- Research article
- Open access
- Published: 07 September 2020

Living with personality disorder and seeking mental health treatment: patients and family members reflect on their experiences
- Karlen R. Barr 1 ,
- Mahlie Jewell 2 ,
- Michelle L. Townsend 1 &
- Brin F. S. Grenyer 1
Borderline Personality Disorder and Emotion Dysregulation volume 7 , Article number: 21 ( 2020 ) Cite this article
15k Accesses
16 Citations
37 Altmetric
Metrics details
Despite effective treatments for personality disorders being developed, consumers and carers often report negative experiences of mental health services, including challenges accessing these treatments.
This qualitative study used separate focus groups to compare the unique perspectives of consumer and carers, and to investigate how to improve services for individuals with personality disorders. Reflexive thematic analysis was used to analyze the data.
Both consumers and carers ( N = 15) discussed the value of providing appropriate information to consumers when they are diagnosed with personality disorder. Consumers and carers described the importance of creating a safe environment for consumers when they present to the emergency department. Both groups discussed experiencing positive and negative treatment from mental health professionals, and suggested that professionals should be trained to understand personality disorder. Limited accessibility and quality of services, and offering peer support to consumers were also described by consumers and carers. Consumers and carers also had perspectives which were unique to their group. Consumers identified the importance of psychological treatment, having a strong therapeutic relationship with a mental health professional, and the benefit of long term psychotherapy with the same professional. Broadening the scope of psychotherapies including creative, animal-assisted, and physical therapies was recommended by consumers. Carers described the importance of assessing for personality disorder and intervening early. Involvement in the assessment, diagnosis, and intervention process was important to carers. The desire to be recognized and supported by mental health professionals was discussed by carers.
Conclusions
This research contributes to the concern that consumers with personality disorder and their carers experience stigma and low quality care within mental health services. In line with these findings, we recommend guidelines for health professionals who work with consumers with personality disorder.
Personality disorders are severe mental disorders characterized by disturbances in affect, identity, and relationships [ 1 ]. Approximately 7.8% of the population has a personality disorder [ 2 ], and people with personality disorders represent about 20% of emergency department and 25% of inpatient mental health admissions [ 3 ]. In mental health and primary care settings, borderline personality disorder (BPD) is the most common personality disorder [ 4 ]. Effective treatments for personality disorder exist, including dialectical behavior therapy (DBT) and psychodynamic therapies [ 5 ]. However, consumers with personality disorder often are not offered or are unable to access evidence-based therapies and thus have negative experiences when receiving mental health services [ 6 ]. In addition, carers supporting consumers with personality disorder often experience high levels of stress, grief, and mental health problems [ 7 , 8 ], and they can experience difficulties accessing appropriate services for themselves and the consumers they support [ 9 ]. Considering the perspectives of consumers and carers is recommended to improve mental health services [ 10 ], and is supported by government [ 11 , 12 ] and mental health professionals [ 13 , 14 ].
Experiences of mental health services have been studied from the perspectives of consumers with various mental illnesses and their carers. Consumers describe the importance of mental health professionals discussing diagnoses with consumers and carers, and providing hope and information regarding diagnosis [ 15 ]. Regarding treatment planning, consumers want to be involved in their treatment decisions [ 16 ], although they are often excluded from participating in decision making [ 17 ]. Further, consumers describe not being prepared for hospital discharge, not being involved in the decision to discharge, and not receiving adequate support following discharge [ 18 ]. Carers supporting consumers with a range of mental health problems express that they have little involvement in mental health services and little access to information on mental health services [ 16 ]. Many carers believe they should have access to information about consumers, and report that confidentiality prevents them from receiving information about the consumer they support. Carers describe wanting respectful treatment for themselves and consumers, and better communication from mental health professionals, including education about specific disorders [ 19 ]. Other barriers described by carers include poor communication between services, limited service accessibility, and receiving little information about consumer treatment plans [ 20 ]. Carers also experience inconsistent assistance from mental health professionals in response to consumer mental health crises [ 21 , 22 ].
Multiple studies have investigated the experiences of consumers with personality disorder regarding mental health services. Consumers with personality disorder often do not receive an explanation of their diagnosis [ 23 ], or experience stigmatizing language and insufficient evidence-based information about their diagnosis [ 6 ]. Consumers have also described negative responses from health professionals in the emergency department [ 24 ]. Other negative experiences include poor communication from professionals, and inappropriate treatment, such as not having concerns taken seriously [ 6 ]. Increasing psychological and emotional support is recommended by consumers with personality disorder [ 6 ], including being supported by health professionals who help them understand their feelings [ 23 ].
Perspectives of mental health services from carers supporting consumers with personality disorder have also been investigated. Carers often experience relationship difficulties with the consumers they support, and do not know where to find help [ 9 ]. The majority of carers want support for themselves but find carer support services are unavailable or difficult to access [ 9 , 25 ]. Carers can also experience difficulty supporting consumers to find mental health professionals and consistent services to provide support to consumers with personality disorder [ 9 ]. In addition, many carers describe not receiving an explanation of the consumer’s diagnosis and not being appropriately involved in treatment decisions [ 25 ]. Carers identified wanting more information about personality disorder and how to respond to crises, and express that they are often expected to make treatment decisions without having sufficient knowledge [ 26 ].
A systematic review of 38 studies examined the perspectives of consumers and carers regarding mental health services for individuals with BPD [ 27 ]. Across the studies, consumers described receiving limited information about the assessment process and BPD diagnosis, negative responses from mental health professionals in the emergency department or inpatient setting, limited information options for therapeutic interventions, and poor communication regarding the availability of services. Studies exploring the carer perspective found that carers wanted their supporting role and their difficulties to be recognized by mental health professionals, be provided more information regarding BPD diagnosis and treatment options, and information about how to effectively respond to the consumer they support. While consumers and carers shared some consistent views, differences in opinion were observed, such as carers focusing on the lack of support they received from professionals. Comparing the consumer and carer experiences was limited because only five studies were found regarding the carer perspective, and only one study included the perspectives of consumers and carers. Therefore, more information is required regarding similarities and differences of consumer and carer views. In addition, few of the included research studies were co-produced with consumers or carers, even though this is known to lead to questions and findings closer to what people with lived experience require [ 28 ].
Problems continue to be present in personality disorder services and programs and require input from consumers and carers regarding possible improvements. It is important to increase knowledge regarding the views of consumers and carers who support someone with personality disorder, to compare views of consumers and carers regarding services for individuals with personality disorder, and to co-produce research on consumer and carer perspectives. The purpose of this study was to bring together all these needs and gaps in the literature: to explore and compare the perspectives of consumers and carers regarding personality disorder services using a co-design approach aimed to inform the development of better services.
Participants
Participants were recruited using a flyer advertisement that was sent to consumer and carer support and advocacy groups, and services which support individuals with personality disorder. Participants were invited to participate if they were either a consumer with a lived experience of personality disorder or a carer or family member supporting someone with a personality disorder. The views of 15 individuals were obtained, a sample large enough for data saturation within a qualitative approach. Table 1 outlines the demographic characteristics of the participants.
Participants provided informed written consent prior to study participation, following study approval from the Institutional Review Board. Two focus group discussions occurred simultaneously; one with consumers and one with carers, as requested by the participants. Both focus groups were co-facilitated by 2 researchers with experience in personality disorders and group facilitation. The consumer focus group was co-facilitated by the consumer researcher. In addition, 1 mental health professional was present in each group to provide assistance to participants if they became distressed. Focus group questions were based on a guide that was co-designed by the authors. Some questions required participants to provide written answers or creative responses. Questions differed slightly for consumer and carer participants. Open-ended questions were followed with relevant follow-up questions as required. Questions explored the quality of care experienced at different services, including mental health services and emergency services, and how the practice of health professionals could improve. Questions included, “What have you found most helpful about the services you have been involved in?”, “Is there anything you wish clinicians and service leaders better understood about individuals living with personality disorder?” and “How can health professionals best support families and carers of individuals who have been recently diagnosed with personality disorder?” The discussions were audio recorded and transcribed. Focus group discussions occurred over a 90-min period. A $50 voucher was provided to participants as compensation for their time.
Data analysis
The data were analyzed using reflexive thematic analysis, which conceptualizes themes as patterns based in meaning [ 29 ]. First, the transcripts were read and re-read and brief notes were made to obtain familiarization with the data. Next, participant statements were coded into nodes through the software NVivo 11. Nodes were created using an inductive orientation to gather statements with similar meanings. Themes were constructed based on the nodes, and were revised as needed to reflect the lived experience of participants. One researcher independently coded the data, which was informed by regular discussions with the research team. The consumer researcher was part of the research team throughout all phases and provided active input into the themes developed. Inter-rater reliability was obtained by all team members arriving at a consensus for the coding. In addition, an independent researcher coded a portion of data to allow us another view on agreement - with Cohen’s kappa coefficient for inter-rater reliability being κ = 0.75, which indicates a relatively high level of agreement [ 30 ].
Consumer perspectives
In this section, the views that were gathered from the consumer focus group are presented.
Theme 1: challenges and successes finding a mental health professional who understands personality disorder
Consumers described how medical and psychiatric registrars often do not have the experience and knowledge base to provide treatment or information to people with personality disorders. Difficulties in finding a mental health professional who has training in and understands personality disorders were described by several participants. “In my long hard, long lived history as a consumer, with an illness, I have been referred and searched high and low for private psychologists who would have knowledge of this particular ill – normality, this illness, and you know, there’s very few out there who are familiar enough with it.” Consumers described various instances when mental health professionals used stigmatizing language, which had a major negative influence on their well-being. “[After multiple stigmatizing comments] I felt so completely let down and failed by the public system. Like my life didn’t matter, like I didn’t matter.”
Several consumers described positive experiences with mental health professionals who specialize in treating personality disorders. Consumers explained the importance of finding a mental health professional that they can connect with, who complements their specific needs. A trial and error process of finding a suitable mental health professional was described , “They’re not always going to be – the right one is not always going to be the first one you get. There’s a lot of trial and error.” Participants valued mental health professionals who were clear about how long they could work with them, admitted to making mistakes, kept them accountable to their goals, and persevered in contacting consumers. “I didn’t turn up three times and she kept calling me. And she kept saying to me, ‘If you won’t come see me, let me send you to someone else.’”
The importance of mental health professionals being specifically trained to work with people with personality disorders was discussed. “They (mental health professionals) should all be, you know, trained to work with people who have BPD. They should understand it.” Communicating with consumer advocates was recommended for mental health professionals to improve their understanding of personality disorders. Consumers discussed how they wanted mental health professionals to understand that people with personality disorders can recover.
Theme 2: the need to improve the assessment and diagnosis process
While some participants reported that they did not respond well to the diagnosis initially, others readily embraced the diagnosis. “I liked my diagnosis. I was, like, yes. I know what it is.” Consumers frequently described being given a diagnosis of personality disorder without any explanation or further information about symptoms, or how being provided with this information would help. One participant described receiving a diagnosis following a quick assessment, without receiving an explanation. “I spoke to her (the psychologist) for, maybe, 60 to 90 minutes, and then she diagnosed me with borderline personality disorder… no one gave me any, sort of, information or anything. I was just stuck with this diagnosis and I knew nothing about it.” Consumers described the potential helpfulness of receiving appropriate treatment options when a diagnosis is given, including referral to specialist clinicians. Factsheets that provide information about personality disorders, including symptoms and treatment options, were suggested to be given to consumers at diagnosis. “I’d like a fact sheet that you could – you know. An actual, just, you – you know, this is your diagnosis, these are the symptoms you have with it, here is the available treatment options, here is what happens through with these treatment options.” Consumers described the importance of health professionals assessing for co-occurring mental health or physical health issues.
Theme 3: the need to improve communication between mental health professionals to ensure continuity of care
Consumers described how improved communication between mental health professionals regarding diagnosis, treatment, and hospital discharge is needed . “Then they referred me to the dietician who never came, and that was it, and then they just discharged me.” Participants described disappointment when mental health professionals did not respond to recommendations made by a consumer’s private psychologist, particularly when consumers are experiencing a crisis. “In spite of my psychologist writing a detailed letter with all of my symptoms, the fact that she’s known me for so long, and that she’s sufficiently worried about my safety at this point in time, they were still willing to try and send me back home.” Professionals listening to the advice of a consumer’s psychologist can help consumers feel cared for and help them trust professionals and the mental health system. “She (my psychologist) tried to visit me a couple of times in locked wards and was not allowed in, um, and – and, um, would have been really helpful if she could have just spoken to them and said, ‘Hey, here’s what works for [the person I support],’ but they wouldn’t listen to her.” In addition, it was recommended that professionals share their resources with one another, such as fact sheets, so that consumers can receive the information they require.
The importance of continuity of care was discussed by many participants. “He (psychiatry registrar) says to me, ‘What are you here for?’ And I say, ‘Well, did you read the notes from my last appointment here?’ He said, ‘No. Tell me all about yourself.’” The capacity of a mental health professional to see a consumer for more than a few months may relieve a consumer from the difficulty of repeatedly sharing their past experiences. When a referral to another mental health professional occurs, it may be helpful to provide information on the consumer to assist continuity of care, if consent from consumers is provided. “There hadn’t been any change over from the previous therapist, so we had to start all over again and tell the story for the umpteenth time.” When referring a consumer to another service, professionals could provide some crisis skills training to help consumers while they are in between services. Following up with information that is communicated to consumers was also described as important. “I had a lot of problems with their continuity of service, in, ‘We’ll call you tomorrow,’ and then three days later you get a call back.”
Theme 4: increasing feelings of safety when consumers are experiencing a crisis
Consumers described how first responders often communicated effectively with them and helped them to feel safe and comfortable. “I feel more safe having police and ambos come to my house than I would have an acute care worker come to my house.” However, inappropriate verbal and physical interactions from first responders were also discussed. Consumers described how identifying with the LGBTIQA+ community can result in negative or poor treatment from some first responders.
Some consumers described how acute care units and emergency departments did not provide a safe environment. Consumers described receiving negative judgments from mental health professionals during crises, including being ignored, shamed, denied services or being told that they are “not trying hard enough.” Simple changes to service environments such as allowing curtains to be drawn or receiving positive communication from mental health professionals were described to increase comfort. “They allow you to have the curtains on, so you can calm yourself down.”
Limitations of inpatient wards and emergency departments were described, such as being locked up and alone. Therefore, alternative safe places were suggested for consumers to go to when experiencing distress, such as cafes, respite homes, or rehabilitation centres. “I can’t be alone because I’m not safe enough to be alone, but I don’t need the acute care centres. I just don’t even need to be talking to someone, but I just need to not be alone.”
Theme 5: providing expanded treatment options and increasing service accessibility
Consumers described various ways that treatments and services could be improved. Some consumers discussed the power of art therapy and creative therapies, animal-assisted therapy, nature therapy, and physical therapy. “I found a sexual assault nurse who actually got balloons and filled them with, um, like, paint, and just gave me, like, darts, basketball shooters, the room was just splattered everywhere. It was so colourful that it was a distraction… I find sometimes just having a psychologist isn’t good enough, you need that art therapy; you need the physical therapy.” Several consumers described how peer support could aid them, including providing support groups and safe places where people with lived experience can connect. Consumers also described the helpfulness of 24-h phone lines. One consumer described the usefulness of e-therapy. “He (my psychologist) was prepared to do some sessions remotely by video-conference. You know, so, we were just about to go into the UK at the time, and then it – I didn’t have to break my therapy.” One consumer discussed the benefit of support being provided to carers. “The support group that my mum has been going to… before she’d often just get upset or angry or - whereas now she just seems to be a lot better at knowing what to do without making it worse, kind of thing. So, it’s good.”
Consumers discussed the limited availability of mental health services for personality disorders. Some barriers to accessing mental health services included homelessness, location, and finances . “I wish clinicians understood how cost-prohibitive consistent treatment is for low-income patients.” Non-government organizations were acknowledged by some participants as providing better care compared to government organizations.
Carer perspectives
In this section, five themes from discussions in the carer focus group are presented.
Theme 1: the importance of carer involvement in early assessment and intervention
Carers described how they wanted to be involved during assessment, diagnosis and intervention. Receiving a diagnosis for the person they support was described as taking a lengthy amount of time. “ My biggest issue was getting the diagnosis. Yeah. That took 10 years. Yeah. And the hardest part was that how quick they seem to have – have wanted to keep sending her home.” Frustration was expressed by carers about how mental health professionals often mislabelled a consumer’s difficulties as anxiety, depression, or ‘normal’ behaviours, before later giving a diagnosis of personality disorder. Carers described working hard to find a mental health professional who would provide an assessment or diagnosis for the person they support, particularly during adolescence. “It took yeah, begging and pleading and we are not taking her home until we spoke to a psychiatrist, to tell them our side, and then we got a diagnosis.” After diagnosis, carers emphasized the importance of mental health professionals explaining a personality disorder diagnosis to consumers and carers. The importance of early diagnosis and assessment was highlighted by many carers, such as when a person first experiences a crisis. “ They hit their absolute lowest before there’s a click or a diagnosis into what’s going on, in comparison to trying to seek help for many years, when you can already see many traits .”
Carers discussed the importance of communicating their perspective of the person they support to inform decisions made by mental health professionals, such as diagnosis. Involving carers as soon as possible was recommended, such as during the consumer’s first crisis. Several participants suggested involving carers in treatment helps them to understand what the person they support is learning and experiencing. Confidentiality was described as a barrier to carers being involved in assessment and treatment. “There is no communication, because of this confidentiality. And I think that could be the worst enemy, basically, standing in the way of the family therapy.”
Theme 2: improving responses and follow-up when consumers present in crisis
Mixed feedback was received from carers in relation to the responses from police and ambulance responders. Some negative interactions were described, including physical force by police rather than a dialogue approach. “In one case, the police came and basically… he was thrown on to the floor, you know, with policemen with the guns. It was so traumatic, instead of first having a dialogue approach.” However, many carers described compassionate treatment from police and ambulance responders towards consumers and carers, which was sometimes experienced as comparably better than treatment provided by other mental health professionals during crises. “The first responders are much more caring for carers, family members and explaining what they’re doing, and in their compassionate treatment.”
Carers discussed how consumers can experience difficulties at the emergency department when there are physical health assessments and long wait times for mental health problems. Several carers discussed how separating mental health problems and physical health problems in the emergency department may result in better care. Providing a safe place within the emergency department “that people can go to in a crisis to calm down and self-soothe” was also recommended.
Carers described how consumers were often sent home from the emergency department without appropriate support. “We went to emergency and were sent home with nothing in our first instant… [the person I support] was just sent home to me, with no explanation of anything .” Following discharge from emergency departments or inpatient services, carers recommended that mental health professionals inform consumers and carers about the treatment that was provided and treatment options for the future. Carers proposed that communication between mental health professionals and carers about a consumer’s hospital discharge can help protect the safety of consumers and others. Several carers described not receiving information from mental health professionals unless it was requested by the carer. “Even when [the person I support] was sent home from hospital two times, she was never sent home with anything… Not unless you ask for it.”
Theme 3: increasing mental health professionals’ understanding of personality disorders and improving communication
Carers described the harms of mental health professionals using inappropriate and stigmatizing language when communicating with consumers and carers. The use of recovery-oriented, strengths-based language was desired by carers, such as expressing an understanding of the difficult experiences faced by carers and consumers. Mental health professionals who provided explanations about mental health problems which can be understood by consumers and carers were valued. “I think if they actually remember that this is the first time someone’s hearing it, they actually may be forthcoming with more information.”
Many carers discussed improving training and awareness of personality disorders for health professionals. “If the training is proper – with the GPs, with the doctors, psychiatrists, psychologists, nurses, we have the system right. It’s a matter of just the right education.” Carers described how mental health professionals need to be aware of support that is available and to explain treatment options. Carers also wanted guidance from mental health professionals on how they can best support consumers. “We (carers) need to know what we can do to help them. We want to understand how they feel and why they act/behave the way they do. Please help us to ensure they get the best care and the treatment they need to recover.”
Carers discussed the value of mental health professionals communicating with one another, including providing referral information. When mental health professionals liaise, it can provide a more holistic picture of a person’s difficulties, including physical and psychological symptoms. “[The person I support] has a lot of physical symptoms that I think are a result of her mental state. But I’m not sure. So, they sent her off for all these tests… but there’s no – no one’s like, pulling it all together. The GPs should be, but they don’t.”
Theme 4: improving accessibility and quality of services for consumers
Several carers described limited availability and quality of services within the mental health system, including the public and private healthcare system. “She’s had stays in private hospitals as well. And to be honest, not a lot better. I mean, it’s much nicer place. But I don’t know that the level of care is much better, really, considering how much you pay for it.” The small amount of psychological sessions provided by the public healthcare system was described by carers as insufficient. The proximity of services was also described negatively, including consumers having long commutes to receive treatment. Long wait times to receive treatment were also discussed. “She was on four waitlists in the city at private clinics. One down here in this region. Couldn’t get her in. Christmas Eve, they rang and said, ‘Oh, we’ve got a bed in the city.’ So October, November, December, she was on 24-hour watch. Because I couldn’t get her in anywhere.”
Carers also recommended personalizing therapy for specific consumers, including offering support in nature. Several carers described the helpfulness of DBT. “She (the person I support) ended up being put through a DBT group… that has by far been one of the best things for our entire family.” Carers described how offering employment assistance and peer support groups for consumers may be beneficial.
Theme 5: improving support for carers
Carers described feeling overwhelmed and stressed by caring for a person with personality disorder and suggested carer respite as a valuable form of support. One carer described feeling hopeless after multiple attempts to find a treatment that would work for the person they support. Financial and work difficulties due to time commitments supporting someone with personality disorder were also described. “The Government needs to know is the financial strain on families… with needing weekly psychologist, regular psychiatrist, not being able to get to work, because you get called home all the time.”
Carers discussed the importance of mental health professionals understanding the difficulties experienced by carers. Carers described receiving little support for themselves from mental health professionals. Mental health professionals asking a carer ‘how are you?’ was described as a positive first step. “I had one registered nurse, who was special… who actually asked me how I was. And that was probably year six of the journey. And until then, not a soul had ever asked me how I was.” Other options for providing support to carers were discussed, including a 24-h phone line, peer support groups, counselling for carers, and promoting self-care. Providing educational resources to carers was recommended, such as having brochures in hospital waiting rooms, offering educational groups, and providing links to online information. Several carers recommended increasing public awareness and understanding of personality disorders through education, which may help others in the general community understand the experiences of consumers and carers.
A comparison of the consumer and carer themes can be found in Table 2 . Both consumers and carers described disturbing stigma and prejudice, but also receiving some exemplar care from some professionals. Broadening support options for both consumers and carers was a priority.
This study explored and compared experiences of personality disorder services from the perspectives of consumers and carers. Consumers and carers described a number of negative and positive experiences with mental health services and provided recommendations on how services could improve.
Both consumers and carers discussed the importance of receiving appropriate information when a person is diagnosed with personality disorder, which is consistent with previous research [ 6 , 23 , 31 , 32 ]. Taking a collaborative stance in working with consumers during the assessment and diagnosis process was identified as a way to reduce stigmatization and empower consumers to engage in treatment [ 33 ]. Safety when in crisis was a major concern, both interpersonally (e.g. through promoting compassionate communication) and physically (e.g. avoiding rough handling by authorities, having safe rooms within emergency settings). Consumers also described creating safe places separate from the emergency department, such as voluntary residential or drop-in programs. Previous research indicates that residential programs may be a beneficial alternative to the emergency department for consumers with BPD [ 34 ]. Investigating the carer perspective of alternative safe places and respite options could also be important.
Both positive and negative experiences with mental health professionals and first responders were described by consumers and carers. The literature suggests that stigmatization and discrimination of personality disorder in mental health services continues to be prominent [ 35 ], although professional attitudes toward personality disorder have improved over time [ 36 ]. During crises, consumers and carers expressed receiving better treatment from first responders, compared to mental health professionals, which may mean that mental health professionals have more stigma of personality disorder compared to first responders [ 37 ]. Both groups suggested improving mental health professionals’ knowledge and understanding regarding personality disorders. Research has shown that training can improve mental health professionals’ understanding and attitudes [ 38 , 39 ]. Increasing the accessibility and awareness of training may be required. Providing training to first responders and increasing public awareness of personality disorder may also help reduce stigma and discrimination [ 35 ].
Consumers and carers described the potential benefit of offering peer support to consumers. Peer support can help consumers with various mental health problems by providing shared experiences which offer validation and hope [ 40 , 41 ]. Increasing the number of peer workers and peer support groups for consumers with personality disorder may be valuable. In addition, both carers and consumers described difficulty accessing personality disorder services. Increasing availability of services and making services more affordable may benefit consumers and carers.
From the consumer perspective, importance was given to the therapeutic relationship with mental health professionals, including finding a clinician they can connect with who specializes in personality disorder. This finding is unsurprising given that a strong therapeutic alliance can facilitate recovery [ 42 ]. Consumers described how mental health professionals, such as medical registrars, often did not have sufficient knowledge and experience to support them, and they requested people with experience who had specialized knowledge of personality disorders. Ensuring registrars who work with consumers with personality disorder have appropriate knowledge prior to in-person interactions and are supported by a specialist mental health professional may be helpful. Regarding referrals, health professionals should increase their awareness of personality disorder treatments available in their area, and offer consumers a range of possible mental health professionals that can support them.
Consumers also discussed the importance of continuity of care, including being able to work long term with a mental health professional. Therefore, it is important for mental health professionals to clarify how long they can work with consumers and to provide appropriate support when a consumer is transitioning from one professional to another. In addition, mental health professionals should communicate with one another to ensure they have all necessary information to support a consumer with personality disorder. Collaboration amongst mental health professionals involved in a consumer’s treatment is associated with improved consumer outcomes [ 43 ]. Further, consumers described the importance of private psychologists being able to communicate with other professionals involved in their care during a crisis. With a consumer’s consent, emergency department and inpatient services should collaborate with a consumer’s primary mental health professional, such as a private psychologist.
Expanded therapy options, such as art and animal-assisted therapy, were also recommended by consumers. Previous research has shown that art therapy can help increase well-being and decrease symptoms in consumers with a personality disorder [ 44 ]. Increasing accessibility and affordability of creative therapies and other approaches is recommended to improve referrals and options for consumers.
For carers, importance was placed on early assessment and intervention, which is supported by evidence and treatment guidelines [ 10 , 45 ]. However, consumers did not discuss early intervention, although they have previously described delays in receiving a diagnosis [ 42 ]. Carers also focussed on being involved in the assessment and treatment of the consumers they support, although consumers did not mention this. While carer involvement in assessment and intervention is important to carers and may help them support consumers [ 46 ], the perspective of consumers should be considered because not all consumers endorse family or friend involvement in their care [ 47 , 48 ]. In addition, carers focussed on improving support for carers, including having mental health professionals checking in on carers. However, consumers can have negative experiences of mental health professionals providing support to their carers [ 47 ]. Therefore, professionals may need to find a balance when providing support to consumers and carers. For example, a professional might provide carers with referral information to a psychological education or carer peer support group after consulting with the consumer and clearly explaining the reason for providing support to carers. Alternatively, carers may seek their own supports through mental health professionals and support groups. Table 3 provides a summary guideline of recommendations for health professionals arising from this research.
Limitations and future research
Although data saturation occurred in the analysis of qualitative interviews, the small sample size used in the study may be a limitation as other views may not have been represented [ 49 ]. We did not investigate further the treatment history, specific diagnoses of the consumers, amount of carer engagement with services, or cultural background of participants, meaning it was difficult to estimate to what extent our sample were representative of the broader consumer and carer population. Statements spontaneously reported by consumers and carers did reflect in detail findings from previous studies supporting that our sample was comparative to others in the literature. Further, the sample was predominately female, and the perspectives of male consumers and carers were limited, and it would be important to increase their participation in future research. Consumers and carers were not always asked the same questions, making it difficult to compare their experiences in some topic areas. The groups were ran as semi-structured focus groups and the facilitators followed a guide, but were all responsive to the participants in the focus group and what they wanted to focus on. For example, consumers were not asked about carer involvement in assessment and treatment. Despite the limitations, the findings provide important information to improve services for individuals living with personality disorder and their carers. Future research could explore safe environments for consumers experiencing crisis, and expanded treatment options for personality disorders, including art therapy and peer support. In addition, there is a need to broaden our understanding of the variety and nature of consumer views of having carers involved in their assessment and treatment.
The current study explored and compared mental health service experiences from the perspectives of consumers with personality disorder and carers. The findings add to the ongoing concern about the stigma, prejudice and poor provision of services for people with personality disorder, despite some examples of high quality work being delivered. In addition, the findings highlight similarities and differences in consumer and carer perspectives. Based on the findings, a number of guidelines are provided to inform the practice of health professionals who support consumers with personality disorder.
Availability of data and materials
Data from the current study will not be made available, as participants did not consent for their transcripts to be publicly released. Extracts of participant responses have been made available within the manuscript.
Abbreviations
Borderline personality disorder
Dialectical behavior therapy
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, D.C: American Psychiatric Association; 2013.
Google Scholar
Winsper C, Bilgin A, Thompson A, Marwaha S, Chanen AM, Singh SP, et al. The prevalence of personality disorders in the community: a global systematic review and meta-analysis. Br J Psychiatry. 2019;216:1–10.
Lewis KL, Fanaian M, Kotze B, Grenyer BFS. Mental health presentations to acute psychiatric services: 3-year study of prevalence and readmission risk for personality disorders compared with psychotic, affective, substance or other disorders. BJPsych Open. 2019;5:1–7.
Korzekwa MI, Dell PF, Links PS, Thabane L, Webb SP. Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Compr Psychiatry. 2008;49(4):380–6.
PubMed Google Scholar
Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74:319–28.
Morris C, Smith I, Alwin N. Is contact with adult mental health services helpful for individuals with a diagnosable BPD? A study of service users views in the UK. J Ment Health. 2014;23(5):251–5.
Bailey RC, Grenyer BFS. Supporting a person with personality disorder: a study of carer burden and well-being. J Personal Disord. 2014;28(6):796–809.
Bailey RC, Grenyer BFS. The relationship between expressed emotion and wellbeing for families and carers of a relative with borderline personality disorder. Personal Ment Health. 2015;9(1):21–32.
Dunne E, Rogers B. “It’s us that have to deal with it seven days a week”: Carers and borderline personality disorder. Community Ment Health J. 2013;49(6):643–8.
Grenyer BFS, Ng FY, Townsend ML, Rao S. Personality disorder: a mental health priority area. Aust N Z J Psychiatry. 2017;51(9):872–5.
Commonwealth of Australia. National standards for mental health services. 2010.
Mental Health Commission of Canada. Changing directions changing lives: The mental health strategy for Canada. 2012.
Jørgensen K, Rendtorff JD. Patient participation in mental health care - perspectives of healthcare professionals: an integrative review. Scand J Caring Sci. 2018;32(2):490–501.
Bee P, Brooks H, Fraser C, Lovell K. Professional perspectives on service user and carer involvement in mental health care planning: a qualitative study. Int J Nurs Stud. 2015;52(12):1834–45.
PubMed PubMed Central Google Scholar
Milton AC, Mullan BA. A qualitative exploration of service users’ information needs and preferences when receiving a serious mental health diagnosis. Community Ment Health J. 2015;51(4):459–66.
Lammers J, Happell B. Mental health reforms and their impact on consumer and carer participation: a perspective from Victoria. Australia Issues Ment Health Nurs. 2004;25(3):261–76.
Stomski NJ, Morrison P. Participation in mental healthcare: a qualitative meta-synthesis. Int J Ment Heal Syst. 2017;11(1):67.
