is critical that applicants follow the instructions in the Research (R) Instructions in the SF424 (R&R) Application Guide except where instructed in this notice of funding opportunity to do otherwise. Conformance to the requirements in the Application Guide is required and strictly enforced. Applications that are out of compliance with these instructions may be delayed or not accepted for review.
Letter of Intent
Although a letter of intent is not required, is not binding, and does not enter into the review of a subsequent application, the information that it contains allows IC staff to estimate the potential review workload and plan the review.
By the date listed in Part 1. Overview Information , prospective applicants are asked to submit a letter of intent that includes the following information:
- Descriptive title of proposed activity
- Name(s), address(es), and telephone number(s) of the PD(s)/PI(s)
- Names of other key personnel
- Participating institution(s)
- Number and title of this funding opportunity
The letter of intent should be sent to:
Yujing Liu, MD, PhD National Institute on Minority Health and Health Disparities (NIMHD) Telephone: 301-827-7815 Email: [email protected]
Page Limitations
All page limitations described in the SF424 Application Guide and the Table of Page Limits must be followed.
The following section supplements the instructions found in the SF424 (R&R) Application Guide and should be used for preparing an application to this NOFO.
SF424(R&R) Cover
All instructions in the SF424 (R&R) Application Guide must be followed.
SF424(R&R) Project/Performance Site Locations
SF424(R&R) Other Project Information
SF424(R&R) Senior/Key Person Profile
All instructions in the SF424 (R&R) Application Guide must be followed, with the following additional instructions:
Travel costs for attending any in-person meetings and STRONG Executive Steering Committee (SESC) meetings must be included.
Funds may not be used for:
- Research infrastructure (such as laboratory supplies, laboratory equipment)
- Alterations or renovations
- Research projects or pilot projects
R&R Subaward Budget
PHS 398 Cover Page Supplement
PHS 398 Research Plan
Research Strategy:
Significance
Explain the needs for institutional research capacity and importance of the problem or critical barrier to progress that the proposed project addresses. Describe the benefits if the proposed aims are achieved with respect to enhanced biomedical research capacity.
Applicants should address the innovative aspects of the proposed needs assessment plans for research capacity. For this program, innovation is considered the use of existing products, tools or processes or creating or adapting evidence-based tools to fit the context and needs of the institutions.
A. Institutional Needs-Assessment for research capacity section describe:
- Physical research facility, research faculty support from institution, faculty teaching workload, human resources, Sponsored program
- Applicant must describe current methods of measuring student/faculty outcomes to take into consideration institutional missions, faculty investment, student populations, student needs, and institutional resource constraints.
- Tools and instruments for needs assessment, monitoring and evaluation of health research capacity development activities at the individual and organizational level
- The types of research facilities available for biomedical research and research training.
- The needs for research infrastructure to conduct biomedical, behavioral or clinical research, potential and current scientific research areas of interest.
- List and describe the outcomes of any capacity-building or infrastructure grants the institution has received over the past ten years, including the source and total costs of each award.
- The investigative team and their relevant expertise in conducting a needs assessment
- Student enrollment in the biomedical areas, including the number and percentage of undergraduate and graduate students, and the enrollment of students who are Pell-grant eligible (for LRA applications); and
- The current level of student and faculty participation in research.
- Describe the sponsored programs administration and how it will inform the needs assessment. The types of services provided by the existing sponsored projects administration (or similar entity). Current levels of sponsored programs productivity (e.g., number of applications submitted, number of applications funded, number of subcontracts).
Describe the approaches for developing an Institutional Action Plan after completing needs assessment for research capacity. The Institutional Action Plan for research capacity is intended to serve as a roadmap for enhancing the infrastructure and capacity at the applicant institution. This section of the application should describe steps that will be undertaken to ensure identified needs assessment activities lead to action plans for the long-term strengthening of research capacity. It must include an institutional commitment to achieving the goals and objectives of the proposed project and activities signed by institutional leadership (e.g., President, Provost, and Deans (see Letters of Support).
C. Governance and structure of steering committees
The Steering Committee (SC) will serve as the primary governing and oversight board for the cooperative agreement funded under this NOFO.
- Describe the composition and the activities of the steering committee. Describe the desired expertise of its members. Include the frequency of meetings and any other relevant information.
- The membership of the SC consists of the PD(s)/PI(s), the NIH Project Coordinator, and any additional stake holders deemed necessary.
Timeline and Milestones:
Describe the timeline for the needs assessment and action plan activities. The timeline should be realistic given the time needed to develop the approaches/tools and collect the proposed data. Describe how the program goals/aims will be aligned with milestones and metrics.
Letters of Support: Provide letters of support for the proposed needs assessment activities following instructions in the SF424 Application Guide.
A. Institutional Eligibility Letter (1-page maximum). S ubmit a letter from the Provost or similar official with institution-wide responsibility that certify that the applicant organization qualifies as one of the following two categories of research active RLI specified in this NOFO:
A mission to serve historically underrepresented populations may be demonstrated by a documented historical and current mission to educate students from underrepresented populations in biomedical research.
The two categories of research active RLIs are:
1) Low Research Active (LRA): An RLI that is an undergraduate or graduate degree granting institution, with at least 35% of undergraduate students supported by Pell grants, and that has had less than six million dollars in NIH research project grant (RPG) support per year in three of the last five years.
2) High Research Active (HRA): An RLI that grants doctoral degrees and has had less than 25 million dollars in NIH RPG support in three of the last five years.
B. Institutional Commitment Letter. The application must include an Institutional Commitment Letter from the President or designated high-ranking official such as the Provost, Vice President or Dean. Describe how the proposed project aligns with the broad institutional vision for enhancing biomedical research. The letter should include a commitment to achieving the goals and objectives of the proposed project and activities.
The letters of support must be included with the application. Applications which lack this letter will be considered incomplete and will be withdrawn and will not be reviewed.
Resource Sharing Plan : Individuals are required to comply with the instructions for the Resource Sharing Plans as provided in the SF424 (R&R) Application Guide.
The following modifications also apply:
Generally, Resource Sharing Plans are expected, but they are not applicable for this FOA.
- A Data Management and Sharing Plan is not applicable for this NOFO.
Appendix: Only limited Appendix materials are allowed. Follow all instructions for the Appendix as described in the SF424 (R&R) Application Guide.
- No publications or other material, with the exception of blank questionnaires or blank surveys, may be included in the Appendix.
PHS Human Subjects and Clinical Trials Information
When involving human subjects research, clinical research, and/or NIH-defined clinical trials (and when applicable, clinical trials research experience) follow all instructions for the PHS Human Subjects and Clinical Trials Information form in the SF424 (R&R) Application Guide, with the following additional instructions:
If you answered Yes to the question Are Human Subjects Involved? on the R&R Other Project Information form, you must include at least one human subjects study record using the Study Record: PHS Human Subjects and Clinical Trials Information form or Delayed Onset Study record.
Study Record: PHS Human Subjects and Clinical Trials Information
Delayed Onset Study
Note: Delayed onset does NOT apply to a study that can be described but will not start immediately (i.e., delayed start).All instructions in the SF424 (R&R) Application Guide must be followed.
PHS Assignment Request Form
3. Unique Entity Identifier and System for Award Management (SAM)
See Part 1. Section III.1 for information regarding the requirement for obtaining a unique entity identifier and for completing and maintaining active registrations in System for Award Management (SAM), NATO Commercial and Government Entity (NCAGE) Code (if applicable), eRA Commons, and Grants.gov
4. Submission Dates and Times
Part I. Overview Information contains information about Key Dates and times. Applicants are encouraged to submit applications before the due date to ensure they have time to make any application corrections that might be necessary for successful submission. When a submission date falls on a weekend or Federal holiday , the application deadline is automatically extended to the next business day.
Organizations must submit applications to Grants.gov (the online portal to find and apply for grants across all Federal agencies). Applicants must then complete the submission process by tracking the status of the application in the eRA Commons , NIH’s electronic system for grants administration. NIH and Grants.gov systems check the application against many of the application instructions upon submission. Errors must be corrected and a changed/corrected application must be submitted to Grants.gov on or before the application due date and time. If a Changed/Corrected application is submitted after the deadline, the application will be considered late. Applications that miss the due date and time are subjected to the NIH Policy on Late Application Submission.
Applicants are responsible for viewing their application before the due date in the eRA Commons to ensure accurate and successful submission.
Information on the submission process and a definition of on-time submission are provided in the SF424 (R&R) Application Guide.
5. Intergovernmental Review (E.O. 12372)
This initiative is not subject to intergovernmental review.
6. Funding Restrictions
All NIH awards are subject to the terms and conditions, cost principles, and other considerations described in the NIH Grants Policy Statement .
Pre-award costs are allowable only as described in the NIH Grants Policy Statement .
7. Other Submission Requirements and Information
Applications must be submitted electronically following the instructions described in the SF424 (R&R) Application Guide. Paper applications will not be accepted.
Applicants must complete all required registrations before the application due date. Section III. Eligibility Information contains information about registration.
For assistance with your electronic application or for more information on the electronic submission process, visit How to Apply Application Guide . If you encounter a system issue beyond your control that threatens your ability to complete the submission process on-time, you must follow the Dealing with System Issues guidance. For assistance with application submission, contact the Application Submission Contacts in Section VII.
Important reminders:
All PD(s)/PI(s) must include their eRA Commons ID in the Credential field of the Senior/Key Person Profile form . Failure to register in the Commons and to include a valid PD/PI Commons ID in the credential field will prevent the successful submission of an electronic application to NIH. See Section III of this NOFO for information on registration requirements.
The applicant organization must ensure that the unique entity identifier provided on the application is the same identifier used in the organization’s profile in the eRA Commons and for the System for Award Management. Additional information may be found in the SF424 (R&R) Application Guide.
See more tips for avoiding common errors.
Upon receipt, applications will be evaluated for completeness and compliance with application instructions by the Center for Scientific Review, NIH. Applications that are incomplete or non-compliant will not be reviewed.
In order to expedite review, applicants are requested to notify the NIMHD Referral Office by email at [email protected] when the application has been submitted. Please include the NOFO number and title, PD/PI name, and title of the application.
Post Submission Materials
Applicants are required to follow the instructions for post-submission materials, as described in the policy
Section V. Application Review Information
1. Criteria
Only the review criteria described below will be considered in the review process. Applications submitted to the NIH in support of the NIH mission are evaluated for scientific and technical merit through the NIH peer review system.
Reviewers will provide an overall impact score to reflect their assessment of the likelihood for the project to exert a sustained, powerful influence on the research field(s) involved, in consideration of the following review criteria and additional review criteria (as applicable for the project proposed).
Reviewers will consider each of the review criteria below in the determination of scientific merit and give a separate score for each. An application does not need to be strong in all categories to be judged likely to have major scientific impact. For example, a project that by its nature is not innovative may be essential to advance a field.
Does the project address an important problem or a critical barrier to progress in the field? Is the prior research that serves as the key support for the proposed project rigorous? If the aims of the project are achieved, how will scientific knowledge, technical capability, and/or clinical practice be improved? How will successful completion of the aims change the concepts, methods, technologies, treatments, services, or preventative interventions that drive this field?
In addition, specific to this NOFO:
How well does the application provide a vision for how the project will serve as a foundation for future research capacity building? To what degree the application describes clear pathways between the need assessment and action plan development research activities and future research efforts? To what extent is the proposed project likely to enhance institutional research capacity to conduct biomedical research?
Are the PD(s)/PI(s), collaborators, and other researchers well suited to the project? If Early Stage Investigators or those in the early stages of independent careers, do they have appropriate experience and training? If established, have they demonstrated an ongoing record of accomplishments that have advanced their field(s)? If the project is collaborative or multi-PD/PI, do the investigators have complementary and integrated expertise; are their leadership approach, governance, and organizational structure appropriate for the project?
To what extent do the PDs/PIs have the appropriate expertise to conduct the needs assessment, implement the proposed project, analyze the outcomes, and develop action plans?
Does the application challenge and seek to shift current research or clinical practice paradigms by utilizing novel theoretical concepts, approaches or methodologies, instrumentation, or interventions? Are the concepts, approaches or methodologies, instrumentation, or interventions novel to one field of research or novel in a broad sense? Is a refinement, improvement, or new application of theoretical concepts, approaches or methodologies, instrumentation, or interventions proposed?
How well does the applicant create approaches to fit their context and needs? Does the application employ novel approaches or methods to fulfill its purpose?
Are the overall strategy, methodology, and analyses well-reasoned and appropriate to accomplish the specific aims of the project? Have the investigators included plans to address weaknesses in the rigor of prior research that serves as the key support for the proposed project? Have the investigators presented strategies to ensure a robust and unbiased approach, as appropriate for the work proposed? Are potential problems, alternative strategies, and benchmarks for success presented? If the project is in the early stages of development, will the strategy establish feasibility and will particularly risky aspects be managed? Have the investigators presented adequate plans to address relevant biological variables, such as sex, for studies in vertebrate animals or human subjects?
If the project involves human subjects and/or NIH-defined clinical research, are the plans to address 1) the protection of human subjects from research risks, and 2) inclusion (or exclusion) of individuals on the basis of sex/gender, race, and ethnicity, as well as the inclusion or exclusion of individuals of all ages (including children and older adults), justified in terms of the scientific goals and research strategy proposed?
To what extent does the applicant describe the tools and instruments for needs assessment, monitoring and evaluation of research capacity development activities? To what degree does the applicant identify metrics and indicators of success that will be used to assess the anticipated outcomes? Is the duration of the initial needs assessment stage adequate to develop action plans for short-term goals? To what degree isthe structure and governance plan likely to lead to implementation of the proposed plan? Are these goals feasible and well developed on the timeline of the award? How well are the program goals/aims aligned with yearly milestones and are the details provided adequate?
Will the scientific environment in which the work will be done contribute to the probability of success? Are the institutional support, equipment, and other physical resources available to the investigators adequate for the project proposed? Will the project benefit from unique features of the scientific environment, subject populations, or collaborative arrangements?
How strong is the level of institutional commitment to the project, including administrative and scientific support, to ensure the success of the project?
How well do the letters of support demonstrate a strong commitment to the proposed activities?
As applicable for the project proposed, reviewers will evaluate the following additional items while determining scientific and technical merit, and in providing an overall impact score, but will not give separate scores for these items.
For research that involves human subjects but does not involve one of the categories of research that are exempt under 45 CFR Part 46, the committee will evaluate the justification for involvement of human subjects and the proposed protections from research risk relating to their participation according to the following five review criteria: 1) risk to subjects, 2) adequacy of protection against risks, 3) potential benefits to the subjects and others, 4) importance of the knowledge to be gained, and 5) data and safety monitoring for clinical trials.
For research that involves human subjects and meets the criteria for one or more of the categories of research that are exempt under 45 CFR Part 46, the committee will evaluate: 1) the justification for the exemption, 2) human subjects involvement and characteristics, and 3) sources of materials. For additional information on review of the Human Subjects section, please refer to the Guidelines for the Review of Human Subjects .
When the proposed project involves human subjects and/or NIH-defined clinical research, the committee will evaluate the proposed plans for the inclusion (or exclusion) of individuals on the basis of sex/gender, race, and ethnicity, as well as the inclusion (or exclusion) of individuals of all ages (including children and older adults) to determine if it is justified in terms of the scientific goals and research strategy proposed. For additional information on review of the Inclusion section, please refer to the Guidelines for the Review of Inclusion in Clinical Research .
The committee will evaluate the involvement of live vertebrate animals as part of the scientific assessment according to the following criteria: (1) description of proposed procedures involving animals, including species, strains, ages, sex, and total number to be used; (2) justifications for the use of animals versus alternative models and for the appropriateness of the species proposed; (3) interventions to minimize discomfort, distress, pain and injury; and (4) justification for euthanasia method if NOT consistent with the AVMA Guidelines for the Euthanasia of Animals. Reviewers will assess the use of chimpanzees as they would any other application proposing the use of vertebrate animals. For additional information on review of the Vertebrate Animals section, please refer to the Worksheet for Review of the Vertebrate Animals Section .
Reviewers will assess whether materials or procedures proposed are potentially hazardous to research personnel and/or the environment, and if needed, determine whether adequate protection is proposed.
For Resubmissions, the committee will evaluate the application as now presented, taking into consideration the responses to comments from the previous scientific review group and changes made to the project.
Not applicable
As applicable for the project proposed, reviewers will consider each of the following items, but will not give scores for these items, and should not consider them in providing an overall impact score.
Reviewers will assess whether the project presents special opportunities for furthering research programs through the use of unusual talent, resources, populations, or environmental conditions that exist in other countries and either are not readily available in the United States or augment existing U.S. resources.
Reviewers will assess the information provided in this section of the application, including 1) the Select Agent(s) to be used in the proposed research, 2) the registration status of all entities where Select Agent(s) will be used, 3) the procedures that will be used to monitor possession use and transfer of Select Agent(s), and 4) plans for appropriate biosafety, biocontainment, and security of the Select Agent(s).
Reviewers will comment on whether the Resource Sharing Plan(s) (e.g., Sharing Model Organisms ) or the rationale for not sharing the resources, is reasonable.
For projects involving key biological and/or chemical resources, reviewers will comment on the brief plans proposed for identifying and ensuring the validity of those resources.
Reviewers will consider whether the budget and the requested period of support are fully justified and reasonable in relation to the proposed research.
2. Review and Selection Process
Applications will be evaluated for scientific and technical merit by (an) appropriate Scientific Review Group(s) convened by NIMHD, in accordance with NIH peer review policy and procedures , using the stated review criteria . Assignment to a Scientific Review Group will be shown in the eRA Commons.
As part of the scientific peer review, all applications will receive a written critique.
Applications may undergo a selection process in which only those applications deemed to have the highest scientific and technical merit (generally the top half of applications under review) will be discussed and assigned an overall impact score.
Applications will be assigned on the basis of established PHS referral guidelines to the appropriate NIH Institute or Center. Applications will compete for available funds with all other recommended applications . Following initial peer review, recommended applications will receive a second level of review by the appropriate national Advisory Council or Board. The following will be considered in making funding decisions:
- Scientific and technical merit of the proposed project as determined by scientific peer review.
- Availability of funds.
- Relevance of the proposed project to program priorities.
- Geographical distribution of the portfolio
- Balance between HRA and LRA awards
3. Anticipated Announcement and Award Dates
After the peer review of the application is completed, the PD/PI will be able to access his or her Summary Statement (written critique) via the eRA Commons . Refer to Part 1 for dates for peer review, advisory council review, and earliest start date.
Information regarding the disposition of applications is available in the NIH Grants Policy Statement .
Section VI. Award Administration Information
1. Award Notices
If the application is under consideration for funding, NIH will request "just-in-time" information from the applicant as described in the NIH Grants Policy Statement .
A formal notification in the form of a Notice of Award (NoA) will be provided to the applicant organization for successful applications. The NoA signed by the grants management officer is the authorizing document and will be sent via email to the recipient's business official.
Recipients must comply with any funding restrictions described in Section IV.6. Funding Restrictions. Selection of an application for award is not an authorization to begin performance. Any costs incurred before receipt of the NoA are at the recipient's risk. These costs may be reimbursed only to the extent considered allowable pre-award costs.
Any application awarded in response to this NOFO will be subject to terms and conditions found on the Award Conditions and Information for NIH Grants website. This includes any recent legislation and policy applicable to awards that is highlighted on this website.
Institutional Review Board or Independent Ethics Committee Approval: Recipient institutions must ensure that protocols are reviewed by their IRB or IEC. To help ensure the safety of participants enrolled in NIH-funded studies, the recipient must provide NIH copies of documents related to all major changes in the status of ongoing protocols.
2. Administrative and National Policy Requirements
All NIH grant and cooperative agreement awards include the NIH Grants Policy Statement as part of the NoA. For these terms of award, see the NIH Grants Policy Statement Part II: Terms and Conditions of NIH Grant Awards, Subpart A: General and Part II: Terms and Conditions of NIH Grant Awards, Subpart B: Terms and Conditions for Specific Types of Grants, Recipients, and Activities , including of note, but not limited to:
- Federal wide Research Terms and Conditions
- Prohibition on Certain Telecommunications and Video Surveillance Services or Equipment
- Acknowledgment of Federal Funding
If a recipient is successful and receives a Notice of Award, in accepting the award, the recipient agrees that any activities under the award are subject to all provisions currently in effect or implemented during the period of the award, other Department regulations and policies in effect at the time of the award, and applicable statutory provisions.
Should the applicant organization successfully compete for an award, recipients of federal financial assistance (FFA) from HHS will be required to complete an HHS Assurance of Compliance form (HHS 690) in which the recipient agrees, as a term and condition of receiving the grant, to administer their programs in compliance with federal civil rights laws that prohibit discrimination on the basis of race, color, national origin, age, sex and disability, and agreeing to comply with federal conscience laws, where applicable. This includes ensuring that entities take meaningful steps to provide meaningful access to persons with limited English proficiency; and ensuring effective communication with persons with disabilities. Where applicable, Title XI and Section 1557 prohibit discrimination on the basis of sexual orientation, and gender identity. The HHS Office for Civil Rights provides guidance on complying with civil rights laws enforced by HHS. Please see https://www.hhs.gov/civil-rights/for-providers/provider-obligations/index.html and https://www.hhs.gov/civil-rights/for-individuals/nondiscrimination/index.html
HHS recognizes that research projects are often limited in scope for many reasons that are nondiscriminatory, such as the principal investigator’s scientific interest, funding limitations, recruitment requirements, and other considerations. Thus, criteria in research protocols that target or exclude certain populations are warranted where nondiscriminatory justifications establish that such criteria are appropriate with respect to the health or safety of the subjects, the scientific study design, or the purpose of the research. For additional guidance regarding how the provisions apply to NIH grant programs, please contact the Scientific/Research Contact that is identified in Section VII under Agency Contacts of this NOFO.
- Recipients of FFA must ensure that their programs are accessible to persons with limited English proficiency. For guidance on meeting the legal obligation to take reasonable steps to ensure meaningful access to programs or activities by limited English proficient individuals see https://www.hhs.gov/civil-rights/for-individuals/special-topics/limited-english-proficiency/fact-sheet-guidance/index.html and https://www.lep.gov .
- For information on an institution’s specific legal obligations for serving qualified individuals with disabilities, including providing program access, reasonable modifications, and to provide effective communication, see https://www.hhs.gov/civil-rights/for-individuals/disability/index.html .
- HHS funded health and education programs must be administered in an environment free of sexual harassment, see https://www.hhs.gov/civil-rights/for-individuals/sex-discrimination/index.html . For information about NIH's commitment to supporting a safe and respectful work environment, who to contact with questions or concerns, and what NIH's expectations are for institutions and the individuals supported on NIH-funded awards, please see https://grants.nih.gov/grants/policy/harassment.htm .
- For guidance on administering programs in compliance with applicable federal religious nondiscrimination laws and applicable federal conscience protection and associated anti-discrimination laws see https://www.hhs.gov/conscience/conscience-protections/index.html and https://www.hhs.gov/conscience/religious-freedom/index.html .
Please contact the HHS Office for Civil Rights for more information about obligations and prohibitions under federal civil rights laws at https://www.hhs.gov/ocr/about-us/contact-us/index.html or call 1-800-368-1019 or TDD 1-800-537-7697.
In accordance with the statutory provisions contained in Section 872 of the Duncan Hunter National Defense Authorization Act of Fiscal Year 2009 (Public Law 110-417), NIH awards will be subject to the Federal Awardee Performance and Integrity Information System (FAPIIS) requirements. FAPIIS requires Federal award making officials to review and consider information about an applicant in the designated integrity and performance system (currently FAPIIS) prior to making an award. An applicant, at its option, may review information in the designated integrity and performance systems accessible through FAPIIS and comment on any information about itself that a federal agency previously entered and is currently in FAPIIS. The Federal awarding agency will consider any comments by the applicant, in addition to other information in FAPIIS, in making a judgement about the applicant’s integrity, business ethics, and record of performance under Federal awards when completing the review of risk posed by applicants as described in 45 CFR Part 75.205 and 2 CFR Part 200.206 Federal awarding agency review of risk posed by applicants. This provision will apply to all NIH grants and cooperative agreements except fellowships.
The following special terms of award are in addition to, and not in lieu of, otherwise applicable U.S. Office of Management and Budget (OMB) administrative guidelines, U.S. Department of Health and Human Services (DHHS) grant administration regulations at 45 CFR Part 75 and 2 CFR Part 200, and other HHS, PHS, and NIH grant administration policies. The administrative and funding instrument used for this program will continue as a cooperative agreement, an "assistance" mechanism (rather than an "acquisition" mechanism), in which substantial NIH programmatic involvement with the recipients is anticipated during the performance of the activities. Under the cooperative agreement, the NIH purpose is to support and stimulate the recipients' activities by involvement in and otherwise working jointly with the award recipients in a partnership role; it is not to assume direction, prime responsibility, or a dominant role in the activities. Consistent with this concept, the dominant role and prime responsibility resides with the recipients for the project as a whole, although specific tasks and activities may be shared among the recipients and the NIH as defined below.
The individual STRONG-RLI recipients will establish steering committees at their institutions with defined roles.
In addition, the PIs of the STRONG-RLI awards and involved NIH staff, and others as needed (ex-officio), will form a STRONG-RLI Executive Steering Committee (SESC) which will oversee the activities of the STRONG-RLI program recipients. There will be a yearly rotating chair of the SESC who will be nominated and selected from the PIs of the awards.
The PDs/PIs will have the primary responsibility for:
- Plan, organize, coordinate, and administer the described activities of the program, including setting project milestones with specific timelines and criteria for Institutional needs assessment and developing action plans.
- Establish Steering Committee, organize, and coordinate SESC meetings
- Ensure compliance with the applicable mandatory NIH regulations and policies
- Participate in the STRONG SESC meetings is a requirement for the PI/PDs.The purpose of the meeting is to share progress, best practices, and address common challenges.
- Work closely with the NIH Program Official and Project Coordinator (see below) in project coordination and management.
- Establish a separate site specific steering committee that will comprise of PI, institute leadership and NIH staff
- Evaluate progress using defined milestones and metrics. Recipients will provide NIH with progress reports at regular intervals as requested.
- Share needs assessment and action plan with the NIH during the award period.
- Recipients will retain custody of and have primary rights to the data and software developed under these awards, subject to Government rights of access consistent with current DHHS, PHS, and NIH policies.
NIH staff will have substantial programmatic involvement that is above and beyond the normal stewardship role in awards, as described below:
The NIH Project Coordinator will :
Work closely with individual PIs and NIH program officials (POs) to facilitate collaborations.
- Interact with each recipient, help coordinate approaches, and contribute to the adjustment of projects/programs or approaches as warranted.
- Advise the recipient in performing project activities (e.g., coordination among RLI recipients for needs assessments; provide access to NIH supported resources; identify other resources for the project);
- Facilitate, not direct, activities.
- Participate on the Steering Committee (see below) or in other functions to help guide the course of the program (e.g., Annual Program Meeting and other Program related meetings).
- Ensure that the directions taken are consistent with the NIH missions and goals.
The Project Coordinator will not participate in the oversight of the funding opportunity announcement, application review, or programmatic and budgetary stewardship of the award.
