- UNC Chapel Hill

History and Physical Examination (H&P) Examples
The links below are to actual H&Ps written by UNC students during their inpatient clerkship rotations. The students have granted permission to have these H&Ps posted on the website as examples.
H&P 1 “77 yo woman – swelling of tongue and difficulty breathing and swallowing”
H&P 2 “47 yo woman – abdominal pain”
H&P 3 “56 yo man – shortness of breath”
H&P 4 “82 yo man – new onset of fever, HTN, rigidity and altered mental status”
H&P 5 “76 yo man – chest pain”
H&P 6 “24 yo man – bilateral knee pain”
H&P 7 “51 yo man – dyspnea on exertion”
H&P 8 “47 yo woman – chest pain, SOB “
H&P 9 “61 yo man – increased weakness and slurred speech”
Essay Writing Service
Have a native essay writer do your task from scratch for a student-friendly price of just per page. Free edits and originality reports.
You are free to order a full plagiarism PDF report while placing the order or afterwards by contacting our Customer Support Team.
Who are your essay writers?

SCOTT T. LARSON, MD, AND JASON WILBUR, MD
Am Fam Physician. 2020;101(2):95-108
Related letter : Differential Diagnosis of Muscle Weakness in Adults
Author disclosure: No relevant financial affiliations.
Although the prevalence of muscle weakness in the general population is uncertain, it occurs in about 5% of U.S. adults 60 years and older. Determining the cause of muscle weakness can be challenging. True muscle weakness must first be differentiated from subjective fatigue or pain-related motor impairment with normal motor strength. Muscle weakness should then be graded objectively using a formal tool such as the Medical Research Council Manual Muscle Testing scale. The differential diagnosis of true muscle weakness is extensive, including neurologic, rheumatologic, endocrine, genetic, medication- or toxin-related, and infectious etiologies. A stepwise approach to narrowing this differential diagnosis relies on the history and physical examination combined with knowledge of the potential etiologies. Frailty and sarcopenia are clinical syndromes occurring in older people that can present with generalized weakness. Asymmetric weakness is more common in neurologic conditions, whereas pain is more common in neuropathies or radiculopathies. Identifying abnormal findings, such as Chvostek sign, Babinski reflex, hoarse voice, and muscle atrophy, will narrow the possible diagnoses. Laboratory testing, including electrolyte, thyroid-stimulating hormone, and creatine kinase measurements, may also be helpful. Magnetic resonance imaging is indicated if there is concern for acute neurologic conditions, such as stroke or cauda equina syndrome, and may also guide muscle biopsy. Electromyography is indicated when certain diagnoses are being considered, such as amyotrophic lateral sclerosis, myasthenia gravis, neuropathy, and radiculopathy, and may also guide biopsy. If the etiology remains unclear, specialist consultation or muscle biopsy may be necessary to reach a diagnosis.
Given its broad differential diagnosis, muscle weakness can be challenging to evaluate in primary care practice. Although its prevalence in the general population is not well described, muscle weakness occurs in 5% of U.S. adults 60 years and older. 1 Physicians must distinguish true muscle weakness from subjective fatigue or pain-related motor impairment with normal motor strength. This requires a history and physical examination, which guide laboratory testing, imaging, electrodiagnostic testing, and muscle biopsy. 2 – 5
Etiology and Differential Diagnosis
The differential diagnosis of muscle weakness in adults is extensive because it can occur when pathology affects any level of the neuromuscular pathway (upper or lower motor neurons, neuromuscular junction, and muscle fibers). Table 1 lists selected causes of muscle weakness and their clinical findings. 5 – 22
Upper motor neurons, which are located in the cerebral cortex, brainstem, and corticospinal tracts, may be injured from stroke, multiple sclerosis, and spinal cord or brain masses. Lower motor neurons, which are located in the anterior horn of the spinal cord, nerve roots, and peripheral nerves, may be damaged by infections, Guillain-Barré syndrome, hereditary sensorimotor disorders (e.g., Charcot-Marie-Tooth disease), compressive neuropathy (e.g., carpal tunnel syndrome), radiculopathy from intervertebral disk herniation, inflammation, spinal muscular atrophy type IV, or amyloid infiltration. 2 , 23 – 25
Upper and lower motor neurons are involved in amyotrophic lateral sclerosis. 24 The neuromuscular junction is the site of pathology in myasthenia gravis and Lambert-Eaton syndrome, which are rare autoimmune-mediated disorders. 7 , 8
Weakness is the predominant feature of primary muscle disorders, or myositides. Some of these disorders, such as dermatomyositis, polymyositis, and necrotizing myositis, present with acute or subacute proximal weakness and may be associated with malignancy or connective tissue disorders. Conversely, inclusion body myositis, which tends to occur in older adults, has a gradual course, affecting distal muscles early and progressing in an asymmetric pattern. 9 , 10 , 26 , 27