Redding A, Maguire N, Johnson G, Maguire T. What is the lived experience of being discharged from a psychiatric inpatient stay? Community Ment Health J. 2017;53(5):568–77.
Goodwin V, Happell B. Consumer and carer participation in mental health care: the carer’s perspective: part 1 - the importance of respect and collaboration. Issues Ment Health Nurs. 2007;28(6):607–23.
Goodwin V, Happell B. Consumer and carer participation in mental health care: the carer’s perspective: part 2—barriers to effective and genuine participation. Issues Ment Health Nurs. 2007;28(6):625–38.
Brennan A, Warren N, Peterson V, Hollander Y, Boscarato K, Lee S. Collaboration in crisis: Carer perspectives on police and mental health professional’s responses to mental health crises. Int J Ment Health Nurs. 2016;25(5):452–61.
Olasoji M, Maude P, McCauley K. Not sick enough: experiences of carers of people with mental illness negotiating care for their relatives with mental health services. J Psychiatr Ment Health Nurs. 2017;24(6):403–11.
CAS PubMed Google Scholar
Lawn S, McMahon J. Experiences of care by Australians with a diagnosis of borderline personality disorder. J Psychiatr Ment Health Nurs. 2015;22(7):510–21.
CAS PubMed PubMed Central Google Scholar
Vandyk A, Bentz A, Bissonette S, Cater C. Why go to the emergency department? Perspectives from persons with borderline personality disorder. Int J Ment Health Nurs. 2019;28(3):757–65.
Lawn S, McMahon J. Experiences of family carers of people diagnosed with borderline personality disorder. J Psychiatr Ment Health Nurs. 2015;22(4):234–43.
Acres K, Loughhead M, Procter N. Carer perspectives of people diagnosed with borderline personality disorder: a scoping review of emergency care responses. Australas Emerg Care. 2019;22(1):34–41.
Lamont E, Dickens GL. Mental health services, care provision, and professional support for people diagnosed with borderline personality disorder: systematic review of service-user, family, and carer perspectives. J Ment Health. 2019:1–15.
Gillard S, Turner K, Neffgen M, Griggs I, Demetriou A. Doing research together: bringing down barriers through the ‘coproduction’ of personality disorder research. Ment Health Rev J. 2010;15(4):29–35.
Braun V, Clarke V, Hayfield N, Terry G. Thematic analysis. In: Liamputtong P, editor. Handbook of research methods in health social sciences. Singapore: Springer Singapore; 2019. p. 843–60.
Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–3.
Buteau E, Dawkins K, Hoffman P. In their own words: improving services and hopefulness for families dealing with BPD. Soc Work Ment Health. 2008;6(1–2):203–14.
Horn N, Johnstone L, Brooke S. Some service user perspectives on the diagnosis of borderline personality disorder. J Ment Health. 2007;16(2):255–69.
Hackmann C, Wilson J, Perkins A, Zeilig H. Collaborative diagnosis between clinician and patient: why to do it and what to consider. BJPsych Adv. 2019;25(4):214–22.
Mortimer-Jones S, Morrison P, Munib A, Paolucci F, Neale S, Hellewell A, et al. Staff and client perspectives of the open Borders programme for people with borderline personality disorder. Int J Ment Health Nurs. 2019;28(4):971–9.
Sheehan L, Nieweglowski K, Corrigan P. The stigma of personality disorders. Curr Psychiatry Rep. 2016;18(1):1–7.
Day NJS, Hunt A, Cortis-Jones L, Grenyer BFS. Clinician attitudes towards borderline personality disorder: a 15-year comparison: attitudes toward borderline personality disorder. Personal Ment Health. 2018;12(4):309–20.
Bonnington O, Rose D. Exploring stigmatisation among people diagnosed with either bipolar disorder or borderline personality disorder: a critical realist analysis. Soc Sci Med. 2014;123:7–17.
Lamph G, Sampson M, Smith D, Williamson G, Guyers M. Can an interactive e-learning training package improve the understanding of personality disorder within mental health professionals? J Ment Health Train Educ Pract. 2018;13(2):124–34.
Welstead HJ, Patrick J, Russ TC, Cooney G, Mulvenna CM, Maclean C, et al. Mentalising skills in generic mental healthcare settings: can we make our day-to-day interactions more therapeutic? BJPsych Bull. 2018;42(3):102–8.
Gillard S, Gibson SL, Holley J, Lucock M. Developing a change model for peer worker interventions in mental health services: a qualitative research study. Epidemiol Psychiatr Sci. 2015;24(05):435–45.
Pallaveshi L, Balachandra K, Subramanian P, Rudnick A. Peer-led and professional-led group interventions for people with co-occurring disorders: a qualitative study. Community Ment Health J. 2014;50(4):388–94.
Ng FYY, Townsend ML, Miller CE, Jewell M, Grenyer BFS. The lived experience of recovery in borderline personality disorder: a qualitative study. Borderline Personal Disord Emot Dysregulation. 2019;6(1):1–9.
Tippin GK, Maranzan KA, Mountain MA. Client outcomes associated with interprofessional care in a community mental health outpatient program. Can J Commun Ment Health. 2016;35(3):83–96.
Haeyen S, van Hooren S, van der Veld WM, Hutschemaekers G. Promoting mental health versus reducing mental illness in art therapy with patients with personality disorders: a quantitative study. Arts Psychother. 2018;58:11–6.
Chanen AM, Thompson KN. Early intervention for personality disorder. Curr Opin Psychol. 2018;21:132–5.
Fitzpatrick S, Wagner AC, Monson CM. Optimizing borderline personality disorder treatment by incorporating significant others: a review and synthesis. Personal Disord Theory Res Treat. 2019;10(4):1–12.
CAS Google Scholar
Wonders L, Honey A, Hancock N. Family inclusion in mental health service planning and delivery: consumers’ perspectives. Community Ment Health J. 2019;55(2):318–30.
Landeweer E, Molewijk B, Hem MH, Pedersen R. Worlds apart? A scoping review addressing different stakeholder perspectives on barriers to family involvement in the care for persons with severe mental illness. BMC Health Serv Res. 2017;17(1):1–10.
Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Download references
Acknowledgements
Charlotte van Schie for inter-rater reliability, and consumers and carers who participated in this study.
NSW Mental Health Commission Lived Experience Framework Implementation Grant, and NSW Ministry of Health support to the Project Air Strategy for Personality Disorders. The funders had no role in the design, recruitment, collection, interpretation, or writing of the study.
Author information
Authors and affiliations.
School of Psychology and Illawarra Health and Medical Research Institute, University of Wollongong, Wollongong, NSW, 2522, Australia
Karlen R. Barr, Michelle L. Townsend & Brin F. S. Grenyer
Project Air Strategy Consumer and Carer Advisory Committee, Wollongong, NSW, Australia
Mahlie Jewell
You can also search for this author in PubMed Google Scholar
Contributions
KRB - study design, participant recruitment, data collection, data analysis, and writing- original draft. MJ and MLT- study design, participant recruitment, data collection, data analysis, and writing- review and editing. BFSG - study design, data collection, and writing- review and editing. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Brin F. S. Grenyer .
Ethics declarations
Ethics approval and consent to participate.
Prior to the start of the study, this study received ethics approval from the University of Wollongong Social Sciences Human Research Ethics Committee (2015/430). All participants were informed of the aims and risks of the study and provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Barr, K.R., Jewell, M., Townsend, M.L. et al. Living with personality disorder and seeking mental health treatment: patients and family members reflect on their experiences. bord personal disord emot dysregul 7 , 21 (2020). https://doi.org/10.1186/s40479-020-00136-4
Download citation
Received : 31 May 2020
Accepted : 11 August 2020
Published : 07 September 2020
DOI : https://doi.org/10.1186/s40479-020-00136-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Personality disorder
- Lived experience
- Qualitative
- Mental health services
Borderline Personality Disorder and Emotion Dysregulation
ISSN: 2051-6673
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
Personality disorder
- Related content
- Peer review
- Orestis Kanter Bax , consultant psychiatrist in medical psychotherapy 1 2 ,
- Dimitrios Chartonas , consultant psychiatrist 2 3 ,
- Jennie Parker , independent lived experience researcher , KUF development lead 2 5 ,
- Spyridon Symniakou , GP partner 6 ,
- Tennyson Lee , consultant psychiatrist in medical psychotherapy , psychoanalyst , honorary senior lecturer 2 4 7 6 8
- 1 Basildon Complex Needs Psychotherapy and Personality Disorder Service, Essex Partnership University NHS Foundation Trust, UK
- 2 Centre for Understanding Personality (CUSP), London
- 3 Camden and Islington Personality Disorder Service, Camden and Islington NHS Foundation Trust
- 4 Deancross Personality Disorder Service, East London NHS Foundation Trust
- 5 Berkshire Healthcare NHS Foundation Trust
- 6 Blithdale Health Centre, Clinical Director East End Health Network
- 7 Institute of Psychoanalysis, British Psychoanalytical Society
- 8 Wolfson Institute, Queen Mary University of London
- Correspondence to O Kanter Bax orestis.kanter-bax{at}nhs.net
What you need to know
Personality disorders are a set of complex emotional difficulties. They are common, often unrecognised, and are associated with mental and physical health comorbidities and reduced life expectancy
Personality disorders are perceived as stigmatising diagnoses. Alternative terms have been proposed. New classification systems help in moving away from rigid use of categorical diagnoses
Assessment and management in primary care require a non-judgmental approach that builds trust through attentiveness, validation, openness, and consistency
Holistic care for people with personality disorders can be improved with reflective practice structures, staff training, collaboration, and team working
Sources and selection criteria
We searched Pubmed, Medline, Embase, the Cochrane Library, CINAHL, PsycINFO, AMED, British Nursing Index, HMIC, and Health Business Elite using the term “personality disorder”. Findings from randomised controlled trials (RCTs), systematic reviews, and meta-analyses were ranked as high in quality (see table 1 ) and we also used our own reference archives, books, and expert contacts to supplement the structured search.
Personality disorders describe a set of long standing complex emotional difficulties, which are common, highly stigmatised, and potentially disabling. They are frequently under-recognised and may run a long course when people lack access to appropriate treatment. Recent developments in evidence, guidelines, and policy have placed an emphasis on public awareness, de-stigmatisation, training professionals in generalist settings, improving access to specialist care, and improving physical health outcomes. 1 2 This article provides an overview of the latest information on the assessment and management of personality disorders in primary care, with an emphasis on borderline personality disorder (also referred to as emotionally unstable personality disorder).
What are personality disorders?
Personality disorders are pervasive and enduring, affecting the emotional, cognitive, and behavioural functioning of a person, expressed in relation to their self (eg, identity, self-evaluation, affect regulation, direction) and others (eg, intimacy, boundaries, sense of security in relationships). People with personality disorders may face difficulties with social functioning at work, with family, and with social life and leisure, and such difficulties may represent a significant deviation from what is expected for the individual’s developmental stage and culture. 3 No consensus exists on a single definition, research in the field is growing rapidly, and controversy surrounds the validity of existing conceptual frameworks. 4 Some people with lived experience and some clinicians question use of the term “personality disorder” altogether, and advocate for its replacement (for example, the term “complex emotional needs” has been proposed). 5
Negative attitudes and biases are still held about people who receive a diagnosis of personality disorder both in the general public 6 7 and among clinicians. 8 Longstanding misconceptions exist about the nature and “untreatability” of personality disorders, but evidence is growing for the efficacy of treatments for borderline personality disorder ( table 1 ) and emerging treatments for antisocial and narcissistic personality difficulties. 12 16
Evidence based treatment for borderline personality disorder 9 10 11
- View inline
What underlies personality disorders?
As with other mental health conditions, genetic and environmental factors contribute to the development of personality disorders. The genetic link is still not well understood 17 18 and evidence on heritability is limited. 19 Genetic factors are thought to interact with the environment to lead to neurobiological changes. 20 Epigenetic effects of the environment on gene expression are also increasingly recognised. 21 Antenatal adversities (eg, increased stress in utero) 22 and adverse childhood experiences, 23 including physical, emotional, and sexual abuse, neglect, and parental mental illness, are associated with an increased risk of a diagnosis of personality disorder in adulthood. 24 In particular, a meta-analysis found that individuals with borderline personality disorder are 13.91 times more likely to report childhood adversity than non-clinical controls and 3.15 times more likely than other people with other psychiatric conditions. 25
Several theoretical models exist that can be clinically useful. Attachment theory provides a model for the understanding of how early disruptions in the infant-caregiver relationship may influence regulation of affect and development of the self. 26 Psychoanalytical object relations theory explains how early internal self and other (object) representations and “patterns” of relating are repeated in adulthood. 27 Adapted cognitive behavioural theory focuses on the effects of conditioning (eg, through invalidating environments) on emotional, cognitive, and behavioural patterns that develop in adulthood. Understanding the complex multi-causal pathways leading to a personality disorder diagnosis can reduce stigma. 28
How common are personality disorders, and who is affected?
Relatively little epidemiological research has been conducted in personality disorders, but estimates of prevalence suggest as many as one in 10 people in the general population has a personality disorder. 29 30 A 2000 study of 303 consecutive primary care attenders estimated that one in four met the criteria for a diagnosis. 31 Estimates of the prevalence in secondary mental healthcare are variable because of heterogeneity of samples, but two literature reviews reported that up to 52% of psychiatric outpatients and up to 70% of patients in inpatient and forensic settings met the criteria for personality disorders, 32 and 12% of patients in outpatient psychiatric clinics and 22% of patients in inpatient psychiatric clinics for borderline personality disorder. 33
Antisocial personality disorder is consistently more common in men than women. 34 There is possible measure or clinician bias in diagnosis of borderline personality disorder in lesbian, gay, and bisexual patients 35 and risk of symptom mislabelling in minority groups, differences in healthcare seeking behaviour between men and women, and mental health risks and barriers for LGBTQ+ populations. 36 Correlation exists between a diagnosis of personality disorder and low socioeconomic status, urbanicity, lower educational attainment, occupational difficulties, and marital discord. 34 Sparse evidence is available on ethnic variations. 37 Clinicians may find it helpful to expand their understanding of the impact of racial trauma 38 and barriers to accessing healthcare for people in black, Asian, and ethnic minority populations.
Prevalence in older populations is about 10%. 39 An underlying and undiagnosed personality disorder may become evident for the first time in older age if disruptions occur in a previously stable life (eg, new onset illness, loss of partner), which lead to decompensation. Differential diagnoses when making a new diagnosis of personality disorder in older people are important (eg, late onset or relapse of other mental or physical illness, including dementia, malignancy, or substance misuse). Evidence suggests a decline in diagnosis of borderline personality disorder with progression of age, indicating a natural improving course in this group. 40 41
How are personality disorders classified?
In ICD-11, 42 released by the World Health Organization in 2018, the clinician is invited to: a) identify the presence of a core problem in functioning of self and interpersonal relating; b) its level of severity (mild, moderate, severe); and c) its main traits : negative affectivity, detachment, dissociality, disinhibition, anankastia (ie, obsessive-compulsive traits), and whether a borderline pattern exists. This classification marked a radical shift away from the categorical classification adopted in ICD-10, DSM-IV, and DSM-5 ( table 2 ), 43 and it allows primary care clinicians to adopt a more pragmatic approach to recognising personality disorder: to look for a core problem, its functional impact and severity, and how this might present in the patient’s relationships and during clinical appointments. 44
Classification systems
DSM-5, which otherwise preserves the categorical approach of DSM-IV, attempts a “hybrid” approach between the categorical and dimensional models, by including an “alternative model” ( table 2 ).
For non-specialist clinicians, awareness of categorical dimensions might be useful, but finer differentiation may be left to the specialist.
How to approach suspected personality disorder
Establishing a specific working framework for the assessment and management of personality disorder can help to prevent exclusion, provide a safe and containing environment, and instil hope. General principles include an open, empathic, and non-judgmental attitude, attentive listening, active and genuine interest, and validation of the patient’s experience. Use a trauma informed approach, which recognises the high prevalence and complex impact of traumatic experiences in personality disorders. 45 46
Box 1 lists some helpful indicators for suspecting personality disorder. Clinicians may be able to incorporate these in their clinical encounters and use them to communicate their patient’s stories and needs to colleagues, while recognising that this list is not exhaustive.
Indicators for personality disorder in non-specialist settings
Strong indicators.
Negative affectivity and affective dysregulation (rapid mood changes, low mood, anxiety, anger, detachment)
Impulse dysregulation (risk taking behaviours, sexual promiscuity, alcohol and substance misuse)
Interpersonal problems: a) In “outside” life (eg, turbulent relationships, violence, dependence, avoidance, isolation); b) In the clinical encounter (eg, increased use of resources, recurrent crises, feeling stuck). In particular, turbulence and volatile relationships tend to be characteristic of borderline personality disorder difficulties
Strong emotional reactions in the clinician during the clinical encounter. Unusual departures from established clinical practice (eg, prescribing out of the ordinary, allocation of clinical time, working outside expertise)
Poor responses to evidence based treatments for other mental health conditions (anxiety, depression, post-traumatic stress disorder)
Additional indicators to look for
Cognitive-perceptual symptoms (rigid or bizarre ideas, antagonism, lack of trust, unusual dissociative or quasi-psychotic symptoms)
Evidence of self-injurious behaviours (scars, marks on skin), significant history of deliberate self-harm and suicidal behaviours
Medically unexplained symptoms 47 48
Parents of children presenting with evidence of deficits in the home environment (eg, neglect, abuse, social adversity, or trauma)
Early adversity and history of trauma (but do not adopt a mechanistic approach, assuming or excluding a diagnosis based on the presence or absence of adversity and trauma)
Childhood diagnosis of emotional disorder, disrupted behaviours, or conduct disorder
Longer initial appointments may be necessary and, where possible, having consistency rather than multiple involved clinicians. Allow time to build trust, tolerate any initial confusion, be open about the service limitations, and adopt an understanding and curious attitude if the person’s requests and demands seem excessive. Strong emotional reactions to patients (positive or negative), observation of unexpected dynamics at play in the doctor-patient interaction or within the team, or deviations from well established practices, may alert the clinician to unconscious repetitions of “patterns” of relating that may complicate the clinical encounter. 49 50
Anxiety, depression, sequelae of a recent trauma or life crisis, or requests relating to an existing diagnosis may in fact be indicators of a personality disorder. Aim to look beyond the apparent presenting symptom and try to understand the individual’s circumstances and their point of view. Simply put, it is essential to get to know a patient and their story. When you formulate their difficulties, try to cover the areas of: 1) sense of self; 2) interpersonal relating; 3) educational and vocational attainment; 4) risk assessment (self-harm and suicide, aggression and violence, risks to dependants and children, risk from others including domestic abuse); 5) hopes and expectations of clinical care. Involve families or carers when appropriate and, with the patient’s consent, seek information from other involved agencies.
Screening tools in primary care are of limited use, but the standardised assessment of personality scale is concise and may help in identifying a personality disorder. 51 Standardised tools can otherwise be used as indicated for mental health screening purposes. 52 Urine drug testing, neuro-imaging, and blood testing may be appropriate in specific cases to exclude other pathologies (eg, in addiction, older adults, and the perinatal period).
Management in primary care
Caring for people with personality disorders in primary care requires a person centred approach that promotes open dialogue and reduces stigma. The goal is not to provide a cure, or “fix” some underlying fault, but to engage in a curious and compassionate way with the person experiencing distress in their attempt to understand and manage their painful experience, even when their wishes and expectations may initially seem unclear or confusing ( box 2 ).
Patient and clinician perspectives on managing personality disorder in primary care
We asked two people to share their experiences of personality disorder. One is a practising GP in the NHS, the other a patient with experience of primary care services during their journey with personality disorder.
It takes a lot to recognise the need for additional support, and once this decision has been made, it can be the start of a very long and emotionally exhausting journey. For most, this starts with a visit to the GP, with the expectation of understanding and perhaps even some answers—medical or other. Someone who can listen without judgment, take the time to get to know us, and show compassion are just a few qualities that can save further distress or misunderstandings on either side. We may not know what we need, or how even to communicate (or comprehend) our thoughts and feelings in a 10 minute appointment. Prior experiences of rejection, abandonment, or attachment difficulties can make it really hard to put our trust in others, including healthcare professionals. Added to this, hidden past or current traumas hinder openness; building a trusting relationship is therefore key to progressing our journey.
We learn to view the world as an unsafe place, where we will not be believed, and that we are not worthy of care. Looking and sounding “OK,” we can come across as malingering—not a term I would choose, but one that fits my interpretation of the invalidating response received at times. All of these are experiences from my own journey over the past 25 years. On reflection, I did expect answers but didn’t really know the question. Part of this journey was through a maze of diagnoses and unhelpful treatments, both medical and psychological. Being referred to services that declined me due to my stigmatising diagnosis, falling between private sector care and the NHS, and repeated assessments or referrals became exhausting and frustrating. The one constant in this journey was my GP practice, perhaps the only place that cannot turn me away and hopefully does not judge based on a mental health label (which I might not even agree with). While I can now see that the remit of a GP is very broad, having someone in the practice that has the skills, time, and compassion to listen and support us in thinking what may be helpful can be invaluable and even life changing.
The question of how we, as a primary care team, can work with people experiencing relational and personality difficulties becomes an almost daily one. In a wider context, primary care unfortunately is becoming increasingly transactional and reactionary, a box ticking exercise, where the complexity of human interaction, continuity as a therapeutic ingredient, and empathy are being replaced by a conveyor belt-like service with e-consultations or orders, and expectations of next day-type delivery by exhausted and burnt out workers. Our commissioners are increasingly relying on numerical indicators to monitor the quantity and quality of our work.
One of the biggest difficulties my team and I face when interacting with a patient with personality disorder is the sense of isolation. Every interaction, especially with someone in need, can be challenging, more so if one has difficulties relating to a person. Lack of trust, breakdown of communication, complexity of presentation, suicidal risk, threatening or dismissive attitude, inconsistencies, lack of a descriptive or explanatory framework can all become barriers to effective clinical practice because they act as magnifying lenses to the difficulties all of us—clinical and non-clinical staff—may experience, and because of the complexity of human nature. This is when I feel most inadequate, full of stress, defensive, persecuted, confused, and hopeless, and this is an experience I share with my team members. But with a reflective space and effective communication between my team and colleagues and the wider mental health and care ecosystem, we can achieve miracles.
Structured management starts with working collaboratively with the person to produce a formulation and understanding of the nature of their difficulties. Consistency, clear communication, and clear boundaries are key. A “contract” between the patient and clinician that will guide their work together from the outset may be helpful 49 to provide clarity about the role and limitations of primary care, establishing clinician and patient responsibilities and modelling realistic expectations. 53
Box 3 outlines management principles, strategies, and techniques that can be used by generalist clinicians and teams.
Management principles, strategies, and techniques
General principles: open, empathic, and non-judgmental attitude; attentive listening; active and genuine interest; validation of the patient’s experience; positive regard that promotes hope; readiness to acknowledge own limitations and mistakes
Acknowledge the patient’s feelings and be aware of your own emotional responses
Be mindful of trauma and its impact on the patient’s life and help-seeking behaviours, and actively aim to avoid re-traumatisation
Be clear and transparent about procedures
Use person centred, co-produced, and mutually agreed treatment plans or “contracts”: negotiated agreements on how the patient and clinician will work with one another to frame the relationship, set goals, establish clear roles and expectations, and manage deviations from what has been agreed
Consider and discuss the use of emotion regulation, distress tolerance, and grounding techniques (muscle relaxation, breathing skills, self-soothing using one’s senses, silence, mindfulness and meditation, yoga postures, exercise)
• Use techniques aimed at improving mentalising during consultations (mentalising refers to the process by which we make sense of ourselves and others, in terms of subjective states and processes (thoughts, feelings, intentions) and impaired mentalising is a core feature of borderline personality disorder 53 )
Share an interview structure plan with the patient, slowing down a chaotic interview and “rewinding” to previously unresolved discussions
Identify and name the underlying emotion: this can help reduce the patient’s levels of anxiety and emotional arousal (anger, elation, sadness/despair, fear) during a consultation
Validate and reflect on the patient experience
Describe your own reflections on the discussion
Invite the patient to reflect from the third position: “What would you tell a friend in this situation?”
Use medications thoughtfully when necessary, and strive to rationalise unnecessary prescribing and polypharmacy; avoid prescribing or changing medications during crises
Encourage lifestyle changes and discuss sleep routines before considering the use of sleeping tablets
Be mindful of mental health comorbidities and treat accordingly, or seek specialist input when required (eg, mood and anxiety disorders, post-traumatic stress disorder, eating disorders, autism spectrum disorder, 54 attention deficit/hyperactivity disorder, intellectual disability 55 56 )
Address problematic alcohol and substances use
Be mindful of increased physical health morbidity, and consider physical health needs
Discuss social needs and encourage structured meaningful activity and social connectedness. Involvement of a primary care mental health practitioner, a social prescriber and peer coach, social care, and third sector organisations may be helpful when indicated
A shared sense of purpose and a culture of cooperation
Team cohesion and mutual support
Formalised regular supervision and reflective practice
Readiness to engage with difficult clinical situations and consider judgment or bias when identified in either colleagues or patients
A culture of reflection and adherence to agreed plans and strategies
Safety management
Establish clear pathways for safety and crisis management
Differentiate and identify an acute escalation in chronic risk and avoid complacency
Have shared safety management plans that are comprehensive and accessible
Encourage strategies to minimise harm in patients who self-harm
Adapting services to meet patients’ needs
Consider what adjustments in service delivery and staff training might improve patient care ( box 4 ). For some patients a long term and trusting relationship with a reliable GP who is genuinely interested may become key in their path to living a more fulfilling life. Chronic difficulties in clinical relationships can develop, however; unhelpful or entangled situations may arise, and this is not rare. Specialist advice or consultation 57 58 may help to resolve this, and reflection can lead to valuable learning from experience for the clinician. Avoid working in isolation, and consider ways to promote reflective spaces and staff wellbeing, to prevent burnout. 59
What can I put in place in my service?
Need specific services and adjustments.
Provide structure and consistency (allocate a named clinician)
Offer scheduled, regular appointments—do not adopt a reactive, crisis management practice
Consider longer appointments (20-30 minutes)
Consider planned telephone contacts with a named doctor
Have reliable and transparent crisis management plans and pathways
Offer bespoke training for first line clinical and reception staff
Put in place regular reflective practice groups across disciplines
Organise peer support, supervision, and clinical practice based meetings with mental health team specialists and/or a local psychiatrist
Establish reliable pathways of communication with local mental health specialists
Offer a tailored-to-need service to resolve complaints and conflict
Integrate a trauma informed approach into policies, procedures, and practices
Shared care, or blended primary and secondary team working, requires reliable communication pathways between all involved agencies. With permission from the patient, make transparent to involved services any treatment “contract” that has been agreed. Openly acknowledge, discuss, and reflect on any deviations from mutual agreements.
Managing safety
Non-suicidal self-injury (self-harm) is common in people with borderline personality disorder (65-80% of cases). 60 The risk of suicide is many times greater than in the general population, 33 with estimates suggesting that up to 10% of people with borderline personality disorder will die by suicide. 61 Plans for safety and crisis management are clinically indicated and actively researched. 62 People who have a personality disorder and are in crisis should access specific local protocols and pathways tailored to their needs. Document up-to-date assessments of the level of risk to self and others, and any safeguarding issues concerning the patient or dependants. Specialist or emergency psychiatry is appropriate for serious and escalating risk patterns.
Medications
Many people with a personality disorder take several drugs, despite an absence of evidence to support the use of any specific medication for the conditions. 63 64 Guidelines from the National Institute for Health and Care Excellence recommend treatment of comorbidities where present as indicated. 65 Recent research highlights the complex interpersonal dynamics that may influence prescribing, especially in patients with personality disorder. 66 67 Reactive prescribing without clear direction, especially during crises, may become a problem. When prescribing, either for physical or mental health, discuss in advance (and in a clear manner) goals, duration of treatment, target symptoms, and potential side effects. Seek informed consent, psychoeducation, and reflection on expectations. 68 69 Consider psychological aspects of resistance to treatment, poor adherence, and medication misuse, and be curious about the meaning of taking and prescribing medication. 70 71 72 If you prescribe without a clear clinical rationale, consider whether this is driven by your emotional reactions in your encounter with the patient. It may be practical to treat symptoms such as insomnia with short courses of medications. We advise specialist input if considering antipsychotic or mood stabilising medications.
When to refer and what to expect
Availability of specialist treatment may vary by region. Involvement of community psychiatry and/or specialist services for personality disorder is indicated for: a) diagnostic clarification; b) assessment of readiness for and choice of specialist treatment; c) case consultation regarding management difficulty and increased risk. Referral to non-specialist talking therapies services—in England through Improving Access to Psychological Therapies (IAPT)—may be appropriate for personality disorder of mild severity and when a full diagnosis is not met. These services may also be appropriate for cases in which focused psychological treatment of a comorbid mental health condition is indicated, if relevant training and resources are available in local provision, but IAPT services may not meet the patients’ needs otherwise. 73
The presence of a diagnosis does not in itself indicate psychological readiness for a specialist treatment programme. The specialist assessment can be demanding, and treatment is not always available or appropriate. In the UK, available specialist programmes are lengthy and require commitment, so that timing and competing priorities need to be considered in advance. Unstable living conditions, uncontrolled alcohol or substance misuse, severe eating disorder, serious risk of harm to self or others, and vulnerability to harm from others may need to be tackled first, with relevant specialist input if necessary (eg, addiction or eating disorder services, adult social services). Canvass patient views, preferences, and goals, based on any previous experience of psychological therapies, at an early stage. 74
Several evidence based treatments, mainly for borderline personality disorder, are available in secondary and tertiary care in the NHS ( table 1 ). No single modality stands out in terms of efficacy, 75 and sometimes multiple treatment attempts may be needed. Brief treatments (such as cognitive behavioural therapy) might not be helpful, and the choice and sequencing of treatments requires specialist involvement. 76
Contact other agencies (eg, probation services, social services, social support agencies for housing, occupation, and activities), as necessary, for support.
Education into practice
What training opportunities could be made available to staff to support their interactions with people who have a personality disorder?
Can you identify one specific barrier that people with a personality disorder may face when trying to access your service?
Useful resources (mainly UK based)
For clinicians.
National Institute for Health and Care Excellence. Personality disorders: borderline and antisocial: https://www.nice.org.uk/guidance/qs88 Updated June 2015.
World Health Organization, ICD-10 Classifications of mental and behavioural disorder: Clinical descriptions and diagnostic guidelines, World Health Organization, 1992: https://icd.who.int/browse10/2016/en
·World Health Organization, ICD-11 Classifications of mental and behavioural disorder: Clinical descriptions and diagnostic guidelines, World Health Organization, 2018: https://icd.who.int/browse11/l-m/en
Balint Society: https://balint.co.uk . Balint group membership provides a space to think about those encounters which leave professionals drained, puzzled, or stuck
Standardised Assessment of Personality—Abbreviated Scale (SAPAS): https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/standardised-assessment-of-personality-abbreviated-scale-sapas-preliminary-validation-of-a-brief-screen-for-personality-disorder/26FB730F35F54B952381AA9C662FF8C2
The Knowledge and Understanding Framework (KUF) national training programme: https://www.westlondon.nhs.uk/our-services/adult/mental-health-services/cassel-hospital/consultation-and-training-services and The National KUF Hub https://twitter.com/nationalkufhub
“Six levels of validation” interpersonal effectiveness skills resource: https://dbtselfhelp.com/dbt-skills-list/interpersonal-effectiveness/validation/
Safer care for patients with personality disorder. National confidential inquiry into suicide and homicide by people with mental illness, University of Manchester. 2018: https://documents.manchester.ac.uk/display.aspx?DocID=37564 Related educational videos “Safer care for patients given a diagnosis of personality disorder: a learning resource”: https://sites.manchester.ac.uk/ncish/resources/safer-care-for-patients-given-a-diagnosis-of-personality-disorder-a-learning-resource/
NHS England and NHS Improvement and the National Collaborating Centre for Mental Health, The Community Mental Health Framework for Adults and Older Adults, September 2019: https://www.england.nhs.uk/wp-content/uploads/2019/09/community-mental-health-framework-for-adults-and-older-adults.pdf
Office for Health Improvement & Disparities Guidance: Working definition of trauma-informed practice and resources: https://www.gov.uk/government/publications/working-definition-of-trauma-informed-practice/working-definition-of-trauma-informed-practice
For patients, families, and carers
For immediate help.
