An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Adv Med Educ Pract

The Effect of Sleep Quality on Students’ Academic Achievement
Rostam jalali.
1 Faculty of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran
Habibollah Khazaei
2 Sleep Disorders Research Center, Kermanshah University of Medical Sciences, Kermanshah, Iran
Behnam Khaledi Paveh
Zinab hayrani, lida menati.
Sleep is an inseparable part of human health and life, which is crucial in learning, practice, as well as physical and mental health. It affects the capacity of individual learning, academic performance, and neural-behavioral functions. This study aimed to determine the relationship between sleep quality and students’ academic achievement among students at Kermanshah University of Medical Sciences.
In this cross-sectional study, 102 medical students from different fields, with maximum variation sampling, completed Pittsburgh Sleep Quality Index (PSQI). For data analysis, SPSS 19 was used through which Pearson correlation test, Spearman test, and t -test were employed.
Based on the quality of sleep questionnaire scores, the results indicated no significant difference between students with high grades and those with low grades. However, there were moderate and sometimes severe sleep disturbances in both groups.
The results showed no significant difference between sleep quality and academic achievement. Nevertheless, longitudinal study should be performed to control for confounding factors.
Sleep is an inseparable part of human health and life, and is pivotal to learning and practice as well as physical and mental health. 1 Studies have suggested that insufficient sleep, increased frequency of short-term sleep, and going to sleep late and getting up early affect the learning capacity, academic performance, and neurobehavioral functions. 2 , 3 Previous studies have indicated that the quantity of sleep reported by individuals as delayed or inappropriate sleep, waking up too late, especially at weekends and daytime sleepiness is associated with compromised academic performance in children and adults. 2 Some studies have emphasized the relationship between delayed starting time of classes and academic success. 4 Reduced overnight sleep or altered sleep patterns has been associated with severe drowsiness and failure in academic success. 5 In a study, people who had enough sleep compared to their sleep-deprived individuals used innovative solutions twice as often when confronted with complex mathematical problems. 6 The chance of academic failure was as long as one or more than 1 year in students with inadequate sleep compared to those with proper sleep. 7 People who sleep less and sleep during the day are more prone to vehicle and work accidents. 8 In some studies, sleep efficiency has been considered as essential for recovery, cognitive processing, and memory integration. 9 On the other hand, lack of sleep has been associated with emotional instability and impaired concentration. 10 In this regard, students are particularly at risk of developing sleep disorders and development of the disorder among them has a negative effect on their academic performance across different grades, 11 – 13 However, there is no consensus in this case and not all studies state that sleep disorders yield a negative effect on academic performance. Eliasson (2010) believes that the time it takes to fall asleep and waking up affect academic performance more than duration of sleep does. 14 Sweileh and colleagues (2011) also believe that there is no relationship between sleep quality and academic success. 15 Similarly, it is claimed there is no relationship between the night sleep before the exam and test scores either. 16
In another study, the author believes stress from lack of sleep causes poor school performance. 17 On the other hand, in a systematic review, the authors could not establish a cause and effect relationship between sleep quality and academic performance. 2 In their meta-analysis study, Dewald and colleagues (2010) emphasized that because of the diversity of the methodology of studies, it is impossible to definitely derive a relationship between sleep quality and academic performance, and thus more longitudinal intervention studies are warranted. 1 According to different conclusions in this respect, the researchers decided to determine the relationship between sleep quality and academic performance among students at Kermanshah University of Medical Sciences.
In this cross-sectional study, through maximum variation sampling, the first three students with highest scores and three last students with lowest scores were selected, and the Pittsburgh Sleep Quality Index (PSQI) was completed for them.
The study population consisted of students of Kermanshah University of Medical Sciences. The samples were also students at each school with the highest GPA (first three high scores) and the lowest GPA (last three lowest scores). The sampling was purposeful sampling with maximum variation. The sample covered a number of disciplines in the third semester and above ( Figures 1 & 2 ). After determining the target students, the questionnaire was given to them and then returned to the researcher after completion.

Abundant distribution of students by field of study.

Frequency distribution of students by semester.
The data collection instruments were demographic form (including age, gender, place of residence, grade, rank in the class, discipline) and Pittsburgh Sleep Quality Index (PSQI). PSQI is a self-report questionnaire which examines the quality of sleep. It has 18 questions which are classified into seven components: the first component is the subjective sleep quality which is determined with Question 9. The second component is related to delays in falling asleep, where the score is calculated by two questions, the mean score of Question 2 and part of Question 5. The third component deals with sleep duration and is determined by Question 4. The fourth component is related to the efficiency and effectiveness of sleeping in patients. Its score is calculated via dividing the total hours of sleep by total hours in the bed multiplied by 100. Then, the fifth component deals with sleep disorders and is achieved by calculating the mean value of Question 5. The sixth component is related to hypnotic drugs and is determined based on Question 6. Finally, the seventh component captures inadequate performance throughout the day and is determined by two questions (mean scores of Questions 7 and 8). Each question is rated between 0 and 3 points where maximum score for each component is 3. The total scores range of the seven components making up the total score range from 0 to 21. Higher scores represent a lower sleep quality, where a score above 6 indicates poor sleep quality. The reliability and validity of this inventory have also been approved in Iran, where the Cronbach’s alpha coefficient of the questionnaire was 0.78 to 0.82. 18 In another study, Cronbach’s alpha for the Persian version was 0.77. In cut-off point 5, the sensitivity and specificity were 94% and 72%, and in cut-off point 6, they were 85% and 84%, respectively. 19
After collecting the questionnaires and introducing students’ demographic data to a computer using SPSS version 16, the relationship between sleep quality scores and grade point average (GPA high and low) was calculated.
The results indicated that 34 cases (33.3%) of the subjects were male. The mean age of the sample 23.10 ± 3.25, where the mean age for females was 22.46± 2.44 and for males was 24.38± 4.19. The participants in the study came from various disciplines including laboratory science, medicine, pharmacology, emergency medicine, obstetrics, radiology, operating room, health technology, and nursing.
Most students lived in dormitories (50%) and 46.1% at home, with 3.9% living in rental houses. The students' educational level ranged between the third semester and twelfth semester.
Among those participating in the study, 67 patients (65.7%) consumed coffee, 90 cases (88.2%) used tea, and 1 (1%) took a drug.
For comparing the mean scores of students and the component of sleep, Spearman test (non-normal data) was employed, where a significant correlation was observed between GPA and hours taking to fall asleep ( Table 1 ).
The Relationship Between Sleep Components and GPA in KUMS Students
Similarly, there was a relationship between sleep components and tea, coffee, hypnotic drugs, and drug ( Table 2 ).
The Relationship Between Sleep Components and Type of Drink or Drug in KUMS Students Kermanshah
On the other hand, independent t -test between Pittsburgh scores in the two groups did not show any significant differences. Nevertheless, impaired sleep quality was moderate to severe in both groups ( Table 3 ).
The Difference Between the Mean Pittsburg Scores in Two Groups (Students with High and Low GPA)
The results indicated that impaired sleep quality between the two groups was not statistically significant. Although the relationship between sleeping and academic success has been introduced in medical literature since a long time, there still no definitive answer in this case. In a meta-analysis study conducted to examine the impact of sleep quality, sleep duration, and sleepiness on adolescents’ academic performance, although all three variables were related to academic achievement (positive relationship between sleep quality and duration of sleep and negative association with sleepiness), this relationship was very trivial. 1
On the other hand, another systematic review study of descriptive studies concluded that sleep disturbance adversely affects different areas such as general health, social status, and academic performance. However, longitudinal studies are required for a more accurate examination. 20 , 21 In an another systematic review of other authors, the authors concluded that under-sleeping would have an impact on learning of some students, and could have a detrimental effect on academic achievement. 22 Further, another review study also suggests a conclusive recommendation which has to be done to modify sleep so that it can be used for academic success. 23
The present study was conducted to explore whether sleep disorder can influence academic achievement or not. Accordingly, a specific sample of accomplished or unachieved students were selected to compare the quality and quantity of sleep. However, no significant difference was between the two groups. Other studies have reached similar conclusions.
Sweileh and his colleagues in a study on 400 Palestinian students concluded that academic achievement was not correlated with sleep quality. 15 In another study on 189 medical students in Pakistan, there was no significant association between lack of sleep and test scores. 16 In this regard, there is a possibility of sleep disorder in students, and this possibility has been expressed for the lack of academic achievement, but it has not been clearly explained. 11 In another study, sleepiness during the day (not the quality and quantity of sleep) was identified as an independent predictor of academic success. 5 In a similar study again the time it takes to fall sleep and the wake-up time (not the total amount of sleep) were associated with academic success, 14 where the total amount of sleep in adolescents with a dynamic mind was not related to their academic achievement. 24 In contrast to such studies that emphasize lack of association or low association, there are other studies that have observed an inverse relationship between sleep disturbance and academic achievement. In a study on 491 first-, second-, and third-year medical students, there was a correlation between academic performance and the amount of nighttime sleep as well as daytime sleepiness. 25 In a similar study on medical students, lack of sleep at night, late going to bed, and daytime sleepiness had a negative effect on the academic performance of the students. 26 Notably, sleep disturbances are likely to yield a negative impact on academic performance, thereby causing a vicious cycle. 25 , 27 Taken together, the studies suggest that most studies have mentioned poor quality sleep among the majority of students. 3 , 26 , 27 Accordingly, concluding the relationship between common sleep disturbance and academic performance should be done with caution. The reason is that academic success can be affected by different factors including the level of family income, the evolutionary process, intake of supplements and vitamins, family size, social media dependency, addiction to social networks, and social issues. In studies these extraneous factors are not under control, thus emphasizing the fact that the presence or absence of correlation between sleep quality and academic performance should be done with caution and using longitudinal studies.
Limitations
The main limitation of this study was the small sample size, but a specific sampling method was chosen to overcome this shortcoming. Another limitation of the study was not controlling for confounding factors in the study. Based on the results of this study and similar studies, further research should be conducted with a better design.
The results indicated no significant difference between sleep quality in achieved and unachieved academic performance. Nevertheless, to conclude with more certainty, longitudinal studies should be performed to control confounding factors.
Acknowledgments
The authors of this article appreciate the collaborations of the Sleep Disorders Research Center.
Funding Statement
Funding for this research was provided by the Kermanshah University of Medical Sciences, Sleep Disorders Research Center (93026).
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Informed consent obtained from all participants in the study and this study conducted by the Sleep Disorders Research Center. Identity letter obtained from deputy of research and technology to collecting data. Ethics approval was received from the ethics committee of deputy of research and technology – Kermanshah University of Medical Sciences, number 93026 on 6 April 2013.
The authors declare that they have no conflict of interest.
- Search Menu
- Advance Articles
- Supplements
- Editor's Choice
- Virtual Issues
- Virtual Roundtables
- Abstract Supplements
- Basic Science
- Circadian Disorders
- Cognitive, Affective and Behavioral Neuroscience of Sleep
- Neurological Disorders
- Sleep Across the Lifespan
- Sleep and Metabolism
- Sleep Disordered Breathing
- Sleep Health and Safety
- Author Guidelines
- Instructions for Reviewers
- Submission Site
- Open Access Options
- Additional Resources
- Self-Archiving Policy
- About SLEEP
- Editorial Board
- Dispatch Dates
- Permissions
- Advertising & Corporate Services
- Journals Career Network
- Reprints and ePrints
- Sponsored Supplements
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- < Previous
Effects of Sleep Deprivation on Performance: A Meta-Analysis
- Article contents
- Figures & tables
- Supplementary Data
June J. Pilcher, Allen I. Huffcutt, Effects of Sleep Deprivation on Performance: A Meta-Analysis, Sleep , Volume 19, Issue 4, June 1996, Pages 318–326, https://doi.org/10.1093/sleep/19.4.318
- Permissions Icon Permissions
To quantitatively describe the effects of sleep loss, we used meta-analysis, a technique relatively new to the sleep research field, to mathematically summarize data from 19 original research studies. Results of our analysis of 143 study coefficients and a total sample size of 1,932 suggest that overall sleep deprivation strongly impairs human functioning. Moreover, we found that mood is more affected by sleep deprivation than either cognitive or motor performance and that partial sleep deprivation has a more profound effect on functioning than either long-term or short-term sleep deprivation. In general, these results indicate that the effects of sleep deprivation may be underestimated in some narrative reviews, particularly those concerning the effects of partial sleep deprivation.
Email alerts
Citing articles via, looking for your next opportunity.
- Recommend to Your Librarian
- Advertising and Corporate Services
Affiliations
- Online ISSN 1550-9109
- Print ISSN 0161-8105
- Copyright © 2024 Sleep Research Society
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 17 June 2021
Relationship between sleep habits and academic performance in university Nursing students
- Juana Inés Gallego-Gómez 1 ,
- María Teresa Rodríguez González-Moro 1 ,
- José Miguel Rodríguez González-Moro 2 ,
- Tomás Vera-Catalán 1 ,
- Serafín Balanza 1 ,
- Agustín Javier Simonelli-Muñoz 3 &
- José Miguel Rivera-Caravaca 4
BMC Nursing volume 20 , Article number: 100 ( 2021 ) Cite this article
94k Accesses
13 Citations
3 Altmetric
Metrics details
Sleep disorders are composed of a group of diseases of increasing prevalence and with social-health implications to be considered a public health problem. Sleep habits and specific sleep behaviors have an influence on the academic success of students. However, the characteristics of sleep and sleep habits of university students as predictors of poor academic performance have been scarcely analyzed. In the present study, we aimed to investigate sleep habits and their influence on academic performance in a cohort of Nursing Degree students.
This was a cross-sectional and observational study. An anonymous and self-administered questionnaire was used, including different scales such as the ‘Morningness and Eveningness scale’, an author-generated sleep habit questionnaire, and certain variables aimed at studying the socio-familial and academic aspects of the Nursing students. The association of sleep habits and other variables with poor academic performance was investigated by logistic regression. The internal consistency and homogeneity of the ‘sleep habits questionnaire’ was assessed with the Cronbach’s alpha test.
Overall, 401 students (mean age of 22.1 ± 4.9 years, 74.8 % females) from the Nursing Degree were included. The homogeneity of the ‘sleep habits questionnaire’ was appropriate (Cronbach’s alpha = 0.710). Nursing students were characterized by an evening chronotype (20.2 %) and a short sleep pattern. 30.4 % of the Nursing students had bad sleep habits. Regarding the academic performance, 47.9 % of the students showed a poor one. On multivariate logistic regression analysis, a short sleep pattern (adjusted OR = 1.53, 95 % CI 1.01–2.34), bad sleep habits (aOR = 1.76, 95 % CI 1.11–2.79), and age < 25 years (aOR = 2.27, 95 % CI 1.30–3.98) were independently associated with a higher probability of poor academic performance.
Conclusions
Almost 1/3 of the Nursing students were identified as having bad sleep habits, and these students were characterized by an evening chronotype and a short sleep pattern. A short sleep pattern, bad sleep habits, and age < 25 years, were independently associated with a higher risk of poor academic performance. This requires multifactorial approaches and the involvement of all the associated actors: teachers, academic institutions, health institutions, and the people in charge in university residences, among others.
Peer Review reports
Introduction
Sleep is a complex phenomenon resulting from the interaction between the neuroendocrine system, biological clock and biochemical processes, with environmental, social and cultural aspects that are very relevant in the life stages of adolescence and youth [ 1 ]. Indeed, the chronic lack of sleep is a recent worry among adolescents and young university students and it is associated with worse health and clinical outcomes [ 2 , 3 ].
Among biological factors determining sleep, there are “chronotypes” and sleep patterns. The first term refers to the personal preferences of scheduling the sleep-wake cycle, emphasizing three basic chronotypes: morning (early-risers), and evening (night-owls) and those who are intermediate, defined as those who do not have clear preferences towards any of the extreme schedules for the fulfilling of their activities [ 4 ]. The sleep pattern refers to the personal schedule of bedtime and wake-up time. In this sense, a circadian rhythm is a natural, internal process, driven by a circadian clock that repeats roughly every 24 h and regulates the sleep-wake cycle [ 5 ].
On the other hand, the sleep habits are in the intersection between biological and cultural values. Endogenous, exogenous or environmental factors are included here, as well as those activities that are developed by the population to induce or maintain sleep, with its study and care becoming a challenge for Nursing [ 6 ]. Currently, spontaneous abusive behaviors regarding sleep habits are becoming frequent, leading to a state of chronic sleep deprivation, which translates to fatigue and somnolence during the day [ 7 ]. Hence, there is a high prevalence of sleep disorders in university students, especially those that affect the wake-sleep rhythm [ 2 ]. For this reason,the interest in establishing relationships between sleep and cognitive processes such as memory, learning ability and motivation, has gained attention during the last years. However, studies that relate sleep with academic problems are scarce, despite previous authors have shown that the reduction of sleep time in teenagers and university students was associated with poor academic performance, accidents and obesity [ 8 , 9 ]. Since good-quality sleep does not only imply sleeping well at night but also an adequate level of attention during the day for performing different tasks, appropriate sleep has an influence in efficient learning processes in university students [ 10 , 11 , 12 ].
Although some scientific evidence has shown a relationship between sleep and low academic performance [ 13 , 14 ], so far, there are no questionnaires to specifically evaluate sleep habits in Nursing students. Considering that this population has special characteristics, they are mostly young, combine hospital training at the same time they attend classes at the university, they present lifestyles that can negatively influence the academic performance. To study the sleep habits using a specific tool, in addition to analyze the sleep pattern and chronotype, could help to identify students with inappropriate sleep habits for developing interventions to modify these habits. This might have a positive impact on their academic performance and avoid potentially serious negative consequences for their physical and mental health. In the present research, we aimed (a) to design a ‘sleep habits questionnaire’, (b) to analyze the sleep habits, sleep pattern and chronotype, and (c) to investigate sleep habits and their influence on academic performance, in a cohort of Nursing Degree students.
Design and study population
This was an observational, prospective and cross-sectional study involving Nursing students, all of them distributed among the 4 years of the Nursing Degree. There were no inclusion criteria, i.e. all Nursing students were suitable for the study, unless those who did not attend class on the day of data collection, or those who did not wish to participate (from 420 students, 19 refused to participate in the study). The study was fully carried out during the first semester of the 2019–2020 academic year.
Study Variables
Circadian rhythm: the reduced “horne & östberg morningness-eveningness questionnaire”.
Preferences of schedule for the sleep-wake cycle and its influence on academic performance were assessed using the reduced version of the Horne & Östberg Morningness-Eveningness Questionnaire (rMEQ) proposed by Adan & Almirall [ 15 ], translated to Spanish, that is composed of 5 items. The score determines the following five types of schedule: clearly morning type (22–25 points), moderately morning type (18–21 points), no preference (12–17 points), moderately evening type (8–11 points), and clearly evening type (4–7 points). The internal consistency of the circadian rhythm scale assessed using the rMEQ by Adan & Almirall is good, as the scores from all the items are correlated among themselves [ 15 , 16 ].
Sleep habits questionnaire
For the initial design of the sleep habits questionnaire, a panel of 10 voluntary experts was included. This panel was composed of 5 registered nurses and 5 physicians, with a minimum of 5 years of experience in sleep. All of them were interviewed and informed individually about the study. Items composing of the questionnaire were obtained according to the scientific literature and the main factors influencing sleep habits as the discretion of the expert panel [ 14 , 17 , 18 ]. Eleven questions were finally included in a self-reported questionnaire, each ranging from 1 to 4 (never (1), sometimes (2), usually (3), always (4)) ( Supplementary file ). Sleep habits, including sleep routines, study schedule preference, and napping were also evaluated. The overall score of the questionnaire ranges from 11 to 44 points, with the highest scores indicating the worst sleep habits. As there is no specific cut-off point for this questionnaire, students over the fourth quartile (4Q, i.e. ≥25 points) were categorized as having inappropriate habits. Therefore, these Nursing students were included in the “bad sleeping habits” group.
- Academic performance
The academic performance was measured by the ratio “failed exams/performed exams” and checked in the student’s academic records. A good academic performance was considered if the final grade of every exam completed during the Nursing Degree was ≥ 5 (in a 0–10 range, where an exam is considered passed if the score is ≥ 5).
Other variables
Other variables such as gender, age and hours of sleep (sleep pattern), were analyzed. To describe the sleep pattern of the Nursing students, we used the classification described by Miró et al. (2002) [ 19 ]. This classification was composed of three categories as a function of the hours slept, so that we found subjects that had a short sleep pattern (< 6 h per day), subjects with a long sleep pattern (≥ 9 h per day), and subjects with an intermediate sleep pattern (6–9 h per day).
Ethical considerations
The study protocol was approved by an accredited Ethics Committee (Reference: CE-6191) and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All students were informed and gave consent to participation in the study. The anonymity and confidentiality were guaranteed.
Statistical analysis
The sample size was calculated by a non-probabilistic sampling technique using Ene 2.0 (GlaxoSmithKline) with a precision ± 5 % and α error = 0.05. This calculation was based on the estimation that the prevalence of bad sleep habits in Nursing students of our university was 30.4 %, which resulted in a minimum sample of 229 subjects.
Categorical variables were expressed as frequencies and percentages. Continuous variables were presented as mean ± standard deviation (SD) or median and interquartile range (IQR), as appropriate.
The Pearson Chi-squared test was used to compare proportions whereas comparison of continuous variables was performed using the Student t test. Correlations between different scales were performed using the Pearson’s correlation test.
In order to investigate if sleep habits and other variables were independently associated with poor academic performance, a logistic regression model (with odds ratios [OR] and two-sided 95 % confidence intervals [CI]) was performed. To measure the internal consistency and homogeneity of the sleep habits questionnaire, the Cronbach’s alpha test was performed.
A p -value < 0.05 was accepted as statistically significant. Statistical analyses were performed using SPSS v. 21.0 (SPSS, Inc., Chicago, IL, USA).
We included 401 Nursing students (100 students from 1st year, 105 from 2nd year, 101 from 3rd year, and 95 from 4th year) in the study. The students were characterized for being predominantly females (300, 74.8 %), with a mean age of 22.1 ± 4.9 years, and the majority of them (88.5 %) were singles.
Sleep habits of the Nursing students were examined using our previously designed (as described in the Methods section) self-reported ‘sleep habits questionnaire’. The homogeneity of the questionnaire was appropriate, with a Cronbach’s alpha value of 0.710. The mean score in the questionnaire was 22.3 ± 3.9, and 30.4 % of the Nursing students had bad sleep habits (i.e. score > 4Q), which were characterized by a clear preference of studying at night, easily lose a night of sleep for work-related or academic tasks that imply staying up late, and showing difficulties in maintaining sleep routines.
Table 1 shows the summarized results for each question of the sleep habits questionnaire.
The Nursing students in our sample were characterized by an evening chronotype (20.2 %, 81) and a short sleep pattern (i.e. <6 h of sleep daily), with 51.1 % (205) of the students sleeping less than 6 h/day, 42.1 % (169) sleeping 6–9 h/day, and 6.7 % (27) sleeping more than 9 h/day. The mean duration of sleep found in the Nursing students was 6.52 ± 1.4 h.
Of note, most of the Nursing students that had an evening chronotype were < 25 years old (22.2 %, p = 0.011). In addition, age showed a positive association with circadian rhythm and as age increased, the students tended to have a predominantly morning chronotype ( R = 0.223, p < 0.001). Nursing students < 25 years of age had also worse sleep habits according to the sleep habits questionnaire than those ≥ 25 years (22.61 ± 3.79 vs. 21.19 ± 4.37, p = 0.005). A negative correlation was found between the overall sleep habits questionnaire score and age as a continuous variable ( R = -0.105, p = 0.03).
In addition, 29.5 % of patients that had bad sleep habits ( p = 0.001), and 23.9 % that had poor academic performance ( p = 0.020), had also an evening chronotype (Table 2 ). A significant negative correlation was found between the sleep pattern and sleep habits ( R = -0.293, p < 0.001), and between circadian rhythm and sleep habits, hence Nursing students with good sleep habits have predominantly a morning circadian rhythm ( R = -0.201, p < 0.001).
Regarding the academic performance, 93 % (373) of the Nursing students attended all the exams planned, and 47.9 % (192) of the students showed poor academic performance. When we investigated specifically if the sleep habits, as assessed by the ‘sleep habits questionnaire’, influenced the academic performance, we found that 32 % (140) of the Nursing students that had bad sleep habits obtained poor academic results ( p < 0.001). Those that had the worst academic results were the ones that did not have a regular hour for waking up and going to sleep (2.66 ± 1.03, p = 0.031), presented difficulties to maintain the sleep during the night (1.73 ± 0.77, p = 0.003), and preferred to study for an exam at night (1.33 ± 0.48, p = 0.030), as well as going to bed late to obtain better results (1.46 ± 0.51, p = 0.041). Also, those students with poorer academic results where those listening to music before going to bed (1.84 ± 1.10, p = 0.007), and going out at night even if they had to get-up early the next day (1.58 ± 0.72, p = 0.012). Overall, those Nursing students whose work or academic activities entailed going to bed late to attain their objectives, had the lowest academic performance (2.25 ± 1.01, p = 0.001). Lastly, we can confirm that the Nursing students that had better academic performance were the ones who had the best sleep habits. Indeed, the overall ‘sleep habits questionnaire’ score was significantly lower compared to those Nursing students who had poor academic performance (21.91 ± 3.90 vs. 24.18 ± 3.55, p < 0.001) (Table 3 ).
Finally, the profile of Nursing students with more failed courses was characterized by an evening circadian rhythm ( R = -0.134, p = 0.007), bad sleep habits ( R = 0.216, p < 0.001), and less hours of sleep daily ( R = -0.211, p < 0.001).
To confirm these observations, a multivariate logistic regression analysis was performed. Therefore, a short sleep pattern (adjusted OR = 1.53, 95 % CI 1.01–2.34), bad sleep habits (adjusted OR = 1.76, 95 % CI 1.11–2.79), and age < 25 years (adjusted OR = 2.27, 95 % CI 1.30–3.98) were independently associated with a higher probability of poor academic performance (Table 4 ).
Sleep is an excellent indicator of the health status and an element that favors good quality of life [ 20 ], but entering university is a change that highly impacts the student in every dimension, including sleep habits [ 21 , 22 ]. A potential barrier for maximizing performance during the university stage is the irregular sleep schedule, which lead to sleep deficit and high prevalence of somnolence during the day [ 23 ]. A review by Shochat et al. (2014) [ 24 ] examined the consequences of lack of sleep among Nursing students, and confirmed the relationship between sleep disorders and changes in sleep patterns with a reduced academic performance. Other studies have established that sleep has an integral role in learning and memory consolidation [ 25 , 26 ]. Therefore, despite some scientific evidence has shown a relationship between sleep and low academic performance [ 13 , 14 ], the originality of our study was to examine the influence that sleep characteristics exert (chronotypes and sleep patterns), as well as sleep habits of the university population on academic performance.
Overall, the academic performance of our Nursing students was suboptimal. When analyzing how sleep pattern, sleep habits, and circadian rhythms influenced this academic performance, we observed that all of them may be determine factors for learning, as other studies have done [ 27 ].
Concerning the sleep pattern, it should be noted that most of the students enrolled in the Nursing Degree slept less than 6 h per day. Of note, our results seem to establish a relationship between the hours slept and the academic performance during the first semester, as gathered from the academic records. This finding is in accordance to observations by other authors in university students from Medicine [ 9 ], Pharmacy [ 2 ] or Nursing [ 28 ], which also showed evidence between the hours slept and the academic achievement. In a previous study, we already observed that university students from the Faculty of Nursing attributed the hours slept with academic performance [ 29 ]. Indeed, it should be highlighted that chronic lack of sleep is not only associated with alterations of attention and academic performance, but also to a series of adverse consequences for health such as risky behaviors, depression, anxiety, alterations in social relations, and obesity, among others [ 30 ].
In addition, our study has evidenced how the sleep habits directly influenced the academic performance of these Nursing students, and approximately 1/3 of the students with bad sleep habits obtained poor academic results. Certainly, the sleep pattern and inadequate sleep habits could be related. Good sleep hygiene includes aspects such as a regular sleep-wake schedule, adequate environment, avoiding stimulating activities before going to bed, and limiting the use of technology in bed or immediately before going to bed. In the present study, 30.4 % of the students had bad sleep habits, characterized by having a clear preference for studying at night, often losing a night of sleep for work or academic activities that imply go to bed late, and show difficulties in maintaining sleep routines. An important proportion of our Nursing degree students declared that they watched television, listened to music, worked or read academic documents during the last hour before going to bed. In this sense, LeBourgeois et al. (2017) [ 31 ] have described the university population as great consumers of technology, and have associated the frequent use of technology before going to bed with problems to sleep and daytime somnolence.
Finally, age was another factor that should be considered in the analysis of sleep habits. According to our results, the Nursing students that were < 25 years of age had the worst sleep habits and used to have more difficulties in maintaining sleep routines, modifying them on the weekends and holidays, preferring to stay up late to obtain better study results, and going out at night without considering that they had to get up early. As other studies [ 21 ], we observed that social activities were a priority in the life of the university adolescents and the substituting of hours of sleep for enjoying and sharing activities with friends and classmates did not constitute a problem for them. These behaviors were added to the physiological delay of the start of sleep that is typical in this stage of life and might unleash deprivation or a chronic deficit of sleep, maintained throughout the entire week. The students then tried to compensate for this lack of sleep by increasing their hours of sleep during the weekend. We agree with previous studies that this circumstance, far from minimizing or compensating the effects of sleep deprivation, aggravates them, worsening the pattern and the quality of sleep of the students [ 22 ].
Further, we found an association between age and circadian type. We observed that most of the university students with evening chronotypes were aged < 25, had bad sleep habits, and a poor academic performance. Physiologically, adolescents and adults tend to have delayed circadian preferences and are “lovers of the night” [ 23 ]. In our study, 20.2 % of students had an evening chronotype, which is lower than that reported in other studies, where 59 % of the students between 18 and 29 years of age described themselves as night owls [ 32 ]. Our results also showed a clear normalization of the evening behaviors of the students. These data are in agreement with other authors who highlighted the influence exerted by the aforementioned normalization of evening habits among the youth on the quality of sleep, leading to a medium to long-term sleep deficit [ 20 ]. As Crowley et al. (2018) [ 33 ], we think that evening behavior leads to asynchrony between the biological rhythm and the social life of the student, having negative consequences on the academic performance. However, how this really affects academic results requires extending researches, since the circadian rhythm was not significantly associated with academic performance.
The results of this study evidence the need to seriously take into consideration the sleep deficits that are associated with inadequate sleep habits, with the aim of developing preventative and educational initiatives to improve the sleep habits of the university population. The challenge ahead starts with the social awareness of the importance of having good-quality sleep since many times, adequate knowledge about sleep does not translate into a change of sleep habits [ 23 ].
Limitations
Some limitations should be noted. Due to the cross-sectional design of the study, we could not establish an exact causal relationship between sleep pattern and academic performance. In addition, it should be note that the ‘sleep habits questionnaire’ is a subjective questionnaire, and therefore the result could be biased if the student did not answer honestly. Another limitation is the difficulty in conceptualizing academic performance, due to its complex and multi-causal character, where many factors intervene. The factors include attitudes, habits, the character of the staff, methodologies, family environment, organization of the educational system, socio-economic condition, as well as other social, economic, and psychological aspects [ 34 ]. Finally, the study was conducted only in Nursing students, so our results must be prospectively validated in University students from a larger variety of academic sectors. Similarly, this study was conducted in a single University, so more studies involving other Universities are also necessary. Despite these circumstances, we believe that our hypothesis that the duration of sleep could lead to better academic performance is based on current scientific data.
Using the 11-item ‘sleep habits questionnaire’, 30.4 % of the Nursing students were identified as having bad sleep habits. In addition, Nursing students included in this research were characterized by an evening chronotype and a short sleep pattern. Regarding academic performance, half of the Nursing students showed a poor one. A short sleep pattern, bad sleep habits, and younger age, were independently associated with a higher risk of poor academic performance. This requires multifactorial approaches and the involvement of all the associated actors: teachers, academic institutions, health institutions, and the people in charge in university residences, among others.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Matricciani L, Bin YS, Lallukka T, Kronholm E, Wake M, Paquet C, Dumuid D, Olds T. Rethinking the sleep-health link. Sleep Health. 2018;4(4):339–348. doi: https://doi.org/10.1016/j.sleh.2018.05.004 .
Article PubMed Google Scholar
Zeek ML, Savoie MJ, Song M, Kennemur LM, Qian J, Jungnickel PW, Westrick SC. Sleep Duration and Academic Performance Among Student Pharmacists. Am J Pharm Educ. 2015;79(5):63. doi: https://doi.org/10.5688/ajpe79563 .
Article PubMed PubMed Central Google Scholar
Dijk DJ, Landolt HP. Sleep Physiology, Circadian Rhythms, Waking Performance and the Development of Sleep-Wake Therapeutics. Handb Exp Pharmacol. 2019;253:441–481. doi: https://doi.org/10.1007/164_2019_243 .
Article CAS PubMed Google Scholar
Zerbini G, Merrow M. Time to learn: How chronotype impacts education. Psych J. 2017;6(4):263–276. doi: https://doi.org/10.1002/pchj.178 .
Huang W, Ramsey KM, Marcheva B, Bass J. Circadian rhythms, sleep, and metabolism. J Clin Invest. 2011;121(6):2133–41. doi: https://doi.org/10.1172/JCI46043 .
Owens H, Christian B, Polivka B. Sleep behaviors in traditional-age college students: A state of the science review with implications for practice. J Am Assoc Nurse Pract. 2017; 29(11):695–703. doi: https://doi.org/10.1002/2327-6924.12520 .
Becerra MB, Bol BS, Granados R, Hassija C. Sleepless in school: The role of social determinants of sleep health among college students. J Am Coll Health. 2020; 68(2):185–191. doi: https://doi.org/10.1080/07448481.2018.1538148 .
Kozak AT, Pickett SM, Jarrett NL, Markarian SA, Lahar KI, Goldstick JE. Project STARLIT: protocol of a longitudinal study of habitual sleep trajectories, weight gain, and obesity risk behaviors in college students. BMC Public Health. 2019;19(1):1720. doi: https://doi.org/10.1186/s12889-019-7697-x .
El Hangouche AJ, Jniene A, Aboudrar S, Errguig L, Rkain H, Cherti M, Dakka T. Relationship between poor sleep quality, excessive daytime sleepiness and poor academic performance in medical students. Adv Med Educ Pract. 2018; 9: 631–638. doi: 10.2147 / AMEP.S162350.
Article Google Scholar
Makino K, Ikegaya Y. Learning Paradigms for the Promotion of Memory, and Their Underlying Principles. Brain Nerve. 2018;70(7):821–828. doi: https://doi.org/10.11477/mf.1416201083 .
Haile YG, Alemu SM, Habtewold TD. Insomnia and Its Temporal Association with Academic Performance among University Students: A Cross-Sectional Study. Biomed Res Int. 2017;2017:2542367. doi: https://doi.org/10.1155/2017/2542367 .
Gianfredi V, Nucci D, Tonzani A, Amodeo R, Benvenuti AL, Villarini M, Moretti M. Sleep disorder, Mediterranean Diet and learning performance among nursing students: inSOMNIA, a cross-sectional study. Ann Ig. 2018; 30(6):470–481. doi: https://doi.org/10.7416/ai.2018.2247 .
Zhao K, Zhang J, Wu Z, Shen X, Tong S, Li S. The relationship between insomnia symptoms and school performance among 4966 adolescents in Shanghai, China. Sleep Health. 2019;5(3):273–279. doi: https://doi.org/10.1016/j.sleh.2018.12.008 .
Alotaibi AD, Alosaimi FM, Alajlan AA, Bin Abdulrahman KA. The relationship between sleep quality, stress, and academic performance among medical students. J Family Community Med. 2020;27(1):23–28. doi: https://doi.org/10.4103/jfcm.JFCM_132_19 .
Adan, A.; Almirall, H. Horne & Östberg Morningnees-Eveningnees Questionnaire: a reduced scale. Pers Individ Dif. 1991, 12, 241–53. doi: https://doi.org/10.1016/0191-8869(91)90110-W
Randler C. German version of the reduced Morningness-Eveningness Questionnaire (rMEQ). Biological Rhythm Research. 2013;44(5):730–736. doi: https://doi.org/10.1080/09291016.2012.739930
Peach H, Gaultney JF. Charlotte Attitudes Towards Sleep (CATS) Scale: A validated measurement tool for college students. J Am Coll Health. 2017;65(1):22–31. doi: https://doi.org/10.1080/07448481.2016.1231688 .
Al-Kandari S, Alsalem A, Al-Mutairi S, Al-Lumai D, Dawoud A, Moussa M. Association between sleep hygiene awareness and practice with sleep quality among Kuwait Zhao University students. Sleep Health. 2017;3(5):342–347. doi: https://doi.org/10.1016/j.sleh.2017.06.004 .
Miró E, Iáñez MA, Cano-Lozano MC. Sleep and health patterns. Int J Clin Health Psychol. 2002;2:301–326.
Google Scholar
Zohal MA, Yazdi Z, Kazemifar AM, Mahjoob P, Ziaeeha M. Sleep Quality and Quality of Life in COPD Patients with and without Suspected Obstructive Sleep Apnea. Sleep Disord. 2014;2014:508372. doi: https://doi.org/10.1155/2014/508372.21
Núñez P, Perillan C, Arguelles J, Diaz E. Comparison of sleep and chronotype between senior and undergraduate university students. Chronobiol Int. 2019;36(12):1626–1637. doi: https://doi.org/10.1080/07420528.2019.1660359 .
Phillips AJK, Clerx WM, O’Brien CS, Sano A, Barger LK, Picard RW, Lockley SW, Klerman EB, Czeisler CA. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci Rep. 2017;7(1):3216. doi: https://doi.org/10.1038/s41598-017-03171-4 .
Niño García JA, Barragán Vergel MF, Ortiz Labrador JA, Ochoa Vera ME, González Olaya HL. Factors Associated with Excessive Daytime Sleepiness in Medical Students of a Higher Education Institution of Bucaramanga. Rev Colomb Psiquiatr. 2019;48(4):222–231. doi: https://doi.org/10.1016/j.rcp.2017.12.002 .
Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014;18:75–87. doi: https://doi.org/10.1016/j.smrv.2013.03.005
Yang G, Lai CS, Cichon J, Ma L, Li W, Gan WB. Sleep promotes branch-specific formation of dendritic spines after learning. Science. 2014;344(6188):1173–8. doi: https://doi.org/10.1126/science.1249098 .
Article CAS PubMed PubMed Central Google Scholar
Bruin EJ, van Run C, Staaks J, Meijer AM. Effects of sleep manipulation on cognitive functioning in adolescents: a systematic review. Sleep Med Rev. 2017; 32: 45–57. doi: https://doi.org/10.1016/j.smrv.2016.02.006 .
Arbabi T, Vollmer C, Dörfler T, Randler C The influence of timing and intelligence on academic performance in elementary school is mediated by awareness, sleep midpoint and motivation. Chronobiol Int. 2015;32(3):349–57. doi: https://doi.org/10.3109/07420528.2014.980508
Menon B, Karishma HP, Mamatha IV. Sleep quality and health complaints among nursing students. Ann Indian Acad Neurol. 2015;18(3):363–4. doi: https://doi.org/10.4103/0972-2327.157252 .
Simonelli-Muñoz AJ, Balanza S, Rivera-Caravaca JM, Vera-Catalán T, Lorente AM, Gallego-Gómez JI. Reliability and validity of the student stress inventory-stress manifestations questionnaire and its association with personal and academic factors in university students. Nurse Educ Today. 2018;64:156–160. doi: https://doi.org/10.1016/j.nedt.2018.02.019 .
Begdache L, Kianmehr H, Sabounchi N, Marszalek A, Dolma N. Principal component regression of academic performance, substance use and sleep quality in relation to risk of anxiety and depression in young adults. Trends Neurosci Educ. 2019;15:29–37. doi: https://doi.org/10.1016/j.tine.2019.03.002 .
LeBourgeois MK, Hale L, Chang AM, Akacem LD, Montgomery-Downs HE, Buxton OM. Digital Media and Sleep in Childhood and Adolescence. Pediatrics. 2017;140(Suppl 2):S92-S96. doi: https://doi.org/10.1542/peds.2016-1758J .
Talero-Gutiérrez C, Durán-Torres F, Pérez-Olmos I. Sleep: general characteristics Physiological and pathophysiological patterns in adolescence. Revista Ciencias de la Salud. 2013;11(3):333–348.
Crowley SJ, Wolfson AR, Tarokh L, Carskadon MA. An update on adolescent sleep: New evidence informing the perfect storm model. J Adolesc. 2018;67:55–65. doi: https://doi.org/10.1016/j.adolescence.2018.06.001 .
Suardiaz-Muro M, Morante-Ruiz M, Ortega-Moreno M, Ruiz MA, Martín-Plasencia P, Vela-Bueno A. Sleep and academic performance in university students: a systematic review. Rev Neurol. 2020;71(2):43–53. doi: https://doi.org/10.33588/rn.7102.2020015 .
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Faculty of Health Sciences, Catholic University of Murcia, 30107, Murcia, Spain
Juana Inés Gallego-Gómez, María Teresa Rodríguez González-Moro, Tomás Vera-Catalán & Serafín Balanza
Department of Pneumology, Alcalá de Henares, Hospital Universitario Príncipe de Asturias, 28805, Madrid, Spain
José Miguel Rodríguez González-Moro
Department of Nursing, Physiotherapy and Medicine, Faculty of Health Sciences,, University of Almería, Ctra. Sacramento, s/n 04120 La Cañada de San Urbano, 04007, Almería, Spain
Agustín Javier Simonelli-Muñoz
Department of Cardiology, Hospital Clínico Universitario Virgen de la Arrixaca, Universidad de Murcia, Instituto Murciano de Investigación Biosanitaria (IMIB-Arrixaca), CIBERCV, 30120, Murcia, Spain
José Miguel Rivera-Caravaca
You can also search for this author in PubMed Google Scholar
Contributions
JIGG, AJSM, MTRGM, TVC, and JMRGM conceptualized and designed the current study, and were major contributors in the data collection, and reviewing of the manuscript. JIGG and AJSM performed data curation, formal analysis, data interpretation, and writing of the original draft manuscript. JMRC and SB were major contributors in the writing and statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Agustín Javier Simonelli-Muñoz .
Ethics declarations
Ethics approval and consent to participate.
The Research Ethics Committee of the Catholic University of Murcia, Spain, approved the current study (Reference: CE-6191). Along with the questionnaire, the researchers provided a letter stating the purpose and methods of the study, the voluntary nature of participation, and the confidentiality of responses. Participants signed an informed consent form.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gallego-Gómez, J.I., González-Moro, M.T.R., González-Moro, J.M.R. et al. Relationship between sleep habits and academic performance in university Nursing students. BMC Nurs 20 , 100 (2021). https://doi.org/10.1186/s12912-021-00635-x
Download citation
Received : 28 February 2021
Accepted : 10 June 2021
Published : 17 June 2021
DOI : https://doi.org/10.1186/s12912-021-00635-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sleep habits
- Circadian rhythm
- Sleep pattern
- Nursing students
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
Media Advisory
Tuesday, April 2, 2024
Irregular sleep and late bedtimes associated with worse grades for high school students
NIH-funded study also links later bed and wake times with school conduct problems.
Irregular sleep and late bedtimes are linked to worse grades and more school-related behavioral problems among teens, suggests a study funded by the National Institutes of Health (NIH). The authors stated that interventions to promote regular sleep schedules may boost adolescents’ academic performance.
The study, conducted by Gina Marie Mathew, Ph.D., and Lauren Hale, Ph.D., of Stony Brook University and colleagues, appears in Sleep . Funding was provided by NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Researchers analyzed data from nearly 800 adolescents participating in a larger study . Participants provided information on grades and school-related behavioral issues. They also wore a wrist accelerometer (a device that records the wearer’s movements) for a week so that study staff could estimate their sleep patterns.
Participants with more variable bedtimes had a greater chance of receiving a D or lower during the last grading period, compared to those with more consistent bedtimes. Adolescents who went to bed later, got up later or varied the number of hours they slept per night had fewer classes in which they received an A. Adolescents were more likely to be suspended or expelled in the last two years if they got up later, varied the number of hours they slept each night or if they varied the time they went to bed each night.
The authors theorized that delayed bedtimes could result in late school arrivals, which could affect learning and behavior. In addition, many adolescents are biologically inclined to later hours, which conflict with early school start times.
Randy Capps, Ph.D., of NICHD’s Population Dynamics Branch, is available for comment.
Mathew, G, et al. Actigraphic sleep dimensions and associations with academic functioning among adolescents. Sleep (2024).
About the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) : NICHD leads research and training to understand human development, improve reproductive health, enhance the lives of children and adolescents, and optimize abilities for all. For more information, visit https://www.nichd.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Connect with Us
- More Social Media from NIH
Inconsistent Sleep Patterns in High School Linked to Academic Struggles

