An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection


Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals
Matthew d mchugh.
a School of Nursing, Center for Health Outcomes and Policy Research, University of Pennsylvania, Philadelphia, PA, USA
Linda H Aiken
Douglas m sloane, carol windsor.
b School of Nursing, Queensland University of Technology, Kelvin Grove, QLD, Australia
c Centre for Healthcare Transformation, Faculty of Health, Queensland University of Technology, Brisbane, QLD, Australia
Clint Douglas
d Metro North Hospital and Health Service, Royal Brisbane and Women's Hospital, Herston, QLD, Australia
Patsy Yates
Associated data.
The nurse survey data cannot be shared in any form as a condition of survey respondent consent. The patient data cannot be shared by the investigators under the data use agreement with Queensland Health; however, the original admitted patient data collection can be requested directly from Queensland Health.
Substantial evidence indicates that patient outcomes are more favourable in hospitals with better nurse staffing. One policy designed to achieve better staffing is minimum nurse-to-patient ratio mandates, but such policies have rarely been implemented or evaluated. In 2016, Queensland (Australia) implemented minimum nurse-to-patient ratios in selected hospitals. We aimed to assess the effects of this policy on staffing levels and patient outcomes and whether both were associated.
For this prospective panel study, we compared Queensland hospitals subject to the ratio policy (27 intervention hospitals) and those that discharged similar patients but were not subject to ratios (28 comparison hospitals) at two timepoints: before implementation of ratios (baseline) and 2 years after implementation (post-implementation). We used standardised Queensland Hospital Admitted Patient Data, linked with death records, to obtain data on patient characteristics and outcomes (30-day mortality, 7-day readmissions, and length of stay [LOS]) for medical-surgical patients and survey data from 17 010 medical-surgical nurses in the study hospitals before and after policy implementation. Survey data from nurses were used to measure nurse staffing and, after linking with standardised patient data, to estimate the differential change in outcomes between patients in intervention and comparison hospitals, and determine whether nurse staffing changes were related to it.
We included 231 902 patients (142 986 in intervention hospitals and 88 916 in comparison hospitals) assessed at baseline (2016) and 257 253 patients (160 167 in intervention hospitals and 97 086 in comparison hospitals) assessed in the post-implementation period (2018). After implementation, mortality rates were not significantly higher than at baseline in comparison hospitals (adjusted odds ratio [OR] 1·07, 95% CI 0·97–1·17, p=0·18), but were significantly lower than at baseline in intervention hospitals (0·89, 0·84–0·95, p=0·0003). From baseline to post-implementation, readmissions increased in comparison hospitals (1·06, 1·01–1·12, p=0·015), but not in intervention hospitals (1·00, 0·95–1·04, p=0·92). Although LOS decreased in both groups post-implementation, the reduction was more pronounced in intervention hospitals than in comparison hospitals (adjusted incident rate ratio [IRR] 0·95, 95% CI 0·92–0·99, p=0·010). Staffing changed in hospitals from baseline to post-implementation: of the 36 hospitals with reliable staffing measures, 30 (83%) had more than 4·5 patients per nurse at baseline, with the number decreasing to 21 (58%) post-implementation. The majority of change was at intervention hospitals, and staffing improvements by one patient per nurse produced reductions in mortality (OR 0·93, 95% CI 0·86–0·99, p=0·045), readmissions (0·93, 0·89–0·97, p<0·0001), and LOS (IRR 0·97, 0·94–0·99, p=0·035). In addition to producing better outcomes, the costs avoided due to fewer readmissions and shorter LOS were more than twice the cost of the additional nurse staffing.
Interpretation
Minimum nurse-to-patient ratio policies are a feasible approach to improve nurse staffing and patient outcomes with good return on investment.
Queensland Health, National Institutes of Health, National Institute of Nursing Research.
Introduction
The years 2020–21 have been designated by WHO as the International Year of the Nurse and Midwife to honour the 200th anniversary of Florence Nightingale's birth. 1 Nightingale, through meticulous records and application of innovative statistics, documented that more British soldiers in military hospitals during the Crimean War died because of unsafe hospital conditions than of wounds in battle. Her solution was the introduction of trained nurses, shown by her research to be associated with reduced hospital deaths. Nurses are still saving lives in modern hospitals, and research suggests that patient harm can be further reduced by investments in nurse staffing.
The Lancet published in 2014 a landmark study showing that patients' risk of dying after surgery varied by the number of patients for whom each nurse had responsibility. 2 Studying outcomes of nearly half a million patients in nine European countries, investigators found that each additional patient added to nurses' average workloads was associated with 7% higher odds of a patient dying within 30 days of admission. Evidence continues to grow that better hospital nurse staffing is associated with better patient outcomes, including fewer hospital acquired infections, shorter length of stay (LOS), fewer readmissions, higher patient satisfaction, and lower nurse burnout. 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 Yet, substantial within-country variation in hospital nurse staffing persists, giving rise to calls for public policy interventions to establish minimum safe staffing standards in hospitals. In 2018, the International Council of Nurses, representing national nursing associations worldwide, issued their Position Statement on Evidence-Based Nurse Staffing, concluding that plenty of evidence supports taking action now to improve hospital nurse staffing, echoing Nightingale's call to action over 150 years ago, that if we have evidence and fail to act, we are going backwards. 15
Research in context
Evidence before this study
We searched PubMed for original research articles published in English between Jan 1, 1985, and March 1, 2020, with the following search terms (separately and in combination): “nursing”, “staffing”, “nurse-to-patient ratios”, and “staffing mandate”. We also did a manual search based on bibliographies of relevant papers. In 2014, The Lancet published the largest international study on the subject, involving hundreds of thousands of patients in 300 hospitals across nine countries, showing that patients in hospitals with better nurse staffing levels were less likely to die in hospital than those being treated in poorly staffed hospitals. This study capped decades of research linking staffing levels to outcomes including mortality, readmissions, length of stay, adverse events, and patient satisfaction. Most research, however, has been cross-sectional; the few longitudinal studies have been done in single or a small number of hospitals. The small number of evaluations of implemented policy were retrospective and relied upon administrative staffing data known to overestimate staffing levels by including nurses who are not in patient care roles (eg, managers).
Added value of this study
Despite being frequently debated, policy tools to achieve safe nurse staffing levels have rarely been implemented—only a few jurisdictions have done so over the past 30 years. In the places that implemented such policies, no prospective evaluations linked with patient outcomes have been done. The absence of such an evaluation has been cited as a reason why similar policies have not been adopted elsewhere. In 2016, Queensland, Australia, implemented a policy establishing minimum nurse-to-patient ratios in medical-surgical wards in 27 public hospitals that care for 83% of patients hospitalised across the state. We report the findings of a first-of-its-kind prospective evaluation of Queensland's policy. In addition to evaluating the effect of the policy on mortality, we examined outcomes with cost implications (ie, readmissions and length of stay) relevant to financial considerations of health ministers and hospital administrators. The findings can directly inform debates in jurisdictions considering similar policies.
Implications of all the available evidence
These results support decades of research that suggested that making changes to improve staffing levels could result in better outcomes. Policy interventions establishing minimum nurse-to-patient ratios are feasible and yield significantly better outcomes for patients and a better return on investment to the public.
The first jurisdictions to implement minimum nurse-to-patient ratios policies were the states of Victoria, Australia, and California, USA, in the late 1990s. 16 , 17 The past 5 years have seen a resurgence of interest in establishing minimum nurse-to-patient ratio policies—Wales and Scotland (UK), Ireland, and Queensland (Australia) have implemented such policies 18 and multiple US states are considering them. 19 Queensland's legislation is noteworthy because an independent prospective evaluation was included. Here, we report the results of that evaluation.
On July 1, 2016, Queensland established minimum nurse-to-patient ratios (the term nurse includes registered and enrolled nurses [nurses with a technical diploma who work under the supervision of a registered nurse]) for adult medical-surgical wards in 27 public hospitals. The legislation required that average nurse-to-patient ratios on morning and afternoon shifts be no lower than 1:4 and on night shifts no lower than 1:7. We collected survey data at the hospital level from thousands of nurses to link with data on patients' clinical characteristics and outcomes from the period before and 2 years after implementation of ratios. Relative to comparison hospitals, we evaluated whether greater staffing improvements occurred at intervention hospitals, whether outcomes improved more at intervention hospitals, and whether the staffing improvements explained, at least partly, any advantage on patient outcomes.
Study design
This prospective panel study (RN4CAST-Australia) was quasi-experimental: we compared changes in measures of outcomes in a prospective panel of hospitals where assignment of the hospital to the treatment condition (the policy intervention) was non-random. We used nurse-reported data to measure medical-surgical nurse staffing levels and standardised patient data to measure outcomes at two timepoints: before implementation of ratios (baseline) and 2 years after implementation (post-implementation). We restricted our staffing measure to medical-surgical staffing and to nurses providing direct patient care. We compared two groups of hospitals: hospitals subject to the policy (intervention hospitals) and hospitals that discharged similar patients but were not subject to ratios (comparison hospitals). Intervention hospitals were chosen by the government to represent regions across the state. Therefore, our study accounted for pre-existing differences between intervention and comparison hospitals through statistical controls, including controls for hospital size and patient's characteristics. We aimed to answer three main questions: first, whether changes in nurse staffing levels were different between intervention and comparison hospitals; second, whether changes in patient outcomes were different between intervention and comparison hospitals; and third, whether the staffing changes were associated with differential patient outcomes after accounting for differences in patient and hospital characteristics.
Ethics approval was obtained from the Queensland University of Technology (Kelvin Grove, QLD, Australia) and the University of Pennsylvania (Philadelphia, PA, USA). Use of the deidentified Queensland Hospital Admitted Patient Data Collection and linked death registry data was approved by Queensland Health in accordance with the Public Health Act 2005.
Study population and data sources
We used the standardised Queensland Hospital Admitted Patient Data Collection from the baseline period (July 1, 2015, to June 1, 2016) and 2 years after implementation of ratios (Jan 1 to Dec 31, 2018). The datafiles provide detailed information on patient demographics, diagnoses, procedures (with coding from the International Classification of Diseases, tenth edition, Australia modification), comorbidities, and discharge status. The files were linked with death records to measure 30-day mortality. Our focus was on adult patients in general medical-surgical wards—the clinical area targeted for change in nurse staffing ratios. Patients undergoing labour and delivery and patients being treated for psychiatric conditions were excluded.
We surveyed registered nurses and enrolled nurses—the types of nurses considered under the policy—before and after policy implementation to gather information on medical-surgical nurse staffing levels in the hospitals where they worked. Surveying bedside nurses, an approach supported by the organisational research literature, 20 yields data on staffing levels with excellent predictive validity 2 , 4 compared with single key-informant reports or administrative data, which often include non-direct care nurses (eg, management) and inflate staffing estimates. We provided respondents with a list of Queensland hospitals, so nurses could identify their hospital and the type of ward where they worked. This allowed us to attribute information from medical-surgical ward respondents to their hospital, aggregate their responses to produce hospital-level measures of medical-surgical ward staffing, and link them to independent data on patient outcomes and hospital size. The baseline survey data were collected between May 1 and May 31, 2016 (before ratio implementation on July 1, 2016). We repeated the survey 2 years after implementation between May 1 and May 31, 2018. We used a modified Dillman 21 approach for email survey campaigns. In the baseline period, we sent emails and reminders to 26 871 nurses and received responses from 8732, giving an overall response rate of 32%. 2 years after implementation, we sent 30 658 emails and received responses from 8278 nurses, giving a response rate of 27%. Although a downward trend in survey responses has been well known in the past decade, these response rates were satisfactory and considered high for email-based surveys. 22 , 23 These rates are consistent with or better than response rates for similar nurse surveys in the USA. 3 , 4 , 24 , 25 The most important issue for the design of this study was to have a sufficient number of responses from nurses in each hospital to provide reliable staffing estimates. Although no threshold has been set for the number of respondents that ensures the reliability of the staffing measure we estimate, our previous work suggests that ten or more nurses per hospital suffice to provide staffing estimates that differ little from, and have the same effect as, measures estimated from 20, 30, or 40 or more nurses. 2 , 3 , 4 The average number of medical-surgical nurse respondents per hospital was sufficient for the purposes of this study—our sample of hospitals (55, with 27 intervention hospitals and 28 comparison hospitals) included almost all hospitals in Queensland with more than 100 beds, represented by an average of 64 nurse respondents per hospital and as many as 588. Of key importance from the standpoint of representativeness, the 36 hospitals in our analyses accounted for 83% of all adult patient admissions to acute care hospitals statewide. Although nurse staffing on every ward probably affects patient outcomes, we restricted our attention to medical-surgical wards because doing so simplified the comparison across intervention and comparison hospitals, and these wards were the targeted setting for the policy.
Our measure of primary interest was hospital-level nurse-to-patient ratio on adult medical-surgical wards (hereafter referred to as nurse-to-patient ratios). By asking each nurse how many nurses and patients were on the ward during the last shift the nurse worked, and by averaging them to ward level and then hospital level, we produced a nurse staffing measure reflecting the average nurse-to-patient ratio across all medical-surgical wards in the hospitals. This method is consistent with the ratios legislation, which allows individual nurses to have a greater (or lesser) number of patients than the prescribed ratio, so long as the ward's average is in compliance during the shift. As in other work, 2 , 4 we expressed the ratio as the number of patients per nurse, allowing us to interpret model results in terms of the effect of each additional patient per nurse on each outcome.
Patient outcomes we assessed were patient 30-day mortality, 7-day readmission, and LOS. We used the Queensland Hospital Admitted Patient Data files to identify patient outcomes. These data were linked with death records, allowing us to capture deaths occurring within 30 days of admission, even those occurring outside the hospital. This eliminated bias due to hospital LOS variation arising from different discharge practices. 26 To measure 7-day readmissions, we established the initial admission for each patient during each time period as the index admission. Patients who died during the index admission were excluded. For each index admission, we created a binary variable coded 0 if the patient was not admitted to any acute care hospital in the 7 days after discharge from index hospitalisation, and 1 if the patient was admitted within 7 days of discharge (except obstetric deliveries). LOS was measured continuously from admission to discharge. The minimum LOS was 1 day. Same-day and long-term (LOS >30 days) patients were excluded.
To adjust for differences in patient mix across hospitals, our readmission and mortality models included risk scores for each outcome derived from models that regressed the different outcomes on 17 indicators (eg, diabetes, cancer, and so on) from the Charlson Comorbidity Index to account for confounding comorbidities, 27 , 28 , 29 , 30 as well as sex, age, and dummy variables for the Diagnosis-Related Group (DRG). These scores were derived from separate logistic regression models in which we estimated a risk score for death or readmission based on the patient characteristics described. These models showed excellent discrimination ( c statistics were approximately 0·90). Readmission models were restricted to short-term patients (LOS ≤30 days) with discharge to home. Models for LOS were also restricted to short-term patients and controlled for whether patients died during hospitalisation and for age, mortality risk, comorbidities, and DRG.
Statistical analysis
We first described the patients in intervention and comparison hospitals before and after implementation of ratios, including their sex, age, comorbidities, and outcomes (ie, mortality, readmissions, and LOS). We then provided the results of estimating multilevel random-intercept logistic regression models for mortality and readmissions and zero-truncated negative binomial regression models (LOS was a count variable) to produce odds ratios (ORs) for mortality and readmissions and incident rate ratios (IRRs) for LOS, indicating the differential change in outcomes between patients in intervention and comparison hospitals, after accounting for hospital characteristics (ie, size and time-invariant factors) and patient characteristics. The specification of multilevel models for panels of macro units with observations on nested micro units is detailed in Fairbrother, 31 and its elaboration in the context of a prospective panel study of nurses nested within hospitals is presented in Sloane and colleagues. 24 Finally, after showing how nurse staffing had changed over time, we used similar models to estimate whether staffing improvements were associated with patient outcome improvements. We did not have missing data; all models were adjusted for clustering of patients in hospitals and controlled for hospital size. Using expected frequencies derived from our models, we estimated the counterfactual for each outcome, that is, what outcomes would we expect in intervention hospitals if ratios had not been implemented. We then used published cost data to make a rough estimate of return on investment derived by preventing additional LOS and readmissions.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
For this study, we included 231 902 patients (142 986 in intervention hospitals and 88 916 in comparison hospitals) assessed at baseline (2016) and 257 253 patients (160 167 in intervention hospitals and 97 086 in comparison hospitals) assessed in the post-implementation period (2018). Patients in intervention hospitals were slightly younger and less likely to be women than those in comparison hospitals ( table 1 ). The differences in comorbidities between timepoints were minimal in most cases for patients in both intervention and comparison hospitals. Although slightly higher rates of diabetes without complications and cancer were observed in patients in comparison hospitals, all other comorbidities were somewhat more common in patients in intervention hospitals.
Patient characteristics by baseline or post-implementation time period and by intervention or comparison hospitals
Data are n (%) or mean (SD). Comorbidities present for fewer than 1% of patients are included in the analyses but excluded from this table. These include peripheral vascular disease, rheumatoid disease, peptic ulcer disease, moderate or severe liver disease, and AIDS.
Regarding the average number of patients per nurse, comparison hospitals averaged 6·13 patients per nurse (SD 0·75) at baseline and improved slightly after implementation to 5·96 patients per nurse (0·98). Intervention hospitals were better staffed on average at baseline (4·84 patients per nurse, SD 1·05) but improved by a greater margin to 4·37 patients per nurse (0·54) after implementation ( table 2 ). The differences in these SDs, while unadjusted, indicate that the variation across intervention hospitals was reduced by half, whereas the variation across comparison hospitals increased somewhat over time. Regarding patient outcomes, 30-day mortality was somewhat higher overall at each timepoint for patients in intervention hospitals than for those in comparison hospitals, but although the percentage of patient deaths increased over time for patients in comparison hospitals, it decreased for those in intervention hospitals ( table 2 ). Readmissions were slightly higher overall and in each timepoint for patients in intervention hospitals than for those in comparison hospitals, though the only change that occurred across timepoints—to the extent there was any change at all—was restricted to patients in comparison hospitals. Fewer than 2·8% of these patients were readmitted at baseline, whereas nearly 3% were readmitted post-implementation ( table 2 ). By contrast, mean LOS was shorter and declined by a greater amount for patients in intervention hospitals than for those in comparison hospitals.
Patient mortality, readmissions, and length of stay, by timepoint and by intervention or comparison hospitals
Data are n/N (%), unless otherwise specified.
These results are tentative because they were not adjusted for differences in patient characteristics (eg, sex, age, and comorbidities) or differences in the size of intervention and comparison hospitals. To make these adjustments and assess differences across the two hospital groups over time, we used multilevel and multivariable models and, in the case of mortality and readmissions, converted percentages and percentage differences to odds and ORs. We first used the full sample of 55 hospitals to address whether the changes in outcomes were different in intervention versus comparison hospitals. We then used the sample of 36 hospitals with staffing data available to address whether, and to what extent, change in the outcomes in the two hospital groups were due to changes in staffing.
At baseline, patients in intervention hospitals had 34% higher 30-day mortality odds than those in comparison hospitals (adjusted OR 1·34, 95% CI 1·09–1·64, p=0·0052; table 3 ). After implementation, patients in comparison hospitals had higher, though not significantly, 30-day mortality odds (1·07, 0·97–1·17, p=0·18) than at baseline, whereas patients in intervention hospitals had significantly lower odds (0·89, 0·84–0·95, p=0·0003) than at baseline. The adjusted OR for the interaction between intervention hospitals and the implementation timepoint (0·84, 0·75–0·93, p=0·0016) implied that the difference in 30-day mortality odds between patients in intervention and comparison hospitals in the post-implementation period was significantly smaller than at baseline—only 12% higher (1·12, 0·91–1·37, p=0·28) and no longer significant ( vs the significant difference of 34% higher at baseline).
Adjusted ORs and IRRs indicating the differences in mortality, readmissions, and length of stay between intervention and comparison hospitals (total n=55) and differential changes in those outcomes across timepoints
ORs for 30-day mortality and 7-day readmissions were estimated with random-intercept logistic regression models. IRRs for length of stay were estimated with zero-truncated negative binomial regression models. All models adjusted for the clustering of patients in hospitals and controlled for hospital size. DRG=Diagnosis-Related Group. IRR=incident rate ratio. OR=odds ratio.
The main ORs and interaction effects for readmissions and IRRs for LOS showed a similar pattern ( table 3 ). Patients in intervention hospitals initially had 15% higher odds on readmissions than those in comparison hospitals (adjusted OR 1·15, 0·98–1·34, p=0·090), and patients in comparison hospitals had a 6% increase in odds of readmission from baseline to post-implementation (1·06, 1·01–1·12, p=0·015). At the same time, no change over time was observed for patients in intervention hospitals (1·00, 0·95–1·04, p=0·92). The adjusted OR for the interaction (0·94, 0·88–0·99, p=0·049) implied that the difference in odds of readmission between patients in intervention and comparison hospitals in the post-implementation period was significantly smaller than at baseline—only 8% higher (1·08, 0·92–1·26, p=0·35) and no longer indicating a significant difference. Patients in intervention hospitals initially had 22% shorter LOS than those in comparison hospitals (adjusted IRR 0·78, 95% CI 0·72–0·84, p<0·0001). For patients in comparison hospitals, we observed a decrease in the average LOS by a factor of 0·95 (0·93–0·98, p=0·0001), or 5%. For patients in intervention hospitals, the decrease in LOS was even greater and equal to 0·91 (95% CI 0·89–0·94, p<0·0001), or by 9%. The adjusted OR for the interaction (0·95, 0·92–0·99, p=0·010) suggests that the difference in LOS between patients in intervention and those in comparison hospitals in the post-implementation period was even greater than at baseline—26% shorter LOS (0·74, 0·68–0·81, p<0·0001).
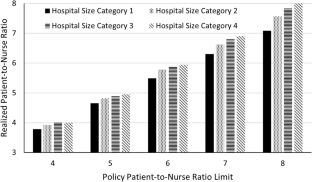
Subsequently, we focused on whether outcomes changes resulted from changes in staffing specifically. We eliminated the interaction between intervention and timepoint considered in the previous analyses and replaced it with an indicator of the staffing change over time and the effect on outcomes. The 36 hospitals for which we had reliable staffing measures included 21 (78%) of 27 intervention hospitals and 15 (54%) of 28 comparison hospitals. Staffing changed from baseline to post-implementation in these 36 hospitals ( figure ). 30 (83%) hospitals had staffing that amounted to more than 4·5 patients per nurse at baseline, whereas the same was true for only 21 (58%) hospitals in the post-implementation period. Notably, only one comparison hospital had a marked decrease in the ratio of patients per nurse between timepoints (ie, from one ratio interval to a lower one in the figure ) and, although average patients per nurse diminished by 0·47 in intervention hospitals, it diminished by 0·17 patients per nurse in comparison hospitals.