Some endocrine disorders can cause weakness. These include hyperthyroidism and hypothyroidism, adrenal insufficiency (Addison disease), endogenous glucocorticoid excess (Cushing syndrome), acromegaly, and primary hyperaldosteronism (Conn syndrome). 3 Diabetic neuropathy may affect motor neurons, including the oculomotor nerve. 28
ELECTROLYTE DISTURBANCES
Numerous electrolyte imbalances are linked to muscle weakness, including disturbances in calcium, phosphate, potassium, and sodium. Hypokalemia is particularly common and can be caused by medications, such as diuretics; Gitelman syndrome (hypokalemic periodic paralysis); renal tubular acidosis; primary hyperaldosteronism; thyrotoxicosis; or infections, such as dengue fever. 3 , 4 , 29 – 31
Muscular dystrophy usually presents during childhood or adolescence, but certain subtypes (e.g., Becker muscular dystrophy, myotonic dystrophy) can present during adulthood. 11 Disorders of lipid and glycogen metabolism and disorders of mitochondria can also cause weakness, myopathy, and rhabdomyolysis; these disorders may be exacerbated by exercise or febrile illnesses and rarely present in adults. 32 , 33
MEDICATIONS
Numerous medications have been reported to cause muscle weakness ( Table 2 4 , 12 – 14 , 34 ) , including several commonly used medications. For example, statins are well known to cause myopathy and rhabdomyolysis, although the mechanism is unclear. 12 , 13 Fluoroquinolones are linked to tendinopathies, rhabdomyolysis, and tendon ruptures. 12 Glucocorticoids can cause a noninflammatory myopathy, primarily affecting postural muscles. 12 , 14 A medication review is thus essential in the evaluation of muscle weakness. 4 , 12 , 35
Exposure to heavy metals, such as arsenic, lead, thallium, and mercury, can cause motor neuropathy; therefore, a toxin review should be completed in patients with muscle weakness . 4 , 35 Organophosphate poisoning causes weakness at the level of the neuromuscular junction, with severe cholinergic effects (toxidrome). Alcohol and certain recreational drugs (e.g., “glue sniffing,” cocaine, amphetamines, opioids) can also cause muscle weakness. Alcohol is neurotoxic and myotoxic at high doses and can cause acute muscle weakness in individuals who binge drink. 15
Envenomation, including from tick bites (tick paralysis) and certain venomous snake bites, may cause weakness. Exposure to Clostridium botulinum toxin from eating contaminated or undercooked food causes acute paralysis by blocking release of acetylcholine into the neuromuscular junction. 4 , 11 , 35
Certain infections are linked to muscle weakness. These include West Nile virus infection, HIV infection, Lyme disease, diphtheria, dengue fever, neurocysticercosis, trichinosis, Chagas disease, rabies, botulism, herpes zoster, cytomegalovirus infection, hepatitis C, and herpes simplex virus 1 infection. Lyme disease, herpes zoster, and potentially herpes simplex virus 1 infection can cause facial nerve palsy (Bell palsy). Poliomyelitis was historically a significant cause of flaccid paralysis but now rarely occurs because of worldwide vaccination efforts. 3 , 23 , 24 , 29 , 30 , 36 , 37
SARCOPENIA AND FRAILTY
When evaluating generalized weakness in older adults, sarcopenia and frailty should be considered in the differential diagnosis. Sarcopenia and frailty are common multifactorial syndromes that typically do not occur in younger people. They are associated with increased morbidity, disability, institutionalization, and mortality. Sarcopenia is thought to be catabolic age-related loss of muscle mass and strength and can be evaluated by measuring grip strength, gait speed, and muscle mass. 38 , 39 Frailty, which often coexists with sarcopenia, can be defined as the presence of three or more of the following: grip weakness, slow gait speed, unintentional weight loss, subjective exhaustion, and low physical activity. 40
Physicians should inquire about onset, duration, and progression of symptoms. Acute onset of weakness (hours to days) should prompt timely evaluation, because it may indicate vascular, infectious, inflammatory, metabolic, or toxin-mediated disorders. Subacute presentation (days to weeks) may suggest electrolyte, inflammatory, or rheumatologic disorders. More gradual progressive weakness often suggests neurologic, genetic, or metabolic disorders or inclusion body myositis. 2 , 9 , 11 , 29
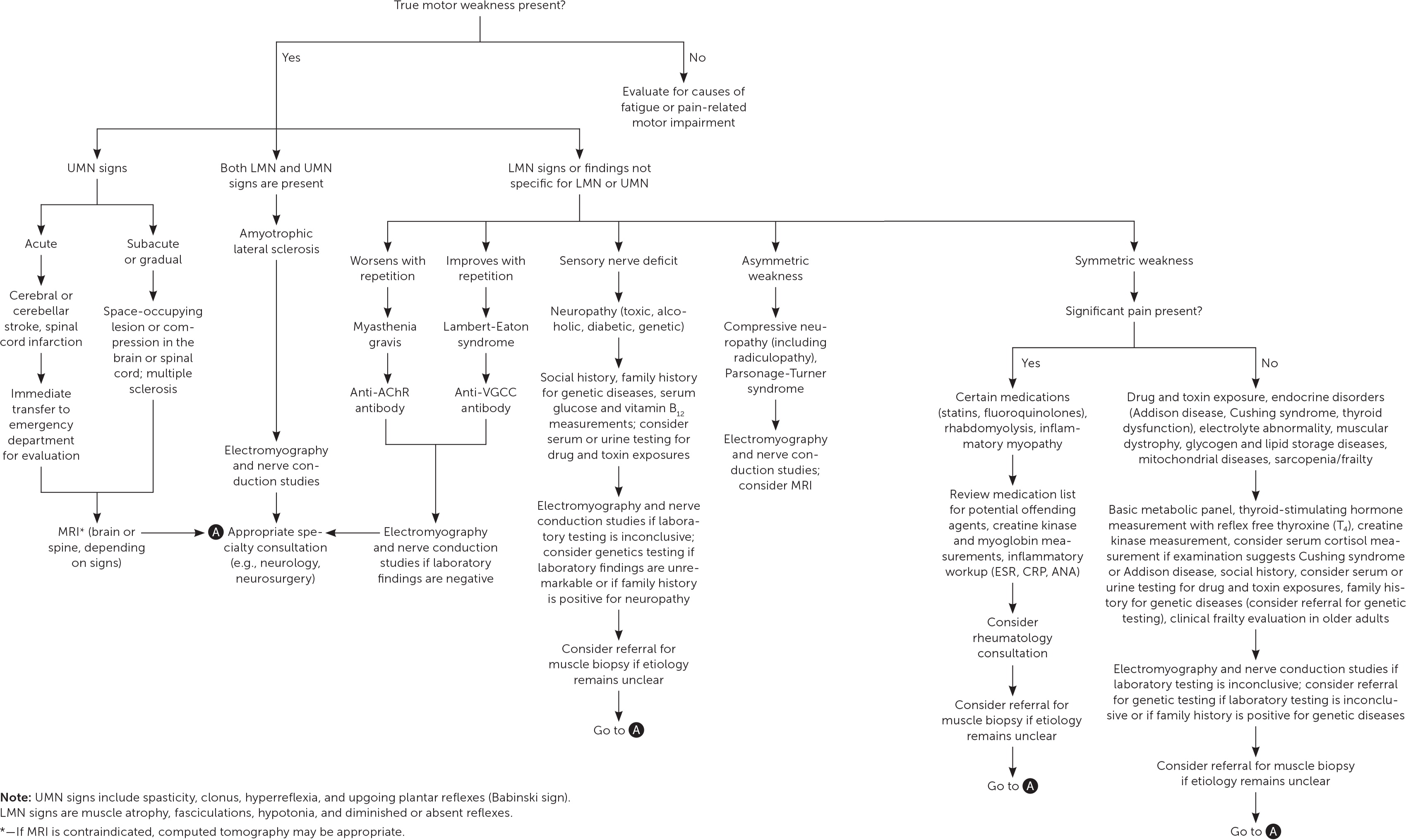
The history should be guided by knowledge of the potential diagnoses and proceed in a stepwise approach ( Figure 1 2 – 5 , 7 – 24 , 26 – 33 , 35 – 38 , 41 – 44 ) . Specific elements of the history may provide diagnostic clues ( Table 3 2 – 4 , 7 – 11 , 13 , 22 – 24 , 26 – 28 , 31 , 35 , 43 , 44 ) .
In particular, identifying the distribution of weakness helps narrow the broad differential diagnosis. Patients with proximal (limb-girdle) weakness may have difficulty rising from a chair, climbing stairs, or lifting their arms overhead to perform activities of daily living (e.g., combing hair). 2 , 26 Proximal weakness is more common in myopathies. Patients with distal weakness may have difficulty opening jars or may drop objects or have foot drop. Distal weakness is more typically caused by certain toxins (e.g., organophosphates), hereditary motor neuropathy, or early inclusion body myositis. 3 , 9 , 16 , 41 Simultaneous proximal and distal weakness may result from inclusion body myositis or Guillain-Barré syndrome.