- Share article
From homework and studying to sports, clubs, and part-time jobs, students often maintain packed and constantly shifting schedules in high school. But those schedules can keep students from getting to bed at a consistent time.
New research in Sleep, the peer-reviewed journal of the Sleep Research Society, suggests irregular sleep—not just overall amount—can play a significant role in students’ academic and behavior problems in high school.
The study was part of ongoing research funded by the National Institute of Child Health and Human Development using data from the longitudinal Future of Families and Child Well-Being study, which tracks the development of 5,000 urban children from birth to age 22. In the current study, Stony Brook University researchers led by Gina Marie Mathew and Lauren Hale analyzed data from about 800 teenagers who reported their school grades and behavior and also wore wrist devices that allowed researchers to track their sleep patterns over several days.

Across the board, the teenagers were sleep deprived. On average, they got about 7.5 hours of sleep a night—somewhat normal for adults but about 1.5 hours less than the American Academy of Pediatrics recommends for adolescents.
A separate 2023 study from the federal Centers for Disease Control and Prevention found students who get at least eight hours of sleep a night have better mental health and academic achievement. But prior studies find teenagers’ sleep habits have grown less consistent and late-night screen time has risen in the last decade.
While adults (including teachers and principals ) can also suffer from irregular sleep, high schoolers are particularly vulnerable, Mathew said, because sleep cycles naturally change during adolescence.
“Instead of wanting to go to bed at nine, you could want to sleep but only at 11:00 p.m. or maybe even 12:00 a.m.,” she said. “But then, especially if you have an early school start time, you’ll get short sleep during the school week and then on the weekend try to make it up by sleeping in later. And so this shifting of bedtimes and wake times across the week increases sleep variability.”
However, researchers found students’ sleep schedules were much more closely linked to their academic progress and behavior than the overall amount they slept. In particular, students who more frequently went to bed later or varied the number of hours they slept, earned an A in fewer classes by the end of the year. Students with more irregular sleep were also more likely to earn a D or worse in multiple classes by the end of the year.
Students who slept inconsistent hours were also more likely to report getting in trouble at school and were more likely to have been suspended or expelled in the last two years.
“Sleep variability is really coming up now as being so important for so many aspects of health and well-being—mental health, for example, and cardiometabolic health,” Mathew said.
It’s not yet clear how much students’ sleep schedules can change before their learning and emotions start to suffer. Although students of color and low-income students are more likely to be sleep deprived overall, the researchers in this study did not look at whether unstable sleep patterns affect some groups of students more than others.
Still, the study may provide additional evidence in favor of later school start times, a schedule change that has been gaining traction in some districts and among educators . While the average secondary school start time in 2023 was 8:07 a.m. (and 10 percent start by 7:30 a.m.) the American Academy of Pediatrics recommends start times no earlier than 8:30 a.m. for adolescents.
“If anything, it supports the idea that we should be shifting school start times to be more aligned with [teenagers’] rhythms and how they work best,” Mathew said.
Sign Up for The Savvy Principal
Edweek top school jobs.
Sign Up & Sign In

ORIGINAL RESEARCH article
Prevalence and related factors of sleep quality among chinese undergraduates in jiangsu province: multiple models' analysis.

