COVID-19 and Chronic Disease: The Impact Now and in the Future
ESSAY — Volume 18 — June 17, 2021

Karen A. Hacker, MD, MPH 1 ; Peter A. Briss, MD, MPH 1 ; Lisa Richardson, MD, MPH 1 ; Janet Wright, MD 1 ; Ruth Petersen, MD, MPH 1 ( View author affiliations )
Suggested citation for this article: Hacker KA, Briss PA, Richardson L, Wright J, Petersen R. COVID-19 and Chronic Disease: The Impact Now and in the Future. Prev Chronic Dis 2021;18:210086. DOI: http://dx.doi.org/10.5888/pcd18.210086 external icon .
PEER REVIEWED
The Problem of COVID-19 and Chronic Disease
Raise awareness, collaborate on solutions and build trust, address long-term covid-19 sequelae, how will the national center for chronic disease prevention and health promotion contribute, acknowledgments, author information.
Chronic diseases represent 7 of the top 10 causes of death in the United States (1). Six in 10 Americans live with at least 1 chronic condition, such as heart disease, stroke, cancer, or diabetes (2). Chronic diseases are also the leading causes of disability in the US and the leading drivers of the nation’s $3.8 trillion annual health care costs (2,3).
The COVID-19 pandemic has resulted in enormous personal and societal losses, with more than half a million lives lost (4). COVID-19 is a disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that can result in respiratory distress. In addition to the physical toll, the emotional impact has yet to be fully understood. For those with chronic disease, the impact has been particularly profound (5,6). Heart disease, diabetes, cancer, chronic obstructive pulmonary disease, chronic kidney disease, and obesity are all conditions that increase the risk for severe illness from COVID-19 (7). Other factors, including smoking and pregnancy, also increase the risk (7). Finally, in addition to COVID-19–related deaths since February 1, 2020, an increase in deaths has been observed among people with dementia, circulatory diseases, and diabetes among other causes (8). This increase could reflect undercounting COVID-19 deaths or indirect effects of the virus, such as underutilization of, or stresses on, the health care system (8).
Some populations, including those with low socioeconomic status and those of certain racial and ethnic groups, including African American, Hispanic, and Native American, have a disproportionate burden of chronic disease, SARS-CoV-2 infection, and COVID-19 diagnosis, hospitalization, and mortality (9). These populations are at higher risk because of exposure to suboptimal social determinants of health (SDoH). SDoH are factors that influence health where people live, work, and play, and can create obstacles that contribute to inequities. Education, type of employment, poor or no access to health care, lack of safe and affordable housing, lack of access to healthy food, structural racism, and other conditions all affect a wide range of health outcomes (10–12). The COVID-19 pandemic has exacerbated existing health inequities and laid bare underlying root causes.
The COVID-19 pandemic has had direct and indirect effects on people with chronic disease. In addition to morbidity and mortality, high rates of community spread and various mitigation efforts, including stay-at-home recommendations, have disrupted lives and created social and economic hardships (13). This pandemic has also raised concerns about safely accessing health care (14) and has reduced the ability to prevent or control chronic disease. This essay discusses the impact that these challenges have or could have on people with chronic disease now and in the future. Exploring the impact of COVID-19 should help the public health and health care communities effectively improve health outcomes.
The challenges we face as public health professionals are divided into 3 categories. The first category involves the current effects of COVID-19 on those with, or at risk for, chronic diseases and those at higher risk for severe COVID-19 illness. Inherent in this category is the need for balance between protecting people with chronic diseases from COVID-19 while assuring they can engage in disease prevention, manage their conditions effectively, and safely receive needed health care.
The second category is the postpandemic impact of COVID-19 on the prevention, identification, and management of chronic disease. COVID-19 has resulted in decreases of many types of health care utilization (15), ranging from preventive care to chronic disease management and even emergency care (16). As of June 2020, 4 in 10 adults surveyed reported delaying or avoiding routine or emergent medical care because of the pandemic (14). Cancer screenings, for example, dropped during the pandemic (17). Decreases in screening have resulted in the diagnoses of fewer cancers and precancers (18), and modeling studies have estimated that delayed screening and treatment for breast and colorectal cancer could result in almost 10,000 preventable deaths in the United States (19). We have lost ground in prevention across the chronic disease spectrum and in other areas, including pediatric immunization (20), mental health (21,22), and substance abuse (21,22).
Some challenges with health care utilization may be improving, but improvement has not been consistent across all health care visit types, providers, patients, or communities (15). Questions about the impact of the pandemic on chronic disease include:
What diseases have been missed or allowed to worsen?
What is the status of prevention and disease management efforts?
Have prevention and disease management efforts been affected by concerns such as job loss, loss of insurance, lack of access to healthy food, or loss of places and opportunities to be physically active?
How have effects of the pandemic on health care systems (staff reductions, health practice closures, disrupted services) (23) and public health organizations’ deployment of personnel away from ongoing chronic disease prevention efforts been experienced nationally?
The effects of COVID-19, whether negative or positive, on health care and public health systems will certainly affect those with chronic disease. To fully understand the consequences of the pandemic, we need to assess its overall impact on incidence, management, and outcomes of chronic disease. This is particularly salient in communities where health inequities are already rampant or communities that are remote or underserved. Will our postpandemic response be strong enough to mitigate the exacerbation of inequities that have occurred? Can public health agencies effectively build trust in science and community health care systems where trust might never have been fully established or where it has been lost?
The third category relates to the long-term COVID-19 sequelae, both as a disease entity and from a population perspective. Has COVID-19 created a new group of patients with chronic diseases, neurologic or psychiatric conditions, diabetes, or effects on the heart, lungs, kidneys, or other organs (24)? Has it worsened existing conditions or caused additional chronic disease? And, at the population level, have the incidence and prevalence of chronic diseases increased because of pandemic-related health behaviors or other challenges, such as decreased food and nutrition security?
Given the rollout of COVID-19 vaccines and the coming end of the pandemic, this is an important time to examine the impact of COVID-19. Solutions at all levels are needed to improve health outcomes and lessen health inequities among people with or at risk for chronic disease. Solutions are likely to include increasing awareness about prevention and care during and after the pandemic, building or enhancing cross-organizational and cross-sector partnerships, innovating to address identified gaps, and addressing SDoH to improve health and achieve equity. So, what can be done?
Additional focus is required on several aspects of awareness about the impact of COVID-19. First, public health and health care practitioners need to allay people’s fears and help them safely return to health care. We need to reemphasize chronic disease prevention and care, explain how to safely access care, and convey the host of mitigation efforts made by health care systems, providers, and public health to ensure that environments are safe (eg, mask requirements, social distancing). Emphasis on safety and mitigation applies to both disease prevention (such as encouraging healthy nutrition and physical activity, screening for cancer and other conditions, and getting oral health care) and disease management (eg, educating patients about medications to control hypertension, diabetes, asthma, and other chronic conditions). Efforts must also include helping those with chronic diseases obtain access to and gain confidence in the COVID-19 vaccine. Given current community rates of COVID-19 and the need to reenter care after the height of the pandemic, information can help patients make informed choices about the need for in-person care, communication at a distance, or temporary delays in care that is more discretionary.
To garner support to help affected communities, there is a need to build awareness about how COVID-19 has disproportionately affected particular communities, including the unequal distribution of disease, morbidity, mortality, and resources, such as access to vaccines. Awareness is dependent on access to data at the granular geographic level, including information on the burden of chronic disease and the status of SDoH. Communities need data to effectively address health inequities in the aftermath of the pandemic.
Public health plays a significant role in addressing health behaviors (healthy eating, physical activity, avoiding tobacco and other substance use) and community solutions to address SDoH that impact prevention and control of chronic disease. Collaborations at both the individual and system levels, however, are required for success. Collaborative partners include other government and nongovernmental organizations, health care organizations, insurers, nonprofit organizations, community and faith-based groups, schools, businesses, and others. Coalitions and community groups are critical change agents. They have worked with local health departments and others to identify solutions, bring residents into discussions, and implement action. We can learn from them about how best to build trust and foster the innovation they are leading. Solutions must also include direct discussions with residents in affected communities to understand their priorities and effectively address their concerns. These relationships are particularly salient to address SDoH. These factors have been amplified as a direct consequence of COVID-19 and will require a multisector approach to problem solving.
To achieve this will require building trust in both the health care system and the public health system. The pandemic has taken a toll on an already fragile relationship between communities and public health and health care institutions where trust has been absent or insufficient. To begin to address the trust challenge will require investments in outreach, engagement, and transparency. Conversations need to be bidirectional, long-term, and conducted by people who are trusted, who are respectful, and who can identify with affected populations.
Creative solutions are needed to engage populations and promote resiliency among those who are disproportionately affected by COVID-19. Efforts that need to be further developed and brought to scale include the following:
Leveraging technology to expand the reach of health care and health promotion (eg, telemedicine, virtual program delivery, wearables, mobile device applications).
Providing more services in community settings, as is increasingly modeled in the National Diabetes Prevention Program (25).
Using community health workers to assist in assessing current conditions and connecting to community resources.
Further enhancing approaches to increase access to and convenience of services (eg, increasing access to home screenings, such as cancer screening) or monitoring (eg, home blood pressure monitoring) where appropriate.
Health care approaches, such as telemedicine, have expanded greatly during the pandemic and seem likely to continue expansion over time. As these and related efforts grow, practitioners will need to ensure that existing disparities are not magnified. Care is needed to ensure that those with the highest health needs can access services. For example, are technological solutions easily accessible, available in multiple languages, compatible with readily available hardware options, such as telephones rather than laptops? Are culturally appropriate resources available to help people use and value these technologies? In addition, computer availability and internet access will need to be expanded. Challenges such as unemployment, food insecurity, limited transportation, substance abuse, and social isolation will require a multisector effort uniquely adapted to local contexts. To begin, health equity–focused policy analyses and health impact assessments will help policy makers understand better how proposed SDoH-related action might either exacerbate or mitigate chronic disease inequities. These actions will help us develop a deeper understanding of what individual communities need to mobilize and build resilience for the future. We face serious public health and population health concerns that should be the focus in the near term — particularly as equitable access to COVID-19 vaccines is a consideration in every community across the nation. We clearly have an enormous amount of work to do as we enter recovery from the pandemic, but with recovery comes enormous opportunity.
A challenge related to long-term COVID-19 sequelae is that we do not know yet the extent that COVID-19 exacerbates chronic disease, causes chronic disease, or will be determined a chronic disease unto itself. Those interested in chronic disease prevention and management need to follow the research to understand better the role they will play with this emerging situation. Long-term studies and longitudinal surveillance will help clarify these issues, and there is much research to be done. The duty of the public health community is to help ensure that the most important issues from the perspectives of patients, providers, health care, and public health systems are addressed; that potential solutions are developed and tested; and that eventual solutions are delivered where they are needed most.
As the US enters the next phase of pandemic response, the work of National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) of the Centers for Disease Control and Prevention is evolving to address health inequities and drive toward health equity with a multipronged approach. This approach includes enhanced access to data at the local level, a focus on SDoH including a shift in the Notice of Funding Opportunity process that emphasizes a health equity lens, and an expansion of partnerships and communications.
Placing data in the hands of communities is critical for local coalitions to determine their burden of chronic disease and COVID-19, their access to resources, and the best policies and practices to implement. Data will be useful for local public health, governments, and health care systems, but can also help human services, planning, and economic development organizations. An initial step is making available data from the PLACES Project (26), which provides data on 27 chronic disease measures at the census tract level, allowing communities to understand their own chronic disease burden. In addition, modules on SDoH are in development to enhance NCCDPHP data surveillance systems. This will increase the ability to overlay chronic disease data and SDoH data at the community level. The need is also a great for core SDoH measures that allow comparisons of related outcomes across communities. NCCDPHP can augment this effort by contributing to and amplifying the SDoH measures identified for Healthy People 2030 (27).
NCCDPHP is focusing on supporting and stimulating SDoH efforts by concentrating on 5 major areas: built environment, social connectedness, food and nutrition security, tobacco policies, and connections to clinical care. For example, SDoH are the foci of recent Notices of Funding Opportunities (available at https://www.grants.gov). NCCDPHP supports multisector partnerships in numerous funding announcements and launched a joint effort with the Association of State and Territorial Health Officials and the National Association of County and City Health Officials to identify best practices in multisector collaboration to address SDoH (28). Evidence will help build a standard for success to support local coalitions in their work. States and local communities are sites of innovation, and promoting lessons learned can help build broader efforts. To address urgent needs and facilitate change, NCCDPHP must link with other sectors outside of public health and health care. The work to evaluate these efforts and determine the most effective strategies to address SDoH, therefore, will be integrated fully into NCCDPHP.
An expansion of the Racial and Ethnic Approaches to Community Health (REACH) Program (29) and other programs that address health inequities will help to target resources where they are needed most. REACH and a recently released investment in community health workers (30) demonstrate NCCDPHP’s commitment to connecting with populations that are disproportionately affected by chronic disease at the local level. These efforts are aimed at addressing the ramifications of COVID-19 while also amplifying chronic disease prevention efforts. NCCDPHP also intends to enhance the use of a health equity lens, among other approaches, to determine the best use of resources and to help assess outcomes in all programmatic activities.
Finally, communication about the impact of COVID-19 on chronic disease, returning to care, and the extent of health inequities is critical to building trust. Efforts under way include a television and digital media campaign aiming to encourage those with chronic disease to return safely to care (31). In addition to expanding work with partner organizations, both external and internal to government, NCCDPHP will embrace new ways of garnering input from affected communities. Successes and failures experienced by communities during the pandemic will continue to be of the utmost importance to NCCDPHP. In addition, important insights gained from working closely with affected communities will help NCCDPHP continually refine its national chronic disease prevention and control goals and objectives. Activities related to SDoH and health equity, data, and communication will address difficult questions now and into the future. These efforts can only be successful with collaboration and partnerships across multiple sectors.
The impact of SARS-CoV-2, the virus that causes COVID-19, on people with or at risk for chronic disease cannot be overstated. COVID-19 has impeded chronic disease prevention and disrupted disease management. The problems and solutions outlined here are critically important to help those committed to chronic disease prevention and intervention to identify ways forward.
NCCDPHP is adjusting, preparing, and implementing multiple strategies to address the future. Although the work will be challenging, opportunities abound. NCCDPHP is committed to working with the health care community and a variety of partners at federal, state, and local levels to help address the realities of the post-COVID era.
The authors have no conflicts of interest to report. No copyrighted materials were used in the preparation of this essay.
Corresponding Author: Karen A. Hacker, MD, MPH, National Center for Chronic Disease Prevention and Health Promotion, 4770 Buford Highway NE, Atlanta, GA 30341. Telephone: 404-632-5062. Email: [email protected] .
Author Affiliations: 1 National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, Georgia.
- Centers for Disease Control and Prevention, National Center for Health Statistics. Leading causes of death. Updated March 1, 2021. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm. Accessed April 8, 2021.
- Buttorff C, Teague R, Bauman M. Multiple chronic conditions in the United States. Santa Monica (CA): RAND Corporation; 2017. https://www.rand.org/pubs/tools/TL221.html. Accessed April 8, 2021.
- Center for Medicare & Medicaid Services. National health expenditures 2019 highlights. https://www.cms.gov/files/document/highlights.pdf. Accessed April 8, 2021.
- Centers for Disease Control and Prevention. COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed April 8, 2021.
- Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw Open 2020;3(12):e2029058. Erratum in: JAMA Netw Open 2021;1:e2036103[REMOVED IF= FIELD] CrossRef external icon
- Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020;584(7821):430–6. CrossRef external icon
- Centers for Disease Control and Prevention. People with certain medical conditions. Updated March 29, 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed April 8, 2021.
- Centers for Disease Control and Prevention, National Center for Health Statistics. Excess deaths associated with COVID-19. Updated April 7, 2021. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm. Accessed April 8, 2021.
- Centers for Disease Control and Prevention. Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Updated March 12, 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed April 8, 2021.
- Centers for Disease Control and Prevention. Health equity considerations and racial and ethnic minority groups. Updated February 12, 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Accessed April 8, 2021.
- Millett GA, Jones AT, Benkeser D, Baral S, Mercer L, Beyrer C, et al. Assessing differential impacts of COVID-19 on Black communities. Ann Epidemiol 2020;47:37–44. CrossRef external icon
- Cordes J, Castro MC. Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spat Spatio-Temporal Epidemiol 2020;34:100355. CrossRef external icon
- Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg 2020;78:185–93. CrossRef external icon
- Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep 2020;69(36):1250–7. CrossRef external icon
- Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D, Schneider EC, et al. The impact of the COVID-19 pandemic on outpatient care: visits return to prepandemic levels, but not for all providers and patients. 2020. https://www.commonwealthfund.org/publications/2020/oct/impact-covid-19-pandemic-outpatient-care-visits-return-prepandemic-levels. Accessed April 8, 2021.
- Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69(23):699–704. CrossRef external icon
- London JW, Fazio-Eynullayeva E, Palchuk MB, Sankey P, McNair C. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform. 2020;4(4):657–65. CrossRef external icon
- Bakouny Z, Paciotti M, Schmidt AL, Lipsitz SR, Choueiri TK, Trinh QD. Cancer screening tests and cancer diagnoses during the COVID-19 pandemic. JAMA Oncol 2021;7(3):458–60. CrossRef external icon
- Sharpless NE. COVID-19 and cancer. Science 2020;368(6497):1290. CrossRef external icon
- Santoli JM, Lindley MC, DeSilva MB, Kharbanda EO, Daley MF, Galloway L, et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration — United States, 2020. MMWR Morb Mortal Wkly Rep 2020;69(19):591–3. CrossRef external icon
- Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep . 2020;69:1049–1057. CrossRef external icon
- Czeisler MÉ, Lane RI, Wiley JF, Czeisler CA, Howard ME, Rajaratnam SMW. Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, September 2020. JAMA Netw Open 2021;4(2):e2037665. CrossRef external icon
- Song Z, Giuriato M, Lillehaugen T, Altman W, Horn DM, Phillips RS, et al. Economic and clinical impact of COVID-19 on provider practices in Massachusetts. New England Journal of Medicine Catalyst Innovations in Care Delivery . Published online September 11, 2020. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0441. Accessed May 19, 2021.
- Rubin R. As their numbers grow, COVID-19 long haulers stump experts. JAMA 2020;324(14):1381–3. CrossRef external icon
- Centers for Disease Control and Prevention. National Diabetes Prevention Program: working together to prevent diabetes. Updated August 10, 2019. https://www.cdc.gov/diabetes/prevention/index.html. Accessed April 8, 2021.
- Centers for Disease Control and Prevention, Division of Population Health. PLACES: local data for better health. Updated December 8, 2020. https://www.cdc.gov/places/about/index.html. Accessed April 8, 2021.
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy people 2030: social determinants of health. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Accessed April 29, 2021.
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. Social determinants of health community pilots. Updated March 17, 2021. https://www.cdc.gov/chronicdisease/programs-impact/SDoH/community-pilots.htm. Accessed April 8, 2021.
- Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity. Racial and ethnic approaches to community health. Updated October 16, 2020. https://www.cdc.gov/nccdphp/dnpao/state-local-programs/reach/index.htm. Accessed April 8, 2021.
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. Community health workers for COVID response and resilient communities (CCR) CDC-RFA-DP21-2109. Updated April 28, 2021. https://www.cdc.gov/chronicdisease/programs-impact/nofo/covid-response.htm. Accessed April 29, 2021.