Number of hospitals with various staffing levels at baseline and post-implementation
When staffing and changes in staffing were taken into account, the difference between intervention and comparison hospitals—the intervention effect—was significant only for LOS, while the overall change—the post-implementation effect—in readmissions and LOS remained significant ( table 4 ). Most notably, the model showed that when staffing improves, or decreases by one patient per nurse, the odds on all three outcomes decrease significantly ( table 4 ).
Adjusted ORs and IRRs indicating the differences in mortality, readmissions, and length of stay between intervention and comparison hospitals and the effect of changes in staffing on those outcomes across timepoints
DRG=Diagnosis-Related Group. IRR=Incident rate ratio. OR=odds ratio.
Using the expected frequencies derived from our models, we estimated that, absent the policy, intervention hospitals could have expected to see 145 more deaths, 255 more readmissions, and 29 222 additional hospital days. It was estimated that 167 full-time equivalents were needed to meet ratio requirements (Mohle B, Queensland Nurses and Midwives' Union, personal communication); at an average cost of AUD$100 000 (on the high end of the wage range) per full-time equivalent per year, 32 the cost to fund these positions would amount to approximately $33 000 000 over the first 2 years post-implementation. Taking our estimates of LOS days and readmissions averted, we can estimate avoided costs. We used data from Australia's Independent Hospital Pricing Authority 33 on average hospital day costs in Queensland ($2312 in 2015–16) as the basis of our estimates. By preventing 255 readmissions with an average LOS of 2·7 days, the average costs avoided would be $1 589 594 (95% CI 1 179 120–2 358 240). By preventing 29 222 hospital days, the average costs avoided would be $67 561 264 (54 049 011–81 073 517).
Our prospective panel study of Queensland hospitals revealed four key findings. First, the nurse-to-patient ratios mandate resulted in nurse staffing improvements at intervention hospitals that were significantly different from those in comparison hospitals, where staffing remained largely unchanged. This suggests that the improvements we observed were not part of a statewide secular trend of better nurse staffing; rather, the change was largely isolated to the hospitals prompted to improve by the policy. Second, intervention hospitals saw greater patient outcome improvements. Although intervention hospitals had patients who were sicker than those in comparison hospitals, and thus had somewhat worse baseline outcomes, their improvement in mortality, LOS, and readmissions was significantly better even after accounting for demographics, comorbidities, DRGs, and hospital size. Third, using data from medical-surgical ward nurses (the setting targeted by the policy), we found that changes in staffing in intervention hospitals accounted for a significant share of the outcome advantage for those hospitals. Finally, our estimates suggest that the policy resulted in significant cost savings.
This study also contributes to the understanding of the causal relationship between improved staffing and patient outcomes. The literature showing better outcomes in better staffed hospitals mostly involves cross-sectional studies; although they highlight clear associations, causality cannot necessarily be inferred. 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 Some studies have examined longitudinal data and have determined that outcomes improve more when staffing similarly improves, 23 but these studies relied on natural staffing change trends. Our study takes the additional step of informing whether direct state intervention yields better staffing, and whether those staffing improvements result in better patient outcomes. The answer to both questions was yes. Although probably not the only policy design that could stimulate staffing improvements and improved outcomes, Queensland's policy implementation is a viable model offering lessons for other countries.
Our study has limitations. We refer to it as a quasi-experimental study, which is appropriate in the broad sense that it involves comparing a sample of comparison hospitals with intervention hospitals before and after the intervention—in this case an improvement in staffing—is observed in one group but not the other and in a natural setting rather than a controlled environment. However, the participating hospitals were not selected at random and were not assigned randomly to intervention and comparison groups—rather, intervention hospitals were chosen by the government. Moreover, comparison hospitals were not matched to intervention hospitals because we did not have the information needed for matching on many relevant characteristics and because the number of potential matches was insufficient for a very complete matching in any event. Therefore, we had to control for differences between hospitals using statistical controls rather than by design, or by using randomly selected and assigned hospitals. The higher prevalence of pre-existing conditions among patients in the intervention hospitals might have been due to the fact that intervention hospitals were larger (all comparison hospitals had fewer than 500 beds, whereas 22 [81%] of 27 intervention hospitals had fewer than 500 beds and five [19%] had more than 500 beds). However, our incorporation of patient-level measures of pre-existing conditions did adjust for a key observable factor that differentiated intervention from comparison hospitals, and the prospective panel design, with a focus on change over time, eliminated unobserved fixed effects that might have distinguished the two hospital groups. An additional limiting factor is that there were not enough medical-surgical nurses in some hospitals to reliably estimate the average staffing on medical-surgical wards, especially in small comparison hospitals. Nonetheless, most relevant patients were covered by the study hospital panel, suggesting that a nurse-to-patient ratio mandate would have a substantial public benefit.
The costs saved because of reduced LOS and readmissions were estimated to be more than twice the costs of the additional staffing needed to comply with the policy while also yielding lower mortality. This information on Queensland offers insights for the jurisdictions that are debating minimum nurse-to-patient ratio policies (eg, New York and Illinois in the USA, and others in Australia) and for the international interest in interventions to improve nurse staffing. The most recent debate over nurse-to-patient ratios was in 2017, in Massachusetts (USA), which proposed a ratios mandate by ballot initiative. 34 The state was flooded with advertising from interested stakeholders against ratios, arguing that the evidence for ratios was insufficient. Opponents raised concerns that there had not been a prospective evaluation of a staffing policy such as the one described in this report, and thus evidence of effectiveness was unclear. Likewise, opponents argued that little information existed about the return on investment from the additional nurses required as a result of a ratios mandate. Our findings fill these gaps.
An argument raised when California implemented ratios was that the policy was inflexible, applying ratios to all nurses at all times—when a nurse needed to go to lunch or take a break, other nurses were needed to cover the patient assignment. But other nurses were often at their limit and couldn't take additional patients, even for a short period, and still comply with the law. This frustrated managers and made implementation difficult for many hospitals, especially early on. By contrast, Queensland mandated a minimum average staffing level at the ward level—an individual nurse could have more or fewer so long as the average number of patients per nurse didn't exceed the ratio limits. This offered more flexibility in patient assignments. Our analysis suggests that Queensland's flexible design is feasible and yields good outcomes. The Queensland evaluation design has prompted similar policy research in the USA, with similar findings. 35 , 36
In conclusion, having enough nurses with manageable workloads has been shown to be important for good patient care and outcomes. The 2018 International Council of Nurses' Position Statement on Evidence-Based Nurse Staffing 16 recommends that governments should take action to ensure safe staffing levels. The results presented here suggest that minimum nurse-to-patient ratio policies are a feasible instrument to improve nurse staffing, produce better patient outcomes, and yield a good return on investment.
Data sharing
Declaration of interests.
We declare no competing interests.
Acknowledgments
This study was supported by grants from Queensland Health and the National Institutes of Health, National Institute of Nursing Research (R01NR014855). The authors are independent and solely responsible for study design, data collection and analysis, findings, and interpretation, which do not necessarily represent views of Queensland Health. We would like to acknowledge Tim Cheney, Frances Hughes, Irene Hung, Beth Mohle, Shelley Nowlan, Natalie Spearing, and Kate Veach for their contributions to this work.
Contributors
All authors contributed to the conception and design of the study. MDM, LHA, CW, CD, and PY contributed to the collection of data. MDM and DMS accessed, verified, and oversaw analysis of the data. All authors contributed to the interpretation of the data and preparation of the manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors approved the final manuscript.
Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals
Affiliations.
- 1 School of Nursing, Center for Health Outcomes and Policy Research, University of Pennsylvania, Philadelphia, PA, USA. Electronic address: [email protected].
- 2 School of Nursing, Center for Health Outcomes and Policy Research, University of Pennsylvania, Philadelphia, PA, USA.
- 3 School of Nursing, Queensland University of Technology, Kelvin Grove, QLD, Australia; Centre for Healthcare Transformation, Faculty of Health, Queensland University of Technology, Brisbane, QLD, Australia.
- 4 School of Nursing, Queensland University of Technology, Kelvin Grove, QLD, Australia; Centre for Healthcare Transformation, Faculty of Health, Queensland University of Technology, Brisbane, QLD, Australia; Metro North Hospital and Health Service, Royal Brisbane and Women's Hospital, Herston, QLD, Australia.
- PMID: 33989553
- PMCID: PMC8408834
- DOI: 10.1016/S0140-6736(21)00768-6
Background: Substantial evidence indicates that patient outcomes are more favourable in hospitals with better nurse staffing. One policy designed to achieve better staffing is minimum nurse-to-patient ratio mandates, but such policies have rarely been implemented or evaluated. In 2016, Queensland (Australia) implemented minimum nurse-to-patient ratios in selected hospitals. We aimed to assess the effects of this policy on staffing levels and patient outcomes and whether both were associated.
Methods: For this prospective panel study, we compared Queensland hospitals subject to the ratio policy (27 intervention hospitals) and those that discharged similar patients but were not subject to ratios (28 comparison hospitals) at two timepoints: before implementation of ratios (baseline) and 2 years after implementation (post-implementation). We used standardised Queensland Hospital Admitted Patient Data, linked with death records, to obtain data on patient characteristics and outcomes (30-day mortality, 7-day readmissions, and length of stay [LOS]) for medical-surgical patients and survey data from 17 010 medical-surgical nurses in the study hospitals before and after policy implementation. Survey data from nurses were used to measure nurse staffing and, after linking with standardised patient data, to estimate the differential change in outcomes between patients in intervention and comparison hospitals, and determine whether nurse staffing changes were related to it.
Findings: We included 231 902 patients (142 986 in intervention hospitals and 88 916 in comparison hospitals) assessed at baseline (2016) and 257 253 patients (160 167 in intervention hospitals and 97 086 in comparison hospitals) assessed in the post-implementation period (2018). After implementation, mortality rates were not significantly higher than at baseline in comparison hospitals (adjusted odds ratio [OR] 1·07, 95% CI 0·97-1·17, p=0·18), but were significantly lower than at baseline in intervention hospitals (0·89, 0·84-0·95, p=0·0003). From baseline to post-implementation, readmissions increased in comparison hospitals (1·06, 1·01-1·12, p=0·015), but not in intervention hospitals (1·00, 0·95-1·04, p=0·92). Although LOS decreased in both groups post-implementation, the reduction was more pronounced in intervention hospitals than in comparison hospitals (adjusted incident rate ratio [IRR] 0·95, 95% CI 0·92-0·99, p=0·010). Staffing changed in hospitals from baseline to post-implementation: of the 36 hospitals with reliable staffing measures, 30 (83%) had more than 4·5 patients per nurse at baseline, with the number decreasing to 21 (58%) post-implementation. The majority of change was at intervention hospitals, and staffing improvements by one patient per nurse produced reductions in mortality (OR 0·93, 95% CI 0·86-0·99, p=0·045), readmissions (0·93, 0·89-0·97, p<0·0001), and LOS (IRR 0·97, 0·94-0·99, p=0·035). In addition to producing better outcomes, the costs avoided due to fewer readmissions and shorter LOS were more than twice the cost of the additional nurse staffing.
Interpretation: Minimum nurse-to-patient ratio policies are a feasible approach to improve nurse staffing and patient outcomes with good return on investment.
Funding: Queensland Health, National Institutes of Health, National Institute of Nursing Research.
Copyright © 2021 Elsevier Ltd. All rights reserved.
Publication types
- Multicenter Study
- Cause of Death
- Health Policy*
- Length of Stay / statistics & numerical data*
- Middle Aged
- Nursing Staff, Hospital / supply & distribution*
- Patient Readmission / statistics & numerical data*
- Personnel Staffing and Scheduling / statistics & numerical data*
- Prospective Studies
- Quality of Health Care / statistics & numerical data*
Grants and funding
- R01 NR014855/NR/NINR NIH HHS/United States
Patient-to-nurse ratios: Balancing quality, nurse turnover, and cost
- Published: 29 November 2023
- Volume 26 , pages 807–826, ( 2023 )
Cite this article
- David D. Cho 1 ,
- Kurt M. Bretthauer 2 &
- Jan Schoenfelder 3 , 4
1359 Accesses
Explore all metrics
We consider the problem of setting appropriate patient-to-nurse ratios in a hospital, an issue that is both complex and widely debated. There has been only limited effort to take advantage of the extensive empirical results from the medical literature to help construct analytical decision models for developing upper limits on patient-to-nurse ratios that are more patient- and nurse-oriented. For example, empirical studies have shown that each additional patient assigned per nurse in a hospital is associated with increases in mortality rates, length-of-stay, and nurse burnout. Failure to consider these effects leads to disregarded potential cost savings resulting from providing higher quality of care and fewer nurse turnovers. Thus, we present a nurse staffing model that incorporates patient length-of-stay, nurse turnover, and costs related to patient-to-nurse ratios. We present results based on data collected from three participating hospitals, the American Hospital Association (AHA), and the California Office of Statewide Health Planning and Development (OSHPD). By incorporating patient and nurse outcomes, we show that lower patient-to-nurse ratios can potentially provide hospitals with financial benefits in addition to improving the quality of care. Furthermore, our results show that higher policy patient-to-nurse ratio upper limits may not be as harmful in smaller hospitals, but lower policy patient-to-nurse ratios may be necessary for larger hospitals. These results suggest that a “one ratio fits all” patient-to-nurse ratio is not optimal. A preferable policy would be to allow the ratio to be hospital-dependent.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Improving patient safety by optimizing the use of nursing human resources.
Christian M. Rochefort, David L. Buckeridge & Michal Abrahamowicz

Evaluating the Costs and Outcomes of Hospital Nursing Resources: a Matched Cohort Study of Patients with Common Medical Conditions
Karen B. Lasater, Matthew D. McHugh, … Jeffrey H. Silber