- 1 Key Laboratory of Human Genetics and Environmental Medicine, School of Public Health, Xuzhou Medical University, Xuzhou, China
- 2 Department of Respiratory Diseases, The Affiliated Huai'an Hospital of Xuzhou Medical University, The Second People's Hospital of Huai'an, Huai'an, Jiangsu, China
- 3 Department of Dermatology, The Affiliated Huai'an Hospital of Xuzhou Medical University, The Second People's Hospital of Huai'an, Huai'an, Jiangsu, China
- 4 Department of Biostatistics, School of Public Health, Xuzhou Medical University, Xuzhou, China
- 5 Center for Medical Statistics and Data Analysis, Xuzhou Medical University, Xuzhou, China
Background and aims: In China, a significant number of undergraduates are experiencing poor sleep quality. This study was designed to investigate the prevalence of poor sleep quality and identify associated factors among undergraduates in Jiangsu Province, China.
Methods: A total of 8,457 participants were collected in 2022 using whole-group convenience sampling. The factors studied included basic demographics, family and social support, personal lifestyles, physical and mental health, mobile phone addiction index (MPAI), and the Connor-Davidson resilience scale (CD-RISC). The Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality. Four models, including weighted multiple linear regression, binary logistic regression, weighted linear mixed model, and logistic regression with random effects, were applied to identify associated factors for sleep quality.
Results: Of the 8,457 participants analyzed, 26.64% (2,253) were classified into the poor sleep quality group with a PSQI score >7. No significant relationship was found between sleep quality and gender, native place, economic level of family, physical exercise, dormitory light, dormitory hygiene, and amativeness matter. Risk factors for sleep quality identified by the four models included lower CD-RISC, higher MPAI, fourth grade or above, smoking, drinking, greater academic pressure, greater employment pressure, roommate sleeping late, noisy dormitory, poorer physical health status, poorer mental health status, and psychological counseling.
Conclusions: These findings provide valuable insights for university administrators, enabling them to better understand the risk factors associated with poor sleep quality in undergraduates. By identifying these factors, administrators can provide targeted intervention measures and counseling programs to improve students' sleep quality.
Introduction
Sleep is a fundamental physiological process that is essential for our overall health. It is also important for our cognitive, emotional, and physical systems ( Baranwal et al., 2023 ). In recent years, sleep quality has declined among undergraduates and received attention from the public and academics ( Wang et al., 2016 ; Ahmed et al., 2020 ; Li Y. et al., 2020 ). Unfortunately, a significant number of undergraduates are experiencing poor sleep quality. In some provinces of China, the proportion of undergraduates with poor sleep quality has crossed more than 30.0%; for example, the proportions in Jilin, Guizhou, and Hong Kong were 33.8%, 53.7%, and 57.5%, respectively ( Suen et al., 2008 ; Li Y. et al., 2020 ; Zhou et al., 2022 ). Sleep quality among undergraduate students has also been poor in other countries such as Ethiopia (57.5%) and India (51.0%) ( Lemma et al., 2012 ; Ghrouz et al., 2019 ). Some studies focusing on medical students also found a high prevalence of poor sleep quality−52.4% in Greece during COVID-19 ( Eleftheriou et al., 2021 ), 76.0% in Saudi Arabia ( Almojali et al., 2017 ), and 27.8% in Inner Mongolia Medical University of China ( Wang et al., 2016 ). In Jiangsu Province, the status of sleep quality among undergraduates is still unknown, and it would be very interesting to investigate the prevalence of poor quality and identify the associated factors in this population.
Research has indicated that sleep deprivation can lead to metabolic disorders and negative effects, such as increased metabolite levels, which can lead to poor memory, poor concentration, lower academic performance, and emotional fluctuations ( Durmer and Dinges, 2005 ; Curcio et al., 2006 ; Basner et al., 2013 ; Davies et al., 2014 ; Lo et al., 2016 ; St-Onge, 2017 ; Gerhardsson et al., 2019 ; Vaccaro et al., 2020 ). In addition, poor sleep quality can also increase the risk of developing mental health problems such as anxiety and depression ( Almojali et al., 2017 ; Shao et al., 2020 ). Given the importance of sleep in maintaining wellbeing, it is essential to understand the factors that contribute to poor sleep quality among undergraduates. Additionally, it is also imperative to identify potential solutions to improve their sleep habits and reduce the negative effects.
Some studies have shown that sleep quality among Chinese undergraduates was a result of various factors. A cross-sectional study reported a few risk factors such as poor academic performance, interpersonal relationship, skipping breakfast, and higher grades ( Wang et al., 2016 ). Another study found that being a freshman, alcohol use, gambling, exercising for more than 30 min a week on <1 day, satisfaction with parental love, and harmonious relationship with classmates were risk factors, while no learning pressure, never having self-injurious behaviors, and harmonious family relationship were protective factors ( Li Y. et al., 2020 ). A gender-specific study in China identified some risk factors for poor sleep quality that were related to weak physical condition and smoking in males, while noisy dormitory, skipping breakfast, drinking coffee, playing games, bad physical condition, and severe academic stress led to poor sleep quality in females ( Zhou et al., 2022 ). A cluster randomized-controlled trial in China showed that good dormitory sleep environments could maintain good sleep quality ( Li et al., 2022 ). In addition, the use of electronic products was also related to poor sleep quality ( Demirci et al., 2015 ; Li L. et al., 2020 ). For example, using mobile phones, computers, and other electronic products at night could affect the regulation of the sleep clock, prolong the time to fall asleep, and shorten sleep time. Besides, there is a significant amount of similar research evaluating related factors for sleep quality ( Nyer et al., 2013 ; Bi et al., 2022 ; Peltz and Rogge, 2022 ; Xian et al., 2022 ). In summary, these factors that are associated with undergraduates' sleep quality can be classified into the following categories: demographics, personal lifestyle, family support, social support, dormitory environment, physical health, and mental health.
Because of the significant social and cultural diversity between different regions in China, previous findings may not fully represent the overall sleep characteristics of the Chinese population, especially undergraduates. Thus, our study not only aimed to examine the prevalence of poor sleep among undergraduates but also provide a comprehensive understanding of the factors that contribute to poor sleep quality among undergraduates in Jiangsu Province, China. The factors examined in this study also included mobile phone addiction and psychological resilience. By enhancing our understanding of these variables, this study may also help to develop effective strategies to improve sleep quality and ultimately promote undergraduates' life quality in China.
Special attention should be paid to the four statistical methods we utilized in association analysis. Except for the usual models of multiple linear regression and binary logistic regression, two mixed effect models were adopted such as linear mixed model and logistic random effect model. All these models are variations of the generalized linear mixed model ( Bolker et al., 2009 ; Stroup, 2013 ). The mixed model is also known as the hierarchical model and contains both fixed and random effects. The random effects model represents the variability between different conditions or blocks, and they are incorporated into the model to account for the correlation between observations. In the present study, the four regression models were conducted with standard diagnostics, ensuring more accurate parameters and p -values. Various studies have utilized regression models to identify risk factors associated with poor sleep quality, but few strictly performed regression diagnostics, which can potentially result in biased results.
Participants and explanatory variables
A whole-group convenience sampling was performed in universities of Jiangsu Province using an electronic questionnaire on the Wenjuanxing platform ( www.wjx.cn ) from October to November 2022. We distributed the link and QR code of the questionnaire to the undergraduates via university teachers and a WeChat group. The questionnaire contained survey instructions explaining the online survey's purpose and significance. Each undergraduate took the survey voluntarily and had the option to withdraw at any moment. The confidentiality of data and student personal information was guaranteed. To ensure the quality and accuracy of data collection, the questionnaire was pre-tested to validate question effectiveness and comprehensibility. The sample size was thoroughly calculated based on the expected prevalence rate of sleep disorders among college students, according to the sample size calculation formula: n = z α 2 × p q / d 2 . When the significance level is α = 0.05, z α = 1.96. Let p be the expected prevalence rate and q = 1− p . Based on the preliminary survey results of this study, the estimated detection rate of sleep disorders among undergraduates is p = 16%. The allowable error is d = 0.1 × p . The estimated sample size needed for the survey is 2017 individuals.
A total of 8,587 undergraduates attended the questionnaire voluntarily, among which 130 participants with incomplete information were excluded, leading to a response rate of 98.49%. So, the final sample consisted of 8,457 participants (5,917 females and 2,540 males). Participants were all students living on campuses and enrolled in 14 majors, including literature, history, philosophy, law, economics, management, education, science, engineering, agronomy, military, art, medicine, and others.
The questions in the questionnaire were organized into continuous, categorical, and ordinal variables (see Table 1 ). In categorical and ordinal variables, some values were merged to avoid extremely small sample sizes in some subgroups. Participants who never smoked were classified as not smoking and those who smoked occasionally or often were classified as smoking. Participants who had never drunk alcohol were classified as not drinking, and those who drank alcohol occasionally or often were classified as drinking.
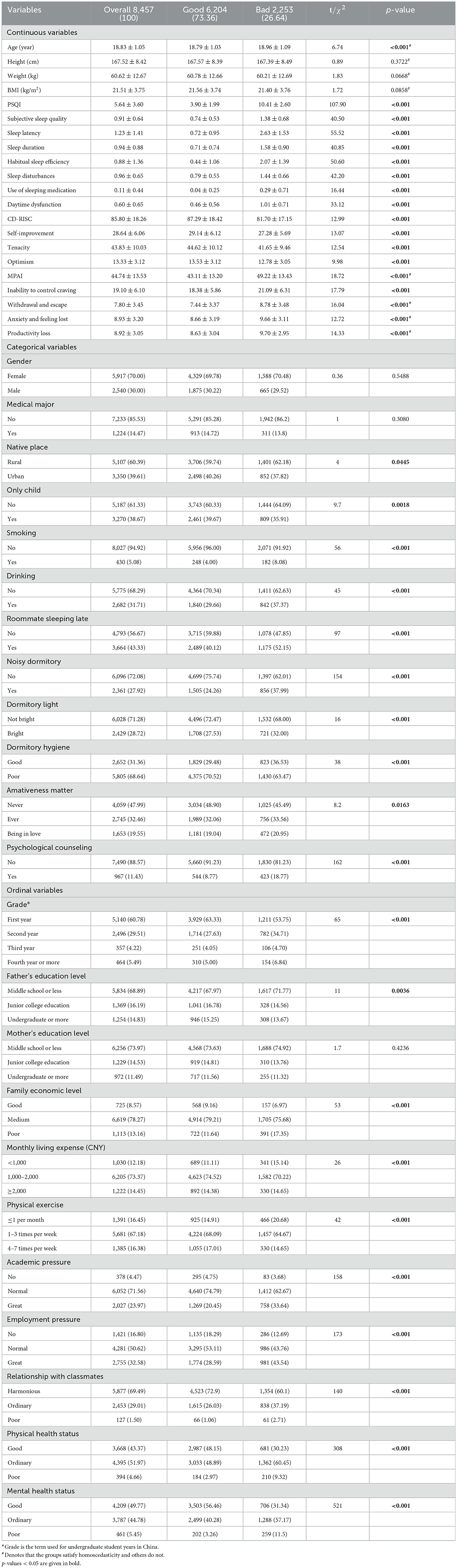
Table 1 . The prevalence of poor sleep quality across basic demographic characteristics.
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI) ( Buysse et al., 1989 ; Chen et al., 1999 ) was adopted to assess the sleep quality of undergraduates by translating it into a Chinese version. PSQI includes 19 self-rated questions, and only the first 18 entries are used to calculate scores. These questions can be grouped into seven dimensions that can evaluate sleep quality in the last month, including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The final PSQI score was calculated by summing the scores from these seven dimensions. The total score ranges from 0 to 21 (0–3 for each component), with higher values indicating poor sleep quality. A final PSQI score of more than 7 indicates poor sleep quality and a score of <7 represents good sleep quality. For the PSQI conducted in this study, Cronbach's alpha was 0.877.
Mobile phone addiction index
The mobile phone addiction index (MPAI) ( Bianchi and Phillips, 2005 ), which was already translated into Chinese and validated for the Chinese population ( Li L. et al., 2020 ), was used to evaluate mobile phone addiction. The MPAI consists of 17 items quantifying four dimensions, including the inability to control craving, withdrawal and escape, anxiety and feeling lost, and productivity loss. Scores range from 1 (not at all) to 5 (always) for each item. The higher total scores indicate a higher level of mobile phone addiction. The Cronbach's alpha for the MPAI of the present study was 0.925.
Connor-Davidson resilience scale
The present study employed the Connor-Davidson resilience scale (CD-RISC) ( Connor and Davidson, 2003 ) to measure the psychological resilience of undergraduates, which reflects how the participants felt over the last month. This scale has been employed in various populations and has also been translated into Chinese ( Xu et al., 2022 ). The CD-RISC consists of 25 items, and each item's score ranges from 0 to 4, representing not true at all, rarely true, sometimes true, usually true, and true almost all the time, respectively. The final CD-RISC score was obtained by summing each score of the items, which ranged from 0 to 100, with higher scores indicating greater resilience. The Cronbach's alpha for the CD-RISC of the present study was 0.969.
Statistical analysis
The software R version 4.3.0 was used for statistical analysis. Extreme values of continuous variables were identified by the interquartile range (IQR) method. The upper and lower fences were defined as Q 3+2 IQR and Q 1 − 2 IQR . Values below (resp., above) the lower (resp., upper) fence were replaced with the lower (resp., upper) fence. For continuous variables, their central and variation trends were described by mean and standard deviation (SD), i.e., x ¯ ± s , and the means between two (resp., or more) groups were compared by t -test (resp. ANOVA) when homoscedasticity was satisfied, otherwise, Welch's t -test (resp., Welch's ANOVA) was employed. A post-hoc test was performed using Tukey's method when homoscedasticity was satisfied; otherwise, the Games-Howell test was performed. In this study, homoscedasticity was measured using Levene's test. The categorical and ordinal variables were described by frequency and constituent ratio, and the differences between groups were compared by Chi-square test. The significant level was set as 0.05.
Statistical models
Multiple linear regression model.
The associated factors for undergraduate sleep quality were identified using a linear regression model with the continuous variable PSQI score as the dependent variable, other variables as explanatory variables, and ordinal variables as continuous. The standard regression diagnostics ( Kabacoff, 2015 ) were processed after the multiple linear regression model (MLR) was implemented with the following steps: (a) Samples containing extreme values, including outliers, high leverage points, and influential points were removed. The outliers were detected if the Bonferroni adjusted p -value of the corresponding absolute studentized residuals was significant; the high leverage points were identified via the hat statistics; the influential points were determined by Cook's distance. In our model, 497 samples were removed in this step. (b) The independence of residuals was checked using the Durbin–Watson's test. In our model, independence was satisfied. (c) Multicollinearity between explanatory variables was detected through variance inflation factor (VIF). In our model, the VIF values of BMI, weight (kg), and height (cm) were all more than 4, which indicated that multicollinearity exists. Hence, weight and height were removed since BMI contains information about both. (d) The normality and homoscedasticity of residuals were checked. Our detection indicated that homoscedasticity was not satisfied. Therefore, weighted MLR was utilized to solve the heteroscedasticity problem, with weights inversely proportional to the variance of the dependent variable. The absolute values of the residuals were regressed against the fitted values, and the resulting fitted values were squared to provide the desired estimate of the variance. (e) The linearity between dependent variables and explanatory variables was checked. The performance of linearity, homoscedasticity, normality, and extreme values after diagnostics is shown in Supplementary Figure S1 . Visual inspection did not reveal any obvious deviations from linearity or normality. It is noteworthy that non-normality is less likely to be a problem when other assumptions are met since Aitken's theorem shows that the regression coefficients obtained from weighted MLR are also the best linear unbiased estimator without the assumption of normality ( Hansen, 2022 ). The linear trend test for a continuous variable was performed by transforming it into a four-valued ordinal variable by quartiles in the weighted MLR model.
Binary logistic regression model
Odds ratios (ORs) of factors associated with poor sleep quality were performed using a binary logistic regression model (BLR). The dependent variable was set as good (coded as 0) and poor (coded as 1) sleep quality based on whether the PSQI score was <7, and other variables were treated in the same way as MLR. The diagnostics ( Kabacoff, 2015 ) were processed with the following steps: (a) Extreme values were detected by the same method as MLR and 408 samples were removed. (b) Multicollinearity was detected by VIF, and weight and height were also excluded. (c) The independence of observations was performed using Durbin–Watson's test, and this assumption was satisfied. (d) The linearity between the log odds and explanatory variables was checked by regressing the log odds against the explanatory variables. The performance of linearity and extreme values after diagnostics is shown in Supplementary Figure S2 . (e) Overdispersion and events per variable (EPV) were checked ( Peduzzi et al., 1996 ). Overdispersion was accessed by the Chi-square test, but it did not exist in our model. There were 28 explanatory variables, including dummy variables, 1,897 samples with good sleep quality, and 6,152 samples with poor sleep quality. Thus, the EPV principle was satisfied. The ratio of these two outcome events was ~1:3; therefore, it can be considered as approximately balanced data. The linear trend test was performed in the same way as the aforementioned method.
Linear mixed model
The linear mixed model (LMM) is an extension of the MLR to allow both fixed and random effects, and it is particularly used in hierarchical analysis ( Stroup, 2013 ). The package “lmerTest” was adopted to implement LMM. In LMM, the continuous variable PSQI served as the dependent variable. The candidate random effect terms were checked by the likelihood ratio test. As random effects, we had intercepts for grade, smoking, drinking, physical health status, mental health status, academic pressure, employment pressure, and psychological counseling, as well as random slopes for the effect of relationship with classmates among academic pressure and employment pressure. Other variables, excluding weight and height due to multicollinearity, were set as fixed effects. No outliers were detected, and the homoscedasticity was violated. Therefore, the weighted LMM was adopted, and the weights were determined in the same way as the weighted MLR. The independence was checked using Durbin–Watson's test, and the results were satisfied. The performance of linearity, homoscedasticity, normality, and extreme values after diagnostics is shown in Supplementary Figure S3 . Visual inspection did not reveal any obvious deviations from linearity or normality.
Logistic regression with random effects
The logistic regression with random effects model (LRRE) is a type of generalized linear mixed model. The dependent variable was set as BLR. We had random intercepts for grade, smoking, drinking, physical health status, mental health status, academic pressure, employment pressure, and psychological counseling, as well as random slopes for the effect of the relationship with classmates against employment pressure and academic pressure. Other variables, excluding weight and height due to multicollinearity, were set as fixed effects. A likelihood ratio test was performed to check the significance of random effects. No outliers were detected. Independency, linearity, and overdispersion were checked in the same way as BLR, and all assumptions were satisfied. The performance of linearity after diagnostics is shown in Supplementary Figure S4 .
Prevalence of poor sleep quality
The Cronbach's alpha for the questionnaire of this study was 0.911, which indicates the internal consistency of the questionnaire was good. The sample consisted of 69.97% male and 30.03% female. Out of the 8,457 undergraduates, 6,204 (73.36%) reported having good sleep quality while 2,253 (26.64%) experienced poor sleep quality, based on the PQSI threshold value of 7. The mean PSQI score of all participants was 5.64 ± 3.60. The prevalence of poor sleep quality in undergraduates is shown in Table 1 , and the PSQI score across different characteristics is shown in Supplementary Table S1 . There was no significant difference between male (5,917) and female (2,540) students in height, weight, BMI, medical major, and non-medical major in terms of PSQI score or sleep quality. Older students and those in higher grades had a higher prevalence of poor sleep quality compared with their counterparts who were younger and in lower grades. The prevalence of poor sleep quality among students from rural areas, only-child families, and fathers with low education levels was nearly 30% higher than among students from urban areas, having siblings and fathers with high education levels. Although the PSQI scores of the three levels of mothers' education were significantly different via Welch's ANOVA, the post hoc result did not show the difference, and the constituent ratios between students with good and poor sleep quality were not significantly different. Approximately 80% of the students with either good or poor sleep quality belonged to families with medium economic levels. Similarly, more than 70% of the students with good or poor sleep quality reported a monthly living expense between 1,000 to 2,000 CNY. In terms of dormitory and personal lifestyle, the constituent ratios between students with good and poor sleep quality were all significantly different, and the corresponding PSQI scores were also significantly different. The worse these parameters were, the higher the prevalence of poor sleep quality.
Undergraduates with poor sleep quality had higher PSQI scores across all seven components compared to those with good sleep quality. The mean PSQI score for undergraduates with poor sleep quality was 10.41, which was significantly higher than their counterparts with good quality sleep ( p < 0.001). The mean scores of CD-RISC and its three components for students with poor sleep quality were all significantly lower than those with good sleep quality ( p < 0.001). The MPAI situation was the opposite.
Results of weighted MLR and BLR
The Akaike Information Criterion (AIC) of MLR and weighted MLR were 38,170.2 and 38,103.3, respectively, which indicates that weighted MLR improved the bias caused by heteroscedasticity in MLR. Table 2 presents the factors associated with PSQI scores, which were identified by weighted MLR, and the risk factors for poor sleep quality identified through BLR. The variables age, MPAI, grade, smoking, drinking, academic pressure, employment pressure, relationship with classmates, roommate sleeping late, noisy dormitory, physical health status, mental health status, and psychological counseling exhibited significant positive associations with the PSQI scores. On the other hand, BMI, CD-RISC, medical major, and father's education level demonstrated significant negative correlations with the PSQI scores. Barring BMI and relationship with classmates, the association between all other factors and PSQI was linear.
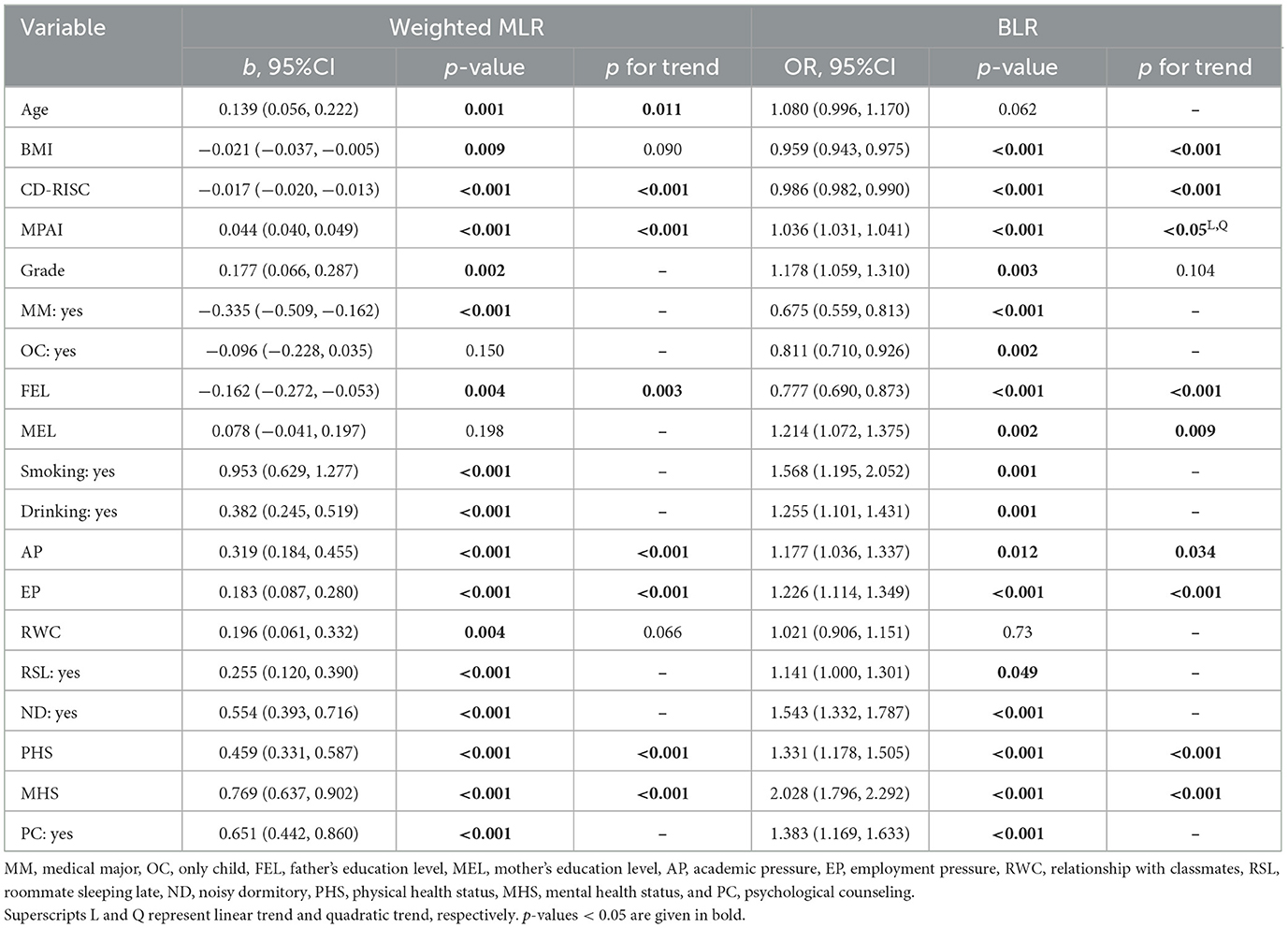
Table 2 . Risk factors for sleep quality identified by weighted MLR and BLR.
The results of BLR showed that students with higher BMI (OR = 0.959, p < 0.001), CD-RISC (OR = 0.986, p < 0.001), and father's education level (OR = 0.777, p < 0.001), had a decreased risk of poor sleep quality. Students with higher MPAI (OR = 1.036, p < 0.001), higher grades (OR = 1.178, p = 0.003), higher mother's education level (OR = 1.214, p = 0.002), greater academic pressure (OR = 1.177, p = 0.012), greater employment pressure (OR = 1.226, p < 0.001), worse physical health status (OR = 1.331, p < 0.001), and worse mental health status (OR = 2.028, p < 0.001) had an increased risk of poor sleep quality. Students who majored in medicine (OR = 0.675, p < 0.001) and were the only child in the family (OR = 0.811, p = 0.002) had a lower risk of poor sleep quality than those who did not major in medicine and were not the only child in the family. Smoking (OR = 1.568, p < 0.001), drinking (OR = 1.255, p < 0.001), and receiving psychological counseling (OR = 1.383, p < 0.001) were significantly associated with poor sleep quality. Roommates sleeping late (OR = 1.141, p = 0.049) and noisy dormitory (OR = 1.543, p < 0.001) were shown to be risk factors for poor sleep quality. The OR of mental health status was the highest, followed by smoking, noisy dormitory, psychological counseling, physical health status, and drinking. The sorted ORs of significant factors for undergraduate poor sleep quality can be found in Figure 1 . Linear trend test showed that MPAI had both significant linear and quadratic trends with respect to poor sleep quality, but no substantial distinction was observed between the two trends on visual inspection (see Supplementary Figure S4 ). Besides, there was also no linear trend between grade and poor sleep quality ( p = 0.104). The receiver operating characteristic (ROC) curve of BLR can be found in Supplementary Figure S5 , and the area under the curve (AUC) was 0.776.
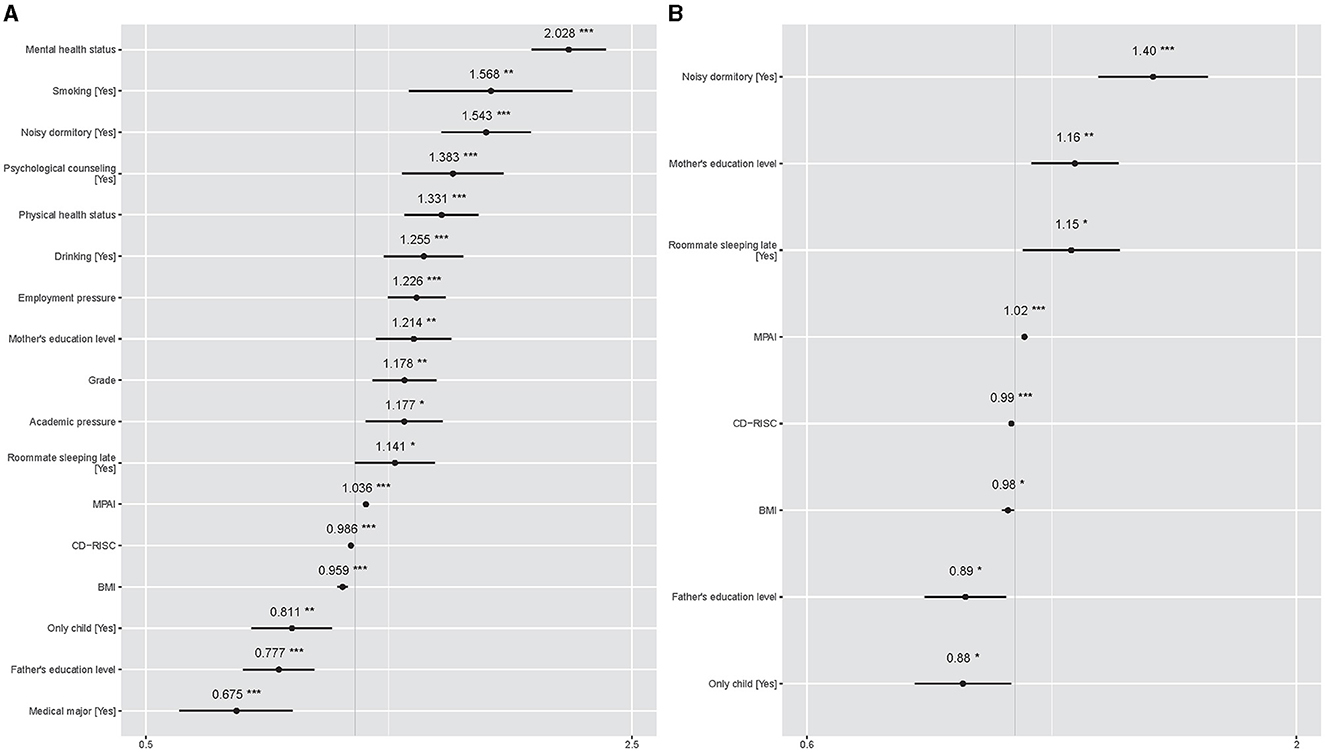
Figure 1 . Sorted ORs of significant factors for undergraduate poor sleep quality. The gray vertical solid line represents OR =1, and the short black horizontal solid line represents 95% CIs of ORs. Symbol * denotes p < 0.05, ** denotes p < 0.01, and *** denotes p < 0.001. (A) Comes from the results of BLR. (B) Comes results of LRRE.
Results of weighted LMM and LRRE
The AICs of LMM and weighted LMM were 43,857.1 and 43,554.2, respectively, which indicates that weighted LMM improved the bias caused by heteroscedasticity in LMM. Table 3 shows fixed and random effects of associated PSQI score factors identified by weighted LMM and related factors for poor sleep quality identified by LRRE. The intraclass correlation coefficients (ICCs) of the two models were 0.123 and 0.130, suggesting that 12.3% and 13.0% of the total variation in the responses were explained by subgroups. The fixed effects of age ( b = 0.142, p = 0.002) and MPAI ( b = 0.043, p < 0.001) exhibited a significant positive association with respect to PSQI scores, while the fixed effect of CD-RISC was the opposite ( b = −0.016, p < 0.001). Students with a roommate sleeping late ( b = 0.303, p < 0.001) and in a noisy dormitory ( b = 0.582, p < 0.001) had significantly higher PSQI scores at an average level compared to those without a roommate sleeping late and in a noisy dormitory. Except for age, all significant continuous factors displayed a linear trend with the PSQI score. However, an analysis of the trend graph between age and PSQI score revealed that the quadratic trend was approximately close to linearity (see Supplementary Figure S6 ). The random effects of weighted LMM explained 15.62% of the total variation. The detailed random effect values of weighted LMM can be found in Figure 2 . For random intercepts, being in the second and fourth grades, having poor mental and physical health status, receiving psychological counseling, smoking, and drinking had the effect of increasing PSQI scores. The random slopes of relationships with classmates varied across the three levels of employment pressure and academic pressure. However, the random effects of the relationship with classmates and employment pressure were not significant. In the subgroup of students without academic pressure, the intercept was −1.200, and the slope of the relationship with classmates was 0.812, suggesting that a poor relationship with classmates had a positive effect on increasing PSQI scores. In the subgroups of students with normal and great academic pressure, the intercepts were 0.496 and 0.704, respectively, indicating that these two subgroups had higher average PSQI scores compared to the subgroups of students without academic pressure. However, the slopes of relationship with classmates across the two subgroups were −0.458 and −0.353, demonstrating that a harmonious relationship with classmates had a positive effect on increasing the PSQI scores.
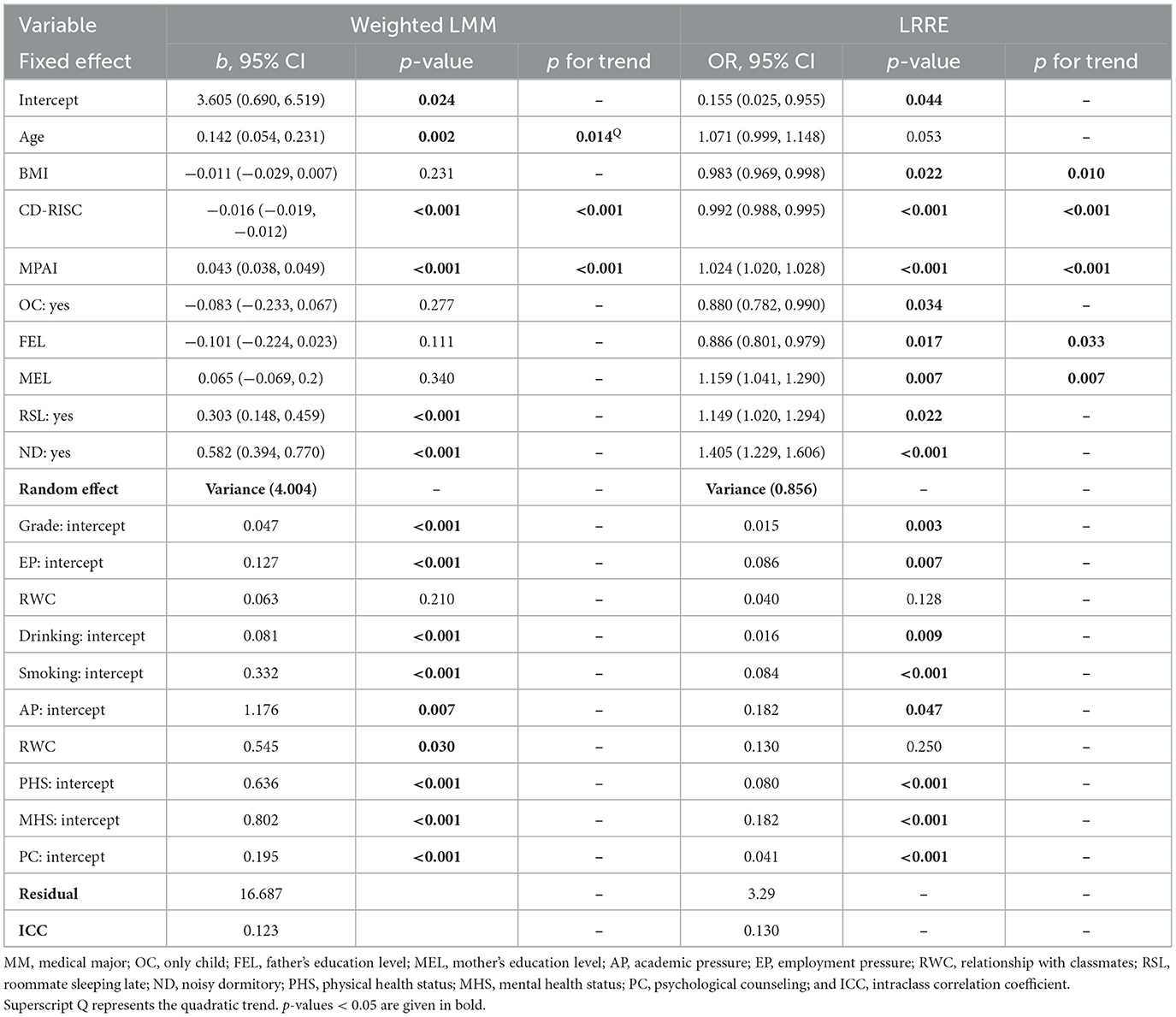
Table 3 . Fixed and random effects of factors for sleep quality by weighted LMM and LRRE.
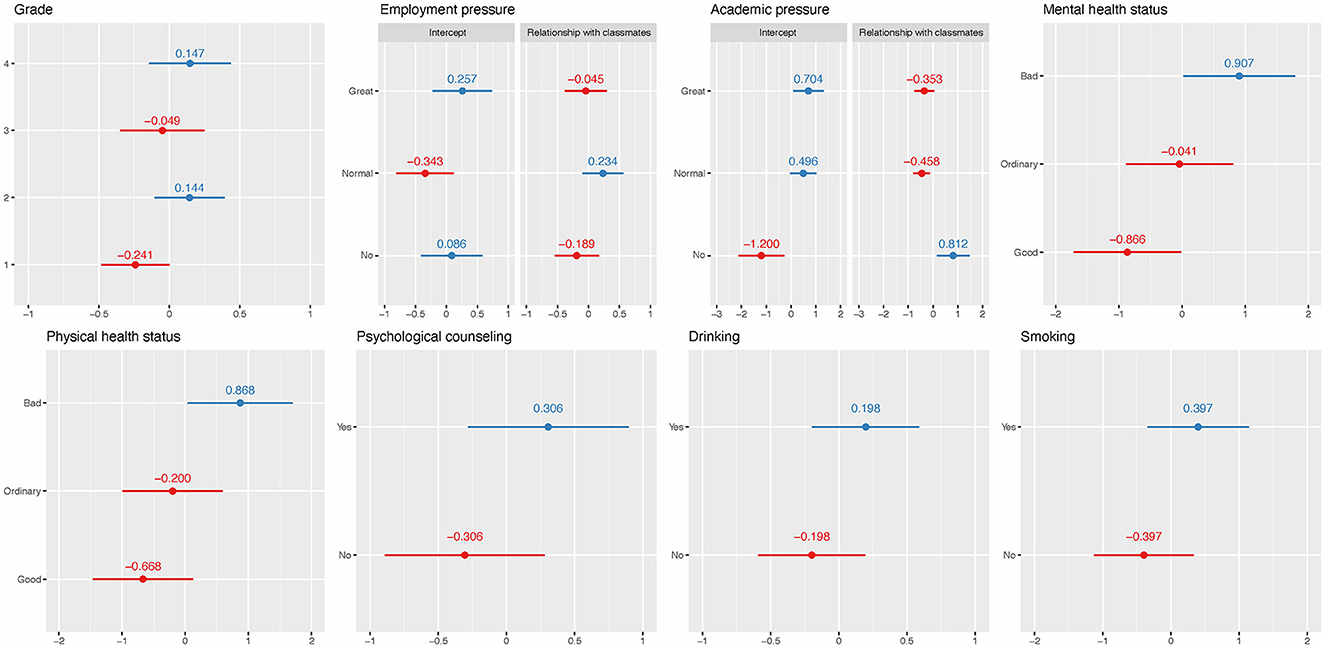
Figure 2 . Random effects of weighted LMM. The red and blue solid dots represent negative and positive effects on PSQI scores, respectively. The short horizontal solid lines represent 95% CI.
For the fixed effect results of LRRE, higher BMI (OR = 0.983, p = 0.022) and CD-RISC (OR = 0.992, p < 0.001) had a decreased risk of poor sleep quality. On the contrary, students with higher MPAI (OR = 1.024, p < 0.001) and mother's education level (OR = 1.159, p = 0.007) had an increased risk of poor sleep quality. Being the only child was a protective factor of poor sleep quality compared to not being the only child (OR = 0.88, p = 0.034). All significant continuous factors had a linear trend with respect to poor sleep quality. A higher risk was also found for students with roommates sleeping late (OR = 1.149, p = 0.022) and noisy dormitories (OR = 1.405, p < 0.001). These results are consistent with previous BLR results. In fixed effects, noisy dormitory had the highest OR, followed by mother's education level and roommates sleeping late. The sorted ORs can be found in Figure 1 . The random effects explained 20.65% of the total variation when the dataset was fitted by LRRE and their ORs, which can be found in Figure 3 . It was found that the variability in students' relationships with classmates (random slopes) did not significantly differ across the three levels of employment pressure and academic pressure. This suggests that students' relationships with classmates were consistent regardless of the degree of pressure experienced. The effects of most random intercepts were consistent with the corresponding counterpart of weighted LMM. Being in the second and fourth grades, experiencing “great” and “not having” employment pressure, poor and normal levels of mental health status, poor physical health status, receiving psychological counseling, smoking, and drinking had a positive effect on poor sleep quality. The ROC curve of LRRE can be found in Supplementary Figure S7 , and the AUC was 0.720.
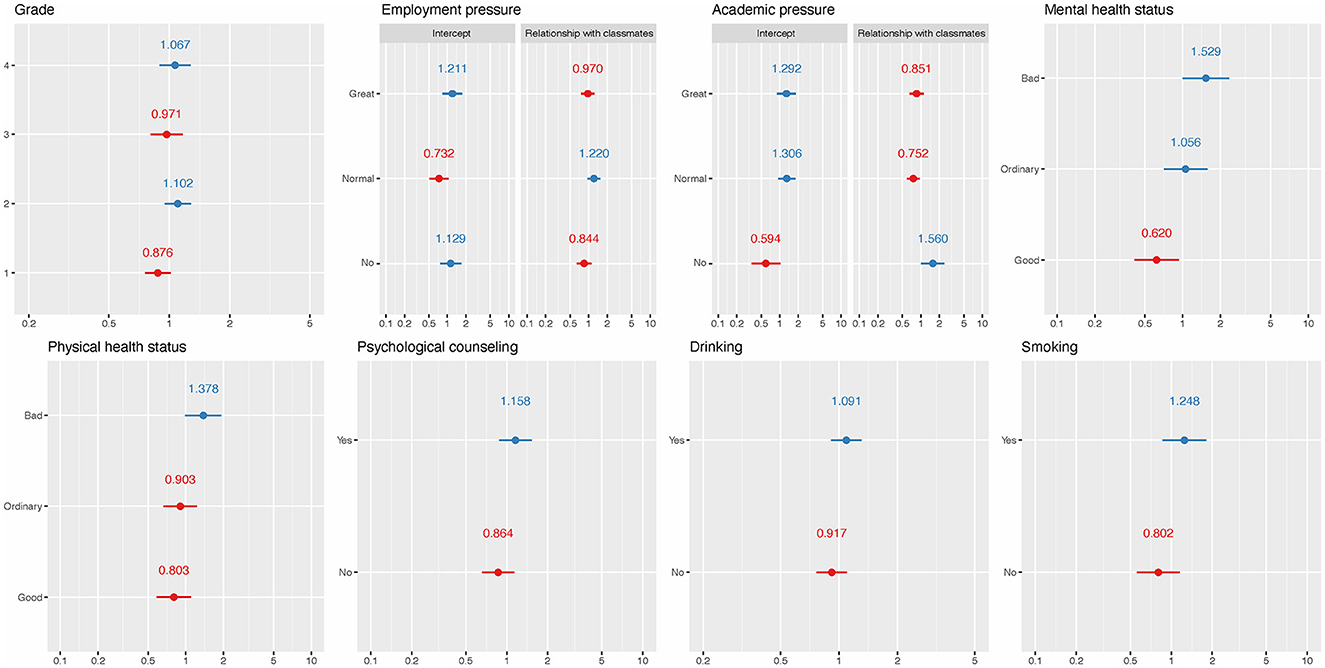
Figure 3 . ORs for random effects of LREE. The red and blue solid dots represent ORs that are <1 and >1, respectively. The short horizontal solid lines represent 95% CI.
This study investigated the prevalence and associated factors of sleep quality among undergraduates in Jiangsu Province, China. The results showed a mean PSQI score of 5.64 ± 3.60 and a prevalence of poor sleep quality of 26.64%, which is consistent with another study on medical college students in China, which showed the prevalence was 27.80% ( Wang et al., 2016 ) but lower than the results obtained in Ethiopia (55.8%) and Taiwan (33.80%) ( Kang and Chen, 2009 ; Lemma et al., 2012 ).
No significant association was found between gender and sleep quality through demographics and the four regression models. Similar results were reported in previous studies ( Lund et al., 2010 ; Wang et al., 2016 ; Li Y. et al., 2020 ). The study also found no significant correlation between sleep quality and native place, family economic level, physical exercise, dormitory light, dormitory hygiene, and amativeness matter through the four regression models. Previous studies ( Lund et al., 2010 ; Wang et al., 2016 ; Li Y. et al., 2020 ) also reported that there was no association between sleep quality and family economic level, physical exercise, and amativeness matter. Some studies showed that sleep quality might be influenced by native places ( Tang et al., 2017 ), but their cutoff values of PSQI score was not seven, and the population was not undergraduates. Our study found that there is no significant correlation between sleep quality and dormitory light brightness or dormitory hygiene; these factors were included in the cluster randomized-controlled trial described in research ( Li et al., 2022 ) to explore comprehensive environmental influences on sleep quality. The rationale for this inclusion is based on the hypothesis that environmental factors, beyond personal habits or demographic characteristics, have a significant impact on sleep quality. Although our findings and the intervention in the cited study did not demonstrate a direct impact of these factors on sleep quality, including them in the analysis will help to provide a holistic view of the environmental influences on sleep.
Since the dependent variable PSQI score in weighted MLR and weighted LMM was continuous, while the dependent variable in BLR and LRRE was dichotomous, the associated factors identified by the two types of models may differ. For example, age was significantly positively associated with PSQI score in weighted MLR and weighted LMM but was not significant in BLR and LRRE. Being the only child and mother's education level were significant in BLR and LRRE but were not in weighted MLR and weighted LMM. This may be because age can affect the PSQI score, but it has a limited impact on PSQI in the bounded range ( Basner et al., 2013 ; Demirci et al., 2015 ).
In the present study, the BLR and LRRE models identified significant associations between only child status and mother's education level with sleep quality. The effects of these factors appeared to be amplified in the dichotomous models (BLR and LRRE) than in the other models, suggesting that these variables may have a more sensitive response to categorical sleep quality measures. This phenomenon may reflect the complex relationship between these sociodemographic characteristics and individuals' daily behavioral patterns. Specifically, students who are the only child may receive more attention and resources within the family and also be subject to higher expectations and pressures from their parents, both of which may affect sleep quality.
Higher levels of maternal education may also imply better cognitive stimulation and family economic conditions, which indirectly affect the child's sleep status. On the other hand, these significant differences may be related to the family's socio-economic status and cultural background, which also affect undergraduates' performance in school or social activities and stress levels, and ultimately affect sleep quality. There was a difference in sleep quality between the only child and non-only child subgroups (see Table 1 ), but the difference in PSQI score was small (see Supplementary Table S1 ), resulting in the linear model not identifying it after adjusting for other factors. The same situation also applies to the mother's education level, in which the three levels had no difference in the PSQI score. BMI and the father's education levels were not significant in the weighted LMM but were significant in the other three models.
Relationship with classmates was significant in weighted MLR and had significant random slopes in weighted LMM but was not significant in BLR and LRRE. Some inconsistencies between weighted MLR and weighted LMM, BLR, and LRRE may be due to the different samples included. Three kinds of extreme values were removed from the weighted MLR and BLR, while LMM and LRRE had relatively few methods to detect extreme values. Weighted LMM and LRRE contained all samples since no extreme values were found in the diagnostic step.
The four regression models identified several common risk factors for sleep quality, including lower CD-RISC, higher MPAI, being in fourth grade or above, smoking, drinking, greater academic pressure, having no or great employment pressure, roommate sleeping late, noisy dormitory, poorer physical health status, poorer mental health status, and psychological counseling. Most of these results are consistent with previous studies. CD-RISC ( Bianchi and Phillips, 2005 ) measured the psychological resilience of undergraduates, and its negative association with CD-RISC was also reported by previous studies ( Li and Guo, 2023 ; Xie et al., 2023 ). A higher MPAI represents a higher level of mobile phone addiction. Mobile phone overuse may disrupt the sleep process and lead to depression. Furthermore, long-term exposure to blue light and electromagnetic fields emitted from the screen may affect melatonin levels and contribute to poor sleep quality ( Demirci et al., 2015 ). However, newer models of cell phones currently have the ability to turn off blue light, and this study did not investigate the condition with blue light turned off, so this finding may have limitations. A gender-specific study ( Zhou et al., 2022 ) found that smoking was a risk factor for poor sleep quality among males, and noisy dormitory and academic pressure were risk factors for poor sleep quality among females. A study on college students of Jilin Province ( Li Y. et al., 2020 ) found that drinking, academic pressure, and relationships with classmates were risk factors for poor sleep quality. A study on medical students ( Shao et al., 2020 ) showed that students with greater employment pressure had more anxiety symptoms, which may affect their sleep quality. A cluster randomized-controlled trial in China ( Li et al., 2022 ) showed that intervening with the sleep schedule of roommates can obtain a good sleep quality for them, suggesting that our findings of roommates sleeping late as a risk factor for poor sleep quality are consistent with it. However, there were some studies that considered low physical activity via the International Physical Activity Questionnaire-Short Form anxiety and depression scores via the Hospital Anxiety and Depression Scale as negative factors for sleep quality ( Ghrouz et al., 2019 ). Another study ( Nyer et al., 2013 ) found that students with depressive symptoms and sleep disturbance endorsed significantly more intense and frequent anxiety and poorer cognitive and physical functioning.
Being in a higher grade was a risk factor for sleep quality in weighted MLR and BLR, but only the random effects of being in the second grade and fourth grade or above were found to be positive in weighted LMM and GLMM, and the random effects of being in the first and third grades were negative. This may be due to the greater pressure faced by students in fourth grade or above, such as postgraduate entrance exams, employment, internships, and graduation thesis issues. Similarly, second grade was the year with the greatest learning pressure, and in addition to regular studies, they also needed to participate in various competitions and innovation training programs. The first grade was still in a transitional adaptation period from high school to college, while the third grade was a comfortable period after adapting to college life. The students in third grade were able to cope easily with previous pressure, and there was no new pressure similar to those in the fourth grade.
In the weighted LMM result, the slope of the relationship with classmates was positive, i.e., 0.812, in the subgroup of having no academic pressure, indicating that a poorer relationship with classmates meant a higher PSQI score. The corresponding slopes were negative, i.e., −0.458 and −0.353, in the subgroups of normal and great academic pressure, respectively, indicating that a poorer relationship with classmates meant a lower PSQI score. This may be because students who have good relationships with classmates need to spend more time dealing with communication or other issues between classmates, resulting in less rest time and high pressure. We recognize that this interpretation is speculative and based on observations from the current data set. Therefore, more comprehensive research is necessary to explore and test this hypothesis. Therefore, we call for further research to explore the complexity of the interplay between social stress, social relationships, and sleep quality.
In the weighted LMM result, the random intercept of having no employment pressure was 0.086, and its corresponding OR in the LRRE result was more than 1, which indicates that having no employment pressure had the effect of increasing the risk of poor sleep quality. This may be caused by the fact that the sample size of students with poor sleep quality and having no employment pressure was extremely low, i.e., 286. Thus, the model may not show the true effect of having no employment pressure. Another reason may be the random slopes of relationships with classmates, whose random effects were not significant.
The associated factors for sleep quality identified in various studies may differ, primarily due to several reasons. Firstly, the survey population and hierarchical structure may vary. Differences in population, region, and composition can yield diverse outcomes. Secondly, the included independent variables may differ; the same variable may have different values. Thirdly, the interaction between variables can lead to discrepancies in results. Furthermore, different models can yield different results. Even when analyzing data using the same model, different researchers may obtain distinct results due to differences in the operational methods of the model. The first two conditions are difficult to control, but we can try to avoid differences in results through standardized operations.
In the present study, four models were utilized to examine the factors associated with sleep quality. To ensure the robustness of the outcomes, we carried out rigorous diagnostics for all four models. After diagnostics, all four models obtained the best linear unbiased estimators (BLUE) or best linear unbiased predictions (BLUP) according to Gauss-Markov's theorem and Atkin's theorem ( Hansen, 2022 ). Regression diagnostics are an important step that has been overlooked by many researchers. Standard diagnostics ensure more accurate parameter estimation and p -values and ultimately improve the overall quality of the analysis. Without diagnostics, some biased results for regression models will be obtained and reported. In the weighted MLR (resp., BLR) model, we found that other levels will increase or decrease PSQI scores (resp., risk of poor sleep quality) relative to the reference level. However, we can obtain detailed effect values of each level through LMM and LRRE. To our knowledge, previous studies have not shown similar results.
Limitations
There are several limitations in the present study. Firstly, the present study selected as many candidate influencing factors as possible for sleep quality, such as family support, social support, personal lifestyle, physical health, mental health, mobile phone addiction, and psychological resilience. However, considering the length of the questionnaire, there were still some potential factors that were not included, such as coffee drinks, depression, and habits. Secondly, this study was cross-sectional, which precluded the establishment of definitive conclusions regarding the direction of causality between sleep quality and risk factors. Further, longitudinal studies are needed to investigate the causal relationships. Thirdly, all questionnaires were self-reported, highlighting the inherent limitations of self-reported measures. Lastly, there were no strict exclusion criteria in this study, which may have resulted in self-selection bias. This means that participants with anxiety and depression are characteristics that are likely to interact with the outcome under investigation, or alternatively, they may have been more likely to participate since the topic is relevant to them.
This study examined the prevalence of risk factors associated with poor sleep quality among undergraduates in Jiangsu Province, China. Our results showed a considerable prevalence of poor sleep quality among this group, with students in higher grades exhibiting a higher likelihood of experiencing poor sleep quality. The study also identified modifiable factors that correlate with poor sleep quality, including psychological resilience, mobile phone addiction, smoking, drinking, and poorer physical health. In response to the factors associated with poor sleep quality identified in our study, we advocate for university administrators to deploy systematic educational programs and interventions tailored to enhance sleep quality among students. These initiatives should directly target modifiable risk factors such as mental health status, academic and employment pressures, and suboptimal dormitory conditions. Specifically, proposed interventions include organizing workshops and seminars on sleep hygiene to educate students about the importance of good sleep practices and the physiological underpinnings of sleep. University administrators should also offer mental health services that provide counseling and stress management strategies. They should facilitate sessions on academic and time management skills to mitigate the impact of academic and employment pressures and improve dormitory living conditions through the establishment of quiet hours and better noise insulation to foster a more sleep-conducive environment. These recommendations illustrate a thoughtfully considered approach to ameliorate the sleep-related challenges faced by university students. University administrators can provide adequate psychological counseling for students to alleviate their pressures and set appropriate dormitory conventions to address dormitory-related issues.
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary material , further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of Xuzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BH: Methodology, Writing—review & editing. WS: Data curation, Funding acquisition, Writing—review & editing. YW: Writing—review & editing. QW: Data curation, Investigation, Writing—review & editing. JL: Writing—review & editing. XX: Writing—review & editing. YH: Writing—review & editing. LX: Data curation, Funding acquisition, Methodology, Writing—original draft. DY: Conceptualization, Writing—review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (grant number 12001470), the China Postdoctoral Science Foundation (grant number 2020M671607), and the Science and Technology Development Fund project of the Affiliated Hospital of Xuzhou Medical University (grant number XYFY202245). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1343186/full#supplementary-material
Supplementary Table S1. Pittsburgh Sleep Quality Index scores of undergraduates with different characteristics.
Supplementary Figure S1. The performance of linearity, homoscedasticity, extreme values, and normality after diagnostics for weighted multiple linear regression model.
Supplementary Figure S2. The performance of linearity and extreme values after diagnostics for binary logistic regression model.
Supplementary Figure S3. The performance of linearity, homoscedasticity, extreme values, and normality after diagnostics for the weighted linear mixed model.
Supplementary Figure S4. The performance of linearity after diagnostics for logistic regression with random effects model.
Supplementary Figure S5. The linear and quadratic trend between MPAI and PSQI score in weighted multiple linear regression.
Supplementary Figure S6. ROC curve of binary logistic regression model.
Supplementary Figure S7. The linear and quadratic trend between age and PSQI score in weighted linear mixed model.
Supplementary Figure S8. ROC curve of logistic regression with random effects model.