The Program Official will be responsible for the normal programmatic stewardship of the award, including funding decisions, and will be named in the award notice. The Program Official will not serve as a voting member of the Steering Committee or partake of the duties of the Project Coordinator.
Areas of joint responsibility
The SECS is the governing and oversight body for the Program. Members, who are appointed by the PDs/PIs of the award, will be comprised of the following:
- The PI of each award will serve as the SESC member.
- NIH Project Coordinators.
- Additional members from the NIH may be appointed, but the total number of NIH votes may not exceed 1/3 of the Executive Steering Committee voting membership. Other government staff may attend the Steering Committee meetings, if their expertise is required for specific discussions.
- Each recipient must plan regular meetings (no less frequently than monthly) to discuss the progress and direction of its activities and to ensure that the necessary interactions are taking place. Recipients will be expected to participate in STRONG RLI program-wide meetings. These meetings may be in the form of phone teleconferencing, videoconferencing, and/or web conferencing, as well as face-to-face meetings. Unwillingness or a consistent inability of a PD/PI to attend may be the basis for administrative action including termination of the award.
The SESC will:
- Serve as the primary steering and oversight board for the awards funded under this NOFO.
- Decide on the schedule of regular and annual meetings. The Executive Steering Committee may also call meetings to address urgent needs and will participate in network meetings and teleconferences as needed.
- Contribute to the development of a cohesive and sustainable program.
- Provide advice on key issues such as needs assessment administration, approaches, and tools for research capacity, and opportunities for growth.
- Ensure that the implementation of the Institutional Needs Assessments and Development of Sustainable Action Plan is occurring on schedule and continues to align with the applicant institution's strategic vision for biomedical research and/or research training.
- Alert NIH to emerging needs and impediments.
- Prepare concise (1-2 page) summaries of the Executive Steering Committee recommendations, which will be delivered to the PDs/PIs and members of the group within 30 days after each meeting.
Dispute Resolution:
Any disagreements that may arise in scientific or programmatic matters (within the scope of the award) between award recipients and the NIH may be brought to dispute resolution. A Dispute Resolution Panel composed of three members will be convened. The three members will be a designee of the STRONG Executive Steering Committee chosen without NIH staff voting, one NIH designee, and a third designee with expertise in the relevant area who is chosen by the other two. In the case of individual disagreement, the first member may be chosen by the individual recipient. This special dispute resolution procedure does not alter the recipient's right to appeal an adverse action that is otherwise appealable in accordance with PHS regulation 42 CFR Part 50, Subpart D and DHHS regulation 45 CFR Part 16.
The NIH reserves the right to withhold funding or curtail the program (of an individual award) in accordance with NIH policy.
3. Data Management and Sharing
Note: The NIH Policy for Data Management and Sharing is effective for due dates on or after January 25, 2023.
Consistent with the NIH Policy for Data Management and Sharing, when data management and sharing is applicable to the award, recipients will be required to adhere to the Data Management and Sharing requirements as outlined in the NIH Grants Policy Statement . Upon the approval of a Data Management and Sharing Plan, it is required for recipients to implement the plan as described.
4. Reporting
When multiple years are involved, recipients will be required to submit the Research Performance Progress Report (RPPR) annually and financial statements as required in the NIH Grants Policy Statement.
A final RPPR, invention statement, and the expenditure data portion of the Federal Financial Report are required for closeout of an award, as described in the NIH Grants Policy Statement . NIH NOFOs outline intended research goals and objectives. Post award, NIH will review and measure performance based on the details and outcomes that are shared within the RPPR, as described at 45 CFR Part 75.301 and 2 CFR Part 200.301.
The Federal Funding Accountability and Transparency Act of 2006 (Transparency Act), includes a requirement for recipients of Federal grants to report information about first-tier subawards and executive compensation under Federal assistance awards issued in FY2011 or later. All recipients of applicable NIH grants and cooperative agreements are required to report to the Federal Subaward Reporting System (FSRS) available at www.fsrs.gov on all subawards over the threshold. See the NIH Grants Policy Statement for additional information on this reporting requirement.
In accordance with the regulatory requirements provided at 45 CFR 75.113 and 2 CFR Part 200.113 and Appendix XII to 45 CFR Part 75 and 2 CFR Part 200, recipients that have currently active Federal grants, cooperative agreements, and procurement contracts from all Federal awarding agencies with a cumulative total value greater than $10,000,000 for any period of time during the period of performance of a Federal award, must report and maintain the currency of information reported in the System for Award Management (SAM) about civil, criminal, and administrative proceedings in connection with the award or performance of a Federal award that reached final disposition within the most recent five-year period. The recipient must also make semiannual disclosures regarding such proceedings. Proceedings information will be made publicly available in the designated integrity and performance system (currently FAPIIS). This is a statutory requirement under section 872 of Public Law 110-417, as amended (41 U.S.C. 2313). As required by section 3010 of Public Law 111-212, all information posted in the designated integrity and performance system on or after April 15, 2011, except past performance reviews required for Federal procurement contracts, will be publicly available. Full reporting requirements and procedures are found in Appendix XII to 45 CFR Part 75 and 2 CFR Part 200 Award Term and Condition for Recipient Integrity and Performance Matters.
Section VII. Agency Contacts
We encourage inquiries concerning this funding opportunity and welcome the opportunity to answer questions from potential applicants.
eRA Service Desk (Questions regarding ASSIST, eRA Commons, application errors and warnings, documenting system problems that threaten submission by the due date, and post-submission issues)
Finding Help Online: https://www.era.nih.gov/need-help (preferred method of contact) Telephone: 301-402-7469 or 866-504-9552 (Toll Free)
General Grants Information (Questions regarding application instructions, application processes, and NIH grant resources) Email: [email protected] (preferred method of contact) Telephone: 301-480-7075
Grants.gov Customer Support (Questions regarding Grants.gov registration and Workspace) Contact Center Telephone: 800-518-4726 Email: [email protected]
Brett Miller, PhD Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Telephone: 301-496-9849 Email: [email protected]
Rina Das, PhD. National Institute on Minority Health and Health Disparities (NIMHD) Telephone: 301-496-3996 Email: [email protected]
Behrous Davani, PhD. National Cancer Institute (NCI) Telephone: 240-276-6170 Email: [email protected]
Olga Kovbasnjuk, Ph.D. National Institutes of General Medical Sciences (NIGMS) E-mail: [email protected]
Kristopher Bough, PhD National Institute of Nursing Research (NINR) Telephone: 301-337-1372 Email: [email protected]
Anissa F Brown, PhD NIDCR - NATIONAL INSTITUTE OF DENTAL & CRANIOFACIAL RESEARCH Phone: 301-594-5006 E-mail: [email protected]
Melissa C. Green Parker, Ph.D. Office of Disease Prevention (ODP) Phone: 301-480-1161 E-mail: [email protected]
Erica K Rosemond NCATS - NATIONAL CENTER FOR ADVANCING TRANSLATIONAL SCIENCES Phone: (301) 594-8927 E-mail: [email protected]
Kristy M. Nicks, PhD National Institute of Arthritis and Musculoskeletal and Skin Diseases Tel: 301-594-5055 Email: [email protected]
Carol Shreffler, PhD National Institute of Environmental Health Sciences (NIEHS) Phone: 984-287-3322 E-mail: s [email protected]
Aria Crump NIDA - NATIONAL INSTITUTE ON DRUG ABUSE Phone: 301-443-6504 E-mail: [email protected]
Diane Adger-Johnson, MPH Office of Research Training and Special Programs (ORTSP) National Institute of Allergy and Infectious Diseases (NIAID) Telephone: 301-594-5945 Email: [email protected]
Damiya Eve Whitaker, PsyD, MA ORWH - Office of Research on Women's Health Phone: 301-451-8206 E-mail: [email protected]
Damali Martin, Ph.D., MPH NATIONAL INSTITUTE ON AGING (NIA) Division of Neuroscience (DN) Phone: 301-402-8310 E-mail: [email protected]
Judith Cooper NIDCD - NATIONAL INSTITUTE ON DEAFNESS AND OTHER COMMUNICATION DISORDERS Phone: (301) 496-5061 E-mail: [email protected]
Xinzhi Zhang, M.D. National Heart, Lung, and Blood Institute Phone: 301-435-6865 Email: [email protected]
Brittany Haynes, Ph.D. National Institute of Mental Health (NIMH) Telephone: 301-496-2767 Email: [email protected]
Beda Jean-Francois, Ph.D. National Center for Complementary & Integrative Health (NCCIH) Phone: 202-313-2144 Email: [email protected]
Elizabeth Powell, PhD National Institute on Alcoholism and Alcohol Abuse ( NIAAA ) Telephone: 301-443-0786 Email: [email protected]
Margaret Young Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Telephone: 301-642-4552 Email: [email protected]
Priscilla Grant, JD National Institute on Minority Health and Health Disparities (NIMHD) Telephone: 301-594-8412 Email: [email protected]
Alania Foster NIGMS - NATIONAL INSTITUTE OF GENERAL MEDICAL SCIENCES E-mail: [email protected]
Randi Freundlich National Institute of Nursing Research (NINR) Telephone: 301-594-5974 Email: [email protected]
Gabriel Hidalgo, MBA NIDCR - NATIONAL INSTITUTE OF DENTAL & CRANIOFACIAL RESEARCH Phone: 301-827-4630 E-mail: [email protected]
Leslie Le NCATS - NATIONAL CENTER FOR ADVANCING TRANSLATIONAL SCIENCES Phone: (301) 435-0856 E-mail: [email protected]
Jenny L Greer NIEHS - NATIONAL INSTITUTE OF ENVIRONMENTAL HEALTH SCIENCES Phone: 984.287.3332 E-mail: [email protected]
Pamela G Fleming NIDA - NATIONAL INSTITUTE ON DRUG ABUSE Phone: 301-480-1159 E-mail: [email protected]
Samuel Ashe National Institute of Allergy and Infectious Diseases ( NIAID ) Telephone: 301-435-4799 Email: [email protected]
Jeni Smits NATIONAL INSTITUTE ON AGING (NIA) E-mail: [email protected]
Anthony Agresti NHLBI - NATIONAL HEART, LUNG, AND BLOOD INSTITUTE Phone: 301-827-8014 E-mail: [email protected]
Tamara Kees National Institute of Mental Health (NIMH) Telephone: 301-443-8811 Email: [email protected]
Debbie Chen, Ph.D. National Center for Complementary and Integrative Health (NCCIH) Telephone: 301-594-3788 Email: [email protected]
Judy Fox National Institute on Alcoholism and Alcohol Abuse (NIAAA) Telephone: 301-443-4704 Email: [email protected]
Section VIII. Other Information
Recently issued trans-NIH policy notices may affect your application submission. A full list of policy notices published by NIH is provided in the NIH Guide for Grants and Contracts . All awards are subject to the terms and conditions, cost principles, and other considerations described in the NIH Grants Policy Statement .
Awards are made under the authorization of Sections 301 and 405 of the Public Health Service Act as amended (42 USC 241 and 284) and under Federal Regulations 42 CFR Part 52 and 45 CFR Part 75 and 2 CFR Part 200.

Note: For help accessing PDF, RTF, MS Word, Excel, PowerPoint, Audio or Video files, see Help Downloading Files .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
The Importance of Individual-Site and System-Wide Community Health Needs Assessments
Associated data.
The datasets generated for this study are available on request to the corresponding author.
In order to fulfill the Patient Protection and Affordable Care Act's Community Health Needs Assessment requirements, hospital systems sometimes vary in detail between individual hospital sites or locations and performing an assessment for the entire system. This article examines needs assessments and their accompanying implementation plans across a large university hospital system and finds support for conducting assessments at the local site-level but evidence that system-wide approaches may also have significant benefits, especially at the implementation phase. It suggests a hybrid approach to the needs assessment process where systems and their individual hospitals work together to maximize health benefits to the communities served.
Introduction
Since the inception of the 2010 Patient Protection and Affordable Care Act's (ACA's) requirement for non-profit hospitals to conduct Community Health Needs Assessments (CHNAs) every 3 years, most hospitals should have completed at least two cycles of identifying health needs in the community, developing implementation plans, and working to improve the health of their local service areas. Large hospital systems, made up of multiple individual hospital locations, have differed in their approach to conducting these CHNAs. Some have completed one CHNA report and its accompanying implementation plan for all hospitals within the system whereas others have completed CHNA and implementation plans for each individual hospital within a system. The 2010 ACA required non-profit hospitals across the United States to complete Community Health Needs Assessments whereby the hospital gathers community input and examines other data sources to identify the most important public health issues facing their service areas. After identification, hospitals must choose health issues to prioritize and create implementation strategies to address those needs. This requirement is tied directly to the tax-exempt status of hospitals and must be completed every 3 years ( 1 ). Activities related to the CHNA implementation plan are reported on the Internal Revenue Service Form 990. Prior literature has indicated the wide variation of quality among CHNAs, ( 2 ) including a lack fo consistency in method and content ( 3 ).
While community benefit has been notoriously hard to capture by non-profit hospitals, it was estimated that spending in 2012 was over 60 billion dollars in the United States ( 4 ). This enormous influx of money, part of which should now be directed toward significant public health need in communities served by these hospitals, underscores the importance of further understanding best practices for CHNA processes and the need for clarity and consistency in CHNA reporting ( 5 ). There is wide variation in the amount of this spending across hospitals, and while research has shown that prior to the CHNA act much of this spending was patient-care related ( 6 ), there is also some variation in how sites have moved this toward higher community benefit spending, tied directly to the level of CHNA implementation planning ( 7 ).
In light of these large sums of public health spending, the CHNA process has potential to be an important mechanism for improving public health at the population level and addressing systemic and environmental factors, including social determinants of health, that have proven to be difficult problems for public health practitioners to solve ( 8 ). Over the past decade there has been a tremendous growth in both the number of hospital systems (more than one hospital formally affiliated with each other) and the number of independent hospitals who have moved toward affiliation with a system ( 9 ). Hospital systems have the potential to reach large populations with both healthcare services and public health interventions through the CHNA process. Systems generally complete separate reports for each site affiliated with the hospital system, although in some cases system reports combine one or more sites into one report ( 10 ). The presence of one overarching report summarizing needs and implementation strategies across all sites within systems also varies from system to system.
Research has pointed to the importance of collaboration across hospital systems ( 11 ) and between hospitals and community partners, both through input from the public ( 12 – 14 ) and with local stakeholders such as health departments ( 15 ). The literature also emphasizes that increasing the scope of collaboration can help increase the resources brought to bear on projects and the benefits of expanded partnerships ( 11 ) and regional coordination ( 16 ). Potential areas where hospitals and other public partners could share needs assessment data have also been highlighted ( 3 ). Using the West Virginia University Medicine hospital system, we identify the variation in responses to the health needs identified by each local hospital siteindependently and determine which health needs were prioritized by each. Further, we attempt to cross-reference implementation strategies across each and discuss the potential for intra-system overlap and collaboration. The findings here, which will lead to a system-wide plan for the specific hospital system, also hold lessons learned for other hospitals who are a part of a larger healthcare system, but potentially also for hospitals who could coordinate or collaborate with other regional hospitals and community partners to extend resource availability for implementation around common public health goals.
Materials and Methods
We examined eight hospitals within the West Virginia University Medicine system who went through a nearly-identical process of CHNA within the past 5 years. Table 1 describes each hospital.
Descriptive statistics of eight hospitals affiliated with the WVU medicine system.
For each hospital we indexed all needs prioritized (prioritized needs were not given in order of importance in the reports) and each implementation strategy chosen by the hospital. We adopted the Healthy People 2020 ( 17 ) list of social and physical determinants of health and coded each hospital implementation strategy into one of the following categories as subcategories of each identified need (obesity strategies, substance abuse strategies, etc.): Social Determinants included:
- Availability of resources to meet daily needs (e.g., safe housing and local food markets)
- Access to educational, economic, and job opportunities
- Access to health care services
- Quality of education and job training
- Availability of community-based resources in support of community living and opportunities for recreational and leisure-time activities
- Transportation options
- Public safety
- Social support
- Social norms and attitudes (e.g., discrimination, racism, and distrust of government)
- Exposure to crime, violence, and social disorder (e.g., presence of trash and lack of cooperation in a community)
- Socioeconomic conditions (e.g., concentrated poverty and the stressful conditions that accompany it)
- Residential segregation
- Language/Literacy
- Access to mass media and emerging technologies (e.g., cell phones, the Internet, and social media)
Physical determinants included:
- Natural environment, such as green space (e.g., trees and grass) or weather (e.g., climate change)
- Built environment, such as buildings, sidewalks, bike lanes, and roads
- Worksites, schools, and recreational settings
- Housing and community design
- Exposure to toxic substances and other physical hazards
- Physical barriers, especially for people with disabilities
- Aesthetic elements (e.g., good lighting, trees, and benches).
Results are presented as % of hospitals who identified and prioritized each need ( Table 2 ) and the number of strategies addressing each need across the system stratified by physical and social determinants of health ( Table 3 ). Since hospitals chose differing numbers of health needs to prioritize and differing numbers of strategies to address each need, the implementation planning numbers in Table 3 can represent more than one strategy within a hospital.
Health needs prioritized by hospitals in the WVU medicine system.
Implementation strategies chosen by hospitals for each prioritized need.
Our scan of CHNAs in the West Virginia University Medicine system indicates substantial overlap in the needs chosen by each hospital in the system. Only six total issues were identified and prioritized across all eight hospitals, with each hospital generally choosing 2–4 strategies each. More than half of the hospitals chose obesity and related disease, cancer, and substance abuse issues indicating these are significant issues across large portions of the system. Three issues (smoking and related disease, access to care, and mental health), however, were chosen by only a few hospitals. These results indicate that there are both substantial overlaps within communities but also strengthen the idea that needs assessment should be done at the local level and not just across the system to identify needs that might exist within smaller pockets of a system's service area and might be best served by an individual hospital site rather than leveraging system resources. A combination of local level data collection [especially considering the need to link local population health data and rankings to the needs selected by individual hospitals ( 18 )] and CHNA reports and a system-wide reporting and implementation planning mechanism would be a strong combination for healthcare systems looking to have an impact on large-scale population health. These findings reiterate findings in the literature speaking to the importance of regional planning for community benefit ( 16 ).
Turning to implementation planning, strategies to address needs varied considerably from site to site. This may be a result of the large differences found within the population size of service areas, the geographic reach of the service areas, and the size of hospital (illustrated in Table 1 by the number of beds) which may also indicate the level of resources available at the local level. As implementation efforts continue, it is important to conduct evaluation of the impact of these efforts to determine which have a substantial impact on the needs identified within the communities. The overall hospital system is in a key position to communicate successful and unsuccessful efforts across the system and leverage additional resources toward successful interventions in order to have a stronger impact on the public health of hospital service areas. This may be especially true if resource-intensive strategies to address health concerns are evaluated and seen to have a larger impact. Small (and largely rural) sites may not have the ability to replicate successes of large hospitals due to lack of resources ( 19 ).
Across the system, the vast majority (96.6%) of implementation strategies addressed social determinants of health. Only two strategies addressed physical determinants of health. We hypothesize this may be a result of individual sites thinking about minimal resources they may have to leverage toward significant health issues. Coordinating a response across the system may increase the ability to address physical determinants of health, especially with the issue of obesity and related chronic diseases. At the same time, there may be other factors that keep hospitals from pursuing strategies related to physical determinants of health ( 20 ), so this issue may require more in-depth study.
These findings also point to a need to replicate a study such as the one conducted by Pennel, et al. ( 2 ) to revisit quality of CHNAs across individual hospitals. Further study could also scope out the varied ways systems are reporting individual site needs, implementation strategies, and how many are combining these into an overall system report.
The major limitation of this study was the ability to look at needs identified and priorities selected only among one hospital system. Further, the community health needs assessments and implementation plans were not all conducted by the same individuals or reported in the same format so there was some variation across plans that were compared.
The results presented above demonstrate both the need for individual sites to conduct their own community health needs assessments to identify unique local health issues, but also suggest there may bestrength in a system-wide approach to addressing common regional health needs. Moving forward, hospitals should consider a system-wide report that breaks down individual sites and looks at where the system could have the most impact on significant needs across its population served. Systems could leverage their larger regional resources to help shape the CHNA process developed by the ACA into a powerful public health tool.
Data Availability Statement
Author contributions.
TB took the lead authorship on this manuscript including the conceptual idea for the manuscript, initial drafting, and majority of writing content. ES developed the data for the tables, conducted the data collection, and assisted with overall writing. CA assisted with conceptualizing the tables, wrote portions of the discussion section, and further developed the determinants of health methodology.
Conflict of Interest
All authors are employees of West Virginia University. The authors have been contracted through the West Virginia University Hospital System to conduct Community Health Needs Assessments in the past and present. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. Funding for the publication fees was paid by the West Virginia University Health Research Center.

Learn if your company is eligible for NIH SBIR or STTR funding, how to apply , and what to expect during each step of the application process. Multiple registrations are required to prepare your application and apply for funding.
- Understanding SBIR and STTR
- Eligibility Criteria
- Grants Policy
- Foreign Disclosure and Risk Management
- SBIR and STTR Grants (NOFO s )
- SBIR Contract Solicitations
- Commercialization Readiness Pilot (CRP)
- Supplemental Funding to Diversify the Entpreneurial Workforce
- How to Apply
- Transition Award (Coming Soon)
Our team can help you maximize the benefits from NIH programs and resources which help you bring your innovations to life.
- TABA Funding
- TABA Needs Assessment
- Pitch Coaching
- SOW Development
- Reimbursement
Explore the benefits of public-private partnership in NIH’s nationwide network of innovators who convert academic discoveries into healthcare solutions.
The NIH is actively turning discovery into health by helping small businesses develop innovative technologies that improve health and save lives. See how .
- Search Technologies from Academic Centers and Hubs
We value diverse perspectives in biomedical innovation and strive to empower scientists and entrepreneurs to bring their discoveries to patients.
- Contact the SEED Team
- Who to Contact and When
- HHS Small Business Program Managers
Technical and Business Assistance (TABA) Needs Assessment
The TABA Needs Assessment Report provides a third-party, unbiased assessment of a Phase I project’s progress in technical and business areas that are critical to success in the competitive healthcare marketplace. There is no cost for this report and the time commitment for participation is minimal.
The Needs Assessment Report helps companies strategize for the project’s next steps. It analyzes the current state of your Phase I project and identifies strengths and weaknesses across four categories. The information in each report will be tailored to the participating company’s project, but the structure and scope of the report are fixed. View a sample Needs Assessment Report .
Intellectual Property/Barriers to Entry
Market & Competitive Awareness
Regulatory, Manufacturing, and/or Clinical Plan
Business Model Profitability
Note: Needs Assessment Reports identify gaps in the four above areas, they do not fill those gaps with knowledge or provide needed data. After receiving the Report, companies are advised to work with their Small Business Program Manager and/or Program Official to identify resources or programs to move their project to the next step.
Why request a TABA Needs Assessment?
Many companies utilize their Needs Assessments to inform their commercialization plan and/or TABA Funding budget for their SBIR/STTR Phase II application, and/or other funding opportunities. For companies that plan to use the Report for their Phase II application, we recommend submitting a request at least 6 months ahead of the Phase II proposal deadline to allow enough time to fully leverage the Report.
Companies that already submitted Phase II applications have used their report to review and adjust their strategies as necessary.
Eligibility
Your company is eligible to participate if your Phase I NIH SBIR or STTR (grant, contract, or Fast-Track)
- Is active or was active within the past two years AND
- Was not awarded TABA funding within the Phase I award budget AND
- Has not already received a TABA Needs Assessment Report or NICHE Assessment for the same Phase I project
Questions? Email [email protected] .
Request a Needs Assessment Report
The TABA Needs Assessment Report is provided by RTI Innovation Advisors through an NIH contract. Recommendations from RTI Innovation Advisors do not represent the views of NIH or NIH staff.

Stay in the Loop
Subscribe to our mailing list for updates on deadlines and important information.
- Small Business Funding
- Product Development Support
- Entrepreneurial Training
- Resources and Events
Fraud, Waste and Abuse
- Report Fraud
HHS Vulnerability Disclosure | Technical Issues: E-mail OER Webmaster

- Open access
- Published: 17 January 2023
A scoping review of community health needs and assets assessment: concepts, rationale, tools and uses
- Hamid Ravaghi 1 ,
- Ann-Lise Guisset 2 ,
- Samar Elfeky 3 ,
- Naima Nasir 4 ,
- Sedigheh Khani 5 ,
- Elham Ahmadnezhad 6 &
- Zhaleh Abdi 7
BMC Health Services Research volume 23 , Article number: 44 ( 2023 ) Cite this article
23k Accesses
14 Citations
2 Altmetric
Metrics details
Community health needs and assets assessment is a means of identifying and describing community health needs and resources, serving as a mechanism to gain the necessary information to make informed choices about community health. The current review of the literature was performed in order to shed more light on concepts, rationale, tools and uses of community health needs and assets assessment.
We conducted a scoping review of the literature published in English using PubMed, Embase, Scopus, Web of Science, PDQ evidence, NIH database, Cochrane library, CDC library, Trip, and Global Health Library databases until March 2021.
A total of 169 articles including both empirical papers and theoretical and conceptual work were ultimately retained for analysis. Relevant concepts were examined guided by a conceptual framework. The empirical papers were dominantly conducted in the United States. Qualitative, quantitative and mixed-method approaches were used to collect data on community health needs and assets, with an increasing trend of using mixed-method approaches. Almost half of the included empirical studies used participatory approaches to incorporate community inputs into the process.
Our findings highlight the need for having holistic approaches to assess community’s health needs focusing on physical, mental and social wellbeing, along with considering the broader systems factors and structural challenges to individual and population health. Furthermore, the findings emphasize assessing community health assets as an integral component of the process, beginning foremost with community capabilities and knowledge. There has been a trend toward using mixed-methods approaches to conduct the assessment in recent years that led to the inclusion of the voices of all community members, particularly vulnerable and disadvantaged groups. A notable gap in the existing literature is the lack of long-term or longitudinal–assessment of the community health needs assessment impacts.
Peer Review reports
The population-based health approach aims to improve the population’s health, promote community resilience and reduce health inequities across the socioeconomic gradient via inter-sectoral partnerships among community groups, government, healthcare systems, and other stakeholders [ 1 ]. One key feature for adopting a population-based health approach is to ensure that it is grounded on a solid understanding of community health needs and assets by triangulating evidence from service providers and community members on services availability, accessibility, utilization and experience [ 2 , 3 ]. The process of identification of unmet health needs in a population is crucial for local authorities seeking to plan appropriate and effective programmes to meet these needs [ 3 , 4 ]. If these needs are ignored, then there is a risk of a top-down approach for providing health services, reflecting what a few people perceive to be the needs of the population rather than what they actually are [ 4 , 5 ].
In this context, community health needs assessment is a means of developing a comprehensive understanding of a community’s health and health needs as well as designing interventions to improve community health [ 6 ]. Though the process of community health needs assessment can be conducted in several ways, the primary purpose is to provide community leaders or healthcare providers with an overview of local policy, systems, and environmental change strategies currently in place and help to identify areas for improvement [ 7 ]. Community health needs assessment can provide them with a more nuanced understanding of the communities they serve, making them aware of pressing issues that require system-level changes and support their efforts for resource mobilization to initiate innovative programmes [ 8 , 9 ]. The process to gather evidence on community health needs can also serve as a springboard to strengthen community engagement [ 10 ].