The Nurse Workforce
Data availability.
The AHA and OSHPD data are publicly available.
Agency for Healthcare Research and Quality (2016) Access and disparities in access to health care. Rockville, MD. https://archive.ahrq.gov/research/findings/nhqrdr/nhqdr15/access.html . Accessed 15 Sept 2022
Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T (2008) Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm 38(5):223–229
Article Google Scholar
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH (2002) Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. J Am Med Assoc 288(16):1987–1993
Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, Diomidous M, Kinnunen J, Kózka M, Lesaffre E, McHugh MD, Moreno-Casbas MT, Rafferty AM, Schwendimann R, Scott PA, Tishelman C, van Achterberg T, Sermeus W (2014) Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. The Lancet 383(9931):1824–1830
Aiken LH, Sloane DM, Cimiotti JP, Clarke SP, Flynn L, Seago JA, Spetz J, Smith HL (2010) Implications of the California nurse staffing mandate for other states. Health Serv Res 45(4):904–921
Aiken LH, Sloane DM, Griffiths P, Rafferty AM, Bruyneel L, McHugh M, Maier CB, Moreno-Casbas T, Ball JE, Ausserhofer D, Sermeus W (2017) Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual Saf 26:559–568
Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, Bruyneel L, Rafferty AM, Griffiths P, Moreno-Casbas MT, Tishelman C, Scott A, Mrzostek T, Kinnunen J, Schwendimann R, Heinen M, Zikos D, Sjetne IS, Smith HL, Kutney-Lee A (2012) Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 344:e1717
Aiken LH, Xue Y, Clarke SP, Sloane DM (2007) Supplemental nurse staffing in hospitals and quality of care. J Nurs Adm 37(7–8):335–342
Ang BY, Lam SWS, Pasupathy Y, Ong MEH (2018) Nurse workforce scheduling in the emergency department: a sequential decision support system considering multiple objectives. J Nurs Manag 26(4):432–441
Bae SH, Mark B, Fried B (2010) Use of temporary nurses and nurse and patient safety outcomes in acute care hospital units. Health Care Manage Rev 35(4):333–344
Ball JE, Bruyneel L, Aiken LH, Sermeus W, Sloane DM, Rafferty AM, Lindqvist R, Tishelman C, Griffiths P (2018) Post-operative mortality, missed care and nurse staffing in nine countries: across-sectional study. Int J Nurs Stud 78:10–15
Benzaid M, Lahrichi N, Rousseau LM (2020) Chemotherapy appointment scheduling and daily outpatient–nurse assignment. Health Care Manag Sci 23(1):34–50
Bond C., Raehl CL, Pitterle ME, Franke T (1999) Health care professional staffing, hospital characteristics, and hospital mortality rates. Pharmacother: J Human Pharmacol Drug Ther 19(2):130–138
Bretthauer KM, Heese HS, Pun H, Coe E (2011) Blocking in healthcare operations: A new heuristic and an application. Prod Oper Manag 20(3):375–391
Brooks Carthon JM, Hatfield L, Brom H, Houton M, Kelly-Hellyer E, Schlak A, Aiken LH (2021) System-level improvements in work environments lead to lower nurse burnout and higher patient satisfaction. J Nurs Care Qual 36(1):7–13
Bureau of Labor Statistics, U.S. Department of Labor (2022) Occupational outlook handbook, registered nurses. http://www.bls.gov/ooh/healthcare/registered-nurses.htm . Accessed 15 Sept 2022
Burke EK, Curtois T (2014) New approaches to nurse rostering benchmark instances. Eur J Oper Res 237(1):71–81
Campbell GM (1999) Cross-utilization of workers whose capabilities differ. Manage Sci 45(5):722–732
Chang AM, Cohen D, Lin A, Augustine J, Handel D, Howell E, Kim H, Pines J, Schuur JD, McConnell KJ, Sun BC (2018) Hospital strategies for reducing emergency department crowding: a mixed-methods study. Ann Emerg Med 71(4):497-505.e4
Cheang B, Li H, Lim A, Rodrigues B (2003) Nurse rostering problems––a bibliographic survey. Eur J Oper Res 151(3):447–460
Chhatwal J, Alagoz O, Burnside ES (2010) Optimal breast biopsy decision-making based on mammographic features and demographic factors. Oper Res 58(6):1577–1591
Cho D, Cattani K (2019) The patient patient: the performance of traditional versus open-access scheduling policies. Decis Sci 50(4):756–785
Cho E, Sloane DM, Kim EY, Kim S, Choi M, Yoo IY, Lee HS, Aiken LH (2015) Effects of nurse staffing, work environments, and education on patient mortality: An observational study. Int J Nurs Stud 52(2):535–542
Cho SH, Ketefian S, Barkauskas VH, Smith DG (2003) The effects of nurse staffing on adverse events, morbidity, mortality, and medical costs. Nurs Res 52(2):71–79
Dall TM, Chen YJ, Seifert RF, Maddox PJ, Hogan PF (2009) The economic value of professional nursing. Med Care 47(1):97–104
Daskin MS, Dean LK (2005) Location of health care facilities. Operations research and health care: a handbook of methods and applications. In: Brandeau M, Sainfort F, Pierskalla WP (eds). Kluwer Academic Publishers. Chapter 3, pp 43–76
De Véricourt F, Jennings OB (2011) Nurse staffing in medical units: a queueing perspective. Oper Res 59(6):1320–1331
Denton BT, Miller AJ, Balasubramanian HJ, Huschka TR (2010) Optimal allocation of surgery blocks to operating rooms under uncertainty. Oper Res 58(4):802–816
Dobson G, Hasija S, Pinker EJ (2011) Reserving capacity for urgent patients in primary care. Prod Oper Manag 20(3):456–473
Dobson G, Lee HH, Pinker E (2010) A model of ICU bumping. Oper Res 58(6):1564–1576
Dobson G, Pinker E, Van Horn RL (2009) Division of labor in medical office practices. Manuf Serv Oper Manag 11(3):525–537
Easton FF (2011) Cross-training performance in flexible labor scheduling environments. IIE Transaction 43(8):589–603
Faridimehr S, Venkatachalam S, Chinnam RB (2021) Managing access to primary care clinics using scheduling templates. Health Care Manag Sci 24(3):482–498
Fagerström L, Kinnunen M, Saarela J (2018) Nursing workload, patient safety incidents and mortality: an observational study from Finland. BMJ Open 8(e016367):1–10
Google Scholar
Gnanlet A, Gilland WG (2009) Sequential and simultaneous decision making for optimizing health care resource flexibilities. Decis Sci 40(2):295–326
Gnanlet A, Gilland WG (2014) Impact of productivity on cross-training configurations and optimal staffing decisions in hospitals. Eur J Oper Res 238(1):254–269
Green, L.V. (2005). Capacity Planning and Management in Hospitals. In: Brandeau, M.L., Sainfort, F., Pierskalla, W.P. (eds) Operations Research and Health Care. International Series in Operations Research & Management Science, vol 70. Springer, Boston, MA. pp 15-41
Green LV, Savin S (2008) Reducing delays for medical appointments: A queueing approach. Oper Res 56(6):1526–1538
Griffiths P, Ball J, Bloor K, Böhning D, Briggs J, Dall’Ora C, De Iongh A, Jones J, Kovacs C, Maruotti A, Meredith P, Prytherch D, Saucedo AR, Redfern O, Schmidt P, Sinden N, Smith G (2018) Nurse staffing levels, missed vital signs and mortality in hospitals: Retrospective longitudinal observational study. Health Serv Deliv Res 6(38)
Gupta D, Denton B (2008) Appointment scheduling in health care: Challenges and opportunities. IIE Transaction 40(9):800–819
Gurses AP, Carayon P, Wall M (2009) Impact of performance obstacles on intensive care nurses’ workload, perceived quality and safety of care, and quality of working life. Health Serv Res 44(2p1):422–443
Halawa F, Madathil SC, Gittler A, Khasawneh MT (2020) Advancing evidence-based healthcare facility design: A systematic literature review. Health Care Manag Sci 23(3):453–480
Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137(6):511–520
Hopp WJ, Tekin E, Van Oyen MP (2004) Benefits of skill chaining in serial production lines with cross-trained workers. Manage Sci 50(1):83–98
Hugonnet S, Chevrolet J, Pittet D (2007) The effect of workload on infection risk in critically ill patients. Crit Care Med 35(1):76–81
Institute of Medicine (2001) Crossing the quality chasm: a new health system for the 21st century. National Academies Press, Washington D.C
Iwashyna TJ, Kramer AA, Kahn JM (2009) Intensive care unit occupancy and patient outcomes. Crit Care Med 37(5):1545–1557
Jones CB (2005) The costs of nurse turnover, part 2: application of the nursing turnover cost calculation methodology. J Nurs Adm 35(1):41–49
Jordan WC, Inman RR, Blumenfeld DE (2004) Chained cross-training of workers for robust performance. IIE Trans 36(10):953–967
Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD (2006) Hospital volume and the outcomes of mechanical ventilation. N Engl J Med 355(1):41–50
Kanai Y, Takagi H (2021) Markov chain analysis for the neonatal inpatient flow in a hospital. Health Care Manag Sci 24(1):92–116
Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ (2007) The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care 45(12):1195–1204
Kosel K, Olivo T (2002) The business case for workforce stability. VHA Research Series 7:1–16
Lankshear AJ, Sheldon TA, Maynard A (2005) Nurse staffing and healthcare outcomes: a systematic review of the international research evidence. Adv Nurs Sci 28(2):163–174
Lee DKK, Zenios SA (2009) Optimal capacity overbooking for the regular treatment of chronic conditions. Oper Res 57(4):852–865
Legrain A, Omer J, Rosat S (2020) An online stochastic algorithm for a dynamic nurse scheduling problem. Eur J Oper Res 285(1):196–210
Lim GJ, Mobasher A, Côté MJ (2012) Multi-objective nurse scheduling models with patient workload and nurse preferences. Management 2(5):149–160
Lin H (2014) Revisiting the relationship between nurse staffing and quality of care in nursing homes: An instrumental variables approach. J Health Econ 37:13–24
Lin YK, Chou YY (2020) A hybrid genetic algorithm for operating room scheduling. Health Care Manag Sci 23(2):249–263
Lopez V, Anderson J, West S, Cleary M (2022) Does the COVID-19 pandemic further impact nursing shortages? Issues Ment Health Nurs 43(3):293–295
Ma C, McHugh MD, Aiken LH (2015) Organization of hospital nursing and 30-day readmissions in Medicare patients undergoing surgery. Med Care 53(1):65–70
Mandelbaum A, Momcilovic P, Tseytlin Y (2012) On fair routing from emergency departments to hospital wards: QED queues with heterogeneous servers. Manage Sci 58(7):1273–1291
May JH, Spangler WE, Strum DP, Vargas LG (2011) The surgical scheduling problem: Current research and future opportunities. Prod Oper Manag 20(3):392–405
McCue M, Mark BA, Harless DW (2003) Nurse staffing, quality, and financial performance. J Health Care Finance 29(4):54–76
Mousavi H, Darestani SA, Azimi P (2021) An artificial neural network based mathematical model for a stochastic health care facility location problem. Health Care Manag Sci 24(3):499–514
Musy SN, Endrich O, Leichtle AB, Griffiths P, Nakas CT, Simon M (2020) Longitudinal study of the variation in patient turnover and patient-to-nurse ratio: Descriptive analysis of a Swiss University Hospital. J Med Internet Res 22(4):e15554
Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K (2002) Nurse-staffing levels and the quality of care in hospitals. N Engl J Med 346(22):1715–1722
Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M (2011) Nurse staffing and inpatient hospital mortality. N Engl J Med 364(11):1037–1045
Needleman J, Buerhaus PI, Stewart M, Zelevinsky K, Mattke S (2006) Nurse staffing in hospitals: Is there a business case for quality? Health Aff 25(1):204–211
Newhouse RP, Johantgen M, Pronovost PJ, Johnson E (2005) Perioperative nurses and patient outcomes—mortality, complications, and length of stay. AORN J 81(3):508–528
NSI Nursing Solutions, Inc. (2021) 2021 NSI national health care retention & rn staffing report. https://www.emergingrnleader.com/wp-content/uploads/2021/04/NSI_National_Health_Care_Retention_Report.pdf . Accessed 12 Mar 2023
Oakley D, Onggo BS, Worthington D (2020) Symbiotic simulation for the operational management of inpatient beds: model development and validation using Δ-method. Health Care Manag Sci 23(1):153–169
OECD/European Union (2014) Health at a glance: Europe 2014. OECD Publishing. https://doi.org/10.1787/health_glance_eur-2014-en
Olivares M, Terwiesch C, Cassorla L (2008) Structural estimation of the newsvendor model: an application to reserving operating room time. Manage Sci 54(1):41–55
Papanicolas I, Woskie LR, Jha AK (2018) Health care spending in the United States and other high-income countries. JAMA 319(10):1024–1039
Peelen L, de Keizer N, Peek N, Jan Scheffer G, van der Voort P, de Jonge E (2007) The influence of volume and intensive care unit organization on hospital mortality in patients admitted with severe sepsis: a retrospective multicentre cohort study. Crit Care 11(2):1–10
Phibbs C, Bartel A, Giovannetti B, Schmitt S, Stone P (2009) The impact of nurse staffing and contract nurses on patient outcomes: New evidence from longitudinal data. Working Paper, Columbia Business School
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH (2007) Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med 356(21):2165–2175
Pinker EJ, Shumsky RA (2000) The efficiency-quality trade-off of cross-trained workers. Manuf Serv Oper Manag 2(1):32–48
Pronovost PJ, Dang D, Dorman T, Lipsett PA, Garrett E, Jenckes M, Bass EB (2001) Intensive care unit nurse staffing and the risk for complications after abdominal aortic surgery. Eff Clin Pract 4(5):199–206
Rauner MS, Gutjahr WJ, Heidenberger K, Wagner J, Pasia J (2010) Dynamic policy modeling for chronic diseases: Metaheuristic-based identification of pareto-optimal screening strategies. Oper Res 58(5):1269–1286
Rerkjirattikal P, Huynh VN, Olapiriyakul S, Supnithi T (2020) A goal programming approach to nurse scheduling with individual preference satisfaction. Math Probl Eng 2020:2379091
Rothberg MB, Abraham I, Lindenauer PK, Rose DN (2005) Improving nurse-to-patient staffing ratios as a cost-effective safety intervention. Med Care 43(8):785–791
Schoenfelder J, Bretthauer KM, Wright PD, Coe E (2020) Nurse scheduling with quick-response methods: Improving hospital performance, nurse workload, and patient experience. Eur J Oper Res 283(1):390–403
Shehadeh KS, Padman R (2021) A distributionally robust optimization approach for stochastic elective surgery scheduling with limited intensive care unit capacity. Eur J Oper Res 290(3):901–913
Silber JH, Rosenbaum PR, McHugh MD, Ludwig JM, Smith HL, Niknam BA, Even-Shoshan O, Fleisher LA, Kelz RR, Aiken LH (2016) Comparison of the value of nursing work environments in hospitals across different levels of patient risk. JAMA Surg 151(6):527–536
Sims CE (2003) Increasing clinical, satisfaction, and financial performance through nurse-driven process improvement. J Nurs Adm 33(2):68–75
Sloane DM, Smith HL, McHugh MD, Aiken LH (2018) Effect of changes in hospital nursing resources on improvements in patient safety and quality of care: a panel study. Med Care 56(12):1001–1008
Spence Laschinger HK, Leiter MP (2006) The impact of nursing work environments on patient safety outcomes: the mediating role of burnout engagement. J Nurs Adm 36(5):259–267
Spetz J (2004) California’s minimum nurse-to-patient ratios: the first few months. J Nurs Adm 34(12):571–578
Stanton MW, Rutherford MK (2004) Hospital nurse staffing and quality of care. Research in Action, Issue 14. Agency for Healthcare Research and Quality, Rockville, Maryland
Sturm H, Rieger MA, Martus P, Ueding E, Wagner A, Holderried M, Maschmann J (2019) Do perceived working conditions and patient safety culture correlate with objective workload and patient outcomes: A cross-sectional explorative study from a German university hospital. Plos One 14(1):e0209487 (1-19)
Theokary C, Ren ZJ (2011) An empirical study of the relations between hospital volume, teaching status, and service quality. Prod Oper Manag 20(3):303–318
Thompson S, Nunez M, Garfinkel R, Dean MD (2009) OR practice–-Efficient short-term allocation and reallocation of patients to floors of a hospital during demand surges. Oper Res 57(2):261–273
Tourangeau AE, Doran DM, Hall LMG, O’Brien Pallas L, Pringle D, Tu JV, Cranley LA (2007) Impact of hospital nursing care on 30-day mortality for acute medical patients. J Adv Nurs 57(1):32–44
Tsai SC, Yeh Y, Kuo CY (2021) Efficient optimization algorithms for surgical scheduling under uncertainty. Eur J Oper Res 293(2):579–593
U.S. General Accounting Office (GAO) (2009) Hospital emergency departments: crowding continues to occur, and some patients wait longer than recommended time frames. Report GAO-09-347
Valouxis C, Gogos C, Goulas G, Alefragis P, Housos E (2012) A systematic two phase approach for the nurse rostering problem. Eur J Oper Res 219(2):425–433
Volland J, Fügener A, Schoenfelder J, Brunner JO (2017) Material logistics in hospitals: a literature review. Omega 69:82–101
Wang WY, Gupta D (2011) Adaptive appointment systems with patient preferences. Manuf Serv Oper Manag 13(3):373–389
White DL, Froehle CM, Klassen KJ (2011) The effect of integrated scheduling and capacity policies on clinical efficiency. Prod Oper Manag 20(3):442–455
Wolbeck L, Kliewer N, Marques I (2020) Fair shift change penalization scheme for nurse rescheduling problems. Eur J Oper Res 284(3):1121–1135
Wright PD, Bretthauer KM (2010) Strategies for addressing the nursing shortage: Coordinated decision making and workforce flexibility. Decis Sci 41(2):373–401
Wright PD, Bretthauer KM, Côté MJ (2006) Reexamining the nurse scheduling problem: Staffing ratios and nursing shortages. Decis Sci 37(1):39–70
Wynendaele H, Willems R, Trybou J (2019) Systematic review: Association between the patient–nurse ratio and nurse outcomes in acute care hospitals. J Nurs Manag 27(5):896–917
Yankovic N, Green LV (2011) Identifying good nursing levels: A queuing approach. Oper Res 59(4):942–955
Yu X, Bayram A (2021) Managing capacity for virtual and office appointments in chronic care. Health Care Manag Sci 24(4):742–767
Zhang X, Tai D, Pforsich H, Lin VW (2018) United States registered nurse workforce report card and shortage forecast: a revisit. Am J Med Qual 33(3):229–236
Download references
No funds, grants, or other support was received.
Author information
Authors and affiliations.
Department of Management, College of Business and Economics, California State University, Fullerton, Fullerton, CA, 92831, USA
David D. Cho
Operations and Decision Technologies Department, Kelley School of Business, Indiana University, Bloomington, IN, 47405, USA
Kurt M. Bretthauer
Health Care Operations / Health Information Management, University of Augsburg, 86159, Augsburg, Germany
Jan Schoenfelder
School of Management, Lancaster University Leipzig, 04109, Leipzig, Germany
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, analysis, and manuscript writing were performed by David D. Cho, Kurt M. Bretthauer, and Jan Schoenfelder. All authors read and approved the final manuscript.
Corresponding author
Correspondence to David D. Cho .
Ethics declarations
Declarations, conflict of interest.
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
1.1 Three case study hospitals
We collected nursing data from three hospitals in the United States. One is located in California and two are located in Indiana. They range in size from 350 to 550 beds. We obtained information on nurse wages, shift types, staff size and mix, shift preferences and availability, patient-to-nurse ratios, and limited bed demand data. Note that detailed and extensive historical patient flow and demand data were not available. Due to the limited bed demand data, we also use data from the American Hospital Association and California Office of Statewide Health Planning and Development to estimate inpatient demand and create hospital size categories, as described in the next subsection. The three hospitals differ in size and nurse wages. Table 5 summarizes the data.
1.2 American hospital association (AHA) data
In addition to the three case study hospitals, we acquired 2015 AHA Annual Survey data from California, New York, and Texas for our numerical experiments. From the dataset, we consider hospitals with the primary service code of “general medical and surgical” and that are coded as either “nongovernment, not-for-profit” or “corporation-owned, for-profit”. We exclude hospitals that do not have any general medical and surgical adult beds. After filtering, the data set contains information on 493 hospitals across the three states of California, New York, and Texas.
Based on the 2015 AHA Annual Survey data, we created four hospital size categories, as shown in Table 6 . While the range of total facility inpatient days for category 3 is relatively wide, the impact of hospital size on the policy patient-to-nurse ratio is still captured effectively with the four categories, as shown by the results in Section 5.1 .
Figure 11 reports the proportion of general medical and surgical beds in the included hospitals according to the AHA data. The AHA data provides total hospital-wide inpatient days, but not unit-specific inpatient days, which is what we need. Therefore, based on Fig. 11 , we estimate that the inpatient days for med/surg units are around 50–80% of the total hospital-wide inpatient days.
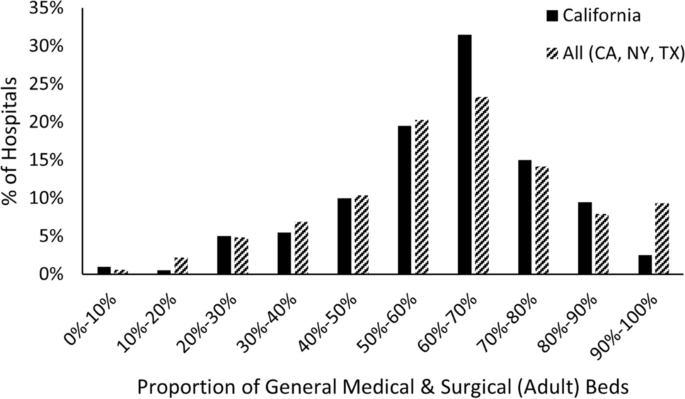
Distribution of medical and surgical bed proportion for hospitals in AHA data set
1.3 California office of statewide health planning and development (OSHPD) data
To further support our estimate of med/surg inpatient days, we also acquired data from the “2014–2015 Fiscal Year Hospital Annual Financial Disclosure Report” provided by California’s Office of Statewide Health Planning and Development (OSHPD). While this data set is limited to hospitals in California, it includes unit-specific information regarding beds and patient (census) days. After applying the identical filter as used for the AHA data set, the OSHPD data set provides information on 198 hospitals in California. Figure 12 shows that our assumption of inpatient days for the med/surg unit being around 50–80% of the total hospital-wide inpatient days is reasonable.