Abbreviations
PSQI, Pittsburgh sleep quality index; MPAI, mobile phone addiction index; CD-RISC, Connor-Davidson resilience scale; IQR, interquartile range; CI, confidence intervals; SD, standard deviation; ANOVA, analysis of variance; VIF, variance inflation factor; EPV, events per variable; BMI, body mass index; OR, odds ratios; MLR, multiple linear regression model; BLR, binary logistic regression model; LMM, linear mixed model; LRRE, logistic regression with random effects; AIC, Akaike Information Criterion; AUC, area under curve; ICC, intraclass correlation coefficient; BLUE, best linear unbiased estimator; BLUP, best linear unbiased prediction.
Ahmed, M. S., Khan, S., Hsan, K., Sen, L. C., Yunus, F. M., and Griffiths, M. D. (2020). Factors affecting sleep quality among the university students in Bangladesh: a cross-sectional structured interview study. Sleep Vigilance 4, 177–184. doi: 10.1007/s41782-020-00106-4
Crossref Full Text | Google Scholar
Almojali, A. I., Almalki, S. A., Alothman, A. S., Masuadi, E. M., and Alaqeel, M. K. (2017). The prevalence and association of stress with sleep quality among medical students. J. Epidemiol. Glob. Health 7, 169–174. doi: 10.1016/j.jegh.2017.04.005
PubMed Abstract | Crossref Full Text | Google Scholar
Baranwal, N., Yu, P. K., and Siegel, N. S. (2023). Sleep physiology, pathophysiology, and sleep hygiene. Prog. Cardiovasc. Dis. 77, 59–69. doi: 10.1016/j.pcad.2023.02.005
Basner, M., Rao, H., Goel, N., and Dinges, D. F. (2013). Sleep deprivation and neurobehavioral dynamics. Curr. Opin. Neurobiol. 23, 854–863. doi: 10.1016/j.conb.2013.02.008
Bi, C., Lin, H., Zhang, J., and Zhao, Z. (2022). Association between sleep quality and depression symptoms in Chinese college students during the COVID-19 lockdown period. Children 9:1237. doi: 10.3390/children9081237
Bianchi, A., and Phillips, J. G. (2005). Psychological predictors of problem mobile phone use. CyberPsychol. Behav. 8, 39–51. doi: 10.1089/cpb.2005.8.39
Bolker, B. M., Brooks, M. E., Clark, C. J., Geange, S. W., Poulsen, J. R., Stevens, M. H., et al. (2009). Generalized linear mixed models: a practical guide for ecology and evolution. Trends Ecol. Evol. 24, 127–135. doi: 10.1016/j.tree.2008.10.008
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., and Kupfer, D. J. (1989). The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. doi: 10.1016/0165-1781(89)90047-4
Chen, M. L., Lin, L. C., Wu, S. C., and Lin, J. G. (1999). The effectiveness of acupressure in improving the quality of sleep of institutionalized residents. J. Gerontol. A Biol. Sci. Med. Sci. 54, M389–M394. doi: 10.1093/gerona/54.8.M389
Connor, K. M., and Davidson, J. R. T. (2003). Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 18, 76–82. doi: 10.1002/da.10113
Curcio, G., Ferrara, M., and De Gennaro, L. (2006). Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 10, 323–337. doi: 10.1016/j.smrv.2005.11.001
Davies, S. K., Ang, J. E., Revell, V. L., Holmes, B., Mann, A., Robertson, F. P., et al. (2014). Effect of sleep deprivation on the human metabolome. Proc. Natl. Acad. Sci. USA. 111, 10761–10766. doi: 10.1073/pnas.1402663111
Demirci, K., Akgönül, M., and Akpinar, A. (2015). Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J. Behav. Addict . 4, 85–92. doi: 10.1556/2006.4.2015.010
Durmer, J. S., and Dinges, D. F. (2005). Neurocognitive consequences of sleep deprivation. Semin. Neurol. 25, 117–129. doi: 10.1055/s-2005-867080
Eleftheriou, A., Rokou, A., Arvaniti, A., Nena, E., and Steiropoulos, P. (2021). Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front. Public Health 9:775374. doi: 10.3389/fpubh.2021.775374
Gerhardsson, A., Åkerstedt, T., Axelsson, J., Fischer, H., Lekander, M., Schwarz, J., et al. (2019). Effect of sleep deprivation on emotional working memory. J. Sleep Res. 28:e12744. doi: 10.1111/jsr.12744
Ghrouz, A. K., Noohu, M. M., Dilshad Manzar, M., Warren Spence, D., BaHammam, A. S., and Pandi-Perumal, S. R. (2019). Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 23, 627–634. doi: 10.1007/s11325-019-01780-z
Hansen, B. E. A. (2022). modern Gauss–Markov theorem. Econometrica 90, 1283–1294. doi: 10.3982/ECTA19255
Kabacoff, R. I. (2015). R in Action: Data Analysis and Graphics with R, Second Edition . Shelter Island: Manning publications Co.
Google Scholar
Kang, J.-H., and Chen, S.-C. (2009). Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health 9:248. doi: 10.1186/1471-2458-9-248
Lemma, S., Gelaye, B., Berhane, Y., Worku, A., and Williams, M. A. (2012). Sleep quality and its psychological correlates among university students in Ethiopia: a cross-sectional study. BMC Psychiatry 12:237. doi: 10.1186/1471-244X-12-237
Li, L., Griffiths, M. D., Mei, S., and Niu, Z. (2020). Fear of missing out and smartphone addiction mediates the relationship between positive and negative affect and sleep quality among Chinese university students. Front. Psychiatry 11:877. doi: 10.3389/fpsyt.2020.00877
Li, M., Han, Q., Pan, Z., Wang, K., Xie, J., Zheng, B., et al. (2022). Effectiveness of multidomain dormitory environment and roommate intervention for improving sleep quality of medical college students: a cluster randomised controlled trial in China. Int. J. Environ. Res. Public Health 19:15337. doi: 10.3390/ijerph192215337
Li, Y., Bai, W., Zhu, B., Duan, R., Yu, X., Xu, W., et al. (2020). Prevalence and correlates of poor sleep quality among college students: a cross-sectional survey. Health Qual. Life Outcomes 18:210. doi: 10.1186/s12955-020-01465-2
Li, Y., and Guo, K. (2023). Research on the relationship between physical activity, sleep quality, psychological resilience, and social adaptation among Chinese college students: a cross-sectional study. Front. Psychol. 14:1104897. doi: 10.3389/fpsyg.2023.1104897
Lo, J. C., Chong, P. L. H., Ganesan, S., Leong, R. L. F., and Chee, M. W. L. (2016). Sleep deprivation increases formation of false memory. J. Sleep Res. 25, 673–682. doi: 10.1111/jsr.12436
Lund, H. G., Reider, B. D., Whiting, A. B., and Prichard, J. R. (2010). Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health 46, 124–132. doi: 10.1016/j.jadohealth.2009.06.016
Nyer, M., Farabaugh, A., Fehling, K., Soskin, D., Holt, D., Papakostas, G. I., et al. (2013). Relationship between sleep disturbance and depression, anxiety, and functioning in college students. Depress. Anxiety 30, 873–880. doi: 10.1002/da.22064
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R., and Feinstein, A. R. A. (1996). simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 49, 1373–1379. doi: 10.1016/S0895-4356(96)00236-3
Peltz, J., and Rogge, R. (2022). Adolescent and parent sleep quality mediates the impact of family processes on family members' psychological distress. Sleep Health 8, 73–81. doi: 10.1016/j.sleh.2021.08.009
Shao, R., He, P., Ling, B., Tan, L., Xu, L., Hou, Y., et al. (2020). Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol 8:38. doi: 10.1186/s40359-020-00402-8
St-Onge, M.-P. (2017). Sleep-obesity relation: underlying mechanisms and consequences for treatment. Obes. Rev. 18(Suppl 1), 34–39. doi: 10.1111/obr.12499
Stroup, W. W. (2013). Generalized Linear Mixed Models: Modern Concepts, Methods and Applications . New York, NY: Taylor and Francis Group.
Suen, L. K. P., Hon, K. L. E., and Tam, W. W. S. (2008). Association between sleep behavior and sleep-related factors among university students in Hong Kong. Chronobiol. Int. 25, 760–775. doi: 10.1080/07420520802397186
Tang, J., Liao, Y., Kelly, B. C., Xie, L., Xiang, Y. T., Qi, C., et al. (2017). Gender and regional differences in sleep quality and insomnia: a general population-based study in Hunan province of China. Sci. Rep. 7:43690. doi: 10.1038/srep43690
Vaccaro, A., Kaplan Dor, Y., Nambara, K., Pollina, E. A., Lin, C., Greenberg, M. E., et al. (2020). Sleep loss can cause death through accumulation of reactive oxygen species in the gut. Cell 181, 1307–1328.e15. doi: 10.1016/j.cell.2020.04.049
Wang, L., Qin, P., Zhao, Y., Duan, S., Zhang, Q., Liu, Y., et al. (2016). Prevalence and risk factors of poor sleep quality among Inner Mongolia medical university students: a cross-sectional survey. Psychiatry Res. 244, 243–248. doi: 10.1016/j.psychres.2016.04.011
Xian, X., Zhang, Y., Bai, A., Zhai, X., Hu, H., Zhang, J., et al. (2022). Association between family support, stress, and sleep quality among college students during the COVID-19 online learning period. Int. J. Environ. Res. Public Health 20:248. doi: 10.3390/ijerph20010248
Xie, G., Wu, Q., Guo, X., Zhang, J., and Yin, D. (2023). Psychological resilience buffers the association between cell phone addiction and sleep quality among college students in Jiangsu Province, China. Front. Psychiatry 14:1105840. doi: 10.3389/fpsyt.2023.1105840
Xu, C., Wang, Y., Wang, Z., Li, B., Yan, C., Zhang, S., et al. (2022). Social support and coping style of medical residents in China: the mediating role of psychological resilience. Front. Psychiatry 13:888024. doi: 10.3389/fpsyt.2022.888024
Zhou, Y., Bo, S., Ruan, S., Dai, Q., Tian, Y., Shi, X., et al. (2022). Deteriorated sleep quality and influencing factors among undergraduates in northern Guizhou, China. PeerJ 10:e13833. doi: 10.7717/peerj.13833
Keywords: sleep quality, undergraduates, risk factors, Connor-Davidson resilience scale, mobile phone addiction index, Pittsburgh Sleep Quality Index
Citation: Hu B, Shen W, Wang Y, Wu Q, Li J, Xu X, Han Y, Xiao L and Yin D (2024) Prevalence and related factors of sleep quality among Chinese undergraduates in Jiangsu Province: multiple models' analysis. Front. Psychol. 15:1343186. doi: 10.3389/fpsyg.2024.1343186
Received: 23 November 2023; Accepted: 22 March 2024; Published: 10 April 2024.
Reviewed by:
Copyright © 2024 Hu, Shen, Wang, Wu, Li, Xu, Han, Xiao and Yin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dehui Yin, yindh16@xzhmu.edu.cn ; Lishun Xiao, xiaolishun@xzhmu.edu.cn
† These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Advertisement
Sleep Duration and Executive Function in Adults
- Open access
- Published: 14 November 2023
- Volume 23 , pages 801–813, ( 2023 )
Cite this article
You have full access to this open access article
- Aayushi Sen 1 , 2 &
- Xin You Tai 1 , 2
6068 Accesses
23 Altmetric
Explore all metrics
Purpose of Review
To review the literature examining the relationship between sleep and cognition, specifically examining the sub-domain of executive function. We explore the impact of sleep deprivation and the important question of how much sleep is required for optimal cognitive performance. We consider how other sleep metrics, such as sleep quality, may be a more meaningful measure of sleep. We then discuss the putative mechanisms between sleep and cognition followed by their contribution to developing dementia.
Recent Findings
Sleep duration and executive function display a quadratic relationship. This suggests an optimal amount of sleep is required for daily cognitive processes. Poor sleep efficiency and sleep fragmentation are linked with poorer executive function and increased risk of dementia during follow-up. Sleep quality may therefore be more important than absolute duration. Biological mechanisms which may underpin the relationship between sleep and cognition include brain structural and functional changes as well as disruption of the glymphatic system.
Sleep is an important modifiable lifestyle factor to improve daily cognition and, possibly, reduce the risk of developing dementia. The impact of optimal sleep duration and sleep quality may have important implications for every ageing individual.
Similar content being viewed by others