Asymmetric weakness is typically neurologic and may be due to central nervous system lesions or peripheral nerve inflammation or compression. The physician should also inquire about the presence of oropharyngeal symptoms (e.g., dysphagia, dysarthria), vision loss, or diplopia, which can be indicative of inflammatory myopathy, multiple sclerosis, or myasthenia gravis, respectively. 2 , 9 – 11 , 27
The presence of accompanying sensory symptoms suggests a neuropathic etiology from intrinsic or extrinsic factors. For example, pain in the same distribution as the weakness suggests nerve compression, inflammatory neuropathy or myopathy, or muscle damage due to toxins or medications. History of fevers, arthralgias, rash, or Raynaud phenomenon suggests inflammatory etiologies. Fever also suggests infectious etiologies. All types of inflammatory myopathy can present with pain and muscle tenderness. 3 , 10 , 26
Patients with myasthenia gravis often present with intermittent blurry vision or diplopia and less commonly with more generalized weakness. In addition, symptoms of myasthenia gravis often fluctuate, worsen throughout the day, and may be exacerbated by elevated temperatures. 7
A family history may help identify hereditary causes of muscle weakness. 2 , 11 , 17 A medication review and screening for substance use should always be performed in patients with muscle weakness. 15 , 35
Physical Examination
Physical examination is crucial to diagnosing the cause of muscle weakness. Weakness should be formally graded and documented with a tool such as the Medical Research Council Manual Muscle Testing scale ( Table 4 45 ) .
NEUROLOGIC EXAMINATION
A neurologic examination should be performed in patients with muscle weakness to observe signs of upper motor neuron vs. lower motor neuron pathology. Upper motor neuron findings include spasticity (e.g., spastic gait), hyperreflexia, upgoing-toe plantar reflexes (positive Babinski reflex), dysarthria, clonus, and poor coordination. Lower motor neuron findings include diminished or absent reflexes, hypotonia, muscle atrophy (e.g., hoarse voice from laryngeal muscle atrophy), and fasciculations. Visual inspection of the muscles with attention to bulk, involuntary movements, and symmetry is also important.
Hyperreflexia can occur with upper motor neuron lesions, hyperthyroidism, and hypercalcemia. Hypocalcemia is suggested with tetany, Chvostek sign (tapping the facial nerve anterior to the earlobe and inferior to the zygomatic arch elicits ipsilateral facial nerve spasm), and Trousseau sign (inflation of a brachial blood pressure cuff induces distal carpopedal spasm). Up to 94% of patients with hypocalcemia present with Trousseau sign, although Chvostek sign is neither sensitive nor specific for hypocalcemia. 43 , 44
Cranial nerve examination can reveal facial nerve weakness suggesting Lyme disease, herpes simplex virus 1 infection, or herpes zoster (Ramsay Hunt syndrome). 37 Ptosis or diplopia may suggest myasthenia gravis. Motor strength worsens with repetition in patients with myasthenia gravis, whereas strength and reflexes may transiently improve after repetitive muscle contraction in patients with Lambert-Eaton syndrome. 7 , 8
The distribution of weakness elicited in the history should be confirmed on physical examination with careful attention to proximal vs. distal strength and symmetric vs. asymmetric strength.
EXTRANEUROLOGIC FINDINGS
Extraneurologic findings may help narrow the diagnosis in patients with muscle weakness. As noted earlier, fever suggests inflammatory or infectious myopathy. Cushingoid appearance (buffalo hump, purple striae) suggests endogenous or exogenous glucocorticoid excess. A violaceous rash on the knuckles and extensor surfaces of the upper extremities (Gottron papules; Figure 2 46 ) , a heliotrope rash, the V-sign (violaceous rash on the upper chest and neck), and the shawl sign (violaceous rash on the back) occur with dermatomyositis. Cardiac arrhythmias may occur with inflammatory myopathy, genetic disorders, and electrolyte imbalances. 3 , 9 , 10 , 14 , 26

Numerous screening tools are available to evaluate weakness in older patients if sarcopenia or frailty is suspected. They include the Fried frailty index, FRAIL (fatigue, resistance, ambulation, illnesses, loss of weight) scale, grip strength analysis, and gait speed analysis. 47 Grip strength can be measured objectively with a dynamometer, and gait speed can be measured by timing a patient's usual walking gait to the examination room or by using the Timed Up and Go test. 48 Age-specific normative values for grip strength and gait speed are available. 38 , 39
Laboratory Evaluation
Depending on clinical findings and suspected diagnosis, focused or expansive laboratory testing may be indicated in patients with muscle weakness.
Creatine kinase elevation is nonspecific but can help narrow the differential diagnosis and confirm myopathy. 26 Creatine kinase levels should not be checked immediately after electrodiagnostic testing because they may be transiently elevated. 5 , 18 Myoglobinuria may also indicate myopathy. 3
Because metabolic abnormalities may contribute to weakness, an electrolyte panel should be considered to determine levels of calcium, potassium, sodium, phosphate, and magnesium. Thyroid function testing and cortisol measurement should also be considered.
Serum testing for infectious etiologies, including HIV infection, Lyme disease, West Nile virus infection, and dengue fever, may be indicated if a pathogen is suspected. Lumbar puncture may be indicated if central nervous system infection is suspected.
Anti–acetylcholine receptor antibodies are present in 80% to 90% of patients with generalized myasthenia gravis but in only 50% to 55% of patients with isolated ocular myasthenia gravis. 7 , 11 If clinical suspicion is high despite negative findings on serum anti–acetylcholine receptor antibody testing, the patient should be referred to a neurologist. 4 , 7 , 11
Specific serum molecular genetic testing may be performed if there is concern for genetic disorders, although this testing is typically ordered by a specialist (e.g., neurologist, rheumatologist, geneticist).
Imaging and Electrodiagnostic Testing
Timely neuroimaging is critical in the evaluation of suspected stroke and cauda equina syndrome. If other neurologic diagnoses (e.g., multiple sclerosis, spinal stenosis, stroke) are suspected, appropriate imaging should be performed. Magnetic resonance imaging and ultrasonography of muscle tissue may be used in the diagnosis of inflammatory myopathy. 5
Electromyography should be performed in patients with muscle weakness if the diagnosis is unclear after a history, physical examination, and targeted laboratory evaluation. 5 , 18 , 19 , 26 Electromyography assists in localizing the cause of weakness to the motor neuron, neuromuscular junction, or muscle. 3 Although electromyography complements the neurologic examination, the findings are not pathognomonic for specific diseases. Abnormal findings on electromyography, with or without muscle imaging, may help localize a suitable site for muscle biopsy. 5 , 18 , 19
Muscle Biopsy
Muscle biopsy is considered the definitive test for diagnosing myopathies; however, it is invasive and used sparingly. Muscle biopsy should be considered to clarify the diagnosis in patients who have objective weakness with elevated creatine kinase levels or abnormal findings on electromyography or on muscle magnetic resonance imaging. 20 , 21 Biopsy may also be necessary in cases of suspected inflammatory myopathy if the skin findings of dermatomyositis are absent. 9 , 10
Muscle biopsy is generally performed as an outpatient procedure by a surgical consultant. The ideal biopsy site is a muscle that exhibits mild-to-moderate clinical weakness. Severely weak muscles should be avoided, because biopsy of a muscle in an advanced stage of myopathy often shows signs of fibrosis or fatty infiltration, yielding nondiagnostic results. 5 , 9 Muscle biopsy in older patients with significant sarcopenia is unlikely to be diagnostic. 5 Complications of muscle biopsy are uncommon but include pain, stiffness, bleeding, and infection. 5 , 21
This article updates a previous article on this topic by Saguil . 6
Data Sources: We searched PubMed, the Cochrane database, and Essential Evidence Plus for the terms muscle weakness, muscle weakness evaluation, myopathy, motor neuropathy, muscle biopsy, neurologic weakness, electrodiagnostic testing weakness, myasthenia gravis, Lambert Eaton, inflammatory myopathy, sarcopenia, frailty, Guillain Barré, Parsonage Turner, hypocalcemia, Chvostek, Trousseau calcium, and multiple sclerosis. Search dates: January 12 to June 13, 2019, and September 22, 2019.