In general, needs assessments are usually designed to evaluate gaps between current situations and desired outcomes, along with possible solutions to address the gaps. Recently, there has been a trend to move away from framing a community with a deficit perspective (need-based approach) to focus on community assets and resources, called community health needs and assets assessment [ 11 , 12 ]. In contrast to a need-based perspective which focuses on local deficits and resources outside the community, an asset-based perspective focuses on honing and leveraging existing strengths within the community to address community needs [ 12 , 13 , 14 ].
Studies have shown that community health needs assessment is used widely by different users and across different settings [ 15 , 16 ]. However, these studies varied widely in terms of purpose, process and methods of conducting community health needs assessment. Furthermore, the extent to which an asset-based approach is used is unclear, beyond the inclusion in guidance and recommendations. Thus, to support national or local decision-makers to make informed choices about the scope, tools, methods and use of community health needs and assets assessment, this scoping review of the literature aimed at: 1) Providing conceptual clarity on community health needs and assets assessment, 2) Determining for what purpose and with what methods community health needs and assets assessment are used globally, 3) Drawing the lessons learnt from previous experience with community health needs and assets assessment: what works in what context and under what conditions, 4) Documenting evidence of impact of community health needs and assets assessment, 5) Consolidating tools and methods used to collect evidence/data underpinning community health needs and assets assessment processes.
Search strategy
Ten databases, including PubMed, Embase, Scopus, Web of Science, PDQ evidence, NIH database, Cochrane library, CDC library, Trip, and Global Health Library were searched in February and March 2021. The search strategy was developed through discussion with experts in the field of population health, a research librarian, and a narrative review of the literature. Preliminary search terms were developed by the research team to reflect a number of core concepts including needs, population, needs assessment, assets assessment and participation. The search process was performed by a librarian with expertise in the use of literature databases (SK). The search terms were pilot-tested and agreed upon within the research team. The PubMed database search strategy presented in Additional file 1 .
Inclusion and exclusion criteria
Studies that focus on community health needs and assets assessment in terms of concepts, rationale, uses and tools were considered in both high-income countries (HICs) and low-and middle-income counties (LIMCs). We included studies in the review if they met the following criteria: 1) Papers providing conceptual clarity and explaining rationale for community health needs and (assets) assessment (This can be articles describing community health needs assessment or community assets assessment or community health needs and assets assessments at the same time or separately). The terms capabilities/ strengths/ resources can be used in place of assets and were considered.); 2) Papers describing or evaluating experiences implementing community health needs (and assets) assessment in a single site or multiple sites; 3) Methodological papers describing tools/approaches for community health needs (and assets) assessment; 4) Review of the literature on community health needs (and assets) assessment.
Types of papers not include in the review were: 1) Studies without a clear description of the community health needs and (assets) assessment methods, 2) Studies assessed a single dimension (i.e. health outcomes only, or healthcare providers’ capabilities only such as patient surveys, health outcomes dashboard, health facility assessment), 3) Studies related to a single disease or programme, 4) Studies focused only on engaging individual patient in their own care, and 5) Studies were not in English.
Three reviewers participated in the selection of the relevant studies (HR, ZA, NN). The eligibility and relevance of the articles were determined by two reviewers independently using the above predefined criteria. In the event of disagreement, a consensus was found between all the reviewers about the status of the article.
Data extraction
Separate data extraction forms were developed for the extraction of the three main categories of papers: conceptual, empirical and review papers. Totally, 121 empirical papers (including 6 review papers) and 48 conceptual and methodological papers were reviewed. Following topics were extracted for empirical papers: 1) General characteristics including author(s), year of publication, country of implementation, study objective(s) and study method; 2) Community health needs and (assets) assessment framing including rational, definitions of community health needs and (assets) assessment/ needs/ assets/ community, initiator(s) or user(s) of the process; 3) Key steps of the process, collected data, data collection tools; 4) Community engagement and the level of engagement; 5) Use of community health needs and (assets) assessment findings, impact of community health needs and (assets) assessment; 6) Facilitators and barriers. Data extraction forms are presented in Additional file 2 .
Data extraction forms were pilot-tested prior to the implementation. Two authors (ZA, HR) independently performed a pilot data extraction of a random sample of ten original articles. After piloting, the authors assessed the extracted data in relation to the scoping review questions and revised them accordingly. The content of the form was finalized by discussion within the team. Regarding conceptual papers, two authors (NN and ZA) initially extracted data from three randomly selected papers and subsequently refined and amended the form having research team inputs.
Four reviewers extracted included studies independently. The data extracted were cross-checked by one of the authors and mutual consensus resolved discrepancies. Individual data extraction forms of empirical papers were then merged into a single, unifying document used for the interpretation and presentation of the results. Following typical scoping review methods, the methodological quality of the included articles was not assessed systematically, however, only peer-reviewed articles were included in our review process [ 17 ].
Synthesis of results
Following reading and extracting conceptual papers, a preliminary conceptual framework (Fig. 1 ) was developed and discussed and agreed upon by team members. The integrative synthesis of the evidence was employed. Specifically, it involved the narrative description of concepts and definitions, key steps of the community health needs assessment and barriers and facilitators of the implementing community health needs assessment.
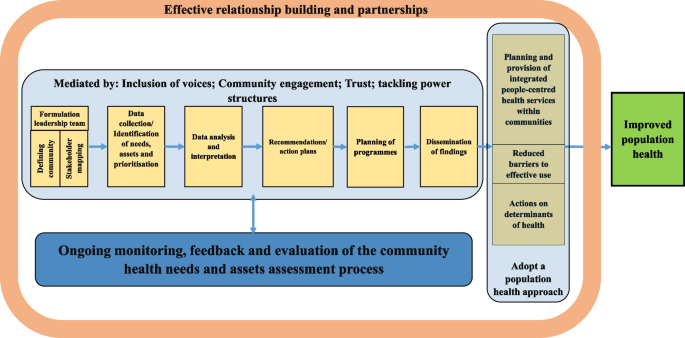
Conceptual framework of the review
The study selection process is summarized in Fig. 2 . Just over 12,000 records were obtained from the ten databases searched. Articles with obviously irrelevant titles were excluded, as were news items, letters, editorials, book reviews, and articles appearing in newsletters or magazines rather than peer review journals. The remaining abstracts were retrieved, read and assessed. A total of 169 articles including both empirical papers and theoretical and conceptual work were ultimately retained for analysis. A list of all studies with a short description, including the year of publication, key focus, study period, and methods, is presented in Additional files 3 and 4 . The first part of the results section focuses on definitions and concepts of community health needs assessment using both conceptual and empirical papers. In the second part of the results section, we describe key steps of the community health needs assessment and tools and methods used to collect data through content analysis of 121 included empirical papers. We also report some important challenges and facilitators faced by included studies while performing community health needs assessment. Role of community participation in the process and the spectrum and types of the participation is discussed in the last part.
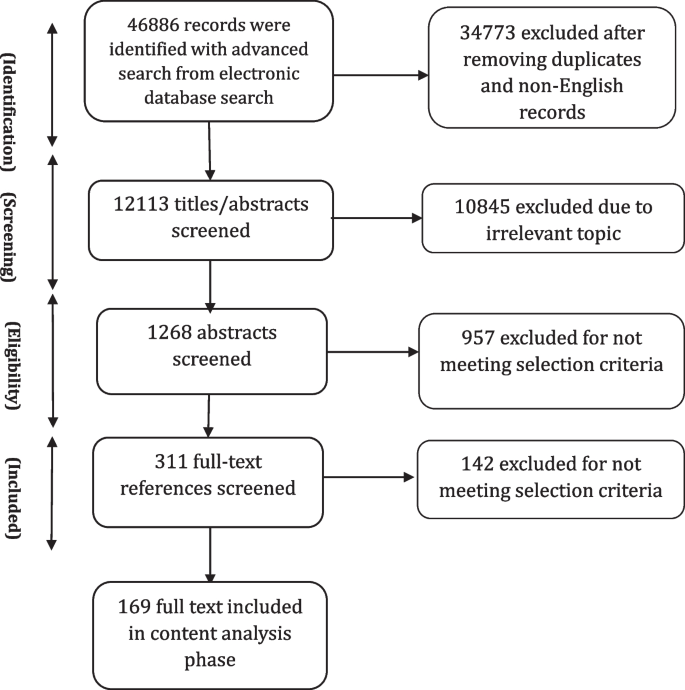
Information flow in scoping review
General characteristics of the included studies
The review showed that community health needs assessment is used widely by different users and across different settings in both HICs and LMICs. Among included empirical studies, 81 (out of 121) were conducted in the United States (US). There were papers from Australia ( n = 4), South Africa ( n = 3), Kenya ( n = 3), Uinted Kingdom (UK) ( n = 2), Canada ( n = 2), China ( n = 2), Dominican Republic ( n = 2), Republic of Ireland ( n = 2), Iran ( n = 2), India (2), Honduras ( n = 1), Netherland ( n = 1), Vietnam ( n = 1), Sudan ( n = 1), New Zealand ( n = 1), Madagascar ( n = 1), Malaysia ( n = 1), Ecuador ( n = 1), Indonesia ( n = 1), Uganda ( n = 1), Taiwan ( n = 1), Kyrgyzstan ( n = 1), Saudi Arabia ( n = 1), Haiti ( n = 1), Honduras ( n = 1) and Korea ( n = 1).
Definition of needs
The review showed “need” was a multi-faceted concept with no universal definition. There was a differentiation between “health need” and “healthcare need” in the reviewed literature. Healthcare needs can benefit from health care (health education, disease prevention, diagnosis, treatment, rehabilitation and terminal care). Healthcare providers usually consider needs in terms of healthcare services that they can supply. However, health needs incorporate the wider social and environmental determinants of health, such as deprivation, housing, diet, education and employment. This broader definition allows looking beyond the confines of the medical model based on health services, to the wider influences on health [ 3 ].
In this review, relatively few empirical studies focus narrowly on healthcare needs, without attention to other determinants of health that can affect health [ 18 , 19 , 20 , 21 , 22 , 23 ]. Most of the included empirical studies looked beyond “physical health needs” to consider wider “social determinants of health” or non-medical factors that can affect a person’s overall health and health outcomes as the conditions—shaped by political, social, and economic forces—in which people are born, grow, live, work, and age [ 24 ]. Notably, the need was recognised as a “dynamic concept” whose definition will vary with time according to context and resources available to address these needs [ 16 ].
Definition of community
In general, “community” has been defined as “people with a basis of common interests and network of personal interactions grouped either based on locality or on a specific shared concerns or both” [ 25 ]. Shared common interests are particularly important as they can be assessed and, hopefully, met at a community level [ 26 ]. Importantly, community is a dynamic concept as individuals can belong to several communities at various times. In our review, community was defined by included studies, particularly those initiated by local authorities or healthcare providers (e.g., hospitals), based on geographical indicators such as county designations or based on the location of the hospital’s/facility’s/authority’s existing or potential service users. Some included empirical studies considered community based on shared interests or characteristics such as race/ethnicity, sexual orientation, or occupation. Medically underserved populations including rural areas [ 27 , 28 , 29 , 30 ], impoverished urban sectors [ 31 ], the homeless [ 32 , 33 , 34 , 35 ], persons in poverty or of low socioeconomic status, vulnerable children and families [ 18 , 28 , 36 , 37 , 38 ], the elderly [ 8 , 39 , 40 , 41 , 42 ], women and girls [ 43 , 44 , 45 , 46 , 47 ], LGBT (Lesbian, gay, bisexual, and transgender) individuals [ 48 , 49 , 50 , 51 ], displaced populations, immigrants and racial, ethnic and religious minority groups [ 12 , 19 , 36 , 42 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 ] and persons with severe and chronic health problems [ 79 ] were considered as a “community” by a number of included studies.
While defining community, a number of its characteristics were determined by included studies including: history, existing groups, physical aspects (i.e. geographic location, community size, its topography and etc.), infrastructure (i.e. health and social care facilities, public transportation, roads, bridges, electricity, mobile telephone services and etc.), demographics (i.e. age, gender, race and ethnicity, marital status, education, number of people in household, first language and etc.), economic conditions, deprivation and/or inequalities, government/politics, community leaders (formal and informal), community culture (formal and informal), existing institutions, crime and community safety, lifestyle and leisure, general health problems and epidemiology.
In our review, community health needs and assets assessment were performed by different organizations as the first step in community health promotion planning, including local health authorities (district/local), community entities [i.e. non-governmental organizations (NGOs), civil society organizations (CSOs), faith-based organizations (FBOs), community-based organizations (CBOs)] and hospitals (public/private). Included studies mostly conducted health needs assessment at the local level (e.g. cities, counties, or other municipalities). The broader understanding of health and its determinants suggests that many public and private entities have a stake in or can affect the community’s health. To engage stakeholders in the process, a number of included empirical studies ( n = 56, 49%) sought representatives from the community that were best positioned to speak about community health based on their specific knowledge or line of work. These stakeholders were individuals from community and entities who may explicitly be concerned with health or not, which varied by the community context and culture. To have a comprehensive overview of a community needs, it was asserted that defining communities needs to be dynamic and socially constructed to take into account all voices and members, especially those not ordinarily included [ 80 ]. Community should be defined in a manner that does not exclude medically underserved, low-income, or minority populations. Integrating community voices is especially important in designing plans and programmes aimed at reducing health disparities in the community [ 58 , 81 , 82 ].
Definition of assets
Overall, there were limited definitions for “community assets” in the reviewed literature. Assets were described as resources, places, businesses, organizations, and people that can be mobilized to improve the community [ 11 , 83 ]. This includes members of the community themselves and their capabilities. Assets can therefore be described as the collective resources which individuals and communities have at their disposal, which protect against adverse health outcomes and promote health status [ 83 , 84 ].
Of 115 included empirical studies, 30 studies addressed community assets while performing community health needs assessment. A wide range of assets, from tangible resources to intangible ones, were considered that can be classified into seven broad categories as follows:
Community demographic characteristics: Literacy rates [ 13 ], youth population [ 58 , 68 ], and elderly population [ 68 ];
Natural capitals: Geographical location and natural resources [ 21 , 81 , 85 ];
Economic and financial capitals: Community business [ 12 , 81 ] community members’ income [ 21 ], and housing land ownership [ 13 ];
Community infrastructure: Level of technology/mobile phone coverage [ 13 , 21 ], transportation [ 86 ], parks and sidewalks [ 12 ], sport and recreational facilities [ 31 , 87 , 88 ], public libraries and community centres [ 88 ];
Community social and educational facilities: Non-profit and non-governmental organizations [ 59 , 87 ], media [ 89 ], educational institutions [ 12 , 31 , 81 , 90 ], faith communities [ 58 , 81 , 90 ], and community associations [ 31 ];
Community health and social facilities: Health and social facilities and providers [ 72 , 81 , 85 , 86 , 89 ], traditional medicine providers [ 72 ], and ongoing health programmes [ 13 , 87 ];
Community’s social and cultural values and resources: Tribal and community culture [ 58 , 68 , 74 , 91 ], cultural diversity [ 81 ], spirituality and religion [ 58 , 74 ], strong family bonds and values [ 59 , 74 ], strong community connections, teamwork and willingness to volunteer [ 21 , 81 , 86 , 91 ], mutual support, social support and networks [ 45 , 58 , 81 , 85 ], unity, community cohesion and collectivity [ 21 , 59 , 74 ], community capacity [ 58 ], community-led activities [ 86 , 91 ], and community values and traditions [ 68 , 74 , 86 ], resiliency [ 58 ], unifying power of communities [ 13 ], community administration units e.g. women’s committees [ 13 ], an existing group of dedicated healthcare providers [ 39 ], a group of concerned citizens [ 39 ], community safety [ 12 ], the knowledge base of the community members themselves [ 39 ] and members’ desire to be healthy [ 58 ].
Various qualitative methods such as individual interviews (one-on-one structured conversations) or focus groups (guided, structured, small group discussions) with community members, or key informants’ interviews (formal and informal conversations with leaders and stakeholder groups) or a combination of these methods were reported as the main methods to collect information on community’s assets among reviewed studies. Of these, focus group was the widely used method in community assets assessment [ 8 , 21 , 31 , 45 , 58 , 59 , 67 , 81 , 82 , 85 , 87 , 90 , 92 , 93 ].
Definition of community health needs (and assets) assessment
The terms “Community Needs Assessment (CNA)”, “Community Health Needs Assessment (CHNA)”, and “Community Health Needs and Assets Assessment (CHNAA)” were used interchangeably in the literature referring to the process of identifying health needs (and assets) of a given community. Since this review focuses on both community needs and assets, we will use the CHNAA term for the description of the process in this paper.
None of the papers reviewed provided a specific definition for CHNAA. In general, reviewed papers defined CHNAA as: A collaborative, community-engaged, systematic, ongoing, continuous, proactive, comprehensive, cyclical, regular, modifying method or process [ 28 , 33 , 69 , 92 , 94 , 95 , 96 , 97 , 98 ]; For the identification, collection, assembly, analysis, distribution, and dissemination of information on key health needs, social needs, concerns, problems, gaps, issues, factors, capabilities, strengths, assets, resources; About communities (or individuals) [ 21 , 23 , 28 , 31 , 33 , 37 , 41 , 45 , 54 , 79 , 89 , 94 , 95 , 96 , 97 , 99 , 100 , 101 , 102 ]; To achieve agreed priorities, create a shared vision, plan actions, garner resources, engage stakeholders, work collaboratively, establish relationships, implement culturally appropriate, multi-sectoral/multilevel intervention strategies, empower residents and enhance community capacity and participation in decision-making process [ 12 , 13 , 20 , 27 , 28 , 37 , 45 , 70 , 79 , 89 , 91 , 92 , 94 , 95 , 97 , 98 , 99 , 101 , 102 , 103 , 104 ]; Towards improving health and wellbeing, building and transforming health of the communities, increasing community benefits, reducing inequalities; Through which primary/secondary healthcare can respond to local and national priorities [ 20 , 23 , 28 , 40 , 51 , 59 , 69 , 97 , 103 , 105 , 106 ].
The included studies listed a number of reasons as the rationale for conducting CHNAA. Legislative requirements were most cited as the main rational for conducting CHNAA, particularly among studies conducted in the UK and US. Since the late 1980s, the concept of health needs assessment has gained increasing prominence within the National Health Service (NHS) in the UK. This has been prompted by a series of policy initiatives requiring health facilities to assess needs of their populations and to use these assessments to set priorities to improve the health of their local population [ 107 , 108 ]. In the US, several national, federal, state, and local funding sources require entities to conduct CHNAA to demonstrate a significant need for their services and programmes to be funded. The most important one is Patient Protection and Affordable Care Act (ACA-2010), requiring non-profit hospitals as tax-exempt entities to perform CHNAAs to maintain non-profit status regularly [ 92 ]. Other reasons were mentioned by included studies as the rationales for conducting CHNAA were: lack of information of health needs of a specific community, to facilitate health research and related interventions in a community, to inform the design of contextually relevant programmes and policies, to develop community health improvement plans or health promotion interventions, to develop or update strategic plans, and to receive resources and funds.
Key steps to conduct CHNAA
The number and nature of CHNAA process steps varied among reviewed studies. However, broadly CHNAAs involved six main steps as follow:
Formulation of a leadership team
Forming a leadership team, which was called by different names such as the steering committee/ the research advisory committee (RAC)/ the collaborative task force/ or the community advisory board (CAB), was known as the preliminary step of a CHNAA process. The steering committee was usually composed of local representatives from local agencies and organizations (e.g. non-profit organizations, community service agencies, media outlets, county and municipal governments, colleges and universities, faith-based organizations, and healthcare providers), community members, community stakeholders and leaders, academic partners, health and social officials, and representatives from the investigator body to help guide the development of the CHNAA project.
Leadership team responsibilities were reported as providing inputs on the research purpose, selecting and verifying study methodology and design, providing inputs and feedback on initial survey/topic content and selecting final survey/ topic guide questions, reviewing survey/topic guide length, and ensuring culturally relevant and resonant wording, comprehension and face validity, and monitoring the progress of the data collection. Feedback and recommendations from the steering committee were incorporated throughout the CHNAA process as well. Steering committees usually met on a regular basis.
Identification of needs, assets and prioritisation
To collect information on community health, needs and assets, both primary and secondary data were utilized by included studies. Secondary data included information on community socio-demographic and indicators on health status, access, utilization and satisfaction with health and social services at different levels (e.g. community, sub-national and national) to develop a picture of the overall community health. Primary data were collected through quantitative and qualitative methods and mixed-methods approaches.
Quantitative studies
Some empirical studies used individual/household surveys as the only source to identify community needs and concerns ( n = 28, 24.%). Surveys were a popular method of gathering opinions, preferences and perceptions of needs. Needs assessment surveys typically have written, closed-ended questions filled through the interview (face to face/telephone) or self-completion (paper or online) by community members. Generally, two main kinds of surveys were used by included studies: a) community health assessment survey, and b) community concerns survey. A number of included studies used health assessment surveys as the key data sources of the CHNAA process ( n = 22, 19%) or along with other types of data, mainly qualitative data ( n = 21, 18.%). Health assessment surveys typically collected information on demographics, socio-economic variables, respondents’ health status, choice of healthcare providers, and healthcare access issues among community members. Survey questionnaires were mostly developed with inputs from the literature review (similar health assessment surveys conducted at the local or national level), community members and project team discussions. Additional file 5 shows the most important data and indicators collected by included studies through conducting community health assessment surveys.
Another form of surveys, used alone or in combination with qualitative methods ( n = 15, 13.5%), was the community concerns survey in which people (community members and/or key informants) are asked to help identify what they see as the most important issues facing their community leading to an inventory of their health priorities [ 12 , 20 , 23 , 27 , 29 , 55 , 69 , 74 , 101 , 103 , 109 , 110 , 111 , 112 , 113 ]. A straightforward way to estimate the needs of a community was to simply ask residents their opinion on what particular services are most needed in the community. The focus of this methodology was to create an agenda based on the perceived needs and concerns of community residents. The concerns surveys were based on either focus group discussion with community members and experts or literature review by the researchers or both. Generally, while filling community concerns survey, individuals were asked to rate the importance of each issue in their community on a scale (e.g. 0 = not important, 5 = extremely important) [ 23 , 27 , 29 , 55 , 74 , 110 ]. Participants could also add and rate concerns or service needs that were not listed. Finally, each health problem identified by the community was weighted based on the frequency it was selected on the survey.
General coverage of the surveys was the population aged 18 or over currently residing in the community for a minimum period of time (at least a few months) and able to provide consent for participation. Most surveys were written, closed-ended questions filled through face to face or telephone interviews or self-completion by community members. In addition to the paper-form survey, some studies used email and social media platforms to allow residents to anonymously complete online surveys [ 29 , 51 , 57 , 96 , 103 , 110 , 114 ]. A few studies reported that residents received monetary or nonmonetary incentives for their participation upon survey completion [ 19 , 71 , 74 , 77 , 110 ]. Sampling techniques commonly used are those that promote participation in CHNAAs such as convenience sampling [ 20 , 35 , 40 , 51 , 52 , 57 , 64 , 65 , 71 , 74 , 75 , 77 , 86 , 96 , 101 , 103 , 104 , 110 , 114 , 115 ]. Only a few studies used random sampling or demonstrated the representativeness of their samples. Their response rates varied between 8 to 95.5%. Most surveys recruited local surveyors and provided them with research training to ensure consistent survey administration to attract community participation. Some studies that assessed health needs among immigrant communities or minority groups recruited bilingual surveyors or/and provided participants with two versions of the instruments, one in the native language to maximize community engagement [ 12 , 27 , 52 , 65 , 71 , 86 , 103 ]. Surveys that took a participatory approach to the design, content, terminology, and language level, were reported more understandable and culturally relevant to the community members [ 52 , 65 , 75 ].
Health needs assessment surveys (both concerns surveys and health assessment surveys) reported limitations to data collection based on the assessment timing, data availability, and sample response. As said earlier, using a convenience sampling and non-representative samples, small sample size and inter-rater reliability between surveyors were among some important methodological limitations reported by these studies, which limited the generalisability of the study findings to the entire community population [ 35 , 57 , 65 , 71 , 74 , 75 , 77 , 96 , 106 , 116 ]. Convenience sampling method and using community events as sampling sites led to sampling bias in some studies (e.g., an over-representation of some specific groups of the population such as women and low –income or high-income groups) [ 57 , 63 , 65 , 66 , 71 , 74 , 75 , 78 , 103 , 114 , 115 ].
Qualitative studies
Among included studies, about 34% ( n = 39) used qualitative methods as the main source of data collection on community needs and assets. Some of these studies justified the use of qualitative approach by explaining how the overreliance on quantitative, population-level data resulted in CHNAAs failing to identify health needs and interests of all community members, particularly those of vulnerable population and underrepresented marginalized segments of the community. In addition, these studies concluded that integrating qualitative methods into the CHNAA process has the potential to involve community members in a more participatory fashion, perhaps improving future collaborations between communities and service providers. Such collaborations can help to design focused initiatives, making them more meaningful and culturally appropriate [ 12 , 59 , 91 , 102 ].
Key informant interviews, individual interviews with community members, focus groups with community members and community forums were among the qualitative data collection techniques used individually or in combination with each other by these studies to collect data on community needs and assets. They asserted that qualitative techniques specifically targeted to underrepresented segments of the population proved to be effective mechanisms to explore the participants’ perceptions on issues surrounding community health needs and assets. The most used technique to elicit community members’ opinions were focus group discussions and key informant interviews.
Small sample size and single-site setting were mentioned as the most cited limitations of the qualitative CHNAAs that limit these studies generalisability. Because the studied communities were unique communities with unique assets, constraints, and health needs, the CHNAA findings cannot be generalised to other communities [ 32 , 39 , 62 , 70 , 72 , 73 , 91 , 117 , 118 ]. Another limitation mentioned by some studies was that the demographic composition of the focus group participants, specifically with regards to race, gender, socio-economic status and age group, did not fully reflect the population of studied community as a whole [ 13 , 61 , 62 , 72 , 97 , 119 ]. Some studies reported that they could not include all influencing key informants in the community to facilitate broader understandings of health needs [ 13 , 120 ].
Mixed- methods studies
A variety of data collection methods were used in a number of included studies to ensure that a comprehensive picture of community health needs and resources was obtained ( n = 48, 42%). Some of these studies were two-phase explanatory mixed-methods studies, with the quantitative phase preceding the qualitative phase ( n = 14, 12%). They conducted targeted focus groups or community listening sessions or interview with community members/key informants following needs assessment survey to supplement the findings from the survey and provide further information about health status, needs of daily living, barrier to health and access to community resources [ 8 , 21 , 41 , 53 , 55 , 66 , 67 , 93 , 94 , 95 , 99 , 113 , 114 , 121 ]. In addition to these studies, some studies used triangulation mixed-method design to obtain complementary qualitative and quantitative data on community health needs and issues ( n = 13, 11%). These studies confirmed that using multiple data sources ensured researchers obtain a complete picture of the community health needs. Applying qualitative methods in the form of focus groups and semi-structured interviews enabled exploration of problems and needs within their social context and provided a wider perspective on issues raised. However, to conduct such studies CHNAA teams had to have members who have qualitative and quantitative expertise. There were some limitations specific to the mixed-method studies, including lack of rigor in integrating qualitative and quantitative findings, relying heavily on quantitative data for health need determination, and absence of the voices of the communities most in need [ 69 , 91 ].