Distribution of medical and surgical patient days proportion for California hospitals in OSHPD data set
Appendix B. Limiting undesirable shifts for each nurse
In Section 5.3 , we minimize the total number of undesirable shifts without incurring any additional schedule costs, but we do not limit the number of undesirable shifts for each nurse. Thus, it is theoretically possible for the remaining undesirable shifts to be assigned disproportionately to a small number of nurses. While this was not a major issue for our numerical experiments in Section 5.3 due to the very low number of remaining undesirable shifts with the second objective function, we can also add constraints ( 27 ) and ( 28 ) that limit the number of undesirable shifts along with second objective function ( 23 ).
where \({\overline{US} }_{i}^{UN}\) and \({\overline{US} }_{i}^{FN}\) are upper limits on the number of undesirable shifts assigned to unit and float nurse \(i\) , respectively.
Because we still do not allow additional schedule costs, our optimal costs do not change in this case. Furthermore, we also do not observe any meaningful differences in total number of undesirable shifts compared to the results presented in Section 5.3 as long as \({\overline{US} }_{i}^{UN}\) and \({\overline{US} }_{i}^{FN}\) are not too low. We note that when the limit is too low (for example, 0 or 1 undesirable shift per nurse), the problem sometimes becomes unsolvable for policy PTN ratio of 4:1 due to the insufficient number of available and desirable shifts to stay under the policy PTN for every shift since we do not allow any increase in costs.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cho, D.D., Bretthauer, K.M. & Schoenfelder, J. Patient-to-nurse ratios: Balancing quality, nurse turnover, and cost. Health Care Manag Sci 26 , 807–826 (2023). https://doi.org/10.1007/s10729-023-09659-y
Download citation
Received : 17 May 2022
Accepted : 04 October 2023
Published : 29 November 2023
Issue Date : December 2023
DOI : https://doi.org/10.1007/s10729-023-09659-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hospital capacity planning
- Nurse staffing
- Patient-to-nurse ratios
- Quality of care
- Operations research
- Operations management
- Optimization
- Find a journal
- Publish with us
- Track your research
Health Care Access & Coverage
What Patient-To-Nurse Ratios Mean for Hospital Patient Health and Outcomes
Pennsylvania legislature pushed to take up patient safety issue it has long avoided.
- Hoag Levins
- Share this page on Twitter
- Share this page on Facebook
- Share this page on LinkedIn
“Should Hospitals be Required to Have a Certain Number of Nurses?” asks a Philadelphia Inquirer headline about the controversy brewing in Harrisburg around the latest efforts to have the Pennsylvania legislature pass a law requiring minimum patient-to-nurse ratios in its hospitals. It’s the latest general media story that seems to infer that this patient-to-nurse issue is a vague, unsettled thing essentially about a nursing labor grievance. But it isn’t. Hard scientific evidence since the 1980s has shown that having insufficient numbers of nurses on a given hospital unit kills and injures more patients than when there are enough nurses available to adequately attend and monitor those patients. The University of Pennsylvania’s School of Nursing and its Center for Health Outcomes and Policy Research (CHOPR) have played a leading international role in these decades of research.
In recent years, the number of highly trained nurses in hospitals has been affected by severe and repeated budget cuts that save money by increasing the patient-to-nurse ratios so that more patients are assigned to each nurse, and/or by using less trained and skilled aides to replace registered nurses. After California became the first state to enact a minimum required nurse staffing law for its hospitals in 1999, other hospitals and their lobbying organizations across the country worked hard to prevent similar legislation from being enacted in other states–despite the evidence that not having adequate patient-to-nurse ratios leads to higher mortality rates and worse patient outcomes.
A 12-Year effort
The latest effort to enact a minimum required nurse staffing law in Pennsylvania began early in May with the announcement of both House Bill 106 and Senate Bill 240 , which together are known as the Pennsylvania Patient Safety Act. Prior to this, similar bills have been introduced every year in the Statehouse since 2010. All have died in Republican-controlled committees.
“It is really an example of how in our democracy a couple of individuals for their own personal reasons can deny legislation that is in the public interest from coming up for a vote,” said Founding Director of CHOPR and LDI Senior Fellow Linda Aiken, PhD, RN .
But now, after last November’s elections, Democrats hold the majority in the Pennsylvania House for the first time in 12 years and this new round of nurse ratio bills is being heavily lobbied by nursing organizations, unions, and public health advocates.
The Pennsylvania Patient Safety Act would set the minimum numbers of patients that could be assigned to individual nurses in a hospital’s various departments. Those ratios vary depending upon the nature of the unit’s focus and severity of patients’ conditions and treatment. ( See the list of the exact ratios the Act specifies for various hospital units .)
Nursing Surveillance
It isn’t all that difficult to understand why patient-to-nurse ratios matter if you think of the times you yourself have been in a hospital bed. Nurses function as your minute-to-minute biomedical and wellbeing surveillance system. Although they may appear to be just taking your temperature, providing scheduled pills, or checking your IV set up, they are doing much more invisibly — for every patient under their care.
The wide variety of conditions and illnesses treated in hospitals are all prone to various sorts of disastrous, and often unexpected complications that, if not recognized and immediately addressed, can lead to increased patient deaths, injury, or permanent disability. Together across a ward or unit, nurses function as a critical surveillance system constantly monitoring each patient for the subtle signs that something in their condition has or is about to change for the worse. This invisible surveillance system by highly trained and experienced registered nurses is the most critical–but least understood–of the services they provide.
But the intensity and effectiveness of that surveillance is determined by how many patients a single nurse is charged with caring for. For instance, a registered nurse caring for four seriously ill patients on a shift can conduct a far more comprehensive surveillance on each than if caring 10 or more seriously ill patients on a shift. Research has shown that each additional patient assigned to a registered nurse beyond the optimum ratio significantly increases the risk of preventable death, longer stays, readmissions, and unfavorable patient satisfaction. It directly results in less effective care, poorer patient outcomes, and higher costs of care.
State-Wide PA Hospital Study
In her testimony earlier this month as lead witness before the Pennsylvania House Health Committee hearing on the Patient Safety Act, Aiken detailed the findings of CHOPR’s recent study of patient-to-nurse variations and health outcomes in 114 Pennsylvania hospitals. Conducted according to a National Institutes of Health-funded research protocol, the project used data from more than half a million patients.
In adult medical and surgical units in the 114 hospitals, researchers found patient-to-nurse ratios variations from 3-11. “This is huge variation in a hospital resource that has been shown in hundreds of studies to be associated with a wide range of patient outcomes including mortality, failure to rescue patients with complications, hospital acquired infections, patient satisfaction, length of stay, readmissions, and patient safety,” they noted.
Further analyzing 33 different aspects of patient severity of illness and hospital organizational characteristics, the researchers determined that “in-hospital mortality increased by 7% for each additional medical patient and 8% for each surgical patient added to nurses’ workloads.” They also found that hospital readmissions increased by 2% for medical patients and 4% for surgical patients for each 1 patient increase in nurses’ patient workloads.”
Preventing 1,155 Unnecessary Deaths
The researchers estimated that if the Patient Safety Act was passed and implemented it would:
- Prevent 1,155 hospital deaths annually in Pennsylvania hospitals
- Avoid 771 hospital readmissions annually
- Reduce length of stay in the aggregate by 39,919 days annually, which would alone save Pennsylvania hospitals $93 million
- Accrue additional savings for hospitals with higher patient satisfaction, avoid Medicare readmission penalties, and reduce nurse turnover which costs Pennsylvania hospitals many millions of dollars annually.
Aiken also provided evidence in the hearing that Pennsylvania has a sufficiently large supply of nurses to meet the standards set by House Bill 106. She said Pennsylvania has a larger supply of nurses per 1,000 residents than all but five other states and Washington, D.C., and a significantly larger supply of nurses than California which has had mandated minimum hospital nurse staffing for 20 years.
“Impossible and Dangerous Workloads”
“The root cause of nurse burnout and turnover is impossible and dangerous workloads and setting a safe nurse staffing level will bring more nurses back to the hospital bedside,” said Aiken.
“The common finding in all our policy outcomes research on nurse staffing,” said Aiken, “is that there is significant variation across hospitals in nurse staffing adequacy with substantial adverse outcomes for the public and that establishing mandated minimum safe hospital nurse staffing standards saves lives and money. Further delays in mandating safe nurse staffing in hospitals are not in the public’s interest and elected officials should act now on the basis of the evidence.”

Editor, Digital Publications
More ldi news.

Population Health
Why Health Privacy Online Is a Myth
Google Knows More About Your Health Than Your Mom, LDI Experts Explain. And Here’s What Can Be Done About It
- Nancy Stedman

How Can We Improve Telemedicine for Patients with Gynecologic Cancer?
Fewer Than 30% of Patients Used Telehealth Even During the Pandemic
- Chris Tachibana, PhD, MS

Eileen Lake and Salimah Meghani Named to International Nurse Researcher Hall of Fame
Cited for Their Work’s Significant Impact on Nursing and Patient Care

Transportation Remains a Big Barrier to Health Care
Caregivers Should Screen for It and Have Options Available, LDI Experts Say
- Mackenzie Bolas

Health Equity
Despite Broad Efforts, U.S. Health Equity Gap Continues to Grow
José Escarce’s Presentation at LDI Lecture Series and Penn Medicine Health Equity Week Conference

Doctors, Nurses, and Managers Received Wage Hikes After Medicaid Expansion While Lower-Paid Workers Did Not
Data From 46 States Suggests No Wage Gains Among Lower-Wage Health Care Workers
- Miles Meline, MBE
American Nurses Association Backs Nurse-Patient Staffing Ratios

- The ANA recently confirmed its support for nurse-to-patient ratio laws.
- Lower nurse-to-patient ratios are associated with both lower patient mortality and lower rates of nurse burnout and turnover.
- A commitment to advocacy from nurses and organizations can help ensure nurse-to-patient ratio legislation is passed.
The American Nurses Association (ANA) recently released a statement announcing its support of nurse-to-patient ratio laws , including one currently working through the halls of Washington.
The legislation, known as the Nurse Staffing Standards for Hospital Patient Safety and Quality Care Act , would establish minimum nurse-to-patient ratios in every hospital across the country. While a few states have already implemented safer nurse staffing laws , this bill would be the first legislation of its kind to be passed on the federal level.
“Inadequate staffing standards exacerbate the work environment challenges nurses already experience, such as workplace violence, burnout, barriers to practice, and attrition,” the ANA told NurseJournal in an email. “We convened a nurse staffing task force this year that crafted a definition of appropriate staffing, which is a dynamic process that aligns the number of nurses, their workload, expertise, and resources with patient needs in order to achieve quality patient outcomes within a healthy work environment. Safe staffing standards and a healthy work environment have the potential to improve nurse and patient outcomes.”
The ANA’s stance is also backed by research. Recent studies have confirmed that lower nurse-to-patient ratios are directly associated with lower patient mortality rates. In other words, safe staffing ratios save lives.
Are Mandated Ratios the Solution to the Nurse Staffing Crisis?
Additional research has proven that high nurse-to-patient ratios result in increased rates of burnout and job dissatisfaction among nurses, which ultimately results in nurse turnover and worsened staffing shortages. In one ANA study , a staggering 89% of nurses admitted that their place of employment was short-staffed.
“Enforceable nurse-to-patient ratios can significantly support nurses particularly if they recognize key factors such as patient acuity, intensity of the unit practice setting, and nurses’ competency,” ANA officials told NurseJournal. “However, ratios alone will not solve this national crisis. ANA urges leaders and policymakers to work towards eliminating mandatory overtime, advancing workplace violence prevention plans, increasing the transparency of nurse reimbursement, and advocating for education funding to support and grow the nursing pipeline. ANA views minimum nurse staffing ratios as one critical aspect to solving the nursing crisis and supports the rights of nurses to advocate for themselves.”
It’s clear that inadequate staffing has a direct correlation to the nursing shortage as more nurses continue to leave the bedside. In addition to nurses leaving the bedside in record numbers , staffing concerns are a primary reason for the widespread surge in nursing strikes across the country. While mandated staffing ratios alone are unlikely to solve the nursing shortage, research suggests they are a worthwhile step in the right direction.
ANA Advocacy Initiatives for Safe Staffing
Legislation and politics are often complicated, to say the least, and nurse staffing regulations are no exception. It can take months or even years for legislation to become law. In this case, that delay could be detrimental to both nurses and patients.
The ANA believes that nursing expertise can play a crucial role in the development of health policy, explaining to NurseJournal:
In addition to supporting the Nurse Staffing Standards for Hospital Patient Safety and Quality Care Act, ANA continues to engage Congressional leaders, the Centers for Medicare & Medicaid Services (CMS) and other key stakeholders to refine approaches to implementing staffing standards. Additionally, ANA launched a Nurse Staffing Think Tank and Task Force and published practice and policy solutions to help end the nurse staffing crisis.
The ANA also encouraged nurses to contact their elected officials in Congress and ask them to support the legislation. The bill currently has 84 cosponsors in the House and seven in the Senate .
What Other Organizations Support Federal Staffing Ratio Laws?
In addition to the ANA, other organizations have announced their support for mandated nurse-patient ratio laws. For example, the American Association for Critical Care Nurses and the U.S. Department of Health and Human Services have both released statements regarding their stance on safe staffing standards. Leaders from several different nursing unions have also endorsed the legislation .
Staffing shortages are one of the most difficult challenges nurses face today. The ongoing staffing crisis affects nurses and the patients they care for. A commitment to advocacy is a critical part of ensuring meaningful legislation is passed so that nurses can perform their jobs safely and effectively.
American Nurses Association Supports the Nurse Staffing Standards for Hospital Patient Safety and Quality Care Act . (2023). ANA
Chen Y, et al. (2019). Patient–Nurse Ratio is Related to Nurses’ Intention to Leave Their Job through Mediating Factors of Burnout and Job Dissatisfaction . NIH
Lasater K, et al. (2021). Patient outcomes and cost savings associated with hospital safe nurse staffing legislation: an observational study . (2021). NIH
NCSBN Research Projects Significant Nursing Workforce Shortages and Crisis . (2023). NCSBN
Pulse on the Nation’s Nurses Survey Series: COVID-19 Two-Year Impact Assessment Survey . (2022). American Nurses Foundation
You might be interested in

Nurse-to-Patient Staffing Ratio Laws and Regulations by State
Nurse-to-patient ratios vary by state. Find out which states have laws and regulations in place for safe staffing ratios.

The Benefits of Nurse-to-Patient Staffing Ratio Laws and Regulations
Mandated staffing ratios are a proven way to ensure patients get the care they need. Find out how nurse-to-patient ratios can improve healthcare.

The Bipartisan Primary Care Act: Everything We Know, Including How it Could Affect Nurses
The Bipartisan Primary Care Act addresses shortages in healthcare professions. Discover how this bill would impact nurse training.
American Profession Guide
Nurse-to-patient ratios: what they mean and why they matter.
Last Updated on November 1, 2023
Introduction
In healthcare settings, nurse-to-patient ratios play a crucial role in ensuring quality care and patient safety. Proper staffing levels impact patient outcomes.
The importance of nurse-to-patient ratios in healthcare settings
Nurse-to-patient ratios are vital as they directly impact the level of care patients receive. When there are sufficient numbers of nurses, they can provide adequate attention, monitoring, and interventions.
Overview of the blog post content
This blog post will delve into the significance of nurse-to-patient ratios and how they affect patient care. We will explore the benefits of appropriate staffing and the risks of understaffing. Additionally, we will discuss the role of legislation in regulating nurse-to-patient ratios and highlight the importance of advocacy in this area.
By understanding the impact of nurse-to-patient ratios, healthcare professionals can advocate for safer staffing levels and improve patient outcomes. Stay tuned for more insights in the upcoming sections of this blog post.
Definition of nurse-to-patient ratios
Nurse-to-patient ratios refer to the number of patients assigned to a single nurse in a healthcare setting.
These ratios are often used as a measure of staffing levels and workload management. For example, a ratio of 1:5 suggests that one nurse is responsible for five patients.
Explanation of what nurse-to-patient ratios mean
Nurse-to-patient ratios indicate the level of individual attention patients can expect to receive from nurses.
Lower ratios generally imply more personalized care and increased availability of nurses for each patient.
Higher ratios, on the other hand, may signal potential compromises in patient safety and quality of care.
Importance of maintaining appropriate ratios for patient safety and quality of care
Maintaining appropriate nurse-to-patient ratios is crucial for ensuring patient safety and quality of care.
When ratios are too high, nurses may be overwhelmed with excessive workloads, increasing the risk of errors and adverse events.
Conversely, adequate ratios allow nurses to properly monitor, assess, and meet the individual needs of each patient.
By ensuring appropriate ratios, healthcare organizations can enhance patient outcomes and overall satisfaction.
Here are some key reasons why nurse-to-patient ratios matter:
- Improved patient safety: Lower ratios enable nurses to promptly identify and respond to patient care needs, reducing the likelihood of medical errors and adverse events.
- Better quality of care: Adequate ratios allow nurses to provide individualized care and spend more time with each patient, resulting in improved patient outcomes and comfort.
- Reduced nurse burnout: When ratios are balanced, nurses are less likely to experience extreme workloads, leading to decreased burnout and increased job satisfaction.
- Enhanced communication and collaboration: Appropriate ratios facilitate effective communication and collaboration among healthcare professionals, promoting coordinated patient care.
- Quick response in emergencies: Lower ratios ensure nurses can promptly attend to emergencies and provide immediate life-saving interventions when needed.
It is important to note that nurse-to-patient ratios should not be viewed as a one-size-fits-all solution.
Factors such as patient acuity, complexity of care required, and nurse skill level should also be considered in determining appropriate ratios.
Healthcare organizations must carefully evaluate these factors to establish ratios that optimize patient safety, quality of care, and nursing resources.
Additionally, ongoing monitoring and adjustment of ratios based on patient needs and nurse workload are essential.
By recognizing the significance of nurse-to-patient ratios and consistently maintaining appropriate levels, healthcare providers can ensure optimal patient outcomes while supporting their nursing staff.
Historical Perspective on Nurse-to-Patient Ratios
In order to understand the significance of nurse-to-patient ratios today, it is important to examine the historical context in which these ratios have evolved.
Overview of How Nurse Staffing Used to be Managed in the Past
Decades ago, nurse staffing was often based on outdated and ineffective methods that did not prioritize patient safety.
- Hospitals and healthcare facilities relied heavily on cost-saving measures and understaffed nursing units.
- Nurse workloads were often overwhelming, leading to increased burnout rates and compromised patient care.
- Staffing decisions were frequently made based on financial constraints rather than patient needs.
- Nurses were expected to care for a large number of patients, often stretching themselves too thin.
- The lack of standardized ratios meant that nurses had to handle an excessive workload and were unable to provide adequate attention to each patient.
The Impact of Nursing Shortages on Ratios
Nursing shortages have had a significant impact on nurse-to-patient ratios. In times of shortage:
- The number of available nurses is insufficient to meet the needs of the patient population.
- Healthcare facilities are forced to increase patient loads on each nurse, potentially compromising patient safety.
- Nurses become overwhelmed and may experience increased levels of stress and fatigue.
- Quality of patient care can suffer, as nurses struggle to provide adequate attention to all patients.
- Nursing professionals may choose to leave the field, exacerbating shortages and creating a vicious cycle.
Why Nurse-to-Patient Ratios Matter Today
Nurse-to-patient ratios have a direct impact on patient outcomes and the overall quality of healthcare provided. The importance of these ratios lies in:
- Patient Safety: Adequate nurse staffing ensures that each patient receives the attention and care they deserve, reducing the risk of medical errors and adverse events.
- Quality of Care: With appropriate staffing, nurses are able to dedicate sufficient time to each patient, leading to improved outcomes and patient satisfaction.
- Nurse Well-being: Reasonable workloads decrease stress and burnout rates among nurses, enhancing their job satisfaction and retention in the profession.
- Reduced Costs: Although increasing staffing levels may seem costly, it can ultimately lead to financial savings by preventing medical complications and legal issues.
- Evidence-Based Practice: Research consistently demonstrates the positive relationship between nurse-to-patient ratios and patient safety, providing a basis for implementing appropriate staffing policies.
Current Efforts to Address Nurse-to-Patient Ratios
Recognizing the crucial role of nurse-to-patient ratios in healthcare, many organizations and policymakers have taken steps to improve staffing standards. These efforts include:
- Legislation: Some states have implemented laws that mandate minimum nurse-to-patient ratios in healthcare settings.
- Advocacy: Nursing associations and professional organizations actively promote safe staffing ratios and advocate for their implementation.
- Research: Ongoing studies continue to highlight the importance of appropriate nurse staffing, guiding decision-makers in creating evidence-based policies.
- Educational Initiatives: Nursing schools emphasize the significance of nurse-to-patient ratios in preparing future nurses and equipping them to advocate for safe staffing.
- Collaboration: Healthcare institutions and nursing leaders collaborate to develop comprehensive strategies for managing nurse staffing and achieving optimal ratios.
Nurse-to-patient ratios have come a long way from the ineffective and unsafe practices of the past. Recognizing their historical context allows us to appreciate the significance of ensuring appropriate staffing levels in healthcare today. By prioritizing safe and adequate nurse-to-patient ratios, we can improve patient outcomes, enhance the quality of care, and support the well-being of nursing professionals.
Read: Navigating Health Insurance and Billing for U.S. Doctors
Impact of Nurse-to-Patient Ratios on Patient Outcomes
Research studies have consistently shown that the nurse-to-patient ratio has a significant impact on patient outcomes. Adequate nurse staffing levels play a crucial role in ensuring patient safety and providing quality care.
The research findings linking nurse staffing levels to patient outcomes
Several research findings have established a direct link between nurse staffing levels and patient outcomes. Studies have shown that when there are fewer nurses to attend to patients, the risk of adverse events increases significantly.
One of the largest studies conducted on this topic, known as the RN4CAST study, found that patients in hospitals with higher nurse-to-patient ratios had lower mortality rates. The study also revealed that higher nurse staffing levels were associated with reduced incidents of medication errors, falls, and hospital-acquired infections.
Examples of adverse events that can occur with inadequate ratios
Inadequate nurse-to-patient ratios can lead to a range of adverse events and negative patient outcomes. When nurses are overwhelmed with too many patients to care for, they may not be able to devote sufficient time and attention to each individual.
Medication errors are more likely to occur when nurses are rushed, stressed, or overburdened with multiple patients. These errors can have severe consequences on patient health and recovery. Ensuring an appropriate nurse-to-patient ratio can significantly reduce the risk of medication errors.
Falls are another common adverse event that can occur due to inadequate nurse-to-patient ratios. When nurses are unable to closely monitor patients, especially those who are at high risk of falling, the likelihood of falls and related injuries increases.
Hospital-acquired infections are a significant concern in healthcare settings. When nurses are stretched thin and cannot follow proper infection control protocols, the risk of transmitting infections between patients also increases.
Additionally, research has shown that higher nurse-to-patient ratios are associated with decreased patient satisfaction. When nurses are unable to provide personalized care and spend adequate time with each patient, patients may feel neglected or ignored, leading to lower satisfaction levels.
On the other hand, when nurse staffing levels are adequate, patients receive better quality care and have improved outcomes. Nurses can promptly respond to patient needs, administer medications on time, and provide necessary interventions without feeling overwhelmed.
Hospitals and healthcare organizations must prioritize appropriate nurse-to-patient ratios to promote patient safety and positive outcomes. Proper staffing not only benefits patients but also supports the well-being and job satisfaction of nurses.
Nurse-to-patient ratios have a significant impact on patient outcomes. Adequate staffing levels are essential to prevent adverse events, ensure patient safety, and maintain high-quality care. Hospitals and healthcare facilities must prioritize proper nurse staffing to provide optimal care and improve patient outcomes.
Read: The Role of Foreign-Trained Doctors in American Healthcare
Factors Affecting Nurse-to-Patient Ratios
When it comes to nurse-to-patient ratios, there are several factors that come into play. Let’s take a closer look at some of these factors and how they can influence staffing levels.
Various factors that influence ratios, such as unit type, acuity level, and nurse experience
- Different units within a healthcare facility may have different nurse-to-patient ratios.
- For example, an intensive care unit (ICU) may require a lower ratio compared to a general medical-surgical unit.
- Specialized units, such as neonatal intensive care units (NICUs) or psychiatric units, may also have specific staffing requirements.
Acuity Level
- The acuity level of patients also plays a significant role in determining nurse-to-patient ratios.
- Patients with complex medical conditions or high acuity levels may require more nursing care.
- On the other hand, patients with stable conditions and lower acuity levels may need fewer nursing resources.
Nurse Experience
- The level of experience and skill of the nursing staff can influence staffing levels.
- Experienced nurses may be able to handle a higher patient load compared to novice nurses.
- Having a mix of experienced and less experienced nurses can help achieve the appropriate balance in staffing ratios.
Variations in Staffing Levels
Due to the complex nature of healthcare environments, staffing levels can vary based on the factors mentioned above.
For example, an ICU may have a nurse-to-patient ratio of 1:2, while a general medical-surgical unit may have a ratio of 1:5. This is because ICU patients require more intensive monitoring and care compared to general unit patients.
Similarly, a unit with higher acuity patients may have a lower nurse-to-patient ratio compared to a unit with lower acuity patients. This ensures that the complex needs of high acuity patients are met effectively.
Nurse experience also plays a vital role in staffing levels. Units with a higher number of experienced nurses may be able to manage larger patient loads while still delivering quality care. Conversely, units with less experienced nurses may require lower nurse-to-patient ratios to ensure patient safety.
Additionally, the availability of resources, such as support staff, technological tools, and adequate supply of medical equipment, can also impact staffing levels. Lack of resources may necessitate lower nurse-to-patient ratios to ensure optimal patient care.
Nurse-to-patient ratios are influenced by various factors, including unit type, acuity level, and nurse experience. These factors contribute to the variations in staffing levels across different healthcare settings. It is crucial to strike a balance that ensures patient safety while also considering the workload and capabilities of nursing staff.
Read: U.S. Medical Malpractice: Myths and Realities

Current guidelines and recommendations for nurse-to-patient ratios
- The American Nurses Association (ANA) suggests a maximum ratio of 1 nurse to 4 patients.
- The National Institute for Occupational Safety and Health (NIOSH) recommends a ratio of 1 nurse to 2 patients.
- The World Health Organization (WHO) advocates for a ratio of 1 nurse to 6 patients.
Overview of national and international organizations’ guidelines on ratios
- The ANA is a leading professional organization that sets standards for nursing practice in the United States.
- NIOSH is a federal agency that focuses on occupational safety and health, including guidelines for nurse staffing.
- The WHO is an international organization that provides health-related guidance and promotes quality healthcare worldwide.