NHS 111 (option 2) can help if you have an urgent medical problem and you’re not sure what to do. Visit https://111.nhs.uk (for people aged 5 and over only) or call 111 (available 24 hours a day, 7 days a week)
With life threatening emergencies, call 999 or go to the nearest emergency department
The Samaritans are there to listen 24 hours a day. Call on 08457 90 90 90 or visit the website at https://www.samaritans.org .
SANEline is a national out-of-hours mental health helpline offering specialist emotional support, guidance, and information to anyone affected by mental illness, including family, friends, and carers. Available every day from 4.30 pm to 10.30 pm on 0300 304 7000: https://www.sane.org.uk/what_we_do/support/helpline
Most areas have a mental health crisis team available 24 hours a day; their contact details should be available via the local council or social services, or they can be contacted via hospital emergency departments.
Text SHOUT: a 24/7 UK based volunteer led text service for anyone in crisis. Developed by the Mental Health Innovations charity: https://www.giveusashout.org/
Other resources
MIND. Personality Disorders leaflet: https://www.mind.org.uk/information-support/types-of-mental-health-problems/personality-disorders/about-personality-disorders/
The National Education Alliance for Borderline Personality Disorder: https://www.borderlinepersonalitydisorder.com/consumer-recovery-resources/ A resource for families and people in recovery, education and training for professionals. (USA)
·The National Service user Network (NSUN) weekly bulletin offers a summary of involvement opportunities as well as policy updates: https://www.nsun.org.uk/
Mindfulness meditation—online resources that some may find helpful: https://www.freemindfulness.org/
Cognitive behavioural therapy based self-help resources and worksheets: https://www.getselfhelp.co.uk/
Dialectical behaviour therapy based self-help resources and worksheets: https://dbtselfhelp.com/
National self-harm network: https://www.nshn.co.uk/
Lifesigns: a user-led organisation working around self-injury: https://www.lifesigns.org.uk/
Rachel Reiland, Get Me Out Of Here: My recovery from borderline personality disorder, Hazelden Publishing, 2002.
Self-injury support: https://www.selfinjurysupport.org.uk/
Multimedia resources
Borderliner Notes: The BORDERLINE film interview Archive: https://www.youtube.com/borderlinernotes
Early Years Parenting Unit at the Anna Freud National Centre for Children and Families, Video Series: EYPU—What is “personality disorder”? https://www.youtube.com/watch?v=38EBpzJDodg What is meant by “good mentalisation”? https://www.youtube.com/watch?v=R5kFPpAMDF0
BBC, Radio I & IXtra Stories. Living with BPD: https://www.bbc.co.uk/programmes/p0700vh4/
BBC Radio 4. Narcissism: https://www.bbc.co.uk/programmes/p06y2j6v
Personality Disorder—subtitles. A film produced by the RCPsych Public Engagement Committee and Damn Fine Media: https://www.youtube.com/watch?v=OnwVTrZcn5s/
Adverse Childhood Experiences (ACEs), Public Health Network Cymru. A short film produced for Public Health Wales and Blackburn with Darwen Local Authority: https://www.youtube.com/watch?v=YiMjTzCnbNQ
RethinkBPD: In conversation: Talks on borderline personality disorder and recovery: https://rethinkbpd.org/
Ending exclusion: research and care for people with complex emotional needs #MHQT: A recording of panel discussion around NIHR mental health policy research unit activities: https://youtu.be/aQoQh66D6N4
Public Health Wales, Adverse Childhood Experience (ACE) and Adult Mental Well-Being Wales infograph. 2016: http://www.wales.nhs.uk/sitesplus/documents/888/embargoed%20final%20-%20ace%20%26%20mental%20well-being%20infograph%20e.pdf
Selected readings
Gask L, Evans M, Kessler D. Personality disorder. BMJ 2013;347:f5276
Schrift M, Personality disorders. BMJ Best Practice. 2019
RCPsych Position statement, services for people diagnosable with personality disorders. 2020
NIMHE Personality disorder: no longer a diagnosis of exclusion—policy implementation guidance for the development of services for people with personality disorder. 2003
NIMHE Breaking the cycle of rejection. The Personality Disorders Capabilities Framework. 2003
Bolton W, Lovell K, Morgan L, Wood H, Meeting the challenge, making a difference. Working effectively to support people with personality disorder in the Community. Project report, Department of Health, London. 2014. http://repository.tavistockandportman.ac.uk/864/1/Heather_Wood_-_MeetingTheChallenge.pdf
Mind, Centre for Mental Health, Royal College of Nursing, The British Association of Social Workers, Royal College of General Practitioners, The British Psychological Society, Anna Freud National Centre for Children and Families, Barnet, Enfield, and Haringey Mental Health NHS Trust. Shining lights in dark corners of people’s lives, The consensus statement for people with complex mental health difficulties who are diagnosed with a personality disorder. 2018: https://www.mind.org.uk/media/21163353/consensus-statement-final.pdf
How patients were involved in the creation of this article
JP, a co-author on this paper, has lived experience of personality disorder. Her insights were essential in giving it its final form. An anonymised patient perspective statement has also been included with consent from the author.
Contributors: OKB is the lead author and guarantor of the content of the paper. OKB designed the initial outline and OKB, DC, JP, SS and TL all contributed equally thereafter to writing the final version.
Competing interests: The BMJ has judged that there are no disqualifying financial ties to commercial companies. The authors declare the following other interests: none.
Further details of The BMJ policy on financial interests are here: https://www.bmj.com/about-bmj/resources-authors/forms-policies-and-checklists/declaration-competing-interests
Provenance and peer review : commissioned; externally peer reviewed.
- Hoffman P ,
- Global Alliance for Prevention and Early Intervention for Borderline Personality Disorder
- American Psychiatric Association
- ↵ Livesley J. Handbook of personality disorders. Second Edition: Theory, research and treatment. Guilford Publications, 2018.
- Sheridan Rains L ,
- Sheehan L ,
- Nieweglowski K ,
- Chartonas D ,
- Kyratsous M ,
- Dracass S ,
- Stoffers JM ,
- Choi-Kain LW ,
- Masland SR ,
- Jenkins JA ,
- Bateman A ,
- O’Connell J ,
- Lorenzini N ,
- Gardner T ,
- Simsek-Duran F ,
- McCormick B ,
- Attwood G ,
- Miloseska K ,
- Diamond D ,
- Yeomans F ,
- Martín-Blanco A ,
- Moffitt TE ,
- Reichborn-Kjennerud T
- Gescher DM ,
- Hillemacher T ,
- Frieling H ,
- Brannigan R ,
- Tanskanen A ,
- Huttunen MO ,
- Battle CL ,
- Johnson DM ,
- Palmier-Claus J ,
- Branitsky A ,
- Mansell W ,
- Warwick H ,
- Johnson BN ,
- Clouthier TL ,
- Caligor E ,
- Hörz-Sagstetter S ,
- Volkert J ,
- Gablonski TC ,
- Torgersen S ,
- Kringlen E ,
- Jenkins R ,
- Blizard R ,
- Beckwith H ,
- Ellison WD ,
- Rosenstein LK ,
- Morgan TA ,
- Zimmerman M
- Roberts A ,
- Rodriguez-Seijas C ,
- Semlyen J ,
- McGilloway A ,
- Nicolas G ,
- Abrams RC ,
- Horowitz SV
- Álvarez-Tomás I ,
- Guilera G ,
- Zanarini MC ,
- Frankenburg FR ,
- ↵ World Health Organization. International statistical classification of diseases and related health problems (11th Revision). 2018. https://icd.who.int/browse11/l-m/en
- van der Kolk BA
- Stubley J ,
- ↵ Royal College of General Practitioners and the Royal College of Psychiatrists, CR152, The management of patients with physical and psychological problems in primary care: a practical guide, Report of a joint working group of the, January ref incomplete??? 2009.
- Hatcher S ,
- Walters P ,
- Thornicroft G ,
- ↵ Schrift M, Personality disorders. BMJ Best Practice. 2019.
- Bateman AW ,
- Lovejoy C ,
- Cassidy S ,
- Allison C ,
- Baron-Cohen S
- Carrington A ,
- Herbert A ,
- British Medical Association, Caring for the Mental Health of the Medical Workforce
- Cornelius J ,
- Borschmann R ,
- Barrett B ,
- Hellier JM ,
- Crawford MJ ,
- Bhatti SF ,
- Stoffers-Winterling JM ,
- Storebø OJ ,
- Pereira Ribeiro J ,
- ↵ National Institute for Health and Care Excellence. Personality disorders: borderline and antisocial. https://www.nice.org.uk/guidance/qs88 2015.
- Martean L ,
- Konstantinidou H
- ↵ Francois D, Roth SD, Klingman D. The efficacy of pharmacotherapy for borderline personality disorder: a review of the available randomized controlled trials. Psychiatric Ann 2015;45:431-7.
- Gabbard G ,
- Weinberg E ,
- Konstantinidou H ,
- Rogalski D ,
- Goddard E ,
- Wingrove J ,
- Roughley M ,
- Maguire A ,
- Cristea IA ,
- Gentili C ,
- Palomba D ,
- Albert EB ,
- Gunderson JG
Loading metrics
Open Access
Peer-reviewed
Research Article
Discovering Relations Between Mind, Brain, and Mental Disorders Using Topic Mapping
* E-mail: [email protected]
Affiliation Imaging Research Center and Departments of Psychology and Neurobiology, University of Texas, Austin, Texas, United States of America
Affiliation NASA Ames Research Center, Mountain View, California, United States of America
Affiliation Department of Electrical and Computer Engineering, University of Texas, Austin, Texas, United States of America
Affiliation Department of Psychology, Colorado University, Boulder, Colorado, United States of America
- Russell A. Poldrack,
- Jeanette A. Mumford,
- Tom Schonberg,
- Donald Kalar,
- Bishal Barman,
- Tal Yarkoni

- Published: October 11, 2012
- https://doi.org/10.1371/journal.pcbi.1002707
- Reader Comments
Neuroimaging research has largely focused on the identification of associations between brain activation and specific mental functions. Here we show that data mining techniques applied to a large database of neuroimaging results can be used to identify the conceptual structure of mental functions and their mapping to brain systems. This analysis confirms many current ideas regarding the neural organization of cognition, but also provides some new insights into the roles of particular brain systems in mental function. We further show that the same methods can be used to identify the relations between mental disorders. Finally, we show that these two approaches can be combined to empirically identify novel relations between mental disorders and mental functions via their common involvement of particular brain networks. This approach has the potential to discover novel endophenotypes for neuropsychiatric disorders and to better characterize the structure of these disorders and the relations between them.
Author Summary
One of the major challenges of neuroscience research is to integrate the results of the large number of published research studies in order to better understand how psychological functions are mapped onto brain systems. In this research, we take advantage of a large database of neuroimaging studies, along with text mining methods, to extract information about the topics that are found in the brain imaging literature and their mapping onto reported brain activation data. We also show that this method can be used to identify new relations between psychological functions and mental disorders, through their shared brain activity patterns. This work provides a new way to discover the underlying structure that relates brain function and mental processes.
Citation: Poldrack RA, Mumford JA, Schonberg T, Kalar D, Barman B, Yarkoni T (2012) Discovering Relations Between Mind, Brain, and Mental Disorders Using Topic Mapping. PLoS Comput Biol 8(10): e1002707. https://doi.org/10.1371/journal.pcbi.1002707
Editor: Olaf Sporns, Indiana University, United States of America
Received: May 14, 2012; Accepted: August 2, 2012; Published: October 11, 2012
Copyright: © Poldrack et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: This work was supported by NIH grant RO1MH082795 (to RAP) and F32NR012081 (to TY) and by the Texas Emerging Technology Fund. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript
Competing interests: The authors have declared that no competing interests exist.
Introduction
The search for clues regarding the underlying causes of mental disorders has led to the notion that these disorders may be best understood in terms of a set of underlying psychological and/or neural mechanisms that stand between genes and environment on the one hand and psychiatric diagnoses on the other hand. Such intermediate phenotypes, or “endophenotypes”, may provide the traction that has eluded research using diagnostic categories as primary phenotypes [1] , [2] . They may also provide the means to better understand the structure the underlying psychological dimensions that appear to underlie overlapping categories of mental disorders [3] , [4] .
The identification of endophenotypes requires an understanding the basic structure of mental functions and their associated brain networks. For more than 30 years, cognitive neuroscientists have used neuroimaging methods (including EEG/MEG, PET, and fMRI) in an attempt to address this question. This work has led to a large body of knowledge about associations between specific psychological processes or tasks and activity in brain regions or networks. However, this knowledge has not led to a commensurate improvement in our understanding of the basic mental operations that may be subserved by particular brain systems. Instead, diverse literatures often assign widely varying functions to the same networks. A prime example is the anterior cingulate cortex, which has been associated with such widespread functions as conflict monitoring, error processing, pain, and interoceptive awareness. In order to understand the unique functions that are subserved by brain regions or networks, a different approach is necessary; namely, we need to analyze data obtained across a broad range of mental domains and understand how these domains are organized with regard to neural function and structure.
The identification of basic operations can be understood statistically as a problem of latent structure identification; that is, what are the latent underlying mental functions and brain networks that give rise to to the broad range of observed behaviors and patterns of brain activity and neuropsychiatric disorders? The focus within cognitive neuroscience on establishing associations between activation and specific hypothesized processes has hindered the ability to identify such latent structures. However, within the fields of machine learning and text mining, a number of powerful approaches have been developed to estimate the latent structure that generates observed data, assuming that large enough datasets are available. In the present work, we take advantage of one class of such generative models to develop a new approach to identifying the underlying latent structure of mental processing and the associated brain functions, which we refer to as “topic mapping”. We examine the latent conceptual structure of the fMRI literature by mining the full text from a large text corpus comprising more than 5,800 articles from the neuroimaging literature, and model the relation between these topics and associated brain activation using automated methods for extracting activation coordinates from published papers. This analysis uncovers conceptual structure and activation patterns consistent with those observed in previous neuroimaging meta-analyses, which provides confirmation of the approach, while also providing some novel suggestions regarding structure/function relationships. We then use this approach to identify the topical structure of terms related neuropsychiatric diseases, and use multivariate methods to identify relations between these the mental and disorder domains based on common brain activation patterns. This approach provides an empirical means of discovering novel endophenotypes that may underlie mental disorders, as well providing new insights into the relations between diagnostic categories.
Within the fields of information retrieval and computer science, research into document retrieval has led to the development of a set of techniques for estimating the latent structure underlying a set of documents. Early work in this area treated documents as vectors in a high-dimensional space, and used matrix decomposition techniques such as singular value decomposition to identify the latent semantic structure of the documents [5] . More recently, researchers in this domain have developed approaches that are based on generative models of documents. One popular approach, known generically as “topic models” [6] , treats each document as a mixture of a small number of underlying “topics”, each of which is associated with a distribution over words. Generating a document via this model involves sampling a topic and then sampling over words within the chosen topic; using Bayesian estimation techniques, it is possible to invert this model and estimate the topic and word distributions given a set of documents. The particular topic modeling technique that we employ here, known as latent Dirichlet allocation (LDA: [7] ), has been shown to be highly effective at extracting the structure of large text corpuses. For example [8] , used this approach to characterize the topical structure of science by analyzing 10 years of abstracts from PNAS , showing that it was able to accurately extract the conceptual structure of this domain.
We characterized the latent structure of the cognitive neuroscience literature by applying latent Dirichlet allocation to a corpus of 5,809 articles (using an expanded version of the corpus developed in [9] ), which were selected on the basis of reporting fMRI activation in a standardized coordinate format. An overview of the entire data processing workflow is presented in Figure 1 . This technique estimates a number of underlying latent “topics” that generate the observed text, where each topic is defined by a distribution over words. The dimensionality (i.e., number of topics) is estimated using a cross-validation approach; the documents are randomly split into 8 sets, and for each set a topic model is trained on the remaining data and then used to estimate the empirical likelihood of the held-out documents [10] . Plots of the empirical likelihood of left-out documents as a function of the number of topics are shown in Figure 2 , and histograms of the number of documents per topic and number of topics per document are shown in figure 3 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pcbi.1002707.g001
https://doi.org/10.1371/journal.pcbi.1002707.g002
https://doi.org/10.1371/journal.pcbi.1002707.g003
Initial application of LDA to the full-text corpus identified a number of topics that were related to mental function, but also many topics related to methodological or linguistic aspects of the documents. Because we were specifically interested in estimating the conceptual structure of mental processes, we examined each document in the corpus and identified each occurrence of any of the 605 terms (both single words and phrases) that are present as mental concepts in the Cognitive Atlas ( http://www.cognitiveatlas.org ); the topic model was then estimated using this limited word set (treating each word or phrase as a single-word token). The Cognitive Atlas is a curated collaborative ontology that aims to describe mental functions, and contains terms spanning across nearly all domains of psychological function [11] . The cross-validation analysis identified 130 as the optimal number of topics for this dataset. Examples of these topics are shown in Figure 4 , and the full list is presented in Table S1 . In large part these topics are consistent with the topics that are the focus of research in the cognitive neuroscience literature. The topics with the highest number of associated documents were those related to very common features of neuroimaging tasks such as movement (topic 20), emotion (topic 93), audition (topic 74), attention (topic 43), and working memory (topic 61). Each of these was associated with more than 400 documents in the corpus. At the other end of the spectrum were more focused topics that loaded on fewer than 200 documents, such as topic 121 (regret,surprise), topic 71 (narrative, discourse), and topic 108 (empathy, pain). The results of this analysis suggest that topic modeling applied to the limited term set of mental functions can successfully extract the conceptual structure of psychological processes at multiple levels within the current text corpus.
https://doi.org/10.1371/journal.pcbi.1002707.g004
In order to further examine the effects of topic dimensionality, we compared the results obtained across several values for the number of topics (10,50, 100, and 250). We chose the term “language” and identified all topics for each model in which that term occurred in the top five terms. We then examined the correlation in the loading vector across documents for each set of levels, in order to identify the hierarchical graph relating topics across levels (see Figure 5 ). This analysis showed that increasing the topic dimensionality resulted in finer-grained topics; for example, with 10 topics there was a single matching topic that included “meaning”, “reading”, and “comprehension”, whereas each of these was split into a separate set of topics in the 50-topic model, and further subdivided as the dimensionality increased. This suggests that although the cross validation resulted in a particular “best” dimensionality, in reality there is relevant information at many different levels which differs in grain size.
All topics with “language in their top 5 terms were first identified from the results for topic models fit to the data at 10, 50, 100, and 250 topics. At each level, each topic is linked to the topic at the previous level with which it had the highest correlation in its document loadings. The values on each edge reflect the correlation in the topic loading vector across documents between the two levels.
https://doi.org/10.1371/journal.pcbi.1002707.g005
Topic mapping
While concordance with the existing literature is reassuring, the true promise of this approach is in its ability to uncover novel associations between functions and activation, and the topic mapping analysis did in fact identify some unexpected associations, particularly when looking at negative associations. Two interesting examples are evident in Figure 4 . First, topic 61 was associated with the bilateral fronto-parietal network usually associated with working memory, but it also exhibited strong and focused negative association in the right amygdala; this means that the amygdala was significantly less likely to be activated in studies that loaded on this topic relative to those that did not. This is particularly interesting in light of further exploration of the literature using the PubBrain tool ( http://www.pubbrain.org ) which identified a number of studies that have noted amygdala activation in association with working memory tasks (cf. [13] ). Another example is topic 71 (associated with auditory processing) which was negatively associated with activation in a broad set of regions previously implicated in emotional function, such as orbitofrontal cortex, striatum, and amygdala. Whether such negative associations reflect truly negative relations in activation between these networks or reflect features of the tasks used in these domains remains to be determined, but such unexpected associations could suggest novel hypotheses about relations between specific brain networks. These are only two examples of potential novel discoveries using Topic Mapping.; future studies will be needed to systematically examine all possible new findings emerging from the usage of this tool.
Mapping the neural basis of neuropsychiatric disorders
Based on the results from the foregoing analyses, we then examined whether it was possible to obtain new insights about the organization of brain disorders using the topic mapping approach developed above. We estimated a set of topics using only terms related to brain disorders, based on a lexicon of mental disorders terms derived from the NIFSTD Dysfunction ontology [14] along with the DSM-IV. The optimal dimensionality of 60 based on cross-validation was found to produce multiple topics with exactly the same word distribution, so we used the largest number of topics yielding a unique set of word distributions across topics, which was 29 topics. Examples of these topics and the associated topic maps are presented in Figure 6 .
Topics are ordered in terms of the number of documents loading on the topic; color maps reflect the correlation coefficient between topic loading and activation across documents. The images are presented in radiological convention (i.e., left-right reversed).
https://doi.org/10.1371/journal.pcbi.1002707.g006
The results of this analysis are largely consistent with results from prior meta-analyses and known functional anatomy of the various disorders, but are novel in highlighting relations between some of the disorders. For example, Topic 7 demonstrates the relations between bipolar disorder, schizophrenia, and mood disorders, with activation centered on the medial prefrontal cortex, basal ganglia, and amygdala. Topic 8 highlights relations between obesity and eating disorders and drug abuse, with activation in the ventral striatum and ventromedial prefrontal cortex. Topic 14 demonstrates relations between a set of externalizing disorders (drug abuse, conduct disorder, alcoholism, antisocial personality disorder, and cannabis related disorder) with activation focused in the striatum, amygdala, orbitofrontal cortex, and dorsal prefrontal cortex. Conversely, Topic 25 demonstrates relations between a set of internalizing disorders (anxiety disorder, panic disorder, phobia, obsessive compulsive disorder, agoraphobia, and post traumatic stress disorder), with a very similar pattern of activation, though notably weaker in the striatum. One striking result of these analyses is the similarity of the patterns of brain activity associated with the mention of all of these different disorders. This could arise either from the fact that this particular set of limbic brain systems is the seat of all major psychiatric disorders, or the fact that these disorders are commonly mentioned in relation to tasks or cognitive domains that happen to preferentially engage these brain systems.
We further characterized the relations between different disorder concepts in their associated neural activations by clustering the disorder topics based on their associated brain activation patterns using hierarchical clustering. The results of this analysis are shown in Figure 7 . The results show the degree to which the neural patterns associated with the use of particular sets of mental disorder terms exhibit a consistent systematic structure. The clustering breaks into four large groups, comprising language disorders, mood/anxiety disorders and drug abuse, psychotic disorders, and autism and memory disorders. What is particularly interesting is that, although none of the topic maps associated with the term “schizophrenia” showed strong activation, the fact that they cluster together in this analysis suggests that they are nonetheless similar in the patterns of activation that are reported in the associated papers; however, this could also reflect the fact that a relatively small number of tasks is used in the literature, and thus any concordance could be driven by overlap of tasks that are commonly mentioned in the context of schizophrenia. Despite such limitations, these results provide further confirmation that the present analysis, while largely based on studies involving healthy adults, can nonetheless accurately characterize the neural basis of mental disorders as described in the literature.
Euclidean distance was used as the distance metric for clustering, and hierarchical clustering was performed using Ward's method. The colored blocks show the four major groupings obtained by cutting the tree at a height of 2.0. Abbreviations: APH: aphasia, DLX:dyslexia, SLI: specific language impairment, DA: drug abuse, AD:Alzheimer's disease, DEP:depressive disorder, MDD:major depressive disorder, ANX:anxiety disorder, PAN: panic disorder, BPD: bipolar disorder, CD: conduct disorder, GAM: gambling, MD: mood disorder, PD: Parkinson's disease, OCD: obsessive compulsive disorder, PHO: phobia, EAT: eating disorder, SZ: schizophrenia, OBE: obesity, COC: cocaine related disorder, PSY: psychotic disorder, PAR: paranoid disorder, SZTY: schizotypal personality disorder, TIC: tic disorder, ALC: alcoholism, ALX: alexia, ADD: attention deficit disorder, AMN: amnesia, AUT: autism, ASP: Asperger syndrome.
https://doi.org/10.1371/journal.pcbi.1002707.g007

Empirical discovery of endophenotypes
https://doi.org/10.1371/journal.pcbi.1002707.t001
The first canonical variate (#0) demonstrated associations between a number of both internalizing and externalizing disorders (anxiety, depression, obesity, gambling) which were centered around the involvement of emotional processes (such as mood and fear) and reward-related decision processes. Another canonical variate (#1) was focused on memory processes, and identified a cluster of disorders including classical memory disorders (amnesia and Alzheimer's disease) as well as schizophrenia. Another (#2) focused on language processes and was associated with activity in left prefrontal, temporal, and parietal regions.
The results of the CCA analysis provide a potential new window into the complex psychological and neural underpinnings of schizophrenia and its relation to other psychiatric disorders. Across different canonical variates, schizophrenia is related to mood and decision making processes (components 0 and 3), memory processes (component 5), and social perception (component 10). These could potentially relate to different aspects of schizophrenic symptomatology, such as the distinctions between positive versus negative symptoms or between cognitive versus affective impairments. Further, they provide novel potential targets for genetic association studies, which have struggled to identify meaningful and replicable associations between schizophrenic symptoms or endophenotypes and genetic polymorphisms (cf. [16] ).
We also performed CCA directly using topic-document loading vectors, in order to determine whether the results differed from CCA computed on neural loading vectors; the results are presented in Table 2 . The results of this analysis are quite concordant with the foregoing analyses based on activation patterns, but one noticeable difference between the two analyses is that the activation-based CCA analysis appeared to cluster disorders more broadly, whereas many of the components found in the text-based analysis had only a single disorder. This may reflect the fact that disorders are less neurally distinct than is suggested by what is written by authors, but could also reflect greater noise in the neural data; further work will be necessary to better understand the unique contributions of activation-based and text-based analyses.
https://doi.org/10.1371/journal.pcbi.1002707.t002
It is clear that neuroimaging can provide important evidence regarding the functional organization of the brain, but one of the most fundamental questions in cognitive neuroscience has been whether it can provide any new insights into psychological function [17] – [19] . The results presented here demonstrate how large databases of neuroimaging data can provide new insights into the structure of psychological processes, by laying bare their relations within a similarity space defined by neural function. The present results highlight the importance of “discovery science” approaches that take advantage of modern statistical techniques to characterize large, high-dimensional datasets (cf. [20] ). Just as the fields of molecular biology and genomics have been revolutionized by this approach [21] , we propose that the hypothesis-generating approach supported by data mining tools can serve as a powerful complement to more standard hypothesis-testing approaches [22] .
There is growing recognition that the diagnostic categories used in psychiatry are not reflective of sharp parallel biological distinctions; instead, a growing body of behavioral, genetic, and neuroimaging data suggest that these different disorders fall along a set of underlying continuous dimensions which likely relate to particular basic psychological processes [3] , [4] . The results presented here are consistent with that viewpoint, and further show how endophenotypes for groups of disorders can be empirically discovered via data mining, even if those disorders were not the primary aims of the studies being mined. This approach would likely be even more powerful using databases that were focused on imaging data from studies of patients. In addition, this approach has the potential to characterize the genetic architecture of these disorders through mining of genetic association data; unfortunately, genetic terms are not sufficiently frequent in the Neurosynth database to support robust mapping of relationships to genes, but future analyses using enhanced databases has the potential to discover additional relations between neurocognitive components and genetic contributions.
The present work is limited by several features of the data that were used in the analyses. The first limitation arises from the fact that we rely upon the presence of particular terms in the text, rather than on manual annotation of the relevance of those terms. Thus, obvious issues such as polysemy (e.g., the multiple senses of the term “working memory”) and negation can be problematic, though these issues could potentially be addressed using more powerful natural language processing. A second limitation arises from the meta-analytic nature of the activation data used in the analyses, which are reconstructed from a very sparse representation of the original data. A third limitation is that the activation maps are associated only with complete documents, not with specific terms within the document, and this coarseness undoubtedly adds a significant amount of noise to the modeling results. These limitations necessitate caution in drawing strong conclusions from the results reported here. At the same time, the concordance of many of the results with previous analyses using different datasets and analysis approaches suggests that these limitations have not greatly undermined the power of the technique. We propose that the approach outlined here is likely to be most useful for inspiring novel hypotheses rather than for confirming existing hypotheses, which means that any such results will be just the first step in a research program that must also include hypothesis-driven experimentation.
Another potential limitation of the present work is that the fact that a number of the parameters in the analyses were set arbitrarily. While the dimensionality of the topic models was determined using an automated method, there remain parameter settings (such as smoothness of the word and topic distributions) that must be chosen arbitrarily (in our case, we chose them based on previously published results). The results of the topic model are quite robust; for example, we saw very similar results when performing the topic models on the original set of 4,393 papers from the earlier paper by Yarkoni et al. compared to the results from the corpus of 5,809 papers. It is also evident from Figure 5 that there is strong continuity in topics across different dimensionalities, with single topics at lower dimensionalities splitting into multiple finer-grained topics at higher dimensionalities. We have chosen model parameters that appear to give sensible results relative to prior findings, but the possibility remains that different parameterizations or analysis approaches could lead to different outcomes; future research will need to explore this question in more detail. We would also note that some of these limitations may be offset by the fact that the analyses presented here are almost fully automated, which removes many possible opportunities for research bias to affect the results.
The present work follows and extends other recent work that has aimed to mine the relations between mental function and brain function using coordinate-based meta-analyses. Smith et al. [23] analyzed the BrainMap database (which is similar to the database used here, but is created via manual annotation and thus has lower coverage but greater specificity and accuracy than the Neurosynth database). This work showed that independent components analysis applied to the meta-analytic data was able to identify networks very similar to those observed in resting-state fMRI time series, and that these could be related to specific aspects of psychological function via the annotations in the BrainMap database. Laird et al [24] extended this by showing that behavioral functions could be clustered together based on these meta-analytic maps. The present work further extends those previous studies by showing that the structure of the psychological domain can be identified in an unsupervised manner using topic modeling across both cognitive function and mental disorder domains, and that these can further be used to identify potential endophenotypes that share common neural patterns across these two domains. Visual examination of the ICA components presented in the Smith and Laird papers shows substantial overlap with the topic maps identified in the present study. In future work, we hope to directly compare the topic mapping results with the maps identified in those papers, to further characterize the utility of each approach.
In summary, we have shown how large neuroimaging and text databases can be used to identify novel relations between brain, mind, and mental disorders. The approach developed here has the potential to enable new discoveries about the neural and cognitive bases of neuropsychiatric disorders, and to provide empirically-driven functional characterizations of patterns of brain activation. The results also highlight the importance of the availability of large open datasets in cognitive neuroscience to enable discovery-based science as a complement to hypothesis-driven research.
Materials and Methods
Code to implement all of the analyses reported here, along with all of the auxiliary files, are available at https://github.com/poldrack/LatentStructure .
Data extraction
The full text from the Neurosynth corpus was used for the text mining analyses. The sources of these data as well as the process for automated extraction of activation coordinates are described in detail in [9] .
Peak image creation
Synthetic activation peak images were created from the extracted activation coordinates by placing a sphere (10 mm radius) at each activation location, at 3 mm resolution using the MNI305 template. Activations detected to be in Talairach space were first converted to MNI305 coordinates using the Lancaster transform [25] .