Data analysis and interpretation
Qualitative data from focus group discussions and key informant interviews were mainly audio-recorded and transcribed verbatim by the research team and all identifying information was removed. Different analytical approaches, mostly content analysis and thematic analysis, were used to identify main themes related to assets, needs and gaps in the service system and priority populations.
Quantitative data from surveys were analysed using statistical software. Descriptive statistics were used to describe the sample in terms of socioeconomic background and present the prevalence of chronic diseases, risk factors, and health behaviours. Statistical analytical tests were also used to compare results between different groups of community members. Results also were compared by those at the state/ national level or from a similar community. Those diseases or risk factors that had a high prevalence among community members are regarded as priorities that to be addressed further.
Formulation of recommendations across various levels (individual, institution, community, policy levels)
Following analysis of the quantitative and qualitative data, the studies included in the review provided a thorough list of health needs and assets of the community. Included studies mainly used CHNAA outputs: 1) as a resource to provide baseline data of community’s health; 2) as a resource to prioritize and plan services; 3) as a resource for writing grant applications; 4) as a resource to guide a comprehensive health promotion strategy.
Not all included CHNAAs proposed interventions to address identified needs and issues. Some of the included studies ( n = 45, 39%) just provided a snapshot of the most important issues faced by the studied community. They demonstrated several areas where CHNAAs provide more information to researchers, community organizations, and policy-makers. On the other hand, not all identified issues and needs were addressed by those studies performed CHNAA in order to implement interventions or strategies. In practice, specific populations or a number of specific health conditions or health risks, or overarching issues such as health inequality and disparities were prioritized by these studies.
In most cases, decisions on implementation were carried out by the CHNAA steering committees or the research teams. Only a number of studies used a clear and explicit set of criteria for deciding the importance of each issue [ 22 , 27 , 43 , 67 , 94 , 118 , 122 ]. A wide range of criteria were used by included studies such as: impact, urgency, community concern, achievability within the set time [ 94 ], seriousness, urgency, solvability, and financial burden of the problems [ 27 ], perception of survey participants on importance of the identified issues and feasibility of intervention, prevalence, fatality, social and cultural stigma [ 22 ], possible interventions, organizational capacity, and community assets and resources [ 13 ], importance and possibility of the effecting change [ 43 ], prevalence, impact on the duration of sickness, impact on mortality, and the availability of treatment [ 122 ], impact of the problem on the overall wellness, quality of life, and resources of their community [ 118 ], factors of health issue, size, seriousness, and effectiveness of available interventions [ 101 ], importance and feasibility [ 67 ].
Different techniques for ranking priorities were applied by included studies such as: 1) Multi-voting technique (decide on priorities by agreeing or disagreeing in group discussions and continuing process/rounds until a final list is developed), 2) Strategy lists (determine if the health needs are of “high or low importance” by placing emphasis on problems whose solutions have maximum impact, with the possibility of limited resource), 3) Nominal group technique (rate health problems from 1 to 10 through group discussion), and 4) Prioritization matrix (weigh and rank multiple criteria for prioritization with numeric values to determine health needs with high importance).
Overall, health priority types were categorized into four main categories by included studies:
Medical conditions (e.g. obesity, diabetes, heart diseases, asthma, mental health disorders, substance abuse, vision/ dental problems, HIV/AIDS and sexually transmitted diseases, injuries and health consultations).
Health behaviours (e.g. physical activity, eating habits/ nutrition, tobacco consumption, teen pregnancy and violence/gangs).
Community conditions (e.g. poverty and unemployment, environmental and infrastructural conditions, such as air quality/pollution, transportation, access to clean water and sanitation, community collaboration, and access to healthy food, exercise facilities and occupational concerns).
Health systems priorities (e.g. access to care, including primary care and higher levels of care, specialty care, mental/ behavioural health care and dental care, quality and acceptability of health services, lack of cultural competence in health systems, flexible hours and waiting time).
However, guided by a community-based participatory research (CBPR) approach, a number of studies involved community members and stakeholders in priority identification or ranking [ 12 , 21 , 22 , 23 , 27 , 29 , 31 , 36 , 41 , 43 , 49 , 53 , 55 , 56 , 58 , 59 , 60 , 62 , 63 , 68 , 70 , 74 , 86 , 87 , 88 , 90 , 92 , 99 , 100 , 103 , 104 , 110 , 114 , 117 , 118 , 119 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 ], in potential strategy selection [ 13 , 19 , 67 , 82 , 89 , 130 ], and in carrying out strategies [ 8 , 37 , 69 , 81 , 93 , 105 , 113 ]. They asserted that by involving the perspectives of the relevant stakeholders, a comprehensive overview of the issues and possible effective solutions was created.
Planning of programmes and interventions, implementation and evaluation
The results of CHNAA were used in various ways by included studies. In some studies, particularly researcher-led studies with limited support or involvement of the local authorities, CHNAA just led to the identification of new, locally relevant issues and priorities without any further actions ( n = 45, 39%). The results of these CHNAAs provided more information to researchers, community organizations, and local policy-makers. Their results also may guide further research agenda in the community [ 18 , 21 , 23 , 29 , 35 , 39 , 40 , 42 , 44 , 48 , 49 , 50 , 52 , 54 , 55 , 62 , 64 , 65 , 66 , 69 , 70 , 71 , 72 , 73 , 76 , 77 , 78 , 85 , 96 , 106 , 122 , 123 , 131 , 132 , 133 , 134 , 135 ]. Some of these studies tried to present their results to the local authorities through various channels in the hope that it would modify existing programmes or implement new ones to meet the needs of the community residents. In addition to identification of relevant issues and priorities, included studies listed at least one outcome associated with the reported CHNAA activity as follows:
Development or modification of health and social policy and programmes: The knowledge provided by CHNAAs helped develop better tailored, and thereby potentially more effective interventions by a number of studies. Further, the information gathered from the CHNAA process was used as the baseline against which to measure future targets for assessment efforts and progress in areas were targeted ( n = 36).
Formation of new partnership: In some cases, a new partnership among entities involved in CHNAA was formed to address health issues. One of the partnerships reported successful was the community–academic partnership in which communities used the research capacity of academic institutions to conduct the CHNAAs ( n = 20). Another type of the partnership reported by some studies was the collaboration among healthcare organizations serving the same geographic area to conduct CHNAA jointly. Conducting a joint CHNAA may avoid duplication of planning efforts and obviate the creation of multiple community health needs assessments for the same population ( n = 5).
Development of new recommendations: Several suggestions were proposed to be considered while designing health improvement interventions in the future by some of the included studies ( n = 18).
Setting or altering strategic direction: Strategic agency direction was established or altered in some cases, which might indicate that the CHNAA was used to redirect resources better to meet the needs of the community ( n = 4).
Raising awareness about health issues: One of the most important insights brought by CHNAA findings was the recognition of the health priorities and contributing factors by the community members, leaders and researchers, leading to an increased awareness of community issues among them ( n = 8).
Engaging and motivating policy-makers and stakeholders: A few studies reported that CHNAAs provided health organizations with the opportunity to identify and interact with key policy-makers, community leaders, and key stakeholders about health priorities and concerns, which might foster a sense of collective ownership and trust in the results and increase the likelihood that the CHNAA will be used ( n = 5).
Having an impact on obtaining resources and resource allocation: The CHNAAs provided the community partners with locally relevant information regarding the current status of health and perceived community needs to inform resource allocation and applications for new grants for the initiation of new programmes ( n = 14)
Contribution to the development of CHNAA process: Some studies reported that the specific methods used in their CHNAA processes could contribute to more relevant and effective community health need assessment process ( n = 10).
Dissemination of findings
Disseminating of the findings and knowledge gained to all partners involved was a foremost step of CHNAAs. The most cited product of the CHNAA process in the included studies was the community needs assessment report. This report includes information about the health of the community as well as the community’s capacity to improve the lives of residents. The report provides the basis for discussion and future actions. In addition to the final report, other channels to disseminate CHNAAs findings were reported as: publishing CHNAA main results in local newspapers, communicating research results with community members and stakeholders in public forums or meetings, presentation results to the steering committee and various stakeholders, posting the report on the local authorities websites, individual meetings with community leaders and stakeholders, posters, and presentation of findings in academic conferences.
Community participation
Among included studies, around 50 studies (44%) reported using participatory approaches and techniques to encourage community members' participation in CHNAA process. Unlike traditional approaches to health needs assessment, participatory approaches aimed to incorporate community inputs at all stages of the research process to enhance capacity building and overcome barriers to research raised by matters of trust, communication, cultural differences, power and representation. A variety of participatory approaches (e.g. community based participatory research (CBPR), participatory rural appraisal, participatory action research (PAR), rapid participatory appraisal (RPA), tribal participatory research, community-based collaborative action research (CBCAR), precede-proceed model, concept mapping and photovoice) were used by these studies to ensure that communities participate in CHNAA, from defining the community to identifying needs and assets and developing new interventions.
Pennel and colleagues classified the depth of the community participation in CHNAA activities into four main categories [ 136 ]. In this classification, depth of the community participation was assessed by the types of activities in which participants were involved throughout the assessment and planning process as follows:
No participation: No attempt to engage community stakeholders or members;
Consultation-only: Engagement of health-related stakeholders, broader community stakeholders, and/or community members to identify health needs through surveys, interviews, and/or focus groups; verified or validated health needs/priorities with local experts;
Moderate participation: Involvement of community stakeholders/ or community members in priority identification; involvement of community stakeholders in strategy selection;
Extensive participation: Involvement of community stakeholders/or community members to develop and carry out strategies.
The above classification was used to assess the depth of the community participation by included studies. Based on the content analysis, community participation in CHNAA process varied considerably across the included empirical studies, from minimal to in-depth participation (Table 1 ). Around 65% of the included studies were involved in consultation-only to identify health needs through one-way communication using tools such as surveys, interviews, and focus group to identify community needs and resources. Around 22% of the included studies solicited moderate participation from the community by involving community in verifying needs and final priority selection and only about 10% of the included studies reported a broad and deep community participation including community involvement in designing and implementing strategies to improve community health.
Three categories of challenges were cited by the reviewed studies while performing CHNAA projects.
Methodological challenges: These are mainly associated with quantitative and qualitative data collection methods, which were discussed earlier. Other methodological challenges cited were: difficulties in aggregating and making sense of data collected from various sources (triangulation), non-generalisability of site-specific data and limitations of the use of existing epidemiological data alone, which does not provide a comprehensive view of health needs, yet is often the most available source of information. Traditional approaches to data collection were challenging where language and literacy barriers existed [ 12 , 52 , 65 , 71 ]. Another major challenge reported by studies used community-based participatory research approaches was the challenge of involving the community in decisions related to research design and data collection methods while maintaining an appropriate level of methodological validity and reliability [ 56 , 81 , 121 ]. In addition, participation was not without challenges. Including the perspectives of stakeholders and residents can lead to differing accounts of what services are seen as essential, and each party may push their own agenda based on their personal or professional interests. Further, linguistic and cultural barriers may be a major factor among minority groups hindering participation in such endeavors [ 81 , 137 ].
Logistical challenges: The major logistical challenges reported were the need for a considerable amount of time (often inadequate), and resources required to conduct a comprehensive assessment [ 80 , 138 ]. Good quality local data on the needs and utilization of health services are usually difficult to obtain [ 9 ]. Financial costs are considerable and the depth of information obtained will ultimately depend upon the methods employed [ 139 , 140 ]. In addition, health professionals, managers and others involved in health services planning and delivery may not have the requisite skills to conduct CHNAAs. This goes beyond technical skills and places an emphasis on soft skills and flexibility including good listening skills, the ability to establish trusting relationships, empathy, working with diverse groups and reflexivity [ 140 , 141 ]. Moreover, limited health information infrastructure and systems in developing countries settings may have hindered the availability of good quality information to conduct CHNAAs [ 13 , 28 , 30 , 142 ].
Ethical challenges: Concerns were raised about the ethical issues associated with community consultation about felt needs followed by priority setting process that leaves many needs unaddressed and the bulk of expectations dashed. Labelling, stigma and stereo- typing are other problems raised by needs assessment [ 143 ]. Needs assessment results may not be utilised, leaving unmet expectations and may require extensive financial and political support to lead to changes in health service planning and delivery [ 9 ]. Comprehensive health needs assessment is likely to produce different, potentially conflicting needs, exposing hidden conflicts and tensions in communities without any mechanisms to address these issues [ 5 ]. Further, local participation may only allow those who are able to voice their needs to do so, leaving behind the silent or hidden voices [ 81 ]. Involvement of the community in the needs assessment process also impacts upon possible outcomes of the project especially since it is likely that expectations of changes to programmes and service delivery may have arisen from local participation [ 144 ].
Facilitators and enablers
CHNAA projects need to be organized in such a way that they have clear objectives, and are adequately resourced by experienced staff. In addition, factors such as clear objectives, decisive leadership, teamwork, communication, sound study design, adequate resourcing, skilled staff, sufficient time and ownership by stakeholders are among those factors that contribute to the successful implementation of CHNAAs [ 15 , 145 ]. Most studies cited community participation as a major facilitator of the CHNAA process and outcomes. Participation was shown to foster bidirectional learning and communications, where both health authorities and the community learnt about needs and priorities. Different benefits for community engagement were mentioned by reviewed literature including, improved participants’ recruitment, enhanced capacity among stakeholders, productive conflict resolution, increased quality of outputs and outcomes, increased sustainability of project goals beyond funding and timelines and development of linguistically and culturally appropriate measures. In addition, incorporating community voices has the potential to inform the development of sound measures to tackle health disparities in the basis of race, social class and ethnicity [ 12 , 27 , 30 , 91 , 103 , 110 , 126 , 146 ].
The main objective of our scoping review was to provide an overview of why and how community health needs and assets assessments (CHNAAs) have been used globally. Substantial variation was found among the studies reviewed concerning definitions, process, participants, methods, goals, and products, yet there were many common characteristics.
Some CHNAAs focused narrowly on health care in assessing needs, with scant attention to other community issues that can affect health. However, most of the included studies looked beyond health needs and considered social and environmental conditions influencing community health. We argue all CHNAAs should approach community health needs assessment holistically, focusing on both individual physical and mental wellbeing as well as casting a social determinants of health lens on the population health.
The review showed that community health needs assessment is used widely by different users and across different settings in both HICs and LMICs. However, in countries such as the US it has become institutionalized and has accordingly been developed, as service providers, particularly hospitals, are mandated to perform CHNAA to compliance with legislative mandates. However, though federal and state laws impose requirements on hospitals to conduct CHNAAs, the methods for needs assessments are generally left to the discretion of each hospital [ 147 ]. As a result, assessment methods vary widely. US-based CHNAAs either develop their own CHNAA processes or utilize a process developed at the state or national level to guide their efforts. A number of toolkits have been provided by different organizations across US to help healthcare providers to conduct CHNAA projects [ 6 , 148 , 149 ]. This highlights the need for consensus guidance across many countries and settings while maintaining the responsiveness to contextual needs, assets and priorities.
Both qualitative and quantitative approaches were employed to collect data on community health needs and assets. Overall, there has been a growing use of mixed-methods approaches to conduct CHNAA in recent years, owing to the recognition in the literature that using qualitative and quantitative approaches simultaneously can provide complementary insights determining community health needs and assets [ 69 , 91 , 104 ]. Although quantitative approaches yield concrete evidence of community needs and assets, qualitative approaches provide a context for how these issues can be addressed using available resources [ 91 , 102 ]. Using qualitative methods in conjunction with more traditional quantitative approaches is especially appropriate for studying complex public health issues and promotes the alignment of implementation plans with the local needs of community members [ 59 , 69 , 91 ]. The growing use of mixed-methods approaches has practical implications for research training and capacity building within entities performing CHNAAs. Organizations who wish to conduct CHNAAs will need to ensure that the competencies and expertise required for mixed-methods studies are available.
Although only a small number of studies provided definitions of assets, there is a growing interest in the literature in asset-based assessment, which examines and mobilizes community assets, instead of focusing on only the needs of communities [ 11 , 84 ]. Unlike need-based or deficit approaches, asset-based approaches document resources and focus on strengths to enhance and preserve rather than deficits to be remedied. Related to principles of empowerment, it postulates that solutions to community problems already exist within a community’s assets. By recognizing existing capacity, communities can become empowered to take ownership of their health and improve as a population [ 11 , 31 , 125 ]. An asset-based approach was recognized as essential for enhancing trust and community coalitions [ 83 ]. Further, it is more participatory in nature through involving community stakeholders throughout the needs assessment process [ 82 , 83 ]. In particular, it highlights community resilience, resources, and opportunities for positive growth rather than focusing solely on health problems or other concerns [ 14 , 84 , 88 ]. In developing countries, assets identified from within the community are crucial for later use in the implementation of health programmes. The shift from a traditional needs-based perspective to an asset-based perspective to health needs assessment can help to address resource constraints in these countries [ 13 , 30 , 150 ].
There was a growing interest in the use of participatory approaches and in their value in identifying and addressing community health needs over recent years among included studies. About half of the reviewed studies applied CBPR or other community-engaged approaches to perform CHNAA. There are several opportunities to fully engage patients, families, and communities in healthcare delivery redesign to ensure that they are provided in a way that address the community members’ needs and preferences. The CHNAA process is one mechanism for this engagement—and a good precursor to deeper engagement and collaboration [ 91 , 97 , 123 ]. Integrating community voices into CHNAA process may be crucially important for confronting health disparities at the community level, which stemming from socio-historical processes, including racial and ethnic discrimination and economic inequality [ 33 , 74 , 86 , 91 ]. To eliminate health disparities, it is critical first to understand social, cultural, and economic determinants of health. CHNAAs, particularly when they include the voices of community residents, can provide an opportunity to understand local processes contributing to health disparities. This knowledge can then be used to inform health and equity initiatives [ 91 , 110 , 126 ]. The development process and implementation of a CHNAA project is an important example of evidence-based public health practice. It is a way to address health and health care disparities experienced by medically underserved populations [ 86 , 92 , 126 ]. Those studies used a participatory approach reported that by having community participation, concerns and issues of the most marginalized and vulnerable populations were voiced. The inclusion of these voices allowed for a broader and deeper understanding of the concerns of those who are typically marginalized and that may be missed in traditional health needs assessment methodologies [ 33 , 56 , 58 , 74 , 86 , 110 , 137 , 146 ]. Hence, defining communities while performing CHNAA needs to be dynamic and socially constructed to take into account all voices and members especially those not ordinarily included. This deeper understanding is critical to move public health practice and research upstream to address structural and social determinants of health necessary for population-level reductions in health inequities [ 80 , 91 ].
Although there is widespread theoretical recognition of the importance of in-depth community participation in CHNAA, this has not been fully embraced in practice based on our review. Included studies reported community involvement in various stages of CHNAA with varying depth reflecting a continuum from no participation to extensive participation, in which most studies were located at the middle of the participation continuum. The literature review suggests while certain community stakeholders were engaged in the CHNAA process, most studies did not involve a broad range of stakeholders through adopting a full participation approach. One reason for this could be that for most studies conducted in the US, CHNAA was performed to comply with ACA requirements, which requires hospitals to incorporate inputs of the population served as part of the CHNAA process. Since community inputs as well as the process as a whole is not well-defined by these regulations [ 20 ], it seems that the majority of included US-based studies tried to meet legislative requirements by incorporating a minimum level of community and stakeholders’ participation in CHNAA process. In addition, the concept of community engagement in health services planning and implementation has evolved over recent years, from one-way consultative processes to bi-directional collaboration and shared leadership. Although undertaking an in-depth participatory approach through extensive participation of community stakeholders in CHNAAs may pose certain challenges for healthcare providers including requiring additional time and other resources to collaborate with community residents, we argue the benefits to this approach are important to improve health, as reported by some included studies [ 80 , 118 , 151 ].
A notable gap in the existing literature is the lack of long-term or longitudinal–assessment of CHNAA. The review showed that additional research into CHNAA implementation and outcomes is needed. Currently, there are limited data describing the impact of CHNAAs on health outcomes. However, there is ample evidence on different short-term impacts associated with CHNAA implementation, including, the development of health and social interventions, forming the new partnership, raising awareness on health issues, engaging policy-makers, and facilitating obtaining resources. In other words, it is unclear how CHNAA projects are linked directly to health outcomes. Furthermore, the mechanisms between the conduct and use of CHNAA remain largely unknown in the literature [ 152 , 153 ]. Clearly, not all CHNAA projects result in changes to policies or programmes, and conversely, many programme and policy decisions are made in the absence of CHNAA data [ 154 , 155 ]. Still, further research to understand these mechanisms and the long term impact of CHNAA is needed to support evidence of its use and value in addressing individual and population health needs.
This scoping review aimed to provide clarity and supplement the evidence on the key concepts, rationale, methods, tools and outcomes of community health needs and assets assessments (CHNAAs). Importantly, it highlights the need for holistic approaches to needs assessments to focus on physical, mental and social wellbeing, along with considering wider systems factors and structural challenges to individual and population health. Furthermore, the findings emphasize the inclusion of community assets in community health assessments, beginning foremost with community capabilities and knowledge. It is encouraging to see the use of pragmatic approaches including both qualitative and quantitative methods in CHNAA process in the literature. This will help to ensure that a robust and in-depth exploration of needs and assets is available to guide decision making. Although we recognize the challenges with providing consensus on definitions, processes and tools for CHNAA, we argue that more clarity is needed on the key considerations, steps and outcomes for this process across various settings. This study attempts to provide some theoretical insights and empirical information concerning the process, which hopefully will provide useful guidance to community organizations, policy- makers, health service providers and researchers seeking to develop and implement community health needs and assets assessment.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Institute of Medicne. The future of the public’s health in the 21st century: National Academy Press; 2003.
Google Scholar
Fuller J, Bentley M, Shotton D. Use of community health needs assessment for regional planning in country South Australia. Aust J Rural Health. 2001;9(1):12–7. https://doi.org/10.1046/j.1440-1584.2001.00353.x .
Article CAS Google Scholar
Wright J, Williams R, Wilkinson JR. Development and importance of health needs assessment. BMJ. 1998;316(7140):1310–3. https://doi.org/10.1136/bmj.316.7140.1310 .
Wright J, Walley J. Assessing health needs in developing countries. BMJ. 1998;316(7147):1819–23. https://doi.org/10.1136/bmj.316.7147.1819 .
Jordan J, Dowswell T, Harrison S, Lilford RJ, Mort M. Health needs assessment: Whose priorities? Listening to users and the public. BMJ. 1998;316(7145):1668–70. https://doi.org/10.1136/bmj.316.7145.1668 .
Myers S, Stoto MA: Criteria for assessing the usefulness of community health assessments; a literature review. 2006. https://www.rand.org/pubs/technical_reports/TR314.html . Accessed 18 Nov 2020.
Centers for Disease Control and Prevention (CDC). Community needs assessment. Atlanta: GA.
Finifter DH, Jensen CJ, Wilson CE, Koenig BL. A comprehensive, multitiered, targeted community needs assessment model: methodology, dissemination, and implementation. Fam Community Health. 2005:293–306. https://doi.org/10.1097/00003727-200510000-00003 .
Stevens A, Gillam S. Needs assessment: from theory to practice. BMJ. 1998;316(7142):1448–52. https://doi.org/10.1136/bmj.316.7142.1448 .
Friedman DJ, Parrish RG. Is community health assessment worthwhile? J Public Health Manag Pract. 2009;15(1):3–9. https://doi.org/10.1097/01.PHH.0000342943.41080.ef .
Article Google Scholar
Altschuld JW, Hung HL, Lee YF. Needs assessment and asset/capacity building: A promising development in practice. New Dir Eval. 2014;2014(144):89–103. https://doi.org/10.1002/ev.20105 .
Jackson KM, Pukys S, Castro A, Hermosura L, Mendez J, Vohra-Gupta S, et al. Using the transformative paradigm to conduct a mixed methods needs assessment of a marginalized community: Methodological lessons and implications. Eval Program Plann. 2018;66:111–9. https://doi.org/10.1016/j.evalprogplan.2017.09.010 .
Mathias KR, Mathias JM, Hill PC. An asset-focused health needs assessment in a rural community in North India. Asia Pac J Public Health. 2015;27(2):NP2623–34. https://doi.org/10.1177/1010539511421193 .
Kirk CM, Johnson-Hakim S, Anglin A, Connelly C. Putting the community back into community health needs assessments: Maximizing partnerships via community-based participatory research. Prog Community Health Partnersh. 2017;11(2):167–73. https://doi.org/10.1353/cpr.2017.0021 .
Coster G, Mays N, Scott C, Cumming J. The impact of health needs assessment and prioritisation on District Health Board planning in New Zealand. Int J Health Plann Manag. 2009;24(4):276–89. https://doi.org/10.1002/hpm.1011 .
Parry-Jones B, Soulsby J. Needs-led assessment: the challenges and the reality. Health Soc Care Community. 2001;9(6):414–28. https://doi.org/10.1046/j.0966-0410.2001.00316.x .
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evidence Implementation. 2015;13(3):141–6. https://doi.org/10.1097/XEB.0000000000000050 .
Anselma M, Chinapaw MJM, Altenburg TM. Determinants of child health behaviors in a disadvantaged area from a community perspective: A participatory needs assessment. Int J Environ Res Public Health. 2018;15(4):644. https://doi.org/10.3390/ijerph15040644 .
Berkley-Patton J, Thompson CB, Bradley-Ewing A, Marcie B, Booker A, Catley D, et al. Identifying health conditions, priorities, and relevant multilevel health promotion intervention strategies in African American churches: A faith community health needs assessment. Eval Program Plann. 2018;67:19. https://doi.org/10.1016/j.evalprogplan.2017.10.012 .
Bias TK, Abildso CG, Vasile E, Coffman J. The impact of community input in community health needs assessments. J Public Health Manag Pract. 2017;23:S29–33. https://doi.org/10.1097/PHH.0000000000000586 .
Cho S, Lee H, Yoon S, Kim Y, Levin P, Kim E. Community health needs assessment: a nurses’ global health project in Vietnam. Int Nurs Rev. 2018;65(4):505–14. https://doi.org/10.1111/inr.12443 .
Kapiriri L, Frithjof NorheimMD PDO. Whose priorities count? Comparison of community-identified health problems and Burden-of-Disease-assessed health priorities in a district in Uganda. Health Expect. 2002;5(1):55–62. https://doi.org/10.1046/j.1369-6513.2002.00161.x .
Li Y, Cao J, Lin H, Li D, Wang Y, He J. Community health needs assessment with precede-proceed model: a mixed methods study. BMC Health Serv Res. 2009;9(1):1–14. https://doi.org/10.1186/1472-6963-9-181 .
World Health Organization. Social Determinants of Health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 . Acessed 10 Oct 2022.
Smithies J, Adams L, Webster G, Beattie A. Community participation in health promotion: Health Education Authority London; 1990.