Looker AC, Wang CY. Prevalence of reduced muscle strength in older U.S. adults: United States, 2011–2012. January 2015. Accessed February 17, 2019. https://www.cdc.gov/nchs/products/databriefs/db179.htm
Barohn RJ, Amato AA. Pattern-recognition approach to neuropathy and neuronopathy. Neurol Clin. 2013;31(2):343-361.
Chawla J. Stepwise approach to myopathy in systemic disease. Front Neurol. 2011;2:49.
Nayak R. Practical approach to the patient with acute neuromuscular weakness. World J Clin Cases. 2017;5(7):270-279.
Rosow LK, Amato AA. The role of electrodiagnostic testing, imaging, and muscle biopsy in the investigation of muscle disease. Continuum (Minneap Minn). 2016;22(6):1787-1802.
Saguil A. Evaluation of the patient with muscle weakness. Am Fam Physician. 2005;71(7):1327-1336. Accessed August 23, 2019. https://www.aafp.org/afp/2005/0401/p1327.html
Juel VC, Massey JM. Myasthenia gravis. Orphanet J Rare Dis. 2007;2:44.
Hülsbrink R, Hashemolhosseini S. Lambert-Eaton myasthenic syndrome. Clin Neurophysiol. 2014;125(12):2328-2336.
Dalakas MC. Inflammatory muscle diseases. N Engl J Med. 2015;372(18):1734-1747.
Lundberg IE, Miller FW, Tjärnlund A, et al. Diagnosis and classification of idiopathic inflammatory myopathies. J Intern Med. 2016;280(1):39-51.
McDonald CM. Clinical approach to the diagnostic evaluation of hereditary and acquired neuromuscular diseases. Phys Med Rehabil Clin NAm. 2012;23(3):495-563.
Klopstock T. Drug-induced myopathies. Curr Opin Neurol. 2008;21(5):590-595.
Thompson PD, Panza G, Zaleski A, et al. Statin-associated side effects. J Am Coll Cardiol. 2016;67(20):2395-2410.
Minetto MA, D’Angelo V, Arvat E, et al. Diagnostic work-up in steroid myopathy. Endocrine. 2018;60(2):219-223.
Simon L, Jolley SE, Molina PE. Alcoholic myopathy: pathophysiologic mechanisms and clinical implications. Alcohol Res. 2017;38(2):207-217.
Andersen H. Motor neuropathy. Handb Clin Neurol. 2014;126:81-95.
Iyadurai SJ, Kissel JT. The Limb-Girdle muscular dystrophies and the dystrophinopathies. Continuum (Minneap Minn). 2016;22(6, Muscle and Neuromuscular Junction Disorders):1954-1977.
Lacomis D. Electrodiagnostic approach to the patient with suspected myopathy. Neurol Clin. 2012;30(2):641-660.
Valls-Solé J. The utility of electrodiagnostic tests for the assessment of medically unexplained weakness and sensory deficit. Clin Neurophysiol Pract. 2016;1:2-8.
Wilson D, Breen L, Lord JM, et al. The challenges of muscle biopsy in a community based geriatric population. BMC Res Notes. 2018;11(1)-830.
Joyce NC, Oskarsson B, Jin LW. Muscle biopsy evaluation in neuromuscular disorders. Phys Med Rehabil Clin N Am. 2012;23(3):609-631.
Reich DS, Lucchinetti CF, Calabresi PA. Multiple sclerosis. N Engl J Med. 2018;378(2):169-180.
Garg N, Park SB, Vucic S, et al. Differentiating lower motor neuron syndromes. J Neurol Neurosurg Psychiatry. 2017;88(6):474-483.
Tiryaki E, Horak HA. ALS and other motor neuron diseases. Continuum (Minneap Minn). 2014;20(5, Peripheral Nervous System Disorders):1185-1207.
Shin SC, Robinson-Papp J. Amyloid neuropathies. Mt Sinai J Med. 2012;79(6):733-748.
Schmidt J. Current classification and management of inflammatory myopathies. J Neuromuscul Dis. 2018;5(2):109-129.
Schmidt K, Schmidt J. Inclusion body myositis: advancements in diagnosis, pathomechanisms, and treatment. Curr Opin Rheumatol. 2017;29(6):632-638.
Callaghan BC, Cheng HT, Stables CL, et al. Diabetic neuropathy. Lancet Neurol. 2012;11(6):521-534.
Kumar Singh A, Kumar Maurya P, Kulshreshtha D, et al. Analysis of clinical and metabolic profile of acute neuromuscular weakness related to hypokalemia. Acta Neurol Taiwan. 2017;26(3):97-105.
Lana-Peixoto MA, Pedrosa D, Talim N, et al. Myelitis and cauda equina involvement following dengue fever. Mult Scler Relat Disord. 2018;20:48-50.
Diringer M. Neurologic manifestations of major electrolyte abnormalities. Handb Clin Neurol. 2017;141:705-713.
Pennisi EM, Garibaldi M, Antonini G. Lipid myopathies. J Clin Med. 2018;7(12):E472.
Frezza E, Terracciano C, Giacanelli M, et al. Late-onset Pompe disease with nemaline bodies. Case Rep Neurol Med. 2018:4127213.
Zhou SF, Xue CC, Yu XQ, et al. Clinically important drug interactions potentially involving mechanism-based inhibition of cytochrome P450 3A4 and the role of therapeutic drug monitoring. Ther Drug Monit. 2007;29(6):687-710.
Mammen AL. Toxic myopathies. Continuum (Minneap Minn). 2013;19(6 Muscle Disease):1634-1649.
Gabbai AA, Castelo A, Oliveira AS. HIV peripheral neuropathy. Handb Clin Neurol. 2013;115:515-529.
Hehir MK, Logigian EL. Infectious neuropathies. Continuum (Minneap Minn). 2014;20(5, Peripheral Nervous System Disorders):1274-1292.
Dodds R, Sayer AA. Sarcopenia and frailty: new challenges for clinical practice. Clin Med (Lond). 2015;15(suppl 6):s88-s91.
Liguori I, Russo G, Aran L, et al. Sarcopenia. Clin Interv Aging. 2018;13:913-927.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146-M156.
Dimachkie MM, Barohn RJ. Distal myopathies. Neurol Clin. 2014;32(3):817-842.
Feinberg JH, Radecki J. Parsonage-Turner syndrome. HSS J. 2010;6(2):199-205.