Topic modeling
We ran two topic modeling analyses using limited sets of terms to obtain focused topics in specific domains. In the first, we used 605 mental concept terms from the Cognitive Atlas database mentioned previously. In the second, we used a set of 55 terms describing mental disorders; these were obtained by taking the NIFSTD Dysfunction ontology and removing all terms not relevant to psychiatric disorders, and then adding a set of missing terms that described additional disorders listed in the DSM-IV. In each case, we processed the full text corpus and created restricted documents containing only terms that were present in the respective term list (along with synonyms, which were mapped back to the base term), and then performed topic modeling on those restricted documents. The median number of terms per document after filtering was 127 for cognitive terms and 3 for disease terms.
For each dataset, the optimal number of topics was determined by performing a grid search across a range of dimensionality values (from 10 to 250 in steps of 10). Each document set was split into 8 random sets of documents, and 8 separate models were trained, in each case leaving out one subset of documents. The empirical likelihood of the left-out documents was then estimated using an importance sampling method as implemented in MALLET [10] .
In order to identify the hierarchical relations between topics across different dimensionalities (as shown in Figure 5 ), the topic models from the first crossvalidation fold for each level (10, 50, 100, and 250 topics) were used; because 1/8 of the data were excluded as test data, these models were thus trained on a total of 5082 documents (using the same documents across all different dimensionalities). Hierarchical relations between levels were identified by computing the correlation between the document loading vectors for each lower-level topic and all higher-level topics, and then assigning the link according to the maximum correlation.
Disorder clustering
Disorders were clustered using hierarchical clustering (Ward's method) applied to the Euclidean distance matrix computed across voxels for the disorder-based topic maps (Pearson r values).
Canonical correlation analysis
Supporting Information
Complete list of topics identified through application of latent Dirichlet allocation to the text corpus filtered for Cognitive Atlas terms. The top 5 words shown for each topic are those which had the highest loading for that topic across documents. The number of documents that loaded on each topic is also listed.
https://doi.org/10.1371/journal.pcbi.1002707.s001
Complete list of topics identified through application of latent Dirichlet allocation to the text corpus filtered for mental disorder terms. The top 5 words shown for each topic are those which had the highest loading for that topic across documents. The number of documents that loaded on each topic is also listed.
https://doi.org/10.1371/journal.pcbi.1002707.s002
Acknowledgments
Thanks to Robert Bilder, Eliza Congdon, Steve Hanson, Oluwasanmi Koyejo, Jonathan Pillow, and Fred Sabb for helpful comments on a draft of this paper and to Daniela Witten for assistance with the R PMA package.
Author Contributions
Conceived and designed the experiments: RAP TS DK BB TY. Performed the experiments: RAP TY. Analyzed the data: RAP JAM TY. Contributed reagents/materials/analysis tools: RAP JAM DK BB TY. Wrote the paper: RAP JAM TS TY.
- View Article
- Google Scholar
- 6. Steyvers M, Griffiths T (2007) Probabilistic topic models. In: Landauer T, McNamara D, Dennis S, Kintsch W, editors. Latent Semantic Analysis: A Road to Meaning.
- 10. Wallach HM, Murray I, Salakhutdinov R, Mimno D (2009) Evaluation methods for topic models. In: Proceedings of the 26th Annual International Conference on Machine Learning. New York, NY, USA: ACM, ICML 2009. pp. 1105–1112. Available: http://doi.acm.org/10.1145/1553374.1553515 .
- 26. McCallum AK (2002) Mallet: A machine learning for language toolkit. Available: http://mallet.cs.umass.edu .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 29 May 2024
Temporal and spatial trend analysis of all-cause depression burden based on Global Burden of Disease (GBD) 2019 study
- Junjiao Liu 1 ,
- Yueyang Liu 2 ,
- Wenjun Ma 1 ,
- Yan Tong 1 &
- Jianzhong Zheng 1
Scientific Reports volume 14 , Article number: 12346 ( 2024 ) Cite this article
172 Accesses
Metrics details
- Health care
- Medical research
Depression has been reported as one of the most prevalent psychiatric illnesses globally. This study aimed to obtain information on the global burden of depression and its associated spatiotemporal variation, by exploring the correlation between the global burden of depression and the social development index (SDI) and associated risk factors. Using data from the Global Burden of Disease study from 1990 to 2019, we described the prevalence and burden of disease in 204 countries across 21 regions, including sex and age differences and the relationship between the global disease burden and SDI. The age-standardized rate and estimated annual percentage change were used to assess the global burden of depression. Individuals with documented depression globally ranged from 182,183,358 in 1990 to 290,185,742 in 2019, representing an increase of 0.59%. More patients experienced major depressive disorder than dysthymia. The incidence and disability-adjusted life years of depression were the highest in the 60–64 age group and much higher in females than in males, with this trend occurring across all ages. The age-standardized incidence and adjusted life-years-disability rates varied with different SDI levels. Relevant risk factors for depression were identified. National governments must support research to improve prevention and treatment interventions.
Similar content being viewed by others

The burden of mental disorders in Asian countries, 1990–2019: an analysis for the global burden of disease study 2019
Incidence, prevalence, and global burden of ADHD from 1990 to 2019 across 204 countries: data, with critical re-analysis, from the Global Burden of Disease study
The burden of schizophrenia in the Middle East and North Africa region, 1990–2019
Introduction.
Mental disorders are a major contributor to the global burden of disease. It commonly results in a higher incidence of physical decline 1 , 2 , 3 , 4 and early death compared with normal age-related deaths 5 . The WHO Mental Health Action Plan 2013–2020 states that individuals suffering from mental illness have elevated rates of disability and death 6 . Individuals with depression and schizophrenia are 40–60% more likely to die suddenly compared to the general population, mainly because of undetected and untreated physical health problems they may be suffering from, such as cancer, cardiovascular disease, diabetes, and HIV infection and even suicide. Suicide is the second most common cause of death for young people in the world 7 .
There is evidence that depression predisposes individuals to myocardial infection and diabetes and having these illnesses increases the chances of developing depression. Many risk factors, such as low social status, alcohol abuse, and stress, are responsible for the development of mental illnesses 8 . Overall, mental illnesses, neurological disorders, and substance use disorders account for 13% of the global disease burden, with depression accounting for 4.3% of the total. Further, these are considered to be one of the main causes of disability worldwide, especially for female.
The economic costs of these health problems are enormous. According to a new study, the total financial costs of mental illness worldwide will reach $16.3 trillion between 2011 and 2030 9 . The Action Plan targets mental illness, stating that by 2020 countries’ suicide rates will have dropped by 10% and there will be a 20% increase in health care services for serious mental illnesses, including psychosis, bipolar disorder, and moderate-to-severe depression 10 .
Mental disorders are recognized as a major contributor to the global burden of disease, accounting for 1566.2 disability-adjusted life years (DALYs) per 100,000 of the global population in 2019. Among these, depressive disorders (major depressive disorder [MDD] and dysthymia) constituted the most significant proportion of mental disorder DALYs (37.3%) 11 . Depression can impair normal body functions and lead to depressive thoughts, which seriously affects people’s quality of life and is one of the most prevalent chronic mental illnesses worldwide. Its main symptoms are depressed emotions, declining interest, slowed thinking, sleep and eating disorders, and even suicidal thoughts in severe cases 12 , 13 , 14 . Around the world, in excess of 300 million people experience depression, which the WHO ranks it as the greatest contributor to global disability 15 . Most concerning of all, youth suffering from major depression have a 30 times higher likelihood of taking their own lives 16 . Despite the fact that depression have become one of the foremost health problems globally, little is known about their complex pathogenesis 17 , 18 .
The Global Burden of Disease (GBD) study offers detailed data on a wide range of diseases for 204 countries in 21 different regions worldwide 19 . The GBD database provides extensive information on the incidence of depression worldwide and categorizes depression into two broad groups: MDD and dysthymia 20 . We explored temporal trends and spatial distributions of depressive disorders, age and sex distributions, and the relationship between the Social Development Index (SDI) and risk factors affecting depression using data on depressive disorders in the GBD database from 1990 to 2019 20 . We described incidence and DALY rates, as well as estimated annual percentage change (EAPC) in incidence and DALY cases. The age-standardized rate (ASR) was considered to be increasing if the EAPC and the corresponding 95% CI were > 0, and the opposite were < 0. Outcomes of this study will contribute to our understanding of the global disease burden of depression, which is of great societal value in controlling and combating depression, and scientifically important for the development of psychology and neuroscience 21 .
Data sources
The data utilized in this study are available on the Global Health Data Exchange GBD Results Tool ( http://ghdx.healthdata.org/gbd-results-tool ) . GBD 2019 estimated incidence, prevalence, mortality, years lived with disability (YLDs), years of life lost (YLLs), and DALYs for 369 diseases and injuries, for males and females, 23 age groups, 204 countries and territories that were geographically grouped into 21 regions from 1990 onwards 11 . All measures are presented as quantities, ratios, and percentages; they can be selected by sex, age group, and region according to the needs of the study 10 . In this study, we extracted data on depression across all age groups and sexes from 21 GBD regions and 204 countries from 1990 to 2019. As not all diseases were estimated for all countries, the GBD 2019 study used the Bayesian meta-regression tool DisMod-MR 2.1 as the principal method to ensure that the incidence, prevalence, and mortality rates for each disease were consistent 22 , 23 .
Classification and definitions
Depressive disorders, mdd, and dysthymia.
In the International Classification of Diseases Tenth Revision (ICD-10), depressive disorders were categorised into two main groups: major depressive disorder (MDD) and dysthymia. Therefore, in the GBD study, both MDD and dysthymia were included in the category of depressive disorders. MDD is an episodic depressive disorder that may recur throughout an individual’s life, with each recurrence varying in severity. Dysthymia is a slow and mild persistent depressive disorder with symptoms less severe than those of MDD, but with a course characterised by persistence. Cases that met the diagnostic criteria for MDD and dysthymia according to the DSM (Diagnostic and Statistical Manual) and ICD (Diagnostic and Statistical Manual) were included in the GBD research disease model 24 .
The SDI is an aggregative metric that measures the development of a country or region, combining data on the total fertility rate for females under 25, the average level of education of females aged 15 and over, and per capita income. The GBD 2019 database categorises the world into five types of regions based on the SDI index: low-SDI (0–0.45), low-middle-SDI (0.45–0.61), middle-SDI (0.61–0.69), high-middle-SDI (0.69–0.81), and high-SDI (0.81–1) 10 , 24 .
Human development index (HDI)
HDI is an aggregative indicator that measure the level of economic and social development of United Nations Member States and consists of three basic variables: life expectancy, educational attainment, and quality of life. We obtained the 2019 HDI data from the United Nations Development Program’s Human Development Report to explore the association of the HDI and the EAPC for incidence and DALYs ( https://hdr.undp.org/en/composite/HDI , accessed on March 27, 2022) 25 .
Age-standardized rate (ASR) is a common indicator in epidemiology. When the composition of age structure is different between several comparison groups, the crude rate of direct comparison groups will lead to bias because it does not indicate whether the high incidence rate in a particular area is due to differences in age composition, and it is usually necessary to compare rates after standardization 26 . Therefore, the age-standardized incidence rate reflects the incidence level that is not affected by age factors, and does not represent the absolute incidence rate, but only to facilitate the comparison of incidence data in different regions or different periods.
The age-standardized rate was calculated on the basis of the following formula:
The age-standardized rate per 100,000 population is equal to the sum of the products of age-specific rates (wi, where i denotes the i th age class) and number of cases (or weight; wi) in the same age subgroup i of the selected reference standard population and then divided by the sum of the standard population weights 27 . Age-standardized rates were calculated considering the GBD world population. In this study, ASR was used to quantify the incidence of two types of depression and the trend of DALYs 28 .
The EAPC provides a well-recognized approach of characterizing ASR using a regression model that quantifies the average annual rate of change during a specific period, with the plus and minus signs representing the direction of change. The regression line was used to estimate the natural logarithm of the rate (i.e., y = α + βx + ϵ, where y = ln(ASR) and x = calendar year). The EAPC was calculated as 100 × (exp (β) − 1), with a 95% CI derived from a linear regression model. All statistics were analysed using R version 4.2.3, and a two-sided P < 0.05 was considered statistically significant 28 . The ASR was decreasing when both the EAPC and the upper limit of its 95% CI were ≤ 0; conversely, the ASR was increasing when both were ≥ 0; otherwise the ASR was stable. All statistical analyses were made with R software 19 .
Analytic strategy
We depicted changes in the prevalence and burden of disease of depression in 204 nations covering 21 distinct regions during the study period. The analysis indices included incidence and DALYs. The ASR was calculated considering the average population structure of the world from 2000 to 2025 as the standard population structure 25 . DALYs = YLDs + YLLs. Because depressive disorders are non-fatal diseases, YLDs are equivalent to DALYs in this instance. This study highlights the state of the burden of disease for depression and temporal and spatial trends from 1990 to 2019 24 . First, the incidence and DALYs of depressive disorders worldwide since 1990 to 2019 were odellin. The burden of depression was then evaluated according to age, sex, country, and region. The extent to which differing development levels affected the burden of depressive disorders was then assessed using the SDI and risk factors for depression 10 . In the result, we present 95% UI for every metric based on the 25th and 975th ordered values of 1000 draws of the posterior distribution. Uncertainty interval (UI) is the interval estimated by GBD research calculation method DisMod-MR, a Bayesian meta-regression tool. It takes into account the differences between different calculation methods in different countries, as well as the uncertainty of multiple filling of missing data values in different countries, which is obtained by repeated sampling calculation through the correlation matrix. Unlike confidence intervals, the UI not only adjusts for sampling error, but also captures uncertainty in multiple stages of analysis modelling and adjusts for the type and quality of data sources 28 .
Ethical committee
The study was compliant with the Guidelines for Accurate and Transparent Health Estimates Reporting, and the University of Washington Institutional Review Board reviewed and approved the waiver of informed consent for GBD 2019.
Since 1990 to 2019, depressive disorder cases have grown from 182,183,358 (95% UI 159,598,111–207,533,227) to 290,185,742 (95% UI 256,024,052–328,260,553), with a 0.59% (95% UI 0.55–0.64) increase in cases of depression for both male and female (see Supplementary Table S1 a). In 2019, 46,863,642 (95% UI 32,929,363–63,797,315) DALYs resulting from depression were documented with an upward trend of 0.61% since 1990 (see Table 1 , Supplementary Table S1 b). The incidence of depression was greater among females than males from 1990 to 2019, as were associated DALYs (see Fig. 1 , Table 1 ). In 2019, depression caused 110,123,422 (95% UI 96,668,365–124,305,433) incidence cases in males globally, and 180,062,320 (95% UI 159,076,846–204,131,417) incidence cases in females, resulting in 18,183,102 (95% UI 12,682,047–24,947,035) DALYs in males, and 28,680,540 (95% UI 20,155,773–39,319,358) DALYs in females. The age-standardised incidence rate (ASIR) of depressive disorders is found to grow with age, reaching a peak during the 60–64 year age group for females and the 80–84 year age group for males. However, there was a small decrease in the 25–29 years age group across both sexes. The age-standardized adjusted life-year disability rate (ASDR) of depression also showed an increasing trend with age. It began to decline in females after reaching a peak in the 55–59 age group. And for males, it peaks in the 60–64 age group and then begins to decline. ASDR for males and females were 452.17 (95% UI 316.79–618.13) and 702.08 (95% UI 492.3–963.58), respectively (see Fig. 2 , Table 1 ). Over all, Females develop a greater ASIR and ASDR than males in the same age group. However, during the period 1990–2019, the DALYs change was higher in males than in females, 0.65% in males (95% UI 0.61–0.69) compared to 0.59% in females (95% UI 0.54–0.63) (see Supplementary Table S1 b).

Temporal trend of global incidence ( a ) and DALYs ( b ) number of depressive disorders.

Age-standardized incidence rate ( a ) and age-standardized DALYs rate ( b ) trends of sex and age distribution.
In terms of the subtypes of depression, the incidence of MDD was much more prevalent than dysthymia at 2,784,803,790 (95% UI 241,280,545–312,774,423) and 15,381,951(95% UI 12,782,128–18,474,451) respectively in 2019. The same was true for DALYs, which were 37,202,742 (95% UI 25,650,205–51,217,042) and 9,660,901 (95% UI 6,311,566–14,421,787) respectively (see Table 1 ). During the period 1990–2019, the global depression ASIR has decreased significantly (EAPC = − 0.29%, 95% UI − 0.38 to − 0.21), whereas the ASDR has markedly increased (EAPC = 0.61%, 95% UI 0.57–0.65) (see Table 1 ).
Global burden and EAPC of depressive disorders by 21 GBD regions
Individuals with depressive disorders increased in all five SDI regions from 1990 through 2019 (see Supplementary Table S1 a). However, the ASIR decreased in the high-middle-SDI (EAPC = − 0.5%, 95% UI − 0.57 to − 0.43), middle-SDI (EAPC = − 0.2%, 95% UI − 0.28 to − 0.13), low-middle-SDI (EAPC = − 0.62%, 95% UI − 0.79 to − 0.44), and low-SDI regions (EAPC = − 0.38%, 95% UI − 0.5 to − 0.26), only increasing in the high-SDI regions (EAPC = 0.31%, 95% UI 0.18–0.44) (see Table 1 ). The same is true for DALYs cases and ASDR (Table 1 , Supplementary Table S1 b). ASDR decreased in the high-middle-SDI (EAPC = − 0.4%, 95% UI − 0.46 to − 0.34), middle-SDI (EAPC = − 0.18%, 95% UI − 0.24 to − 0.13), low-middle-SDI (EAPC = − 0.51%, 95% UI − 0.66 to − 0.36) and low-SDI regions (EAPC = − 0.3%, 95% UI − 0.4 to − 0.2), only increasing in the high-SDI regions (EAPC = 0.23%, 95% UI 0.14–0.33) (see Table 1 , Supplementary Table S1 b).
The incidence of depressive disorders grew in all regions, with a decline only in Central and Eastern Europe (see Fig. 3 a). Central Sub-Saharan Africa saw the maximum rate of increase (1.4%, 95% UI 1.29–1.51), followed by Western Sub-Saharan Africa (1.25%, 95% UI 1.22–1.28) and Eastern Sub-Saharan Africa (1.17%, 95% UI 1.13–1.21), with the decline being most marked in Eastern Europe (− 0.08%, 95% UI − 0.1 to − 0.05) (see Supplementary Table S1 a). There was a marked rise in ASR across high-income North America (EAPC = 0.62, 95% UI 0.32–0.92) and a marked drop in South Asia (EAPC = − 0.85, 95% UI − 1.1 to − 0.6) (see Table 1 ).
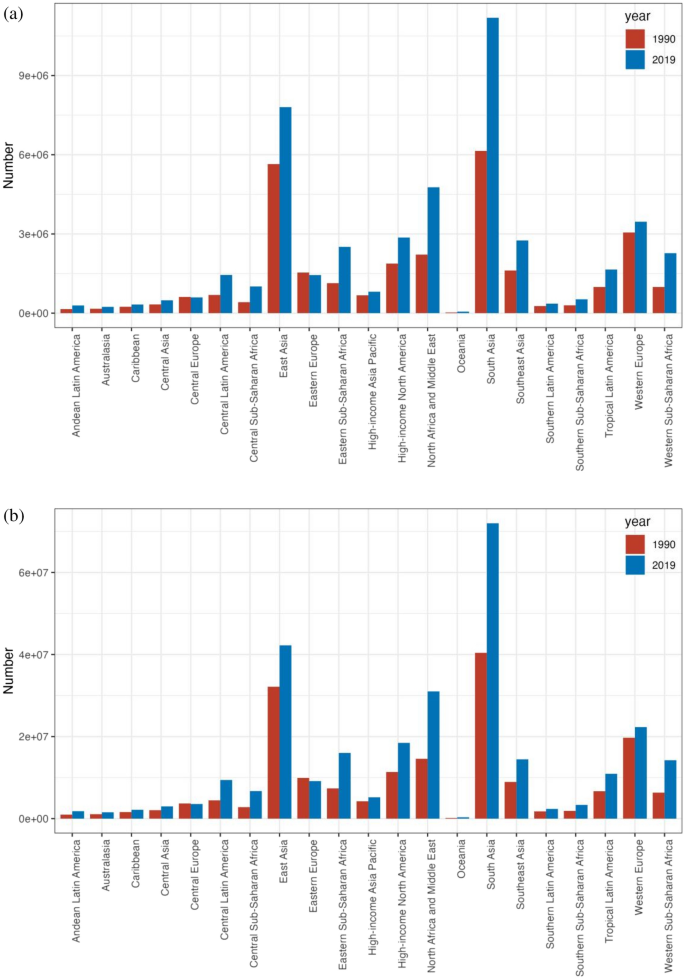
The incident cases ( a ) and DALYs ( b ) of depression at a regional level. The left column in each group is case data in 1990 and the right column in 2019.
DALYs corresponding to depressive disorders grown in all geographical regions, with a decline only in Central and Eastern Europe (see Fig. 3 b). The largest increase was occurred in Central Sub-Saharan Africa (1.43%, 95% UI 1.33–1.54), followed by Western Sub-Saharan Africa (1.29%, 95% UI 1.26–1.32) and Eastern Sub-Saharan Africa (1.21%, 95% UI 1.17–1.25), with the decline being most marked in Eastern Europe (− 0.06%, 95% UI − 0.08 to − 0.04) (Supplementary Table S1 b). There was a marked rise in ASR in Central Sub-Saharan Africa (EAPC = 1.43, 95% UI 1.33–1.54) and a decline in South Asia (EAPC = − 0.71, 95% UI − 0.92 to − 0.5) (see Table 1 ).
Global burden and EAPC of depressive disorders across 204 countries and territories
The ASIR for depression varied dramatically across 204 countries and territories in 2019 (see Fig. 4 a, Supplementary Table S2 a). The ASIR was highest in Uganda (8062.76, 95% UI 6946.5–9436.97), followed by Palestine (7864.2, 95% UI 6719.71–9216.83) and the Central African Republic (7230.55, 95% UI 6121.98–8465.86), and was lowest in Myanmar (1393.92, 95% UI 1188.1–1612.65), followed by Brunei Darussalam (1,575.58, 95% UI 1346.16 to 1854.56) and Indonesia (1794.07, 95% UI 1557.18–2060.02). Of the 204 countries and territories under analysed, the ASDR for depressive disorders in 2019 differed considerably (see Fig. 4 a, Supplementary Table S2 b), with the highest being in Uganda (1212.09, 95% UI 824.6–1696.26), followed by Palestine (1168.68, 95% UI 802.95–1624.31) and Greenland (1098.69, 95% UI 750.76–1540.82), and the lowest in Brunei Darussalam (260.29, 95% UI 177.62–360.71), followed by Myanmar (298.19, 95% UI 203.44–421.71) and Indonesia (350.26, 95% UI–242.89–488.45).

The global disease burden of depression for both sexes in 204 countries and territories. ( a1 ) The ASIR of depression in 2019; ( a2 ) the ASDR of depression in 2019; ( b1 ) the relative change in incident cases of depression between 1990 and 2019; ( b2 ) the relative change in DALYs number of depression between 1990 and 2019; ( c1 ) the EAPC of depression ASIR from 1990 to 2019; ( c2 ) the EAPC of depression ASDR from 1990 to 2019. ASIR age-standardized incidence rate, ASDR age-standardized DALYs rate, EAPC estimated annual percentage change (Image generated in R software version 4.2.3 ( https://cran.r-project.org )).
The global incidence of depression grew by 0.59% from 182,183,358 in 1990 to 290,185,742 in 2019. Qatar had the greatest growth (5.89%, 95% UI 5.34–6.51), followed by the United Arab Emirates (4.81%, 95% UI 4.09–5.53) and Equatorial Guinea (2.42%, 95% UI 2.19–2.67) (see Fig. 4 b, Supplementary Table S2 a). From 1990 to 2019, depression declined in 23 nations, with Latvia experiencing the largest reduction (− 0.32%, 95% UI − 0.38 to − 0.24), followed by Bosnia and Herzegovina (− 0.3%, 95% UI − 0.38 to − 0.21) and Estonia (− 0.27%, 95% UI − 0.34 to − 0.19). The DALYs for depression worldwide rose from 29,089,267 in 1990 to 46,863,642 in 2019, which is a 0.61% increase. Qatar had the most significant growth (5.99%, 95% UI 5.45–6.57), followed by the United Arab Emirates (4.91%, 95% UI 4.24 to 5.65) and Equatorial Guinea (2.48%, 95% UI 2.26 to 2.73) (see Fig. 4 b, Supplementary Table S2 b). DALYs for depression declined in 21 countries, with Latvia experiencing the largest decline from 1990 to 2019 (− 0.31%, 95% UI − 0.37 to − 0.24), followed by Bosnia and Herzegovina (− 0.29%, 95% UI − 0.36 to − 0.21) and Estonia (− 0.26%, 95% UI − 0.33 to − 0.19).
Among the 204 countries and territories, the greatest rise of ASIR occurred in Spain (EAPC = 1.05, 95% UI 0.78–1.31), next is Mexico (EAPC = 0.81, 95% UI 0.73 to 0.89) and Malaysia (EAPC = 0.79, 95% UI 0.59–1.00) (see Fig. 4 c, Supplementary Table S2 a). The most significant drop in ASR was Singapore (EAPC = − 1.97, 95% UI − 2.22 to − 1.73), then Sri Lanka (EAPC = − 1.23, 95% UI − 1.4 to − 1.06) and Slovenia (EAPC = − 1.15, 95% UI − 1.23 to − 1.07). Among all 204 countries and territories, Spain had the greatest rise in ASDR (EAPC = 0.94, 95% UI 0.69–1.18), then Mexico (EAPC = 0.74, 95% UI 0.67–0.81) and Malaysia (EAPC = 0.69, 95% UI 0.53–0.86) (see Fig. 4 c, Supplementary Table S2 b). The greatest decline in ASR was in Singapore (EAPC = − 1.83, 95% UI − 2.06 to − 1.59), next is Cuba (EAPC = − 1.23, 95% UI − 1.36 to − 1.1) and Estonia (EAPC = − 1.23, 95% UI − 1.36 to − 1.1).
The correlation of SDI with the global burden of depressive disorders
Substantial correlation was observed among the SDI and depression prevalence and also among the SDI and DALYs, as illustrated in Fig. 5 . A number of regions exceeded the expected levels of prevalence, including Central Sub-Saharan Africa and Australasia, while a number of regions fell below the expected levels of prevalence, including South-East Asia and the high-income regions Asia and the Pacific (see Fig. 5 a).

Age-standardized incidence rate ( a ) and age-standardized DALYs rate ( b ) for depression for 21GBD regions and 204 countries and territories ( c , d ) by Socio-demographic Index(SDI),1990–2019 (the black line indicates the correlation between all SDI regions and the incidence rate or DALY expected value).
Of the 204 countries and territories whose association with the 2019 SDI was recognised, most had a negative association with the SDI, with a few countries significantly above or below the expected level. Uganda and Palestine were significantly higher than expected, while Myanmar and Brunei were significantly lower than expected (see Fig. 5 c).
DALYs declined in many areas as the SDI became higher, with the exception of certain regions. For instance, the DALYs rate in Western Sub-Saharan Africa fell briefly, then rose, and then kept falling, forming an inverted U-curve. The DALYs rate of Tropical Latin America, which has a low-middle SDI rank, remained stable at first, then increased, before declining sharply. The rate of Southern Latin America, which has a middle SDI rank, remained stable at first, then decreased, and then continued to remain stable. The DALYs rate of Eastern Europe, which has a high-middle SDI, rose slightly, then fell sharply, remained stable for a period, and then fell slightly. High SDI ratios in high-income Asia–Pacific regions fell briefly and then rose, before falling slightly (see Fig. 5 b).
Since 1990 to 2019, the DALY rates obtained in high SDI-ranking regions, such as Western Europe, were mostly consistent with expectations. However, during the study period, some regions (e.g., high-income Asia–Pacific) continued to have DALYs far lower than expected, while others (e.g., Australasia and high-income North America) continued to have DALYs higher than expected (see Fig. 5 b). At the country level during 2019, following a similar pattern to the association of morbidity and SDI, there was a marked adverse correlation between DALYs and SDI, with a few exceptions (R = − 0.375, p < 0.001) (see Fig. 5 d) 28 .
The relationship between the HDI and the global burden of depressive disorders
No significant relationship was found between the EAPC for 1990 morbidity and morbidity (ρ = − 0.064, p = 0.363). An inverse association was identified with EAPC in DALYs and DALYs in 1990 (ρ = − 0.057, p = 0.014) (see Fig. 6 a). In view of the fact that the EAPC was below zero, the number of DALYs attributable to depressive disorders decreased more rapidly in countries with higher DALYs in 1990. In addition, a significant negative correlation was identified for EAPC with the 2019 HDI, suggesting that prevalence rates declined more rapidly in areas with higher HDI. The same association was identified with DALYs rate and HDI (ρ = − 0.213, p = 0.007) (see Fig. 6 b).

The EAPCs of depressive disorders at global, regional and national level. ( a ) The correlation between EAPC and age-standardized rate of depressive disorders incidence and ( b ) DALYs rate in 1990. ( c , d ) The correlation between EAPC and HDI in 2019. The circles represent countries that were available on HDI data. The size of circle is increased with the cases of depressive disorders cases. The ρ indices and p values presented were derived from Pearson correlation analysis. ( a ) ρ = − 0.064, p = 0.363 ( b ) ρ = − 0.057, p = 0.014 ( c ) ρ = − 0.198, p = 0.013 ( d ) ρ = − 0.213, p = 0.007.
Risk factors of depressive disorders
For the world as a whole, a small fraction of DALYs were ascribed to the three risk factors for which GBD estimates were obtainable, of which 6.7% attributable to intimate partner violence, 3.6% to bullying victimisation, and 4.4% to childhood sexual abuse (see Fig. 7 ). There is regional variation in the contributions of these risk factors. For instance, intimate partner violence had the greatest impact in Central Sub-Saharan Africa (9.6% of DALYs were attributable to intimate partner violence) and Southern Sub-Saharan Africa (9.1%), where intimate partner violence remains prevalent, and is lowest in Southeast Asia (3.8%). As well, the contribution of bullying vicitimisation was greatest in Central Sub-Saharan Africa (6.2% of DALYs attributable to bullying victimisation) and high-income North America (5.6%), and was lowest in Central Asia, where bullying victimisation is relatively low. In addition, the impact of childhood sexual abuse was greatest in Western Sub-Saharan Africa (8.5% of DALYs were attributable to childhood sexual abuse) and lowest in Central Asia. However, given that there were only three risk factors relevant to depressive disorders among the GBD study, the percentage of DALYs resulting from these three risk factors remains small when viewed as a whole, which means that there is a need for further study on the key influences of depression.

Proportion of depressive disorders DALYs attributable to intimate partner violence, bullying victimization, and childhood sexual abuse, for 21 GBD regions, 2019.
Depression, as a serious public health problem, is associated with adverse health outcomes and reduced life-expectancy 30 . This study presents the global burden of depression through GBD data, focusing on the temporal trends and spatial distribution of depression from 1990 to 2019, with a specific focus on EAPC. The outcome of the study offers an important reference value for all regional governments when formulating relevant prevention and treatment measures for depression 19 .