Jack K, Holt M. Community profiling as part of a health needs assessment. Nurs Stand. 2008;22(18):51–8. https://doi.org/10.7748/ns2008.01.22.18.51.c6311 .
Ahari SS, Habibzadeh S, Yousefi M, Amani F, Abdi R. Community based needs assessment in an urban area; A participatory action research project. BMC Public Health. 2012;12(1):1–8. https://doi.org/10.1186/1471-2458-12-161 .
Shin H, Lee SJ, Lee Y-n, Shon S. Community health needs assessment for a child health promotion program in Kyrgyzstan. Eval Program Plann. 2019;74:1–9. https://doi.org/10.1016/j.evalprogplan.2019.02.005 .
Birdwell SW, Calesaric H. Identifying Health Care Needs of Rural Ohio Citizens: An Evaluation of a Two-stage Methodology. J Rural Health. 1996;12(2):130–6. https://doi.org/10.1111/j.1748-0361.1996.tb00784.x .
Pepall E, Earnest J, James R. Understanding community perceptions of health and social needs in a rural Balinese village: results of a rapid participatory appraisal. Health Promot Int. 2007;22(1):44–52. https://doi.org/10.1093/heapro/dal042 .
Moore de Peralta A, Davis L, Brown K, Fuentes M, Falconer NS, Charles J, et al. Using Community-Engaged Research to Explore Social Determinants of Health in a Low-Resource Community in the Dominican Republic: A Community Health Assessment. Hisp Health Care Int. 2020;18(3):127–37. https://doi.org/10.1177/1540415319874812 .
Ake T, Diehr S, Ruffalo L, Farias E, Fitzgerald A, Good SD, et al. Needs assessment for creating a patient-centered, community-engaged health program for homeless pregnant women. J Patient Cent Res Rev. 2018;5(1):36. https://doi.org/10.17294/2330-0698.1591 .
Kiser T, Hulton L. Addressing health care needs in the homeless population: a new approach using participatory action research. SAGE Open. 2018;8(3):2158244018789750. https://doi.org/10.1177/2158244018789750 .
Schaffer MA, Mather S, Gustafson V. Service learning: A strategy for conducting a health needs assessment of the homeless. Health Care Poor Underserved. 2000;11(4):385–99. https://doi.org/10.1353/hpu.2010.0746 .
Kehn M, Ho P, Kroll T. Identifying the health service needs of homeless adults with physical disabilities. Public Health. 2013;127(8):785–7. https://doi.org/10.1016/j.puhe.2013.01.011 .
Sangalang CC, Ngouy S, Lau AS. Using community-based participatory research to identify health issues for Cambodian American youth. Fam Community Health. 2015;38(1):55. https://doi.org/10.1097/FCH.0000000000000056 .
Jeffery V, Ervin K. Responding to rural health needs through community participation: addressing the concerns of children and young adults. Aust Prim Health. 2011;17(2):125–30. https://doi.org/10.1071/PY10050 .
Harrison L, Scarinci I. Child health needs of rural Alabama Latino families. J Community Health Nurs. 2007;24(1):31–47. https://doi.org/10.1080/07370010709336584 .
Averill J. Keys to the puzzle: Recognizing strengths in a rural community. Public Health Nurs. 2003;20(6):449–55. https://doi.org/10.1046/j.1525-1446.2003.20605.x .
Din NC, Ghazali SE, Ibrahim N, Ahmad M, Said Z, Ghazali AR, et al. Health needs assessment of older people in an agricultural plantation. Int J Gerontol. 2014;8(3):120–6. https://doi.org/10.1016/j.ijge.2013.12.003 .
Nolin J, Wilburn ST, Wilburn KT, Weaver D. Health and social service needs of older adults: Implementing a community-based needs assessment. Eval Program Plann. 2006;29(3):217–26. https://doi.org/10.1016/j.evalprogplan.2006.06.003 .
Lee LL, Lin SH, Philp I. Health needs of older Aboriginal people in Taiwan: a community-based assessment using a multidimensional instrument. J Clin Nurs. 2015;24(17–18):2514–21. https://doi.org/10.1111/jocn.12842 .
Núñez AE, Robertson-James C, Reels S, Weingartner RM, Bungy BL. Conducting a needs assessment for women and girls using a gender analysis framework: The Philadelphia Ujima coalition for a healthier community experience. Womens Health Issues. 2012;22(6):e527–34. https://doi.org/10.1016/j.whi.2012.08.002 .
Urrutia RP, Merisier D, Small M, Urrutia E, Tinfo N, Walmer DK. Unmet health needs identified by Haitian women as priorities for attention: a qualitative study. Reprod Health Matters. 2012;20(39):93–103. https://doi.org/10.1016/s0968-8080(12)39602-x .
Zimmermann K, Khare MM, Wright C, Hasler A, Kerch S, Moehring P, et al. Application of a gender-based approach to conducting a community health assessment for rural women in Southern Illinois. Eval Program Plann. 2015;51:27–34. https://doi.org/10.1016/j.evalprogplan.2014.12.004 .
Dell EM, Erikson SL, Andrianirina E, Smith G. Women’s knowledge in Madagascar: A health needs assessment study. Global public health. 2012;7(1):29–41. https://doi.org/10.1080/17441692.2011.557083 .
Chhabra R, Teitelman N, Silver EJ, Raufman J, Bauman LJ. Vulnerability Multiplied: Health Needs Assessment of 13–18-Year-Old Female Orphan and Vulnerable Children in Kenya. World Med Health Policy. 2018;10(2):129–45. https://doi.org/10.1002/wmh3.267 .
Stepleman LM, Yohannan J, Scott SM, Titus LL, Walker J, Lopez EJ, et al. Health needs and experiences of a LGBT population in Georgia and South Carolina. Homosex. 2019;66(7):989–1013. https://doi.org/10.1080/00918369.2018.1490573 .
Wilson BD, Neubauer LC, Park A, Abuor P, Harper GW. The sexual health needs of sexual minority women in Western Kenya: An exploratory community assessment and public policy analysis. Glob Public Health. 2019;14(10):1495–508. https://doi.org/10.1080/17441692.2019.1611895 .
Zajac C, Godshall KC. Empowerment through accessibility: Community needs assessment data for LGBTQ communities. Soc Work Public Health. 2020;35(6):483–93. https://doi.org/10.1080/19371918.2020.1798322 .
Coleman JD, Irwin JA, Wilson RC, Miller HC. The South Carolina LGBT needs assessment: A descriptive overview. Homosex. 2014;61(8):1152–71. https://doi.org/10.1080/00918369.2014.872515 .
Bhimla A, Yap L, Lee M, Seals B, Aczon H, Ma GX. Addressing the health needs of high-risk Filipino Americans in the greater Philadelphia region. J Community Health. 2017;42(2):269–77. https://doi.org/10.1007/s10900-016-0252-0 .
Bopp M, Fallon EA, Bolton DJ, Kaczynski AT, Lukwago S, Brooks A. Conducting a Hispanic Health Needs Assessment in rural Kansas: Building the foundation for community action. Eval Program Plann. 2012;35(4):453–60. https://doi.org/10.1016/j.evalprogplan.2012.02.002 .
Burns JC, Teadt S, Bradley WW Sr, Shade GH Jr. Enhancing Adolescent and Young Adult Health Services! A Review of the Community Needs Assessment Process in an Urban Federally Qualified Health Center. Health Equity. 2020;4(1):218–24. https://doi.org/10.1089/heq.2019.0108 .
Corona R, Gonzalez T, Cohen R, Edwards C, Edmonds T. Richmond Latino needs assessment: A community-university partnership to identify health concerns and service needs for Latino youth. J Community Health. 2009;34(3):195–201. https://doi.org/10.1007/s10900-008-9140-6 .
Doyle E, Rager R, Bates D, Cooper C. Using community-based participatory research to assess health needs among migrant and seasonal farmworkers. Am J Health Educ. 2006;37(5):279–88. https://doi.org/10.1080/19325037.2006.10598916 .
Ghimire S, Cheong P, Sagadraca L, Chien L-C, Sy FS. A health needs assessment of the Filipino American community in the greater Las Vegas area. Health Equity. 2018;2(1):334–48. https://doi.org/10.1089/heq.2018.0042 .
Hebert-Beirne J, Felner JK, Castañeda Y, Cohen S. Enhancing themes and strengths assessment: leveraging academic-led qualitative inquiry in community health assessment to uncover roots of community health inequities. J Public Health Manag Pract. 2017;23(4):370–9. https://doi.org/10.1097/phh.0000000000000478 .
Hebert-Beirne J, Hernandez SG, Felner J, Schwiesow J, Mayer A, Rak K, et al. Using community-driven, participatory qualitative inquiry to discern nuanced community health needs and assets of Chicago’s La Villita, a Mexican immigrant neighborhood. J Community Health. 2018;43(4):775–86. https://doi.org/10.1007/s10900-018-0484-2 .
Hernandez SG, Genkova A, Castañeda Y, Alexander S, Hebert-Beirne J. Oral histories as critical qualitative inquiry in community health assessment. Health Educ Behav. 2017;44(5):705–15. https://doi.org/10.1177/1090198117728546 .
Lee S, Ma GX, Juon H-S, Martinez G, Hsu CE, Bawa J. Assessing the needs and guiding the future: findings from the health needs assessment in 13 Asian American communities of Maryland in the United States. J Immigr Minor Health. 2011;13(2):395–401. https://doi.org/10.1007/s10903-009-9310-3 .
Martinez IL, Carter-Pokras O. Assessing health concerns and barriers in a heterogeneous Latino community. J Health Care Poor Underserved. 2006;17(4):899–909. https://doi.org/10.1353/hpu.2006.0129 .
Mannix TR, Austin SD, Baayd JL, Simonsen SE. A community needs assessment of urban Utah American Indians and Alaska natives. J Community Health. 2018;43(6):1217–27. https://doi.org/10.1007/s10900-018-0542-9 .
Montano JJ, Acosta-Deprez V, Sinay T. Assessing the health care needs of Filipino Americans in greater Long Beach. Public Admin Manag. 2009;14(1):156.
Patel VV, Rajpathak S, Karasz A. Bangladeshi immigrants in New York City: a community based health needs assessment of a hard to reach population. J Immigr Minor Health. 2012;14(5):767–73. https://doi.org/10.1007/s10903-011-9555-5 .
Su D, Garg A, Wiens J, Meyer E, Cai G. Assessing health needs in African American churches: a mixed-methods study. J Relig Health. 2021;60(2):1179–97. https://doi.org/10.1007/s10943-019-00924-5 .
Suiter SV. Community health needs assessment and action planning in seven Dominican bateyes. Eval Program Plann. 2017;60:103–11. https://doi.org/10.1016/j.evalprogplan.2016.10.011 .
Thomas LR, Donovan DM, Sigo RL. Identifying community needs and resources in a Native community: A research partnership in the Pacific Northwest. Int J Ment Health Addict. 2010;8(2):362–73. https://doi.org/10.1007/s11469-009-9233-1 .
Weathers B, Barg FK, Bowman M, Briggs V, Delmoor E, Kumanyika S, et al. Using a mixed-methods approach to identify health concerns in an African American community. Am J Public Health. 2011;101(11):2087–92. https://doi.org/10.2105/AJPH.2010.191775 .
Dong X, Chang E, Wong E, Wong B, Skarupski KA, Simon MA. Assessing the health needs of Chinese older adults: Findings from a community-based participatory research study in Chicago's Chinatown. J Aging Res. 2010. https://doi.org/10.4061/2010/124246 .
Sarsour L, Tong VS, Jaber O, Talbi M, Julliard K. Health assessment of the Arab American community in southwest Brooklyn. J Community Health. 2010;35(6):653–9. https://doi.org/10.1007/s10900-010-9260-7 .
Thein K, Zaw KT, Teng R-E, Liang C, Julliard K. Health Needs in Brooklyn's Chinatown: A Pilot Assessment Using Rapid Participatory Appraisal. J Health Care Poor Underserved. 2009;20(2):378–94. https://doi.org/10.1353/hpu.0.0140 .
Careyva BA, Hamadani R, Friel T, Coyne CA. A social needs assessment tool for an urban Latino population. J Community Health. 2018;43(1):137–45. https://doi.org/10.1007/s10900-017-0396-6 .
Johnson CV, Bartgis J, Worley JA, Hellman CM, Burkhart R. Urban Indian voices: a community-based participatory research health and needs assessment. Am Indian Alsk Native Mentl Health Res. 2010;17(1):49–70. https://doi.org/10.5820/aian.1701.2010.49 .
Puertas B, Schlesser M. Assessing community health among indigenous populations in Ecuador with a participatory approach: implications for health reform. J Community Health. 2001;26(2):133–47. https://doi.org/10.1023/a:1005281314274 .
Miller K, Yost B, Abbott C, Thompson Buckland S, Dlugi E, Adams Z, et al. Health needs assessment of five Pennsylvania Plain populations. Int J Environ Res Public Health. 2019;16(13):2378. https://doi.org/10.3390/ijerph16132378 .
Tendulkar SA, Hamilton RC, Chu C, Arsenault L, Duffy K, Huynh V, et al. Investigating the myth of the “model minority”: a participatory community health assessment of Chinese and Vietnamese adults. J Immigr Minor Health. 2012;14(5):850–7. https://doi.org/10.1007/s10903-011-9517-y .
Peak T, Gast J, Ahlstrom D. A needs assessment of Latino men’s health concerns. Am J Mens Health. 2010;4(1):22–32. https://doi.org/10.1177/1557988308327051 .
Brock KE, Allen KE, Barton C, Shapiro R, Weintraub B, Wasilewski-Masker K, et al. A Methodologic Approach to Conducting a Statewide Community Needs Assessment of Pediatric Palliative Care and Hospice Resources. J Pain Symptom Manag. 2020;60(3):531–8. e538. https://doi.org/10.1016/j.jpainsymman.2020.04.004 .
Franz BA, Skinner D, Murphy JW. Defining “Community” in community health evaluation: perspectives from a sample of nonprofit Appalachian hospitals. Am J Eval. 2018;39(2):237–56. https://doi.org/10.1177/1098214017722857 .
Clark MJ, Cary S, Diemert G, Ceballos R, Sifuentes M, Atteberry I, et al. Involving communities in community assessment. Public Health Nurs. 2003;20(6):456–63. https://doi.org/10.1046/j.1525-1446.2003.20606.x .
Van Gelderen SA, Krumwiede KA, Krumwiede NK, Fenske C. Trialing the community-based collaborative action research framework: supporting rural health through a community health needs assessment. Health Promot Pract. 2018;19(5):673–83. https://doi.org/10.1177/1524839917754043 .
Goldman KD, Schmalz KJ. “Accentuate the positive!” using an asset-mapping tool as part of a community-health needs assessment. Health Promot Pract. 2005;6(2):125–8. https://doi.org/10.1177/1524839904273344 .
Sharpe PA, Greaney ML, Lee PR, Royce SW. Assets-oriented community assessment. Public Health Rep. 2000;115(2–3):205. https://doi.org/10.1093/phr/115.2.205 .
Mathias K, Rawat M, Thompson A, Gaitonde R, Jain S. Exploring community mental health systems–A participatory health needs and assets assessment in the Yamuna valley, North India. Int J Health Policy Manag. 2020. https://doi.org/10.34172/ijhpm.2020.222 .
deValpine MG, Trull LH. Health Equity in Community Assessments: A Participatory Approach in Rural Virginia. SAGE Open. 2019;9(1):2158244019838925. https://doi.org/10.1177/2158244019838925 .
Lewis H, Rudolph M, White L. Rapid appraisal of the health promotion needs of the Hillbrow Community, South Africa. Int J Healthc Technol Manag. 2003;5(1–2):20–33. https://doi.org/10.1504/IJHTM.2003.003338 .
Talmage C, Mercado M, Yoder G, Hamm K, Wolfersteig W. Critiquing Indicators of Community Strengths in Community Health Needs Assessments. Int J Community Well-Being. 2021:1–22. https://doi.org/10.1007/s42413-020-00106-2 .
Idali Torres M. Assessing health in an urban neighborhood: community process, data results and implications for practice. J Community Health. 1998;23(3):211–26. https://doi.org/10.1023/a:1018720515644 .
Garrettson M, Walline V, Heisler J, Townsend J. New medical school engages rural communities to conduct regional health assessment. Fam Med. 2010;42(10):693.
Cain CL, Orionzi D, O’Brien M, Trahan L. The power of community voices for enhancing community health needs assessments. Health Promot Pract. 2017;18(3):437–43. https://doi.org/10.1177/1524839916634404 .
Grant CG, Ramos R, Davis JL, Green BL. Community health needs assessment: a pathway to the future and a vision for leaders. Health Care Manag (Frederick). 2015;34(2):147–56. https://doi.org/10.1097/hcm.0000000000000057 .
Robinson A, Cherry TS, Elliott M, Davis M, Bagwell G. Leveraging university-community partnerships in rural Georgia: A community health needs assessment template for hospitals. J Ga Public Health Assoc. 2016:365–72. https://doi.org/10.21633/JGPHA.5.409 .
Alfano-Sobsey E, Ledford SL, Decosimo K, Horney JA. Community health needs assessment in Wake County, North Carolina: partnership of public health, hospitals, academia, and other stakeholders. N C Med J. 2014;75(6):376–83. https://doi.org/10.18043/ncm.75.6.376 .
Waling A, Fildes D. ‘Don't fix what ain’t broke’: evaluating the effectiveness of a Men's Shed in inner-regional A ustralia. Health Soc Care Community. 2017;25(2):758–68. https://doi.org/10.1111/hsc.12365 .
Witten NA, Orr MP, Maskarinec GG. Medical School Hotline: An Online, Quantitative Community Health Needs Assessment of Hale ‘iwa and Waialua, O ‘ahu, Hawai ‘i. H Hawaii J Health Soc Welf. 2020;79(10):306.
Woodyard CD, Przybyla S, Hallam JS. A community health needs assessment using principles of community-based participatory research in a Mississippi Delta community: a novel methodological approach. Community Dev. 2015;46(2):84–99. https://doi.org/10.1080/15575330.2015.1006240 .
O’Kelly C, Cullen W, O’Kelly S, O’Kelly F, Bury G. A primary care-based health needs assessment in inner city Dublin. Ir J Med Sci. 2010;179(3):399–403. https://doi.org/10.1007/s11845-010-0483-5 .
Knox S, Chapman P, Your health—your say. A case study of community involvement in a community health needs assessment project in a regional city of Australia. Cities. 1995;12(2):111–4. https://doi.org/10.1016/0264-2751(95)00011-a .
Murray SA, Tapson J, Turnbull L, McCallum J, Little A. Listening to local voices: adapting rapid appraisal to assess health and social needs in general practice. BMJ. 1994;308(6930):698–700. https://doi.org/10.1136/bmj.308.6930.698 .
Stanley SA, Stein DS. Health Watch 2000: community health assessment in south central Ohio. J Community Health Nurs. 1998;15(4):225–36. https://doi.org/10.1207/s15327655jchn1504_4 .
Ying L, Daikun L, Jia H, Kai S, HongHong L, Hu Z. Assessment of community health needs of Chongqing residents. a qualitative study. Mil Med Res. 2008;23(5):289–99. https://doi.org/10.1016/S1000-1948(08)60056-8 .
Kwan K, Do-Reynoso V, Zarate-Gonzalez G, Goldman-Mellor S. Development and implementation of a community health survey for public health accreditation: Case study from a rural county in California. Eval Program Plann. 2018;67:47–52. https://doi.org/10.1016/j.evalprogplan.2017.11.004 .
Green S, Parkinson L, Bonevski B, Considine R. Community health needs assessment for health service planning: realising consumer participation in the health service setting. Health Promot J Austr. 2004;15(2):142–9. https://doi.org/10.1071/HE04142 .
Horne M, Costello J. A public health approach to health needs assessment at the interface of primary care and community development: findings from an action research study. Prim Health Care Res Dev. 2003;4(4):340–52. https://doi.org/10.1191/1463423603pc173oa .
Lundeen SP. Health needs of a suburban community: a nursing assessment approach. J Community Health Nurs. 1992;9(4):235–44. https://doi.org/10.1207/s15327655jchn0904_5 .
Jordan J, Wright J. Making sense of health needs assessment. Br Gen Pract. 1997;47(424):695.
CAS Google Scholar
Hensher M, Fulop N. The influence of health needs assessment on health care decision-making in London health authorities. J Health Serv Policy. 1999;4(2):90–5. https://doi.org/10.1177/135581969900400206 .
Asadi-Lari M, Farshad A, Assaei S, Mahdavi MV, Akbari M, Ameri A, et al. Applying a basic development needs approach for sustainable and integrated community development in less-developed areas: report of ongoing Iranian experience. Public Health. 2005;119(6):474–82. https://doi.org/10.1016/j.puhe.2004.08.014 .
Akintobi TH, Lockamy E, Goodin L, Hernandez ND, Slocumb T, Blumenthal D, et al. Processes and outcomes of a community-based participatory research-driven health needs assessment: a tool for moving health disparity reporting to evidence-based action. Prog Community Health Partnersh. 2018;12(1 Suppl):139. https://doi.org/10.1353/cpr.2018.0029 .
Yoo IY, Cho WJ, Chae SM, Kim MJ. Community health service needs assessment in Korea using OMAHA Classification System. Int J Nurs Stud. 2004;41(6):697–702. https://doi.org/10.1016/j.ijnurstu.2004.02.007 .
Louw J, Carolissen R. Community health needs, community participation, and evaluation research. Eval Program Plann. 1995;18(4):365–9.
Plescia M, Koontz S, Laurent S. Community assessment in a vertically integrated health care system. Am J Public Health. 2001;91(5):811. https://doi.org/10.2105/AJPH.91.5.811 .
Sampson G, Gearin KJM, Boe M. A rural local health department–hospital collaborative for a countywide community health assessment. J Public Health Manag Pract. 2015;21(1):23–30. https://doi.org/10.1097/phh.0000000000000088 .
Vyas AN, Chaudhary N, Ramiah K, Landry M. Addressing a Growing Community’s Health Needs: Project SAHNA (South Asian Health Needs Assessment). J Immigr Minor Health. 2013;15(3):577–83. https://doi.org/10.1007/s10903-012-9655-x .
Van Rie A, West N, Schwartz S, Mutunga L, Hanrahan C, Ncayiyana J, et al. The unmet needs and health priorities of the urban poor: Generating the evidence base for urban community health worker programmes in South Afric. S Afr Med J. 2018;108(9). https://doi.org/10.7196/SAMJ.2018.v108i9.13054 .
Dennis MK, Momper SL. An urban American Indian health clinic's response to a community needs assessment. Am Indian Alsk Native Ment Health Res. 2016;23(5). https://doi.org/10.5820/aian.2305.2016.15 .
Schutte DL, Goris ED, Rivard JL, Schutte BC, Committee CCRA. Community Health Needs Assessment in a Rural Setting. Foundation for a Community–Academic Partnership. J High Educ Outreach Engagem. 2016;20(2):85–108.
Velonis AJ, Molnar A, Lee-Foon N, Rahim A, Boushel M, O’Campo P. “One program that could improve health in this neighbourhood is _?” using concept mapping to engage communities as part of a health and human services needs assessment. BMC Health Serv Res. 2018;18(1):1–12. https://doi.org/10.1186/s12913-018-2936-x .
Torres Stone RA, Cardemil EV, Keefe K, Bik P, Dyer Z, Clark KE. A community mental health needs assessment of a racially and ethnically diverse population in New England: Narratives from community stakeholders. Community Ment Health J. 2020;56(5):947–58. https://doi.org/10.1007/s10597-020-00562-2 .
Agrusti T, Bohn J, Dunn E, Bell C, Ziegler A. The story so far: a mixed-methods evaluation of county-level behavioral health needs, policies, and programs. Soc Work Ment Health. 2020;18(3):257–73. https://doi.org/10.1080/15332985.2020.1720889 .
Palmer CA. Rapid appraisal of needs in reproductive health care in southern Sudan: qualitative study. BMJ. 1999;319(7212):743–8. https://doi.org/10.1136/bmj.319.7212.743 .
Lazenbatt A, Lynch U, O'Neill E. Revealing the hidden ‘troubles’ in Northern Ireland: the role of participatory rapid appraisal. Health Educ Res. 2001;16(5):567–78. https://doi.org/10.1093/her/16.5.567 .
Kingery FP, Naanyu V, Allen W, Patel P. Photovoice in Kenya: Using a community-based participatory research method to identify health needs. Qual Health Res. 2016;26(1):92–104. https://doi.org/10.1177/1049732315617738 .
Sabin AV, Levin PF. The Journey to Meet Emerging Community Benefit Requirements in a Rural Hospital: A Case Study. Online J Issues Nurs. 2016;21(1). https://doi.org/10.3912/OJIN.Vol21No01PPT01 .
Lightfoot AF, De Marco MM, Dendas RC, Jackson MR, Meehan EF. Engaging underserved populations in Affordable Care Act-required needs assessments. J Health Care Poor Underserved. 2014;25(1):11–8. https://doi.org/10.1353/hpu.2014.0060 .
Amendola MG, Nazario N, Sanchez V. Using CBPR to assess client needs at a social service agency. Public Health Nurs. 2016;33(2):167–75. https://doi.org/10.1111/phn.12204 .
Harmon BE, Pichon LC, Powell TW, Rugless F, McCann L, Minor LL, et al. Developing a Congregational Health Needs Assessment: Lessons Learned from Using a Participatory Research Approach. Prog Community Health Partnersh. 2021;15(1):47–58. https://doi.org/10.1353/cpr.2021.0004 .
Mulvihill BA, Pass MA, Miller TM, Mulvihill FX, Klerman LV. Collaborative needs assessment and systems development in Alabama: Process and products. Am J Prev Med. 1996;12(4):14–9.
Santilli A, Carroll-Scott A, Ickovics JR. Applying community organizing principles to assess health needs in New Haven, Connecticut. Am J Public Health. 2016;106(5):841–7. https://doi.org/10.2105/ajph.2016.303050 .
Milaat W, Bani I, Aqeely H, Makeen A, Salih A, Alnagaar M. Jazan Health needs assessment: a key informant approach. J Public Health Med. 2007;6:105–10.
Kulig JC, Wilde I. Collaboration between communities and universities: Completion of a community needs assessment. Public Health Nurs. 1996;13(2):112–9. https://doi.org/10.1111/j.1525-1446.1996.tb00228.x .
Running A, Martin K, Tolle LW. An innovative model for conducting a participatory community health assessment. J Community Health Nurs. 2007;24(4):203–13. https://doi.org/10.1080/07370010701645869 .
Smith SM, Long J, Deady J, O'Keeffe F, Handy D, O'Dowd T. Adapting developing country epidemiological assessment techniques to improve the quality of health needs assessments in developed countries. BMC Health Serv Res. 2005;5(1):1–7. https://doi.org/10.1186/1472-6963-5-32 .
Wood EA, Chapman KS, Beau de Rochars VM, Mckune SL. Community-based health needs assessment in Léogâne and Gressier, Haiti: six years post-earthquake. J Int Humanit Action. 2017;2(1):1–8. https://doi.org/10.1186/s41018-017-0026-z .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. A mixed-methods approach to understanding community participation in community health needs assessments. J Public Health Manag Pract. 2017;23(2):112–21. https://doi.org/10.1097/PHH.0000000000000362 .