- The National Association of Chronic Disease Directors. Your health beyond COVID-19 matters! https://yourhealthbeyondcovid.org. Accessed April 29, 2021.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 74, Issue 11
- The COVID-19 pandemic and health inequalities
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-1294-6851 Clare Bambra 1 ,
- Ryan Riordan 2 ,
- John Ford 2 ,
- Fiona Matthews 1
- 1 Population Health Sciences Institute, Newcastle University Institute for Health and Society , Newcastle upon Tyne , UK
- 2 School of Clinical Medicine, Cambridge University , Cambridge , UK
- Correspondence to Clare Bambra, Population Health Sciences Institute, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne NE1 4LP, UK; clare.bambra{at}newcastle.ac.uk
This essay examines the implications of the COVID-19 pandemic for health inequalities. It outlines historical and contemporary evidence of inequalities in pandemics—drawing on international research into the Spanish influenza pandemic of 1918, the H1N1 outbreak of 2009 and the emerging international estimates of socio-economic, ethnic and geographical inequalities in COVID-19 infection and mortality rates. It then examines how these inequalities in COVID-19 are related to existing inequalities in chronic diseases and the social determinants of health, arguing that we are experiencing a syndemic pandemic . It then explores the potential consequences for health inequalities of the lockdown measures implemented internationally as a response to the COVID-19 pandemic, focusing on the likely unequal impacts of the economic crisis. The essay concludes by reflecting on the longer-term public health policy responses needed to ensure that the COVID-19 pandemic does not increase health inequalities for future generations.
- DEPRIVATION
- Health inequalities
This article is made freely available for use in accordance with BMJ's website terms and conditions for the duration of the COVID-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
https://doi.org/10.1136/jech-2020-214401
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
INTRODUCTION
In 1931, Edgar Sydenstricker outlined inequalities by socio-economic class in the 1918 Spanish influenza epidemic in America, reporting a significantly higher incidence among the working classes. 1 This challenged the widely held popular and scientific consensus of the time which held that ‘the flu hit the rich and the poor alike’. 2 In the COVID-19 pandemic, there have been similar claims made by politicians and the media - that we are ‘all in it together’ and that the COVID-19 virus ‘does not discriminate’. 3 This essay aims to dispel this myth of COVID-19 as a socially neutral disease, by discussing how, just as 100 years ago, there are inequalities in COVID-19 morbidity and mortality rates—reflecting existing unequal experiences of chronic diseases and the social determinants of health. The essay is structured in three main parts. Part 1 examines historical and contemporary evidence of inequalities in pandemics—drawing on international research into the Spanish influenza pandemic of 1918, the H1N1 outbreak of 2009 and the emerging international estimates of socio-economic, ethnic and geographical inequalities in COVID-19 infection and mortality rates. Part 2 examines how these inequalities in COVID-19 are related to existing inequalities in chronic diseases and the social determinants of health, arguing that we are experiencing a syndemic pandemic . In Part 3, we explore the potential consequences for health inequalities of the lockdown measures implemented internationally as a response to the COVID-19 pandemic, focusing on the likely unequal impacts of the economic crisis. The essay concludes by reflecting on the longer-term public health policy responses needed to ensure that the COVID-19 pandemic does not increase health inequalities for future generations.
PART 1. HISTORICAL AND CONTEMPORARY EVIDENCE OF INEQUALITIES IN PANDEMICS
More recent studies have confirmed Sydenstricker’s early findings: there were significant inequalities in the 1918 Spanish influenza pandemic. The international literature demonstrates that there were inequalities in prevalence and mortality rates: between high-income and low-income countries, more and less affluent neighbourhoods, higher and lower socio-economic groups, and urban and rural areas. For example, India had a mortality rate 40 times higher than Denmark and the mortality rate was 20 times higher in some South American countries than in Europe. 4 In Norway, mortality rates were highest among the working-class districts of Oslo 5 ; in the USA, they were highest among the unemployed and the urban poor in Chicago, 6 and across Sweden, there were inequalities in mortality between the highest and lowest occupational classes—particularly among men. 7 In contrast, countries with smaller pre-existing social and economic inequalities, such as New Zealand, did not experience any socio-economic inequalities in mortality. 8 9 An urban–rural effect was also observed in the 1918 influenza pandemic whereby, for example, in England and Wales, the mortality was 30%–40% higher in urban areas. 10 There is also some evidence from the USA that the pandemic had long-term impacts on inequalities in child health and development. 11
Several studies have also demonstrated inequalities in the 2009 H1N1 influenza pandemic. For example, globally, Mexico experienced a higher mortality rate than that in higher-income countries. 12 In terms of socio-economic inequalities, themortality rate from H1N1 in the most deprived neighbourhoods of England was three times higher than in the least deprived. 13 It was also higher in urban compared to rural areas. 13 Similarly, a Canadian study in Ontario found that hospitalisation rates for H1N1 were associated with lower educational attainment and living in a high deprivation neighbourhood. 14 Another study found positive associations between people with financial issues (eg, financial barriers to healthcare access) and influenza-like illnesses during the 2009 H1N1 pandemic in the USA. 15 Various studies on cyclical winter influenza in North America have also found associations between mortality, morbidity and symptom severity and socio-economic status among adults and children. 16 17
Just as in 1918 and 2009, evidence of social inequalities is already emerging in relation to COVID-19 from Spain, the USA and the UK. Intermediate data published by the Catalonian government in Spain suggest that the rate of COVID-19 infection is six or seven times higher in the most deprived areas of the region compared to the least deprived. 18 Similarly, in preliminary USA analysis, Chen and Krieger (2020) found area-level socio-spatial gradients in confirmed cases in Illinois and positive test results in New York City, with dramatically increased risk of death observed among residents of the most disadvantaged counties. 19 With regard to ethnic inequalities in COVID-19, data from England and Wales have found that people who are black, Asian and minority ethnic (BAME) accounted for 34.5% of 4873 critically ill COVID-19 patients (in the period ending April 16, 2020) and much higher than the 11.5% seen for viral pneumonia between 2017 and 2019. 20 Only 14% of the population of England and Wales are from BAME backgrounds. Even more stark is the data on racial inequalities in COVID-19 infections and deaths that are being released by various states and municipalities in the USA. For example, in Chicago (in the period ending April 17, 2020), 59.2% of COVID-19 deaths were among black residents and the COVID-19 mortality rate for black Chicagoans was 34.8 per 100 000 population compared to 8.2 per 100 000 population among white residents. 21 There will likely be an interaction of race and socio-economic inequalities, demonstrating the intersectionality of multiple aspects of disadvantage coalescing to further compound illness and increase the risk of mortality. 22
PART 2. THE SYNDEMIC OF COVID-19, CHRONIC DISEASE AND THE SOCIAL DETERMINANTS OF HEALTH
The COVID-19 pandemic is occurring against a backdrop of social and economic inequalities in existing non-communicable diseases (NCDs) as well as inequalities in the social determinants of health. Inequalities in COVID-19 infection and mortality rates are therefore arising as a result of a syndemic of COVID-19, inequalities in chronic diseases and the social determinants of health. The prevalence and severity of the COVID-19 pandemic is magnified because of the pre-existing epidemics of chronic disease—which are themselves socially patterned and associated with the social determinants of health. The concept of a syndemic was originally developed by Merrill Singer to help understand the relationships between HIV/AIDS, substance use and violence in the USA in the 1990s. 23 A syndemic exists when risk factors or comorbidities are intertwined, interactive and cumulative—adversely exacerbating the disease burden and additively increasing its negative effects: ‘A syndemic is a set of closely intertwined and mutual enhancing health problems that significantly affect the overall health status of a population within the context of a perpetuating configuration of noxious social conditions’ [24 p13]. We argue that for the most disadvantaged communities, COVID-19 is experienced as a syndemic—a co-occurring, synergistic pandemic that interacts with and exacerbates their existing NCDs and social conditions ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
The syndemic of COVID-19, non-communicable diseases (NCDs) and the social determinants of health (adapted from Singer 23 and Dahlgren and Whitehead 25 ).
Minority ethnic groups, people living in areas of higher socio-economic deprivation, those in poverty and other marginalised groups (such as homeless people, prisoners and street-based sex workers) generally have a greater number of coexisting NCDs, which are more severe and experienced at at a younger age. For example, people living in more socio-economically disadvantaged neighbourhoods and minority ethnic groups have higher rates of almost all of the known underlying clinical risk factors that increase the severity and mortality of COVID-19, including hypertension, diabetes, asthma, chronic obstructive pulmonary disease (COPD), heart disease, liver disease, renal disease, cancer, cardiovascular disease, obesity and smoking. 26–29 Likewise, minority ethnic groups in Europe, the USA and other high-income countries experience higher rates of the key COVID-19 risk factors, including coronary heart disease and diabetes. 28 Similarly, the Gypsy/Roma community—one of the most marginalised minority groups in Europe—has a smoking rate that is two to three times the European average and increased rates of respiratory diseases (such as COPD) and other COVID-19 risk factors. 29
These inequalities in chronic conditions arise as a result of inequalities in exposure to the social determinants of health: the conditions in which people ‘live, work, grow and age’ including working conditions, unemployment, access to essential goods and services (eg, water, sanitation and food), housing and access to healthcare. 25 30 By way of example, there are considerable occupational inequalities in exposure to adverse working conditions (eg, ergonomic hazards, repetitive work, long hours, shift work, low wages, job insecurity)—they are concentrated in lower-skill jobs. These working conditions are associated with increased risks of respiratory diseases, certain cancers, musculoskeletal disease, hypertension, stress and anxiety. 31 In addition to these long-term exposures, inequalities in working conditions may well be impacting the unequal distribution of the COVID-19 disease burden. For example, lower-paid workers (where BAME groups are disproportionately represented)—particularly in the service sector (eg, food, cleaning or delivery services)—are much more likely to be designated as key workers and thereby are still required to go to work and rely on public transport for doing so. All these increase their exposure to the virus.
Similarly, access to healthcare is lower in disadvantaged and marginalised communities—even in universal healthcare systems. 32 In England, the number of patients per general practitioner is 15% higher in the most deprived areas than that in the least deprived areas. 33 Medical care is even more unequally distributed in countries such as the USA where around 33 million Americans—from the most disadvantaged and marginalised groups—have insufficient or no healthcare insurance. 27 This reduced access to healthcare—before and during the outbreak—contributes to inequalities in chronic disease and is also likely to lead to worse outcomes from COVID-19 in more disadvantaged areas and marginalised communities. People with existing chronic conditions (eg, cancer or cardiovascular disease (CVD)) are less likely to receive treatment and diagnosis as health services are overwhelmed by dealing with the pandemic.
Housing is also an important factor in driving health inequalities. 34 For example, exposure to poor quality housing is associated with certain health outcomes, for example, damp housing can lead to respiratory diseases such as asthma while overcrowding can result in higher infection rates and increased risk of injury from household accidents. 34 Housing also impacts health inequalities materially through costs (eg, as a result of high rents) and psychosocially through insecurity (eg, short-term leases). 34 Lower socio-economic groups have a higher exposure to poor quality or unaffordable, insecure housing and therefore have a higher rate of negative health consequences. 35 These inequalities in housing conditions may also be contributing to inequalities in COVID-19. For example, deprived neighbourhoods are more likely to contain houses of multiple occupation and smaller houses with a lack of outside space, as well as have higher population densities (particularly in deprived urban areas) and lower access to communal green space. 27 These will likely increase COVID-19 transmission rates—as was the case with H1N1 where strong associations were found with urbanity. 13
The social determinants of health also work to make people from marginalised communities more vulnerable to infection from COVID-19—even when they have no underlying health conditions. Decades of research into the psychosocial determinants of health have found that the chronic stress of material and psychological deprivation is associated with immunosuppression. 36 Psychosocial feelings of subordination or inferiority as a result of occupying a low position on the social hierarchy stimulate physiological stress responses (eg, raised cortisol levels), which, when prolonged (chronic), can have long-term adverse consequences for physical and mental health. 37 By way of example, studies have found consistent associations between low job status (eg, low control and high demands), stress-related morbidity and various chronic conditions including coronary heart disease, hypertension, obesity, musculoskeletal conditions, and psychological ill health. 38 Likewise, there is increasing evidence that living in disadvantaged environments may produce a sense of powerlessness and collective threat among residents, leading to chronic stressors that, in time, damage health. 39 Studies have also confirmed that adverse psychosocial circumstances increase susceptibility—influencing the onset, course and outcome of infectious diseases—including respiratory diseases like COVID-19. 40
PART 3. THE GREAT LOCKDOWN: THE COVID-19 ECONOMIC CRISIS AND HEALTH INEQUALITIES
The impact of COVID-19 on health inequalities will not just be in terms of virus-related infection and mortality, but also in terms of the health consequences of the policy responses undertaken in most countries. While traditional public health surveillance measures of contact tracing and individual quarantine were successfully pursued by some countries (most notably by South Korea and Germany) as a way of tackling the virus in the early stages, most other countries failed to do so, and governments worldwide were eventually forced to implement mass quarantine measures—in the form of lockdowns. These state-imposed restrictions—usually requiring the government to take on emergency powers—have been implemented to varying levels of severity, but all have in common a significant increase in social isolation and confinement within the home and immediate neighbourhood. The aims of these unprecedented measures are to increase social and physical distancing and thereby reduce the effective reproduction number (eR0) of the virus to less than 1. For example, in the UK, individuals were only allowed to leave the home for one of four reasons (shopping for basic necessities, exercise, medical needs, travelling for work purposes). Following Wuhan province in China, most of the lockdowns have been implemented for 8 to 12 weeks.
The immediate pathways through which the COVID-19 emergency lockdowns are likely to have unequal health impacts are multiple—ranging from unequal experiences of lockdown (eg, due to job and income loss, overcrowding, urbanity, access to green space, key worker roles), how the lockdown itself is shaping the social determinants of health (eg, reduced access to healthcare services for non-COVID-19 reasons as the system is overwhelmed by the pandemic) and inequalities in the immediate health impacts of the lockdown (eg, in mental health and gender-based violence). However, arguably, the longer-term and largest consequences of the ‘great lockdown’ for health inequalities will be through political and economic pathways ( figure 1 ). The world economy has been severely impacted by COVID-19—with almost daily record stock market falls, oil prices have crashed and there are record levels of unemployment (eg, 5.2 million people filed for unemployment benefit in just 1 week in April 2020 in the USA), despite the unprecedented interventionist measures undertaken by some governments and central banks—such as the £300 billion injection by the UK government to support workers and businesses. The pandemic has slowed China’s economy with a predicted loss of $65 billion as a minimum in the first quarter of 2020. Economists fear that the economic impact will be far greater than the financial crisis of 2007/2008, and they say that it is likely to be worse in depth than the Great Depression of the 1930s. Just like the 1918 influenza pandemic (which had severe impacts on economic performance and increased poverty rates), the COVID-19 crisis will have huge economic, social and—ultimately—health consequences.
Previous research has found that sudden economic shocks (like the collapse of communism in the early 1990s and the global financial crisis (GFC) of 2008 41 ) lead to increases in morbidity, mental ill health, suicide and death from alcohol and substance use. For example, following the GFC, worldwide an excess of suicides were observed in the USA, England, Spain and Ireland. 42 There is also evidence of other increases in poor mental health after the GFC including self-harm and psychiatric morbidity. 41 42 These health impacts were not shared equally though—areas of the UK with higher unemployment rates had greater increases in suicide rates and inequalities in mental health increased with people living in the most deprived areas experiencing the largest increases in psychiatric morbidity and self-harm. 43 Further, unemployment (and its well-established negative health impacts in terms of morbidity and mortality 38 ) is disproportionately experienced by those with lower skills or who live in less buoyant local labour markets. 27 So, the health consequences of the COVID-19 economic crisis are likely to be similarly unequally distributed—exacerbating heath inequalities.
However, the effects of recessions on health inequalities also vary by public policy response with countries such as the UK, Greece, Italy and Spain who imposed austerity (significant cuts in health and social protection budgets) after the GFC experiencing worse population health effects than those countries such as Germany, Iceland and Sweden who opted to maintain public spending and social safety nets. 41 Indeed, research has found that countries with higher rates of social protection (such as Sweden) did not experience increases in health inequalities during the 1990s economic recession. 44 Similarly, old-age pensions in the UK were protected from austerity cuts after the GFC and research has suggested that this prevented health inequalities increasing amongst the older population. 45 These findings are in keeping with previous studies of the effects of public sector and welfare state contractions and expansions on trends in health inequalities in the UK, USA and New Zealand. 27 46–49 For example, inequalities in premature mortality and infant mortality by income and ethnicity in the USA decreased during the period of welfare expansion in the USA (‘war on poverty’ era 1966 to 1980), but they increased again during the Reagan–Bush period (1980–2002) when welfare services and healthcare coverage were cut. 46 Similarly, in England, inequalities in infant mortality rates reduced as child poverty decreased in a period of public sector and welfare state expansion (from 2000 to 2010), 47 but increased again when austerity was implemented and child poverty rates increased (from 2010 to 2017). 48
So this essay makes for grim reading for researchers, practitioners and policymakers concerned with health inequalities. Historically, pandemics have been experienced unequally with higher rates of infection and mortality among the most disadvantaged communities—particularly in more socially unequal countries. 8 9 Emerging evidence from a variety of countries suggests that these inequalities are being mirrored today in the COVID-19 pandemic. Both then and now, these inequalities have emerged through the syndemic nature of COVID-19—as it interacts with and exacerbates existing social inequalities in chronic disease and the social determinants of health. COVID-19 has laid bare our longstanding social, economic and political inequalities - even before the COVID-19 pandemic, life expectancy amongst the poorest groups was already declining in the UK and the USA and health inequalities in some European countries have been increasing over the last decade. 50 It seems likely that there will be a post-COVID-19 global economic slump—which could make the health equity situation even worse, particularly if health-damaging policies of austerity are implemented again. It is vital that this time, the right public policy responses (such as expanding social protection and public services and pursuing green inclusive growth strategies) are undertaken so that the COVID-19 pandemic does not increase health inequalities for future generations. Public health must ‘win the peace’ as well as the ‘war’.
Acknowledgments
We would like to thank Chris Orton from the Cartographic Unit, Department of Geography, Durham University, for his assistance with the graphics for figure 1 .
- Sydenstricker E
- Lawrence AJ
- SkyNews (27/03/20)
- Murray CJ ,
- Chin B , et al.
- Mamelund SE
- Grantz KH ,
- Salje H , et al.
- Bengtsson T ,
- Summers JA ,
- Stanley J ,
- Baker MG , et al.
- Chowell G ,
- Bettencourt LMA ,
- Johnson N , et al.
- Majia LSF , et al.
- Rutter PD ,
- Mytton OT ,
- Mak M , et al.
- Lowcock EC ,
- Rosella LC ,
- Foisy J , et al.
- Biggerstaff M ,
- Reed C , et al.
- Yousey-hindes K ,
- Crighton EJ ,
- Elliott SJ ,
- Moineddin R , et al.
- Catalan Agency for Health Quality and Assessment (AQuAS)
- Intensive Care National Audit and Research Centre
- Chicago Department of Public Health
- Gkiouleka A ,
- Beckfield J , et al.
- Dahlgren G ,
- Whitehead M
- Zhang X , et al.
- Public health England
- European commission
- WHO - World Health. Organisation
- Copeland A ,
- Kasim A , et al.
- Lacobucci G
- Petticrew M ,
- Bambra C , et al.
- McNamara CL ,
- Thomson KH , et al.
- Segerstrom SC ,
- Whitehead M ,
- Pennington A ,
- Orton L , et al.
- Stuckler D ,
- Corcoran P ,
- Griffin E ,
- Arensman E , et al.
- Kinderman P ,
- Whitehead P
- Nylen L , et al.
- Mattheys K , et al.
- Krieger N ,
- Rehkopf DH ,
- Chen JT , et al.
- Robinson T ,
- Norman P , et al.
- Taylor-Robinson D ,
- Wickham S , et al.
- Beckfield J ,
- Forster T ,
- Kentikelenis A ,
Twitter Clare Bambra @ProfBambra.
Funding CB is a senior investigator in the National Institute for Health Research (NIHR) ARC North East and North Cumbria, NIHR Policy Research Unit in Behavioural Science, NIHR School of Public Health Research, the UK Prevention Research Partnership SIPHER: Systems science in Public Health and Health Economics Research consortium, and the Norwegian Research Council Centre for Global Health Inequalities Research. JF is a senior investigator in the NIHR ARC East of England. FM is a senior investigator in the NIHR Policy Research Unit in Ageing and Frailty. The views expressed in this publication are those of the authors and not necessarily those of the funders.
Competing interests We have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.
Patient consent for publication Not required.
Data sharing statement Data sharing not applicable as no datasets generated and/or analysed for this study.
Provenance and peer review Not commissioned; internally peer reviewed.
Read the full text or download the PDF:
How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.
Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College
You May Also Like
Protests boil over on college campuses.
Lauren Camera April 22, 2024