Impact of sleep duration on executive function and brain structure
Xin You Tai, Cheng Chen, … Masud Husain

Sleep-Related Changes Prior to Cognitive Dysfunction
Laura Pérez-Carbonell & Alex Iranzo
Poorer sleep impairs brain health at midlife
Tergel Namsrai, Ananthan Ambikairajah & Nicolas Cherbuin
Avoid common mistakes on your manuscript.
Introduction
Sleep is an integral part of human life and is linked to optimal performance across a broad range of physiological and psychological functions [ 1 , 2 , 3 , 4 ]. The relationship between sleep and executive function is an area of intense interest as optimising sleep may be one avenue to improve cognition as we grow older. Executive function, a critical cognitive domain for day-to-day living, has been closely linked to sleep patterns as we grow older. For instance, sleep deprivation is associated with increased frequency of mistakes by shift workers [ 5 ] and increased reliance on habits rather than goal-directed decisions that require executive control [ 6 ]. Despite a growing body of literature, the exact nature of the relationship between sleep and cognition remains unclear. Importantly, what is the optimal amount of sleep required for cognitive functioning? Does this change as we age? These are not straightforward questions, as studies have highlighted different sleep lengths as detrimental or beneficial for cognitive performance. Additionally, how strong is the causal relationship between sleep and cognition? This is crucial if sleep is to be considered a key modifiable lifestyle factor to optimise cognition and mitigate risk of certain brain disorders, especially dementia.
This article offers an overview of the current literature examining sleep duration and executive function in mid-to-late life and will explore key issues including potential underlying mechanisms, the link with brain structural health, and potential contribution to developing dementia.
The Importance of Executive Function
Executive function is the orchestration of goal-oriented processes that include attention, problem solving, planning, and working memory. This includes the ability to hold information in your short-term memory, manipulate that information, and decide which part of the information is important for the task at hand. Executive functioning is particularly developed in humans compared to other animals, and is important for performing everyday tasks ranging from getting dressed, following a recipe, driving a car to more complex problems [ 7 ]. During adulthood, executive function declines with age along with several other cognitive domains [ 8 , 9 , 10 ]. Furthermore, executive function is commonly affected across a wide range of neurological and psychological disorders such as dementia (particularly fronto-temporal dementia), stroke, and head trauma [ 11 , 12 , 13 , 14 ]. It is therefore critical to understand modifiable factors, such as sleep, that could potentially optimise executive function.
How is Executive Function Tested?
Executive function is tested in several ways. Common measures include goal-oriented tasks like the trail-making test [ 15 ], digit-symbol substitution test (DSST) [ 16 ], Wisconsin card sorting test [ 17 ], or the Stroop test [ 18 , 19 ]. Such tasks require a combination of attention, online processing of information, and cognitive effort. Some tasks will engage cognitive control, whereby participants have to decide when to act (‘GO’) but also when not to act (‘NO-GO’), while others may require a participant to place themselves in the mind of another person (theory of mind). More general questionnaires of cognition, such as the Mini Mental State Examination (MMSE) [ 20 ] and Montreal Cognitive Assessment (MoCA) [ 21 ], may have subcomponents of executive function. These can be useful as scalable tests of cognitive ability for large-scale studies but do not assess executive function with the detail of dedicated tasks. By contrast, there are specific cognitive tasks of executive function created to answer specific questions [ 22 , 23 ], but these may be hard to incorporate into larger studies. Box 1 demonstrates 3 tests you can try yourself.
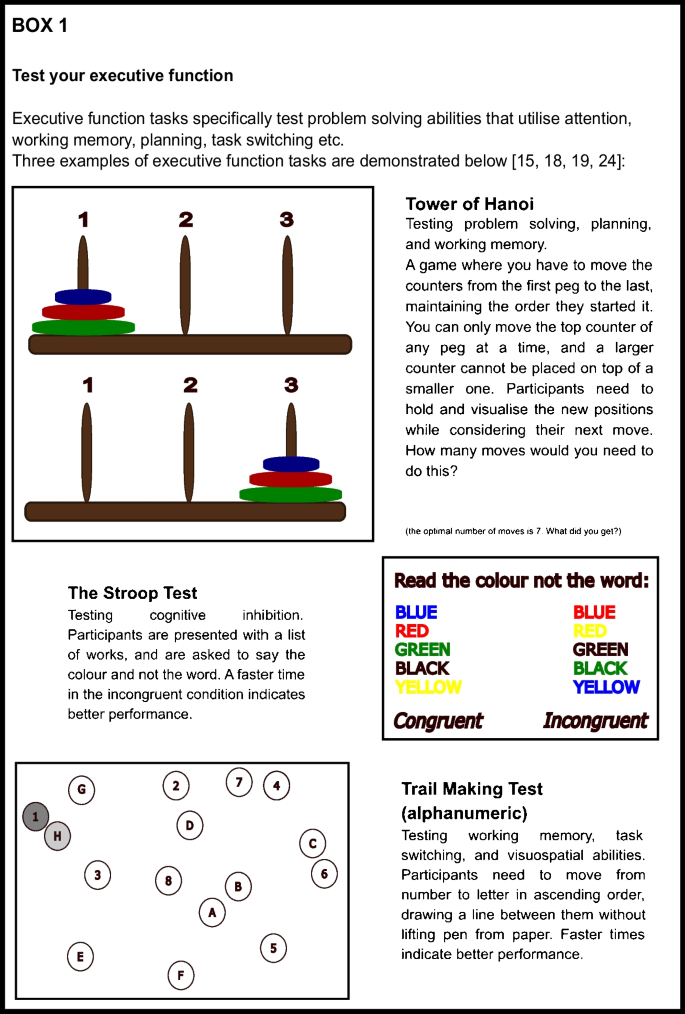
Sleep deprivation is common, with 11.8% of respondents reporting less than 5 h sleep on average in a large US survey [ 25 ]. Deficits in motor performance due to sleep deprivation are equivalent to blood alcohol content of 0.05–0.1%, which is comparable to the legal driving limit of 0.08% [ 26 ] in England and the USA. A single night of sleep deprivation has been shown to affect several components of executive function such as sustained attention, reaction time, and working memory, as well as other cognitive domains of consolidation of episodic and procedural memory [ 27 ].
Sleep deprivation experiments can involve keeping participants awake for an extended period of time (usually over 24 h), or restricting sleep to only a few hours over multiple days. Cognition is tested before, during, and after sleep deprivation periods. Tasks requiring sustained attention show worse performance over 28 h of sleep deprivation [ 28 ]; with more pronounced effects, the more mundane the task is [ 29 ]. Creative thought processes are affected more than rule-based processes [ 30 ], and people revert to habitual actions rather than goal-directed actions for the task at hand [ 6 ].
The real-life impact of sleep deprivation is exemplified in studies of risk aversion, with several prominent studies examining occupations such as the military. Sleep-deprived individuals have impaired risk perception, where they performed worse in a simulated balloon overinflation experiment after 36 h of staying awake. Doing well on this task requires participants to pay attention to the balloon; contextualise it with previous inflation attempts; assess, in real time, the odds of the balloon popping; and inhibit the urge to score higher with a bigger balloon. Interestingly, poor performance in sleep-deprived participants corresponded to altered brain measures of network connectivity, compared to when the same individual was not sleep deprived [ 31 ]. This intra-subject analysis suggests that sleep deprivation may alter the way information is communicated through the brain. A meta-analysis, which pooled large amounts of data from multiple studies, involving 1341 sleep restricted military participants identified a significant negative effect on reaction times, processing speed, accuracy, and moral decision making [ 32 ].
In addition to executive function, sleep has been shown to be important for memory consolidation. Even short naps (as little as 6 min) can improve memory retention, with longer durations being particularly useful for procedural memory. Behaviourally relevant memories are favoured in sleep-dependent consolidation [ 33 ]. Therefore, unsurprisingly, sleep deprivation can negatively affect the consolidation of new memories, especially episodic [ 33 , 34 ] and procedural memory [ 35 , 36 , 37 ]. Importantly, sleep recovery (being able to sleep a ‘normal’ amount) over the course of a week can lead to improved performance in previously sleep-deprived individuals, back to the level of controls [ 36 ].
Sleep extension (sleeping longer than normal) in the short term can reduce the effect of sleep deprivation on sustained attention tasks [ 38 ] and memory [ 36 ]. There are also interesting studies investigating factors that affect resilience against sleep deprivation. Older adults showed worse performance, compared to younger adults, following sleep deprivation in multiple cognitive tasks, including those testing vigilance and reaction times [ 39 ]. By contrast, older adults did not get a benefit from interval sleep after a motor-sequence learning task, unlike their younger counterparts [ 40 ], indicating unequal reliance on sleep for different ages and types of memory consolidation. This effect has not been observed in related non-motor learning paradigms [ 41 ].
Therefore, there is robust experimental and real-life evidence that acute periods of sleep deprivation can detrimentally affect cognition. A different question remains—what is the optimal daily duration of sleep to maximise our cognitive functioning? This is relevant to the daily lifestyle habits of all ageing individuals, and may provide insight into those with the worst cognitive functioning, such as in dementia.
Long-Term Effect of Sleep: Both Short and Long Sleep Durations are Associated with Poorer Executive Function
Numerous studies examine the relationship between average sleep duration and executive function. A common way to probe this question has been to ask participants to self-report the average hours of sleep they had recently, and combine it with cognitive tests of executive function administered at a time point within the study. Using this approach, important findings have emerged.
Short and Long Sleep Durations are Related to Worse Executive Function in Cross-sectional Studies
Earlier cross-sectional studies have associated worse executive function with either short or long extremes of sleep duration [ 42 , 43 , 44 , 45 , 46 , 47 , 48 ], while more recent studies tend to link both short and long sleep durations with poor executive function [ 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 ]. There may be several reasons for these mixed findings.
Firstly, studies tend to use a variety of methods to test cognition. One study of 3212 individuals aged over 60 demonstrated a worse MMSE score for every hour over 7 h of sleep per day in a linear analysis, but no difference in short sleepers [ 42 ]. Similar findings were also identified in a study which accounted for sleep-disordered breathing, which is often cited as a missed confounder in long sleep duration and cognitive impairment [ 50 ]. A linearly worsening trend at longer sleep durations was also seen in a study of executive function (testing DSST). This trend persisted after adjusting for sex, age, education, and BMI, but unfortunately, hypertension and hypnotic medications were not accounted for [ 44 ]. A smaller study of 189 individuals interestingly showed significantly lower MoCA scores with long sleep duration, but not MMSE scores [ 45 ]. In contrast with these studies however, worse MMSE scores [ 59 , 60 ] and immediate and delayed recall [ 60 ] have also been associated with shorter sleep. One study showed a linear relationship of worsening global cognition over 2 years with every hour of sleep less than 7 h, when adjusted for sex, age, education, and BMI [ 61 ]. Therefore, the broad nature of these cognitive tests may have contributed to different findings.
Secondly, different definitions and thresholds of sleep durations have been applied across studies as ‘long’ sleep duration can range from greater than 7 h to greater than 11 h [ 42 , 43 , 44 , 45 , 47 , 48 ]. Conversely, a ‘short’ sleep duration can range from less than 8 h to less than 4 h depending on the specific study [ 56 , 59 , 60 , 61 , 62 , 63 ], which may also contribute to the heterogeneity of results.
Sleep thresholds are now less important, as recent studies have been able to investigate how every hour of sleep reported relates to executive function. This has been made possible by large study cohorts which have consistently identified a quadratic, or inverted ‘U’-shaped, relationship between self-reported sleep duration and executive function with increasingly worse performance with both less and more sleep around a baseline of 7–8 h [ 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 64 , 65 ]. A study of around 480,000 individuals, aged 38–73 years, showed that 7 h of sleep per day was associated with the highest executive function performance, using a measure derived from specific computer-based tasks of attention and working memory. Furthermore, there was a parametric decline in executive function associated with every hour of sleep below and above 7 h suggesting an optimal sleep duration (Fig. 1 ). This finding was consistent for individuals who were below and above the age of 60 years, suggesting that an optimal sleep duration exists as individuals age. This study also showed a similar quadratic relationship between sleep duration and brain volume across 46 different cortical regions which highlights how sleep may be important for brain health [ 54 •].
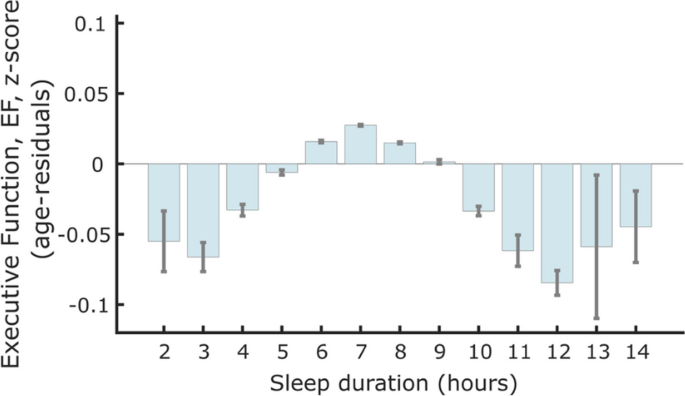
Association between sleep duration and standardised executive function score from a study of 474,417 individuals in the UK Biobank. Seven hours of self-reported sleep duration was associated with the highest executive function score. A negative relationship was present with sleeping less than 6 h and more sleep from 8 h (Tai et al. 2022, reproduced with permission from the author)
The quadratic relationship between executive function and sleep [ 54 , 64 ] is observed in other cognitive domains including memory [ 51 , 53 , 57 , 64 ], visuospatial abilities [ 51 , 65 ], verbal fluency [ 49 , 57 ], and global cognitive tests like the MMSE [ 50 , 55 , 56 ]. This quadratic association is also observed in a large study of around 513,000 participants, aged 15–89 years old, in a non-supervised, online ‘game-based’ test of processing speed, working memory, arithmetic, and visuospatial memory [ 66 ]. These findings are additionally confirmed in a more recent meta-analysis that self-reported short and long sleep increased the odds of cognitive impairment by 1.40 and 1.58 respectively [ 58 ]. Therefore, cross-sectional studies indicate both long and shorter sleep durations may be detrimental to executive functioning and, importantly, not just the extremes of sleep deprivation and over-sleeping.
Longitudinal Measurements of Sleep Duration Identify Similar Patterns with Executive Function
Cross-sectional studies compare executive function and sleep duration at a single time point. A limitation of this approach is the inability to infer causality. Longitudinal studies, which are more costly to run, offer more information in this regard although cannot strictly determine causality either. Several longitudinal studies have examined sleep duration and executive function. A study where both cognition and self-reported sleep were measured at 3 time points over 10 years showed that long sleep duration was associated with worse global cognition, but not specific cognitive domains. Unfortunately, this study failed to adjust for confounders such as depression, hypnotic use, and sleep apnoea [ 67 ]. Another longitudinal study used a combination of EEG measurement and self-reported sleep following 100 participants over 4 years, and showed worsening cognition over time was associated with both short and long sleep durations, similar to cross-sectional studies [ 68 •]. A change in sleep duration out of the optimal range, over a 5-year follow-up, was also related to worse performance in MMSE, fluency, and reasoning tasks, but had no effect on memory [ 69 ]. Longitudinal studies therefore indicate that average sleep duration, in a similar pattern to cross-sectional studies, can affect executive function and cognitive ability in the future.
Sub-optimal Sleep Duration May Predict Dementia Onset
An important consideration is whether worsening executive function over time may represent the development of dementia. One study of 2457 elderly participants from the Framingham cohort showed double the risk in those who reported long sleep to be diagnosed with dementia, even when adjusted for a genetic predisposition for Alzheimer’s. Transitioning to long sleep was also associated with a higher risk, than those who previously slept for long durations [ 70 ]. Two 2019 meta-analyses support the findings of long sleep being associated with incident dementia [ 71 , 72 ]. However, a well-controlled longitudinal study of 7959 participants of the Whitehall II study over 25 years indicated that self-reported short sleep duration in mid-life was associated with incident dementia when elderly. They further confirmed this association with objective sleep measures in a subpopulation of 3888 participants. There was no link with long sleep, which they report is due to the fact they are looking at sleep durations from mid-life, whereas other studies focus on the elderly—when any impending dementia may already be affecting sleep patterns [ 73 ••]. Therefore, there is evidence that both short and long reported sleep duration may be associated with developing dementia.
Objective Measurements of Sleep Duration and Executive Function
Why are both long and short durations associated with worse executive function? There may be biological reasons, which will be discussed below, as well as practical reasons. Self-reported sleep habits from large cross-sectional studies may not represent true sleep characteristics, as individuals may either over- or under-estimate how long they sleep. Generally, people tend to report ‘time in bed’ rather than actual time asleep [ 74 ]. There are also a tendency for those with insomnia to under-report sleep duration and a tendency of those with fragmented sleep (e.g. those with obstructive sleep apnoea (OSA) or depression) to over-report sleep duration [ 75 , 76 ].
More accurate data comes from electroencephalography (EEG) or actigraphy studies, which objectively measure when an individual is sleeping and delineate sleep stages. While EEG studies are more difficult to carry out and often have smaller sample sizes, actigraphy is increasingly used in large samples to investigate sleep duration [ 46 , 77 , 78 ]. Results from some EEG and actigraphy studies conflict with self-reported sleep data, with total sleep time showing little association with executive function. Blackwell et al. found that total sleep time (TST) measured by actigraphy was related to MMSE score, but not to the trail-making test [ 46 ], while Suemoto et al. demonstrated no impairments related to actigraphy-measured TST (10-word list, verbal fluency, and trail-making tests) [ 79 ]. Similarly, a meta-analysis of actigraphy and EEG studies showed no associations with TST. Importantly though, early studies were limited by the use of linear analysis models, which may have missed the quadratic relationship recently described between sleep duration and performance. However, a longitudinal study that used both EEG measurement and self-reported sleep had findings consistent with cross-sectional studies with worsening cognition over time in short and long sleep durations [ 68 •]. These objective sleep studies hint at a relationship between sleep and cognition that may go beyond just length of sleep.
In summary, recent literature has emphasised the quadratic relationship between sleep duration and executive function and suggests that there may be an optimal duration of sleep to maximise our cognitive performance. This has both personal and public health implications. However, an interesting and important question that has emerged from objective sleep monitoring studies is whether total sleep duration alone is the best measure of sleep. In the next section, we consider how sleep characteristics other than sleep duration may be relevant to the relationship with executive function.
Sleep Quality May Be More Relevant for Long-Term Cognitive Outcomes than Absolute Duration
Sleep quality may be more important than sleep duration alone when considering the impact on executive function. Evidence from studies with objective sleep recording rather than self-reported sleep duration indicates that time spent in different sleep stages and sleep fragmentation may correlate better to cognitive function than total sleep time alone [ 78 , 79 , 80 , 81 , 82 , 83 ]. Subjective sleep quality, such as asking whether the participants felt well rested, also correlates better to cognitive function over absolute duration [ 84 ].
There are three main reasons for why this effect of sleep ‘quality over quantity’ in relation to cognition may be relevant. Firstly, as discussed previously, there may be several biases with self-reported sleep duration [ 74 , 75 , 76 ], which may mean the extremes of self-reported sleep durations are acting as a surrogate for poor sleep quality.
Secondly, conditions associated with poor sleep quality are also often related to poor general cognition. This could confound the relationship between sleep and executive function. For example, individuals with OSA can wake numerous times overnight with brief apnoeic spells resulting in poor sleep. This condition is associated with obesity and resistant hypertension [ 85 , 86 ], which can lead to a decline in cognition via small vessel disease in the brain. Thirdly, sleep architecture evolves with age. Sleep efficiency (SE) (time spent asleep between first falling asleep and waking in the morning) decreases from 89 to 79% from middle age to 70 years old, and the change accelerates over the age of 70 [ 87 ]. Given there is concurrent cognitive decline naturally in this time [ 8 , 9 , 10 ], parsing out the effect of sleep and other factors is difficult but important.
Several studies have explored the link between sleep quality and executive function using various methods. Actigraphy uses a wearable device that measures movements when going to bed to assess parameters like total sleep time (TST), sleep onset latency (SOL), wake after sleep onset (WASO), and general restlessness to gauge quality of sleep. EEG studies tend to use time in slow wave sleep (SWS), rapid eye movement sleep (REM), and non-REM sleep (nREM), as well as the presence and density of sleep spindles [ 88 , 89 ]. Other studies rely on participants reporting whether or not they had a restful and restorative sleep [ 83 , 84 ]. Together, these may be used to give an indication of ‘sleep quality’, or of ‘sleep fragmentation’, rather than self-reported sleep duration.
Feeling rested after sleep or not, regardless of actual time reported asleep, was reported to be more indicative of speed and flexibility of processing [ 67 ]. Similarly, Teräs et al. reported better executive function in those who reported restorative sleep, in a cross-sectional study of healthy mid-old age participants [ 83 ]. Those with more restful nights did better in memory tasks, and those with decreased SOL did better in executive function tasks in a meta-analysis of actigraphy-measured sleep and cognition [ 81 ••]. More time in REM was associated with better executive function in adults aged 20–84 (tested with a goal neglect task), and more SWS and sleep spindles were associated with faster response times, an indication of attention and reaction time [ 80 ]. Sleep spindle density was also recently reported to be associated with better executive function (using DSST, card sorting, and Stroop) and MoCA scores in a cross-sectional study of sedentary 63 middle-older aged participants [ 90 ].
A recent prospective study investigating incident cognitive impairment 4 years after baseline polysomnography found a small, but statistically significant, association of shorter average sleep cycle length and average REM duration [ 82 ]. A similar study published in 2023 additionally reported no association on executive function or global cognitive performance with actigraphy-measured TST or SOL. They did however have small associations between lower SE and poorer visuospatial ability. A limitation of the study was only having follow-up data on 70% of the original participants. They also commented on different associations seen between the (self-identified) White and Black participants; with poor sleep having a greater effect on Black participants [ 91 ].
In summary, executive function appears to be reliably related to sleep quality as measured by sleep onset latency, wake after sleep onset, and whether participants seem rested or not. EEG studies indicate that time in REM and SWS may be important to the mechanism by which sleep affects cognition. Sleep quality should be considered and investigated specifically in any future studies investigating the link between sleep and executive function.
Biological Mechanisms Underlying the Link Between Sleep and Executive Function
Why is sleep so important to executive function? Studies have explored several biological mechanisms that may underlie the link between sleep and executive function. These include potential changes in brain volume, alterations in brain connectivity, accumulation of neurodegenerative proteins, and disrupted glymphatic drainage (summarised in Fig. 2 ).
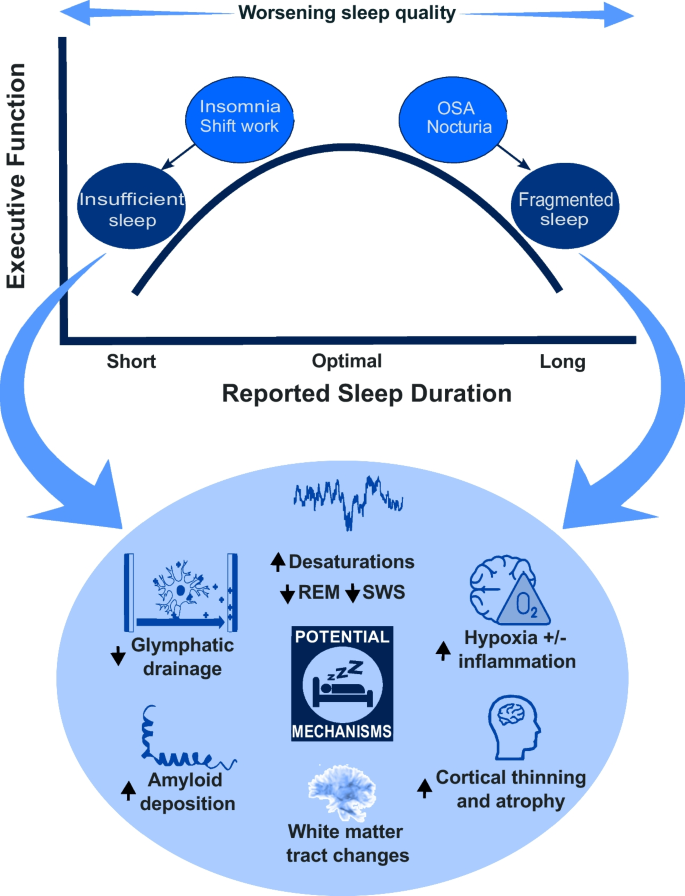
A summary diagram illustrating the relationship between self-reported sleep duration and executive function and the potential mechanisms by which this may occur. SWS slow wave sleep, REM rapid eye movement, OSA obstructive sleep apnoea
Poor sleep may lead to reduced brain volume which affects cognition. A large imaging study has demonstrated a quadratic relationship between sleep duration and executive function and multiple areas of reduced cortical volume [ 54 •]. Cortical thinning was seen with reduced REM sleep [ 92 ] and in patients with severe OSA and sleep fragmentation; this was, importantly, shown to be partially reversible after 18 months of CPAP therapy [ 93 ].
Changes in brain connectivity may also underpin the effects of sleep deprivation. Diffusion tensor imaging, used to visualise white matter tracts in the brain, has demonstrated changes in structural brain connectivity after just one night of sleep deprivation [ 27 , 94 ] and with prolonged sleep restriction [ 95 , 96 ]. A study of young healthy volunteers indicated that goal-directed learning mainly recruited the ventro-medial prefrontal cortex (vmPFC) on fMRI; after sleep deprivation, this activation was less pronounced reflecting worse functional brain connectivity [ 6 ].
Beyond changes in brain structure, studies using positron emission tomography (PET) imaging [ 97 ] suggest accumulation of neurodegenerative proteins is associated with sleep deprivation [ 98 ]. Beta-amyloid is one of two main pathological proteins described in Alzheimer’s disease, the most common form of dementia. Increased amyloid plaques on PET scan, along with reduced cerebrospinal fluid (CSF) amyloid (indicating increased amyloid deposition) over 2 years, were described in 208 cognitively healthy elderly people with OSA [ 99 ]. Beta-amyloid plaques are also increased in cognitively intact adults who have shorter and poorer quality reported sleep, as well as those with poor objective sleep quality [ 100 ]. While not the remit of this review, there is a growing animal model literature which corroborates findings of accelerated amyloid plaque and tau tangle formation in sleep-deprived states [ 101 ].
More recently, the role of glymphatic drainage, representing the waste clearance system of the brain, has been proposed as a mechanism by which amyloid and other toxic metabolites are removed from the brain. One line of evidence suggests that amyloid production in Alzheimer’s may be the same as in healthy people, but that clearance is significantly slowed [ 100 ]. The glymphatic system is primarily active during sleep and affected by several factors including sleep architecture (more active during SWS) and the general physiological milieu including hormones like cortisol and noradrenaline [ 100 , 102 , 103 ]. Amyloid uptake shows an inverse relationship with nREM slow wave activity [ 104 ]. Amyloid levels in the interstitia are higher in wakefulness in mice, and a small human study found similar results [ 105 ], indicating that sleep deprivation may lead to higher amyloid plaque levels via reduced clearance from the brain. This offers a tangible mechanism linking poor sleep to worse cognitive functions and, possibly, increased risk of dementia.
In summary, there are several mechanisms in which poor sleep may contribute to impaired executive function with reduced quality of sleep. The underlying process is likely to be multifactorial involving a complex relationship between these biological processes (Fig. 2 ). Future studies must consider this complexity to better understand the causal nature between sleep and cognition.
Conclusion and Future Directions
The prospect that sleep may be a modifiable lifestyle factor that can improve our executive function and reduce risk of dementia is both tantalising and real. This is important, especially considering that the worldwide prevalence of dementia is expected to increase by 117% from 2019 to 2050 [ 106 ]. There is consistent evidence for an optimal duration of sleep for cognitive function which is relevant to the personal health of every ageing individual. It is important, however, to remember that these findings reflect a group effect and the exact optimal duration may differ between individuals. Furthermore, other sleep factors may be equally important as the duration of sleep.
Future studies should consider both objective sleep duration and quality by incorporating detailed sleep measurements using actigraphy or EEG where possible. The potential benefits justify the costs of such studies at large scale, while the advent of machine learning and artificial intelligence will allow better data processing and interpretation. Development of short, pragmatic cognitive batteries [ 107 ] which can be performed remotely and are not culturally specific would improve the feasibility of large-scale, standardised multicentre studies. These technologies would allow longitudinal tracking of cognition and sleep in which, as described, very little research has been conducted to date. The causal direction between sleep and executive function should be further explored through interventional trials which may have an active arm of individuals with targeted sleep advice and support compared to match controls. Furthermore, using alternate approaches such as Mendelian randomisation to leverage genetic information [ 108 ] should be performed in larger, diverse populations.
From a scientific perspective, we must better understand the underlying mechanisms linking sleep to cognition and, especially, to the risk of dementia. Moving forward, sleep studies in humans would benefit from the arrival of plasma biomarkers of neurodegeneration such as beta-amyloid, phosphorylated tau, and neurofilament light chain [ 109 ]. Such in vivo and minimally invasive measurements of pathological processes have revolutionised the current landscape of dementia research and clinical trials. It is a clear next step for the study of sleep, cognition, and dementia.