How these guidelines can vary based on the type of healthcare setting
The recommended nurse-to-patient ratios can vary depending on the type of healthcare setting:
In general medical-surgical units, the ANA recommends a ratio of 1 nurse to 4 patients.
For intensive care units (ICUs), the ratio decreases to 1 nurse for every 1-2 patients.
Emergency departments
The ANA suggests a ratio of 1 nurse per 3-4 patients in emergency departments.
Due to the unpredictable nature of emergencies, optimal ratios may vary depending on the circumstances.
Long-term care facilities
The ratio in long-term care facilities can range from 1 nurse for every 5-10 residents, based on their acuity level.
Highly skilled nursing homes may have lower ratios compared to assisted living or residential care facilities.
Home healthcare
For home healthcare, the ANA recommends a ratio of 1 nurse to 1 patient to ensure personalized care.
This allows nurses to provide comprehensive assessments and interventions in the comfort of patients’ homes.
Outpatient clinics
Outpatient clinics often have a higher volume of patients, and the ratio can be around 1 nurse to 6-8 patients.
This allows nurses to efficiently manage the diverse needs of patients seeking outpatient care.
Specialized units
In specialized units like operating rooms or labor and delivery, the ratio may vary widely.
These units often require highly skilled nurses who can handle complex procedures and emergencies.
It is essential to note that these guidelines serve as a framework and may need to be adjusted based on individual patient needs and nurse experience. Adequate nurse staffing is crucial for patient safety, outcomes, and overall healthcare quality. Striking the right balance in nurse-to-patient ratios is a continuous challenge that healthcare organizations and policymakers strive to achieve.
Read: Telemedicine: The Future of Healthcare in the USA?
The Role of Nurse-to-Patient Ratios in Nurse Job Satisfaction and Burnout
The importance of nurse-to-patient ratios cannot be overstated when it comes to nurse job satisfaction and burnout. When ratios are inadequate, it not only affects patient care but also significantly impacts the well-being of nurses themselves.
The Relationship between Ratios and Nurse Workload/Stress Levels
The nurse-to-patient ratio directly affects the workload and stress levels experienced by nurses. When the ratio is high, nurses are often overwhelmed with multiple responsibilities, leading to increased stress and feelings of being overworked.
Explanation of How Inadequate Ratios Can Contribute to Dissatisfaction and Burnout Among Nurses
- Increased nurse workload: Inadequate ratios result in nurses having to care for more patients simultaneously, leading to a heavier workload. This increased workload often negatively impacts job satisfaction and contributes to burnout.
- Reduced availability for individualized care: With insufficient ratios, nurses struggle to provide individualized care to each patient. This results in dissatisfaction as nurses are unable to fulfill their professional obligations and deliver quality care.
- Higher stress levels: Inadequate ratios amplify stress levels among nurses. The constant pressure and demands arising from an unbalanced nurse-to-patient ratio can lead to physical and emotional exhaustion, ultimately causing burnout.
- Poor patient outcomes: When nurses are stretched thin due to inadequate ratios, patient outcomes tend to suffer. Nurses may not have enough time to devote to each patient, leading to increased medical errors and preventable complications, further exacerbating nurse dissatisfaction and burnout.
Benefits of Adequate Nurse-to-Patient Ratios
- Enhanced ability to deliver high-quality care
- Improved patient safety and reduced medical errors
- Opportunity to establish meaningful patient-nurse relationships
- Decreased stress levels and job burnout among nurses
- Increased job satisfaction and overall morale within nursing teams
Consequences of Inadequate Nurse-to-Patient Ratios
- Decreased patient satisfaction and trust in healthcare systems
- Increased nurse turnover rates and difficulty in retaining experienced nurses
- Potential compromise of patient outcomes and overall quality of care
- Higher healthcare costs as a result of preventable complications
- Negative impact on the reputation of healthcare facilities, leading to reduced patient admissions
Nurse-to-patient ratios play a crucial role in nurse job satisfaction and burnout. Inadequate ratios contribute to dissatisfaction, burnout, and increased stress levels among nurses. Additionally, inadequate ratios hinder the delivery of high-quality patient care, leading to negative consequences for both patients and healthcare organizations. It is essential for healthcare systems to recognize the significance of appropriate nurse-to-patient ratios and work towards implementing measures that ensure the well-being of nurses and the provision of quality care.
The Advocacy for Appropriate Nurse-to-Patient Ratios
Nurse-to-patient ratios refer to the number of nurses assigned to provide care for a specific number of patients. In recent years, there has been a growing emphasis on advocating for appropriate nurse-to-patient ratios in healthcare settings. This blog section will explore the significance of this advocacy, as well as provide an overview of the initiatives and organizations advocating for safe staffing ratios.
Overview of Initiatives and Organizations Advocating for Safe Staffing Ratios
Several initiatives and organizations have recognized the importance of safe nurse-to-patient ratios and have actively advocated for improvements in staffing. These initiatives aim to ensure better patient outcomes, enhance the quality of care, and support the well-being of nurses.
One such organization is the American Nurses Association (ANA), which has been at the forefront of fighting for safe staffing ratios. The ANA has developed guidelines and standards to promote appropriate staffing levels and has been actively lobbying for legislation to enforce these ratios.
Another prominent organization is the National Nurses United (NNU). NNU has been a strong advocate for safe nurse-to-patient ratios, recognizing that understaffing can lead to increased patient complications and nurse burnout. They have organized various campaigns and protests to raise awareness about the importance of appropriate staffing levels.
In addition to these organizations, individual nurses themselves play a crucial role in advocating for changes in nurse-to-patient ratios. Nurses are the frontline providers of care and witness firsthand the impacts of understaffing. Their involvement in advocating for safe staffing ratios brings a unique perspective and lends credibility to the cause.
The Importance of Nurse Involvement in Advocating for Changes
Nurses are the backbone of healthcare systems, and their involvement in advocating for appropriate nurse-to-patient ratios is vital. They possess valuable insights into the challenges faced in their daily practice due to inadequate staffing levels.
When nurses articulate their concerns and advocate for safe staffing ratios, they amplify the voices of both patients and healthcare providers. Nurses understand the potential risks and consequences of inadequate staffing, and their involvement brings a human element to the advocacy efforts.
Research has consistently shown that appropriate nurse-to-patient ratios directly impact patient outcomes. Adequate staffing results in reduced mortality rates, decreased hospital-acquired infections, and improved overall patient satisfaction. These positive outcomes are directly linked to the presence of an adequate number of nurses to deliver high-quality care.
Furthermore, optimal nurse-to-patient ratios also benefit nurses themselves. Adequate staffing reduces nurse burnout, promotes job satisfaction, and improves retention rates. By advocating for safe staffing ratios, nurses are not only advocating for their patients but also for their own well-being.
Advocating for appropriate nurse-to-patient ratios is crucial for ensuring quality healthcare delivery. Initiatives and organizations like the American Nurses Association and National Nurses United have been at the forefront of this advocacy. However, the involvement of individual nurses is equally important in promoting changes for safe staffing ratios. By working together, healthcare professionals and organizations can advocate for improvements that will benefit both patients and nurses, ultimately leading to better healthcare outcomes for all.
In this blog post, we discussed the significance of nurse-to-patient ratios in healthcare settings. We learned that these ratios are crucial for patient safety and quality of care.
Firstly, we explored the key points that highlight the importance of nurse-to-patient ratios. We discussed how higher ratios can lead to increased patient mortality rates, medication errors, and burnout among nurses.
Next, we examined the impact of understaffing and why proper staffing levels are essential. We saw how adequate nurse-to-patient ratios help in reducing wait times, improving patient satisfaction, and ensuring timely interventions.
Furthermore, we highlighted the benefits of appropriate nurse-to-patient ratios. These ratios contribute to better patient outcomes, decreased healthcare costs, improved nurse morale, and increased job satisfaction.
It is worth noting that nurse-to-patient ratios also play a role in the recruitment and retention of nurses. When nurses feel supported and able to provide high-quality care, they are more likely to remain in their positions and contribute to a positive work environment.
Nurse-to-patient ratios are not mere numbers but have a significant impact on healthcare outcomes. By maintaining appropriate ratios, healthcare organizations can ensure safer and more effective patient care, enhance nurse well-being, and ultimately improve the overall quality of the healthcare system.
- Navigating the Ethical Challenges of Nursing in America
- Telehealth Nursing: The Future of Patient Care in the USA?
You May Also Like

The Journey: From Medical School to Residency in the USA
Innovative Pharmacy Services: US Case Studies and Insights

ADA’s Role in Shaping American Dentistry Today
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Registered Nurse-to-Patient Ratios by State Guide [2024]

Table of Contents
Find your state’s current nurse-to-patient ratios.
You’ve seen nurses protest, demanding better working conditions. You’ve read the headlines announcing the introduction of numerous bills aiming to regulate nurse-to-patient ratios once and for all.
Have these efforts borne fruit?
What is the current state of RN-to-patient staffing ratio laws?
This ultimate guide to registered nurse-to-patient ratios provides specific regulations by state to help you understand the current laws in your area.
Why Are Nurse-to-Patient Ratios Important?
With physicians spending only 30 to 45 minutes a day with even critically ill patients, nurses stand out as essential healthcare providers, responsible for monitoring patients’ status, providing potentially lifesaving care, and acting as liaisons between physicians, pharmacists, patients, their families, and all other members of the healthcare team.
However, the quality of care nurses are able to provide is directly related to the number of patients they must take care of.
If nurses must care for more patients than they realistically can, considering the setting and level of acuity of their patients, their ability to provide safe care naturally decreases. For example, a British study found that a higher number of patients per nurse was strongly associated with episodes of missed nursing care. The consequences of missed nursing care for patients include medication errors, infections, falls, pressure injuries, readmissions, and failure to rescue.
Furthermore, a systematic review published in 2007 found that a higher RN-to-patient ratio was associated with:
- lower hospital-related mortality,
- death from complications,
- cardiac arrest, and
- healthcare-associated infections.
More recent studies have supported these findings with evidence of associations between staffing ratios and healthcare-associated infections, medication errors, and patient falls.
What Are Safe Nurse Staffing Ratios?
A nurse staffing ratio is the minimum number of nurses required to provide nursing care safely. Nurse staffing ratios can vary significantly from one healthcare setting to the next. For example, a safe nurse-to-patient ratio in an intensive care unit (ICU) differs from a safe ratio in a long-term care setting .
The Nursing Home Reform Act of 1987 required that nursing homes participating in Medicare and Medicaid have a minimum of eight hours per day of registered nursing (RN) service and 24 hours per day of licensed nursing (LN) service. Additionally, federal regulations require nursing homes to provide “sufficient nursing staff to attain or maintain the highest practicable...well-being of each resident.” However, the Nursing Home Reform Act did not mandate a specific staff-to-resident ratio or minimum hours per resident day for resident care.
Fast forward to September 1, 2023.
The Centers for Medicare & Medicaid Services (CMS) issued the Minimum Staffing Standards for Long-Term Care (LTC) Facilities and Medicaid Institutional Payment Transparency Reporting proposed rule. This proposed rule establishes comprehensive nurse staffing requirements to hold nursing homes accountable for providing safe and high-quality care daily for the over 1.2 million people in Medicare- and Medicaid-certified long-term care facilities.
The rule’s three main staffing proposals are as follows:
- Minimum nurse staffing standards of 0.55 hours per resident day (HPRD) for registered nurses and 2.45 HPRD for nurse aides (NAs)
- A requirement to have an RN onsite 24 hours a day, seven days a week
- Enhanced facility assessment requirements
What Are the Nurse-to-Patient Staffing Ratios by State?
In 2003, the Office of Disability, Aging and Long-Term Care Policy of the U.S. Department of Health and Human Services identified 36 states with established minimum nursing staff ratios in nursing facilities based on a review of published and unpublished literature on state standards.
According to the American Nurses Association , as of March 2022, only 16 states addressed hospital nurse staffing through either laws or regulations. Although 2022 may seem pretty close in the past, nurse-to-patient staffing ratios have come a long way since then, with additional states mandating specific ratios and others requiring disclosure and/or reporting of actual ratios. In numerous states, bills have been introduced to address this pressing issue, so stay tuned for updates on nurse-to-patient staffing ratios in your state.
Find your state in the following table to learn about RN-to-patient staffing ratio laws that may apply to you.
RN-to-Patient Staffing Ratios by State
How can facilities maintain safe nurse-to-patient ratios.
Federal and state regulations mandating safe nurse-to-patient ratios only partially solve staffing challenges. Many hospitals and other healthcare facilities struggle to hire and retain sufficient nursing professionals to meet their patients’ or residents’ needs.
In this context, PRN nursing jobs can be valuable solutions for immediate problems. Short-staffed hospitals and other facilities can turn to PRN nurses to maintain safe nurse-to-patient ratios. Nurses also benefit from this work model since PRN jobs offer clinicians flexibility and high hourly pay.
Nursa offers healthcare facilities and nurses a way to connect directly and reach the common goal of safe nurse-to-patient ratios. Within minutes, you can create an account to begin posting or picking up PRN nursing jobs .
Are you also interested in staffing ratios for certified nursing assistants (CNAs)? Read our CNA-to-Patient Staffing Ratios by State Guide .
- Centers for Medicare & Medicaid Services
- American Nurses Association

Laila is a contributing copywriter and editor at Nursa who specializes in writing compelling long-form content about nursing finances, per diem job locations, areas of specialization, guides, and resources that help nurses navigate their career paths.
Related Blog Posts
![research on nurse patient ratio Registered Nurse-to-Patient Ratios by State Guide [2024]](https://assets-global.website-files.com/63a1cbc81b0e903002cf9cec/65ccb76a748494b7852f63f4_rn%20staffing%20ratio.jpg)
Choose Multiple PRN Shifts on Your Schedule
Nursa isn't just about finding a job ; it's about crafting your ideal work schedule by selecting shifts. Once you create a Nursa profile, you will experience the convenience of scheduling shifts in real-time.
See More Shifts and Apply Now
Explore and find where you would like to work
Pick Up a Job Today
Find per diem PRN job opportunities in your area . High paying CNA, LPN and RN and many more are now available now.
Post Your Jobs Today
Facilities who use Nursa fill 3 times as many open per diem shifts , on average, compared to trying to fill the shifts themselves.