Cooper MS, Gittoes NJ. Diagnosis and management of hypocalcaemia [published correction appears in BMJ . 2008;336(7659):10.1136/bmj.a334]. BMJ. 2008;336(7656):1298-1302.
Hujoel IA. The association between serum calcium levels and Chvostek sign: a population-based study. Neurol Clin Pract. 2016;6(4):321-328.
Naqvi U, Sherman AI. Muscle strength grading. StatPearls. Accessed February 17, 2019. https://www.ncbi.nlm.nih.gov/books/NBK430685/
Kim HS, Kim SM, Lee JD. Erythematous papules on dorsum of both hands. Am Fam Physician. 2017;95(12):803-804. Accessed August 26, 2019. https://www.aafp.org/afp/2017/0615/p803.html
Cesari M, Calvani R, Marzetti E. Frailty in older persons. Clin Geriatr Med. 2017;33(3):293-303.
Savva GM, Donoghue OA, Horgan F, et al. Using Timed Up-and-Go to identify frail members of the older population. J Gerontol A Biol Sci Med Sci. 2013;68(4):441-446.
Continue Reading
More in AFP
More in pubmed.
Copyright © 2020 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Curr Rev Musculoskelet Med
- v.14(6); 2021 Dec


Physical Examination and Patellofemoral Pain Syndrome: an Updated Review
Donald kasitinon.
1 Department of Orthopaedic Surgery, Stanford University School of Medicine, Stanford, CA USA
2 Department of Physical Medicine and Rehabilitation, University of Texas Southwestern Medical Center, Dallas, TX USA
Wei-Xian Li
Eric xue song wang, michael fredericson, purpose of review.
Patellofemoral pain syndrome (PFPS) accounts for 25 to 40% of all knee disorders. Diagnosis of PFPS is primarily based on history and physical examination, but the findings on physical examination are often subtle and do not consistently correlate with symptoms described. Yoon and Fredericson published a review article in 2006 detailing the physical examination maneuvers most frequently used to assist clinicians in the accurate diagnosis and treatment of PFPS, and our aim in this review is to provide an update on this previous article focusing on the literature published over the past 15 years regarding the topic.
Recent Findings
Since publication of Fredericson’s original review article, there have been studies building on the literature specifically surrounding Q angle, patellar tilt, crepitus, strength and functional testing, and physical examination maneuver clustering. Additionally, multiple studies have been conducted on the use of musculoskeletal ultrasound (US) as a diagnostic tool for PFPS.
Recent literature has further supported Q angle (when measured utilizing a standardized protocol), crepitus, weakness of hip abductors and extensors, and weakness detected in functional testing as predictors of PFPS while finding inconsistent evidence behind lateral patellar tilt as a predictor of PFPS. The reliability of most physical examination tests alone remain low, but clustering physical examination findings may provide better sensitivities and specificities in diagnosing PFPS. Musculoskeletal US is rapidly gaining popularity, and decreased vastus medialis obliquus (VMO) volume, asymmetry in gluteus medius thickness, intra-articular effusions, and quadriceps and patellar tendon thicknesses have shown value in diagnosing those with PFPS. Additionally, US has the advantage of providing dynamic examination as well as evaluation of the patellofemoral joint in newborns and infants as a predictor of future patellofemoral instability. Further studies are needed to establish the gold standard for diagnosing PFPS and what US findings are truly predictive of PFPS.
Introduction
Patellofemoral pain syndrome (PFPS) is a common condition that accounts for 25 to 40% of all knee disorders [ 1 ••, 2 – 4 ]. The condition is multifactorial in origin and includes conditions previously referred to as chondromalacia patella and runner’s knee [ 1 ••]. PFPS is defined as pain around or behind the patella aggravated by activities that load or compress the patellofemoral joint such as squatting, ascending and descending stairs, jumping, and running [ 2 , 5 – 7 ]. Up to 78% of PFPS patients report chronic pain 5–20 years after rehabilitation [ 8 – 10 ], and a study of patellofemoral osteoarthritis (PFOA) patients waiting to undergo an arthroplasty showed that 22% of them described preceding PFPS in their adolescence and early adult years [ 11 ]. Emerging evidence has suggested that these two conditions are on a continuum [ 12 ] and that underlying biomechanical factors that may predispose to PFPS may also predispose to PFOA, such as weak hip abductors [ 13 ] and patella shape [ 14 ]. It is important to note here that biomechanical studies, including these two, are often cross-sectional so inherently can suggest association but cannot prove causation. Large cohort prospective studies would be required to prove causation. Either way, an accurate diagnosis of PFPS is imperative to begin appropriate management early in order to prevent lingering issues [ 1 ••].
Diagnosis of PFPS is primarily based on history and physical examination because although imaging can show signs of patellar maltracking and/or patellofemoral chondrosis suggestive of PFPS, these findings are often non-specific, and there are patients with completely unremarkable imaging who still have pain [ 1 ••]. Unfortunately, the findings on physical examination for the condition are often subtle and do not consistently correlate with symptoms described [ 15 ], and clinical studies have not always demonstrated biomechanical differences between patients with PFPS and healthy individuals [ 16 – 18 ]. However, a systematic physical examination can still call attention to factors that contribute to patellofemoral malalignment and thus be used to guide treatment [ 19 ].
Yoon and Fredericson published a review article in 2006 detailing the physical examination maneuvers most frequently used to assist clinicians in the accurate diagnosis and treatment of PFPS [ 19 ]. Our aim in this review is to provide an update on this previous article focusing on the literature published over the past 15 years regarding the topic. Since publication of Fredericson’s original review article, there have been studies building on the literature specifically surrounding Q angle, patellar tilt, crepitus, strength and functional testing, and physical examination maneuver clustering. Additionally, musculoskeletal ultrasound (US) has become increasingly prevalent and available for clinicians and is considered an extension of the physical examination. We have thus included studies highlighting the utilization of US as a diagnostic tool for PFPS. This updated review will further assist clinicians in the accurate diagnosis and treatment of this common, yet difficult to accurately diagnose, disorder.
An extensive literature search was performed via MEDLINE based on the following keywords: patellofemoral pain syndrome, anterior knee pain, extensor mechanism disorder, lateral patellar compression, physical exam, muscle strength, Q angle, patellar tilt, patellar tracking, crepitus, and ligamentous laxity. The search included journal articles published between 2005 and 2021. A total of 368 articles resulted, and all their abstracts were reviewed. Emphasis was placed on those evaluating the description and reliability of physical exam maneuvers assessing anterior knee pain and patellofemoral pain syndrome. Articles that met these criteria were pulled from the Stanford Lane Online Library in their entirety and evaluated.
Updates on Physical Examination Findings and Maneuvers
Please refer to Table Table1 1 for a summary of recent findings on the topics as discussed below.