In this review, we have tried to identify what is currently understood around sleep and executive function. We have highlighted the expansive literature around sleep duration and executive function and the growing importance of examining sleep quality. We have considered important questions around causality and underlying mechanisms while showing broadly what is currently understood. Finally, we have discussed areas of future research that may expand our understanding around sleep as a modifiable lifestyle factor for cognition, specifically executive function, and the global problem of dementia.
Data Availability
Not applicable.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Tarokh L, Saletin JM, Carskadon MA. Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev. 2016;70:182–8. https://doi.org/10.1016/j.neubiorev.2016.08.008 .
Article PubMed PubMed Central Google Scholar
Luyster FS, Strollo PJ, Zee PC, Walsh JK. Sleep: a health imperative. Sleep. 2012;35:727–34. https://doi.org/10.5665/sleep.1846 .
Depner CM, Stothard ER, Wright KP. Metabolic consequences of sleep and circadian disorders. Curr Diab Rep. 2014;14:507. https://doi.org/10.1007/s11892-014-0507-z .
Article CAS PubMed PubMed Central Google Scholar
Swanson CM, Kohrt WM, Buxton OM, Everson CA, Wright KP, Orwoll ES, Shea SA. The importance of the circadian system & sleep for bone health. Metabolism. 2018;84:28–43. https://doi.org/10.1016/j.metabol.2017.12.002 .
Article CAS PubMed Google Scholar
Yeo H, Lee J, Jeon S, Lee S, Hwang Y, Kim J, Kim SJ. Sleep disturbances, depressive symptoms, and cognitive efficiency as determinants of mistakes at work in shift and non-shift workers. Front Public Health. 2022;10:1030710. https://doi.org/10.3389/fpubh.2022.1030710 .
Chen J, Liang J, Lin X, Zhang Y, Zhang Y, Lu L, Shi J. Sleep deprivation promotes habitual control over goal-directed control: behavioral and neuroimaging evidence. J Neurosci. 2017;37:11979–92. https://doi.org/10.1523/JNEUROSCI.1612-17.2017 .
Benarroch EE. Neuroscience for clinicians: basic processes, circuits, disease mechanisms, and therapeutic implications. 1st ed. Oxford University Press; 2021.
Book Google Scholar
Park DC, Lautenschlager G, Hedden T, Davidson NS, Smith AD, Smith PK. Models of visuospatial and verbal memory across the adult life span. Psychol Aging. 2002;17:299–320. https://doi.org/10.1037/0882-7974.17.2.299 .
Article PubMed Google Scholar
Cansino S, Hernández-Ramos E, Estrada-Manilla C, Torres-Trejo F, Martínez-Galindo JG, Ayala-Hernández M, Gómez-Fernández T, Osorio D, Cedillo-Tinoco M, Garcés-Flores L, Beltrán-Palacios K, García-Lázaro HG, García-Gutiérrez F, Cadena-Arenas Y, Fernández-Apan L, Bärtschi A, Rodríguez-Ortiz MD. The decline of verbal and visuospatial working memory across the adult life span. Age (Dordr). 2013;35:2283–302. https://doi.org/10.1007/s11357-013-9531-1 .
Hale S, Rose NS, Myerson J, Strube MJ, Sommers M, Tye-Murray N, Spehar B. The structure of working memory abilities across the adult life span. Psychol Aging. 2011;26:92–110. https://doi.org/10.1037/a0021483 .
Pohjasvaara T, Leskelä M, Vataja R, Kalska H, Ylikoski R, Hietanen M, Leppävuori A, Kaste M, Erkinjuntti T. Post-stroke depression, executive dysfunction and functional outcome. Eur J Neurol. 2002;9:269–75. https://doi.org/10.1046/j.1468-1331.2002.00396.x .
Azouvi P, Arnould A, Dromer E, Vallat-Azouvi C. Neuropsychology of traumatic brain injury: an expert overview. Rev Neurol (Paris). 2017;173:461–72. https://doi.org/10.1016/j.neurol.2017.07.006 .
Olney NT, Spina S, Miller BL. Frontotemporal dementia. Neurol Clin. 2017;35:339–74. https://doi.org/10.1016/j.ncl.2017.01.008 .
Zhang S, Shen L, Jiao B. Cognitive dysfunction in repeat expansion diseases: a review. Front Aging Neurosci. 2022;14: 841711. https://doi.org/10.3389/fnagi.2022.841711 .
Bowie CR, Harvey PD. Administration and interpretation of the trail making test. Nat Protoc. 2006;1:2277–81. https://doi.org/10.1038/nprot.2006.390 .
Boake C. From the Binet-Simon to the Wechsler-Bellevue: tracing the history of intelligence testing. J Clin Exp Neuropsychol. 2002;24:383–405. https://doi.org/10.1076/jcen.24.3.383.981 .
Lezak MD. Neuropsychological Assessment. Oxford University Press; 2004.
Google Scholar
Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18:643–62. https://doi.org/10.1037/h0054651 .
Article Google Scholar
Periáñez JA, Lubrini G, García-Gutiérrez A, Ríos-Lago M. Construct validity of the stroop color-word test: influence of speed of visual search, verbal fluency, working memory, cognitive flexibility, and conflict monitoring. Arch Clin Neuropsychol. 2021;36:99–111. https://doi.org/10.1093/arclin/acaa034 .
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. https://doi.org/10.1016/0022-3956(75)90026-6 .
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9. https://doi.org/10.1111/j.1532-5415.2005.53221.x .
Richter FR, Yeung N. Memory and cognitive control in task switching. Psychol Sci. 2012;23:1256–63. https://doi.org/10.1177/0956797612444613 .
Ledochowski J, Andrade BF, Toplak ME. A novel unstructured performance-based task of executive function in children with attention-deficit/hyperactivity disorder. J Clin Exp Neuropsychol. 2019;41:445–59. https://doi.org/10.1080/13803395.2019.1567694 .
Yochim BP, Baldo JV, Kane KD, Delis DC. D-KEFS Tower Test performance in patients with lateral prefrontal cortex lesions: the importance of error monitoring. J Clin Exp Neuropsychol. 2009;31:658–63. https://doi.org/10.1080/13803390802448669 .
Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of Healthy Sleep Duration among Adults — United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65:137–141. https://doi.org/10.15585/mmwr.mm6506a1
Williamson A, Feyer A. Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med. 2000;57:649–55. https://doi.org/10.1136/oem.57.10.649 .
Krause AJ, Ben Simon E, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, Walker MP. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18:404–18. https://doi.org/10.1038/nrn.2017.55 .
Pilcher JJ, McClelland LE, Moore DD, Haarmann H, Baron J, Wallsten TS, McCubbin JA. Language performance under sustained work and sleep deprivation conditions. Aviat Space Environ Med. 2007;78:B25-38.
PubMed Google Scholar
Pilcher JJ, Band D, Odle-Dusseau HN, Muth ER. Human performance under sustained operations and acute sleep deprivation conditions: toward a model of controlled attention. Aviat Space Environ Med. 2007;78:B15-24.
Killgore WDS. Effects of sleep deprivation on cognition. In: Kerkhof GA, van Dongen HPA, editors. Progress in brain research. Elsevier; 2010. p. 105–29.
Chen J, Gong X, Wang L, Xu M, Zhong X, Peng Z, Song T, Xu L, Lian J, Shao Y, Weng X. Altered postcentral connectivity after sleep deprivation correlates to impaired risk perception: a resting-state functional magnetic resonance imaging study. Brain Sci. 2023;13:514. https://doi.org/10.3390/brainsci13030514 .
Petrofsky LA, Heffernan CM, Gregg BT, Smith-Forbes EV. Effects of sleep deprivation in military service members on cognitive performance: a systematic review. Mil Behav Health. 2022;10:202–20. https://doi.org/10.1080/21635781.2021.1982088 .
Diekelmann S, Born J. The memory function of sleep. Nat Rev Neurosci. 2010;11:114–26. https://doi.org/10.1038/nrn2762 .
Berres S, Erdfelder E. The sleep benefit in episodic memory: an integrative review and a meta-analysis. Psychol Bull. 2021;147:1309–53. https://doi.org/10.1037/bul0000350 .
Stepan ME, Fenn KM, Altmann EM. Effects of sleep deprivation on procedural errors. J Exp Psychol Gen. 2019;148:1828–33. https://doi.org/10.1037/xge0000495 .
Kurniawan IT, Cousins JN, Chong PLH, Chee MWL. Procedural performance following sleep deprivation remains impaired despite extended practice and an afternoon nap. Sci Rep. 2016;6:36001. https://doi.org/10.1038/srep36001 .
Newbury CR, Crowley R, Rastle K, Tamminen J. Sleep deprivation and memory: meta-analytic reviews of studies on sleep deprivation before and after learning. Psychol Bull. 2021;147:1215–40. https://doi.org/10.1037/bul0000348 .
Arnal PJ, Sauvet F, Leger D, van Beers P, Bayon V, Bougard C, Rabat A, Millet GY, Chennaoui M. Benefits of sleep extension on sustained attention and sleep pressure before and during total sleep deprivation and recovery. Sleep. 2015;38:1935–43. https://doi.org/10.5665/sleep.5244 .
Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half-century of multidisciplinary research. Perspect Psychol Sci. 2015;10:97–137. https://doi.org/10.1177/1745691614556680 .
Spencer RMC, Gouw AM, Ivry RB. Age-related decline of sleep-dependent consolidation. Learn Mem. 2007;14:480–4. https://doi.org/10.1101/lm.569407 .
Aly M, Moscovitch M. The effects of sleep on episodic memory in older and younger adults. Memory. 2010;18:327–34. https://doi.org/10.1080/09658211003601548 .
Faubel R, López-García E, Guallar-Castillón P, Graciani A, Banegas JR, Rodríguez-Artalejo F. Usual sleep duration and cognitive function in older adults in Spain. J Sleep Res. 2009;18:427–35. https://doi.org/10.1111/j.1365-2869.2009.00759.x .
Kondo R, Miyano I, Lee S, Shimada H, Kitaoka H. Association between self-reported night sleep duration and cognitive function among older adults with intact global cognition. Int J Geriatr Psychiatry. 2021;36:766–74. https://doi.org/10.1002/gps.5476 .
Low DV, Wu MN, Spira AP. Sleep duration and cognition in a nationally representative sample of U.S. older adults. Am J Geriatr Psychiatry. 2019;27:1386–96. https://doi.org/10.1016/j.jagp.2019.07.001 .
Malek-Ahmadi M, Kora K, O’Connor K, Schofield S, Coon D, Nieri W. Longer self-reported sleep duration is associated with decreased performance on the montreal cognitive assessment in older adults. Aging Clin Exp Res. 2016;28:333–7. https://doi.org/10.1007/s40520-015-0388-2 .
Blackwell T, Yaffe K, Ancoli-Israel S, Schneider JL, Cauley JA, Hillier TA, Fink HA, Stone KL, Study of Osteoporotic Fractures Group. Poor sleep is associated with impaired cognitive function in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2006;61:405–10. https://doi.org/10.1093/gerona/61.4.405 .
Benito-León J, Louis ED, Bermejo-Pareja F. Cognitive decline in short and long sleepers: a prospective population-based study (NEDICES). J Psychiatr Res. 2013;47:1998–2003. https://doi.org/10.1016/j.jpsychires.2013.09.007 .
Kim H-B, Myung S-K, Lee S-M, Park YC, Group TKM-A (KORMA) S. Longer duration of sleep and risk of cognitive decline: a meta-analysis of observational studies. NED. 2016;47:171–80. https://doi.org/10.1159/000454737 .
Ma Y, Liang L, Zheng F, Shi L, Zhong B, Xie W. Association between sleep duration and cognitive decline. JAMA Netw Open. 2020;3:e2013573. https://doi.org/10.1001/jamanetworkopen.2020.13573 .
Ramos AR, Dong C, Elkind MSV, Boden-Albala B, Sacco RL, Rundek T, Wright CB. Association between sleep duration and the mini-mental score: the Northern Manhattan study. J Clin Sleep Med. 2013;9:669–73. https://doi.org/10.5664/jcsm.2834 .
Li M, Wang N, Dupre ME. Association between the self-reported duration and quality of sleep and cognitive function among middle-aged and older adults in China. J Affect Disord. 2022;304:20–7. https://doi.org/10.1016/j.jad.2022.02.039 .
Kyle SD, Sexton CE, Feige B, Luik AI, Lane J, Saxena R, Anderson SG, Bechtold DA, Dixon W, Little MA, Ray D, Riemann D, Espie CA, Rutter MK, Spiegelhalder K. Sleep and cognitive performance: cross-sectional associations in the UK Biobank. Sleep Med. 2017;38:85–91. https://doi.org/10.1016/j.sleep.2017.07.001 .
Xu L, Jiang CQ, Lam TH, Liu B, Jin YL, Zhu T, Zhang WS, Cheng KK, Thomas GN. Short or long sleep duration is associated with memory impairment in older chinese: the Guangzhou Biobank Cohort Study. Sleep. 2011;34:575–80. https://doi.org/10.1093/sleep/34.5.575 .
• Tai XY, Chen C, Manohar S, Husain M. Impact of sleep duration on executive function and brain structure. Commun Biol. 2022;5:201. https://doi.org/10.1038/s42003-022-03123-3 . ( A large study investigating sleep duration and executive function with a whole brain volumetric analysis in individuals from the UK Biobank. )
Chen W-C, Wang X-Y. Longitudinal associations between sleep duration and cognitive impairment in Chinese elderly. Front Aging Neurosci. 2022;14:1037650. https://doi.org/10.3389/fnagi.2022.1037650 .
Devore EE, Grodstein F, Schernhammer ES. Sleep duration in relation to cognitive function among older adults: a systematic review of observational studiNeuroepidemiology. 2016;46:57–78. https://doi.org/10.1159/000442418 .
Kronholm E, Sallinen M, Suutama T, Sulkava R, Era P, Partonen T. Self-reported sleep duration and cognitive functioning in the general population. J Sleep Res. 2009;18:436–46. https://doi.org/10.1111/j.1365-2869.2009.00765.x .
Lo JC, Groeger JA, Cheng GH, Dijk D-J, Chee MWL. Self-reported sleep duration and cognitive performance in older adults: a systematic review and meta-analysis. Sleep Med. 2016;17:87–98. https://doi.org/10.1016/j.sleep.2015.08.021 .
Deng X, Pan X, Cheng X, Zhang J, Wang L, Sang S, Zhong C, Fei G. Sleep duration positively correlates with global cognition in the non-demented older adults with high school or above education. J Integr Neurosci. 2022;21:168. https://doi.org/10.31083/j.jin2106168 .
Winer JR, Deters KD, Kennedy G, Jin M, Goldstein-Piekarski A, Poston KL, Mormino EC. Association of short and long sleep duration with amyloid-β burden and cognition in aging. JAMA Neurol. 2021;78:1187–96. https://doi.org/10.1001/jamaneurol.2021.2876 .
Lo JC, Loh KK, Zheng H, Sim SKY, Chee MWL. Sleep duration and age-related changes in brain structure and cognitive performance. Sleep. 2014;37:1171–8. https://doi.org/10.5665/sleep.3832 .
Tworoger SS, Lee S, Schernhammer ES, Grodstein F. The association of self-reported sleep duration, difficulty sleeping, and snoring with cognitive function in older women. Alzheimer Dis Assoc Disord. 2006;20:41–8. https://doi.org/10.1097/01.wad.0000201850.52707.80 .
Ohayon MM, Vecchierini M-F. Daytime sleepiness and cognitive impairment in the elderly population. Arch Intern Med. 2002;162:201–8. https://doi.org/10.1001/archinte.162.2.201 .
Ramos AR, Tarraf W, Daviglus M, Davis S, Gallo LC, Mossavar-Rahmani Y, Penedo FJ, Redline S, Rundek T, Sacco RL, Sotres-Alvarez D, Wright CB, Zee PC, González HM. Sleep duration and neurocognitive function in the hispanic community health study/study of Latinos. Sleep. 2016;39:1843–51. https://doi.org/10.5665/sleep.6166 .
Wild CJ, Nichols ES, Battista ME, Stojanoski B, Owen AM. Dissociable effects of self-reported daily sleep duration on high-level cognitive abilities. Sleep. 2018;41:zsy82. https://doi.org/10.1093/sleep/zsy182 .
Richards A, Inslicht SS, Metzler TJ, Mohlenhoff BS, Rao MN, O’Donovan A, Neylan TC. Sleep and cognitive performance from teens to old age: more is not better. Sleep. 2017;40:zsw029. https://doi.org/10.1093/sleep/zsw029 .
van Oostrom SH, Nooyens ACJ, van Boxtel MPJ, Verschuren WMM. Long sleep duration is associated with lower cognitive function among middle-age adults - the Doetinchem Cohort Study. Sleep Med. 2018;41:78–85. https://doi.org/10.1016/j.sleep.2017.07.029 .
• Lucey BP, Wisch J, Boerwinkle AH, Landsness EC, Toedebusch CD, McLeland JS, Butt OH, Hassenstab J, Morris JC, Ances BM, Holtzman DM. Sleep and longitudinal cognitive performance in preclinical and early symptomatic Alzheimer’s disease. Brain. 2021;144:2852–62. https://doi.org/10.1093/brain/awab272 . ( A well-designed longitudinal study investigating objective sleep measures, executive function, and incident dementia )
Ferrie JE, Shipley MJ, Akbaraly TN, Marmot MG, Kivimäki M, Singh-Manoux A. Change in sleep duration and cognitive function: findings from the Whitehall II Study. Sleep. 2011;34:565–73. https://doi.org/10.1093/sleep/34.5.565 .
Westwood AJ, Beiser A, Jain N, Himali JJ, DeCarli C, Auerbach SH, Pase MP, Seshadri S. Prolonged sleep duration as a marker of early neurodegeneration predicting incident dementia. Neurology. 2017;88:1172–9. https://doi.org/10.1212/WNL.0000000000003732 .
Fan L, Xu W, Cai Y, Hu Y, Wu C. Sleep duration and the risk of dementia: a systematic review and meta-analysis of prospective cohort studies. J Am Med Dir Assoc. 2019;20:1480-1487.e5. https://doi.org/10.1016/j.jamda.2019.06.009 .
Liang Y, Qu L-B, Liu H. Non-linear associations between sleep duration and the risks of mild cognitive impairment/dementia and cognitive decline: a dose-response meta-analysis of observational studies. Aging Clin Exp Res. 2019;31:309–20. https://doi.org/10.1007/s40520-018-1005-y .
•• Sabia S, Fayosse A, Dumurgier J, van Hees VT, Paquet C, Sommerlad A, Kivimäki M, Dugravot A, Singh-Manoux A. Association of sleep duration in middle and old age with incidence of dementia. Nat Commun. 2021;12:2289. https://doi.org/10.1038/s41467-021-22354-2 . ( A large, well-controlled, longitudinal study investigating sleep duration and incident dementia )
Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Sleep duration: how well do self-reports reflect objective measures? The CARDIA Sleep Study. Epidemiology. 2008;19:838–45. https://doi.org/10.1097/EDE.0b013e318187a7b0 .
Trimmel K, Eder HG, Böck M, Stefanic-Kejik A, Klösch G, Seidel S. The (mis)perception of sleep: factors influencing the discrepancy between self-reported and objective sleep parameters. J Clin Sleep Med. 2021;17:917–24. https://doi.org/10.5664/jcsm.9086 .
Scarlett S, Nolan HN, Kenny RA, O’Connell MDL. Discrepancies in self-reported and actigraphy-based sleep duration are associated with self-reported insomnia symptoms in community-dwelling older adults. Sleep Health. 2021;7:83–92. https://doi.org/10.1016/j.sleh.2020.06.003 .
Luik AI, Zuurbier LA, Hofman A, Van Someren EJW, Ikram MA, Tiemeier H. Associations of the 24-h activity rhythm and sleep with cognition: a population-based study of middle-aged and elderly persons. Sleep Med. 2015;16:850–5. https://doi.org/10.1016/j.sleep.2015.03.012 .
Blackwell T, Yaffe K, Laffan A, Ancoli-Israel S, Redline S, Ensrud KE, Song Y, Stone KL, Osteoporotic Fractures in Men (MrOS) Study Group. Associations of objectively and subjectively measured sleep quality with subsequent cognitive decline in older community-dwelling men: the MrOS sleep study. Sleep. 2014;37:655–63. https://doi.org/10.5665/sleep.3562 .
Suemoto CK, Santos RB, Giatti S, Aielo AN, Silva WA, Parise BK, Cunha LF, Souza SP, Griep RH, Brunoni AR, Lotufo PA, Bensenor IM, Drager LF. Association between objective sleep measures and cognitive performance: a cross-sectional analysis in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) study. J Sleep Res. 2023;32: e13659. https://doi.org/10.1111/jsr.13659 .
Della Monica C, Johnsen S, Atzori G, Groeger JA, Dijk D-J. Rapid eye movement sleep, sleep continuity and slow wave sleep as predictors of cognition, mood, and subjective sleep quality in healthy men and women, aged 20–84 years. Front Psychiatry. 2018;9:255. https://doi.org/10.3389/fpsyt.2018.00255 .
•• Qin S, Leong RLF, Ong JL, Chee MWL. Associations between objectively measured sleep parameters and cognition in healthy older adults: a meta-analysis. Sleep Med Rev. 2022;67: 101734. https://doi.org/10.1016/j.smrv.2022.101734 . ( Recent meta-analysis of 72 studies investigating objectively measured sleep and cognition. )
Suh SW, Han JW, Lee JR, Byun S, Kwak KP, Kim BJ, Kim SG, Kim JL, Kim TH, Ryu S-H, Moon SW, Park JH, Seo J, Youn JC, Lee DY, Lee DW, Lee SB, Lee JJ, Jhoo JH, Yoon IY, Kim KW. Short average duration of NREM/REM cycle is related to cognitive decline in an elderly cohort: an exploratory investigation. J Alzheimers Dis. 2019;70:1123–32. https://doi.org/10.3233/JAD-190399 .
Teräs T, Rovio S, Spira AP, Myllyntausta S, Pulakka A, Vahtera J, Stenholm S. Associations of accelerometer-based sleep duration and self-reported sleep difficulties with cognitive function in late mid-life: the Finnish Retirement and Aging Study. Sleep Med. 2020;68:42–9. https://doi.org/10.1016/j.sleep.2019.08.024 .
Zavecz Z, Nagy T, Galkó A, Nemeth D, Janacsek K. The relationship between subjective sleep quality and cognitive performance in healthy young adults: evidence from three empirical studies. Sci Rep. 2020;10:4855. https://doi.org/10.1038/s41598-020-61627-6 .
Lombardi C, Tobaldini E, Montano N, Losurdo A, Parati G. Obstructive sleep apnea syndrome (OSAS) and cardiovascular system. Med Lav. 2017;108:276–82. https://doi.org/10.23749/mdl.v108i4.6427 .
O’Donnell C, O’Mahony AM, McNicholas WT, Ryan S. Cardiovascular manifestations in obstructive sleep apnea: current evidence and potential mechanisms. Pol Arch Intern Med. 2021;131:550–60. https://doi.org/10.20452/pamw.16041 .
Pace-Schott EF, Spencer RMC. Age-related changes in the cognitive function of sleep. Prog Brain Res. 2011;191:75–89. https://doi.org/10.1016/B978-0-444-53752-2.00012-6 .
Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, Dulin H, Berkman LF, Buxton OM. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36:1747–55. https://doi.org/10.5665/sleep.3142 .
Walia HK, Mehra R. Chapter 24 - Practical aspects of actigraphy and approaches in clinical and research domains. In: Levin KH, Chauvel P, editors. Handbook of Clinical Neurology. Elsevier; 2019. p. 371–9.
Guadagni V, Byles H, Tyndall AV, Parboosingh J, Longman RS, Hogan DB, Hanly PJ, Younes M, Poulin MJ. Association of sleep spindle characteristics with executive functioning in healthy sedentary middle-aged and older adults. J Sleep Res. 2021;30:e13037. https://doi.org/10.1111/jsr.13037 .
Owusu JT, Rabinowitz JA, Tzuang M, An Y, Kitner-Triolo M, Zipunnikov V, Wu MN, Wanigatunga SK, Schrack JA, Thorpe RJ Jr, Simonsick EM, Ferrucci L, Resnick SM, Spira AP. Associations between objectively measured sleep and cognition: main effects and interactions with race in adults aged ≥50 years. J Gerontol: Series A. 2023;78:454–62. https://doi.org/10.1093/gerona/glac180 .
Sanchez-Espinosa MP, Atienza M, Cantero JL. Sleep deficits in mild cognitive impairment are related to increased levels of plasma amyloid-β and cortical thinning. Neuroimage. 2014;98:395–404. https://doi.org/10.1016/j.neuroimage.2014.05.027 .
Kim H, Joo E, Suh S, Kim J-H, Kim ST, Hong SB. Effects of long-term treatment on brain volume in patients with obstructive sleep apnea syndrome. Hum Brain Mapp. 2016;37:395–409. https://doi.org/10.1002/hbm.23038 .
Voldsbekk I, Groote I, Zak N, Roelfs D, Geier O, Due-Tønnessen P, Løkken L-L, Strømstad M, Blakstvedt TY, Kuiper YS, Elvsåshagen T, Westlye LT, Bjørnerud A, Maximov II. Sleep and sleep deprivation differentially alter white matter microstructure: a mixed model design utilising advanced diffusion modelling. Neuroimage. 2021;226:117540. https://doi.org/10.1016/j.neuroimage.2020.117540 .
Khalsa S, Hale JR, Goldstone A, Wilson RS, Mayhew SD, Bagary M, Bagshaw AP. Habitual sleep durations and subjective sleep quality predict white matter differences in the human brain. Neurobiol Sleep Circadian Rhythms. 2017;3:17–25. https://doi.org/10.1016/j.nbscr.2017.03.001 .
Lee M-H, Lee Y, Hwang YH, Min A, Han BS, Kim DY. Impact of sleep restriction on the structural brain network. NeuroReport. 2016;27:1299–304. https://doi.org/10.1097/WNR.0000000000000687 .
Kolanko MA, Win Z, Loreto F, Patel N, Carswell C, Gontsarova A, Perry RJ, Malhotra PA. Amyloid PET imaging in clinical practice. Pract Neurol. 2020;20:451–62. https://doi.org/10.1136/practneurol-2019-002468 .
Shokri-Kojori E, Wang G-J, Wiers CE, Demiral SB, Guo M, Kim SW, Lindgren E, Ramirez V, Zehra A, Freeman C, Miller G, Manza P, Srivastava T, De Santi S, Tomasi D, Benveniste H, Volkow ND. β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proc Natl Acad Sci U S A. 2018;115:4483–8. https://doi.org/10.1073/pnas.1721694115 .
Sharma RA, Varga AW, Bubu OM, Pirraglia E, Kam K, Parekh A, Wohlleber M, Miller MD, Andrade A, Lewis C, Tweardy S, Buj M, Yau PL, Sadda R, Mosconi L, Li Y, Butler T, Glodzik L, Fieremans E, Babb JS, Blennow K, Zetterberg H, Lu SE, Badia SG, Romero S, Rosenzweig I, Gosselin N, Jean-Louis G, Rapoport DM, de Leon MJ, Ayappa I, Osorio RS. Obstructive sleep apnea severity affects amyloid burden in cognitively normal elderly. a longitudinal study. Am J Respir Crit Care Med. 2018;197:933–43. https://doi.org/10.1164/rccm.201704-0704OC .
Boespflug EL, Iliff JJ. The emerging relationship between interstitial fluid–cerebrospinal fluid exchange, amyloid-β, and sleep. Biol Psychiat. 2018;83:328–36. https://doi.org/10.1016/j.biopsych.2017.11.031 .
Di Meco A, Joshi YB, Praticò D. Sleep deprivation impairs memory, tau metabolism, and synaptic integrity of a mouse model of Alzheimer’s disease with plaques and tangles. Neurobiol Aging. 2014;35:1813–20. https://doi.org/10.1016/j.neurobiolaging.2014.02.011 .
• Chong PLH, Garic D, Shen MD, Lundgaard I, Schwichtenberg AJ. Sleep, cerebrospinal fluid, and the glymphatic system: a systematic review. Sleep Med Rev. 2022;61:101572. https://doi.org/10.1016/j.smrv.2021.101572 . ( A comprehensive systematic review summarising the literature on the glymphatic system, especially in the context of sleep. )
Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O’Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373–7. https://doi.org/10.1126/science.1241224 .
Ward SA, Pase MP. Advances in pathophysiology and neuroimaging: implications for sleep and dementia. Respirology. 2020;25:580–92. https://doi.org/10.1111/resp.13728 .
Kang J-E, Lim MM, Bateman RJ, Lee JJ, Smyth LP, Cirrito JR, Fujiki N, Nishino S, Holtzman DM. Amyloid-beta dynamics are regulated by orexin and the sleep-wake cycle. Science. 2009;326:1005–7. https://doi.org/10.1126/science.1180962 .
Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F, Abdoli A, Abualhasan A, Abu-Gharbieh E, Akram TT, Hamad HA, Alahdab F, Alanezi FM, Alipour V, Almustanyir S, Amu H, Ansari I, Arabloo J, Ashraf T, Astell-Burt T, Ayano G, Ayuso-Mateos JL, Baig AA, Barnett A, Barrow A, Baune BT, Béjot Y, Bezabhe WMM, Bezabih YM, Bhagavathula AS, Bhaskar S, Bhattacharyya K, Bijani A, Biswas A, Bolla SR, Boloor A, Brayne C, Brenner H, Burkart K, Burns RA, Cámera LA, Cao C, Carvalho F, Castro-de-Araujo LFS, Catalá-López F, Cerin E, Chavan PP, Cherbuin N, Chu D-T, Costa VM, Couto RAS, Dadras O, Dai X, Dandona L, Dandona R, la Cruz-Góngora VD, Dhamnetiya D, da Silva DD, Diaz D, Douiri A, Edvardsson D, Ekholuenetale M, Sayed IE, El-Jaafary SI, Eskandari K, Eskandarieh S, Esmaeilnejad S, Fares J, Faro A, Farooque U, Feigin VL, Feng X, Fereshtehnejad S-M, Fernandes E, Ferrara P, Filip I, Fillit H, Fischer F, Gaidhane S, Galluzzo L, Ghashghaee A, Ghith N, Gialluisi A, Gilani SA, Glavan I-R, Gnedovskaya EV, Golechha M, Gupta R, Gupta VB, Gupta VK, Haider MR, Hall BJ, Hamidi S, Hanif A, Hankey GJ, Haque S, Hartono RK, Hasaballah AI, Hasan MT, Hassan A, Hay SI, Hayat K, Hegazy MI, Heidari G, Heidari-Soureshjani R, Herteliu C, Househ M, Hussain R, Hwang B-F, Iacoviello L, Iavicoli I, Ilesanmi OS, Ilic IM, Ilic MD, Irvani SSN, Iso H, Iwagami M, Jabbarinejad R, Jacob L, Jain V, Jayapal SK, Jayawardena R, Jha RP, Jonas JB, Joseph N, Kalani R, Kandel A, Kandel H, Karch A, Kasa AS, Kassie GM, Keshavarz P, Khan MA, Khatib MN, Khoja TAM, Khubchandani J, Kim MS, Kim YJ, Kisa A, Kisa S, Kivimäki M, Koroshetz WJ, Koyanagi A, Kumar GA, Kumar M, Lak HM, Leonardi M, Li B, Lim SS, Liu X, Liu Y, Logroscino G, Lorkowski S, Lucchetti G, Saute RL, Magnani FG, Malik AA, Massano J, Mehndiratta MM, Menezes RG, Meretoja A, Mohajer B, Ibrahim NM, Mohammad Y, Mohammed A, Mokdad AH, Mondello S, Moni MAA, Moniruzzaman M, Mossie TB, Nagel G, Naveed M, Nayak VC, Kandel SN, Nguyen TH, Oancea B, Otstavnov N, Otstavnov SS, Owolabi MO, Panda-Jonas S, Kan FP, Pasovic M, Patel UK, Pathak M, Peres MFP, Perianayagam A, Peterson CB, Phillips MR, Pinheiro M, Piradov MA, Pond CD, Potashman MH, Pottoo FH, Prada SI, Radfar A, Raggi A, Rahim F, Rahman M, Ram P, Ranasinghe P, Rawaf DL, Rawaf S, Rezaei N, Rezapour A, Robinson SR, Romoli M, Roshandel G, Sahathevan R, Sahebkar A, Sahraian MA, Sathian B, Sattin D, Sawhney M, Saylan M, Schiavolin S, Seylani A, Sha F, Shaikh MA, Shaji KS, Shannawaz M, Shetty JK, Shigematsu M, Shin JI, Shiri R, Silva DAS, Silva JP, Silva R, Singh JA, Skryabin VY, Skryabina AA, Smith AE, Soshnikov S, Spurlock EE, Stein DJ, Sun J, Tabarés-Seisdedos R, Thakur B, Timalsina B, Tovani-Palone MR, Tran BX, Tsegaye GW, Tahbaz SV, Valdez PR, Venketasubramanian N, Vlassov V, Vu GT, Vu LG, Wang Y-P, Wimo A, Winkler AS, Yadav L, Jabbari SHY, Yamagishi K, Yang L, Yano Y, Yonemoto N, Yu C, Yunusa I, Zadey S, Zastrozhin MS, Zastrozhina A, Zhang Z-J, Murray CJL, Vos T. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. The Lancet Public Health. 2022;7:e105–25. https://doi.org/10.1016/S2468-2667(21)00249-8 .
Geddes MR, O’Connell ME, Fisk JD, Gauthier S, Camicioli R, Ismail Z. Remote cognitive and behavioral assessment: report of the Alzheimer Society of Canada Task Force on dementia care best practices for COVID-19. Alzheimers Dement (Amst). 2020;12:e12111. https://doi.org/10.1002/dad2.12111 .
Henry A, Katsoulis M, Masi S, Fatemifar G, Denaxas S, Acosta D, Garfield V, Dale CE. The relationship between sleep duration, cognition and dementia: a Mendelian randomization study. Int J Epidemiol. 2019;48:849–60. https://doi.org/10.1093/ije/dyz071 .
Cullen NC, Leuzy A, Janelidze S, Palmqvist S, Svenningsson AL, Stomrud E, Dage JL, Mattsson-Carlgren N, Hansson O. Plasma biomarkers of Alzheimer’s disease improve prediction of cognitive decline in cognitively unimpaired elderly populations. Nat Commun. 2021;12:3555. https://doi.org/10.1038/s41467-021-23746-0 .
Download references
Author information
Authors and affiliations.
Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, UK
Aayushi Sen & Xin You Tai
Division of Clinical Neurology, John Radcliffe Hospital, Oxford University Hospitals Trust, Level 6 West Wing, Oxford, UK
You can also search for this author in PubMed Google Scholar
Contributions
Design, literature review, manuscript writing, critical revisions, figure preparation (AS and XYT).
Corresponding author
Correspondence to Aayushi Sen .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Sen, A., Tai, X.Y. Sleep Duration and Executive Function in Adults. Curr Neurol Neurosci Rep 23 , 801–813 (2023). https://doi.org/10.1007/s11910-023-01309-8
Download citation
Accepted : 26 September 2023
Published : 14 November 2023
Issue Date : November 2023
DOI : https://doi.org/10.1007/s11910-023-01309-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sleep duration
- Sleep quality
- Executive function
- Find a journal
- Publish with us
- Track your research