The outcomes of this study suggest that the overall burden of depression has increased rapidly within three decades, but the increase has not been uniform across age groups, sexes, or regions 10 . The further increase in the burden of depression observed in our study is in agreement with the outcomes by Liu et al. 29 . This is likely driven by the increasing social pressure brought about by economic development and population growth, and the serious aging of the population. In addition, with the economic development and the gradual improvement of people’s living standards, the demand for medical services is also rising, especially the increasing emphasis on mental health, in this case, the search for mental health services has also increased. It is also important to note that the continuous improvement of depression screening tools has made it possible for medical institutions and government agencies to obtain more comprehensive and accurate data. Our research suggests that MDD accounts for a large proportion of depression cases and is the most prevalent psychiatric category of depression, a finding which aligns with those of a 2022 study by Li et al. 31 .
Our research shows that females have higher rates of depression and DALYs than males across all age groups. The prevalence and DALYs rates of depression were highest in people aged 60–64 years. There are many reasons for this. The psychological characteristics of people in this age group undergo a major shift from concern for external things to their own bodies, the feeling of loneliness and isolation increases, and the intellect begins to diminish, which leads to emotional instability. Females are more prone to experience negative events and emotions, including postpartum mood swings, domestic violence, sexual abuse, and bullying, all of which may contribute to higher rates of depression 32 , 33 , 34 . Additionally, related reports have found that females are more selfless than males and are thus more prone to depression 35 . This finding partly explains sex differences in the onset of depression.
Our reports indicate that the rates of the two subtypes of depression, dysthymia and major depressive disorders, have remained largely stable globally and regionally over the study period, with the majority of patients suffering from MDD. The World Mental Health Survey estimated the annual prevalence of MDD to be 4.4% and the lifetime prevalence to be approximately 10% -15% 36 , 37 . With the continuous development of the social economy, accelerated pace of life, and increasingly fierce social competition, people’s psychological pressure is gradually increasing, and the incidence of MDD is increasing annually. MDD not only seriously affects the psychological condition and quality of life of patients, but also imposes tremendous mental and economic burdens to families and society 38 . In 2008, the WHO listed MDD as the third largest contributor to the global disease burden and predicted that MDD would be the leading contributor to the burden of disease by 2030 39 . Currently, about 300 million people worldwide suffer from MDD; therefore, effective control of major depressive disorders is an effective approach to preventing and managing depression 40 .
The findings suggest that Uganda’s relatively concentrated population and high prevalence of tropical diseases, malaria, AIDS, Ebola virus, sleeping sickness, viral hepatitis, and tuberculosis may be associated with its highest global ASR and ASDR for depression. Although the peak of the epidemic in Uganda, which had one of the world’s highest HIV prevalence rates, has passed and the rate of new cases has diminished in recent years, the number of people infected with the virus and living with the disease remains high, especially in rural areas. People living with HIV experience social prejudice and discrimination, which can lead to unemployment, poverty, family disintegration, and physical and psychological problems that can lead to low self-esteem, low mood, and even depression 41 , 42 . This shows that the prevention and control of HIV can affect depression.
The most significant rise in depression and DALYs was identified in Qatar, with the United Arab Emirates and Equatorial Guinea next. Significant increases in depression and DALYs were observed in the medium–high SDI and high-SDI regions. It could be because the level of economic development and education in these regions is relatively high, and the social pressure generated by residents is greater, leading to the increased prevalence of depression. Studies have found that individuals with different education levels have different levels of cognitive ability. Education level influences depression in individuals and can also impact spouses 43 . It is also true that social stress is an acknowledged risk factor for depression, and research have indicated that the higher the level of economic development, the more social stress people experience. Notably, the country with the most decline in depression and DALYs was Latvia, followed by Bosnia and Herzegovina, and Estonia 19 .
The ASIR and ASDR increased the most in Spain, followed by Mexico and Malaysia. These countries are reported to have higher economic incomes and sociodemographic indices, which confirm our statistics. However, in terms of ASR, the greatest decline in ASIR was in Singapore, then Sri Lanka and Slovenia; and the maximum decline in ASDR was in Singapore, Cuba, and Estonia 19 .
Further analysis of the relationship between illness and sociodemographic and geographic factors suggests that depression is more pronounced in terms of incidence in high-SDI and high-income countries, while the burden of depression is significantly higher in low-income and low-SDI countries.
In conclusion, the burden of depression varies across regions for a number of reasons. These include each region’s level of economic development, level of education, level of medical development and capacity to diagnose the illness, as well as the level of importance that governments attach to the illness 44 , 45 , 46 . Additionally, there are cultural differences that contribute to the different burdens of depression in different regions, such as customs and religious beliefs. The incidence of depression is still high, and the burden of the disease remains heavy, but the pathogenesis is unclear, which is an obstacle to the effective prevention and control of depression. This study nalysed the possible risk factors, such as domestic violence, bullying victimisation, and childhood sexual abuse. However, the GBD data show that the implication of these three risk factors on depression is small; that is, these three risk factors are not likely to be key risk factors for depression, indicating that this requires further investigation 47 .
To effectively prevent and control depression, governments must support depression-related research while taking appropriate steps to effectively address depression. For example, they should strengthen education on prevention and treatment, improve the capacity for early diagnosis and standardised treatment, establish mental health service measures for key populations, and carry out psychological intervention in a timely manner 19 .
This study performed the most comprehensive assessment of the depression burden to date. All the data used in this study were obtained from the GBD database, which offers a large sample size and high data quality, offering this study a distinct advantage in terms of data reliability. While numerous research have been conducted on the prevalence of depression in GBD 2019, the majority of these studies evaluate the condition using the age-period-cohort analytic approach, and their study regions, study objects, and focus subtypes of depression vary. Li et al., for instance, used the age-period cohort analytic approach to study the prevalence of depression among teenagers in the Western Pacific region 48 . In addition, Xu Y et al. used the age-period-cohort analytic method and limited their research to the incidence of depression across all areas, leaving unfinished business regarding studies on the burden of disorders like DALY 49 . Major depression is a subtype of depression, and Li et al. focused on examining gender variations in its illness burden. They discovered that women are more likely than males to experience major depression 31 . The disease burden of anxiety and major depression caused by bullying was examined by Hong C et al. as a risk factor. The findings indicated that from 1990 to 2019, there was a rising trend in both the DALY number and DALY rate of anxiety and major depression caused by bullying. Adopting effective techniques is necessary to eradicate bullying among children and adolescents 50 . Additionally, Yang F et al. used the age-period-cohort analysis method to conduct a thorough study on the prevalence of depression in 204 countries from 1990 to 2019. Findings from our study, such as the nations with the greatest and lowest incidence and DALY of depression, are in line with their conclusions. Moreover, the connection between the regional SDI and the depression incidence trend. But there isn’t any research on the prevalence and DALY of two distinct subtypes of depression, or on the connection between the HDI and depression burden, as well as the risk factors of depression 51 . This study comprehensively analysed the impact of depression and the temporal and spatial changes in disease burden at the global, 21 regional and 204 national levels. These include age-specific differences in the burden of depression, sex differences, and disease burden differences between the two subtypes of depression. Incidence, DALYs, ASIR, ASDR and EAPC (the change rate of ASIR and ASDR) are used to comprehensively describe the burden of disease from different perspectives and provide specific quantified values respectively. And most importantly, this study nalysed the relationship between the burden of depression and HDI, this is what is missing from all the relevant studies above. Finally, this study examined the depression risk factor data that was accessible in the GBD database. This will offer a crucial foundation for upcoming research on depression and its risk factors. All of the linked research mentioned above lack the analysis of risk variables. Nonetheless, this study possesses limitations. First, the GBD data used in this study were collected from a large amount of epidemiological survey data, processed, and integrated using corresponding statistical methods. The lack of original data in many countries and regions may have led to a bias in the differences in disease burden. Second, the comorbidity of MDD and dysthymia was excluded in this study. We hope that in the future the GBD database can further distinguish these disorders to facilitate a more complete analysis 52 , 53 .
Depression remains a serious challenge worldwide, and its burden of disease remains heavy. By analysing the global burden of depression, this study clarifies the current situation of depression in various countries and provides a scientific reference basis for governments to formulate active and effective prevention and treatment strategies. Countries, especially those with a high burden of depression, must vigorously strengthen mental health education, actively prevent risk factors, and adopt targeted interventions to raise the level of awareness of depression among their populations, and concurrently, call for the reform of the relevant systems and the elimination of policy barriers to better prevent and treat mental health disorders 54 , 55 .
Data availability
The dataset generated for this study can be found in the GBD at http://ghdx.healthdata.org/gbd-results-tool .
Lawrence, D., Kisely, S. & Pais, J. The epidemiology of excess mortality in people with mental illness. Can. J. Psychiatry . 55 , 752–760. https://doi.org/10.1177/070674371005501202 (2010).
Scott, K. M. et al . Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry 73 , 150–158. https://doi.org/10.1001/jamapsychiatry.2015.2688 (2016).
Wahlbeck, K., Westman, J., Nordentoft, M., Gissler, M. & Laursen, T. M. Outcomes of Nordic mental health systems: Life expectancy of patients with mental disorders. Br. J. Psychiatry 199 , 453–458. https://doi.org/10.1192/bjp.bp.110.085100 (2011).
Scott, K. M. et al. Associations between DSM-IV mental disorders and subsequent heart disease onset: beyond depression. Int. J. Cardiol. 168 , 5293–5299 (2013).
Article PubMed Google Scholar
Piao, J. et al. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: A systematic analysis for the Global Burden of Disease study. Eur. Child Adolesc. Psychiatry. 31 (1827–1845), 14. https://doi.org/10.1007/s00787-022-02040-4(2022)(Epub (2022).
Article Google Scholar
Thomas, S. P. World Health Assembly adopts comprehensive Mental Health Action Plan for 2013–2020. Issues Ment. Health Nurs. 34 , 723–724. https://doi.org/10.3109/01612840.2013.831260 (2013).
Upthegrove, R., Marwaha, S. & Birchwood, M. Depression and schizophrenia: Cause, consequence, or trans-diagnostic issue?. Schizophr. Bull. 43 , 240–244. https://doi.org/10.1093/schbul/sbw097 (2017).
Kessler, R. C. et al. The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiol. Psichiatr. Soc. 18 , 23–33. https://doi.org/10.1017/s1121189x00001421 (2009).
Article PubMed PubMed Central Google Scholar
Wang, P. S. et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 370 , 841–850. https://doi.org/10.1016/S0140-6736(07)61414-7 (2007).
Piao, J. et al. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: A systematic analysis for the Global Burden of Disease study. Eur. Child Adolesc. Psychiatry 31 , 1827–1845. https://doi.org/10.1007/s00787-022-02040-4.[Epub2022July14] (2022).
GBD. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 9 , 137–150. https://doi.org/10.1016/S2215-0366(21)00395-3 (2022).
Cui, R. Editorial: A systematic review of depression. Curr. Neuropharmacol. 13 , 480. https://doi.org/10.2174/1570159x1304150831123535 (2015).
Article CAS PubMed Google Scholar
Luo, Y., Zhang, S., Zheng, R., Xu, L. & Wu, J. Effects of depression on heart rate variability in elderly patients with stable coronary artery disease. J. Evid. Based Med. 11 , 242–245. https://doi.org/10.1111/jebm.12310 (2018).
Seligman, F. & Nemeroff, C. B. The interface of depression and cardiovascular disease: Therapeutic implications. Ann. N. Y. Acad. Sci. 1345 , 25–35. https://doi.org/10.1111/nyas.12738 (2015).
Article ADS CAS PubMed Google Scholar
Smith, K. Mental health: A world of depression. Nature 515 , 181. https://doi.org/10.1038/515180a (2014).
Stringaris, A. Editorial: What is depression?. J. Child. Psychol. Psychiatr. 58 , 1287–1289. https://doi.org/10.1111/jcpp.12844 (2017).
Gross, M. Silver linings for patients with depression?. Curr. Biol. 24 , R851–R854. https://doi.org/10.1016/j.cub.2014.08.059 (2014).
Ménard, C., Hodes, G. E. & Russo, S. J. Pathogenesis of depression: Insights from human and rodent studies. Neuroscience 321 , 138–162. https://doi.org/10.1016/j.neuroscience.2015.05.053 (2016).
Solmi, M. et al. Incidence, prevalence, and global burden of autism spectrum disorder from 1990 to 2019 across 204 countries. Mol. Psychiatry 27 , 4172–4180 (2022).
Liu, Q. et al. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J. Psychiatr. Res. 126 , 134–140. https://doi.org/10.1016/j.jpsychires.2019.08.002 (2020).
Peng, H. et al. The global, national, and regional burden of dysthymia from 1990 to 2019: Insights from the Global Burden of Disease 2019 study. J. Affect. Disord. 333 , 524–526. https://doi.org/10.1016/j.jad.2023.04.024 (2023).
GBD. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2 (2020).
Hong, C. et al. Global trends and regional differences in the burden of anxiety disorders and major depressive disorder attributed to bullying victimisation in 204 countries and territories, 1999–2019: an analysis of the Global Burden of Disease Study. Epidemiol. Psychiatr. Sci. 31 , e85. https://doi.org/10.1017/S2045796022000683 (2022).
Article CAS PubMed PubMed Central Google Scholar
Ren, X. et al. Burden of depression in China, 1990–2017: Findings from the global burden of disease study 2017. J. Affect. Disord. 268 , 95–101. https://doi.org/10.1016/j.jad.2020.03.011 (2020).
Dai, H. et al. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: An analysis of the Global Burden of Disease Study. PLOS Med. 17 , e1003198. https://doi.org/10.1371/journal.pmed.1003198 (2020).
Hankey, B. F. et al. Partitioning linear trends in age-adjusted rates. Cancer Causes Control 11 , 31–35. https://doi.org/10.1023/a:1008953201688 (2000).
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet . 396 , 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
Yue, T., Zhang, Q., Li, G. & Qin, H. Global burden of nutritional deficiencies among children under 5 years of age from 2010 to 2019. Nutrients 14 , 2685. https://doi.org/10.3390/nu14132685 (2022).
Liu, Q. et al. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J. Psychiatr Res. 126 , 134–140. https://doi.org/10.1016/j.jpsychires.2019.08.002 (2019).
Ogbo, F. A., Mathsyaraja, S., Koti, R. K., Perz, J. & Page, A. The burden of depressive disorders in South Asia, 1990–2016: findings from the global burden of disease study. BMC Psychiatry 18 , 333. https://doi.org/10.1186/s12888-018-1918-1 (2018).
Li, S. et al. Sex difference in global burden of major depressive disorder: Findings from the global burden of disease study 2019. Front. Psychiatry. 21 (13), 789305. https://doi.org/10.3389/fpsyt.2022.789305 (2022).
Keita, G. P. Psychosocial and cultural contributions to depression in women: Considerations for women midlife and beyond. J. Manag. Care Pharm. 13 (Supp 9), 12–15 (2007).
Google Scholar
Patel, V., Rodrigues, M. & DeSouza, N. Gender, poverty, and postnatal depression: A study of mothers in Goa India. Am. J. Psychiatr. 159 (1), 43–47 (2002).
Trivedi, J. K., Sareen, H. & Dhyani, M. Rapid urbanization-its impact on mental health: A south Asian perspective. Indian J. Psychiatry. 50 (3), 161 (2008).
Ahmad, O. B. et al . Age standardization of rates: a new WHO standard. GPE Discussion Paper Series: No 31, 10–12. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf (2001).
Ferrari, A. J. et al. Burden of depressive disorders by country, sex, age, and year: Findings from the global burden of disease study 2010. PLOS Med. 10 , e1001547. https://doi.org/10.1371/journal.pmed.1001547 (2013).
Bachner-Melman, R., Watermann, Y., Lev-Ari, L. & Zohar, A. H. Associations of self-repression with disordered eating and symptoms of other psychopathologies for men and women. J. Eat. Disord. 10 , 41. https://doi.org/10.1186/s40337-022-00569-y (2022).
Kessler, R. C. et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA 289 , 3095–3105. https://doi.org/10.1001/jama.289.23.3095 (2003).
Bromet, E. et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 9 , 90 (2011).
Sheehan, D. V. et al. Restoring function in major depressive disorder: A systematic review. J. Affect. Disord. 215 , 299–313 (2017).
Malhi, G. S. & Mann, J. J. Depression. Lancet 392 , 2299–2312 (2018).
Yang, L. et al. The effects of psychological stress on depression. Curr. Neuropharmacol. 13 , 494–504. https://doi.org/10.2174/1570159x1304150831150507 (2015).
Ironson, G., Henry, S. M. & Gonzalez, B. D. Impact of stressful death or divorce in people with HIV: A prospective examination and the buffering effects of religious coping and social support. J. Health Psychol. 25 , 606–616. https://doi.org/10.1177/1359105317726151 (2020).
Junqueira, P., Bellucci, S., Rossini, S. & Reimão, R. Women living with HIV/AIDS: Sleep impairment, anxiety and depression symptoms. Arq. Neuropsiquiatr. 66 , 817–820. https://doi.org/10.1590/s0004-282x2008000600008 (2008).
Lee, J. Pathways from education to depression. J. Cross. Cult. Gerontol. 26 , 121–135. https://doi.org/10.1007/s10823-011-9142-1 (2011).
Alonso, J. et al. Treatment gap for anxiety disorders is global: Results of the World Mental Health Surveys in 21 countries. Depress. Anxiety 35 , 195–208. https://doi.org/10.1002/da.22711 (2018).
Perez, M. I. et al. Obsessive-compulsive disorder misdiagnosis among mental healthcare providers in Latin America. J. Obsessive Compuls. Relat. Disord. 32 , 100693. https://doi.org/10.1016/j.jocrd.2021.100693 (2022).
Li, Z. B. et al. Burden of depression in adolescents in the Western Pacific Region from 1990 to 2019: An age-period-cohort analysis of the Global Burden of Disease study. Psychiatry Res. 336 , 115889. https://doi.org/10.1016/j.psychres.2024.115889 (2024).
Xu, Y. et al. Global, regional, and national incidence trends of depressive disorder, 1990–2019: An age-period-cohort analysis based on the Global Burden of Disease 2019 study. Gen. Hosp. Psychiatry. 88 , 51–60. https://doi.org/10.1016/j.genhosppsych.2024.03.003 (2024) ( Epub 2024 Mar 16 ).
Hong, C. et al. Global trends and regional differences in the burden of anxiety disorders and major depressive disorder attributed to bullying victimisation in 204 countries and territories, 1999–2019: An analysis of the Global Burden of Disease Study. Epidemiol. Psychiatr. Sci. 28 (31), e85. https://doi.org/10.1017/S2045796022000683 (2022).
Yang, F. et al. Thirty-year trends of depressive disorders in 204 countries and territories from 1990 to 2019: An age-period-cohort analysis. Psychiatry Res. 328 , 115433. https://doi.org/10.1016/j.psychres.2023.115433 (2023) ( Epub 2023 Aug 27 ).
Baca, E., Lázaro, J. & Hernández-Clemente, J. C. Historical perspectives of the role of Spain and Portugal in today’s status of psychiatry and mental health in Latin America. Int. Rev. Psychiatry 22 , 311–316. https://doi.org/10.3109/09540261.2010.501165 (2010).
Mullins, N. & Lewis, C. M. Genetics of depression: Progress at last. Curr. Psychiatry Rep. 19 , 43. https://doi.org/10.1007/s11920-017-0803-9 (2017).
McGrath, J. J. et al. Comorbidity within mental disorders: A comprehensive analysis based on 145 990 survey respondents from 27 countries. Epidemiol. Psychiatr. Sci. 29 , e153. https://doi.org/10.1017/S2045796020000633 (2020).
Article MathSciNet CAS PubMed PubMed Central Google Scholar
Plana-Ripoll, O. et al. Nature and prevalence of combinations of mental disorders and their association with excess mortality in a population-based cohort study. World Psychiatry 19 , 339–349. https://doi.org/10.1002/wps.20802 (2020).
Download references
Author information
Authors and affiliations.
College of Public Health, Shanxi Medical University, Taiyuan, Shanxi, China
Junjiao Liu, Wenjun Ma, Yan Tong & Jianzhong Zheng
Second Clinical Medical College, Nanchang University, Nanchang, Jiangxi, China
Yueyang Liu
You can also search for this author in PubMed Google Scholar
Contributions
JL performed the statistical analyses and wrote the manuscript. YL solved technical problems during the statistical analyses and participated in the conceptualization and design of the study, and the interpretation of the results. WM contributed to the conceptualization and design of the study.YT and JZ participated in the design of the study and critically evaluated and revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Yan Tong or Jianzhong Zheng .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Liu, J., Liu, Y., Ma, W. et al. Temporal and spatial trend analysis of all-cause depression burden based on Global Burden of Disease (GBD) 2019 study. Sci Rep 14 , 12346 (2024). https://doi.org/10.1038/s41598-024-62381-9
Download citation
Received : 20 September 2023
Accepted : 16 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1038/s41598-024-62381-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Introduction
- Conclusions
- Article Information
Hazard ratios with 95% CIs for the associations between having 1 or more than 1 ninth-grade classmate with any of the examined mental disorder diagnoses ( International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, codes F10-F50 or F90-F98) and later risk of being diagnosed with a mental disorder in 4 follow-up time windows. The Cox proportional hazards models were adjusted for sex, birth year, school class size, school’s ninth grade size, area-level urbanicity, area-level morbidity, area-level educational level, area-level employment rate, parental educational level, parental income, and parental mental health, with a random intercept per school. For the diagnosis-specific results with the 3-level exposure, see Figure 2; eFigure 2 in Supplement 1 .
Hazard ratios with 95% CIs shown for mood ( International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ ICD-10 ], codes F30-F39) (A), anxiety ( ICD-10 codes F40-F48) (B), and internalizing (C) and externalizing (D) disorders in 4 follow-up time windows. The Cox proportional hazards models were adjusted for sex, birth year, school class size, school’s ninth grade size, area-level urbanicity, area-level morbidity, area-level educational level, area-level employment rate, parental educational level, parental income, and parental mental health, with a random intercept per school. For the diagnosis-specific associations for substance misuse, schizophrenia spectrum, eating, and behavioral and emotional disorders, see eFigure 2 in Supplement 1 .
eTable 1. Annual Number of Mental Disorder Diagnoses Together With the Number of Exposed/Unexposed Classes and Cohort Members
eTable 2. Additional Descriptive Statistics of the Study Population
eFigure 1. Schoenfeld Residuals for the Diagnosis Categories
eTable 3. Diagnosis-Specific Associations Between Having Ninth Grade Classmates With a Mental Disorder Diagnosis and Later Risk of Being Diagnosed With a Mental Disorder
eFigure 2. Diagnosis-Specific Associations Between Having Ninth Grade Classmates With a Mental Disorder Diagnosis and Later Risk of Being Diagnosed With a Mental Disorder
eFigure 3. Diagnosis-Specific Associations Between Having Ninth Grade Classmates With a Mental Disorder Diagnosis and Later Risk of Being Diagnosed With a Mental Disorder Using Binary Exposure
eTable 4. Sensitivity Analyses on the Associations Between Having Diagnosed Ninth Grade Classmates and Later Risk of Being Diagnosed With a Mental Disorder
eTable 5. Series of Cox Regression Models Indicating the Respective Confounding Influences of Each Covariate Domain (School-Level, Parental-Level, and Area-Level)
eTable 6. The Associations Between Having Ninth Grade Classmates With a Mental Disorder Diagnosis and Later Risk of Being Diagnosed With a Mental Disorder Stratified Into Three Shorter Time Periods
Data Sharing Statement
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Alho J , Gutvilig M , Niemi R, et al. Transmission of Mental Disorders in Adolescent Peer Networks. JAMA Psychiatry. Published online May 22, 2024. doi:10.1001/jamapsychiatry.2024.1126
Manage citations:
© 2024
- Permissions
Transmission of Mental Disorders in Adolescent Peer Networks
- 1 Department of Psychology, University of Helsinki, Helsinki, Finland
- 2 School of Business and Economics, University of Jyväskylä, Jyväskylä, Finland
- 3 Centre for Mental Health and Safety, Division of Psychology & Mental Health, University of Manchester, Manchester Academic Health Sciences Centre, Manchester, United Kingdom
- 4 National Institute for Health and Care Research Greater Manchester Patient Safety Research Collaboration, Manchester, United Kingdom
- 5 Finnish Institute for Health and Welfare, Helsinki, Finland
Question Is having peers with a mental disorder in the same social network during adolescence associated with later risk of mental disorder?
Findings In this cohort study including more than 700 000 individuals in Finland, analysis of nationwide, interlinked registry data found that having classmates diagnosed with a mental disorder in the ninth grade of comprehensive school was associated with increased risk of receiving a mental disorder diagnosis later in life. Increased risk remained after adjusting for an array of parental, school-level, and area-level confounders.
Meaning The findings of this study suggest that mental disorders might be socially transmitted within adolescent peer networks.
Importance Previous research indicates that mental disorders may be transmitted from one individual to another within social networks. However, there is a lack of population-based epidemiologic evidence that pertains to the full range of mental disorders.
Objective To examine whether having classmates with a mental disorder diagnosis in the ninth grade of comprehensive school is associated with later risk of being diagnosed with a mental disorder.
Design, Setting, and Participants In a population-based registry study, data on all Finnish citizens born between January 1, 1985, and December 31, 1997, whose demographic, health, and school information were linked from nationwide registers were included. Cohort members were followed up from August 1 in the year they completed ninth grade (approximately aged 16 years) until a diagnosis of mental disorder, emigration, death, or December 31, 2019, whichever occurred first. Data analysis was performed from May 15, 2023, to February 8, 2024.
Exposure The exposure was 1 or more individuals diagnosed with a mental disorder in the same school class in the ninth grade.
Main Outcomes and Measures Being diagnosed with a mental disorder during follow-up.
Results Among the 713 809 cohort members (median age at the start of follow-up, 16.1 [IQR, 15.9-16.4] years; 50.4% were males), 47 433 had a mental disorder diagnosis by the ninth grade. Of the remaining 666 376 cohort members, 167 227 persons (25.1%) received a mental disorder diagnosis during follow-up (7.3 million person-years). A dose-response association was found, with no significant increase in later risk of 1 diagnosed classmate (HR, 1.01; 95% CI, 1.00-1.02), but a 5% increase with more than 1 diagnosed classmate (HR, 1.05; 95% CI, 1.04-1.06). The risk was not proportional over time but was highest during the first year of follow-up, showing a 9% increase for 1 diagnosed classmate (HR, 1.09; 95% CI, 1.04-1.14), and an 18% increase for more than 1 diagnosed classmate (HR, 1.18; 95% CI, 1.13-1.24). Of the examined mental disorders, the risk was greatest for mood, anxiety, and eating disorders. Increased risk was observed after adjusting for an array of parental, school-level, and area-level confounders.
Conclusions and Relevance The findings of this study suggest that mental disorders might be transmitted within adolescent peer networks. More research is required to elucidate the mechanisms underlying the possible transmission of mental disorders.
Mental disorders are major contributors to the global disease burden, having detrimental individual, societal, and economic impacts. 1 - 3 When investigating the impacts of mental disorders, the focus has typically been on the directly affected individual. It is, however, well established that the immediate family members are also adversely affected. 4 Empirical findings suggest that harmful effects extend beyond the immediate family to friends and peers via social networks. 5 - 8 For example, a longitudinal cohort study where a social network of 12 067 adults was followed up over 20 years indicated that depressive symptoms appear to transmit from person to person. 7
Investigating the transmission of mental disorders is especially important in childhood and adolescence. These are key developmental periods when the onset of many mental disorders is most likely to occur 9 and when enduring peer networks and behaviors are established, 10 particularly in the context of peer relationships. 11 , 12 Understanding the role of peer effects in early-life mental health problems would also offer tools for more successful prevention and intervention measures, thus reducing the economic and societal burden of mental disorders. Yet, despite a few survey studies reporting that adolescents may experience increased mental health symptoms when exposed to friends or peers with mental health problems, 6 , 13 large-scale studies on the potential peer influences of mental disorders in youth are lacking.
When analyzing network associations, an additional difficulty arises from people’s tendency to network with others who have similar traits. Such self-selection bias (or homophily) can be mitigated by using institutionally imposed networks, such as school classes, which are not formed endogenously by the pupils choosing similar others as classmates. In Finland, parents also cannot directly choose their children’s comprehensive school; instead, the school is selected based on the proximity to the residential location. Moreover, school class constitutes arguably the most substantial peer network in childhood and adolescence due to the amount of time spent together with classmates. 14 - 16 In the present study, we combined the use of registry data and institutionally imposed peer networks to study the possible transmission of mental disorders among peers. More specifically, we used nationwide, interlinked Finnish registers to examine whether mental disorders are transmitted within peer networks formed by adolescents who were in the same class in the ninth grade of comprehensive school.
The study population comprised all Finnish citizens born between January 1, 1985, and December 31, 1997, whose demographic, health, and school information was linked from several nationwide registers based on unique identification numbers, assigned to all Finnish residents since 1969. Death or emigration before the start of follow-up, move to the municipality of the school later than 3 years before the start of follow-up, and, for those who were born outside Finland, immigration to Finland after school starting age (ie, August 1 in the year they turn 7 years) were used as exclusion criteria. The ethics committee of the Finnish Institute for Health and Welfare approved the study plan (THL/184/6.02.01/2023§933). Data were linked with the permission of Statistics Finland (TK-53-1696-16) and the Finnish Institute for Health and Welfare. According to Finnish law, informed consent is not required from participants in register-based studies. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
The school information was based on the National Joint Application Register. It discloses school class divisions in the final year (ie, ninth grade) of comprehensive school. Individuals with missing or insufficient school class information were excluded. To exclude the smallest classes and omit incorrect registry information (eg, implausibly large classes), individuals in classes with fewer than 10 or more than 40 pupils were excluded. Of the remaining 713 809 individuals, 47 433 had a mental disorder diagnosis ( International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ ICD-10 ] diagnoses F10-F50 or F90-F98) before follow-up commenced and were therefore excluded from follow-up. The remaining 666 376 individuals in 860 schools and 39 992 classes (median, 6 [IQR, 4-7] classes per grade) formed the outcome population and were followed up from August 1 in the year during which they completed ninth grade (approximately aged 16 years) until the first diagnosed mental disorder, death, emigration, or end of follow-up on December 31, 2019, whichever occurred first. The maximum length of follow-up was thus from August 1, 2001, to December 31, 2019. For the annual number of mental disorder diagnoses and proportion of exposed classes and individuals in the outcome population, see eTable 1 in Supplement 1 .
Information on mental disorders was acquired from the Care Register for Health Care of the Finnish Institute for Health and Welfare. It contains information on all inpatient hospital admissions in Finland since 1970, hospital outpatient care since 1998, and primary care since 2011. Mental disorders were diagnosed according to the International Statistical Classification of Diseases Spectrum Health Problems, Eighth Revision , from 1970 to 1986; International Classification of Diseases, Ninth Revision , from 1987 to 1995; and ICD-10 since 1996.
For the study population, we used the following mental disorder diagnosis categories: substance misuse disorders (F10-F19), schizophrenia spectrum disorders (F20-F29), mood disorders (F30-F39), anxiety disorders (F40-F48), eating disorders (F50), and behavioral and emotional disorders (F90-F98). Additionally, categories of internalizing disorders (F30-F39, F40-F48, F93-F94) and externalizing disorders (F10-F19, F90-F92) were constructed.