Update on studies for patellofemoral pain syndrome (PFPS) tests
CI confidence interval, US ultrasound, VMO vastus medialis obliquus, ROC receiver operating characteristic, ES effect size
The Q angle was first defined by Brattstrom [ 29 ] and is a measure of the patellar tendency to move laterally when the quadriceps muscle is contracted. The greater the angle, the greater this tendency that may predispose a patient to PFPS [ 19 ]. The Q angle is formed by the line connecting the anterosuperior iliac spine (ASIS) to the center of the patella and the line connecting the center of the patella to the middle of the anterior tibial tuberosity. Aglietti et al. previously cited normal values of 14° ± 3° for men and 17° ± 3° for women [ 30 ]. Grelsamer et al. found similar mean values of 13.3° for men and 15.7° for women. Interestingly, they also found that men and women of equal height demonstrated similar Q angles (with taller people having slightly smaller Q angles) so concluded that the slight difference in Q angles between men and women is more likely explained by the fact that men tend to be taller than women rather that the unproven explanation that women have a wider pelvis than men [ 20 ]. Either way, Q angle values in the past have been found to be highly variable which can be attributed to the lack of standardization when measuring the Q angle (e.g., standing versus sitting and quadriceps muscle activated versus quadriceps muscle relaxed) as well as examiner variance [ 30 , 31 ]. This variability may explain the unclear relationship between a higher Q angle and PFPS as some studies have showed a clear relationship between a higher Q angle and PFPS [ 30 ], while others have failed to demonstrate a difference between patients with PFPS and healthy individuals [ 18 , 19 , 32 ].
The value of measuring the Q angle has been brought into question due to these inconsistent results [ 33 ] and has led to the development of the tibial tubercle to trochlear groove (TT-TG) distance which utilizes magnetic resonance imaging (MRI) rather than the physical examination to assess tubercle lateralization. However, lateralization of the tibial tubercle is still known to play a role in normal functioning of the patellofemoral joint, and the Q angle remains the only method to assess lateralization of the tibial tubercle without resorting to expensive, and perhaps unnecessary, imaging studies [ 34 ••]. Smith et al. [ 21 ] thus recommended establishing a “standardized clinical Q angle protocol.”
In order to do this, Merchant et al. [ 34 ••] utilized a practical, standard protocol for measuring the Q angle. Subjects were placed supine, knees extended, and relaxed on the examination table with the patella pointing up (anteriorly). The examiner then marked the center of the tibial tubercle with a small ink dot. Draper et al. [ 35 ] had previously found that measuring with a long-armed goniometer was more accurate than a short-armed one, so Merchant et al. used an eight inch plastic goniometer with an extendable long arm to reach the ASIS. The subject was asked to hold the long arm at his or her ASIS. The examiner then placed the goniometer pivot at the center of the patella and assured that the patella and goniometer pivot were centered over the distal femur at the trochlear entrance with one hand. Using the other hand, the Q angle was measured with the short arm of the goniometer. With this protocol for the “standard Q angle,” the mean Q angle was 14.8° with a 95% confidence interval (CI) of ±5.4° for all subjects. For men, the mean was 13.5° with a 95% CI of ±5.2°, and for women, the mean was 15.9° with a 95% CI of ±4.8°. There was no significant difference between right and left knees of males or females, and the 2.4° difference between male and female means was found to be due to the average height difference between the two groups. Merchant et al. were thus able to provide a standardized Q angle measurement protocol to assess tibial tubercle lateralization without resorting to expensive imaging studies and provide a reliable reference for clinical comparison [ 34 ••].
Patellar Tilt
Excessive lateral tilt of the patella can lead to decreased medial patellar mobility and abnormally high forces between the lateral facet of the patella and the lateral trochlea of the femur [ 22 ]. The method of performing the patellar tilt test has been described by Grelsamer and McConnell [ 36 ]: the test is performed with the knee extended and the quadriceps relaxed with the patient in supine position. To determine the degree of medial and lateral patellar tilting, you compare the height of the medial patellar border with that of the lateral patellar border. The examiner places his or her thumb and index finger on the medial and lateral border of the patella, and both digits should be of equal height. The patella is laterally tilted if the digit palpating the medial border is more anterior than the digit palpating the lateral border and vice versa [ 19 ].
More recently, Nunes et al. performed a meta-analysis looking at the diagnostic accuracy of physical examination maneuvers to diagnose PFPS and found that two tests, the patellar tilt test and squatting, showed a trend for the diagnosis of PFPS. However, their statistical values did not represent clear evidence regarding diagnostic properties as suggested previously in the literature [ 37 ].
Crepitus is often present as a symptom or sign in patients with PFPS, but there is no close association between crepitus and pain. Previously, Johnson et al. [ 38 ] found that 94% of healthy women and 45% of healthy men studied exhibited patellofemoral crepitus. Oliveira Silva et al. observed that crepitus was more common in women with PFPS (50.7%) compared to healthy controls (33.3%). Women who presented with knee crepitus had four times greater odds to have PFPS compared to healthy controls. However, knee crepitus had no relationship with self-reported clinical outcomes of women with PFPS [ 39 ].
Muscle Strength
Quadriceps muscle weakness is commonly seen in patients with PFPS [ 23 , 24 , 40 ], as is weakness in hip abduction and external rotation [ 41 ]. More recent studies have continued to support this as Nunes et al. studied 32 physically active people (16 with PFPS, 16 controls) and found isometric strength deficits in hip abduction and extension in those with PFPS compared to those without [ 25 ].
In athletes, manual muscle testing does not consistently detect muscle strength deficits. Thus functional testing may be preferred. Previously Loudon et al. [ 26 ••] found that five different functional performance tests (anteromedial lunge, stepdown, single-leg press, bilateral squat, and balance and reach) to have high intra-rater reliability and to correlate with changes in pain scale. Nunes et al. recently tested patients with PFPS and controls with functional tasks and found that PFPS patients were slower climbing stairs, performed 12% fewer chair stands, and forward hopped 20% shorter [ 27 ]. This emphasizes the importance of both strengthening (of the core, hip girdle, and knee musculature) and neuromuscular retraining in the treatment of those with PFPS.
Clustering Physical Examination Findings
Since there is no single diagnostic test for PFPS, Merchant [ 28 ] previously recommended that the diagnosis be based on a cluster of objective findings from physical examination [ 19 ]. Decary et al. attempted to do this formally by looking at 279 patients, 75 of which had a diagnosis of PFPS (26.9%). They identified different diagnostic clusters combining elements from history and physical examination and found two with high specificities (93% and 96%, respectively) for the diagnosis of PFPS. Cluster 1 was age less than 40 years old and either isolated anterior knee pain or medial patellar facet tenderness. Cluster 2 was age 40–58 years old, isolated anterior or diffuse knee pain, mild to moderate difficulty descending stairs, medial patellar facet tenderness, and full passive knee extension. Interestingly, they also found three clusters with high sensitivities to exclude PFPS. Cluster 1 was age less than 58 years old; medial, lateral, or posterior knee pain; and medial or lateral patellar facet tenderness. Cluster 2 was age less than 58 years old, diffuse or lateral knee pain, medial or lateral patellar facet tenderness, and restricted passive knee extension. Cluster 3 was age 58 years old or older [ 1 ••].