Explained: The Relationship Between Sleep And Academic Performance
Without enough sleep, we all become tall two-year-olds.” — JoJo Jensen, Dirt Farmer Wisdom
If one were to determine the three pillars of physical health- which are irrevocably linked to mental health, they would be sleep, exercise and what we eat. It would perhaps be a safe assumption that many of us tend not to take care of one or all of these pillars…even as adults.
Most parents have enough experience and information on how children who do not get enough sleep are exhausted, cranky and irritable.
How lack of sleep is affecting students
As children grow, most parents are also perturbed by the fact that a lack of sleep will interfere with their child performing well academically.
They worry that lack of sleep will affect cognitive abilities such as memory, attention, and problem-solving skills, which are crucial for academic performance. A meta-analysis by Lim J et al in 2010 found that total sleep deprivation leads to poorer short-term memory, attention, and processing speed.
Reasons for lack of sleep among students
The struggle with sleep and its discipline peaks around the ages of 2 and also in adolescence.
Melatonin is the naturally occurring hormone that is cyclically released in anticipation of darkness and is credited with preparing humans to sleep. It turns out that adolescents have a delayed release of regular daily melatonin, which causes them to become sleepy later at night, hours after nightfall.
Early school timings make 8- 10 hours of sleep quite improbable. Because most teenagers are awake, they spend time on social media and thus, device usage and its resulting brain stimulation adds to the lack of sleep.
Sleep hygiene and habits play an important role in getting adequate sleep. Sufficient sleep can improve focus, mood, and overall health, leading to better academic outcomes.
How to get a good sleep
Some strategies that can support creating a consistent sleep schedule are:
Having a fixed time of going to bed every night. Fluctuating times of going to bed interfere with the body creating its own bio-rhythm.
Avoiding heavy meals for at least 3 hours before bedtime and caffeine for 7 hours
In a research for adolescents, Crowley SJ, found that avoiding too much light in the evening hours may be a reasonable method of preventing melatonin suppression and the resulting delay in melatonin release. Yellow/ warm golden lights in rooms would work better than white light.
As a family, have a cut-off time for using devices at night. Role modelling the habits we expect from our child goes a long way in them adopting the same.
The last hour before sleep is best used for winding down activities- storytelling, colouring, calming music, warm water bath, and a warm beverage- for all ages.
If the child is older and needs a device to study at night, suggest and support them to plan the portion of the study that does not require the device at night.
Reward the efforts of the child to get a routine into place
As a parent, try not to connect the child’s sleeping habits with the device or spend time with friends. While it may indeed be a vicious cycle, the blame game leads to resentment and a lack of connection between parent and adolescent
If you cannot sleep- try not to worry about being unable to sleep because that builds a stress loop and keeps one further awake. Instead, lie with eyes closed, practice deep breathing, hear some relaxing music or a sleep meditation and invite sleep as and when it comes.
If you can’t sleep for more than half an hour, get up and do something calming and boring and try again after half an hour
For those who worry and overthink- especially middle school students and adolescents- create a thought journal to “empty” your thoughts before bedtime. Resolve the ones you can and suggest to yourself that the rest will be dealt with tomorrow. “Now it is time to sleep” is an auto-suggestion one can give oneself
As it is said, there is nothing one cannot achieve after a good night’s sleep. Building good sleep habits and prioritising sleep is one of the most important decisions we can make for ourselves. So… why not?
About the author: Nooraa Sinha is the Head of Counselling and Wellbeing Department SNS, Noida. All views/opinions expressed in the article are of the author.