We included the following demographic, socioeconomic, and intergenerational variables as covariates: sex (0 = male, 1 = female), birth year, degree of urbanicity in residential location (0 = unknown, 1 = urban, 2 = semiurban, 3 = rural) based on the urban-rural classification of the Finnish Environment Institute, morbidity index of the municipality by the Finnish Institute for Health and Welfare in quintiles (0 = 1st quintile, 1 = 2nd quintile, 2 = 3rd quintile, 3 = 4th quintile, 4 = 5th quintile; as data were not available for 2001, data from 2002 were used instead), proportion of people without upper secondary or higher educational levels in the municipality in quintiles (0 = 1st quintile, 1 = 2nd quintile, 2 = 3rd quintile, 3 = 4th quintile, 4 = 5th quintile), proportion of unemployed people in the municipality in quintiles (0 = 1st quintile, 1 = 2nd quintile, 2 = 3rd quintile, 3 = 4th quintile, 4 = 5th quintile), size of school class (number of pupils), size of school’s ninth grade (number of pupils), parental education level at time of child’s ninth grade (0 = comprehensive, 1 = upper secondary, 2 = higher education), parental income level in quintiles relative to study population at time of child’s ninth grade (0 = unknown, 1 = 1st quintile, 2 = 2nd quintile, 3 = 3rd quintile, 4 = 4th quintile, 5 = 5th quintile), and parental mental health history at the time of child’s ninth grade (0 = no mental disorder diagnosis, 1 = any mental disorder diagnosis). The median population of Finnish municipalities in 2001-2013 was 6530 inhabitants. Any mental disorder diagnosis (F00-F99) was used for parental mental health history.
Data analysis was conducted from May 15, 2023, to February 8, 2024. We used mixed-effects Cox proportional hazards regression models with a random intercept per school to estimate the association between having a classmate with a mental disorder diagnosis and later risk of being diagnosed with a mental disorder. Random intercept per school was included to account for the varying predisposition to mental health problems between schools. Results are reported as hazard ratios (HRs). Schoenfeld residuals were calculated to test the proportional hazards assumption of Cox regression models and estimate the time dependence of the HR throughout the entire follow-up period. We also separately estimated the HRs in shorter intervals: first year of follow-up, years 2 and 3, years 4 and 5, and after year 5. In the primary analyses, all models were adjusted for sex, birth year, area-level urbanicity, area-level morbidity, area-level educational level, area-level employment rate, school class size, school’s ninth grade size, parental educational level, parental income, and parental mental health, and included a 3-level exposure variable for diagnosed classmates (0 = none, 1 = 1, 2 = >1).
As a sensitivity analysis, we estimated the Cox proportional hazards regression models separately for all the mental disorder diagnosis categories (with the same category both as exposure and outcome). Since the number of cases where more than 1 diagnosed classmate was low for some diagnosis categories, a binary variable indicating the presence or lack of individuals diagnosed in the class (0 = no, 1 = yes) was used as a secondary exposure. As additional sensitivity analyses, we limited exposure diagnoses to 3 years preceding the start of follow-up, specifically focusing on diagnoses received during lower secondary education (grades 7-9) and, to control for incorrect registry information regarding school class divisions (eg, implausibly large classes), only considered school classes with sizes falling within 5th and 95th percentiles (corresponding to classes with 12-25 pupils). We also assessed the attenuating impact of the covariates and random intercepts by adding a random intercept per school and covariates in 3 domains (parental, school-level, and area-level) separately in a crude model adjusted for sex and birth year. Moreover, to elucidate possible differences in the 2001-2013 study period, we stratified it into 3 shorter time periods: 2001-2004, 2005-2008, and 2009-2013. A 2-tailed P value <.05 was considered to indicate statistical significance. The statistical analyses were done using Stata, version 16.1 (StataCorp LLC) and R Statistical Software, version 4.2.2 (R Foundation for Statistical Computing) survival (version 3.4.0) and coxme (version 2.2.18.1) packages.
Among the 713 809 cohort members, 50.4% were male and 49.6% were female. Median age at the start of follow-up was 16.1 (IQR, 15.9-16.4) years. Descriptive statistics of the exposure and outcome populations are reported in Table 1 (additional descriptive statistics are provided in eTable 2 in Supplement 1 ). During 7.3 million person-years of follow-up time, with a median of 11.4 (IQR, 7.4-14.4) years, 167 227 cohort members (25.1%) were diagnosed with a mental disorder, corresponding to an incidence rate of 2283 per 100 000 person-years at risk. Table 2 reports the incidence rates and HRs for the association between classmates diagnosed with a mental disorder and later risk of being diagnosed with a mental disorder for each diagnosis category. Having more than 1 diagnosed classmate with any of the examined mental disorders was associated with a 5% higher risk of later diagnosis (HR, 1.05; 95% CI, 1.04-1.06). The SD of the random intercepts for schools was 0.12, indicating that pupils in a school that was 1 SD above the mean had (e 0.12 = 1.13) 13% higher risk of being diagnosed with a mental disorder. Diagnosis-specific analyses revealed positive associations for mood, anxiety, and eating disorders, as well as the internalizing disorders category, even with only 1 diagnosed classmate. For behavioral and emotional disorders, as well as the externalizing disorders category, the findings were significant only with more than 1 diagnosed classmate.
Schoenfeld residual-based tests showed that the proportional hazards assumption held only for the schizophrenia spectrum, eating, and behavioral and emotional disorders models. In contrast, models for other diagnosis categories displayed larger coefficient values (or HRs) earlier in follow-up (eFigure 1 in Supplement 1 ). Figure 1 shows the HRs for the association between diagnosed classmates and later risk of being diagnosed with any of the examined mental disorders in 4 shorter follow-up time windows ( Figure 2 ; eFigure 2 and eTable 3 in Supplement 1 provide diagnosis-specific results). During the first year of follow-up, the risk of being diagnosed was 9% higher with 1 diagnosed classmate (HR, 1.09; 95% CI, 1.04-1.14) and 18% higher with more than 1 diagnosed classmate (HR, 1.18; 95% CI, 1.13-1.24). After the first year of follow-up, the risk of being diagnosed was statistically significant during years 4 and 5 with 1 diagnosed classmate with a mental disorder and in all 3 time windows with more than 1 diagnosed classmate with a mental disorder.
eFigure 3 in Supplement 1 shows the HRs for the association using binary exposure (see also eTable 4a in Supplement 1 ). The risk of being diagnosed with any mental disorder was 3% higher during the entire follow-up period (HR, 1.03; 95% CI, 1.02-1.04), 13% higher during the first year of follow-up (HR, 1.13; 95% CI, 1.08-1.18), and significantly increased also in the later time windows. Diagnosis-specific analyses showed that the risk was significantly increased for mood, anxiety, and internalizing disorders in each follow-up time window, with the greatest risks observed during the first year. For example, the risk of being diagnosed with a mood disorder was 21% higher during the first year of follow-up when a pupil was exposed to mood disorder (HR, 1.21; 95% CI, 1.13-1.29).
The results remained similar when considering only more recent exposure (diagnosis received during lower secondary education, ie, grades 7-9) as opposed to all previous childhood diagnoses (eTable 4b in Supplement 1 ), the most noticeable difference being that the association became statistically significant for schizophrenia spectrum disorders (HR, 1.17; 95% CI, 1.02-1.34). When repeating the analysis by limiting school class sizes within the 5th and 95th percentiles (12-25 pupils), the results remained similar, with no notable differences (eTable 4c in Supplement 1 ).
Assessing the impact of the different covariate domains, a crude model adjusted only for sex and birth year without a random intercept per school showed the highest HRs for all diagnosis categories. In contrast, a model including additional covariates describing area-level characteristics showed the largest reduction in HRs (eTable 5 in Supplement 1 ). For example, having classmates with a mood disorder diagnosis was associated with a 32% higher risk of being diagnosed with a mood disorder during the first year of follow-up (HR, 1.32; 95% CI, 1.23-1.41) in a model adjusted for sex and birth year without a random intercept per school. Including a random intercept per school decreased the risk to 24% (HR, 1.24; 95% CI, 1.16-1.32) and including covariates describing area-level characteristics further decreased the risk to 22% (HR, 1.22; 95% CI, 1.14-1.30). We also assessed differences in the 2001-2013 study period by stratifying it into 3 shorter periods (eTable 6 in Supplement 1 ). While the HRs showed a slight increase trend from the earliest to the latest period, the differences between the periods were statistically nonsignificant.
In our analysis of nationwide, interlinked registry data, including more than 700 000 individuals from 860 comprehensive schools in Finland, we found an association between having peers diagnosed with a mental disorder during adolescence and an increased risk of receiving a mental disorder diagnosis later in life. This risk was most pronounced in the first year of follow-up. The association showed a dose-response relationship, with higher risk when multiple diagnosed individuals were in the peer network. Of the mental disorders examined, the risk was greatest for mood, anxiety, and eating disorders. These associations were not explained by differences in area-level general morbidity or socioeconomic characteristics, parental mental disorders or socioeconomic position during childhood, or random differences in predisposition to mental health problems occurring among schools’ student populations.
To our knowledge, the present study is the largest and most comprehensive investigation on this topic to date. Our findings are consistent with previous studies reporting clustering of mood and/or anxiety symptoms in social networks of adolescents 6 , 13 and adults, 5 , 7 , 8 as well as with evidence suggesting similar social transmission of eating disorders. 17 For example, a longitudinal survey study with a school-based design showed that exposure to peers with depressive symptoms in the same school grade was associated with more depressive symptoms in a sample of 8290 adolescents. 6 Although using institutionally imposed peer network (eg, school grade or class) mitigates the self-selection bias often compromising studies on network peer effects, the study by Lee and Lee 6 is not immune to biases related to selection and attrition that are typical in longitudinal survey studies. We sought to minimize these biases by using institutionally imposed peer networks (school classes) in combination with population-wide registry data and found that exposure to a peer with a mental disorder is associated with an increased risk of mental disorder across several different diagnosis categories.
If mental disorders are transmitted socially via peer networks, the phenomenon could be explained by several mechanisms. One plausible mechanism is the normalization of mental disorders through increased awareness and receptivity to diagnosis and treatment when having individuals with diagnosis in the same peer network. 18 Similarly, having individuals with no diagnosis in the peer network might discourage seeking help for any underlying mental health problems. The observed higher risks of being diagnosed during the first year of follow-up after the exposure are consistent with this mechanism. Namely, due to diagnostic delay, the brief latency between exposure and diagnosis challenges the likelihood of harmful contagion occurring without an already existing, undiagnosed disorder. For some diagnosis categories, such as eating disorders, transmission could also occur through processes of peer social influence to which adolescents are particularly susceptible. 19 Another possible mechanism facilitating the transmission of certain mental disorders, such as depression, pertains to direct interpersonal contagion. For instance, it is conceivable that long-term exposure to a depressive individual could lead to gradual development of depressive symptoms through the well-established neural mechanisms of emotional contagion. 20
The primary strengths of the present study are its use of a nationwide study population tracked from adolescence up to age 34 years, inclusion of interlinked primary and secondary health care registry data, and reliance on institutionally imposed peer networks within a comprehensive school setting, mitigating self-selection bias. However, our findings should be interpreted in the context of the study’s limitations. First, while the observed associations were statistically significant, the HRs were relatively small. Therefore, we cannot rule out residual confounding due to unmeasured or inaccurately measured covariates in this cohort study. Second, it is expected that some individuals with underlying mental disorders refrain from seeking help from health care services, which implies that the reported mental disorder diagnoses are likely an underestimate of the true underlying prevalence of these disorders. Third, school class as an indicator for peer network is quite crude and the National Joint Application Register discloses information on school class divisions only for the final year (ie, ninth grade) of comprehensive school. Furthermore, although school classes in Finland are predominantly institutionally imposed without the freedom for pupils to choose their classmates, some schools have classes with special emphasis (eg, music or bilingual teaching) to which pupils are selected based on aptitude tests. 21 That said, classes within comprehensive schools in the Finnish educational system, particularly during lower secondary education (grades 7-9), are generally stable and transitions between classes are infrequent. 22 In addition, since Finland is a relatively small and homogeneous Nordic country with a health care system providing universal access to services for all citizens, replications of this study in other countries are necessary to evaluate the generalizability of our findings.
Based on a nationwide cohort of over 700 000 Finnish individuals, the results of this cohort study suggest a dose-response association between the number of persons with a mental disorder diagnosis in the same peer network during adolescence and later risk of being diagnosed with a mental disorder, even after accounting for a broad set of potential individual and environmental confounders. The association was most clearly present for mood, anxiety, and eating disorders. These findings suggest that mental disorders may be transmitted within adolescent peer networks. Consequently, prevention and intervention measures that consider potential peer influences on early-life mental health could substantially reduce the disease burden of mental disorders in society. Further research is required to clarify the mechanisms that explain these observed associations.
Accepted for Publication: March 15, 2024.
Published Online: May 22, 2024. doi:10.1001/jamapsychiatry.2024.1126
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Alho J et al. JAMA Psychiatry .
Corresponding Author: Jussi Alho, PhD, University of Helsinki, PO Box 21, 00014 Helsinki, Finland ( [email protected] ).
Author Contributions: Drs Alho and Hakulinen had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Alho, Gutvilig, Niemi, Elovainio, Hakulinen.
Acquisition, analysis, or interpretation of data: Alho, Gutvilig, Niemi, Komulainen, Böckerman, Webb, Hakulinen.
Drafting of the manuscript: Alho, Hakulinen.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Alho, Gutvilig, Niemi, Webb.
Obtained funding: Elovainio, Hakulinen.
Administrative, technical, or material support: Hakulinen.
Supervision: Hakulinen.
Conflict of Interest Disclosures: None reported.
Funding/Support: This study was funded by the European Union (ERC, MENTALNET, 101040247) and the Academy of Finland (354237 to Dr Hakulinen; 339390 to Dr Elovainio). Dr Webb is funded by the National Institute for Health and Social Care Research (NIHR) Manchester Biomedical Research Centre (NIHR203308) and by the NIHR Greater Manchester Patient Safety Research Collaboration (NIHR204295).
Role of the Funder/Sponsor: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: Views and opinions expressed in this article are those of the authors only and do not necessarily reflect those of the European Union or the European Research Council, or the NIHR or the Department of Health and Social Care.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World Psychiatry
- v.23(1); 2024 Feb
- PMC10786009
Borderline personality disorder: a comprehensive review of diagnosis and clinical presentation, etiology, treatment, and current controversies
Falk leichsenring.
1 Department of Psychosomatics and Psychotherapy, University of Giessen, Giessen Germany
2 Department of Psychosomatics and Psychotherapy, University of Rostock, Rostock Germany
Peter Fonagy
3 Research Department of Clinical, Educational and Health Psychology, University College London, London UK
Nikolas Heim
4 International Psychoanalytic University, Berlin Germany
Otto F. Kernberg
5 Personality Disorders Institute, Weill Cornell Medical College, New York NY, USA
Frank Leweke
Patrick luyten.
6 Faculty of Psychology and Educational Sciences, University of Leuven, Leuven Belgium
Simone Salzer
Carsten spitzer, christiane steinert.
Borderline personality disorder (BPD) was introduced in the DSM‐III in 1980. From the DSM‐III to the DSM‐5, no major changes have occurred in its defining criteria. The disorder is characterized by instability of self‐image, interpersonal relationships and affects. Further symptoms include impulsivity, intense anger, feelings of emptiness, strong abandonment fears, suicidal or self‐mutilation behavior, and transient stress‐related paranoid ideation or severe dissociative symptoms. There is evidence that BPD can be reliably diagnosed and differentiated from other mental disorders by semi‐structured interviews. The disorder is associated with considerable functional impairment, intensive treatment utilization, and high societal costs. The risk of self‐mutilation and suicide is high. In the general adult population, the lifetime prevalence of BPD has been reported to be from 0.7 to 2.7%, while its prevalence is about 12% in outpatient and 22% in inpatient psychiatric services. BPD is significantly associated with other mental disorders, including depressive disorders, substance use disorders, post‐traumatic stress disorder, attention‐deficit/hyperactivity disorder, bipolar disorder, bulimia nervosa, and other personality disorders. There is convincing evidence to suggest that the interaction between genetic factors and adverse childhood experiences plays a central role in the etiology of BPD. In spite of considerable research, the neurobiological underpinnings of the disorder remain to be clarified. Psychotherapy is the treatment of choice for BPD. Various approaches have been empirically supported in randomized controlled trials, including dialectical behavior therapy, mentalization‐based therapy, transference‐focused therapy, and schema therapy. No approach has proved to be superior to others. Compared to treatment as usual, psychotherapy has proved to be more efficacious, with effect sizes between 0.50 and 0.65 with regard to core BPD symptom severity. However, almost half of the patients do not respond sufficiently to psychotherapy, and further research in this area is warranted. It is not clear whether some patients may benefit more from one psychotherapeutic approach than from others. No evidence is available consistently showing that any psychoactive medication is efficacious for the core features of BPD. For discrete and severe comorbid anxiety or depressive symptoms or psychotic‐like features, pharmacotherapy may be useful. Early diagnosis and treatment of BPD can reduce individual suffering and societal costs. However, more high‐quality studies are required, in both adolescents and adults. This review provides a comprehensive update of the BPD diagnosis and clinical characterization, risk factors, neurobiology, cognition, and management. It also discusses the current controversies concerning the disorder, and highlights the areas in which further research is needed.
The term “borderline” was introduced in the psychiatric literature by Stern 1 and Knight 2 , to identify a patient group showing a level of functioning situated between neuroses and schizophrenic disorders. This patient group was not well defined. An important progress occurred with Kernberg's introduction of the concept of borderline personality organization 3 , 4 , marked by the use of primitive defense mechanisms such as splitting or projective identification, identity diffusion (shifting between all‐good and all‐bad), and severely disturbed object relationships 3 . Reality testing was largely intact, differentiating individuals with borderline personality organization from psychotic patients 3 . Another early contribution was provided by Grinker et al 5 , who empirically identified four features of the “borderline syndrome”: anger, impaired close relationships, identity problems, and depressive loneliness.
In 1980, borderline personality disorder (BPD) was introduced in the DSM‐III 6 , based on a study by Spitzer et al 7 , who drew both on research by Gunderson and colleagues 8 , 9 and on Kernberg's concept of borderline personality organization 3 , by including specific problems of identity and interpersonal relationships characterized by sudden shifts from one extreme to another (e.g., from all‐good to all‐bad or vice versa). This early research showed that BPD could be discriminated with sufficient accuracy from both schizophrenia and (neurotic) depression, as well as from other personality disorders 10 , 11 .
In the following more than four decades, a plethora of research has been carried out on BPD, much more than on any other personality disorder. This research has focused on the diagnosis of BPD, its etiology (including genetics, neurobiology, and interactions between genetics/neurobiology and adverse childhood experiences), epidemiology, course and prognosis, cognition, and the effectiveness of pharmacotherapies and psychotherapies 12 , 13 , 14 , 15 , 16 , 17 , 18 .
BPD remains a challenging disorder, from both research and clinical perspectives. At present, for example, there is still controversy concerning its conceptualization as either a specific personality disorder or a level of general impairment in personality functioning 19 , 20 , 21 . The treatment of BPD remains challenging as well. As to pharmacotherapy, there is no consistent evidence showing that any psychoactive medication is efficacious for the core features of the disorder 16 . Indeed, no medications have been approved by regulatory agencies for treating BPD 16 , 22 . According to the UK National Institute for Health and Care Excellence (NICE), pharmacotherapy should only be used to treat discrete and severe comorbid anxiety or depressive symptoms or psychotic‐like features, or to manage acute crises, and should be administered for the shortest time possible 22 . Psychotherapy is the treatment of choice for BPD, with various approaches having proved to be efficacious in randomized controlled trials (RCTs) 14 , 17 , 22 . However, almost 50% of BPD patients do not respond sufficiently to psychotherapy 23 , so that further research in this area is clearly warranted. Whether specialized methods of psychotherapy or more generalist approaches are required for the treatment of BPD is a debated issue 24 , 25 , 26 .
This paper provides a comprehensive review of BPD diagnosis and clinical characterization, course, epidemiology, risk factors, neurobiology, social cognition and neurocognition, and management. Current controversies (e.g., categorical vs. dimensional approaches to diagnosis; specific vs. generalist psychotherapy interventions) are also discussed, and major areas in which further research is warranted are highlighted.
DIAGNOSIS AND CLINICAL CHARACTERIZATION
The DSM‐5 characterizes BPD as a pervasive pattern of instability of interpersonal relationships, self‐image and affects, and marked impulsivity, emerging by early adulthood and present in a variety of contexts, as indicated by five or more of a set of nine criteria 27 (see Table 1 ).
DSM‐5 criteria for borderline personality disorder 27
The DSM‐5 alternative dimensional model requires for BPD the presence of moderate or greater impairment in personality functioning, manifested by difficulties in at least two of the following areas: an unstable self‐image (identity); unstable goals and values (self‐direction); compromised ability to recognize the feelings and needs of others (empathy); and intense, unstable and conflicted close relationships (intimacy). In addition, four or more of the seven following personality traits are required (at least one of which must be impulsivity, risk taking or hostility): emotional lability, anxiousness, separation insecurity, depressivity, impulsivity, risk taking, and hostility. Impairments in personality functioning and pathological personality traits are required to be relatively pervasive and stable 27 (see Table 2 ).
Proposed criteria for borderline personality disorder in the alternative DSM‐5 model for personality disorders 27
An important aspect omitted in the DSM‐5 criteria for BPD is regression proneness (i.e., showing emotions or behaviors not adequate to age) in unstructured situations, one of the reasons for many of the treatment problems occurring with the disorder 28 . Regression proneness has been empirically demonstrated by use of unstructured psychological tests such as the Rorschach or the Thematic Apperception Test (TAT) 29 , 30 , 31 , 32 . In these tests, patients with BPD tend to show bizarre‐idiosyncratic primary process thinking, usually associated with the activation of low‐level defense mechanisms and object relations 31 , 32 , 33 .
In the ICD‐11, the categorical system of personality disorders has been replaced by a dimensional approach similar to the DSM‐5 alternative model 34 . Of the DSM‐5 personality disorders, only BPD remains distinct and unique, by use of the “borderline pattern specifier”. In the ICD‐11, a diagnostician's task is to rate the severity level of personality dysfunction as “mild”, “moderate” or “severe”. In addition, the patient may be described on five domains (negative affectivity, detachment, dissociality, disinhibition, and anankastia). While in the clinical setting most patients with BPD can be expected to be classified as having a severe personality disorder, the ICD‐11 allows to rate BPD patients in whom some areas of personality functioning are relatively less affected as suffering from a moderate personality disorder 35 .
The ICD‐11 borderline pattern specifier may be applied in the presence of at least five of the following requirements: a) frantic efforts to avoid real or imagined abandonment; b) unstable and intense interpersonal relationships, which may be characterized by vacillations between idealization and devaluation; c) identity disturbance, manifested in unstable self‐image; d) a tendency to act rashly in states of high negative affect, leading to potentially self‐damaging behaviors; e) recurrent episodes of self‐harm; f) emotional instability due to marked reactivity of mood; g) chronic feelings of emptiness; h) inappropriate intense anger or difficulty controlling anger; and i) transient dissociative symptoms or psychotic‐like features. Further manifestations which may be present include a view of the self as inadequate; an experience of the self as profoundly different and isolated from other people; and proneness to rejection hypersensitivity (see Table 3 ).
Requirements for the borderline pattern specifier in the ICD‐11 34
Proposals to describe BPD by the five‐factor model of personality 36 characterize it by high levels of both neuroticism (anxiousness, angry hostility, depressiveness, impulsiveness, vulnerability) and openness (high openness to feelings and actions), and by low levels of both agreeableness (low compliance) and conscientiousness (low deliberation) 37 , 38 . Another approach to define and conceptualize BPD focuses on major dimensions of psychopathology: most researchers agree that the dimensions which capture the essence of the disorder are emotional dysregulation, impulsivity and behavioural dysregulation, and interpersonal hypersensitivity 38 .
With nine DSM‐5 criteria and a threshold for diagnosis of five positive criteria, there are 256 theoretically possible ways to meet the criteria for BPD 39 . Thus, despite conceptual coherence 40 , BPD appears to be a heterogeneous diagnostic category which may include patient subtypes 41 . A cluster analysis, for example, found three clusters: a large one with “core” BPD symptoms; an extravert/externalizing one characterized by high levels of histrionic, narcissistic and antisocial features; and a small one of patients with marked schizotypal and paranoid features 42 .
Although still utilized with caution, the diagnosis of BPD in adolescents is no longer controversial. Early detection of BPD (or subthreshold features of the disorder) facilitates a timely treatment of these young patients, reducing individual suffering and societal costs 43 . In the past, several arguments were used against BPD diagnosis prior to the age of 18, including the not uncommon occurrence of affective instability and irritation regarding self‐image in adolescents, and the potential harm due to stigmatization. Today, there is a consensus regarding the potential appropriateness and usefulness of BPD diagnosis in the youth. This is also reflected by the latest developments in the ICD‐11 and DSM‐5 27 , 34 , where the age threshold for the diagnosis has been omitted. The diagnosis of BPD can be regarded as being as reliable and valid in adolescence as in adulthood 44 , 45 . A community‐based study conducted in the US found a point prevalence for adolescents at around 1% and a cumulative prevalence of 3% up to the age of 22 46 . As in adults, prevalence rates in outpatient and inpatient psychiatric settings are considerably higher 47 , 48 .
In older patients with BPD, symptoms shift to more depression, emptiness and somatic complaints 49 , 50 . Emotional dysregulation, unstable interpersonal relationships, anger and attachment insecurity persist, whereas impulsivity and identity disturbances decrease 49 , 50 . Self‐harm may take other forms, such as non‐adherence to medical regimes or misuse of medication 50 .
Individuals with BPD are likely to have co‐occurring lifetime mood disorders (83%), anxiety disorders (85%), substance use disorders (78%), and other personality disorders (53%) 51 , 52 , 53 . BPD and bipolar I or II disorder co‐occur in about 10‐20% of patients with either disorder 54 , 55 . Although BPD is often comorbid with major depressive disorder or bipolar disorder, the additional diagnosis of BPD should not be made in an episode of those disorders if there is no evidence that the typical BPD symptomatological pattern persists over time.
Among people with attention‐deficit/hyperactivity disorder, the lifetime rate of BPD was found to be 37.7% 56 . Eating disorders are also common among individuals with BPD, with median rates of 6% for anorexia nervosa, 10% for bulimia nervosa and 22% for eating disorders not otherwise specified 53 . Of individuals with BPD, 30% were diagnosed with post‐traumatic stress disorder (PTSD), and 24% of individuals with this latter disorder were diagnosed with BPD 57 .
Although there is a considerable overlap between BPD and the construct of complex PTSD (CPTSD) introduced in the ICD‐11 – both disorders include problems in affect regulation, self‐concept and interpersonal relationships – there is evidence that they can be empirically differentiated 58 , 59 . In particular, difficulties in affect regulation in CPTSD are ego‐dystonic, stressor‐specific and variable over time, whereas in BPD they tend to be ego‐syntonic and persistent. Moreover, in contrast with the unstable self‐concept in BPD, individuals with CPTSD have a consistently negative sense of self. Finally, the high rates of impulsivity and suicidal and self‐injurious behaviors of BPD are not observed in CPTSD 59 .
The above high levels of comorbidity may be an artefact of the categorical approach to psychiatric disorders, as also evidenced by the considerable overlap between BPD and the general psychopathology or p factor 60 , 61 , 62 , 63 . It has been argued that this overlap may represent a more parsimonious way not only to explain the high “comorbidity” associated with BPD, but also its large negative impact on functioning 64 .
BPD can be reliably diagnosed by semi‐structured interviews. Several reliable and validated interview methods exist 65 , 66 , 67 , 68 , 69 . In addition, self‐report questionnaires and projective techniques such as the Rorschach or the TAT have proved to be helpful, especially with regard to assessing the level of personality functioning 28 , 29 , 31 , 32 , 54 (see Table 4 ). Sensitive diagnostic instruments for BPD in the elderly, however, need to be developed 50 .
Major diagnostic interviews, self‐report questionnaires, and projective techniques available for borderline personality disorder (BPD)
BPD seems to be less stable over time than traditionally believed 54 . Considerable rates of recovery and relatively low rates of relapse have been reported in both short‐term and long‐term naturalistic follow‐up studies 54 , 82 . In a 10‐year prospective follow‐up study, 50% of patients with BPD achieved recovery (i.e., symptomatic remission and good social and vocational functioning during the past two years), while 93% of them showed symptomatic remission lasting two years, and 86% remission lasting four years 82 . Thirty‐four percent of patients lost their recovery and 30% their remission status after a two‐year long remission 82 . Of note, most individuals received pharmacotherapy or psychotherapy, so that the above remission rates may not reflect the natural history of untreated BPD 83 .
A meta‐analysis of studies on the long‐term course (≥5 years) of BPD reported a mean remission rate of 60%, associated with high heterogeneity between studies (I 2 =80.9%) 84 . Excellent recovery (i.e., remission of symptoms and good social and full‐time vocational functioning) was achieved in 39% of BPD patients compared with 73% in other personality disorders 85 .
Patients with BPD show poorer social functioning than those with other mental disorders, including major depressive disorder and other personality disorders 86 , 87 . Only approximately 16% of people with BPD were reported to be married or living with a partner 88 . Social functioning was found to be unstable and highly associated with the symptomatic status 83 , 88 , 89 . Those patients who experienced change in personality pathology showed some improvements in functioning 83 , 88 , 89 , 90 , 91 . There is evidence that changes in personality traits (defined by the five‐factor model) are followed by changes in BPD psychopathology, but not vice versa 92 . Traits were found to be more unstable in BPD than in patients with other personality disorders, indicating a “stable instability” 93 .
BPD features tend to decline over time, and this process seems to be in part influenced by temperament 94 . However, diagnostic instruments may not be sensitive enough to tap the shift in symptoms in older populations to more depression, emptiness and somatic complaints 49 , 50 .
EPIDEMIOLOGY
The age of onset of BPD varies, but symptoms are usually manifest in early adulthood 27 . In the adult general population, rates for BPD range between 0.7 and 2.7% 95 , 96 . In primary care, psychiatric outpatients and psychiatric inpatients, prevalence rates of 6%, 11‐12% and 22%, respectively, have been found 96 , 97 . In a US community sample, 2.7% of individuals had been diagnosed with BPD in their lifetime, with only slightly higher rates for women compared to men (3% vs. 2.4%) 52 . In a psychiatric outpatient setting, however, considerably higher rates of BPD were found in women compared to men (72% vs. 28%) 97 . There are gender differences in comorbidity: men with BPD display more frequently substance abuse and antisocial personality disorder, while women more frequently present with mood, anxiety and eating disorders, and PTSD 98 .
The rate of death by suicide is higher among individuals with BPD than in patients with other personality disorders (5.9% vs. 1.4%) 99 . These results are consistent with those of a recent meta‐analysis which reported suicide rates of 2 to 5% (mean 4%) over follow‐up periods of 5 to 14 years among people with BPD 84 . Suicide attempts occurred in more than 75% of BPD individuals 100 .
In addition, BPD patients have a higher prevalence of somatic comorbidities – such as endocrine, metabolic, respiratory, cardiovascular and infectious (e.g., human immunodeficiency virus infection, HIV; hepatitis) diseases – than persons without BPD 101 , 102 . Mortality by non‐suicide causes is clearly increased, with 14% of BPD patients and 5.5% of those with non‐BPD personality disorders dying over a 24‐year follow‐up 99 . Compared with patients without BPD who had other mental disorders or medical conditions, BPD was associated with a 2.3‐fold increase in mortality rate during a 2‐year follow‐up 101 .
Patients with BPD die on average 14‐32 years earlier than subjects in the general population 99 , while some studies report lower lifetime loss (6‐7 years) 101 . Loss of lifetime years is more pronounced in men 101 . Compared to individuals without BPD, men with BPD had a poorer lifetime expectancy than women with BPD, with an odds ratio (OR) of 2.40 (95% CI: 1.93‐2.54) vs. 2.21 (95% CI: 2.08‐2.77) 101 .