Supporting Low-Income College Applicants
Shavar Jeffries April 16, 2024

Supporting Black Women in Higher Ed
Zainab Okolo April 15, 2024

Law Schools With the Highest LSATs
Ilana Kowarski and Cole Claybourn April 11, 2024

Today NAIA, Tomorrow Title IX?
Lauren Camera April 9, 2024

Grad School Housing Options
Anayat Durrani April 9, 2024

How to Decide if an MBA Is Worth it
Sarah Wood March 27, 2024

What to Wear to a Graduation
LaMont Jones, Jr. March 27, 2024

FAFSA Delays Alarm Families, Colleges
Sarah Wood March 25, 2024

Help Your Teen With the College Decision
Anayat Durrani March 25, 2024

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 03 October 2022
How COVID-19 shaped mental health: from infection to pandemic effects
- Brenda W. J. H. Penninx ORCID: orcid.org/0000-0001-7779-9672 1 , 2 ,
- Michael E. Benros ORCID: orcid.org/0000-0003-4939-9465 3 , 4 ,
- Robyn S. Klein 5 &
- Christiaan H. Vinkers ORCID: orcid.org/0000-0003-3698-0744 1 , 2
Nature Medicine volume 28 , pages 2027–2037 ( 2022 ) Cite this article
39k Accesses
122 Citations
491 Altmetric
Metrics details
- Epidemiology
- Infectious diseases
- Neurological manifestations
- Psychiatric disorders
The Coronavirus Disease 2019 (COVID-19) pandemic has threatened global mental health, both indirectly via disruptive societal changes and directly via neuropsychiatric sequelae after SARS-CoV-2 infection. Despite a small increase in self-reported mental health problems, this has (so far) not translated into objectively measurable increased rates of mental disorders, self-harm or suicide rates at the population level. This could suggest effective resilience and adaptation, but there is substantial heterogeneity among subgroups, and time-lag effects may also exist. With regard to COVID-19 itself, both acute and post-acute neuropsychiatric sequelae have become apparent, with high prevalence of fatigue, cognitive impairments and anxiety and depressive symptoms, even months after infection. To understand how COVID-19 continues to shape mental health in the longer term, fine-grained, well-controlled longitudinal data at the (neuro)biological, individual and societal levels remain essential. For future pandemics, policymakers and clinicians should prioritize mental health from the outset to identify and protect those at risk and promote long-term resilience.
Similar content being viewed by others