UTSA to host 2024 American Athletic Conference Academic Symposium this weekend
APRIL 11, 2024 — Researchers, administrators and student-athletes from the across the American Athletic Conference’s member institutions will descend on San Antonio this weekend as UTSA hosts the conference’s 2024 Academic Symposium from Friday, April 12, to Sunday, April 14, at the Main Campus.
The symposium is the banner event for the American Athletic Conference Academic Consortium, which funds grants for research focused on student-athlete success and well-being. The Academic Symposium brings together student-athletes, scholars and athletics staff from across The American’s 15 universities to learn about the results of the consortium’s funded research and encourage collaborative efforts to enhance the student-athlete experience.
“We are proud to bring our 2024 Academic Symposium to the UTSA campus,” said Mike Aresco , commissioner of the American Athletic Conference. “Our symposium has proven to be one of our most important annual events due to the direct positive impact it has had on the student-athlete experience. The research that has been sponsored by our academic consortium has produced tangible improvements in physical, mental and social health and has also led to outstanding collaboration between faculty and students across our institutions.”
UTSA has the unique privilege of hosting the symposium while still in its first academic year as a member of the American Athletic Conference. For many of the symposium’s visitors, the event will provide them an introduction to the Alamo City and a glimpse at what the university is building — from its emergence as a Carnegie R1 research institution to its swelling impact in college athletics .
“We really embrace this opportunity,” said Lisa Campos , UTSA vice president for intercollegiate athletics. “Not only do we get to showcase UTSA, our city and all of the important research that’s going on here, but now we get to bring together all of these great people from across the American Athletic Conference institutions to share what they’ve found in their research.”

“There’s so much more we still need to learn about the student-athlete experience, and it’s important that we try to improve it every day.”
As the symposium’s host institution, UTSA will serve as a meaningful voice in the deep, wide-ranging conversations about student-athlete success and well-being throughout the weekend. Topics such as mental health, psychological readiness, heat illness and student-athlete employment will be explored through the symposium’s five research presentations and three student panels.
“There’s so much more we still need to learn about the student-athlete experience, and it’s important that we try to improve it every day,” Campos said. “We’re talking about name, image and likeness. We’re talking about sleep deprivation. We’re talking about mental health and human performance. Any research that could improve their day-to-day lives is something we all want to know more about.”
Faculty and staff from UTSA will participate in two of the symposium’s research presentations and two of the student-athlete panel discussions. The goal is for representatives from UTSA and the American’s 14 other universities to network and leverage the findings presented at the symposium to foster ongoing dialogue and collaboration between academia and athletics for years to come.
“Collaboration is really the name of the game. We’re all part of the same enterprise that brings together academics and athletics. We’re all about creating a transformative experience for our students and developing new innovations for the benefit of our community,” said Gregg Michel , associate professor in the UTSA Department of History and UTSA’s faculty athletics representative. “It will be great to see those collaborations at the symposium, to see the ways in which academic researchers are conducting programs and developing ideas that directly impact student-athletes.”
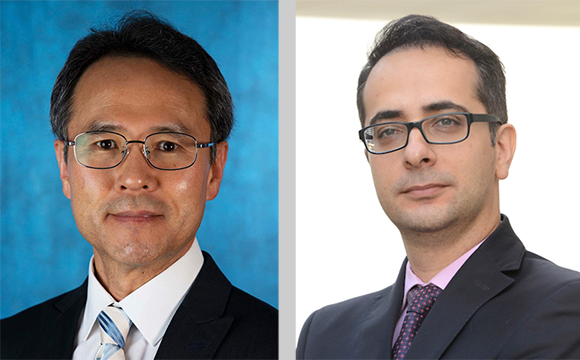
Seok Kang , professor in the UTSA Department of Communication, and Adel Alaeddini , professor in the UTSA Department of Mechanical Engineering, will be the first team to present their research at the symposium. The pair has been investigating the factors that influence the well-being, athletic and academic performance of athletes at NCAA Division I schools (including UTSA). Their study took a unique approach to data analysis called computational communication. They not only analyzed numeric data gathered through surveys, but also clustered textual data using natural language processing. This gave them the ability to draw richer analysis and provide more elaborate suggestions for theory and practices that could benefit student-athletes.
“The key takeaway is that a student-athlete’s well-being is crucial in improving their motivation, self-confidence and performance,” Kang explained.
Their research found that student-athletes are largely motivated by inspiration, role models and belongingness. These factors trigger their well-being, which helps them set goals, feel fulfilled, develop work ethics and display discipline, resilience and compassion. All of these factors have a positive impact on their academic and athletic performance. Conversely, student-athletes often grapple with depression, anxiety, stress and pressure.
Kang and Alaeddini suggest that universities develop more student-athlete well-being programs that emphasize positive attitudes toward athletics, inspiration, family, self-development and the importance of leaving a positive influence on others. Such programs would help student-athletes mitigate pressure, negative influences and overwhelming feelings. Some examples would include family day events, meetings with role-model athletes, stress-coping programs and activities that encourage conversations between coaches and athletes.
Kang added that he plans to conduct a second study on this subject and is looking forward to gleaning valuable information from the other presenters at the Academic Symposium. “All the findings by researchers will be applicable to improving student-athletes’ successful college life and life after graduation,” Kang said. “With this opportunity, student-athletes’ college life will get better, and they will be able to better prepare for their future.”

Mentorship programs have also proven beneficial for student-athletes — and that’s the subject that another Roadrunner duo will be covering in their research presentation. Kelly Cheever , assistant professor in the UTSA Department of Kinesiology, and Summer Rolin , director of sports psychology and sports medicine for UTSA and UT Health San Antonio, will share their findings about how mentorship programs can improve psychological readiness, academic performance and persistence among student-athletes.
“When I reviewed all the literature on the positive impact of mentorship on psychological readiness, I could see the potential of such a program,” Rolin said.
“I’m interested in seeing how we can help athletes help each other.” Cheever added. “There is a lot of research that suggests that individuals are more willing to listen to and talk to their peers.”
Rolin and Cheever met through their work with UTSA Athletics and bonded over a shared interest in improving the welfare of student-athletes, a population they have often watched struggle through rigorous demands. Ultimately, they hope their research can lead to creative approaches that will address the unique human condition faced by modern collegiate athletes.
“Our responsibility to our athletes is to have these meaningful conversations to address how we can develop pathways and programming to have positive outcomes and affect change. UTSA has a great opportunity to advance our mission by collaborating in this effort with our new conference peers,” Rolin said. “Our athletes give everything to their sport, and we can give back to them by acting as stewards for their well-being.”

All research presentations and student-athlete panel discussions will take place on Saturday, April 13, and Sunday, April 14, at the H-E-B Student Union Ballroom. A welcome reception will be held in the evening on Friday, April 12. The symposium will kick off with opening remarks on Saturday by UTSA President Taylor Eighmy and Interim Provost and Executive Vice President for Academic Affairs Heather Shipley . A keynote conversation will follow with special guests R.C. Buford , CEO of San Antonio Spurs Sports & Entertainment, and Frank Harris B.A. ’21, M.P.A.’23 , former UTSA quarterback and local sports legend.
Other research presentations at the symposium will include:
- Heat illness in elite athletes: Defining modifiable factors in heat stress physiology and the utility of a preseason heat illness prevention acclimatization protocol Presenter: Rebecca Lopez, University of South Florida
- Student-athlete mental health in the American Athletic Conference: Development and implementation of a standardized screening process Presenter: Trent Petrie, University of North Texas
- Exploring mental health in athletics: A post-COVID-19 review of athletic department practices and student-athlete barriers to mental health Presenter: Phillip Mullins, Wichita State University
Student panels at the symposium will include:
- Student-athlete mental health Moderator: Summer Rolin, UTSA
- Building positive team cultures Moderator: Brooke Williams, UTSA
- Student-athletes as employees Moderator: Paul Rogers, Southern Methodist University
— Shea Conner
UTSA Today is produced by University Communications and Marketing , the official news source of The University of Texas at San Antonio. Send your feedback to [email protected] . Keep up-to-date on UTSA news by visiting UTSA Today . Connect with UTSA online at Facebook , Twitter , Youtube and Instagram .
2024 American Athletic Conference Academic Symposium
UTSA hosts the 2024 American Athletic Conference Academic Symposium, a showcase for research across the conference focused on student-athlete success and well-being.
Fiesta FitFest San Antonio
Celebrate fitness with Fiesta FitFest, an official Fiesta event, from April 12-14, that includes a world-class amateur cycling event, 5K and 10K runs, free fitness classes and an athletes' village and expo.
UTSA Day of Service
UTSA Day of Service is an annual tradition where volunteers from UTSA come together give back to community partners across the San Antonio area.
2024 San Antonio Book Festival
A free, open and all-day event, the Book Festival features national, regional, local and emerging authors in presentation, signings, panel discussions and more.
UTSA Football Fiesta Spring Game
The UTSA Football Fiesta Spring Game, an official Fiesta San Antonio event, will be held at 2 p.m. on Saturday, April 13. Admission is free. Doors will open to the public at 1 p.m.
Resiliencia y Más Corazón: Las Tejanas, The Soul of Mexican American Music
This community event is hosted by the UTSA Mexican American Studies Program. It is a lecture/performance that examines the contributions of Tejana musicians to the evolution of Mexican American music.
Text Analysis Using Python
This workshop will introduce participants to the basics of text analysis using Python and Jupyter Notebook on the Constellate Lab platform. We will create datasets in Constellate to analyze patterns, trends, and relationships of contents and more.
Submit an Event

University of Texas at San Antonio receives ‘transformational’ $40M gift
Utsa’s mission.
The University of Texas at San Antonio is dedicated to the advancement of knowledge through research and discovery, teaching and learning, community engagement and public service. As an institution of access and excellence, UTSA embraces multicultural traditions and serves as a center for intellectual and creative resources as well as a catalyst for socioeconomic development and the commercialization of intellectual property - for Texas, the nation and the world.
UTSA’s Vision
To be a premier public research university, providing access to educational excellence and preparing citizen leaders for the global environment.
UTSA’s Core Values
We encourage an environment of dialogue and discovery, where integrity, excellence, inclusiveness, respect, collaboration and innovation are fostered.
UTSA’S Destinations
- UTSA will be a model for student success
- UTSA will be a great public research university
- UTSA will be an innovative place to work, learn and discover
UTSA is a proud Hispanic Serving Institution (HSI) as designated by the U.S. Department of Education .
Our Commitment to Inclusivity
The University of Texas at San Antonio, a Hispanic Serving Institution situated in a global city that has been a crossroads of peoples and cultures for centuries, values diversity and inclusion in all aspects of university life. As an institution expressly founded to advance the education of Mexican Americans and other underserved communities, our university is committed to promoting access for all. UTSA, a premier public research university, fosters academic excellence through a community of dialogue, discovery and innovation that embraces the uniqueness of each voice.
Related Links
- News Archive
- Sombrilla Magazine
- 50th Anniversary
- Social Media
- For the Media
- News, Analysis & Insights on Nutrition, Supplements, and Health
Study finds single high dose of creatine boosts cognitive performance during sleep deprivation
03-Apr-2024 - Last updated on 05-Apr-2024 at 10:34 GMT
- Email to a friend

Published in the journal Nature , the study was conducted by a team of researchers from the Institute of Neuroscience and Medicine and Aachen University Hospital in Germany who hypothesized that a combination of increased creatine availability and intracellular energy consumption would temporarily increase central creatine uptake.
"Our study showed the effect of a high dose of creatine against sleep deprivation-induced deterioration in cognitive performance, lasting up to 9 h and showing its maximum cognitive effect at 4 h after oral administration," they reported.
Creatine and sleep deprivation
The study noted that the modern lifestyle is often propped up by psychoactive substances like caffeine and accompanied by sleep deprivation, a state which lends itself to negative outcomes ranging from reduced performance to chronic disease.
While creatine supplementation has been extensively studied for its ergogenic benefits in sports nutrition (with the muscle loaded over time), research has also revealed its potential cognitive benefits, as well as changes in creatine-related metabolites linked to sleep disorders and states of sleep deprivation.
"The inverse effects of creatine supplementation and sleep deprivation on high energy phosphates, neural creatine and cognitive performances suggest that creatine is a suitable candidate for reducing the negative effects of sleep deprivation," the researchers wrote.
Commenting independently on the current study, Dr. Ralf Jäger, FISSN, CISSN, MBA, managing member of global consulting firm Increnovo, explained that creatine seems to be most effective during times of stress—either as a result of sleep deprivation, hypoxia, more demanding cognitive tasks or in people with low creatine levels like vegetarians.
"This new study showed that even an acute supplementation with creatine can be effective to enhance mental performance, which is an exciting new finding, and in contrast to what is needed for physical performance," he said.
Study details
For this double-blind, randomized, prospective crossover trial, 15 participants between the ages of 20 and 28 (8 female) performed cognitive tests during sleep deprivation after consuming either a high single dose (0.35 g/kg) of creatine monohydrate (Alzchem) or a corn starch placebo. After a minimum interval of five days, they switched test groups.
Evaluations included two consecutive 31 P-magnetic resonance spectroscopy (MRS) scans and 1 H-magnetic resonance spectroscopy (MRS) used to quantify biochemical compounds or metabolites in the brain tissue, along with a collection of cognitive tests performed at evening baseline and at 3 hours, 5.5 hours, and 7.5 hours after supplementation.
Findings indicated that sleep deprivation led to a profound cognitive and metabolic response and that acute creatine was bio-available to the brain as suggested by increased total creatine (tCR)/total N-acetylaspartate (tNAA) and reduced subjective fatigue compared to placebo.
"Creatine alleviated changes in phosphates, pH levels and fading of cognitive performance evoked by sleep deprivation," the researchers reported. "Creatine induced increases in PCr/Pi, declines in ATP and improvements in cognitive performance and processing speed exceeding wake baseline."
They suggested that the crucial factor to overcoming marginal intracellular creatine uptake was, as hypothesized, the increased energy demand of the neuronal cells in combination with an increased extracellular creatine availability.
"It can be concluded that creatine has the potential to be used in prolonged cognitive activity during sleep deprivation," the study noted, calling for future research to investigate appropriate dosage and to specify the time point at which creatine reaches peak effect.
Source: Nature doi: 10.1038/s41598-024-54249-9 “Single dose creatine improves cognitive performance and induces changes in cerebral high energy phosphates during sleep deprivation” Authors: Ali Gordji‐Nejad et al.
Related news

Related products

Lactium® is a natural and effective solution to help your pet cope with stress-related symptoms
Content provided by Ingredia SA | 04-Apr-2024 | Application Note
600 caracLactium® is a milk protein hydrolysate that contains a bioactive decapeptide with calming properties, a-casozepine.

Formulate for women’s health – formulate empowerment
Content provided by Verdure Sciences | 26-Mar-2024 | Product Brochure
Women’s health trends are mirroring bigger conversations of empowerment and wellbeing. Within the women’s health category, upticks in areas of lean muscle...

Go Beyond the Ordinary: Cognitive Health-BacoMind
Content provided by Natural Remedies Private Limited | 27-Feb-2024 | White Paper
Experience the potency of BacoMind®, the #1 branded bacopa with 9 key bioactives for unparalleled cognitive support.
Nootropics Report 2.0: Brain Health Insights
Content provided by dsm-firmenich | 22-Feb-2024 | Insight Guide
The brain health market is constantly growing and evolving, with more consumers looking for innovative ways to support total mind and body wellness.
Related suppliers
- IGY Life Sciences
- Ingredia SA
- Natural Remedies Private Limited
- Lactium® is a natural and effective solution to help your pet cope with stress-related symptoms Ingredia SA | Download Application Note
- Reality and Fantasy: Dietary Supplement Formulations Gemini Pharmaceuticals, Inc | Download Technical / White Paper
- Support children’s eyes & brains with Lutemax Kids OmniActive Health Technologies | Download Product Brochure
- Formulate for women’s health – formulate empowerment Verdure Sciences | Download Product Brochure
- Pycnogenol® for Sport: eNOS and Beyond Horphag Research | Download Technical / White Paper
Upcoming editorial webinars
- 25 Apr 2024 Thu Webinar The botanical supply chain
On-demand webinars
- Mitigating safety: Challenges in pet food manufacturing Webinar
- Premium categories: Does the humanization trend still have legs? Webinar
- Sustainable sourcing: Limiting pet industry impact on ecosystems Webinar
- Mining the microbiome: Balance is everything Webinar
- Shifting the paradigm with psychobiotics for sleep Novozymes OneHealth
- Spotlight On - Opportunities & insights in a dynamic gummy market Spotlight On

Promotional Features

NutraIngredients-USA
- Advertise with us
- Apply to reuse our content
- Press Releases – Guidelines
- Contact the Editor
- Report a technical problem
- Subscription Benefits
- Why Register
- Whitelist our newsletters
- Editorial Calendar
- Event Calendar

IMAGES
VIDEO
COMMENTS
Sleep is an inseparable part of human health and life, which is crucial in learning, practice, as well as physical and mental health. It affects the capacity of individual learning, academic performance, and neural-behavioral functions. This study aimed to determine the relationship between sleep quality and students' academic achievement ...
In adolescents aged 14-18 years, not only did sleep quality affect academic performance (Adelantado-Renau, Jiménez-Pavón, et al., 2019) but one night of total sleep deprivation negatively ...
While this study reveals that sleep deprivation may affect academic performance, the study obtains 95% confidence that respondents show a mean between 6.85 hours and 7.40 hours 6. This indicates ...
Sleep disturbances are associated with academic performance (Galván, 2020; Vedaa et al., 2019), and 77 (15%) of the studies in the evidence map focused on academic or cognitive performance. However, only 10% of these studies were intervention studies, indicating that we lack appropriate sleep health interventions to enhance academic performance.
New novel sleep measures have emerged. Sleep consistency measures how likely a student is to be awake or asleep at the same time each day. Students with greater sleep consistency have better academic performance. A morning circadian preference and earlier classes are associated with higher grades.
Generally, sleep is associated with academic performance in school. Sleep deficit has been associated with lack of concentration and attention during class. 19 While a few studies report null ...
The beginning of the university brings together maturational, psychosocial and academic changes that make university students more prone to suffer from insufficient or poor quality sleep, which can negatively influence their academic performance. The period of taking exams is a key part of the academic year. However, there are few studies that analyze sleep during this period of time. Our aim ...
The complex interaction of stress, sleep and academic performance also highlights the importance of resilience to externally imposed stressors and factors as well as flexibility. Flexibility is a key aspect for the entrainment of biological (circadian) rhythms with external activities schedule. Such a flexibility will facilitate that ...
We examined the relationship between sleep and the affective components of subjective well-being as well as psychological well-being, and between sleep and academic performance, of full-time undergraduate students in a residential college at the National University of Singapore. The aspects of sleep considered were self-reported sleep duration ...
To quantitatively describe the effects of sleep loss, we used meta-analysis, a technique relatively new to the sleep research field, to mathematically summarize data from 19 original research studies. Results of our analysis of 143 study coefficients and a total sample size of 1,932 suggest that overall sleep deprivation strongly impairs human ...
Background Sleep disorders are composed of a group of diseases of increasing prevalence and with social-health implications to be considered a public health problem. Sleep habits and specific sleep behaviors have an influence on the academic success of students. However, the characteristics of sleep and sleep habits of university students as predictors of poor academic performance have been ...
Strong evidence shows that sleep deprivation can affect a student's ability to learn and academic performance. While delayed sleep-wake phase disorder was prevalent among young adults, available ...
Students with high sleep-related impairment scores and longer sleep duration had better academic performance than those with low sleep-related impairment scores or shorter sleep duration. A simple linear regression was undertaken to predict participants' academic ranking based on their sleep-related impairment scores ( F (1, 97) = 6.36, p < 0. ...
to ensure optimal patient care. Sleep deprivation can result in greater procedural errors, which places the clients at risk. Insufficient sleep negatively affects the nervous system, resulting in poor brain function. Because of the cognitive decline that is associated with sleep deprivation, academic performance is often decreased.
Abstract: This study determined the effects of sleep deprivation on the academic performance of 2nd-year education students. of the University of Science and Technology of Southern Philippines ...
controlled sleep deprivation studies have shown that lack of sleep ... short-term benefits of sleep on academic performance in college. ... and McGovern Institute for Brain Research ...
Irregular sleep and late bedtimes are linked to worse grades and more school-related behavioral problems among teens, suggests a study funded by the National Institutes of Health (NIH). The authors stated that interventions to promote regular sleep schedules may boost adolescents' academic performance.
While adults (including teachers and principals ) can also suffer from irregular sleep, high schoolers are particularly vulnerable, Mathew said, because sleep cycles naturally change during ...
Research has indicated that sleep deprivation can lead to metabolic disorders and negative effects, such as increased metabolite levels, which can lead to poor memory, poor concentration, lower academic performance, and emotional fluctuations (Durmer and Dinges, 2005; ...
Sleep deprivation is common, with 11.8% of respondents reporting less than 5 h sleep on average in a large US survey [].Deficits in motor performance due to sleep deprivation are equivalent to blood alcohol content of 0.05-0.1%, which is comparable to the legal driving limit of 0.08% [] in England and the USA.A single night of sleep deprivation has been shown to affect several components of ...
They worry that lack of sleep will affect cognitive abilities such as memory, attention, and problem-solving skills, which are crucial for academic performance. A meta-analysis by Lim J et al in ...
The current study findings showed a significant association between poor sleep quality and unfavourable academic performance; this was similar to the finding of Rose S et al. [17] who also ...
Now, researchers at Monash University in Australia endeavoring to develop a blood test for sleep deprivation have detected certain elements in blood that may help identify when someone has been awake for more than 24 hours. To develop the test, the researchers enrolled 23 young and healthy participants with no known sleep disorders.
We're talking about sleep deprivation. We're talking about mental health and human performance. Any research that could improve their day-to-day lives is something we all want to know more about." Faculty and staff from UTSA will participate in two of the symposium's research presentations and two of the student-athlete panel discussions.
For this double-blind, randomized, prospective crossover trial, 15 participants between the ages of 20 and 28 (8 female) performed cognitive tests during sleep deprivation after consuming either a ...