These data suggest recommending BPD patients to engage in regular medical check‐ups 103 . Increased health problems and associated higher mortality may reflect both unhealthy lifestyle and more direct neurobiological dysregulation of the stress and immune system associated with high levels of early adversity in BPD. Indeed, chronic physical diseases are strongly associated with “immature” personality 104 , for which BPD may serve as a prominent example.
BPD is associated with intensive treatment utilization, and with societal costs exceeding those of anxiety and depressive disorders, diabetes, epilepsy and Parkinson's disease 54 , 87 , 101 , 105 . Thus, BPD constitutes a significant public health concern.
RISK FACTORS
It is currently hypothesized that, in BPD, genetic factors and adverse childhood experiences interact to influence brain development via hormones and neuropeptides 54 , 106 . Adverse childhood experiences are thought to modulate gene expression and lead to stable personality traits that may predispose to BPD 54 .
There is familial aggregation of BPD 54 , 107 , with recent data from a Swedish population‐based study estimating heritability at 46% 108 . The risk of receiving a BPD diagnosis was increased 4.7‐fold for full siblings 108 . The hazard ratio in identical twins was 11.5 (95% CI: 1.6‐83.3). However, no single nucleotide polymorphisms associated with BPD have been identified 38 , 109 , and some evidence of a genetic overlap of BPD with bipolar disorder, major depression and schizophrenia has emerged 109 . Results of epigenetic studies yielded inconsistent results and are often limited by small sample size 38 , 110 . Further large scale studies that are sufficiently powered to detect effects of genes on BPD phenotype are required 38 . In addition, more reliable measures of this phenotype are needed.
Adverse childhood experiences – including physical, sexual and emotional abuse, and neglect – are significantly associated with BPD 111 , 112 . Consistent with these findings, BPD has been associated with high levels of disorganized and unresolved patterns of attachment 113 . Borderline personality traits were associated with prior significant negative experiences in 12‐year‐old children 107 . This effect was more pronounced when families had psychiatric histories. While multiple psychosocial factors, including maltreatment, are associated with an increased risk for BPD, these findings do not seem to be disorder‐specific 111 .
Inherited and environmental risk factors are thought to contribute independently and interactively to the etiology of BPD. Recent findings on familial clustering and heritability of clinically diagnosed BPD, which revealed a 54% contribution from unshared, individually unique environmental factors, point in this direction 108 .
There is increasing evidence that BPD is associated with both early and later adversity, leading to vicious interpersonal cycles. This is, for instance, evidenced by high levels of revictimization in romantic relationships and bully‐victim relationship with peers, leading to increasing levels of distrust in others and social isolation 114 , 115 , 116 , 117 , 118 . Moreover, there is growing evidence that social deprivation and societal inequality may increase the risk for BPD, which may be related to high levels of distrust and sensitivity to social rejection and injustice in individuals with BPD 119 , 120 , 121 . These results point to the need of considering vulnerability to BPD from a broad, socio‐ecological and transactional perspective 113 , 115 .
NEUROBIOLOGY
A large number of studies have been conducted on the neurobiological underpinnings of BPD. Although several brain areas and neurotransmitters have been identified as potentially involved, only few findings have been confirmed by meta‐analyses.
At the neuroendocrinological level, dysfunctions of the hypothalamic‐pituitary‐adrenal (HPA) axis, with altered levels of cortisol, have been suggested to underlie the impaired stress responses characteristic of BPD. One meta‐analysis found significantly lower mean basal cortisol levels in individuals with BPD compared to non‐psychiatric controls, with a small effect size of g=–0.32 (95% CI: –0.56 to –0.06, N=546, n=12, I 2 =53%) 122 . Yet, a more comprehensive meta‐analysis found no significant differences in singular cortisol assessments between individuals with BPD and healthy controls or individuals with other mental disorders, although heterogeneity between studies was high and moderate, respectively 123 . In a sub‐analysis of five studies investigating continuous cortisol output, BPD patients’ cortisol response to psychosocial challenges was blunted relative to healthy controls as well as to individuals with other personality disorders 123 . It is unclear whether disturbed HPA axis functioning is specifically associated with BPD or may rather be understood as a consequence of trauma exposure common in many psychiatric disorders 124 . However, research evidence is consistent with the allostatic load hypothesis, suggesting that the blunted cortisol response in BPD reflects a compensatory down‐regulation consequent to adversity and stress.
Oxytocin has been also implicated in BPD, with particular relevance for interpersonal functioning, given its purported role in attachment behavior and social cognition 125 . A recent meta‐analysis found decreased oxytocin levels among women with BPD (standardized mean difference, SMD=–0.46, 95% CI: –0.90 to –0.02; N=131, n=4, I 2 =64%) 126 . However, the number of studies included was small, heterogeneity was moderate, and there were no significant differences with other personality disorders 126 . Furthermore, the administration of exogenous oxytocin in BPD patients has yielded inconsistent and paradoxical effects 127 . Further research is required to determine the role of oxytocin in BPD, in particular whether the observed impairments in the oxytocinergic system reflect a transdiagnostic vulnerability factor associated with early adversity and disturbed parent‐infant attachment 125 , or psychopathology in general 126 .
In terms of neural systems, the most widely held hypothesis suggests a fronto‐limbic imbalance in BPD, in which emotion dysregulation is mediated by hyperactivity of limbic structures (e.g., amygdala, hippocampus and anterior cingulate cortex) and abnormal functioning of prefrontal structures 128 . However, only tentative conclusions can be drawn on the neurobiology of BPD, as most neuroimaging studies are severely underpowered 129 .
The most robust meta‐analytic result of neuroimaging studies in BPD is hyperactivity of the amygdala and hippocampal area during emotional processing experiments 130 , 131 , 132 , which seems to be accompanied by impairments in habituation of the amygdala to repeated negative stimuli 133 , 134 , 135 , 136 , 137 , 138 . While earlier meta‐analyses found a reduction in hippocampal and amygdala volume in BPD 139 , 140 , a more recent and comprehensive meta‐analysis reported no gray matter alterations 141 . Although the amygdala is assumed to be involved in emotional evaluation and recognition of subjectively dangerous situations, its exclusive role in processing negative emotions has recently been challenged, as studies have shown that amygdala activation is only marginally involved in the prediction of subjective fear ratings 142 , correlates with the experiencing of positive emotions 143 , and might rather indicate saliency for faces than threats 144 . Furthermore, despite the common conceptualization of the amygdala as the brain's “fear center”, inconsistent meta‐analytic evidence has been found for its involvement in processing threats 145 , 146 . Hence, negative emotional experiencing cannot be confidently inferred from amygdala hyperactivity in BPD 147 .
Research on abnormal prefrontal functioning lacks spatial specificity in BPD 147 , 148 , and meta‐analyses have yielded conflicting results, with an earlier one finding abnormal functioning in prefrontal areas 131 , while the most recent and comprehensive one reported no significant differences to healthy controls 132 , although again the marked heterogeneity of BPD may be an important factor explaining inconsistent findings.
Connectivity analyses could test assumptions of reduced prefrontal top‐down regulation on limbic areas such as the amygdala. However, only very few studies have investigated connectivity during emotion regulation tasks in BPD 149 . A considerable number of studies have investigated resting‐state connectivity in BPD, yielding conflicting results with respect to the fronto‐limbic imbalance hypothesis 150 , 151 , 152 .
Taken together, to date there is only weak evidence that a fronto‐limbic imbalance underlies emotion dysregulation in BPD 147 . Moreover, most neuroimaging findings lack specificity to BPD and might rather relate to transdiagnostic factors of psychopathology 131 , 153 or to childhood maltreatment 134 , 147 , 154 , 155 , 156 , 157 . Recent research efforts point to the possible role in BPD of impairments in the temporoparietal junction 158 , which is thought to play a crucial role in distinguishing self from other, so that its impairments might underlie the typical self‐other distinction problems (i.e., identity diffusion) observed in BPD patients. However, meta‐analyses are not yet available and the small number of studies preclude drawing strong conclusions.
In summary, although brain areas and neurotransmitters have been identified as potentially involved in BPD, an integrated and empirically supported neurobiological model of the disorder does presently not exist. Research on the neurobiology of BPD is complicated by several factors, including the high prevalence of comorbidities, the heterogeneity of the condition, the use of medication, as well as substantial differences in experimental designs.
SOCIAL COGNITION AND NEUROCOGNITION
Over the past decade, empirical studies on social cognition have advanced our understanding of interpersonal and emotional dysfunction in BPD. The disorder appears to be characterized by relatively severe impairments in mentalizing, i.e., the capacity to understand the self and others in terms of intentional mental states, as a result of largely affect‐driven, externally‐cued processing of social information. Results are not always consistent, which may be due to the type of tasks used (e.g., some social cognition tasks show ceiling effects or primarily rely on “cold” social cognition, whilst mentalizing impairments mainly tend to emerge in high‐arousal contexts in BPD patients) and the influence of factors involved in the etiology of the condition (e.g., severity of trauma or attachment style).
A recent systematic review 159 of experimental studies on social cognition in BPD based on the Systems for Social Processes approach of the Research Domain Criteria included four meta‐analyses, concerning more basic (i.e., emotion recognition accuracy and reaction time) and more complex (i.e., understanding of mental states and ostracism) features of mentalizing with regard to others. Individuals with BPD showed reduced accuracy for recognizing facial emotional expression in others compared to healthy controls, with a significant moderate effect size of g=–0.41 (95% CI: –0.57 to –0.25; n=18, I 2 =21%). There was no evidence for differences with respect to reaction time in detecting facial emotions (g=0.27, 95% CI: –0.04 to 0.59, n=8, I 2 =27%). As to the widely held hypothesis of an anger bias in BPD, the evidence of the systematic review was inconsistent, although the number of included studies was very small (n=4). Another meta‐analysis found evidence for an attentional bias to negative and personally relevant negative words rather than an attentional bias towards facial stimuli 160 .
Strong rejection sensitivity (ostracism) was found in BPD. Following perceived social exclusion, individuals with BPD experienced substantially more negative emotions and reported a greater threat to needs relative to healthy controls, with a large effect size (g=1.13, 95% CI: 0.67‐1.59, n=10) 159 . Although there was significant heterogeneity and evidence for publication bias, people with BPD showed greater levels of ostracism compared to individuals with other mental disorders (e.g., social anxiety disorder, major depressive disorder), with a medium effect size (g=0.67, 95% CI: 0.16‐1.18). These findings from experimental studies are consistent with those of other meta‐analyses, reporting strong expectancy of social rejection assessed by self‐report in BPD compared to normal controls 120 , 161 , 162 . However, heterogeneity between studies was again large, and there was evidence for publication bias.
Notably, one meta‐analysis found a larger difference in negative affectivity following social inclusion (d=1.00, 95% CI: 0.76‐1.25, I 2 =78%) than social rejection (d=0.68, 95% CI: 0.57‐0.80, I 2 =68%) in individuals with BPD compared to non‐BPD groups 120 . However, heterogeneity was high and significant. Although these findings await confirmation, disturbed perceptions of both social exclusion and inclusion might be one explanation for the marked instability in close relationships in BPD. Further evidence for this comes from a meta‐analysis of 26 studies on romantic attachment in BPD patients 163 . The disorder was significantly correlated with attachment anxiety (r=0.48, I 2 =77%), but also with attachment avoidance (r=0.30, I 2 =74%) 163 . Heterogeneity was significant. Hence, a combination of both forms of attachment difficulties might underlie BPD, which is consistent with the assumption that the disorder, and its severe cases in particular, is related to a disorganization of the attachment system characterized by strong push‐pull cycles in close interpersonal relationships 164 , 165 .
The above‐mentioned meta‐analysis of experimental studies 159 also found, in BPD patients compared to healthy controls, a significantly poorer understanding of mental states in others, as assessed with Theory of Mind (ToM) tasks 166 , with a medium effect size (g=–0.45, 95% CI: –0.75 to –0.16, n=24). However, there was high heterogeneity between studies (I 2 =85%). Individuals with BPD also showed greater deficits in inferring others’ mental states in comparison to people with other mental disorders, with a medium effect size (g=–0.53, 95% CI: –1.03 to –0.03). Heterogeneity was high (I 2 =64%). These findings are largely consistent with those of other meta‐analyses of studies using ToM tasks 167 , 168 .
Moreover, in a meta‐analytic evaluation 169 , significant impairments were found in studies of mentalizing involving ToM tasks in BPD compared to healthy controls (d=0.36, 95% CI: 0.24‐0.48, n=31, N=2,737, I 2 =50%). Deficits in mentalizing assessed by self‐report were more pronounced (d=1.84, 95% CI: 1.64‐2.04, n=4, N=595, I 2 =0%). These findings are consistent with a meta‐analysis finding a strong correlation between deficits in mentalizing with regard to the self, assessed in terms of emotional awareness or alexithymia, in BPD compared to healthy controls (r=0.52, 95% CI: 0.41‐0.61, n=15) 170 .
Yet, one recent meta‐analysis found evidence for a role of excessive mentalizing or hypermentalizing in BPD (r=0.26, 95% CI: 0.12‐0.39, n=10), which was, however, comparable to other mental disorders 171 . Although hypermentalizing may be related to psychopathology in general rather than BPD in particular, these findings suggest that BPD is not simply associated with general deficits in mentalizing, but with a specific imbalance which can be expressed in hypomentalizing as well as hypermentalizing. This interpretation is consistent with research findings suggesting that BPD is associated with a predominance of automatic, affect‐driven and largely externally‐based mentalizing, with little possibility for more controlled, cognitive and internally‐based mentalizing, specifically in high‐arousal contexts 172 . However, more longitudinal research is needed, as there is evidence that mentalizing problems and BPD features reciprocally interact over time, and meta‐analytic evidence for a specific mentalizing profile in BPD patients is currently lacking.
A meta‐analysis of 3,543 participants 173 found that BPD symptomatology was associated with less frequent use of adaptive emotion regulation strategies (i.e., cognitive reappraisal, problem solving, and acceptance) and more frequent use of maladaptive ones (i.e., suppression, rumination, and avoidance). The role of rumination as a dysfunctional emotion regulation strategy in BPD was also confirmed by two recent meta‐analyses 174 , 175 . Furthermore, a meta‐analysis found stronger self‐report of experienced shame in comparison to healthy controls, with a large effect size of d=1.44 (n=10, N=3,543) 176 . However, there was significant heterogeneity and evidence for publication bias.
Lastly, there is preliminary evidence of negative self‐evaluation 159 , 177 , lack of cooperation/trust 178 , 179 , impairments in self‐other distinction 180 , disturbed interoception 181 , and splitting 179 in BPD patients, but meta‐analytic evaluations have yet to confirm these hypothesized deficits.
Deficits in neurocognition in BPD were demonstrated in a meta‐analysis of 207 effect sizes across cognitive domains, reporting a medium overall effect size for impaired neuropsychological functions in BPD compared to healthy controls (d=–0.48, 95% CI: –0.58 to –0.43, N=9,332) 182 . However, heterogeneity was significant. The strongest impairments were found for decision making (d=–1.41, 95% CI: –0.91 to –1.91), memory (d=–0.57, 95% CI: –0.64 to –0.58), and executive functioning (d=–0.54, 95% CI: –0.64 to –0.43) 198 . These results are in line with other meta‐analyses 183 , 184 .
In summary, meta‐analyses support a complex pattern of alterations in social cognition and neurocognition in BPD. The most robust findings are impairments in emotion recognition accuracy, an attentional bias towards negative stimuli, marked rejection sensitivity following social exclusion as well as inclusion, imbalances in mentalizing, dysfunctional emotion regulation, and deficits in neurocognition. Limitations are that most meta‐analyses showed substantial heterogeneity, and results are often not specific to BPD. Further research is required to develop a more comprehensive understanding of the role of social cognition and neurocognition in BPD.
As a first step of management, BPD patients need to be informed about the diagnosis, expected course, putative risk factors, and treatment options 54 . Psychotherapy should be recommended as the first‐line treatment, with pharmacotherapy as a possible adjunctive treatment in specific situations. Clear boundaries should be set, response to provocative behavior should be avoided, and a consistent approach should be agreed upon with all involved clinicians, in order to prevent a situation in which some of them are regarded as “bad” and others as “good”. If present, life‐threatening behaviors need to be addressed first.
Managing life‐threatening behaviors
Life‐threatening behaviors (e.g., suicidal, self‐mutilating or high‐risk behaviors, attacks against others) must be given priority. Verbal interventions entail a calm attitude, understanding the crisis from the person's point of view, empathic open questions, and stimulating reflections about solutions. Sedative or antipsychotic medications may be used for the treatment of crises, but for no longer than one week 185 .
For understanding and managing suicidality, the following recommendations can be given 186 , 187 . The therapist needs to clarify the acute danger of committing suicide (e.g., has the patient already developed a plan on how to commit suicide; has the patient previously made a suicide attempt; is impulse control severely impaired, e.g. by substance misuse; is there a lack of social support system; is the patient trustful with regard to agreements?). It should then be explored whether there is a major depressive disorder requiring pharmacotherapy or inpatient treatment. If this is not the case, clarifying the trigger of the present suicidality is required (e.g., interpersonal loss, shift from all‐good to all‐bad). Suicide may be experienced by the patient as a solution of a problem (e.g., stopping anxiety, despair, loneliness, emptiness, or anger). Discussing what makes life intolerable may help to move the focus from suicide to life's wounds. Other solutions may emerge. Focusing on black‐and‐white images of the self or of others related to the triggering situation may be helpful.
Suicidal threats may be used by the patient to force the clinician not to abandon him/her (as others may have done). As a result, the clinician may feel as helpless or angry as the patient, or being tortured. The clinician is recommended not to counteract aggressively – e.g., by trying to get rid of the patient (thus confirming the patient's experiences and expectations). Instead, the clinician may convey that he/she is concerned and trying to help the patient to reduce his/her suicidal pressure, but that ultimately it will be up to the patient to decide what to do. It is recommended to make a contract that commits the patient not to act on suicidal impulses, but to discuss them in the sessions or to go to emergency psychiatric services if he/she feels that suicidal impulses cannot be controlled. Evidence‐based psychotherapies for BPD include detailed recommendations about how to treat suicidality 187 , 188 , 189 (see below).
Pharmacotherapy
Up to 96% of patients with BPD seeking treatment receive at least one psychotropic drug 190 . Polypharmacy is common 191 , 192 : almost 19% of patients with BPD report taking four or more psychotropic drugs 193 . However, no class of psychoactive medications has consistently proven to be efficacious, and no medication has been approved by the US Food and Drug Administration (FDA) for BPD 194 .
Pharmacotherapy is not recommended for the treatment of any core symptom of BPD, but only for addressing discrete and severe comorbid disorders such as severe depression or anxiety or transient psychotic symptoms, and only for the shortest possible time and as a treatment in crises 22 . It should be noticed, however, that there are only a few RCTs focusing on BPD with distinct comorbidities 16 , as most trials excluded patients with comorbid major depressive disorder, bipolar disorder, psychotic disorders or substance‐related disorders. Short‐term symptoms of depression or anxiety that are part of the BPD emotional instability and can be related to specific triggering situations must not be misinterpreted as reflecting comorbid disorders. For insomnia in BPD, general advice about sleep hygiene without medication prescription is recommended 22 . For severe insomnia, Z‐drugs (e.g., zolpidem or eszopiclone) may be prescribed 22 . Due to concerns over dependence, the use of Z‐drugs is recommended only for severe insomnia, with the lowest possible dose and for no longer than four weeks 195 .
Acute suicidality or psychotic crises may necessitate psychotropic medication, as well as severe agitation or dissociative states, or pronounced difficulties in controlling aggression. At present, no RCTs exist on the use of psychotropic drugs in manifest crises of patients with BPD 194 . Due to the high comorbidity of BPD with addictive disorders 196 , 197 , the use of substances with dependence potential should be avoided as far as possible. Sedative antihistamines (such as promethazine) or low‐potency antipsychotics (such as quetiapine) may be preferred. After the acute crisis has subsided, the medication should be discontinued.
Psychotherapy
Psychotherapy is regarded as the first‐line treatment for BPD 22 , 54 , 198 . Guidelines do not recommend brief forms of psychotherapy lasting less than three months 22 . However, although a number of specialist treatments – i.e., dialectical behavioral therapy (DBT), mentalization‐based therapy (MBT), transference‐focused psychotherapy (TFP), and schema therapy (ST) – for BPD have been developed and empirically supported, their implementation in routine clinical practice remains patchy. If evidence‐based methods of psychotherapy are not available, experienced mental health professionals may apply psychoeducation or crisis management 26 .
Evidence has emerged for generalist models of treating patients with BPD, that incorporate features of specialized evidence‐based treatments, and can be carried out by experienced clinicians without a training in those treatments 199 . Of note, however, these treatment models, which typically served as comparison conditions in trials of specialized methods of psychotherapy, followed manuals or manual‐like guidelines, and therapists received supervision by experts as well 200 , 201 , 202 . Thus, as discussed in more detail below, further research is required to establish whether generalist models are as efficacious as the specialized treatments with respect to all outcomes.
Further efforts are needed to decrease the stigma associated with BPD among both the general public and health care workers. It often takes many years before individuals with BPD seek help and, when they do, they are unfortunately often still met with stigma with regard to the nature and treatability of their problems in many health care settings 203 , 204 .
In the following sections, we discuss the various methods of psychotherapy that have proven to be efficacious for BPD in RCTs 17 , 205 . For family members of BPD patients who suffer from considerable burden, helpful psychoeducational methods have been developed 206 .
Dialectical behavior therapy ( DBT )
DBT 189 , 207 , 208 is a structured outpatient psychotherapy based on cognitive‐behavioral principles. This therapy is “dialectical” in the sense that both acceptance and change are regarded as necessary for improvement. It consists of four components: individual therapy, group skills training, telephone coaching, and team consultations of therapists.
Individual therapy is conducted by the patient's primary therapist. It focuses on six main areas. Parasuicidal behavior is explored in detail, and problem‐solving behaviors – including short‐term distress management techniques – are emphasized. Therapy‐interfering behaviors are addressed (e.g., non‐adherence, breaking agreements), as well as behaviors with impact on the quality of life (e.g., substance abuse, high‐risk sexual, interpersonal, legal, financial or health‐related behavior). Acquired behavioral skills are discussed and applied to patient's daily life. Trauma history is addressed when the patient is ready, including remembering the abuse, validation of memories, acknowledging emotions related to abuse, reducing self‐blame and stigmatization, addressing denial and intrusive thoughts regarding abuse (e.g., by exposure techniques), and reducing polarization or supporting a dialectical view of the self and the abuser 208 . The therapist consistently reinforces the patient's self‐respect behaviors.
Group skills training focuses on deficits in behavioral skills, including the unstable sense of self, unstable interpersonal relationships, fear of abandonment, impulsivity and emotional lability. Training includes four modules: core mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance. Group meetings take place weekly for two hours. The four modules are worked through in about six months. Modules may be repeated, and the skills training group is recommended for at least one year. Patients are assigned homework to reinforce skills. Diary cards are used to document the use of skills and are discussed with the individual therapist.
Core mindfulness skills have been adopted from Eastern meditation practice. To target BPD patients' impulsivity and emotion‐driven behavior, they are taught to observe and participate fully in the present moment. To target their tendency to idealize and devaluate both themselves and others, they are taught to focus on one thing at a time with a non‐judgmental mindset. Doing so also prevents patients from ruminating about past and worrying about future events.
Interpersonal effectiveness skills training teaches patients to ask for what they need, to say “no”, and to deal with interpersonal conflicts. Emotion regulation skills include identifying and labelling emotions; identifying obstacles to change of emotions, including parasuicidal behaviors; learning to avoid vulnerable situations; increasing events which lead to positive emotions; learning to tolerate painful emotions. Distress tolerance skills include techniques for self‐soothing or distracting, as well as for transforming intolerable pain into tolerable suffering.
Telephone coaching can be used in times of crises between regular sessions. Patients can learn how to ask for help in an adequate, non‐abusive manner. Reinforcement for parasuicidal behaviors is minimized by making an agreement that the patient is expected to call the therapist before enacting a parasuicidal behavior, and is not allowed to call the therapist for 24 hours after a parasuicidal behavior act, unless there are life‐threatening injuries.
Weekly team consultations of therapists form an integral part of treatment, aiming to monitor treatment fidelity, enhance therapeutic skills, and maintain therapists’ motivation in working with this particular group of patients. Team consultation may promote empathy and acceptance of the patient.
Mentalization‐based therapy ( MBT )
MBT 209 is a structured treatment that combines individual and group psychotherapy. It focuses on addressing suicidality and self‐harm, emotional processing, and relational instability in BPD patients, through a consistent focus on improving their capacity for mentalizing and social learning.
BPD is characterized by imbalances in mentalizing, as expressed in high levels of automatic, affect‐driven and externally‐based mentalizing, and frequent loss of the capacity for balanced mentalizing, particularly within close interpersonal relationships. This is associated with a dominance of experiencing the self and others in non‐mentalizing modes, such as: a) the psychic equivalence mode (equating thoughts and feelings with reality), b) the teleological mode (only recognizing observable reality as a determinant of mental states), and c) the pretend mode (characterized by excessive mentalizing severed from reality).
These unmentalized or “alien‐self” experiences are assumed to give rise to very intense and often unbearable feelings (e.g., high levels of anger, sadness or rejection), and as a result there is a tendency to externalize these unmentalized feelings through acting‐out behaviors (e.g., self‐harm, substance abuse), in an attempt to regulate them.
MBT also focuses on improving the capacity for epistemic trust, i.e., the capacity to trust knowledge conveyed by others and to use this knowledge for salutogenetic purposes (i.e., to be able to benefit from positive resources in the social environment).
The therapeutic stance of the MBT therapist is guided by the following basic principles: a) management of anxiety and arousal is central in MBT, as high levels of arousal easily lead to a loss of mentalizing, whereas low levels typically result in pretend mode functioning (excessive mentalizing severed from reality); b) interventions are aimed at restoring more balanced mentalizing, as patients with BPD easily resort to automatic, highly affect‐driven and externally‐based mentalizing, with little ability for more balanced, controlled mentalizing that integrates cognition and affect, and externally‐based and internally‐based social information; c) the patient and the therapist are equal, conversational partners attempting to reconstruct and better understand what is happening in the patient's interpersonal relationships, and how interpersonal issues are associated with the patient's presenting problems; d) a focus on the recovery of mentalizing implies that the therapist is primarily concerned with the “how” of mental processes, rather than the “what” and “why”; e) contingent and marked responses of empathic emotional validation are another key feature of MBT, aiming to restore a sense of agency and understanding in the patient.
MBT uses a spectrum of interventions, which include: supportive interventions (empathic and normalizing interventions that primarily serve to regulate anxiety and arousal, and foster epistemic trust by restoring a sense of agency through experiences of marked mirroring); interventions aimed at clarification and elaboration of subjective experiences; interventions aimed at restoring basic mentalizing (e.g., stop‐and‐rewind, stop‐stand‐and‐explore, stop‐stand‐and‐challenge); interventions aimed at mentalizing the therapeutic relationship; interventions aimed at translating and generalizing knowledge acquired within the therapeutic process to interpersonal relationships outside of the therapeutic context. Two types of MBT for BPD have been developed and empirically supported: intensive outpatient MBT and day‐hospitalization‐based MBT for adults 210 .
MBT includes an initial phase, a treatment phase, and a final or ending phase, each with their specific goals and strategies that are directly rooted in the evolving understanding of the condition.
The initial phase involves: psychoeducation provided through an MBT introductory group course; case formulation developed collaboratively with the patient; a focus on developing a treatment alliance based on an understanding of the patient's attachment history; safety planning; formulation of a mentalizing profile, i.e., the identification of specific imbalances in mentalizing, including triggers of mentalizing problems.
The treatment phase comprises general and specific strategies. General strategies include: stabilization of risky behaviors; supportive, empathic validation to regulate anxiety/arousal and to enable the (re)activation of mentalizing; the use of elaboration and clarification to foster basic mentalizing, particularly of highly affective states; a strong focus on interpersonal relationships and events to enable an exploration of alternative perspectives (i.e., relational mentalizing); a focus on repairing alliance ruptures. Specific strategies include: management of impulsivity by mentalizing events that trigger impulsive behavior; activation of the attachment system in both group and individual therapy, allowing for the development of basic mentalizing; linking experiences in therapy to daily life, with a focus on social exclusion/inclusion and rejection; increasing mentalizing capacity when under stress; recovering mentalizing capacity when a loss of mentalizing occurs; mentalizing traumatic experiences when indicated.
The final phase focuses primarily on the following issues: review of the therapy with a focus on the experience of ending for both patient and therapist; a focus on issues associated with ending that trigger BPD‐specific concerns (e.g., fears of abandonment or rejection); generalization of stable mentalizing and learned social understanding; considering how to continue the therapeutic process after ending.
Transference‐focused psychotherapy ( TFP )
TFP represents a specific extension of psychoanalytic therapy for treatment of individuals with personality disorders 187 , 211 . Within the framework of psychoanalytic object relations theory, unconscious conflicts activated in the transference are seen as expressions of conflictual, affectively invested internalized object relations. Unconscious conflicts are represented as dyadic units composed of a representation of the self interacting with a representation of a significant other, framed by a particular affect state. These dyadic structures come to be enacted, or lived, by the patient in his/her interactions with the therapist.
In TFP, the therapist's focus is on exploration and interpretation of patient's behaviors in the treatment that reflect the activation of specific transferences, associated internalized object relations, and the conflicts they imply. The activation of dominant internalized object relations is interpreted both in their defensive function, that is, as a protection against the opposite relationships that they attempt to avoid, and in their “impulsive” or expressive function, as a reflection of deeper primitive, affectively motivated behaviors pushing for actualization.
Within the setting of a borderline structure, unconscious conflict takes the form of a fundamental conflict, or split, between positively charged, idealized sectors of experience and negatively charged, paranoid sectors. Each internalized object relation can, at different moments, serve impulsive or defensive functions. These idealized and persecutory internalized object relations are activated and then enacted in the transference.
The main psychoanalytic techniques employed in TFP are interpretation, transference analysis, technical neutrality, and countertransference utilization. Affective dominance refers to material that, in the perception of the therapist, is most strongly present and affectively salient in the patient's verbal and, in particular, nonverbal communications at any moment of the session 211 . Affective dominance signifies the major area of conflict currently active in the therapy session, and thus, the material that becomes the most suitable and productive focus of the therapeutic intervention.
Interpretation is the establishment of hypotheses involving unconscious conflicts. They derive from the combined analysis of the content of the patient's communications, his/her nonverbal behavior, and the dominant countertransference. Interpretations focus predominantly, but not exclusively, on the transference. Affect dominance determines the focus of interpretation.
Transference analysis represents the main therapeutic instrument. It refers to the analysis of unconscious conflicts activated in the dyadic relations between patient and therapist that replicate the conflictual internalized relation between self and others (“objects”) from the past, modified by present context.
Technical neutrality is the observing attitude of the therapist, who keeps a concerned objectivity in his/her interpretive interventions, and maintains himself/herself outside the patient's activated internal conflicts.
Countertransference utilization refers to the therapist's ongoing observation of his/her emotional reactions to the patient, utilizing them to more sharply understand the emotional conflicts activated in the transference, and to interpret the transference in this light without direct communication to the patient of his/her own countertransference.
An early stage of TFP involves clarification of self and object representation of the activated internalized object relationship, their predominant affective implication, the distribution of self and object roles to patient and therapist, and their potential interchange. A more advanced stage involves the patient's emotional learning that he/she is, at a deeper level of unconscious experience, identified with both self and other in both idealized and persecutory internalized relationships, with decrease in the splitting of idealized and persecutory states of mind. In this advanced stage of treatment, the patient learns and tolerates the reasons for his/her splitting of polar opposite love‐ and hatred‐dominated relationships, and integrates the concepts of his/her self and the respective concepts of significant other. Normalization of personal identity is achieved, and a realistic capacity for relationships with significant others develops. Modulation of affect states, increased affect control, and increased capacity for non‐conflictual investment in work and profession, love and sex, and gratifying social relations may evolve.