A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging
Parminder Raina, Christina Wolfson, … CLSA team
Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis
Surapon Nochaiwong, Chidchanok Ruengorn, … Tinakon Wongpakaran
The effects of the COVID-19 pandemic on neuropsychiatric symptoms in dementia and carer mental health: an international multicentre study
Grace Wei, Janine Diehl-Schmid, … Fiona Kumfor
In 2019, the COVID-19 outbreak was declared a pandemic by the World Health Organization (WHO), with 590 million confirmed cases and 6.4 million deaths worldwide as of August 2022 (ref. 1 ). To contain the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) across the globe, many national and local governments implemented often drastic restrictions as preventive health measures. Consequently, the pandemic has not only led to potential SARS-CoV-2 exposure, infection and disease but also to a wide range of policies consisting of mask requirements, quarantines, lockdowns, physical distancing and closure of non-essential services, with unprecedented societal and economic consequences.
As the world is slowly gaining control over COVID-19, it is timely and essential to ask how the pandemic has affected global mental health. Indirect effects include stress-evoking and disruptive societal changes, which may detrimentally affect mental health in the general population. Direct effects include SARS-CoV-2-mediated acute and long-lasting neuropsychiatric sequelae in affected individuals that occur during primary infection or as part of post-acute COVID syndrome (PACS) 2 —defined as symptoms lasting beyond 3–4 weeks that can involve multiple organs, including the brain. Several terminologies exist for characterizing the effects of COVID-19. PACS also includes late sequalae that constitute a clinical diagnosis of ‘long COVID’ where persistent symptoms are still present 12 weeks after initial infection and cannot be attributed to other conditions 3 .
Here we review both the direct and indirect effects of COVID-19 on mental health. First, we summarize empirical findings on how the COVID-19 pandemic has impacted population mental health, through mental health symptom reports, mental disorder prevalence and suicide rates. Second, we describe mental health sequalae of SARS-CoV-2 virus infection and COVID-19 disease (for example, cognitive impairment, fatigue and affective symptoms). For this, we use the term PACS for neuropsychiatric consequences beyond the acute period, and will also describe the underlying neurobiological impact on brain structure and function. We conclude with a discussion of the lessons learned and knowledge gaps that need to be further addressed.
Impact of the COVID-19 pandemic on population mental health
Independent of the pandemic, mental disorders are known to be prevalent globally and cause a very high disease burden 4 , 5 , 6 . For most common mental disorders (including major depressive disorder, anxiety disorders and alcohol use disorder), environmental stressors play a major etiological role. Disruptive and unpredictable pandemic circumstances may increase distress levels in many individuals, at least temporarily. However, it should be noted that the pandemic not only resulted in negative stressors but also in positive and potentially buffering changes for some, including a better work–life balance, improved family dynamics and enhanced feelings of closeness 7 .
Awareness of the potential mental health impact of the COVID-19 pandemic is reflected in the more than 35,000 papers published on this topic. However, this rapid research output comes with a cost: conclusions from many papers are limited due to small sample sizes, convenience sampling with unclear generalizability implications and lack of a pre-COVID-19 comparison. More reliable estimates of the pandemic mental health impact come from studies with longitudinal or time-series designs that include a pre-pandemic comparison. In our description of the evidence, we, therefore, explicitly focused on findings from meta-analyses that include longitudinal studies with data before the pandemic, as recently identified through a systematic literature search by the WHO 8 .
Self-reported mental health problems
Most studies examining the pandemic impact on mental health used online data collection methods to measure self-reported common indicators, such as mood, anxiety or general psychological distress. Pooled prevalence estimates of clinically relevant high levels of depression and anxiety symptoms during the COVID-19 pandemic range widely—between 20% and 35% 9 , 10 , 11 , 12 —but are difficult to interpret due to large methodological and sample heterogeneity. It also is important to note that high levels of self-reported mental health problems identify increased vulnerability and signal an increased risk for mental disorders, but they do not equal clinical caseness levels, which are generally much lower.
Three meta-analyses, pooling data from between 11 and 61 studies and involving ~50,000 individuals or more 13 , 14 , 15 , compared levels of self-reported mental health problems during the COVID-19 pandemic with those before the pandemic. Meta-analyses report on pooled effect sizes—that is, weighted averages of study-level effect sizes; these are generally considered small when they are ~0.2, moderate when ~0.5 and large when ~0.8. As shown in Table 1 , meta-analyses on mental health impact of the COVID-19 pandemic reach consistent conclusions and indicate that there has been a heterogeneous, statistically significant but small increase in self-reported mental health problems, with pooled effect sizes ranging from 0.07 to 0.27. The largest symptom increase was found when using specific mental health outcome measures assessing depression or anxiety symptoms. In addition, loneliness—a strong correlate of depression and anxiety—showed a small but significant increase during the pandemic (Table 1 ; effect size = 0.27) 16 . In contrast, self-reported general mental health and well-being indicators did not show significant change, and psychotic symptoms seemed to have decreased slightly 13 . In Europe, alcohol purchase decreased, but high-level drinking patterns solidified among those with pre-pandemic high drinking levels 17 . When compared to pre-COVID levels, no change in self-reported alcohol use (effect size = −0.01) was observed in a recent meta-analysis summarizing 128 studies from 58 (predominantly European and North American) countries 18 .
What is the time trajectory of self-reported mental health problems during the pandemic? Although findings are not uniform, various large-scale studies confirmed that the increase in mental health problems was highest during the first peak months of the pandemic and smaller—but not fully gone—in subsequent months when infection rates declined and social restrictions eased 13 , 19 , 20 . Psychological distress reports in the United Kingdom increased again during the second lockdown period 15 . Direct associations between anxiety and depression symptom levels and the average number of daily COVID-19 cases were confirmed in the US Centers for Disease Control and Prevention (CDC) data 21 . Studies that examined longer-term trajectories of symptoms during the first or even second year of the COVID-19 pandemic are more sparse but revealed stability of symptoms without clear evidence of recovery 15 , 22 . The exception appears to be for loneliness, as some studies confirmed further increasing trends throughout the first COVID-19 pandemic year 22 , 23 . As most published population-based studies were conducted in the early time period in which absolute numbers of SARS-CoV2-infected individuals were still low, the mental health impacts described in such studies are most likely due to indirect rather than direct effects of SARS-CoV-2 infection. However, it is possible that, in longer-term or later studies, these direct and indirect effects may be more intertwined.
The extent to which governmental policies and communication have impacted on population mental health is a relevant question. In cross-country comparisons, the extent of social restrictions showed a dose–response relationship with mental health problems 24 , 25 . In a review of 33 studies worldwide, it was concluded that governments that enacted stringent measures to contain the spread of COVID-19 benefitted not only the physical but also the mental health of their population during the pandemic 26 , even though more stringent policies may lead to more short-term mental distress 25 . It has been suggested that effective communication of risks, choices and policy measures may reduce polarization and conspiracy theories and mitigate the mental health impact of such measures 25 , 27 , 28 .
In sum, the general pattern of results is that of an increase in mental health symptoms in the population, especially during the first pandemic months, that remained elevated throughout 2020 and early 2021. It should be emphasized that this increase has a small effect size. However, even a small upward shift in mental health problems warrants attention as it has not yet shown to be returned to pre-pandemic levels, and it may have meaningful cumulative consequences at the population level. In addition, even a small effect size may mask a substantial heterogeneity in mental health impact, which may have affected vulnerable groups disproportionally (see below).
Mental disorders, self-harm and suicide
Whether the observed increase in mental health problems during the COVID-19 pandemic has translated into more mental disorders or even suicide mortality is not easy to answer. Mental disorders, characterized by more severe, disabling and persistent symptoms than self-reported mental health problems, are usually diagnosed by a clinician based on the International Classification of Diseases, 10th Revision (ICD-10) or the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria or with validated semi-structured clinical interviews. However, during the COVID-19 pandemic, research systematically examining the population prevalence of mental disorders has been sparse. Unfortunately, we can also not strongly rely on healthcare use studies as the pandemic impacted on healthcare provision more broadly, thereby making figures of patient admissions difficult to interpret.
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic has led to a 28% (95% uncertainty interval (UI): 25–30) increase in major depressive disorders and a 26% (95% UI: 23–28) increase in anxiety disorders. It should be noted that these estimations come with high uncertainty as the assumption that transient pandemic-related increases in mental symptoms extrapolate into incident mental disorders remains disputable. So far, only four longitudinal population-based studies have measured and compared current mental (that is, depressive and anxiety) disorder prevalence—defined using psychiatric diagnostic criteria—before and during the pandemic. Of these, two found no change 30 , 31 , one found a decrease 32 and one found an increase in prevalence of these disorders 33 . These studies were local, limited to high-income countries, often small-scale and used different modes of assessment (for example, online versus in-person) before and during the pandemic. This renders these observational results uncertain as well, but their contrast to the GBD calculations 29 is striking.
Time-series analysis of monthly suicide trends in 21 middle-income to high-income countries across the globe yielded no evidence for an increase in suicide rates in the first 4 months of the pandemic, and there was evidence of a fall in rates in 12 countries 34 . Also in the United States, there was a significant decrease in suicide mortality in the first pandemic months but a slight increase in mortality due to drug overdose and homicide 35 . A living systematic review 36 also concluded that, throughout 2020, there was no observed increase in suicide rates in 20 studies conducted in North America, Europe and Asia. Analyses of electronic health record data in the primary care setting showed reduced rates of self-harm during the first COVID-19 pandemic year 37 . In contrast, emergency department visits for self-harm behavior were unchanged 38 or increased 39 . Such inconsistent findings across healthcare settings may reflect a reluctance in healthcare-seeking behavior for mental healthcare issues. In the living systematic review, eight of 11 studies that examined service use data found a significant decrease in reported self-harm/suicide attempts after COVID lockdown, which returned to pre-lockdown levels in some studies with longer follow-up (5 months) 36 .
In sum, although calculations based on survey data predict a global increase of mental disorder prevalence, objective and consistent evidence for an increased mental disorder, self-harm or suicide prevalence or incidence during the first pandemic year remains absent. This observation, coupled with the only small increase in mental health symptom levels in the overall population, may suggest that most of the general population has demonstrated remarkable resilience and adaptation. However, alternative interpretations are possible. First, there is a large degree of heterogeneity in the mental health impact of COVID-19, and increased mental health in one group (for example, due to better work–family balance and work flexibility) may have masked mental health problems in others. Various societal responses seen in many countries, such as community support activities and bolstering mental health and crisis services, may have had mitigating effects on the mental health burden. Also, the relationship between mental health symptom increases during stressful periods and its subsequent effects on the incidence of mental disorders may be non-linear or could be less visible due to resulting alternative outcomes, such as drug overdose or homicide. Finally, we cannot rule out a lag-time effect, where disorders may take more time to develop or be picked up, especially because some of the personal financial or social consequences of the COVID pandemic may only become apparent later. It should be noted that data from low-income countries and longer-term studies beyond the first pandemic year are largely absent.
Which individuals are most affected by the COVID-19 pandemic?
There is substantial heterogeneity across studies that evaluated how the COVID pandemic impacted on mental health 13 , 14 , 15 . Although our society as a whole may have the ability to adequately bounce back from pandemic effects, there are vulnerable people who have been affected more than others.
First, women have consistently reported larger increases in mental health problems in response to the COVID-19 pandemic than men 13 , 15 , 29 , 40 , with meta-analytic effect sizes being 44% 15 to 75% 13 higher. This could reflect both higher stress vulnerability or larger daily life disruptions due to, for example, increased childcare responsibilities, exposure to home violence or greater economic impact due to employment disruptions that all disproportionately fell to women 41 , thereby exacerbating the already existing pre-pandemic gender inequalities in depression and anxiety levels. In addition, adolescents and young adults have been disproportionately affected compared to younger children and older adults 12 , 15 , 29 , 40 . This may be the result of unfavorable behavioral and social changes (for example, school closure periods 42 ) during a crucial development phase where social interactions outside the family context are pivotal. Alarmingly, even though suicide rates did not seem to increase at the population level, studies in China 43 and Japan 44 indicated significant increases in suicide rates in children and adolescents.
Existing socio-cultural disparities in mental health may have further widened during the COVID pandemic. Whether the impact is larger for individuals with low socio-economic status remains unclear, with contrasting meta-analyses pointing toward this group being protected 15 or at increased risk 40 . Earlier meta-analyses did not find that the mental health impact of COVID-19 differed across Europe, North America, Asia and Oceania 13 , 14 , but data are lacking from Africa and South America. Nevertheless, a large-scale within-country comparison in the United States found that the mental health of Black, Hispanic and Asian respondents worsened relatively more during the pandemic compared to White respondents. Moreover, White respondents were more likely to receive professional mental healthcare during the pandemic, and, conversely, Black, Hispanic, and Asian respondents demonstrated higher levels of unmet mental healthcare needs during this time 45 .
People with pre-existing somatic conditions represent another vulnerable group in which the pandemic had a greater impact (pooled effect size of 0.25) 13 . This includes people with conditions such as epilepsy, multiple sclerosis or cardiometabolic disease as well as those with multiple comorbidities. The disproportionate impact may reflect this groupʼs elevated COVID-19 risk and, consequently, more perceived stress and fear of infection, but it could also reflect disruptions of regular healthcare services.
Healthcare workers faced increased workload, rapidly changing and challenging work environments and exposure to infections and death, accompanied by fear of infecting themselves and their families. High prevalences of (subthreshold) depression (13% 46 ), depressive symptoms (31% 47 ), (subthreshold) anxiety (16% 46 ), anxiety symptoms (23% 47 ) and post-traumatic stress disorder (~22% 46 , 47 ) have been reported in healthcare workers. However, a meta-analysis did not find a larger mental health impact of the pandemic as compared to the general population 40 , and another meta-analysis (of 206 studies) found that the mental health status of healthcare workers was similar to or even better than that of the general population during the first COVID year 48 . However, it is important to note that these meta-analyses could not differentiate between frontline and non-frontline healthcare workers.
Finally, individuals with pre-existing mental disorders may be at increased risk for exacerbation of mental ill-health during the pandemic, possibly due to disease history—illustrating a higher genetic and/or environmental vulnerability—but also due to discontinuity of mental healthcare. Already before the pandemic, mental health systems were under-resourced and disorganized in most countries 6 , 49 , but a third of all WHO member states reported disruptions to mental and substance use services during the first 18 months of the pandemic 50 , with reduced, shortened or postponed appointments and limited capacity for acute inpatient admissions 51 , 52 . Despite this, there is no clear evidence that individuals with pre-existing mental disorders are disproportionately affected by pandemic-related societal disruptions; the effect size for pandemic impact on self-reported mental health problems was similar in psychiatric patients and the general population 13 . In the United States, emergency visits for ten different mental disorders were generally stable during the pandemic compared to earlier periods 53 . In a large Dutch study 22 , 54 with multiple pre-pandemic and during-pandemic assessments, there was no difference in symptom increase among patients relative to controls (see Fig. 1 for illustration). In absolute terms, however, it is important to note that psychiatric patients show much higher symptom levels of depression, anxiety, loneliness and COVID-fear than healthy controls. Again, variation in mental health changes during the pandemic is large: next to psychiatric patients who showed symptom decrease due to, for example, experiencing relief from social pressures, there certainly have been many patients with symptom increases and relapses during the pandemic.
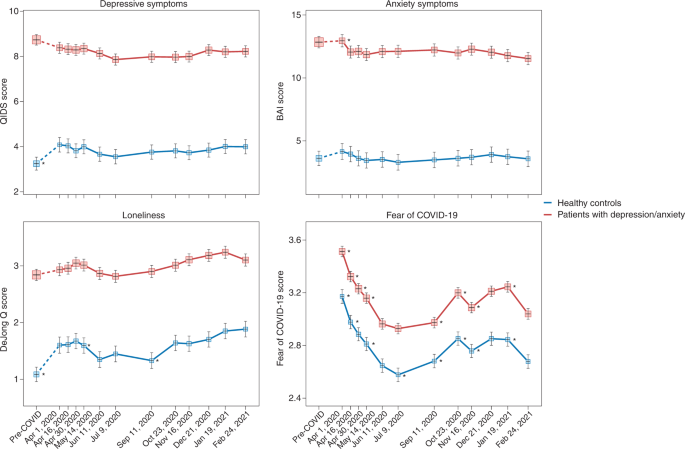
Trajectories of mean depressive symptoms (QIDS score), anxiety symptoms (BAI score), loneliness (De Jong questionnaire score) and Fear of COVID-19 score before and during the first year of the COVID-19 pandemic in healthy controls (blue line, n = 378) and in patients with depressive and/or anxiety disorders (red line, n = 908). The x -axis indicates time with one pre-COVID assessment (averaged over up to five earlier assessments conducted between 2006 and 2019) and 11 online assessments during April 2020 through February 2021. Symbols indicate the mean score during the assessment with 95% CIs. As compared to pre-COVID assessment scores, the figure shows a statistically significant increase of depression and loneliness symptoms during the first pandemic peak (April 2020) in healthy controls but not in patients (for more details, see refs. 22 , 54 ). Asterisks indicate where subsequent wave scores differ from the prior wave scores ( P < 0.05). The figure also illustrates the stability of depressive and anxiety symptoms during the first COVID year, a significant increase in loneliness during this period and fluctuations of Fear of COVID-19 score that positively correlate with infection rates in the Netherlands. Raw data are from the Netherlands Study of Depression and Anxiety (NESDA), which were re-analyzed for the current plots to illustrate differences between two groups (healthy controls versus patients). BAI, Beck Anxiety Inventory; QIDS, Quick Inventory of Depressive Symptoms.
Impact of COVID-19 infection and disease on mental health and the brain
Not only the pandemic but also COVID-19 itself can have severe impact on the mental health of affected individuals and, thus, of the population at large. Below we describe acute and post-acute neuropsychiatric sequelae seen in patients with COVID-19 and link these to neurobiological mechanisms.
Neuropsychiatric sequelae in individuals with COVID-19
Common symptoms associated with acute SARS-CoV-2 infection include headache, anosmia (loss of sense of smell) and dysgeusia (loss of sense of taste). The broader neuropsychiatric impact is dependent on infection severity and is very heterogeneous (Table 2 ). It ranges from no neuropsychiatric symptoms among the large group of asymptomatic COVID-19 cases to milder transient neuropsychiatric symptoms, such as fatigue, sleep disturbance and cognitive impairment, predominantly occurring among symptomatic patients with COVID-19 (ref. 55 ). Cognitive impairment consists of sustained memory impairments and executive dysfunction, including short-term memory loss, concentration problems, word-finding problems and impaired daily problem-solving, colloquially termed ‘brain fog’ by patients and clinicians. A small number of infected individuals become severely ill and require hospitalization. During hospital admission, the predominant neuropsychiatric outcome is delirium 56 . Delirium occurs among one-third of hospitalized patients with COVID-19 and among over half of patients with COVID-19 who require intensive care unit (ICU) treatment. These delirium rates seem similar to those observed among individuals with severe illness hospitalized for other general medical conditions 57 . Delirium is associated with neuropsychiatric sequalae after hospitalization, as part of post-intensive care syndrome 58 , in which sepsis and inflammation are associated with cognitive dysfunction and an increased risk of a broad range of psychiatric symptoms, from anxiety to depression and psychotic symptoms with hallucinations 59 , 60 .
A subset of patients with COVID-19 develop PACS 61 , which can include neuropsychiatric symptoms. A large meta-analysis summarizes 51 studies involving 18,917 patients with a mean follow-up of 77 days (range, 14–182 days) 62 . The most prevalent neuropsychiatric symptom associated with COVID-19 was sleep disturbance, with a pooled prevalence of 27.4%, followed by fatigue (24.4%), cognitive impairment (20.2%), anxiety symptoms (19.1%), post-traumatic stress symptoms (15.7%) and depression symptoms (12.9%) (Table 2 ). Another meta-analysis that assessed patients 12 weeks or more after confirmed COVID-19 diagnosis found that 32% experienced fatigue, and 22% experienced cognitive impairment 63 . To what extent neuropsychiatric symptoms are truly unique for patients with COVID remains unclear from these meta-analyses, as hardly any study included well-matched controls with other types of respiratory infections or inflammatory conditions.
Studies based on electronic health records have examined whether higher levels of neuropsychiatric symptoms truly translate into a higher incidence of clinically overt mental disorders 64 , 65 . In a 1-year follow-up using the US Veterans Affairs database, 153,848 survivors of SARS-CoV-2 infection exhibited an increased incidence of any mental disorder with a relative risk of 1.46 and, specifically, 1.35 for anxiety disorders, 1.39 for depressive disorders and 1.38 for stress and adjustment disorders, compared to a contemporary group and a historical control group ( n = 5,859,251) 65 . In absolute numbers, the incident risk difference attributable to SARS-CoV-2 for mental disorders was 64 per 1,000 individuals. Taquet et al. 64 analyzed electronic health records from the US-based TriNetX network with over 81 million patients and 236,379 COVID-19 survivors followed for 6 months. In absolute numbers, 6-month incidence of hospital contacts related to diagnoses of anxiety, affective disorder or psychotic disorder was 7.0%, 4.5% and 0.4%, respectively. Risks of incident neurological or psychiatric diagnoses were directly correlated with COVID-19 severity and increased by 78% when compared to influenza and by 32% when compared to other respiratory tract infections. In contrast, a medical record study involving 8.3 million adults confirmed that neuropsychiatric disorders were significantly elevated among COVID-19 hospitalized individuals but to a similar extent as in hospitalized patients with other severe respiratory disease 66 . In line with this, a study using language processing of clinical notes in electronic health records did not find an increase in fatigue, mood and anxiety symptoms among COVID-19 hospitalized individuals when compared to hospitalized patients for other indications and adjusted for sociodemographic features and hospital course 67 . It is important to note that research based only on hospital records might be influenced by increased health-seeking behavior that could be differential across care settings or by increased follow-up by hospitals of patients with COVID-19 (compared to patients with other conditions).
Consequently, whether PACS symptoms form a unique pattern due to specific infection with SARS-CoV-2 remains debatable. Prospective case–control studies that do not rely on hospital records but measure the incidence of neuropsychiatric symptoms and diagnoses after COVID-19 are still scarce, but they are critical for distinguishing causation and confounding when characterizing PACS and the uniqueness of neuropsychiatric sequalae after COVID-19 (ref. 68 ). Recent studies with well-matched control groups illustrate that long-term consequences may not be so unique, as they were similar to those observed in patients with other diseases of similar severity, such as after acute myocardial infarction or in ICU patients 56 , 66 . A first prospective follow-up study of COVID-19 survivors and control patients matched on disease severity, age, sex and ICU admission found similar neuropsychiatric outcomes, regarding both new-onset psychiatric diagnosis (19% versus 20%) and neuropsychiatric symptoms (81% versus 93%). However, moderate but significantly worse cognitive outcomes 6 months after symptom onset were found among survivors of COVID-19 (ref. 69 ). In line with this, a longitudinal study of 785 participants from the UK Biobank showed small but significant cognitive impairment among individuals infected with SARS-CoV-2 compared to matched controls 70 .
Numerous psychosocial mechanisms can lead to neuropsychiatric sequalae of COVID-19, including functional impairment; psychological impact due to, for example, fear of dying; stress of being infected with a novel pandemic disease; isolation as part of quarantine and lack of social support; fear/guilt of spreading COVID-19 to family or community; and socioeconomic distress by lost wages 71 . However, there is also ample evidence that neurobiological mechanisms play an important role, which is discussed below.
Neurobiological mechanisms underlying neuropsychiatric sequelae of COVID-19
Acute neuropsychiatric symptoms among patients with severe COVID-19 have been found to correlate with the level of serum inflammatory markers 72 and coincide with neuroimaging findings of immune activation, including leukoencephalopathy, acute disseminated encephalomyelitis, cytotoxic lesions of the corpus callosum or cranial nerve enhancement 73 . Rare presentations, including meningitis, encephalitis, inflammatory demyelination, cerebral infarction and acute hemorrhagic necrotizing encephalopathy, have also been reported 74 . Hospitalized patients with frank encephalopathies display impaired blood-brain barrier (BBB) integrity with leptomeningeal enhancement on brain magnetic resonance images 75 . Studies of postmortem specimens from patients who succumbed to acute COVID-19 reveal significant neuropathology with signs of hypoxic damage and neuroinflammation. These include evidence of BBB permeability with extravasation of fibrinogen, microglial activation, astrogliosis, leukocyte infiltration and microhemorrhages 76 , 77 . However, it is still unclear to what extent these findings differ from patients with similar illness severity due to acute non-COVID illness, as these brain effects might not be virus-specific effects but rather due to cytokine-mediated neuroinflammation and critical illness.
Post-acute neuroimaging studies in SARS-CoV-2-recovered patients, as compared to control patients without COVID-19, reveal numerous alterations in brain structure on a group level, although effect sizes are generally small. These include minor reduction in gray matter thickness in the various regions of the cortex and within the corpus collosum, diffuse edema, increases in markers of tissue damage in regions functionally connected to the olfactory cortex and reductions in overall brain size 70 , 78 . Neuroimaging studies of post-acute COVID-19 patients also report abnormalities consistent with micro-structural and functional alterations, specifically within the hippocampus 79 , 80 , a brain region critical for memory formation and regulating anxiety, mood and stress responses, but also within gray matter areas involving the olfactory system and cingulate cortex 80 . Overall, these findings are in line with ongoing anosmia, tremors, affect problems and cognitive impairment.
Interestingly, despite findings mentioned above, there is little evidence of SARS-CoV-2 neuroinvasion with productive replication, and viral material is rarely found in the central nervous system (CNS) of patients with COVID-19 (refs. 76 , 77 , 81 ). Thus, neurobiological mechanisms of SARS-CoV-2-mediated neuropsychiatric sequelae remain unclear, especially in patients who initially present with milder forms of COVID-19. Symptomatic SARS-CoV-2 infection is associated with hypoxia, cytokine release syndrome (CRS) and dysregulated innate and adaptive immune responses (reviewed in ref. 82 ). All these effects could contribute to neuroinflammation and endothelial cell activation (Fig. 2 ). Examination of cerebrospinal fluid in patients with neuroimaging findings revealed elevated levels of pro-inflammatory, BBB-destabilizing cytokines, including interleukin-6 (IL-6), IL-1, IL-8 and mononuclear cell chemoattractants 83 , 84 . Whether these cytokines arise from the periphery, due to COVID-19-mediated CRS, or from within the CNS, is unclear. As studies generally lack control patients with other severe illnesses, the specificity of such findings to SARS-CoV-2 also remains unclear. Systemic inflammatory processes, including cytokine release, have been linked to glial activation with expression of chemoattractants that recruit immune cells, leading to neuroinflammation and injury 85 . Cerebrospinal fluid concentrations of neurofilament light, a biomarker of neuronal damage, were reportedly elevated in patients hospitalized with COVID-19 regardless of whether they exhibited neurologic diseases 86 . Acute thromboembolic events leading to ischemic infarcts are also common in patients with COVID-19 due to a potentially increased pro-coagulant process secondary to CRS 87 .
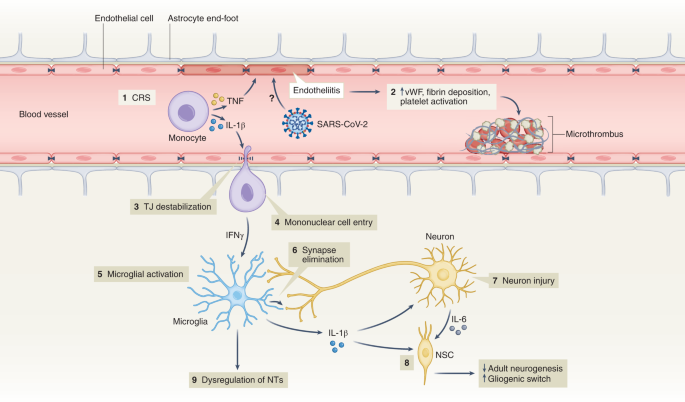
(1) Elevation of BBB-destabilizing cytokines (IL-1β and TNF) within the serum due to CRS or local interactions of mononuclear and endothelial cells. (2) Virus-induced endotheliitis increases susceptibility to microthrombus formation due to platelet activation, elevation of vWF and fibrin deposition. (3) Cytokine, mononuclear and endothelial cell interactions promote disruption of the BBB, which may allow entry of leukocytes expressing IFNg into the CNS (4), leading to microglial activation (5). (6) Activated microglia may eliminate synapses and/or express cytokines that promote neuronal injury. (7) Injured neurons express IL-6 which, together with IL-1β, promote a ‘gliogenic switch’ in NSCs (8), decreasing adult neurogenesis. (9) The combination of microglial (and possibly astrocyte) activation, neuronal injury and synapse loss may lead to dysregulation of NTs and neuronal circuitry. IFNg, interferon-g; NSC, neural stem cell; NT, neurotransmitter; TJ, tight junction; TNF, tumor necrosis factor; vWF, von Willebrand factor.
It is also unclear whether hospitalized patients with COVID-19 may develop brain abnormalities due to hypoxia or CRS rather than as a direct effect of SARS-CoV-2 infection. Hypoxia may cause neuronal dysfunction, cerebral edema, increased BBB permeability, cytokine expression and onset of neurodegenerative diseases 88 , 89 . CRS, with life-threatening levels of serum TNF-α and IL-1 (ref. 90 ) could also impact BBB function, as these cytokines destabilize microvasculature endothelial cell junctional proteins critical for BBB integrity 91 . In mild SARS-CoV-2 infection, circulating immune factors combined with mild hypoxia might impact BBB function and lead to neuroinflammation 92 , as observed during infection with other non-neuroinvasive respiratory pathogens 93 . However, multiple studies suggest that the SARS-CoV-2 spike protein itself may also induce venous and arterial endothelial cell activation and endotheliitis, disrupt BBB integrity or cross the BBB via adoptive transcytosis 94 , 95 , 96 .
Reducing neuropsychiatric sequelae of COVID-19
The increased risk of COVID-19-related neuropsychiatric sequalae was most pronounced during the first pandemic peak but reduced over the subsequent 2 years 64 , 97 . This may be due to reduced impact of newer SARS-CoV-2 strains (that is, Omicron) but also protective effects of vaccination, which limit SARS-CoV-2 spread and may, thus, prevent neuropsychiatric sequalae. Fully vaccinated individuals with breakthrough infections exhibit a 50% reduction in PACS 98 , even though vaccination does not improve PACS-related neuropsychiatric symptoms in patients with a prior history of COVID-19 (ref. 99 ). As patients with pre-existing mental disorders are at increased risk of SARS-CoV-2 infection, they deserve to be among the prioritization groups for vaccination efforts 100 .
Adequate treatment strategies for neuropsychiatric sequelae of COVID-19 are needed. As no specific evidence-based intervention yet exists, the best current treatment approach is that for neuropsychiatric sequelae arising after other severe medical conditions 101 . Stepped care—a staged approach of mental health services comprising a hierarchy of interventions, from least to most intensive, matched to the individual’s need—is efficacious with monitoring of mental health and cognitive problems. Milder symptoms likely benefit from counseling and holistic care, including physiotherapy, psychotherapy and rehabilitation. Individuals with moderate to severe symptoms fulfilling psychiatric diagnoses should receive guideline-concordant care for these disorders 61 . Patients with pre-existing mental disorders also deserve special attention when affected by COVID-19, as they have shown to have an increased risk of COVID-19-related hospitalization, complications and death 102 . This may involve interventions to address their general health, any unfavorable socioenvironmental factors, substance abuse or treatment adherence issues.
Lessons learned, knowledge gaps and future challenges
Ultimately, it is not only the millions of people who have died from COVID-19 worldwide that we remember but also the distress experienced during an unpredictable period with overstretched healthcare systems, lockdowns, school closures and changing work environments. In a world that is more and more globalized, connectivity puts us at risk for future pandemics. What can be learned from the last 2 years of the COVID-19 pandemic about how to handle future and longstanding challenges related to mental health?
Give mental health equal priority to physical health
The COVID-19 pandemic has demonstrated that our population seems quite resilient and adaptive. Nevertheless, even if society as a whole may bounce back, there is a large group of people whose mental health has been and will be disproportionately affected by this and future crises. Although various groups, such as the WHO 8 , the National Health Commission of China 103 , the Asia Pacific Disaster Mental Health Network 104 and a National Taskforce in India 105 , developed mental health policies early on, many countries were late in realizing that a mental health agenda deserves immediate attention in a rapidly evolving pandemic. Implementation of comprehensive and integrated mental health policies was generally inconsistent and suboptimal 106 and often in the shadow of policies directed at containing and reducing the spread of SARS-CoV-2. Leadership is needed to convey the message that mental health is as important as physical health and that we should focus specific attention and early interventions on those at the highest risk. This includes those vulnerable due to factors such as low socioeconomic status, specific developmental life phase (adolescents and young adults), pre-existing risk (poor physical or somatic health and early life trauma) or high exposure to pandemic-related (work) changes—for example, women and healthcare personnel. This means that not only should investment in youth and reducing health inequalities remain at the top of any policy agenda but also that mental health should be explicitly addressed from the start in any future global health crisis situation.
Communication and trust is crucial for mental health
Uncertainty and uncontrollability during the pandemic have challenged rational thinking. Negative news travels fast. Communication that is vague, one-sided and dishonest can negatively impact on mental health and amplify existing distress and anxiety 107 . Media reporting should not overemphasize negative mental health impact—for example, putative suicide rate increases or individual negative experiences—which could make situations worse than they actually are. Instead, communication during crises requires concrete and actionable advice that avoids polarization and strengthens vigilance, to foster resilience and help prevent escalation to severe mental health problems 108 , 109 .
Rapid research should be collaborative and high-quality
Within the scientific community, the topic of mental health during the pandemic led to a multitude of rapid studies that generally had limited methodological quality—for example, cross-sectional designs, small or selective sampling or study designs lacking valid comparison groups. These contributed rather little to our understanding of the mental health impact of the emerging crisis. In future events that have global mental health impact, where possible, collaborative and interdisciplinary efforts with well-powered and well-controlled prospective studies using standardized instruments will be crucial. Only with fine-grained determinants and outcomes can data reliably inform mental health policies and identify who is most at risk.
Do not neglect long-term mental health effects
So far, research has mainly focused on the acute and short-term effects of the pandemic on mental health, usually spanning pandemic effects over several months to 1 year. However, longer follow-up of how a pandemic impacts population mental health is essential. Can societal and economic disruptions after the pandemic increase risk of mental disorders at a later stage when the acute pandemic effects have subsided? Do increased self-reported mental health problems return to pre-pandemic levels, and which groups of individuals remain most affected in the long-term? We need to realize that certain pandemic consequences, particularly those affecting income and school/work careers, may become visible only over the course of several years. Consequently, we should maintain focus and continue to monitor and quantify the effects of the pandemic in the years to come—for example, by monitoring mental healthcare use and suicide. This should include specific at-risk populations (for example, adolescents) and understudied populations in low-income and middle-income countries.