Lillie-Blanton M, Hoffman SC. Conducting an assessment of health needs and resources in a racial/ethnic minority community. Health Serv Res. 1995;30(1 Pt 2):225.
Irani P, Bohn C, Halasan C, Landen M, McCusker D. Community health assessment: driving the need for current, easily accessible population health data. J Public Health Manag Pract. 2006;12(2):113–8. https://doi.org/10.1097/00124784-200603000-00002 .
Alberti P. Community health needs assessments: filling data gaps for population health research and management. EGEMS. 2014;2(4). https://doi.org/10.13063/2327-9214.1174 .
Skinner D, Franz B, Kelleher K. What challenges do nonprofit hospitals face in taking on community health needs assessments? A qualitative study from Appalachian Ohio. J Rural Health. 2018;34(2):182–92. https://doi.org/10.1111/jrh.12246 .
Stoto MA, Davis MV, Atkins A. Making better use of population health data for community health needs assessments. EGEMs. 2019;7(1). https://doi.org/10.5334/egems.305 .
Smith LU, Burdine JN. Community health assessment opportunities and challenges in the 21st century: Implications for professional development. J Public Health Manag Pract. 2017;23:S63–4. https://doi.org/10.1097/PHH.0000000000000601 .
Hawe P. Needs assessment must become more change-focused. Aust N Z J Public Health. 1996;20(5):473–8. https://doi.org/10.1111/j.1467-842x.1996.tb01624.x .
Jordan J, Wright J, Wilkinson J, Williams R. Assessing local health needs in primary care: understanding and experience in three English districts. Qual Health Care. 1998;7(2):83–9. https://doi.org/10.1136/qshc.7.2.83 .
Curtis DC. Evaluation of community health assessment in Kansas. J Public Health Manag Pract. 2002:20–5. https://doi.org/10.1097/00124784-200207000-00005 .
Kim S, Flaskerud JH, Koniak-Griffin D, Dixon EL. Using community-partnered participatory research to address health disparities in a Latino community. J Prof Nurs. 2005;21(4):199–209. https://doi.org/10.1016/j.profnurs.2005.05.005 .
Crossley M. Tax-exempt hospitals, community health needs and addressing disparities. Howard Law J. 2011;55:687.
Schifferdecker KE, Bazos DA, Sutherland KA, LaFave LRA, Fedrizzi R, Hoebeke J. A review of tools to assist hospitals in meeting community health assessment and implementation strategy requirements. J Healthc Manag. 2016;61(1):44.
Becker KL. Conducting community health needs assessments in rural communities: Lessons learned. Health Promot Pract. 2015;16(1):15–9. https://doi.org/10.1177/1524839914555887 .
Pepall E, James R, Earnest J. Guidelines for conducting rapid participatory appraisals of community health needs in developing countries: experience from Tulikup, Bali. Asia Pac J Public Health. 2006;18(3):42–8. https://doi.org/10.1177/10105395060180030801 .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. Community health needs assessment: potential for population health improvement. Popul Health Manag. 2016;19(3):178–86. https://doi.org/10.1089/pop.2015.0075 .
Solet D, Ciske S, Gaonkar R, Horsley K, McNees M, Nandi P, et al. Effective community health assessments in King County, Washington. J Public Health Manag Pract. 2009;15(1):33–40. https://doi.org/10.1097/PHH.0b013e3181903c11 .
Spice C, Snyder K. Reviewing self-reported impacts of community health assessment in local health jurisdictions. J Public Health Manag Pract. 2009;15(1):18–23. https://doi.org/10.1097/PHH.0b013e3181903c57 .
Diaz HJ-M, Ainsworth D, Schmidtlein MC. Funding priorities: data-driven approach for prioritizing community health needs in vulnerable communities. Health Promot Pract. 2019;20(4):616–23. https://doi.org/10.1177/1524839918771977 .
Franz B, Cronin CE, Singh S. Are nonprofit hospitals addressing the most critical community health needs that they identify in their community health needs assessments? J Public Health Manag Pract. 2021;27(1):80–7. https://doi.org/10.1097/phh.0000000000001034 .
Cramer GR, Singh SR, Flaherty S, Young GJ. The progress of US hospitals in addressing community health needs. Am J Public Health. 2017;107(2):255–61. https://doi.org/10.2105/AJPH.2016.303570 .
Kazda MJ, Beel ER, Villegas D, Martinez JG, Patel N, Migala W. Methodological complexities and the use of GIS in conducting a community needs assessment of a large US municipality. J Community Health. 2009;34(3):210–5. https://doi.org/10.1007/s10900-008-9143-3 .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D. Nonprofit hospitals’ approach to community health needs assessment. Am J Public Health. 2015;105(3):e103–13. https://doi.org/10.2105/ajph.2014.302286 .
Vance RA, Basta TB, Bute JJ, Denham SA. Identifying the health needs in rural Appalachian Ohio: Outcomes of a rural community-academic partnership. Am J Health Sci. 2012;3(2):115–24. https://doi.org/10.19030/ajhs.v3i2.6942 .
Bias T, Abildso C, Sarkees E. The Importance of Individual-Site and System-Wide Community Health Needs Assessments. Front Public Health. 2020;20. https://doi.org/10.3389/fpubh.2020.00020 .
Billings JR, Cowley S. Approaches to community needs assessment: a literature review. J Adv Nurs. 1995;22(4):721–30. https://doi.org/10.1046/j.1365-2648.1995.22040721.x .
Brazil K, Anderson M. Assessing health service needs: Tools for health planning. HealthC Manage Forum. 1996:22–7. https://doi.org/10.1016/S0840-4704(10)60940-4 .
Campbell S. Assessing community healthcare needs: lessons from Africa. Nurs Stand. 2001;15(47):41. https://doi.org/10.7748/ns2001.08.15.47.41.c3070 .
Carlton EL, Singh SR. Joint community health needs assessments as a path for coordinating community-wide health improvement efforts between hospitals and local health departments. Am J Public Health. 2018;108(5):676–82. https://doi.org/10.2105/ajph.2018.304339 .
Declercq ER, Bichell TJV, Center JK. Population-based needs assessment: bringing public health to midwifery practice. J Nurse Midwifery. 1997;42(6):478–88. https://doi.org/10.1016/s0091-2182(97)00081-5 .
Evans-Agnew R, Reyes D, Primomo J, Meyer K, Matlock-Hightower C. Community health needs assessments: Expanding the boundaries of nursing education in population health. Public Health Nurs. 2017;34(1):69–77. https://doi.org/10.1111/phn.12298 .
Guareschi PA, Jovchelovitch S. Participation, health and the development of community resources in Southern Brazil. J Health Psychol. 2004;9(2):311–22. https://doi.org/10.1177/1359105304040896 .
Holakouie NK, Ahmadvand A, Ahmadnezhad E, Alami A. A community assessment model appropriate for the Iranian community. Iran J Public Health. 2014;43(3):323.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173–202. https://doi.org/10.1146/annurev.publhealth.19.1.173 .
King CJ, Roach JL. Community health needs assessments: a framework for America’s hospitals. Popul Health Manag. 2016;19(2):78–80. https://doi.org/10.1089/pop.2015.0053 .
Misra R, Ballard D. Community needs and strengths assessments as an active learning project. J Sch Health. 2003;73(7):269–71. https://doi.org/10.1111/j.1746-1561.2003.tb06577.x .
Powell RE, Doty AM, Rising KL, Karp DN, Baehr A, Carr BG. A content analysis of nonprofit hospital community health needs assessments and community benefit implementation strategies in Philadelphia. J Public Health Manag Pract. 2018;24(4):326–34. https://doi.org/10.1097/phh.0000000000000621 .
Reece SM. Community analysis for health planning: strategies for primary care practitioners. The. Nurse Pract. 1998;23(10):46 49, 53-46 passim.
Stoto MA, Straus SG, Bohn C, Irani P. A web-based tool for assessing and improving the usefulness of community health assessments. J Public Health Manag Pract. 2009;15(1):10–7. https://doi.org/10.1097/01.PHH.0000342944.48703.21 .
Wetta RE, Pezzino G, LaClair B, Orr S, Brown MB. Voices across Kansas: community health assessment and improvement efforts among local health departments. J Public Health Manag Pract. 2014;20(1):39–42. https://doi.org/10.1097/phh.0b013e3182a9572a .
Download references
Acknowledgements
We acknowledge contribution of the research assistants helped with data extraction.
This work was funded by department of UHC Life course/Integrated Health Services (IHS), World Health Organization (WHO) headquarter (HQ). ZA received the research grant. The authors HR, AS, and SE from WHO commissioned the study, contributed to the direction of the work, and commented on the drafts.
Author information
Authors and affiliations.
Department of Universal Health Coverage/Health Systems (UHS), World Health Organization, Regional Office for the Eastern Mediterranean, Cairo, Egypt
Hamid Ravaghi
Department of Integrated Health Services (IHS), World Health Organization, Headquarters, Geneva, Switzerland
Ann-Lise Guisset
Department of Healthier Populations (DHP), World Health Organization, Regional Office of Eastern Mediterranean Region, Cairo, Egypt
Samar Elfeky
Center for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Naima Nasir
National library and Archives of Iran, Tehran, Iran
Sedigheh Khani
National Institute of Health Research (NIHR), Tehran University of Medical Sciences, Tehran (TUMS), Tehran, Iran
Elham Ahmadnezhad
Zhaleh Abdi
You can also search for this author in PubMed Google Scholar
Contributions
AG, HR and SE conceived the study and participated in its design. SK conducted the literature search and prepared the search results for analysis. NN developed the study framework, the data abstraction forms and the manuscript outline. The literature was analysed by ZA, EA and NN under the supervision of HR and AG. ZA drafted the final version of the manuscript and HR, NN, AG and SE reviewed it. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Zhaleh Abdi .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors have no competing interests. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the World Health Organization (WHO).
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
PubMed database search strategy.
Additional file 2.
Content of the extraction forms.
Additional file 3.
List of included empirical papers [ 156 – 159 ].
Additional file 4.
List of included non-empirical papers [ 160 -– 175 ] .
Additional file 5.
Health indicators collected by community health assessment surveys.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ravaghi, H., Guisset, AL., Elfeky, S. et al. A scoping review of community health needs and assets assessment: concepts, rationale, tools and uses. BMC Health Serv Res 23 , 44 (2023). https://doi.org/10.1186/s12913-022-08983-3
Download citation
Received : 20 May 2022
Accepted : 19 December 2022
Published : 17 January 2023
DOI : https://doi.org/10.1186/s12913-022-08983-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health Needs Assessment
- Needs Assessment
- Assets Assessment
- Population Health
- Scoping Review
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
REVIEW article
A systematic review of midwives’ training needs in perinatal mental health and related interventions.

- 1 Centre referent de rehabilitation psychosociale, GCSMS REHACOOR 42, Saint-Étienne, France
- 2 University Claude Bernard Lyon1, Research on Healthcare Performance (RESHAPE) INSERM U1290, Lyon, France
- 3 AURORE Perinatal Network, Hospices civiles de Lyon, Croix Rousse Hospital, Lyon, France
- 4 Departments of Psychiatry and Child & Adolescent Psychiatry, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
- 5 Medical Library, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
- 6 University Hospital of Saint-Étienne & EA 7423 (Troubles du Comportement Alimentaire, Addictions et Poids Extrêmes (TAPE), Université Jean Monnet - Saint-Etienne), Saint-Etienne, France
- 7 University Hospital of Saint-Étienne, Department of Child and Adolescent Psychiatry, France & Marc Jeannerod Institute of Cognitive Sciences UMR 5229, CNRS & Claude Bernard University, Lyon, France
Background: Midwives may be key stakeholders to improve perinatal mental healthcare (PMHC). Three systematic reviews considered midwives’ educational needs in perinatal mental health (PMH) or related interventions with a focus on depression or anxiety. This systematic review aims to review: 1) midwives’ educational/training needs in PMH; 2) the training programs in PMH and their effectiveness in improving PMHC.
Methods: We searched six electronic databases using a search strategy designed by a biomedical information specialist. Inclusion criteria were: (1) focus on midwives; (2) reporting on training needs in PMH, perinatal mental health problems or related conditions or training programs; (3) using quantitative, qualitative or mixed-methods design. We used the Mixed Methods Appraisal Tool for study quality.
Results: Of 4969 articles screened, 66 papers met eligibility criteria (47 on knowledge, skills or attitudes and 19 on training programs). Study quality was low to moderate in most studies. We found that midwives’ understanding of their role in PMHC (e.g. finding meaning in opening discussions about PMH; perception that screening, referral and support is part of their routine clinical duties) is determinant. Training programs had positive effects on proximal outcomes (e.g. knowledge) and contrasted effects on distal outcomes (e.g. number of referrals).
Conclusions: This review generated novel insights to inform initial and continuous education curriculums on PMH (e.g. focus on midwives’ understanding on their role in PMHC or content on person-centered care).
Registration details: The protocol is registered on PROSPERO (CRD42021285926)
1 Introduction
Perinatal Mental Health Problems (PMHPs) affect parents during pregnancy and the first year after childbirth and commonly consist of anxiety, non-psychotic depressive episode, psychotic episodes, post-traumatic stress disorder and adjustment disorder. Despite being often associated with poor parental and child outcomes ( 1 ), PMHPs remain predominantly unrecognized, undiagnosed and untreated ( 2 ).
Given their role in perinatal care providing multiple occasions to discuss perinatal mental health ( 3 ) - midwives may be key stakeholders to improve the detection, referral and management of PMHPs. Parents usually welcome midwives’ interest in their mental health and report to prefer discussing mental health issues with obstetric providers than with mental health providers ( 4 , 5 ). Assessing perinatal mental health (PMH) and detecting symptoms of postpartum depression, anxiety and psychosis are part of the essential competencies for midwifery practice according to the International Confederation of Midwives (2019) ( 6 ). However, and despite being in general interested in assessing perinatal mental health (PMH) and wellbeing ( 7 ), midwives report feeling less comfortable with putting competencies related to PMH into practice compared to those related physical health ( 8 , 9 ).
To our knowledge, three literature reviews have been conducted on midwives’ educational needs in perinatal mental health ( 7 , 10 , 11 ). These reviews reported a lack of knowledge, skills and confidence influential at different levels of the care pathway, e.g. detection, decision-making about referral and support. However, there remain some limitations to the current body of evidence. First, all reviews found low-to-moderate quality studies coming predominantly from high-income countries. Second, two out of three reviews ( 10 , 11 ) - conducted in 2017 (n=17 articles) and 2022 (43 articles) - focused on perinatal depression or perinatal anxiety and did not cover the full range of PMHPs as well as related conditions (e.g. substance use disorder, serious mental illness (SMI)) or autism). The third review ( 7 ) conducted in 2017 (n=22 articles) covered a wider range of PMHPs using an integrative review design, the other two ( 10 , 11 ) being systematic reviews. Third, previous reviews ( 7 , 10 , 11 ) focused on midwives’ knowledge, skills and attitudes and context-related factors. However, it remains unclear whether improvements in these areas translate into in routine clinical practice (e.g. improved detection of PMHPs or facilitated decision-making about referral to mental health providers). Fourth, case identification - using formal or informal screening methods - have contrasted effects on referral rates ( 7 ) and patient outcomes [e.g. limited effects of screening on depressive symptoms ( 12 , 13 )]. Fifth, two systematic reviews reported on training programs in perinatal depression [n=7 studies ( 10 ), n=12 studies ( 14 )]. However, these reviews included mixed samples [e.g. 37% midwives in Wang et al., 2022 ( 14 ) and 54% midwives in Legere et al., 2017 ( 10 )] and did not target the same set of skills [e.g. improving knowledge and detection ( 10 ); providing evidence-based interventions ( 14 )]. Reviews either investigated midwives’ training needs ( 7 , 11 ) or training interventions ( 10 , 14 ). The literature on training programs in PMH for student midwives and midwives remains scarce [n=4 studies ( 10 )]. A synthesis of evidence before this study is presented on Table 1 .
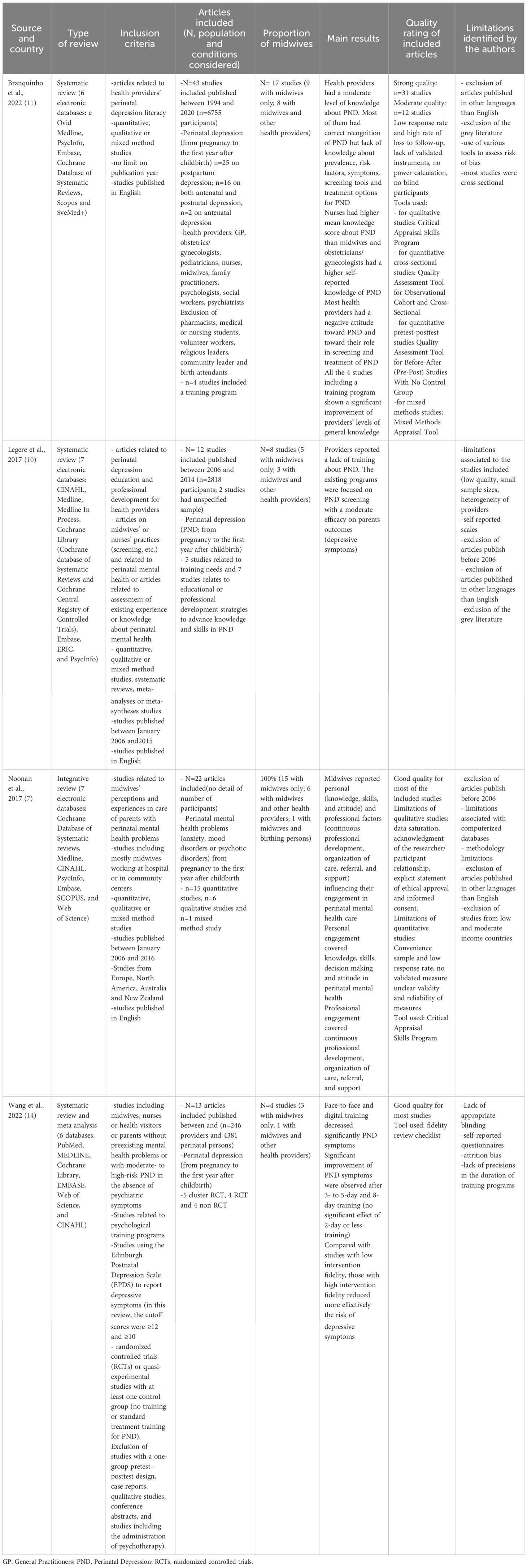
Table 1 Evidence before this study.
The present review primarily aims to identify and review: 1) midwives’ educational/training needs in PMH (i.e. beyond perinatal depression or anxiety to include PMHPs, SMI, substance use disorder, and autism); 2) the existing interventions and their effectiveness in improving detection and management of PMHPs.
2.1 Search strategy
The protocol for this systematic review was reported according to PRISMA guidelines ( 15 ). The search strategy was designed by a biomedical information specialist (WMB) from the Medical Library of Erasmus MC, University Medical Center Rotterdam ( 16 ). We searched Embase, MEDLINE, Web of Science, Cochrane Central Register of Controlled Trials, CINAHL and, PsycINFO for published, peer reviewed original articles. The search combined terms for (1) perinatal mental health problems, serious mental illness (i.e. schizophrenia, mood disorders, personality disorders, anxiety), eating disorders, substance use disorders or autism, and (2) midwives’ knowledge, attitudes, skills or training needs, as well as existing training programs for midwives on PMH. We included only published articles in English or French. No time restriction was set. The search was updated prior to publication on 21 June 2023. We hand-searched the reference list of three systematic literature reviews ( 7 , 10 , 11 ) for additional relevant articles. The full search strategy, search terms and syntax are presented in online Supplementary Table 1 .
2.2 Inclusion/exclusion criteria
To be included, articles had to meet all the following criteria: 1) focus on midwives (included midwives, nurse-midwives, registered midwives, registered midwives tutors, registered midwives prescribers and registered advanced midwives practitioners - referred as “midwives” in this review); 2) reporting on midwives’ training needs in PMH, PMHPs or related conditions or existing training programs that focus on the use of screening tools to detect PMHPs, on PMH in general or specific aspects of PMH; 3) using quantitative, qualitative or mixed-methods design. For training programs, we included uncontrolled and controlled studies (placebo, TAU or active comparators).
Our exclusion criteria were: 1) no full text available or studies published in languages other than English or French; 2) grey literature because the aim of this systematic review was to guide the development of future interventions; 3) training programs on psychological interventions (e.g. cognitive behavior therapy) because this review focused on interventions aiming at improving midwives’ training on essential competencies related to PMH (e.g. PMH assessment, detection, referral and support of parents with PMHPs).
2.3 Selection and coding
The screening process was conducted in two separate stages: 1) Two authors (M.D. and J.D) independently screened the title and abstracts of all non-duplicated papers excluding those not relevant. Potential discrepancies were resolved by consensus; 2) Two authors (M.D. and J.D) independently applied eligibility criteria and screened the full-text papers to select the included studies. Disputed items were solved discussing together and reading further the paper to reach a final decision. Supplementary Tables 2 , 3 present the list of included/excluded studies. Inter-rater reliability was calculated (kappa=0.90).
2.4 Data extraction
Two authors (MD and JD) performed independently the data extraction. For each study, we extracted the following information: general information (author, year of publication, country, design, type of study, population considered, period), assessment tools or methods, cultural aspects, the main findings and variables relating to quality assessment. For studies reporting on training programs, we also extracted information about the intervention (nature, type, length, targeted skills or outcomes, format), outcome measures and effectiveness on midwives’ knowledge, attitude, skills or routine use of screening tools to detect PMHPs or parents’ outcomes (e.g. depressive symptoms). Tables 2 – 6 present the factors associated with knowledge, skills, confidence and decisions about screening, referral or support. Supplementary Tables 4 , 5 present the detailed characteristics of the included studies.
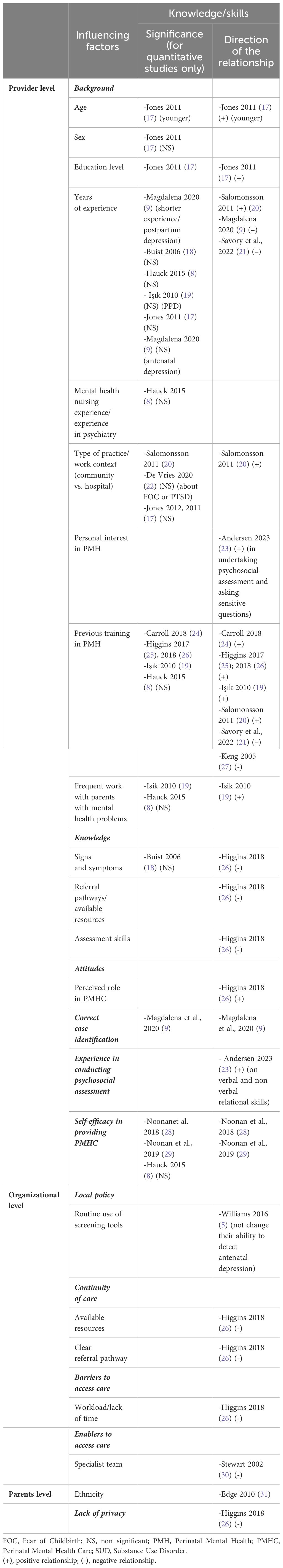
Table 2 Factors influencing the level of knowledge and skills.
Table 3 Factors influencing confidence and the perception of being well-equipped.
Table 4 Factors influencing decisions about screening.
Table 5 Factors influencing decisions about referral.
Table 6 Factors influencing decisions about support.
2.5 Quality assessment
Quality assessment was realized using the Mixed Methods Appraisal Tool (MMAT) ( 61 ). MMAT is a validated instrument to assess the methodological quality of qualitative, randomized controlled trials, non-randomized trials, descriptive studies, and mixed methods studies. It is comprised of five 5-item subscales assessing different aspects of quality (e.g. appropriateness of the selected design/methods/measurements, integration of quantitative and qualitative parts for mixed-methods studies). Two researchers (MD and JD) independently assessed methodological quality using the MMAT and extracted MMAT scores for each article. Discrepancies were resolved through consensus. The MMAT overall quality score and detailed scores are provided in Supplementary Tables 4 , 5 . The study protocol was registered on PROSPERO on November 1, 2021 (CRD42021285926).
Of the 9650 articles found during searches from inception to June 26 th 2023, 4969 references remained after removing all duplicates. Based on titles and abstracts, 4772 papers were excluded for lack of relevance. Our search strategy yielded 197 full-text articles. After conducting a full-text analysis of all these papers, we ended up with 66 relevant papers (47 on knowledge, skills or attitudes and 19 on training programs; PRISMA diagram on Figure 1 ).
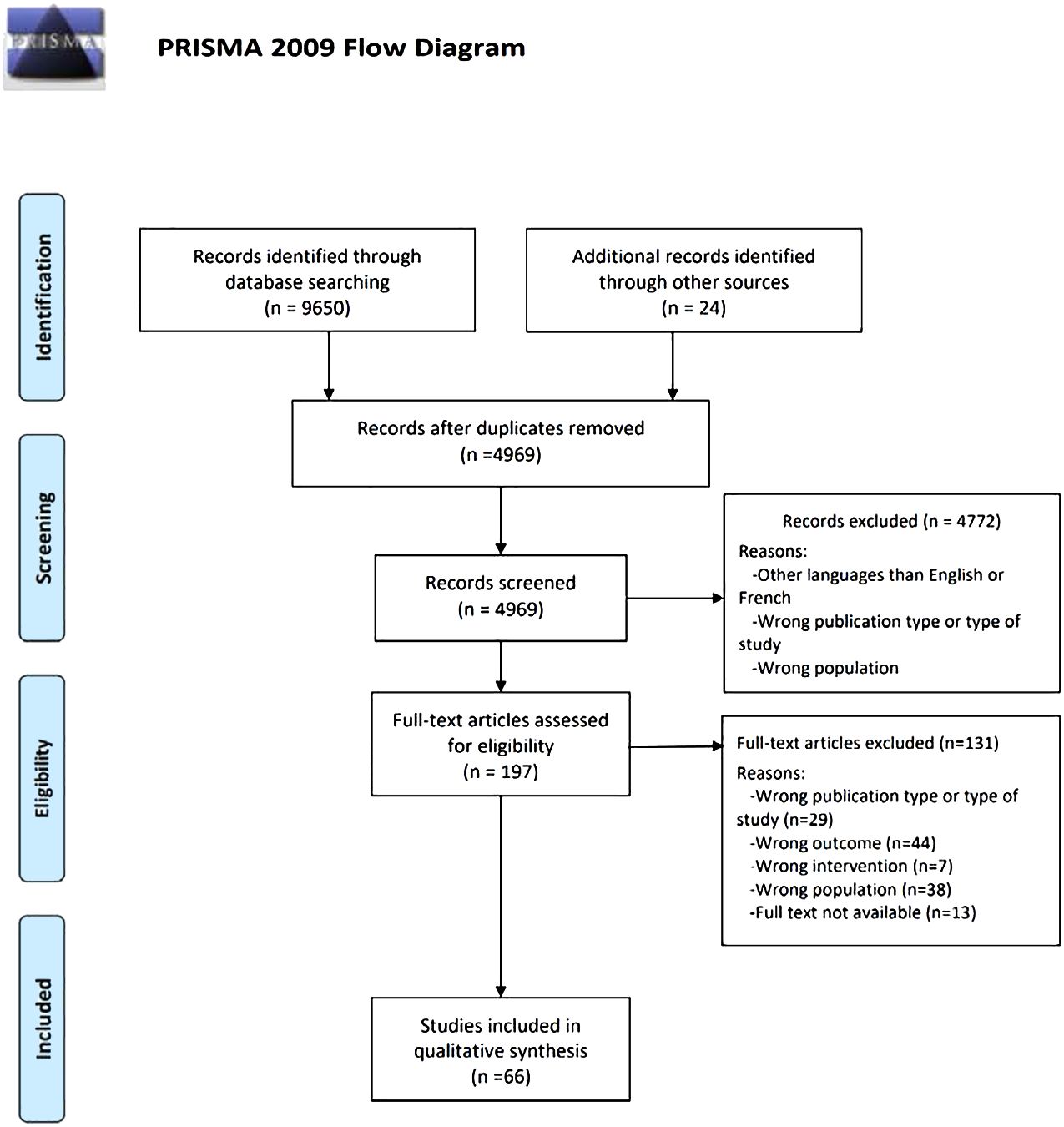
Figure 1 PRISMA diagram.