Schema therapy ( ST )
ST 212 , 213 draws on cognitive‐behavioral, psychodynamic, attachment and emotion‐focused approaches. It addresses four dysfunctional life schemas characteristic of BPD: the abandoned/abused child; the angry/impulsive child; the detached protector; and the punitive parent. In addition, some presence of the healthy adult is assumed. The development of the healthy adult is one of the goals of ST, first embodied in the therapist and internalized by the patient during the therapeutic process.
The abandoned/abused child mode is characterized by feeling isolated, lost, unloved, and frantic, obsessive with finding a parental figure who will take care of him/her. This mode is regarded as a core state of being for the BPD patient. ST recommends the therapist to envision BPD patients as functioning as a young child.
In the angry/impulsive child mode, the patient expresses rage about mistreatment and unmet emotional needs. This mode is activated in situations of real or perceived abandonment, deprivation or mistreatment. Tragically, this mode makes it even less likely that the patient's needs are met. In addition, the punitive parent may be activated and punish the angry child. Outburst of rage may be followed by cutting or other forms of self‐punishment.
In the detached protector mode, the patient avoids investing emotionally in people or activities; he/she may feel numb or empty, withdraw socially, excessively fantasize or seek stimulation or distraction. This mode interferes with therapeutic progress.
The punitive parent mode represents the patient's identification with an abusive parental figure. By internalizing this figure, the inner abuse continues. In this mode, patients feel “evil” or “dirty” and may engage in parasuicidal behaviors. The therapist helps the patient to recognize this part of himself/herself, and gives it a descriptive name (e.g., “your punishing father”). Thus, the patient may achieve some distance from this part of himself/herself and may fight back.
Four processes are regarded as core mechanisms of change in ST: “limited reparenting”, emotion‐focused work, cognitive restructuring and education, and behavioral pattern breaking.
“Limited reparenting” is regarded as the most important change mechanism 235 . Therapists try to compensate for the deficits in parenting that patients with BPD experienced during their childhood, while maintaining professional boundaries. They act in a warm and sympathetic way, providing safety, stability and acceptance. They may disclose themselves if they believe it will be beneficial to patients. They provide the patients with their home phone number for use in crises, give extra session time, and have phone sessions and email exchange as needed. Patients who have problems related to separation and abandonment may be provided with check‐in calls, flashcards or other transitional objects.
ST uses emotion‐focused techniques, including imagery work, dialogues and letter writing. Patients are asked to bring up images and memories of difficult situations they experienced in the past. The therapist can enter into the childhood scenes, and protect and support the abandoned/abused child, functioning as the healthy adult. After the therapist has done so, the patient takes on the healthy adult role, by entering into the image and protecting the child mode. Traumatic memories are worked through more slowly and only with the patient's permission. ST uses dialogues between the therapist and the patient to nurture the abandoned child, to protect the misused child, and to fight the punitive parent. These dialogues can be done in imagery or through Gestalt chair work. The latter helps to locate the punitive voices outside the patient. By role‐playing, the therapist helps the patient to strengthen his/her healthy adult mode. As a third technique, therapists encourage the patients to write a letter to those who have mistreated them in which they express their feelings and needs. The letters are not intended to be sent.
Cognitive techniques used in ST include education and cognitive restructuring. Patients are taught about normal needs and emotions. Thus, the therapist validates the patient's rights to have these needs met, while also teaching the patient to negotiate the desires in a reciprocal way, respecting others. This applies to emotions and specifically to anger. However, patients are taught to adequately express their emotions, not using a “black‐and‐white” thinking. In addition, patients are taught not to blaming themselves for setbacks during therapy.
Finally, the patients are guided to generalize to the life outside what they have learnt during sessions. For this purpose, traditional behavioral techniques may be used, such as relaxation training, assertiveness training, anger management, self‐control strategies, or graduate exposure. Flashcards or dialogues may also be used. Therapists and patients identify the most serious behaviors as targets for change. In vivo exercises may be used to disconfirm distorted expectations, for example of others acting as punitive parents. In sessions, role‐playing and behavioral rehearsals can be used.
ST includes three phases: bonding and emotional regulation, schema mode change, and development of autonomy.
The bonding and emotional regulation phase aims at establishing a relationship with the therapist which is an antidote to the abusive or punitive one that the patient experienced as a child. Thus, a “holding environment” 214 , a safe place for the patient, is developed. After that, childhood and adolescent experiences are explored. During these explorations, the patient is kept in the abandoned/abused child mode, in order to allow him/her to make a new relational experience. The patient begins to internalize the experience with the therapist as a healthy parent. Anger may be expressed, but in a controlled way, in order to avoid that it becomes counterproductive. All the patient's needs and longings that have been unmet are activated, allowing the therapist to engage in a limited reparenting behavior.
While working on changing schema modes, the therapist maintains a relationship with the abandoned/abused child. The therapist praises the patient and calls him/her “generous, loving, intelligent, sensitive, creative, empathic, passionate, or loyal” 215, p.335 , reparenting the patient. The punitive parent mode may be triggered, and the patient may reject these affirmations.
If the patient is flooded with anxiety and painful emotions, the detached protector mode could be triggered. This is a survival mechanism developed by the patient, but can interfere with the therapeutic process. When it emerges in the therapeutic process, this mode is identified, and its benefits and costs are discussed. The situation can be addressed by adjusting the intensity and frequency of affective work carefully. Furthermore, the use of medication can be considered to reduce the intensity of affects.
In the final stage of treatment, the therapist shifts the attention from reparenting within the therapeutic relationship to developing independence outside sessions. The focus is on interpersonal relationships and on the sense of identity. Relationships are explored to see how the various modes are interacting. With regard to developing a sense of identity, the therapist and the patient work together to explore what resonates with the patient.
Efficacy of psychotherapy in BPD
A meta‐analysis aggregating the effect sizes achieved by psychotherapy in comparison to treatment‐as‐usual (TAU) in BPD yielded an overall SMD of –0.52 (95% CI: –0.70 to –0.33, n=22, N=1,244), which corresponds to a clinically relevant reduction in symptom severity 17 (see Table 5 ). Thus, psychotherapy of BPD is among the few treatments for common mental disorders achieving medium or large effect sizes in comparison to TAU 217 . For self‐harm (SMD=−0.32, 95% CI: −0.49 to −0.14, n=13, N=616), suicide‐related outcomes (SMD=−0.34, 95% CI: −0.57 to −0.11, n=13, N=666) and psychosocial functioning (SMD=−0.45, 95% CI: −0.68 to −0.22, n=22, N=1,314), psychotherapy was significantly superior to TAU as well, but with low‐quality evidence and effect sizes below clinical relevance 17 . There is no evidence that psychotherapy is associated with a higher rate of serious adverse events compared with TAU (risk ratio, RR=0.86, 95% CI: 0.14‐5.09; n=4, N=571, p=0.86) 17 . Generic methods of psychotherapy (e.g., general psychiatric management, structured clinical management, client‐centered therapy, supervised team management) were found to be inferior to specialized psychotherapies such as DBT, MBT or schema therapy 216 .
Meta‐analytic evidence for efficacy of psychotherapies vs. treatment as usual (TAU) for borderline personality disorder (BPD)
Major forms of psychotherapy include dialectical behavior therapy, psychodynamic therapies, cognitive‐behavior therapy, schema therapy, and acceptance and commitment therapy. Psychodynamic therapies include mentalization‐based therapy, transference‐focused therapy, and dynamic deconstructive therapy. SMD – standardized mean difference.
For the main types of evidence‐based psychotherapy, the effect sizes achieved in comparison with TAU in BPD patients do not differ significantly 17 . This applies to symptom severity (X 2 =6.88, df=4, p=0.14, I 2 =41.8%) and psychosocial functioning (X 2 =0.67, df=3, p=0.88, I 2 =0%). The most recent network meta‐analysis confirmed the lack of significant differences between specialized psychotherapies in reducing BPD symptom severity, with only two exceptions: ST was superior to DBT (SMD=0.72, 95% CI: 0.03‐1.41) and cognitive‐behavior therapy (CBT) (SMD=0.90, 95% CI: 0.12‐1.69) 216 . However, these results should be interpreted with caution, as some of these differences were based on only a few trials 216 . Between DBT, TFP and MBT, no statistically significant differences were found in reducing BPD symptom severity, with small between‐group effect sizes 216 . For suicidal behavior, no differences in efficacy were found between specialized psychotherapies 216 .
With regard to individual types of psychotherapy, most studies are available for DBT 17 . DBT achieved a medium clinically significant effect size compared to TAU for BPD severity (SMD= −0.60, 95% CI: −1.05 to −0.14, n=3, N=149, I 2 =42%). It achieved small and clinically not significant effect sizes for self‐harm (SMD=−0.28, 95% CI: −0.48 to −0.07, n=7, N=376, I 2 =0%) and psychosocial functioning (SMD=−0.36, 95% CI: −0‐69 to −0.03, n=6, N=225, I 2 =31%) 17 . In these studies, DBT had a duration of 2.5 to 12 months 17 . A recent RCT found DBT of 6‐month duration to be non‐inferior to 12‐month DBT with regard to self‐harm (primary outcome), as well as for general psychopathology and coping skills, at 24‐month follow‐up 218 . There were no differences in dropout rates between treatments. A briefer form of DBT may reduce barriers to treatment access.
For psychodynamic therapies in BPD, ten RCTs presently exist (five for MBT 25 , 219 , 220 , 221 , 222 , three for TFP 200 , 223 , 224 , and four for other methods, such as dynamic deconstructive therapy 201 , 225 , 226 , 227 ). In these RCTs, psychodynamic therapy was compared to TAU or to other active treatments. It had a duration of 5‐24 months, except for one study, in which it had a 3‐year duration 224 . A meta‐analysis comparing psychodynamic therapies with TAU found medium effect sizes in favor of the former for core BPD symptoms (g=−0.65, 95% CI: −0.99 to −0.32, n=4, N=213, I 2 =15.4%), suicide‐related outcomes (g=−0.67, 95% CI: −1.13 to −0.20, n=5, N=354, I 2 =40.1%) and psychosocial functioning (g=−0.57, 95% CI: −1.04 to −0.10, n=5, N=392, I 2 =60.1%), with low or moderate heterogeneity 228 . Effect sizes were clinically significant, except for functioning. This meta‐analysis did not find significant differences in efficacy between psychodynamic therapies and other active psychotherapies, including DBT and ST (g=0.05, 95% CI: −0.52 to 0.62, n=4, N=394, I 2 =64%). Excluding one outlier 224 reduced heterogeneity (g=−0.08, 95% CI: −0.55 to 0.39, n=3, N=308, I 2 =19%).
Due to the limited number of RCTs, meta‐analyses specifically focusing on between‐group effect sizes with ST are not available 229 . The most recent meta‐analysis on psychotherapy for BPD included only three RCTs of ST 216 . As noted above, in reducing BPD symptoms, ST was found to be superior to DBT and CBT, but not MBT or TFP 216 . However, these results should be interpreted with caution, due to the limited number of RCTs on which they were based. With regard to individual studies, a large RCT (N=495) found combined individual and group ST to be superior to both TAU (d=1.14, 95% CI: 0.57‐1.71, p<0.001) and predominantly group ST (d=0.84, 95% CI: 0.09‐1.59, p=0.03) in reducing severity of BPD symptoms, with large effect sizes 230 . Predominantly group ST was not superior to TAU (d=0.30, 95% CI: −0.29 to 0.89, p=0.32) 230 . Both treatments were delivered over a period of two years, with combined individual and group ST encompassing 124 sessions and predominantly group ST 122‐135 sessions. Another RCT found ST to be superior to TFP 224 . These results, however, have been critically discussed with regard to the question whether TFP was adequately implemented 231 , 232 . In a pilot study, brief ST (20 sessions) was not found to be superior to TAU 233 .
Research on psychotherapy for BPD has several limitations. The number of studies is still relatively limited, and the quality of evidence is moderate 17 . In many studies, risk of bias was high 17 , 205 , possibly inflating effect sizes 205 . Dropout rates are high 234 and differ considerably between studies 235 . Furthermore, treatment effects are found to be unstable at follow‐ups 17 , 205 . Regarding publication bias affecting outcomes, results are heterogeneous 17 , 205 . Moreover, rates of non‐response vary considerably between studies and treatments, which may also in part be due to different definitions of response used 23 . For psychotherapy alone, non‐response was on average 48.8% 23 when the definition of response required either no longer meeting criteria for BPD or change of BPD symptomatology below a cut‐off (e.g., 50% or 25% reduction) 23 . The mean rate of non‐response was similar for DBT (47%), ST (42%) and psychodynamic therapies (42%) 23 . For TAU, it was 64% 23 . Thus, the proportion of non‐responders is considerable, and psychotherapy needs to be further improved.
There is limited evidence that psychotherapy for BPD is also effective under real‐world conditions. For instance, more than a dozen of naturalistic studies have found that MBT is associated with clinically significant improvements in BPD symptoms, general psychiatric symptoms, suicidality and self‐harm 236 . For TFP, a naturalistic study reported a remission rate of 58% as well as improvements in BPD symptom severity and functioning (N=19) 237 . An inpatient treatment which combined TFP with modules of DBT skills training was reported to achieve significant improvements in identity diffusion and symptoms (N=32) 238 . In another naturalistic study, both DBT (N=25) and dynamic deconstructive psychotherapy (N=27) achieved significant reductions in symptoms of BPD, depression, and disability by 12 months of treatment 239 . This was not true for a non‐randomized TAU condition (N=16). A naturalistic study found no differences in outcomes between MBT and DBT after 12 months of treatment 240 .
Psychotherapy in adolescents
A recent Cochrane review concluded that adolescent patients with BPD do benefit from psychotherapy, but to a lesser extent than adult patients 17 . Disorder‐specific treatments such as DBT, TFP and MBT have been adapted for adolescents. Studies often include young patients with subthreshold BPD pathology, and use naturalistic or even hybrid study designs with randomized assignment in a naturalistic setting. In these studies, high attrition rates are quite common.
Some reasonably robust studies on psychotherapeutic interventions for adolescents with BPD are, however, available. A quasi‐experimental investigation compared DBT (N=29) with TAU (N=82) among suicidal outpatient adolescents who also met DSM‐IV criteria for BPD 241 . The DBT group had significantly fewer hospital admissions, but no differences were found in suicide attempts. In a Norwegian randomized control trial of 77 adolescents with recent and repetitive self‐harm, DBT (N=39) was compared to enhanced usual care (EUC) (N=38) 242 . Participants met at least two DSM‐IV criteria for BPD plus the self‐destructive criterion, or at least one DSM‐IV BPD criterion plus at least two below‐threshold criteria. The authors found DBT to be superior to EUC. The former remained superior in reducing self‐harm, but not for other outcomes (including BPD symptoms), over a follow‐up period of 52 weeks 243 . For DBT, a recent meta‐analysis including five RCTs and three controlled clinical trials reported a medium effect size compared to control groups (g=–0.44, 95% CI: –0.81 to –0.07, n=7, I 2 =80%) in reducing self‐harm, and a small effect size (g=–0.31, 95% CI: –0.52 to –0.09, n=6, I 2 =44%) in reducing suicidal ideation 244 .
The adolescent identity treatment (AIT) 245 integrates behavioral elements with TFP. In a naturalistic study, 60 adolescents diagnosed with BPD or subthreshold BPD pathology received either DBT or AIT 246 . Both treatments significantly improved BPD symptoms, depression, and psychosocial and personality functioning. Overall, AIT was found to be not inferior to DBT and even more effective in reducing BPD symptoms.
TFP was evaluated in a naturalistic day‐clinic setting 247 . One hundred twenty adolescents with personality pathologies (BPD as a majority) received either TFP or TAU. Contrary to the TAU group, patients treated with TFP showed a significant reduction in self‐harm.
MBT was compared with TAU in 80 adolescents exhibiting self‐harm behavior and comorbid depression, of whom 73% met the criteria for BPD. MBT was more effective than TAU in reducing self‐harm and depression 248 . A reduction in BPD traits after the end of MBT was also reported.
The efficacy of the psychoanalytic‐interactional method (PiM) was examined in an inpatient setting 249 . This RCT included 66 adolescents with the primary diagnosis of a mixed disorder of social behavior and emotions (F92 according to the ICD‐10) compared with a mixed control group (waiting list and TAU). The ICD‐10 F92 diagnosis was used as an indicator of BPD features. The sample comprised severely impaired patients with high rates of comorbidity. Patients in the treatment group had a significantly higher rate of remission (OR=26.41, p<0.001) and a significantly greater improvement in behavioral problems and strengths. At six‐month follow‐up, treatment effects were stable. A subsequent analysis assessed 28 adolescents fulfilling DSM‐IV diagnostic criteria for BPD who had started inpatient treatment 250 . At the end of treatment, 39.3% of these patients no longer met the diagnostic criteria and were therefore classified as remitted.
However, a recent systematic review and meta‐analysis of psychotherapy for adolescents with BPD or BPD features 251 , including ten RCTs with a high risk of bias and very low quality, found that only a few trials demonstrated superiority of the intervention over the control condition. Thus, the authors stated that it is difficult to derive conclusions about the efficacy of psychotherapy in BPD adolescents, and that further high‐quality studies with larger samples are required.
CONTROVERSIES
Diagnostic issues.
A first debated issue is whether BPD should be regarded as a separate disorder (“there has been a notable absence of sound scientific evidence that it is a unified syndrome” 19, p.394 ). In fact, the BPD criteria were found to show a high loading only on a general personality pathology factor, whereas other personality disorders showed loadings either on both the general and a specific factor or largely only on a specific factor 62 .
Furthermore, BPD has been critiqued for missing stability in studies with long‐term follow‐ups, with some typical symptoms of BPD being associated with a higher stability than others 252 , 253 , 254 . However, the percentage of BPD patients who retain their personality disorder diagnosis in a 2‐year follow‐up (44%) is not substantially different from that of patients with obsessive‐compulsive (40%), schizotypal (39%) and avoidant (50%) personality disorder 252 . Furthermore, the decrease in proportion of criteria met across time does not differ significantly between the various personality disorders 252 .
Some authors have argued that the high overlap with the general factor of personality pathology, and the intrinsic experience of self and interpersonal dysfunction, suggest that the BPD criteria reflect general impairments in personality functioning rather than a distinct personality disorder 60 , 62 . This notion is consistent with Kernberg's concept of borderline personality organization 3 , 255 , and is compatible with the DSM‐5 and ICD‐11 dimensional model of personality disorders 35 , 60 .
Another critical issue is the number of criteria that have to be fulfilled in order to be able to assign a diagnosis of BPD. A patient with intense feelings of emptiness, highly unstable interpersonal relationships, severe identity disturbance, and self‐harm, for example, may not fulfill the diagnostic criteria due to missing a fifth criterion, despite severe impairment in functioning. Furthermore, with five of nine criteria required for the diagnosis, there are 256 possible ways to meet the DSM‐5 criteria of BPD 39 , suggesting considerable heterogeneity among BPD patients. This heterogeneity represents a challenge for research on etiology and treatment 38 .
Another critical argument refers to the fact that clinical features typical of BPD are well represented within the ICD‐11 system, with its two‐step approach of firstly assigning a core personality disorder diagnosis (mild, moderate, severe) based – among others – on self and interpersonal functioning, and secondly the specification via trait dimensions, most notably negative affectivity (e.g., emotional lability, anxiety), disinhibition (e.g., reckless behavior, impulsivity), and dissociality (e.g., hostility, aggression) 21 , 35 . On the other hand, proponents of a categorical model emphasize that BPD is a clinically useful diagnosis and one of the best researched ones, especially with regard to the development and testing of psychotherapeutic interventions 254 . Moreover, it is argued that some of the most important concepts related to our understanding of mental disorders and psychopathology – such as mentalization and its neurobiology, trauma, and relationship dynamics – have been stimulated by research on BPD 256 , 257 , 258 .
The final decision to include a “borderline specifier” in the ICD‐11 was preceded by intense discussion and controversy 19 . This decision has been seen as a political and practical compromise in order to strengthen the acceptance of the new system 19 , 21 . Considering that there is a lot of ongoing research and funding related to BPD, and that several academic careers have been built upon its research and treatment, abolishing it has been likely seen as too far‐reaching. Additionally, the new system, including both options, will likely lead to interesting research options (e.g., studying milder forms of personality disorder in combination with typical borderline domains, or comparing the old versus the new model) 21 .
Treatment issues
Some meta‐analyses suggest limited differences in efficacy between specialized and non‐specialized treatments for BPD, particularly at long‐term follow‐up and when controlling for publication bias 205 . This has led some authors and guidelines to conclude that non‐specialist treatments may be as effective as specialist ones 199 . Of course, non‐specialist treatments may have the advantage of being more cost‐effective and thus the potential to greatly increase access to effective psychotherapy for patients with BPD. Yet, as noted, several meta‐analyses have instead found clinically significant differences in efficacy between specialist and non‐specialist treatments for BPD 17 , 216 . Moreover, non‐specialist treatments evaluated in clinical trials are typically manualized, with clinicians being trained and supervised in the approach, and thus may often not be truly “non‐specialized” treatments.
Because of their problems with self‐coherence and trust in others, patients with BPD might be particularly sensitive and responsive to treatments that offer coherence, consistency and continuity 24 . This assumption is also borne out by studies suggesting that the effect sizes of specialist treatments for BPD considerably decrease when offered under suboptimal conditions 259 . Moreover, some studies suggest that specialist treatments may be particularly more effective compared to non‐specialist ones in more complex patients 260 , 261 . Finally, the effectiveness of “non‐specialist” treatments evaluated in RCTs has dramatically increased over time, suggesting that they have increasingly incorporated effective principles of “specialist” treatments or, at the very least, have discontinued the use of iatrogenic practices such as unfocused exploratory and supportive interventions 24 .
Although more research concerning the (cost‐)effectiveness of specialist and non‐specialist treatments, and their implementation in routine clinical care, is needed to investigate the above assumptions, the good news is that there is growing convergence among different treatment approaches as regards effective practices in patients with BPD.
CONCLUSIONS
BPD is a common mental disorder, associated with considerable functional impairment, intensive treatment utilization, and high societal costs. The construct of BPD is internally consistent and more homogeneous than often assumed 262 . However, it is still controversial whether BPD is better represented by a categorical or dimensional approach 19 . Future research is required to clarify this issue. This is also true for the elucidation of the risk factors, the neurobiological underpinnings, and the role of social cognition and neurocognition in the disorder.
With regard to treatment of BPD, pharmacotherapy is presently only recommended for severe and discrete comorbid mental disorders and for the short‐term treatment of crises. Psychotherapy has proven to be efficacious in BPD 17 and is recommended as first‐line treatment 22 . With regard to the different types of psychotherapy, there is presently no reliable evidence that one method is superior to others 17 , 216 . Some differences in efficacy that were recently reported are based on a few trials 216 . As a limitation, rates of non‐response and relapse are relatively large 23 . Thus, psychotherapy needs to be further improved.
Future studies of psychotherapy in BPD are recommended to focus on patients at risk of non‐response and on improving long‐term effects, as well as on reducing self‐harm behavior and suicidal ideation 263 . Taking the high dropout rate into account 234 , an‐other focus should be on patients prematurely terminating treatments. By studying dropouts, researchers can learn which aspects of a treatment are experienced by patients as not beneficial or even harmful, and in which way treatments may be improved. Thus, patients who drop out of a treatment can provide important information 264 .
As another limitation, the quality of psychotherapy studies was found to be modest 17 , 216 . Further high‐quality studies are required, in both adults and adolescents. Taking the shift from categorical to dimensional concepts into account 20 , research on psychotherapy of BPD (and of personality disorders in general) needs to take dimensional outcome measures (e.g., Level of Personality Functioning Scale 27 ), as well as personality traits, into account. Treatment research on dimensionally defined (severe) personality disorders is required 265 .
In addition, high‐quality head‐to‐head comparisons of the major forms of psychotherapy with a sufficient statistical power, adequate treatment implementation, and control of bias and researcher allegiance are needed. Such trials may also examine presumed mechanisms of change. For these head‐to‐head comparisons, proponents of each approach need to be included on an equal basis (adversarial collaboration) 266 . Funding organizations are encouraged to support these comparative trials, since large samples may be required to detect small but clinically significant differences, implying considerable study costs. As the differences in efficacy between the major psychotherapeutic approaches do not seem to be substantial at the group level 17 , 216 , identifying what works for whom seems to be a promising strategy. Individual participant data meta‐analysis may be helpful in this regard 216 .
ACKNOWLEDGEMENT
The authors are grateful to J.R. Keefe for providing the data for BPD only from Barber et al's meta‐analysis.

IMAGES
VIDEO
COMMENTS
Overall, the position papers on psychological perspectives converge on several strengths of the European research field: i.e. a substantial body of expertise and knowledge in both basic and clinical research, strong and increasingly more intimate collaborative ties to the biomedical field, and a broader coverage of mental health issues as ...
When it comes to the severity of the disorder, it appears that meta-emotions ("emotions that occur in response to other emotions (e.g., guilt about anger)" ) have a role to play in depression . A determinant that has received much attention in mental health research concerns rumination.
Table 3. DSM-5 definition of mental disorder. A mental disorder is a syndrome characterized by clinically significant disturbance in an individual's cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or development processes underlying mental functioning.
The findings revealed a 19% concurrent comorbidity between these disorders, and in 65% of the cases, social phobia preceded major depressive disorder by at least 2 years. In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety ...
In this essay, we have briefly reviewed a selected range of key discoveries that neuroscientific research has made on the topic of depressive disorders in the last decades. ... Garvey M, et al. (2010) Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry 167(7 ...
This issue of the Journal also presents original research articles that address topics related to the treatment of bipolar disorder, the use of a new transcranial magnetic stimulation (TMS) strategy for treatment of refractory depression, and the effects of gender-affirming interventions on the treatment of mood and anxiety disorders in ...
This article discusses the approaches to describing and classifying mental disorders taken by three key organizations: the World Health Organization (WHO), 2 which is in the process of developing the 11th revision of the International Classification of Diseases (ICD), scheduled to be released for use by WHO member states in 2018; the American Psychiatric Association (APA), which published the ...
Background Despite effective treatments for personality disorders being developed, consumers and carers often report negative experiences of mental health services, including challenges accessing these treatments. Methods This qualitative study used separate focus groups to compare the unique perspectives of consumer and carers, and to investigate how to improve services for individuals with ...
In each issue of Personality Disorders: Theory, Research, and Treatment one accepted manuscript will be selected to serve as an "Editor's Choice" paper. Selection will follow discussion by the editor and associate editor and consider issues such as overall contribution, clinical implications, or the highlighting of important theoretical ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on PSYCHOLOGICAL DISORDERS. Find methods information, sources, references or conduct a literature review ...
We review the interdisciplinary evidence of the bidirectional causal relationship between poverty and common mental illnesses—depression and anxiety—and the underlying mechanisms. Research shows that mental illness reduces employment and therefore income, and that psychological interventions generate economic gains.
In modern research and clinical practice, it will be crucial to define which phase one is facing in the psychotic disorder. Considering mental disorders as disorders with a significant overlap between the different diagnostic groups is, as previously mentioned, is called a dimensional perspective.
### What you need to know ### Sources and selection criteria We searched Pubmed, Medline, Embase, the Cochrane Library, CINAHL, PsycINFO, AMED, British Nursing Index, HMIC, and Health Business Elite using the term "personality disorder". Findings from randomised controlled trials (RCTs), systematic reviews, and meta-analyses were ranked as high in quality (see table 1) and we also used our ...
Unfortunately, the trend toward under treating mental disorders is not limited to the USA. A national survey of 16-64 year olds in Great Britain over a 7-year period (1993-2000) reported that only a quarter of people with a mental disorder were receiving some kind of treatment in 2007, unchanged from 2000 (Jenkins et al., 2009).
research findings concerning the etiology and treatment of psychological disorders are based on criteria set 554 Chapter 15 Psychological Disorders This content is available for free at https ...
Trauma, Resilience, Anxiety Disorders, and PTSD. Stress and trauma are well known to be critical factors in the development and maintenance of psychopathology. In some stress-related disorders, such as anxiety and depression, stress can play an etiological role, whereas in other disorders like schizophrenia, stress can precipitate and ...
Author Summary One of the major challenges of neuroscience research is to integrate the results of the large number of published research studies in order to better understand how psychological functions are mapped onto brain systems. In this research, we take advantage of a large database of neuroimaging studies, along with text mining methods, to extract information about the topics that are ...
Personality disorders are highly prevalent in clinical practice. With the introduction of the Diagnostic Statistical Manual - 5th Edition (DSM-5) the multi-axial system of diagnosis for mental disorders has disappeared, which has led to an increase in research on personality disorders (e.g. Emmelkamp & Meyerbröker, 2020).In this Special Issues, several recent developments are discussed.
Mental disorders are a major contributor to the global burden of disease. It commonly results in a higher incidence of physical decline 1,2,3,4 and early death compared with normal age-related ...
Otto Rank (Reference Rank 1911) wrote the first psychoanalytic paper focusing on narcissism, and this was followed by the publication of Freud's now classic text On Narcissism ... The growth and development of research on personality disorders: A bibliometric study. Personality and Mental Health, Vol. 16, Issue. 4, p. 290. CrossRef; Google Scholar;
Hazard ratios with 95% CIs for the associations between having 1 or more than 1 ninth-grade classmate with any of the examined mental disorder diagnoses (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, codes F10-F50 or F90-F98) and later risk of being diagnosed with a mental disorder in 4 follow-up time windows.
A total of 7908 mental disorder cases reported in the medical college hospital, 5564 (70.36%) were males and 2344 (29.64%) were females. Most cases occurred in the age group of 30-44 years. Mental disorder was more among females than males in 0-29 years and ≥ 60 years, but in 30-59 years males were more. In each year, mental disorders were ...
Recently published articles from subdisciplines of psychology covered by more than 90 APA Journals™ publications. For additional free resources (such as article summaries, podcasts, and more), please visit the Highlights in Psychological Research page. Browse and read free articles from APA Journals across the field of psychology, selected by ...
problems get classified as "mental disorders," and sometimes they don't. In addition, the reasons why people experience problems are highly complex. Indeed, psychological disorders are at least as complex as why people ex-perience or do anything else. It is important for students to understand the complexity of psychological disorders.
Personality disorders (PDs) can be described as the manifestation of extreme personality traits that interfere with everyday life and contribute to significant suffering, functional limitations, or both. They are common and are frequently encountered in virtually all forms of health care. PDs are associated with an inferior quality of life (QoL ...
Background: Recognizing the positive or negative effects of students' mental health promotes personal development, well-being, and academic success. Academic life exposes college students to multiple adjustments, demands, and vulnerabilities that can cause stress and mental health problems. This study aims to identify psychological well-being and psychological distress effects on college ...
Shapiro Administration Highlights Mental Health and Substance Use Disorder Resources for Older Pennsylvanians, Governor's Proposed Investments in Behavioral Health Funding. Contact DHS. County Assistance Offices (CAOs) Child Support Contact Information. Helpful Telephone Numbers
The term "borderline" was introduced in the psychiatric literature by Stern 1 and Knight 2, to identify a patient group showing a level of functioning situated between neuroses and schizophrenic disorders.This patient group was not well defined. An important progress occurred with Kernberg's introduction of the concept of borderline personality organization 3, 4, marked by the use of ...