Pay attention to mental health consequences of infectious diseases
Even though our knowledge on PACS is rapidly expanding, there are still many unanswered questions related to who is at risk, the long-term course trajectories and the best ways to intervene early. Consequently, we need to be aware of the neuropsychiatric sequelae of COVID-19 and, for that matter, of any infectious disease. Clinical attention and research should be directed toward alleviating potential neuropsychiatric ramifications of COVID-19. Next to clinical studies, studies using human tissues and appropriate animal models are pivotal to determine the CNS region-specific and neural-cell-specific effects of SARS-CoV-2 infection and the induced immune activation. Indeed, absence of SARS-CoV-2 neuroinvasion is an opportunity to learn and discover how peripheral neuroimmune mechanisms can contribute to neuropsychiatric sequelae in susceptible individuals. This emphasizes the importance of an interdisciplinary approach where somatic and mental health efforts are combined but also the need to integrate clinical parameters after infection with biological parameters (for example, serum, cerebrospinal fluid and/or neuroimaging) to predict who is at risk for PACS and deliver more targeted treatments.
Prepare mental healthcare infrastructure for pandemic times
If we take mental health seriously, we should not only monitor it but also develop the resources and infrastructure necessary for rapid early intervention, particularly for specific vulnerable groups. For adequate mental healthcare to be ready for pandemic times, primary care, community mental health and public mental health should be prepared. In many countries, health services were not able to meet the population’s mental health needs before the pandemic, which substantially worsened during the pandemic. We should ensure rapid access to mental health services but also address the underlying drivers of poor mental health, such as mitigating risks of unemployment, sexual violence and poverty. Collaboration in early stages across disciplines and expertise is essential. Anticipating disruption to face-to-face services, mental healthcare providers should be more prepared for consultations, therapy and follow-up by telephone, video-conferencing platforms and web applications 51 , 52 . The pandemic has shown that an inadequate infrastructure, pre-existing inequalities and low levels of technological literacy hindered the use and uptake of e-health, both in healthcare providers and in patients across different care settings. The necessary investments can ensure rapid upscaling of mental health services during future pandemics for those individuals with a high mental health need due to societal changes, government measures, fear of infection or infection itself.
Even though much attention has been paid to the physical health consequences of COVID-19, mental health has unjustly received less attention. There is an urgent need to prepare our research and healthcare infrastructures not only for adequate monitoring of the long-term mental health effects of the COVID-19 pandemic but also for future crises that will shape mental health. This will require collaboration to ensure interdisciplinary and sound research and to provide attention and care at an early stage for those individuals who are most vulnerable—giving mental health equal priority to physical health from the very start.
WHO Coronavirus (COVID-19) Dashboard (WHO, 2022; https://covid19.who.int/
Rando, H. M. et al. Challenges in defining long COVID: striking differences across literature, electronic health records, and patient-reported information. Preprint at https://www.medrxiv.org/content/10.1101/2021.03.20.21253896v1 (2021).
Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. 27 , 601–615 (2021).
Article CAS PubMed PubMed Central Google Scholar
Abbafati, C. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1204–1222 (2020).
Article Google Scholar
Penninx, B. W., Pine, D. S., Holmes, E. A. & Reif, A. Anxiety disorders. Lancet 397 , 914–927 (2021).
Article PubMed PubMed Central Google Scholar
Herrman, H. et al. Time for united action on depression: a Lancet –World Psychiatric Association Commission. Lancet 399 , 957–1022 (2022).
Article PubMed Google Scholar
Radka, K., Wyeth, E. H. & Derrett, S. A qualitative study of living through the first New Zealand COVID-19 lockdown: affordances, positive outcomes, and reflections. Prev. Med. Rep. 26 , 101725 (2022).
Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact (WHO, 2022).
Dragioti, E. et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 94 , 1935–1949 (2022).
Zhang, S. X. et al. Mental disorder symptoms during the COVID-19 pandemic in Latin America—a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 31 , e23 (2022).
Zhang, S. X. et al. Meta-analytic evidence of depression and anxiety in Eastern Europe during the COVID-19 pandemic. Eur. J. Psychotraumatol . 13 , 2000132 (2022).
Racine, N. et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 175 , 1142–1150 (2021).
Robinson, E., Sutin, A. R., Daly, M. & Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 296 , 567–576 (2022).
Article CAS PubMed Google Scholar
Prati, G. & Mancini, A. D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 51 , 201–211 (2021).
Patel, K. et al. Psychological distress before and during the COVID-19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Netw. Open 5 , e227629 (2022).
Ernst, M. et al. Loneliness before and during the COVID-19 pandemic: a systematic review with meta-analysis. Am. Psychol . 77 , 660–677 (2022).
Kilian, C. et al. Changes in alcohol use during the COVID-19 pandemic in Europe: a meta-analysis of observational studies. Drug Alcohol Rev . 41 , 918–931 (2022).
Acuff, S. F., Strickland, J. C., Tucker, J. A. & Murphy, J. G. Changes in alcohol use during COVID-19 and associations with contextual and individual difference variables: a systematic review and meta-analysis. Psychol. Addict. Behav. 36 , 1–19 (2022).
Varga, T. V. et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg. Health Eur . 2 , 100020 (2021).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8 , 141–149 (2021).
Jia, H. et al. National and state trends in anxiety and depression severity scores among adults during the COVID-19 pandemic—United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 70 , 1427–1432 (2021).
Kok, A. A. L. et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in Dutch case–control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J. Affect. Disord. 305 , 85–93 (2022).
Su, Y. et al. Prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic: a systematic review and meta-analysis. Int. Psychogeriatr. https://doi.org/10.1017/S1041610222000199 (2022).
Knox, L., Karantzas, G. C., Romano, D., Feeney, J. A. & Simpson, J. A. One year on: what we have learned about the psychological effects of COVID-19 social restrictions: a meta-analysis. Curr. Opin. Psychol. 46 , 101315 (2022).
Aknin, L. B. et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health 7 , e417–e426 (2022).
Lee, Y. et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J. Affect. Disord. 290 , 364–377 (2021).
Wu, J. T. et al. Nowcasting epidemics of novel pathogens: lessons from COVID-19. Nat. Med. 27 , 388–395 (2021).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 , 912–920 (2020).
Santomauro, D. F. et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398 , 1700–1712 (2021).
Knudsen, A. K. S. et al. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: a population-based repeated cross-sectional analysis. Lancet Reg. Health Eur . 4 , 100071 (2021).
Ayuso-Mateos, J. L. et al. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol. Psychiatr. Sci . 30 , e49 (2021).
Vloo, A. et al. Gender differences in the mental health impact of the COVID-19 lockdown: longitudinal evidence from the Netherlands. SSM Popul. Health 15 , 100878 (2021).
Winkler, P. et al. Prevalence of current mental disorders before and during the second wave of COVID-19 pandemic: an analysis of repeated nationwide cross-sectional surveys. J. Psychiatr. Res. 139 , 167–171 (2021).
Pirkis, J. et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 8 , 579–588 (2021).
Faust, J. S. et al. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic, March–August 2020. JAMA 326 , 84–86 (2021).
John, A. et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review. F1000Res. 9 , 1097 (2020).
Steeg, S. et al. Temporal trends in primary care-recorded self-harm during and beyond the first year of the COVID-19 pandemic: time series analysis of electronic healthcare records for 2.8 million patients in the Greater Manchester Care Record. EClinicalMedicine 41 , 101175 (2021).
Rømer, T. B. et al. Psychiatric admissions, referrals, and suicidal behavior before and during the COVID-19 pandemic in Denmark: a time-trend study. Acta Psychiatr. Scand. 144 , 553–562 (2021).
Holland, K. M. et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry 78 , 372–379 (2021).
Kunzler, A. M. et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health 17 , 34 (2021).
Flor, L. S. et al. Quantifying the effects of the COVID-19 pandemic on gender equality on health, social, and economic indicators: a comprehensive review of data from March, 2020, to September, 2021. Lancet 399 , 2381–2397 (2022).
Viner, R. et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: a systematic review. JAMA Pediatr. 176 , 400–409 (2022).
Zheng, X. Y. et al. Trends of injury mortality during the COVID-19 period in Guangdong, China: a population-based retrospective analysis. BMJ Open 11 , e045317 (2021).
Tanaka, T. & Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 5 , 229–238 (2021).
Thomeer, M. B., Moody, M. D. & Yahirun, J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J. Racial Ethn. Health Disparities https://doi.org/10.1007/s40615-021-01006-7 (2022).
Hill, J. E. et al. The prevalence of mental health conditions in healthcare workers during and after a pandemic: systematic review and meta-analysis. J. Adv. Nurs. 78 , 1551–1573 (2022).
Marvaldi, M., Mallet, J., Dubertret, C., Moro, M. R. & Guessoum, S. B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 126 , 252–264 (2021).
Phiri, P. et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine 34 , 100806 (2021).
Jorm, A. F., Patten, S. B., Brugha, T. S. & Mojtabai, R. Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry 16 , 90–99 (2017).
Third Round of the Global Pulse Survey on Continuity of Essential Health Services during the COVID-19 Pandemic (WHO, 2021).
Baumgart, J. G. et al. The early impacts of the COVID-19 pandemic on mental health facilities and psychiatric professionals. Int. J. Environ. Res. Public Health 18 , 8034 (2021).
Raphael, J., Winter, R. & Berry, K. Adapting practice in mental healthcare settings during the COVID-19 pandemic and other contagions: systematic review. BJPsych Open 7 , e62 (2021).
Anderson, K. N. et al. Changes and inequities in adult mental health-related emergency department visits during the COVID-19 pandemic in the US. JAMA Psychiatry 79 , 475–485 (2022).
Pan, K. Y. et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case–control cohorts. Lancet Psychiatry 8 , 121–129 (2021).
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W. & Kelley, K. W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. Neurosci. 9 , 46–56 (2008).
Nersesjan, V. et al. Central and peripheral nervous system complications of COVID-19: a prospective tertiary center cohort with 3-month follow-up. J. Neurol. 268 , 3086–3104 (2021).
Wilson, J. E. et al. Delirium. Nat. Rev. Dis. Prim . 6 , 90 (2020).
Rawal, G., Yadav, S. & Kumar, R. Post-intensive care syndrome: an overview. J. Transl. Intern. Med. 5 , 90–92 (2017).
Pandharipande, P. P. et al. Long-term cognitive impairment after critical illness. N. Engl. J. Med. 369 , 1306–1316 (2013).
Girard, T. D. et al. Long-term cognitive impairment after hospitalization for community-acquired pneumonia: a prospective cohort study. J. Gen. Intern. Med. 33 , 929–935 (2018).
Crook, H., Raza, S., Nowell, J., Young, M. & Edison, P. Long covid—mechanisms, risk factors, and management. BMJ 374 , n1648 (2021).
Badenoch, J. B. et al. Persistent neuropsychiatric symptoms after COVID-19: a systematic review and meta-analysis. Brain Commun . 4 , fcab297 (2021).
Ceban, F. et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav. Immun. 101 , 93–135 (2022).
Taquet, M., Geddes, J. R., Husain, M., Luciano, S. & Harrison, P. J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8 , 416–427 (2021).
Xie, Y., Xu, E. & Al-Aly, Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ 376 , e068993 (2022).
Kieran Clift, A. et al. Neuropsychiatric ramifications of severe COVID-19 and other severe acute respiratory infections. JAMA Psychiatry 79 , 690–698 (2022).
Castro, V. M., Rosand, J., Giacino, J. T., McCoy, T. H. & Perlis, R. H. Case–control study of neuropsychiatric symptoms following COVID-19 hospitalization in 2 academic health systems. Mol. Psych. (in the press).
Amin-Chowdhury, Z. & Ladhani, S. N. Causation or confounding: why controls are critical for characterizing long COVID. Nat. Med. 27 , 1129–1130 (2021).
Nersesjan, V. et al. Neuropsychiatric and cognitive outcomes in patients 6 months after COVID-19 requiring hospitalization compared with matched control patients hospitalized for non-COVID-19 illness. JAMA Psychiatry 79 , 486–497 (2022).
Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604 , 697–707 (2022).
Zhang, H. et al. Psychological experience of COVID-19 patients: a systematic review and qualitative meta-synthesis. Am. J. Infect. Control 50 , 809–819 (2022).
Mazza, M. G. et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 89 , 594–600 (2020).
Moonis, G. et al. The spectrum of neuroimaging findings on CT and MRI in adults With COVID-19. AJR Am. J. Roentgenol. 217 , 959–974 (2021).
Asadi-Pooya, A. A. & Simani, L. Central nervous system manifestations of COVID-19: a systematic review. J. Neurol. Sci . 413 , 116832 (2020).
Lersy, F. et al. Cerebrospinal fluid features in patients with Coronavirus Disease 2019 and neurological manifestations: correlation with brain magnetic resonance imaging findings in 58 patients. J. Infect. Dis. 223 , 600–609 (2021).
Thakur, K. T. et al. COVID-19 neuropathology at Columbia University Irving Medical Center/New York Presbyterian Hospital. Brain 144 , 2696–2708 (2021).
Cosentino, G. et al. Neuropathological findings from COVID-19 patients with neurological symptoms argue against a direct brain invasion of SARS-CoV-2: a critical systematic review. Eur. J. Neurol. 28 , 3856–3865 (2021).
Tian, T. et al. Long-term follow-up of dynamic brain changes in patients recovered from COVID-19 without neurological manifestations. JCI Insight 7 , e155827 (2022).
Lu, Y. et al. Cerebral micro-structural changes in COVID-19 patients—an MRI-based 3-month follow-up study. EClinicalMedicine 25 , 100484 (2020).
Qin, Y. et al . Long-term microstructure and cerebral blood flow changes in patients recovered from COVID-19 without neurological manifestations. J. Clin. Invest . 131 , e147329 (2021).
Matschke, J. et al. Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 19 , 919–929 (2020).
Shivshankar, P. et al. SARS-CoV-2 infection: host response, immunity, and therapeutic targets. Inflammation 45 , 1430–1449 (2022).
Manganotti, P. et al. Cerebrospinal fluid and serum interleukins 6 and 8 during the acute and recovery phase in COVID-19 neuropathy patients. J. Med. Virol. 93 , 5432–5437 (2021).
Farhadian, S. et al. Acute encephalopathy with elevated CSF inflammatory markers as the initial presentation of COVID-19. BMC Neurol . 20 , 248 (2020).
Francistiová, L. et al. Cellular and molecular effects of SARS-CoV-2 linking lung infection to the brain. Front. Immunol . 12 , 730088 (2021).
Paterson, R. W. et al. Serum and cerebrospinal fluid biomarker profiles in acute SARS-CoV-2-associated neurological syndromes. Brain Commun . 3 , fcab099 (2021).
Cryer, M. J. et al. Prothrombotic milieu, thrombotic events and prophylactic anticoagulation in hospitalized COVID-19 positive patients: a review. Clin. Appl. Thromb. Hemost . 28 , 10760296221074353 (2022).
Nalivaeva, N. N. & Rybnikova, E. A. Editorial: Brain hypoxia and ischemia: new insights into neurodegeneration and neuroprotection. Front. Neurosci . 13 , 770 (2019).
Brownlee, N. N. M., Wilson, F. C., Curran, D. B., Lyttle, N. & McCann, J. P. Neurocognitive outcomes in adults following cerebral hypoxia: a systematic literature review. NeuroRehabilitation 47 , 83–97 (2020).
Del Valle, D. M. et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 26 , 1636–1643 (2020).
Daniels, B. P. et al. Viral pathogen-associated molecular patterns regulate blood–brain barrier integrity via competing innate cytokine signals. mBio 5 , e01476-14 (2014).
Reynolds, J. L. & Mahajan, S. D. SARS-COV2 alters blood brain barrier integrity contributing to neuro-inflammation. J. Neuroimmune Pharmacol. 16 , 4–6 (2021).
Bohmwald, K., Gálvez, N. M. S., Ríos, M. & Kalergis, A. M. Neurologic alterations due to respiratory virus infections. Front. Cell. Neurosci . 12 , 386 (2018).
Khaddaj-Mallat, R. et al. SARS-CoV-2 deregulates the vascular and immune functions of brain pericytes via spike protein. Neurobiol. Dis . 161 , 105561 (2021).
Qian, Y. et al. Direct activation of endothelial cells by SARS-CoV-2 nucleocapsid protein is blocked by simvastatin. J Virol. 95 , e0139621 (2021).
Rhea, E. M. et al. The S1 protein of SARS-CoV-2 crosses the blood–brain barrier in mice. Nat. Neurosci. 24 , 368–378 (2021).
Magnúsdóttir, I. et al. Acute COVID-19 severity and mental health morbidity trajectories in patient populations of six nations: an observational study. Lancet Public Health 7 , e406–e416 (2022).
Antonelli, M. et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case–control study. Lancet Infect. Dis. 22 , 43–55 (2022).
Wisnivesky, J. P. et al. Association of vaccination with the persistence of post-COVID symptoms. J. Gen. Intern. Med . 37 , 1748–1753 (2022).
De Picker, L. J. et al. Severe mental illness and European COVID-19 vaccination strategies. Lancet Psychiatry 8 , 356–359 (2021).
Cohen, G. H. et al. Comparison of simulated treatment and cost-effectiveness of a stepped care case-finding intervention vs usual care for posttraumatic stress disorder after a natural disaster. JAMA Psychiatry 74 , 1251–1258 (2017).
Vai, B. et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry 8 , 797–812 (2021).
Xiang, Y. T. et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7 , 228 (2020).
Newnham, E. A. et al. The Asia Pacific Disaster Mental Health Network: setting a mental health agenda for the region. Int. J. Environ. Res. Public Health 17 , 6144 (2020).
Article CAS PubMed Central Google Scholar
Dandona, R. & Sagar, R. COVID-19 offers an opportunity to reform mental health in India. Lancet Psychiatry 8 , 9–11 (2021).
Qiu, D. et al. Policies to improve the mental health of people influenced by COVID-19 in China: a scoping review. Front. Psychiatry 11 , 588137 (2020).
Su, Z. et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Global Health 17 , 4 (2021).
Petersen, M. B. COVID lesson: trust the public with hard truths. Nature 598 , 237 (2021).
van der Bles, A. M., van der Linden, S., Freeman, A. L. J. & Spiegelhalter, D. J. The effects of communicating uncertainty on public trust in facts and numbers. Proc. Natl Acad. Sci. USA 117 , 7672–7683 (2020).
Titze-de-Almeida, R. et al. Persistent, new-onset symptoms and mental health complaints in Long COVID in a Brazilian cohort of non-hospitalized patients. BMC Infect. Dis. 22 , 133 (2022).
Carfì, A., Bernabei, R. & Landi, F. Persistent symptoms in patients after acute COVID-19. JAMA 324 , 603–605 (2020).
Bliddal, S. et al. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Sci. Rep. 11 , 13153 (2021).
Kim, Y. et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect. Dis . 22 , 93 (2022).
Download references
Acknowledgements
The authors thank E. Giltay for assistance on data analyses and production of Fig. 1 . B.W.J.H.P. discloses support for research and publication of this work from the European Union’s Horizon 2020 research and innovation programme-funded RESPOND project (grant no. 101016127).
Author information
Authors and affiliations.
Department of Psychiatry, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands
Brenda W. J. H. Penninx & Christiaan H. Vinkers
Amsterdam Public Health, Mental Health Program and Amsterdam Neuroscience, Mood, Anxiety, Psychosis, Sleep & Stress Program, Amsterdam, The Netherlands
Biological and Precision Psychiatry, Copenhagen Research Center for Mental Health, Mental Health Center Copenhagen, Copenhagen University Hospital, Copenhagen, Denmark
Michael E. Benros
Department of Immunology and Microbiology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark
Departments of Medicine, Pathology & Immunology and Neuroscience, Center for Neuroimmunology & Neuroinfectious Diseases, Washington University School of Medicine, St. Louis, MO, USA
Robyn S. Klein
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Brenda W. J. H. Penninx .
Ethics declarations
Competing interests.
The authors declare no conflicts of interest.
Peer review
Peer review information.
Nature Medicine thanks Jane Pirkis and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Penninx, B.W.J.H., Benros, M.E., Klein, R.S. et al. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med 28 , 2027–2037 (2022). https://doi.org/10.1038/s41591-022-02028-2
Download citation
Received : 06 June 2022
Accepted : 26 August 2022
Published : 03 October 2022
Issue Date : October 2022
DOI : https://doi.org/10.1038/s41591-022-02028-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Mental health disturbance in preclinical medical students and its association with screen time, sleep quality, and depression during the covid-19 pandemic.
- Tjhin Wiguna
- Valerie Josephine Dirjayanto
- Erik Kinzie
BMC Psychiatry (2024)
Protocol for a pilot cluster randomised controlled trial of a multicomponent sustainable return to work IGLOo intervention
- Oliver Davis
- Jeremy Dawson
- Fehmidah Munir
Pilot and Feasibility Studies (2024)
Impact of COVID-19 first wave on the mental health of healthcare workers in a Front-Line Spanish Tertiary Hospital: lessons learned
- Juan D. Molina
- Franco Amigo
- Gabriel Rubio
Scientific Reports (2024)
Long-term risk of psychiatric disorder and psychotropic prescription after SARS-CoV-2 infection among UK general population
- Daniel Prieto-Alhambra
Nature Human Behaviour (2024)
Possible temporal relationship between SARS-CoV-2 infection and anti-NMDA receptor encephalitis: a meta-analysis
- Veronika Vasilevska
- Paul C. Guest
- Johann Steiner
Translational Psychiatry (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Loading metrics
Open Access
Peer-reviewed
Research Article
Identifying the impact of COVID-19 on health systems and lessons for future emergency preparedness: A stakeholder analysis in Kenya
Contributed equally to this work with: Dosila Ogira, Ipchita Bharali, Joseph Onyango
Roles Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing
* E-mail: [email protected] (DO); [email protected] (IB)
Affiliation Institute of Healthcare Management, Strathmore Business School, Strathmore University, Nairobi, Kenya
Roles Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing
Affiliation Center for Policy Impact in Global Health, Duke Global Health Institute, Duke University, Durham, North Carolina, United States of America
Roles Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing
Roles Methodology, Supervision, Validation, Writing – review & editing
Roles Project administration, Validation, Writing – review & editing
Roles Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing – review & editing
Roles Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing
- Dosila Ogira,
- Ipchita Bharali,
- Joseph Onyango,
- Wenhui Mao,
- Kaci Kennedy McDade,
- Gilbert Kokwaro,
- Gavin Yamey