Download the App Now
- Open access
- Published: 08 April 2024
Patient satisfaction with preoperative nursing care and its associated factors in surgical procedures, 2023: a cross-sectional study
- Bizuayehu Atinafu Ataro 1 ,
- Temesgen Geta 2 ,
- Eshetu Elfios Endirias 1 ,
- Christian Kebede Gadabo 3 &
- Getachew Nigussie Bolado 1
BMC Nursing volume 23 , Article number: 235 ( 2024 ) Cite this article
153 Accesses
Metrics details
To enhance patient satisfaction, nurses engaged in preoperative care must possess a comprehensive understanding of the most up-to-date evidence. However, there is a notable dearth of relevant information regarding the current status of preoperative care satisfaction and its impact, despite a significant rise in the number of patients seeking surgical intervention with complex medical requirements.
To assess patient satisfaction with preoperative nursing care and its associated factors in surgical procedures of, 2023.
A cross-sectional study was conducted, and the data was collected from the randomly selected 468 patients who had undergone surgery during the study period. The collected data was entered into Epidata version 3.1 and analyzed using SPSS version 25 software.
The complete participation and response of 468 participants resulted in a response rate of 100%. Overall patient satisfaction with preoperative nursing care was 79.5%. Sex (Adjusted odds ratio (AOR): 1.14 (95% confidence interval (CI): 0.21–2.91)), payment status for treatment (AOR: 1.45 (95% CI: 0.66–2.97)), preoperative fear and anxiety (AOR: 1.01, 95% CI: 0.49–2.13)), patient expectations (AOR: 3.39, 95% CI: 2.17–7.11)), and preoperative education (AOR: 1.148, 95% CI: 0.54–2.86)) exhibited significant associations with patient satisfaction with preoperative nursing care.
It is important to exercise caution when interpreting the level of preoperative nursing care satisfaction in this study. The significance of preoperative nursing care satisfaction lies in its reflection of healthcare quality, as even minor deficiencies in preoperative care can potentially lead to life-threatening complications, including mortality. Therefore, prioritizing the improvement of healthcare quality is essential to enhance patient satisfaction.
Peer Review reports
Preoperative care encompasses the provisions given prior to surgery, wherein the patient’s unique requirements are considered to undertake physical and psychological preparations in anticipation of the procedure [ 1 ]. This phase commences upon the patient’s admission to the hospital or surgical facility and extends until the commencement of the actual procedure [ 1 , 2 , 3 , 4 ]. The primary emphasis in preoperative preparation should lie in the advancement of techniques aimed at mitigating the emotional distress experienced by surgical patients [ 5 ]. In this context, nurses play a crucial role in formulating, developing, expanding, and implementing interventions and modifications [ 5 , 6 ].
The primary goal of a healthcare system is to ensure the provision of medical care that is of the utmost quality and safety [ 7 ]. In this context, patient safety has emerged as a paramount concern and is currently placed at the forefront of priorities [ 8 , 9 ]. A systematic review conducted in Saudi Arabia and Turkey concluded that preoperative nursing assessment plays a vital role in mitigating preoperative complications by alleviating anxiety and enhancing patients’ understanding of the surgical procedure. This, in turn, has a substantial positive impact on patient satisfaction [ 10 , 11 ]. The review also emphasized the necessity of nurses receiving proper training and education in preoperative assessment, as the absence of adequately trained nursing staff elevates patient anxiety levels and renders them susceptible to potential complications [ 2 , 10 ].
Patient satisfaction is defined as a subjective reaction to the context, process, and result of the service experience one has received [ 12 , 13 ]. The measurement of quality is closely linked to the satisfaction levels expressed by patients regarding the care they have received [ 14 , 15 ]. Both the practice environment and the personal characteristics of nurses serve as significant indicators of the quality of patient care [ 16 ]. Enhancing working conditions and achieving improved patient outcomes, including reduced mortality rates, are facilitated by a positive relationship between the work environment attributes of nurses and their levels of proficiency and personal capabilities [ 17 ]. Additionally, various aspects of the workplace, such as the physical setting, working hours, and the level of fatigue among nursing staff, have been found to influence the safety and quality of patient care [ 18 ].
Comprehensive nursing interventions should be implemented throughout the entire perioperative phase to prevent complications and adverse events in the surgical domain [ 19 ]. Although the impact of perioperative nursing interventions on patient health outcomes may not be fully comprehended, it is substantial in its significance [ 20 ]. Through the provision of care during the postoperative period, nurses can effectively mitigate the occurrence of adverse events, even though certain studies have identified nurses’ workload and time constraints as predominant barriers to effective nurse-patient communication [ 21 , 22 , 23 , 24 ]. Preoperative nursing assessment plays a pivotal role in delineating and discerning the patient’s risk factors throughout their perioperative care, extending beyond the confines of the surgical procedure itself [ 25 , 26 ].
To optimize patient care and enhance postoperative outcomes, it is imperative for nurses engaged in patient assessment and preoperative care to possess comprehensive knowledge and understanding of the latest research in this field [ 27 ]. Throughout the preoperative phase, nurses provided comfort, guidance, and rehabilitation to the patients. However, they failed to involve the patients in their treatment [ 28 , 29 ]. An unfortunate number of patients endured minor injuries due to improper utilization of theater equipment, such as diathermy devices, along with inadequate implementation of safety precautions by the nursing staff during the surgical procedure [ 28 , 30 ]. Furthermore, patients were left feeling bewildered and unsettled due to the nurses’ deficient communication [ 28 , 31 ].
The perioperative environment possesses distinctive characteristics, encompassing intricate clinical care delivered by specialized teams, substantial costs, utilization of advanced technologies, and a vast array of challenging-to-manage resources [ 30 , 32 ]. These factors can contribute to the development of highly intricate settings prone to adverse events concerning patient safety [ 32 , 33 ]. Medication errors, omissions, patient misidentification, and surgical site misidentification are among the various types of mistakes that can occur during surgical procedures [ 34 ]. Birmingham-based research showcased that reducing waiting times, enhancing patient satisfaction, and upholding the efficacy of clinical services were the outcomes of evaluating patient load and the delivery system within the clinic [ 35 , 36 ]. To optimize patient satisfaction, nurses involved in preoperative care must possess up-to-date knowledge and understanding of the most recent research [ 27 ]. Despite the significant increase in the number of patients requiring surgery, with complex medical needs, a scarcity of pertinent data exists regarding the satisfaction levels and impacts associated with preoperative care.
Studies conducted in Ethiopia showed varying levels of patient satisfaction with preoperative nursing care in surgical procedures. The cross-sectional study carried out in Addis Ababa, Western Amhara referral hospitals, University of Gondar Comprehensive Specialized Hospital, East Amhara referral hospitals and Gamo and Gofa zone showed that the patient satisfaction with preoperative care ranges from 36.6 to 84% [ 12 , 37 , 38 , 39 , 40 ]. According to the study conducted at Sohag University, the overall satisfaction score of patients who underwent surgery was determined to be 61.9% [ 41 ].
Various factors play key roles in influencing patient satisfaction with preoperative nursing care, both related to the hospital and nursing environment (such as ward/unit dynamics, length of hospitalization, surgical specialization, waiting times, nurse responsiveness), patient and family characteristics (including financial status, prior hospitalizations, service expectations, health conditions, procedure types, complications, discharge plans, anxiety levels, illness duration, family size), and preoperative education can seriously influence satisfaction levels of patients with preoperative nursing care. Additionally, sociodemographic factors like gender, age, income, residence, marital status, religion, ethnicity, education level, and occupation may also significantly impact patient satisfaction [ 1 , 10 , 12 , 32 , 37 , 38 , 39 , 40 , 41 , 42 ].
Enhancing patient satisfaction with preoperative nursing care is vital for patient-centered healthcare. This study investigates the factors influencing patient satisfaction in surgical procedures, aiming to improve care quality. By identifying areas for enhancement, the research informs healthcare practices, potentially leading to better patient experiences and outcomes. Contributing to the existing literature, this contemporary study provides updated insights into patient preferences, guiding efforts toward optimized preoperative care delivery and improved surgical outcomes. This research can also pave the way for advancements in patient-centered care approaches and potentially lead to positive impacts on healthcare outcomes and patient experiences in surgical settings.
Most of the previous research conducted in Ethiopia has primarily focused on evaluating patient satisfaction with the overall hospital services. However, this particular study honed in on specifically examining the satisfaction levels of preoperative nursing care services. This focus was chosen due to the profound impact that such care has on surgical outcomes and subsequent postoperative recovery. Notably, this study stands as the first of its kind within our study area; as far as we know, no prior study of this nature has been conducted. It is also worth noting that while some previous studies had utilized nurses as study participants, this study appropriately selected patients, as they possess indispensable insights into the quality of nursing care and ultimately determine the level of satisfaction experienced. Additionally, this study introduced previously unstudied variables, such as patient flow per shift and nurses’ willingness to listen and respond to questions, which hold the potential for significant associations with satisfaction levels regarding preoperative nursing care services. Therefore, this study aimed to comprehensively assess patient satisfaction with preoperative nursing care and its associated factors in surgical procedures.
Methods and materials
Study area and period.
This study was carried out in the Wolaita Zone, located 329 km away from Addis Ababa, the capital of Ethiopia. Currently, Wolaita Sodo serves as the capital city of southern Ethiopia. Known for its high population density, the zone boasts 290 individuals per square kilometer, making it one of the most densely populated regions in the country. According to the 2021 population projection by the Central Statistical Agency of Ethiopia, the Wolaita Zone is home to a total population of 6,142,063 people residing within an area of 4,208.64 square kilometers (1,624.96 sq. mi). Within this zone, there are nine public hospitals, with Wolaita Sodo University Comprehensive Specialized Hospital being the sole specialized healthcare facility. The hospital provides a broad range of surgical services spanning multiple departments, including general surgery, orthopedic surgery, urologic surgery, obstetrics and gynecologic surgery, and maxillofacial surgery. The study was conducted from July 15 to July 30, 2023.
Study design:
Facility-based cross-sectional study was employed because it allows for the exploration of relationships between variables at a specific moment, providing valuable insights into the prevalence of patient satisfaction and associated factors concurrently.
Populations
Source population:.
All surgical patients who have undergone surgery.
The study sample:
All surgical patients that are available during a study period.
Eligibility
Inclusion criteria:.
All adult patients aged ≥ 18 years who have undergone surgery and have been admitted to a surgical, obstetrics/gynecology ward, ophthalmic, orthopedic, or other department were included.
Exclusion criteria:
Patients who sought treatment as outpatients, individuals who were severely ill and unconscious, as well as patients with known mental health issues, were excluded from the study.
Sample size determination and procedure
The sample size was determined using a formula for a single population proportion, taking into account the following assumptions: a prevalence of 52.75% for patient satisfaction with nursing care in Eastern Ethiopia [ 25 ], a confidence level of 95%, a margin of error of 5%, a nonresponse rate of 10% as follows:
n- The minimum sample size required.
P- Prevalence of satisfaction with preoperative nursing care.
d- Margin of error.
Z 𝛼 /2- Standard normal distribution at 95% confidence level
After accounting for a 10% contingency for potential non-response, the final sample size for this study amounted to 468 subjects.
Study variables
Dependent variable:.
Patients’ satisfaction.
Independent variables:
Sociodemographic variables (sex, age, monthly income, residence, marital status, religion, ethnicity, educational, occupational status); Hospital and nurse-related variables (ward/unit, length of hospital stay, surgical specialty, surgery waiting time, patient flow per shift, nurses’ willingness to listen and respond to questions); Patient and family factors (payment status, previous admission, patient service expectations, co-morbidity, surgery type, complications, discharge destination, preoperative fear and anxiety, duration of the illness, family size), and Preoperative education.
Data collection tools and procedures
The data was collected through a meticulously tested, structured, interview-administered questionnaire originally written in English and then translated into the local language, Wolaitigna, to ensure accessibility and accurate comprehension among the participants. The questionnaire was divided into six sections and was obtained from previous studies conducted in Ethiopia and other locations internationally [ 12 , 13 , 31 , 39 ]. The first part of the questionnaire contains the sociodemographic characteristics of the patients. The second part contains institution- or health facility-related variables affecting patients’ preoperative nursing care services. Items in the third and fourth sections assessed the nurse-related factors and patient- and family-related variables influencing patients’ preoperative nursing care services, respectively. One of the patient-related factors was preoperative fear and anxiety and it was measured by tools adapted from previous studies conducted in Ethiopia and Iraq [ 43 , 44 ]. The fifth part of the question contains items used to measure preoperative education containing 16 questions [ 12 ]. The final part contains items to measure the level of preoperative nursing care satisfaction among nurses. The instruments utilized to assess patient satisfaction with preoperative nursing care comprised a set of 22 Likert-scale questions. Each question was rated on a scale from 1, indicating “very unsatisfied,” to 5, indicating “very satisfied”. This tool was valid in Ethiopia and had internal consistency with Cronbach’s alpha of 0.96. The overall patient satisfaction with preoperative nursing care in surgical procedures was classified into two categories: satisfied and unsatisfied [ 12 , 31 , 37 ].. A team of four nursing professionals who held BSc degrees was specifically assigned to take on the role of data collectors. They were closely supervised by two BSc-qualified nurse professionals throughout the study, who were selected from Sodo Health Center.
Data processing and analysis
The collected data were cleaned, coded, and entered using Epidata software and exported into Statistical Package for the Social Sciences (SPSS) Version 26 to facilitate analysis. To explore the relationship between the dependent and independent variables, both bivariable and multivariable logistic regression techniques were utilized. In the bivariable logistic regression model, all independent variables with a p-value less than 0.25 were subsequently entered into the multivariable logistic regression model. The evaluation of significance relied on the adjusted odds ratio (AOR), accompanied by a 95% confidence interval (CI) and a p-value less than 0.05, allowing for meaningful interpretation of the obtained associations. Descriptive statistics, such as tables, graphs, frequencies, and percentages, were employed to provide an overview of the characteristics observed within the sample.
Data quality control
A preliminary assessment, commonly referred to as a pilot study, of the questionnaire, took place at Grace Primary Hospital, which lies outside the scope of the target hospitals. This pre-test was conducted on a subset of the sample size, comprising 5%, a week before the commencement of the actual data collection period. Based on the outcomes of the pre-test, necessary modifications were made to address issues such as unclear questions, typographical errors, and ambiguous wording. Furthermore, the reliability of the Likert-scale items was assessed using Cronbach’s alpha, yielding a coefficient of 0.82. To ensure proficient data collection, a comprehensive one-day training session was provided to the data collectors, encompassing instructions on both the data collection tool and the collection process itself. The principal investigator oversaw the data collection process and monitored its completeness, accuracy, and consistency daily. To enhance data integrity, a double-entry method was employed, involving two separate data clerks who independently entered the collected data into SPSS. The consistency of the entered data was cross-verified by comparing the two versions of the data to identify any discrepancies.
Socio-demographic characteristics of the participants
The response rate for this study was an impressive 100%. Out of the total of 468 respondents, the majority were female (55.1%), and the mean age of the participants was 34 years with a standard deviation of 8.9. Notably, a significant proportion (21.6%) fell within the age bracket of 25 to 34 years. Among the respondents, 210 (44.9%) resided in urban areas, while 258 (55.1%) hailed from rural regions. Regarding marital status, the majority (68.6%) were married, and adherents of the Protestant faith constituted more than 50% of the participants. Approximately 60% of the respondents were illiterate, and 138 (29.5%) identified themselves as farmers. Furthermore, 131 (28.0%) were engaged in the role of housewives, and 107 (22.9%) were students. Out of the total 468 respondents, 223 (47.6%) reported earning less than 1000 ETB per month (Table 1 ).
Patient satisfaction with preoperative nursing care
The overall satisfaction with preoperative nursing care among patients who have undergone surgical procedures at Wolaita Sodo University Comprehensive Specialized Hospital was 79.5% (75.4–83.6) (Fig. 1 ).
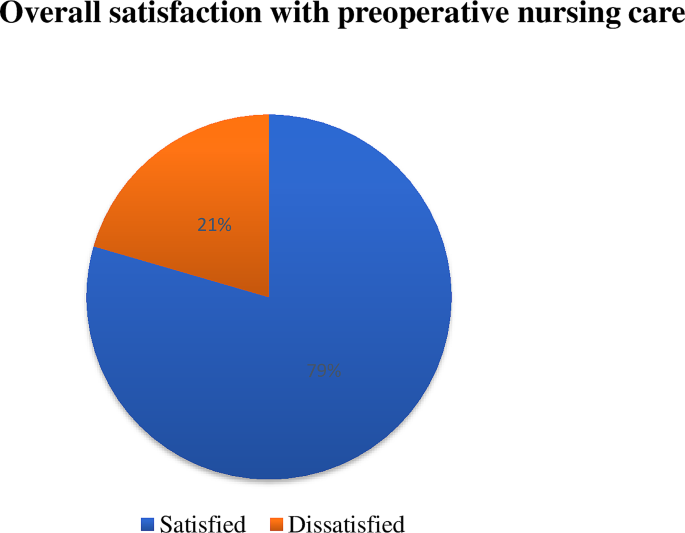
Patient satisfaction with preoperative nursing care in surgical procedures at Wolaita Sodo University Comprehensive Specialized Hospital
Variables influencing patient satisfaction with preoperative nursing care
Hospital and nurse-related variables.
Among the participants, a substantial majority (84.8%) were admitted to the surgical unit of the hospital, highlighting the prevalence of surgical cases in the study sample. In terms of the duration of hospital stay, 289 (61.8%) reported a stay of less than seven days, indicating relatively shorter periods of hospitalization. When it came to interactions with surgeons, the participants disclosed that 151 (32.2%) had contact with surgeons specializing in general surgery, while 129 (27.6%) had contact with surgeons specializing in traumatology. Regarding the waiting time for surgery, more than half of the participants (53.2%) indicated a waiting period of less than one month. Moreover, a majority of the participants (55.3%) acknowledged that there was a high number of patient or a high patient flow during their waiting period, suggesting the burden on the healthcare system. Disturbingly, 277 (59.2%) of the participants reported dissatisfaction with the nurses’ willingness to listen and respond to their concerns, indicating poor communication and responsiveness on the part of the nursing staff (Table 2 ).
Patient and family variables
Among the respondents who participated in this study, a significant proportion (61.3%) revealed that they had fewer than three family members, while 148 (31.6%) reported having four to six family members. More than half of the participants (53.4%) reported receiving free-of-charge treatment from the hospital, indicating a reliance on the hospital’s financial support. Additionally, a considerable number of respondents (63.7%) recalled previous admissions for various health issues. Similarly, 171 (63.5%) of the patients reported having co-morbidities during their initial diagnosis, further complicating their healthcare journey. A substantial proportion of the participants (83.3%) experienced complications related to their current surgery, with pain being the most prevalent complication, affecting 324 (83.1%) of those experiencing complications. The majority of the participants (40.2%) reported that their illness had persisted for several days before undergoing surgery. Abdominal surgery was the most common surgical procedure among the participants, accounting for 119 (25.4%) cases. As for the anticipated discharge destination, 301 (64.3%) participants stated that they would be returning home upon discharge, emphasizing the preference for familiar surroundings. Unsurprisingly, preoperative fear and anxiety were prevalent among the participants, with 373 (79.9%) reporting experiencing high fear and anxiety. Moreover, a significant majority (78.6%) had high service expectations from the hospital, indicating the importance of quality care and support during the preoperative period (Table 3 ).
Patient satisfaction with preoperative education
The overall patient satisfaction with preoperative education on surgical procedures was 79.5% (Fig. 2 ).
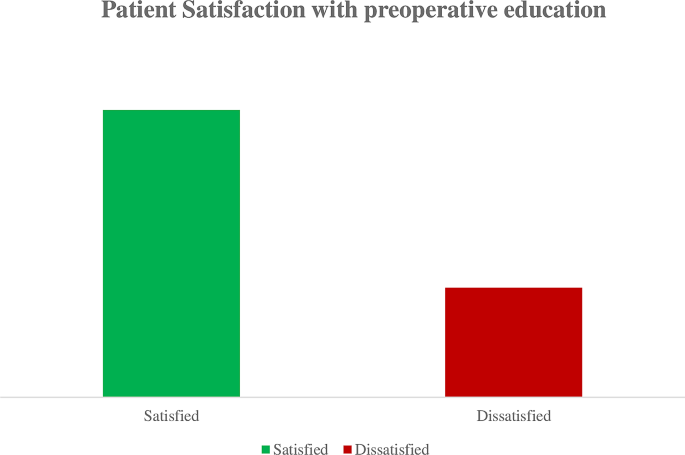
Overall patient satisfaction with preoperative education on surgical procedures at Wolaita Sodo University Comprehensive Specialized Hospital
Factors associated with satisfaction with preoperative nursing care
Sex, age, educational status, monthly income, length of hospital stays, surgery waiting time, nurses’ willingness to listen and respond, payment status for treatment, complications, duration of illness, preoperative fear and anxiety, patient expectations, and preoperative education were all evaluated as potential factors in the bivariable logistic regression analysis (p < 0.25) to determine their association with patient satisfaction with preoperative nursing care. In the multivariable logistic regression, it was found that sex, payment status for treatment, preoperative fear and anxiety, patient expectations, and preoperative education exhibited significant associations with patient satisfaction with preoperative nursing care (p < 0.05). Male patients were found to be 1.14 times more likely to report satisfaction with preoperative nursing care compared to female patients (AOR: 1.14 (95% CI: 0.21–2.91)). Patients who received free treatment were found to be 1.45 times more likely to express satisfaction with preoperative nursing care compared to those who had to pay for their treatment (AOR: 1.45 (95% CI: 0.66–2.97)). Participants who did not experience preoperative fear and anxiety were found to be 1.01 times more likely to report satisfaction with preoperative nursing care compared to those who did have preoperative fear and anxiety (AOR: 1.01, 95% CI: 0.49–2.13). Patients who had low expectations of hospital services were found to be 3.39 times more likely to express satisfaction with preoperative nursing care compared to those who had high service expectations from the hospital (AOR: 3.39, 95% CI: 2.17–7.11). Participants who received preoperative education from nurses were 1.15 times more likely to be satisfied with preoperative nursing care compared to those who did not receive such education from nurses (AOR: 1.148, 95% CI: 0.54–2.86) (Table 4 ).
The primary objective of this study was to determine the level of patient satisfaction with preoperative nursing care at Wolaita Sodo University Comprehensive Specialized Hospital. Furthermore, the study sought to identify factors significantly associated with patient satisfaction with preoperative nursing care. Consequently, the findings of this study demonstrated that the level of patient satisfaction with perioperative nursing care was 79.5%.
This finding was lower when compared with the previous studies conducted at the University of Gondar Teaching Hospital (98.1%) [ 31 ] and Public hospitals in Addis Ababa (84%) [ 12 ]. This disparity can potentially be attributed to various factors, including differences in patient variables such as sociodemographic characteristics, variations in hospital settings, potential inadequacies in the provision of preoperative education and care within the hospitals examined in this study, an increased influx of patients, heightened health-seeking behaviors among individuals, as well as elevated patient expectations regarding the quality of services rendered by the hospitals.
Nevertheless, it is noteworthy that the current finding exhibited a higher level of satisfaction when compared with previous studies conducted at Sohag University (61.9%) [ 41 ], Western Amhara referral hospitals (68.7%) [ 37 ], Gondar University Comprehensive Specialized Hospital (74%) [ 39 ], East Amhara referral hospitals (38.5%) [ 40 ], and Gamo and Gofa zones (36.6%) [ 38 ]. This discrepancy could potentially be attributed to various factors such as differences in the time gaps between the studies, variations in the study participants (for example, the study in East Amhara referral hospitals focused on nurses instead of patients), discrepancies in the services assessed (for instance, the study in the University of Gondar Comprehensive Specialized Hospital solely evaluated satisfaction related to anesthesia services), as well as variances in the perception of the services provided by the patients themselves and the methodologies employed in the studies.
The sex of the patient was significantly associated with patient satisfaction with preoperative nursing care. Male patients were found to be 1.14 times more likely to report satisfaction with preoperative nursing care compared to female patients. This was in line with the study conducted in Barcelona, Spain, [ 13 ] which, strengthens that men patients were more satisfied with preoperative nursing care than women. This finding may be attributed to the fact that women reported experiencing more challenges with hospital care when compared to men. This disparity could potentially arise from the fact that female patients place greater emphasis on their health and often assume the role of evaluators and even administrators of care practices, not just for themselves but also for other family members [ 22 ].
Similarly, payment status for treatment had a significant association with patient satisfaction with preoperative nursing care. Patients who received free treatment were found to be 1.45 times more likely to express satisfaction with preoperative nursing care compared to those who had to pay for their treatment. This could be because patients who receive treatment for free may view it as a gesture of kindness or support, which can enhance their overall experience and level of satisfaction with the preoperative care they receive. Furthermore, patients who do not have to pay for their medical needs may feel less stressed and anxious about the expense, which frees them up to concentrate more on the quality of nursing care they receive. Furthermore, patients who receive free treatment could feel appreciative of the hospital or healthcare system, which could affect how they feel about the care they receive and raise their satisfaction levels.
In this study, patients with preoperative fear and anxiety had also a significant association with satisfaction with preoperative nursing care. Patients who did not experience preoperative fear and anxiety were found to be 1.01 times more likely to report satisfaction with preoperative nursing care compared to those who did have preoperative fear and anxiety. A similar finding was reported in the study conducted in public hospitals in Addis Ababa [ 12 ]. This could be because patients who approach their surgery feeling emotionally stable and at ease may be more receptive to the nursing care they receive. Their ability to maintain composure and relaxation may have a favorable impact on how they view the nursing care they receive, increasing their level of satisfaction. Additionally, patients who do not experience worry or panic before surgery could be better able to express their needs and concerns to the nursing staff. They will be more satisfied as a consequence of this excellent communication, which can improve the standard of care and support they receive. Furthermore, people who are not experiencing preoperative worry or fear may have a more upbeat and hopeful view. This optimistic outlook may lead to a more favorable perception.
Patient expectation of the services was also significantly associated with satisfaction with preoperative nursing care. Participants who had low expectations of hospital services were found to be 3.39 times more likely to express satisfaction with preoperative nursing care compared to those who had high service expectations from the hospital. The possible explanation for this could be that patients who have modest expectations may possess a more pragmatic understanding of the limitations and complexities inherent in the healthcare system. As a consequence, they may display greater gratitude towards the care and attention delivered by the nursing staff, even if it falls short of their initial expectations. Conversely, patients with high service expectations might establish unattainable standards or possess excessively demanding criteria. Consequently, if their expectations are not met, they may experience a sense of disappointment or dissatisfaction with the preoperative nursing care, even if it is of exemplary quality. In contrast, individuals with lower expectations are more likely to find the care they receive to be satisfactory, even if it does not reach the lofty heights of their anticipations.
Likewise, preoperative education was significantly associated with satisfaction with preoperative nursing care. Participants who received preoperative education from nurses were 1.15 times more likely to be satisfied with preoperative nursing care compared to those who did not receive such education from nurses. This finding was similar to the finding of the study conducted at the University of Gondar referral hospital and public hospitals in Addis Ababa [ 12 , 31 ]. The possible reason for this might be that patients who receive preoperative education from nurses are better prepared for surgery by having knowledge and comprehension of the procedures and expectations surrounding their experience. They feel less nervous and uncertain as a result of this instruction, which may improve how they see the nursing care they get. Preoperative education also increases the likelihood that participants will feel powerful and engaged in their care. They can be more engaged in their healing process and may comprehend the significance of specific nursing interventions. A greater sense of participation and teamwork with the nursing staff may be a factor in increased satisfaction [ 12 ].
This study’s results were flavored by Kolcaba’s Comfort Theory, which centers on improving patient satisfaction through attending to their comfort requirements. The study showed that aspects aligning with the theory’s relief component can be improved by meeting particular comfort needs to alleviate pain or discomfort. Additionally, the maintenance of the ease component can be achieved through proactive measures to prevent discomfort to prevent known risk factors that would keep a patient from feeling comfortable, while fulfillment of the transcendence component involves providing patients experiencing physical or emotional discomfort with peace, significance, or opportunities for personal growth through preoperative education and creating a positive nurse-patient relationship through the lens of communication, trust, and empathy in preoperative care.
Implication of the study
In the context of nursing practice, the findings of this study can help nurses in practice by illuminating the variables influencing patients’ satisfaction with preoperative nursing care. Nurses can create tailored methods of care delivery that improve patient experiences and satisfaction by having a greater understanding of the effects of variables including patient gender, treatment costs, preoperative anxiety, and service expectations. Regarding nursing education, the study emphasizes how crucial it is to include preoperative education and communication skills in nursing curricula. It emphasizes how important it is to give nurses the skills and information they need to properly counsel and assist patients before surgery, allaying their anxieties, controlling expectations, and encouraging favorable patient outcomes. The study establishes the foundation for future research endeavors aimed at delving deeper into the topic of patient satisfaction with preoperative nursing treatment. Additional factors that might affect satisfaction, the efficacy of certain interventions or educational initiatives, and the long-term effects of preoperative nursing care on patient outcomes are all potential areas for further research. This information can support evidence-based procedures and guidelines meant to enhance patients’ overall surgical experiences.
Conclusion and recommendation
The study revealed patient satisfaction with preoperative nursing care was high, even though there is room for improvement to ensure optimal healthcare quality. Preoperative care satisfaction is a critical indicator, as even slight deficiencies in this area can have severe consequences, including fatal outcomes. Factors significantly associated with satisfaction in preoperative nursing care were sex, payment status for treatment, preoperative fear and anxiety, patient expectations, and preoperative education.
To address these findings, hospital managers and health policymakers must develop comprehensive strategies aimed at enhancing satisfaction with preoperative nursing care. Initiatives could involve the implementation of tailored training programs for nurses in collaboration with the Ethiopian Federal Ministry of Health, regional health bureaus, and non-governmental organizations. These programs should prioritize equipping nurses with the necessary skills and knowledge to deliver high-quality preoperative care. It is essential to emphasize the need for further research to fully comprehend the specific factors and their impact on patient satisfaction with preoperative nursing care. This research would contribute to a deeper understanding of how nurses can enhance satisfaction levels, ultimately informing the development of evidence-based practices and policies in this crucial healthcare domain.
Strength of the study
To enhance the representativeness and generalizability of our study findings, we employed a substantial sample size and incorporated variables that were overlooked in the previous literature. This approach contributes to a more comprehensive understanding of the factors influencing satisfaction with preoperative nursing care and ensures that our findings encompass a wider range of variables, thereby increasing the validity and applicability of the study results.
Limitations of the study
It is important to acknowledge that the cross-sectional nature of our study design only allows us to establish associations and correlations between the dependent and independent variables, rather than establishing a cause-and-effect relationship. Furthermore, as the quantitative data were collected through a self-administered questionnaire, there is a possibility of response bias from the respondents, which could introduce some limitations to the validity of the data.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations
Adjusted Odds Ratio
Confidence Interval
Crude Odds Ratio
Obstetrics and Gynecology
Statistical Package for Social Sciences
Makau PM, Mbithi BW, J.J.A.J.o.H S, Odero. Factors affecting compliance to preoperative patient care guidelines among nurses working in surgical wards of a tertiary referral hospital in Nairobi, Kenya. 2023. 36(2): p. 124–30 https://doi.org/10.4314/ajhs.v36i2.4 .
Turunen E et al. An integrative review of a preoperative nursing care structure. 2017. 26(7–8): p. 915–930 https://doi.org/10.1111/jocn.13448 .
Soydaş Yeşilyurt D, Yildiz Findik Ü. Effect of preoperative video information on anxiety and satisfaction in patients undergoing abdominal surgery. 2019. 37(8): p. 430–6 https://doi.org/10.1097/cin.0000000000000505 https://journals.lww.com/cinjournal/fulltext/2019/08000/effect_of_preoperative_video_information_on.7.aspx .
Mulugeta H et al. Patient satisfaction with nursing care in Ethiopia: a systematic review and meta-analysis. 2019. 18: p. 1–12 https://doi.org/10.1186/s12912-019-0348-9 .
Dos Santos MMB, Martins JCA, L.M.N.J.R.d.E R, Oliveira. Anxiety, depression and stress in the preoperative period of surgical patients. 2014. 4(3): p. 7–15 https://doi.org/10.12707/RIII1393 .
Health F. Continuous Health Care Quality Improvement through Knowledge Management. Federal Democratic Republic of Ethiopia Ministry of Health, 2019: p. 5 https://www.healthynewbornnetwork.org/resource/continuous-health-care-quality-improvement-through-knowledge-management-in-ethiopia/ .
Van der Voorden M, Ahaus K. and A.J.B.o. Franx, explaining the negative effects of patient participation in patient safety: an exploratory qualitative study in an academic tertiary healthcare centre in the Netherlands. 2023. 13(1): p. e063175 https://doi.org/10.1136/bmjopen-2022-063175 .
Gómara AOJEc. The occurrence of adverse events potentially attributable to nursing care in hospital units. 2014. 24(6): p. 356–7 https://doi.org/10.1016/j.enfcli.2014.08.001 .
Heslop L, Lu S. and X.J.J.o.a.n. Xu, nursing-sensitive indicators: a concept analysis. 2014. 70(11): p. 2469–82 https://doi.org/10.1111/jan.12503 .
Almalki ATA et al. Effectiveness of preoperative nursing assessments in reducing Preoperative complications across Saudi Arabia; a Sysetmatic Review based study. 2023. 30(17): p. 973–83 https://doi.org/10.53555/jptcp.v30i17.2667 .
Oner B et al. Nursing-sensitive indicators for nursing care: a systematic review (1997–2017). 2021. 8(3): p. 1005–22 https://doi.org/10.1002/nop2.654 .
Deressa D et al. Satisfaction with preoperative education and surgical services among adults elective surgical patients at selected public hospitals in Addis Ababa, Ethiopia. 2022. 10: p. 20503121221143219 https://doi.org/10.1177/20503121221143219 .
Sillero Sillero A. and A.J.S.o.m. Zabalegui, satisfaction of surgical patients with perioperative nursing care in a Spanish tertiary care hospital. 2018. 6: p. 2050312118818304 https://doi.org/10.1177/2050312118818304 .
Lake ET et al. Missed nursing care is linked to patient satisfaction: a cross-sectional study of US hospitals. 2016. 25(7): p. 535–43 https://doi.org/10.1136/bmjqs-2015-003961 .
Lake ET et al. Higher quality of care and patient safety associated with better NICU work environments. 2016. 31(1): p. 24–32 https://doi.org/10.1097/NCQ.0000000000000146 .
Stimpfel AW et al. Common predictors of nurse-reported quality of care and patient safety. 2019. 44(1): p. 57–66 https://doi.org/10.1097/HMR.0000000000000155 .
Hill B. J.B.J.o.N., do nurse staffing levels affect patient mortality in acute secondary care? 2017. 26(12): p. 698–704 https://doi.org/10.12968/bjon.2017.26.12.698 .
Van Bogaert P, et al. Nurse work engagement impacts job outcome and nurse-assessed quality of care: model testing with nurse practice environment and nurse work characteristics as predictors. 5. 2014;p(1261). https://doi.org/10.3389/fpsyg.2014.01261 .
Arakelian E et al. The meaning of person-centred care in the perioperative nursing context from the patient’s perspective–an integrative review. 2017. 26(17–18): p. 2527–44 https://doi.org/10.1111/jocn.13639 .
Ball JE et al. Post-operative mortality, missed care and nurse staffing in nine countries: a cross-sectional study. 2018. 78: p. 10–5 https://doi.org/10.1016/j.ijnurstu.2017.08.004 .
Wune G et al. Nurses to patients communication and barriers perceived by nurses at Tikur Anbessa Specilized Hospital, Addis Ababa, Ethiopia., 2018. 2020. 12: p. 100197 https://doi.org/10.1016/j.ijans.2020.100197 .
Sillero-Sillero A. and A.J.R.l.-a.d.e. Zabalegui, Safety and satisfaction of patients with nurse’s care in the perioperative. 2019. 27 https://doi.org/10.1590/1518-8345.2646.3142 .
Gonçalves MAR, Cerejo MdNR, J.C.A.J.R.d.E R, Martins. The influence of the information provided by nurses on preoperative anxiety. 2017. 4(14): p. 17–25 https://doi.org/10.12707/RIV17023 .
Alvarado LE, Bretones FD, J.A.J.F.i P, Rodríguez. The effort-reward model and its effect on burnout among nurses in Ecuador. 2021. 12: p. 760570 https://doi.org/10.3389/fpsyg.2021.760570 .
Ahmed T et al. Levels of adult patients’ satisfaction with nursing care in selected public hospitals in Ethiopia. 2014. 8(4): p. 371 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4350891/ .
Malley A et al. The role of the nurse and the preoperative assessment in patient transitions. 2015. 102(2): p. 181. e1-181. e9 https://doi.org/10.1016/j.aorn.2015.06.004 .
Liddle CJNS. An overview of the principles of preoperative care. 2018. 33(6) https://doi.org/10.7748/ns.2018.e11170 .
Adugbire BA, Aziato L, F.J.I.J.o.A NS, Dedey. Patients’ experiences of pre and intra operative nursing care in Ghana: A qualitative study. 2017. 6: p. 45–51 https://doi.org/10.1016/j.ijans.2017.04.001 .
Sadia H et al. Assessment of nurses’ knowledge and practices regarding prevention of surgical site infection. 2017. 3(6): p. 585–95 https://doi.org/10.21276/sjmps .
Fetene MB et al. Perioperative patient satisfaction and its predictors following surgery and anesthesia services in North Shewa, Ethiopia. A multicenter prospective cross-sectional study. 2022. 76: p. 103478 https://doi.org/10.1016/j.amsu.2022.103478 .
Gebremedhn EG, G.F.J.P.A.M.J., Lemma. Patient satisfaction with the perioperative surgical services and associated factors at a University Referral and Teaching Hospital, 2014: a cross-sectional study. 2017. 27(1) https://doi.org/10.11604/pamj.2017.27.176.10671 .
Kibru EA et al. Patient satisfaction with post-operative surgical services and associated factors at Addis Ababa City government tertiary hospitals’ surgical ward, cross-sectional study, 2022. 2023. 45 https://doi.org/10.11604/pamj.2023.45.189.38416 .
Trinh LN, Fortier MA, Kain ZNJPM. Primer on adult patient satisfaction in perioperative settings. 2019. 8: p. 1–13 https://doi.org/10.1186/s13741-019-0122-2 .
Astier A et al. What is the role of technology in improving patient safety? A French, German and UK healthcare professional perspective. 2020. 25(6): p. 219–24 https://doi.org/10.1177/2516043520975661 .
Tadesse F, Yohannes Z, J.R.R.J.H L. Knowledge and practice of pain assessment and management and factors associated with nurses’ working at Hawassa University Referral Hospital, Hawassa city, South Ethiopia. 2016. 6(3): p. 24–8.
Criscitelli TJAj. Improving efficiency and patient experiences: the perioperative surgical home model. 2017. 106(3): p. 249–53 https://doi.org/10.1016/j.aorn.2017.07.009 .
Alemu ME, Worku WZ, Berhie AYJH. Patient satisfaction and associated factors towards surgical service among patients undergoing surgery at referral hospitals in western Amhara Regional State, Ethiopia. 2023. 9(3) https://doi.org/10.1016/j.heliyon.2023.e14266 .
Alito GA, Madebo WE, Eromo NC, Quality of Perioperative Informations Provided and it’s Associated Factors Among Adult Patients Who Undergone Surgery in Public Hospitals of Gamo &Gofa Zones: A Mixed Design Study, Ethiopia S. 2019. 2019 https://gssrr.org/index.php/JournalOfBasicAndApplied/article/view/11761 .
Endale Simegn A et al. Patient Satisfaction Survey on Perioperative Anesthesia Service in University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia, 2021. 2021. 2021 DOI: https://doi.org/10.1155/2021/3379850 .
Tadesse B et al. Preoperative Patient Education Practices and Predictors Among Nurses Working in East Amhara Comprehensive Specialized Hospitals, Ethiopia, 2022. 2023: p. 237–247 https://doi.org/10.2147/JMDH.S398663 .
Findik UY et al. Patient satisfaction with nursing care and its relationship with patient characteristics. 2019. 12(2): p. 162–9 https://doi.org/10.1111/j.1442-2018.2009.00511.x .
Teng K, Norazliah SJJEH. Surgical patients’ satisfaction of nursing care at the orthopedic wards in hospital universiti sains Malaysia (HUSM). 2012. 3(1): p. 36–43.
Dawood KSJM-LU. Preoperative anxiety and fears among adult Surgical patients in Baghdad Teaching Hospital, Iraq. 2020. 20(1) https://doi.org/10.37506/v20/i1/2020/mlu/194433 .
Dibabu AM et al. Preoperative anxiety and associated factors among women admitted for elective obstetric and gynecologic surgery in public hospitals, Southern Ethiopia: a cross-sectional study. 2023. 23(1): p. 728 https://doi.org/10.1186/s12888-023-05005-2 .
Download references
Acknowledgements
We extend our sincere appreciation and gratitude to Wolaita Sodo University and our supervisors for their invaluable advice and supportive mentorship throughout this study. We would also like to express our thanks to the management and staff of the health institution, as well as the dedicated data collectors who played a crucial role in gathering the necessary data. Moreover, we are deeply grateful to the study participants and all other groups and individuals who contributed their time and effort to make this research possible. Their valuable contributions have been instrumental in the success of this study.
No funding was received.
Author information
Authors and affiliations.
Adult Health Nursing, School of Nursing, College of Health Science and Medicine, Wolaita Sodo University, Sodo, Ethiopia
Bizuayehu Atinafu Ataro, Eshetu Elfios Endirias & Getachew Nigussie Bolado
Maternity and Child Health Nursing, School of Nursing, College of Health Science and Medicine, Wolaita Sodo University, Sodo, Ethiopia
Temesgen Geta
Pediatrics and Child Health Nursing, School of Nursing, College of Health Science and Medicine, Wolaita Sodo University, Sodo, Ethiopia
Christian Kebede Gadabo
You can also search for this author in PubMed Google Scholar
Contributions
BAA wrote a manuscript, conceived data and designed a study, supervised the data collection, performed the analysis, interpreted data, drafted a manuscript, and revised and approved a manuscript for publication. TG, EEE, and GNB assisted in designing the study, were involved in data analysis and interpretation, and critically reviewed the manuscript. All authors reviewed the manuscript.
Corresponding authors
Correspondence to Bizuayehu Atinafu Ataro or Getachew Nigussie Bolado .
Ethics declarations
Ethics approval and consent to participate.
We obtained ethical clearance from the Ethical Review Committee of the Wolaita Sodo University Institutional Review Board (IRB-WSU). Written informed consent was obtained from respondents during data collection after explaining the purpose of the study. Information was also collected anonymously after obtaining written consent from each respondent, ensuring confidentiality by omitting their name and personal identification throughout the data collection period. The study identification number went from 001 to 468. This code was stored in electronic format, encrypted using the encryption software Mac OS X version 10.9.8, and password-protected on the principal investigator’s personal computer. No other identifier was collected, such as a name or the participant’s home address. Participants were also informed that they have the right to refuse, stop, or withdraw at any time during data collection. Finally, participants were informed that there was no incentive or harm to their participation in this study. This declaration was obtained according to the Helsinki form.
We, the undersigned, affirm that this paper is an original piece of work conducted by us and has not been previously presented or published in any Journal. We are fully aware of the importance of academic integrity and understand that plagiarism is strictly prohibited. Any direct quotations or material taken from other sources have been appropriately referenced and credited.
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The authors declare the absence of any other conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ataro, B.A., Geta, T., Endirias, E.E. et al. Patient satisfaction with preoperative nursing care and its associated factors in surgical procedures, 2023: a cross-sectional study. BMC Nurs 23 , 235 (2024). https://doi.org/10.1186/s12912-024-01881-5
Download citation
Received : 10 January 2024
Accepted : 18 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1186/s12912-024-01881-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preoperative nursing care
- Patient satisfaction
- Surgical procedure
- Associated factors
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Press Release
Maine nurses call on gov. mills to support nurse-to-patient ratios.