3.1 Study characteristics
The characteristics of the 66 included studies are presented on Tables 7 , 8 . Most studies were conducted in high-income countries (89.4%) and published after 2015 (50%). Study designs were quantitative (n=33; 50%), qualitative (n=22; 33.3%) or mixed-methods (n=11; 16.7%). Samples included qualified midwives (n=37; 56.0%), qualified midwives and other perinatal health providers (n=17; 25.8%) and student midwives (n=11; 16.7%). Qualified midwives had a variable level of training in PMH ranging from none to 90% (specified in 24 studies; most covered topics: general information about PMH and PMHPs; least covered topics: interviewing/counseling skills, psychopharmacology and suicide risk assessment). Eight studies (12.1%) reported on midwives’ mental health nursing experience (ranging from 0.8% to 30%) or placement experience in a mental health setting or a mother-baby unit during their studies (ranging to 9% to 23.2%). Four studies (6%) mentioned family or personal experience of mental health problems ranging from 25% to 66.3%. Most studies covered the entire perinatal period (n=44; 66.7%) and reported on PMHPs (n=32; 48.5%). The definition of PMHPs was highly variable across the studies (e.g. inclusion of conditions usually not considered as PMHPs, such as schizophrenia, bipolar disorder, personality disorders, self-harm, suicide eating disorders or SUD in 16 studies; definition restricted to anxiety, depression, postpartum psychosis and/or posttraumatic stress disorder in 9 studies; unspecified in 7 studies). One third of the included studies used validated instruments to assess outcomes (n=16; 36.4%). Five studies (7.6%) investigated the influence of cultural aspects on the detection and management of PMHPs.
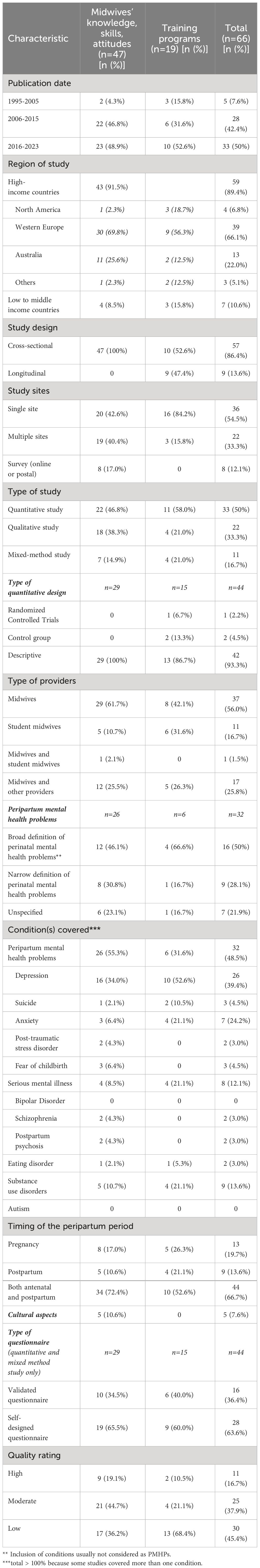
Table 7 Research characteristics of the 66 studies included in the review.
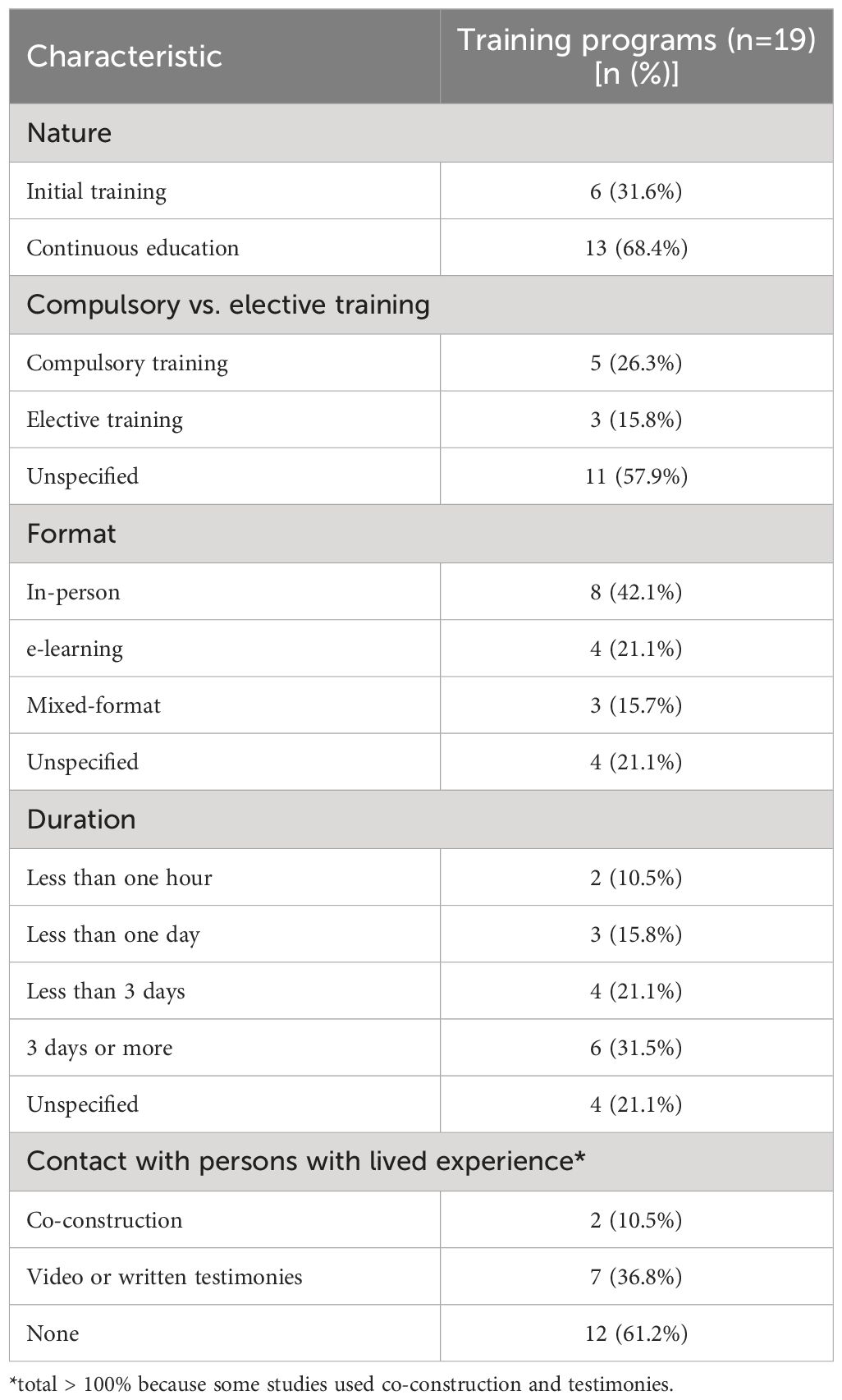
Table 8 Research characteristics of the training programs included in the review.
Of 15 studies reporting on a training program using a quantitative or a mixed-methods design, three used a waiting-list control group (20%; one randomized controlled trial (RCT)) and 13 (86.7%) were uncontrolled. Sample size was small in most studies (< 50 participants; n=9 studies). Nine studies (47.3%) reported contact with persons with lived experience when designing their training program. The training programs were heterogeneous in nature (initial training, n=6, 31.6%; continuous education, n=13, 68.4%), type, format and duration (ranging from 2 minutes to a fifteen-week module). All studies assessed training outcomes either immediately after (n=15; 79%) or up to 3 months after the intervention is delivered (n=4; 21%).
3.2 Quality assessment
The overall assessment score ranged from low (n=30, 45.4%; n=13, 68.4% for training programs) to high (n=11, 16.7%; n=2, 10.5%). For quantitative or mixed-methods studies, the reasons were convenience sampling (n=61 studies, 92.4%), sample size, low response rate (n=18 studies > 60%), limited use of validated outcome measures (36.4%), use of self-reported measures, absence or short duration of the follow-up period, limited integration of the results in mixed-methods studies and lack of controlled/RCT studies to evaluate the effectiveness of training programs. For qualitative studies, the reasons were interpretation bias (e.g. no investigator triangulation, the data being analyzed by only one researcher), absence of data saturation and lack of reflexivity.
3.3 Narrative review
Many studies found that midwives felt ill equipped to care for parents with PMHPs [e.g. ranging from 69.2% of 815 midwives in Jones et al., 2011 ( 17 ) to 82.2% of 157 midwives in Noonan et al., 2018 ( 28 )]. The reasons included insufficient initial training/continuous education on PMH (n=2 studies), perception that PMH assessment is not part of their role (n=2 studies), lack of knowledge about the detection, referral and management of PMHPs (n=12 studies). Compared with other perinatal health providers (GPs, health visitors, maternal child health nurses; n=11 studies), midwives had lower knowledge on PMH (n=2), felt less confident in the detection, referral or management of PMHPs (n=3) and had more negative attitudes toward their role in perinatal mental healthcare (PMHC) ( 57 ) or suicide prevention ( 40 ). Self-reported barriers to discuss PMH issues or self-reported interviewing skills did not differ between nurses and midwives ( 25 ). Student midwives’ knowledge, skills and attitudes in PMH did not clearly differ from those of qualified midwives (n=5 studies). On the job experience, learning from peers and attending to workshops/conferences were midwives’ main sources of knowledge (n=3 studies).
The factors positively associated with knowledge about PMHPs included the perception to be well equipped to provide PMHC (66.7% significance), previous training in PMH (50% significance), younger age ( 17 ), shorter work experience in general and as a midwife (20% significance), frequent contact with parents with PMHPs (50% significance) and type of practice (33.3% significance). Mental health nursing experience was positively associated with the perception to be well equipped to provide PMHC, but not with higher knowledge about PMH ( 8 ). No significant association was found between confidence in providing PMHC and other factors [e.g. age, personal experience of mental health problems, frequent contact with parents with PMHPs ( 29 )], except for PMH education and case identification ( 8 ). Compared with suicide risk assessment and other conditions (e.g. postpartum psychosis, SMI, eating disorders or posttraumatic stress disorder; n=4 studies), midwives reported higher knowledge, better skills and more confidence in detecting and managing perinatal depression and anxiety. Midwives felt in general ill equipped to care for postpartum psychosis, eating disorders, posttraumatic stress and SMI (n=10 studies) and reported ambivalent or negative attitudes toward parents with these conditions (n=7 studies). Knowledge about PMHPs varied according to the assessment method [i.e. higher self-report knowledge than researcher-rated knowledge ( 19 , 43 )] and the timing of perinatal period (i.e. higher in the postpartum than during pregnancy, n=5 studies).
3.3.1 Detection/screening
The practices and policies around screening for PMHPs varied across studies. There was a considerable overlap between the factors influencing the decision to screen, refer and support parents with PMHPs. Midwives’ attitudes toward their role in PMHC (e.g. personal interest in PMHPs and perception that it is part of their role) played a central role in decision-making about opening discussions about PMH (n=12 studies), referral ( 42 , 57 ) and support parents with PMHPs (n=6). Cultural aspects and stigma toward parents with ethnic minority background (e.g. underestimation of depression and suicide risks) impacted midwives’ ability to detect and manage PMHPs and parents’ maternity care experiences (n=4 studies). Other common factors included lack of knowledge about PMHPs (n=20 studies), referral pathways (n=8) and treatment options (n=10), lack of time/clear referral pathways (n=22) and stigma related to preexisting mental health problems/SMI (n=8).
Midwives considered routine universal screening as useful in two studies ( 5 , 56 ). Facilitators included self-efficacy in screening (n=10 studies), person-centered care (n=3), the presence of a specialist team (n=2 studies) and mandatory routine screening (n=2). Barriers to screening included longer work experience ( 42 ), lack of knowledge about screening tools (n=11 studies), local/national guidelines on screening (ranging from 12.8% to 53%, n=4 studies), and negative attitudes toward the use of formal screening tools (n=12 studies). The relationship between personal/family experience of PMHPs was either positive [e.g. reduces stigma and allows to relate with parents ( 29 )] or negative ( 45 ). For student midwives, the presence of specialist midwives was both a facilitator [e.g. provides referral options and placement opportunities ( 50 )] and a barrier to screening [e.g. perception that it is not part of their role ( 43 )]. Of note, specialist midwives reported to lack confidence in opening discussions about PMH and to lack knowledge about SMI ( 21 ).
The reasons underlying negative attitudes toward the use of formal screening tools included perceiving the questions as intrusive (n=3 studies), not clearly understanding the purpose of doing so (n=3 studies), inexperience in conducting assessment and feeling compelled to undertake it as a standardized survey ( 23 ), the fear of “not doing it right” (n=2) and discomfort when disclosure occurs (n=7 studies). Some studies reported a flexible use of screening tools (e.g. modified wording or timing of the questions; n=4 studies) and one study outlined the importance of person-centered care in conducting assessment ( 23 ). Conversely, midwives who lacked clarity about their role in PMHC reported feelings of inadequacy resulting in a non-flexible use of screening tools and a distant and superficial manner of asking questions ( 23 ). Midwives reported to feel more comfortable in opening discussions about PMH during follow-up visits compared with the booking appointment (n=5 studies). Alternatives to formal screening included assessing previous psychiatric history/current symptoms ( 28 ), using general open-ended questions (n=5 studies), behavioral observation (n=4 studies) and labor debriefing ( 46 ). Training needs covered knowledge about PMHPs (n=9 studies), screening tools (n=4 studies) and cultural issues and interviewing/distress management skills (n=10 studies).
3.3.2 Referral/support
Midwives reported to feel confident in their ability to refer parents with PMHPs to other health providers including specialist mental health services (n=7 studies). The opposite was found for parents with postpartum psychosis, eating disorders or SMI. High self-reported confidence in referring parents to other providers did not in practice lead to a higher number of referrals ( 37 ). The proportion of midwives indicating to feel confident in supporting parents with PMHPs in self-report questionnaires ranged from 34% to 53% (n=5 studies). Accurate case identification ( 9 ), an established diagnosis of PMHP ( 53 ) and parents’ preferences ( 53 ) influenced decision-making about referral. Other factors included the intention to collaborate with other providers (n=2) or conversely a lack of trust/a reluctance to disclose sensitive information to other providers (n=3 studies).
3.3.3 Training outcomes
All training programs reported improved self-rated knowledge, skills, attitudes and confidence in screening, referring and supporting parents with PMHPs (n=19). Few significant positive training effects were reported due to small-sized samples and lack of controlled/RCT studies. Results included positive effects on empathic communication skills ( 62 , 63 ), case identification ( 64 , 65 ) and the detection of PMHPs in maternity wards ( 66 – 68 ). Contrasted results were found on the number of referrals [n=2 studies; 50% significance; positive effect on self-reported referrals in Pearson et al. (2019) ( 69 ) and no significant effect in Wickberg et al. (2005, 70 )]. No significant effects were found on depressive symptoms ( 70 ) and attitudes toward providing psychological support to parents with PMHPs ( 63 ). Participants’ satisfaction rates were high, the insight provided by parents with lived experience of PMHP being determinant for student midwives (n=4 studies). Barriers included an excessive workload ( 71 ) and for student midwives, elective participation and late delivery within midwifery studies ( 72 ). No difference related to the format of the intervention was reported.
4 Discussion
To our knowledge, this systematic review of 66 studies is one of the first exploring both the training needs in PMH identified by student midwives and midwives and the training programs designed for this population. Overall, a main finding of this systematic review is that although detection, referral and support of parents with PMHPs are part of the essential competencies for midwifery practice according to the ICM (2019) ( 6 ), their effective translation into routine clinical practice may depend on midwives’ understanding of their role in PMHC, i.e. finding meaning in opening discussions about PMH with all parents and the perception that this is part of their routine clinical duties. This suggests that this factor should be targeted by raining interventions aiming at improving detection and management of PMHPs, above and beyond knowledge, confidence, and skills.
Extending the findings of previous reviews ( 7 , 10 , 11 ), we found that although most midwives consider they have a role in PMHC (this aligning with ICM essential competencies for midwifery practice; 2019 ( 6 )), their understanding of that role remains often unclear. Several potential explaining factors have been identified. First, while this topic may be central for a meaningful engagement into providing PMHC, only a few training programs explored the role of midwives in PMHC ( 71 , 73 ). Second, there is a view - in particular in student midwives - that addressing PMH needs is less a priority than addressing physical health needs and that other providers should assume this responsibility ( 31 , 35 , 39 , 43 , 50 , 52 ). The interaction between this view, mental illness stigma and racism toward parents with ethnic minority background contributed to poorer maternity experiences and under-detection of PMHPs ( 19 , 35 , 73 ).
Third, some midwives consider their role as limited to assessing PMH and wellbeing and as appropriate, referring to other health providers ( 9 , 18 , 55 , 57 , 58 ), whereas others have a broad perception of their role that include providing support, psychoeducation and with adequate training counseling interventions ( 21 , 24 , 25 , 42 ). Recent meta-analyses showed positive effects of midwife-led counseling on anxiety and depressive symptoms after at least 3 days of training ( 14 , 74 ). This concurs with recent calls for a better integration of mental health and perinatal health care and an extension of the scope of midwifery practice to include strengths-based case management and psychological interventions for parents with PMHPs ( 50 , 75 – 77 ). Given there is some degree of difference between midwives’ perception of their role in PMHC and what is required as essential competencies for midwifery practice (ICM, 2019) ( 6 ), an explicit focus on midwives’ role in PMHC should be made in initial and continuous midwifery education ( 72 , 73 , 76 , 78 ). Fourth, most student midwives, midwives and specialist midwives reported negative attitudes toward parents with suicide ideations, postpartum psychosis and SMI ( 21 , 35 , 40 , 43 , 57 , 79 ). Aligning with this, Hawthorne et al. (2020) ( 79 ) found that student midwives had more negative attitudes toward persons with mental illness compared with mental health nursing students. However, other studies reported that midwives consider caring for parents with these conditions as part of their role but felt ill equipped to do so and expressed the need for additional training ( 8 , 28 , 29 , 34 , 39 , 49 ).
4.1 Implications for training interventions
While the need to improve midwives’ initial and continuous education in PMH is now well established ( 7 , 10 ), student midwives, midwives and even specialist midwives continue reporting to feel ill prepared to care for parents with PMHP in particular in case of co-occurring SMI ( 9 , 21 , 24 , 33 , 34 , 36 ). Moreover, the proportion of midwives who received education in PMH - in particular in topics such as mental health/suicide risk assessment - remains consistently low. Given suicide is the leading cause of maternal mortality in the 1 st year postpartum in high-income countries, this is concerning ( 1 , 80 ).
Aligning with previous research ( 7 , 10 , 11 ), this systematic review found that education/training programs had positive effects on proximal outcomes (e.g. midwives’ knowledge, skills, attitudes and confidence in providing PMHC) and contrasted effects on distal outcomes (e.g. screening in maternity wards, the number of referrals or depressive symptoms). This could be related to methodological bias (e.g. lack of RCT or quasi-experimental studies). There is a need for high-quality studies on interventions designed following the Medical Research Council framework for complex interventions ( 81 ), which proposes among other core elements to: 1) take into account the context of delivery; 2) use a clear theoretical basis (e.g. how the intervention is expected to produce positive effects and under which conditions) and; 3) promote a meaningful engagement of persons with lived experience among other relevant stakeholders.
According to Wadephul et al. (2018) ( 82 ) framework for assessing midwifery practice in PMH, knowledge, confidence, attitudes and organizational factors influence midwives’ ability to detect and manage PMHPs. However, higher knowledge about PMH does not necessarily translate into higher confidence in providing PMHC and the opposite ( 8 ). As reported in one of the articles included in this review ( 42 ) and aligning with the theory of planned behavior ( 82 ), additional factors such as individual values, e.g. personal interest in PMH, and behavioral intent (e.g. the intention to open discussions about PMH) could influence detection and decision-making about referral and support in PMHPs and thus be relevant for midwifery education.
To improve midwives’ engagement into PMHC, training programs should put PMH in context (e.g. the positive outcomes that could be achieved with appropriate support) before covering topics related to specific knowledge or skills ( 5 , 38 , 49 , 50 , 53 , 54 ). Instead of focusing only on biomedical aspects (e.g. the signs, risk factors, consequences and treatments of PMHPs), programs should propose a continuum approach of PMH that covers the positive aspects of the person’s life including wellbeing and personal recovery ( 83 – 86 ).
Extending the findings of previous reviews ( 7 , 10 , 11 ), training programs should target student midwives, midwives and specialist midwives and cover interviewing and distress management skills with a focus on specific aspects (e.g. opening discussions without feeling intrusive, using flexibly screening tools and reacting in case of a positive answer) ( 5 , 21 , 38 , 45 , 49 , 50 , 53 , 54 ). In addition, training programs should include clinical supervision by mental health providers during and after intervention delivery ( 14 ). Future studies should include a longer follow-up period, as the embedding of practice change requires a minimum of nine months after the intervention is delivered ( 87 ).
Finally, while contact with persons with lived experience is one of the most effective strategies to reduce mental illness stigma in the general public and in frontline health providers ( 88 , 89 ), this review found a very low proportion of training programs that engaged persons with lived experience in the conception and delivery of the intervention. Initial and continuous midwifery education curriculums on PMH should involve persons with lived experience - co-design and co-intervention - and include content about personal recovery/person-centered care ( 72 , 73 , 81 , 84 , 90 – 92 ).
4.2 Limitations
There are limitations. First, despite a growing number of published studies on midwives’ training needs in PMH and training interventions designed for this population (n=66 studies in this review vs. n=22 ( 7 ); n=17 ( 10 ); n=43 ( 11 );), the quality of the included studies remains low to moderate, a concerning finding given the clinical relevance of this topic that is also a considerable limitation. Among other methodological bias, the absence of a clear theoretical basis for designing interventions ( 81 ), the small or unjustified sample sizes, the lack of RCT/quasi-experimental studies, the absence of control groups (or active comparators in controlled studies) and the absence or short duration of follow-up makes unclear whether interventions have positive effects on proximal or distal outcomes. Future high-quality studies on this topic are therefore needed. Despite these limitations, the inclusion of quantitative, qualitative and mixed-methods studies provided a complete synthesis of the available evidence and consistent messages emerged across studies. Second, relevant studies may have been missed since we excluded studies published in other languages than English or French and did not include the grey literature in our searches.
5 Conclusion
This review generated novel insights to inform initial and continuous midwifery education curriculums on PMH (e.g. co-design with persons with lived experience, focus on midwives’ understanding on their role in PMHC or inclusion on content on person-centered care).
Author contributions
MD: Conceptualization, Formal analysis, Writing – original draft. CD: Writing – review & editing. ML: Conceptualization, Writing – review & editing. WB: Conceptualization, Data curation, Methodology, Writing – review & editing. CM: Writing – review & editing. JD: Conceptualization, Formal analysis, Project administration, Supervision, Validation, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors wish to thank Dr. M.F.M. Engel and Mrs. C.D. Niehot medical information specialist from the Erasmus MC Medical Library for updating the search strategies. The authors are grateful to the reviewers of a previous version of the manuscript for their helpful comments.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1345738/full#supplementary-material
Supplementary Table 1 | Search strategy, search terms and syntax.
Supplementary Table 2 | List of excluded studies.
Supplementary Table 3 | List of included studies.
Supplementary Table 4 | Characteristics of included studies about midwives' knowledge, skills and attitude.
Supplementary Table 5 | Characteristics of included studies about midwives' needs for peripartum mental health training program.
Supplementary Table 6 | List of abbreviations.
1. Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry . (2020) 19:313–27. doi: 10.1002/wps.20769
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Cox EQ, Sowa NA, Meltzer-Brody SE, Gaynes BN. The perinatal depression treatment cascade: baby steps toward improving outcomes. J Clin Psychiatry . (2016) 77:1189–200. doi: 10.4088/JCP.15r10174
3. Moss KM, Reilly N, Dobson AJ, Loxton D, Tooth L, Mishra GD. How rates of perinatal mental health screening in Australia have changed over time and which women are missing out. Aust N Z J Public Health . (2020) 44:301–6. doi: 10.1111/1753-6405.12999
4. Kingston D, McDonald S, Tough S, Austin MP, Hegadoren K, Lasiuk G. Public views of acceptability of perinatal mental health screening and treatment preference: a population based survey. BMC Preg. Childbirth . (2014) 14:67. doi: 10.1186/1471-2393-14-67
CrossRef Full Text | Google Scholar
5. Williams CJ, Turner KM, Burns A, Evans J, Bennert K. Midwives and women’s views on using UK recommended depression case finding questions in antenatal care. Midwifery . (2016) 35:39–46. doi: 10.1016/j.midw.2016.01.015
6. International Confederation of Midwives (ICM). Essential competences for midwifery practice (2019). Available online at: file:///C:/Users/marin/Downloads/icm-competencies-en-print-october-2019_final_18-oct-5db05248843e8.pdf .