- Published: December 21, 2022
- https://doi.org/10.1371/journal.pgph.0001348
- Peer Review
- Reader Comments
The coronavirus pandemic (COVID-19) has triggered a public health and economic crisis in high and low resource settings since the beginning of 2020. With the first case being discovered on 12 th March 2020, Kenya has responded by using health and non-health strategies to mitigate the direct and indirect impact of the disease on its population. However, this has had positive and negative implications for the country’s overall health system. This paper aimed to understand the pandemic’s impact and develop lessons for future response by identifying the key challenges and opportunities Kenya faced during the pandemic. We conducted a qualitative study with 15 key informants, purposefully sampled for in-depth interviews from September 2020 to February 2021. We conducted direct content analysis of the transcripts to understand the stakeholder’s views and perceptions of how COVID-19 has affected the Kenyan healthcare system. Most of the respondents noted that Kenya’s initial response was relatively good, especially in controlling the pandemic with the resources it had at the time. This included relaying information to citizens, creating technical working groups and fostering multisectoral collaboration. However, concerns were raised regarding service disruption and impact on reproductive health, HIV, TB, and non-communicable diseases services; poor coordination between the national and county governments; shortage of personal protective equipment and testing kits; and strain of human resources for health. Effective pandemic preparedness for future response calls for improved investments across the health system building blocks, including; human resources for health, financing, infrastructure, information, leadership, service delivery and medical products and technologies. These strategies will help build resilient health systems and improve self-reliance, especially for countries transitioning from donor aid such as Kenya in the event of a pandemic.
Citation: Ogira D, Bharali I, Onyango J, Mao W, McDade KK, Kokwaro G, et al. (2022) Identifying the impact of COVID-19 on health systems and lessons for future emergency preparedness: A stakeholder analysis in Kenya. PLOS Glob Public Health 2(12): e0001348. https://doi.org/10.1371/journal.pgph.0001348
Editor: Veena Sriram, The University of British Columbia, CANADA
Received: February 28, 2022; Accepted: November 10, 2022; Published: December 21, 2022
Copyright: © 2022 Ogira et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: This paper has included all the data used in the analysis.
Funding: This study is part of the ongoing project “Driving health progress during disease, demographic, domestic finance and donor transitions (the “4Ds”): policy analysis and engagement with six transitioning countries”, under the project award No. OPP1199624, funded by The Bill and Melinda Gates Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared no competing interests.
Introduction
Since the beginning of 2020, the COVID-19 pandemic has spread rapidly worldwide, causing devastating consequences for patients, health care workers, health systems, and economies [ 1 ]. As of January 14 th 2022, more than 318 million cases had been confirmed and more than 5.5 million deaths were recorded worldwide [ 2 ]. Out of this, the African continent recorded 10,201,488 cases of COVID-19 and 232,770 deaths [ 3 ]. This represents approximately 3% of the total cases worldwide. In a bid to protect the population and mitigate the impact of COVID-19 infection, various efforts have made in research and development of vaccines, several of which have since been rolled out [ 4 , 5 ]. With over 11.9 billion doses administered worldwide, 817 million doses were received in Africa out of which 577.8 million were issued as of May 2022 [ 2 , 6 ].
The pandemic has put considerable strain on national health systems worldwide, including in relatively highly resourced settings [ 1 , 7 ]. For instance, high-income countries (HICs), including those in Asia, Europe and North America recorded initial high morbidity and mortality rates [ 8 ]. This resulted in a surge in hospitalization rates, which saw the strain of healthcare workers and healthcare infrastructure, shortages in medication believed to alleviate COVID-19 symptoms and personal protective equipment (PPEs) [ 9 – 11 ].
The COVID-19 pandemic has also had profound consequences for resource-poor settings in low- and middle-income countries, including African countries [ 12 ]. The region is challenged by limited access to safe water and sanitation facilities, urban crowding and a large informal economy, creating added health risks [ 13 ]. Additionally, vulnerabilities in the health care system including, scarcity of resources such as oxygen and poor health infrastructure in the region create multiple health challenges in the era of the COVID-19 pandemic [ 14 ]. Many countries in Sub-Saharan Africa are also donor dependent. Large segments of their health systems are financed through external donors, leading to difficult trade-offs about interventions to prioritize [ 15 – 17 ]. In a bid to control infections, initial mitigation measures aimed at limiting the movement of people through lockdowns and quarantines were put in place. However, these policy directions also affected the access to other health services such as HIV, tuberculosis (TB), and malaria reversing the gains made in curbing these diseases [ 18 ].
COVID-19 in Kenya
Kenya reported its first case of COVID-19 on 12 th March 2020 [ 19 ]. Since then, the numbers have risen and as of January 16, 2022, almost two years after the confirmation of the first case, Kenya had recorded 317,634 cases and 5,488 deaths [ 20 ]. Like most countries globally, Kenya embarked on a countrywide vaccination program on March 5, 2021 [ 21 ]. As of January 16, 2022, the country had administered over 11 million vaccinations with the Country’s capital Nairobi presenting the highest percentage uptake of 36% [ 20 ].
Throughout the COVID-19 pandemic, the Kenyan government has responded through various health and non-health strategies to mitigate the impact of the pandemic on its population [ 22 , 23 ]. Some of the public health and socio-economic policies included; establishing the National Emergency Response Committee, international travel ban, closure of schools and workplaces, dawn to dusk curfew, provision of food aid, tax relief, and expansion of health insurance for healthcare workers [ 24 – 27 ]. Based on the Oxford Coronavirus Government Response Tracker, a composite measure of nine metrics calculating the stringency index of policy measures undertaken by countries to control the COVID-19 pandemic [ 28 ], Kenya’s responses were considered moderate at the beginning. However, the measures progressively became high, peaking at 93.52 out of 100 from early May 2020 to late June 2020 with an increase in the number of cases [ 29 ].
Despite the government of Kenya putting the mitigation measures in place, concerns were raised over their effectiveness. For instance, due to the physical distancing measures, some groups were disproportionately affected including; those living in informal settlements, pregnant mothers, school going children, persons living with disability among others [ 30 – 34 ]. Additionally, cases of misappropriation of funds designated for COVID-19 were witnessed. This was believed to have a ripple effect, including crippling the country’s ability to acquire sufficient medical supplies and employ an adequate number of human resources for health [ 35 , 36 ].
Although major strides have since been made in fighting the COVID-19 pandemic with the development of vaccines, various lessons have been learnt for long-term health system strengthening to build resilience, including; global collaboration in crisis response, surveillance, stockpiling, health work force surge capacity, among other measures [ 37 – 39 ]. While diverse frameworks have been used to evaluate health system strengthening practices by countries, we adopted the Word Health Organization (WHO) health system building block framework to present the Kenyan case [ 40 ]. The framework outlines the interaction across the core components of the health system and has been widely applied for crisis response [ 41 – 43 ]. This study aimed to understand the key measures adopted in Kenya to tackle the COVID-19 pandemic, how the pandemic impacted the health sector and the population more broadly, and how future policy priorities and health emergency preparedness can be strengthened through the lessons learnt from the COVID-19 pandemic response.
Study setting and participants
We used purposive sampling to identify Kenya stakeholders from different national and county fields [ 44 ]. This included those who had a firm understanding of how the COVID-19 pandemic has affected the Kenyan healthcare system and were willing to take part in the study. A total of 15 virtual interviews were conducted with key informants, out of which, 5 represented government institutions (3 from the national level and 2 from the regional level), 3 represented donors and development partners, 5 representatives from healthcare professionals (3 providers and 2 from professional bodies) and 2 representatives from non-governmental organizations (NGO) and civil society organizations (CSO), respectively.
Study design and data collection
The study used a qualitative cross-sectional design. We conducted 15 in-depth interviews using a semi-structured interview guide ( S1 Appendix ) which was developed to ensure that the desired area of inquiry was covered during individual interview sessions and to aid comparability of information obtained across the respondents. The interviews were conducted virtually between September 2020 and February 2021 by two research members of the team (JO and GK) with experience in conducting qualitative interviews. All supplementary notes were taken by one researcher (DO). All interviews were conducted in English and took an average of one hour. Interviews were recorded after obtaining oral consent from respondents.
Data management and analysis
All interviews were transcribed and coded for analysis using NVivo software. Data analysis was done using the Framework approach [ 45 ]. Deductive content analysis was used for this study. We started with the WHO building blocks framework to guide the analysis and further modified it based on findings to develop new themes not covered by the framework but mentioned in interviews. One researcher (DO) initially read through all the transcripts, line by line to develop an initial coding framework with input from (JO). This was then shared with (IB) who read through and double coded five transcripts, selected across the participant’s category to refine the coding framework. With input from other study team members (GY, GK, WM, KKM), the differences in the coding framework were then reconciled and coding was done on the themes and sub-themes identified in the final framework. Two researchers (DO and IB) then applied the final coding framework to present results, which were then reviewed by the other study team members (GY, GK, JO, WM, KKM). The data was stored in a password protected shared directory on the Strathmore server based on Strathmore University ICT data protection policy. Additionally, since the study was collaborative research with Duke University, it approved data back up and sharing by Duke IT Security Offices. All personal identifiers were removed from the dataset prior to archiving in the Duke University data repository.
Ethical approval and consideration
Ethical approval was obtained from Strathmore University’s Institutional Review Board (0891/20) and the Duke University Campus Institutional Review Board (2019–0366). Informed consent was sought from participants send in advance through email. Since all the interviews were done virtually, verbal informed consent was obtained from all the participants after providing information about the study and the potential benefits and risks of their involvement. The interviews were conducted virtually to mitigate the risk to participants due to the COVID-19 pandemic.
The stakeholders discussed various dimensions of the COVID response in Kenya and identified key challenges and opportunities for future preparedness and response efforts. While taking into account the WHO’s health systems building block framework [ 40 ], the findings are categorized into three broad themes: (1) Stakeholder perceptions on the country’s COVID-19 response, which captures the views on the adequacy of resources used and the measures taken by the government to effectively in fighting the COVID-19 pandemic; (2) Impact of the pandemic on Kenya’s health system and the population; (3) Opportunities to improve future pandemic preparedness and health system strengthening based on stakeholders’ recommendations.
Stakeholders’ perceptions on Kenya’s COVID-19 response
Provision of emergency supplies..
Majority of the respondents noted that the availability of supplies, such as personal protective equipment (PPEs), testing kits and reagents, was inadequate. This was attributed to the disruption of the international supply chain due to travel bans and border closures, which created a global shortage. Additionally, the high demand across countries resulted in an initial spike in prices of supplies rendering them expensive to acquire. However, while the country resorted to local manufacturing of PPEs to avert the shortages, concerns were raised about the poor quality and, therefore, the potential risk to healthcare workers exposed to infections.
“ So , in terms of the supply chain , we notice that the availability of PPEs was a problem , the cost was just out of this world , I think that at this point in time possibly we are buying PPEs at 10% or less of the cost that was reported in the beginning of the pandemic . And especially most of the countries did not have access to COVID-19 test kits , so I would say our biggest challenge at that point was supplies .” Key Informant 1
Rigid procurement processes both at the national and county levels during the pandemic was faulted as one of the challenges that led to shortage of supplies. Respondents recommended that exceptions and favorable provisions should be made for emergencies.
Surveillance and health information systems.
Several concerns were raised regarding the robustness of the health information systems in the country at the beginning of the pandemic. It was noted that historically, the healthcare information system has been fragmented and most of the information, including patient records and files, are still paper based. This posed an initial challenge in receiving real-time information that could have been used for critical decision making, especially with the surge in COVID-19 cases. Few respondents pointed out that there is also an opportunity to embrace technology and digitize data that can be leveraged in critical decision-making.
“ Digital surveillance platforms are easier to analyze and could be producing all these dashboards in real time . I think we adopted it at some stage but in the earlier stages , I think we really were on paper-based approach which sometimes is hard to put on digital platforms and analyze and be able to make decisions .” Key Informant 15
Although there were efforts to undertake mass testing at the initial stage of the pandemic, the process was largely faulted by most of the respondents. First, the initial turnout was low, and the information received was not sufficient to make concrete policy recommendations. Secondly, it was noted that the tests were not being analyzed locally, causing delays and risks of transmission during the wait period. In terms of contact tracing, inaccurate contact information provided by some tested people presented a challenge in reaching them. One of the respondents attributed the provision of wrong information to the initial stigma associated with handling positive cases.
“ I think a lesson that we can learn , right from the initial stages , how do we approach contact tracing without necessarily coming closer to criminalizing it , I think that was the bigger challenge in the initial stages .” Key Informant 15
Almost all the respondents acknowledged that the country responded well in terms of sharing information on the COVID-19 pandemic with the public. They lauded the Ministry of Health for continually informing the public on developments regarding the pandemic. Some of the respondents felt that cross-border exchange of information from countries that were already experiencing the pandemic, such as China, provided an opportunity for Kenya to put stronger mechanisms in place and improve preparedness.
“… I must commend the government and the Ministry of Health in terms of giving information to the public . We had enough materials circulated in the media and even through the facilities . We had regular memos from the Ministry of Health and particularly the acting director-general informing the healthcare workers in terms of what needs to be done .” Key Informant 3
Availability of human resources for health.
Several challenges were highlighted regarding human resources for health during the pandemic. First, respondents pointed out that the available workforce was inadequate and misallocated and poorly trained on the management of COVID-19. While there was a bid to increase the workforce through temporary hiring and redeployment from other programmes to COVID isolation and quarantine sites, some of the respondents felt that this move was not well thought out since: (i) the hiring was done on a short-term basis and posed a challenge to sustainability in the long run; (ii) the few workers left in the facilities were stretched and not working efficiently. Secondly, the inadequate supply and poor quality of PPEs created fear of infection among the healthcare workers, taking a toll on their mental health due to concerns about exposing themselves and their families to the COVID-19 infection.
“ The number of the healthcare workers that were available , number two the protection of healthcare workers by offering quality protective PPEs , and number three in terms of training . You realize from the Ministry of Health data , most counties were below per in terms of the number of people that were training for COVID-19 , and you notice in some areas we had some health workers running away when they heard patients had signs of COVID and this shows anxiety among them because of lack of training …” Key Informant 1
Adequacy of health infrastructure.
There was consensus most respondents regarding the inadequacy of healthcare infrastructure. Some of the respondents’ challenges were the government’s capacity to provide adequate quarantine facilities, leading to overcrowding in the few designated and posing a more considerable infection risk. Additionally, the pandemic revealed the initial insurmountable capacity gap of Intensive Care Units (ICU), with approximately 500 ICU beds available across the entire country to care for critical patients. As a result, some patients lost their lives due to lack of hospital bed space for critical care services.
“.. the public health system is not well equipped in terms of the facilities , in terms of the equipment … The challenge which the Kenyan health system has faced mainly is number one capacity to accommodate those people requiring admission … We don’t have capacity in terms of hospital beds , in terms of ICU capacity and then the number of facilities we have are very limited .” Key Informant 3
Adequacy of financing for COVID-19.
Most of the respondents felt that the health sector in Kenya is significantly underfunded and was further strained by the COVID-19 pandemic. Some argued that the onset of the COVID-19 pandemic created competing needs in the healthcare sector, thereby necessitating efficient and effective way of prioritizing and coordinating the financial resources.
“ The outright answer is our resources have not been enough; both financial , supplies and by a large extent … If you look at the budget allocation in the health sector , we have been oscillating between 5 . 6% and 6% or about 6 . 7% over the last 4 to 5 years , against the Abuja Declaration of 15% . If you look at it from the GDP point of view , we have to push for about 5% of GDP going into the health sector , I think we are oscillating between 1 . 5% and 2% , which means we are still way below the financing and therefore if anything comes on board that destabilizes the balance …” Key Informant 14
A few of the respondents raised concerns regarding the misuse of funds that had been mobilized domestically and from donors to curb the pandemic. Coordination of funding priorities between national and county levels was also highlighted as a challenge. Other issues including improper utilization of funds, delayed disbursements, skewed priorities and lack of expertise among officials were said to impact health financing decision-making.
“ I think for COVID , and we don’t know how many other pandemics we are yet to get into , is how efficient we are in our Public Finance Management , especially in fund flows to getting the money to where it is needed in good time . … we failed in terms of timely disbursements . This serves a lesson for in future how do we get such emergencies taken care of in good time , to get the money where it is needed .” Key Informant 15
When asked about the role of external aid and support in facilitating the COVID response in Kenya, respondents talked about instances where various local and international actors, and agencies offered financial and technical support to the country, including supplies such as PPEs and testing kits. Some agencies, such as USAID were said to have repurposed some of the funds to optimize the fight against the pandemic, while others such as the World Bank offered technical and financial support.
“ From the World Bank , we have these multilateral agreements … one of them was activated very quickly to make that 5 billion Kenya Shillings (Approximately 50 million USD) available . There was support from the EU for example , there was support from DANIDA , and then there was some support from the US government also through USAID and others but working through their implementing partners . And of course the local contribution from the private sector through the resource mobilization committee .” Key Informant 8
Coordination between the national and county governments.
Despite the initial move to set up an inter-governmental and multi-sectoral emergency response committee comprising of the health, security, education, transport, finance and trade sectors, some respondents felt that it was poorly executed in the beginning, with unclear roles and each arm operating autonomously in a situation that called for collaboration. Concerns were also raised by some of the respondents regarding the coordination between the national and county governments. For instance, the COVID-19 isolation centers were initially set up at three hospitals in the country’s capital. Patients who lacked alternatives in their own counties were turned away due to poor referral systems and overcrowding.
“ When surveillance was devolved , contact tracing and all these things , we saw that hampered very much by the ability of the county to activate or facilitate response teams . When the county failed , they said the county failed and yet this is a national emergency .” Key Informant 12
However, opportunities were also leveraged through enhanced county level responses as illustrated by one of the respondents;
“… and borrowing the lessons of COVID-19 , we must remain alert , prepared and be able to work together . And I can give you an example . In my county , my governor set up different committees and I chair one committee where all development partners with a county commissioner and the governor himself , we all sit down to track how the pandemic is moving and mobilize additional resources .” Key Informant 5
Impact of COVID-19 on the health sector, population and the economy
Impact on health services provision..
The onset of the COVID-19 pandemic in Kenya presented a shift in the provision of some healthcare services deemed non-essential. This saw the government closing some of the outpatient clinics and peripheral facilities and reallocating resources, including human and financial, to cater to the COVID-19 response. Majority of the respondents cited that health services, including maternal and child health (MCH), non-communicable diseases (NCDs), HIV, TB and elective surgeries were negatively affected. Under MCH services, sexual reproductive health, family planning services and immunization had to be stopped periodically. Additionally, it was pointed out that some counties converted their maternal units to COVID-19 isolation units, which impacted mothers’ access to care. Although various policies were developed and put in place, some of them lacked clarity, including those for essential and emergency services, hence negatively affecting service provision and health seeking behaviours among the public. Fear of contracting COVID-19 and seeking services past curfew hours as well as capacity and supplies gaps were also highlighted as some of the reasons as to why most people avoided seeking care at health facilities, with others resorting to home based care.
“ You find that antenatal care is considered elective therefore , mothers did not go , even immunization was considered elective , therefore , children did not go for immunization , so those services were affected . And also , family planning access may have been seen as elective and further on surgery , elective surgeries , NCDs , checkups and clinics , medical clinics and surgical clinics may have been considered elective .” Key Informant 12
Some of the respondents also reported that the pandemic highly impacted patients, especially those who needed continuous and routine care (i.e., cancer patients seeking care in the country’s capital Nairobi), due to the imposed lockdown and cessation of the provision of these services that were now considered elective.
“ Many people , including cancer patients who used to come and get their chemotherapy , and get their radiotherapy , those services went down dramatically … some people who were waiting to be given chemotherapy , cancer patients , could have missed several cycles and perhaps lost their lives .” Key Informant 3
Impact on the pathway towards UHC.
While discussing the long-term impacts of the COVID-19 pandemic on the country’s journey towards achieving Universal Health Coverage (UHC), respondents felt that progressively, this would result in decline in coverage and reverse the gains that have been made in these fronts in the country, especially in the case of NCDs and routine care services, like cancer treatments, dialysis etc. Respondents also pointed out that the government was not providing health insurance for the larger population, including the healthcare workers at the onset of the pandemic. Individuals were expected to make out of pocket payments which led to instances of financial hardship. This also affected the willingness of individuals to come forth to get tested or seek treatment at designated COVID-19 facilities.
“ One of the big impact of COVID is the fact that some of the other health conditions , have fallen back behind and therefore it means that in our attainment of UHC there is a lot more that will need to be done because now . I am sure we will have more people affected by different conditions and most notably I would say the NCDs , one , either because people have not then been seeking care at the health facility because of the perception that they will actually get infected , and maybe not taken their medication in the right way that they should .” Key Informant 13
Impact on vulnerable population groups.
Almost all respondents acknowledged that although the COVID-19 pandemic affected the whole population, there were certain sub-sets that were more negatively impacted. One of groups singled out by majority of the key informants were those working in the informal sector or daily wage earners, who constitute almost 80% of the Kenyan population and mostly reside in informal settlements. This is because some of the initial containment measures put in place including lockdown and closing some sectors of the economy such as bars and restaurants, increased their vulnerability by affecting their jobs and livelihoods. Additionally, public health measures that required the purchase of masks and sanitizers presented a challenge to those living in informal settlements and with limited resources.