Today, nurses publicly called on Gov. Janet Mills to support LD 1639, a bill that would create mandated nurse-to-patient ratios based on patients’ needs in Maine’s acute-care hospitals, announced Maine State Nurses Association (MSNA). Gov. Mills has not yet taken a position on the bill. Nurses say the governor’s support is critical to pass the bill, now pending in the House.
At the event, nurses revealed a letter in support of LD 1639 sent to Gov. Mills today , and signed by more than 500 Maine nurses, pointing out that "Understaffing is not a new issue. Hospitals intentionally understaff to maximize profits and excess revenue. ... The current staffing crisis was foreseeable and preventable. We can fix it if we act now."
The letter also asked Gov. Mills to:
- “Meet with nurses, face-to-face, hear our stories, and truly understand the moral distress and injury that we face every day, in every hospital across our state.”
- “Look carefully at the powerful evidence that has been compiled over decades to show the efficacy and the necessity of enforceable nurse-to-patient ratios." And,
- “Stand in support of nurses, patients, and The Maine Quality Care Act and make Maine the next state to take real steps to address our state and national nurse staffing crises."
The Maine Quality Care Act (LD 1639), sponsored by State Sen. Stacy Brenner (D-Scarborough), passed the Maine Senate with a bipartisan 22-13 vote on March 27. In her floor speech introducing the bill, Sen. Brenner stated, “The bill in front of you today accomplishes two primary goals: increasing patient safety and encouraging nurse retention. Not all of us are going to practice as nurses but at some point in life, we are all either going to be a patient or going to have a loved one as a patient.”
Janel Crowley, chief nurse representative and neonatal ICU nurse at Maine Medical Center said, “All of us know of nursing colleagues who have left the bedside because of poor working conditions. The good news is we also know nurses who would come back to the bedside if conditions improved.”
Another Maine Med RN, Anthony Abdallah, who works in the cardiac intensive care unit, said, “We hold vulnerable people’s lives in our hands. It makes sense that reasonable ratios will improve patient outcomes and protect nurses. We are not asking for the moon. We are only asking for what decades of research backs up: Safe staffing saves lives.”
The hospital industry has vehemently opposed the Maine Quality Care Act, citing what it calls a “nursing shortage.” But MSNA President Cokie Giles, RN said, “There is no nursing shortage in our state or our country. There is only a shortage of nurses who are willing to work in the unsafe conditions they’re being given. The Maine Quality Care Act will bring nurses back to the bedside, which is what our state and nation need right now.”
Maine State Nurses Association is part of National Nurses Organizing Committee, representing 4,000 nurses and other caregivers from Portland to Fort Kent. NNOC is an affiliate of National Nurses United, the largest and fastest-growing labor union of registered nurses in the United States with nearly 225,000 members nationwide.
Maine nurses urge Gov. Mills to support bill mandating patient ratios
by Stephanie Grindley , CBS13 I-Team
PORTLAND (WGME) – Maine nurses held signs outside Maine Medical Center reading, "Safe staffing saves lives,” Thursday.
It was a message directed to Governor Janet Mills ahead of a House vote in the coming days.
Hundreds of nurses signed a letter asking Mills to support mandated nurse-to-patient ratios.
- Also read: Maine Senate passes bill that mandates nurse-to-patient ratios
A bill passed by the Senate with bipartisan support is now heading to the House.
It would set a maximum number of patients a nurse can take on, depending on the department.
For example, in an ICU setting, a nurse said it would create a limit of two patients in her care, instead of the four she is currently managing.
"What they're experiencing right now is basically what we call ‘assembly line nursing,’ Registered Nurse Janel Crowley said. “You go in, you pass meds, you do your assessment, you move on to the next patient, because you don't have time to focus on each individual patient."
- Also read: Winthrop nursing home blames lack of state funding for upcoming closure
Those with the Maine State Nurses Association say ratios will lower patient deaths and readmission rates and prevent leaving patients in hospital beds alone for hours at a time.
MaineHealth has come out against mandated ratios. It says it takes away divvying power among nurses who know how many patients they can handle and will only keep more patients in the hospital waiting room.
"I hope that it is rejected and that we are able to maintain our own decisions on staffing,” MaineHealth Chief Nursing Officer Sharon Baughman said. “I'm very worried about access to care. If the bill passes, we'll see more patients are going to need to wait in the ED."
Nurses say they need the governor's support for this bill to pass the House.
The CBS13 I-Team reached out to her administration Thursday afternoon.
- Also read: Health care professionals push for more funding for care facilities for older Mainers
A spokesperson from her office pointed us to testimony provided last year indicating the administration opposes the bill.
They cited ongoing, significant workforce challenges that have persisted from the COVID pandemic.
Press Herald
Account Subscription: ACTIVE
Questions about your account? Our customer service team can be reached at [email protected] during business hours at (207) 791-6000 .
- Health care
- Local & State
After intense lobbying, Maine Senate backs bill to set minimum nurse staffing in hospitals
The legislation would set required ratios in an effort to improve working conditions and ease a nursing shortage. Opponents say the measure would reduce access to care.