Google Scholar
7. Noonan M, Doody O, Jomeen J, Galvin R. Midwives’ perceptions and experiences of caring for women who experience perinatal mental health problems: An integrative review. Midwifery . (2017) 45:56–71. doi: 10.1016/j.midw.2016.12.010
8. Hauck YL, Kelly G, Dragovic M, Butt J, Whittaker P, Badcock JC. Australian midwives knowledge, attitude and perceived learning needs around perinatal mental health. Midwifery . (2015) 31:247–55. doi: 10.1016/j.midw.2014.09.002
9. Magdalena CD, Tamara WK. Antenatal and postnatal depression - Are Polish midwives really ready for them? Midwifery . (2020) 83:102646. doi: 10.1016/j.midw.2020.102646
10. Legere LE, Wallace K, Bowen A, McQueen K, Montgomery P, Evans M. Approaches to health-care provider education and professional development in perinatal depression: a systematic review. BMC Preg. Childbirth . (2017) 17:239. doi: 10.1186/s12884-017-1431-4
11. Branquinho M, Shakeel N, Horsch A, Fonseca A. Frontline health professionals’ perinatal depression literacy: A systematic review. Midwifery . (2022) 111:103365. doi: 10.1016/j.midw.2022.103365
12. Waqas A, Koukab A, Meraj H, Dua T, Chowdhary N, Fatima B, et al. Screening programs for common maternal mental health disorders among perinatal women: report of the systematic review of evidence. BMC Psychiatry . (2022) 22:54. doi: 10.1186/s12888-022-03694-9
13. Beck A, Hamel C, Thuku M, Esmaeilisaraji L, Bennett A, Shaver N, et al. Screening for depression among the general adult population and in women during pregnancy or the first-year postpartum: two systematic reviews to inform a guideline of the Canadian Task Force on Preventive Health Care. Syst Rev . (2022) 11:176. doi: 10.1186/s13643-022-02022-2
14. Wang TH, Tzeng YL, Teng YK, Pai LW, Yeh TP. Evaluation of psychological training for nurses and midwives to optimise care for women with perinatal depression: a systematic review and meta-analysis. Midwifery . (2022) 104:103160. doi: 10.1016/j.midw.2021.103160
15. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev . (2015) 4:1. doi: 10.1186/2046-4053-4-1
16. Bramer WM, Milic J, Mast F. Reviewing retrieved references for inclusion in systematic reviews using EndNote. J Med Libr Assoc . (2017) 105:84–7. doi: 10.5195/jmla.2017.111
17. Jones CJ, Creedy DK, Gamble JA. Australian midwives’ knowledge of antenatal and postpartum depression: a national survey. J Midwifery Womens Health . (2011) 56:353–61. doi: 10.1111/j.1542-2011.2011.00039.x
18. Buist A, Bilszta J, Milgrom J, Barnett B, Hayes B, Austin MP. Health professional’s knowledge and awareness of perinatal depression: results of a national survey. Women Birth . (2006) 19:11–6. doi: 10.1016/j.wombi.2005.12.001
19. Işık SN, Bilgili N. Postnatal depression: Midwives’ and nurses’ knowledge and practices. Erciyes Med J . (2010) 32:265–74.
20. Salomonsson B, Alehagen S, Wijma K. Swedish midwives’ views on severe fear of childbirth. Sex Reprod Healthc . (2011) 2:153–9. doi: 10.1016/j.srhc.2011.07.002
21. Savory NA, Sanders J, Hannigan B. Midwives’ experiences of supporting women’s mental health: A mixed-method study. Midwifery . (2022) 111:103368. doi: 10.1016/j.midw.2022.103368
22. de Vries NE, Stramrood CAI, Sligter LM, Sluijs AM, van Pampus MG. Midwives’ practices and knowledge about fear of childbirth and postpartum posttraumatic stress disorder. Women Birth . (2020) 33:e95–e104. doi: 10.1016/j.wombi.2018.11.014
23. Andersen CG, Thomsen LLH, Gram P, Overgaard C. ‘It’s about developing a trustful relationship’: A Realist Evaluation of midwives’ relational competencies and confidence in a Danish antenatal psychosocial assessment programme. Midwifery . (2023) 122:103675. doi: 10.1016/j.midw.2023.103675
24. Carroll M, Downes C, Gill A, Monahan M, Nagle U, Madden D, et al. Knowledge, confidence, skills and practices among midwives in the republic of Ireland in relation to perinatal mental health care: The mind mothers study. Midwifery . (2018) 64:29–37. doi: 10.1016/j.midw.2018.05.006
25. Higgins A, Downes C, Carroll M, Gill A, Monahan M. There is more to perinatal mental health care than depression: Public health nurses reported engagement and competence in perinatal mental health care. J Clin Nurs . (2017) 27:e476–87. doi: 10.1111/jocn.13986
26. Higgins A, Downes C, Monahan M, Gill A, Lamb SA, Carroll M. Barriers to midwives and nurses addressing mental health issues with women during the perinatal period: The Mind Mothers study. J Clin Nurs . (2018) 27:872–1883. doi: 10.1111/jocn.14252
27. Keng SL. Malaysian midwives’ views on postnatal depression. Br J Midwifery . (2005) 13:78–86. doi: 10.12968/bjom.2005.13.2.17465
28. Noonan M, Jomeen J, Galvin R, Doody O. Survey of midwives’ perinatal mental health knowledge, confidence, attitudes and learning needs. Women Birth . (2018) 31:e358–66. doi: 10.1016/j.wombi.2018.02.002
29. Noonan M, Galvin R, Jomeen J, Doody O. Public health nurses’ perinatal mental health training needs: A cross sectional survey. J Adv Nurs . (2019) 75:2535–47. doi: 10.1111/jan.14013
30. Stewart C, Henshaw C. Midwives and perinatal mental health. Br J Midwifery . (2002) 10:117–21. doi: 10.12968/bjom.2002.10.2.10186
31. Edge D. Falling through the net - black and minority ethnic women and perinatal mental healthcare: health professionals’ views. Gen Hosp Psychiatry . (2010) 32:17–25. doi: 10.1016/j.genhosppsych.2009.07.007
32. Whitehead R, O’Callaghan F, Gamble J, Reid N. Contextual influences experienced by Queensland midwives: a qualitative study focusing on alcohol and other substance use during pregnancy. Int J Childbirth . (2019) 9:80–91. doi: 10.1891/2156-5287.9.2.80
33. Cunningham C, Galloway S. Let’s end the postcode lottery. Community Practitioner . (2019) 92:26–9.
34. Dubreucq M, Jourdan S, Poizat A, Dubreucq J. Ressenti des sages-femmes dans la prise en charge en suites de couche des patientes avec troubles psychiques sévères: une analyse qualitative (Midwives’ feelings about the post-partum care of women with severe mental illness: A qualitative analysis). Encephale . (2020) 46:226–30. doi: 10.1016/j.encep.2019.07.009
35. Phillips L. Assessing the knowledge of perinatal mental illness among student midwives. Nurse Educ Pract . (2015) 15:463–9. doi: 10.1016/j.nepr.2014.09.003
36. Bye A, Shawe J, Bick D, Easter A, Kash-Macdonald M, Micali N. Barriers to identifying eating disorders in pregnancy and in the postnatal period: a qualitative approach. BMC Preg. Childbirth . (2018) 18:114. doi: 10.1186/s12884-018-1745-x
37. Jones CJ, Creedy DK, Gamble JA. Australian midwives’ awareness and management of antenatal and postpartum depression. Women Birth . (2012) 25:23–8. doi: 10.1016/j.wombi.2011.03.001
38. Oni HT, Buultjens M, Blandthorn J, Davis D, Abdel-Latif M, Islam MM. Barriers and facilitators in antenatal settings to screening and referral of pregnant women who use alcohol or other drugs: A qualitative study of midwives’ experience. Midwifery . (2020) 81:102595. doi: 10.1016/j.midw.2019.102595
39. McCauley K, Elsom S, Muir-Cochrane E, Lyneham J. Midwives and assessment of perinatal mental health. J Psychiatr Ment Health Nurs . (2011) 18:786–95. doi: 10.1111/jpm.2011.18.issue-9
40. Lau R, McCauley K, Barnfield J, Moss C, Cross W. Attitudes of midwives and maternal child health nurses towards suicide: A cross-sectional study. Int J Ment Health Nurs . (2015) 24:561–8. doi: 10.1111/inm.12162
41. Sanders LB. Attitudes, perceived ability, and knowledge about depression screening: a survey of certified nurse-midwives/certified midwives. J Midwifery Womens Health . (2006) 51:340–6. doi: 10.1016/j.jmwh.2006.02.011
42. Fontein-Kuipers YJ, Budé L, Ausems M, de Vries R, Nieuwenhuijze MJ. Dutch midwives’ behavioural intentions of antenatal management of maternal distress and factors influencing these intentions: an exploratory survey. Midwifery . (2014) 30:234–41. doi: 10.1016/j.midw.2013.06.010
43. Jarrett P. Student midwives’ knowledge of perinatal mental health. Br J Midwifery . (2015) 23:32–9. doi: 10.12968/bjom.2015.23.1.32
44. Shahid Ali S, Letourneau N, Rajan A, Jaffer S, Adnan F, Asif N, et al. Midwives’ perspectives on perinatal mental health: A qualitative exploratory study in a maternity setting in Karachi, Pakistan. Asian J Psychiatr . (2023) 80:103356. doi: 10.1016/j.ajp.2022.103356
45. Fletcher A, Murphy M, Leahy-Warren P. Midwives’ experiences of caring for women’s emotional and mental well-being during pregnancy. J Clin Nurs . (2021) 30:1403–16. doi: 10.1111/jocn.15690
46. Gibb S, Hundley V. What psychosocial well-being in the postnatal period means to midwives. Midwifery . (2007) 23:413–24. doi: 10.1016/j.midw.2006.07.005
47. Asare SF, Rodriguez-Muñoz MF. Understanding healthcare professionals’ Knowledge on perinatal depression among women in a tertiary hospital in Ghana: A qualitative study. Int J Environ Res Public Health . (2022) 19:15960. doi: 10.3390/ijerph192315960
48. Jomeen J, Glover LF, Davies SA. Midwives’ illness perceptions of antenatal depression. Br J Midwifery . (2009) 17:296–303. doi: 10.12968/bjom.2009.17.5.42221
49. McGlone C, Hollins Martin CJ, Furber C. Midwives’ experiences of asking the Whooley questions to assess current mental health: a qualitative interpretive study. J Reprod infant Psychol . (2016) 34:383–93. doi: 10.1080/02646838.2016.1188278
50. McGookin A, Furber C, Smith DM. Student midwives’ awareness, knowledge, and experiences of antenatal anxiety within clinical practice. J Reprod Infant Psychol . (2017) 35:380–93. doi: 10.1080/02646838.2017.1337270
51. Ross-Davie M, Elliott S, Sarkar A, Green L. A public health role in perinatal mental health: are midwives ready? Br J Midwifery . (2006) 14:330–4. doi: 10.12968/bjom.2006.14.6.21181
52. Schouten BC, Westerneng M, Smit AM. Midwives’ perceived barriers in communicating about depression with ethnic minority clients. Patient Educ Couns . (2021) 104:2393–9. doi: 10.1016/j.pec.2021.07.032
53. Madden D, Sliney A, O’Friel A, McMackin B, O’Callaghan B, Casey K, et al. Using action research to develop midwives’ skills to support women with perinatal mental health needs. J Clin Nurs . (2018) 27:561–71. doi: 10.1111/jocn.13908
54. Jarrett P. Attitudes of student midwives caring for women with perinatal mental health problems. Br J Midwifery . (2014) 22:718–24. doi: 10.12968/bjom.2014.22.10.718
55. Jones CJ, Creedy DK, Gamble JA. Australian midwives’ attitudes towards care for women with emotional distress. Midwifery . (2012) 28:216–21. doi: 10.1016/j.midw.2010.12.008
56. Willey SM, Gibson-Helm ME, Finch TL, East CE, Khan NN, Boyd LM, et al. Implementing innovative evidence-based perinatal mental health screening for women of refugee background. Women Birth . (2020) 33:e245–55. doi: 10.1016/j.wombi.2019.05.007
57. Rothera I, Oates M. Managing perinatal mental health: A survey of practitioners’ views. Br J Midwifery . (2011) 19:04–313. doi: 10.12968/bjom.2011.19.5.304
58. McCann TV, Clark E. Australian Bachelor of Midwifery students’ mental health literacy: an exploratory study. Nurs Health Sci . (2010) 12:14–20. doi: 10.1111/j.1442-2018.2009.00477.x
59. Salomonsson B, Wijma K, Alehagen S. Swedish midwives’ perceptions of fear of childbirth. Midwifery . (2010) 26:327–37. doi: 10.1016/j.midw.2008.07.003
60. Nyberg K, Lindberg I, Öhrling K. Midwives’ experience of encountering women with posttraumatic stress symptoms after childbirth. Sex Reprod Healthc . (2010) 1:55–60. doi: 10.1016/j.srhc.2010.01.003
61. Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed methods appraisal tool (MMAT), version 2018. Registration of copyright (#1148552) . (2018) Canadian Intellectual Property Office, Industry Canada.
62. Fox D, Solanki K, Brown G, Catling C, Scarf V, Sheehy A, et al. Perinatal mental healthcare: Developing skills in midwifery students. Women Birth . (2023) 36:167–70. doi: 10.1016/j.wombi.2022.11.005
63. Shinohara E, Ohashi Y, Hada A, Usui Y. Effects of 1-day e-learning education on perinatal psychological support skills among midwives and perinatal healthcare workers in Japan: a randomised controlled study. BMC Psychol . (2022) 10:133. doi: 10.1186/s40359-022-00832-6
64. Badiya PK, Siddabattuni S, Dey D, Hiremath AC, Nalam RL, Srinivasan V, et al. Task-sharing to screen perinatal depression in resource limited setting in India: Comparison of outcomes based on screening by non-expert and expert rater. Asian J Psychiatr . (2021) 62:102738. doi: 10.1016/j.ajp.2021.102738
65. Yamashita H, Ariyoshi A, Uchida H, Tanishima H, Kitamura T, Nakano H. Japanese midwives as psychiatric diagnosticians: application of criteria of DSM-IV mood and anxiety disorders to case vignettes. Psychiatry Clin Neurosci . (2007) 61:226–33. doi: 10.1111/j.1440-1819.2007.01659.x
66. Elliott S, Ross-Davie M, Sarkar A, Green L. Detection and initial assessment of mental disorder: the midwife’s role. Br J Midwifery . (2007) 15:759–64. doi: 10.12968/bjom.2007.15.12.27791
67. Jardri R, Maron M, Pelta J, Thomas P, Codaccioni X, Goudemand M, et al. Impact of midwives’ training on postnatal depression screening in the first week post delivery: a quality improvement report. Midwifery . (2010) 26:622–9. doi: 10.1016/j.midw.2008.12.006
68. Toler S, Stapleton S, Kertsburg K, Callahan TJ, Hastings-Tolsma M. Screening for postpartum anxiety: A quality improvement project to promote the screening of women suffering in silence. Midwifery . (2018) 62:161–70. doi: 10.1016/j.midw.2018.03.016
69. Pearson P, Klima C, Snyder M. Reducing barriers that hinder obstetric providers from addressing perinatal depression: A provider education module. J Dr Nurs Pract . (2019) 12:212–24. doi: 10.1891/2380-9418.12.2.212
70. Wickberg B, Tjus T, Hwang P. Using the EPDS in routine antenatal care in Sweden: a naturalistic study. J Reprod infant Psychol . (2005) 23:33–41. doi: 10.1080/02646830512331330956
71. Forrest E, Poat A. Perinatal mental health education for midwives in Scotland. Br J Midwifery . (2010) 18:280–4. doi: 10.12968/bjom.2010.18.5.47853
72. Higgins A, Carroll M, Sharek D. It opened my mind: student midwives’ views of a motherhood and mental health module. MIDIRS Midwifery Digest . (2012) 22:287–92.
73. Larkin V, Flaherty A, Keys C, Yaseen J. Exploring maternal perinatal mental health using a blended learning package. Br J Midwifery . (2014) 22:210–7. doi: 10.12968/bjom.2014.22.3.210
74. Wang TH, Pai LW, Tzeng YL, Yeh TP, Teng YK. Effectiveness of nurses and midwives-led psychological interventions on reducing depression symptoms in the perinatal period: A systematic review and meta-analysis. Nurs Open . (2021) 8:2117–30. doi: 10.1002/nop2.764
75. Laios L, Rio I, Judd F. Improving maternal perinatal mental health: integrated care for all women versus screening for depression. Australas Psychiatry . (2013) 21:171–5. doi: 10.1177/1039856212466432
76. Coates D, Foureur M. The role and competence of midwives in supporting women with mental health concerns during the perinatal period: A scoping review. Health Soc Care Community . (2019) 27:e389–405. doi: 10.1111/hsc.12740
77. WHO. Guide for integration of perinatal mental health in maternal and child health services . Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO (2022).
78. Higgins A, Carroll M, Sharek D. Impact of perinatal mental health education on student midwives’ knowledge, skills and attitudes: A pre/post evaluation of a module of study. Nurse Educ Today . (2016) 36:364–9. doi: 10.1016/j.nedt.2015.09.007
79. Hawthorne A, Fagan R, Leaver E, Baxter J, Logan P, Snowden A. Undergraduate nursing and midwifery student’s attitudes to mental illness. Nurs Open . (2020) 7:1118–28. doi: 10.1002/nop2.494
80. ENCMM 6e rapport de l’Enquête Nationale Confidentielle sur les Morts Maternelles, 2013-2015. In: Les morts maternelles en France: mieux comprendre pour mieux prévenir . Santé publique France, Saint-Maurice. Available at: www.santepubliqueFrance.fr . 237 p.
81. Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ . (2021) 374:n2061. doi: 10.1136/bmj.n2061
82. Wadephul F, Jarrett PM, Jomeen J, Martin CR. A mixed methods review to develop and confirm a framework for assessing midwifery practice in perinatal mental health. J Adv Nurs . (2018) 74:2258–72. doi: 10.1111/jan.13786
83. Williams P. Mothers’ descriptions of recovery from postpartum depression. MCN Am J Matern Child Nurs . (2013) 38:276–81. doi: 10.1097/NMC.0b013e3182993fbf
84. Slade M, Bird V, Clarke E, Le Boutillier C, McCrone P, Macpherson R, et al. Supporting recovery in patients with psychosis through care by community-based adult mental health teams (REFOCUS): a multisite, cluster, randomised, controlled trial. Lancet Psychiatry . (2015) 2:503–14. doi: 10.1016/S2215-0366(15)00086-3
85. Law S, Ormel I, Babinski S, Plett D, Dionne E, Schwartz H, et al. Dread and solace: Talking about perinatal mental health. Int J Ment Health Nurs . (2021) 30 Suppl 1:1376–85. doi: 10.1111/inm.12884
86. Powell C, Bedi S, Nath S, Potts L, Trevillion K, Howard L. Mothers’ experiences of acute perinatal mental health services in England and Wales: a qualitative analysis. J Reprod Infant Psychol . (2022) 40:155–67. doi: 10.1080/02646838.2020.1814225
87. Kirkpatrick DL, Kirkpatrick JD. Evaluating training programs: the four levels . 3rd ed. San Francisco, CA: Berrett-Koehler Publishers, Inc (2006).
88. Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry . (2002) 1:16–20.
PubMed Abstract | Google Scholar
89. Kohrt BA, Jordans MJD, Turner EL, Rai S, Gurung D, Dhakal M, et al. Collaboration with people with lived experience of mental illness to reduce stigma and improve primary care services: A pilot cluster randomized clinical trial. JAMA Netw Open . (2021) 4:e2131475. doi: 10.1001/jamanetworkopen.2021.31475
90. Davies L, Page N, Glover H, Sudbury H. Developing a perinatal mental health module: An integrated care approach. Br J Midwifery . (2016) 24:118–21. doi: 10.12968/bjom.2016.24.2.118
91. Verbiest S, Tully K, Simpson M, Stuebe A. Elevating mothers’ voices: recommendations for improved patient-centered postpartum. J Behav Med . (2018) 41:577–90. doi: 10.1007/s10865-018-9961-4
92. Hooks C. Attitudes toward substance misusing pregnant women following a specialist education programme: An exploratory case study. Midwifery . (2019) 76:45–53. doi: 10.1016/j.midw.2019.05.011
Keywords: midwifery, perinatal care, mental health services, education, attitude of health personnel, literature review
Citation: Dubreucq M, Dupont C, Lambregtse-Van den Berg MP, Bramer WM, Massoubre C and Dubreucq J (2024) A systematic review of midwives’ training needs in perinatal mental health and related interventions. Front. Psychiatry 15:1345738. doi: 10.3389/fpsyt.2024.1345738
Received: 28 November 2023; Accepted: 02 April 2024; Published: 22 April 2024.
Reviewed by:
Copyright © 2024 Dubreucq, Dupont, Lambregtse-Van den Berg, Bramer, Massoubre and Dubreucq. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marine Dubreucq, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
A community health needs assessment is not a one-off activity but a developmental process that is added to and amended over time. It is not an end in itself but a way of using information to plan health care and public health programmes in the future. The steps of community health needs assessment are as follows.
Community health needs assessment (CHNA) is a process for determining the needs in a particular community or population through systematic, comprehensive data collection and analysis, and leveraging results to spur community change. CHNA has long been best practice within the field of public health and prompts those working to improve community ...
The five steps of health needs assessment. Step 1 - Getting started. Step 2 - Identifying health priorities. Step 3 - Assessing a health priority for action. Step 4 - Action planning for change. Step 5 - Moving on/project review. 4. HNA skills required and tools available. 5.
Community needs assessment surveys can help identify and address these health inequalities. A community needs assessment offers comprehensive information about the health needs, critical issues, and resources of a specific community. During the assessment process, researchers engage with communities to best address their most pressing priorities.
A community needs assessment should focus on: a selected community as defined by the team, such as a region or neighborhood. sectors within that area, such as health care and work sites. community components to assess within each sector, such as nutrition, chronic disease management and tobacco use.
Community health needs and assets assessment is a means of identifying and describing community health needs and resources, serving as a mechanism to gain the necessary information to make informed choices about community health. The current review of the literature was performed in order to shed more light on concepts, rationale, tools and ...
A community health assessment (sometimes called a CHA), also known as community health needs assessment (sometimes called a CHNA), refers to a state, tribal, local, or territorial health assessment that identifies key health needs and issues through systematic, comprehensive data collection and analysis. Community health assessments use such ...
In this view, assessment of need must include an assessment of the effectiveness of interventions to meet identified health needs ( Mooney 1992; Pencheon et al. 2001 ). The assumption is that the relative total need can be measured sufficiently by just a few factors such as standardized mortality or morbidity rates.
This chapter begins with a consideration of the technical processes used for conducting health needs assessment. The relationship between health needs assessment and health economics is then examined and the philosophy of utilitarianism and its influence on health economics is explored. Cost utility analysis and its links to studies of quality ...
Abstract. Health needs assessment (HNA) is one of the approaches used to provide intelligence and inform decision-making on the planning and deploying of resources to address the health priorities of local populations. Need is an important concept in public health but is also a multifaceted one that represents different things to different people.
"Health needs assessment" is a process of determining the health and health care needs of any given population or sub-group in an area. It is a complex task requiring epidemiological expertise, the ability to work across organizational boundaries as well as an understanding of, and an ability to engage with all appropriate population groups
Health needs assessment is a way for health visitors and school nurses to gain a more in depth understanding of their communities and the needs that exist, enabling effective planning ...
Needs Assessment and Evaluation. Needs assessments and evaluations are key parts of public health methods. Needs assessments aim to understand the health needs and achievements of a community. Evaluation is used to understand how well interventions or program work across the entire span of the project. Aiken, J.A., & Griner, S.B. (2021).
Health needs assessment is the systematic approach to ensuring that the health service uses its resources to improve the health of the population in the most efficient way. It involves epidemiological, qualitative, and comparative methods to describe health problems of a population; identify inequalities in health and access to services; and ...
Example 2: IRC Salt Lake City Purpose: HNA used by IRC Salt Lake City for determining community needs around Afghan women's health.; Assessment Type: Survey with facilitator scripts and notes; Implementation: This sample includes a call script to introduce the HNA and recruit participants, notes to help guide facilitators in each section of the HNA, and different questions around women's ...
Every 3 years, Kaiser Permanente conducts Community Health Needs Assessments, which guide and inform Kaiser Permanente's investments and business decisions. They are a critical tool for identifying and measuring community needs and assets, which lets us better tailor our engagement with communities and use our organizational resources to ...
A health needs assessment is a method used by nongovernment organizations in order to check, review, assess, analyze and evaluate a community's health needs, the public's health needs, or even a specific family's health needs. This assessment consists of a series of questions in the form of a checklist. The assessment is given to the ...
Community Health Needs Assessment - Prisma Health HSA305 - Week 4 Assignment Professor Cole 04/25/ Teresa M. Howe. The data from the C.H.N for Prisma Health in South Carolina identifies several main health concerns in this area.
interRAI assessment process. interRAI is a suite of clinical assessment instruments used to assess an older person's care needs both in the community and residential care. Needs Assessment Service Coordination agencies (NASCs) operate the needs assessment and service coordination process on behalf of Te Whatu Ora.
Rapid urbanisation exacerbates health and wellbeing disparities in vulnerable contexts and underscores the imperative need to develop innovative and participatory co-creation approaches to understand and address the specificities of these contexts. This paper presents a method to develop an assessment framework that integrates top-down dimensions with bottom-up perspectives to monitor the ...
The Adult Needs and Strengths Assessment is a multipurpose tool developed for adult behavioral health services. It is intended to prevent duplicate assessments by multiple parties, decrease unnecessary psychological testing, aid in identifying placement and treatment needs, and inform case planning decisions. Its assessments help support decision making, including level of care and service ...
National Institute on Minority Health and Health Disparities National Heart, Lung, and Blood Institute ... SAM registration includes the assignment of a Commercial and Government Entity (CAGE) Code for domestic organizations which have not already been assigned a CAGE Code. ... A. Institutional Needs-Assessment for research capacity section ...
It suggests a hybrid approach to the needs assessment process where systems and their individual hospitals work together to maximize health benefits to the communities served. Keywords: social determinants of health, physical determinants of health, community health needs assessment, non-profit hospitals, public health, affordable care act. Go to:
The values, lifestyle and needs of the residents of Moscow are driven by the city's unique economic, financial, transport and social position. ... of health services, ensure that the supply of these services is aligned with the incidence of diseases and people's needs, and keep abreast with cutting-edge achievements in medical science. ...
The Needs Assessment Report helps companies strategize for the project's next steps. It analyzes the current state of your Phase I project and identifies strengths and weaknesses across four categories. The information in each report will be tailored to the participating company's project, but the structure and scope of the report are fixed.
Community health needs and assets assessment is a means of identifying and describing community health needs and resources, serving as a mechanism to gain the necessary information to make informed choices about community health. The current review of the literature was performed in order to shed more light on concepts, rationale, tools and uses of community health needs and assets assessment.
France is more likely to protect people from financial hardship caused by out-of-pocket payments for health care than most other countries in the European Union (EU), but gaps in coverage remain a challenge for households with low incomes, a new WHO/Europe report reveals.According to the report, "Can people afford to pay for health care? New evidence on financial protection in France", the ...
Three systematic reviews considered midwives' educational needs in perinatal mental health (PMH) or related interventions with a focus on depression or anxiety. This systematic review aims to review: 1) midwives' educational/training needs in PMH; 2) the training programs in PMH and their effectiveness in improving PMHC. ...
The COVID-19 pandemic and related lockdowns around the world led to a general decline in physical and mental health because of isolation, lack of social interaction, restriction of movement and travel, and dramatic lifestyle changes [].The COVID-19 pandemic also demonstrated the importance of having access to green and blue spaces for human health and well-being during pandemics [2,3,4].
Walking tour around Moscow-City.Thanks for watching!MY GEAR THAT I USEMinimalist Handheld SetupiPhone 11 128GB https://amzn.to/3zfqbboMic for Street https://...