“… we are aware that with that [COVID-19 pandemic] came quite a number of restrictions that of course closed the economy and we know that over 80% of Kenyans are either poor or near poor , meaning they are one incident away from poverty , so any single incident will push them into poverty and COVID-19 is one of such incidences where if they don’t get a salary for one month then they would be literally be below the poverty line .” Key Informant 14
Some stakeholders pointed out that women and girls were disproportionately affected by the pandemic. Cases of gender-based violence, especially against women, were on the rise due to economic stress in households and social isolation resulting from movement restrictions. Additionally, some stakeholders pointed out that the school system offered security to girls from communities that practice early marriages and female genital mutilation, and school closure resulted in an increase in these cases.
“ On one side , communities that practice early child marriage and female genital mutilation , we saw these things increasing because now girls were at home , they were more vulnerable , they were not going to school … girls who come from poor families and rural communities who would depend on the government supply of sanitary commodities could no longer access them because now they were at home and those sanitary commodities are largely supplied through schools .” Key Informant 12
Commenting on the pandemic’s impact on school and education, a few of the respondents mentioned that children in rural and remote settings were affected by the temporarily closure of learning institutions due to lack of access to the internet and laptops. Additionally, some of the children in the rural counties relying on government-supported school feeding programmes saw reduced access to food. Few respondents noted that children with special needs, who mostly rely on teachers with special needs training, affected their learning. Additionally, people with disability were also affected due to the social distancing measures put in place.
“… and then you have persons who are disabled so they need physical support , they actually need someone to pull and to push their wheelchair , or they need someone to hold them and help them get into a matatu [minibus used for transport] , and so on … so , this physical distancing measures were disproportionately affecting people that are blind , people that cannot walk , people that cannot talk; so , the disabled were disproportionately affected . Key Informant 4
Impact on donor transitions in the health sector.
Due to the heavy reliance on donor funding in the health sector, majority of the respondents expressed their concerns about its impact on the health sector more generally, and the impact of COVID-19 on donor transitions in Kenya. Some of them felt the donor countries are likely to shift their resources to focus more on their own needs in dealing with the pandemic. In contrast, others felt that donors would reevaluate transition timelines and be more forthcoming to boost investments in a bid to curb the pandemic and strengthen health systems.
“… most countries having experienced the pandemic and economic crisis which they have not had in the past , we expect that they will focus more on their individual country’s needs as opposed to donations , and of course lower middle-income countries like Kenya , we need to prepare for that and set priorities in the health system to ensure that the little funds that we have are used in an efficient way .” Key Informant 2
Opportunities to improve future pandemic preparedness
Greater financial flexibility and improved coordination to respond to pandemics..
Various recommendations were made to improve health financing arrangements and strengthen financial prioritization and coordination to tackle future health emergencies. First, there were suggestions to create an emergency fund within the Ministry of Health that can be tapped and easily accessed in emergencies. Second, stakeholders urged for reforming the public financial management laws to allow flexibility and improve financial decision-making during an emergency. Third, respondents called for introducing financial laws and regulations that are responsive to unique situations such as pandemics that would facilitate improved fund utilization at the national and county levels. Respondents argued that counties and facilities should be given the financial autonomy to carry their duties, such as hiring more health workers during an emergency without overtly relying on the national government. Respondents also called for fostering stronger public private partnerships to mobilize resources to tackle future pandemics.
“ For financing , we must have an emergency fund that is backed by law , that this percentage must be put for emergencies even though it keeps revolving every year . Because , if we have to start forming committees to get funds or to start fundraising now , you see the delays in the response .” Key Informant 9
Improving self-reliance through increased domestic health investments.
Respondents generally agreed that Kenya should prioritize resource mobilization and spend efficiently to minimize the financial strain and service gaps resulting from the COVID-19 pandemic and impending donor transitions. Respondents urged for better donor transition planning and improved accountability in using available external resources to build a resilient health system. Apart from improved resource mobilization, few respondents cited that the country should emphasize efficiency improvements in the health sector by adopting mechanisms such as health technology assessments. Additionally, there were views to foster a more robust consultation between African countries, the national and county governments in resource allocation, and leveraging on public-private partnerships to seal the gap that will result from donor exit.
“ I would ask that especially in the health sector , we adopt health technology assessment as a key intervention that helps us understand where we have the highest return on investment . We do not need to add more resources maybe right now , but we need to ensure that we know where our money is and what our money is doing and looking at how best can we maximize on our efficiencies . " Key Informant 14
“ 25% of the Kenyan healthcare sector is financed by donors … we have transitioned into a lower middle-income country … when you look at HIV AIDS , vaccines , malaria in the country , the dependency is much higher . If we don’t have a plan for how we will replace the funds that we get from donors , then we are going to lose the gains that we have made on those specific disease …” Key Informant 4
Improved financial protection for individuals to achieve UHC.
Given the catastrophic health expenses borne by families at the onset of the pandemic due to lack of coverage by both public and private insurance schemes, there were suggestions to increase protection through social and private insurance that can be adjusted to accommodate the larger population in instances of a pandemic. Additionally, to increase the country’s health system resilience, there were suggestions to increase equity in resource allocation, coupled with political goodwill in a bid to achieve UHC.
“ In terms of health financing and UHC , COVID presents a fantastic opportunity for us to reengineer our health systems ;… no one is safe until everyone is safe … if we don’t bring everyone under a mechanism of ensuring that they have access to care then it does no good to all of us because the fact that your neighbor is not covered or is unable to access a treatment on COVID or preventive measures on COVID , then that means you are not protected in the first place .” Key Informant 15
Addressing gaps in health infrastructure.
Despite the challenges linked to infrastructural gaps, some of the respondents reported that setting up urgent health facilities created an opportunity for increased structural capacity that can still be used post-COVID. There was also recommendation to increase investments in health systems infrastructure such as ICU to cater to future pandemics and other ailments.
“ Now , we have been able to put capacity in most of our health facilities , there are counties which would not have had ICUs in many years to come . I am sure even after COVID , those ICUs will be used for other ailments going forward .” Key Informant 2
Strengthening human resources health.
There were suggestions to rethink human resources development sustainably, including expanding the health workforce and greater focus on tackling health emergencies. Additionally, some respondents also highlighted the need to continuously train the healthcare workforce on emergency preparedness by embedding it in their curriculum to create better and timely response in case of future pandemics.
“ The workforce , the preparedness among our people to deal with the pandemic needs to be done well in advance … I mean , we know this might happen . It should becomes part of our curriculum in our medical schools and nursing schools and schools of public health …” Key Informant 6
Fostering cross-sectoral collaborations for maintaining essential health services during health emergencies.
Several respondents mentioned that despite these challenges, the pandemic provided an opportunity for multisectoral collaboration, which helped ease the pandemic’s impact. In terms of progressive response, respondents mentioned that, through partnerships fostered between the Ministry of Health and private sector players, guidelines and outreach for MCH, TB and HIV programs filled the initial service provision gaps created by the pandemic. There were recommendations for the government to invest in the delivery of essential services during a pandemic in two major ways; prioritization of continuity of services and dedication of funds for the provision of essential services.
“.. we have to put a lot of effort towards maintaining the essential healthcare services that have been going on . Indeed services were negatively affected , not that people stopped being sick , but people feared the pandemic , they did not seek healthcare services . So , even as we respond to any pandemic , we also need to be aware that we need to respond to the existing conditions …” Key Informant 10
Various opportunities were witnessed in the country’s policy response and measures, including creating local testing capacity by leveraging technology and innovation and strengthening public and private sector collaborations. Additionally, some of the respondents recommended that there should be a deliberate effort to map and support the vulnerable population since their economic and social state directly correlates with the larger health outcomes.
“ Our second level of preparedness should now be looking at the impact of each sector of the economy and mobilize those multi sectoral responses for mitigation . Those mitigation measures in each of those sectors of the economy are what is going to put in place a firm foundation for dealing with potential long-term impacts , making sure that there are certain policy changes that may have to be addressed .” Key Informant 8
Stakeholders also noted that there is an opportunity to strengthen local manufacturing of healthcare commodities to help reduce import costs and mitigate shortages in instances where the global supply chain is affected.
“ We have also realized that in the very initial stages we were importing some of the very simple materials from China and other countries . As we talk now , in the country , actually we deliberately decided to take a route where we are creating capacity to be able to produce things locally . The net effect is that there was serious significant reduction of cost in terms of what we were spending to access some of those things !" Key Informant 2
Incorporating lessons learnt from previous health emergencies and other country experiences.
The majority of the respondents acknowledged that lessons learnt from previous pandemics, including SARS, Ebola, and HIV were progressively incorporated and helped Kenya leverage the existing systems and policies to fight the COVID-19 pandemic.
“ But as it were , before the pandemic , we had the laws and the policies which were actually supposed to direct us on what to do in case of any new emerging disease . And they are very many , as you can recall , we had SARS , we had Ebola … Although the initial reaction was not immediate and some services had been disrupted , we quickly adopted some of the strategies we had .” Key Informant 9
Most of the respondents felt that the capacity of all health systems across the world was tested during the pandemic. However, some mentioned that countries in the continent such as Senegal, the Democratic Republic of Congo, and Uganda had dealt with previous pandemics such as Ebola in earlier years and had better surveillance and response to the pandemic since they leveraged existing systems. Respondents suggested that Kenya should use a blend of lessons from all the countries to develop a solution that will work best in the Kenyan context.
“ If you talk around institutionalizing disease surveillance as a long-term thing , I think Uganda is a country we can learn from . They have a reasonably good disease surveillance process , virology centre they have built , and I think this is because of their Marburg and Ebola outbreaks in the past . Senegal started off with a very early lab information system where all tests were put onto a lab information system , you could see who is testing , how the tests are followed . So , we may not learn the whole response from one country , but we can learn aspects country by country . Key Informant 12
This study explored perspectives of key stakeholders in Kenya’s health system on the country’s response to the COVID-19 pandemic, its impact on the health sector, and implications for future pandemic preparedness. The COVID-19 pandemic presented Kenya with multiple challenges that disrupted the health system and had ripple effects on the entire economy. Shortcomings related to the WHO building blocks were mentioned frequently in our study. Given their complex interaction, there is need to strengthen the healthcare system in the event of a future pandemic of similar magnitude. Addressing these challenges can contribute to improved responsiveness, risk protection of the population and delivery of quality and efficient health services.
The initial negative impact of the pandemic on continuity of essential and non-essential/general health services was revealed in our study. MCH, TB, HIV, assistance for patients requiring routine and continued care were some of the categories highlighted, with attribution to factors such as government directives to discontinue these services and redeployment of staff to offer COVID-19 relief and support services being mentioned. These findings were comparable with other studies from both high and low resource settings which saw a significant disruption in health service provision [ 31 , 39 , 46 – 50 ]. However, not all services were affected as outlined in these studies from Kenya [ 51 ] and Ethiopia [ 52 ]. As a COVID-19 post recovery strategy for protecting the public health gains made for these services, it is pertinent to strengthen governance, coordination and informed decision making across the health service delivery network [ 53 – 55 ]. This will help in promoting provision of quality health services that are essential in ensuring achievement of UHC even in times of public health crisis [ 55 ].
Reduction in individuals’ health-seeking behavior, as seen in our study, was also seen in other countries [ 56 , 57 ]. This was associated with the discontinuation of some health services, lockdowns, curfews, and the fear of infections. Previous studies undertaken in past pandemics such as Ebola have also outlined changes in health seeking behaviors [ 58 , 59 ]. As recommended by our key informants and seen in other studies, a key measure to ensuring continuity of services in the event of a pandemic is to foster multi-sectorial collaboration and developing a resilient health system that is able to cater for needs from a pandemic while maintaining routine health services [ 41 , 60 , 61 ].
Apart from the gaps in effective pandemic response, our study highlights several existing issues such as inadequate healthcare financing, lack of infrastructure, and human resource capacity constraints that have important implications for achieving UHC in Kenya. These challenges can severely impact overall health system resilience, especially as Kenya is undergoing a transition from concessional donor assistance and needs to become more self-reliant in providing services for its population [ 62 ]. Strengthening primary health care and adopting the right mix of Global Health Security (GHS) and UHC domains has been argued as an approach to resolve the health system gaps [ 63 , 64 ]. Additionally, improving public financial management for improved budget allocation and accountability can be integrated by the Country to enhance its future preparedness [ 65 , 66 ].
The respondents in our study revealed the authorities’ initial shortcomings to manage adequate provision for testing, isolation, and quarantine services. However, these services are seen at the heart of effective public health responses to COVID-19. Respondents noted that while the government took appropriate public health measures to curb the pandemic, it fell short on several fronts owing to overwhelmed health facilities and personnel, lack of adequate resources, and issues with capacity and coordination. These findings mirror those from an analysis to understand lessons that Kenya can learn from the pandemic while linking it to historical gaps in the country’s health system [ 67 ]. The resource shortages were attributed to long-standing gaps in the health sector stemming from poor leadership and governance that have preceded the pandemic. Good leadership and governance form part of the key ingredients that determine how a country respond’s to public health emergencies [ 68 ].
Our findings highlighted the prompt response of the government to introduce measures to curb the spread of the virus, share information and raise awareness about the pandemic among the public. These findings are similar to that of two other studies aimed at assessing the knowledge, attitude and practices among the youth and households in informal settlements in Kenya [ 69 , 70 ], and a scoping review assessing the same for Sub-Saharan Africa [ 71 ]. In the three studies, the results indicated that there was high knowledge of the COVID-19 symptoms and preventive strategies, owing to active awareness campaigns by various governments. However, these studies also revealed that a high level of knowledge does not necessarily translate to preventive measures. Respondents raised concerns about the robustness of the HIS and mentioned that its fragmentation hindered timely relay of information for critical decision making at the onset of the pandemic. The use of information technology has been seen to act as an enabling factor for health care utilization by increasing the availability and accessibility of health services, especially for people from rural and remote areas, which will also make it more affordable and less time constraints [ 72 – 74 ]. Additionally, adopting a framework that collects the right data that can be used for future forecast in the event of a pandemic, both at the national and subnational level, is essential in strengthening the country’s health security [ 75 , 76 ].
Strengths and limitations
This study focused on Kenya’s health system’s early responses and overall preparedness to tackle COVID-19. The interviews were conducted during the second wave of the COVID pandemic in Kenya while response measures were still evolving. While the study focuses on various public health measures and controls adopted to curb spread of the pandemic, it does not focus on COVID-19 vaccination strategies, which is critical to ending the pandemic. Participants in the study do not include health care service recipients during the pandemic.
This is among the first studies in Kenya that focused on understanding the impact, response, and policy implications of the COVID-19 pandemic in Kenya through interviews with key stakeholders who were involved first-hand in handling the pandemic in Kenya. The study results provide important insights for future policy and planning to respond more effectively and deliver health services during future health emergencies in Kenya.
This study provides an overview of the early responses to the COVID pandemic in Kenya, pointing out the impact and key challenges that affect how Kenya can improve preparedness for dealing with future pandemics. Improving health sector investments by identifying strategies to minimize the effects of essential health systems could help improve pandemic response in the future. Stakeholders also called for better coordination, more flexibility in financial decision-making, and improved self-reliance to manage the pandemic better.
Supporting information
S1 appendix. topic guide for key informant interviews..
https://doi.org/10.1371/journal.pgph.0001348.s001
Acknowledgments
We would like to acknowledge Dr. Indermit Singh Gill, current Vice President for Equitable Growth, Finance and Institutions at the World Bank and former Professor of Public Policy at Duke University and Dr. Osondu Ogbuoji of Duke University, Center for Policy Impact in Global Health for providing valuable insights and guidance in designing this study. The authors also wish to thank all key informants who provided valuable information for the study.
- View Article
- Google Scholar
- 2. World Health Organization. WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data [Internet]. 2022 [cited 2022 Jun 7]. https://covid19.who.int/
- 3. Africa CDC. Coronavirus Disease 2019 (COVID-19)–Africa CDC [Internet]. 2022 [cited 2022 Jan 17]. https://africacdc.org/covid-19/
- 4. World Health Organization. COVID-19 vaccine tracker and landscape [Internet]. 2022 [cited 2022 Jun 7]. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
- 5. Gavi. There are four types of COVID-19 vaccines: here’s how they work [Internet]. 2022 [cited 2022 Jun 7]. https://www.gavi.org/vaccineswork/there-are-four-types-covid-19-vaccines-heres-how-they-work
- 6. Africa CDC. COVID-19 Vaccination–Africa CDC [Internet]. 2022 [cited 2022 Jun 7]. https://africacdc.org/covid-19-vaccination/
- PubMed/NCBI
- 13. World Bank. For Sub-Saharan Africa, Coronavirus Crisis Calls for Policies for Greater Resilience [Internet]. 2020 [cited 2021 Jul 19]. https://www.worldbank.org/en/region/afr/publication/for-sub-saharan-africa-coronavirus-crisis-calls-for-policies-for-greater-resilience
- 16. Ogbuoji O, Bharali I, Emery N, McDade KK. Closing Africa’s health financing gap [Internet]. Brookings Blog. 2019 [cited 2021 Oct 25]. https://www.brookings.edu/blog/future-development/2019/03/01/closing-africas-health-financing-gap/
- 19. Ministry of Health Kenya. First case of Corona Virus Disease confirmed in Kenya [Internet]. 2020 [cited 2021 Jul 19]. https://www.health.go.ke/first-case-of-coronavirus-disease-confirmed-in-kenya/
- 20. Ministry of Health Kenya. Update on COVID-19 in the country and response measures, as at April 22, 2021. 2021;573–6. https://www.health.go.ke/wp-content/uploads/2021/04/NERC-MOH-CS-COVID-UPDATE-22.4.2021.pdf
- 21. Ministry of Health Kenya. National COVID-19 Vaccine Deployment Plan, 2021. 2021;(January):1–24.
- 25. Ouma M. Kenya’s Social Policy Response to Covid-19: Tax Cuts, Cash Transfers and Public Works. Vol. 27. Universität Bremen; 2021.
- 26. Government of Kenya. Executive Office of the President State House—Registry. Executive Order No. 2 of 2020 [Internet]. 2020 [cited 2021 Jul 19]. p. 1–6. https://www.health.go.ke/wp-content/uploads/2020/06/Executive-Order-No-2-of-2020_National-Emergency-Response-Committee-on-Coronavirus-28.2.20.pdf
- 27. Government of Kenya. The eighth (8th) presidential address on the coronavirus pandemic Saturday, June 6th 2020 | The Presidency [Internet]. 2020 [cited 2021 Jul 19]. https://www.president.go.ke/2020/06/06/the-eighth-8th-presidential-address-on-the-coronavirus-pandemic-state-house-saturday-june-6th-2020/
- 29. World in Data. Kenya: Coronavirus Pandemic Country Profile—Our World in Data [Internet]. 2020 [cited 2021 Jul 19]. https://ourworldindata.org/coronavirus/country/kenya
- 30. Barasa E, Mothupi C. Mamothena, Guleid F, Nwosu C, Kabia E, Araba D, et al. Health and Socio-Economic Impacts of Physical Distancing for Covid-19 in Africa. 2020; https://www.aasciences.africa/sites/default/files/2020-05/DFID Report- Rapid Review of Physical Distancing in Africa—19052020-compressed.pdf
- 35. Igunza E. Coronavirus corruption in Kenya: Officials and businesspeople targeted [Internet]. BBC News. 2020 [cited 2021 Oct 26]. https://www.bbc.com/news/world-africa-54278417
- 36. Transparency International. The Ignored Pandemic behing COVID-19-The impact of Corruption on Healthservice Delivery. 2020;
- 40. World Health Organization. Everybody’s business—strengthening health systems to improve health outcomes: WHO’s framework for action. World Health Organization; 2007. p. 44 p.
- 48. World Health Organization. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a rapid assessment [Internet]. Geneva PP—Geneva: World Health Organization; 2020. https://apps.who.int/iris/handle/10665/334136
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Effects of COVID-19 pandemic in daily life
Dear Editor,
COVID-19 (Coronavirus) has affected day to day life and is slowing down the global economy. This pandemic has affected thousands of peoples, who are either sick or are being killed due to the spread of this disease. The most common symptoms of this viral infection are fever, cold, cough, bone pain and breathing problems, and ultimately leading to pneumonia. This, being a new viral disease affecting humans for the first time, vaccines are not yet available. Thus, the emphasis is on taking extensive precautions such as extensive hygiene protocol (e.g., regularly washing of hands, avoidance of face to face interaction etc.), social distancing, and wearing of masks, and so on. This virus is spreading exponentially region wise. Countries are banning gatherings of people to the spread and break the exponential curve. 1 , 2 Many countries are locking their population and enforcing strict quarantine to control the spread of the havoc of this highly communicable disease.
COVID-19 has rapidly affected our day to day life, businesses, disrupted the world trade and movements. Identification of the disease at an early stage is vital to control the spread of the virus because it very rapidly spreads from person to person. Most of the countries have slowed down their manufacturing of the products. 3 , 4 The various industries and sectors are affected by the cause of this disease; these include the pharmaceuticals industry, solar power sector, tourism, Information and electronics industry. This virus creates significant knock-on effects on the daily life of citizens, as well as about the global economy.
Presently the impacts of COVID-19 in daily life are extensive and have far reaching consequences. These can be divided into various categories:
- • Challenges in the diagnosis, quarantine and treatment of suspected or confirmed cases
- • High burden of the functioning of the existing medical system
- • Patients with other disease and health problems are getting neglected
- • Overload on doctors and other healthcare professionals, who are at a very high risk
- • Overloading of medical shops
- • Requirement for high protection
- • Disruption of medical supply chain
- • Slowing of the manufacturing of essential goods
- • Disrupt the supply chain of products
- • Losses in national and international business
- • Poor cash flow in the market
- • Significant slowing down in the revenue growth
- • Service sector is not being able to provide their proper service
- • Cancellation or postponement of large-scale sports and tournaments
- • Avoiding the national and international travelling and cancellation of services
- • Disruption of celebration of cultural, religious and festive events
- • Undue stress among the population
- • Social distancing with our peers and family members
- • Closure of the hotels, restaurants and religious places
- • Closure of places for entertainment such as movie and play theatres, sports clubs, gymnasiums, swimming pools, and so on.
- • Postponement of examinations
This COVID-19 has affected the sources of supply and effects the global economy. There are restrictions of travelling from one country to another country. During travelling, numbers of cases are identified positive when tested, especially when they are taking international visits. 5 All governments, health organisations and other authorities are continuously focussing on identifying the cases affected by the COVID-19. Healthcare professional face lot of difficulties in maintaining the quality of healthcare in these days.
Declaration of competing interest
None declared.