You are able to gift 5 more articles this month.
Anyone can access the link you share with no account required. Learn more .
With a Press Herald subscription, you can gift 5 articles each month.
It looks like you do not have any active subscriptions. To get one, go to the subscriptions page .
Loading....
The Maine Senate voted Wednesday in favor of mandatory nurse staffing ratios for the state’s hospitals, bringing back a controversial issue that has divided hospital officials and the state nurses’ union.
The Mills administration opposed the bill when it was introduced last year, arguing that the measure could have the unintended consequence of reducing services in the health care industry at a time when there are acute nursing shortages in some areas. Unable to meet mandated ratios, the hospitals would need to cut services and reduce patient counts to comply, state officials have said.
The bill was tabled and never received a vote in 2023, but Democratic lawmakers brought it back for a vote on Wednesday.
Senators voted 22-13 in favor of the bill, which now goes to the Maine House for an initial vote.
Maine nurses split over whether state mandate of staff ratios would help
“Maine does not have a shortage of nurses,” said Sen. Stacy Brenner, D-Scarborough, a former nurse and the bill’s sponsor. “We have workplace conditions that are unacceptable to nurses. Let’s change those conditions so nurses will come back to bedsides.”
She and other supporters said the strain placed on nurses is harming the quality of care they can give to patients. Advertisement
The number of registered nurses has increased slightly, from 14,490 in 2019 to 14,610 in 2022, the latest year statistics are available, according to the U.S. Bureau of Labor. Maine’s higher education system has graduated increasing numbers of nurses in recent years, in an attempt to meet demand.
But Maine’s overall health care practitioner workforce – including doctors, nurse practitioners, nurses and other health professions – has shrunk form 42,390 in 2019 to 41,110 in 2022, while Maine’s population has grown and aged.
And while the number of nurses has increased, there are areas of acute shortages, including direct care nurses and in some hospital departments. Hospitals have had to rely on expensive traveling nurses for years, straining budgets.
Bill would mandate nurse-to-patient ratios in Maine hospitals
State Sen. Eric Brakey, R-Auburn, said that strict ratios are not a solution.
“We certainly have a nursing shortage in our state, but we can’t mandate it away,” Brakey said.
The bill would set minimum nurse-to-patient staffing ratios that would vary depending on the service, so, for instance, emergency department ratios would be different than oncology. The ratios would also vary depending on the type of patients and severity of a patient’s condition. The bill sets ratios depending on patient needs, ranging from one-on-one care up to one nurse caring for four patients. Advertisement
There are national guidelines for safe nursing staff levels, although there is no standard nurse-to-patient ratio. The American Nurses Association does not recommend specific ratios, but advises that each hospital develop safe staffing plans with input from nurses.
If signed into law, Maine would join California and Oregon as the only states that mandate nurse ratios, although several states have considered adopting ratios. Oregon passed its staffing ratio bill last year, while California’s has been on the books for about 20 years.
Jeff Austin, vice president of government affairs for the Maine Hospital Association, said in a written statement that the “Senate voted to support government control of staffing decisions at hospitals.”
“We firmly believe the Legislature should not substitute its judgment for that of experienced nurse leaders,” Austin said. “The bill deviates from recommendations of the leading national care organizations and will harm patients and communities.”
Austin said over half of Maine’s hospitals are losing money.
“They can’t hire 1,000 nurses that don’t exist, with $100 million they don’t have,” Austin said.
But Cokie Giles, president of the Maine State Nurses Association union, which represents nurse unions at Eastern Maine Medical Center in Bangor and Maine Medical Center in Portland, said that the bill would “protect nurses and their patients.”
The nurses’ union contends that the bill would stop unsafe practices, such as eliminating breaks for hospital workers and mandating overtime.
“We are ecstatic that this bill has taken another important step forward to becoming law in our great state,” Giles said. “Nurses know that safe staffing saves lives.”
Related Headlines
Success. Please wait for the page to reload. If the page does not reload within 5 seconds, please refresh the page.
Enter your email and password to access comments.
Forgot Password?
Don't have a commenting profile? Create one.
Hi, to comment on stories you must create a commenting profile . This profile is in addition to your subscription and website login. Already have a commenting profile? Login .
Invalid username/password.
Please check your email to confirm and complete your registration.
Create a commenting profile by providing an email address, password and display name. You will receive an email to complete the registration. Please note the display name will appear on screen when you participate.
Already registered? Log in to join the discussion.
Only subscribers are eligible to post comments. Please subscribe or login first for digital access. Here’s why .
Use the form below to reset your password. When you've submitted your account email, we will send an email with a reset code.
Send questions/comments to the editors.
Maine Political Report
- Email address
- Name This field is for validation purposes and should be left unchanged.
House censures Republican lawmakers who said Lewiston shooting was God’s response to abortion expansion
Maine lawmakers endorse higher tax brackets for wealthier residents, maine bill limiting tobacco sales would impact just 1 store, foulmouthed brewing to close; new brewery to take its place in south portland, jury finds man not guilty in deadly 2016 shooting at portland apartment, member log in.
Please enter your username and password below. Already a subscriber but don't have one? Click here .
Not a subscriber? Click here to see your options
- Skip to navigation
- Skip to content
- UMB Shuttle
University of Maryland, Baltimore
About UMB History, highlights, administration, news, fast facts
- Accountability and Compliance
- Administration and Finance
- Center for Information Technology Services
- Communications and Public Affairs
- Community Engagement
- Equity, Diversity, and Inclusion
- External Relations
- Government Affairs
- Philanthropy
- Office of the President
- Office of the Provost
- Research and Development
- University Counsel
- Administrative Officers
- Boards of Visitors
- Faculty Senate
- Staff Senate
- Center for Health and Homeland Security
- Council for the Arts & Culture
- Interprofessional Education
- Leaders in Education: Academy of Presidential Scholars
- Middle States Self-Study
- President's Council for Women
- President's Symposium and White Paper Project
- For the Media
- Steering Committee Roster
- Logistics Committee Roster
- UMB Police and Public Safety
- Graduation Celebration 2024
- Founders Week
- UMB Holiday Craft Fair
Academics Schools, policies, registration, educational technology
- School of Dentistry
- Graduate School
- School of Medicine
- School of Nursing
- School of Pharmacy
- School of Social Work
- Carey School of Law
- Health Sciences and Human Services Library
- Thurgood Marshall Law Library
Admissions Admissions at UMB are managed by individual schools.
- Carey School of Law Admissions
- Graduate School Admissions
- School of Dentistry Admissions
- School of Medicine Admissions
- School of Nursing Admissions
- School of Pharmacy Admissions
- School of Social Work Admissions
- Tuition and Fees by School
- Student Insurance
- Academic Calendar
- Financial Assistance for Prospective Students
- Financial Assistance for Current Students
- Financial Assistance for Graduating Students
Research Offices, contracts, investigators, UMB research profile
- Organized Research Centers and Institutes
- UMB Institute for Clinical & Translational Research
- Sponsored Programs Administration
- Sponsored Projects Accounting and Compliance (SPAC)
- Kuali Research
- Clinical Trials and Corporate Contracts
- CICERO Log-in
- Conflict of Interest
- Human Research Protections
- Environmental Health and Safety
- Export Compliance
- Effort Reporting
- Research Policies and Procedures
- Center for Innovative Biomedical Resources
- Baltimore Life Science Discovery Accelerator (UM-BILD)
- Find Funding
- File an Invention Disclosure
- Global Learning for Health Equity Network
- Manage Your Grant
- Research Computing
- UM Research HARBOR
- Center for Violence Prevention
- Office of Research and Development
- Center for Clinical Trials and Corporate Contracts
- Technology Transfer/UM Ventures
- Contact Research and Development
Services For students, faculty, and staff, international and on-campus
- Student Health Resources
- Educational Support and Disability Services
- Writing Center
- URecFit and Wellness
- Intercultural Leadership and Engagement
- Educational Technology
- Student Counseling Center
- UMB Scholars for Recovery
- UMB Student Affairs
- Human Resource Services
- Travel Services
- Strategic Sourcing and Acquisition Services
- Office of the Controller
- Office of the Ombuds
- Employee Assistance Program (EAP)
- Workplace Mediation Service
- Faculty Center for Teaching and Learning
- UMB Travel: Start Here
- International Students, Scholars, and Employees
- Center for Global Engagement
- International Travel SOS
- International Operations
- Parking and Transportation Services
- UMB shuttle
- SMC Campus Center Event Services
- Donaldson Brown Riverfront Event Center
- All-Gender Bathrooms
- Environmental Services
- Interprofessional Program for Academic Community Engagement
University Life Alerts, housing, dining, calendar, libraries, and recreation
- Emergency Reference Guide
- Campus Life Weekly with USGA
- Starting a New Universitywide Organization
- University Student Government Association
- Planned Closures
- Intramural Sports
- Safety Education
- About URecFit and Wellness
- How to Get Your One Card
- One Card Uses
- Lost One Card
- One Card Policies
- Photo Services
- One Card Forms
- One Card FAQs
- Office Hours and Directions
Give to UMB Sustain excellence and meet UMB's educational needs for today and tomorrow.

Thank You for Your Gift to UMB
The University of Maryland, Baltimore (UMB) is excited to share its new online giving page.
With enhanced searchability, a streamlined checkout process, and new ways to give such as Venmo, PayPal, Apple Pay, and Google Pay in addition to credit card, donors can support UMB quickly and securely.
- Ways to Give
- Where to Give
- Staying Connected: You and UMB
- The UMB Foundation
- Office of Philanthropy
- Maryland Charity Campaign

- Archived News
Search UMB News:
There are no reported emergencies on campus at this time. Sign up for UMB Alerts.
Nursing Rises in ‘U.S. News’ Best Graduate Schools Rankings
April 9, 2024 | By Mary Therese Phelan
Continuing its mission of shaping the nursing profession and the health care environment by developing leaders in education, research, and practice, the University of Maryland School of Nursing (UMSON) has again ranked in the top 10 across the board for public schools of nursing — and moved up in all six categories in which the school is ranked — in the newly released 2024 edition of U.S. News & World Report ’s “ America’s Best Graduate Schools ,” out of 651 accredited nursing schools surveyed.
Both UMSON’s Doctor of Nursing Practice (DNP) and its Master of Science in Nursing (MSN) programs climbed in the rankings among all schools surveyed, with DNP tied at No. 8 (up from No. 15 last year) and MSN at No. 20 overall (up from No. 25 last year). Among public schools of nursing, the DNP program is tied at No. 4 and the MSN is ranked No. 9.
Two UMSON specialties lead the way in the rankings, both ranked No. 1 (tied) nationwide among public schools of nursing:
- The DNP Adult-Gerontology Primary Care Nurse Practitioner specialty, tied at No. 4 among all ranked schools
- The MSN Health Services Leadership and Management specialty, No. 2 among all ranked schools
UMSON also is ranked in the top 10 among public schools of nursing for its:
- Family Nurse Practitioner Doctor of Nursing Practice specialty (No. 3)
- DNP Nurse Anesthesia specialty (No. 7, tied)
“It is gratifying to continue to be recognized nationally for our Doctor of Nursing Practice program and our Master of Science in Nursing program,” said Yolanda Ogbolu, PhD, NNP, FNAP, FAAN , the Bill and Joanne Conway Dean of the University of Maryland School of Nursing. “The School of Nursing plays a vital role in our collective efforts in Maryland and nationally to increase the number of nurses with advanced education, particularly at the doctoral level. It is essential that we have nurses who are well prepared to meet the changing needs of patients, their families, and our communities at a time when we face increasing complexity in our health care system, growing diversity in our population, and persistent gaps in access to needed care.”
The U.S. News & World Report rankings are based on a variety of indicators, including student selectivity and program size, faculty resources, and research activity, and on survey data from deans of schools of nursing that are accredited by the Commission on Collegiate Nursing Education or the Accreditation Commission for Education in Nursing.
In fall 2023 and early 2024, U.S. News surveyed 651 nursing schools with master’s or doctoral programs. In total, 292 nursing programs responded to the survey. Of those, 216 provided enough data to be included in the rankings of nursing master’s programs and 188 provided enough data to be eligible for inclusion in the ranking of DNP programs. Many institutions were ranked in both, using overlapping data.
The University of Maryland, Baltimore is the founding campus of the University System of Maryland. 620 W. Lexington St., Baltimore, MD 21201 | 410-706-3100 © 2023-2024 University of Maryland, Baltimore. All rights reserved.

IMAGES
COMMENTS
The first jurisdictions to implement minimum nurse-to-patient ratios policies were the states of Victoria, Australia, and California, USA, in the late 1990s.16, 17 The past 5 years have seen a resurgence of interest in establishing minimum nurse-to-patient ratio policies—Wales and Scotland (UK), Ireland, and Queensland (Australia) have ...
Introduction. A nurse/midwife-to-patient ratio is a minimum number of nurses or midwives allocated to a specific number of patients for whom they provide care (Lesman et al., Citation 2019).Minimum nurse/midwife-to-patient ratios have been implemented in many jurisdictions internationally, as one of a number of different staffing methods intended to maintain manageable nurse workloads ...
Queensland Health, National Institutes of Health, National Institute of Nursing Research. ... Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals Lancet. 2021 May 22;397(10288):1905-1913. doi: 10.1016/S0140-6736(21)00768-6.
Research on Healthcare Performance Lab, Inserm U1290, Université Claude Bernard Lyon 1, Health Data Department, Hospices Civils de Lyon, Lyon 69424, France. ... Minimum nurse-to-patient ratio policies are a feasible approach to improve nurse staffing and patient outcomes with good return on investment. Full-Text
To address these issues and answer the research questions introduced in Section 1, we develop a nurse staffing model that incorporates results from empirical studies on how patient-to-nurse ratios impact patient length-of-stay and nurse turnover (research question 1). Using this model, we show that lower patient-to-nurse ratios do not ...
The world authority in nurse-to-patient ratio research Professor Linda Aiken and her team (2002) found that for every extra patient over four patients per nurse in a general medical or surgical ward, there is a direct impact on a patient's recovery and the risk of serious complications and/or death.
A study published in The Lancet assesses the effects of such a policy implemented in Queensland, Australia, in 2016. The study found that minimum nurse-to-patient ratio policies are feasible, improve patient outcomes, and provide a good return on investment. Read the full paper, or view the key stats below. Download PDF.
No research prior to this study has considered the association of patient-to-nurse staffing ratios and recommended evidence-based sepsis care bundles on outcomes for sepsis patients. In this study, we directly evaluate whether patient-to-nurse staffing ratios are associated with clinical outcomes for patients admitted with sepsis in 116 New ...
Nurse-to-patient ratios influence many patient outcomes, most markedly inhospital mortality. More studies need to be conducted on the association of nurse-to-patient ratios with nurse-sensitive patient outcomes to offset the paucity and weaknesses of research in this area.
Research has shown that each additional patient assigned to a registered nurse beyond the optimum ratio significantly increases the risk of preventable death, longer stays, readmissions, and unfavorable patient satisfaction. It directly results in less effective care, poorer patient outcomes, and higher costs of care. State-Wide PA Hospital Study
In one ANA study, a staggering 89% of nurses admitted that their place of employment was short-staffed. "Enforceable nurse-to-patient ratios can significantly support nurses particularly if they recognize key factors such as patient acuity, intensity of the unit practice setting, and nurses' competency," ANA officials told NurseJournal.
nurse-to-patient ratios, patient satisfaction scores, and hospital profitability. Purpose Statement. The purpose of this quantitative correlational study was to examine the relationship between nurse-to-patient ratios, patient satisfaction scores, and hospital profitability. The targeted population for this study was hospitals located in Southern
Definition of nurse-to-patient ratios. Nurse-to-patient ratios refer to the number of patients assigned to a single nurse in a healthcare setting. These ratios are often used as a measure of staffing levels and workload management. For example, a ratio of 1:5 suggests that one nurse is responsible for five patients.
California. The following are minimum nurse-to-patient staffing ratios in hospitals: Critical care unit: 1:2. Labor and delivery suite of the perinatal service: 1:2 (active labor patients) and 1:4 (antepartum patients who are not in active labor) Postpartum area of the perinatal service: 1:4 (mother-baby couplets)
Nurse managers who interact purposefully with each registered nurse on their team have lower turnover, with monthly interactions such as recognitions, check-ins or corrective actions driving a 7-percentage-point improvement in the team's annual turnover rate, according to a new report by the American Organization for Nursing Leadership and Laudio Insights.
To enhance patient satisfaction, nurses engaged in preoperative care must possess a comprehensive understanding of the most up-to-date evidence. However, there is a notable dearth of relevant information regarding the current status of preoperative care satisfaction and its impact, despite a significant rise in the number of patients seeking surgical intervention with complex medical requirements.
Today, nurses publicly called on Gov. Janet Mills to support LD 1639, a bill that would create mandated nurse-to-patient ratios based on patients' needs in Maine's acute-care hospitals, announced Maine State Nurses Association (MSNA). Gov. ... We are only asking for what decades of research backs up: Safe staffing saves lives." ...
Those with the Maine State Nurses Association say ratios will lower patient deaths and readmission rates and prevent leaving patients in hospital beds alone for hours at a time. MaineHealth has ...
The ratios would also vary depending on the type of patients and severity of a patient's condition. The bill sets ratios depending on patient needs, ranging from one-on-one care up to one nurse ...
Continuing its mission of shaping the nursing profession and the health care environment by developing leaders in education, research, and practice, the University of Maryland School of Nursing (UMSON) has again ranked in the top 10 across the board for public schools of nursing — and moved up in all six categories in which the school is ranked — in the newly released 2024 edition of U.S ...