Musculoskeletal Ultrasound
Musculoskeletal US has become increasingly prevalent and available in recent years, and there has been a good amount of literature published on its use as a diagnostic tool for PFPS. The use of US has the advantage of avoiding radiation, being non-invasive, and being easily performed in the clinic setting, all while having less of a financial burden than other advanced imaging modalities such as MRI. Many studies have looked at different ways to formally evaluate the patellofemoral joint and its different muscle attachments.
Jan et al. studied differences in sonographic findings of the vastus medialis oblique (VMO) in patients with PFPS and healthy adults. Jan et al. found that the insertion level, fiber angle, and VMO volume were all significantly smaller in the PFPS group than in the control group [ 42 •]. Payne et al. measured gluteus medius muscle thickness at rest and during contraction in patients with PFPS and controls. Muscle activation was calculated as the percentage change between the two. Both of these variables were found not to be significantly different between those with PFPS and healthy controls. Interestingly, PFPS patients did have significantly larger left-right side imbalances in gluteus medius muscle activation than controls. Additionally, among those with PFPS, the magnitude of asymmetry of gluteus medius muscle activation correlated with knee pain scores [ 43 ••]. Nunes et al. also found no difference when comparing gluteus medius muscle thickness (and proportion of non-contractile tissue of the gluteal musculature) measured by US in PFPS patients versus controls [ 25 ]. Thus, asymmetry rather than the actual thickness of the gluteus medius muscle at rest and during contraction is what seems to be the main indicator of symptoms in patients with PFPS. Once again, causation cannot be inferred as these are cross-sectional studies. Siev-Ner et al. studied 67 young female dancers (54% diagnosed with PFPS) and found that patients with PFPS had a significantly higher prevalence of intra-articular effusions [ 44 •]. Kizilkaya et al. measured quadriceps tendon thickness in patients with PFPS and controls and found that quadriceps tendon thickness of ≥0.54 cm had 80% sensitivity and 71% specificity for PFPS. They also measured patellar tendon thickness and found that patellar tendon thickness of ≥ 0.35 cm had 66.7% sensitivity and 67.7% specificity for PFPS diagnosis [ 45 •].
In addition to convenience, US gives the clinician the added benefit of capturing dynamic measurements of the patellofemoral joint during knee movement. However, due to the complex multiplanar movement of the patella, only a few US methods have been studied. Shih et al. developed a method for dynamic tracking of the patella which has been the most studied. In this method, patients are fitted with a modified functional knee brace with a mounted ultrasound probe. The probe was placed perpendicular to the skin at the lateral edge of the superior border of the patella. Patella positioning was then measured by taking the distance between the patella and the lateral condyle of the femur. Using this measurement, the researchers were able to track the position of the patella and degree of movement during the knee’s entire motion arc. They took measurements in several other knee movements such as squatting, stepping, and sitting and found significant differences in lateral tracking [ 46 ••, 47 , 48 ]. They were able to validate their study comparing it to dynamic MRI and found good inter and intra-rater reliability [ 49 , 50 ]. Unfortunately, the accuracy of the system was reduced near full knee extension, which can be problematic as the highest degree of patellar maltracking typically occurs with full knee extension [ 50 ]. Furthermore, if a patient has a patella that laterally displaces further than the femoral condyle, obtaining this measurement becomes extremely difficult.
To address this limitation, a novel but less proven US technique has been proposed by Bailowitz et al. In this method, the distance between the midpoint of the patella and the highest point of the lateral trochlear groove is used as a way to quantify lateral patellar displacement at full extension with quadriceps contraction [ 51 ••]. However, this study is still undergoing validation and has not been tested on symptomatic patients yet.
Another area where US can have a significant impact is in the evaluation of the patellofemoral joint in newborns or infants as a predictor of future patellofemoral instability. Due to lack of complete ossification of bones, radiographs are of limited value in this patient population, and MRIs are often difficult to obtain without high costs and sedation. Similar to how US has aided in the early identification of hip dysplasia, US is starting to be used to assess for patellofemoral dysplasia as well and shows promise as a screening tool for trochlea dysplasia. Both Oye et al. and Kohlhof et al. evaluated different ultrasonographic values and found that measurements including the trochlea sulcus angle, trochlea index, and lateral to medial trochlear facet ratio can all be accurately assessed by ultrasound with good reproducibility and low operator dependency [ 52 , 53 ].
At this time, we do not feel that the use of US for the diagnosis of PFPS has been well-established enough to change standard clinical practice. Current limitations include validation of measuring methods and the ability to prove causation between certain US findings and PFPS. Additionally, musculoskeletal US remains operator dependent. This, however, should improve as more providers are being trained in its use. Once these limitations are addressed, routine US examination in office for patient with potential PFPS may be deemed useful in the future.
Conclusions
We have provided an updated review on Fredericson’s previous article on the most common methods for the clinical diagnosis of PFPS. Recent literature has further supported Q angle (when measured utilizing a standardized protocol), crepitus, weakness of hip abductors and extensors, and weakness detected in functional testing as predictors of PFPS while finding inconsistent evidence behind lateral patellar tilt as a predictor of PFPS. The reliability of most physical examination tests alone remain low and can be variable, but there has been more evidence showing that clustering physical examination findings may provide better sensitivities and specificities in diagnosing PFPS. Musculoskeletal US is rapidly gaining popularity among clinicians and is a major area to build upon in the diagnosis of PFPS. Some studies have shown decreased VMO volume, asymmetry in gluteus medius thickness, intra-articular effusions, and quadriceps and patellar tendon thicknesses to have value in diagnosing those with PFPS. Additionally, US has the advantage of providing dynamic examination of the patellofemoral joint as well as evaluation of the patellofemoral joint in newborns and infants as a predictor of future patellofemoral instability. The clinical diagnosis of PFPS remains difficult even as we develop more reliable methods of measuring anatomical structures and function because of our inability to directly measure pain. Also as noted earlier in the paper, the majority of studies on PFPS are cross-sectional, which inherently can show association but not causation. Further studies, especially those that are longitudinal in design, are needed to establish the gold standard for diagnosing PFPS and what US findings are truly predictive of PFPS.
Declarations
This article does not contain studies with human or animal subjects performed by any of the authors.
Donald Kasitinon, Wei-Xian Li, Eric Xue Song Wang, and Michael Fredericson declare that they have no conflicts of interest.
This article is part of the Topical Collection on Non-Operative Management of Anterior Knee Pain
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Donald Kasitinon, Email: [email protected] .
Wei-Xian Li, Email: ude.drofnats@1ilnaix .
Eric Xue Song Wang, Email: moc.liamg@32gnawxe .
Michael Fredericson, Email: ude.drofnats@2derfm .
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance

We hire a huge amount of professional essay writers to make sure that our essay service can deal with any subject, regardless of complexity. Place your order by filling in the form on our site, or contact our customer support agent requesting someone write my essay, and you'll get a quote.
Finished Papers
Getting an essay writing help in less than 60 seconds
- History Category
- Psychology Category
- Informative Category
- Analysis Category
- Business Category
- Economics Category
- Health Category
- Literature Category
- Review Category
- Sociology Category
- Technology Category

Finished Papers

Customer Reviews

We suggest our customers use the original top-level work we provide as a study aid and not as final papers to be submitted in class. Order your custom work and get straight A's.