COMMENTS
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
The Coronavirus disease 2019 (COVID-19), the global pandemic, causing Severe Acute Respiratory Syndrome Corona virus -2 (SARS CoV-2), has devastated the world resulting in several million infections and close to five million deaths till late October 2021 ().Though COVID-19 pandemic has affected all sectors directly or indirectly, the crisis is worse on the already overburdened health systems ...
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the ...
essay, the lens of health inequalities, and perspective of relationships as interconnecting elements in a broader system, is used to explore the varying impact of these disruptions. The essay concludes by providing recommendations for longer term recovery ensuring that the social relational cost of COVID-19 is adequately
From lifestyle changes to better eating habits, people are using this time to get healthier in many areas. Since the pandemic started, nearly two-thirds of the survey's participants (62%) say ...
This essay discusses the impact that these challenges have or could have on people with chronic disease now and in the future. Exploring the impact of COVID-19 should help the public health and health care communities effectively improve health outcomes. Top. Challenges. The challenges we face as public health professionals are divided into 3 ...
Physical distancing due to the COVID‐19 outbreak can have drastic negative effects on the mental health of the elderly and disabled individuals. Physical isolation at home among family members can put the elderly and disabled person at serious mental health risk. It can cause anxiety, distress, and induce a traumatic situation for them.
4. Impact of COVID-19 on the energy domain. COVID-19 has not only impacted health, society and the economy but it has also had a strong impact on the energy sector (Chakraborty and Maity, 2020; Abu-Rayash and Dincer, 2020). World energy demand fell by 3.8% in the first quarter (Q1) of 2020 compared with Q1 2019.
As of 31 December 2020, COVID-19 had infected over 82 million people and killed more than 1.8 million worldwide. But preliminary estimates suggest the total number of global "excess deaths" directly and indirectly attributable to COVID-19 in 2020 amount to at least 3 million, 1.2 million higher than the official figures reported by ...
This essay examines the implications of the COVID-19 pandemic for health inequalities. It outlines historical and contemporary evidence of inequalities in pandemics—drawing on international research into the Spanish influenza pandemic of 1918, the H1N1 outbreak of 2009 and the emerging international estimates of socio-economic, ethnic and geographical inequalities in COVID-19 infection and ...
Please use one of the following formats to cite this article in your essay, paper or report: APA. Cuffari, Benedette. (2022, July 05). How has the COVID-19 Pandemic Impacted Global Health?.
Horrific history. Looking back, the COVID-19 pandemic stands as arguably the most disruptive event of the 21st century, surpassing wars, the September 11, 2001, terrorist attacks, the effects of climate change, and the Great Recession. It has killed more than seven million people to date and reshaped the world economy, public health, education ...
1. Introduction. The coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented changes in people's daily lives, with implications for mental health and well-being [1-4], both at the level of a given country's population, and when considering specific vulnerable groups [5-7].In order to mitigate the untoward impact of the pandemic (including lockdown) and support mental health ...
The World Health Organization declared coronavirus disease of 2019 as an epidemic and public health emergency of international concern on January 30th, 2020. Different factors during a pandemic can contribute to low quality of life in the general population. Quality of life is considered multidimensional and subjective and is assessed by using patient reported outcome measures. The aim and ...
COVID-19 anD ITS IMpaCT: SEVEn ESSayS On REFRaMInG GOVERnMEnT The COVID-19 pandemic has changed economic, social, and health care activities across the world, and the consequences of this historically significant global event will have lasting effects . The loss of life and the fear caused by the pandemic disrupted governments around the world at
A Crisis in Public Health. The United States has 4% of the world's population but, as of July 16, approximately 26% of its Covid-19 cases and 24% of its Covid-19 deaths. 17 These startling ...
Writing About COVID-19 in College Essays. Experts say students should be honest and not limit themselves to merely their experiences with the pandemic. The global impact of COVID-19, the disease ...
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
The coronavirus pandemic (COVID-19) has triggered a public health and economic crisis in high and low resource settings since the beginning of 2020. With the first case being discovered on 12th March 2020, Kenya has responded by using health and non-health strategies to mitigate the direct and indirect impact of the disease on its population. However, this has had positive and negative ...
The COVID-19 pandemic has challenged and, in many cases, exceeded the capacity of hospitals and intensive care units (ICUs) worldwide. Health-care workers have continued to provide care for patients despite exhaustion, personal risk of infection, fear of transmission to family members, illness or death of friends and colleagues, and the loss of many patients. Sadly, health-care workers have ...
Presently the impacts of COVID-19 in daily life are extensive and have far reaching consequences. These can be divided into various categories: Closure of places for entertainment such as movie and play theatres, sports clubs, gymnasiums, swimming pools, and so on. This COVID-19 has affected the sources of supply and effects the global economy.
The impact of COVID-19 on mental health cannot be made light of. 16 June 2022. One of the biggest global crises in generations, the COVID-19 pandemic has had severe and far-reaching repercussions for health systems, economies and societies. Countless people have died, or lost their livelihoods.
We nd that the substantial variation in the impact of COVID-19 on students tracked with existing socioeconomic divides. For example, compared to their more a uent peers, lower-income students are 55% more likely to delay graduation due to COVID-19 and are 41% more likely to report that COVID-19 impacted their major choice.