Finished Papers
Andre Cardoso

Who will write my essay?
On the website are presented exclusively professionals in their field. If a competent and experienced author worked on the creation of the text, the result is high-quality material with high uniqueness in all respects. When we are looking for a person to work, we pay attention to special parameters:
- work experience. The longer a person works in this area, the better he understands the intricacies of writing a good essay;
- work examples. The team of the company necessarily reviews the texts created by a specific author. According to them, we understand how professionally a person works.
- awareness of a specific topic. It is not necessary to write a text about thrombosis for a person with a medical education, but it is worth finding out how well the performer is versed in a certain area;
- terms of work. So that we immediately understand whether a writer can cover large volumes of orders.
Only after a detailed interview, we take people to the team. Employees will carefully select information, conduct search studies and check each proposal for errors. Clients pass anti-plagiarism quickly and get the best marks in schools and universities.
Customer Reviews
Finished Papers
- Plagiarism report. .99
- High priority status .90
- Full text of sources +15%
- 1-Page summary .99
- Initial draft +20%
- Premium writer +.91

VIDEO
COMMENTS
Examination can be easily performed by lifting lips with mouth closed and by opening the mouth. Examine the teeth for evidence of discoloration, fracture, or excessive tartar formation. Common diseases of oral cavity may cause loss of appetite, difficulty chewing and halitosis. Oropharyngeal examination continued.
Exercise 7.9 Case Study: History and Physical Examination Findings. 8: Preventive Health Programs. Exercise 8.1 Terms and Definitions: Preventative Health Programs ... Exercise 37.7 Case study #1: Helping Clients Through The Grieving Process. Product details. No. of pages: 472. Language: English. Edition: 10.
a normal resting pulse rate in an adult horse is 17 to 27 breaths per min. true. normal horses cannot breath through their mouths. true. most murmurs heard in horses are ejection murmurs and are not signs of valvular abnormalities. false. a horses height is measured in hands, with each hand being 6 inches. true.
MCCURNIN'S EXERCISE 9.9 CASE STUDY #1: WEIGHT LOSS Use McCurnin's pages 335-336 to help you with this assignment. "Suzie," a 5-year-old, spayed, female mixed-breed dog presents to your clinic. The new owners are concerned about her excessive weight gain over a 4-month period. After obtaining a good history, it is learned that there is a toddler in the family and the recent addition of ...
Test results plus findings from the history and physical examination may confirm or refute the main and differential diagnoses, setting up either a management plan or the need for an alternative hypothesis. ... In any case, the stethoscope must ... The classic findings on physical examination of the chest in some common pulmonary disorders are ...
The students have granted permission to have these H&Ps posted on the website as examples. "77 yo woman - swelling of tongue and difficulty breathing and swallowing". "47 yo woman - abdominal pain". "56 yo man - shortness of breath". "82 yo man - new onset of fever, HTN, rigidity and altered mental status". "76 yo man ...
History. The primary clinical manifestation of spinal stenosis is chronic pain. In patients with severe stenosis, weakness and regional anesthesia may result. Among the most serious complications of severe spinal stenosis is central cord syndrome. Central cord syndrome is the most common incomplete cord lesion.
When working with EssayService you can be sure that our professional writers will adhere to your requirements and overcome your expectations. Pay your hard-earned money only for educational writers. Research Paper. 100% Success rate. ID 173. Exercise 7 9 Case Study History And Physical Examination Findings -.
The pain is typically constant and present both at rest and with exercise. 21 Physical exam, ultrasound ... The decision to perform a fasciotomy is based on history, physical exam findings, and/or compartment pressure measurements. ... 7 In-flow lesions are treated first to see if symptoms resolve which is commonly the case. If symptoms persist ...
History and physical examination findings should guide laboratory testing, imaging, electromyography, and muscle biopsy in patients with muscle weakness. 2 - 5 C Usual practice and expert opinion
The History and Physical examination (H&P) is the foundation of the physician-patient interaction. In medical parlance, the H&P refers to a document describing a clinical encounter, as well as the process by which the physician conducts the clinical encounter. Through the H&P process, a physician obtains key objective information from the ...
Physical examination The patient is a slightly obese male who appears in moderate distress. His blood pressure is 145/85 and his heart rate is 85. His cardiac and respiratory examination is within normal limits. His abdomen is soft and non-tender, and he has normal active bowel sounds. Examination of
Purpose of Review. Patellofemoral pain syndrome (PFPS) accounts for 25 to 40% of all knee disorders. Diagnosis of PFPS is primarily based on history and physical examination, but the findings on physical examination are often subtle and do not consistently correlate with symptoms described. Yoon and Fredericson published a review article in ...
History. The first step in the evaluation of hematuria is a detailed review of the history and a thorough physical examination. The presence or absence of hypertension or proteinuria helps to decide how extensively to pursue the diagnostic evaluation. The initial evaluation should be directed toward important and potentially life-threatening ...
The patient species, breed, age, sex, and reproductive status. Stertor. a sign of upper airway disease. Stridor. A harsh, high-pitched respiratory sound usually caused by obstruction of airflow at the pharynx or larynx. Study with Quizlet and memorize flashcards containing terms like Abdominal pinging, Alopecia, Aortic Sentosis and more.
Laboratory tests and physical examination can provide important information about comorbid medical sequelae of BN, but diagnosis requires a thorough diagnostic interview and clinical history. ... Physical findings may include the following: ... Case Study. A 21-year-old woman is brought into an outpatient clinic by her mother, who complains ...
Order. To get the online essay writing service, you have to first provide us with the details regarding your research paper. So visit the order form and tell us a paper type, academic level, subject, topic, number and names of sources, as well as the deadline. Also, don't forget to select additional services designed to improve your online ...
It is not necessary to write a text about thrombosis for a person with a medical education, but it is worth finding out how well the performer is versed in a certain area; terms of work. So that we immediately understand whether a writer can cover large volumes of orders. Only after a detailed interview, we take people to the team.
Exercise 7 9 Case Study History And Physical Examination Findings | Best Writing Service. From a high school essay to university term paper or even a PHD thesis. Flexible discount program. Specifically, buying papers from us you can get 5%, 10%, or 15% discount. Article review, Ethics, 1 page by Robert Sharpe. 695.
Particularly in children, include investigation of suspicion of accidental ingestion (eg, accidental ingestion of rat poison in toddlers). Next: Physical Examination. Epistaxis, or bleeding from the nose, is a common complaint. It is rarely life threatening but may cause significant concern, especially among parents of small children.
REVIEWS HIRE. 1 (888)814-4206 1 (888)499-5521. Research papers can be complex, so best to give our essay writing service a bit more time on this one. Luckily, a longer paper means you get a bigger discount! Hire a Writer. 4.8/5. 4240 Orders prepared.
Susan Devlin. #7 in Global Rating. 1811Orders prepared. ID 4817. Degree: Bachelor's. 928Orders prepared. Essay (Any Type), Geography, 1 page by Gombos Zoran. offers three types of essay writers: the best available writer aka. standard, a top-level writer, and a premium essay expert. Every class, or type, of an essay writer has its own pros ...